Purchase kytril us
A fascial rent may cause a hernia medicine to stop diarrhea buy kytril 1mg on-line, particularly if there was previous upper abdominal surgery. Compression of the nerve roots by a herniated disc, thoracic spondylosis, or a spinal cord tumor is possible, but unlikely. Systemic conditions, such as lead colic and porphyria, and involvement of another organ, such as the kidney, must be considered (pyelonephritis or renal colic). Utilizing the methods applied above, what is your list of possible causes at this point Further history reveals the pain is colicky; she is the mother of four children and had a few similar attacks in the past 5 years but never this severe. In the first layer are the skin, abdominal wall, and ribs; in the second layer, the spleen, colon, and stomach; and in the third layer, the pancreas, adrenal gland, kidney, aorta, and spine. Abdominal wall and ribs: Pain will occur most commonly from herpes zoster, contusion, hernia, rib fracture, or metastatic tumor. A ruptured spleen is an important consideration in abdominal injuries, particularly those in children and in patients with infectious mononucleosis. Episodic obstruction of the stomach in the "cascade stomach" should be considered in the differential diagnosis. Less commonly, the colon develops a perforating or constricting carcinoma in this area, which obstructs the bowel. Approach to the Diagnosis the presence or absence of other symptoms and signs will be most helpful in the diagnosis. For this reason, the astute clinician will want to have a good list of possibilities in mind. Visualizing the structures, layer by layer, one finds the skin and abdominal wall in the first layer; the terminal ileum, cecum, appendix, and Meckel diverticulum in the second layer; the ureters, tubes, and ovaries (in women) in the third layer; and the muscles, spine, and terminal aorta in the fourth layer. The following discussion emphasizes the most important diseases in the differential diagnosis. Terminal ileum: Regional ileitis, tuberculosis, or typhoid and intussusceptions may involve the ileum and cause severe pain. Meckel diverticulum: this congenital anomaly may become obstructed and inflamed, develop a pancreatitis or a perforated peptic ulcer, or communicate with a periumbilical cellulitis. Ovarian cysts may twist on their pedicles or rupture, causing pain, as may the rupture of a small graafian follicle in the normal cycle (mittelschmerz). Three significant lesions may involve the tube: salpingitis, endometriosis, and ectopic pregnancy. Aorta: Dissecting aneurysms or emboli of the terminal aorta and its branches may seize the patient with acute pain. Pelvis and spine: Osteoarthritis, ruptured disc, metastatic carcinoma, Pott disease, and rheumatoid spondylitis should be considered here. Referred pain from pneumonia or pulmonary infarct has encouraged some surgeons to insist on a chest x-ray prior to surgery. A pregnancy test should be ordered for women of childbearing age to help rule out a ruptured ectopic pregnancy, but ultrasonography is even better. Surprisingly, many patients get to the operating room without a rectal or vaginal examination. If these are not diagnostic, further investigation with colonoscopy, cystoscopy, culdoscopy, or laparoscopy may be needed. There are fewer structures to deal with; thus, the differential diagnosis is not difficult. Visualizing the structures layer by layer, there are the skin and abdominal wall in the first layer; the sigmoid colon, omentum, and portions of small intestine in the second layer; the ureter, fallopian tubes, and ovaries (in women) in the third layer; and the 107 aorta, pelvis, and spine beneath all these structures. The following discussion emphasizes the most important diseases that must be considered in the differential diagnosis. Small intestine: Regional ileitis, intussusception, adhesion, volvulus, and other conditions that cause intestinal obstruction should be considered here. Sigmoid colon: Diverticulitis, ischemic colitis, mesenteric adenitis and infarct, and granulomatous colitis are important causes. The tubes may cause pain if there is an ectopic pregnancy, if they are inflamed by a salpingitis, or if they are infiltrated by endometriosis. Aorta: Dissecting aneurysms and emboli of the terminal aorta may cause acute lower quadrant pain. Pelvis and spine: Osteoarthritis, a ruptured disc, metastatic carcinoma, Pott disease, and rheumatoid spondylitis should be considered here. Referred pain from pneumonia, pleurisy, and myocardial infarction is uncommon but must be considered. Metabolic conditions that cause generalized abdominal pain and that should be remembered are listed on page 30. Approach to the Diagnosis There is no doubt about the value of a good history and physical examination, including both the rectal and pelvic areas. After this, the signs and symptoms should be summarized and grouped together; in many 108 cases, this technique will pinpoint the diagnosis. Further history reveals she had intermittent vaginal bleeding for 2 weeks and she was treated for a vaginal discharge several months ago. Anatomy, therefore, is the basic science used to develop this differential diagnosis. The skin may be the site of the pain in herpes zoster, as it is in other types of pain, although it is less likely to be midline. However, muscle and fascial conditions may be missed if one does not specifically think of this layer. Thus, epigastric hernia, hiatal hernia, or contusion of the muscle will be missed, as will diaphragmatic abscesses and trichinosis of the diaphragm. The stomach and duodenum are the next organs encountered; both are prominent causes of epigastric pain. Pyloric stenosis (from whatever cause), cascade stomach, diverticula, and carcinoma or sarcoma round out the differential diagnosis here. The colon and small intestines lie just below the stomach, so one must not forget ileitis, colitis (ulcerative or granulomatous), appendicitis, diverticulitis, Meckel diverticulum, and transverse colon carcinoma that ulcerates through the wall. Intestinal parasites and mesenteric thrombosis are additional causes that originate here. The various forms of intestinal obstruction are more important than parasites and mesenteric thrombosis. The pancreas sits at the next layer, and acute pancreatitis is a particularly severe form of epigastric pain. Chronic pancreatitis, carcinoma, cysts of the pancreas, and mucoviscidosis cause less severe forms of epigastric pain. The lymph nodes may be involved by Hodgkin lymphoma and lymphosarcoma, leading to intestinal obstruction, but mesenteric adenitis is a much more likely cause. The blood vessels are contained in the next layer, and one is reminded of aortic aneurysm, abdominal angina, periarteritis nodosa, and other forms of vasculitis. The sympathetic and parasympathetic nerves are involved by lead colic, porphyria, and black widow spider venom. Cord tumor, tuberculosis, herniated disc, osteoarthritis, and rheumatoid spondylitis can all lead to midepigastric pain. Omission of the systemic diseases and diseases of other abdominal 112 organs that sometimes cause epigastric pain is inexcusable. Pneumonia, myocardial infarction (inferior wall, particularly), rheumatic fever, epilepsy, and migraine are just a few systemic conditions that are associated with epigastric or generalized abdominal pain. Cholecystitis, hepatitis, and pyelonephritis are some local diseases that also produce midepigastric or generalized abdominal pain, which is why the target system has a useful application here. The center circle of the target is the stomach, the pancreas, and other organs in Table 11. Approach to the Diagnosis the approach to the diagnosis of midepigastric pain is identical to that for generalized abdominal pain (see page 29). Hypogastric Pain Anatomy is the basic science that will open the door to this differential diagnosis. Visualizing the structures in the hypogastrium, one sees the abdominal wall, the bladder and urinary tract, the female genital tract, the sigmoid colon and rectum, the iliac vessels, the aorta and vena cava, and the lumbosacral spine. Occasionally, other organs fall into the hypogastrium; thus, they must be considered too. A pelvic kidney, visceroptosis of the transverse colon, and a pelvic appendix all may occur.
