Famciclovir 250 mg mastercard
These agents also help Sulfur kleenex anti viral pocket packs purchase famciclovir cheap online, sodium sulfacetamide, resorcin, and salicylic acid Although benzoyl peroxide, retinoids, and topical antibiotics have largely supplanted these older medications, sulfur, resorcin, and salicylic acid preparations are still useful and moderately helpful if the newer medications are not tolerated. Sulfacetamidesulfur combination products are mildly effective in both acne and rosacea, but should be avoided in patients with known hypersensitivity to sulfonamides. Azelaic acid this dicarboxylic acid is usually well tolerated and has mild efficacy in both inflammatory and comedonal acne. Azelaic acid may help to lighten postinflammatory hyperpigmentation and is in pregnancy category B. Combination topical therapy Several products are available that combine antibiotics such as clindamycin and benzoyl peroxide or combine retinoids and either antibiotics or benzoyl peroxide. In general, these medications increase adherence because they require less frequent application, and they may also limit irritation compared with the cumulative topical application of each product separately. However, combination topical therapy limits flexibility and may cause more irritation than a single product used alone. Oral antibiotics Oral antibiotics are indicated for moderate to severe acne; in patients with inflammatory disease who do not tolerate or respond to topical combinations; for the treatment of chest, back, or shoulder acne; and in patients for whom absolute control is deemed essential, such as those who scar with each lesion or who develop inflammatory hyperpigmentation. It is appropriate for this as-yet unproved (except with rifampin, which is not used for acne) association to be discussed with patients and a second form of birth control offered. Vertigo may occur, and beginning minocycline therapy with a single dose in the evening may be prudent. An extended-release preparation is also available, which limits the vestibular side effects. Pigmentation in areas of inflammation, of oral tissues, in postacne osteoma or scars, in a photodistributed pattern, on the shins, or in the sclera, nail bed, ear cartilage, or teeth or in a generalized pattern may also be seen. Additionally, lupuslike syndromes, a hypersensitivity syndrome (fever, hepatitis, and eosinophilia), serum sickness, pneumonitis, and hepatitis are uncommon but potentially serious adverse effects of minocycline. Amoxicillin For those who cannot take tetracyclines because of side effects, or in pregnant women requiring oral antibiotic therapy, amoxicillin may be useful. Amoxicillin can be given in doses ranging from 250 mg daily to 500 mg three times daily. Many patients of acne age have taken amoxicillin in the past and are aware of their ability to tolerate the medicine without allergic reactions. Photosensitivity reactions can occur with this form of tetracycline and can be dramatic. To reduce the incidence of esophagitis, tetracyclines should not be taken at bedtime. Staining of growing teeth occurs, precluding use of tetracyclines in pregnant women and in children under age 9 or 10. Subantimicrobial-dose doxycycline (doxycycline hyclate, 20 mg) may be given twice daily. The advantage of this is that the anti-inflammatory activity is being utilized, but no antibiotic resistance results because of the low dose. Its absorption is less affected by milk and food than Clindamycin Past experience has shown that clindamycin provides an excellent response in the treatment of acne. However, the potential for the development of pseudomembranous colitis and the availability of isotretinoin have limited its use. The initial dose of clindamycin is 150 mg three times daily, reduced gradually as control is achieved. Other antibiotics Sulfonamides may be effective in many cases unresponsive to other antibiotics; however, the potential for severe drug eruptions limits their use by dermatologists. Bacterial resistance Propionibacterium acnes antimicrobial resistance has been a clinically relevant problem. However, with the limited use of erythromycin, clindamycin, and tetracycline, this consideration is less problematic. Doxycycline resistance may occur, and minocycline is a suitable alternative if this problem is suspected. Also, close contacts, including treating dermatologists, may harbor such drug-resistant bacteria. Strategies to prevent antibiotic resistance include limiting the duration of treatment, stressing the importance of adherence to the treatment plan, restricting the use of antibiotics to inflammatory acne, encouraging repeat treatment with the same antibiotic unless it has lost its efficacy, avoiding the use of dissimilar oral and topical antibiotics at the same time, and using isotretinoin if unable to maintain clearance without oral antibacterial therapy. Hormonal therapy Hormonal interventions in women may be beneficial even in the absence of abnormal laboratory tests. The workup for the woman with signs of hyperandrogenism, such as acne, menstrual irregularities, hirsutism, or androgenic alopecia, is presented earlier. Results take longer to be seen with these agents, with first evidence of improvement often not apparent for 3 months and continued improved response seen for at least 6 months. Women with acne primarily located on the lower face and neck and with deep-seated nodules that are painful and long-lasting are often quite responsive to hormonal intervention, which may be considered a first-line therapy in some women. One third of patients cleared, one third had marked improvement, one quarter showed partial improvement, and 7% had no response. Corticosteroids are effective in the treatment of adult-onset adrenal hyperplasia, but antiandrogens are often used in this setting. Prednisone Although corticosteroids may produce steroid acne, they are also effective anti-inflammatory agents in severe and intractable acne vulgaris. In severe cystic acne and acne conglobata, corticosteroid treatment is effective; however, side effects restrict its use. Prednisone is generally only given to patients with severe inflammatory acne during the first 1 or 2 months of treatment with isotretinoin, for initial reduction of inflammation, and to reduce isotretinoin-induced flares. Other hormonal agents Finasteride, flutamide, estrogen, gonadotropin-releasing agonists, and metformin (by decreasing testosterone levels) have all showed a beneficial effect on acne. Because of side effects, expense, and other considerations, however, these agents are not typically used. The progestins that these contain have either low androgenic activity or antiandrogenic activity. Oral retinoid therapy Isotretinoin Isotretinoin is approved only for severe cystic acne. However, it is useful in less severe forms of acne to prevent the need for continuous treatment and the repeated office visits often required. A consensus of experts found that oral isotretinoin is warranted for severe acne, poorly responsive acne that improves by less than 50% after 6 months of therapy with combined oral and topical antibiotics, acne that relapses after oral treatment, scars, and acne that induces psychological distress. Other indications are gram-negative folliculitis, inflammatory rosacea, pyoderma faciale, acne fulminans, and acne conglobata. For severe truncal acne in patients who tolerate higher doses, up to 2 mg/kg/day may be given. The product is the total number of 40-mg capsules needed to reach the low end of the dosage spectrum. These patients had a lower relapse rate, although side effects may limit tolerance of such dosages. The major advantage of isotretinoin is that it is the only acne therapy that is not open ended. Approximately one third of the relapsing patients will need only topical therapy, with the others requiring oral treatments. Many patients in the latter category prefer to be re-treated with isotretinoin because of its reliable efficacy and predictable side effects, which will be similar to those experienced in the first course. Many treated patients will require at least a second course of isotretinoin in 2 years.
