Safe ampicillin 250 mg
In the latter antibiotic 3 days uti generic ampicillin 500mg without prescription, depending on the organs involved, symptoms and signs at presentation may include fractures, splenomegaly, pleural effusion, or ascites. Radiologic Features Imaging studies in general show multiple lytic lesions in the bones. Gross Pathology the liver is usually markedly enlarged, with multiple, cystic, white-tan, irregular lesions containing clear or chylous fluid. These spaces are lined by bland endothelial cells and do not contain red blood cells. Lymphangioma can be distinguished from hemangioma by the absence of red blood cells and presence of lymph. Lymphangiomatosis has been mistaken for polycystic liver disease or metastatic lesions. There is 589 Practical Hepatic Pathology: A Diagnostic Approach one notable case report of successful liver transplantation for hepatic lymphangiomatosis, with recurrent disease detected 19 years later in the transplanted liver. This group also includes clear cell (sugar) tumor and lymphangioleiomyomatosis of the lung. Unlike renal angiomyolipoma, only a few cases of hepatic angiomyolipoma are associated with tuberous sclerosis. When present in the context of tuberous sclerosis, liver tumors are always associated with renal tumors. Clinical Manifestations Angiomyolipomas are usually solitary and may be more than 30 cm in diameter, causing abdominal pain, discomfort, and distention. Gross Pathology Angiomyolipomas contain variable amounts of fat, smooth muscle, and vascular tissue, and the gross appearance varies with the predominant component. Tumors with significant fat content tend to be soft and yellow, whereas tumors with predominantly smooth muscle content tend to be firm, with a tan-white cut surface. Microscopic Pathology Angiomyolipoma of the liver morphologically resembles its counterpart in the kidney. They can be subcategorized as lipomatous, myomatous, or angiomatous depending on the predominant component. In addition, hepatic angiomyolipoma often contains hematopoietic elements, including megakaryocytes as well as erythroid and myeloid precursors. In addition, irregular and hyperchromatic nuclei can be encountered in the smooth muscle cells. The vascular component is typically made of thick-walled hyalinized arterial or venous-like vessels with abnormally thickened hyperplastic elastic fibers. Differential Diagnosis the main differential diagnosis of epithelioid angiomyolipoma is hepatocellular carcinoma or hepatocellular adenoma (Table 36. Tumors with a predominant fat component may be mistaken for focal fatty change or hepatocellular adenoma (Table 36. Tumors with predominantly spindled smooth muscle cells may be mistaken for sarcomas. In addition, S-100 protein has been reported to be focally positive in angiomyolipoma. Treatment and Prognosis Angiomyolipomas are benign tumors, and surgical resection is curative. Lesions detected simultaneously in other organs represent multifocality rather than metastatic disease. These usually take the form of sarcomatous transformation, accompanied by vascular invasion in portal tracts distant from the main tumor. Histologic Features When smooth muscle cells with epithelioid, clear cells, or oncocytic features predominate, histologic features mimic hepatocellular carcinoma, but no pseudoglandular structures or bile production is seen. Immunohistochemical staining, is generally not useful in differentiating hepatocellular adenoma from carcinoma. Positive for inhibin and A103 (melan A); occasionally for synaptophysin, neuron-specific enolase, cytokeratins, and vimentin. Most common cytomorphology is clear cell, with trabecular architecture and hypervascularity. Clusters of tumor cells in trabecular or pseudoglandular configuration in delicate fibrovascular stroma; tumor cells with characteristic finely stippled chromatin and lack of prominent nucleoli. Adrenal cortical carcinoma Patients may have large tumor mass inferior to liver in region of adrenal gland, which may directly involve liver. Histologic Features Localized area of multiple lobules with marked macrovesicular steatosis. Tumor consists of variable amount of mature adipose tissue, vessels, and smooth muscle. Angiomyolipoma Incidental finding or presenting with abdominal pain and distention. Pseudolipoma Encapsulated lesion of mature adipose tissue with degeneration or necrosis, often calcified, commonly on surface of liver; thick and hyalinized capsule; no blood vessels. Hepatocellular carcinoma 591 Practical Hepatic Pathology: A Diagnostic Approach Focal Fatty Change Focal fatty change is a localized zone of hepatocytes that shows severe steatosis in an architecturally normal liver. Incidence and Demographics Focal fatty change is an incidental finding in approximately 10% to 20% of livers. Clinical Manifestations Focal fatty change is usually subcapsular in location with geographic margins. Injection or intraperitoneal administration of insulin in patients with peritoneal hemodialysis has led to unusual patterns of focal liver steatosis in the subcapsular region. Portal tracts and terminal hepatic veins are present throughout the lesion in a normal architectural pattern. The adjacent nonsteatotic liver parenchyma may be congested without fibrosis or cirrhosis. Differential Diagnosis the differential diagnosis of focal fatty change includes metastatic tumor and benign hepatic tumor such as hepatocellular adenoma or angiomyolipoma with a predominant fat component (see Table 36. Treatment and Prognosis Focal fatty change is a benign and often incidental lesion requiring no treatment. Although lymphomas often involve the liver as part of a systemic process, they rarely occur as a primary hepatic disease. The term hepatosplenic lymphoma has been loosely used for primary hepatic lymphoma, because the spleen is often involved at the time of detection. However, it is more appropriately reserved for a subtype of aggressive lymphoma known as hepatosplenic T-cell lymphoma (detailed discussion in the following section). Incidence and Demographics the liver is involved in 70% of cases of systemic Hodgkin and nonHodgkin lymphomas, often with only mildly abnormal liver function tests and no significant functional deficits. Most affected patients have non-Hodgkin lymphoma of B-cell phenotype, of which the majority of cases are diffuse large B-cell lymphoma. Diffuse large neoplastic cells with scant cytoplasm, vesicular nuclei, and prominent nucleoli. Normal liver architecture with well-differentiated lymphoid infiltrate, predominantly in portal tracts. Association with chronic hepatitis B and C as well as primary biliary cholangitis. Can be difficult to distinguish from recurrent chronic hepatitis or rejection in posttransplant patients. Variant of diffuse large B-cell lymphoma with few large neoplastic B cells scattered among numerous small T cells and histiocytes. Histologically may mimic chronic inflammatory diseases, including chronic hepatitis with interface hepatitis or Hodgkin disease. Occurs in adolescents and young adults, and is more common in males, with hepatosplenomegaly and thrombocytopenia. Diffuse, large, pleomorphic cells with prominent nucleoli and horseshoe-shaped or multiple nuclei.
