Cheap 75mg diclofenac free shipping
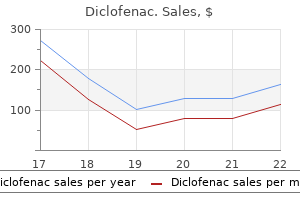
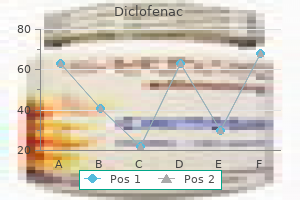
The peritoneum may be used as an additional layer or injuries near the peritoneal re ection arthritis swollen knee exercises 50 mg diclofenac for sale. During repair, a digit in the rectum exposes the de ect, tissues surrounding the de ect are mobilized, the site is copiously irrigated, and appropriate antibiotic prophylaxis is provided or 24 hours (Ho man, 1999). In general, small (< 2 cm) rectal injuries recognized and repaired at the time o vaginal surgery tend to heal well without complications or stula ormation (Mathevet, 2001). Diet can be advanced as tolerated, but a stool so tener is recommended once the patient is taking solid oods (Ho man, 1999). J Appl Biomater 4:241, 1993 Baxter Healthcare: Floseal hemostatic matrix: instructions or use. Am J Surg 188(3):307, 2004 Bose P, Regan F, Paterson-Brown S: Improving the accuracy o estimated blood loss at obstetric haemorrhage using clinical reconstructions. Obstet Gynecol 85:269, 1995 Bucknall E: Factors in uencing wound complications: a clinical and experimental study. Am Surgeon 61(11):980, 1995 Carney J, McDonell J, Ochana A, et al: the transversus abdominis plane block provides e ective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 107:2056, 2008 Chanrachakul B, Likittanasombut P, Prasertsawat P, et al: Lidocaine versus plain saline or pain relie in ractional curettage: a randomized controlled trial. Obstet Gynecol 98(4):592, 2001 Chappell D, Jacob M, Ho mann-Kie er K, et al: A rational approach to perioperative uid management. Urology 46(4):575, 1995 Cicinelli E, Didonna, Ambrosi G, et al: opical anaesthesia or diagnostic hysteroscopy and endometrial biopsy in postmenopausal women: a randomised placebo-controlled double-blind study. J Reprod Med Obstet Gynecol 43(12):1014, 1998 Colombo M, Maggioni A, Parma G, et al: A randomized comparison o continuous versus interrupted mass closure o midline incisions in patients with gynecologic cancer. Gynecol Oncol 100(2):283, 2006 Amaral J: Electrosurgery and ultrasound or cutting and coagulating tissue in minimally invasive surgery. In Soper N, Swanstrom L, Eubanks W (eds): Mastery o Endoscopic and Laparoscopic Surgery. Philadelphia, Lippincott Williams & Wilkins, 2005, p 67 American College o Obstetricians and Gynecologists: the role o cystourethroscopy in the generalist obstetrician-gynecologist practice. New York, Appleton-Century-Cro ts, 1980 Anderton J, Keen R, Neave R: the lithotomy position. Obstet Gynecol 70(5):706, 1987 Barrington J, Dalury D, Emerson R, et al: Improving patient outcomes through advanced pain management techniques in total hip and knee arthroplasty. New York, McGraw-Hill Education, 2015 Demirci F, Ozdemir I, Sa ak A, et al: Comparison o colour Doppler indices o pelvic arteries in women with bilateral hypogastric artery ligation and controls. J Obstet Gynaecol 25(3):273, 2005 De Oliveira G Jr, Agarwal D, Benzon H: Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis o randomized trials. Anesth Analg 114:424, 2012 De Oliveira G Jr, Castro-Alves L, Nader A, et al: ransversus abdominis plane block to ameliorate postoperative pain outcomes a ter laparoscopic surgery: a meta-analysis o randomized controlled trials. Am J Surg 181(2):128, 2001 Franchi M, Ghezzi F, Zanaboni F, et al: Nonclosure o peritoneum at radical abdominal hysterectomy and pelvic node dissection: a randomized study. Obstet Gynecol 99(5 Pt 1):745, 2002 Gilmour D, Das S, Flowerdew G: Rates o urinary tract injury rom gynecologic surgery and the role o intraoperative cystoscopy. Eur J Obstet Gynecol Reprod Biol 20(6):385, 1985 Goodnough L: Autologous blood donation. Anesthesiol Clin North Am 23(2):263, 2005 Gorgas D: rans usion therapy: blood and blood products. Clin Obstet Gynecol 45(2):481, 2002 Grantcharov P, Rosenberg J: Vertical compared with transverse incisions in abdominal surgery. Am J Obstet Gynecol 178(4):796, 1998 Guvenal, Duran B, Kemirkoprulu N, et al: Prevention o super cial wound disruption in P annenstiel incisions by using a subcutaneous drain. Int J Gynecol Obstet 77:151, 2002 Gyr, Ghezzi F, Arslanagic S, et al: Minimal invasive laparoscopic hysterectomy with ultrasonic scalpel. Obstet Gynecol 113:6, 2009 Irvin W, Andersen W, aylor P, et al: Minimizing the risk o neurologic injury in gynecologic surgery. Gastric bypass and on-Q pump: e ectiveness o soaker catheter system on recovery o bariatric surgery patients. Am J Obstet Gynecol 189(2):423, 2003 Joint Commission: Universal protocol or preventing wrong site, wrong procedure, and wrong person surgery. Oakbrook errace, Joint Commission, 2009 Joshi G: Intraoperative uid restriction improves outcome a ter major elective gastrointestinal surgery. Dermatol Surg 25(9):686, 1999 Kauko M: New techniques using the ultrasonic scalpel in laparoscopic hysterectomy. Acta Clin Belg 51(3):156, 1996 Kolle D, amussino K, Hanzal E, et al: Bleeding complications with the tension- ree vaginal tape operation. Acta Obstet Gynecol Scand 81(1):72, 2002 Kvist-Poulsen H, Borel J: Iatrogenic emoral neuropathy subsequent to abdominal hysterectomy: incidence and prevention. Crit Care Med 34(5 Suppl):S102, 2006 Makinen J, Johansson J, omas C, et al: Morbidity o 10110 hysterectomies by type o approach. In Nichols D, DeLancey J (eds): Clinical Problems, Injuries and Complications o Gynecologic and Obstetric Surgery. Baltimore, Williams & Wilkins, 1995, p 14 Mathevet P, Valencia P, Cousin C, et al: Operative injuries during vaginal hysterectomy. Br J Haematol 113(1):24, 2001 Nagpal K, Vats A, Ahmed K, et al: A systematic quantitative assessment o risks associated with poor communication in surgical care. Obstet Gynecol 85:412, 1995 Neuman M, Eidelman A, Langer R, et al: Iatrogenic injuries to the ureter during gynecologic and obstetric operations. In Newton M, Newton E (eds): Complications o Gynecologic and Obstetric Management. Am J Obstet Gynecol 163(5 Pt 1):1485, 1990 Patel H, Bhatia N: Universal cystoscopy or timely detection o urinary tract injuries during pelvic surgery. Baltimore, Urban and Schwarzenberg, 1986, p 48 Perel P, Roberts I, Ker K: Colloids versus crystalloids or uid resuscitation in critically ill patients. Am J Obstet Gynecol 186(6):1304, 2002 Philosophe R: Avoiding complications o laparoscopic surgery. Pacing Clin Electrophysiol 25(10):1496, 2002 Popert R: echniques rom the urologists. In Steege J, Metzger D, Levy B (eds): Chronic Pelvic Pain: an Integrated Approach. Eur J Obstet Gynecol Reprod Biol 101(2):179, 2002 Santoso J, Dinh A, Omar S, et al: Surgical blood loss in abdominal hysterectomy. Am J Obstet Gynecol 187:1438, 2002 Schwartz D, Kaplan K, Schwartz S: Hemostasis, surgical bleeding, and trans usion. Primary among these are patient actors, availability o appropriate instrumentation, and surgeon skill. T us, laparoscopy is appropriate or many, although modi cations are warranted or certain clinical situations. Prior Surgeries With laparoscopy, adhesive disease increases the risk o visceral and vascular injury during abdominal entry. Adhesions are also associated with higher conversion rates to laparotomy because long and tedious adhesiolysis may be completed by some surgeons more quickly with open surgical dissection techniques. T us, during preoperative physical examination, a surgeon notes the location o previous surgical scars and ascertains the risk o possible intraabdominal adhesive disease (Table 41-1). Similarly, a history o endometriosis, pelvic in ammatory disease, or radiation treatment may predispose to adhesions. In addition, abdominal wall hernias or hernia repairs and any reparative mesh are identi ed and avoided during trocar insertion. I abnormal ndings are ound during this preoperative evaluation, plans or an alternative entry site are considered (p. With laparoscopy, small abdominal incisions provide access to introduce an endoscope and surgical instruments into the abdomen. As such, laparoscopy provides a minimally invasive option or women undergoing intraabdominal gynecologic surgery. Hysteroscopy uses an endoscope and uterine cavity distending medium to provide an internal view o the endometrial cavity. This tool permits both the diagnosis and operative treatment o intrauterine pathology. Laparoscopic Physiology Compared with traditional open laparotomy, laparoscopy produces several distinct cardiovascular and pulmonary physiologic changes. These changes are typically tolerated by those in generally good health but may be less so in those with cardiovascular or pulmonary compromise.