Discount famciclovir 250 mg online
SusokL symptoms of hiv infection in toddlers discount 250 mg famciclovir free shipping,etal: Complete clearance of reticular erythematous mucinosis with quinacrine monotherapy. Histologically, follicular mucinosis demonstrates large collections of mucin within the sebaceous gland and outer root sheath. The additional finding of the presence of syringolymphoid hyperplasia should raise concern that lymphoma is or will become evident. T-cell receptor gene rearrangement studies that indicate clonality are also supportive but do not alone predict an aggressive course. Spontaneous involution of primary follicular mucinosis may occur, especially in young children. ZvulunovA,etal: Clinical and histopathologic spectrum of alopecia mucinosa/follicular mucinosis and its natural history in children. Lesions are asymptomatic and usually occur on the face, neck, trunk, or extremities. Histologically, the lesion is characterized by a loose dermal stroma containing large quantities of mucin together with numerous dendritic-shaped fibroblasts. The clinical appearance is not distinctive and at times may suggest a cyst, basal cell carcinoma, or neurofibroma. When a synovial cyst is present beneath the proximal nailfold, a characteristic groove may be formed in the nail plate by pressure of the lesion on the nail matrix. Those located beneath the nail cause a transverse nail curvature and a red or blue discoloration of the lunula. Nail integrity typically is compromised, leading to distal or longitudinal splitting or onycholysis. These cysts do not have an epithelial lining, but rather a compacted fibrous wall. The repeated puncture technique for cysts located beneath the proximal nailfold may achieve a cure rate of up to 70%, but multiple punctures (>40) may be required. Surgical approaches that reflect the skin overlying the cyst and either excise or tie off the communication to the joint, which may be visualized by injecting the myxoid cyst with methylene blue, have a cure rate greater than 90%. They may occur as asymptomatic swellings of the proximal nailfold, as subungual growths, or over the distal interphalangeal joint. Women are more frequently affected, and osteoarthritis is often present in the adjacent distal interphalangeal joint. Myxoid cysts that can be reduced with pressure communicate directly with the joint space. It is a chronic, superficial, inflammatory disease with a predilection for the scalp, eyebrows, eyelids, nasolabial creases, lips, ears. An oily type, pityriasis steatoides, is accompanied by erythema and an accumulation of thick crusts. Other types of seborrheic dermatitis on the scalp include arcuate, polycyclic, or petaloid patches and psoriasiform, exudative, or crusted plaques. The disease frequently spreads beyond the hairy scalp to the forehead, ears, postauricular regions, and neck. On these areas, the patches have convex borders and are reddish yellow or yellowish. In dark-skinned individuals, arcuate and petaloid lesions typically involve the hairline. In extreme cases, the entire scalp is covered by a greasy, dirty crust with an offensive odor. In infants, yellow or brown scaling lesions on the scalp, with accumulated adherent epithelial debris, are called "cradle cap. The edges of the lids may be erythematous and granular (marginal blepharitis), and the conjunctivae may be injected. If the glabella is involved, fissures in the wrinkles at the inner end of the eyebrow may accompany the fine scaling. In the nasolabial creases and on the alae nasi, there may be yellowish or reddish yellow scaling macules, sometimes with fissures. In the ears, seborrheic dermatitis may be mistaken for an infectious otitis externa. There is scaling in the aural canals, around the auditory meatus, usually with marked pruritus. In the axillae, the eruption begins in the apices, bilaterally, and later progresses to neighboring skin. This pattern resembles that of allergic contact dermatitis to deodorant, but differs from that of clothing dermatitis (which involves periphery of axillae but spares the vault). The involvement may vary from simple erythema and scaling to more pronounced petaloid patches with fissures. Seborrheic dermatitis is common in the groin and gluteal crease, where its appearance may closely simulate tinea cruris or candidiasis. In fact, many of these patients have an overlap of the two conditions (sebopsoriasis or 10 seborrhiasis) in the groin, as well as the scalp. The lesions may also become generalized and progress to an exfoliative erythroderma (erythroderma desquamativum), especially in infants. In adults, generalized eruptions may be accompanied by adenopathy and may simulate mycosis fungoides or psoriatic erythroderma. A unilateral injury to the innervation of the face, or a stroke, may lead to unilateral localized seborrheic dermatitis. Diabetes mellitus (especially in obese persons), sprue, malabsorption disorders, epilepsy, neuroleptic drugs. Etiologyandpathogenesis the etiology of this common disorder is complex but may be related to the presence of the lipophilic yeast Malassezia ovalis (Pityrosporum ovale), which produces bioactive indoles, oleic acid, malssezin, and indole-3-carbaldehyde. The density of yeast has been correlated with the severity of the disease, and reduction of the yeast occurs with response to therapy. Histology the epidermis demonstrates regular acanthosis with some thinning of the suprapapillary plates. A characteristic finding is the presence of a focal scale crust adjacent to the follicular ostia. Differentialdiagnosis Some cases of seborrheic dermatitis bear a close clinical resemblance to psoriasis, and the two conditions may overlap. Patients with psoriasis tend to have more pronounced erythema and heavier silvery scales that peel in layers. Characteristic psoriasis elsewhere (nail pitting, balanitis) may resolve the question. Impetigo of the scalp, especially when associated with pediculosis, may cause difficulty in differentiation. Scalp impetigo can be an indolent crusted dermatosis associated with failure to thrive. Langerhans cell histiocytosis may also resemble seborrheic dermatitis, but typically demonstrates yellow-brown perifollicular papules and groin fissuring. Crusted scabies of the scalp can also be confused with seborrheic dermatitis, and Trichophyton tonsurans often produces a subtle seborrheic scale. The antifungals are now available in a wide range of vehicles to include foams, gels, and liquids. Patients generally tolerate these agents better after initial treatment with a corticosteroid. An open, randomized, prospective, comparative study of topical pimecrolimus 1% cream versus topical ketoconazole 2% cream found the two to be equally effective, but side effects were somewhat more common with pimecrolimus. Preliminary studies suggest oral itraconazole and oral terbinafine may show some efficacy. When secondary bacterial infection is present, a topical or oral antibiotic may be required. Lithium gluconate 8% ointment has compared favorably with ketoconazole 2% emulsion in healthy adults and was more effective in terms of control of scaling and symptoms. Sodium sulfacetamide products, with or without sulfur, are effective in some refractory patients. For scalp disease, selenium sulfide, ketoconazole, tar, zinc pyrithione, fluocinolone, and resorcin shampoos are effective. In many patients, these agents may be used two to three times a week, with a regular shampoo used in between as required. White patients often prefer antifungal foams and gels, as well as corticosteroid solutions, foams, gels, and sprays, whereas some black patients prefer ointment or oil preparations. Some patients require the use of a class 1 corticosteroid on weekends to control refractory pruritus.
Diseases
- Mucormycosis
- Dwarfism mental retardation eye abnormality
- Schwartz lelek syndrome
- Hypo-alphalipoproteinemia primary
- Mehta Lewis Patton syndrome
- Cassia Stocco Dos Santos syndrome
- Temporomandibular ankylosis
- Bacterial vaginosis
Purchase 250mg famciclovir free shipping
Histologically hiv infection time frame buy 250 mg famciclovir free shipping, the lesions demonstrate a patchy superficial and deep perivascular and periadnexal lymphoid infiltrate that frequently affects the eccrine coil. Usually, the overlying skin is normal, but overlying discoid or tumid lesions may occur. Histologic sections demonstrate lymphoid nodules in the subcutaneous septa, necrosis of the fat lobule, and fibrinoid or hyaline degeneration of the remaining lipocytes. The overlying epidermis may show basal liquefaction and follicular plugging or may be normal. Dermal lymphoid nodules or vertical columns of lymphoid cells may be seen in fibrous tract remnants. Dermal mucin may be prominent, and dermal collagen hyalinization (resembling that seen in morphea) may be present. Important clues include the presence of lipocytes, rimmed by atypical lymphocytes with nuclear molding, and the presence of constitutional symptoms. Erythrophagocytosis may be present focally, and T-cell clonality can usually be demonstrated. Lesions are scaly and evolve as polycyclic annular lesions or psoriasiform plaques. The scale is thin and easily detached, and telangiectasia or dyspigmentation may be present. Follicles are not involved; the lesions tend to be transient or migratory, and there is no scarring. Lesions tend to occur on sun-exposed surfaces of the face and neck, the V portion of the chest and back. Skin involvement occurs in 80% of cases and is often helpful in arriving at a diagnosis. Neurologic disorders (seizures or psychosis in the absence of other known causes) 8. A dustlike particulate deposition of IgG in epidermal nuclei of Ro-positive patients may be present and is a helpful diagnostic finding. These infants have no skin lesions at birth, but develop them during the first few weeks of life. Telangiectasia or dermal mucinosis in an acral papular pattern may be the predominant findings in some cases. Telangiectatic macules or angiomatous papules may be found in sun-protected sites such as the diaper area, may occur independently of active lupus skin lesions, and may be persistent. The skin lesions usually resolve spontaneously by 6 months of age, and usually heal without significant scarring, although atrophy and telangiectatic mats may persist. Although the skin lesions are transient, half the patients have an associated isolated congenital heart block, usually third degree, which is permanent. In children with cutaneous involvement, thrombocytopenia and hepatic disease may occur as frequently as cardiac disease. Biopsies at all sites show interface dermatitis and a scant perivascular lymphoid infiltrate. Heterozygous deficiency of either complement component C4A or C4B has a frequency of approximately 20% in white populations. In bullous lesions, there is a subepidermal bulla or superficial dermal edema containing neutrophils. Neutrophils are found in or below the lamina densa on immunofluorescent electron microscopy. The recognition of this subset as distinct is made clear by its often dramatic therapeutic response to dapsone. Capillary loops in the Osler-WeberRendu syndrome demonstrate ectasia of half the capillary loop. The palms, soles, elbows, knees, or buttocks may become persistently erythematous or purplish, sometimes with overlying scale. Leg ulcers, typically deeply punched out and with very