Order nizoral with a visa
Uncal herniation: uncus is displaced medially and inferiorly over the free edge of the tentorium cerebelli antifungal activity order cheap nizoral on-line. Monitor blood sugar and attempt glucose control between 5 and 15 mmol/L but with close monitoring and avoidance of hypoglycaemia. Increased permeability of capillary endothelial cells, tumour, abscess, around a haemorrhage, contusion, meningitis. Failure of the normal homeostatic mechanisms that maintain cell size: neurons, glia, and endothelial cells swell. Hypoxic ischaemic/infarction, osmolar injury, some toxins; part of the secondary injury sequence following head trauma. Interstitial or transependymal: characterised by an increase in the water content of the periventricular white matter. Coiling aneurysms: neuro-interventionalist (neuroradiologist or 541 neurosurgeon or neurologist) packs detachable platinum coils into the aneurysms to induce thrombosis. Studies have shown that patients with a ruptured aneurysm tend to do better in the long term after a coiling procedure. Biopsy: may be indicated to get tissue samples of areas within the brain that are suspicious for tumours or infections. Stereotactic biopsy may be needed for deepseated lesions, multiple lesions, or lesions in a surgically poor candidate who cannot tolerate anaesthesia. Debulking tumours: those that cannot be resected completely a palliative debulking can take place to slow progression and symptoms. Aetiology: destruction of cartilage begins within 48 h due to pressure, proteases and cytokines from macrophages, bacteria and inflammatory cells. Management: urgent consult with orthopaedics as requires joint aspiration especially if prosthesis. In older adults the vertebral bodies are more likely to be infected, due to changes in blood flow with spinal osteomyelitis. Management: rapid diagnosis and orthopaedic and microbiology liaison to choose optimal antimicrobial therapy. Surgical: debridement and removal of necrotic tissue and drainage of any abscess or collections. Clinical: co-existing urethritis, conjunctivitis, diarrhoeal illness, males > females. Plain films may be needed if fracture is a concern or erosive arthritis in chronic gout. Identify and manage both the cause of the fall and any co-morbidities such as anaemia, anticoagulation, volume depletion, electrolyte imbalance, uncontrolled diabetes, uncontrolled heart failure, correctable cardiac arrhythmia or ischaemia, acute chest infection, exacerbation of chronic chest conditions so as not to delay surgery. Surgical management: schedule hip fracture surgery on a planned trauma list same day if possible. Perform replacement arthroplasty (hemiarthroplasty or total hip replacement) in patients with a displaced intracapsular fracture. Offer total hip replacements to those with a displaced intracapsular fracture who were able to walk independently out of doors with no more than the use of a stick, who are not cognitively impaired and are medically fit for anaesthesia and the procedure. Use 548 extramedullary implants such as a sliding hip screw in preference to an intramedullary nail in patients with trochanteric fractures above and including the lesser trochanter. Surgery and fixation or total hip replacement improves pain control and mobility and outcome compared with non-operative approach. Operate on patients with the aim to allow them to fully weight bear (without restriction) in the immediate post-operative period. Those at the more benign end often come to medicine for management of pain and rehabilitation. They must first be reviewed by those specialised in trauma and orthopaedics especially to exclude other injuries. Fractures of pubic rami with insignificant or minimal trauma can be a presentation of osteoporosis. Be careful with those on anticoagulation as pelvic bleeds can be severe and the Hb can drop. The most important part of any eye exam is detecting reversible reductions in vision. It is surprising how patients with structural brains lesions do not appreciate their hemianopia even when gross. Non-arteritic anterior ischaemic optic neuropathy: atherosclerotic or thromboembolic occlusion of posterior ciliary artery which supplies optic 550 nerve. Carotid doppler may show plaques or stenosis on affected side; assess and manage vascular risk factors. If seen within first hour, sudden pressure and release to the globe may dislodge embolism or propel it peripherally. Refer all patients who present with retinal artery occlusion within 24 hours of the symptoms to ophthalmologist to attempt dislodging the embolus causing the occlusion. Fundi - Retina is red with haemorrhage with bloody venous infarction and engorged dilated retinal veins. If seen within first hour sudden pressure and release to the globe may dislodge embolism or propel it peripherally. In retinal detachment, the inner sensory retina detaches from the underlying pigmented epithelium of the retina. Patients also describe a shadow or curtain that comes across their field of vision. The most common cause of retinal detachment is a tear or hole in the retina that may be secondary to a posterior vitreous detachment or an ocular trauma. May give homonymous hemianopia but bilateral strokes may occur depending on aetiology. Occipital/parietal/temporal tumour: visual loss and hemianopia progressive +/- headache. Steroids for acute pituitary insufficiency and urgent neurosurgical decompression if vision affected (Section 5. Any involvement of cornea or visual loss or glaucoma or orbital cellulitis or severe symptoms needs ophthalmic review. Patients with a red eye should go straight to eye casualty but may be misdirected to the general take. Watch for acute angle closure glaucoma in older patients where the presentation can be unclear. Conjunctiva is red and injected and there may be a discharge and anything from tingling to pain. Occasionally due to gonorrhoea where it is very severe with discharge and chemosis, preauricular node enlargement. Both redness, tearing and ocular pain on palpation over the sclera and involvement of the anterior chamber which can blur vision. Always check visual acuity with some form of quantitative assessment that can be repeated. Three main diagnoses are lateral medullary syndrome, apical lung tumour and carotid dissection. Ophthalmoplegic migraine: recurrent episodes of headache and associated symptoms and diplopia which resolves. Pathology: Granulomatous infiltration, Disruption of the internal elastic lamina, Proliferation of the intima, Occlusion of the lumen. Activated charcoal is estimated to reduce absorption of some substances by up to 60%.
Buy nizoral 200 mg visa
Such damage to the alveolar membrane would lead to an alteration of the alveolar microenvironment anti fungal cleanse purchase nizoral 200mg with amex, the release of multiple cytokines, particularly of Th2 type. Myofibroblasts are key cells in the healing process, mainly via the deposition of extracellular matrix. In lung fibrosis, this deposition is more than necessary and results in the accumulation of extracellular matrix and scarring [44]. Telocytes are a type of stromal cell, which may have a role in the regulation of tissue homeostasis, suggesting that this loss could be implicated in the pathogenesis of fibrosis [45]. Their precise role is still unknown but they could be involved in the development of microvascular pulmonary damage. Other studies will be needed to establish precisely their role in the physiopathology of fibrosis. The vasculitic process can also involve many other organs 184 Interstitial lung diseases Table 10. The most common pulmonary manifestations are lung nodules, lung cavities, pulmonary fibrosis, and alveolar hemorrhage [48,49]. The activation of neutrophils, endothelial cells, and B cells may also be involved. Non-necrotizing granuloma observed in the submucosa is voluminous, cohesive, and associated with or without the fibrosis. Its incidence is higher in women, in Nordic regions, in black people, as well as those in the 20th or 30th year of life [61]. A response of the immune system to various environmental substances, such as respiratory irritants, allergens, inorganic particles, insecticides, construction materials, and microorganisms, mainly bacteria, has been suggested [62]. Indeed, some studies have shown an increased prevalence of this disease in first- and seconddegree relatives of index cases [63]. Various alleles could predispose to the development of the disease such as class I antigens. Those granulomas are noncaseating and made of various cells, such as macrophages, lymphocytes, epithelial, and multinucleated giant cells. In the lung, the majority of granulomas are localized close to or within bronchi at the subpleural level or in perilobular spaces (lymphatic distribution) [66]. A secondary hyperglobulinemia can be observed following an increase in the activation of B-lymphocytes [69]. At the level of lung function tests, patients with sarcoidosis usually have a restrictive syndrome, with a reduction of the total lung capacity. The mechanisms of this airway obstruction are diverse and may include: (1) a reduction of bronchial caliber from bronchial granulomatosis, bronchial stenosis, distal bronchiolitis, or peribronchial fibrosis, (2) a bronchial distortion secondary to pulmonary fibrosis, and/or (3) a bronchial compression from hypertrophic thoracic adenopathy [70]. In addition to the thoracic features, many other organs may be involved with different frequencies (Table 10. Organ damage by sarcoidosis can resolve spontaneously in 1 or 2 years or, in some cases, progress toward an evolving pulmonary fibrosis and irreversible damage to the affected organs. Many factors will influence the evolution of the disease, mainly the race (black race is associated with an increased prevalence of severe multisystemic disease), the initial radiologic stage (Table 10. In the majority of cases, no treatment will be needed but in some specific situations, particularly when granulomas affect organ function, corticosteroid and/or immunosuppressive treatment can be indicated. Histopathologic characteristics of these various diseases provide the basis of this classification. Classically, the lung lesions have