Buy 1 mg kytril free shipping
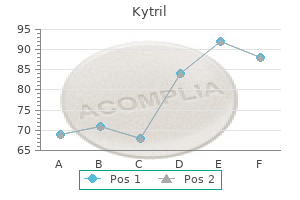
Classifications of myelodysplasia have traditionally focused on clinical and pathological features but now take into account other prognostic features symptoms xeroderma pigmentosum discount kytril 1 mg online, notably cytogenetics (see Box 288. Additional risk classifications, including multiple scoring systems, have been used to define prognosis in myelodysplasia and to evaluate its potential for transformation to acute myeloid leukaemia. The International Prognostic Scoring System takes into account specific cytopenias, age, and cytogenetics, in addition to bone marrow morphology. It defines four risk categories, Low, Intermediate-1, Intermediate-2, and High, which indicate both survival and evolution to acute myeloid leukaemia. Copyright (2009) World Health Organization General features Myelodysplasia is mainly a disease of the elderly, and is becoming more common as the population ages. Most cases arise de novo, but myelodysplasia develops occasionally in patients who have been treated with radiation and/or cytotoxic chemotherapy for some other condition. The condition usually presents as a mild symptomatic, refractory anaemia or comes to light following a routine blood count. Platelets and neutrophils may also be morphologically abnormal with giant platelets and neutrophil hypogranularity with reduced nuclear lobulation. The marrow is usually hypercellular and shows abnormal cellular and nuclear maturation with evidence of ineffective haemopoiesis and intra-medullary cell death. Thus, despite apparent increased cellular activity, output of blood cells is reduced. In around 10% of cases, the marrow is hypocellular; here, there is overlap with aplastic anaemia. Over 600 different cytogenetic abnormalities have been described, although only a few occur commonly. Translocations are rare: the commonest affect Chromosome 8 (gain), Chromosome 5 (deletion or loss), and Chromosome 7 (deletion or loss). There is a tendency for abnormalities to accumulate as the disease progresses, and complex (multiple) abnormalities carry a worse prognosis. Isolated deletion of the long arm of Chromosome 5-del(5q)-is associated with a specific form of refractory anaemia characterized by a high prevalence in elderly females and a relatively good prognosis. It is characterized by a macrocytic anaemia, a normal or high platelet count, a modest leucopenia without excess blasts in the marrow, and a particular megakaryocyte appearance. The risk of leukaemic transformation is about 30% overall in primary myelodysplasia but much higher in secondary cases. Acute myeloid leukaemia arising from myelodysplasia responds very poorly to chemotherapy, and cure is realistically only feasible following allogeneic bone marrow transplantation. Treatment is supportive in the early stages, with blood and platelet transfusion and prompt treatment of infection as required. The thalidomide analogue lenalidomide has shown a beneficial effect on anaemia in ~80% of patients with del(5q) and in ~50% of other low-risk patients. Cytotoxic therapy is inappropriate (and usually harmful) in most cases unless acute leukaemia develops, and is usually unsuccessful when it does. An exception may be younger patients (less than 65 years) who have a suitable donor, in which case they should be considered for bone marrow transplantation. Within the B-cell non-Hodgkin lymphomas, there are clinically aggressive (high-grade) forms and much more indolent (low-grade) forms. In these cases, mediastinal nodal enlargement may present with cough, breathlessness, or superior vena cava obstruction; porta hepatis nodal enlargement may present with obstructive jaundice; and pelvic nodal enlargement may present with a deep vein thrombosis or bilateral lower limb oedema. Systemic symptoms Common symptoms include fatigue, anorexia, weight loss, fever, and night sweats. Pruritus is also not uncommon, and alcohol-induced pain is a rare but characteristic feature of lymphoid malignancy. Lymphoma may, however, present in any number of ways, depending mainly on the sites of involvement. Less common systemic effects of lymphomas are also well documented, including a paraprotein-induced peripheral neuropathy and a nephrotic syndrome caused by unknown mechanisms. Demographics of the disease the incidence of lymphoma is roughly 19 per 100 000 of the population per year, representing the fifth most common form of cancer. Overall, lymphoma is 50% more common in men and affects white Americans 50% more than black Americans. Other agents Human T-lymphotropic virus 1 is associated with adult T-cell leukaemia/lymphoma. For example, endemic Burkitt lymphoma is found almost exclusively in equatorial Africa, whereas adult T-cell leukaemia/lymphoma is most common in Japan and the Caribbean basin. A proportion of indolent lymphomas will, however, undergo a large-cell transformation and then behave as aggressive, high-grade lymphomas. Systemic T-cell lymphomas are usually rapidly progressive and generally respond poorly to treatment. Cutaneous T-cell lymphomas (which will not be dealt with further) often have excellent outcomes, however. Acceptable diagnostic alternatives to the gold standard There is really no alternative to obtaining good quality biopsy material. Occasionally, the diagnosis can be made on bone marrow trephine only but biopsy of a lymph node or extra-nodal mass is usually preferable first. As for Hodgkin lymphoma, involved field radiotherapy is used in some centres to sites of bulky or extra-nodal disease. In patients who are fit enough, second remissions are then consolidated with high-dose chemotherapy combined with autologous stem cell support. If patients are not deemed fit enough to undergo this procedure, a palliative approach is frequently adopted. Therefore, the aim of treatment is to keep the patient as healthy as possible for as long as possible. Initiation of treatment is only indicated for symptoms or critical organ impairment such as bone marrow failure. As for high-grade disease, the addition of rituximab has been demonstrated to improve responses and survival. Subsequent relapses are treated with further rounds of chemotherapy, although subsequent remissions tend to be of reducing duration. Certain interventions may prolong subsequent remissions, such as the use of high-dose chemotherapy with autologous stem cell support, the use of maintenance rituximab infusions, or the use of radioimmunotherapy (which utilizes a monoclonal antibody conjugated to a radioisotope). Note: the addition of rituximab has significantly improved the 5-year survival rates in each prognostic category. Important side effects include neuropathy (from the vinblastine) and lung toxicity (from the bleomycin). Adjunctive involved field radiotherapy may be used at sites of bulk disease or at extra-nodal sites. Due to the high survival rates, concern has shifted to the late toxic effects of treatment. Efforts are being made to reduce toxicity of treatment while maintaining the excellent disease control. Relapsed Hodgkin lymphoma is treated where possible with salvage chemotherapy (consisting of different agents from those initially used to minimize the effects of drug resistance). If the disease remains chemo-responsive, the patient usually receives high-dose chemotherapy with autologous stem cell support. This procedure enables high-dose chemotherapy to be given while minimizing the resulting period of myelosuppression. Although initial responses are often seen, relapses are frequent and difficult to treat. When a plasma cell clone is only detected in one site (either bony or soft tissue), it is termed a plasmacytoma.