Purchase ampicillin 500mg with visa
Since her last visit bacteria 8000 cheap 250 mg ampicillin amex, she has noticed a tremor in both hands instead of only her left hand as it was previously. During her off periods, she says her muscles are "stiff as a board," and she moves very slowly and has trouble maintaining balance occasionally. This affects her in the kitchen preparing food, and she is unable to walk her dog, an activity she enjoys that also provides her exercise. She reports a history of constipation that is somewhat improved from increased dietary fiber. Recently, she has had to use the restroom more often at night which disrupts her sleep. The disease may begin in the autonomic system, olfactory system, or vagus nerve in the lower brainstem and then spread to the upper brainstem and cerebral hemisphere affecting dopamine pathways later in the course of disease progression. Offending agents include drugs that deplete dopamine such as antipsychotics, metoclopramide, and certain antiemetics such as prochlorperazine. The hand tremor can appear as if the patient is rolling a pill between his or her fingers. Patients usually describe rigidity as stiffness, and muscles often display uniform resistance on examination. Bradykinesia is defined as hesitancy in movement initiation, slowness in movement performance, or rapid fatiguing during movement. Patients may have a decrease in automatic movements, such as eye blinking, hypomimia, or a decrease in arm swing while walking. Postural instability results from the loss of reflexes necessary to maintain balance when ambulating. Gait abnormalities may include slow shuffling, leg dragging, festination, propulsion, retropulsion, or freezing. Rigidity and bradykinesia may make handwriting difficult as evidenced by micrographia. Dementia and depression occur frequently with the latter likely due to abnormalities in dopamine and serotonin activity. Often comorbid with depression, anxiety has been noted in up to 66% of patients with motor fluctuations. Motor complications include delayed peak response, early and unpredictable "wearing off," freezing, and dyskinesias. Risk factors for developing motor complications include younger age at diagnosis, high dosage of levodopa, and longer duration and severity of disease. Wearing off can be conceptualized as the therapeutic window of levodopa narrowing over time. This clinician and patient rated scale has four parts that can be used individually or in combination. It takes about 30 minutes to complete, so it may not be collected in its entirety at each visit. These commonly include sleep disturbances, autonomic impairment, psychological disturbances, and others such as anosmia or sensory disturbances. Visual problems such as difficulty reading, double vision, decreased blinking, and burning or itchy eyes are the result of impairment of the ocular mucles. Orthostatic hypotension may cause dizziness, lightheadedness, fainting upon standing, or fall-related injuries. Sexual dysfunction manifests as decreased libido or inability to achieve orgasm in both sexes and erectile or ejaculatory dysfunction in men. The most common interventions include maintaining good nutrition, physical condition, and social interactions. Coordinated care with an optometrist/ophthalmologist, dentist, dietician, physical therapists, speech therapist, and social worker is needed to maximize patient outcomes. This procedure electrically stimulates the subthalamic nucleus or globus pallidus interna. Describe nonpharmacologic and pharmacologic treatments that are available for the patient. The best time to initiate dopaminergic therapy is controversial and patient specific. The American Academy of Neurology and the Movement Disorder Society determined that it is reasonable to start treatment with either levodopa or a dopamine agonist. Starting with a dopamine agonist may help to delay the onset of dyskinesias and the on and off fluctuations seen with long-term levodopa use. However, this approach may result in less motor benefit and greater risk of hallucinations or somnolence. Levodopa results in greater motor improvement and should be used as initial therapy in the elderly (greater than 75 years) and in those with cognitive impairment. Individual doses may be increased the first 3 days and doses may be given up to five times a day based on individual response; patients previously on immediate release levodopa should follow recommended conversions. Hepatic or Renal Adjustments Dosage reduction needed in creatinine clearance < 50 mL/min (0. Increase by 2 mg/day in 1-week intervals; Extended-release tablet maximum dose is 24 mg/day. If symptoms continue, add 5 mg at noon; Tablet, capsule 5 mg daily may be as clinically effective as 10 mg daily with fewer side effects. Levodopa is absorbed in the small intestine and distributed into the plasma and brain compartments by an active transport mechanism. Levodopa is metabolized by dopa decarboxylase, monoamine oxidase, and catechol-O-methyltransferase. Large neutral amino acids in food compete with levodopa for intestinal absorption (transport across gut endothelium to plasma). They also compete for transport into the brain (plasma compartment to brain compartment). Food and Ach delay gastric emptying resulting in levodopa degradation in the stomach and a decreased amount of levodopa absorbed. If the interaction becomes a problem, administer levodopa 30 minutes before or 60 minutes after meals. Dyskinesias related to dopamine concentrations can be managed by decreasing the dose, frequency, or use of medications that may enhance dopamine concentrations. If a dopaminergic medication is to be discontinued, it should be decreased gradually and the patient monitored for worsening of symptoms. They minimize resting tremor and drooling, but are not as effective as other agents for rigidity, bradykinesia, and gait problems. Side effects include dry mouth, blurred vision, constipation, cognitive impairment, hallucinations, urinary retention, orthostatic hypotension, temperature sensitivity, and sedation. They are usually avoided or used with caution in patients older than 70 years because of an increased risk of cognitive impairment. There is concern that this may translate to an increased risk of Alzheimer disease. Side effects include nausea, dizziness, livedo reticularis, peripheral edema, orthostatic hypotension, hallucinations, restlessness, anticholinergic effects, and insomnia. It should be avoided in the elderly who cannot tolerate its anticholinergic effects. They may provide a mild symptomatic benefit for patients who choose to delay dopaminergic medications, and they reduce off time when added to levodopa therapy. It requires premedication with an antiemetic because it causes nausea and vomiting. Side effects of selegiline are minimal but include nausea, confusion, hallucinations, headache, jitteriness, and orthostatic hypotension. The labeling of rasagiline states that restriction of tyramine-containing foods is not ordinarily required at recommended dosages, but certain foods with extremely high levels of tyramine and exceeding recommend dosing of rasagiline may increase the risk of hypertensive crisis. Because of risks of serotonin syndrome and hypertensive crisis, patients should avoid or use these medications cautiously with narcotic analgesics, antidepressants, and other serotonergic agents, or sympathomimetic amines (cold and weight loss products). They are useful as initial therapy, as suggested by the 2010 Scottish Intercollegiate Guidelines.