little inflammation, may be seen on the pretibial or malleolar areas. Many of these patients present with a livedoid pattern, and many have an antiphospholipid antibody. Sneddon syndrome is composed of livedo reticularis and strokes related to a hyalinizing vasculopathy. These reddish purple to skin-colored lesions are often present on the trunk and arms or head and neck. These skin-colored to erythematous lesions with a smooth, ulcerated or umbilicated surface may show vasculitis or, in older lesions, a palisaded granulomatous inflammation. This eruption has been referred to as palisaded neutrophilic and granulomatous dermatitis of immune complex disease. The earliest changes noted may be transitory or migratory arthralgia, often with periarticular inflammation. Arthralgia is often the earliest abnormality and may remain the sole symptom for some time. Thrombosis in vessels of various sizes and thromboembolism may be a recurring event. Renal involvement may be of either nephritic or nephrotic type, leading in either case to chronic renal insufficiency with proteinuria and azotemia. Pericarditis, the most frequent cardiac manifestation, and endocarditis also occur. Raynaud phenomenon occurs in about 15% of patients, who have less renal disease and consequently lower mortality. Coombs-positive hemolytic anemia, neutropenia, and lymphopenia are other hematologic findings. Pulmonary involvement with pleural effusions, interstitial lung disease, and acute lupus pneumonitis may be present. Overlap with any of the connective tissue diseases may be seen, occurring in approximately 25% of patients. Muscular atrophy may accompany extreme weakness so that dermatomyositis may be suspected. Myopathy of the vacuolar type may produce muscular weakness, myocardial disease, dysphagia, and achalasia of the esophagus. A history of exposure to excessive sunlight before the onset of the disease or before an exacerbation is sometimes obtained. Some patients may have only mild constitutional symptoms for weeks or months, but immediately after exposure to strong sunlight, they may develop the facial eruption and severe disease complications. The skin manifestations may be the typical butterfly eruption on the face and photosensitivity. In addition, there may be morbilliform, bullous, purpuric, ulcerating, or nodose lesions. Weight loss, fatigue, hepatosplenomegaly, lymphadenopathy, and fever are other manifestations. Risk of fetal death is increased in women with a previous history of fetal loss and anticardiolipin or anti-Ro antibodies. For the patient with these antibodies but without a history of previous fetal loss, the risk of fetal loss or neonatal lupus is low. Minimal credible data exist regarding other possible aggravating dietary factors, but some reports have implicated excess calories, excess protein, high fat (especially saturated and -6 polyunsaturated fatty acids), excess zinc, and excess iron. IgG levels may be high, the albumin/globulin ratio is reversed, and serum globulin is increased, especially the -globulin or 2 fraction. Linkage varies in different ethnic groups and different clinical subsets of lupus. Overproduction of -globulins by B cells and reduced clearance of immune complexes by the reticuloendothelial system may contribute to complement-mediated damage. These are associated with a syndrome that includes venous thrombosis, arterial thrombosis, spontaneous abortions, and thrombocytopenia. These antibodies may occur in association with lupus and other connective tissue disease, or as a solitary event. Thalidomide can be effective, but its use is limited by the risk of teratogenicity and neuropathy.
Order famciclovir overnight delivery
Pharmacologic agents hiv infection through food buy famciclovir 250mg on-line, such as pilocarpine and cevimeline, are helpful to stimulate salivation. In all trials, mechanical stimulation by the lozenge may play a significant role in improvement of symptoms, as reflected in a high placebo response. Acid maltose lozenges are less expensive and remain useful for symptomatic relief. Pilocarpine, in doses of 10 mg/day, has been shown to have a beneficial effect on subjective eye symptoms, as well as improvement of rose bengal staining. An increase in tear production, as measured by the Schirmer-I test, was not substantiated. There may be annular erythemas, purpura, bullae, shallow ulcers, and gangrene of the extremities. Biologic agents are being used with increasing frequency, although traditional drugs such as methotrexate still have a role. Of interest to dermatologists, extracts from the Rhus family of plants have shown some benefit in limited studies. Neutrophils and neutrophilic debris may be noted in association with the fibrin, and over time, the surrounding histiocytes are replaced by fibrosis. Rheumatoid nodules are differentiated from Heberden nodes, which are tender, hard, bony exostoses on the dorsolateral aspects of the distal interphalangeal joints of patients with degenerative joint disease. Nodules or tophi of gout are characterized by masses of feathery urate crystals surrounded by a chronic inflammatory infiltrate often containing foreign body giant cells. This variant of rheumatoid disease without destructive joint disease is designated "rheumatoid nodulosis. These are localized purpura, cutaneous ulceration, and gangrene of the distal parts of the extremities. Additionally, papular lesions located primarily on the hands have been described as rheumatoid papules. Prednisone and cytotoxic agents are frequently used, as in other forms of vasculitis. They may arise anywhere on the body but most frequently are found over the bony prominences, especially on the extensor surface of the forearm just below the elbow and the dorsal hands. The lesions are nontender, firm, skin-colored, round nodules, which may or may not be attached to the underlying tissue. Frequently, they are attached to the fibrous portions of the periarticular capsule, or they may be free in the subcutaneous tissue. Rheumatoid nodules can easily be mistaken for xanthomas because of a yellow color (pseudoxanthomatous variant). The differential diagnosis includes erythema elevatum diutinum and Sweet syndrome. Relatedpalisadinggranulomas Interstitial granulomatous dermatitis with arthritis is a condition with a range of clinical presentations. It can present with round to oval erythematous or violaceous plaques on the flanks, axillae, inner thighs, and lower abdomen. Severe systemic vasculitis causing renal disease has responded to corticosteroids with or without cyclophosphamide. Arthritis may occur before, during, or after the eruption and tends to affect multiple joints of the upper extremities. Some presentations are paraneoplastic, associated with a range of solid and hematopoietic tumors. Histologically, a moderate to dense inflammatory infiltrate is seen through the reticular dermis, composed mostly of histiocytes distributed interstitially around discrete bundles of sclerotic collagen. The eruption is typically asymptomatic and may spontaneously involute after many months or years. If therapy is required, intralesional corticosteroids, methotrexate, etanercept, ustekinumab, tocilizumab, and cyclosporine have been used. It often presents with eroded or ulcerated, symmetrically distributed umbilicated papules or nodules on the elbows, knuckles, and knees. The biopsy may reveal leukocytoclastic vasculitis and collagen degeneration in early lesions or palisaded granulomatous infiltrates with dermatofibrosis and scant neutrophilic debris in older lesions. Methotrexate-induced papular eruption appears in patients with rheumatic diseases during methotrexate therapy. They present with erythematous indurated papules, usually located on the proximal extremities. Histopathologic examination reveals an inflammatory infiltrate composed of histiocytes interstitially arranged between collagen bundles of the dermis, intermingled with few neutrophils. At times, small rosettes composed of clusters of histiocytes surrounding a thick, central collagen bundle are present in the deep reticular dermis. An eruption consisting of evanescent, nonpruritic, salmon-pink, macular, or papular lesions on the trunk and extremities may precede the onset of joint manifestations by many months. The systemic symptoms of fever and serositis usually recur over weeks each afternoon. The dose-response curve for methotrexate plateaus with parenteral administration of 15 mg/ m2/week. Refractory disease has been treated with pulse methylprednisolone, tocilizumab, and cyclophosphamide. Standard therapy includes immunosuppressive agents, typically methotrexate and oral corticosteroids, although some patients have responded to physical therapy without immunosuppressive treatment. Patients with new onset of rheumatologic disease should be screened for signs and symptoms suggesting neoplasm. Symmetricsynovitis Symmetric seronegative synovitis is an idiopathic form of arthritis sometimes associated with idiopathic edema. Both genders are equally affected, with age at onset usually in the fourth to fifth decade. During bouts of inflammation, the bright-red involvement of the ears is confined to the cartilaginous portion while the earlobes remain conspicuously normal. There may be conductive deafness as a result of the obstruction produced by the swollen cartilage. The nasal septal cartilage is similarly involved to produce rhinitis, with crusting and bleeding and eventually saddle nose. Involvement of the bronchi, larynx, and epiglottis produces hoarseness, coughing, and dyspnea. Patients evaluated for chest pain are often released without treatment and with a diagnosis of costochondritis. Cell-mediated immunity to cartilage has been demonstrated in vitro, with a degree of response correlated with disease activity. A second connective tissue disease or other autoimmune disease is present in about one third of patients with relapsing polychondritis, and some cases appear to be paraneoplastic, occurring in association with hematopoietic malignancies. Histologically, a predominantly neutrophilic infiltrate is noted in the perichondrium. Dapsone, 100 mg once or twice daily for an adult, reduces the frequency of flares but is usually inadequate to control relapsing polychondritis. Sustained response to etanercept has been reported, even after failure to respond to infliximab. Endobronchial ultrasonography has been used to facilitate the diagnosis of relapsing polychondritis and estimate the size of the involved airway for placement of stents. These acid mucopolysaccharides, produced by fibroblasts, are highly hygroscopic, binding about 1000 times their own volume in water. They are critical in holding water in the dermis and are responsible for dermal volume and texture. Normally, the sulfated acid mucopolysaccharide chondroitin sulfate and heparin are the primary dermal mucins. In certain diseases, fibroblasts produce abnormally large amounts of acid mucopolysaccharides, usually hyaluronic acid. These acid mucopolysaccharides (mucin) accumulate in large amounts in the dermis and may be visible as pale-blue, granular or amorphous material between collagen bundles. They are often not visualized with hematoxylin and eosin stains because the water they bind is removed in processing, so the presence of increased mucin is suspected by the presence of large, empty spaces between the collagen bundles.