Order kytril overnight delivery
In addition medicine vicodin kytril 1 mg sale, alcohol consumption and viral hepatitis are preventable causes of liver disease, liver failure, and hepatic cancer. There is a well-established association between Helicobacter pylori and gastric cancer, and several observational studies from Japan and China have shown that eradication of Helicobacter pylori reduces the incidence of stomach cancer. However, this result cannot be transferred to general medical practice without larger studies, as these findings may relate to the higher incidence of stomach cancer in these countries. Colorectal cancer the most effective preventive measure for colorectal cancer is the establishment of screening programmes. The aim is to identify people with early and therefore treatable cancers, and also people with colorectal adenomatous polyps. Other etiological factors known to increase the risk of bowel cancer include diets high in fat and cholesterol, and red meat, especially processed meat. Many patients who attend hospital harbour concerns of developing cancer, and all of these factors can be discussed with them as potential preventive measures. Conversely, studies have shown that regular aspirin ingestion can reduce the incidence of colorectal adenomatous polyps and colon cancer. Alcohol It is well recognized that excess alcohol consumption is associated with a wide range of different disease processes. In addition to liver disease, alcohol consumption is also an etiological factor in many cancers, and is estimated to be the cause of 6% of cancer deaths. The concept that red wine can reduce cancer risk has been disputed by large studies, and should not be supported in clinical practice. Gastrointestinal physicians will see many patients with deranged liver function related to alcohol consumption, and it is important that the patient is educated appropriately: reducing alcohol consumption not only reduces the risk of liver disease and cirrhosis, but also reduces the risk of cancer. Prevention is difficult and dependent on patient commitment, so support services should be made available. Smoking Smoking is an etiological factor in many diseases: 50% of smokers die from cancer or smoking-related diseases, and 25% of these deaths will be in patients under the age of 70 years. Smoking has been closely associated with oesophageal, gastric, and liver cancer and, consequently, smoking prevention should reduce the incidence of these and other smoking-related conditions. Conversely, ulcerative colitis is more frequent with non-smokers, and often presents for the first time when former smokers stop. An interesting corollary of this is that life-expectancy in ulcerative colitis is equal to or greater than in the general population. There is no definitive evidence that this will reduce the incidence of oesophageal adenocarcinoma as yet, but the combination of earlier diagnosis and treatment of highgrade dysplasia is expected to have this effect. Peptic ulcer disease the two main treatment options for patients with peptic ulcer disease are proton-pump inhibitors and eradication of Helicobacter pylori, as both treatments improve ulcer healing. However, there is no evidence that either treatment can be used a primary preventive measure. Usually, prophylactic treatment is reserved for patients who would have a poor prognosis should they develop peptic ulcers, for example, elderly patients receiving anticoagulation medication. The major routes of transmission are vertical, from mother to child, mainly in the Far East, and horizontal, from shared needles, unprotected sexual intercourse, and non-sterile shared equipment, for instance in tattooing. The development of a vaccine for hepatitis B offers the chance to eliminate the risk of transmission. Research hopes to develop a vaccine but, even if such research is successful, reaching patients at risk of contracting the virus will be difficult. There is limited evidence of sexual transmission, and blood products are now routinely screened. Gastrointestinal infection the most important preventive measure to reduce the incidence of gastrointestinal infections is to maintain good sanitation, with handwashing and hygienic food preparation. The main barrier to this worldwide is the lack of safe, uncontaminated drinking water, poor sanitary facilities, and poverty. These are obviously also etiological factors for ischaemic heart disease; thus, patients receive additional benefit from controlling each factor. Weight loss, together with control of blood pressure, cholesterol levels, and diabetes, is expected to slow the progression of liver disease, preventing the development of steatohepatitis and subsequent cirrhosis. It is estimated that one-third of consultations with general practitioners involve neurological complaints, and neurological disorders are present in one-third of patients admitted to hospital. In considering how to reduce the incidence of neurological disease, one must take into account the feasibility of prevention, and the overall morbidity caused by the disease. In stroke, which is very common, interventions which reduce incidence by a small percentage have the potential to have a large impact on a population basis. A disorder such as migraine, while not life-limiting, accounts for significant morbidity and time off work (one study suggests that there are the equivalent of 112 million bedridden days per year due to migraine alone), so, again, interventions that reduce the frequency of episodes even by a small percentage can have great overall impact. In this chapter, we consider the major categories of neurological disease based on pathogenesis, and current and future approaches to prevention. Prevention in vascular neurological disease Prevention of stroke Stroke is the main cause of neurological morbidity in adults and the third most common cause of death worldwide after ischaemic heart disease and cancer (all forms combined). Preventive strategies for stroke, due to either ischaemia or haemorrhage, are discussed in Chapter 348. Prevention of epileptic seizures Epilepsy is another of the common, serious brain disorders, with a prevalence of just under 1% of the population. If such priming does occur, it is even more important to try to prevent seizures in those who have already suffered an event. Overall, around 60% of people with epilepsy are well controlled (rendered seizure-free) by using a single drug at appropriate therapeutic dose; 70% are well controlled on two drugs; and around 75% on three drugs. Other measures that can be effective at reducing seizure frequency include ensuring sufficient sleep, maintaining a regular routine with regular meals, and avoiding triggers as appropriate, such as flickering lights where photosensitivity has been demonstrated. Some seizures are the result of underlying structural or metabolic disease (see Table 347. Neurosurgery to remove an identified epileptogenic focus (such as may occur with congenital brain malformations) can be extremely effective at reducing the frequency, or even eliminating, seizures in appropriately selected patients. Current first-line anticonvulsant drugs have many fewer long-term side effects than previously used drugs such as phenytoin and phenobarbital, although side effects such as somnolence and mental dulling or weight gain are still reported and undoubtedly influence compliance. Overall, there is no increased risk of seizures in pregnancy, but some women, concerned about the possible teratogenic effects of anticonvulsants, will reduce or stop their medications in pregnancy and thus be at increased risk of seizures. Women need clear advice on the safest and most appropriate anticonvulsants to take during pregnancy and breastfeeding, and should be referred for appropriate specialist advice, ideally prior to conceiving. Another area of epilepsy prevention to consider is that of prophylactic use of anticonvulsants following head trauma or in relation to brain surgery. Factors that increase the risk of a seizure following head injury include the severity of the injury, whether there is depression of a skull fracture, the presence of focal neurological signs and/or intracranial haematoma, and the duration Table 347. Age is a further important factor, with young children having the highest risk of seizures post head trauma, and the risk progressively decreasing throughout life. There is reasonable evidence to support the use of prophylactic anticonvulsant medications for 6 months following severe head injury or brain surgery, but the evidence for prophylaxis decreasing the risk of later post-traumatic seizures is less secure. While these latter diseases are, fortunately, quite rare, they cause huge suffering to individuals, carers, and families; thus, any interventions that might reduce their incidence would be highly valuable. Some of the theories proposed to account for the increasing incidence of these disorders with age include decreased mitochondrial efficiency and function, increased cellular oxidative stress with decreased repair mechanisms, and the impairment of pathways of autophagy and protein turnover. Epidemiological studies have identified environmental risk factors for the disease (see Box 347. One theory relates to the fact that nicotine can stimulate postsynaptic dopamine receptors and so protect against their downregulation. The prevalence increases exponentially with age from 65 onwards, such that between 5% and 10% of people aged between 65 and 74 years are affected, rising to between 30% and 40% of the population aged over 85 years. The key features of memory loss, personality decline, and cognitive decline progress over years such that, by the advanced stages of the disease, individuals can no longer recognize close family and friends, are mute, incontinent, and cachectic, and may suffer seizures. Some of these factors, confirmed in large, prospective studies, are listed in Box 347. The key to successful treatment in bacterial meningitis is to recognize the symptoms. Cerebral malaria, caused by the plasmodium falciparum parasite, is one of the most serious forms of malaria, with about a fifth of cases being fatal, and young children being particularly susceptible to severe infection. Of those who survive the acute illness, around 10% will have severe sequelae, such as hemiplegia, ataxia, seizures, or cognitive impairment. Preventive strategies against infection include the use of insecticide-treated mosquito nets, and indoor spraying of insecticide in endemic areas.
