Buy discount clozapine 100mg
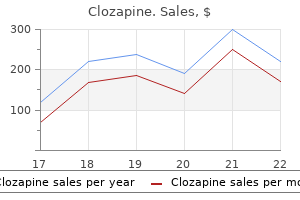
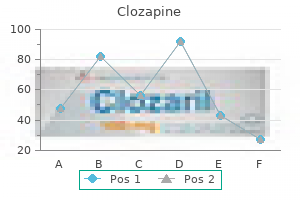
She is admitted to the intensive care unit and started on intravenous prostacyclin anxiety 6 months postpartum cheap clozapine 100mg. Shortly after starting the therapy, she develops acute shortness of breath and her chest X-ray reveals pulmonary edema. Symptoms are nonspecific and include fatigue, shortness of breath, syncope, and chest pain. Findings on physical examination may include a loud P2, crackles on lung auscultation, and lower extremity edema. Echocardiography will reveal elevated right ventricle systolic pressures and evidence of right heart strain. A ventilation-perfusion scan is often normal or may show patchy perfusion defects. Though definitive diagnosis would require histological examination of the lung, open lung biopsy carries significant risk in these patients, and noninvasive diagnosis can usually be made based upon clinical exam, imaging, hemodynamics, and response to therapy. There is also evidence of alveolar hemosiderosis indicating prior bleeding into the alveolar spaces. These proliferating capillaries infiltrate the interstitium of the lung, the walls of small pulmonary vessels, bronchi, and pleura. Pulmonary venoocclusive disease and pulmonary capillary hemangiomatosis: a clinicopathologic study of 35 cases. Case 28 A 40-year-old nonsmoking female presents with chronic nonproductive cough for the last 3 years. Bronchoscopy with transbronchial biopsies is unrevealing, so the patient undergoes video-assisted thoracoscopic surgery lung biopsy. Once the neuroendocrine cells invade beyond the basement membrane, they are termed tumorlets if their diameter is 5 mm, or carcinoid tumors if the nodule diameter is >5 mm. Patients may present with nonproductive cough, wheezing, and dyspnea or be referred for evaluation of incidentally found pulmonary nodule or nodules. Pulmonary function tests may reveal an obstructive ventilatory defect or a mixed obstructive/restrictive profile. Histological association with carcinoid tumors and changes of constrictive bronchiolitis are often found. Serum chromogranin A as a tumor marker was found to be elevated in approximately half of patients in one study with no correlation with the number or size of tumors. Various management strategies have been reported including observation in mild cases, surgical resection, inhaled and systemic corticosteroids, chemotherapy, bronchodilators, and somatostatin analogs. There is debate on whether somatostatin analogs improve symptoms or alter the course of the disease. The majority of patients have a stable clinical course, with a few progressing to respiratory failure. Patients with severe progressive disease may be referred for lung transplantation. Brief report: idiopathic diffuse hyperplasia of pulmonary neuroendocrine cells and airways disease. Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia: a systematic overview. Case 29 A 52-year-old male presents with exertional shortness of breath for the last 4 months as well as bilateral lower extremity pain without swelling. He has no history of smoking or drug abuse, and no personal or family history of cancer or lung disease. Imaging of his lower extremities reveals bilateral symmetrical sclerotic lesions of the distal femur and proximal tibia. It commonly presents in adults in their 50s to 70s with a slight male predominance. Pulmonary involvement is uncommon but is a major cause of morbidity and mortality in these patients. Symptomatic patients will often complain of a nonproductive cough and shortness of breath. Imaging findings that suggest the diagnosis include symmetrical osteosclerosis of the long bones, hairy kidneys, aortic coating, and right atrial pseudotumor. Case 30 A 52-year-old male was evaluated for shortness of breath 3 days after undergoing extracorporeal shock wave lithotripsy for renal stones. His vital signs were stable, and on examination he had dullness to percussion and decreased breath sounds over the right lung. It was first described by Corriere in 1969 and since has been reported to occur secondary to malignancy, obstructive uropathy, trauma, and after a urological or obstetric procedure. The pleural effusion occurs as a result of disruption of the urinary tract leading to leakage of urine into the retroperitoneal space and from there into the pleural space through anatomical defects in the diaphragm. Effusions are often unilateral on the same side as the urinary flow disruption or obstruction, but contralateral effusions have been reported. Unilateral obstructions do not cause urinothorax as along as the contralateral kidney remains functioning. Thus bilateral obstruction at the level of the bladder or urethra or physical disruption of the urinary system is required to form a urinothorax. Traumatic/iatrogenic urinothorax Patients may be asymptomatic with the effusion being detected incidentally on imaging. Symptomatic patients may complain of shortness of breath, chest discomfort, and fevers. Diagnosis is established based on finding of a pleural creatinine to serum creatinine ratio >1. The use of renal scintigraphy with a radioactive tracer can also help confirm the diagnosis and establish the location of defect. Management consists of correcting the underlying cause, for example relieving the urinary obstruction or surgically repairing tears in the urinary system. Thoracentesis may be sufficient for diagnosis and relief of symptoms in patients with small effusions, but chest tube placement may be required in patients with severe dyspnea or hypoxia. Case 31 A 31-year-old male presents with intermittent fevers, a nonproductive cough, and shortness of breath on exertion that started 3 weeks ago. He is a nonsmoker, has no known medical problems, and does not partake in recreational drugs. He works as an accountant and does not recall any recent significant exposures to birds, feathered duvets, hay, or hot tubs. He does report that there was a flood in the basement of his home 1 month ago, and he has been working in the basement, cleaning and fixing the plumbing for the last few weeks. Patients often present with complaints of dyspnea and a nonproductive cough, but may also have fevers, chills, weight loss, chest pain, and arthralgia. Diagnosis is often overlooked, as symptoms are nonspecific and a history of relevant exposures is not obtained. As such, the importance of obtaining a detailed and thorough exposure, occupational, and social history cannot be stressed enough as this may determine the inciting factor. It has been observed that the disease is more common in nonsmokers, possibly related to the inhibitory effects of nicotine. However, despite a detailed history and workup, no causative agent is found in approximately 30% of cases. In cases where the etiology cannot be determined and there is lack of response to corticosteroids, treatment with other immunosuppressive therapies can be attempted. A high degree of suspicion and thorough environmental and occupational history are required to determine inciting factor. Avoidance of precipitating agent and corticosteroids are mainstay of treatment in acute and subacute form. Inhibitory effect of nicotine on experimental hypersensitivity pneumonitis in vivo and in vitro. Case 32 A 34-year-old female with a history of albinism and gastrointestinal complaints presents with complaints of progressive shortness of breath on exertion for the last year. She is a nonsmoker, has no significant exposures, no significant family medical history, and her parents are originally from Puerto Rico. On examination, she has hypopigmentation of the skin and hair as well as bruising on the skin.