also a temporal heterogeneity, being of different age [5,74]. Lesions are found in both lungs, preferentially at lung bases and at the periphery (subpleural zone) of the lungs. Some risk factors have been identified, such as smoking, infections, exposure to environmental pollutants, gastroesophageal reflux, and genetic factors [75]. For many years, the main hypothesis has been that an inflammatory response was preceding the lung fibrosis. This hypothesis was first based on animal models suggesting that inflammation could be observed before the fibrotic process and that the suppression of this alveolitis decreased the subsequent fibrosis. In this context, new hypotheses and a new classification of interstitial pneumopathies were proposed. This process would be initiated by an epithelial injury with epithelial shedding and alveolar basement membrane lesions. These myofibroblasts would then be involved in the overproduction of extracellular matrix proteins. This fibrin acts as a temporary matrix and reservoir of fibroblast and inflammatory cells growth factors. Furthermore, thrombin would favor fibroblast proliferation and their transformation into myofibroblasts, leading to extracellular matrix deposition in the lung interstitium [97]. Many factors contributing to this increased collagen production have been identified. First, a disequilibrium could exist between interstitial collagenases and tissue inhibitors of metalloproteinases [85,98]. This phenomenon could result in a reduction of the proteolytic activity and then lead to the progressive deposition of extracellular matrix proteins. This increased survival of myofibroblasts could explain their persistence in the damaged epithelial zones [85]. Finally, fibroblasts could be resistant to the antiproliferative properties of prostaglandins E2 [99]. Such uninhibited proliferation would then contribute to the excessive deposition of collagen. Indeed, in addition to the secretion of proteins of the extracellular matrix responsible for the fibrosis observed, myofibroblasts would produce free radicals (oxidants) promoting alveolar epithelial cell apoptosis [100]. Furthermore, alveolar epithelial cells would have a procoagulant activity that could compromise normal migration of cells necessary to the extracellular matrix repair. In the last two decades, the prognosis of this condition has not been significantly changed despite an increase in knowledge of its underlying mechanisms. With the recognition of the role of fibroblasts, strategies are now oriented toward various agents with antifibrotic properties, hoping to inhibit this process, once initiated. There is typically an inflammatory cell infiltrate and fibrosis of variable intensity. The initial event leading to the formation of organized pneumonia is an injury to alveolar epithelial cells, causing a desquamation of pneumocytes, followed by denudation of the basement membrane [115]. This process will cause the formation of gaps in the basement membrane from which inflammatory cells (lymphocytes, neutrophils, eosinophils, plasma cells, and mast cells), and then fibroblasts, will infiltrate the alveolar interstitium, forming clusters (buds) of fibroinflammatory cells [116]. Following activation of the coagulation cascade, intra-alveolar deposition of fibrin will be observed, promoting migration of cells such as fibroblasts and favoring the fibrinogenesis. Progressively, the inflammatory cells will decrease in number at the alveolar interstitium and most of the fibroblasts will transform to myofibroblasts, leading to the production of collagen. Finally, an alveolar cell proliferation will allow a progressive re-epithelialization of the basement membrane and a return to its initial integrity. The cause of these differences remains unknown but some hypotheses have been raised. These two interstitial pathologies are characterized by an accumulation of pigmented macrophages. In regard to its strong association with smoking, the first treatment is smoking cessation. Its exact pathogenic mechanisms are still unknown but many inflammatory mediators seem to be involved. There are two main consecutive phases: (1) an exudative phase developing the first week following the initial insult and (2) an organization phase starting during the second week. Survivors can recover a normal pulmonary function but some will present some recurrence of the disease and/or an evolution toward chronic fibrosing pneumopathy. Most cases are considered idiopathic, although few cases are familial or have nonspecific antibodies.
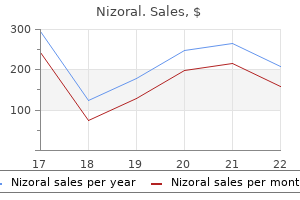
| Comparative prices of Nizoral | ||
| # | Retailer | Average price |
| 1 | Office Depot | 456 |
| 2 | PetSmart | 248 |
| 3 | Trader Joe's | 642 |
| 4 | Target | 929 |
| 5 | DineEquity | 908 |
Cheap nizoral 200mg mastercard
These lymphocytes are fungus jeopardy answer sheet cost of nizoral, indeed, specialized in fighting intracellular pathogens and can also trigger apoptosis in infected cells expressing viral antigens at their surface. This process is very important for the recruitment of circulating cells to the periphery, including the lungs. Chemokines are classified based on their primary structure but can also be regrouped according to the type of cells that they can attract. Unfortunately, it is unknown where these mechanisms occur in the chronology of disease as well as the full extent of their role. The most important genetic factor involved in the pathogenesis of emphysema is the Z alpha-1 antitrypsin allele, an important elastase 110 Chronic obstructive pulmonary disease inhibitor. The results of these studies on polymorphism are still debated as these findings could be attributed to ethnic differences. Effect of pharmacological treatment on pulmonary inflammatory response Aside smoking cessation, no pharmacological treatment has been shown to slow down disease progression or lower disease-related mortality [22,99]. Few studies have looked at the effect of those therapies on the pulmonary inflammation response. Recent reports also suggest that tiotropium can Conclusions and future perspectives 111 inhibit viral activation of inflammation [108,109]. In addition to their antimicrobial activity, macrolides have significant immunomodulatory/anti-inflammatory properties related to the macrocyclic lactone ring [115]. The significance of these observations is still under debate with regards to their extrapulmonary impacts. People afflicted with severe emphysema also have a significant decrease of their peripheral muscle mass [133,134]. This phenomenon can be attributable to malnutrition, systemic inflammation, inactivity, local oxidative stress, use of corticosteroids, and hypoxemia. The loss of peripheral muscle mass is not a negligible issue as it has been shown that, in patients with similar lung function, loss of muscle mass is associated with unfavorable prognosis and increased disease-related mortality [135]. There has been increased and renewed interest in this research from people with all kinds of background including immunologists, geneticists, and specialists in molecular and cell biology. Because of these various contributions, the role of the immune system in the pathogenesis of emphysema-related pulmonary changes is no longer debated. Unfortunately, the exact reasons as to why tobacco smoke triggers in only some smokers, the pathogenic mechanisms of emphysema are still largely unknown 112 Chronic obstructive pulmonary disease and poorly understood. Current research efforts are focusing on a better understanding of the inflammatory response including the exact role of both innate and adaptive immunity triggered by tobacco smoke exposure. A comparison of the quantitative anatomy of the bronchi in normal subjects, in status asthmaticus, in chronic bronchitis, and in emphysema. Goblet cell hyperplasia and epithelial inflammation in peripheral airways of smokers with both symptoms of chronic bronchitis and chronic airflow limitation. Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Inflammatory reaction in pulmonary muscular arteries of patients with mild chronic obstructive pulmonary disease. Morphologic changes in the muscular pulmonary arteries: Relationship to cigarette smoking, airway disease, and emphysema. Impairment of endothelium-dependent pulmonary artery relaxation in chronic obstructive lung disease. Inflammatory response of lung macrophages and epithelial cells to tobacco smoke: A literature review of ex vivo investigations. The effects of chronic bronchitis and chronic airflow obstruction on lung cell populations recovered by bronchoalveolar lavage. Inflammatory cells and mediators in bronchial lavage of patients with chronic obstructive pulmonary disease. Differences in interleukin-8 and tumor necrosis factor-alpha in induced sputum from patients with chronic obstructive pulmonary disease or asthma. Severity of airflow limitation is associated with severity of airway inflammation in smokers. Cell migration in the immune system: the evolving inter-related roles of adhesion molecules and proteinases. A possible experimental approach to the association of hereditary alpha-1-antitrypsin deficiency and pulmonary emphysema. Excessive neutrophil elastase in bronchoalveolar lavage fluid in subclinical emphysema. Neutrophil granule proteins in bronchoalveolar lavage fluid from subjects with subclinical emphysema. Elevated levels of matrix metalloproteinases in bronchoalveolar lavage fluid of emphysematous patients. Lung matrix metalloproteinase-9 correlates with cigarette smoking and obstruction of airflow. Releases and activity of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 by alveolar macrophages from patients with chronic obstructive pulmonary disease. Cigarette smoke impairs clearance of apoptotic cells through oxidant-dependent activation of RhoA. Alveolar macrophages from subjects with chronic obstructive pulmonary disease are deficient in their ability to phagocytose apoptotic airway epithelial cells. Alveolar epithelial and endothelial cell apoptosis in emphysema: What we know and what we need to know. What is autoimmunity and why is it likely to be important in chronic lung disease Lymphocyte population and apoptosis in the lungs of smokers and their relation to emphysema. Subepithelial immunopathology of the large airways in smokers with and without chronic obstructive pulmonary disease. Perforin, granzyme B, and FasL expression by peripheral blood T lymphocytes in emphysema. Endothelial cell death and decreased expression of vascular endothelial growth factor and vascular endothelial growth receptor 2 in emphysema. Biochemical intermediates in alpha 1-antitrypsin deficiency: Residual family resemblance for total alpha 1-antitrypsin, oxidized alpha 1-antitrypsin, and immunoglobulin E after adjustment for the effect of the Pi locus. Association between alpha-1-antichymotrypsin polymorphism and susceptibility to chronic obstructive pulmonary disease. Tissue inhibitor of metalloproteinases-2 gene polymorphisms in chronic obstructive pulmonary disease. Microsatellite polymorphism in the heme oxygenase-1 gene promoter is associated with susceptibility to emphysema. Antioxidant gene polymorphisms and susceptibility to a rapid decline in lung function in smokers. Association of tumor necrosis factor alpha gene promoter polymorphism with the presence of chronic obstructive pulmonary disease. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. Antiinflammatory effects of salmeterol/fluticasone propionate in chronic obstructive lung disease. Corticosteroids and adrenoceptor agonists: the complements for combination therapy in chronic airways diseases. Tiotropium attenuates virus-induced pulmonary inflammation in cigarette smoke-exposed mice. Inhibitory effects of tiotropium on rhinovirus infection in human airway epithelial cells. Roflumilast in symptomatic chronic obstructive pulmonary disease: Two randomized clinical trials. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long acting bronchodilators: Two randomised clinical trials. Anti-inflammatory effects of the phosphodiesterase-4 inhibitor cilomilast (Ariflo) in chronic obstructive pulmonary disease.
Order 200 mg nizoral
If the patient is thin antifungal body wash walmart generic nizoral 200 mg free shipping, the proximal cephalic vein is easily seen at the elbow and may be used for anastomosis to the brachial artery in the cubital fossa. A transverse incision is made a little proximal to the cubital fossa, and the brachial artery is mobilized distally to the level of the bicipital tendon. At times, the basilic vein can be mobilized from the level of the wrist to the middle of the forearm and then tunnelled subcutaneously for anastomosis to the radial artery. It is also possible to anastomose the basilic vein to the ulnar artery, but this should not be done if there has been a previous radiocephalic fistula in that arm because of the high chance of compromising the circulation to the hand since the radial artery is usually occluded. Basilic vein-to-branchial artery fistulas are used when there is no available cephalic vein present. Disadvantages of the basilic vein for use as an outflow source includes its deeper anatomic location relative to the cephalic vein and its location in the medial arm. Approximately 6 weeks later, if there is clinical evidence that the fistula has matured, transposition to a more superficial and lateral location is performed. Of note, transposition may assist in maturation of the fistula if large collateral branches are present in the basilic vein. Cooper and colleagues performed a recent metaanalysis which demonstrated no differences in failure and patency rates between the one- and two-stage approaches. Eventually it may fail due to sclerosis of the veins as a result of repeated venipuncture or following renal transplant, when changes occur in the blood that restore coagulation to normal. Failure is usually most expeditiously managed by construction of another access site. If another Cimino fistula cannot be constructed or the old site revised, then a prosthetic bridge fistula is constructed. If the artery and vein are some distance apart, the bridge graft lies in a straight or curved line. Care should be taken to avoid kinking of the fistula material, and in particular, it should not pass over joints where flexion will restrict flow and lead to graft clotting. The larger the artery used to provide flow through the fistula, the lower the rate of fistula thrombosis. For this reason, thigh fistulas, using the common or superficial femoral artery, are less likely to clot. In addition, they can 822 Principles of vascular access surgery be easily utilized by the patient, who has both hands free, for home dialysis, but they have the major disadvantage of a higher postoperative infection rate. Location of the fistula in the arm is almost always the first-choice site and is the mandatory position in the older patient with significant leg vessel atherosclerosis or the obese patient who has dermatitis in the groin. The bovine heterograft was developed over a decade ago, by enzyme debridement of fresh bovine carotid arteries, followed by tanning with dialdehyde. At one time, it was thought that bovine heterografts should be utilized primarily rather than a Cimino fistula. However, some 5 years after introduction of bovine grafts, it was evident that they were prone to infection and aneurysm formation. Progressive degeneration of the graft material occurs so that the whole graft tends to undergo aneurysmal dilation or forms nonanastomotic aneurysms. These grafts also develop stenosis at the venous anastomosis together with other prosthetic materials, which leads to graft blood f low restriction and then clotting. Recent improvements in the manufacturing and collagen cross-linking of these bioprosthetic grafts have led to recent re-evaluation of their use as hemodialysis conduits. Heparin molecules are covalently bonded to the graft surface and maintain bioactivity. Over two-thirds of these infections are found within the first 4 months of use, and the majority requires removal of the graft for resolution. If the infection involves the anastomosis, it is not uncommon that the artery will need to be reconstructed with an autogenous patch or interposition vein graft. The diameter of the graft is selected to be larger than that of the supply artery to ensure maximum fistula flow. The size, if too large, also increases the likelihood of developing high-output cardiac failure and distal limb ischemia. Experience has shown that grafts of 6 mm in diameter provide good flow and retain their patency while being uncommonly associated with the foregoing complications. If this is a concern, then a preoperative angiogram may be helpful in planning further patient management. Puncture should be delayed for about 2 weeks until the prosthesis has been incorporated in the surrounding tissue. The conduit is tunnelled through the subcutaneous tissue on the radial side of the forearm to allow the arm to lie comfortably during dialysis. Bridge fistulas in the arm have a shorter useful patency than those in the thigh, since clotting is more likely because of the lower fistula flow rates. On the other hand, bridge fistulas in the arm are less likely to become infected than thigh fistulas, which are in proximity to the bacteria of the heavily colonized groin skin. Upon failure, the arterial end of the fistula can be moved to the more proximal femoral artery. With long-term hemodialysis, the surgeon can be called on to create multiple vascular access sites, because each will eventually fail. It is conceivable that some patients could potentially outlive their available limb access sites. Differences in compliance between the vein and the prosthetic material result in turbulence and hydraulic trauma to the vein. At times, outflow obstruction is appreciated early before the graft thromboses by the dialysis nurse who observes a rise in pressure at the venous end of the conduit or notes that the blood in the venous chamber is becoming dark during dialysis. This is best performed through an incision sited near the venous end of the graft. A 2 cm long incision is made in the graft just proximal to the venous anastomosis. The patient is heparinized, and a small Fogarty embolectomy catheter is passed into the vein to remove any thrombus. If this fails to restore good flow in the graft, it is then necessary to explore the arterial end to remove clots. If these manoeuvres result in good flow and good pulsation with a strong thrill, then the operation may be terminated. However, if this does not occur, then an angiogram should be obtained to determine if there is any correctable stenosis at the arterial or venous ends of the fistula. Such a lesion at the venous anastomosis is managed by a patch angioplasty or constructing a more proximal venous anastomosis or grafting from the fistula to a more proximal vein. This may be due to poor vessels (an atherosclerotic radial artery or small veins) or technical factors such as obstruction at the venous anastomosis. With time, the Cimino fistula is more likely to remain patent than a bridge fistula. Thrombosis occurring 3 months or more following construction of a Cimino fistula is commonly due to fibrosis of the veins, following the repeated trauma of needle punctures. When late clotting of a Cimino fistula occurs, it may be most expedient to convert it to a bridge prosthetic fistula. Late thrombosis of a graft due to intimal hyperplasia in the infection Infection is second to cardiovascular disease as a cause of mortality and morbidity in patients on chronic dialysis. The highest rate of infection is found with tunnelled hemodialysis catheters, while the lowest is with the Cimino fistula. Needling of fistulas can produce a hematoma, which then becomes infected with skin organisms. Involvement of the anastomotic site with infection may lead to endovasculitis, septicemia and metastatic abscess formation. Grafts may become infected at the time of implantation from skin organisms and poor aseptic technique. To lower the likelihood of this, perioperative antibiotics effective against skin organisms, particularly Staphylococcus epidermidis and Staphylococcus aureus, are routinely used. On occasion, a superficial soft tissue infection overlying a graft will resolve; however, graft infections usually require removal of the prosthetic material for complete resolution.
