Purchase 100 mg udenafil free shipping
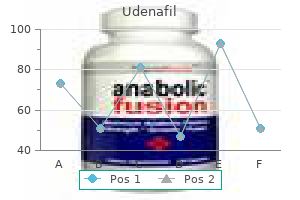
Whether cerebral autoregulation is impaired in the elderly is still debatable (see Chapter 65) impotence exercises for men purchase 100 mg udenafil free shipping. Nausea and vomiting may be associated with neuraxial block in as much as 20% of patients and they are primarily related to gastrointestinal hyperperistalsis caused by unopposed parasympathetic (vagal) activity. However rare, respiratory arrest associated with spinal anesthesia is often unrelated to phrenic or inspiratory dysfunction but rather to hypoperfusion of the respiratory centers in the brainstem. Supportive evidence for this concept is observed after resuscitation, when apnea almost always disappears as soon as pharmacologic and intravascular fluid therapies have restored cardiac output and arterial blood pressure. For example, in orthopedic patients undergoing hip replacement, bladder catheterization was no more frequent after spinal or epidural anesthesia than it was after general anesthesia and opioid analgesics. In any case, excessive volumes of intravenous crystalloid solutions should not be given to patients undergoing spinal anesthesia. The requirement for voiding before discharge in low-risk ambulatory surgery patients after short-acting spinal or epidural anesthetics should be encouraged. The use of intrathecal and/or epidural opioids either alone or in combination with local anesthetics can provide excellent quality pain relief65,66,66a and are an analgesic mainstay in labor and delivery,67,68 during and after hip69 or knee replacement,70 in laparotomy,71 in thoracotomy,72 and increasingly even in cardiac surgery. Indications At the most basic level, neuraxial blockade is indicated when the surgical procedure can be accomplished with a sensory level of anesthesia that does not produce adverse patient outcomes. The level of anesthesia or analgesia required is of prime importance because the physiologic effects of a high-level block may be untenable. Some of the most important include patient refusal, localized sepsis, and an allergy to any of the drugs planned for administration. Spinal anesthesia is most commonly used for patients who require surgical anesthesia for procedures of known duration that involve the lower extremities, perineum, pelvic girdle, or lower abdomen. Descriptions of spinal anesthesia as the primary surgical anesthetic have more recently expanded to include lumbar spine surgery,61 as well as upper abdominal procedures, such as laparoscopic cholecystectomy. Epidural anesthesia can also be used for the lower extremities, perineum, pelvic girdle, or lower abdomen, but by virtue of intermittent or continuous catheter-based local anesthetic delivery, the duration of surgical anesthesia is not necessarily finite as it is with single-injection spinal anesthesia. Continuous catheter-based spinal anesthesia is both less conventional and less commonly used than either single-shot spinal anesthesia or catheter-based epidural anesthesia, but may be especially useful when insertion of an epidural catheter is challenging63 or in the setting of severe cardiac disease when the reliability of a single-shot spinal anesthetic must be combined with more hemodynamically stable incremental dosing. A preexisting neurologic deficit can in theory worsen the extent of any injury in this group of patients (so-called double-crush phenomenon). While many reports suggest central neuraxial techniques may be used safely, there is no definitive evidence. The association between neuraxial techniques and the exacerbation of back pain symptoms is not documented. Patients with spinal stenosis appear to be at increased risk of neurologic complications after neuraxial blockade,81 but the relative contribution of surgical factors and natural history of the spinal pathology itself is unknown. Using a lower mass of local anesthetic may in theory reduce the risk if spinal anesthesia is undertaken in the setting of spinal stenosis. Previous spine surgery does not predispose patients to an increased risk of neurologic complications after neuraxial blockade. Depending on the severity of the neural tube defect, patients with spina bifida may have a tethered cord and the ligamentum flavum may be absent, thereby increasing the potential for traumatic needle injury to the spinal cord. Neuraxial techniques have been successfully used in isolated spina bifida occulta patients, but are not advised in the setting of severe neural tube defects such as diastematomyelia or tethered cord. If, after consideration of risks and benefits, a neuraxial technique is to be undertaken in a patient with a neural tube defect, a careful clinical and radiologic evaluation of neurologic status must first be undertaken and noted along with documentation of the discussion of the risks and benefits. The safety of neuraxial techniques in patients with common bleeding diatheses is not well documented. Hemorrhagic complications after neuraxial techniques in patients with known hemophilia, von Willebrand disease, or idiopathic thrombocytopenic purpura appear infrequently when factor levels are more than 0. The unpredictable speed and extent to which systemic vascular resistance is reduced after spinal anesthesia may cause many providers to avoid spinal anesthesia in preloaddependent patients and try to prevent a dangerous decrease in coronary perfusion. This concern is borne of theoretic risk and a great deal of caution rather than evidence. A catheter-based neuraxial anesthetic, whether it is an epidural or intrathecal catheter, allows for the repeated administration of small doses of local anesthetic, with potentially more control over hemodynamic changes, and may be a logical alternative choice. An extension of patients who are preloaddependent, hypovolemic patients may exhibit an exaggerated hypotensive response to the vasodilatory effects of neuraxial blockade. Infection Theoretic concerns based on animal data and laboratory and case reports in humans87-89 suggest iatrogenic seeding of the neuraxis in the setting of a systemic infection. A definitive causative relationship between existing systemic infection and meningitis or epidural abscess after a neuraxial technique has never been shown. In fact, a lumbar puncture is a critical component of the investigation of fever of unknown origin, yet there are no definitive data linking lumbar puncture to increased risk of neuraxial infection in this setting. Yet patients with evidence of systematic infection may safely undergo neuraxial anesthesia once antibiotic therapy has been initiated and the patient has demonstrated a response to the antibiotics. The provider must recall that intraabdominal structures such as the peritoneum (T4), bladder (T10), and uterus (T10) have a spinal segment innervation that may be much more cephalad compared with that of the corresponding skin incision used to operate on these structures. Drug, patient, and procedural factors can all affect the distribution of local anesthetic spread within the intrathecal space, some of which are more clinically relevant than others. Density is defined as the mass per unit volume of solution (g/mL) at a specific temperature. Density may be compared between different substances by calculating the specific gravity, which is the ratio of the density of a solution to the density of water. The spread of hyperbaric solutions is more predictable,93 with less interpatient variability. Dextrose and sterile water are commonly added to render local anesthetic solutions either hyperbaric or hypobaric, respectively. The clinical importance of baricity is the ability to influence the distribution of local anesthetic spread based on gravity. Hyperbaric solutions will preferentially spread to the dependent regions of the spinal canal, whereas hypobaric solutions will spread to nondependent regions. For example, the administration of hyperbaric local anesthetic to patients in the lateral decubitus position will result in a preferential anesthetic effect on the dependent side, whereas the opposite is true for the administration of a hypobaric solution. A thoughtful understanding of the natural curvatures of the vertebral column can help predict local anesthetic spread in patients placed in the horizontal supine position immediately after intrathecal administration. Hyperbaric local anesthetics injected, while sitting, at the L3-L4 or L4-L5 interspace will spread with gravity from the height of the lumbar lordosis down toward the trough of the thoracic kyphosis in the horizontal supine position, resulting in a higher level of anesthetic effect than isobaric or hypobaric solutions. Nevertheless, increasing temperature decreases density of a solution and warming of local anesthetic solution to body temperature, therefore making it more hypobaric, increases the block height in patients who remain seated for several minutes after injection. The choice of local anesthetic itself does not influence spread if all other factors are controlled. However, opioids do seem to increase mean spread,91,99 possibly as a result of pharmacologic enhancement at the extremes of the spread where the local anesthetic block alone would have been subclinical. Within the range of "normal-sized" adults, patient height does not seem to affect the spread of spinal anesthesia. This is likely because the length of the lower limb bones rather than the vertebral column contributes most to adult height. A correlation has been found between the vertebral column length and local anesthetic spread102 and, at extremes of height, consideration should be given to altering the dose accordingly. This has indeed been demonstrated using hypobaric solutions,103,104 which are characterized by more variable spread anyway, but not hyperbaric solutions (see Chapter 58). Although this may affect relative baricity of local anesthetics, the clinical variation in spread is probably unimportant. Further, the nerve roots appear more sensitive to local anesthetic in the aged population. In the lateral position, the broader shoulders of males relative to their hips make the lateral position slightly more head-up. The reverse is true in females who have a slightly head-down tilt in the lateral position compared with males. Despite this, there is little objective data that males have a slightly less cephalad spread than females in the lateral position. Scoliosis, although it possibly makes insertion of the needle more difficult, will have little effect on local anesthetic spread if the patient is turned supine. Kyphosis, however, in a supine patient may affect the spread of a hyperbaric solution.