500mg ampicillin otc
Monitor complete blood cell count antibiotics dairy purchase online ampicillin, as melphalan therapy is associated with delayed and prolonged nadir. Metabolized in the liver by methylation to inactive metabolites and via oxidation by xanthine oxidase to inactive metabolites. About 50% of parent drug and metabolites is eliminated in urine within the first 24 hours. Distributes into third-space fluid collections such as pleural effusion and ascites. Warfarin-Methotrexate may enhance the anticoagulant effect of warfarin through competitive displacement from plasma proteins. Thymidine-Thymidine rescues the toxic effects of methotrexate and may also impair the antitumor activity. Folic acid supplements-These supplements may counteract the antitumor effects of methotrexate and should be discontinued while on therapy. This is an especially important issue for patients receiving high-dose methotrexate. Use with caution in patients with third-space fluid collections such as pleural effusion and ascites, as the half-life of methotrexate is prolonged, leading to enhanced clinical toxicity. Use with caution in patients with bladder cancer status post-cystectomy and ileal conduit diversion, as they are at increased risk for delayed elimination of methotrexate and subsequent toxicity. With high-dose therapy, methotrexate doses > 1 g/m2, important to vigorously hydrate the patient with 2. Methotrexate blood levels should be monitored in patients receiving high-dose therapy, patients with renal dysfunction (CrCl < 60 mL/min) regardless of dose, and patients who have experienced excessive toxicity with prior treatment with methotrexate. Glucarpidase is indicated for the treatment of toxic plasma methotrexate concentrations (> 1 mM) in patients with delayed drug clearance due to impaired renal function. Intrathecal administration of methotrexate may lead to myelosuppression and/or mucositis as therapeutic blood levels can be achieved. Methotrexate overdose can be treated with leucovorin, L-leucovorin, and/ or thymidine. Caution patients about drinking carbonated beverages, as they can increase the acidity of urine, resulting in impaired drug elimination. Transient elevation in serum transaminases and bilirubin may be observed with high-dose therapy. Pneumonitis characterized by fever, cough, and interstitial pulmonary infiltrates. Chronic, demyelinating encephalopathy observed in children months to years after intrathecal methotrexate and presents as dementia, limb spasticity, and in advanced cases, coma. Elimination is mainly in feces (95%), predominantly as metabolites (91%) and only 4% of unchanged midostaurin. Patients should take midostaurin with food, twice daily at approximately 12-hour intervals. Use with caution in patients with severe hepatic impairment, as the effect on midostaurin metabolism and elimination is not known. Dose adjustment is not required in patients with mild or moderate renal impairment. Use with caution in patients with severe renal impairment, as the pharmacokinetics of the drug is not well known in this setting. Parent compound and its metabolites are excreted mainly through the hepatobiliary system into feces. Risk of myelosuppression is increased when used in combination with other myelosuppressive agents. Risk of pulmonary toxicity increased with cumulative doses of mitomycin-C > 50 mg/m2. Monitor for signs of hemolytic-uremic syndrome (anemia with fragmented cells on peripheral blood smear, thrombocytopenia, and renal dysfunction), especially when total cumulative doses of mitomycin-C are > 50 mg/m2. Myelosuppression is dose-limiting, and cumulative toxicity with leukopenia is more common than thrombocytopenia. Extravasation can lead to tissue necrosis and chemical thrombophlebitis at the site of injection. Consists of microangiopathic hemolytic anemia (hematocrit < 25%), thrombocytopenia (< 100,000/mm3), and renal failure (serum creatinine > 1. Other complications include pulmonary edema, neurologic abnormalities, and hypertension. May occur at any time during treatment but usually when cumulative doses > 50 mg/m2. Presents with dyspnea, non-productive cough, and interstitial infiltrates on chest X-ray. Mitotane is slowly released, with drug levels being detectable for up to 10 weeks. Parent compound and its metabolites are excreted mainly through the hepatobiliary system into feces (60%). Adrenal insufficiency may develop, and adrenal steroid replacement with glucocorticoid and/or mineralocorticoid therapy is indicated. Distributes in high concentrations in liver, bone marrow, heart, lung, and kidney. Elimination is mainly through the hepatobiliary route, with 25% of the drug excreted in feces. Avoid extravasation, but ulceration and tissue injury are rare when drug is properly diluted. Risk of cardiac toxicity is higher in elderly patients > 70 years of age, in patients with prior history of hypertension or pre-existing heart disease, in patients previously treated with anthracyclines, or in patients with prior radiation therapy to the chest. Patients may experience blue-green urine for up to 24 hours after drug administration. Myelosuppression is dose-limiting, with neutropenia more common than thrombocytopenia. Chronic toxicity is manifested in the form of a dilated cardiomyopathy with congestive heart failure. Cumulative doses of 140 mg/m2 in patients with no prior history of anthracycline therapy and 120 mg/m2 in patients with prior anthracycline therapy are associated with increased risk for developing congestive cardiomyopathy. Mogamulizumab-kcpc most likely undergoes proteolytic degradation into small peptides and amino acids via catalytic pathways. Monitor for infusion-related reactions, and interrupt the infusion for any grade reaction and treat accordingly. If an infusion reaction occurs, acetaminophen and an antihistamine should be administered for all subsequent infusions. May need to perform skin biopsy to differentiate between drug eruption and disease progression. Skin toxicity with maculopapular rash, lichenoid dermatitis, scaly plaques, pustular eruption, folliculitis, non-specific dermatitis, and psoriasiform dermatitis. It is presumed that moxetumomab pasudotox undergoes proteolytic degradation into small peptides and amino acids via catalytic pathways. Patients should be premedicated with acetaminophen, antihistamine, and H2-receptor antagonist prior to all infusions. Patients should be monitored during and for at least 1 hour after the completion of the infusion. Patients may need to take oral antihistamines and acetaminophen and even oral steroids for up to 24 hours after drug infusion.