Best purchase for nizoral
The onset of symptoms is often insidious fungus that causes hair loss order 200 mg nizoral with amex, and they can worsen over a period of weeks, months, or years. It can have a detrimental effect on the overall quality of life, causing problems such as inability to sleep, concentrate, and continue with a daily routine. Due to the high prevalence of the disease, this leads to a significant problem in the Western world. Stiffness of joints is another common complaint, with patients having difficulty initiating movement, for example, when moving from a seated position after a prolonged position. A careful discussion of what the patient hopes to achieve with any form of intervention, in particular surgical, is also essential to meet realistic expectations and rehabilitation goals. Other disease processes may be important if surgery is to be undertaken, such as the presence of systemic disease. Careful neurovascular assessment and range of movement of the limb and their documentation are also crucial pre and post operatively. A thorough examination of the joint itself is essential to ensure that any surgical intervention will bring success. Typical findings during the examination will include tenderness on palpation of the joint, swelling in or around the joint, auditory or palpatory crepitus on movement, and loss of function, often seen as a loss of range of movement in the joint. Assessment of the alignment of the whole limb to look for biomechanical problems must be undertaken. The joints proximal and distal to the joint under review should also be carefully assessed, to look for any sources of referred pain. Investigations can be used to confirm the diagnosis, but are also a useful adjunct to confirm the degree of severity of joint involvement. This is ideal for more complex bony articulations, and is commonly used in guiding foot and ankle surgery. Treatment options Conservative interventions Treatment options can be thought of as nonsurgical (conservative and medical or pharmacological) or surgical. There is an increasing focus on early and nonsurgical interventions in the primary care setting with the aim of disease prevention and slowing down progression (Table 17. Simple advice for symptom management may include the use of physiotherapy in some cases, use of analgesia, use of bracing and walking aids, activity modification, intra articular injections, and psycho social interventions to make patient expectations of the disease process realistic and manageable. Minimally invasive interventions Interventions can also be used with investigations. The use of contrast dye, local anaesthesia, corticosteroid, or hyaluronan injections into the joint via ultrasound or radiography are commonly used, particularly in the foot and ankle surgery. Specific indications include locking, and giving way in the presence of loose bodies or displaced meniscal tears. It involves inserting a camera into the joint using a mini surgical approach for both diagnostic and therapeutic indications. In some cases, the procedure is diagnostic, with the aim to assess the severity of the disease process before further interventions are carried out. Arthroscopy can also be used to alter the disease process, with debridement and washout of the diseased joint as a therapeutic intervention. There is an increasing demand with which health care systems are currently struggling with the cost implications of an ageing population to find effective and durable interventions. Arthroplasty/joint reconstruction Arthroplasty is one of the most widely performed surgical procedures. Its aim is to either partially or totally replace the native and diseased joint with an artificial joint. However, due to its success, patient expectations have changed, as well as a change in the symptom threshold for the procedure. This has led to a constant attempt at improving modern joint replacements function. Some of these are aimed at improving the life span of the artificial joint, as one of the major concerns with the use of artificial joints in the younger patients is their early failure rate. There has also been a trend towards joint preserving replacements, such as patella femoral or medial uni compartmental knee replacements, particularly if the anterior cruciate ligament is intact. Arthrodesis of the joint means that the bones around the joint are fused together, so that they are no longer a source of pain, but at the cost of restricting range of movement. In fact, most patients are content to make that compromise to achieve pain relief after years. The spine, the shoulder, and the hand are other sites where arthrodesis is still used as a relatively common surgical procedure. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. SpAs are classically characterised by: sacroiliitis, inflammatory back pain, and enthesitis, made up of several conditions that often overlap. Inflammatory back pain and limitation of lumbar spine movement are a hallmark of the disease. It is thought to be multifactorial, with both genetic and environmental factors playing a role. The onset of the disease is often insidious, with morning stiffness, weight loss, and malaise. Extra articular features are associated with increased overall morbidity and premature mortality. Checking liver and renal function is essential, as it might influence the choice of medications. Care is usually led by a consultant rheumatologist, but general practitioners, orthopaedic surgeons, nurse specialists, occupational therapists, physiotherapists, and podiatrists have important roles. Operative: Surgical opinion is sought in patients who suffer with persistent pain due to joint damage, deformity, or disability in the form of arthroscopy, arthrodesis, and arthroplasty. Blood pressure and cholesterol monitoring are important in reducing risk of heart attack and stroke. Aetiology the aetiology of spondyloarthropathies is complex and may be an interplay between genetic and environmental factors. Peripheral Most common site is the Achilles tendon arthritis Swelling of the entire digit. Back pain is the predominant complaint in patients suffering from SpAs, and it is important to differentiate between mechanical and inflammatory causes of back pain (Table 18. Systemic constitutional features include symptoms such as weight loss and night sweats. Making the diagnosis is often challenging because there may be few objective signs in early disease. Examination the modified Schober test is the standard examination to assess limitation of forward flexion and hyperextension. The distance between these marks should increase from 15cm to 20cm with forward flexion. The characteristic "question mark posture" develops with advance disease due to loss of lumbar lordosis, exaggeration of thoracic kyphosis, and inability to extend the neck. Surgery is a last resort for addressing complications that ranges from arthroplasty, spinal fracture fixation, and correction of deformity. Cardinal rule: A hot swollen joint should be treated as septic arthritis until proven otherwise Other inflammatory arthritides Reactive arthritis Reactive arthritis (ReA) is defined as a form of spondyloarthritis that arises following an infection. Despite the link with infection, cultures of synovial fluid are often sterile and there is no role for antibiotics in treating the arthritis. Sometimes there is no history of infection, suggesting that subclinical infections or other environmental factors might play a role in the pathogenesis of the disease. Urethritis the bacteria commonly associated with reactive arthritis include: Salmonella species Shigella species Yersinia enterocolitica Campylobacter jejuni Clostridium difficile Chlamydia trachomatis Most patients achieve complete remission within 6 months. The presence of oral ulceration, erythema nodosum, or pyoderma gangrenosum should alert the clinicians to evaluate for the presence of underlying bowel pathology. Other conditions with intestinal involvement and arthritis are outlined in Table 18.