Purchase 100 mg udenafil with visa
The anterior and deep portion of the cord (gray matter) is most prone to ischemia (leading to anterior horn motor neuron injury erectile dysfunction best pills purchase discount udenafil on line, or anterior spinal syndrome) because there are fewer anterior medullary feeder vessels than posterior feeder vessels. Likewise, the midthoracic part of the spinal cord (from T3 to T9) is most at risk where segmental medullary feeder vessels are rare. Venous drainage of the spinal cord follows a similar distribution as the spinal arteries. There are three longitudinal anterior spinal veins and three posterior spinal veins that communicate with the segmental anterior and posterior radicular veins before draining into the internal vertebral venous plexus in the medial and lateral components of the epidural space. There are no veins in the posterior epidural space except those caudal to the L5-S1 disk. Specifically, Hogan and Toth14,15 have shown that there is considerable interindividual variability in nerve root size. These differences may help to explain the interpatient differences in neuraxial block quality when equivalent techniques are used on seemingly similar patients. Another anatomic relationship may affect neuraxial blocks; although generally larger than the ventral (motor) roots, the dorsal (sensory) roots are often blocked more easily. This apparent paradox is explained by organization of the dorsal roots into component bundles, which creates a much larger surface area on which the local anesthetics act, possibly explaining why larger sensory nerves are blocked more easily than smaller motor nerves. Another study by Hogan18 has also shown in cadavers that the spread of solution after epidural injection into the tissues of the epidural space is nonuniform, and he postulated that this accounts for the clinical unpredictability of epidural drug spread. There is evidence that adipose tissue in the epidural space diminishes with age,19 and this decrease in epidural space in adipose tissue may dominate the age-related changes in epidural dose requirements (see Chapter 65). Mechanism of Action Local anesthetic binding to nerve tissue disrupts nerve transmission, resulting in neural blockade. For spinal and epidural anesthesia, the target binding sites are located within the spinal cord (superficial and deep portions) and on the spinal nerve roots in the subarachnoid and epidural spaces. Nerves in the subarachnoid space are highly accessible and easily anesthetized, even with a small dose of local anesthetic, compared with the extradural nerves, which are often ensheathed by dura mater (the "dural sleeve"). Anatomic studies show that the S1 and L5 posterior roots are the largest and thus most resistant to blockade during epidural anesthesia. For example, the small preganglionic sympathetic fibers (B fibers, 1-3 m, minimally myelinated) are most sensitive to local anesthetic blockade. The A-beta fibers (5-12 m, myelinated), which conduct touch sensation, are the last to be affected among the sensory fibers. The larger A-alpha motor fibers (12-20 m, myelinated) are more resistant than any of the sensory fibers. Regression of blockade ("recovery") follows in the reverse order: motor function followed first by touch, then pinprick, and finally cold sensation. For example, the level of anesthesia to cold sensation (also an approximate level of sympathetic blockade) is most cephalad and is on average one to two spinal segments higher than the level of pinprick anesthesia, which in turn is one to two segments higher than the level of touch anesthesia. This likely facilitates the cephalad distribution of local anesthetic from the lumbar subarachnoid space to the basal cisterns within 1 hour of injection. Drug distribution in the epidural space is more complex, with possible contributions from one, some, or all of the following mechanisms: (1) crossing the dura mater into the subarachnoid space, (2) rostral and caudal (longitudinal) spread within the epidural space, (3) circumferential spread within the epidural space, (4) exit of the epidural space through the intervertebral foramina, (5) binding to epidural fat, and (6) vascular absorption into the epidural vessels. Longitudinal spread of local anesthetic by bulk flow within the epidural space may occur after the administration of a larger dose. Factors that may enhance the distribution of local anesthetic within the epidural space are small caliber (greater spread in the thoracic space), increased epidural space compliance, decreased epidural fat content, decreased local anesthetic leakage through the intervertebral foramina. Finally, the direction of drug spread varies with the vertebral level-that is, epidural spread is mostly cephalad in the lumbar region, caudad after a high thoracic injection, and spread mostly cephalad after a low thoracic njection. The rate of elimination is also dependent on the distribution of local anesthetic; greater spread will expose the drug to a larger area for vascular absorption and thus a shorter duration of action. Physiologic Effects Safe conduct of spinal, epidural, and caudal anesthesia requires an appreciation of their physiologic effects. Neuraxial anesthesia evokes blockade of the sympathetic and somatic (sensory and motor) nervous systems, along with compensatory reflexes and unopposed parasympathetic activity. The decrease in arterial blood pressure is believed to be more gradual and of less magnitude with epidural than with spinal anesthesia of comparable sensory block levels. However, when tetracaine (10 mg) spinal anesthesia was compared with lidocaine (20-25 mL of a 1. Venous and arterial vasodilation reduces preload (venous return) and afterload (systemic vascular resistance), respectively. Because of the large amount of blood that resides in the venous system (approximately 75% of the total blood volume), the venodilation effect predominates, owing to the limited amount of smooth muscle in venules; in contrast, the vascular smooth muscle on the arterial side of the circulation retains a considerable degree of autonomous tone. Cardiac output is thought to be either maintained or slightly decreased during the onset of spinal anesthesia. Yet a biphasic response, characterized by an early transient increase followed by an eventual decrease in cardiac output,30 has been observed. This initial increase is caused by a greater magnitude of decline in the systemic vascular resistance than by venous return, especially in elderly patients with preexisting hypertension and high baseline systemic vascular resistance (also see Chapter 65). The extent of the sympathectomy is typically described as extending for two to six dermatomes above the sensory block level with spinal anesthesia and at the same level with epidural anesthesia. In elderly patients with cardiac disease, systemic vascular resistance may decrease almost 25% after spinal anesthesia, whereas cardiac output decreases only 10%. Heart rate may also decrease in the presence of extensive peripheral sympathectomy (T5-L2), with venous pooling in the lower extremity and the abdominal and pelvic viscera. Although hypotension will trigger a compensatory baroreceptor sympathetic response (vasoconstriction and increased heart rate) above the level of blockade, the reduction in venous return and right atrial filling causes a decrease in signal output from intrinsic chronotropic stretch receptors located in the right atrium and great veins,31 leading to a marked increase in parasympathetic activity (vagal tone). The two opposing responses are usually in check with a minimal change in heart rate (or a slight reduction). However, when neuraxial anesthesia is extended to the T1 level, blockade of the cardioaccelerator fibers in addition to a marked reduction in venous return may result in severe bradycardia and even asystole because of unopposed parasympathetic activity. However rare, the likelihood of cardiac arrest appears to be more likely in young, healthy, and conscious patients. Extraction of oxygen was unchanged because myocardial work, as expressed by myocardial use of oxygen, paralleled the decrease in mean arterial blood pressure and coronary blood flow (16 to 7. Treatment the clinical question of what level of decrease in arterial blood pressure after a neuraxial block is acceptable without a significant decrease in organ perfusion. Once arterial blood pressure decreases to a level at which treatment is believed to be necessary, ephedrine, a mixed adrenergic agonist, provides more appropriate therapy for the noncardiac circulatory sequelae of neuraxial block than does a pure -adrenergic agonist (see Chapter 14), unless the patient has a specific and defined arterial blood pressure requirement. Specifically, 250- to 2000-mL preblock hydration regimens may temporarily increase preload and cardiac output but do not consistently increase arterial blood pressure or prevent hypotension. In a study of elderly patients who had hypotension during bupivacaine spinal anesthesia, Minville and colleagues demonstrated a significant but transient decrease of middle cerebral artery blood flow velocity and an increase in cerebral vascular resistance, both of which suggest a decrease in cerebral perfusion. Procedure Factors Patient position, needle type and alignment, and the level of injection are each procedure-related factors that can affect block height. Combined with the baricity and local anesthetic dose, patient position is the most important factor in determining the block height. When larger hyperbaric doses are administered, however, the block can still extend cephalad despite maintaining the sitting position for a prolonged period of time. With hypobaric solutions, cephalad alignment of the orifice of Whitacre, but not Sprotte, needles produces greater spread. When directing the needle orifice to one side (and using hyperbaric anesthetic), a more marked unilateral block is achieved again when using a Whitacre, rather than a Quincke, needle. Most studies have demonstrated that, even when the difference is only one interspace more cephalad, the block height is greater119-122 when using isobaric bupivacaine. The level of injection does not appear to influence the spread of hyperbaric solutions. Other maneuvers that do not appear to affect block height are coughing and straining after local anesthetic injection. For example, the duration of surgical anesthesia is less than the time for complete block resolution. In addition, surgical anesthesia depends on the surgical site because anesthesia is more prolonged at the lower lumbar and sacral levels than at those more cephalad from where the block regresses first. Duration is affected primarily by the dose,97,125 the intrinsic properties of the local anesthetic (which affect elimination from the subarachnoid space), and the use of additives (if applicable). However, it is not commonly used because of a more frequent failure rate than lidocaine, significantly more nausea, and a slower time to recovery.