Best buy kytril
The rash preferentially affects the trunk in most cases and occurs on the palms and soles in around half of infections symptoms gerd order 2mg kytril otc. The primary lesion may not have healed by the time secondary syphilis symptoms develop, and the two may be present simultaneously. There are multiple other potential, less common, but clinically significant presentations of secondary syphilis; these are summarized in Table 313. Other diseases that should be considered Syphilis can present very non-specifically and can resemble multiple other pathologies. In general, any systemic vasculitic process should be considered in the differential diagnosis. Certain manifestations of secondary syphilis can be sampled for microscopy, such as condylomata lata (wart-like genital lesions) and mucous patches. As dark-field microscopy requires an experienced clinician and microscopist, its general application is limited. The majority of syphilis diagnoses are made via interpretation of a combination of serological investigations, which include specific treponemal antibody/antigen tests. Common test results corresponding to stages of infection are summarized in Table 313. Complications of the disease Tertiary stage syphilis is the result of untreated, long-standing infection. Pre-antibiotic-era studies suggest that 40% of untreated individuals will advance to tertiary stage infection. If the tertiary stage occurs, it can present anywhere from 2 to 15 years after the initial infection. Treatment and its effectiveness the mainstay of treatment is parenteral penicillin, given for a sufficiently long period to cover the slow replication time of T. Other agents such as cephalosporins and tetracyclines have also been shown to be effective. National guidelines for the treatment of syphilis exist, and an expert opinion should also be sought prior to initiating treatment. Syphilis: Review with emphasis on clinical, epidemiologic, and some biologic features. If treatment is delayed for several years, disabling and life-threatening complications can result; therefore, individuals at high risk should undergo regular screening. Rickettsial infections are caused by a variety of obligate intracellular, Gram-negative bacteria from the genera Rickettsia, Orientia, Ehrlichia, and Anaplasma. Rickettsia is further subdivided into the spotted fever group and the typhus group. Bartonella and Coxiella burnetii bacteria are similar to rickettsiae and cause similar diseases. Animals are the predominant reservoir of infection, and transmission to people is usually through ticks, mites, fleas, or lice, during blood-feeding or from scarification of faeces deposited on the skin. Natural history of African tick typhus, and complications, of the disease the mean incubation period is usually 6 days for both infections and, in African tick-bite fever, complications, such as reactive arthritis, are rare. Approach to diagnosing African tick typhus African tick typhus should be considered in any febrile traveller returning from sub-Saharan Africa, particularly when an eschar, lymphadenitis, or rash is present. There has been considerable overlap historically between the two, but it is now well recognized that they are distinct diseases, with different epidemiology, bacteriology, and disease presentations. Other diagnoses that should be considered aside from African tick typhus Common infections in febrile returning travellers must be considered, particularly malaria (which does not cause a rash or lymphadenopathy), typhoid, other rickettsioses, and meningococcal disease. A risk assessment should also be undertaken for the possibility of a viral haemorrhagic fever. Diagnostic antibody titres are often only seen in convalescent samples and may not appear in those treated early with appropriate antibiotics. Aetiology of African tick typhus African tick-bite fever is caused by Rickettsia africae and is transmitted by hard ticks (Amblyomma spp. The ticks act as both vectors and reservoirs of the disease, and humans are accidental hosts. Cell culture can also be performed from clinical specimens but has several limitations and is not routinely undertaken. Typical symptoms of African tick typhus, and less common symptoms the majority of patients with African tick typhus present with features common to most rickettsial infections, including fever, severe headache, and malaise. In addition, in African tick-bite fever there is often prominent neck muscle myalgia, regional lymphadenitis (43%), and multiple eschars (49%). Other relevant investigations for African tick typhus In African tick typhus, elevated levels of C-reactive protein and liver enzymes are often seen in combination with mild thrombocytopenia and lymphopenia. Treatment of African tick typhus, and its effectiveness the treatment of African tick typhus should be based on clinical suspicion and should not be delayed for confirmatory serology. The tetracycline class of antibiotics is most commonly utilized, with a high degree of efficacy and minimal toxicity. Demographics of African tick typhus Epidemiological data suggest that Rickettsia africae exists widely throughout sub-Saharan Africa and the eastern Caribbean. It is the most widespread and commonest of the pathogenic spotted fever group of rickettsiae. It is thought that most rural indigenous populations are infected in childhood with mild clinical disease. However, it is increasingly reported amongst travellers to endemic areas, and seroprevalence studies in travellers have shown incidence rates of up to 5%. In Africa, Rickettsia conorii occurs mainly in Algeria, Morocco, Egypt, and Libya, but has also been isolated in countries such as Kenya, Zimbabwe, and South Africa. It is a zoonosis caused by the Gram-negative intracellular coccobacillus Coxiella burnetii. Its diagnosis can be difficult, due to the variety of clinical presentations, and the delay involved in serological confirmation. A wide variety of ticks, birds, rodents, and wild mammals can be infected, but domestic ruminants (sheep, cattle, and goats) are the most frequent sources of human infection. Aerosols are the major route of transmission to humans, either from direct exposure to infected tissues or from indirect exposure through contaminated dust. Phase I IgG of 1:800 at 6 months is considered diagnostic of chronic infection and is one of the major modified Duke criteria for endocarditis. Other diagnostic methods for Q fever Culture for Q fever is not routine, and requires Biosafety Level 3 laboratories, but is available from specialist laboratories. Typical symptoms of Q fever, and less common symptoms the most typical manifestation of Q fever is an undifferentiated febrile illness similar to influenza, but other common presentations include atypical pneumonia and hepatitis. The hepatitis is usually asymptomatic; however, patients with only mild biochemical abnormalities may have significant histological changes, and hepatic coma and death has been reported. Neurological symptoms are recognized in 4%-22% of all Q fever cases, with meningoencephalitis, meningitis, and myelitis being the most common neurological presentations. Other relevant investigations for Q fever All patients with confirmed Q fever should have a transthoracic echocardiogram, but it is recognized that cardiac vegetations are evident in only 12% of patients with chronic infection. Repeat serological testing looking for evidence of progression to chronic infection should be undertaken. Prognosis for Q fever Death is rare in acute infection and, with effective antibiotic therapy for endocarditis, mortality is less than 10%. However, relapse rates of over 50% after cessation of antibiotic therapy can occur, and delay in diagnosis has an important effect on the prognosis of chronic Q fever. Q fever is associated with certain risk occupations, including farming, working in an abattoir, and meat packing, but, frequently, there is no history of obvious exposure. Pregnancy, valvular heart disease, and immunosuppression are factors associated with more severe disease and progression to chronic infection. Co-trimoxazole is used in women who are pregnant or breast feeding, and in children under 12.
