Order 10 mg maxalt with amex
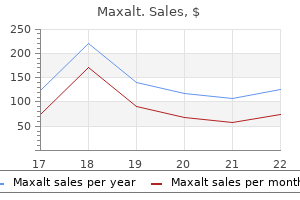
Effect of doxazosin gastrointestinal therapeutic system as third-line antihypertensive therapy on blood pressure and lipids in the Anglo-Scandinavian Cardiac Outcomes Trial shoulder pain treatment exercises purchase 10 mg maxalt fast delivery. Adrenergic blockade improved insulin resistance in patients with morning hypertension: the Japan Morning Surge-1 Study. Dihydroergotamine, ergotamine, methysergide and sumatriptan-basic science in relation to migraine treatment. The pathophysiological and pharmacological basis of current drug treatment of migraine headache. Prazosin for the treatment of nightmares related to posttraumatic stress disorder: a review of the literature. It is one of the most common diseases affecting adults living in industrialized nations. In the United States, for example, hypertension occurs in approximately 30 percent of the general population aged 20 and over. Although there is a general consensus regarding the adverse effects of hypertension, some debate exists as to exactly how much of an increase in blood pressure constitutes hypertension. Generally, diastolic values greater than 90 mm Hg and/or systolic values greater than 140 mm Hg warrant a diagnosis of hypertension. Patients are classified as prehypertensive, stage 1, or stage 2, depending on the extent of their elevated blood pressure. Hypertension is often described as a silent killer because of the lack of symptoms throughout most of the disease course. As might be expected, the incidence of morbidity and mortality increases as the hypertension becomes more severe. Hence, pharmacological and nonpharmacological methods are implemented to decrease blood pressure to an optimal diastolic value of 80 mm Hg or less and an optimal systolic value less than 120 mm Hg. When you are dealing with hypertensive patients, you are usually treating a problem other than the increased blood pressure-that is, hypertension is not the reason the patient is referred to physical therapy and occupational therapy. Due to the prevalence of hypertension, however, many patients receiving therapy for other problems will also be taking antihypertensive drugs. These drugs can also affect heart rate and vascular responses to aerobic exercise, mobility training, physical agents, and various other rehabilitation interventions. Hence, it is essential that you have knowledge of the pharmacology of these agents. The pharmacological management of hypertension has evolved to where blood pressure can be controlled for extended periods in most patients. Several major categories of antihypertensive agents are currently available, and new drugs are continually being added to the antihypertensive arsenal. Each group of antihypertensive drugs is discussed under the appropriate section in this chapter, as well as how several different drugs can be used together when treating hypertension. To help you better understand how these drugs work in decreasing blood pressure, the first section is a brief review of the normal control of blood pressure and the possible mechanisms that generate a hypertensive state. The relevance of this simple equation to antihypertensive therapy will become apparent as different drugs are discussed. The longterm management of blood pressure is accomplished primarily by the kidneys through their control of fluid balance. Although the control of blood pressure is a fairly complex subject, the actual factors that determine blood pressure can be simplified. At any given time, blood pressure is the product of cardiac output and the total resistance in the peripheral vasculature. In secondary hypertension, the elevated blood pressure can be attributed to some specific abnormality such as chronic kidney disease, renal artery stenosis, certain drugs, catecholamine-producing tumors, endocrine disorders, or cerebral damage. The treatment of secondary hypertension is rather straightforward, with efforts focusing on correcting the underlying pathology. Secondary hypertension, however, accounts for less than 10 percent of the patients diagnosed with hypertension. In essential hypertension, there is no clear, readily discernible cause of the elevated blood pressure. Consequently, the exact cause of hypertension in the majority of patients is unknown. Many theories have been proposed to explain how blood pressure increases and eventually becomes sustained in essential hypertension. The literature dealing with potential causes and mechanisms of essential hypertension is voluminous and cannot be reviewed extensively in this chapter. Possible Mechanisms in Essential Hypertension It appears there is a rather complex interaction of genetic and environmental factors that ultimately leads to adaptive changes in the cardiovascular system of patients with essential hypertension. These factors seem to be more influential in certain patients, suggesting a possible genetic predisposition to hypertension. Other risk factors such as cigarette smoking and alcohol abuse clearly play a role in potentiating the onset and maintenance of hypertension. Obesity is also an important risk factor for hypertension and various other types of cardiovascular disease. The exact way in which these factors interact probably varies from person to person, so the cause of this disease must be regarded individually rather than being based on one common etiology. Although the exact cause of hypertension is unknown, studies in humans and in animal models that mimic essential hypertension have suggested that the sympathetic nervous system may be a final common pathway in mediating and perpetuating the hypertensive state-that is, the factors described earlier may interact in such a way as to cause a general increase in sympathetic activity, which then becomes the common denominator underlying the elevated blood pressure in essential hypertension. Increased sympathetic drive may initially increase blood pressure by increasing cardiac output. In later stages, cardiac output often returns to normal levels, with the increased blood pressure being due to an increase in vascular resistance. The reasons for the shift from elevated cardiac output to elevated peripheral vascular resistance are somewhat unclear, but a sustained increase in sympathetic activity may be the initiating factor that begins a sequence of events ultimately resulting in essential hypertension. Once blood pressure becomes elevated, hypertension seems to become self-perpetuating to some extent. For example, mechanisms that control blood pressure (the baroreceptor reflex) may decrease in sensitivity, thus blunting the normal response to elevated pressure. Although the exact link between hypertension and metabolic syndrome is not clear, it is apparent that a chronic elevation in blood pressure is associated with metabolic impairments that further jeopardize the health of patients with this disease. Ultimately, certain environmental factors may turn on the sympathetic division of the autonomic nervous system in susceptible individuals. Increased sympathetic discharge then creates a vicious cycle whereby increased sympathetic effects-in conjunction with the increased blood pressure itself-help perpetuate hypertension. Various factors interact to turn on sympathetic outflow to the kidneys, heart, and peripheral vasculature, resulting in elevated blood pressure. Hypertension also causes structural and functional changes in the vasculature that help maintain the elevated pressure. Structural/functional change in heart and vasculature Increased blood pressure understood and may in fact vary from patient to patient. Hopefully future studies will elaborate on the exact role of factors causing essential hypertension, and treatment can then be focused on preventing the changes that initially increase blood pressure. These drugs are used as antihypertensive agents because of their ability to increase the renal excretion of water and sodium, thus decreasing the volume of fluid within the vascular system. This is somewhat analogous to the decrease in pressure that occurs inside a balloon when some of the air inside leaks out. Consequently, diuretics appear to have a rather direct effect on blood pressure through their ability to simply decrease the amount of fluid in the vascular system. The primary sites of action and effects of each category are summarized in Table 21-2. This section surveys the mechanism of action, rationale for use, specific agents, and adverse effects of drugs in each category. These drugs can be used alone or combined with other antihypertensives as needed to control hypertension in specific clinical situations (see "Drug Selection for Specific Patients With Hypertension"). Although they differ chemically, all diuretics exert their beneficial effects by acting directly on the kidneys to increase water and sodium excretion. The classifications include thiazide, loop, and potassium-sparing drugs (Table 21-3). These drugs act primarily on the early portion of the distal tubule of the nephron, where they inhibit sodium reabsorption. By inhibiting sodium reabsorption, more sodium is retained within the nephron, creating an osmotic force that also retains more water in the nephron.