Generic clozapine 50mg line
They carry rheumatoid factor activity and are associated with Hepatitis C mood disorder adolescent buy 100mg clozapine overnight delivery, chronic inflammatory diseases, autoimmune disorders, and lymphoproliferative conditions. Patients with mixed cryoglobulinemia usually present with palpable purpura, generalized weakness, renal disease, and arthralgia or arthritis. In a small number of cases, severe disease with multi-organ involvement may occur. Systemic manifestations include glomerulonephritis, low complement levels, pulmonary symptoms, and nervous system involvement, usually peripheral neuropathy. There is no standard treatment for the pulmonary disease associated with cryoglobulinemia. Case reports have described the use of various therapies including high-dose corticosteroids, immunosuppressive agents, antiviral agents, and plasmapheresis, usually with little success. Life-threatening cryoglobulinemic patients with hepatitis C: clinical description and outcome of 279 patients. Case 27 A 52-year-old female is evaluated after being admitted to the hospital complaining of progressive shortness of breath over the last 4 months. An echocardiogram shows normal left ventricle function and ejection fraction but elevated right ventricle systolic pressures and an enlarged and hypertrophied right ventricle. Pulmonary function testing reveals normal spirometry and lung volumes with an isolated reduction in diffusing capacity (36% of predicted). The syndrome is characterized by the triad of oculocutaneous albinism, platelet dysfunction, and lysosomal accumulation of ceroid lipofuscin. These manifestations occur as a result of abnormal formation and trafficking of intracellular vesicles such as melanosomes, platelet dense granules, and lysosomes, respectively. The ceroid lipofuscin accumulation in lysosomes is believed to be the cause of the systemic manifestations, such as pulmonary fibrosis and granulomatous colitis. Patients with lung involvement may present in their early 30s with pro gressive shortness of breath and coughing. On examination, there is evidence of albinism as evident by the hypopigmented skin, hair, and iris on transillumination. Examination of the platelets under electron microscopy would reveal absence of dense granules. The bleeding diathesis is prevented and treated with desmopressin and platelet transfusions. Pulmonary fibrosis accounts for the mortality of 50% of patients by their fifth decade. There are published reports of the use of pirfenidone to slow disease progression but further research is required. Case 33 A 28-year-old male with a history of cerebral vein thrombosis presents with fevers, chills, and coughing up blood for the last 3 days. He is a nonsmoker, does not use recreational drugs, and has no significant environmental exposures. His examination is unremarkable with no evidence of skin rashes, mouth or genital ulcers. Ultrasound examination of the lower extremities reveals bilateral deep vein thrombosis. It is characterized by the presence of pulmonary artery aneurysms and systemic thrombosis. The disease usually affects young males in their 20s to 30s, with patients often presenting with fevers, chills, cough, chest pain, and hemoptysis. Mouth and genital ulcers, as well as eye involvement seen in Behcet disease, are absent in patients with Hughes-Stovin syndrome. Neurological symptoms including headache, diplopia, and seizures may occur in the setting of cerebral venous sinus thrombosis. Management includes treatment with corticosteroids and immunotherapy, particularly cyclophosphamide. Those with acute onset of hemoptysis may require embolization of the bleeding vessel. When bleeding is very severe, surgical management with lobectomy or even pneumonectomy may be required. Patients may be treated with anticoagulation therapy for deep vein thrombosis, but should be monitored closely for any evidence of bleeding. In some cases, they may require surgical intervention or embolization of pulmonary aneurysms. Case 34 A 64-year-old male is evaluated for acute onset of hypoxia that started within 30 min after an elective right total knee arthroplasty. The patient had an uneventful intraoperative course, but shortly after surgery was noted to be tachycardic, tachypneic, hypotensive, and hypoxic. A computed tomography scan of the chest with contrast was negative for pulmonary embolism, but showed patchy bilateral ground-glass opacities. An echocardiogram demonstrated a preserved left ventricle ejection fraction of 55%, elevated right ventricle systolic pressures, and reduced right ventricular function. The patient did not suffer from any neurological derangement and did not have any skin rashes on examination. He is transferred to the intensive care unit and recovers after fluid resuscitation and supportive care. It was first described in 1970, and it occurs during or immediately after surgery. Risk is highest in elderly patients with cardiovascular disease undergoing cemented prosthetic replacement for fracture repair. This results in the release of histamines, complement activation, and endogenous cannabinoid (anandamide and 2-arachidonoylglycerol)-induced vasodilatation. It manifests as the triad of respiratory failure, neurological impairment, and petechial rash (Bergman triad). Other findings may include the presence of fever, bradycardia, jaundice, the presence of fat particles in the blood, renal insufficiency, and retinal involvement. The systemic and pulmonary hemodynamic changes of right heart failure due to the elevated pulmonary arterial pressure and pulmonary vascular resistance, and reduced cardiac output secondary to bulging of the interventricular septum into the left ventricle, are transient and resolve with adequate fluid resuscitation and vasopressor therapy. In light of right heart failure, the use of sympathetic 1-agonist vasopressor is recommended. The altered mental status that may occur is believed to be a result of femoral content embolization through a patent foramen ovale. Case 35 A 54-year-old male with history of hypothyroidism presents to the hospital complaining of cough, shortness of breath on exertion, weight loss, and fevers that have been progressively worsening over the last 2 weeks. Over the next couple of days, his symptoms fail to improve and he undergoes a bronchoscopy with transbronchial biopsies. The first reported descriptions of elevated IgG4 levels involved patients with pancreatic manifestations, thereafter giving rise to the term systemic IgG4related disease. It has also been associated with multiple organ involvement, including the lungs and mediastinum. The disease is more commonly described in males, usually between the ages 55 and 65 years. Whether the IgG4 antibodies are responsible for the pathogenesis of the disease or are the result of an inflammatory response remains to be determined. Other pulmonary manifestations include ground-glass opacities, pulmonary infiltrates, bronchiectasis, pulmonary reticulations, tracheobronchial stenosis, lung entrapment, fibrosing mediastinitis, pleural effusions, pleural nodules, and interstitial lung disease. Patients may be asymptomatic or present with nonspecific symptoms of cough, shortness of breath, hemoptysis, and chest pain. There is accompanying inflammation, obliterative phlebitis or arteritis, and fibrosis that have a characteristic storiform pattern. This storiform or "whorled" fibrosis pattern is often minimal or absent in the lungs where a collagenized fibrosis pattern is often seen with active fibroblastic proliferation.
