Order cyklokapron visa
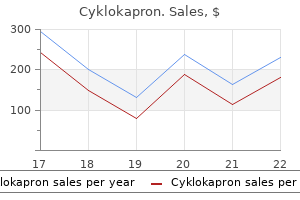
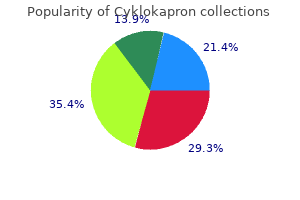
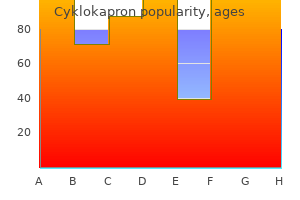
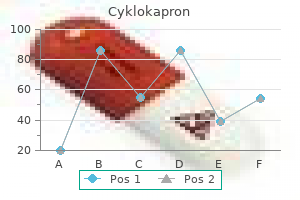
Puerperal sterilization procedures follow cesarean or vaginal delivery and approximately 7 percent of all live births in the United States (Moniz treatment nausea order cyklokapron on line, 2017). Nonpuerperal tubal sterilization is done at a time unrelated to recent pregnancy and is also termed interval sterilization. Moreover, abdominal laxity allows easy repositioning of the incision over each uterine cornu. On our service, puerperal tubal ligation is performed by a surgical team dedicated to this role the morning after delivery. This timing minimizes hospital stay but lowers the likelihood that postpartum hemorrhage would complicate recovery following surgery. In contrast, some prefer to perform sterilization immediately following delivery and use neuraxial analgesia already placed for labor. In this model, barriers to sterilization can be lessened by designating these postpartum surgeries as urgent, especially in high-volume labor and delivery units, which usually prioritize limited operating-room availability for intrapartum procedures (American College of Obstetricians and Gynecologists, 2016; Potter, 2013). In general, a midtubal segment of fallopian tube is excised, and the severed ends seal by fibrosis and peritoneal regrowth. Commonly used methods of puerperal sterilization include the Parkland, Pomeroy, and modified Pomeroy techniques (American College of Obstetricians and Gynecologists, 2017a). Irving and Uchida techniques or Kroener fimbriectomy are rarely used because of their increased required dissection or unfavorably high failure rates. Also, in the absence of uterine or other pelvic disease, hysterectomy solely for sterilization at the time of cesarean delivery, early in the puerperium, or even remote from pregnancy is difficult to justify. It carries significantly increased surgical morbidity compared with tubal sterilization. Evidence suggests that the fallopian tube may be the origin of pelvic serous carcinomas, especially those of the ovary. With this knowledge, the Society of Gynecologic Oncologists (2013) and American College of Obstetricians and Gynecologists (2017b) recommend consideration of salpingectomy to lower cancer risks. Specifically, for women at average risk of ovarian cancer, risk-reducing salpingectomy should be discussed and considered with patients at the time of abdominal or pelvic surgery, at hysterectomy, or in lieu of tubal ligation. Spinal analgesia is typically selected for cases scheduled for the first postpartum day. If done more proximate to delivery, the same epidural catheter used for labor analgesia can be used for sterilization analgesia. General anesthesia may be less desirable due to residual pregnancy-related airway vulnerabilities (Bucklin, 2003). Second, the umbilicus usually remains the thinnest portion of the anterior abdominal wall and requires less subcutaneous dissection to reach the linea alba fascia. Third, an infraumbilical incision offers fascia with sufficient integrity to provide a closure that has minimal risk for later incisional hernia. Last, incisions that follow the natural curve of the lower umbilical skin fold yield suitable cosmesis. A 2- to 4-cm transverse or vertical skin incision is usually sufficient for normal-weight women. For obese women, a 4- to 6-cm incision may be needed for adequate abdominal access. Beneath this incision, the subcutaneous tissue is bluntly separated to reach the linea alba fascia. For this, an Allis clamp can be opened and closed as downward pressure is exerted. Similarly, the blades of two army-navy retractors both pulling in downward yet opposite directions can part the subcutaneous layer. Clearing this fatty tissue away from the fascia isolates the fascia for incision and for later closure without intervening fat, which may impede wound healing. The fascial incision may be transverse or vertical and follows the same orientation of the skin incision. For this, once the linea alba is reached, it is grasped with two Allis clamps-one placed on either side of the planned fascial incision. The purchase of tissue with each clamp should be substantial and creates a small roll of fascia to be incised. Notably, if the initial fascial incision is too small, it can be extended with curved Mayo scissors. Adequate exposure is critical, and army-navy or appendiceal retractors are suitable. For obese women, a slightly larger incision and narrow deeper retractors may be required. If bowel or omentum is obstructing, Trendelenburg position can help displace these cephalad. Digitally packing with a single, moist, fanned-out piece of surgical gauze can also be used, but a hemostat should always be attached to the distal end to avert its retention. At times, tilting the entire table to the opposite side of the tube being exposed assists tube isolation. The fallopian tube is identified and grasped at its midportion with a Babcock clamp, and the distal fimbria confirmed. A common reason for sterilization failure is ligation of the wrong structure, typically the round ligament. Therefore, identification and isolation of the distal tube prior to ligation is necessary. Whenever the tube is inadvertently dropped, it is mandatory to repeat this identification process. An avascular site in the mesosalpinx adjacent to the fallopian tube is perforated with a small hemostat. The jaws are opened to separate the fallopian tube from the adjacent mesosalpinx for approximately 2. The intervening segment of approximately 2 cm is excised, and the excision site is inspected for hemostasis. This method was designed to avoid the initial intimate proximity of the cut ends of the fallopian tube inherent with the Pomeroy procedure. During ligation of a midsegment tubal loop, plain catgut is used to ensure prompt absorption of the ligature and subsequent separation of the severed tubal ends. The umbilical incision generally will need to be larger to allow an adequate view of the tube and mesosalpinx and to place clamps. With total salpingectomy, the entire mesosalpinx must be divided to free the fallopian tube. At the cornu, clamps are placed across the fallopian tube and its adjacent mesosalpinx prior to tubal transection. With salpingectomy and cesarean delivery, total blood loss rates were not statistically higher (Powell, 2017; Shinar, 2017). Most women have an uncomplicated course and are discharged on the first postoperative day. A detailed description and illustration of these can be found in Williams Gynecology, 3rd edition (Thompson, 2016). In the United States, a laparoscopic approach to interval tubal sterilization is the most common. The procedure is frequently performed in an ambulatory surgical setting under general anesthesia. Minilaparotomy using a 3-cm suprapubic incision is also popular, especially in resource-poor countries. Although not often used, the peritoneal cavity can be entered through the posterior vaginal fornix via colpotomy to perform tubal interruption. First, surgical errors occur and include transection of the round ligament or only partial transection of the tube. Second, a fistulous tract or spontaneous reanastomosis may form between the severed tubal stumps. Approximately 30 percent of pregnancies that follow a failed tubal sterilization procedure are ectopic. This rate is 20 percent for those following a postpartum procedure (Peterson, 1996, 1997). Thus, any symptoms of pregnancy in a woman after tubal sterilization must be investigated, and an ectopic pregnancy excluded. Other Effects Overall, risks for ovarian cancer decline and for breast cancer are unaffected following sterilization (Gaudet, 2013; Pearce, 2015). Women who have undergone tubal sterilization are highly unlikely to subsequently have salpingitis (Levgur, 2000).