Syndromes
- Enlarged liver (hepatomegaly)
- Heart
- Problems with eye development (retinopathy of prematurity) and blindness
- Stiff neck (meningismus)
- Acromegaly
- 4 months
Cheap nizoral 200mg otc
Ascites recurs in 90% of patients if diuretics not begun and in 20% despite diuretics antifungal skin cream cheap nizoral 200mg amex. Hyponatraemia: ratio of Na >126 mmol/L, no need for H2O restriction and continue diuretics if renal function stable. If Na <125 mmol/L consider stopping diuretics, especially if Na <121 mmol/L if creatinine rising (>150 mol/L), volume expansion maintaining renal function is crucial. Aetiology: systemic vasodilation and renal hypoperfusion and afferent renal vasoconstriction. Precipitated by spontaneous bacterial peritonitis (25% of patients), bleed or infection. Criteria for diagnosis of hepatorenal syndrome in cirrhosis: (1) cirrhosis with ascites + serum creatinine >133 mol/L (1. Clinical: fatigue, malaise, progressive uraemia with oliguria without significant proteinuria. Liver transplantation is usually indicated in Types 1 and 2 and is the main definitive therapy. Identify likely precipitants: sepsis: chest, urine, biliary, spontaneous bacterial peritonitis. Clinical: reversal of day/night sleeping, psychomotor dysfunction, impaired memory. Sensory abnormalities, poor concentration, disorientation, tremor, shuffling gait. Grades of encephalopathy Stage I: anxiety, mild confusion, reversed sleep/wake cycles, apathy, asterixis. Management: antibiotics are the first line in therapy and then some require open or radiologically guided percutaneous drainage depending on the response (see below). Management: surgery remains the primary treatment and the only hope for complete cure. Risks: seen mainly in females, middle age and beyond, obesity, those on Octreotide. Inflammation is more likely chemical rather than infective as bile is usually sterile. Pathophysiology and clinical presentations of gallstones Biliary colic Acute cholecystitis Gallstone stuck at cystic duct. Similar to 338 cholecystitis Acalculous cholecystitis Chronic cholecystitis Gallbladder perforation Acute cholangitis Gallstone acute pancreatitis cholecystitis. Identifies thickened wall gallbladder and gallbladder distension (>4 cm short axis) and pericholecystic fluid. Surgical Management: A laparoscopic cholecystectomy should be carried out urgently or within 5 days of onset of symptoms otherwise the patient is prone to further episodes. In those with biliary colic alone which settles within 6 h and no cholecystitis can go home with adequate pain control and have surgical review later. Acalculous cholecystitis can occur with no stones seen but a typical acute cholecystitis picture. Causes Gallstones (45%) A gallstone in ampulla of Vater can allow bile reflux into pancreatic duct activating enzymes. Alcohol (45%) Hypertriglyceridaemia Primary hyperparathyroidism Cancer Miscellaneous Drugs Congenital Pancreatic cancer, biliary cancer. Aetiology: Activation of trypsin, lipase and amylase and autodigestion leads to an inflamed oedematous/haemorrhagic pancreas. On-going tissue damage can activate complement with a progressive systemic inflammatory response syndrome. Two types of acute pancreatitis (interstitial oedematous pancreatitis and necrotising pancreatitis). A level of >1000 is more diagnostic, but there is not a close correlation between amylase level and clinical severity. Very rarely a normal amylase suggests little remaining amylase-producing 342 pancreatic tissue left. Best done at or after 3 days to support diagnosis and determine full extent of pancreatic necrosis and the presence of any fluid. In a patient older than 40 years, a pancreatic tumour should always be considered as a cause. Pancreatic pseudocyst and fluid collections: can form around the pancreatic mass and may need laparoscopic drainage. Chronic pancreatitis: repeated episodes of pancreatic injury often alcohol related and frequent admissions. Develops exocrine and later endocrine dysfunction with steatorrhoea and weight loss. Differential is autoimmune pancreatitis, inherited causes that start in early adult life and pancreatic cancer. Treatment is alcohol avoidance, nutritional support, manage exocrine and endocrine needs. Acutely these patients may be seen for mainly pain relief and managing acute flares. Nutrition: In mild/mod disease normal oral feeding can be considered if no significant gastroparesis and there are normal bowel sounds and no signs of ileus. Calcium and magnesium should be checked and replaced if needed and adequate hydration given. Diabetes: variable rate insulin infusion initially if hyperglycaemic or known diabetes convert to regular regimen. Try to avoid parenteral nutrition unless the enteral route is not available, not tolerated, or insufficient for caloric requirements. A pancreatic necrosectomy involves removing dead pancreatic tissue, which may be done by laparoscopy. Asymptomatic pseudocysts may be observed and often resolve but some may need to be managed endoscopically. Behavioural: offer advice and help with good nutrition and in cessation of alcohol and smoking. Excess blood loss/destruction of red cells, acute or chronic bleeding, chronic or acute haemolysis. Causes/notes on anaemia Acute haemorrhage Acute blood loss and haemodilution later with a lower Hb. Iron deficiency B12 deficiency 347 Folate deficiency Dietary or malabsorption, drugs. Anaemia chronic disease Haemoglobinopathy Congenital abnormal Hb reduces red cell half life with chronic anaemia. Caution with giving Hb in pernicious anaemia with circulatory overload, if future need for bone marrow transplant, check if need irradiated blood (Section 8. Focused management on determining cause and replacing components or treating disorder. Reaction to vessel wall injury is rapid adhesion of platelets to the subendothelium and formation of a haemostatic plug, composed primarily of platelets. Significant quantitative or qualitative platelet dysfunction results in mucocutaneous bleeding. Low platelets can be due to a fall in production or increased consumption or sequestration. Causes of low platelets Sampling error: platelet clumping can spuriously lower platelet count. Pregnancy-related thrombocytopenia: usually mild thrombocytopenia in an otherwise healthy pregnancy. Pre-eclampsia/eclampsia syndrome: causes increased platelet turnover, even when the platelet count is normal. Drug-induced thrombocytopenia: drugs such as gold, ibuprofen, quinine, quinidine, methotrexate, amiodarone, valproate, cimetidine, captopril, carbamazepine, sulfonamides, glibenclamide, tamoxifen, ranitidine, phenytoin, vancomycin, piperacillin, cocaine. Severe fever with thrombocytopenia syndrome: infectious disease with a 12% case-fatality rate in China due to a novel bunyavirus.
Buy nizoral on line
After obtaining proximal and distal control fungus with blisters generic nizoral 200mg otc, the aneurysm with associated skin erosion is resected and an interposition bovine carotid heterograft is used to revise the fistula. Several currently available devices use a combination of pharmacologic thrombolysis with fragmentation and removal of the thrombus burden. The AngioJet thrombectomy system utilized high-speed saline jets which are injected through the catheter lumen backwards at high speed and which fragment adjacent thrombus through a Venturi effect. Thrombolytic agents can also be injected into the vessel lumen to deliver medication directly into the clot. Complications associated with AngioJet thrombectomy include embolization of the thrombus burden, intravascular hemolysis and vessel perforation. Kakkos and colleagues demonstrated excellent results using the AngioJet device in their series of 207 declotting procedures. Balloon angioplasty and stenting the primary cause of failure for hemodialysis fistulas and grafts is the development of intimal hyperplasia at the venous anastomosis resulting in stenosis and/or occlusion. Traditionally, open surgical thrombectomy and patch angioplasty of the venous outflow was the main method of treatment. Percutaneous balloon angioplasty and stenting are effective treatments for venous outflow stenoses and should be performed once the thrombus burden has been removed. Potential complications of these techniques include vessel perforation and migration of the stent if it is undersized. Invariably, late recurrence of intimal hyperplasia at the stent implantation site occurs and these patients frequently require repeat intervention to maintain access patency. The use of covered stents is also commonly used to treat both stenoses at the venous end of the hemodialysis fistula and central vein stenoses. Primary, primary-assisted and secondary patencies were 56%, 86% and 100% at 12 months, respectively. The use of drug-eluting balloons for use in failed hemodialysis access is not currently the standard of care. However, some reports demonstrate early promise for this developing technology to treat outflow intimal hyperplasia in these patients. Katsanos and colleagues reported the 6-month results of a prospective randomized trial comparing paclitaxel-coated balloons vs. Larger randomized trials are needed to justify the cost difference between these two distinct modalities. Chronic hemodialysis using venipuncture and surgically created arteriovenous fistula. Real-time ultrasound guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Realtime ultrasound-guided catheterization of the internal jugular vein: A prospective comparison with the landmark technique in critical care patients. Similar failure and patency rates when comparing one- and two-stage basilic vein transposition. A prospective randomized study of heparin-bonded graft (Propaten) versus standard graft in prosthetic arteriovenous access. Bovine carotid artery (Artegraft) as a hemodialysis access conduit in patients who are poor candidates for native arteriovenous fistulae. Outcomes of arteriovenous fistulae compared with heparin-bonded and conventional grafts for hemodialysis access. Secondary patency of thrombosed prosthetic vascular access grafts with aggressive surveillance, monitoring and endovascular management. Longterm outcomes of primary angioplasty and primary stenting of central venous stenosis in hemodialysis patients. Balloon angioplasty vs nitinol stent placement in the treatment of venous anastomotic stenoses of hemodialysis grafts after surgical thrombectomy. Efficacy of covered stent placement for central venous occlusive disease in hemodialysis patients. Stentgrafts versus angioplasty and/or bare metal stents for failing arteriovenous grafts: A cross-over longitudinal study. The clinical presentations are extremely protean and can range from an asymptomatic birthmark to fulminant, life-threatening congestive heart failure. Attributing any of these extremely varied symptoms that a patient may present with to a vascular malformation can be challenging to the most experienced clinician. If a clinician sees one patient every few years, it is extremely difficult to gain a learning curve to diagnose and optimally treat them. Typically, these patients bounce from clinician to clinician only to experience disappointing outcomes, complications and recurrence or worsening of their presenting symptoms. As catheter delivery systems and embolic agents improved, embolotherapy has since emerged as a primary mode of therapy in the management of vascular anomalies. Anatomically, vascular malformations are often in surgically difficult or inaccessible areas which have led to increased reliance on the sophisticated endosurgical skills of the interventional radiologist and interventional neuroradiologist in the management of these problematic patients. Because the clinical and angiographic manifestations can be extremely varied, hemangiomas and vascular malformations are always difficult to classify. Moreover, numerous descriptive terms have been applied to impressive clinical examples in the hopes of distinguishing them as distinct syndromes. This has resulted in