Cheap clozapine uk
Membrane potential plays a key role in transport mood disorder 6 game best 50mg clozapine, energy conversion, and excitability. Ratio of Protein to Lipid in Different Membranes Proteins equal or exceed the quantity of lipid in nearly all membranes. Factors Affecting the Melting Temperature the properties of fatty acids and lipids derived from them are markedly dependent on chain length and degree of saturation. At temperatures below the Tm increases fluidity At temperatures above the Tm decreases fluidty. Lipid bilayer A bilayer of such amphipathic lipids is the basic structure in biologic membranes. Micelle When a critical concentration of these lipids is present in an aqueous medium, they form micelles. Aggregation of bile salts into micelles and liposomes and the formation of mixed micelles with the products of fat digestion are important in facilitating absorption of lipids from the intestine. Fatty Acid + Alcohol (Glycerol/Sphingosine) + Phosphate + Nitrogenous base Glycerophospholipids the alcohol in this group is Glycerol. Which of the following disease occurs due to the deficiency of glucocerebrosidase Deficiency of phosphorylating enzymes for the formation of which of the following recognitior marker leads to I- cell disease Citrate (Ref: Harper 30/e p237) Allosteric regulation of Acetyl CoA carboxylase of Acetyl CoA Carboxylase by CitrateQ Palmitoyl CoA is an inhibitor of Acetyl CoA Carboxylase Oxidation of Fatty Acid and Disorders 16. Adrenaline (Ref: Harper 30/e p267) Specialized Products of Cholesterol Bile Acids [Excretory form of Cholesterol] Vitamin D Sex Hormones Corticosteroids 33. The conjugated double bond of Purine and Pyrimidine nucleotide is responsible for it. Minor Purine Bases are: Hypoxanthine-6 oxo purine Xanthine-2, 6 dioxopurine Uric Acid-2, 6, 8 trioxopurine. Pyrimidine Bases are Cytosine, Uracil and Thymine Cytosine-2 oxo 4 amino Pyrimidine Uracil-2, 4 dioxo Pyrimidine Thymine-2, 4 dioxo 5 methyl Pyrimidine. Modified Nitrogenous bases Dihydrouracil Pseudouridine 5-Methyl Cytosine Dimethyl amino adenine 7-methyl Guanine. Allopurinol is converted in the body to oxypurinol (alloxanthine), which inhibits xanthine oxidase. Important Points of Pyrimidine Synthesis In de novo Purine Synthesis amphibolic intermediates are added on Ribose 5 Phosphate. But in Pyrimidine Synthesis, amphibolic intermediates are not added on a ribose 5 phosphate.
Cheap clozapine 100mg line
The most common precipitating events for pediatric cardiac arrest involve respiratory insufficiency bipolar depression and divorce order clozapine 50 mg line. Overventilation can be due to frequent breaths (hyperventilation), which can interfere with the generation of negative intrathoracic pressure during the relaxation phase of chest compression or it can be due to too large breaths (overdistension) that may excessively increase intrathoracic pressure, pulmonary vascular resistance, and inhibit venous return. An additional concern in nonintubated patients is that delaying compressions to interpose ventilations increases the number of pauses in chest compression delivery and can contribute to worse survival outcomes. The final concern is that continued overventilation during into postresuscitation care may cause alkalosis, cerebral vasoconstriction, and limit cerebral blood flow. Epinephrine, atropine, naloxone, and lidocaine may be administered via the endotracheal route. Absorption into the circulation after endotracheal administration depends on dispersion over the respiratory mucosa, pulmonary blood flow, and matching of the ventilation (drug dispersal) to perfusion. The use of high-dose epinephrine does not improve survival, may be associated with a worse neurologic outcome, and is not recommended for initial or rescue therapy. Vasopressin is a long-acting endogenous hormone that mediates systemic vasoconstriction (V1 receptor) and reabsorption of water in the renal tubule (V2 receptor). The increased afterload with this long-acting agent may exacerbate postresuscitation myocardial dysfunction. Vasopressin has comparable efficacy, but has not improved outcome compared with epinephrine. Calcium administration is only recommended during cardiac arrest for 66 hypocalcemia, hyperkalemia, hypermagnesemia, and calcium-channel-blocker overdose. Calcium administration has not improved outcome in cardiac arrest and may worsen reperfusion injury. Cardiac arrest results in lactic acidosis from inadequate organ blood flow and oxygen delivery. Acidosis depresses myocardial function, reduces systemic vascular resistance, and inhibits defibrillation. Sodium bicarbonate is indicated for arrest from hyperkalemia, tricyclic antidepressant overdose, or sodium-channel-blocker poisoning. Side effects include hypernatremia, hyperosmolarity, metabolic alkalosis and hypercarbia. In children and adults, after an unsuccessful defibrillation attempt, epinephrine (with or without vasopressin) is administered before a subsequent attempt to defibrillate. Fever following cardiac arrest, brain trauma, stroke, and ischemia is associated with poor neurologic outcome. Postarrest myocardial stunning occurs commonly and is pathophysiologically similar to sepsis-related or postcardiopulmonary bypass myocardial dysfunction (increases in inflammatory mediator and nitric oxide production). Hyperglycemia following adult cardiac arrest is associated with worse neurologic outcome after controlling for duration of arrest and presence of cardiogenic shock. Postresuscitation hyperglycemia is usually transient and children may be at increased risk for hypoglycemia after treatment. Hypertrophic cardiomyopathy occurs among 1 in 500 in the general population with an annual risk of death of 1%, often caused by ventricular arrhythmias. It is the most common cause of sudden cardiac death among young athletes and often has no preceding symptoms. Coronary artery abnormalities (generally aberrant coronary arteries with extrinsic obstruction) are the second leading cause of sudden death in athletes. Up to 17% of sudden deaths among young athletes have been attributed to anomalous coronary arteries. Training, Certification, and Licensure Most transport teams are multidisciplinary with highly trained hospital-based providers and include members with expertise in communications and out-of-hospital care. No uniform national curriculum exists for critical care transport clinicians, either adult or pediatric. Reimbursement for critical care transport varies among states and insurance providers. Legal Considerations In the United States, interfacility patient transfer is regulated by federal laws that protect patients with emergent conditions who present to Medicare-participating hospitals. Risk Management and Insurance Collisions and crashes involving pediatric or neonatal teams are uncommon, with one collision or crash for every 1000 patient transports. Collisions or crashes resulting in serious