Buy genuine maxalt on-line
Likewise pain stomach treatment discount 10 mg maxalt fast delivery, alpha blockers may be a good choice for men with advanced hypertension and benign prostatic hypertrophy because these drugs may help resolve both problems simultaneously. Chapter 20 covers the drugs that inhibit the presynaptic synthesis and storage of norepinephrine. These agents have been available for several decades, but their use has declined over the years in favor of newer antihypertensives that are often better tolerated. Hence, reserpine is the only drug in this category that is still used commonly in the United States to treat hypertension (see Table 21-4). A slow heart rate (bradycardia) and other arrhythmias are sometimes a problem with reserpine. Ganglionic Blockers Drugs that block synaptic transmission at autonomic ganglia will dramatically and effectively reduce blood pressure by decreasing systemic sympathetic activity. Because of the effect of these agents on both divisions of the autonomic nervous system, ganglionic blockers are used sparingly in treating hypertension. In the past, these drugs were used to reduce blood pressure in hypertensive emergencies. Ganglionic blockers such as trimethaphan may be used to rapidly decrease blood pressure in certain emergencies, such as acute aortic dissection or autonomic crisis in people with spinal cord injury. As might be expected, ganglionic blockers produce a multitude of side effects because of the inhibition of both sympathetic and parasympathetic responses. Fortunately, ganglionic blockers are usually not used for extended periods because the patient is placed on other antihypertensive drugs when the hypertensive crisis is resolved. Centrally Acting Agents Several antihypertensives work by inhibiting sympathetic discharge from the brainstem (see Table 21-4). Sympathetic discharge from the vasomotor center appears to be influenced by two types of neuronal receptors located in the brainstem: alpha-2 adrenergic receptors and imidazoline type I1 receptors. Stimulation of these receptors results in a decrease in sympathetic discharge to the heart and vasculature. Centrally acting sympatholytics are therefore characterized as agonists for either one or possibly both types of these receptors. Clonidine, for example, is considered to be primarily an alpha-2 agonist, although this drug also has some ability to stimulate imidazoline receptors. Of the primary drugs in this category, clonidine, guanabenz, and guanfacine act directly on the alpha-2 receptor, whereas methyldopa acts as an alpha-2 agonist after being converted in vivo to alpha-methylnorepinephrine. At therapeutic doses, these drugs are associated with some troublesome but relatively minor side effects, including dry mouth, dizziness, and sedation. Hence, agents that are more selective for imidazoline receptors may seem better tolerated because patients are more alert and have less psychomotor slowing. These drugs are not usually the first medications used in patients with hypertension but tend to be added to the drug regimen if other agents. As indicated earlier, hypertension may be perpetuated by a defect in the production of nitric oxide by the vascular endothelium. It follows that providing nitric oxide directly or administering precursors for nitric oxide production may help reduce vascular resistance and decrease arterial pressure in specific hypertensive syndromes. Adverse Effects Although vasodilators are effective in lowering blood pressure, these drugs are associated with several adverse effects. Reflex tachycardia often occurs because the baroreceptor reflex attempts to compensate for the fall in vascular resistance that these drugs produce. This side effect is analogous to the increased heart rate occurring when alpha blockers are used to decrease peripheral vascular resistance. Other common reactions include dizziness, orthostatic hypotension, weakness, nausea, fluid retention, and headache. Minoxidil also increases hair growth on the face, ears, forehead, and other hairy body surfaces. This increased hair growth is often a cause for the discontinuation of this drug in women. Some men, however, have applied minoxidil cutaneously to treat baldness, and a topical preparation of this drug (Rogaine) is marketed as a potential hair-growth stimulant. When blood pressure falls, renin is released from the kidneys into the systemic circulation. Angiotensinogen is a peptide that is produced by the liver and circulates continually in the bloodstream. When renin contacts angiotensinogen, angiotensinogen is transformed into angiotensin I. The converting enzyme is located in the vasculature of many tissues, especially the lungs. Aldosterone directly increases sodium reabsorption from the kidneys, which creates osmotic forces in the kidneys that encourage water reabsorption, thus helping maintain plasma volume. Hence, some sources consider aldosterone an integral part of renin-angiotensin function and often refer to the "renin-angiotensin-aldosterone system" to identify the more comprehensive aspects of this system. Exactly what goes wrong with the renin-angiotensin system in patients with essential hypertension is not fully understood. Some patients display increased levels of circulating renin, hence their classification as having high-renin hypertension. Nonetheless, activation of the renin-angiotensin system is extremely detrimental in people with high blood pressure. These drugs can be used alone or in conjunction with other drugs for the long-term control of high blood pressure. This reaction usually disappears when the dosage is reduced or when administration is discontinued. Patients may also experience a persistent, dry cough that is annoying but relatively harmless. Although the incidence is rare, hematological effects (neutropenia, agranulocytosis) and renal problems (glomerulonephritis, renal failure) may occur in susceptible patients; these drugs should be use cautiously in certain patients with preexisting blood or kidney diseases. Calcium channel blockers are now recognized as being beneficial in the treatment of essential hypertension. Certain calcium channel blockers, known as the dihydropyridine agents (nifedipine, amlodipine, and others; see Table 21-5), block calcium entry into vascular smooth muscle. This action will inhibit the contractile process, leading to vasodilation and decreased vascular resistance. These nonhydropyridine agents may be more useful in treating certain arrhythmias, although they can also treat high blood pressure because of their inhibitory effect on heart rate and myocardial contraction force. As mentioned earlier, several agents are also available in longer-acting (sustained-release) forms, and use of these agents may help reduce the risk of cardiovascular side effects. Because calcium channel blockers are important in treating angina, the pharmacology of these drugs is discussed in more detail in Chapter 22. Adverse Effects these drugs may cause excessive vasodilation as evidenced by swelling in the feet and ankles, and some patients may also experience orthostatic hypotension. Abnormalities in heart rate (too fast, too slow, irregular) may also occur, and reflex tachycardia-caused by excessive peripheral vasodilation-has been noted with certain drugs, such as the short-acting form of nifedipine. In patients with uncomplicated stage 1 hypertension (see Table 21-1), initial drug therapy often consists of a single "first-line" drug such as a thiazide-type diuretic, calcium channel blocker, or renin-angiotensin system inhibitor. Clearly, there are many options for the initial treatment of uncomplicated hypertension, and the choice of a specific drug or drugs is ultimately left to the discretion of the prescribing physician. Drug selection is also influenced by any comorbidities or "compelling indications" in each patient. As indicated, certain drug regimens are preferred if other factors are present that may also affect blood pressure and organ function. These recommendations still enable the prescribing physician to tailor drug therapy by selecting specific drugs from each category and adjusting dosages to provide optimal treatment. Recommendations for drug treatment will continue to be reevaluated as new drugs become available, and additional clinical trials help investigate the effects of various drug interventions. Hence, changes in lifestyle and behavior can positively influence blood pressure, and these changes should be encouraged in all hypertensive patients, even if blood pressure is reduced pharmacologically. Ideally, successful implementation of these lifestyle changes can control blood pressure to the point where drug therapy is no longer necessary in some people. These drugs produce a diverse array of side effects that can influence the rehabilitation session. Because the major action of these drugs is to lower blood pressure, physical therapists and occupational therapists should be cautious when their patients change posture suddenly or engage in other activities that may lower blood pressure.
Diseases
- Gerodermia osteodysplastica
- Anonychia
- Rett syndrome
- Bork Stender Schmidt syndrome
- Nesidioblastosis of pancreas
- Ganser syndrome
- Uncombable hair syndrome
- Chromosome 4, Trisomy 4p
- Urachal cancer
- Camptocormism
Buy generic maxalt 10 mg online
Moreover pain management during shingles maxalt 10mg without a prescription, it remains to be seen whether the added toxicity of any of these approaches is balanced by substantial survival gains. Preoperative chemotherapy Multiple randomized trials have evaluated the benefit of chemotherapy administered prior to surgery. The outcome in the metabolic non-responder group was significantly worse than in the metabolic responders, despite the more intense treatment. The potential benefit of neoadjuvant chemotherapy was not offset by a higher post-operative mortality. After a median follow-up time of six years, the surgically treated patients had significantly better local control (two-year local progression-free survival 64% versus 41%; p = 0. For example, in one study the three-year survival rate was 70% versus 35%, respectively [137, 138]. In one prospective study (the Municon trial), after two weeks of initial cisplatin-based induction therapy metabolic non-responders were treated with immediate surgery whereas metabolic responders received a full course of neoadjuvant chemotherapy before surgery [139]. Compared to metabolic non-responders, the metabolic responders had a better median event-free survival (29. In conclusion, although no significant survival advantage of surgical treatment was proven in these studies, there is a significant advantage for locoregional control in favour of surgical treatment. Patients with gastro-oesophageal junction adenocarcinoma appeared to derive the same benefit as those with non-cardia gastric cancer. However, others do not, and there are no randomized trials proving benefit as compared to surgery alone, or indeed post-operative chemotherapy [151]. For patients who are found to have advanced disease after surgery alone, the addition of post-operative, additional therapy (chemotherapy with or without radiotherapy) should be considered in an effort to improve outcome. Most individual trials in Western patients did not show benefit, while the trials in Asia with adjuvant chemotherapy (predominantly S1) in mainly gastric adenocarcinoma showed benefit. A large meta-analysis on adjuvant chemotherapy in adenocarcinoma based on individual patient data, however, showed a statistically significant and relevant benefit in favour of post-operative chemotherapy compared to surgery alone [148]. The authors concluded that, post-operative adjuvant chemotherapy based on fluorouracil Palliative treatment Palliative systemic therapy the prognosis of patients with metastatic oesophageal cancer remains very poor. The development of regimens for therapy in oesophageal cancer is impeded, in part, by two histologies (squamous cell and adenocarcinoma) as well as the relatively small number of patients fit for clinical trials in developed countries. For squamous cell cancers, regimens are typically selected that are used in squamous cell cancer of the lung or head and neck cancer, such as platinum compounds and taxanes, or regimens from trials which included both oesophageal histologies. An exhaustive search of clinical trial registries in late 2013 revealed no large trials of systemic therapies alone for oesophageal squamous cell cancers. In general, doublet therapy is preferred in first-line treatment, with second-line treatments comprising those drugs/classes not previously used. In Japan, there is a significant benefit for the oral fluoropyrimidine S1 plus cisplatin over S1 alone in terms of response survival [154]. For refractory or second-line therapies, active single agents are frequently used if not already given in first-line treatment. This drug is likely to be approved in many countries, as a non-chemotherapy approach for this patient population. Palliative local therapy Dysphagia is undoubtedly the most important symptom in patients with advanced oesophageal cancer. Palliative resection is nowadays only seldom considered, and should probably be avoided. Endoscopic interventions include dilatation, laser therapy, endoscopic mucosal resection, and placement of self-expanding metal or plastic stents. Dysphagia improved more rapidly after stent placement than after brachytherapy, but long-term relief of dysphagia was better after brachytherapy. Stent placement also had more complications than brachytherapy (33% versus 21%, p = 0. However, both groups did not significantly differ for persistent or recurrent dysphagia, or for median survival. For patients with complete oesophageal obstruction, surgical or radiologic placement of jejunostomy or gastrostomy tubes may be necessary to provide adequate hydration and nutrition. A meta-analysis of lymph node metastasis rate for patients with thoracic oesophageal cancer and its implication in delineation of clinical target volume for radiation therapy. Single-dose brachytherapy versus metal stent placement for the palliation of dysphagia from oesophageal cancer: multicentre randomised trial. Cancer of the esophagus and esophagogastric junction: data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union Against Cancer Cancer Staging Manuals. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Patterns of food and nutrient consumption in northern Iran, a high-risk area for esophageal cancer. Red and processed meat consumption and the risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Correlation of epidermal growth factor receptor overexpression with increased epidermal growth factor receptor gene copy number in esophageal squamous cell carcinomas. Role of endoscopic ultrasonography in the staging and follow-up of esophageal cancer. Quality control of endoscopic ultrasound in preoperative staging of esophageal cancer. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Fluorodeoxyglucose-positron emission tomography in adenocarcinomas of the distal esophagus and cardia. Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. Accuracy of staging in early oesophageal cancer using high resolution endoscopy and high resolution endosonography: a comparative, prospective, and blinded trial. The first successful case of resection of the thoracic portion of the oesophagus for carcinoma. Nodal metastasis and sites of recurrence after en bloc esophagectomy for adenocarcinoma. Principles of surgical treatment for carcinoma of the esophagus: analysis of lymph node involvement. Extracapsular lymph node involvement is a negative prognostic factor in T3 adenocarcinoma of the distal esophagus and gastroesophageal junction. Quality indicators of surgery for adenocarcinoma of the esophagus and gastroesophageal junction. Assessing the quality of reports of randomized clinical trials: is blinding necessary Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Single-layered cervical esophageal anastomoses: a prospective study of two suturing techniques. Eliminating the cervical esophagogastric anastomotic leak with a side-to-side stapled anastomosis. Terminalized semimechanical side-to-side suture technique for cervical esophagogastrostomy. Incidence and management of benign anastomotic stricture after cervical oesophagogastrostomy. Predictive value of early postoperative esophagoscopy for occurrence of benign stenosis after cervical esophagogastrostomy. Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Esophagectomy for carcinoma of the esophagus in the elderly: results of current surgical management. Transhiatal esophagectomy without thoracotomy for carcinoma of the thoracic esophagus.
Generic maxalt 10 mg with visa
However treatment pain ball of foot cheap maxalt 10 mg visa, specificity is only a relative term, and drugs that bind preferentially to one receptor subtype may still produce a variety of responses. The directacting cholinergic stimulants and the rationale for their use are presented first. Direct-Acting Cholinergic Stimulants Direct-acting stimulants bind directly to the cholinergic receptor to activate it, which in turn initiates a cellular response. These stimulants may be considered true cholinergic agonists, and they function in a manner similar to the acetylcholine molecule. Exogenously administered acetylcholine is not used therapeutically, however, because it is degraded rapidly and extensively by the acetylcholinesterase enzyme, which is found ubiquitously throughout the body. As mentioned previously, there are many pharmacological agents that can directly stimulate cholinergic receptors. A certain degree of drug specificity is desirable, though, when considering these agents for therapeutic purposes. For instance, drugs that have a greater specificity for the muscarinic cholinergic receptor are more beneficial. These muscarinic cholinergic stimulants will primarily affect the peripheral tissues while exerting a minimal effect on the cholinergic receptors located in the autonomic ganglia and the neuromuscular junction. For systemic administration, bethanechol (Urecholine, others) is the primary direct-acting cholinergic stimulant (see Table 19-1). Other direct-acting cholinergic stimulants such as carbachol are typically limited to topical use in ophthalmologic conditions, especially glaucoma. These antiglaucoma drugs produce too many side effects if administered systemically but are relatively specific when administered directly to the eye. Chemically, many agents are capable of potently and effectively stimulating cholinergic activity. However, only a few drugs exhibit sufficient safety and relative specificity for use in clinical situations. These clinically relevant drugs can be subdivided into two categories, depending on their mechanism of action. Indirect-acting stimulants inhibit the cholinesterase enzyme, thus allowing acetylcholine to remain in the synaptic cleft. Agents used for other problems are given systemically by oral administration or injection. Clinical applications of direct-acting cholinergic stimulants are summarized in Table 19-1. Indirect-Acting Cholinergic Stimulants Indirect-acting stimulants increase activity at cholinergic synapses by inhibiting the acetylcholinesterase enzyme. Indirect-acting stimulants inhibit the acetylcholinesterase, thus allowing more acetylcholine to remain at the synapse. Because of their effect on the acetylcholinesterase enzyme, indirect-acting stimulants are also referred to as cholinesterase inhibitors or anticholinesterase agents. The exact way in which these drugs inhibit the acetylcholinesterase enzyme varies depending on the individual agent. These drugs tend to inhibit the acetylcholinesterase found at many cholinergic synapses. Indirect-acting stimulants such as neostigmine, for example, tend to predominantly affect the skeletal neuromuscular junction and peripheral tissues containing muscarinic receptors. Still, none of the indirect-acting cholinergic stimulants affect only one type of tissue, and some adverse side effects can be caused by their relatively nonspecific activity. Indirect-acting cholinergic stimulants currently in use include neostigmine and pyridostigmine. Several other agents are also used therapeutically to treat systemic conditions such as myasthenia gravis, ophthalmologic disorders such as glaucoma, and diminished acetylcholine activity associated with degenerative brain syndromes such as Alzheimer disease (see Table 19-1). As a result, intestinal peristalsis is diminished or absent, and the urinary bladder becomes distended, leading to urinary retention. Under normal circumstances, acetylcholine released from parasympathetic postganglionic neurons would stimulate smooth-muscle contraction in these tissues. Indirectacting stimulants are also used to treat glaucoma, myasthenia gravis, and in Alzheimer disease and to reverse the effects from an overdose of other drugs, such as neuromuscular blocking agents and anticholinergics. Glaucoma Glaucoma is an increase in intraocular pressure brought on by an accumulation of aqueous humor within the eye. To treat glaucoma, direct-acting and indirectacting cholinergic drugs are usually applied topically to the eye by placing the drug directly within the conjunctival sac (see Table 19-1). This application concentrates the action of the drug, thus limiting the side effects that might occur if these agents were given systemically. These agents are not typically the first drugs used to treat glaucoma, but they can be used if other agents are not effective. It is characterized by neuronal atrophy and other pathological changes in neuron structure and function throughout the brain (neurofibrillary tangles, formation of plaques, and so forth). Included in this neuronal degeneration are cholinergic neurons that are critical in memory, cognition, and other higher cortical functions. Regrettably, these drugs do not alter the progression of Alzheimer disease, and they tend to lose effectiveness as the disease progresses into the advanced stages. In advanced stages, the patient requires respiratory support because of a virtual paralysis of the respiratory musculature. In myasthenia gravis, the number of functional cholinergic receptors located postsynaptically at the neuromuscular junction is diminished. The decreased receptivity of the muscle cell accounts for the clinical symptoms of weakness and fatigue. Myasthenia gravis appears to be caused by an autoimmune response whereby an antibody is produced that affects the neuromuscular cholinergic receptor and enzymes related to the skeletal neuromuscular junction. These indirect-acting cholinergic agonists inhibit the acetylcholinesterase enzyme at the neuromuscular junction, allowing the endogenous acetylcholine released from the presynaptic terminal to remain at the myoneural junction for a longer period of time. The endogenously released acetylcholine is able to provide adequate excitation of the skeletal muscle cell and thus allow a more sustained muscular contraction. By inhibiting acetylcholine breakdown, indirect-acting stimulants enable endogenously released acetylcholine to overcome the anticholinergic drug effects. Problems and Adverse Effects of Cholinergic Stimulants Cholinergic stimulants are frequently associated with several adverse side effects caused by the relative nonspecificity of these drugs. Even bethanechol, which is relatively specific for muscarinic receptors, may stimulate muscarinic receptors on many different tissues. The adverse effects associated with both the directand indirect-acting cholinergic stimulants mimic the effects that occur during exaggerated parasympathetic activity. This notion is logical considering that the parasympathetic autonomic division exerts its effects on peripheral tissues by releasing acetylcholine from postganglionic neurons. Increased sweating and vasodilation of facial cutaneous blood vessels (flushing) may also occur because of an effect on the respective tissues supplied by special sympathetic postganglionic neurons that release acetylcholine. The incidence of these side effects varies from patient to patient, but the onset and severity increases as higher drug doses are administered. Reversal of Neuromuscular Blockage Anesthesia providers often use drugs that block transmission at the skeletal neuromuscular junction to maintain skeletal muscle paralysis during surgical procedures requiring general anesthesia (see Chapter 11). For instance, an accelerated recovery from the paralytic effects of these neuromuscular blockers may be desired at the end of the surgical procedure. Consequently, indirect-acting cholinergic stimulants are sometimes used to inhibit the acetylcholinesterase enzyme at the neuromuscular junction, thus allowing endogenously released acetylcholine to remain active at the synaptic site and effectively overcome the neuromuscular blockade until the curare-like agents have been metabolized. This binding blocks the receptor from the effects of endogenously released acetylcholine, thus diminishing the cellular response to cholinergic stimulation. These antinicotinic drugs are sometimes used to treat extremely high blood pressure and hypertensive emergencies (see Chapter 21). As mentioned earlier, anesthesia providers may use antinicotinic drugs that block the skeletal neuromuscular junction. Atropine and similar agents antagonize the effects of acetylcholine by blocking muscarinic cholinergic receptors. Atropine is a naturally occurring substance that can be obtained from the extract of plants such as belladonna and jimsonweed. Other natural, semisynthetic, and synthetic antimuscarinic anticholinergic agents are available that are similar in structure or function to atropine. As mentioned previously, antimuscarinic anticholinergic drugs all share the same basic mechanism of action: They block the postsynaptic cholinergic muscarinic receptor. However, certain antimuscarinic agents seem to preferentially affect some tissues more than others.