Diclofenac 50mg mastercard
Autologous blood donation or cell saver devices may be considered i great blood loss is expected bacterial arthritis in dogs discount 50mg diclofenac mastercard. In addition, uterine artery embolization may be per ormed the morning o surgery or large uteri to minimize blood loss. However, loss o pseudocapsule planes around the tumors and greater risk o recurrence due to missed smaller leiomyomas is the trade-of. A uller evidence-based discussion o these same preoperative options is ound in Section 43-10 (p. Instruments Many instruments required or laparoscopic myomectomy are ound in a standard laparoscopy instrument set. However, a laparoscopic injection needle may be required or vasopressin injection, and a suction irrigation system is requently needed to remove blood ollowing tumor enucleation. A myoma screw or tenaculum is help ul to create needed tissue tension and countertension or enucleation. A ter tumor excision, removal may be accomplished by several techniques described on page 1031. As with most laparoscopic procedures, the patient is placed in low dorsal lithotomy position in booted support stirrups a ter adequate general anesthesia has been delivered. A bimanual examination is completed to determine uterine size to aid port placement. Because o the risk o hysterectomy and because colpotomy may be used or tumor removal, both the vagina and abdomen are surgically prepared. I planned, indigo carmine or methylene blue dye is mixed with 50 to 100 mL o sterile saline or injection through the cervical cannula. Port placement is customized to assist uterine manipulation, leiomyoma excision, and hysterotomy repair. Depending on uterine height, the primary port may need to be placed supraumbilically. In general, a distance o at least 4 cm above the level o the undus is helpul to provide a global view o the uterus. I use o an electric morcellator is planned, one o the cannulas should be at least 12 mm to accommodate the morcellator. A ter the abdomen is sa ely entered, a diagnostic laparoscopy is per ormed, and the serosal uterine sur ace should be inspected to identi y leiomyomas to be removed. Correlating with preoperative imaging, the surgeon selects the optimal uterine incision to minimize myometrial disruption and to remove the maximum number o tumors thorough one incision. It is ef ective in limiting uterine blood loss during myomectomy because o its ability to cause vascular spasm and uterine muscle contraction. Compared with placebo, vasopressin injection has been shown to signi cantly decrease blood loss during myomectomy (Frederick, 1994). Suitable doses or myomectomy include 20 U diluted in a range rom 30 to 100 mL o saline (Fletcher, 1996; Iverson, 1996). Vasopressin is typically injected along the planned serosal incision(s), between the myometrium and leiomyoma capsule. A laparoscopic needle placed through one o the accessory ports or a 22-gauge spinal needle placed directly through the abdominal wall is suitable or injection. The anesthesiologist is in ormed o vasopressin injection, as a sudden increase in patient blood pressure may potentially occur ollowing injection. For this reason, injection o vasopressin is discontinued 20 minutes prior to uterine repair to allow evaluation o bleeding rom myometrial incisions (Hutchins, 1996). The main risks associated with local vasopressin injection result rom inadvertent intravascular in ltration and include transient increases in blood pressure, bradycardia, atrioventricular block, and pulmonary edema (Hobo, 2009; ulandi, 1996). For these reasons, patients with a medical history o cardiac or pulmonary disease may be poor candidates or vasopressin use. Because o postoperative adhesion ormation risks, surgeons minimize the number o serosal incisions and attempt to place incisions on the anterior uterine wall. A ter vasopressin injection, hysterotomy may be per ormed using a Harmonic scalpel, monopolar electrode, or laser. For most patients, an anterior midline vertical uterine incision allows removal o the greatest number o leiomyomas through the ewest incisions. Once the hysterotomy is created, the myometrium will generally retract, and the rst leiomyoma may be grasped with a laparoscopic single-toothed tenaculum. Alternatively, a leiomyoma screw can also retract tissue to create tension between the myometrium and mass. The same general principles o myometrial closure or abdominal myomectomy are employed during laparoscopic myomectomy. In one method, or deep myometrial closure, a needle driver can be used with 0-gauge delayedabsorbable suture on a C -2 needle in a continuous running ashion. The primary incision(s) is then closed in layers to improve hemostasis and prevent hematoma ormation. A gauge o su cient strength to prevent breakage during muscle approximation is selected, typically 0 to 2-0 gauge. Alternatively, barbed sutures can close myometrial de ects during laparoscopic myomectomy. These obviate the need or knot tying and yield consistent wound opposition (Einarsson, 2010; Greenberg, 2008). Closure o the serosal incision using a running suture line with 4-0 or 5-0 gauge mono lament delayedabsorbable suture may help to limit adhesion ormation. Moreover, absorbable adhesion barriers have been shown to reduce the incidence o adhesion ormation ollowing myomectomy and may be introduced through laparoscopic ports (Ahmad, 2008). However, no substantial evidence documents that adhesion barrier use improves ertility, decreases pain, or prevents bowel obstruction (American Society or Reproductive Medicine, 2013). Once amputated, the myomas must be removed, and options include minilaparotomy, colpotomy, and tissue morcellation. The procedure is initiated as described above, and abdominal cavity assessment, uterine inspection, and incision o the serosa and myometrium are per ormed adjacent myometrium. Areas requiring sharp dissection rom the myometrium may be reed with any o the electrosurgical instruments that were used or the uterine incision. Hemorrhage during myomectomy primarily develops during tumor enucleation and positively correlates with preoperative uterine size, total weight o leiomyomas removed, and operating time (Ginsburg, 1993). For this reason, surgeons must watch or these vessels, coagulate them prior to transection when possible, and be ready to immediately ulgurate remaining bleeding vessels. Speci cally, tumor enucleation and uterine closure are completed through a 2- to 4-cm minilaparotomy incision placed suprapubically. With this, the pneumoperitoneum and visualization through the laparoscope are lost. The uterus and leiomyoma are brought to the sur ace o the anterior abdominal wall and through the laparotomy incision. This open incision also allows or conventional suturing techniques and aids suturing o large de ects that require a multilayer closure. Advantages include decreased operative time, technical simplicity, improved tactile sensation to detect deep intramural leiomyomas, and easier removal o very large tumors (Prapas, 2009; Wen, 2010). LaMorte and colleagues (1993) noted only a 2-percent rate o pelvic in ection in their analysis o 128 open myomectomy cases. Hospitalization typically varies rom 0 to 1 days, and ebrile morbidity and return o normal bowel unction usually dictate this course (Barakat, 2011). Postoperative activity in general can be individualized, although vigorous exercise is usually delayed until 4 weeks a ter surgery. Subsequent Pregnancy There are no clear guidelines as to the timing o pregnancy attempts ollowing myomectomy. Darwish and colleagues (2005) per ormed sonographic examinations on 169 patients ollowing open myomectomy. Following myometrial indicators, they concluded that wound healing is usually completed within 3 months. There are no clinical trials that address the issue o uterine rupture and there ore route o delivery o pregnancies occurring a ter myomectomy (American College o Obstetricians and Gynecologists, 2014a). In general, large incisions or those entering the endometrial cavity avor cesarean delivery. These include signi cant lower analgesia requirements, shorter hospital stays, rapid recovery, greater patient satisaction, and lower rates o wound in ection and hematoma ormation (Kluivers, 2007; Schindlbeck, 2008). Disadvantageously, surgical time is lengthened, although the learning curve may be a actor. However, a wide bulky uterus with minimal mobility may make it di cult to visualize vital structures, to manipulate the uterus during surgery, and to remove it vaginally.