Discount 100 mg udenafil fast delivery
Tonicity is important in determining in vivo distribution of fluids across a cell membrane and is sensed by the hypothalamic osmoreceptors jack3d impotence buy udenafil with visa. It can be estimated by subtracting urea and glucose concentrations from measured osmolality. Oncotic Pressure Oncotic pressure is the component of total osmotic pressure that is due to the colloids, that is, large molecular-weight particles, predominantly proteins (albumin, globulins, fibrinogen). Of the total plasma osmotic pressure of 5545 mm Hg, 25 to 28 mm Hg is due to plasma oncotic pressure. The negative charge on proteins has the net effect of retaining a small excess of Na+ ions within the plasma (the Gibbs-Donnan effect), which effectively increases the oncotic pressure above what would be predicted by calculations based purely on protein concentration. As the most abundant plasma protein, albumin is responsible for 65% to 75% of plasma oncotic pressure. This is the fundamental mechanism by which ionic concentration gradients are maintained, which in turn drive a variety of biologic processes, including water and solute movement and electrical impulse transmission in excitable tissues. This process is termed cotransport when the solute is also moving down its concentration gradient or countertransport when the solute is being moved against its concentration gradient. The processes of endocytosis and exocytosis are involved in the transport of large proteins and polypeptides across cell membranes. Cell Membrane the cell membrane separates the intracellular and extracellular compartments and as a lipid bilayer is impermeable to large hydrophilic molecules and charged particles such as free ions. Other than by passive diffusion of certain molecules, solutes may cross cell membranes in several ways. Vascular Endothelium the barrier function of the vascular endothelium is particularly relevant perioperatively because of its key role in maintaining intravascular fluid volume. Surgical tissue trauma typically leads to loss of intravascular volume through surgical blood loss or inflammation-related shifts to other tissue compartments. In the blood-brain barrier, these breaks are small (1 nm) and infrequent (zona occludens tight junctions), permitting passage of only the smallest non-lipid soluble molecules. In other tissues, the breaks are larger (5-8 nm) and more frequent (macula occludens loose junctions). The effective pore size is reduced further to 6 nm by podocytes; thus, proteins not usually filtered. Revised Starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Our understanding of this area has been refined by experimental physiologic models and techniques. The most common capillary type is the nonfenestrated capillary, comprising continuous basement membrane and a single layer of endothelial cells joined by junctions that are punctuated by breaks. In addition to its functions in preventing platelet and leukocyte adhesion, it has emerged as an important semipermeable layer contributing to endothelial barrier function. The movement of fluid across the capillary membrane was initially described by Starling and then further refined. Much of this water was previously thought to be reabsorbed into the vascular space toward the venular end of the capillary, where the outward hydrostatic pressure is lower and the inward oncotic pressure gradient is increased by exclusion of proteins from the capillary filtrate by the capillary endothelium. More recent experimental and modeling techniques have integrated the role of the glycocalyx into a revised Starling equation and updated model of capillary fluid movement:4 Jv = Kf ([Pc -Pi] - [c -sg]) where Jv is the transcapillary flow, Kf is the filtration coefficient, Pc is capillary hydrostatic pressure, Pi is the interstitial hydrostatic pressure, is the reflection coefficient (the degree to which the tendency of a macromolecule to cross the endothelial barrier is resisted), c is the capillary oncotic pressure, and sg is the subglycocalyx oncotic pressure. The key differences and their clinical relevance are as follows3: At steady state, continuous capillaries do not exhibit fluid reabsorption toward the venous end of the capillary (the "no-absorption" rule). An exception to the no-absorption rule occurs in acutely subnormal capillary pressures; a transient period of autotransfusion may occur, limited to approximately 500 mL. If subnormal pressures persist beyond this, Jv will approach zero, but ongoing reabsorption does not occur. Infused crystalloid has been thought to distribute evenly throughout the extracellular compartments as a result of capillary filtration (Jv), leaving approximately one fourth or one fifth of the original volume within the circulating blood volume, whereas colloids were presumed to initially remain largely within the intravascular volume. Furthermore, context sensitivity is responsible for the observation that clearance of crystalloid from its central compartment (the intravascular volume) is slower under anesthesia than in awake subjects. However, it is likely to be closer to the measured values in critical illness than the theoretic values traditionally used. Hypoalbuminemia is well recognized as a marker of disease severity in critical illness. Finally, the importance of the endothelial glycocalyx is highlighted by studies showing that its degradation significantly impairs endothelial barrier function. Here, an increase in the number of large pores, and a reduction in interstitial hydrostatic pressure favor Jv, with an increase in edema in compliant tissues such as the lung, muscles, and loose connective tissue. Impaired glycocalyx function will further favor Jv and lead to endothelial platelet aggregation and leukocyte adhesion. Maintenance of glycocalyx integrity is therefore gaining interest as a therapeutic target in perioperative fluid management. Water intake does not usually depend on thirst because of social drinking behavior; thirst acts as a backup mechanism when the normal intake is inadequate. This results in water reabsorption down its osmotic gradient and formation of concentrated urine. Acute Disturbances in Circulating Volume Acute variation in the intravascular volume leads to compensatory mechanisms over minutes to hours in an attempt to correct the acute abnormality. The sensor organs for the acute change are the low-pressure and high-pressure baroreceptors, and initial changes are mediated through increased sympathetic outflow. The overall result is increased renal salt and water retention, increased peripheral vascular resistance, and increased cardiac output. Conversely, the rapid infusion of fluid to a normovolemic healthy adult leads to an initial rise in venous and arterial pressure and cardiac output. Several mechanisms act rapidly to bring these cardiovascular parameters toward normal, including pressure receptor-mediated venodilation and venous blood pooling and reduction in systemic vascular resistance. At a tissue level, autoregulatory responses lead to arteriolar vasoconstriction to maintain constant blood flow in the face of increased perfusion pressure. Finally, increased arterial blood pressure promotes the excretion of excess water and salt. This is the pressure-volume control mechanism, one of the key mechanisms for the long-term maintenance of normal blood volume. However, arterial blood pressure is only slowly restored by cardiovascular reflexes after acute hypervolemia. It may take several days for a 20 mL/kg dose of isotonic salt solution to be fully excreted. Long-Term Control of Circulating Intravascular Volume the Guyton-Coleman model is the archetypal representation of the circulation. Despite calls to refine the mathematic modeling of the long-term control of arterial blood pressure, it remains the most widely used model to explain the chronic control of blood volume and arterial pressure. The kidneys are the primary organ regulating this equilibrium, largely through pressure natriuresis and diuresis. Indeed, in the chronic setting, arterial pressure subserves the renal requirement to excrete ingested Na+ and water rather than simply being a product of cardiac output, vascular compliance, and resistance. In many models of chronic hypertension, the renal excretion mechanism is reset such that natriuresis occurs only at higher arterial pressures and excessive exogenous water and salt results in higher blood pressure. Total body Na+ content is approximately 4000 mmol, of which only 10% is intracellular. Na+ intake is typically far in excess of minimum daily requirements, which are 2 to 3 mEq/kg/day at birth and decrease to 1 to 1. Loss is predominantly by the renal route, with minor contributions from feces, sweat, and skin (10 mEq/day each). In the chronic setting, arterial pressure (Pa) depends on daily water and sodium intake (dripping tap) and the renal pressure-natriuresis relationship (represented by the height of the holes in the arterial column) rather than cardiac output Q and peripheral resistance (R). This may be represented by kidney holes positioned further up the arterial column. Natriuresis occurs to a degree similar to that in normotension, so as to maintain a stable body water volume, but requires a higher arterial pressure to do so. Long-term ingestion of excess salt combined with low potassium ingestion contributes to hypertension, a condition not seen in populations with daily salt intake less than 50 mmol.