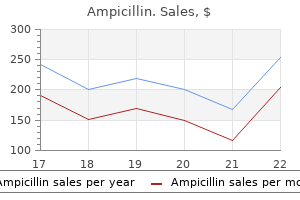
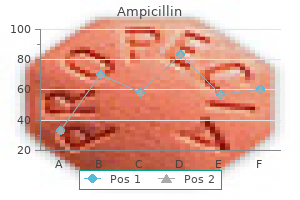
| Comparative prices of Ampicillin | ||
| # | Retailer | Average price |
| 1 | Sears Holdings | 340 |
| 2 | Trader Joe's | 321 |
| 3 | Walgreen | 931 |
| 4 | Safeway | 574 |
| 5 | Lowe's | 973 |
Purchase ampicillin uk
If acid reduction is necessary antibiotic resistance animals cheap ampicillin on line, treatment with antacids and H2-receptor antagonists should be used. Patients should be educated to take dacomitinib at least 6 hours before or 10 hours after the H2-receptor antagonist. Dacomitinib can cause fetal harm, and effective contraception should be practiced during treatment with dacominitib and for at least 17 days after the last dose of drug. Most of drug is eliminated in unchanged form by hepatobiliary (50%) and renal (20%) excretion. Contraindicated in patients actively infected with chickenpox or herpes zoster, as generalized infection may result in death. Onset within the first 2 hours of therapy, lasts for up to 24 hours, and may be severe. Radiation-recall reaction with erythema and desquamation of skin observed with prior or concurrent radiation therapy. Administer daratumumab in a clinical facility with immediate access to resuscitative measures. Administer oral corticosteroids (20 mg methylprednisolone) on the first and second days after all infusions to reduce the risk of delayed infusion reactions. Daratumumab may interfere with an accurate assessment of the myeloma response, as the drug may be detected on serum protein electrophoresis and immunofixation assays that are used to monitor for endogenous M-protein levels. Peak plasma concentrations are observed between 30 minutes and 6 hours of oral ingestion. Oral dasatinib tablets can be taken with or without food but must not be crushed or cut. Closely monitor electrolyte status, especially calcium and phosphate levels, as oral calcium supplementation may be required. Avoid Seville oranges, starfruit, pomelos, grapefruit, and grapefruit juice while on dasatinib therapy. Patients should be closely monitored for depressive symptoms and suicide ideation while on therapy. Widely distributed to tissues, with high concentrations in heart, liver, lungs, kidneys, and spleen. Careful administration of the drug, usually through a central venous catheter, is necessary as the drug is a strong vesicant. Cumulative doses of > 550 mg/m2 are associated with increased risk for cardiotoxicity. Chronic form associated with a dose-dependent, dilated cardiomyopathy and congestive heart failure. Extravasation can lead to tissue necrosis and chemical thrombophlebitis at the injection site. Small, steady-state volume of distribution (6 L) in contrast to the parent drug, daunorubicin. Metabolism in the liver, but the primary metabolite, daunorubicinol, is present only in low concentrations. Risk of cardiotoxicity is higher in patients > 70 years of age, in patients with prior history of hypertension or pre-existing heart disease, and in patients previously treated with anthracyclines or prior radiation therapy to the chest. Cumulative doses of > 320 mg/m2 are associated with increased risk for cardiotoxicity. Infusion should be discontinued until symptoms resolve and then resumed at a slower rate. Occurs within the first 5 minutes of infusion and manifested by back pain, flushing, and tightness in chest and throat. Daunorubicin is metabolized in the liver, with formation of one of its primary metabolites, daunorubicinol, which has antitumor activity. Cytarabine undergoes extensive metabolism, with approximately 70% of the drug being recovered in the urine as the uracil arabinoside (ara-U) metabolite. Hepatotoxic agents-Concomitant use with other hepatotoxic agents may increase the risk of hepatotoxicity. Has not been studied in patients with serum bilirubin levels > 3 mg/dL, and caution should be used in this setting. Has not been studied in patients with severe renal dysfunction or end-stage renal disease, and caution should be used in these settings. In the presence of mild or moderate infusion reactions, the rate of infusion should be interrupted or slowed, and symptoms should be treated appropriately. If severe or lifethreatening reactions occur, the drug should be discontinued permanently, the symptoms should be treated, and the patient closely monitored until all symptoms resolve. Use with caution in patients previously treated with radiation therapy, as daunorubicin can cause a radiation-recall skin reaction. Patients should be cautioned to avoid sun exposure and to wear sun protection when outside. Aberrantly silenced genes, such as tumor suppressor genes, are then reactivated and expressed. Precise route of elimination and metabolic fate of decitabine is not known in humans. One of the elimination pathways is via deamination by cytidine deaminase, found principally in the liver but also in plasma, granulocytes, intestinal epithelium, and peripheral tissues. Serum testosterone levels decrease to castrate levels within 3 days of initiation of therapy. Local discomfort at the site of injection with erythema, swelling, and/or induration. Low serum albumin levels place patient at increased risk for vascular leak syndrome. Patients should be monitored closely throughout the entire treatment, including vital signs, pre- and post-infusion weights, and evidence of peripheral edema. Myelosuppression is uncommon, with anemia occurring more frequently than neutropenia. Hepatotoxicity with elevations in serum transaminases and hypoalbuminemia (albumin < 2. Usually occurs during the first course and resolves within 2 weeks of stopping therapy. Normal dynamic process of microtubule network is inhibited, leading to inhibition of mitosis and cell division. Less than 10% is eliminated as the parent compound, with the majority being eliminated as metabolites. Renal clearance is relatively minor, with less than 10% of drug clearance via the kidneys. Hypersensitivity reactions with generalized skin rash, erythema, hypotension, dyspnea, and/or bronchospasm. Usually prevented by premedication with steroid; overall incidence decreased to less than 3%. Presents as weight gain, peripheral and/or generalized edema, pleural effusion, and ascites. Metabolized extensively in the liver to the active hydroxylated metabolite, doxorubicinol, as well as to inactive metabolites. Important to be able to distinguish between hemorrhagic cystitis and the normal red-orange urine observed with doxorubicin therapy. Avoid using veins over joints or in extremities with compromised venous and/or lymphatic drainage. Use of a central venous catheter is recommended for patients with difficult venous access and mandatory for prolonged infusions.