injuries or death are less common, with a rate of 0. Disability coverage is important to provide financial security following an accident or workrelated injury. Transfer Agreements Transfer agreements define administrative procedures and the roles and responsibilities of the 69 referring and receiving facilities. The medical director should oversee the posttransport case review process, including audits of charts, recorded audiotapes, and morbidity and mortality conferences. Less than 10% of ambulance calls nationwide are for infants and children; few involve advanced life support, and even less can be classified as critical care. This fact should be considered when selecting the appropriate mode of interfacility transport for an ill or injured child. Mobile Intensive Care 70 Both ground and air transports result in noise levels that can prohibit auscultation of lung and heart sounds. Vehicular motion and vibration can result in artifacts in pulse oximetry, electrocardiography, and oscillometric blood pressure monitoring. Handheld and portable devices that enable point-of-care testing permit the analysis of whole-blood chemistries and blood gases. Ground Transport Considerations Transport by ground is the most common modality of interfacility and prehospital transport. The advantages of ground transport include virtually ubiquitous access, low cost, and ability to respond in most weather conditions. The disadvantages of ground transport include the impact of severe winter weather, traffic congestion, and road and highway conditions. Aeromedical Transport Both rotor-wing (helicopter) and fixed-wing (airplane) aircraft can be adapted for critical care transport vehicles. Barometric pressure is the sum of the partial pressures of each component gas in the atmosphere. Total barometric pressure decreases with increasing altitude and the partial pressure of each gas is reduced. An infant with cyanotic heart disease is similarly vulnerable to developing a critical level of tissue hypoxia. A decrease in the ambient barometric pressure also has the potential to affect gas-filled compartments in the body. If ground level represents sea level, then barometric pressure will decrease by 20% at 5000 feet, with a consequent 20% 71 increase in gas volume. Most commercial aircraft maintain a cabin pressure equivalent to ~8000 feet above sea level, producing a 30% decrease in barometric pressure and a 30% increase in the volume of air-filled spaces. It is essential to anticipate and address the potential for gas expansion by such interventions as gastric drainage, pleural decompression, and replacement of air in an endotracheal tube cuff (using saline) prior to transport. Rotor-Wing (Helicopter) Transport Helicopter transport is generally faster than ground transport for patients >45 miles from the receiving facility. Hypothermia is a major risk for infants during helicopter transport if an Isolette is not used. In the unpressurized cabin, ambient air has less moisture, leading to increased risk of airway plugging. Fixed-Wing (Airplane) Transport Fixed-wing transport is typically reserved for travel over long distances or open water. Additional advantages include cabin pressurization, which minimizes the adverse physiologic effects of altitude, and the ability to fly in weather conditions that may not be favorable for helicopter transport. Safety Considerations Ground transport providers should be familiar with state and local regulations regarding child restraint, which often do not exempt emergency vehicles. Communication Initial communication should include a conversation between the referring and receiving physicians. The receiving physician may be asked for medical advice regarding patient management. The risks and benefits of interfacility transfer must be explained to family members and consent obtained, either in person or by phone. When ambiguity exists or family members appear uncertain, it is preferable for them to accompany the patient on the transport if possible (see Family Presence section). Death on Transport 72 It is unusual for children to die during interfacility transport.
Order 100mg clozapine with mastercard
At least 3 consecutive stool specimens should be examined microscopically for characteristic larvae (not eggs) depression extrovert purchase clozapine 50 mg amex, but stool concentration techniques may be required to establish the diagnosis. The use of agar plate culture methods can have greater sensitivity than fecal microscopy, and examination of duodenal contents obtained using the string test (Entero-Test) or a direct aspirate through a flexible endoscope may also demonstrate larvae. Serodiagnosis is sensitive and should be considered in all people with unexplained eosinophilia, especially if immunomodulatory therapy is being considered. In disseminated strongyloidiasis, filariform larvae can be isolated from sputum or bronchoalveolar lavage fluid as well as spinal fluid. Gram-negative bacillary meningitis is a common associated finding in disseminated disease and carries a high mortality rate. An alternative agent is albendazole, although it is associated with lower cure rates. Prolonged or repeated treatment may be necessary in people with hyperinfection and disseminated strongyloidiasis, and relapse can occur. Courtesy of Centers for Disease Control and Prevention/Emerging Infectious Diseases. Free-living cycle: the rhabditiform larvae passed in the stool (1) (see Parasitic cycle) can molt twice and become infective filariform larvae (direct development) (6) or molt 4 times and become free-living adult males and females (2) that mate and produce eggs (3), from which rhabditiform larvae hatch (4). The latter, in turn, can develop (5) into a new generation of free-living adults (as represented in 2) or into infective filariform larvae (6). The filariform larvae penetrate the human host skin to initiate the parasitic cycle. Parasitic cycle: Filariform larvae in contaminated soil penetrate human skin (6) and are transported to the lungs, where they penetrate the alveolar spaces; they are carried through the bronchial tree to the pharynx, are swallowed, and then reach the small intestine (7). The females live threaded in the epithelium of the small intestine and by parthenogenesis produce eggs (9), which yield rhabditiform larvae. The rhabditiform larvae can be passed in the stool (1) (see Free-living cycle) or can cause autoinfection (10). To date, occurrence of autoinfection in humans with helminthic infections is recognized only in Strongyloides stercoralis and Capillaria philippinensis infections. Infected neonates and infants can have hepatosplenomegaly, snuffles (copious nasal secretions), lymphadenopathy, mucocutaneous lesions, pneumonia, osteochondritis and pseudoparalysis, edema, rash, hemolytic anemia, or thrombocytopenia at birth or within the first 4 to 8 weeks of age. Skin lesions or moist nasal secretions of congenital