Udenafil 100 mg with mastercard
For a laparoscopic approach erectile dysfunction psychological treatment techniques udenafil 100 mg on-line, distension of the peritoneum may produce hemodynamic changes because of the intragastric pressure generated by carbon dioxide insufflation. Special considerations for robotic surgery include protecting the patient against any injury related to the robot and not moving the operating room table while the robot is being used. The thoracoscopic-assisted esophagectomy has several advantages including less blood loss, less pain, and a shorter length of hospitalization. Patients undergoing esophagectomy usually require a nasogastric tube, which must be well-secured at the end of the operation. Respiratory complications, including the development of an acute lung injury, may be present after an esophagectomy. Intrathoracic anastomotic leakage is a feared major complication after esophageal surgery, and carries a high mortality rate of 4% to 30%. Severe leakage usually occurs in the early postoperative period as a consequence of gastric necrosis, and it may present with respiratory symptoms and signs of shock. Even though there is a very high mortality rate, prompt surgical intervention is recommended. Patients older than 80 years have an increased risk of mortality after esophagectomy, independent of comorbidity. Although most patients with gastroesophageal reflux have a hiatal hernia, most patients with a hiatal hernia do not have significant reflux. Type I hernias, also called sliding hernias, make up approximately 90% of esophageal hiatal hernias. The lower esophageal sphincter is cephalad to the diaphragm and may not respond appropriately to increased abdominal pressure. Thus a reduced barrier-pressure during coughing or breathing leads to regurgitation. The goal of surgical repair of a sliding hernia is to obtain competence of the gastroesophageal junction. Since restoration of the normal anatomy is not always successful in preventing subsequent reflux, several antireflux operations have been developed, such as the Nissen fundoplication. Repair of a hiatal hernia can be performed via a thoracotomy or laparotomy, or minimally invasively. Chronic reflux of acidic gastric contents can lead to ulceration, inflammation, and eventually stricture of the esophagus. The pathologic changes are reversible if the acidic gastric contents cease their contact with the esophageal mucosa. There are two types of surgical repair, both of which are usually approached via a left thoracoabdominal incision. Gastroplasty after esophageal dilatation interposes the fundus of the stomach between esophageal mucosa and the acidic milieu of the stomach. The remaining fundus may be sewn to the lower esophagus to create a valvelike effect. The second type of repair is resection of the stricture and the creation of a thoracic end-to-side esophagogastrostomy. Vagotomy and antrectomy are performed to eliminate stomach acidity, and a Roux-en-Y gastric drainage procedure is performed to prevent alkaline intestinal reflux. There are multiple causes of esophageal perforation, including foreign bodies, endoscopy, bougienage, traumatic tracheal intubation, gastric tubes, and oropharyngeal suctioning. Iatrogenic causes are the most common, with upper gastrointestinal endoscopy being the most frequent cause. A rupture is a burst injury often due to uncoordinated vomiting, straining associated with weight-lifting, childbirth, defecation, and crush injuries to the chest and abdomen. The rupture is usually located within 2 cm of the gastroesophageal junction on the left side. Rupture is the result of a sudden increase in abdominal pressure with a relaxed lower esophageal sphincter and an obstructed esophageal inlet. In contrast to a perforation, in the presence of a rupture, the stomach contents enter the mediastinum under high pressure and the patient becomes symptomatic much more abruptly. In addition to chest and/or back pain, patients with intrathoracic esophageal perforation or rupture may develop hypotension, diaphoresis, tachypnea, cyanosis, emphysema, and hydrothorax or hydropneumothorax. Major injuries will rapidly develop mediastinitis and sepsis if not treated surgically, so repair and drainage is an emergency procedure usually performed via a left or right thoracotomy. Achalasia is a disorder in which there is a lack of peristalsis of the esophagus and a failure of the lower esophageal sphincter to relax in response to swallowing. Clinically, the patients have esophageal distention that may lead to chronic regurgitation and aspiration. Dilatation, which carries with it the risk of perforation, can be achieved by mechanical, hydrostatic, or pneumatic means. The surgical repair consists of a Heller myotomy, which is an incision through the circular muscle of the esophagogastric junction. The myotomy is often combined with a hiatal hernia repair to prevent subsequent reflux. Occasionally, the fistula is benign, and may be due to injury by a tracheal tube, trauma, or inflammation. In contrast to the pediatric patient with esophagorespiratory tract fistulae, which usually connect the distal esophagus to the posterior tracheal wall, these fistulae may connect to any part of the respiratory tract. It arises from a weakness at the junction of the thyropharyngeus and cricopharyngeus muscles just proximal to the esophagus. It is commonly considered as an esophageal lesion because of its proximity to the upper esophagus and because the underlying cause may be a failure of relaxation of the upper esophageal sphincter during swallowing. Early symptoms may be nonspecific with dysphagia and complaints of food sticking in the throat. As the diverticulum enlarges patients describe noisy swallowing, regurgitation of undigested food, and supine coughing spells. The major concern for anesthesia is the possibility of aspiration on induction of general anesthesia for excision of the diverticulum. The best method to empty the diverticulum is to have the patient express and regurgitate the contents immediately prior to induction. Since the diverticulum orifice is almost always above the level of the cricoid cartilage, cricoid pressure during a rapid-sequence induction does not prevent aspiration and may contribute to aspiration by causing the sac to empty into the pharynx. The safest method of managing the airway for these patients may be awake fiberoptic intubation. However, intubation has been managed without incident using a modified rapid-sequence induction without cricoid pressure and with the patient supine and in a head-up position of 20 to 30 degrees. Other considerations in these patients include the possibility of perforation of the diverticulum when passing an orogastric or nasogastric tube or an esophageal bougie. For patients who have operable tumors, approximately 80% undergo segmental resection with primary anastomosis, 10% undergo segmental resection with prosthetic reconstruction, and the remaining 10% undergo placement of a T-tube stent. Bronchoscopy for a patient with tracheal stenosis should be carried out in the operating room where the surgical and anesthesia teams are present and ready to intervene should loss of airway occur. An advantage of rigid bronchoscopy over flexible bronchoscopy is that it can bypass the obstruction and provide a ventilation pathway if complete obstruction occurs. During surgery, all patients should have an invasive arterial catheter placed to facilitate measurement of arterial blood gases, as well as measure arterial blood pressure. Induction of anesthesia in patients with a compromised airway requires good communication between the surgical team and the anesthesiologist. The surgeon should always be in the operating room during induction and available to manage a surgical airway if this becomes necessary. The airways of patients with congenital or acquired tracheal stenosis are unlikely to collapse during induction of anesthesia. However, intratracheal masses may lead to airway obstruction with induction of anesthesia and should be managed similarly to anterior mediastinal masses (discussed later in chapter). Ventilation is done via a sterile anesthetic circuit with an airway gas sampling catheter passed across the drapes into the surgical field (this technique is commonly referred to a "cross-field ventilation"). With a low tracheal lesion, a right thoracotomy provides the optimal surgical exposure.