Buy famciclovir now
Snails and other water animals eat the contaminated plants antiviral drink generic famciclovir 250mg otc, and carnivorous insects eat the plant-consuming molluscs. When these insects bite a human, they inoculate the mycobacteria into the host and begin the infection. Infection in the human is again associated with the production of the biofilm, which makes treatment difficult. This explains the association between infection and exposure to water, especially swampy water. Interestingly, being repeatedly bitten by these carnivorous insects results in the production of antibodies against the insect salivary contents. Whether the mosquitoes carry the infection by the same mechanism as the carnivorous water insects is unknown. Preulcerative lesions give the highest culture results, because ulcerative lesions contain fewer organisms and are contaminated. Daily observed treatment for 8 weeks with streptomycin, 15 mg/kg intramuscularly, and rifampin, 10 mg/kg orally, is dramatically effective. The overall efficacy of this treatment regimen was 73% of patients and 96% in lesions less than 10 cm in diameter (early lesions) without surgery. Healing is slow, with half of lesions healing by 24 weeks (with only 8 weeks of antibiotic treatment) and some requiring more than 9 months to heal. In larger lesions (>15 cm) and in lesions failing antibiotic treatment alone, surgical excision with delayed grafting is the standard treatment offered. In a large series of more than 200 patients, all patients who completed the full course of antibiotics with or without surgery were cured-a success rate of 100% by 3 months after the antibiotics were completed. Severe scarring can result from untreated and large lesions, leading to contracture deformity or amputation. Bone lesions are uncommon and in three quarters of patients, occur at a site distant from the primary Buruli ulcer. Papules, plaques (at times cellulitis-like), and dermal or subcutaneous nodules are the primary lesions. Cutaneous infections after acupuncture, following application of permanent eyebrow makeup, and within tattoos have been reported in immunocompetent and immunosuppressed patients. Rapidlygrowingmycobacteria the organisms of the Mycobacterium fortuitum group and M. Others progress to large, fluctuant abscesses, which are quite painful and can ulcerate. It is distinct taxonomically, similar in epidemiology, but is distinguished by its susceptibility to cefoxitin. Only occasional reports of immunocompetent patients with inoculation-type lesions have been reported. Therapy for disseminated infection is undertaken with at least three agents, most often clarithromycin or azithromycin, ethambutol, and rifabutin. In renal transplant patients, tender, nodular lesions of the legs are most common. Since these infections on the skin are indolent and the organisms grow rapidly, waiting for susceptibilities can be considered. Monotherapy may allow resistance to occur, but this rarely happens in immunocompetent patients with simple skin infections. In severe cases and in the setting of immunosuppression, combination treatment should be used. Tobramycin, amikacin, linezolid, clarithromycin, and tigecycline have the highest percentage of susceptible isolates Mycobacterium kansasii Mycobacterium kansasii rarely causes skin infection, usually after minor trauma. Treatment is not standardized, but initial treatment with isoniazid, rifampin, and ethambutol until 12 months after clearing has been proposed. However, individual cases have responded to single-agent therapy with minocycline or erythromycin. In immunosuppressed patients, cutaneous lesions can occur through hematogenous dissemination, and a visceral source, especially pulmonary, should be sought. ChanyA-C,etal: History, biology and chemistry of Mycobacterium ulcerans infections (Buruli ulcer disease). ConejeroR,etal: Infeccion por Mycobacterium chelonae en paciente en tratamiento con adalimumab. DucharletK,etal: Recurrent Mycobacterium haoemophilum in a renal transplant recipient. EberstE,etal: Epidemiological, clinical, and therapeutic pattern of Mycobacterium marinum infection. FowlerJ,etal: Localized cutaneous infections in immunocompetent individuals due to rapidly growing mycobacteria. GiulieriS,etal: Outbreak of Mycobacterium haemophilum infections after permanent makeup of the eyebrows. Guevara-PatinoA,etal: Soft tissue due to Mycobacterium fortuitum following acupuncture: a case report and review of the literature. JacobsS,etal: Disseminated Mycobacterium marinum infection in a hematopoietic stem cell transplant recipient. LopezAventinD,etal: Mycobacterium fortuitum infection in continuous subcutaneous insulin infusion sites. MacenteS,etal: Disseminated folliculitis by Mycobacterium fortuitum in an immunocompetent woman. NakanagaK,etal: Nineteen cases of Buruli ulcer diagnosed in Japan from 1980 to 2010. QuinonesC,etal: An outbreak of Mycobacterium fortuitum cutaneous infection associated with mesotherapy. Elimination (not eradication) is considered as a prevalence of less than 1 case in 10,000 persons in any country. In the southeastern states, cases may be related to exposure to armadillos, a natural host for the infectious agent. It is believed that more than 90% of persons exposed to Mycobacterium leprae are able to resist infection. Thus, although many persons can be transiently infected, they apparently are able to resist overt clinical infection. Numerous genes have been identified as possibly conferring susceptibility to infection with M. Different genes have been identified in different populations, suggesting that multiple genetic causes of susceptibility to infection are possible with M. The latency period between exposure and overt signs of disease is usually 5 years for paucibacillary cases and an average of 10 years in multibacillary cases. Rarely, tattooing or other penetrating injury to the skin can be the route of infection. Multibacillary cases are much more infectious than paucibacillary cases, so the nature of the source case is the most important factor in transmission. This is a weakly acid-fast organism that has not been successfully cultured in vitro. The organism may be cultivated in mouse footpads and most effectively in armadillos, whose lower body temperature is more optimal for growth of M. In infected tissues, the leprosy bacillus favors intracellular locations, within macrophages and nerves. The genome of the leprosy bacillus has been sequenced and compared to its close relative, the tuberculous bacillus. Biopsies from skin or nerve lesions, stained for the bacillus with Fite-Faraco stain, are usually performed in the developed world. Smears are taken from lesions and cooler areas of the skin, such as the earlobes, elbows, and knees. If the results of skin smears are negative (and there are five or fewer lesions), the patient is called paucibacillary. Nerve involvement is detected by enlargement of peripheral nerves and lesional loss of sensation.