syphilis are highly infectious. However, organisms are rarely found in lesions more than 24 hours after treatment has begun. Untreated infants, regardless of whether they have manifestations in early infancy, can develop late manifestations, which usually appear after 2 years of age and involve the central nervous system, bones and joints, teeth, eyes, and skin. Acquired Syphilis Infection with T pallidum in childhood or adulthood can be divided into 3 stages. The primary stage (or "primary syphilis") appears as one or more painless indurated ulcers (chancres) of the skin or mucous membranes at the site of inoculation. Lesions most commonly appear on the genitalia but can appear elsewhere, depending on the sexual contact responsible for transmission (eg, oral). Chancres are sometimes not recognized clinically and are sometimes still present during the secondary stage of syphilis. The secondary stage (or "secondary syphilis"), beginning 1 to 2 months later, is characterized by rash, mucocutaneous lesions, and lymphadenopathy. The polymorphic maculopapular rash is generalized and typically includes the palms and soles. In moist areas around the vulva or anus, hypertrophic papular lesions (condyloma lata) can occur and can be confused with condyloma acuminata secondary to human papillomavirus infection. Generalized lymphadenopathy, fever, malaise, splenomegaly, sore throat, headache, alopecia, and arthralgia can be present. Secondary syphilis can be mistaken for other conditions because its signs and symptoms are nonspecific. This stage also resolves spontaneously without treatment in approximately 3 to 12 weeks, leaving the infected person completely asymptomatic. A variable latent period follows but is sometimes interrupted during the first few years by recurrences of symptoms of secondary syphilis. Latent syphilis is defined as the period after infection when patients are seroreactive but demonstrate no clinical manifestations of disease. Patients who have latent syphilis of unknown duration should be managed clinically as if they have late latent syphilis. The tertiary stage of infection occurs 15 to 30 years after the initial infection and can include gumma formation (soft, noncancerous growths that can destroy tissue), cardiovascular involvement (including aortitis), or neurosyphilis. Neurosyphilis is defined as infection of the central nervous system with T pallidum. Manifestations of neurosyphilis can include syphilitic meningitis, uveitis, and (typically years after infection) dementia and posterior spinal cord degeneration (tabes dorsalis). Epidemiology Syphilis, which is rare in much of the industrialized world, persists in the United States and in resource-limited countries. The incidence of acquired and congenital syphilis increased dramatically in the United States during the late 1980s and early 1990s but decreased subsequently; in 2000, the incidence was the lowest since reporting began in 1941. Since 2001, however, the rate of primary and secondary syphilis has increased, primarily among men who have sex with men. The highest rates of primary and secondary syphilis and congenital syphilis are in the Southern United States. Late or limited prenatal care and failure of health care professionals to follow maternal syphilis screening recommendations have been shown to contribute to the incidence of congenital syphilis. Primary and secondary rates of syphilis are highest in black, non-Hispanic people and in males compared with females. Congenital syphilis is contracted from an infected mother via transplacental transmission of T pallidum at any time during pregnancy or, possibly, at birth from contact with maternal lesions. Among women with untreated early syphilis, as many as 40% of pregnancies result in spontaneous abortion, stillbirth, or perinatal death. The rate of transmission is 60% to 100% during primary and secondary syphilis and slowly decreases with later stages of maternal infection (approximately 40% with early latent infection and 8% with late latent infection). Acquired syphilis is almost always contracted through direct sexual contact with ulcerative lesions of the skin or mucous membranes of infected people. Relapses of secondary syphilis with infectious mucocutaneous lesions have been observed 4 years after primary infection. In most cases, identification of acquired syphilis in children must be reported to state child protective service agencies. Physical examination for signs of sexual abuse and forensic interviews may be conducted under the auspices of a pediatrician with expertise in child abuse or at a local child advocacy center. Diagnostic Tests Definitive diagnosis is made when spirochetes are identified by microscopic darkfield examination of lesion exudate, nasal discharge, or tissue, such as placenta, umbilical cord, or autopsy specimens. Specimens should be scraped from moist mucocutaneous lesions or aspirated from a regional lymph node. Specimens from mouth lesions can contain nonpathogenic treponemes that can be difficult to distinguish from T pallidum by darkfield microscopy. Although such testing can provide a definitive diagnosis, serologic testing is also necessary. Presumptive diagnosis is possible using nontreponemal and treponemal serologic tests. These tests measure antibody directed against lipoidal antigen from T pallidum, antibody interaction with host tissues, or both. These tests are inexpensive and performed rapidly and provide semiquantitative results. Quantitative results help define disease activity and monitor response to therapy.
Discount 100 mg clozapine with visa
A disseminated cutaneous form with multiple lesions is rare clinical depression definition dsm order generic clozapine canada, usually occurring in children who are immunocompromised. Extracutaneous sporotrichosis is uncommon, with cases occurring primarily in immunocompromised patients or, in adults, those who are alcoholic or have chronic obstructive pulmonary disease. Pulmonary sporotrichosis clinically resembles tuberculosis and occurs after inhalation or aspiration of aerosolized conidia. Disseminated disease generally occurs after hematogenous spread from primary skin or lung infection. Disseminated sporotrichosis can involve multiple foci (eg, eyes, pericardium, genitourinary tract, central nervous system) and occurs predominantly in immunocompromised patients. The related species Sporothrix brasiliensis, Sporothrix globosa, and Sporothrix mexicana also cause human infection. Epidemiology S schenckii is a ubiquitous organism that has worldwide distribution but is most common in tropical and subtropical regions of Central and South America and parts of North America and Japan. The fungus is isolated from soil and plant material, including hay, straw, sphagnum moss, and decaying vegetation. Thorny plants, such as roses and Christmas trees, are commonly implicated because pricks from their thorns or needles inoculate