Trusted 100 mg udenafil
If conduction does not occur across the lesion erectile dysfunction cleveland clinic 100 mg udenafil with visa, resection of the damaged nerve and nerve cable grafting is performed. Incomplete myelination of specific tracts that carry sensory or motor signals is the primary source of the challenges. In addition, adaptive strategies need to be applied by the monitoring team to overcome the effects of myelination delays and other developmental factors (Table 39. Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals. One example is selective dorsal rhizotomies for relief of spasticity associated with cerebral palsy. This procedure involves interrogation of lower extremity dorsal root subdivisions (rootlets) and evaluating the compound action potentials generated in response. Infant/ toddler hearing evaluations may require the use of auditory brainstem response tests under anesthesia. Alpha and theta patterns emerge under anesthesia at 4 months of age but differ from those of older children and adults. Although the data seem promising, only a few patients have been studied, with very few corroborating studies. In addition, this type of monitoring is extremely costly in time, personnel, and equipment. Given the lack of convincing outcome data, the cost-to-benefit ratio is unclear at best. None of the currently available studies and recommendations would support an evidence-based justification for their routine application. Probe placement instability and inability to obtain signals in some patients also have limited the use of this monitor intraoperatively. Many techniques of neurologic monitoring discussed earlier are used in the intensive care unit. Generally, however, techniques that require the continued presence of skilled technologists, such as monitoring of evoked potentials, are prohibitively expensive and of less practical value than techniques that provide data that easily integrates into the physiologic support provided through intensive care or techniques that can be performed as daily assessments. Some of this neurophysiologic data can provide important prognostic information in comatose patients and guide decision making. It facilitates timely intervention for specific diagnoses, such as nonconvulsive seizures, as the underlying cause of a fluctuating neurologic status, or point to focal problems such as regional ischemia due to vasospasm after subarachnoid hemorrhage. It can be difficult to detect in patients who are either comatose or sedated, but can occur even in patients with adequate cerebral perfusion pressure. Sjvo2 monitoring is used most extensively in the intensive care unit to monitor patients with traumatic brain injury. The data have been used to guide blood pressure and ventilatory management to optimize blood flow. Sjvo2 monitoring has had a major effect on ventilatory management of head-injured patients and has significantly reduced the routine use of hyperventilation in neurosurgical patients. Increases in Sjvo2 may occur in response to therapy, or they may be an ominous sign if the increase is caused by falling demand because of neuronal death. Such narrowing occurs 12 to 24 hours before the onset of clinical symptoms, thus allowing therapy to be initiated before the onset of clinical symptoms. Subanesthetic doses of intravenous and inhaled anesthetics usually produce an increase in frontal beta activity and abolish the alpha activity normally seen in the occipital leads in an awake, relaxed patient with the eyes closed. As the patient loses consciousness with general anesthesia, the brain waves become larger in amplitude and slower in frequency. In the frontal areas, small beta activity seen in an awake patient slows to the alpha range and increases in size. In combination with the loss of the occipital alpha activity, this phenomenon produces the appearance of a "shift" of the alpha activity from the posterior cortex to the anterior cortex. Assessment of prognosis must be separated from the insult that precipitated the coma by more than 24 hours. More than 24 hours after the insult, spontaneous sustained burst suppression correlates strongly with severe irreversible brain injury. With further increases in intracranial pressure, a characteristic to-and-fro pattern of flow is established, which is consistent with clinical brain death. Further increases in dose result in lengthening periods of suppression interspersed with periods of activity (burst suppression). All of these drugs have been reported to cause epileptiform activity in humans, but epileptiform activity is clinically significant only after methohexital and etomidate when given in subhypnotic doses. Anesthesia with ketamine is characterized by frontally dominant rhythmic, high-amplitude theta activity. Increasing doses produce intermittent polymorphic delta activity of very large amplitude interspersed with low-amplitude beta activity. If no further doses of opiates are given, alpha and beta activity return as drug redistribution occurs. Epileptiform activity occurs in humans and in animals receiving large to supraclinical doses of opioids. Sharp wave activity is common after induction of anesthesia with fentanyl, with 20% of patients showing this phenomenon after 30 g/kg; 60%, after 50 g/kg; 58%, after 60 g/kg; and 80%, after 70 g/kg. Isolated epileptiform patterns sometimes can be seen during intersuppression activity at 1. Used alone, nitrous oxide causes a decrease in amplitude and frequency of the dominant occipital alpha rhythm. Hyperventilation with high concentrations of enflurane increases the length of suppression, decreases the duration of bursts, but increases the amplitude and main frequency component of the intersuppression epileptiform activity. In limited clinical studies, there has been no evidence of epileptiform activity with desflurane, despite hyperventilation and 1. Intravenous drugs have significantly less effect than "equipotent" doses of inhaled anesthetics 2. Subcortical (spinal or brainstem) sensory-evoked responses are very resistant to the effects of anesthetic drugs. The "no" designation indicates that any effects that do occur would not be called clinically significant by clinicians experienced in intraoperative monitoring. Effects of halothane, enflurane, isoflurane, and nitrous oxide on somatosensory-evoked potentials in humans. Doses of anesthetic drugs causing significant depression of the response to be monitored must be prevented. In our experience, end-tidal concentrations of inhaled anesthetic drugs totaling greater than 1. Equally important, anesthetic concentration should not be changed during the critical periods of intraoperative monitoring. At typical clinical doses required for general anesthesia, propofol has minimal effects on somatosensoryevoked responses recorded along the somatosensory pathway up to the early cortical potentials. In cats, the early potentials persisted with increases in latency even to very high pentobarbital doses. Opioid-induced changes must be taken into account, however, when evaluating the recordings. Note dramatically increased amplitude and clarity of the signal in the cortical (Cort) channels (marked by arrows), which both are recorded with the same amplification scale. As the use of this drug increases, more data should become available, but at this time, use of dexmedetomidine does not seem to be clearly problematic. When responses are recorded from muscle, neuromuscular blocking drugs should be monitored quantitatively, maintaining T1 twitch height at around 30% of control values to prevent excessive movement during the operation. Note similarity of the change pattern, except that in the anesthetic-induced change, the responses in the upper extremity also changed. Responses from four muscle groups in each lower extremity are shown directly below. Ant tib, M tibialis anterior; gast, m gastrocnemius; L, left; quad, m quadriceps femoris; R, right; then, thenar. Although hundreds of such case reports are in the literature, as well as many in our experience, cost-effectiveness of such monitoring is unclear. Immediate angiography revealed acute carotid occlusion and completely changed the operation performed with this patient, and the patient recovered completely.