Cheap famciclovir 250mg line
CoreyL hiv infection after 1 year symptoms cheap 250mg famciclovir with amex,etal: Once-daily valacyclovir to reduce the risk of transmission of genital herpes. ElangovanS,etal: Hospital-based emergency department visits with herpetic gingivostomatitis in the United States. GarceauR,etal: Herpes simplex virus type 1 is the leading cause of genital herpes in New Brunswick. GazzolaR,etal: Herpes virus outbreaks after dermal hyaluronic acid filler injections. HirokawaD,etal: Treatment of recalcitrant herpes simplex virus with topical imiquimod. KanY,etal: Imiquimod suppresses propagation of herpes simplex virus 1 by upregulation of cystatin A via the adenosine receptor A1 pathway, J Virol 2012; 86:10338. KimM,etal: Topical calcineurin inhibitors compromise stratum corneum integrity, epidermal permeability and antimicrobial barrier function. KoheletD,etal: Herpes simplex virus infection after vacuum-assisted vaginally delivered infants of asymptomatic mothers. KotzbauerD,etal: Clinical and laboratory characteristics of central nervous system herpes simplex virus infection in neonates and young infants. LautenschlagerS,EichmannA: Urethritis: an underestimated clinical variant of genital herpes in men LubbeJ,etal: Adults with atopic dermatitis and herpes simplex and topical therapy with tacrolimus: what kind of prevention MulunehB,etal: Successful clearance of cutaneous acyclovir-resistant, foscarnet-refractory herpes virus lesions with topical cidofovir in an allogeneic hematopoietic stem cell transplant patient. PichlerM,etal: Premature newborns with fatal intrauterine herpes simplex virus-1 infection: first report of twins and review of the literature. SchoenfeldJ,etal: Cutaneous co-infected cytomegalovirus and herpes simplex virus perigenital ulcers in human immunodeficiency virus patients. TakahashiR,etal: Pathological role of regulatory T cells in the initiation and maintenance of eczema herpeticum lesions. TuokkoH,etal: Herpes simplex virus type 1 genital herpes in young women: current trend in Northern Finland. WollenbergA,etal: Predisposing factors and clinical features of eczema herpeticum: a retrospective analysis of 100 cases. YossepowitchO,etal: Penile herpes simplex virus type 1 infection presenting two and a half years after Jewish ritual circumcision of an infant. Varicella Varicella, commonly known as chickenpox, is the primary infection with the varicella-zoster virus. More than 90% of adults in temperate countries have evidence of prior infection and are "immune" to varicella. In tropical countries, however, varicella tends to be a disease of teenagers, and only 60% of adults are "immune" serologically. Transmission is by the respiratory route and less often by direct contact with the lesions. A susceptible person may develop varicella after exposure to the lesions of herpes zoster. There is an initial viral replication in the nasopharynx and conjunctiva, followed by viremia and infection of the reticuloendothelial system (liver, spleen) between days 4 and 6. The severity of the disease is age dependent, with adults having more severe disease and a greater risk of visceral disease. As with most viral infections, immunosuppression may worsen the course of the disease. Lifelong immunity follows varicella, and second episodes of "varicella" indicate either immunosuppression or another viral infection such as coxsackievirus. The eruption starts with faint macules that develop rapidly into vesicles within 24 h. Successive fresh crops of vesicles appear for a few days, mainly on the trunk, face, and oral mucosa. Initially, the exanthem may be limited to sunexposed areas, the diaper area of infants, or sites of inflammation. Since the lesions appear in crops, lesions of various stages are present at the same time, a useful clue to the diagnosis. Lesions tend not to scar, but larger lesions and those that become secondarily infected may heal with a characteristic round, depressed scar. Secondary bacterial infection with Staphylococcus aureus or a streptococcus is the most common complication of varicella. Rarely, it may be complicated by osteomyelitis, other deep-seated infections, or septicemia. Pneumonia is uncommon in normal children but is seen in 1 in 400 adults with varicella. Asymptomatic myocarditis and hepatitis may occur in children with varicella, but rarely are significant and resolve spontaneously with no treatment. Reye syndrome, with hepatitis and acute encephalopathy, is associated with the use of aspirin to treat the symptoms of varicella. Any child with varicella and severe vomiting should be referred immediately to exclude Reye syndrome. Symptomatic thrombocytopenia is a rare manifestation of varicella, which can occur either with the exanthem or several weeks after. Purpura fulminans, a form of disseminated intravascular coagulation associated with low levels of proteins C and S, may complicate varicella. Tzanck smear from a vesicle will usually show characteristic multinucleate giant cells. Therapy does not seem to alter the development of adequate immunity to reinfection. Because the complications of varicella are infrequent in children, routine treatment is not recommended; therapeutic decisions are made on a case-by-case basis. Acyclovir therapy appears mainly to benefit secondary cases within a household, which tend to be more severe than the index case. Therapy does not return children to school sooner, however, and the impact on parental workdays missed is not known. The dose of acyclovir is 20 mg/kg, maximum 800 mg per dose, four times daily for 5 days. Aspirin and other salicylates should not be used as antipyretics in varicella because their use increases the risk of Reye syndrome. Topical antipruritic lotions, oatmeal baths, dressing the patient in light, cool clothing, and keeping the environment cool may all relieve some of the symptomatology. Children living in warm homes and kept very warm with clothing have anecdotally been observed to have more numerous skin lesions. Smokers and those with preexisting lung disease (but not asthma) are at increased risk. Adults with varicella and at least one other risk factor should be evaluated with physical examination, pulse oximetry, and chest radiography. Antiviral treatment is recommended in all adolescents and adults (13 and older) with varicella. Patients with varicella should not be admitted to wards with immunocompromised hosts or to pediatric wards, but rather are best placed on wards with healthy patients recovering from acute trauma. All varicella in pregnancy should be treated with oral acyclovir, 800 mg five times daily for 7 days, except perhaps during the first month, when a specialist should be consulted. Its use should be limited to seronegative women because of its cost and the high rate of asymptomatic infection in U. The lack of a history of prior varicella is associated with seronegativity in only 20% or fewer of the U. Infection of the fetus in utero may result in zoster occurring postnatally, often in the first 2 years of life.
Cherokee Rosehip. Famciclovir.
- Dosing considerations for Cherokee Rosehip.
- Male sexual dysfunction, gynecologic problems, night sweats, frequent urination, bedwetting, chronic cough, high blood pressure, diarrhea, intestinal swelling (inflammation), and other conditions.
- Are there safety concerns?
- What is Cherokee Rosehip?
- Are there any interactions with medications?