10mg maxalt overnight delivery
Tumour stroma and local immune and inflammatory response Given the increasing recognition of the tumour microenvironment in determining immune cell and inflammatory responses (see above) there is increasing interest in the role of the stroma in determining tumour growth and spread knee joint pain treatment order generic maxalt on-line. De Wever and Mareel [27] proposed that changes in the stroma drive the key hallmarks of cancer, invasion and metastases. In particular, the appearance of myofibroblasts, cells sharing characteristics of smooth muscle cells and fibroblasts, was associated with increased cancer cell invasion. It may be that tumour necrosis, as a result of a tumour outgrowing its blood supply, becoming relatively hypoxic and inducing the up-regulation of cellular stress genes in the tumour and the inflammatory cell infiltrate, is important in the induction of immune and inflammatory responses. Indeed, it has been postulated that the combination of inflammation and necrosis provides an environment in which the epigenetic regulation of genes, cell death, cell proliferation, and mutagenesis occurs [3]. At sites of chronic inflammation, cells are continuously dying as a consequence of hypoxic stress, an event in turn promoting growth and proliferation of the local epithelium. These inflammatory pathways are now recognized to be important for angiogenesis, stromagenesis, and the promotion of epithelial proliferation, all of which are required for tumour growth. In summary, most innate and adaptive immune cell types have been reported to play a role in tumour immune responses. Taken together the evidence suggests that a strong coordinated cytotoxic T-cell (adaptive) response is associated with improved cancer survival. Therefore, a pronounced tumour inflammatory cell infiltrate appears to primarily reflect a down-regulation and up-regulation of the innate and adaptive immune systems, respectively, in the tumour microenvironment. In order that the above information is consolidated into the routine assessment of patients with cancer, standardized measurements of the tumour inflammatory cell infiltrate are required. A higher density of tumour T-regulatory-lymphocyte infiltrate has been associated with poorer survival in a variety of common solid tumours. Again, these reports may simply reflect that many inflammatory cell types increase together, and the independence of such an association with improved outcome requires further investigation. A recently described subset of helper T lymphocytes is the Th17 group which is also capable of exerting pro- and anti-tumour activity based on surrounding mediators and site [35]. Pro-tumour effects may include stimulation of angiogenesis and recruitment of myeloid cells. The concept of suppressor cells that undermine cytotoxic T-lymphocyte responses was developed in the 1980s by Schreiber and co-workers. Clearly, if such work is to have clinical relevance there is a need to have routine assessment tools that can be simply reported and understood. However, the routine assessment of the tumour inflammatory cell infiltrates and their use to predict outcome in patients with cancer is in its infancy and such tools are in rapid development. A relatively simple but subjective assessment of the tumour cell infiltrate was introduced as part of the Jass classification in the mid-1980s [38]. However, the reproducibility of the assessment was repeatedly questioned and the assessment was not incorporated into routine practice. In addition, over the last decade, many adaptive immune cell markers have been studied using immunohistochemistry. Consistent with this is that there are significant associations between these systemic inflammatory response markers [44]. There is also robust evidence of their prognostic value in other gastrointestinal cancers and lung cancer. It is becoming clear what the optimal thresholds for these systemic inflammatory response markers are and the optimal combination of these markers for the prediction of survival [45]. Due to the simplicity and reliability of these markers, this is an area currently subject to intensive investigation and consolidation. Systemic innate immune and inflammatory response the circulating innate immune cells, according to number, include neutrophils, monocytes/macrophages, mast cells, dendritic cells, basophils and eosinophils, and natural killer cells. Increased numbers of these circulating cells are associated with a non-specific response to infection or cell injury. Accounting for the majority of circulating white cells, elevated numbers of circulating neutrophils are associated with increasing tumour stage and poorer survival in a variety of common solid tumours including colorectal cancer. Furthermore, the role of neutrophils in effectively stratifying patient response to treatment is becoming clearer [46]. Further, in similar patients receiving palliative chemotherapy, a neutrophil/ lymphocyte ratio >5 was independently associated with poorer survival [43]. Therefore, an elevated pretreatment neutrophil count appears to be a strong independent predictor of poor outcome in patients with cancer [46, 45]. Moreover, it would appear that neutrophils, similar to other inflammatory cells, are capable of polarization of N1 and N2 phenotypes, a matter that is currently the subject of investigation [46]. In addition, although they are less numerous, elevated numbers of circulating monocytes have been reported to be associated with increasing tumour stage and poorer survival in colorectal cancer [44]. Unlike tumour cell infiltration, little work has been carried out to examine the relationship between the phenotype of such circulating monocytes and cancer outcome. However, it is clear from work in other disease states that monocytes leave the bloodstream and migrate into tissues where, following conditioning by the local inflammatory milieu, they differentiate into macrophage or dendritic cell populations. Although passage of monocytes is essential for effective control of infections, such monocytes also contribute to the pathogenesis of inflammatory disease states [47] and possibly cancer. Few studies have examined the associations between circulating mast cells, dendritic cells, basophils and eosinophils, and natural killer cells and survival. The acute phase proteins, including the prototypical C-reactive protein, rise during a period of infection, tissue injury, or necrosis. In response to such stimulus, circulating C-reactive protein concentrations may rise up to 50,000-fold. As its half-life is constantly circulating, concentrations of C-reactive protein are mainly determined by the rate of production in the liver. C-reactive protein is considered to be part of the innate immune response since it is thought to assist in complement binding to foreign and damaged cells and enhances phagocytosis by macrophages (opsonin-mediated phagocytosis). Indeed, there is evidence that neutrophils and macrophages have Fc receptors that can be activated by C-reactive protein. It is also of interest that circulating C-reactive protein concentrations were directly associated with tumour size and necrosis [50]. Therefore, it may be that C-reactive protein plays both an indirect and a direct role in tumour progression that ultimately leads to its strong association with poorer cancer-specific survival in patients with cancer. Systemic humoral immune and inflammatory response It is of interest that circulating concentrations of a number of the molecules that are associated with the activation of the components of the humoral immune and inflammatory response in patients with cancer have been reported to have prognostic value independent of tumour-based factors. Given that the function of the humoral immune and inflammatory mediators is to connect local and systemic response, these are ideally suited to sense tumour immune surveillance. It is therefore surprising that these molecules have not been subject to more investigation and exploited as prognostic and therapeutic markers. Again, there is a considerable and pressing need to extend and consolidate such findings into routine investigation of patients with cancer. Mediators linking local and systemic immune and inflammatory responses There are a number of plausible mediators linking local and systemic inflammatory responses. For example, Kantola and colleagues [58] have reported the pattern of alterations of 13 serum cytokine concentrations between >80 normal controls and patients newly diagnosed with colorectal cancer. Sex, tumour site, and N stage had little association with the serum cytokine alterations reported. These findings are consistent with the hypothesis that tumour necrosis (which increases with T stage) plays an important in both linking local and systemic inflammatory responses in patients with colorectal cancer [50]. It has long been recognized that tumour-associated macrophages localize to hypoxic regions of the tumour microenvironment. Alternatively, recent work has suggested that an accumulation of myeloid-derived suppressor cells in the tumour microenvironment may be important in these observations. Therapeutic intervention in immune and inflammatory responses There is great interest in potential strategies to manipulate immune and inflammatory responses in cancer for therapeutic gain. Generally speaking, this will involve restoration of a targeted anti-tumour-cell mediated immune response. Potential strategies that may improve oncological outcome include targeting both local and systemic innate and adaptive immune responses: for example, at a local level, repolarization of tumour-associated neutrophils and macrophages towards N1 and M1 phenotypes, respectively, and inhibition of myeloid-derived suppressor cell activity, as well as repolarization towards Th1 anti-tumour cytotoxic T-cell responses and suppressing T-regulatory cell activity.