Cheap udenafil 100 mg otc
It should be reserved for patients with severely limited cardiopulmonary function or complex aortic reconstruction impotence due to diabetes purchase udenafil with mastercard. The invasive monitoring catheters can be placed before or after induction of general anesthesia. With selective use, accurate interpretation of data, and rational treatment strategies, pulmonary artery catheter monitoring may be beneficial in high-risk patients undergoing complex aortic reconstruction. Yet the clinical value of pulmonary artery catheter monitoring in high-risk patients has not been established. Patients requiring supraceliac aortic cross-clamping have significant increases in the end-diastolic area and significant decreases in ejection fraction on echocardiography that are not completely normalized with vasodilators and frequently are not detected by pulmonary artery catheter monitoring. The clinical usefulness of any monitoring technique ultimately depends on patient selection, accurate interpretation of data, and appropriate therapeutic intervention. The routine use of cell salvage during aortic surgery may not be cost-effective and thus it may best be reserved for a select group of patients with an expected large blood loss. A costeffective option is to use the cell salvage reservoir for blood collection and activate the full salvage process only if large blood loss occurs. Cell Salvage Intraoperative cell salvage is a widely used technique combined with allogenic blood transfusion and in some centers is considered routine. An early, nonrandomized study reported a 75% reduction in the number Anesthetic Drugs and Techniques Various anesthetic techniques, including general anesthesia, regional (epidural) anesthesia, and combined techniques, have been used successfully for abdominal aortic reconstruction. Combined techniques most commonly use a lumbar or low thoracic epidural catheter in addition to general anesthetic. Local anesthetics, opioids, or, more commonly, a combination of the two may be administered by bolus or continuous epidural infusion. Maintenance of vital organ perfusion and function by the provision of stable perioperative hemodynamics is more important to overall outcome than is the choice of anesthetic drug or technique. Given the frequent incidence of cardiac morbidity and mortality in patients undergoing aortic reconstruction, factors that influence ventricular work and myocardial perfusion are of prime importance. Induction of general anesthesia should ensure that stable hemodynamics are maintained during loss of consciousness, laryngoscopy and endotracheal intubation, and the immediate postinduction period. The addition of a short-acting, potent opioid such as fentanyl or sufentanil usually provides stable hemodynamics during and after induction of anesthesia. Volatile anesthetics may be administered in low concentrations before endotracheal intubation during assisted ventilation as an adjunct to blunt the hyperdynamic response to laryngoscopy and endotracheal intubation. Esmolol 10 to 25 mg, sodium nitroprusside 5 to 25 g, nitroglycerin 50 to 100 g, or clevidipine 100 mcg and phenylephrine 50 to 100 g should be available for bolus administration during induction if needed to maintain appropriate hemodynamics. Maintenance of anesthesia may be accomplished with a combination of a potent opioid (fentanyl or sufentanil) and an inhaled anesthetic (sevoflurane, desflurane, or isoflurane). Patients with severe left ventricular dysfunction may benefit from a pure opioid technique, but a balanced anesthetic technique allows the clinician to take advantage of the most desirable characteristics of potent opioids and inhaled volatile anesthetics while minimizing their undesirable side effects. Nitrous oxide can be used to supplement either an opioid or an inhaled anesthetic. Various regional anesthetic and analgesic techniques have been used effectively during and after aortic reconstruction. For over 2 decades, interest has focused on the use of regional anesthetic and analgesic techniques to reduce the incidence of perioperative morbidity in patients undergoing aortic reconstruction. In a randomized trial using epidural morphine in patients undergoing aortic surgery, Breslow and associates72 found attenuation of the adrenergic response and a less frequent incidence of hypertension in the postoperative period. A large randomized trial reported no reduction in nonsurgical complications with the use of intrathecal opioid. Four randomized trials, with nearly 450 combined patients undergoing aortic reconstruction, failed to demonstrate a reduction in the incidence of perioperative,14,73 intraoperative,74 or postoperative70 myocardial ischemia when epidural techniques were used. Additionally, randomized trials have not demonstrated a reduction in the incidence of cardiovascular, pulmonary, or renal complications after aortic surgery with the use of epidural techniques. Length of hospital stay may therefore be considered the outcome variable most directly proportional to an integrated final negative effect of all significant perioperative morbidity (excluding in-hospital death) and the variable most likely to be altered by the anesthetic or analgesic technique. Randomized trials have not demonstrated any reduction in length of hospital stay after aortic surgery with the use of regional techniques. Norris and colleagues14 reported the results of a randomized clinical trial comparing alternative combinations of intraoperative anesthesia. The study rigorously protocolized perioperative management, standardized postoperative surgical care, and optimized postoperative pain management. The overall incidence of postoperative complications in the trial was low and not different based on anesthetic or analgesic technique. Postoperative pain was well controlled overall, with similar pain scores in both analgesic treatment groups. This design allows the inclusion of all four possible combinations on intraoperative anesthesia and postoperative analgesia and the ability to separate the influences of time period and technique. Data analysis by treatment group, intraoperative treatment, postoperative treatment, and any epidural activation, as well as simultaneous consideration of both intraoperative and postoperative treatments in the same model (factorial analysis), is possible and allows improvement in outcome to be attributed to the intraoperative anesthesia, postoperative analgesia, the combination of the two, or to unrelated factors. The use of epidural local anesthetics in combination with general anesthesia during aortic reconstruction poses several problems, including hypotension at the time of aortic unclamping and the need for increased intravascular fluid and vasopressor requirements. Supraceliac aortic crossclamping may significantly exaggerate these disadvantages, and, as a result, some clinicians avoid running local anesthetics in the epidural around the period of aortic clamping and unclamping. Epidural opioids without local anesthetics can be used in the interim and local anesthetic can be given later, after aortic unclamping, when hemodynamics and intravascular volume have stabilized. Although elective aortic reconstruction via the retroperitoneal approach using straight epidural anesthesia (no general anesthetic) has been reported, this technique is not recommended for routine use. Hypertension and tachycardia are aggressively controlled during emergence by the use of short-acting drugs such as esmolol, nitroglycerin, clevidipine, or sodium nitroprusside. Emergence from anesthesia should be conducted after restoration of circulation and establishment of adequate organ perfusion. Temperature Control Postoperative hypothermia is associated with many undesirable physiologic effects and may contribute to adverse outcomes (see also Chapter 80). If significant hypothermia occurs early in the procedure, normothermia is extremely difficult to achieve, and emergence and tracheal extubation may be delayed. During surgery, all fluids and blood products should be warmed before administration. Surgical repair is required for a spectrum of disease, including degenerative aneurysm, acute and chronic dissection, intramural hematoma, mycotic aneurysm, pseudoaneurysm, penetrating aortic ulcer, coarctation, and traumatic aortic tear. These advances have led to significant reductions in operative mortality and perioperative complications. However, even in centers where numerous procedures are performed, morbidity and mortality are frequent, especially in patients with dissecting or ruptured aneurysms. Intraoperative management requires a team effort with intimate cooperation among surgeons, anesthesiologists, perfusionists, nurses, and electrophysiologic monitoring staff. Endovascular stent-graft repair of lesions that affect the descending thoracic and thoracoabdominal aorta is evolving rapidly. As discussed later, accumulating experience with stent-graft repair of thoracic aortic aneurysm, dissection, and traumatic tear has demonstrated this modality to be an effective alternative to open repair for select patients. The increasing diameter is associated with increased wall tension, even when arterial pressure is constant (law of Laplace). The frequent incidence of associated systemic hypertension enhances aneurysm enlargement. Additional symptoms can be caused by compression of organs or structures adjacent to the aneurysm. Rupture of the thoracic and abdominal segments occurs with equal frequency and primarily in patients with aneurysms larger than 5 cm. Surgical repair is usually recommended when aneurysm diameter exceeds 6 cm, but earlier repair may be offered to patients with Marfan syndrome and those with a strong family history of an aortic aneurysm. In addition to cause, aneurysms of the thoracoabdominal aorta may be classified according to their anatomic location. Type I aneurysms involve all or most of the descending thoracic aorta and the upper abdominal aorta. Even with extracorporeal circulatory support, an obligatory period occurs when blood flow to these organs is interrupted because the origin of the blood flow is between the cross-clamps. For this reason, protective measures to prevent ischemic injury are important in reducing morbidity.