- How does Cherokee Rosehip work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96865
Generic famciclovir 250 mg on line
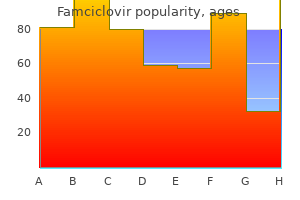
Acne typically begins at puberty and is often the first sign of increased sex hormone production antiviral ppt discount 250 mg famciclovir fast delivery. It may remain mild in its expression, with only an occasional inflammatory papule. However, as hormone levels rise into the middle teenage years, more severe inflammatory pustules and nodules occur, with spread to other sites. Young men tend to have an oilier complexion and more severe widespread disease than young women. Women may experience a flare of their papulopustular lesions about 1 week before menstruation. This acne frequently manifests as papules, pustules, and deep, painful, persistent nodules on the jawline, chin, and upper neck. Acne is primarily a disease of the adolescent, with 85% of all teenagers being affected to some degree. Generally, involution of the disease occurs before age 25; however, great variability in age at onset and of resolution occurs. About 12% of women and 3% of men will continue to have clinical acne until age 44. Neonatal acne is a common condition that develops a few days after birth, has male preponderance, and is characterized by transient facial papules or pustules that usually clear spontaneously in a few days or weeks. Infantile acne includes cases that persist beyond the neonatal period or that have an onset after the first 6 weeks of life. Most neonatal acne patients remit by age 1 year, although occasionally cases extend into childhood and through puberty. In prolonged cases, topical benzoyl peroxide, erythromycin, or the retinoids may be effective. With more inflammatory disease, oral erythromycin, 125 mg twice daily, or trimethoprim, 100 mg twice daily, may be added to topical medications. Midchildhood acne may evolve from persistent infantile acne or begin after age 1 year. Grouped comedones, papules, pustules, and nodules can occur alone or in any combination, usually limited to the face. The duration is variable, from a few weeks to several years, and occasionally extends into more severe pubertal acne. A pediatric endocrinology workup is indicated for midchildhood acne and for earlier-onset patients with physical findings suggestive of a hormonal disorder, such as sexual precocity, virilization, or growth abnormality. This is the time of adrenarche, and unless there are signs of androgen excess, no workup is needed. Pathogenesis Acne vulgaris is exclusively a follicular disease, with the principal abnormality being comedo formation. It is produced by the impaction and distention of the follicles with a keratinous plug in the lower infundibulum. The keratinous plug is caused by hyperproliferation and abnormal differentiation of keratinocytes of unknown causes. Androgens, alterations in lipid composition, and an abnormal response to local cytokines are all hypothesized to be important. Acne begins after sebum secretion increases, and women with hyperandrogenic states often manifest acne, along with hirsutism and menstrual abnormalities. Treatment directed at reducing sebaceous secretion, such as isotretinoin, estrogens, or antiandrogens, is effective in clearing acne. Disruption of the follicular epithelium permits discharge of the follicular contents into the dermis. The combination of keratin, sebum, and microorganisms, particularly Propionibacterium acnes, leads to the release of proinflammatory mediators and the accumulation of lymphocytes, neutrophils, and foreign body giant cells. This in turn causes the formation of inflammatory papules, pustules, and nodulocystic lesions. Additional factors may exacerbate acne or, in a predisposed patient, cause the onset of acne. Comedogenic greasy or occlusive products such as hair pomades may induce closed comedones and at times inflammatory lesions. Other types of cosmetics may initiate or worsen acne, but acne cosmetica is uncommon because most cosmetics are tested for comedogenicity. Acne neonatorum is explained by infantile production of androgens, which wanes at 6 to 12 months. Occasional patients have persistent acne, although acne developing after age 1 and before age 7 (with onset of adrenarche) may be a form of acne cosmetica, acne venenata, or drug-induced acne or part of an endocrinologic disorder. A workup should be initiated if acne develops between ages 1 and 7 and no obvious external factor is present. In the absence of any discovered abnormalities, the qualitative or quantitative alteration of cutaneous androgen, metabolism, and increased end-organ sensitivity could be postulated as pathogenic mechanisms for preadolescent acne. Pathology Comedones reveal a thinned epithelium and a dilated follicular canal filled with lamellar lipid-impregnated keratinous material. In pustular cases, there are folliculocentric abscesses surrounded by a dense inflammatory exudate of lymphocytes and polymorphonuclear leukocytes. In addition to these findings, indolent nodular lesions frequently show plasma cells, foreign body giant cells, and proliferation of fibroblasts. A key feature of mechanical or frictional acne is an unusual distribution of the acne lesions. Provocative factors include chin straps, violins, hats, collars, surgical tape, orthopedic casts, chairs, and seats. One acne patient who had laser hair removal developed flares of inflammatory lesions localized to the acne-prone sites after each laser session; the legs and abdomen were spared. All these factors are likely to irritate the follicular epithelium and exacerbate the changes that lead to comedogenesis and follicular rupture. Prophylactic measures designed to interdict these various mechanical forces are beneficial. In all women or children with acne, the possibility of a hyperandrogenic state should be considered. In women, the presence of irregular menses, hirsutism, seborrhea, acanthosis nigricans, or androgenic alopecia increases the likelihood of finding clinically significant hyperandrogenism. Additionally, gynecologic endocrine evaluation may be indicated in women who have acne resistant to conventional therapy, who relapse quickly after a course of isotretinoin, or who experience sudden onset of severe acne. It is not clear that screening for adult-onset 21-hydroxylase deficiency improves patient outcome. The dose, timing, combinations, side effects, and response to interventions should be obtained. Corticosteroids, anabolic steroids, neuroleptics, lithium, and cyclosporine may worsen acne. A family history of acne and, if present, its tendency to scarring should be noted. Women should be queried regularly about menstrual irregularities and hair growth in a male pattern, as well as use of cosmetics. Treatment may fail because of drug interactions, coexisting conditions, or antibiotic resistance, but the most common and important cause is lack of adherence to the treatment plan. Utilizing medications that are well tolerated, have convenient dosing regimens, and are cosmetically acceptable will help. However, thorough patient education is essential: explaining how lesions form, defining the expected response to and the duration and side effects of treatment, and giving clear, unambiguous instructions. Patients should know the difference between active inflammatory lesions and the purplish red or hyperpigmented macules of inactive resolved lesions. Topical application should be to the entire affected area rather than to specific lesions, and oral and topical medications should be used daily as preventive treatment.
Order famciclovir 250mg with amex
Routine "age-appropriate screening" may be inadequate to uncover a significant number of malignancies hiv infection rates canada buy famciclovir 250mg fast delivery. Periodic rescreening may be of value, but the appropriate interval for screening has not been established. The presence of leukocytoclastic vasculitis might indicate a higher potential for malignancy. The more common Brunsting type has a slow course, progressive weakness, calcinosis, and steroid responsiveness. Internal malignancy is seldom seen in children with either type, but insulin resistance may be present. The deltoid, trapezius, and quadriceps muscles seem to be almost always involved and are good biopsy sites. Muscle bundles demonstrate lymphoid inflammation and atrophy, which preferentially affects the periphery of the muscle bundle. This has also been demonstrated in patients with other connective tissue diseases, such as scleroderma. The finding may be an epiphenomenon or may be part of a pathogenic alloimmune response. Viral or bacterial infections may produce an abnormal immune response, and human herpesvirus 6 reactivation has been reported. Cases associated with terbinafine may be related to apoptosis induced by the drug. Cytoid bodies are often seen, although continuous granular staining with IgG, IgM, and IgA may be seen. X-ray studies with barium swallow may show weak pharyngeal muscles and a collection of barium in the piriform sinuses and valleculae. Aldosteronism, with adenoma of adrenal glands and hypokalemia, may also cause puffy heliotrope eyelids and face. Etanercept has also been used, but some studies have found little improvement or flares of muscle disease. Onset of calcinosis is associated with delays in diagnosis and treatment, as well as longer disease duration. The skin lesions may respond to systemic therapy; however, response is unpredictable, and skin disease may persist despite involution of the myositis. In pregnant patients who require treatment, evidence supports the use of topical corticosteroids and topical calcineurin inhibitors. Published evidence also suggests that systemic corticosteroids, hydroxychloroquine, and azathioprine may be used in pregnancy when necessary. Cutaneous types may be categorized as morphea (localized, generalized, profunda, atrophic, and pansclerotic types) or linear scleroderma (with or without melorheostosis or hemiatrophy). Early aggressive therapy in juvenile cases is associated with a lower incidence of disabling calcinosis cutis. Cutaneoustypes Localizedmorphea the morphea form of scleroderma is twice as common in women as men and occurs in childhood as well as adult life. It presents most often as macules or plaques a few centimeters in diameter, but also may occur as bands or in guttate lesions or nodules. The margins of the areas are generally surrounded by a lilac border or by telangiectases. Within the patch, skin elasticity is lost, and when it is picked up between the thumb and index finger, it feels rigid. The follicular orifices may be unusually prominent, leading to a condition that resembles pigskin. In guttate morphea, multiple small, chalk-white, flat or slightly depressed macules occur over the chest, neck, shoulders, or upper back. Panscleroticmorphea Pansclerotic morphea manifests as sclerosis of the dermis, panniculus, fascia, muscle, and at times the bone. Morpheaprofunda Morphea profunda involves deep subcutaneous tissue, including fascia. There is clinical overlap with eosinophilic fasciitis, eosinophilia myalgia syndrome, and the Spanish toxic oil syndrome. The latter two conditions were related to contaminants found in batches