the organism from the soil or moss around the bush or tree. Zoonotic spread from infected cats or scratches from digging animals, such as armadillos, has led to cutaneous disease. Incubation Period 7 to 30 days after cutaneous inoculation, but can be as long as 3 months. Diagnostic Tests Culture of Sporothrix species from a tissue, wound drainage, or sputum specimen is diagnostic. Culture of Sporothrix species from a blood specimen is definite evidence for the disseminated form of infection associated with immunodeficiency. Histopathologic examination of tissue may not be helpful because the organism seldom is abundant. Special fungal stains to visualize the oval or cigar-shaped organism are required. Serologic testing and polymerase chain reaction assay show promise for accurate and specific diagnosis but are available only in research laboratories. Itraconazole is the drug of choice for children with lymphocutaneous and localized cutaneous disease. After clinical response to amphotericin B therapy is documented, itraconazole can be substituted and should be continued for at least 12 months. Pulmonary and disseminated infections respond less well than cutaneous infection, despite prolonged therapy. Surgical debridement or excision may be necessary to resolve cavitary pulmonary disease. Sporothrix schenckii, mold phase (48-hour potato dextrose agar, lactophenol cotton blue preparation); small tear-shaped conidia forming rosettelike clusters. Test results on stained smears of purulent material aspirated from a cervical lymph node were negative. Localized infections include cellulitis, skin and soft tissue abscesses, pustulosis, impetigo (bullous and nonbullous), paronychia, mastitis, ecthyma, erythroderma, hordeola, furuncles, carbuncles, peritonsillar abscesses (quinsy), omphalitis, parotitis, lymphadenitis, and wound infections. Bacteremia can be complicated by septicemia; osteomyelitis; arthritis; endocarditis; pneumonia; pleural empyema; pericarditis; soft tissue, muscle, or visceral abscesses; septic thrombophlebitis of small and large vessels; and other foci of infection. Primary S aureus pneumonia can also occur after aspiration of organisms from the upper respiratory tract and is typically associated with mechanical ventilation or viral infections in the community (eg, influenza). Meningitis is rare unless accompanied by an intradermal foreign body (eg, ventriculoperitoneal shunt) or a congenital or acquired defect in the dura. S aureus infections can be fulminant and are often associated with metastatic foci and abscess formation, requiring drainage, foreign body removal, and prolonged antimicrobial therapy to achieve cure. Certain chronic diseases, such as diabetes mellitus, malignancy, prematurity, immunodeficiency, nutritional disorders, surgery, and transplantation, increase the risk for severe S aureus infections. Toxic shock syndrome toxin-1 acts as a superantigen that stimulates production of tumor necrosis factor and other mediators that cause capillary leak, leading to hypotension and multiorgan failure. Toxic shock syndrome can also occur in males and females without a readily identifiable focus of infection. Bacteremia is rare, but dehydration and superinfection can occur with extensive exfoliation. Of the isolates that do not represent contamination, most come from infections associated with health care, such as patients with obvious disruptions of host defenses caused by surgery, medical device insertion, immunosuppression, or developmental maturity (eg, very low birth weight neonates). Muscular: severe myalgia or creatinine phosphokinase concentration greater than twice the upper limit of reference range 3. Renal: serum urea nitrogen or serum creatinine concentration greater than twice the upper limit of reference range or urinary sediment with 5 white blood cells/high-power field or greater in the absence of urinary tract infection 5. Hepatic: total bilirubin, aspartate transaminase, or alanine transaminase concentration greater than twice the upper limit of reference range 6. Blood, throat, or cerebrospinal fluid cultures; blood culture may be positive for Staphylococcus aureus 2. Coagulase-negative staphylococci are responsible for bacteremia in children with intravascular catheters or those with vascular grafts or intracardiac patches, prosthetic cardiac valves, or pacemaker wires. Mediastinitis after openheart surgery, endophthalmitis after intraocular trauma, and omphalitis and scalp abscesses in preterm neonates have been described. Coagulase-negative staphylococci can also enter the bloodstream from the respiratory tract of mechanically ventilated preterm neonates or from the gastrointestinal tract of neonates with necrotizing enterocolitis. S aureus is the only species that produces coagulase, although not all S aureus produce coagulase. Staphylococci are ubiquitous and can survive extreme conditions of drying, heat, and low-oxygen and high-salt environments. S aureus has many surface proteins, including the microbial surface components recognizing adhesive matrix molecule receptors, which allow the organism to bind to tissues and foreign bodies coated with fibronectin, fibrinogen, and collagen. This permits a low inoculum of organisms to adhere to sutures, catheters, prosthetic valves, and other devices. S aureus colonizes the skin and mucous membranes of 30% to 50% of healthy adults and children. The anterior nares, throat, axilla, perineum, vagina, and rectum are usual sites of colonization. Rates of carriage of more than 50% occur in children with desquamating skin disorders or burns and in people with frequent needle use (eg, diabetes mellitus, hemodialysis, illicit drug use, allergy shots). Transmission of S aureus S aureus is most often transmitted by direct contact in community settings and indirectly from patient to patient via transiently colonized hands of health care professionals in health care settings. Health care professionals and family members who are colonized with S aureus in the nares or on skin can also serve as a reservoir for transmission. Contaminated environmental surfaces and objects can also play a role in transmission of S aureus, although their contribution for spread is probably minor. Although not routinely transmitted by the droplet route, S aureus can be dispersed into the air over short distances. Dissemination of S aureus from people with nasal carriage, including infants, is related to density of colonization, and increased dissemination occurs during viral upper respiratory tract infections. S aureus Colonization and Disease Nasal, skin, vaginal, and rectal carriage are the primary reservoirs for S aureus. Although domestic animals can be colonized, data suggest colonization is acquired from humans. Heavy cutaneous colonization at an insertion site is the single most important predictor of intravenous catheter-related infections for short-term percutaneously inserted catheters.