Order udenafil 100 mg overnight delivery
Cardioplegia can be administered in antegrade fashion through a special needle placed in the ascending aorta between the aortic valve and the aortic cross-clamp impotence quiz buy generic udenafil 100 mg online. Retrograde cardioplegia can be delivered directly into the coronary sinus through a special balloon-tipped cannula. Vent cannulas are used to decompress the heart while the aorta is clamped and to remove bubbles before cross-clamp removal. The alternative approaches of axillary or femoral artery cannulation are used in procedures that require the manipulation of much of the aortic root, arch, or both. Axillary artery cannulation is generally facilitated by the anastomosis of a tube graft to the side of the axillary artery to provide access for the arterial cannula without interrupting blood flow to the right arm. An added benefit of axillary cannulation for aortic arch procedures is that clamping the innominate artery allows antegrade cerebral perfusion to be performed during a period of circulatory arrest. Femoral arterial cannulation involves inserting the cannula through the femoral artery and into the abdominal aorta. Ischemia of the cannulated limb is a risk commonly associated with femoral arterial cannulation, and dissection of the cannulated artery is a risk associated with the cannulation of any arterial site. Iatrogenic aortic dissection at the cannulation site occurs in approximately 200 procedures annually in the United States, with a resultant mortality of 48%. With venous and arterial cannulas in place, the heart and the lungs can be bypassed. For example, cardioplegia cannulas can be placed in the ascending aorta, and then the aorta can be occluded by placing a large vascular clamp. During the period when the aorta is cross-clamped, this blood volume will distend the left side of the heart and the pulmonary vasculature if the blood is not actively removed. The 10- to 14-Fr cannula used for this purpose offers significantly better venting capacity than does the root vent. Unfortunately, numerous case reports exist of injuries to patients that resulted from air being pumped into the heart through malfunctioning vent lines. The proper function of the vent pump should be confirmed at the field before the pump is connected to the patient. The arterial trace usually becomes nonpulsatile as the heart is emptied and the pumping force is changed from the ventricle to the nonpulsatile heart and lung machine. If right-sided heart pressure does not reduce to 0 mm Hg, the arterial trace remains pulsatile, and arterial pump flow cannot be increased to full flow; in that case, the position of the venous cannula must be reevaluated. Arterial blood gas is drawn to assess the performance of the oxygenator and to monitor the patient for the development of acidosis. It is common to augment this reduction with hypothermia by administering cold cardioplegia solution. Once the surgical procedure is completed, myocardial arrest can be reversed by reperfusing the coronary arteries with warm normokalemic blood. The ingredients of cardioplegia solutions vary considerably from institution to institution, save that potassium is always used as the arrest agent. Whereas some centers may use a very simple solution of potassium-enriched whole blood, others may choose a more complex solution with a variety of chemical additives. The trend in clinical practice has been not to use purely crystalloid cardioplegia solutions; instead, most centers now use some form of blood cardioplegia. Typically, solutions with two different potassium concentrations are used during the procedure. For inducing cardioplegic arrest, a "high-K" solution with a potassium concentration of approximately 20 to 30 mEq is used. After isoelectric arrest is induced, the solution is changed to a "low-K" mixture with a potassium concentration of approximately 10 mEq. These solutions can be administered in antegrade fashion into the coronary arteries via the aortic root, through a needle placed between the aortic cannula and the aortic valve, or in retrograde fashion into the coronary veins, via a balloon-tipped cannula placed in the coronary sinus. In fact, it is not uncommon for cardioplegia to be delivered simultaneously in both antegrade and retrograde fashion. After an initial arrest dose of approximately 1000 to 1500 mL of "high-K" solution is administered, perfusion of the heart is suspended for a period of 10 to 40 minutes while the surgeon operates on the heart. Then, periodically throughout the procedure, 200- to 500-mL doses of "low-K" solution are administered to deliver nutrients to the cells and maintain the potassium concentration. If the vent lines are not keeping the heart empty, it will warm more quickly and the heart muscle will be under tension. This state increases myocardial oxygen consumption and compromises myocardial protection. To reinstitute the electromechanical activity of the heart, warm, normokalemic blood is infused into the coronary arteries. This may be done by administering a "hot shot" through the cardioplegia cannulas or by simply removing the cross-clamp. Before weaning and termination, the patient should be rewarmed and the heart de-aired. Regular cardiac electrical activity should be confirmed and supported with a pacemaker if necessary. Ventilation of the lungs must be resumed and laboratory values confirmed and corrected if needed. When the patient is hemodynamically stable, protamine can be administered to reverse the anticoagulatory effect of heparin. The administration of protamine to the patient is a sentinel event that must be communicated clearly by the anesthesiologist to the perfusionist and surgeon. Protamine inactivates heparin by irreversibly binding with the strongly acidic heparin molecule to form a stable salt with no anticoagulant effects. Protamine should be administered slowly over a period of 5 to 10 minutes to reduce the risk of hypotension. Deep hypothermia unquestionably confers cerebral protection when the circulation must be arrested during cardiac surgery. Various suggested mechanisms for the neuroprotective effects of hypothermia have been tested in animal models (Table 54. Hypothermia not only reduces the metabolic rate but also delays the release of excitatory amino acids, neurotransmitters that play an important role in the process of neuronal death. Additionally, hypothermia reduces the permeability of brain arterioles and prevents blood-brain barrier dysfunction. Hypothermia may also interfere with the inflammatory response by suppressing the adhesion of polymorphonuclear leukocytes in the damaged region. Hypothermia is always initiated after aortic cannulation and the onset of bypass, but macroembolization to the brain is unlikely during this period because the heart is excluded from the circulation by the aortic cross-clamp. Hyperthermia delays neuronal metabolic recovery and increases excitotoxic neurotransmitter release, oxygen free radical production, intracellular acidosis, and blood-brain barrier permeability, with subsequent multifocal breakdown at sites in the thalamus, hippocampus, and striatum (see Table 54. Hyperthermia also affects protein kinase activity and destabilizes the cytoskeleton. Clinically, fever and hyperthermia worsen the prognosis of hospitalized patients with stroke. In the 1990s, some centers began using normothermic cardioplegia to improve cardiac outcomes while avoiding deliberate hypothermia. This practice of "warm heart surgery" was debated because of concern that the neuroprotective effects of hypothermia would be lost. Subsequent studies produced inconsistent results with respect to the incidence of stroke and postoperative neurocognitive decline. Such differences in neurologic outcome may have resulted from variations in the temperature management strategies used in different "warm heart surgery" studies; these variations ranged from allowing a downward "drift" that resulted in actual mild hypothermia to active rewarming that may have led to inadvertent cerebral hyperthermia. Brain parenchymal temperature cannot be measured directly during cardiac surgery; rather, it must be estimated from tympanic, nasopharyngeal, esophageal, rectal, bladder, skin surface, pulmonary arterial, or jugular venous bulb temperature.