Purchase discount diclofenac
This histologic diversity explains why only a small number o conserved eatures are use ul as diagnostic criteria psoriatic arthritis elimination diet order diclofenac master card. As a result, reproducible scoring o cytologic atypia is o ten challenging, particularly with a small amount o tissue rom a biopsy sample. Using this system, anovulatory or prolonged estrogen-exposed endometria without atypia are generally designated as endometrial hyperplasias. The qualities re ect glandular volume, architectural complexity, and cytologic abnormality. This classi cation is endorsed by the Society o Gynecologic Oncology and American College o Obstetricians and Gynecologists (2015) but has not been universally implemented. In this sagittal view, the markedly thickened endometrium, which is measured by the calipers, suggests endometrial hyperplasia. In postmenopausal women, endometrial stripe thickness measurements 4 mm are associated with bleeding that is attributed to endometrial atrophy (American College o Obstetricians and Gynecologists, 2013). Cystic endometrial changes suggest polyps, homogeneously thickened endometrium may indicate hyperplasia, and a heterogeneous structural pattern is suspicious or malignancy. For premenopausal women, transvaginal sonography is o ten per ormed to exclude structural sources o abnormal bleeding. However, endometrial thicknesses can vary considerably among premenopausal women during normal menstrual cycling. From studies, suggested evidencebased abnormal thresholds range rom > 4 mm to > 16 mm (Breitkop, 2004; Goldstein, 1997; Shi, 2008). T us, consensus or an endometrial thickness threshold has not been established or this group. The abnormal endometrium is thickened, echogenic, and heterogeneous in echotexture and contains tiny cystic foci. Biopsy revealed grade 1 endometrioid adenocarcinoma, which was confirmed at surgery. Occasionally, an adnexal mass may be palpable during examination and in most cases is a benign ovarian cyst. These tumors produce excess estrogen that results in up to a 30-percent risk o endometrial hyperplasia or less commonly, endometrial carcinoma (Chap. In most cases, a orm o progestin therapy is used to treat endometrial hyperplasia without atypia. But, a ected postmenopausal patients who have a contraindication to progestin therapy or who cannot tolerate the therapy can be expectantly managed. Complex hyperplasia without atypia is usually treated chronically with progestins. With either complex or simple hyperplasia without atypia, o ce endometrial biopsy is recommended every 3 to 6 months until lesion resolution is achieved. In cases o endometrial hyperplasia without atypia, the risk o progression to endometrial cancer is low (1 to 3 percent). The overall clinical and pathologic regression rates to progestin therapy range rom 70 to 80 percent or nonatypical endometrial hyperplasia (Rattanachaiyanont, 2005; Reed, 2009). It can be increased even up to 160 mg twice daily i no regression is initially achieved. Again, a clinician must con rm that hormonal ablation has occurred by resampling the endometrium a ter a suitable therapeutic interval, usually 3 to 6 months. Hysterectomy may also be considered or lesions that are re ractory to medical management. In cases in which hyperplasia has been proven or is suspected, the uterus is removed in toto and without morcellation, which might disseminate the lesion. Because the lesion may extend into the lower uterine segment or upper endocervix, supracervical hysterectomy is not appropriate or women undergoing hysterectomy or treatment o endometrial hyperplasia. There is some inconsistency o diagnosis and uncertainty in predicting the stability o individual lesions. In addition, there is no way to anticipate which types will involute with progestin therapy. However, as long as an endometrial sample is representative and a provider has no reason to suspect a coexisting invasive carcinoma, the decision to treat endometrial hyperplasia through hormonal or surgical means relies on clinical judgment. H owever, progestins are generally used to address the underlying etiology, that is, chronic anovulation and excess estrogen (erakawa, 1997). Premenopausal women with nonatypical endometrial hyperplasia typically require a 3- to 6-month course o low-dose progestin therapy. T us, once hyperplastic changes resolve, patients are continued on progestins and observed until menopause. However, it is particularly important in older women to be con dent that the sample obtained is adequate or excluding cytologic atypia. D & C may be indicated in some Atypical Endometrial Hyperplasia Hysterectomy is the pre erred treatment or women with atypical endometrial hyperplasia because the risk o progression to cancer over time approximates 29 percent. There is also a high rate o nding concurrent invasive malignancy coexistent with the atypical hyperplasia (Horn, 2004; rimble, 2006). In postmenopausal women, a hysterectomy with removal o both tubes and ovaries is recommended. In premenopausal women who have completed childbearing, hysterectomy is per ormed or atypical hyperplasia. Riskreducing salpingectomy is encouraged to potentially lower cancer risk that arises rom the allopian tubes (American College o Obstetricians and Gynecologists, 2015d). Premenopausal women who strongly wish to preserve ertility can be treated with progestins (rimble, 2012). High-dose progestin therapy, megestrol acetate 80 mg orally twice daily, is an option or motivated patients who will be compliant with surveillance (Randall, 1997). Poor surgical candidates may also warrant an Endometrial Cancer attempt at hormonal ablation with progestins. Resolution o the hyperplasia must be con rmed by serial endometrial biopsies every 3 months until response is documented. Following hyperplasia resolution, surveillance and progestins continue long-term due to the potential or eventual progression to carcinoma (Rubatt, 2005). Participants underwent hysterectomy within 3 months o their biopsy, and 43 percent were ound to have a concurrent endometrial carcinoma (rimble, 2006). Results demonstrate the di culty in attaining an accurate diagnosis be ore hysterectomy and the potential risks o conservative hormonal treatment. At a minimum, peritoneal washings are obtained prior to per orming a hysterectomy. From this, a rozen section analysis can be per ormed to search or concurrent cancer and determine grade and depth o invasion i ound. Any suspicion or myometrial invasion is an appropriate indication or intraoperative consultation with a gynecologic oncologist. Prevention Education can be e ective prevention, as many endometrial cancer risks are alterable. For women at average risk or increased risk, routine screening o hyperplasia or endometrial cancer is not advocated. Instead, at the onset o menopause, women are counseled on the risks and symptoms o endometrial cancer and strongly encouraged to report unexpected bleeding or spotting to their provider. Genetic testing criteria have been published to identi y the individual with Lynch syndrome (Table 33-4) (Lancaster, 2015). Lynch syndrome cancers include colon, endometrium, small bowel, renal pelvis and ureter, and ovary, among others (Vasen, 1999). Re erral or genetic counseling can urther clari y which patients may bene t rom speci c germline testing (Balmana, 2006; Chen, 2006). Endometrial cancer is the most common "sentinel cancer," thus, obstetrician-gynecologists play a pivotal role in the identi cation o women with Lynch syndrome (Lu, 2005). They are estrogen-dependent, low grade, and derived rom atypical endometrial hyperplasia. The two pathways o endometrial cancer pathogenesis have signi cant overlap and thus result in a spectrum o histologic eatures.