of tryptophan or cooking oil. Unlike eosinophilic fasciitis, morphea profunda shows little response to corticosteroids and tends to run a more chronic debilitating course. Linearscleroderma these linear lesions may extend the length of the arm or leg and may follow lines of Blaschko. Lesions may also occur parasagittally on the frontal scalp and extend partly down the forehead (en coup de sabre;. The Parry-Romberg syndrome, which manifests as progressive hemifacial atrophy, epilepsy, exophthalmos, and alopecia, may be a form of linear scleroderma. When the lower extremity is involved, there may be associated spina bifida, faulty limb development, hemiatrophy, or flexion contractures. Melorheostosis, seen on radiographs as a dense, linear cortical hyperostosis, may occur. Physical therapy of the involved limb is of paramount importance to prevent contractures and frozen joints. Generalizedmorphea Widespread involvement by indurated plaques with pigmentary change characterizes generalized morphea. Patients may lose their wrinkles as a result of the firmness and contraction of skin. Spontaneous involution is less common with generalized morphea than with localized lesions. The disease consists of brownish gray, oval, round or irregular, smooth atrophic lesions depressed below the level of the skin, with a welldemarcated, sharply sloping border. Some of the appearance of depression is an optical illusion related to the color change. Linear atrophoderma of Moulin is a related condition that follows lines of Blaschko. Biopsies of atrophoderma demonstrate a reduction in the thickness of the dermal connective tissue. Because the changes may be subtle, a biopsy should include normalappearing skin so that a comparison may be made. Patients may present with sclerodactyly, severe heartburn, or telangiectatic mats. The mats tend to have a smooth outline, in contrast to the mats of the Osler-Weber-Rendu syndrome, which tend to exhibit an irregular outline with more radiating vessels. Digital pitting scars of the fingertips or loss of substance of the distal finger pad 3. Bilateral basilar pulmonary fibrosis Localized forms of scleroderma must be excluded. These criteria have been shown to be 97% sensitive and 98% specific for the diagnosis. Skin changes: tightness, thickening, and nonpitting induration, sclerodactyly, proximal scleroderma; changes proximal to the metacarpophalangeal or metatarsophalangeal joints and affecting other parts of the extremities, face, neck, or trunk (thorax or abdomen), digital pitting, loss of substance from the finger pad, bilateral firm but pitting finger or hand edema, abnormal skin pigmentation (often "pepper and salt"). The changes are usually bilateral and symmetric and almost always include sclerodactyly. Raynaud phenomenon: at least two-phase color change in fingers and often toes consisting of pallor, cyanosis, and reactive hyperemia 3. Visceral manifestations: bibasilar pulmonary fibrosis not attributable to primary lung disease, lower (distal) esophageal dysphagia, lower (distal) esophageal dysmotility, colonic sacculations Skin findings In the earlier phases of scleroderma, affected areas are erythematous and swollen. The skin becomes smooth, yellowish, and firm and shrinks so that the underlying structures are bound down. The earliest changes often occur insidiously on the face and hands, and in more advanced stages, these parts become "hidebound," so the face is expressionless, the mouth is constricted. The facial skin appears drawn, stretched, and taut, with loss of lines of expression.
Proven 250mg famciclovir
Appropriate antibiotics antiviral lip cream purchase 250mg famciclovir fast delivery, surgical drainage, and surgical excision are methods used to treat botryomycosis. Blastomycosis-likepyoderma Large, verrucous plaques with elevated borders and multiple pustules occur. Most patients with blastomycosis-like pyoderma have some underlying systemic or local host compromise. Antibiotics appropriate for the organism isolated are curative; however, response may be delayed and prolonged therapy required. Pyomyositis Staphylococcus aureus abscess formation within the deep, large, striated muscles usually presents with fever and muscle pain. Pyomyositis is more common in the tropics, where it may affect adults but most frequently occurs in children. Swelling and occasionally erythema or yellow or purplish discoloration are visible signs of pyomyositis, but these are late findings. Drainage of the abscess and appropriate systemic antibiotics are the recommended treatment. Impetigocontagiosa Impetigo contagiosa is a staphylococcal, streptococcal, or combined infection characterized by discrete, thin-walled vesicles that rapidly become pustular and then rupture. Impetigo occurs most frequently on the exposed parts of the body: the face, hands, neck, and extremities. The disease begins with 2-mm erythematous macules, which may shortly develop into vesicles or bullae. As soon as these lesions rupture, a thin, straw-colored, seropurulent discharge is noted. The exudate dries to form loosely stratified, goldenyellow crusts, which accumulate layer upon layer until they are thick and friable. The crusts can usually be removed readily, leaving a smooth, red, moist surface that soon collects droplets of fresh exudate again; these are spread to other parts of the body by fingers or towels. As the lesions spread peripherally and the skin clears centrally, large circles are formed by fusion of the spreading lesions to produce gyrate patterns. In streptococcal-induced impetigo, regional lymphadenopathy is common, but not serious. Streptococci may represent an early pathogen in the development of impetigo, with staphylococci replacing streptococci as the lesion matures. Group B streptococci are associated with newborn impetigo, and groups C and G are rarely isolated from impetigo, unlike the usual group A. Common sources of infection for children are pets, dirty fingernails, and other children in schools, day care centers, or crowded housing areas; sources for adults include infected children and self-inoculation from nasal or perineal carriage. Nephritogenic streptococci are generally associated with impetigo rather than with upper respiratory tract infections. The circinate patches are frequently mistaken for ringworm, but clinically are quite different. Impetigo is characterized by superficial, very weepy lesions covered by thick, bright-yellow or orange crusts with loose edges, which do not resemble the scaling patches with peripheral erythema seen in tinea. Impetigo may be mistaken for Toxicodendron dermatitis, but it is more crusted and pustular and more likely to involve the nostrils, corners of the mouth, and ears. Treatment Systemic antibiotics combined with topical therapy are recommended for patients with impetigo contagiosa. It is necessary to soak off the crusts frequently, after which an antibacterial ointment should be applied. If the lesions are localized, especially if facial, and are present in an otherwise healthy child, topical therapy may be effective as the sole treatment. Applying antibiotic ointment as a prophylactic to sites of skin trauma will prevent impetigo in high-risk children attending day care centers. In one study, infections were reduced by 47% with antibiotic ointment versus 15% with placebo. Additionally, if recurrent staphylococcal impetigo develops, a culture of the anterior nares may yield this organism. Bullousimpetigo the bullous variety of impetigo occurs characteristically in newborns, although it may occur at any age. In most cases, the disease begins between the fourth and tenth days of life with the appearance of bullae, which may appear on any part of the body. Constitutional symptoms are absent at first, but weakness and fever or a subnormal temperature may be present later. When these rupture, they leave circinate, weepy, or crusted lesions, and in this stage it may be called impetigo circinata. Children with bullous impetigo may give a history of an insect bite at the site of onset of lesions. It occurs rarely in adults, usually with renal compromise or immunosuppression as a predisposing factor. They also extend far beyond areas of actual staphylococcal infection, by action of the exfoliative exotoxins types 250 A and B, elaborated by the staphylococcus in remote sites. Usually, staphylococci are present at a distant focus, such as the pharynx, nose, ear, or conjunctiva. Generalized exfoliation follows within the next hours to days, with large sheets of epidermis separating. If taken, cultures should be obtained from the mucous membranes because the skin erythema and desquamation are caused by the distant effects of the exfoliative toxins, unlike in bullous impetigo, where S. Treatment of choice is a penicillinase-resistant penicillin such as dicloxacillin combined with fluid therapy and general supportive measures. Currently, cases are most often caused by infections in wounds, catheters, contraceptive diaphragms, or nasal packing. Mortality in these nonmenstrual cases is higher (up to 20%) compared with menstrual-related cases (<5%), probably as a result of delayed diagnoses. Also, a similar syndrome has been defined in which the cause is group A, or rarely group B, streptococci. The streptococci are usually of M-types 1 and 3, with 80% of the isolates producing pyrogenic exotoxin A. In addition, serologic tests for Rocky Mountain spotted fever, leptospirosis, and rubeola, and cultures of blood, urine, and cerebrospinal fluid should be negative. Procalcitonin, an indicator of severe bacterial infection, may be a biologic marker for the toxic shock syndromes. Cases now usually occur in women using contraceptive sponges, in patients with nasal packing after rhinoplasty, and in patients with staphylococcal infections of bone, lung, or soft tissue. Histologic findings are spongiosis and neutrophils scattered throughout the epidermis, individual necrotic keratinocytes, perivascular and interstitial infiltrates composed of lymphocytes and neutrophils, and edema of the papillary dermis. AntoniouT,etal: Prevalence of community-associated methicillinresistant Staphylococcus aureus colonization in men who have sex with men. DattaR,etal: Risk of infection and death due to methicillin-resistant Staphylococcus aureus in long-term carriers. DuruptF,etal: Prevalence of Staphylococcus aureus toxins and nasal carriage in furunculosis and impetigo. OuchiT,etal: A case of blastomycosis-like pyoderma caused by mixed infection of Staphylococcus epidermidis and Trichophyton rubrum. PiechowiczL,etal: Outbreak of bullous impetigo caused by Staphylococcus aureus strains of phage type 3C/71 in a maternity ward linked to nasal carriage of a healthcare worker. VanRijenM,etal: Mupirocin ointment for preventing Staphylococcus aureus infections in nasal carriers. The lesions tend to heal after a few weeks, leaving scars, but rarely may proceed to gangrene when resistance is low. Treatment is cleansing with soap and water after soaking off the crust with compresses, followed by the application of mupirocin, retapamulin, or bacitracin ointment, twice daily. Scarletfever Scarlet fever is a diffuse, erythematous exanthem that occurs during the course of streptococcal pharyngitis.