Ampicillin 500mg overnight delivery
Because the histopathologic sampling of resection specimens antibiotics long term effects order ampicillin visa, both in those who have received presurgical chemotherapy and those who have not, markedly affects final tumor classification and therefore risk stratification, standardized work-up of these specimens is essential. The embryonal phenotype is the most commonly encountered pattern and is usually found intimately admixed with fetal-type tissue, the mixed embryonal/fetal subtype. Embryonal histology resembles the morphology of the liver at 6 to 8 weeks of gestation; the cells are arranged in sheets interrupted by immature tubule-like profiles or rosettes. I expect the latter subgroup to be of standard risk and the former to exhibit the more aggressive behavior that has been associated with this subtype. Fetal-type cells with a "dark" cytoplasm are more strongly stained for cytokeratin 8 than clear cells. The bland appearance and central portal tract-like structure may be mistaken for normal liver. The embryonal cells are more basophilic and commonly tend to form a rim around fetal areas. Fibrous or sclerosed nodules, called "regression spheres," may be seen embedded in a more diffuse fibrous area. Currently, two main staging systems for primary malignant liver tumors of childhood are in use. When applying a stage, it is important to distinguish actual involvement of the respective section from mere compression by the adjacent tumor. This refinement of criteria allows identification of patients who would benefit from a high-risk treatment protocol. A, Contracted tumor nodules with a fibrous capsule and variegated cut surface are seen macroscopically. G, So-called regression sphere with central blood remnants, likely to be an altered tumor blood vessel. As described in the text, the liver is divided into four sections, and the stage depends on the number of contiguous sections not involved by tumor. Immunohistochemically, the cholangiocellular components are reactive for cytokeratins 7 and 19. Ductal plate tumors of the liver are a recently proposed entity5 and are defined as liver cell neoplasms in the form of cholangiocellular structures that morphologically mimic the embryonal ductal plate. A distinctive tumor belonging to the stromal-epithelial group is the nested stromal epithelial tumor of the liver. In this cytokeratin immunostain, nodules of immature hepatoid cells are encircled by a structure that resembles the ductal plate. C, Variant of a ductal plate tumor with irregular clusters of hepatoid cells associated with foci of ductular profiles. Genetics and Molecular Pathology Hepatoblastomas exhibit complex patterns of chromosomal aberrations characterized by either gains or losses involving several chromosomes (eg, 1q, 2q, 4q, 8, 11q, 17q, and 20). Detailed analyses of the respective loci are not yet available, but molecular studies have uncovered several genetic changes involved in cell fate, growth, apoptosis, signaling pathways, and differentiation. The molecular basis of Beckwith-Wiedemann syndrome is complex and involves deregulation of imprinted genes found in two domains within the 11p15 region. A, Typically shaped epithelial nests are surrounded by a stromal mantle of spindle cells. Mutations in the degradation box of the -catenin gene cause proteasome bypassing of -catenin and its accumulation in the nucleus, where it can then be detected by immunohistochemistry. These findings suggest a distinct tumor microarchitecture driven by heterogeneous expression of genetic events, especially in the -catenin signaling pathway. B, the distinctly placed nests show marked nuclear reactivity for -catenin, whereas the surrounding cells show membranous staining. D, the nest cells show low proliferative activity (Ki-67) and are surrounded by a zone of marked proliferation. E, Poor mitochondrial content of nest cells in comparison with the surrounding better differentiated cells (mitochondrial immunostain). The lesions are of the expanding type with pushing borders, and they sometimes exhibit large central necrosis. Introduction of effective cisplatin-based chemotherapeutic regimens in the mid-1980s and the efforts of large international cooperative trials have led to current cure rates of at least 70%. The 3-year overall and progression-free survival was 91% and 89% for the standard-risk group, and 53% and 48% for the high-risk group, respectively. A, Tumor with a diffuse growth pattern, consisting of cells intermediate between hepatoblasts and hepatocytes. In contrast with most liver tumors, approximately two thirds arise in the left lobe. In a study of 41 patients, median tumor size was 9 cm (range, 3 to 17 cm); of these patients, 36% of cases had vascular invasion and 50% had lymph node metastasis. The tumor cells are variably positive for fibrinogen, which in many cases stains the pale bodies previously described, as well as ferritin and alpha-1 antitrypsin. B, Large and eosinophilic tumor cells are embedded in a rich and partially hyalinized fibrolamellar stroma. C, Part of the tumor cells contain large, lightly eosinophilic inclusions, the so-called pale bodies (eSlide 35. More than two thirds of cases occur in children older than 10 years of age, and very few cases occur in children younger than 5 years of age. For solitary tumors, three main gross Liver Tumors of Childhood prominent eosinophilic nucleoli (eSlide 35. Increasing grades are associated with increasing nuclear irregularity, hyperchromasia, and nuclear-cytoplasmic ratio, and with decreasing cytologic differentiation. Radical tumor resection or liver transplantation in selected patients remains the only curative approach. A, Trabecular growth pattern below the dotted line shows well-differentiated hepatocyte-like cells (grade 1), whereas tumor above the dotted line shows cells with larger nuclei (grade 2). Abdominal pain associated with anorexia and nausea/vomiting may occur but is not usually a prominent feature. In the pediatric age group, about 90% of the lesions are asymptomatic and present as a mass found incidentally or during routine examination. The few symptomatic cases show abdominal pain, nausea and vomiting, and/or diarrhea. Other Rare Malignant Epithelial Tumors Cholangiocarcinoma is exceedingly rare in children, unlike in adults. The cut surface usually shows few to multiple cystic spaces, which do not communicate with the biliary tract. Cystic structures occur in 85% of cases, but very young patients may have tumors without cysts, suggesting that cystic change develops over time. Larger cysts have a gray to tan lining and contain amber to yellow fluid or a gelatinous material. Microscopic Pathology Microscopically, the tumor consists of a complex mixture of loose connective tissue, multiple small bile ducts, hepatocyte cords, and variably sized cysts (eSlide 35. There is evidence that small bile ducts and their associated periductal mesenchymal sheath form a "tissue pacemaker" in the liver. Differential Diagnosis the major clinicoradiologic differential diagnosis is infantile hemangioma. It is predominantly solitary and solid but often shows a central cyst or multiple cystic spaces, hemorrhage, and necrosis. The main cell types include spindle cells, stellate cells, and polymorphous elements (eSlide 35. These ducts are not usually present in deeper parts of the tumor and are therefore thought to be preexisting ducts entrapped by the invading tumor. Immunohistochemically, the expression patterns are complex and depend on the cell lineages involved. The tumor occurs mainly in children at a median age of 3 years, with a clear preponderance of boys. B, the interface of tumor with adjacent liver is well-delimited but unencapsulated. The tumor is lobulated and contains ductal structures surrounded by a rim of loose mesenchyme. C, At higher magnification, the bile ducts reveal a collagenous collar separating them from the loose mesenchyme. D, Cells within the mesenchyme, which is rich in glycosaminoglycans, are stellate or fibroblastoid.