Syndromes
- Bend forward, backward, and sideways
- Weak, ineffective coughing
- Have diabetes, premenstrual syndrome, an underactive thyroid, or rheumatoid arthritis.
- Checking the temperature of bath water to prevent burns
- Liver scarring and poor liver function (cirrhosis)
- BUN and creatinine blood test
- This episode of back pain has lasted longer than 4 weeks
- New or recurrent bedwetting
- Paroxysmal cold hemoglobinuria
- Get plenty of exercise. Women who need to lose or keep off weight should get at least 60 - 90 minutes of moderate-intensity exercise on most days. To maintain your health, get at least 30 minutes of exercise a day, preferably at least 5 days a week.
Cheap 10 mg maxalt mastercard
Transcription-coupled nucleotide excision repair in mammalian cells: molecular mechanisms and biological effects innovative pain treatment surgery center of temecula purchase 10mg maxalt otc. A multistep damage recognition mechanism for global genomic nucleotide excision repair. Xeroderma pigmentosum: a glimpse into nucleotide excision repair, genetic instability, and cancer. Breast cancer susceptibility: current knowledge and implications for genetic counselling. Chromatid cohesion defects may underlie chromosome instability in human colorectal cancers. Systematic genome instability screens in yeast and their potential relevance to cancer. The human Ha-ras oncogene induces genomic instability in murine fibroblasts within one cell cycle. Molecular signaling mechanisms of apoptosis in hereditary non-polyposis colorectal cancer. In tumour cells this number may vary by a factor of two with substantial impact on the cellular radiosensitivity. Differences in the repair kinetics, especially in the final plateau, indicate defects either in damage response, chromatin organization, repair pathways, or repair regulation. Adapted from Springer Verlag, the Impact of Tumor Biology on Cancer Treatment and Multidisciplinary Strategies, 2009, pp. However, in many tumours this hierarchy is disturbed so that these two pathways are more active. The mechanisms leading to this cetuximab-mediated improved tumour control are not yet fully understood. However, an even stronger effect was seen for erlotinib, for which no cellular radiosensitization was seen. Probably, targeting of these two signalling pathways is more effective, because it cannot be compensated by other signalling cascades. Radiotherapy is combined with chemotherapy in an adjuvant or neo-adjuvant regimen but also may be given simultaneously. However, for most of the conventional drugs used there is rarely a synergistic effect observed but mostly only an additive effect, even for the often applied combination of radiation and cisplatin. When combined with external irradiation, tumour control is already achieved with fairly low doses. It should, however, be noted that a difference in repair capacity of 1% has already been shown to have a strong effect on cell survival [19]. This technique may also be applied for tumour tissue slides irradiated both in situ or ex-vivo [18, 20]. However, there are still numerous problems to be solved such as hypoxic regions as well as contamination by normal tissue before this technique can be used in a daily clinical routine. Substantial variations in the amount of repair proteins have been reported in tumours both intra- and inter-individually. It should, however, be considered that this technique only allows determination of the relative amount of the protein present. There are several studies showing an excellent correlation between a specific gene expression profile and tumour radiosensitivity [24, 25]. Chk1 und Chk2 In most tumours, the G1/S checkpoint is not active because p53 is mutated. There are several inhibitors available targeting either or both of these kinases which are already used in the clinics. Huge differences in cellular radiosensitivity due to only very small variations in double-strand break repair capacity. Epidermal growth factor receptor and response of head-and-neck carcinoma to therapy. Gene expression profiling to predict outcome after chemoradiation in head and neck cancer. At the top of the cellular organization, normal adult stem cells maintain tissues during homoeostasis and facilitate their regeneration, for example in response to infection or to cell loss due to injury or chemotherapy. Indeed, as early as 1937, Furth and Kahn could demonstrate that one single mouse leukaemic cell is able to seed and form a new tumour in a healthy recipient mouse. The clonality of human cancers assessed by genetic markers was also demonstrated later on, confirming that cancers can arise from one transformed initiating cellular clone [8]. A clonal evolution model or multistep carcinogenesis model has subsequently been proposed to explain cancer development [9]. This model proposes that cells acquire tumorigenicity by accumulating mutations or genetic alterations, which occur stochastically in all neoplastic cells. This ultimately leads to the development of tumours, from benign to highly aggressive, depending on the type and number of newly acquired genetic alterations. However, accumulating evidence indicates that neoplastic cells do not always acquire tumorigenicity stochastically. Instead, tumours are often hierarchically organized, as are adult tissues [2, 10]. The differentiated progeny was no longer able to form tumours in secondary recipients, contrary to non-differentiated cells. Although considered state of the art, this assay has limitations and only imperfectly recapitulates the in vivo situation found in patients. Indeed, the immunocompromised mouse models lack an adaptive immune system (neither mouse nor human) and express cytokines/chemokines and other environmental components of mouse origin, such as the tumour vasculature. In the first five columns, the main parameters influencing the efficiency of tumour engraftment are listed. From left to right: the tumour entity, the type of immunocompromised mouse strain used, the route of transplantation of human tumour cells, preconditioning of the recipient mice, treatment of mice during the assay, and whether the tumour cells were mixed with matrigel upon transplantation. For example, clonal analysis of human colon cancer xenografts revealed long-term transient as well as dormant clones. The latter ones only appeared in secondary and tertiary transplants suggesting that there is a significant fluctuation during the progression of tumour growth over time. Interestingly, slow-cycling dormant clones showed the highest resistance to chemotherapy showing that the clones that drive initial tumour growth might be distinct from the ones that reinitiate growth and relapse after therapy. Importantly, these data demonstrate that tumour heterogeneity is not exclusively the consequence of genetic heterogeneity, but also caused by epigenetically distinct tumour cells following the cancer stem cell model [15, 41]. Reproduced with permission from the Journal of Cell Biology, the evolving concept of cancer and metastasis stem cells, Volume 198, Issue 3, pp. Importantly, in vitro studies of drug-sensitive tumour cell lines suggest that cancer cells might transiently and reversibly acquire drug resistance, indicating that drug resistance might not always be a stable trait [60]. Extracellular matrix proteins such as periostin and Tenascin-C are critical for the outgrowth of breast cancer metastatic cells in the lung, possibly by coordinating the interaction with neighbouring cells and by enhancing signalling mediated by growth-promoting signalling factors [63]. In leukaemia and in prostate carcinoma cancer, cells could hijack existing physiological stem cell niches. For instance, embryonic stem cells can form teratomas when transplanted subcutaneously in recipient mice. For instance, progenitors derived from stem cells that already carry initiating genetic mutations acquire further mutations during differentiation that will finally lead to transformation. For instance, during the last few years, various genome-wide gene expression profiling efforts combined with biomarker and clinical approaches have led to the sub-classification of breast cancers into increasing numbers of molecular subtypes [80, 81]. Thus, these cells do not de-differentiate, but rather acquire self-renewal potential after loss of tumour suppressors [75]. First, differences in methods could be responsible for these differences [34, 38]. As a consequence, tumours might not be faithfully represented by single-headed hierarchical structures bur rather might resemble more oligarchic structures, displaying multiple heads: if one head, i. However, the toxicity of this molecule on physiological stem cells remains unexplored.