significant confusion in the categorization and treatment of these complex vascular lesions. Some of the confusing terms include congenital arteriovenous aneurysm, cirsoid aneurysm, serpentine aneurysm, capillary telangiectasia, angioma telangiectaticum, angioma arteriale 829 830 Diagnosis and management of vascular anomalies racemosum, angioma simplex, angioma serpiginosum, naevus angiectoides, hemangioma simplex, lymphangioma, hemangiolymphangioma, naevus flammeus, verrucous hemangioma, capillary hemangioma, cavernous hemangioma and venous angioma. This classification system, based on endothelial cell characteristics, has removed much of the confusion in terminology that is present in the literature today. Once all clinicians understand and utilize this important classification system, ambiguity and confusion will be removed and all clinicians can speak a common language. As Reid has stated: In view of the common development on each side of the vascular tree, and in view of the enormous constructive and destructive changes necessary before the final pattern of the vascular tree is reached, it is a marvel not that abnormal congenital communication occasionally, or rarely, occur, but that they do not occur more often. Because of the complex nature of hemangiomas, the proliferative phase may continue as the involutive phase slowly begins to dominate. Involuting hemangiomas show diminished endothelial cellularity and replacement with fibrofatty deposits, exhibit a unilamellar basement membrane, demonstrate no uptake of tritiated thymidine into endothelial cells and have normal mast cell counts. Because of the landmark research of Mulliken and co-workers, studying these issues at the cellular level, not the macro-level, has allowed these diagnoses to be differentiated and defined. Trauma, surgery, hormonal influences caused by birth control pills and the hormonal swings during puberty and pregnancy may cause a lesion to expand and grow hemodynamically. As the embryo matures, the interlacing system of blood spaces becomes differentiated by partial resorption of the primitive vascular spaces and the formation of mature arterial and venous vascular spaces with intervening capillary beds. The classically outlined sequence of events includes (1) the undifferentiated capillary network stage; (2) the retiform developmental stage, characterized by coalescence of the original equipotential capillaries into large, interconnecting, plexiform vascular spaces without an intervening capillary bed; and (3) the final developmental stage, characterized by the resorption of the primitive vascular elements and the formation of mature arterial, capillary, venous and lymphatic elements. Failure of orderly resorption of vascular elements from the retiform developmental stage results in the retention of interconnecting channels of immature arteries and veins without an intervening capillary bed. Other errors in embryologic morphogenesis during the retiform developmental stage could result in other types of vascular malformations. Another example would be retention of primitive capillary elements, which would explain capillary malformations found in port-wine stains. However, due to the constant breakdown and formation of vascular spaces in the embryo, these stages can overlap. This can lead to retained mixed vascular lesions that are complex Concepts in patient management 831 endothelial cell proliferation, contain large vascular channels lined by flat endothelium, have a unilamellar basement membrane, do not incorporate tritiated thymidine into endothelial cells and have normal mast cell counts. Vascular malformations are true structural anomalies resulting from inborn errors of vascular morphogenesis and the failure of orderly resorption of these primitive vascular elements. Vascular malformations are categorized into malformed arterial, capillary, venous, lymphatic, and combinations of these malformed primitive vascular elements.
Nizoral 200 mg discount
The subacromial bursa becomes inflamed (bursitis) antifungal agents discount 200mg nizoral overnight delivery, as may the supraspinatus (tendinitis). Primary treatment involves injection of steroid into the subacromial bursa and physiotherapy. Resorption of the calcium, which is most commonly situated within the supraspinatus tendon, leads to pressure build up within the tendon and an associated bursitis. It rarely requires acute intervention, as symptoms of pain and weakness are minimal. Symptomatic tears can be treated conservatively with steroid injection into the subacromial space and physiotherapy to strengthen the remaining cuff muscles and parascapular muscles. Many tears are amenable to repair (either arthroscopic or open); however, larger and more chronic tears with tendon retraction and muscle atrophy are often irreparable. This is a difficult situation for which there are several treatment options that have varying degrees of success. Young patients may be best treated with a tendon transfer (latissimus dorsi and teres major for supraspinatus and infraspinatus tears). Newer experimental treatments not supported yet by medium or long term outcome data include balloon interposition arthroplasty and superior capsular plication. Yet, in the presence of cuff arthropathy (proximal migration of the humeral head towards the acromion followed by glenohumeral chondrolysis and humeral head collapse), the only viable option is reverse geometry total shoulder arthroplasty. Passive range of movement should be full, but actively the range may be reduced, although the deltoid may compensate for chronic tears. Resisted external rotation tests are for tears of infraspinatus and teres minor, and the belly press test and lift off test in internal rotation test are for the subscapularis. Adhesive capsulitis (frozen shoulder) Adhesive capsulitis occurs in the fifth and sixth decades, more commonly in women, and is associated with diabetes and other endocrine disorders. It is a self limiting condition that will resolve with no treatment within 2 years in the vast majority of patients. Treatment consists of pain relief in the form of analgesics and steroid injection. Surgical interventions such as manipulation under anaesthetic or capsular release are appropriate for resistant cases that are affecting function. The position of apprehension in anterior instability is in abduction and external rotation. The relocation test relieves apprehension by applying a posterior force on the proximal humerus. Combined flexion, adduction, and internal rotation reproduces posterior apprehension. Traumatic Trauma to the arm in an abducted and externally rotated position leads to translation of the humeral head in an anterior direction, leading to detachment of the antero inferior labrum (Bankart lesion) and anterior dislocation. Nerve palsy There is an association between anterior dislocations and axillary nerve palsy, presenting with loss of sensation in the regimental badge area of the lateral deltoid and weakness of the deltoid muscle. Atraumatic Atraumatic instability may be multidirectional and has an association with increased joint laxity. Both shoulders may be affected, and the patients are often capable of relocating the joint themselves. Other A third, much less common, group of patients with muscle patterning may present to Emergency Department with an acute dislocation. Proximal humeral fractures Fractures of the proximal humerus is common, especially among the geriatric population who sustain falls. Follow up in clinic, analgesia, and physiotherapy can return the patient to almost full function within months. There must be a balance between the benefits and risks of surgery, especially on geriatric patients with comorbidities and pre morbid low functional state. Chronology of management options consist of analgesia, physiotherapy, (image guided), joint injections, and finally, joint replacement. The bigger the procedure, the more restricted is post operative range of movement. Elbow conditions Tendinopathies around the elbow account for the majority of presentations of elbow pain. Resisted wrist and finger flexion provokes pain, and treatment options mirror those of tennis elbow. Distal biceps tendon rupture Distal biceps tendon rupture occurs suddenly on lifting. Olecranon bursitis Olecranon bursitis presents as a fluid filled collection at the posterior aspect of the elbow, superficial to the proximal ulna. It may be difficult to distinguish from an infected olecranon bursitis, which presents with spreading cellulitis and raised inflammatory blood markers. Aspiration has a high incidence of recurrence and sinus formation, and should only be performed for chronic cases, using strict antiseptic technique. A patient with septic arthritis of the elbow joint will be unwell, have a raised temperature, swelling, and redness not isolated to the posterior aspect of the elbow, and will have a marked restriction in range of motion due to severe pain. End stage disease may need surgical treatment to debride and release the joint capsule in the presence of stiffness or require total joint replacement when symptoms of pain and stiffness are uncontrolled. Severe compression leads to weakness of the small muscles of the hand, leading to weakness and difficulty with fine motor function. General clinical assessment the treatment goal is to restore function not only to the affected area but also the whole upper extremity. Enquiring about the occupational and recreational activities are also paramount to a successful outcome in the management of both chronic conditions and acute trauma. An understanding of what helps to relieve and aggravate their symptoms is essential in determining treatment (Table 7. Social history, including smoking Traumatic conditions the history ought to elicit the mechanism of injury, time of injury, and the environment in which this occurred. Many of these patients can later become involved in compensation, and therefore, it is essential to have clear documentation (Table 7. Physical examination the assessment of the hand and wrist typically follows the standard musculoskeletal assessment of look, feel, and movement, followed by special tests, assessment of the neurovascular status, and detailed functional evaluation. The physical examination begins with range of movement of the neck, shoulder, and elbows, as the hand is useful only if it can be positioned in space. Observation of the resting hand should include the posture of the hand and digits, and comparisons should be made to the opposite side (Table 7. As stiffness has a significant effect on hand function, range of movement should be recorded carefully for later comparison testing. Vascular status Vascular function can be determined by evaluating capillary refill or a Doppler ultrasound evaluation of pulses distal to the laceration. Pressure is released from one artery, and capillary refill should be noted in the fingertips within 5 seconds. Neurological status Where nerve laceration or compression is suspected, a detailed neurological function should be tested. Light touch is easy to test in clinic, but two point discrimination or Semmes Weinstein monofilament threshold testing can also be used. The integrity of the radial and ulnar digital nerve to each finger can be assessed by testing sensation on each side of each finger pulp. Careful observation for swelling and palpation of each bone will guide towards specific radiographic views to obtain fracture diagnosis. Presentation the hallmark symptoms are tingling, numbness, and pain in the median nerve distribution, which can wake the patient from sleep or occur during the day with hand elevation and gripping. Symptoms are sometimes relieved with hanging the affected hand over the side of the bed or shaking it off. The first line treatment where there is a temporary cause, such as in pregnancy, is a steroid injection into the tunnel (not the nerve). This can also be helpful where the diagnosis is unclear; however, relief of symptoms is usually temporary.