Discount ampicillin online master card
The spectrum continues with diuretic-resistant ascites virus 65 cheap ampicillin master card, where the kidneys are unable to excrete sufficient sodium to clear the fluid even with the use of diuretic medications. The predominant theory (termed the "Underfill" theory) is that blood vessels in the renal circulation are constricted as a result of the dilation of blood vessels in the splanchnic circulation, which is mediated by factors released because of the liver disease. The consequence of this phenomenon is a decrease in the "effective" volume of blood sensed by the juxtaglomerular apparatus, leading to the secretion of renin and the activation of the renin-angiotensin system, which results in the vasoconstriction of vessels systemically and in the kidney specifically. However, the effect of this is insufficient to counteract the mediators of vasodilation in the splanchnic circulation, leading to persistent "underfilling" of the renal circulation and worsening renal vasoconstriction, leading to renal failure. The vasodilation resulting from liver failure results in a direct vasodilatory effect in the lungs, resulting in increased blood flow in relation to ventilation and a ventilation-perfusion mismatch. This is seen clinically as a right-to-left shunt and the patient experiences dyspnea. Jaundice, ascites, edema, malnutrition, fatigue, and encephalopathy are all commonly seen. Resolution of these derangements can be immediate, as with encephalopathy, or can take months to reverse, as with malnutrition. Posttransplant supportive care is critical and many of these patients require intensive physical and occupational therapy before they are able to safely return to normal activities of daily living. Unfortunately, outcomes vary greatly depending upon the age, size, and general health status of the child at the time of transplant. These children have limited reserve, can be very ill, and are at high risk of hepatic artery thrombosis, which is often a fatal complication. The waitlist time for a small child can be prolonged as deceased donor organs of this size are infrequently available. Many centers now offer living donor transplantation using the left lateral segment of an adult liver, if it is of an appropriate size. These reduced size grafts now have survival rates in the pediatric population that are similar to or better than whole organ grafts. Children older than age 3 have significantly better outcomes, they have more physiologic reserve, and are often not as severely decompensated. Also, there are more viable organs available for these children simply because of increasing size of the abdomen. Although chronic diseases are less common, pediatric patients can experience significant decompensation from their liver disease and present with severe malnutrition, ascites, edema, portal hypertension, and hepatorenal and hepatopulmonary syndromes. Patients who become critically ill before transplantation, requiring mechanical ventilation or dialysis, have markedly diminished posttransplant survival. These retransplants may be urgent and carry a high risk of mortality because of the difficulty in finding a replacement allograft of the appropriate size. Other indications for retransplantation include disease recurrence, primary nonfunction, and chronic rejection. Chronic rejection is commonly related to noncompliance and is often seen in the teenage years. Efforts to increase donation rates and to expand the donor supply in recent years have met with limited success (Box 37. Use of partial liver grafts has become more common in providing donor organs in a timely fashion to recipients in need. This approach takes advantage of the unique ability of the liver to rapidly regenerate and may provide additional organs not previously available. Unfortunately, recent studies suggest that use of these partial liver grafts imparts a significant risk to live donors, and may have a lower recipient and graft survival when compared with deceased donor livers in select patients. The newly derived donor risk index includes a partial graft transplant as an independent predictor of worse transplant outcome. Partial graft transplant in this donor risk index formula carries a risk of graft loss similar to a donor older than age 60 years or to donation after cardiac death. In addition, for living donation, there are societal costs in subjecting some of the healthiest persons in the general population to the elective donor surgery with significant risk of morbidity and mortality. There are ongoing efforts to address this disparity; however, a solution is not straightforward. In these situations, patients may self-select by referral to these centers or by being listed simultaneously at multiple centers. These options are acceptable within the current system but tend to discriminate against those without the resources to seek care at multiple sites. This suggests that greater use of extended criteria donors is warranted whereas use of partial graft donors should be minimized when possible. Because of the complexity of this decision process of matching a donor organ to specific recipient, a surgeon at one center may choose to use a particular organ, whereas a surgeon at another center may reject the organ for use. Presumably, however, when a given liver graft has been rejected by multiple centers, it carries an accumulated risk felt by many surgeons to be excessive. Local centers have the first option to accept a donor liver, followed by regional allocation for those donor livers not used locally, and finally, national allocation for those donor livers not accepted regionally (Table 37. For an organ to be offered for national sharing in the United States, it has been previously rejected by a minimum of five, and as many as 20, other liver transplant centers. There is no consensus definition for extended criteria organs in liver transplantation. Of all deceased liver donor physiologic and medical history characteristics, the only two factors that consistently demonstrate decreased allograft survival are donor age and severe steatosis. Older donor livers have a higher rate of primary nonfunction, delayed graft function, and lower long-term survival. These studies do not negate the ability of an individual center to successfully transplant liver allografts from elderly donors into appropriate recipients. However, care must be taken to match the donor and recipient and to minimize any other additional high-risk factors in the donor other than old age. The use of elderly donor livers may be most appropriate for a similarly aged recipient, and their use should be minimized in the very young and in patients who are critically ill. There are several factors that may contribute to the lower survival for elderly livers. Certainly, there are physiologic changes including a decreased total hepatocyte mass and total gross size, there is increased baseline stiffness to the liver that may result in increased portal pressures, and the arterial vasculature may be thickened with poorer flow. In general, we will not accept an older donor liver if we anticipate cold ischemia time greater than 8 hours. Frequently, these livers can be reperfused at our center within 4 hours of donor aortic cross clamp. Again, these allografts can and should be used, but the older donor must be carefully scrutinized. Hepatic steatosis in the donor liver has a well-known association with primary nonfunction. This steatosis is generally described as macrovesicular, microvesicular, or total steatosis. Most centers consider macrosteatosis to be more important in the evaluation of the donor organ, although other centers consider total steatosis in their decision. Most graft losses associated with a steatotic liver occur in the first few weeks after transplant, with long-term survival being equivalent to nonsteatotic livers when these early graft losses are censored. Resolution of the steatosis in the transplant liver occurs rapidly and complete resolution can be seen in as early as 5 to 7 days. This suggests that hepatic steatosis is a very dynamic process, and resolution of the steatosis seems to persist when the liver is placed into the new physiologic environment of the recipient. Hepatic macrosteatosis of 20% to 30% is considered the upper range for transplantation depending upon donor age (less for older donors). Liver allografts are frequently refused for transplantation because of elevated liver function enzymes in the donor. The enzymes may be elevated for a variety of reasons including donor hypotension, mechanical trauma, drug toxicity, administration of parenteral nutrition in the intensive care unit, hepatic vascular injury, and simultaneous presence of a severe brain injury. Careful analysis of the etiology of the enzyme elevation is critical in determining the transplant potential for the liver. Bedside biopsy is often helpful and may reveal information useful in the decision-making process. For these patients, consent can be obtained for withdrawal of life support under controlled conditions. A physician who is not affiliated with the organ procurement team independently declares death after withdrawal of support.