Diseases
- EPP (erythropoietic protoporphyria)
- Hairy palms and soles
- Keratosis follicularis spinulosa decalvans
- Tyrosinemia
- Chromosome 13q-mosaicism
- Chromosome 10, monosomy 10p
- Peters congenital glaucoma
- Warm-reacting-antibody hemolytic anemia
Buy kytril 1mg cheap
Other single-gene defects are even rarer medications medicaid covers buy 1 mg kytril visa, with only few reported cases for some conditions. Reprinted from Journal of Allergy and Clinical Immunology, volume 124, issue 6, Notarangelo et al, Primary immunodeficiencies: 2009 update, pp. Other sites of infection include the skin, the joints, the gastrointestinal tract, and the urinary tract. However, enteroviral meningoencephalitis has been reported in patients with X-linked agammaglobulinaemia. The current practice of maintaining a higher-trough IgG level has significantly reduced the incidence of this complication. Other non-infectious complications include polyclonal lymphocytic infiltration, frank lymphoma, enteropathy, and liver abnormalities. Treatment and its effectiveness the mainstay of treatment for primary antibody deficiency is replacement immunoglobulin therapy, along with judicious use of antibiotics for the treatment of acute infections as well as for prophylaxis in individual patients. Currently, immunoglobulin replacement can be achieved effectively either intravenously or subcutaneously. Both methods have been shown to be safe and efficacious in decreasing the incidence and severity of infections in patients with antibody deficiencies. Prognosis and how to estimate it Treatment of patients with antibody deficiency syndromes with replacement immunoglobulin therapy and aggressive antibiotic treatment significantly improves the prognosis, with a reduction in the number of infection episodes and infection-related complications, such as the development or progression of bronchiectasis. This, however, does not alter the natural course of the condition or the development of non-infectious complications. Infection outcomes in patients with common variable immunodeficiency disorders: Relationship to immunoglobulin therapy over 22 years. Defective T-cell function is associated with chronic intestinal and biliary colonization with Cryptosporidium spp. The lack of lymph node germinal centres due to defective interaction between T-cells and B-cells is a characteristic histological feature. These comprise mutations in genes encoding for purine pathway enzymes, and a range of molecules involved in signal transduction, including tyrosine kinases, cytokine receptors, and key cell surface receptors. Typically, patients have elevated serum IgM levels, accompanied by reduced IgG and IgA, due to a failure to switch from IgM to other classes of immunoglobulin when mounting a secondary immune response against pathogens. This figure is likely to be higher in those populations with a high degree of consanguineous marriages. The preponderance of genes encoding important immunological functions on the X-chromosome leads to a predominance of affected boys. Very rarely, intestinal lymphangiectasia may be associated with T-cell lymphopenia and a low serum IgG as a direct consequence of loss of IgG and efflux of lymphocytes via aberrant lymphatic channels. Clinically significant drug-induced combined T-cell and B-cell defects may occur in some patients who have received chemotherapy for cancer or immunosuppressive therapy for autoimmune disease. Drugs responsible for such iatrogenic immune defects include corticosteroids, cyclophosphamide, fludarabine, methotrexate, azathioprine, mycophenolate mofetil, and ciclosporin. Where significant drug-induced immune deficiency associated with T-cell and B-cell defects does develop, they do not usually pose a diagnostic challenge because of the clinical context in which immunodeficiency develops. Essentials of Clinical Immunology, Sixth edition, Helen Chapel, Maneel Haeney, Siraj Misbah and Neil Snowden. However, precise molecular diagnosis is essential for purposes of genetic counselling, prenatal diagnosis, assessing prognosis, and, in the future, using gene therapy. Acceptable diagnostic alternatives to the gold standard In view of the ease with which serum immunoglobulins and circulating lymphocytes can be measured, there is little need for alternative surrogate tests of T-cell and B-cell function. In a resource-limited setting where access to flow cytometry may be limited, the finding of an absolute lymphopenia would be highly indicative of T-cell lymphopenia, since T-cells constitute approximately 70% of the circulating lymphocyte count. Similarly, the absence of a thymic shadow on a chest X-ray would point to a T-cell defect, but its utility as a diagnostic marker is limited by the occurrence of thymic atrophy in acutely ill babies. In pursuing this diagnosis, it is essential to obtain evidence of combined T-cell and B-cell dysfunction, as evidenced by the presence of T-cell lymphopenia, impaired lymphocyte proliferation, and hypogammaglobulinaemia. Measurement of serum immunoglobulins and specific antibodies serve as markers of B-cell function. While the circulating lymphocyte surface marker profile provides useful clues as to the underlying molecular defect, definitive diagnosis requires sequencing of the relevant gene to identify disease-causing mutations. Imaging of the chest followed by bronchoalveolar lavage, where possible, is important to explore the possibility of pneumocystis infection. The mortality in the remainder of cases has been due to severe infection, with reactivated cryptosporidial disease being a particular problem. The main physiological functions of the complement system include defence against pyogenic bacterial infections, clearance of immune complexes and products of inflammatory damage, and acting as a bridge between the innate and adaptive immune system (see Table 299. The complement system is regulated by various complement inhibitors (regulatory proteins) that are present in both the classical pathway and the alternate pathway and which regulate and prevent spontaneous activation of the complement system, thereby preventing complement-mediated damage to tissues under normal circumstances. Acquired complement deficiency may occur as a consequence of autoantibody-mediated inhibition of complement proteins, as evidenced by anti-C1-inhibitor and acquired angioedema and anti-C3 nephritic factor and mesangiocapillary glomerulonephritis. Inherited defects affecting the inhibitors or regulatory proteins of the complement system, namely C1-inhibitor and factors H and I, have also been described. C1-inhibitor deficiency is the most well characterized; it is inherited in an autosomal dominant manner and is associated with hereditary angioedema. Mutations in the gene coding for C1-inhibitor result in either an absent or a non-functional protein. C1-inhibitor deficiency may be acquired secondary to a range of lymphoproliferative conditions, including chronic lymphocytic leukaemia and multiple myeloma. In addition to disease-causing mutations, genetic polymorphisms have been described for many complement components. Typical symptoms of the disease, and less common ones Recurrent infections Patients with inherited complement defects have an increased susceptibility to pyogenic infections. Properdin deficiency and defects in the components of the terminal lytic pathway are particularly associated with an increased susceptibility to neisserial infections, indicating the importance of the cytolytic property of the terminal membrane attack complex in host defence against Neisseria. Aetiology of the disease Genetic defects are described for nearly all the components of the complement system. Most of the defects in the classical complement pathway are inherited as autosomal recessive traits. Natural history and complications of the disease Natural history of infections in complement disorders, and their complications the most common presentation of patients with complement deficiencies is an increased susceptibility to recurrent infections by encapsulated bacteria, particularly Neisseria meningitides (Table 299. Homozygous C3 deficiency is also associated with increased susceptibility to Streptococcus pneumoniae and Haemophilus influenza sino-pulmonary infections and meningitis. While the majority of the infections occur in childhood, there is a reduction in frequency and severity of infections as the adaptive immune response matures. Bridge between innate and adaptive Complement antibody responses Enhance immunological memory Waste disposal Clearance of immune complexes and apoptotic cells C1q Covalently bound fragments of C3 C3b and C4b C3 receptors on B-cells C3 receptors on antigen-presenting cells of these components in clearing immune complexes and apoptotic debris. Deficiency of C1-inhibitor leads to inappropriate generation