Cheap cyklokapron amex
The great decline in uterine cavity surface area simultaneously throws the fetal membranes-the amniochorion and the parietal decidua-into innumerable folds schedule 9 medications best cyklokapron 500 mg. These are then peeled off the uterine wall, partly by further contraction of the myometrium and partly by traction that is exerted by the separated placenta as it descends during expulsion. Completion of the third stage is also accomplished by alternately compressing and elevating the fundus, while exerting minimal traction on the umbilical cord. The retroplacental hematoma either follows the placenta or is found within the inverted sac formed by the membranes. In this process, known as the Schultze mechanism of placental expulsion, blood from the placental site pours into the membrane sac and does not escape externally until after extrusion of the placenta. In the other form of placental extrusion, known as the Duncan mechanism, the placenta separates first at the periphery and blood collects between the membranes and the uterine wall and escapes from the vagina. In this circumstance, the placenta descends sideways, and its maternal surface appears first. This increase coincides with a greater uterine contractile responsiveness to oxytocin. Prolonged gestation is associated with a delay in the rise of these receptor levels (Fuchs, 1984). Oxytocin-literally, quick birth-was the first uterotonin to be implicated in parturition initiation. This nanopeptide is synthesized in the magnocellular neurons of the supraoptic and paraventricular neurons. The prohormone is transported with its carrier protein, neurophysin, along the axons to the neural lobe of the posterior pituitary gland in membrane-bound vesicles for storage and later release. The prohormone is converted enzymatically to oxytocin during transport (Gainer, 1988; Leake, 1990). In addition to its effectiveness in pharmacologically inducing labor at term, oxytocin is a potent uterotonin and occurs naturally in humans. Subsequent observations provide additional support for this theory: (1) the number of oxytocin receptors strikingly rises in myometrial and decidual tissues near the end of gestation; (2) oxytocin acts on decidual tissue to promote prostaglandin release; and (3) oxytocin is synthesized directly in decidual and extraembryonic fetal tissues and in the placenta (Chibbar, 1993; Zingg, 1995). Although little evidence suggests a role for oxytocin in phase 2 of parturition, abundant data support its important role during second-stage labor and in the puerperium-phase 4 of parturition. Specifically, maternal serum oxytocin levels are elevated: (1) during second-stage labor, which is the end of phase 3 of parturition; (2) in the early puerperium; and (3) during breastfeeding (Nissen, 1995). Immediately after delivery of the fetus, placenta, and membranes, which completes parturition phase 3, firm and persistent uterine contractions are essential to prevent postpartum hemorrhage. Prostaglandins Although their role in phase 2 of parturition in uncomplicated pregnancies is less well defined, a critical role for prostaglandins in phase 3 of parturition is clear (MacDonald, 1993). First, levels of prostaglandins-or their metabolites-in amnionic fluid, maternal plasma, and maternal urine are increased during labor. Third, treatment of pregnant women with prostaglandins, by any of several administration routes, causes abortion or labor at all gestational ages. Last, prostaglandin treatment of myometrial tissue in vitro sometimes causes contraction, dependent on the prostanoid tested and the physiological status of the tissue treated. During labor, prostaglandin production within the myometrium and decidua is an efficient mechanism of activating contractions. For example, prostaglandin synthesis is high and unchanging in the decidua during phase 2 and 3 of parturition. Their greatest elevation in concentration within amnionic fluid, however, is demonstrable after labor begins. These higher levels likely result as the cervix dilates and exposes decidual tissue. These higher levels in the forebag, compared with those in the upper compartment, are believed to follow an inflammatory response that signals the events leading to active labor. Together, the rise in cytokine and prostaglandin concentrations further degrade the extracellular matrix, thus weakening fetal membranes. The endothelin A receptor is preferentially expressed in smooth muscle, and when activated, it effects a rise in intracellular calcium. Endothelin-1 is produced in myometrium of term gestations and is able to induce synthesis of other contractile mediators such as prostaglandins and inflammatory mediators (Momohara, 2004; Sutcliffe, 2009). The requirement of endothelin-1 in normal parturition physiology remains to be established. This directly compresses large uterine vessels and allows thrombosis of their lumens to prevent hemorrhage. This is typically augmented by endogenous and pharmacological uterotonic agents (Chap. Uterine involution and cervical repair are prompt remodeling processes that restore these organs to the nonpregnant state. These protect the reproductive tract from invasion by commensal microorganisms and restore endometrial responsiveness to normal hormonal cyclicity. During the early puerperium, lactogenesis and milk let-down begin in mammary glands (Chap. However, it is dependent on the duration of breastfeeding and lactation-induced, prolactin-mediated anovulation and amenorrhea. Mol Hum Reprod 11(4):279, 2005 Badir S, Bajka M, Mazza E: A novel procedure for the mechanical characterization of the uterine cervix during pregnancy. J Mech Behav Biomed Mater 27:143, 2013 Benedetto C, Petraglia F, Marozio L, et al: Corticotropin-releasing hormone increases prostaglandin F2 alpha activity on human myometrium in vitro. Am J Obstet Gynecol 171(1):126, 1994 Berkane N, Verstraete L, Uzan S, et al: Use of mifepristone to ripen the cervix and induce labor in term pregnancies. Biol Reprod 67(1):184, 2002 Bollapragada S, Youssef R, Jordan F, et al: Term labor is associated with a core inflammatory response in human fetal membranes, myometrium, and cervix. J Clin Invest 91(1):185, 1993 Chwalisz K: the use of progesterone antagonists for cervical ripening and as an adjunct to labour and delivery. Am J Pathol 170:578, 2007 Erlebacher A: Mechanisms of T cell tolerance towards the allogeneic fetus. New York, Raven, 1988 Garcia-Verdugo I, Tanfin Z, Dallot E, et al: Surfactant protein A signaling pathways in human uterine smooth muscle cells. Deutsche Medizinische Wochenschrift 21:565, 1895 Hermanns-Le T, Pierard G, Quatresooz P: Ehlers-Danlos-like dermal abnormalities in women with recurrent preterm premature rupture of fetal membranes. Eur J Obstet Gynecol Reprod Biol 144 Suppl 1:S65, 2009 Jeyasuria P, Wetzel J, Bradley M, et al: Progesterone-regulated caspase 3 action in the mouse may play a role in uterine quiescence during pregnancy through fragmentation of uterine myocyte contractile proteins. Endocrinology 155(2):605, 2014 Kimura T, Takemura M, Nomura S, et al: Expression of oxytocin receptor in human pregnant myometrium. J Immunol 184(11):6479, 2010 Leonhardt A, Glaser A, Wegmann M, et al: Expression of prostanoid receptors in human lower segment pregnant myometrium. J Clin Endocrinol Metab 76(5):1332, 1993 Mahendroo M: Cervical remodeling in term and preterm birth: insights from an animal model. Mol Endocrinol 13(6):981, 1999 Malpas P: Postmaturity and malformations of the foetus. Am J Obstet Gynecol 186(2):257, 2002 McLean M, Bisits A, Davies J, et al: A placental clock controlling the length of human pregnancy. Nat Med 1(5): 460, 1995 Meera P, Anwer K, Monga M, et al: Relaxin stimulates myometrial calcium-activated potassium channel activity via protein kinase A. J Clin Endocrinol Metab 87(6):2924, 2002 Momohara Y, Sakamoto S, Obayashi S, et al: Roles of endogenous nitric oxide synthase inhibitors and endothelin-1 for regulating myometrial contractions during gestation in the rat. Acta Biomater 4(1):104, 2008 Nadeem L, Shynlova O, Matysiak-Zablocki E, et al: Molecular evidence of functional progesterone withdrawal in human myometrium. Rev Endocr Metab Disord 6(4):291, 2005 Parra-Saavedra M, Gomez L, Barrero A, et al: Prediction of preterm birth using the cervical consistency index. Ultrasound Obstet Gynecol 38(1):44, 2011 Patel B, Elguero S, Thakore S, et al: Role of nuclear progesterone receptor isoforms in uterine pathophysiology.