Buy clozapine 25 mg with mastercard
Less frequent manifestations include anorexia symptoms of depression clozapine 100mg with mastercard, vomiting, conjunctivitis, nuchal rigidity, and photophobia. The disease is mild compared with Rocky Mountain spotted fever, and no rickettsialpox-associated deaths have been described; however, disease is occasionally severe enough to warrant hospitalization. Etiology Rickettsialpox is caused by Rickettsia akari, a gram-negative intracellular bacillus, which is classified with the spotted fever group rickettsiae and related antigenically to other members of that group. Epidemiology the natural host for R akari in the United States is Mus musculus, the common house mouse. The disease can occur wherever the hosts, pathogens, and humans coexist but is most frequently reported in large urban settings. In the United States, rickettsialpox has been described predominantly in northeastern metropolitan centers, especially New York. It has also been confirmed in many other countries, including Croatia, Ukraine, Turkey, Russia, South Korea, and Mexico. Diagnostic Tests R akari can be isolated in cell culture from blood and eschar biopsy specimens during the acute stage of disease, but culture is not attempted routinely. Because antibodies to R akari have extensive cross-reactivity with antibodies against Rickettsia rickettsii (the cause of Rocky Mountain spotted fever) and other spotted fever group rickettsiae, an indirect immunofluorescent antibody assay for R rickettsii can be used to demonstrate a 4-fold or greater change in antibody titers between acute and convalescent serum specimens taken 2 to 6 weeks apart. Use of R akari antigen is recommended for a more accurate serologic diagnosis but may only be available in specialized research laboratories. Direct fluorescent antibody or immunohistochemical testing of formalin-fixed, paraffin-embedded eschars or papulovesicle biopsy specimens can detect rickettsiae in the samples and are useful diagnostic techniques, but because of crossreactivity, these assays are not able to confirm the etiologic agent. Treatment Doxycycline is the drug of choice in all age groups and is effective when given for 3 to 5 days. Doxycycline will shorten the course of disease; symptoms typically resolve within 12 to 48 hours after initiation of therapy. There are limited data describing the utility of other antimicrobials, including azithromycin and fluoroquinolones. Chloramphenicol is an alternative drug but is not available as an oral formulation in the United States. Fever, myalgia, severe headache, photophobia, nausea, vomiting, and anorexia are typical presenting symptoms. The rash usually begins within the first 6 days of symptoms as erythematous macules or maculopapules. The rash usually appears first on the wrists and ankles, often spreading within hours proximally to the trunk and distally to the palms and soles. Although early development of a rash is a useful diagnostic sign, the rash can be atypical or absent in up to 20% of cases. A petechial rash is typically a late finding and indicates progression to severe disease. Thrombocytopenia, hyponatremia (observed in 20% of cases), and elevated liver transaminase concentrations develop in many cases, are frequently mild in the early stages of disease, and worsen as disease progresses. If not treated, the illness can last as long as 3 weeks and can be severe, with prominent central nervous system, cardiac, pulmonary, gastrointestinal tract, and renal involvement; disseminated intravascular coagulation; and shock leading to death. Rocky Mountain spotted fever can progress rapidly, even in previously healthy people. Delay in appropriate antimicrobial treatment beyond the fifth day of symptoms is associated with severe disease and poor outcomes. Patients treated early in the course of symptoms may have a mild illness, with fever resolving in the first 48 hours of treatment. Etiology Rickettsia rickettsii, an obligate, intracellular, gram-negative bacillus and a member of the spotted fever group of rickettsiae, is the causative agent. The primary targets of infection in mammalian hosts are endothelial cells lining the small blood vessels of all major tissues and organs. Epidemiology the pathogen is transmitted to humans by the bite of a tick of the Ixodidae family (hard ticks). Other wild animals and dogs have been found with antibodies to R rickettsii, but their role as natural reservoirs is not clear. People with occupational or recreational exposure to the tick vector (eg, pet owners, animal handlers, people who spend more time outdoors) are at increased risk of acquiring the organism. Laboratory-acquired infection has occasionally resulted from accidental inoculation and aerosol contamination. Mortality is highest in males, people older than 50 years, children 5 to 9 years of age, and people with no recognized tick bite or attachment. Factors contributing to delayed diagnosis include absence of rash or difficulty in its recognition, especially in individuals with darker complexions; initial presentation before the fourth day of illness; and onset of illness during months of low incidence. Most cases are reported in the south Atlantic, southeastern, and south central states, although most states in the contiguous United States record cases each year. The principal recognized vectors of R rickettsii are Dermacentor variabilis (the American dog tick) in the eastern and central United States and Dermacentor andersoni (the Rocky Mountain wood tick) in the western United States. Another common tick throughout the world that feeds on dogs, Rhipicephalus sanguineus (the brown dog tick), has been confirmed as a vector of R rickettsii in Arizona and Mexico and may play a role in other regions. Rocky Mountain spotted fever also occurs in Canada, Mexico, Central America, and South America. Immunoglobulin (Ig) G and IgM antibodies begin to increase around day 7 to 10 after onset of symptoms; an elevated acute titer may represent past exposure rather than acute infection. Mildly elevated antibody titers can be an incidental finding in a significant proportion of the general population in some regions. A 4-fold or greater rise in antigen-specific IgG between acute and convalescent sera obtained 2 to 6 weeks apart confirms the diagnosis. Cross-reactivity may be observed between antibodies to other spotted fever group rickettsiae. Treatment is most effective if started in the first few days of symptoms; treatment started after the fifth day of symptoms is less likely to prevent death or other adverse outcomes. Chloramphenicol is an alternative treatment but should be considered only in rare cases, such as severe doxycycline allergies or during pregnancy. Antimicrobial treatment should be continued until the patient has been afebrile for at least 3 days and has demonstrated clinical improvement; the usual duration of therapy is 7 to 10 days. This tick is a vector of several zoonotic diseases, including human monocytic ehrlichiosis and rocky mountain spotted fever. This photograph depicts a dorsal view of a male rocky mountain wood tick, Dermacentor andersoni. This tick species is a known North American vector of Rickettsia rickettsii, which is the etiologic agent of rocky mountain spotted fever. Courtesy of Centers for Disease Control and Prevention/James Gathany; William Nicholson. The rickettsiae multiply in the endothelial cells of small blood vessels, resulting in vasculitis. There were subcutaneous erythematous lesions on the hands, and she had 5 or 6 lesions on her feet. The diagnosis of rocky mountain spotted fever was confirmed serologically, and she was treated without any complications. Autopsy findings included myocarditis, interstitial nephritis, pneumonitis, and encephalitis. A, Lymphohistiocytic inflammatory cell infiltrates in the myocardium (hematoxylin-eosin stain, original magnification x25). B, immunohistochemical detection of spotted fever group rickettsiae (red) in perivascular infiltrates of heart (immunoalkaline phosphatase with naphthol-fast red substrate and hematoxylin counterstain, original magnification x250). Courtesy of Centers for Disease Control and Prevention/Emerging Infectious Diseases and Dora Estripeaut. Courtesy of Centers for Disease Control and Prevention/Emerging Infectious Diseases and marylin Hidalgo. In moderate to severe cases, dehydration, electrolyte abnormalities, and acidosis can occur.