Buy generic diclofenac 100mg on line
They range rom connective tissue structures that support the bony pelvis and pelvic organs to smooth muscle and loose areolar tissue that add no signi cant support arthritis pain reliever order diclofenac discount. The sacrospinous, sacrotuberous, and anterior longitudinal ligaments o the sacrum consist o dense connective tissue that joins bony structures and contributes signi cantly to bony pelvis stability. The round and broad ligaments consist o smooth muscle and loose areolar tissue, respectively. Pelvic parietal ascia provides muscle attachment to the bony pelvis and serves as anchoring points or visceral ascia, also termed endopelvic ascia. The arcus tendineus levator ani is a condensation o parietal ascia covering the medial sur ace o the obturator internus muscle. This structure serves as the point o origin or parts o the very important levator ani muscle. Also shown is the arcus tendineus ascia pelvis, a condensation o parietal ascia covering the medial aspects o the obturator internus and levator ani muscles. Physiologically, normal levator ani muscles maintain a constant state o contraction, thus providing a stable oor, which supports the weight o the abdominopelvic contents against intraabdominal orces. The levator ani muscle is a complex unit, which consists o several muscle components with di erent origins and insertions and there ore di erent unctions. The pubococcygeus, puborectalis, and iliococcygeus muscles are the three components. O these, the pubococcygeus muscle is urther divided into the pubovaginalis, puboperinealis, and puboanalis muscles according to their ber attachments. Due to the signi cant attachments o the pubococcygeus muscle to the walls o the pelvic viscera, the term pubovisceral muscle is requently used (Kerney, 2004; Lawson, 1974). Pubococcygeus Muscle the anterior ends o the pubococcygeus (pubovisceral muscle) arise on either side rom the inner sur ace o the pubic bone. The pubovaginalis re ers to the medial bers that attach to the lateral walls o the vagina. Although there are no direct attachments o the levator ani muscles to the urethra in emales, those bers o the muscle that attach to the vagina are responsible or elevating the urethra during a pelvic muscle contraction and hence may contribute to urinary continence (DeLancey, 1990). The puboperinealis re ers to the bers that attach to the perineal body and draw this structure toward the pubic symphysis. The puboanalis re ers to the bers that attach to the anus at the intersphincteric groove between the internal and external anal sphincters. These bers elevate the anus and, along with the rest o the pubococcygeus and puborectalis bers, keep the urogenital hiatus narrowed. This diaphragm consists o the levator ani and coccygeus muscles, along with their superior and in erior investing ascial layers. In erior to the pelvic diaphragm, the perineal membrane and perineal body also contribute to the pelvic oor (p. The urogenital hiatus is the U-shaped opening in the pelvic oor muscles through which the urethra, vagina, and rectum pass. Levator Ani Muscles These are the most important muscles in the pelvic oor and provide critical pelvic organ support. Puborectalis Muscle the puborectalis represents the medial and in erior bers o the levator ani muscle that arise on either side rom the pubic bone and orm a U-shaped sling behind the anorectal junction. The action o the puborectalis draws the anorectal junction toward the pubis, contributing to the anorectal angle. This muscle is considered part o the anal sphincter complex and may contribute to ecal continence (Chap. Iliococcygeus Muscle this muscle is the most posterior and thinnest part o the levator ani muscle and has a primarily supportive role. Muscle bers rom one side join those rom the opposite side in the midline between the anus and the coccyx. In addition to the iliococcygeus muscle, some bers o the pubococcygeus muscle pass behind the rectum and attach to the coccyx. These muscle bers course cephalad or deep to the iliococcygeus muscle and may also contribute to the anococcygeal raphe. This portion o the levator muscles orms a supportive shel on which the rectum, upper vagina, and uterus rest. The levator plate in women with normal support has a mean angle o 44 degrees relative to a horizontal re erence line during Valsalva, although earlier studies suggested no elevation (Berglas, 1953; Hsu, 2006). During Valsalva, women with prolapse have a statistically greater levator plate angle compared with controls. Such separate innervation may explain why some women develop pelvic organ prolapse and others develop urinary or ecal incontinence (Heit, 1996). This tissue connects the pelvic viscera to the pelvic walls and is termed visceral or endopelvic " ascia. Visceral ascia is intimately associated with the walls o the viscera and cannot be dissected in the same way that parietal ascia can be separated rom its skeletal muscle. Condensations o visceral connective tissue that have assumed special supportive roles have been given di erent names. Some examples include the cardinal and uterosacral ligaments and the vesicovaginal and rectovaginal ascia. Neuromuscular injury to the levator muscles may lead to eventual sagging or vertical inclination o the levator plate and opening o the urogenital hiatus. Consequently, the vaginal axis becomes more vertical, and the cervix is oriented over the opened hiatus. The mechanical e ect o this change is to increase strain on connective tissues that support the pelvic viscera. Increased urogenital hiatus size has been shown to correlate with increased prolapse severity (DeLancey, 1998). The pelvic organs are supplied by the visceral branches o the internal iliac (hypogastric) artery and by direct branches rom the abdominal aorta. Clinically, the internal iliac artery can be separated into an anterior and posterior division in the area o the greater sciatic oramen. The iliolumbar, lateral sacral, and superior gluteal arteries are the three parietal branches o the posterior division. The internal pudendal, obturator, and in erior gluteal arteries are parietal branches that most commonly arise rom the anterior division. The remaining branches o the anterior division supply pelvic viscera (bladder, uterus, vagina, and rectum). These include the uterine, vaginal, and middle rectal arteries and the superior vesical arteries. The superior vesical arteries commonly arise rom the patent part o the umbilical arteries (Table 38-2). Internal iliac branches that supply the in erior and middle portions o the bladder are present in women, but their origin is highly variable. The middle rectal arteries are generally very small-caliber vessels but may be absent. The two most important direct branches o the aorta that contribute to pelvic organ blood supply are the superior rectal and ovarian arteries. The superior rectal artery, which is the terminal branch o the in erior mesenteric artery, anastomoses with the middle rectal arteries, thus contributing blood supply to the Pelvic Floor Innervation the pelvic diaphragm muscles are primarily innervated by direct somatic e erents rom the second through the th sacral nerve roots (S2-5). The pelvic or superior sur ace o the muscles is supplied by direct e erents rom S2-5, collectively known as the nerve to the levator ani muscle. This latter relationship has been challenged, and investigators suggest that the pudendal nerve does not contribute to levator muscle innervation (Barber, 2002). The ovarian arteries arise directly rom the aorta just in erior to the renal vessels and anastomose with the ascending branch o the uterine artery. Other important anastomoses between the aorta and internal iliac arteries include anastomoses between the middle sacral and lateral sacral arteries and anastomoses between the lumbar and iliolumbar arteries. In addition, the in erior hypogastric plexus generally receives contributions rom the sacral sympathetic trunk. With variability, bers o the in erior hypogastric plexus accompany the branches o the internal iliac artery to the pelvic viscera. Extensions o the in erior hypogastric plexus reach the perineum along the vagina and urethra to innervate the clitoris and vestibular bulbs.