Order 500 mg cyklokapron with amex
The cause is usually maternal Graves disease with transplacental passage of IgG thyroid-stimulating immunoglobulins medications you can give your cat buy 500 mg cyklokapron fast delivery. Fetal blood sampling may confirm the diagnosis (Duncombe, 2001; Heckel, 1997; Srisupundit, 2008). During this, if the mother develops hypothyroidism, she is given supplemental levothyroxine (Hui, 2011). Fetal Hypothyroidism In a woman receiving medication for Graves disease, transplacental passage of methimazole or propylthiouracil may cause fetal hypothyroidism (Bliddal, 2011a). Other potential causes of fetal hypothyroidism resulting in goiter include transplacental passage of thyroid peroxidase antibodies, fetal thyroid dyshormonogenesis, and maternal overconsumption of iodine supplements (Agrawal, 2002; Overcash, 2016). Goitrous hypothyroidism may lead to hydramnios, neck hyperextension, and delayed bone maturation. If the mother is receiving antithyroid medication, discontinuation is generally recommended, along with intraamnionic levothyroxine injection. However, optimal dosage and frequency have not been established, and reported dosages range from 50 to 800 g every 1 to 4 weeks (Abuhamad, 1995; Bliddal, 2011b; Ribault, 2009). Open fetal surgery is a highly specialized intervention performed at relatively few centers in the United States and for only a few fetal conditions. In many cases, data regarding the safety and efficacy of these procedures are limited. The Agency for Healthcare Research and Quality stresses that when considering fetal surgery, the overriding concern must be maternal and fetal safety. Guiding Principles for Fetal Surgical Procedures Accurate prenatal diagnosis for the defect is available, with staging if applicable the defect appears isolated, with no evidence of other abnormality or underlying genetic syndrome that would significantly worsen survival or quality of life the defect results in a high likelihood of death or irreversible organ destruction, and postnatal therapy is inadequate the procedure is technically feasible, and a multidisciplinary team is in agreement regarding the treatment plan Maternal risks from the procedure are well documented and considered acceptable There is comprehensive parental counseling It is recommended that there be an animal model for the defect and procedure Data from Deprest, 2010; Harrison, 1982; Vrecenak, 2013; Walsh, 2011. Some abnormalities amenable to fetal surgical treatment, antepartum or intrapartum, are shown in Table 16-2. An overview of these procedures, their indications, and complications is provided here to assist with initial patient evaluation and counseling. The mother must undergo general endotracheal anesthesia to suppress both uterine contractions and fetal responses. Using intraoperative sonographic guidance to avoid the placental edge, a low-transverse hysterotomy incision is made with a stapling device that seals the edges for hemostasis. To replace amnionic fluid losses, warmed fluid is continuously infused into the uterus thorough a rapid infusion device. The fetus is gently manipulated to permit pulse oximetry monitoring and to establish venous access, in case fluids or blood are emergently needed. Tocolysis typically includes intravenous magnesium sulfate for 24 hours, oral indomethacin for 48 hours, and, at some centers, oral nifedipine until delivery (Wu, 2009). Prophylactic antibiotics are also administered and generally continued for 24 hours following the procedure. In a review of 87 open procedures, Golombeck and coworkers (2006) reported the following morbidities: pulmonary edema-28 percent, placental abruption-9 percent, blood transfusion-13 percent, premature rupture of membranes-52 percent, and preterm delivery-33 percent. Wilson and associates (2010) reviewed subsequent pregnancy outcomes following open fetal surgery and reported that 14 percent of women experienced uterine rupture and 14 percent had uterine dehiscence. Other potential risks include maternal sepsis and fetal death during or following the procedure, particularly if hydrops is present. Damage is postulated to result from abnormal embryonic neurulation and from ongoing exposure of neural elements to amnionic fluid (Adzick, 2010; Meuli, 1995, 1997). Fetal myelomeningocele meets the criteria listed in Table 16-1 and is the first nonlethal birth defect for which fetal surgery has been offered. With the edges of both the laparotomy and hysterotomy incisions retracted, the skin around the defect is incised. Subsequently, the neural placode is sharply dissected from the arachnoid membrane. The dural membrane is reflected to the midline to cover the neural placode and is reapproximated using suture. Women at risk for preterm birth or placental abruption, those with a contraindication to fetal surgery, and women with body mass index >35 kg/m2 were excluded. Children who had undergone prenatal surgery were twice as likely to walk independently by 30 months. They had significantly less hindbrain herniation and were only half as likely to undergo ventriculoperitoneal shunting by the age of 1 year. A primary outcome was a composite score that was derived from the Bayley Mental Development Index and from the difference between the functional and anatomical level of the lesion at 30 months. For example, despite improvements in the proportion with independent ambulation, most children who received fetal surgery were not able to ambulate independently, and nearly 30 percent were not able to ambulate at all. Prenatal surgery did not confer improvements in fetal or neonatal death rates or in the Bayley Mental Development Index score at age 30 months. And, as shown in Table 16-3, surgery was associated with a small but significant risk for placental abruption and maternal pulmonary edema. Moreover, nearly half were delivered before 34 weeks, which significantly increased the risk for respiratory distress syndrome (Adzick, 2011). At a median follow-up of 10 years, these children have higher rates of behavioral problems and adverse executive functioning compared with population norms (Danzer, 2016). Thoracic Masses In the past, if hydrops developed in a fetus with a large pulmonary sequestration or cystic adenomatoid malformation without a dominant cyst, open fetal surgery with lobectomy was the only treatment available other than preterm delivery. Most thoracic masses are small and have a benign prognosis, and larger masses are generally treated with corticosteroids (p. Fetal surgery is generally reserved for cases prior to 32 weeks in which hydrops is developing, and in selected cases, the survival rate following open lobectomy approximates 60 percent (Vrecenak, 2013). Use of the ex-utero intrapartum treatment procedure in the treatment of fetal lung masses at delivery is discussed later on page 327. Sacrococcygeal Teratoma this germ cell tumor has a prevalence of approximately 1 per 28,000 births (Derikx, 2006; Swamy, 2008). Hydramnios is common, and hydrops may develop from high-output cardiac failure, either as a consequence of tumor vascularity or secondary to bleeding within the tumor and resultant anemia. Mirror syndrome-maternal preeclampsia developing along with fetal hydrops-may occur in this setting (Chap. Following laparotomy and hysterotomy, the caudal portion of the fetus has been delivered onto the surgical field. Fetal loss rates approach 100 percent if hydrops or placentomegaly develop (Vrecenak, 2013). Because tumor debulking interrupts the pathological vascular steal, normal fetal physiology may be restored. Fetoscopic Surgery As with open fetal surgeries, these procedures are performed at highly specialized centers, and some are considered investigational. To accomplish them, fiberoptic endoscopes only 1 to 2 mm in diameter are used to penetrate the maternal abdominal wall, the uterine wall, and membranes. Instruments such as lasers fit through 3- to 5-mm cannulas that surround the endoscope. Morbidities are generally lower than with open fetal surgery, but they still may be formidable, particularly if maternal laparotomy is required for access (Golombeck, 2006). For the procedure, a fetoscope is used to view the vascular equator that separates the placental cotyledons supplying each twin. At the end, amnioreduction is performed to decrease the single deepest pocket of amnionic fluid to below 5 cm, and antibiotics are injected into the amnionic cavity. The fetoscope is inserted into the recipient-twin sac and positioned over the vascular equator, which lies in between the two placental cord insertion sites. Arteriovenous anastomoses along the placental surface are individually photocoagulated using the laser. The latter is a feto-fetal transfusion characterized by large differences in hemoglobin concentrations between a pair of monochorionic twins. With this, after selective photocoagulation, the laser is used to coagulate the entire vascular equator, from one edge of the placenta to the other (Slaghekke, 2014a). Also, placental dye-injection studies confirm a significant reduction in the number of residual anastomoses (Ruano, 2013; Slaghekke, 2014b). Families should have reasonable expectations of procedural success and potential complications. Following laser therapy, the anticipated perinatal mortality rate approximates 30 to 50 percent, with a 5- to 20-percent risk for long-term neurological handicap (Society for Maternal-Fetal Medicine, 2013). Associated anomalies occur in 40 percent of cases and confer a considerably lower survival rate.