Cheap generic famciclovir uk
CallewaertB hiv infection rate condom purchase famciclovir online,etal: Comprehensive clinical and molecular analysis of 12 families with type 1 recessive cutis laxa. The condition may affect young adults, in whom a preceding inflammatory phase presents with episodes of lid swelling. Biopsy shows lack of elastic fibers, and abundant IgA deposits have been demonstrated in some cases, possibly binding to fibulin and fibronectin. Sequelae include excess thin skin, fat herniation, lacrimal gland prolapse, ptosis, blepharophimosis, pseudoepicanthic fold, proptosis, conjunctival injection and cysts, entropion, and ectropion. Ascher syndrome consists of progressive enlargement of the upper lip and blepharochalasis. The minor salivary glands of the affected areas are inflamed, resulting in superfluous folds of mucosa, giving the appearance of a double lip. Treatment is generally by surgical correction, although successful medical treatment has been reported with systemic acetazolamide in combination with topical hydrocortisone cream. KaraconjiT,etal: Doxycycline for treatment of blepharochalasis via inhibition of matrix metalloproteinases. The usual locations are the trunk, especially on the shoulders, the upper arms, and thighs. Screening for antiphospholipid antibodies is of particular importance because these may produce a prothrombotic state, and some patients fulfill criteria for the antiphospholipid syndrome. The antibodies may be detected as anticardiolipin antibodies, anti-2glycoprotein-I antibodies, or a lupus anticoagulant. Patients may experience recurrent fetal loss, recurrent strokes, or recurrent deep vein thrombosis. Anetoderma of prematurity (congenital anetoderma) occurs in premature infants and may be related to pressure, adhesives, or changes in flow of ions or water under monitor leads. In the acute stage, a neutrophilic, lymphoid, or granulomatous response may be noted. Ablative laser treatment has been reported as helpful in some patients with anetoderma. Striae occur in response to changes in weight or muscle mass and skin tension, such as that induced by weightlifting. They are common on the abdomen during and after pregnancy (striae gravidarum) and on the breasts after lactation. They also occur on the buttocks and thighs, the inguinal areas, and over the knees and elbows in children during the growth spurt of puberty. Cushing syndrome, either endogenous or induced by systemic corticosteroid treatment, is a frequent cause of striae, and they may occur after application of potent topical corticosteroid preparations, especially under occlusion or in folds. In some early lesions, perivascular and interstitial infiltration of lymphocytes and sometimes eosinophils is noted. The collagen of the upper dermis is decreased, and thin collagen bundles lie parallel to the overlying epidermis, as in a scar. Elastic tissue often appears increased, but this may result from a loss of collagen in many cases. A Cochrane review found no high-quality evidence to support the use of any topical preparation for the prevention of stretch marks during pregnancy. Both silicone gel and placebo have demonstrated some positive effects in clinical studies, complicating interpretation of results. Topical tretinoin and vascular lasers may produce some improvement in appearance, although the benefits are more marked in the early erythematous phase. Pulsed dye lasers (585 nm) result in a moderate decrease in erythema in striae rubra. Although the total collagen per gram of dry weight increases in striae treated with pulsed dye laser, this change may not result in a clinically evident change in striae alba. Intense pulsed light has also demonstrated potential for improvement in the appearance of some striae, although with greater risk and lower efficacy in darker skin types. Fractional photothermolysis has been used in a variety of skin types for both rubra and alba types of striae. ChantesA,etal: Clinical improvement of striae distensae in Korean patients using a combination of fractionated microneedle radiofrequency and fractional carbon dioxide laser. Ud-DinS,etal: A double-blind controlled clinical trial assessing the effect of topical gels on striae distensae (stretch marks): a noninvasive imaging, morphological and immunohistochemical study. HodakE,etal: Primary anetoderma and antiphospholipid antibodies: review of the literature. Histologically, increased elastic fibers are seen, characterized by thin, wavy, and elongated as well as fragmented bundles. Electron microscopy reveals thin, elongated, irregularly shaped, swollen elastic fibers with degenerative changes. This condition is reviewed with bacterial infections in Chapter 14, since it results from Borrelia infection. There are seven recognized forms based on differences in clinical presentation and bone architecture. Deafness develops in many patients by the second decade of life and is audiologically indistinguishable from otosclerosis. The skin is thin and translucent, and healing wounds result in spreading atrophic scars. Some patients experience unusual bruisability, probably from a structural defect in either the blood vessel wall or the supporting dermal connective tissue. The basic defect is abnormal collagen synthesis, resulting in type I collagen of abnormal structure. Specifically, cyclic pamidronate therapy has been shown to suppress bone turnover, reduce bone pain and fracture incidence, and increase bone density and level of ambulation. Gene therapy is promising but is complicated by the genetic heterogeneity of the disease. This sort of abnormality presents greater challenges for gene therapy than simple replacement of a missing enzyme, but gene and stem cell transfer research is ongoing. ZhangZ,etal: Phenotype and genotype analysis of Chinese patients with osteogenesis imperfecta type V. It represents beta-pleated sheet forms of various host-synthesized molecules processed into this configuration by host cells. The systemic types can deposit amyloid in multiple organs, and all are related to an overproduction of a host protein that cannot be adequately excreted or metabolized by the host. The excess protein is metabolized into amyloid precursors that interact with tissue proteoglycans/ glycosaminoglycans, forming soluble amyloid oligomers. In all forms of amyloid, the pattern of deposition is characteristic, although there can be overlap between various forms. The diagnosis of a specific type of amyloid should only be made if the clinical features are characteristic and if the deposited protein is identified histochemically. Primary localized amyloidosis (also called primary cutaneous amyloidosis when the skin is affected) is very common and of importance to the dermatologist. Rare familial syndromes may be complicated by secondary systemic amyloidosis or may have genetic defects that lead to amyloid deposition (heredofamilial amyloidosis). Heredofamilial amyloidosis All forms of amyloid have relatively identical histologic and electron microscopic findings. The amyloid in all forms is made up of three distinct components: protein-derived amyloid fibers, amyloid P component (about 15% of amyloid), and ground substance. The protein-derived amyloid fibers are those that differ among the various forms of amyloid. Amyloid stained with Congo red exhibits apple-green birefringence under polarized light. In most cases, specific antibodies against the protein component should be used to confirm the type of amyloidosis. Because amyloid substance P is present in all forms of amyloid, immunoperoxidase staining against this component will stain all forms of amyloid. About 90% of patients will have the Ig fragment detectable in the serum or urine; in the other 10%, the serum free light-chain assay will detect a clear excess of one of the light chains (or), confirming the diagnosis. Also, reduction of the urine free light chains by more than 50% correlates with substantial benefit from treatment.