Order maxalt 10 mg amex
American society of clinical oncology statement: toward individualized care for patients with advanced cancer pain treatment center of america discount maxalt 10 mg with mastercard. Therapeutic misconception, misestimation, and optimism in participants enrolled in phase 1 trials. Ethical, scientific, and regulatory perspectives regarding the use of placebos in cancer clinical trials. Randomized discontinuation design: application to cytostatic antineoplastic agents. Recruiting terminally ill patients into non-therapeutic oncology studies: views of health professionals. Physician recruitment of patients to non-therapeutic oncology clinical trials: ethics revisited. Toward improved understanding of the ethical and clinical issues surrounding mandatory research biopsies. Use of research biopsies in clinical trials: are risks and benefits adequately discussed Impact of oncology drug shortages on patient therapy: unplanned treatment changes. Unpredictable drug shortages: an ethical framework for short-term rationing in hospitals. Coping with critical drug shortages: an ethical approach for allocating scarce resources in hospitals. Limits to health care: fair procedures, democratic deliberation, and the legitimacy problem for insurers. How much is life worth: cetuximab, non-small cell lung cancer, and the $440 billion question. American Society of Clinical Oncology guidance statement: the cost of cancer care. Delivery of cancer therapy requires both an effective intervention and the ability to provide access to the intervention for patients in need. Much of the research of recent decades has been devoted, appropriately, to developing effective interventions in a variety of cancer settings. However, it is now clear that providing access to these interventions to patients in need is a global challenge requiring providers and policy makers to address the costs of cancer care both in the clinic for individual patients and at the level of the healthcare system. At the level of national healthcare systems, the costs of healthcare in general, and the costs of cancer care in particular, are high. High costs are threatening to undermine or actively undermining the sustainability of national budgets. In the United States in 2011 it was estimated that total healthcare expenditures reached $2. Though there are considerable differences in the ways healthcare is financed and administered in different nations, there is a common need to deliver high-quality care at sustainable costs. At the level of the individual patient, there is again considerable variation in the cost of care on the basis of their disease and setting. Both the total cost of care for a given patient and the percentage of that cost, if any, that will be paid out of pocket directly by the patient varies by national system and insurance coverage. This chapter will review recent estimates of the aggregate costs of cancer care, discuss methods for determining cost-effectiveness or value in cancer care, provide a framework for understanding the components of cost at the societal and individual levels, and discuss efforts to control cost while preserving or improving quality and outcomes. This represents less than 5% of total healthcare spending and is generally consistent with the percentage of total spending attributable to cancer estimated for other developed countries [6]. Total spending is a very crude way to estimate where and why money is being spent in cancer care. Many streams of spending contribute to total costs, including hospital fees, physician services, ancillary services (nursing, physical therapy), drug costs, surgical costs, radiation therapy, and durable medical goods. In addition to considering costs of cancer care by service or intervention, we can attempt to break down costs by individual cancer. Thus, we appear to be spending the most money on the most prevalent cancers, as would be expected. Obtaining data at this level of granularity is difficult, particularly in a healthcare system with multiple payers and limited public availability of data. However, this level of detail is needed to identify areas that may be experiencing higher than expected inflation, or where spending is not consistent with disease prevalence or clinical benefit. Effort to understand and control total spending without this level of detail should proceed with a large dose of caution. While oncology is only a small part of total healthcare spending by some estimates, there is concern that through a combination of higher incidence of disease, increased care delivery per patient, and rising costs for prescription drugs and other aspects of care that inflation in this area will contribute a disproportionate amount to increased healthcare spending and must be addressed now. Identifying the factors and specific elements of spending that are responsible for the aggregate increases in cost can be challenging from available data. Using available data from the public system, Medicare, which covers care for older and disabled patients, Warren et al. During this period, the percentage of patients with breast cancer receiving chemotherapy increased from 11% to 24% and the cost of chemotherapy increased from roughly $6,000 per patient to almost $13,000 [9]. Radiology may be a disproportionate driver of costs due both to innovation and relatively high margins on services. Rising aggregate costs of cancer care derive both from the cost of treating individual patients and from the number of patients who require treatment. Demographic, environmental, and behavioural factors that modify the risk of cancer in a population can have a large impact on societal costs of care. While cancer can strike at any age, it is predominantly a disease of older patients. Projected growth of the percentage of patients aged 50 years and older, and particularly an increase in the percentage of elderly patients in the population, are expected to translate into a dramatic increase in the number of patients with cancer unless there are countervailing advances in cancer prevention. Cancer is also rapidly becoming more common in developing countries as populations are living longer due to improvements in nutrition, successful treatment of infectious disease, reductions in infant mortality, and improvements in paediatric care [11]. In 1990, there were close to six million deaths from cancer estimated worldwide, but by 2010 roughly eight million cancer deaths occurred, a 38% increase [12]. In China, dominant factors include chronic infection, including hepatitis B leading to liver cancer, and tobacco use [14]. In France, it is estimated that roughly 24% of cancer deaths are attributable to tobacco use, and obesity may contribute to 3% of cancer deaths [15]. From a policy perspective, prevention through modification of risk factors across a population may be one of the most effective means to control total societal costs without adverse impact on the quality of care for individuals diagnosed with cancer. It should be noted that the societal costs of cancer care delivery are only a portion of the total economic consequences of cancer for society. The societal economic burden of cancer includes costs for care delivery, but also indirect costs caused by loss of economic productivity of individuals suffering the morbidity and mortality caused by cancer, as well as their family members who become caregivers. In Germany, for example, it was estimated that the direct cost of cancer care in 2004 was 12. The indirect cost, virtually all related to lost production due to cancer deaths, was estimated at 14. Thus, in considering the costs of cancer care to society, we must consider not only the spending on care delivery but also the downstream impact of that spending. If spending on radiology leads to earlier diagnosis and improved treatment and outcomes, spending on a genomic predictor of recurrence leads to a decision to forgo systemic therapy, or spending on an expensive targeted adjuvant therapy improves cure rates, spending on some aspects of care may rise, but the overall economic impact may be favourable. Impact of costs on individual patients In addition to the impact of cancer care costs on societal budgets, the impact on individual patients can be considerable. In all settings, costs can impact the individual due to decisions made at the national level regarding coverage and access. Assigning value implies that we can define the overall worth of an intervention and make choices between options that take into account the totality of benefits, harms, and costs, and to some degree, alternatives. However, there are well-validated methods of assessing relative clinical benefit and cost that move us in the direction of defining value. All methods to evaluate clinical benefit relative to cost have at their core a goal of allowing us to assess value and make decisions about whether a given component of care should or should not be provided. Assigning value is not equivalent, per se, to rationing, which can be defined as a programme of distribution for scarce goods and services according to a rational prespecified framework. However, assigning value can be fairly seen as a necessary step in guiding medical decision that considers financial costs and that predictably will result in some level of constraints on care on the basis of factors other than clinical benefit alone.