Buy generic nizoral 200 mg on-line
Irritant-induced asthma can occur after acute or repeated inhalation of such toxic/highly irritant substances fungus gnats vector buy nizoral 200mg cheap. Etiology More than 450 substances can induce occupational asthma and this number keeps increasing. We can find the updated list of those substances on specialized internet sites, such as Asmapro or Haz-map. In the case of immune mechanisms, this type of asthma appears generally after a latency period of variable duration between the 232 Occupational respiratory diseases Table 12. Atopic subjects have a slight increase in the risk of developing this type of asthma following the exposure to this type of agents. Sensitizing subjects could present asthmatic responses even at low concentration of these agents; it is therefore of major importance to stop the exposure when the diagnosis is established. With isocyanates and red cedar, the airways can show a predominant lymphocytic response. These agents can also act in activating nervous sensory receptors to release substance P and other neuropeptides although the role of these agents in the physiopathology of this type of asthma remains to be explored. Withdrawal from exposure to the sensitizing agent could lead to a complete or partial remission of symptoms and lung function abnormalities. Hypersensitivity pneumonitis (Extrinsic allergic alevolitis) this disease has been described in Chapter 10. More than 300 agents have been suspected to cause a development of allergic alveolitis. The description of the physiopathology of this disease can be found in Chapter 10. Its etiology is multifactorial and is identified based on epidemiologic, clinical, radiologic, or functional criteria. Airflow limitation can result from different factors: chronic inflammation of the bronchial mucosa, bronchial secretions, bronchoconstriction, and bronchoalveolar remodeling. The association of bronchial ailments with some types of work leading to marked exposure to organic and inorganic dusts has been reported since the nineteenth century. Occupational bronchitis can be found in miners, foundry workers, welders, aluminum industry workers (potrooms), and grain workers (elevators, longshoremen, and farmers). As smoking is very common in these workers, sometimes it is difficult to determine if the problem is caused by smoking or workplace exposure. Occupational infections Some types of work bring a risk of infections for the workers. Infection can originate from a sick animal or human, or be transmitted from biological products that are handled. The main types of workers at risk are health care workers (physicians, dentists, nurses, technicians, hospital employees, home elderly, etc. Infections include mainly tuberculosis, tularemia, and deep mycosis (histoplamosis, blastomycosis). Cancers of occupational origin There are more than 300 workplace substances with a carcinogenic potential. Despite pessimistic predictions of epidemiologists, less than 10% of respiratory cancers are of occupational origin, 85% being caused by smoking, and 5% being associated with other cancers. No specific chemical or morphological characteristic can distinguish bronchial cancers of occupational origin from those caused by smoking. Quantification of mineral particles in the lung tissue can help to establish a causal link with some types of occupational exposures. Acute inhalation accidents Acute bronchopneumopathies from irritant gas exposures Inhalation of toxic gas can cause variable clinical pictures, sometimes difficult to classify in a coherent category. We can observe a transient irritation of the bronchial tree, asphyxia, acute pulmonary edema, bronchiolitis, systemic response, and mycotoxicosis. Intoxication with weak doses can simply cause bronchial irritation with a transient cough, while massive exposure may result in hemorrhagic pulmonary edema. Corrosive gas, very soluble, can cause its main effects on the proximal airways (larynx, trachea). Less soluble gases can penetrate more deeply in the lung and affect bronchioles and parenchyma more intensely. For the irritant gases, the intensity of exposure and solubility of the gas in the water are the main factors determining severity of the picture and the site of damage. During a fire, inhalation by the victims or firemen of large quantities of smoke can cause extensive damage to the bronchial tree. Combustion and degradation of various materials by heat (plastics, resins, coatings, etc. The treatment includes humidity, oxygen, corticosteroids, and ventilator support if necessary in addition to antibiotics. Metal fumes fever this febrile syndrome of limited evolution has been described in 1832 by Thackrah in a brass foundry. It is caused by inhalation of metallic vapors such as zinc or brass, mainly during the welding of galvanized metals [35]. It constitutes the most frequent problem caused by inhalation of organic dust in the agricultural world. These particles come from hay or cereals contaminated by mushrooms and actinomycetes, wood particles, and can be found, for example, in confined environments in the pork industry. Inhalation of dust is generally massive being about 10 times higher than what could be causing an extrinsic allergic alveolitis [39]. We generally observe fever, lleucocytosis, and sometimes, on chest auscultation, crackling rales or wheezing. If the individual survives, asphyxia can leave some sequelae, neurological mainly, according to its duration, to the severity of hypoxia and extension of tissue damage. Bioactive asphyxia products are gases with a specific toxicity that can interfere with cell respiration by mechanisms indicated in Table 12. Carboxyhemoglobin is a stable compound, which sequesters hemoglobin, and reduces its capacity to transport oxygen in causing an anemic hypoxemia. The normal carboxyhemoglobin level is less than 2%, while in smokers it can vary between 5% and 10%. Multiple mechanisms are involved as we have shown and could affect mainly the bronchial tree or lung parenchyma or other thoracic structures. A respiratory and environmental questionnaire associated with a physical examination and some blood tests. The diagnosis and attribution of asbestos-related diseases in an Australian context: Report of the Adelaide Workshop on Asbestos-Related Diseases. Induced sputum markers of fibrosis and decline in pulmonary function in asbestosis and silicosis: A pilot study. The beryllium lymphocyte proliferation test: Relevant issues in beryllium health surveillance. An official American Thoracic Society statement: Diagnosis and management of beryllium sensitivity and chronic beryllium disease. Structural changes and airway remodelling in occupational asthma at a mean interval of 14 years after cessation of exposure. Airway inflammation after removal from the causal agents in occupational asthma due to high and low molecular weight agents. Lung function decline, chronic bronchitis, and occupational exposures in young adults. Differential respirable dust related lung function effects between current and former South African coal miners. Organic dust toxic syndrome: An acute febrile reaction to organic dust exposure distinct from hypersensitivity pneumonitis. Exposure to microorganisms associated with allergic alveolitis and febrile reactions to mold dust in farmers.