Diseases
- Mount Reback syndrome
- Epidermolysis bullosa, junctional, with pyloric atrophy
- Sinus histiocytosis
- Retrolental fibroplasia
- Cone-rod dystrophy
- Chromosome 19 ring
- Cutis laxa, recessive type 1
- Muscular dystrophy limb-girdle with beta-sarcoglycan deficiency
- DiGeorge syndrome
- Hiccups
Order diclofenac 75 mg line
Ultrasound Obstet Gynecol 34:188 arthritis young living oils order diclofenac 75mg with visa, 2009 Palenzuela G, Martin E, Meunier A, et al: Comprehensive staging allows or excellent outcome in patients with localized malignant germ cell tumor o the ovary. Ann Surg 248:836, 2008 Pavlakis K, Messini I, Vrekoussis, et al: Intraoperative assessment o epithelial and non-epithelial ovarian tumors: a 7-year review. Am J Surg Pathol 20:823, 1996 Piura B, Nemet D, Yanai-Inbar I, et al: Granulosa cell tumor o the ovary: a study o 18 cases. N Engl J Med 360:2719, 2009 Sharony R, Aviram R, Fishman A, et al: Granulosa cell tumors o the ovary: do they have any unique ultrasonographic and color Doppler ow eatures Int J Gynecol Cancer 23(2):249, 2013 Shimizu Y, Komiyama S, Kobayashi, et al: Success ul management o endodermal sinus tumor o the ovary associated with pregnancy. Obstet Gynecol 87:737, 1996 Suita S, Shono K, ajiri, et al: Malignant germ cell tumors: clinical characteristics, treatment, and outcome. A report rom the study group or Pediatric Solid Malignant umors in the Kyushu Area, Japan. J Pediatr Surg 37:1703, 2002 akemori M, Nishimura R, Yamasaki M, et al: Ovarian mixed germ cell tumor composed o polyembryoma and immature teratoma. Gynecol Oncol 69:260, 1998 alukdar S, Kumar S, Bhatla N, et al: Neo-adjuvant chemotherapy in the treatment o advanced malignant germ cell tumors o ovary. Gynecol Oncol 132(1):28, 2014 angir J, Zelterman D, Ma W, et al: Reproductive unction a ter conservative surgery and chemotherapy or malignant germ cell tumors o the ovary. Obstet Gynecol 101:251, 2003 eilum G: Classi cation o endodermal sinus tumour (mesoblastoma vitellinum) and so-called "embryonal carcinoma" o the ovary. Mod Pathol 18 (Suppl 2):S61, 2005 Uygun K, Aydiner A, Saip P, et al: Clinical parameters and treatment results in recurrent granulosa cell tumor o the ovary. Chin Med J 117:1592, 2004 Zagame L, Pautier P, Duvillard P, et al: Growing teratoma syndrome a ter ovarian germ cell tumors. Am J Surg Pathol 8:405, 1984 Zanagnolo V, Pasinetti B, Sartori E: Clinical review o 63 cases o sex cord stromal tumors. Eur J Gynaecol Oncol 25:431, 2004 Zanetta G, Bonazzi C, Cantu M, et al: Survival and reproductive unction a ter treatment o malignant germ cell ovarian tumors. The outlook or preservation o ertility and or success ul subsequent pregnancy outcomes is equally bright (Vargas, 2014; Wong, 2014). Although historically higher incidence rates have been reported in parts o Asia, some o this disparity may re ect discrepancies between population-based and hospital-based data collection (Chong, 1999; Kim, 2004; Matsui, 2003). Improved socioeconomic conditions and dietary changes may be partly responsible as well. T at said, certain Southeast Asian populations as well as Hispanics and Native Americans living in the United States do have increased incidences (Drake, 2006; Smith, 2003; T am, 2003). This association is much greater or complete moles, whereas the risk o partial molar pregnancy varies relatively little with age. Moreover, compared with the risk in those aged 15 years or younger, the degree o risk is much greater or women 45 years (1 percent) or older (17 percent at age 50) (Savage, 2010; Sebire, 2002a). One explanation relates to ova rom older women having higher rates o abnormal ertilization. Similarly, older paternal age has been associated with increased risk (La Vecchia, 1984; Parazzini, 1986). For example, previous spontaneous abortion at least doubles the risk o molar pregnancy (Parazzini, 1991). The requency in a subsequent conception is approximately 1 percent, and most cases mirror the same type o mole as the preceding pregnancy (Garrett, 2008; Sebire, 2003). Furthermore, ollowing two episodes o molar pregnancy, 23 percent o later conceptions result in another molar gestation (Berkowitz, 1998). These tumors require ormal staging and typically respond avorably to chemotherapy. These moles classically have swollen enlarged villi, some of which show cistern formation, that is, central cavitation within the large villi (black asterisks). Complete moles also typically show trophoblastic proliferation (yellow asterisk), which may be focal or widespread. Normal term placenta showing smaller, nonedematous villi and absence of trophoblastic proliferation. Many o these associations, however, are weak and could be explained by con ounding actors other than causality (Parazzini, 2002). Some epidemiologic characteristics di er markedly between complete and partial moles. For example, vitamin A de ciency and low dietary intake o carotene are associated only with an increased risk o complete moles (Berkowitz, 1985, 1995; Parazzini, 1988). Partial moles have been linked to higher educational levels, smoking, irregular menstrual cycles, and obstetric histories in which only male in ants are among the prior live births (Berkowitz, 1995; Parazzini, 1986). Hydatidi orm moles are categorized as either complete hydatidiform moles or partial hydatidiform moles (Table 37-2). Complete Hydatidiform Mole These molar pregnancies di er rom partial moles with regard to their karyotype, their histologic appearance, and their clinical presentation. The chromosomes, however, in these pregnancies are entirely o paternal origin, and thus, the diploid set is described as diandric. Speci cally, complete moles are ormed by androgenesis, in which the ovum is ertilized by a haploid sperm that then duplicates its own chromosomes a ter meiosis. One quarter o women will present with uterine size greater than dates, but the incidence o anemia is less than 10 percent. Moreover, hyperemesis gravidarum, preeclampsia, and symptomatic theca-lutein cysts are now rare (Soto-Wright, 1995). Last, plasma thyroxine levels are o ten increased in women with complete moles, but clinical hyperthyroidism is in requent. Partial moles may be formed if two sperm, either 23,X- or 23,Y -bearing, both fertilize a 23,X-containing haploid egg, whose genes have not been inactivated. Microscopically, complete moles display enlarged, edematous villi and abnormal trophoblastic proli eration. Macroscopically, these changes trans orm the chorionic villi into clusters o vesicles with variable dimensions. Indeed, the name hydatidiform mole literally stems rom this "bunch o grapes" appearance. In addition, hyperemesis gravidarum, preeclampsia, and theca-lutein cysts developed in approximately one quarter o women (Soto-Wright, 1995). These moles di er rom complete hydatidi orm moles clinically, genetically, and histologically. The degree and extent o trophoblastic proli eration and villous edema are decreased compared with those o complete moles. Moreover, most partial moles contain etal tissue and amnion, in addition to placental tissues. As a result, patients with partial moles typically present with signs and symptoms o an incomplete or missed abortion. The mole completely fills this uterine cavity, and calipers are placed on the outer uterine borders. Similarly, preeclampsia, theca-lutein cysts, hyperthyroidism, or other dramatic clinical eatures are rare. The coexisting etus present with a partial mole is nonviable and typically has multiple mal ormations with abnormal growth (Jauniaux, 1999). O ten, the diagnosis commonly is not made until a ter histologic review o the abortal specimen. Histopathology the histopathologic changes typical o hydatidi orm moles are listed in able 37-2.