of bradykinin, with resultant increased vascular permeability. Patients with C1-complex or C4 deficiency present early in life, and both sexes may be equally affected. Factor H deficiency is also associated with membranoproliferative glomerulonephritis or dense deposition disease, predominantly in children. Demographics of the disease Defects and deficiencies of complement components are rare, but are being increasingly recognized and reported. Homozygous C3 deficiency is a rare autosomal recessive disease which is associated with recurrent bacterial infections and defects in adaptive immune responses. Approximately 1 in 10 000 individuals are reported to be deficient in one of the terminal complement components, but geographical and ethnic differences in prevalence and incidence have been noted. Properdin deficiency is the most common defect associated with the alternative pathway and is transmitted as an X-linked recessive condition. Hereditary angioedema due to C1-inhibitor deficiency is the beststudied inherited defect of complement regulators. The prevalence is Recurrent pyogenic infections Neisserial infections Note: All of the above disorders may present either in children or in adults. Individuals with early complement defects, however, do not have an increased risk of development of any other systemic or organ-specific autoimmune disease. Acceptable diagnostic alternatives A working diagnosis of complement defects may be established using the clinical history supported by appropriate functional assays, but definitive testing requires referral to a specialist complement laboratory.
Cost of kytril
These techniques provide a way to identify premature disease and to track the progression of disease and the impact of therapy medicine 5 rights discount kytril 1 mg overnight delivery. This score is a strong predictor of coronary heart disease events and overall mortality, providing predictive information beyond that of standard risk factors across different racial and age groups. It correlates with the presence of coronary atherosclerosis and represents an independent risk factor for coronary events as well as stroke and transient ischaemic attacks. It is an independent predictor of cardiovascular events: when reductions in left ventricular mass result from antihypertensive therapy, they are associated with reductions in cardiovascular events, independently of blood pressure reduction. For stroke and thromboembolism, prevention can be primary (to reduce risk of first stroke) or secondary (preventing recurrent strokes). On the other hand, in the primary prevention of stroke, the three drugs showed some differences in relation to efficacy and bleeding. Thus, it is critical to clarify the level of prevention when considering the impact of different screening and prevention strategies. The area in bold represents people with symptoms of non-anginal chest pain, who would not be investigated for stable angina routinely. Asymptomatic left ventricular dysfunction Asymptomatic left ventricular dysfunction progresses to symptomatic heart failure at rates of up to 10% per year, if untreated. Therefore, early detection, if achievable, is important because randomized trials have shown that appropriate drug therapy can significantly improve survival and cardiovascular outcomes. Because the signs and symptoms of heart failure are so non-specific, many patients who have suspected heart failure and are 1200 referred for echocardiography are not found to have an important cardiac abnormality. A normal natriuretic peptide level has a high specificity; that is, in an untreated patient, it virtually excludes significant cardiac disease, removing the need for echocardiography. Community-based studies have highlighted the high prevalence of heart failure (both systolic and diastolic) in patients with risk factors for cardiovascular disease. However, at present, further trials of targeted echocardiography are required before widespread echocardiographic screening is advocated. Currently, screening strategies have tended to focus on risk factors rather than established disease, due to many factors, including resource constraints, lack of prospective evidence, and sociocultural factors. In addition, the body of randomized evidence in diagnostic and prognostic studies has lagged behind the exponential growth of trials in the therapeutic arena. Given the importance of screening in both high-risk and population approaches to the prevention of cardiovascular disease, more research is urgently needed. Developed in collaboration with American Society of Echocardiography, American Society of Nuclear Cardiology, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. American Heart Association Guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Cardiovascular Disease: Risk Assessment and Reduction, Including Lipid Modification. Summary In this chapter, we have focused on screening for cardiovascular disease via risk factors, surrogate markers, and detecting established disease. While screening has the potential to improve quality of life through early diagnosis and management, it is not an easy process and cannot offer a guarantee of protection. Cystic fibrosis Neonatal screening has helped early diagnosis of cystic fibrosis before any symptoms may have developed and there is evidence to suggest screening provides better pulmonary outcomes. Screening helps affected parents to have genetic counselling to avoid the birth of a second child with cystic fibrosis in a family where the first child may have been undiagnosed. These can lead to long-term psychosocial consequences for the families involved in the screening until further diagnostic testing is done. Carrier screening looking for mutation analysis is available for those who have a relative known to have cystic fibrosis and a relative or a partner known to be a carrier of cystic fibrosis. Prenatal screening trials have been done in the past using different approaches in hospital and primary care settings. Stepwise screening and couple screening methods have been used, with the former first testing the pregnant woman and then only testing her partner if she is found to be a carrier. There is now evidence to suggest that prenatal screening of at-risk couples identified by the newborn screening programme has resulted in a reduction in the live-birth prevalence of cystic fibrosis. Patients should be identified from port of arrival reports, registration with primary care, entry to education, and links with voluntary groups. The main drawbacks of lung cancer screening trials are lack of control for occupational exposures and family history, possible bias from the screening of healthy individuals, and the lack of completely unscreened control groups. This can sometimes lead to over-diagnosis and to patients having to deal with the psychological issues arising from stress and anxiety. The best way of control is preventing the spread from smear-positive cases, and screening contacts. More than 50 000 patients have been enrolled and the results will not be available until later this year. This study has also tried to address some important issues, such as all causes of death in groups screened for lung cancer, the cost-effectiveness of screening, the quality of life for those who test positive, and the influence of screening on smoking behaviour and beliefs. The identification of biomarkers has led to a greater understanding of the molecular pathways of lung cancer. However, despite extensive studies thus far, few have turned out to be useful and, even those used do not show enough sensitivity, specificity, and reproducibility for general use. Recognition of alpha-1 antitrypsin deficiency can prompt specific interventions such as genetic counselling, screening of family members, smoking cessation advice, and consideration of augmentation therapy. Evidence from previous studies suggests that targeted detection has generally produced a higher rate of detecting disease than large-scale population-based screening has. In the future, improved awareness campaigns and easy and cheaper sampling techniques may improve the detection rates, resulting in better treatment options such as augmentation therapy, which may well help preserve lung function in asymptomatic individuals. Individuals can still end up transmitting the mutations to their children but may never acquire the disease due to variable penetrance. One way of screening would be to do genetic testing and counselling of these individuals, with detailed explanation of the limitations and risks involved. Echocardiography should always be performed in cases of suspected pulmonary hypertension. Pulmonary hypertension is defined as a mean pulmonary arterial pressure 25 mm Hg on Doppler measurements but these values can be inaccurate in some individuals. Underestimation of pulmonary