Order cyklokapron 500 mg amex
Pillai and James (1990) reported increased baseline variability with advancing gestation medicine venlafaxine cyklokapron 500 mg with mastercard. Up to 30 weeks, baseline characteristics were similar during both fetal rest and activity. After 30 weeks, fetal inactivity was associated with diminished baseline variability, but fetal activity enhanced it. Last, the baseline fetal heart rate becomes more physiologically fixed (less variable) as the rate rises. This phenomenon presumably reflects less cardiovascular physiological wandering as beat-to-beat intervals shorten with a higher heart rate. A common cause of diminished beat-to-beat variability is administration of analgesic drugs during labor (Chap. Various central nervous system depressant drugs can cause transient diminished beat-to-beat variability. Included are narcotics, barbiturates, phenothiazines, tranquilizers, and general anesthetics. As one specific example, variability regularly diminishes within 5 to 10 minutes following intravenous meperidine administration, and the effects may last up to 60 minutes or longer (Hill, 2003; Petrie, 1993). And, chronically administered buprenorphine suppresses fetal heart rate and movement (Jansson, 2017). Magnesium sulfate, widely used in the United States for tocolysis or management of hypertensive gravidas, is associated with diminished beat-to-beat variability. In a study of nearly 250 term gestations, magnesium sulfate administration led to decreased variability but without evidence of adverse neonatal effects (Duffy, 2012). With magnesium sulfate tocolysis of preterm labor, variability was also diminished in most reviewed studies (Nensi, 2014; Verdurmen, 2017). Of greatest concern, diminished beat-to-beat variability can be an ominous sign indicating a seriously compromised fetus. Paul and coworkers (1975) reported that loss of variability in combination with decelerations was associated with fetal acidemia. Severe maternal acidemia can also lower fetal beat-to-beat variability, for example, in a mother with diabetic ketoacidosis. According to Dawes (1985), metabolic acidemia that causes depression of the fetal brainstem or the heart itself creates the loss of variability. Thus, diminished beat-to-beat variability, when it reflects fetal compromise, likely reflects acidemia rather than hypoxia. Indeed, mild degrees of fetal hypoxemia have been reported actually to enhance variability, at least initially (Murotsuki, 1997). Reduced baseline heart rate variability is the single most reliable sign of fetal compromise. Smith and coworkers (1988) performed a computerized analysis of beat-to-beat variability in growth-restricted fetuses before labor. In contrast, Samueloff and associates (1994) evaluated variability in 2200 consecutive deliveries and concluded that variability by itself could not be used as the only indicator of fetal well-being. They also warned that good variability should not be interpreted as necessarily reassuring. Blackwell and associates (2011) found that even experts often disagreed as to whether variability was absent or minimal (5 bpm). In sum, beat-to-beat variability is affected by fetal physiology, and its meaning differs depending on the clinical setting. Decreased variability in the absence of decelerations is unlikely to reflect fetal hypoxia (Davidson, 1992). A persistently flat fetal heart rate baseline-absent variability-within the normal baseline rate range and without decelerations may reflect a previous fetal insult that has resulted in neurological damage (Freeman, 2003). Cardiac Arrhythmia When fetal cardiac arrhythmias are first suspected using electronic monitoring, findings can include baseline bradycardia, tachycardia, or most commonly in our experience, abrupt baseline spiking. An arrhythmia can only be documented, practically speaking, when scalp electrodes are used. Because only a single lead is obtained, analysis and interpretation of rhythm and rate disturbances are severely limited. The normal newborn was delivered spontaneously and had normal cardiac rhythm in the nursery. Southall and associates (1980) studied fetal cardiac rate and rhythm disturbances in 934 normal pregnancies between 30 and 40 weeks. Arrhythmias, episodes of bradycardia <100 bpm, or tachycardia >180 bpm were encountered in 3 percent. Most supraventricular arrhythmias are of little significance during labor unless there is coexistent fetal heart failure as evidenced by hydrops. Many supraventricular arrhythmias disappear in the immediate neonatal period, although some are associated with structural cardiac defects (Api, 2008). Antepartum evaluation of the fetus with an identified arrhythmia and potential treatment options are discussed in Chapter 16 (p. Most fetal arrhythmias without comorbid fetal hydrops are inconsequential during labor, but they may hinder interpretation of fetal heart rate tracings. Generally, in the absence of fetal hydrops, neonatal outcome is not measurably improved by pregnancy intervention. At Parkland Hospital, intrapartum fetal cardiac arrhythmias, especially those associated with clear amnionic fluid, are typically managed conservatively. The last may stem from anti-D alloimmunization, fetomaternal hemorrhage, twin-twin transfusion syndrome, fetal parvoviral infection, or vasa previa with bleeding. Insignificant sinusoidal patterns have been reported following administration of meperidine, morphine, alphaprodine, and butorphanol (Angel, 1984; Egley, 1991; Epstein, 1982). An important characteristic of this pattern when due to narcotics is the sine frequency of 6 cycles per minute. A sinusoidal pattern also has been described with chorioamnionitis, fetal distress, and umbilical cord occlusion (Murphy, 1991). Young (1980a) and Johnson (1981) with their coworkers concluded that intrapartum sinusoidal fetal heart patterns were not generally associated with fetal compromise. Although these criteria were selected to define a sinusoidal pattern that is most likely ominous, they observed that the pattern associated with alphaprodine is indistinguishable. Other investigators have proposed a classification of sinusoidal heart rate patterns into mild-amplitude 5 to 15 bpm, intermediate-16 to 24 bpm, and major-25 bpm to quantify fetal risk (Murphy, 1991; Neesham, 1993). Some have defined intrapartum sine wavelike baseline variation with periods of acceleration as pseudosinusoidal. Murphy and colleagues (1991) reported that pseudosinusoidal patterns were seen in 15 percent of monitored labors. Mild pseudosinusoidal patterns were associated with use of meperidine and epidural analgesia. Intermediate pseudosinusoidal patterns were linked to fetal sucking or transient episodes of fetal hypoxia caused by umbilical cord compression. Egley and associates (1991) reported that 4 percent of fetuses demonstrated sinusoidal patterns transiently during normal labor. The pathophysiology of sinusoidal patterns is unclear, in part due to various definitions. There seems to be general agreement that antepartum sine wave baseline undulations portend severe fetal anemia. The sinusoidal pattern has been reported to develop or disappear after fetal transfusion (Del Valle, 1992; Lowe, 1984). Ikeda and associates (1999) proposed that the pattern is related to waves of arterial blood pressure, reflecting oscillations in the baroreceptor-chemoreceptor feedback mechanism. Periodic Fetal Heart Rate Changes these refer to deviations from baseline that are temporally related to uterine contractions. Acceleration refers to a rise in fetal heart rate above baseline, and deceleration is a drop below the baseline rate. The nomenclature most commonly used in the United States is based on the timing of the deceleration in relation to contractions-thus, early, late, or variable.