Buy generic maxalt on-line
The exact cause of type 1 diabetes is unknown kidney pain treatment natural best maxalt 10 mg, but there is considerable evidence that the beta cell destruction characteristic of this disease may be caused in many patients by an autoimmune reaction. Whereas insulin cannot be produced in type 1 diabetes, the problem in type 2 diabetes is somewhat more complex. The resistance may be caused by a primary (intrinsic) defect at the target cell that results in a decreased response of the cell to insulin. The decreased insulin response most likely occurs because of changes in the way the cell responds after insulin binds to the surface receptor. Problems in postreceptor signaling-such as altered protein phosphorylation, impaired production of chemical mediators, and a lack of glucose transporters-have been suggested as intracellular events that could help explain insulin resistance. Hence, insulin resistance appears to be a complex phenomenon caused by changes in the cellular response to insulin at the tissue level. However, the exact defects in insulin receptor signaling and postreceptor function remain to be determined. As indicated above, a defect in pancreatic beta cell function may also contribute to the manifestations of type 2 diabetes. Moreover, repeated hyperglycemia seems to cause additional damage to beta cells, resulting in a further decrease in beta cell function and response to glucose. Patients with conditions such as hypertension, obesity, and certain hyperlipidemias are also found to have decreased tissue sensitivity to circulating insulin. This results from a relative lack of insulin-mediated glucose uptake and use by peripheral tissues. Hyperglycemia initiates several complex and potentially serious acute metabolic changes. For example, it is usually accompanied by increased glucose excretion by the kidneys (glycosuria). Glycosuria is caused by an inability of the kidneys to adequately reabsorb the excess amount of glucose reaching the nephron. Increased glucose excretion creates an osmotic force that promotes fluid and electrolyte excretion, thus leading to dehydration and electrolyte imbalance. Increased use of fats and protein leads to the formation of acidic ketone bodies in the bloodstream. Perhaps the most devastating complications associated with this disease result from the development of abnormalities in small blood vessels. Maintenance of blood glucose at or close to normal levels-referred to as tight glycemic control-will prevent acute metabolic derangements and greatly reduce the risk of the chronic neurovascular complications associated with this disease. Insulin may also be administered in some cases of type 2 diabetes to complement other drugs (oral antidiabetic agents) and to supplement endogenous insulin release. Insulin Preparations There are many different forms of insulin, depending on the chemical structure and the length of pharmacological effects of each compound (Table 32-2). These sources were obtained by extracting the hormone from the pancreas of the host animal. The animal forms of insulin were effective in controlling glucose metabolism in humans, even though pork insulin has one amino acid that is different from the human insulin sequence, and beef insulin differs from human insulin by 3 amino acids. Certain contemporary forms of insulin are identical to the structure and effects of human insulin. By altering the amino acid sequence slightly, researchers discovered that certain biosynthetic insulins could be absorbed more rapidly than regular human insulin. These intermediate- or long-acting forms provide a sustained background (basal) level of insulin effects throughout the day or night. In addition, pharmacologists have produced biosynthetic longacting insulin glargine and insulin detemir by adding and substituting specific amino acids (glargine) or attaching fatty acids (detemir) to the regular insulin molecule. For instance, a long-acting preparation can provide basal insulin effects, and a rapid-acting agent used around mealtime can provide optimal glycemic control. Finally, several commercial preparations are now available that combine two forms of insulin in the same product. Products that combine two different forms of insulin can help provide optimal control of blood glucose levels while minimizing the number of injections needed to achieve this control. Administration of Insulin Insulin, a large polypeptide, is not suitable for oral administration. Typically, a small syringe or a needle-tipped "pen" that contains a cartridge of a specific type of insulin can be set to inject a given amount of insulin. Patients on long-term insulin therapy are usually trained to administer their own medication. In order to safely use insulin, it is important to provide adequate storage of the preparation, to maintain sterile syringes, to accurately measure the dose and fill the syringe, and to use a proper injection technique. The optimal dosage of insulin varies greatly from patient to patient, as well as within each patient. Factors such as exercise and dietary modification can change the insulin requirements for each individual. However, many patients can make their own insulin adjustments based on periodic blood glucose measurement. Home glucose-monitoring devices permit patients to routinely check their own blood glucose levels. This process of glucose self-monitoring and insulin dosage adjustment permits optimal management of blood glucose levels on a day-to-day basis. Insulin pumps were also developed as a more convenient and precise way to administer insulin. These pumps can deliver a continuous (background) infusion of insulin that can also be supplemented at mealtime by manually activating the pump. These pumps can be worn outside the body, with insulin administered subcutaneously through a small catheter and needle that is held in place by skin tape. These pumps may also provide better control over blood glucose levels while reducing the risk of side effects such as severe hypoglycemia. Currently, the major drawback of insulin pumps is that they can malfunction, primarily because the catheter delivering insulin becomes occluded or obstructed. Nonetheless, insulin pumps currently offer a convenient way to administer insulin, and technological improvements in these devices will continue to improve their safety and reliability. During insulin treatment, insulin is not released exclusively after a meal, as it would be during normal function. Insulin administered from an exogenous source may be present in the bloodstream even if the patient fails to provide glucose by eating. Hence, insulin may reduce blood glucose below normal levels because of the lack of a periodic replenishment of blood glucose from dietary sources. Exercise generally produces an insulinlike effect, meaning that it accelerates the movement of glucose out of the bloodstream and into the peripheral tissues (skeletal muscle) where it is needed. The combined effects of exercise and insulin may produce an exaggerated decrease in blood glucose, thus leading to hypoglycemia. To avoid exercise-induced hypoglycemia, the insulin dose should be decreased proportionally depending on the type, intensity, and duration of the activity. Initial symptoms of hypoglycemia include headache, fatigue, hunger, tachycardia, sweating, anxiety, and confusion. Symptoms progressively worsen as blood glucose continues to decrease, and severe hypoglycemia may lead to loss of consciousness, convulsions, and death. Typically, administration of the equivalent of 15 to 20 g of D-glucose is recommended to restore blood glucose in the early stages of hypoglycemia. To achieve this goal, an administration strategy known as intensive insulin therapy has been developed for persons who require exogenous insulin. Patients, of course, must be motivated and committed to achieve adequate intensive insulin therapy. Although allergic reactions were more common from the animal forms of insulin, they can still occur with the biosynthetic insulins. Hence, this immunological response may be due to either the insulin molecule or to preservatives added to the insulin preparation. These drugs act directly on pancreatic beta cells and stimulate the release of insulin,121,122 which is released directly into the hepatic portal vein and subsequently travels to the liver, inhibiting hepatic glucose production. These drugs seem to be most effective in people who are in the early stages of the disease and still have reasonable beta cell function.
Buy cheap maxalt 10mg on-line
The relationship between total dose pain treatment herniated disc maxalt 10mg on line, fraction size, and late toxicity is, however, complex (Table 38. Almost 60% of the patients suffered faecal incontinence, impairing their social life [112]. The lateral nodes along aa rectales inferiores and aa obturatorii and the internal iliac nodes up to the bifurcation from aa iliac communes should be included in tumours below the peritoneal reflection, i. The risk of lateral node involvement in the Western world is not properly known, but studies from Asia show that these lymph nodes are rarely involved in low-mid-rectal pT1-2 tumours and in high tumours irrespective of T stage [105]. External iliac nodes should only be included if an anterior organ like the urinary bladder, prostate, or female sexual organs is involved. The medial inguinal nodes need only to be prophylactically irradiated when the tumour grows below the dentate line [106]. Fossae ischiorectales should only be included when the levator muscles and the internal and external sphincters are involved, since the fascia inside the levators is a strong barrier to tumour cell penetration [107]. The large adjuvant trials have included comparatively few patients with rectal cancer or have focused on colon cancer alone. The trials evaluating the value of oxaliplatin have so far only included colon cancer patients. From the randomized trials, we have good evidence of morbidity after 5 x 5 Gy [76]. Increased risks of poor anal and sexual function, small bowel toxicity with obstruction, and secondary malignancies have been reported. However, in patients given adjuvant chemotherapy, the local recurrence rate was reduced from 17% to 9% (P = 0. However, a beneficial effect from adjuvant chemotherapy on local recurrences is also supported by pooled analyses of several trials [134, 135], but pooling of data from different trials may easily introduce bias. For such therapy given post-operatively, most data show that adjuvant chemotherapy provides no major benefit [136, 137]. The low level of scientific evidence for benefit from adjuvant chemotherapy in rectal cancer is acknowledged in authoritative treatment guidelines and by expert groups that still often conclude that such treatment should be considered based on the principles used for colon cancer [63, 116]. Based on this report, it is possible to conclude that adjuvant treatment for rectal cancer could be given as it is for colon cancer. Based upon the report of a few randomized studies in 2014 and 2015, two additional meta-analyses, one of which was based on individual patient data, have been published in 2015 [119, 120]. Adjuvant chemotherapy following surgery alone this treatment setting, in most cases not relevant today in the Western world, except for the early stages, has mostly been studied in Japan. The groups were too small to show statistically significant differences but all showed point estimates indicating benefit from adjuvant chemotherapy. One possibility is a lower sensitivity of rectal cancer compared with colon cancer in the adjuvant setting based on differences in tumour biology. In colon cancer the efficacy of adjuvant chemotherapy is attenuated by time of start after surgery [138]. Starting with the systemic rather than the locoregional treatment in rectal cancer could approach the relevance of the timing effect. Follow-up the rationale for follow-up of patients after rectal cancer surgery is to find metachronous tumours for quality control and audit. Metachronous metastases and new primary colorectal tumours the most common places for a recurrence are the liver or the lungs. Therefore follow-up programmes include scanning of these organs, potentially allowing radical metastasectomy if recurrence occurs. Post-operatively the patient should be investigated with the same type of scan so that it is possible to compare the findings. In many centres worldwide patients are seen every sixth month or sometimes even more often during the first years, but the literature is very scarce and there is no data to support intense follow-up. The impression is also that these patients mostly do well during those extra months. This impression has been substantiated in trials where quality of life (QoL) estimations have been performed. A number of small steps have been taken, together resulting in median survival of patients included in trials being prolonged from about six to eight months to about 24 months or even slightly longer if molecular selection is done (Table 38. The discrepancy between survival of about one year in the entire population and above two years in the most recent trials clearly indicates that patients included in trials are selected [149]. It is important to focus on reasons for this selection and develop treatments that not only benefit the fittest patients. Based upon a Danish trial, where 600 patients were randomized to colonoscopy every year or every fifth year it is sufficient to investigate most patients every fifth year [145]. Quality control Since rectal cancer surgery is a major procedure with many complications, it behooves patients to be seen post-operatively. In many countries nurse practitioners perform this in cooperation with the surgeon [146]. The patient has to be checked by the operating surgeon some weeks after discharge to disclose problems which can hopefully then be corrected. Based upon that follow-up visit it might be necessary to see the patient several times, if post-operative complications persist. Once the post-operative period is over a follow-up programme for metachronous metastases should be followed, as outlined previously. Most gains with high statistical significance have been shown in individual trials or in meta-analyses of the trials [150, 151]. More toxicity and higher economic costs have accompanied each improvement in treatment results. The cost increase is particularly true for the development that has taken place in the past decade. It is important that all departments handling rectal cancer patients are aware of their results concerning both early and late complications and oncology outcome, and can break down the data on the individual surgeons. Treatment of metastatic disease In colon and rectum cancer, about 20% of the patients in Western populations have synchronous metastases, and another 20% will later develop metastases. The most common site is the liver, but lung metastases are also frequent, particularly if the primary is in the rectum. If the disease is metastatic, the primary tumour site is less important since it has not been possible to detect any clinically relevant differences in tumour behaviour or response to medical therapy. The primary tumour site is of relevance in synchronous disease if surgery of the primary, for cure or for palliation, is planned. Although one may question whether the gains achieved have been sufficient in proportion to the efforts, the gains have markedly influenced clinical routines. Median survival in most recent Patient selection and better treatments are most important for this prolongation in median survival. Supportive evidence for survival gains also comes from trials in the secondand third-line situation after failure on previous regimens [162]. Trials randomizing between chemotherapy and no/delayed chemotherapy or comparing different schedules have shown that the QoL of individual patients can be improved by treatment, or at least remain stable even if the treatment may cause disabling toxicity [162, 163]. This is the same using combinations of drugs, which more frequently result in objective responses, although increased toxicity to the treatments may temporarily counterbalance this [164, 165]. Even if age per se is not a prognostic factor in most of the trials [170, 171], the great majority of the elderly population is never evaluated for trial participation. However, there are exceptions and a reasonably high chronological age should not be an absolute contraindication to initiating therapy. What may need further discussion is whether all incremental gains are sufficiently large in relation to toxicity, other inconveniences, and costs to qualify as routine therapy. Most clinicians agree that statistical significance does not necessarily indicate clinical relevance.