hypertension can happen in patients with severe tricuspid regurgitation, and overestimation by >10 mm Hg is also common; hence, Doppler echo is not ideal for screening asymptomatic or patients with mild pulmonary hypertension. Screening and early detection for those with mild or moderate airflow obstruction could benefit from smoking cessation advice and annual influenza vaccination. Pharmacological therapy to these individuals may help prevent exacerbations but may not change hospitalization rates in those with severe disease. It is not known whether pharmacological therapy in patients who are asymptomatic but meet spirometric criteria for moderate-to-severe disease would have the same benefit as in those who are symptomatic with severe airflow obstruction. There is a risk of false-positive diagnosis in those over 70 years of age, due to the natural decline of lung function. Although influenza vaccination may reduce exacerbations, there is not much evidence to indicate that spirometry screening improves influenza vaccination rates or promotes smoking cessation. It should also aim to improve exercise tolerance and health status and provide a reduction in mortality. Contrast echocardiography or V/Q scanning could also be used as first-line screening in patients with a high index of suspicion. Abnormal pulmonary artery pressure response in asymptomatic carriers of primary pulmonary hypertension gene. Tuberculosis: Clinical Diagnosis and Management of Tuberculosis, and Measures for its Prevention and Control. American Thoracic Society/ European Respiratory Society Statement: Standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Renal disease is common and, with routine reporting of estimated glomerular filtration rates, impairment of renal function is increasingly being recognized. Screening for kidney disease should include a serum creatinine measurement and, in most circumstances, a urine dipstick.
Generic kytril 2mg
In contrast medications beginning with z discount kytril 2mg mastercard, vascular injuries in term infants more often affect the territory of the middle cerebral artery. Congenital malformations, growth retardation, maternal hypotension, infection, thyroid disease, and exposure to toxins are part of a long list of prenatal, gestational risk factors. Even in these cases, the clinical deficit may not become apparent until much later in development. Spastic cerebral palsy is further subdivided on the basis of the affected body regions into diplegic (affecting both legs, usually with lesser involvement of the arms), hemiplegic, and quadriplegic types. In premature infants, spastic diplegia is often a result of periventricular leukomalacia or haemorrhage. Dyskinetic cerebral palsy is characterized by choreoathetoid movements, but combinations of dystonia, myoclonus, tremor, and hemiballismus can also be seen. Historically, kernicterus (neonatal hyperbilirubinaemia) was the most frequent cause. The adult physician most usually encounters cerebral palsy in the context of an acute or subacute deterioration in functioning on the background of prior clinical stability. The challenge is then to identify and appropriately treat the cause of this deterioration. First, intercurrent infections or metabolic disturbances can more profoundly affect patients with preexisting brain pathology than might otherwise be the case and, in this context, apparent new focal deficits can sometimes be seen. Second, like the wider population, cerebral palsy patients remain at risk of developing further neurological disease such as strokes, infective encephalitis, or even neurodegenerative pathology, and are at an increased risk of seizures. Finally, the label of cerebral palsy may be erroneous, and the patient instead suffers from a different, progressive pathology. Nevertheless, the priority of the acute medical team lies with assessing the first and second possibilities. Chiari malformations Chiari malformations are congenital abnormalities of the anatomy and structural relationships of the cerebellum, brainstem, and foramen magnum. In contrast, Chiari I malformations are by far the most common and least severe defects, and are often diagnosed in adult life. The key abnormality here is displacement of the cerebellar tonsils below the level of the foramen magnum. Commonly, this is an incidental and unexpected finding but, on other occasions, symptomatic Chiari I malformations require surgical treatment. The adult physician therefore needs to be familiar with the neurological signs and symptoms which may result from a Chiari I malformation. Herniation of the tonsils can compress the cerebellar structures themselves (resulting in dysmetria, ataxia, and other cerebellar signs and symptoms). The tonsils can additionally compress the cervicomedullary junction in the foramen magnum (giving lower cranial nerve dysfunction and/ or upper cervical myelopathy). When these symptoms can be correlated with the imaging abnormalities, surgical decompression is indicated, and can result in resolution of any associated syrinx. Surgical intervention is not warranted outwith this context or for the treatment of non-cough-impulse headaches or neck pain. As such, the diagnosis is usually made in infants who have signs and symptoms of brainstem dysfunction. Dysraphism (spina bifida) Dysraphism is a failure of opposition of anatomical structures which are normally fused. Spinal dysraphism is synonymous with spina bifida, a failure of embryological fusion of the neural tube. There is an association with maternal folate deficiency, pregestational diabetes, antiepileptic drug exposure (particularly sodium valproate), and certain chromosomal abnormalities. Complications arise from shunt obstruction, shunt infection, renal impairment, and urinary tract infections secondary to the neurogenic bladder, and from the long-term effects of reduced lower limb function, such as contractures and pressure sores. Spina bifida oculta Spina bifida oculta is usually an incidental and asymptomatic finding, and is likely to be very common. Although there is a defect in the vertebral arch, the meninges and neural tissue remain in the spinal canal. Tethered cord syndromes the tethered cord syndromes involve a restriction of the normal cephalad migration of the conus during life. Combinations of upper and lower motor neuron signs, sensory disturbance in the legs, sphincter dysfunction, and scoliosis are found. A tethered cord is a contraindication to lumbar puncture, while spina bifida oculta itself is not, and may make the procedure easier. Spina bifida cystica Spina bifida cystica involves protrusion of the meningeal sac through the vertebral defect. If the sac contains part of the spinal cord or roots it is termed a myelomeningocele. Discounting spina bifida occulta, myelomeningocele is by far the most common type of spina bifida and, indeed, the most common major birth defect. With neurological involvement, the level of the defect generally relates to the resultant level of impairment. Spina bifida cystica is treated with early neurosurgical closure to prevent infection and significantly improve survival. Existing myelopathic and radiculopathic symptoms are likely to persist, with varying degrees of lower limb paralysis and sensory loss. If hydrocephalus is present, shunting allows the development of normal intelligence. A seizure can be defined as a transient excessive discharge of nerve cells within the brain, causing an event which is discernible to the person experiencing the seizure or to an observer. The seizures are usually brief but frequently cause injury due to the sudden falls. Symptoms the symptoms of epilepsy vary according to the extent of the seizure activity, and the site of onset of the seizure. Generalized seizures involve the rapid engagement of bilaterally distributed networks of seizure activity. Focal (partial) seizures Focal (partial) seizures have their onset in a localized area of cerebral cortex, although they may spread to involve the rest of the cerebral cortex. Focal seizures without loss of awareness were previously termed simple partial seizures. They generally reflect the function of the area in which they arise; thus, occipital seizures commonly take the form of visual hallucinations. Focal dyscognitive (complex partial) seizures occur when the seizure discharge spreads further such that loss of awareness occurs. They commonly (but not exclusively) arise in the temporal lobes, and may be characterized by a motionless stare, lip smacking or chewing, fiddling, rubbing, and undressing or wandering. Focal seizures may progress further to become bilateral convulsive (secondarily generalized) seizures. A postictal phase follows, with headache, drowsiness, and confusion being common symptoms. The patient abruptly appears blank, as if in a trance, usually for around 10 seconds.