Buy 250mg ampicillin with visa
Evaluate patient history and physical examination findings to determine the etiology of cirrhosis antibiotics ointment for acne order on line ampicillin. Recommend a specific treatment regimen for a patient with cirrhosis that includes lifestyle changes, nonpharmacologic therapy, and pharmacologic therapy. Scarring is accompanied by loss of viable hepatocytes, the functional cells of the liver. Cirrhosis is irreversible and leads to portal hypertension, which in turn is responsible for the complications of advanced liver disease. Infection with one or more strains of viral hepatitis causes acute, potentially reversible, hepatic inflammation, whereas chronic infection with hepatitis B or C can lead to cirrhosis. It also places an enormous economic and social burden on society from hospitalizations, lost wages, decreased productivity, and emotional strain of the disease on both patients and their families. Alcohol ingestion and viral hepatitis C infection are the most common causes of cirrhosis in the United States, whereas hepatitis B accounts for the majority of cases worldwide. It develops more quickly in women than men, even after taking body weight into account. Estimates vary, but alcoholic cirrhosis can develop after as few as two to three daily drinks in women and three to four drinks in men, although five to eight daily drinks is more typical. Portal flow accounts for approximately 75% of blood delivered to the liver, and the hepatic artery provides the remaining 25% in the form of oxygenated blood from the abdominal aorta. Normal portal vein pressure is 5 to 10 mm Hg, and portal hypertension, which is a consequence of increased resistance to hepatic blood flow, occurs when portal pressure exceeds 10 to 12 mm Hg. This article focuses on the most common cause of portal hypertension, which is intrahepatic (sinusoidal) damage. Sinusoids transport systemic blood that contains ingested substances (eg, food, drugs, toxins) to the hepatocytes. Splenic platelet sequestration secondary to splenomegaly is one of the causes of thrombocytopenia in cirrhotic patients. Portal hypertension mediates systemic and splanchnic arterial vasodilation by increasing production of nitric oxide and other vasodilators in an attempt to counteract the increased pressure gradient. The umbilical vein, which is usually eradicated in infancy, may become patent as a result of the increased pressure and cause prominent dilated veins that are visible on the surface of the abdomen. This phenomenon is called caput medusae because it resembles the head of the mythical Gorgon Medusa. It is the most common condition associated with decompensated cirrhosis and indicates a dire prognosis. Cirrhotic changes and subsequent decreases in synthetic function lead to decreased albumin production (hypoalbuminemia). Albumin is the primary intravascular protein responsible for maintaining vascular oncotic pressure; low serum albumin levels, elevated hydrostatic pressure, and increased capillary permeability allow fluid to leak from the vascular space into body tissues. Obstruction of hepatic sinusoids and hepatic lymph nodes also allows fluid to seep into the peritoneal cavity, further contributing to ascitic fluid formation. The subsequent increase in intravascular volume furthers the imbalance of intravascular oncotic pressure, allowing even more fluid to escape to the extravascular spaces, increasing ascites and peripheral edema. Unchecked, these combined effects enable the cycle of portal pressure and ascites to continue, creating a selfperpetuating loop of ascites formation. The progressive destruction of hepatocytes combined with an increase in fibroblasts and connective tissue culminates in cirrhosis. Fibrosis scar tissue nodules modify the basic architecture of the liver, disrupting hepatic blood flow and normal liver function. Reduced hepatic blood flow significantly alters normal metabolic processes and decreases protein synthesis. Hepatic drug metabolism is reduced, which can result in higher drug concentrations and extended half-life of drugs normally eliminated by the liver, especially those with high first-pass metabolism. Decreased hepatic metabolism can also reduce or delay prodrug activation and cause therapeutic failure. The liver processes metabolic waste products for excretion; in cirrhosis, bilirubin (from the enzymatic breakdown of heme) can accumulate, causing jaundice (yellowing of the skin), scleral icterus (yellowing of the sclera), and tea-colored urine (urinary bilirubin excreted as urobilinogen). Changes in steroid hormone production, conversion, and handling are prominent features of cirrhosis. These changes manifest as decreased libido, gynecomastia (development of breast tissue in men), testicular atrophy, and feminization in men. Another effect of changes in sex hormone metabolism is development of palmar erythema and spider angiomata (nevi). Spider angiomata are vascular lesions found mainly on the trunk and have a central arteriole (body) surrounded by radiating "legs. Renal artery vasoconstriction (stimulated by the sympathetic nervous system) and decreased mean arterial pressure (mediated by nitric oxide) decrease renal perfusion and precipitate renal failure. Production of renin stimulates a cascade that causes fluid retention and peripheral vasoconstriction in an attempt to increase renal blood flow. Prostaglandin E2 and prostacyclin production are increased to stimulate renal vasodilation. Because of this, even minor changes in these laboratory test results should be monitored closely; small changes in values may represent large changes in renal function. In portal hypertension, there is resistance to drainage from the originating organ; collateral vessels (varices) develop in the esophagus, stomach, and rectum to compensate for the increased blood volume. Varices divert blood meant for hepatic circulation back to the systemic circulation, which decreases clearance of medications and potential toxins through loss of first-pass metabolism. Varices are weak superficial vessels; any additional increase in pressure can cause them to rupture and bleed. These substances bind to both the -aminobutyric acid and benzodiazepine receptors and act as agonists at the active receptor sites. Patients with previously stable cirrhosis who develop acute encephalopathy often have an identifiable precipitating event that can account for the increased production and/or decreased elimination of toxins. This flow diagram illustrates the importance of portal hypertension with splanchnic vasodilation in the development of ascites. The liver manufactures procoagulant and anticoagulant factors essential for blood clotting and maintenance of blood homeostasis. In advanced disease, the liver is unable to synthesize these proteins, resulting in extended clotting times (eg, prothrombin time) and bleeding irregularities. This results from decreased platelet production in the bone marrow caused by reduced hepatic thrombopoietin synthesis and splenic sequestration of formed platelets. Macrocytic anemia occurs because of decreased intake, metabolism, and storage of folate and vitamin B12. Individuals who continue to drink alcohol exacerbate blood abnormalities because ethanol is toxic to bone marrow. Alcoholic Liver Disease Alcoholic liver disease progresses through several distinct phases-from fatty liver to alcoholic hepatitis and finally cirrhosis. Changes in metabolism account for the fatty liver, hypertriglyceridemia, and acidemia observed in alcoholic liver disease. Fatty liver and alcoholic hepatitis may be reversible with cessation of alcohol intake. The scarring of cirrhosis is permanent, but maintaining abstinence from alcohol can decrease complications and slow progression to end-stage liver disease. Ethanol metabolism begins prior to absorption; alcohol dehydrogenase in the gastric mucosa oxidizes a portion of ingested alcohol to acetaldehyde. Alcohol dehydrogenase oxidizes ethanol in body tissues, primarily the liver, causing inflammation and fibrosis. When it is overwhelmed, the microsomal ethanol oxidizing system takes over the detoxification process. In severe hepatic disease, systemic circulation bypasses the liver; substances that are normally hepatically metabolized accumulate in the systemic circulation. In a normally functioning liver, hepatocytes degrade ammonia to form urea, which is renally excreted. In cirrhosis, conversion to urea is reduced and ammonia accumulates, resulting in encephalopathy. These diseases vary widely in prevalence, disease progression, and treatment options.