Order udenafil 100 mg with amex
In severe hypoosmolar hyponatremia with neurologic symptoms statistics for erectile dysfunction buy generic udenafil 100 mg on-line, hypertonic saline may be used. The symptoms of hyponatremia are related to cerebral edema and increased intracranial pressure and are highly dependent on how rapidly the hyponatremia occurred. In acute onset, symptoms typically occur when Na+ concentrations are as low as 120 to 125 mEq/L (higher in children and premenopausal females) with headache, confusion, agitation, vomiting, and lethargy. At Na+ concentrations less than 110 mEq/L, symptoms progress to seizures and coma. In the chronic setting, clinical features may be absent even at concentrations less than 120 mEq/L. In all cases of hyponatremia, potential underlying causes such as steroid deficiency, renal disease, and cardiac disease should be identified and treated. Chronic hyponatremia (>48 hours or of unknown duration) should be treated cautiously because of cerebral compensation for the hypoosmolar state; sudden increases in osmolality lead to cerebral water loss and osmotic demyelination. Treatment options for other scenarios are listed below: Hypovolemic hyponatremia: Symptoms are unusual because osmotic shifts in the brain are limited by the loss of both Na+ and water. Loop diuretics (rather than thiazides, which impair urinary dilution) can be used to excrete free water once a negative Na+ balance has been achieved. Chronic, asymptomatic hyponatremia: No immediate correction of hyponatremia is required, and the underlying cause should be treated. Symptomatic hyponatremia (typically euvolemic or hypervolemic): In patients with moderate symptoms (confusion, lethargy, nausea, and vomiting), hypertonic 3% saline may be used at an initial rate of 1 mL/kg/h with the goal of increasing [Na+] by 1 mEq/L/h for 3 to 4 hours, after which electrolytes should be rechecked. The infusion rate should be modified to ensure that [Na+] is increased by no more than 10 mEq/L in the first 24 hours of treatment. Severely symptomatic hyponatremia (coma, seizures, often with [Na+] <120 mEq/L) is typically of acute onset and the risks of undertreating are more than those of osmotic demyelination. A bolus of 100 mL of 3% saline should initially be given with the aim of acutely increasing [Na+] by 2 to 3 mEq/L. If no improvement in neurologic status occurs, this approach may be repeated once or twice at 10-minute intervals. After this, treatment should continue as for moderately symptomatic patients, with a similar goal of increasing [Na+] by no more than 10 mEq/L in the first 24 hours. Hypernatremia ([Na] >145 mEq/L) is less common than hyponatremia but may affect up to 10% of critically ill patients. Clinical features of hypernatremia include altered mental status, lethargy, irritability, seizures, hyperreflexia, and spasticity. Diagnosis is based on assessment of intravascular volume status, urinary osmolality, and Na+ concentration. Diagnostic criteria include an inappropriately dilute urine (<300 mOsm/kg) in combination with hypernatremia and high serum osmolality (>305 mOsm/kg). Treatment is tailored to the intravascular volume status, but as with hyponatremia, correction of the Na+ concentration should be no more rapid than 10 mEq/L/day unless the onset has been very acute. Hypovolemic hypernatremia: correction of the intravascular volume deficit with isotonic saline and correction of the underlying cause. Higher acute doses may have a prolonged effect with the risk for water intoxication. Because of the key role of K+ on excitable tissue resting membrane potential, dyskalemia can lead to life-threatening cardiac arrhythmias in the perioperative period. Sampling artifacts may be introduced into laboratory tests of K+; anticoagulated samples typically give results 0. Hemolysis also artificially increases K+ levels and may be introduced by poor sampling technique or delayed processing of samples. Such treatment is of prime importance when acute arrhythmias exist, and K+ should be maintained at greater than 4 to 4. K+ solutions of concentration more than 40 mEq/L may be an irritant to veins and should be administered via a central venous catheter. Ratios between intracellular and extracellular K+ concentrations may be very abnormal with acute hyperkalemia. Acute hyperkalemia sufficient to induce electrocardiographic changes is a medical emergency that requires rapid treatment. This may be particularly severe and prolonged in patients with hepatic impairment, in whom citrate metabolism is reduced. Although Ca2+ plays an important role in coagulation, coagulopathy specifically attributable to hypocalcemia only occurs at ionized Ca2+ concentrations less than 1. After parathyroidectomy, Ca2+ levels should be checked frequently until they have stabilized, because Ca2+ and vitamin D supplementation may be required in both the short and long term. In critical illness, total Ca2+ levels may be reduced because of hypoalbuminemia; however, Ca2+ supplementation should be required only if the ionized levels are low. Ca2+ may be given intravenously as 10% (weight/volume) calcium gluconate or 10% (weight/volume) CaCl2. Calcium gluconate may be preferable for peripheral administration because the tissue injury from inadvertent extravasation is less severe than with CaCl2. Mg2+ levels are often low during hypocalcemia and should also be corrected, particularly when hypocalcemia has been caused by infusion of isotonic saline or colloids in large volumes. The symptoms are related to the severity and speed of onset of the abnormality, so mild chronic hypercalcemia is usually asymptomatic. Treatment should address the underlying cause, including surgical parathyroidectomy in cases of severe hyperparathyroidism, or cessation of thiazide diuretics. In addition, the treatment of symptomatic hypercalcemia should aim to increase renal Ca2+ excretion by volume expansion with isotonic saline and possibly loop diuretics. Zoledronic acid is a newer bisphosphonate that may be even more effective and is given intravenously at a dose of 4 mg. Glucocorticoids may also be given for hypercalcemia associated with lymphoproliferative disease or ectopic vitamin D production. Serum Mg2+ concentration may be a poor indicator of total body content because of its large distribution in the intracellular compartment and slow equilibration with bone stores. Intraerythrocyte or intralymphocyte Mg2+ levels may give a better approximation of total body and tissue stores, but are more complex to process. Mg2+ has many other therapeutic indications, even in the absence of hypomagnesemia, as outlined earlier. A few of these patients are likely to have total body Mg2+ depletion that has not been detected by serum Mg2+ levels. Symptoms reflect the effect of Mg2+ on neurologic and cardiac function and relate to the serum concentration18: Mg2+ administration should therefore be performed with several important caveats. First, serum Mg2+ levels should be monitored closely during therapeutic administration. Second, because excretion is renal, doses should be decreased for patients with kidney disease. Third, it should be used with extreme caution in patients with a background impairment of neuromuscular transmission (myasthenia gravis, Lambert-Eaton myasthenic syndrome). Fourth, coadministration of neuromuscular blockers during anesthesia should be performed in reduced doses titrated to neuromuscular monitoring, because Mg2+ potentiates the effects of both depolarizing and nondepolarizing neuromuscular blockers. Treatment of acute hypermagnesemia includes promoting renal excretion by administration of fluids intravenously and diuresis. Definitive treatment, particularly in the presence of renal disease, may require dialysis. Hypophosphatemia may be related to impaired enteral uptake, increased renal excretion, or shifts to the cellular compartment or bone (Table 47. Symptoms of hypophosphatemia may be precipitated by hyperventilation in patients with chronic depletion. Refeeding syndrome may be observed on commencement of enteral or parenteral nutrition after a period of prolonged starvation and may manifest postoperatively. The consequent fat and protein catabolism results in intracellular electrolyte depletion despite normal plasma levels, particularly phosphate. Investigation and treatment of these "matched" electrolyte imbalances should initially target the dysnatremia. In "low-risk" minor surgery, fluid strategies may influence the incidence of relatively minor morbidity such as nausea and vomiting,133,134 whereas in major surgery the focus is on the potential for fluid administration to affect postoperative morbidity, length of stay, and mortality. This may involve manipulation of not just circulating volume but also of cardiac output and vascular resistance.