Order kytril paypal
Non-capsulate strains of Haemophilus influenzae are a commonly recognized cause of both pneumonia and acute exacerbations of chronic obstructive pulmonary disease treatment ear infection cheap 2mg kytril. The Hib vaccine was the first where the capsular polysaccharide, extracted from Hib cultures, was conjugated to a carrier protein molecule to increase the immunogenicity particularly in young children. In the previous 3 years, there had been approximately 900 cases reported of invasive Hib disease in England and Wales. Due to the production of beta-lactamase by many strains of Haemophilus influenzae, antibiotic therapy is usually with co-amoxiclav or a cephalosporin. Neisseria species Neisseria are Gram-negative cocci that have a characteristic paired arrangement that resembles coffee beans. Numerous species exist of which two are important human pathogens: Neisseria meningitidis and Neisseria gonorrhoeae. Antibiotic culture media for the recovery of Neisseria meningitidis and Neisseria gonorrhoeae are made selective by the use of an antibiotic cocktail to aid recovery from mixed throat and genital tract flora. The organisms are then identified by Gram stain, a positive oxidase test, and by at least two of the following modes of identification: utilization of sugars, detection of specific preformed enzymes, or immunological tests. Gonorrhoea is a sexually transmitted infection primarily of the mucous membranes of the urethra, the endocervix, the rectum, the pharynx, and the conjunctiva. Common symptoms include urethral and/or cervical discharge and dysuria, but infection may be asymptomatic in up to 50% of cases. Complications include epididymitis, pelvic inflammatory disease, and haematogenous spread. In addition to routine microscopy and culture methods, molecular amplification techniques are increasingly being used for the detection of Neisseria gonorrhoeae. As resistance profiles continue to change over time, these are a key part of the management of both the individual patient and his or her contacts, and the maintenance of up-to-date local and national treatment guidelines. Meningococcal infection most commonly presents as either meningitis or septicaemia or a combination of both. Disease usually occurs from 2 to 7 days after acquisition of the organism in the nasopharynx. However, approximately 10% of adults, and a higher proportion of adolescents, carry meningococci without developing disease. When disease occurs, there may be a prodrome, but the disease is often acute with symptoms that include pyrexia, malaise, headache, neck stiffness, photophobia, and vomiting. A petechial or purpuric non-blanching rash may accompany meningococcal Bacterial enteric pathogens Acute infectious diarrhoea may be caused by any one of a number of bacterial pathogens. Each one requires a somewhat different culture technique to recover it from a faecal sample, making the routine microbiological investigation of this common syndrome both complex and expensive. Nevertheless, the importance of understanding the cause of acute infectious diarrhoea both for the patient and for epidemiological purposes justifies routine investigation. The common species that cause human gastrointestinal infection are Campylobacter jejuni and Campylobacter coli. These pathogens cause acute diarrhoea which is often associated with severe abdominal pain and malaise. However, the infective dose is small, and transmission to humans usually occurs from undercooked poultry or unpasteurized milk. There is an unexplained seasonality associated with Campylobacter infection, with a peak incidence in late spring. Salmonella species (other than Salmonella typhi and Salmonella paratyphi) cause gastrointestinal infection via the consumption of contaminated food. As Salmonella bacteria colonize the gastrointestinal tracts of many farm animals, food contamination can occur in uncooked or undercooked meat, poultry, eggs, and unpasteurized milk. In addition, contamination of green vegetables and fruit can occur on the farm, and contamination of shellfish can occur from the contamination of seawater with sewage. Salmonella are sought by examination of faecal samples for non-lactose fermenting coliforms on selective agar plates. Faecal samples are also enriched by using a specialized broth and then subculture, to ensure any small numbers of Salmonella bacteria present are recovered. Salmonella species are identified using serological tests to confirm the antigenic structure of the capsule and flagellae. The most commonly isolated serospecies are Salmonella enteritidis and Salmonella typhimurium. Many other serospecies are known, often bearing the name of the place where that strain was first identified. Some less common species can be acquired from the gastrointestinal tracts of reptiles kept as pets. Infants, the elderly, and the immunosuppressed are at greater risk of more serious infection. The four species of Shigella responsible for bacillary dysentery are Shigella dysenteriae, Shigella flexneri, Shigella boydii, and Shigella sonnei. All are non-lactose fermenting and are sought from faecal samples in much the same way as Salmonella spp. The inoculum required for infection with these organisms is small compared to that for other enteric pathogens. Infection is associated with contaminated milk, contaminated water, undercooked minced beef, and undercooked beef burgers. Prostatic enlargement in older men may cause obstruction of the urinary tract, thereby increasing the risk of infection. Urinary tract infection is confirmed by a combination of microscopy and semi-quantitative culture. Laboratory microscopy is now frequently undertaken by an automated system, either one based on flow cytometry or one based on high-speed microphotography with image recognition. The key elements reported are white blood cells, red blood cells, epithelial cells, and casts. This will not be reported but, together with the cell counts, may aid the laboratory in determining the chance of bacterial growth being found on culture and, therefore, the utility of performing a full culture. Semi-quantitative culture usually relies on the use of a calibrated bacteriological loop. It must be remembered, however, that, with suprapubic aspirates or other surgically obtained urine samples, a pure growth of 104 colony-forming units/ml may be clinically significant. It is not necessary to send a urine specimen to the laboratory from every patient. Non-pregnant women who are between teenage years and menopause and who have urinary tract infection symptoms. The four principal analytes are nitrite (bacteria reduce dietary nitrates to nitrites), leucocyte esterase (an enzyme present in white blood cells), protein, and blood. While these tests have very low sensitivity and specificity individually, the negative predictive value of an overall negative test. The ability of the multitest dipstick to predict a positive culture result is lower. However, in premenopausal non-pregnant women with clear symptoms of urinary tract infection, the positive dipstick test can be seen as confirmation of infection and empirical antibiotic therapy can be started. Urinary tract infection occurring in pregnant women, children, men, or the elderly, or one that either recurs or ascends to the upper tract, should be considered complicated. Infection of the upper tract produces symptoms such as fever, nausea, malaise, or loin pain. All patients with complicated urinary tract infection should have a midstream urine sample sent for microscopy, culture, and sensitivity, and treatment should be based on the results. In general, treatment of complicated urinary tract infection should be for 7 days.