Buy cyklokapron 500 mg otc
Importantly treatment nurse order cyklokapron cheap online, 3 percent of women who underwent transabdominal cerclage had serious operative complications, whereas there were none in the transvaginal group. Whittle and coworkers (2009) described 31 women in whom transabdominal cervicoisthmic cerclage was done laparoscopically between 10 and 16 weeks. The procedure was converted to laparotomy in 25 percent, and there were four failures due to chorioamnionitis. Complications Principal among these are membrane rupture, preterm labor, hemorrhage, infection, or combinations thereof. In the multicenter study by Owen and colleagues (2009), of 138 procedures, there was one instance each of ruptured membranes and bleeding. In the trial by MacNaughton and associates (1993), membrane rupture complicated only 1 of more than 600 procedures done before 19 weeks. In our view, clinical infection mandates immediate removal of the suture with labor induced or augmented. Similarly, with imminent abortion or delivery, the suture should be removed at once because uterine contractions can tear through the uterus or cervix. Following cerclage, if subsequent cervical thinning is detected by sonographic assessment, then some consider a reinforcement cerclage. In one retrospective study, however, reinforcing cerclage sutures placed later did not significantly prolong pregnancy (Contag, 2016). Membrane rupture during suture placement or within the first 48 hours following surgery is considered by some to be an indication for cerclage removal because of the likelihood of serious fetal or maternal infection (Kuhn, 1977). Definitions used to evaluate these statistically include: (1) abortion ratio-the number of abortions per 1000 live births, and (2) abortion rate-the number of abortions per 1000 women aged 15 to 44 years. Overall, abortions most likely are underreported in the United States because clinics inconsistently list medically induced abortions. For example, the Guttmacher Institute found that 926,000 procedures were performed in 2014 (Jones, 2017). But for 2013, only about 664,400 elective abortions were reported to the Centers for Disease Control and Prevention (Jatlaoui, 2016). Classification Therapeutic abortion refers to termination of pregnancy for medical indications. Inclusive medical and surgical disorders are diverse and discussed throughout this text. The most frequent indication currently is to prevent birth of a fetus with a significant anatomical, metabolic, or mental deformity. The term elective abortion or voluntary abortion describes the interruption of pregnancy before viability at the request of the woman, but not for medical reasons. Most abortions done today are elective, and thus, it is one of the most frequently performed medical procedures. Abortion in the United States Legal Influence the legality of elective abortion was established by the United States Supreme Court in the case of Roe v. The Court defined the extent to which states might regulate abortion and ruled that first-trimester procedures must be left to the medical judgment of the physician. After this, the state could regulate abortion procedures in ways reasonably related to maternal health. Finally, subsequent to viability, the state could promote its interest in the potential of human life and regulate and even proscribe abortion, except for preservation of the life or health of the mother. The 1976 Hyde Amendment forbids use of federal funds to provide abortion services except in case of rape, incest, or lifethreatening circumstances. Casey and upheld the fundamental right to abortion, but established that regulations before viability are constitutional as long as they do not impose an "undue burden" on the woman. Subsequently, many states introduced counseling requirements, waiting periods, parental consent for minors, facility requirements, and funding restrictions. One major choice-limiting decision was the 2007 Supreme Court decision that reviewed Gonzales v. This was problematic because there is no medically approved definition of partial-birth abortion according to the American College of Obstetricians and Gynecologists (2014a). With this, the justices noted that abortion laws must confer health safety benefits that outweigh burdens on access. Provider Availability the American College of Obstetricians and Gynecologists (2014a, 2017d) supports the legal right of women to obtain an abortion prior to fetal viability and advocates for improved access. The College also (2017a) supports abortion training, and the Accreditation Council for Graduate Medical Education mandates that obstetrics and gynecology residency education must include access to experience with induced abortion. Ryan Residency Training Program was established in 1999 to work with residency programs to improve abortion and contraceptive training. Moreover, postresidency training in these techniques is available in formal 2-year Family Planning fellowships. Other residency programs are less codified, but teach residents technical aspects through their management of early spontaneous abortions and pregnancy interruption for fetal death, severe fetal anomalies, and life-threatening medical or surgical disorders. The College (2016g) respects the need and responsibility of health-care providers to determine their individual positions on induced abortion. It also advocates for counseling and timely referral if providers have individual beliefs that preclude pregnancy termination. Three basic choices available to a woman considering an abortion are: (1) continued pregnancy with its risks and parental responsibilities; (2) continued pregnancy with arranged adoption; or (3) termination of pregnancy with its risks. Knowledgeable and compassionate counseling should objectively describe and provide information regarding these choices to permit informed decision-making (Templeton, 2011). In the absence of serious maternal medical disorders, abortion procedures do not require hospitalization (Guiahi, 2012). However, outpatient surgical facilities should have the ability to provide emergency resuscitation and immediate transfer to a hospital (American College of Obstetricians and Gynecologists, 2014b). Surgical Abortion Preoperative Preparation Surgical evacuation is performed transvaginally through an appropriately dilated cervix. For this, preoperative cervical ripening is favored by many and is typically associated with less manual intraoperative cervical dilation, a technically easier procedure, less pain, and shorter operative times (Kapp, 2010; Webber, 2015). On balance, cervical preparation adds a surgical delay and potential side effects. In a selective approach, some recommend cervical priming for first-trimester suction curettage only for those at greater risk of complications from intraoperative cervical dilation, such as those with cervical stenosis and adolescents (Allen, 2016). Of note, surgical steps presented here apply to both induced abortion and miscarriage, discussed earlier (p. For ripening, hygroscopic dilators, also called osmotic dilators, are devices that draw water from surrounding tissues and expand to gradually dilate the endocervical canal. One type is derived from various species of Laminaria algae that are harvested from the ocean floor. These come in different diameters, which allow the number of inserted devices, also called tents, to be customized to a given cervix. Each type expands to an ultimate diameter three to four times that of its dry state. However, Dilapan-S achieves this in 4 to 6 hours, which is faster than the 12 to 24 hours needed for laminaria (Fox, 2014). With each type, the dry unit (left) expands exponentially when exposed to water (right) as in the endocervical canal. With hygroscopic dilators, shallow insertion yields insufficient internal os dilation or tent expulsion, but deep placement risks dislodgement into the uterine cavity. Once tents are inserted, several gauze sponges at the external os help prevent spontaneous tent expulsion. Laminaria immediately after being appropriately placed with its upper end just through the internal os. Several hours later the laminaria is now swollen, and the cervix is dilated and softened. Laminaria inserted too far through the internal os; the laminaria may rupture the membranes. Of 17 women who chose to continue their pregnancy, there were 14 term deliveries, two preterm deliveries, and one miscarriage 2 weeks later. None suffered infection-related morbidity, including three untreated women with cervical cultures positive for Chlamydia trachomatis.