Buy generic ampicillin
Daily left prefrontal repetitive transcranial magnetic stimulation for acute treatment of medication resistant depression antimicrobial office supplies order ampicillin 500 mg without a prescription. Adverse effects from antidepressant treatment: Randomized controlled trial of 601 depressed individuals. Individualized pharmacological treatment of depressive disorders state of the art and recent developments. Major depressive disorder: New clinical, neurobiological and treatment perspectives. Stressful life events, chronic difficulties, and the symptoms of clinical depression. Age-related changes in antidepressant pharmacokinetics and potential drug-drug interactions: A comparison of evidence-based literature and package insert information. Changes in intensity of serotonin syndrome caused by adverse interaction between monoamine oxidase inhibitors and serotonin reuptake blockers. Selective versus multi-transmitter antidepressants: Are two mechanisms better than one Clinical results for patients with major depressive disorder in the Texas Medication Algorithm Project. Meta-analysis on the efficacy and tolerability of the augmentation of antidepressants with atypical antipsychotics in patients with major depressive disorder. Treatment-resistant depression: Definitions, review of the evidence, and algorithmic approach. The use of contemporary antidepressants during breastfeeding: A proposal for a specific safety index. Treatment of depression in the elderly: A review of the recent literature on the efficacy of singleversus dual action antidepressants. Recognize the symptoms of a manic episode and depressive episode in patients with bipolar disorder. Recommend individualized drug therapy for acute treatment and relapse prevention based on patientspecific data. Recommend monitoring methods for assessment of therapeutic and adverse effects of drugs used in the treatment of bipolar disorder. Recommend treatment approaches for special populations of patients with bipolar disorder, including pediatric patients, geriatric patients, and pregnant patients. Educate patients with bipolar disorder about their illness, drug therapy required for effective treatment, and the importance of adherence. Disability and other consequences (eg, increased risk of suicide) can be devastating to patients and families. Correct and early diagnosis and treatment are essential to prevent complications and maximize response to treatment. Hypomania is an abnormally and persistently elevated, expansive, or irritable mood but not of sufficient severity to cause significant impairment and does not require hospitalization. When including the entire spectrum of bipolar disorders, the prevalence is approximately 3%. The most common comorbid conditions are anxiety, substance abuse, and impulse control disorders. An early onset is associated with greater comorbidities, more mood episodes, a greater proportion of days depressed, and greater lifetime risk of suicide attempts compared with later onset. Substance abuse and anxiety disorders are more common in patients with early onset. Patients with bipolar disorder have higher rates of suicidal thoughts, attempts, and completed suicides than the general population. Thought to be genetically based, bipolar disorder is influenced by a variety of factors that may enhance gene expression. These include trauma, environmental factors, anatomical abnormalities, and exposure to chemicals or drugs. The patient states she has only come for the appointment because her family insisted and was concerned because she was "not acting like myself. Joan is a single, well-nourished, well-developed African American woman appearing her stated age. She is attired in a low-cut blouse and short skirt, very high heels, and is wearing bright lipstick, false eyelashes, purple eye shadow, and an excessive amount of perfume. She seems to have difficulty maintaining an appropriate social distance during the interview and is at times flirtatious and somewhat seductive. She states she is very energetic and enjoyed partying with her friends over spring break, getting approximately 1 to 2 hours of sleep each night but feeling fine the following day. Although Joan has been an excellent student in the past, her grades this semester have been slipping, as she has found it difficult to complete assignments and is now in danger of failing. She states she is not concerned about her classes as she is considering going to New York to become a model. Although Joan has always been a good money manager, recently she has gone on extensive shopping sprees, buying clothing and jewelry she cannot afford. One hypothesis is that bipolar disorder is caused by an imbalance of cholinergic and catecholaminergic activity. A variety of neurotransmitters are involved that interact with multiple neurochemical and neuroanatomic pathways. Lithium, valproate, and carbamazepine all have similar effects on neuronal growth that are reversible by inositol, supporting a hypothesis that bipolar disorder may be related to inositol disturbance. The defining feature of bipolar disorder is one or more manic or hypomanic episodes in addition to depressive episodes that are not caused by a medical condition, substance abuse, or other psychiatric disorder. She states none of her relationships has lasted more than a few weeks, although she would like to eventually get married. She is presently majoring in mathematics and previously aspired to be a high school teacher; however, she has failing grades in most of her classes this semester. She does admit to smoking marijuana on a daily basis, has experimented with cocaine in the past, and drinks heavily on the weekends. Positive bowel sounds in all four quadrants Exts: Without clubbing, cyanosis, or edema. Factors that increase risk are early age at onset, high number of depressive episodes, comorbid alcohol abuse, personal history of antidepressant-induced mania, and family history of suicidal behavior. During the same period of illness, there have been delusions or hallucinations for at least 2 weeks in the absence of prominent mood symptoms. The two diagnoses are distinguished by the predominance of mood symptoms and the episodic course of bipolar disorder in contrast to the stability and persistence of the behavioral patterns of personality disorders. The prominence of mood symptoms and the history of mood episodes distinguish bipolar disorder and schizophrenia. In addition, psychosis of schizophrenia occurs in the absence of prominent mood symptoms. Schizoaffective disorder may also be considered when developing a differential diagnosis. Schizoaffective disorder is characterized by a period of illness during which there is a major depressive episode or a manic episode, concurrent with symptoms that Lifetime prevalence rates of comorbidity with bipolar disorder are as high as 58%. Comorbidities also place the patient at risk for a poorer outcome, high rates of suicidality, onset of depression, and higher costs of treatment. General the patient may present in a hypomanic, manic, depressed, or mixed state and may or may not be in acute distress. There are no laboratory examinations, brain imaging studies, or other procedures that confirm the diagnosis, but such testing can be done to rule out other medical diagnoses. Your plan should include (a) a statement of the drug-related needs or problems, (b) the goals of therapy, (c) a patient-specific therapeutic plan, and (d) a plan for follow-up to assess therapeutic response and adverse effects.