Diclofenac 75mg otc
The negative pressure generated by such devices provides three wound care actions: (1) evacuates wound drainage to reduce bacterial Superficial Wound Dehiscence Treatment Wet to dry Dressing Changes arthritis knee exercises video buy diclofenac 50 mg without prescription. With initial wound management, all hematomas, seromas, or pus are evacuated, and necrotic tissue is debrided. Selected Interventions for Surgical Site Infection Prevention Preoperative Reduce hemoglobin A1c levels to < 7% before operation Stop smoking 30 d before operation (Table 1-4, p. Wound Care Products Product Antifungal cream Calcium alginate Description Topical cream used as treatment for superficial fungal infections of the periwound skin; contains 2% miconazole nitrate. Calcium alginate is a solid that exchanges calcium ions for sodium ions when it contacts any substance containing sodium such as wound fluid. The resulting sodium alginate is a gel that is nonadhesive, nonocclusive, and conformable to the wound bed. Topical solution that breaks down necrotic tissue by directly digesting the components of slough or by dissolving the collagen that holds necrotic tissue to the underlying wound bed. Thin, transparent polyurethane sheets coated on one side with acrylic, hypoallergenic adhesive. The adhesive will not stick to moist surfaces, and the film is impermeable to fluids and bacteria, but semipermeable to oxygen and water vapor. Polyurethane sheets containing open cells capable of holding fluids and pulling them away from the wound bed. A ter suf cient debridement o necrotic or in ected tissue under general anesthesia, ascial closure may be per ormed. However, i primary ascial closure is under signi cant tension, a synthetic mesh bridge may be required. Wet-to-dry dressing changes are per ormed until the decision is made to proceed with delayed primary closure or allow secondary intention to compete the process (Cliby, 2002). Negative pressure is created by one end of tubing placed within the sponge and the other attached to a suction-generating device. The sponge and wound are covered by an occlusive adhesive dressing, which helps to maintain the suction seal. N Engl J Med 342(20):1493, 2000 Akarsu, Karaman S, Akercan F, et al: Preemptive meloxicam or postoperative pain relie a ter abdominal hysterectomy. Clin Exp Obstet Gynecol 31:133, 2004 Al-Sunaidi M, ulandi: Adhesion-related bowel obstruction a ter hysterectomy or benign conditions. Obstet Gynecol 108:1162, 2006 Al- ook S, Platt R, ulandi: Adhesion-related small-bowel obstruction a ter gynecologic operations. Am J Obstet Gynecol 180:313, 1999 American Geriatrics Society: Postoperative delirium in older adults: best practice statement rom the American Geriatrics Society. J Am Coll Surg 220(2): 136, 2015 American Psychiatric Association: Diagnostic and Statistical Manual o Mental Disorders, Fi th Edition. Arlington, American Psychiatric Association, 2013 American T oracic Society: Guidelines or the management o adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Ann Surg 232:242, 2000 Assalia A, Schein M, Kopelman D, et al: T erapeutic e ect o oral Gastrogra n in adhesive, partial small-bowel obstruction: a prospective, randomized trial. Crit Care Med 20(1):69, 1992 Bodker B, Lose G: Postoperative urinary retention in gynecologic patients. J Vasc Surg 18:914, 1993 Canet J, Ricos M, Vidal F: Early postoperative arterial oxygen desaturation. Anesth Analg 69(2):207, 1989 colonization, (2) promotes release o cytokines that are help ul in wound healing, and (3) increases blood ow and oxygenation to tissues to uni ormly reduce wound size and improve angioneogenesis (Fabian, 2000; Morykwas, 1997; Sullivan, 2009). The two most commonly used dressings are oam and moistened nonadherent cotton gauze. A ter the initial application, the dressing is typically changed within 48 hours and then two to three times a week therea ter. A ter the dressing is covered with an adhesive lm dressing, a suction-generating evacuation tube runs through the dressing to help draw excessive exudates away rom the wound and into a canister attached at the other end. Approximately 4 days a ter wound disruption and resolution o subcutaneous in ection, a super cial vertical mattress closure with delayed-absorbable suture may be used to reapproximate tissue edges (Wechter, 2005). Depending on wound depth and patient tolerances, this can be completed in the operating room or at the bedside using a local anesthetic complemented by systemic analgesia. Overall, this strategy reduces healing time by 5 to 8 weeks and signi cantly decreases the number o postoperative visits. Fascial Dehiscence Treatment Early recognition o abdominal wall separation is critical in reducing the serious morbidity and mortality rates. Fascial dehiscence is regarded as a surgical emergency, and a gynecologist must rst determine i it is associated with evisceration o abdominal content. I abdominal contents are extruded, sterile towels soaked in saline and an outer abdominal binder can be used to cover and gently replace abdominal contents. Broadspectrum antibiotics are generally recommended to minimize ensuing peritonitis. Am Surg 66:1136, 2000 Ferrer M, Liapikou A, Valencia M, et al: Validation o the American T oracic Society-In ectious Diseases Society o America guidelines or hospitalacquired pneumonia in the intensive care unit. Clin Obstet Gynecol 57(1):43, 2014 Holzer P: Opioids and opioid receptors in the enteric nervous system: rom a problem in opioid analgesia to a possible new prokinetic therapy in humans. Chest 141:e419S, 2012 Keita H, Diou E, ubach F, et al: Predictive actors o early postoperative urinary retention in the postanesthesia care unit. Anesth Analg 101:592, 2005 Khalili G, Janghorbani M, Saryazdi H, et al: E ect o preemptive and preventive acetaminophen on postoperative pain score: a randomized, double-blind trial o patients undergoing lower extremity surgery. Surg Clin North Am 89(2):365, 2009 Kleeman S, Goldwasser S, Vassallo B, et al: Predicting postoperative voiding ef ciency a ter operation or incontinence and prolapse. Ann Surg 215:503, 1992 Lau H, Lam B: Management o postoperative urinary retention: a randomized trial o in-out versus overnight catheterization. Clin Dermatol 25(1):9, 2007 Li S, Liu Y, Peng Q, et al: Chewing gum reduces postoperative ileus ollowing abdominal surgery: a meta-analysis o 17 randomized controlled trials. Dig Dis Sci 35:121, 1990 Lundquist H, Hedenstierna G, Strandberg A, et al: C assessment o dependent lung densities in man during general anaesthesia. Clin Obstet Gynecol 45:537, 2002 Nelson R, Edwards S, se B: Prophylactic nasogastric decompression a ter abdominal surgery. Curr Surg 61:341, 2004 Ono H, aguchi, Kido Y, et al: the use ulness o bright light therapy or patients a ter oesophagectomy. Urology 13:494, 1979 Steele A, Gowrishankar M, Abrahamson S, et al: Postoperative hyponatremia despite near-isotonic saline in usion: a phenomenon o desalination. Stress-related alterations o gut motor unction: role o brain corticotropin-releasing actor receptors. Am J Physiol Gastrointest Liver Physiol 280:G173, 2001 ammela, Kontturi M, Lukkarinen O: Postoperative urinary retention: I. Scand J Urol Nephrol 20:197, 1986 aylor G, Herrick, Mah M: Wound in ections a ter hysterectomy: opportunities or practice improvement. Am J Surg 121:96, 1971 Zimmerman J, Fromm R, Meyer D, et al: Diagnostic marker cooperative study or the diagnosis o myocardial in arction. Either vertical or transverse incisions may be used, and each o ers particular advantages. Vertical incisions may be midline or paramedian, but o the two, the midline is chosen more o ten. This incision o ers quick entry, minimal blood loss, superior access to the upper abdomen, generous operating room, and the exibility or easy wound extension i greater space or access is needed. Despite advantages, midline incisions are more requently associated with greater postoperative pain, poorer cosmetic results, and increased risks o wound dehiscence or incisional hernia compared with low transverse incisions. Last, or those with prior laparotomy, the incision type is typically repeated or subsequent surgeries. Additionally, the chance o bowel or bladder injury is present with any abdominal entry, especially when extensive adhesions are encountered. Prophylaxis Laparotomy per se does not require antibiotic prophylaxis or bowel preparation. These are Surgeries for Benign Gynecologic Disorders dictated by the planned procedure. Prevention or venous thromboembolism is warranted, and options are described in Chapter 39 (p. I needed, hair in the path o the planned incision is clipped; a Foley catheter is placed; and abdominal preparation is completed. The skin is incised vertically in the midline beginning 2 to 3 cm above the symphysis pubis and extending cephalad to within 2 cm o the umbilicus.