Buy discount cyklokapron 500 mg
The etiology of this association is not well studied symptoms carpal tunnel discount 500mg cyklokapron with amex, but chromosomal abnormalities in spermatozoa likely play a role (Sartorius, 2010). Spontaneous Abortion Clinical Classification Threatened Abortion this diagnosis is presumed when bloody vaginal discharge or bleeding appears through a closed cervical os during the first 20 weeks. This bleeding in early pregnancy must be differentiated from that with implantation, which some women have at the time of their expected menses. Aside from this, almost one fourth of women develop bleeding during early gestation that may persist for days or weeks. It may be accompanied by suprapubic discomfort, mild cramps, pelvic pressure, or persistent low backache. Of symptoms, bleeding is by far the most predictive risk factor for pregnancy loss. Even if miscarriage does not follow threatened abortion, rates of later adverse pregnancy outcomes are increased as shown in Table 18-1. Weiss and coworkers (2004) noted greater risks for adverse outcomes in later pregnancy if early bleeding was heavy rather than light. Compared with those without bleeding, women with first-trimester bleeding in an initial pregnancy have higher recurrence rates in their second (Lykke, 2010). Adverse Outcomes That Are Increased in Women with Threatened Abortion Every woman with an early pregnancy, vaginal bleeding, and pain should be evaluated. Because these are not 100-percent accurate to confirm early embryo death or location, repeat evaluations are often necessary. Although a less-used marker, serum progesterone concentrations <5 ng/mL suggest a dying pregnancy. The gestational sac-an anechoic fluid collection that represents the exocoelomic cavity-may be seen by 4. Another caveat is that a gestational sac may appear similar to other intrauterine fluid accumulations-the so-called pseudogestational sac. This pseudosac may be blood derived from a bleeding ectopic pregnancy and is easier to exclude once a yolk sac is seen. If anemia or hypovolemia is significant, then pregnancy evacuation is generally indicated. In cases in which there is a live fetus, some instead may choose transfusion and further observation. Incomplete Abortion During abortion, bleeding follows partial or complete placental separation and dilation of the cervical os. Thus, tissue may remain entirely within the uterus or partially extrude through the cervix. Products lying loosely within the cervical canal can be easily extracted with ring forceps. The last two are deferred in clinically unstable women or those with uterine infection. However, misoprostol and expectant care are associated with unpredictable bleeding, and some women will undergo unscheduled curettage. Expectant management of spontaneous incomplete abortion has failure rates that approximate 25 percent in randomized trials (Nadarajah, 2014; Nielsen, 1999; Trinder, 2006). Some observational studies have shown failure rates of 10 to 15 percent (Blohm, 2003; Casikar, 2012; Luise, 2002). Medical therapy carries failure rates of 5 to 30 percent (Dao, 2007; Shochet, 2012; Trinder, 2006). In many studies for this, an oral misoprostol dose of 600 g has been used (American College of Obstetricians and Gynecologists, 2009). Alternatively, an 800-g vaginal or a 400-g oral or sublingual misoprostol dose is suitable. Last, curettage usually results in a quick resolution that is 95- to 100percent successful. Complete Abortion At times, complete expulsion of the entire pregnancy may ensue, and the cervical os subsequently closes. Patients are encouraged to bring in passed tissue, in which a complete gestation should be discerned from blood clots or a decidual cast. The latter is a layer of endometrium in the shape of the uterine cavity that when sloughed can appear as a collapsed sac. If an expelled complete gestational sac is not identified, transvaginal sonography is performed to differentiate a complete abortion from threatened abortion or ectopic pregnancy. Characteristic findings of a complete abortion include a minimally thickened endometrium without a gestational sac. Condous and associates (2005) described 152 women with heavy bleeding, an empty uterus with endometrial thickness <15 mm, and a diagnosis of completed miscarriage. Thus, a complete abortion cannot be surely diagnosed unless: (1) true products of conception are seen grossly or (2) unless sonography confidently documents first an intrauterine pregnancy and then later an empty cavity. Calipers measure uterine length and anteroposterior thickness in a sagittal plane. During scanning, because of theoretical temperature elevation in tissues exposed to pulsed Doppler beam, this modality is applied only when needed for additional diagnostic purposes. M-mode should be used to document cardiac activity and measure the rate (Lane, 2013). In addition to the diagnostic parameters of Table 18-3, other softer sonographic markers may portend early pregnancy failure. Values for yolk sac diameters (measured inner-to-inner ring) for each gestational week in normal pregnancy have been established. A slower heart rate is unfavorable, especially those <85 bpm (Laboda, 1989; Stefos, 1998). Last, subchorionic hematoma, that is, blood collected between the chorion and uterine wall, often accompanies threatened miscarriage. Studies are contradictory as to its association with ultimate pregnancy loss (Pedersen, 1990; Stabile, 1989; Tuuli, 2011). Bennett and associates (1996) noted that miscarriage risk correlated with larger hematoma size, older maternal age, and bleeding at a gestational age 8 weeks. With rapid confirmation of embryonic or fetal death, surgical or medical evacuation or expectant observation is an option. As with induced abortion, nonsurgical options balance their noninvasiveness against heavier procedural bleeding, longer completion times, and lower success rates. Of options, expectant care underperforms medical or surgical options, and failure rates range from 15 to 50 percent (Luise, 2002; Trinder, 2006; Zhang, 2005). Also, weeks may pass between pregnancy failure diagnosis and actual spontaneous miscarriage. A single 800-g dose vaginally is a common standard (American College of Obstetricians and Gynecologists, 2016c). It may be repeated in 1 to 2 days, and one large trial reported that 22 percent of women required a second dose (Zhang, 2005). Overall, failure rates range from 15 to 40 percent (Petersen, 2014; Trinder, 2006). Unlike induced abortion, adding mifepristone does not add value (Stockheim, 2006). Contraindications mirror those listed in the section describing induced abortion (p. That said, there is no consensus on an endometrial thickness threshold that mandates additional intervention. Rupture may be spontaneous or may follow an invasive procedure such as amniocentesis or fetal surgery. A gush of vaginal fluid that is seen pooling during sterile speculum examination confirms the diagnosis. In suspect cases, amnionic fluid will fern on a microscope slide or will have a pH >7, or oligohydramnios will be seen on sonography (Sugibayashi, 2013). Also, amnionic fluid proteins placental alpha microglobulin-1 and insulin growth factor binding protein-1, described in Chapter 22 (p. In iatrogenic cases, defects are typically higher in the uterus and tend to self seal. Also, an occlusive plug-termed an amniopatch-can be created by intraamnionic instillation of autologous platelets and cryoprecipitate. Considered investigational, it is used to seal some surgical leaks (Richter, 2013). Spontaneous rupture in the first trimester is nearly always followed by either uterine contractions or infection, and termination is typical.