Buy clozapine 50mg lowest price
Dysfunctional apoptosis as a result of defective Fas/FasL signaling may also be involved in histiocyte proliferation depression workbook cheap clozapine express. Patients may present with respiratory symptoms depending on the site of intrathoracic involvement. Chest computed tomography findings vary and may include cervical and thoracic adenopathy that are hypermetabolic on positron emission tomography scan imaging. Histologically, there is lymph node pericapsular fibrosis and sinus infiltration and expansion by lymphoplasmacytic cells and histiocytes. Emperipolesis (histiocyte engulfment of lymphocytes and erythrocytes) is evident and is considered as a hallmark of the disease. In patients with organ involvement and significant symptoms, treatment is directed at symptom management and may include surgical debulking of lymph nodes causing compression of adjacent structures. Systemic corticosteroids, immunosuppressive agents, and radiotherapy have been tried for severe disease; however, their efficacy remains unclear. Case 54 A 27-year-old female presents with acute onset shortness of breath that started 2 days ago, along with a low-grade fever and a nonproductive cough. She has no significant medical history and does not smoke or use recreational drugs. She states that she was at a silicone pumping party the day before the onset of her symptoms. A chest X-ray and chest computed tomography scan are performed showing evidence of peripheral, patchy bilateral lung opacities. She undergoes bronchoscopic evaluation that is unremarkable, lavage cultures are all negative and a workup for vasculitis and other autoimmune conditions are normal. She undergoes a video-assisted thoracoscopic surgery wedge biopsy of the right lung. The histology reveals silicone vacuoles in the alveolar spaces and interalveolar walls. Adverse pulmonary consequences are often the result of illicit subcutaneous silicone injections that are inadvertent injected directly into a vein resulting in acute pneumonitis, diffuse alveolar hemorrhage, and acute respiratory distress syndrome. Presentation is very similar to fat embolism syndrome, with fever, dyspnea, cough, hypoxia, respiratory distress, hemoptysis, and altered mental status occurring within the first 72 h after an injection. Pulmonary function tests may be normal or have a restrictive pattern and bronchoalveolar lavage analysis will show a neutrophil predominant lavage. Lung biopsy shows silicone vacuoles in the alveolar spaces, interalveolar walls, pulmonary capillaries, and within alveolar macrophages. It is associated with silicone breast implants, manifesting years after the implantation surgery. As in acute silicone embolization syndrome, lung histology will show silicone microemboli within the alveolar capillaries, interstitium and alveolar spaces, in association with histiocytes and multinucleated giant cells. The chronic form of the disease rarely occurs in patients with silicone breast implants. Case 55 A 52-year-old male presents with a nonproductive cough of 3 months duration. During this period, he has been prescribed multiple courses of antibiotics for a recurring left leg infection. A chest X-ray and chest computed tomography scan confirm the presence of anterior mediastinal mass that on biopsy is found to be a thymoma. Given the patients relapsing left leg infection and diarrhea, he undergoes a workup for infection that does not reveal any pathogens. Robert Good first reported the association between thymoma and hypogammaglobulinemia in 1954. The etiology of the immunodeficiency in Good syndrome remains unclear but seems to arise in the bone marrow where B-cell development is arrested. Patients frequently have diarrhea that may be as a result of mucosal lesions resembling villous atrophy resulting in malabsorption or perhaps making these patients susceptible to gastrointestinal pathogens. The immunodeficiency associated with thymomas is usually not responsive to corticosteroids and other immunosuppressive therapies. Patients with persistent infections may require long-term antibiotic therapy in some cases. A thoracentesis is performed that reveals a slightly bloody exudative pleural effusion. The pleural serosal surface is most often involved with patients presenting with symptoms related to the location of the malignant effusion. The effusions are lymphocytic predominant exudates on analysis with evidence of large clonal neoplastic cells on flow cytometry. She is asymptomatic with no complaints of shortness of breath, chest pain, cough, palpitations, or syncope. If all the pulmonary veins are involved, it is termed total anomalous pulmonary venous return, a congenital cardiovascular anomaly that is detected early in infancy and is incompatible with life in the absence of a right to left shunting process. Patients may be asymptomatic or present with symptoms related to the degree of left to right shunting such as shortness of breath, chest pain, and palpitations and may even progress to develop pulmonary hypertension and right-sided heart failure. Symptomatic patients will require cardiac catheterization in order to determine the degree of pulmonary to systemic blood flow (Qp:Qs) shunting. It is also referred to as pulmonary venolobar syndrome or hypogenetic lung syndrome. Patients also have anomalous systemic arterial blood supply from the aorta to the right lung. The name is derived from the shape of a Turkish sword with a curved blade, given the curvilinear pattern seen by the pulmonary vein adjacent to right side of the heart and draining into the inferior vena cava on chest imaging (scimitar sign). The condition may also be associated with pulmonary artery hypoplasia, pulmonary sequestration, horseshoe lung, and accessory diaphragm. Patients may also present with recurrent episodes of pneumonia or hemoptysis if associated with pulmonary sequestration. Treatment of symptomatic patients with increase shunting is by surgical correction. These patients are usually asymptomatic due to absence of left to right shunting, and there is no need for treatment. Classic Scimitar syndrome is almost always right sided and is associated with lung hypoplasia and dextroposition of the heart. It is important to determine where the anomalous pulmonary vein terminates in order to differentiate meandering right pulmonary vein from classic Scimitar syndrome and its other variants. Incidental meandering right pulmonary vein, literature review and proposed nomenclature revision. Case 58 A 43-year-old male presents with progressive shortness of breath on exertion over the last year. He denies any leg swelling, hemoptysis, coughing, fevers, night sweats, or chest pain. Symptomatic patients may complain of progressive dyspnea on exertion, lower extremity swelling, fatigue, and syncope. Pulmonary function testing findings of isolated reduction in diffusion capacity of the lungs for carbon monoxide may be present. First-line treatment option for patients who are surgical candidates is pulmonary endarterectomy at an experienced center. This curative procedure, when done at a specialized center, carries a low mortality risk (<4%). Percutaneous transluminal pulmonary angioplasty with dilation of the narrowed pulmonary arteries is emerging as a treatment option for nonsurgical patients. Other treatment options include riociguat and percutaneous transluminal pulmonary angioplasty. She has been treated as an outpatient with oral antibiotics for pneumonia on three different occasions in the last 6 months. She has no significant past medical history of note, is a nonsmoker with no history of recreational drug use, and with no relevant medical family history. A complete workup for immunodeficiencies, cystic fibrosis, alpha-1 antitrypsin deficiency, and connective tissue disorders is unrevealing. She undergoes a video-assisted thoracoscopic surgery right lung biopsy, pathology revealing multiple large cysts with a pseudostratified ciliated columnar epithelium lining.