Order online nizoral
At the anterior margin of the thalamus antifungal cream for jock itch in india discount 200mg nizoral mastercard, the body of the fornix separates into two columns that arch along the superior and anterior margins of the foramen of Monro. The columns of the fornix then split, passing predominantly posterior to the anterior commissure, and are directed inferiorly and posteriorly through the lateral wall of the third ventricle to reach the mammillary bodies at the floor of the third ventricle. Although macroscopically fused and gathered into a "core" that is covered laterally by the insula, the basal ganglia and the thalamus are embryologically and functionally distinct structures. The basal ganglia are telencephalic structures, and the thalamus is a diencephalic structure. The basal ganglia consist of four nuclei: the striatum (caudate nucleus, putamen, and the nucleus accumbens), globus pallidus, substantia nigra, and subthalamic nucleus. The caudate nucleus is a C-shaped structure that wraps around the thalamus; it has a head, body, and tail. The head and body are lateral walls of the frontal horn and body of the lateral ventricle. Each lateral ventricle wraps around the superior, inferior, and posterior surfaces of the thalamus. The anterior tubercle of the thalamus is the posterior limit of the foramen of Monro; the posterior part, called the pulvinar (pillow) of the thalamus, is the wall of three compartments in the cerebrum: the posterolateral part of the pulvinar is the lateral half of the anterior wall of the atrium; the posteromedial part is covered by the crus of the fornix and is part of the superolateral wall of the quadrigeminal cistern; the inferolateral part of the pulvinar is the roof of the wing of the ambient cistern. The hippocampus occupies the medial part of the floor of the temporal horn and is divided into three parts: the head, body, and tail. The head of the hippocampus, the anterior and largest part, is directed anteriorly and inferiorly and then medially. At the medial end of the tip of the temporal horn, it turns up vertically and bends over laterally, forming the medial wall of the tip of the temporal horn ahead of the choroidal fissure. The head of the hippocampus is free of choroid plexus and is characterized by three or four hippocampal digitations; its overall shape resembles a feline paw, and it is directed toward the posterior segment of the uncus. Its posterior limit is characterized by the initial segment of the fimbria and the choroidal fissure. Superiorly, the head of the hippocampus is related to the posteroinferior portion of the amygdala. Anteriorly, it is related to the uncal recess of the temporal horn, which is the anterior continuation of the collateral eminence. The emergence of the choroid plexus, the fimbria, and the choroidal fissure marks the beginning of the body of the hippocampus. The body of the hippocampus has an anteroposterior and inferosuperior direction and narrows as it approaches the atrium of the lateral ventricle. Posterior to the head of the hippocampus, the medial wall of the temporal horn is the choroidal fissure. At the atrium of the lateral ventricle, the body of the hippocampus changes direction and has its longitudinal axis oriented transversely to become the tail of the hippocampus. The tail of the hippocampus is slender and constitutes the medial part of the floor of the atrium; medially, the tail of the hippocampus fuses with the calcar avis. The temporal amygdala is composed of a series of gray matter nuclei classified into three main groups: basolateral, corticomedial, and central. From the neurosurgical viewpoint, the temporal amygdala can be considered as being entirely located within the boundaries of the uncus: superiorly, the amygdala blends into the globus pallidus; inferiorly, the temporal amygdala bulges inferiorly into the most anterior portion of the roof of the temporal horn above the hippocampal head and the uncal recess; medially, it is related to the anterior and posterior segments of the uncus. It is a C-shaped arc that extends from the foramen of Monro through the body and atrium to the temporal horn. The choroid plexus is attached to the fornix and to the thalamus by ependymal coverings called the taenia fornicis and taenia choroidea, respectively; in the temporal part, the taenia fimbriae attaches the choroidal plexus to the fimbria. The arrows indicate the anterior opercular compartment of the sylvian fissure, located between the posterior portion of the orbital gyri and the planum polare. ThirdVentricle the third ventricle is a narrow, funnel-shaped, unilocular, midline cavity. The first layer is the fornix; the body of the fornix is the anterior part of the roof of the third ventricle, and the crura and the hippocampal commissure are the roof of the posterior portion. The second layer is the superior membrane of the tela choroidea, which passes thorough the forniceal side of the choroidal fissure to cover the choroid plexus of the lateral ventricle. The third layer is the vascular layer located in a space between the superior and inferior membranes of the tela choroidea called the velum interpositum, which contains internal cerebral veins and branches of the medial posterior choroidal arteries. The fourth layer is the inferior membrane of the tela choroidea, which forms the floor of the velum interpositum. The posterior part of the inferior membrane of the tela choroidea is attached to the superior surface of the pineal body. The fifth layer is the choroidal plexus of the third ventricle, usually represented by two parallel strands of choroid plexus projecting backward on each side of the midline. At the inner angle formed by the roof and the anterior wall is the anterior commissure. Frequently, there is another commissure in the cavity of the third ventricle located posteriorly to the foramen of Monro called massa intermedia, which connects both thalami. The lateral wall of the third ventricle is constituted by thalamus above and hypothalamus below, separated by hypothalamic sulcus, a shallow groove extending from the foramen of Monro to the aqueduct. The thalamus is located above the midbrain and extends laterally above the oculomotor nerve and the parahippocampal gyrus. The floor of the frontal horn is located above the optic nerve and the planum sphenoidale. The head of the caudate nucleus is located above the bifurcation of the carotid artery, anterior clinoid process, and anterior perforated substance. The splenium of the corpus callosum is located above the vein of Galen, and the pineal gland is located just anterior to the inferior surface of the vein of Galen. The M2 or insular segment extends from the limen insulae to the superior and inferior circular sulci of insula; it runs in the insular compartment of the sylvian fissure and is constituted by the superior and the inferior trunks and their branches. After reaching the superior or inferior circular sulcus of insula, the M2 branches enter the opercular compartment and are called the M3 segment. The M3 or opercular segment runs in the opercular compartment and is related to the frontal and parietal opercula superiorly and to the temporal operculum inferiorly. The loop of the most posterior M3 segment branch that exits from the sylvian fissure is called the M point or sylvian point. The fourth segment is the M4 or cortical segment, which extends from the sylvian fissure to the lateral surface of the cerebrum (Videos 2-15 and 2-16). Lateral Surface: Venous Relationships the superficial venous system drains the superficial one fifth of the thickness of the cerebrum, whereas the deep venous system drains the other four fifths of the depth of the cerebrum. On the lateral surface of the cerebrum, the superficial venous drainage system is accomplished by venous channels adjacent to the lobes. On the frontal and parietal lobes, the venous drainage can direct superiorly toward the superior sagittal sinus or inferiorly toward the superficial sylvian vein; on the temporal lobe, the veins can drain superiorly toward the superficial sylvian vein or inferiorly toward the dural sinuses below the temporal lobe. In the region of the pterion, it enters the dura and runs along the lesser wing of the sphenoid, in the sphenoparietal sinus or sinus of the lesser wing of the sphenoid, to enter the anterior end of the cavernous sinus through the medial end of the superior orbital fissure, then drains into the basilar sinus and the inferior petrosal sinus. The vein of Trolard, or superior anastomotic vein, is the largest anastomotic vein crossing the lateral surface of the brain between the superior sagittal sinus and the sylvian fissure. The deep part of the sylvian fissure is related to the deep sylvian or middle cerebral vein and its tributaries. The tributaries of the deep sylvian vein come mainly from the sulci of the insula. The blue arrows indicate the superior limiting sulcus of the insula; the red arrows indicate the inferior limiting sulcus of the insula; the yellow arrow indicates the anterior limiting sulcus of the insula. C, Frontal view of venous angiographic magnetic resonance imaging to display the basal vein. The olfactory tract and sulcus divide the basal surface of the frontal lobe in two uneven parts: a smaller and medial part is the rectus gyrus; and a larger and lateral part, the orbital surface, is located above the orbit and composed of orbital gyri. The orbital surface is divided by the orbital sulcus, a complex sulcus that presents a rough configuration of the letter "H," into four quadrants: anterior, medial, posterior, and lateral orbital gyri. The pars orbitalis of the inferior frontal gyrus is continuous with the posterior part of the lateral orbital gyrus and with the lateral part of the posterior orbital gyrus.