Purchase cyklokapron 500 mg line
The physiological processes that regulate parturition-the bringing forth of young-and the onset of labor continue to be defined medications osteoarthritis pain buy discount cyklokapron online. Viewed simplistically, the first is the functional loss of pregnancy maintenance factors. The third suggests that the mature fetus is the source of the initial signal for parturition commencement. However, labor onset clearly represents the culmination of a series of biochemical changes in the uterus and cervix. These result from endocrine and paracrine signals emanating from both mother and fetus. Their relative contributions vary between species, and it is these differences that complicate elucidation of the exact factors that regulate human parturition. When parturition is abnormal, then preterm labor, dystocia, or postterm pregnancy may result. Of these, preterm labor remains the major contributor to neonatal mortality and morbidity. In contrast to skeletal or cardiac muscle, the smooth muscle cell is not terminally differentiated and therefore is readily adaptable to environmental changes. Varied stimuli such as mechanical stretch, inflammation, and endocrine and paracrine signals can modulate the transition of the smooth muscle cell among phenotypes that provide cell growth, proliferation, secretion, and contractility. In addition to this phenotypic plasticity, several smooth muscle qualities confer advantages for uterine contraction efficiency and fetal delivery. First, the degree of smooth muscle cell shortening with contractions may be one order of magnitude greater than that attained in striated muscle cells. This differs from the contraction force generated by skeletal muscle, which is always aligned with the axis of the muscle fibers. In myometrium, the thick and thin filaments are found in long, random bundles throughout the cells. Last, greater multidirectional force generation in the uterine fundus compared with that of the lower uterine segment permits versatility in expulsive force directionality. Lining the thick muscular uterine walls, the endometrium is transformed by pregnancy hormones and is then termed decidua. Composed of stromal cells and maternal immune cells, the decidua serves to maintain the pregnancy via unique immunoregulatory functions that suppress inflammatory signals during gestation. With this, the decidua transitions to induce inflammatory signals and withdraw active immunosuppression, which contribute to parturition initiation. During pregnancy, the cervix has multiple functions that include: (1) maintenance of barrier function to protect the reproductive tract from infection, (2) maintenance of cervical competence despite greater gravitational forces as the fetus grows, and (3) orchestration of extracellular matrix changes that allow progressively greater tissue compliance. In nonpregnant women, the cervix is closed and firm, and its consistency is similar to nasal cartilage. By the end of pregnancy, the cervix is easily distensible, and its consistency is similar to the lips of the oral cavity. Observations in threedimensional sonography and magnetic resonance imaging show increases in the cross-sectional area of the cervical canal and in the cervical stroma from early to late pregnancy (House, 2009; Lang, 2010). Concurrent with expansion of the stroma, the cervical epithelia proliferate and exert a pregnancy-specific immunoprotection. Placenta In addition to providing the exchange of nutrients and waste between mother and fetus, the placenta is a key source of steroid hormones, growth factors, and other mediators that maintain pregnancy and potentially aid the transition to parturition. The fetal membranes-amnion and chorion and adjacent decidua-make up an important tissue shell around the fetus that serves as a physiological, immunological, and metabolic shield to protect against untimely parturition initiation. This avascular tissue is highly resistant to penetration by leukocytes, microorganisms, and neoplastic cells. It also constitutes a selective filter to prevent fetal particulate-bound lung and skin secretions from reaching the maternal compartment. In this manner, maternal tissues are protected from amnionic fluid constituents that could prematurely accelerate decidual or myometrial activation or could promote adverse events such as amnionic fluid embolism. The role of decidual activation in parturition is unclear but may involve local progesterone metabolism and higher prostaglandin receptor concentrations, thus enhancing uterine prostaglandin actions and cytokine production. It is also enriched with enzymes that inactivate uterotonins, which are agents that stimulate contractions. Inactivating enzymes include prostaglandin dehydrogenase, oxytocinase, and enkephalinase (Cheung, 1990; Germain, 1994). And, the removal of progesterone, that is, progesterone withdrawal, directly precedes progression of parturition. In addition, providing progesterone to some species will delay parturition via a decline in myometrial activity and continued cervical competency (Challis, 1994). In humans, however, it seems most likely that both estrogen and progesterone are components of a broader molecular system that maintains uterine quiescence. Plasma levels of estrogen and progesterone in normal pregnancy are enormous and in great excess of the affinity constants for their receptors. For this reason, it is difficult to comprehend how relatively subtle changes in the ratio of their concentrations could modulate physiological processes during pregnancy. The teleological evidence, however, for an increased progesterone-to-estrogen ratio in the maintenance of pregnancy and a decline in this ratio for parturition is overwhelming. These include cervical ripening, greater cervical distensibility, and augmented uterine sensitivity to uterotonins (Bygdeman, 1994; Chwalisz, 1994b; Wolf, 1993). The exact role of estrogen in regulation of human uterine quiescence and cervical competency is less well understood. That said, estrogen can advance progesterone responsiveness and, in doing so, promote uterine quiescence. At the end of pregnancy, estrogen aids processes that mediate uterine activation and cervical ripening. Both progesterone and estrogen bind to nuclear receptors that regulate gene transcription in a cell- and context-specific pattern. In parturition, they play a prominent role in myometrial contractility, relaxation, and inflammation. Prostaglandins are produced using plasma membrane-derived arachidonic acid, which usually is released by the action of phospholipase A2 or C. Through prostaglandin isomerases, prostaglandin H2 is converted to active prostaglandins. Isomerase expression is tissue-specific and thereby controls the relative production of various prostaglandins. Expression of this enzyme is upregulated during pregnancy in the uterus and cervix, which provides the important ability to rapidly inactivate prostaglandins (Giannoulias, 2002; Kishore, 2014). Thus, myometrial responses to prostaglandins stem from a balance between prostaglandin synthesis versus metabolism, from the relative expression of various prostaglandin receptors, or from a switch in receptor-signaling pathways (Kandola, 2014; Lyall, 2002; Olson, 2007; Smith, 2001). It is entirely possible that prostanoids contribute to myometrial relaxation at one stage of pregnancy and to myometrial contractions after parturition initiation (Myatt, 2004). In addition to the myometrium, the amnion synthesizes several bioactive peptides and prostaglandins that cause myometrial relaxation or contraction. Accordingly, many hypothesize that prostaglandins regulate events leading to parturition. The amnion is likely the major source for amnionic fluid prostaglandins, and their role in the activation of cascades that promote membrane rupture is clear. The influence of amnion-derived prostaglandins on uterine quiescence and activation, however, is less delineated. These phases of parturition include: (1) a prelude to it, (2) the preparation for it, (3) the process itself, and (4) recovery. Importantly, the phases of parturition should not be confused with the clinical stages of labor, that is, the first, second, and third stages-which make up phase 3 of parturition. The curve is based on analysis of data derived from a large, nearly consecutive series of women. The first stage is divided into a relatively flat latent phase and a rapidly progressive active phase. In the active phase, there are three identifiable parts: an acceleration phase, a linear phase of maximum slope, and a deceleration phase. This phase 1 normally comprises 95 percent of pregnancy and is characterized by uterine smooth muscle tranquility with maintenance of cervical structural integrity. All manner of molecular systems-neural, endocrine, paracrine, and autocrine-are likely called to implement and coordinate a state of relative uterine unresponsiveness. Moreover, a complementary "fail-safe" system that protects the uterus against agents that could perturb the tranquility of phase 1 also must be in place.