Order diclofenac uk
Reasons or conversion during diagnostic laparoscopy include ailure to gain abdominal access arthritis diet nhs buy diclofenac amex, organ injury during entry, or extensive adhesions. Patient Preparation In general, laparoscopy is associated with lower rates o postoperative in ection and venous thromboembolism (V E) compared with laparotomy. In addition, or most patients, bowel preparation is not 1004 Atlas of Gynecologic Surgery administered. However, i extensive adhesiolysis is anticipated and the risk o bowel injury is thereby increased, bowel preparation can be considered. Alternatively, a ter measurement o the uterine cavity with a uterine sound, the balloon end o an endometrial cavity manipulator may be threaded into the endometrial cavity, and the balloon in ated. The outer pair o surgical gloves is removed, and the surgeon moves to either side o the patient. Abdominal access may be attained by any o the our basic techniques described in Chapter 41 (p. These include Veress needle insertion, direct trocar insertion, optical-access insertion, or open entry methods. A 5-mm or 10-mm umbilical port will house a suitable laparoscope or diagnostic examination. Generally, starting with a 5-mm incision and laparoscope will allow or adequate visualization o the abdominopelvic cavity. Once sa e initial entry is con rmed, the abdomen is insu ated to reach an intraabdominal pressure o 15 mm Hg or less. However, bilateral lower quadrant ports may be desired i lysis o adhesions or greater tissue manipulation is required. These are placed under direct laparoscopic visualization as described in Chapter 41 (p. All laparoscopic procedures begin with a systematic and thorough diagnostic inspection o the entire peritoneal cavity, including the pelvis and upper abdomen. Once sa e initial entry is con rmed, the area directly below the primary trocar entry site is evaluated or bleeding or other signs o entry trauma. Speci cally, the liver surace, gallbladder, alci orm ligament, stomach, omentum, and right and le t hemidiaphragms are inspected. A ter rendelenburg positioning, bowel and omentum all toward the upper abdomen to expose the retroperitoneal structures. Now ree o intestines, the area directly beneath the initial entry site is examined again. Previously unappreciated trauma to this area rom initial abdominal entry might then be seen. First, the uterus is retroexed with the aid o the uterine manipulator to provide clear viewing o the anterior cul-de-sac. T en, the manipulator tilts the uterus up and to the right to permit le t pelvic sidewall inspection. During this, endometriotic implants, peritoneal de ects or windows, adhesions, brosis, or studding concerning or malignancy are sought. Next, both ureters are visualized coursing rom the pelvic brim, along the pelvic sidewall, and to the cervix. In doing so, the tubes and ovaries are li ted rom the posterior cul-de-sac or ovarian ossa or inspection. A ter visual assessment o the pathology ound, indicated procedures are then perormed. During this process, all secondary cannulas are removed using laparoscopic visualization. This allows exclusion o bleeding rom punctured vessels that may have been tamponaded by these cannulas. Additionally, it prevents herniation o bowel or omentum up through the cannula track and into the anterior abdominal wall. Accordingly, potential bleeding sites are reinspected as the pneumoperitoneum is released. Next, the primary cannula is removed while leaving the laparoscope in the abdomen. Last, the laparoscope is slowly removed to visualize the abdomen and entry site or any evidence o bleeding and to prevent viscera rom being pulled into the port site. O these, a blunt probe and atraumatic grasper are valuable to manipulate abdominal organs. A uterine manipulator that allows or chromopertubation is also considered i per orming diagnostic laparoscopy or in ertility evaluation. Either agent is diluted into 50 to 100 mL o sterile saline or injection through the cervical cannula. Most laparoscopic surgery is per ormed in an operating room and requires general anesthesia. Much less commonly, ino ce microlaparoscopy using 2- to 3-mm microlaparoscopes has been reported or second-look evaluation o cancer treatment, sterilization, and pelvic pain and in ertility evaluation (Franchi, 2000; Mazdisnian, 2002; Mercorio, 2008; Palter, 1999). In most cases, ollowing anesthesia induction, the patient is placed in low dorsal lithotomy position in booted support stirrups to permit manipulation o the uterus. Correct patient positioning is critical to avoid nerve injury and is discussed in Chapter 41 (p. I a longer procedure is anticipated, a Foley catheter may be required as a ull bladder can obstruct the operating view or increase the risk o bladder injury. Although not mandatory, a uterine manipulator may be placed to move the uterus during evaluation o the pelvis. For closure, interrupted or running suture line using 0-gauge delayed absorbable suture is suitable. I open entry was used, then sutures originally placed in the ascia are unthreaded rom the trocar. Each o these sutures then is brought to the midline o the incision, and square knots are tied to close the ascial de ect. Skin incisions are closed with a subcuticular stitch o 4-0 gauge delayed-absorbable suture. Alternatively, the skin may be closed with cyanoacrylate tissue adhesive (Dermabond opical Skin Adhesive) or skin tape (Steri-Strips) (Chap. For most, physical activities and diet can be resumed according to patient com ort. Approximately hal o these ollow pregnancy delivery or termination, but the others are per ormed independent o pregnancy and are termed interval sterilization (Chan, 2010). Most interval procedures are per ormed laparoscopically, and most requently they involve tubal occlusion by electrosurgical coagulation, by mechanical clips, by Silastic bands, or by suture ligation (Pati, 2000). Current sterilization practices will likely change with recommendations now encouraging consideration o prophylactic salpingectomy at the time o sterilization, abdominal or pelvic surgery, or hysterectomy or women at average risk o ovarian cancer (American College o Obstetricians and Gynecologists, 2015). The rationale or this practice change to help decrease rates o certain epithelial ovarian cancers is described in Chapter 35 (p. Sterilizing clips and bands routinely all rom around the tube once occluded ends necrose and brose. Most ectopic clips are incidental ndings without untoward patient ef ects, but less commonly they can incite local oreign body reactions. Rarely, cases o clip migration to sites such as the bladder, uterine cavity, and anterior abdominal wall have been reported (Gooden, 1993; Kesby, 1997; an, 2004). Contraceptive ailure and pregnancy rates related to each procedure are also discussed with the patient (Chap. Overall, these rates are low, and tubal sterilization is an ef ective method o contraception. Bipolar coagulation has the highest risk or this complication compared with that o clips or bands (Malacova, 2014; Peterson, 1996). T ough results have varied, one metaanalysis suggests some bene t in diminishing immediate postoperative pain with these practices (Brennan, 2004; Harrison, 2014; Schytte, 2003; Wrigley, 2000). Uterine size will af ect placement o the accessory trocar, and inclination will direct positioning o the uterine manipulator, i used.