Purchase 10mg maxalt with amex
Nevertheless joint pain treatment natural maxalt 10mg on line, recent studies including M1 and M2 markers have related high M2 density to improved outcome. A number of studies have reported that increasing tumour neutrophil infiltration was associated with improved survival. However, this may be confounded by the observation that many inflammatory cell types increase together and are associated with improved survival [23], and therefore any association of a particular immune cell type with improved survival is not necessarily causal. Mast cells are other innate immune cells capable of degranulation of pro-inflammatory mediators. For example, in six out of the seven published studies in colorectal cancer, high numbers of mast cells were associated with improved survival particularly when present at the invasive margin. In addition, although eosinophils make up a small proportion of tumour inflammatory cell infiltrates (approximately 2%), based on five of six published studies, high numbers when present are associated with improved outcome [11]. Finally, natural killer cells when present in increasing numbers are associated with an improved prognosis in patients with colorectal cancer. Again, the above relationships may be confounded by the fact that many inflammatory cell types increase together [23]. More recently, this insight has been applied to the prediction of outcome in patients undergoing surgery for colorectal cancer. Higher numbers of stromal myofibroblasts, identified using specific staining, have been reported to be associated with shorter disease-free survival, independent of tumour stage [28]. Similar associations, independent of tumour stage, have been reported using routine H&E slides and calculating the proportion of tumour cells to stroma [29]. However, the relationship between the proportion of stroma and nature of the inflammatory cell infiltrate is not, as yet, clear. Indeed, the association between a pronounced lymphocytic infiltrate and improved survival within breast and gastrointestinal tumours has been appreciated for more than 30 years [10, 11]. B lymphocytes have a role in mediating and regulating immune responses and also act as antigen-presenting cells to stimulate T-lymphocyte responses. However, their role in cancer is not as well established as that of T lymphocytes. Indeed, there remains ongoing controversy given that they may have pro and anti-T-lymphocyte effects effects in differing tumour microenvironments. The humoral response can be considered to include the complement pathways, opsonins, and antibodies, and these are intimately linked to promote tumour cell lysis and phagocytosis. Indeed, there is good evidence from animal models to indicate their importance in determining innate and adaptive immune responses in the tumour microenvironment and the likelihood of tumour progression. Therefore, there is a considerable and pressing need to translate such findings from animal work into patient investigation of the tumour microenvironment. Other promising future strategies may include specific immune cell depletion or inactivation, and, at a systemic level, maintaining cell-mediated adaptive immune responses and suppressing development of non-specific innate cellular responses such that the host systemic inflammatory response and its associated detrimental effects on body composition and quality of life and survival are abrogated. Such therapeutic goals may be achieved using non-selective anti-inflammatory agents or using highly selective agents subtly to attenuate targeted mediators or pathways of the immune and inflammatory responses to cancer. Systemic adaptive immune and inflammatory response the circulating adaptive immune cells, according to number, primarily include T and B lymphocytes. Therefore, it is somewhat surprising that little in vivo work has been carried out to examine the relationship between circulating T lymphocyte subsets and outcome in patients with cancer, particularly since blood measurements are more readily available to assess and to monitor patient response to treatment. Therefore, an alteration of circulating T-lymphocyte subpopulations appears to be a feature of common solid tumours and is consistent with impaired immune function at the systemic level. However, to date little work has been carried out to characterize the phenotype of circulating innate and adaptive immune cells. Nevertheless, the systemic inflammatory response appears primarily to reflect an up-regulation and down-regulation of the circulating innate and adaptive immune processes, respectively. Non-selective agents Aspirin and non-steroidal anti-inflammatory drugs including cyclooxygenase-2 inhibitors have been described as potential chemotherapeutic agents, most commonly in colorectal cancer. There is consistent evidence of a chemo-preventative reduction in colorectal cancer incidence and mortality, based on epidemiological studies [64]. However, they are known to have a number of pleiotropic effects on cell proliferation, angiogenesis, inflammation, and endothelial cell function. A number of epidemiological studies have reported a reduction in risk of colorectal cancer with statin use[71]. In particular, there is evidence from clinical trials of a 90% reduction in risk of inflammatory bowel-disease-related colorectal cancer [72]. Statins have a variety of actions that may potentially alter immune and inflammatory responses in cancer. For example, in cardiovascular disease prevention trials there are clearly identified anti-inflammatory effects, with down-regulation of pro-inflammatory cytokines and increased cardiovascular risk reduction in patients with elevated serum inflammatory markers [73]. Selective agents With the increasing knowledge of the immune and inflammatory dysfunction in patients with cancer, specific and selective immunomodulatory agents are having an emerging role in oncological practice. In general, these include targeted agents aiming at specific manipulation of cytokines/chemokines or blocking cellular responses to encourage a rebalancing of immune and inflammatory responses. Novel methods of achieving this goal include the development of cancer vaccines and adoptive cell transfer. The lead for such work has come from the newer treatments of chronic inflammatory diseases in non-cancer conditions. Finally, there has been recent interest in the use of autologous dendritic cell pulsed with tumour peptides and injected as a vaccine directly into tumour tissue. Sipuleucel-This a novel dendritic-cell-based vaccine that has been employed successfully in castration-resistant metastatic prostate cancer. In summary, along with the now widespread appreciation of the pivotal role of the immune/inflammatory responses in dictating human cancer outcome, there has been a recent rapid expansion of therapies aimed at manipulation of these responses. Broad-spectrum anti-inflammatory drugs have long been appreciated as playing a role in oncological progression; however, stratification using more accurate immune/inflammatory or molecular profiling may help to identify those patients who may derive greatest therapeutic benefit. Recently, there have been impressive results observed in melanoma and renal cell cancer. It remains to be determined whether the use of such immunotherapies will apply to most tumour types. Conclusion It is clear that immune and inflammatory responses, both local and systemic, are intimately linked and impact on cancer survival. However, the mechanisms by which these inflammatory responses are activated, maintained, and interact are not clear. It also may be, at least in non-hereditary disease, that inflammation becomes the key hallmark on which all the other hallmarks of cancer are dependent. Therapeutic intervention using non-selective anti-inflammatory agents is widely advocated and likely to become part of routine clinical practice in the near future. Selective therapeutic intervention directed at the immune and inflammatory responses in cancer is in its infancy. Statins and the risk of colorectal cancer: a meta-analysis of 18 studies involving more than 1. The relationship between components of tumour inflammatory cell infiltrate and clinicopathological factors and survival in patients with primary operable invasive ductal breast cancer. Targeting of the innate immunity/inflammation as complementary anti-tumor therapies. Targeting tumor-infiltrating macrophages decreases tumor-initiating cells, relieves immunosuppression, and improves chemotherapeutic responses. Prognostic significance of tumor-associated macrophages in solid tumor: a meta-analysis of the literature. The distribution of macrophages with a M1 or M2 phenotype in relation to prognosis and the molecular characteristics of colorectal cancer. Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. Enhancement of antibody-dependent mechanisms of tumor cell lysis by a targeted activator of complement. Modulation of protective T cell immunity by complement inhibitor expression on tumor cells. Interactions between lymphocytes and myeloid cells regulate pro- versus anti-tumor immunity. Granzyme B and perforin are important for regulatory T cell-mediated suppression of tumor clearance.