Discount cyklokapron 500 mg with visa
With scheduled cesarean delivery treatment 3rd degree heart block cheap cyklokapron 500 mg otc, the cerclage may be removed at 37 weeks or deferred until the time of regional analgesia and delivery. During extraction, particularly with a Shirodkar cerclage or a cerclage using Mersilene tape, analgesia helps ensure patient comfort and adequate visualization. Transabdominal Cerclage At times, suture placed at the uterine isthmus can be used and left until completion of childbearing. Because of significantly greater risks of bleeding and complications during placement, this approach is reserved for selected instances of severe cervical anatomical defects or prior transvaginal cerclage failure. Placement of a cervicoisthmic cerclage was originally described using laparotomy, but several reports additionally detail laparoscopic or robotically assisted cervicoisthmic cerclages. Placement before pregnancy and during pregnancy was similar, whether performed laparoscopically or by laparotomy. Following incision and sharp dissection in the vesicouterine space, the bladder is mobilized caudally. At the level of the internal os, a window is made in free space medial to the uterine vessels. In this case, the knot is tied anteriorly, and the vesicouterine peritoneum is closed with absorbable suture in a running fashion. In similar circumstances with four second-trimester terminations, Siedhoff and Cremer (2009) described two preterm and two term deliveries. The typical dose is 400 g administered sublingually, buccally, or placed into the posterior vaginal fornix 3 to 4 hours prior to surgery. Instead, oral administration proves less effective and may take longer (Allen, 2016). Another effective cervicalripening agent is the antiprogestin mifepristone, 200 mg given orally 24 to 48 hours before surgery (Ashok, 2000). Its cost and greater delay to the procedure, however, typically favor misoprostol use instead. In comparing hygroscopic dilators and misoprostol for ripening, randomized studies show equal or slightly greater dilation with hygroscopic dilators. Other surgical parameters do not vary significantly (Bartz, 2013; Burnett, 2005; MacIsaac, 1999). Hygroscopic dilators extend procedure time and can be uncomfortable, whereas misoprostol introduces fever, bleeding, and gastrointestinal side effects. If not done as part of early prenatal care, hemoglobin level and Rh status are assessed. Screening for gonorrhea, for syphilis, and for human immunodeficiency virus, hepatitis B, and chlamydial infections is also completed. To prevent postabortal infection after a first- or second-trimester surgical evacuation, prophylactic doxycycline, 100 mg orally 1 hour before and then 200 mg orally after, is provided (Achilles, 2011; American College of Obstetricians and Gynecologists, 2016a). Prophylaxis specifically for infective endocarditis prevention in those with valvular heart disease is not required in the absence of active infection (Nishimura, 2017). No recommendations specifically address venous thromboembolism prophylaxis for suction curettage in low-risk gravidas. Vacuum Aspiration Also called suction dilation and curettage or suction curettage, vacuum aspiration is a transcervical approach to surgical abortion. For this, a rigid cannula is attached either to an electric-powered vacuum source or to a handheld 60-mL syringe for its vacuum source. Sharp dilation and curettage (D & C) in which contents are mechanically scraped out solely by a sharp curette is currently not recommended for pregnancy evacuation due to greater blood loss, pain, and procedural time (National Abortion Federation, 2016; World Health Organization, 2012). Importantly, this practice is distinguished from brief sharp curettage following initial aspiration. After bimanual examination is performed to determine uterine size and orientation, a speculum is inserted, and the cervix is swabbed with povidone-iodine or equivalent solution. Thus, vacuum aspiration at minimum requires intravenously or orally administered sedatives or analgesics, and some add a paracervical or intracervical blockade with lidocaine (Allen, 2009; Renner, 2012). Uterine sounding measures the depth and inclination of the cavity before other instrument insertion. If required, the cervix is further dilated with Hegar, Hank, or Pratt dilators until a suction cannula of the appropriate diameter can be inserted. Pratt and Hank dilators are sized in French units, which can be converted to millimeters by dividing the French number by three. With dilation, the fourth and fifth fingers of the hand introducing the dilator should rest on the perineum and buttocks as the instrument is pushed through the internal os. This technique minimizes forceful expansion and provides a safeguard against uterine perforation. Note that the fourth and fifth fingers rest against the perineum and buttocks, lateral to the vagina. This maneuver is an important safety measure because if the cervix relaxes abruptly, these fingers prevent a sudden and uncontrolled thrust of the dilator, a common cause of uterine perforation. Following dilation, for most first-trimester aspiration procedures, an 8- to 12mm Karman cannula is appropriate. Small cannulas carry the risk of leaving retained intrauterine tissue postoperatively, whereas large cannulas risk cervical injury and more discomfort. The cannula is gradually pulled back toward the os and is slowly turned circumferentially to cover the entire surface of the uterine cavity. In the movement of the curette, only the strength of these two fingers should be used. To identify placenta, the aspirated contents are rinsed in a strainer to remove blood, and then placed in a clear plastic container with saline and examined with back lighting (MacIsaac, 2000). With gestations 7 weeks, the failed abortion rate approximates 2 percent (Kaunitz, 1985; Paul, 2002). Abortion Complications In women undergoing abortion, complication rates rise with gestational age. Of these, uterine perforation and lower-genital-tract laceration are uncommon but potentially serious. In one systematic review of first-trimester abortion, the uterine perforation rate was 1 percent, as was the cervical or vaginal laceration rate (White, 2015). Perforation is usually recognized when the instrument passes without resistance deep into the pelvis. Risk factors include operator inexperience, prior cervical surgery or anomaly, adolescence, multiparity, and advanced gestational age (Allen, 2016; Grimes, 1984). If the uterine perforation is small and fundal, as when produced by a uterine sound or narrow dilator, observation of vital signs and for uterine bleeding is usually sufficient. If a suction cannula or sharp curette passes into the peritoneal cavity, considerable intraabdominal damage can ensue. In these cases, laparotomy or laparoscopy to thoroughly examine the abdominal contents is often the safest course. Uterine perforation is not a contraindication to completing the curettage under direct guidance during laparoscopy or laparotomy (Owen, 2017). Following curettage, uterine synechiae may form, and the risk of synechiae increases with the number of procedures. However, of Asherman syndrome cases, one series found that two thirds were linked to first-trimester curettage (Schenker, 1982). Other first-trimester abortion complications are hemorrhage, incomplete removal of products, and postoperative infections, and these are germane to both surgical and medical abortion techniques. One supported by the Society for Family Planning is bleeding that prompts a clinical response or bleeding in excess of 500 mL (Kerns, 2013). For first-trimester surgical abortions, hemorrhage complicates 1 percent (White, 2015). Atony, abnormal placentation, and coagulopathy are frequent sources, whereas surgical trauma is a rare cause.