Discount 50mg diclofenac free shipping
Treatment of the Infertile Couple because o postsurgical adhesion ormation rheumatoid arthritis virus generic 50 mg diclofenac with amex, which converted endo120,000 crinologic sub ertility to mechanical sub ertility (Adashi, 1981; 100,000 Buttram, 1975; Stein, 1939). However, medical ovula0 tion induction, as discussed ear1980 1990 2000 2010 2013 lier, has limitations. Number of twin births in the United led to temporary, higher rates States from 1980 to 2006. Number of triplet and higher-order multifetal births in the United o spontaneous postoperative States for the same time period. Recommended Limits on the Numbers of than 18 millimeters in diameter were present (Guzick, 1999). The endocrine changes ollowing surgery are thought to convert the adverse androgen-dominant intra ollicular environment to an estrogenic one and to restore the hormonal environment to normal by correcting ovarian-pituitary eedback disturbances (Aakvaag, 1985; Balen, 1993). T us, both local and systemic e ects are thought to promote ollicular recruitment and maturation and subsequent ovulation. Risks o ovarian drilling include postoperative adhesion ormation and the other risks o laparoscopic surgery (Chap. Additionally, theoretical risks o diminished ovarian reserve and premature ovarian ailure remain to be well investigated. As surgery is more invasive, ovarian drilling is generally not o ered prior to consideration o medical therapies. It typically results rom prior pelvic in ection and may be associated with concomitant adnexal adhesions. Such pressure will likely overcome most instances o tubal spasm or plugging by mucus or debris. I tubal patency cannot be reestablished, an inner catheter with guide wire is used to cannulate the tube. Expectant management may also be considered, although the likelihood o pregnancy is low. Some types o tubal blockage have a much better prognosis with surgical therapy than others. For example, hysteroscopic cannulation o allopian tubes can treat some types o proximal obstruction in a ashion similar to selective salpingography (Section 44-18, p. Hysteroscopic cannulation is best per ormed with concurrent laparoscopy to veri y distal tubal patency. Proximal obstruction not amenable to cannulation techniques can be treated with segmental resection and reanastomosis. In most cases, this can be done as an outpatient procedure through a minilaparotomy incision. However, obstruction extending into the interstitial portion o the tube is more technically challenging to repair and more prone to repeated obstruction postoperatively. From a patient perspective, outpatient tubal reanastomosis avoids ovarian stimulation and increased risk or multi etal gestation and provides an ability to conceive normally. In general, although the monthly probability o pregnancy ollowing tubal reversal is likely lower than that or age-matched controls without prior sterilization, the cumulative chance o pregnancy is high. For example, in cases o sterilization completed by mbriectomy, neosalpingostomy can be corrective. The three primary types o anatomic abnormalities include tubal actors, peritoneal actors, and uterine actors. Tubal Factors ubal occlusion can arise rom congenital abnormality, in ection, or iatrogenic causes. For example, proximal tubal occlusion, distal tubal occlusion, and tubal absence di er markedly in their treatment. Proximal tubal occlusion describes obstruction proximal to the mbria and may develop at the tubal ostium, isthmus, or ampulla. Proximal tubal occlusion may be secondary to tubal Treatment of the Infertile Couple is common (Bayrak, 2006). Moreover, hydrosalpinges that are dilated more than 3 cm in diameter, that are associated with signi cant adnexal adhesions, or that display an obviously attenuated endosalpinx yield a poor prognosis. However, the end result is decreased endometrial receptivity and reduced likelihood o embryo implantation. The scarred portion of the tube is sharply excised until nonfibrotic tubal tissues are reached. Importantly, the risk o subsequent ectopic pregnancy ollowing reanastomosis or midtubal occlusion is 3 to 5 percent (Gordts, 2009). The "reversibility" o sterilization can generally be determined by review o the operative report and also the pathology report i the procedure involved segmental resection. I operative records are unavailable or suggest that reanastomosis may not be easible, laparoscopy is per ormed prior to laparotomy to assess chances o surgical success. Robotic control may be help ul or this but may increase operating time and expense. Following pelvic in ammatory disorders, normal mbrial anatomy may be destroyed, or mbria may be encased by adnexal adhesions. In these cases, neosalpingostomy can be per ormed at minilaparotomy or laparoscopy. However, women desiring neosalpingostomy or treatment o distal occlusion are counseled that the risk o ectopic pregnancy is high, the likelihood o pregnancy is 50 percent or lower, and postoperative reocclusion Leiomyomas are common benign tumors o the uterus and have been associated with in ertility in some women (Chap. Retrospective studies have suggested a bene t rom surgically removing certain tumors to increase ef cacy o both natural and assisted conception (Grif ths, 2006). There are no randomized controlled trials to clearly demonstrate that myomectomy improves ertility. However, in view o the many retrospective observational studies that suggest this, it is reasonable to o er myomectomy to well-selected in ertile women, especially i tumors are large or impinge on the endometrial cavity. Myomectomy can be per ormed using hysteroscopy, laparoscopy, or laparotomy, and selection o the approach is discussed in Chapter 9 (p. Currently, no studies validate one method compared with another in terms o ef cacy. There ore, clinical judgment should determine the most appropriate technique rom the standpoint o sa ety, restoration o normal uterine anatomy, and speed o recovery. The distal end of the clubbed fallopian tube is opened sharply or with electric or laser energy. I amenorrhea or hypomenorrhea result, the condition is termed Asherman syndrome (Chap. Dilatation and curettage (D & C) and abdominal approaches have previously been used. However, with the advantages o hysteroscopy, the role o these other techniques has been minimized. However, women whose uterine undus is completely obscured and those with a markedly narrowed, brotic cavity present the greatest therapeutic challenge. Several techniques have been described or these dif cult cases, but outcome is ar worse than in patients with small band adhesions. In those women with severe Asherman syndrome that is not amenable to reconstructive surgery, gestational carrier surrogacy is a valuable option (p. Endometrial Polyps These so t, eshy endometrial growths are commonly diagnosed during in ertility evaluation. Several studies suggest good pregnancy rates ollowing polypectomy, although the mechanism by which polyps impair ertility has not been established.