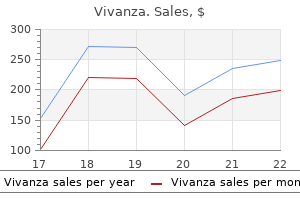
Buy vivanza 20 mg cheap
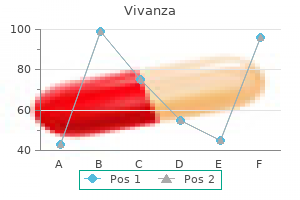
Aetiology of the disease Antibody deficiencies result from inherited or acquired disorders that lead to abnormalities in the development erectile dysfunction doctor philippines order cheap vivanza on-line, maturation, and/or function of B-lymphocytes. Impaired functioning of B-cells leads to decreased immunoglobulin production, which manifests clinically as an increased susceptibility to infections. Some of these diseases occur due to single-gene mutations which affect the development or function of B-lymphocytes. B-cells are derived from the common lymphoid progenitor and develop within the bone marrow. The final stages of maturation occur within the germinal centre of secondary lymphoid organs (lymph nodes, spleen) on encounter with the specific antigen. From the point of view of clinical investigation, it is useful to classify antibody deficiency in terms of circulating B-cell numbers and the pattern of reduction of serum immunoglobulins (see Table 297. While the absence of B-cells is highly suggestive of an inherited defect interfering with B-cell development, an elevated serum IgM in association with reduced IgG and or IgA points to a defect in immunoglobulin Demographics of the disease the overall prevalence of clinically significant primary antibody deficiency is estimated to vary from 1: 25 000 to 1: 110 000. The commonest immunodeficiency is selective IgA deficiency with a prevalence of 1:500 to 1:700, but a majority of these patients remain asymptomatic. Other single-gene defects are even rarer, with only few reported cases for some conditions. Reprinted from Journal of Allergy and Clinical Immunology, volume 124, issue 6, Notarangelo et al, Primary immunodeficiencies: 2009 update, pp. Other sites of infection include the skin, the joints, the gastrointestinal tract, and the urinary tract. However, enteroviral meningoencephalitis has been reported in patients with X-linked agammaglobulinaemia. The current practice of maintaining a higher-trough IgG level has significantly reduced the incidence of this complication. Other non-infectious complications include polyclonal lymphocytic infiltration, frank lymphoma, enteropathy, and liver abnormalities. Treatment and its effectiveness the mainstay of treatment for primary antibody deficiency is replacement immunoglobulin therapy, along with judicious use of antibiotics for the treatment of acute infections as well as for prophylaxis in individual patients. Currently, immunoglobulin replacement can be achieved effectively either intravenously or subcutaneously. Both methods have been shown to be safe and efficacious in decreasing the incidence and severity of infections in patients with antibody deficiencies. Prognosis and how to estimate it Treatment of patients with antibody deficiency syndromes with replacement immunoglobulin therapy and aggressive antibiotic treatment significantly improves the prognosis, with a reduction in the number of infection episodes and infection-related complications, such as the development or progression of bronchiectasis. This, however, does not alter the natural course of the condition or the development of non-infectious complications. Infection outcomes in patients with common variable immunodeficiency disorders: Relationship to immunoglobulin therapy over 22 years. Defective T-cell function is associated with chronic intestinal and biliary colonization with Cryptosporidium spp. The lack of lymph node germinal centres due to defective interaction between T-cells and B-cells is a characteristic histological feature. These comprise mutations in genes encoding for purine pathway enzymes, and a range of molecules involved in signal transduction, including tyrosine kinases, cytokine receptors, and key cell surface receptors. Typically, patients have elevated serum IgM levels, accompanied by reduced IgG and IgA, due to a failure to switch from IgM to other classes of immunoglobulin when mounting a secondary immune response against pathogens. This figure is likely to be higher in those populations with a high degree of consanguineous marriages. The preponderance of genes encoding important immunological functions on the X-chromosome leads to a predominance of affected boys. Very rarely, intestinal lymphangiectasia may be associated with T-cell lymphopenia and a low serum IgG as a direct consequence of loss of IgG and efflux of lymphocytes via aberrant lymphatic channels. Clinically significant drug-induced combined T-cell and B-cell defects may occur in some patients who have received chemotherapy for cancer or immunosuppressive therapy for autoimmune disease. Drugs responsible for such iatrogenic immune defects include corticosteroids, cyclophosphamide, fludarabine, methotrexate, azathioprine, mycophenolate mofetil, and ciclosporin. Where significant drug-induced immune deficiency associated with T-cell and B-cell defects does develop, they do not usually pose a diagnostic challenge because of the clinical context in which immunodeficiency develops. Essentials of Clinical Immunology, Sixth edition, Helen Chapel, Maneel Haeney, Siraj Misbah and Neil Snowden. However, precise molecular diagnosis is essential for purposes of genetic counselling, prenatal diagnosis, assessing prognosis, and, in the future, using gene therapy. Acceptable diagnostic alternatives to the gold standard In view of the ease with which serum immunoglobulins and circulating lymphocytes can be measured, there is little need for alternative surrogate tests of T-cell and B-cell function. In a resource-limited setting where access to flow cytometry may be limited, the finding of an absolute lymphopenia would be highly indicative of T-cell lymphopenia, since T-cells constitute approximately 70% of the circulating lymphocyte count. Similarly, the absence of a thymic shadow on a chest X-ray would point to a T-cell defect, but its utility as a diagnostic marker is limited by the occurrence of thymic atrophy in acutely ill babies. In pursuing this diagnosis, it is essential to obtain evidence of combined T-cell and B-cell dysfunction, as evidenced by the presence of T-cell lymphopenia, impaired lymphocyte proliferation, and hypogammaglobulinaemia. Measurement of serum immunoglobulins and specific antibodies serve as markers of B-cell function. While the circulating lymphocyte surface marker profile provides useful clues as to the underlying molecular defect, definitive diagnosis requires sequencing of the relevant gene to identify disease-causing mutations. Imaging of the chest followed by bronchoalveolar lavage, where possible, is important to explore the possibility of pneumocystis infection. The mortality in the remainder of cases has been due to severe infection, with reactivated cryptosporidial disease being a particular problem. The main physiological functions of the complement system include defence against pyogenic bacterial infections, clearance of immune complexes and products of inflammatory damage, and acting as a bridge between the innate and adaptive immune system (see Table 299. The complement system is regulated by various complement inhibitors (regulatory proteins) that are present in both the classical pathway and the alternate pathway and which regulate and prevent spontaneous activation of the complement system, thereby preventing complement-mediated damage to tissues under normal circumstances. Acquired complement deficiency may occur as a consequence of autoantibody-mediated inhibition of complement proteins, as evidenced by anti-C1-inhibitor and acquired angioedema and anti-C3 nephritic factor and mesangiocapillary glomerulonephritis. Inherited defects affecting the inhibitors or regulatory proteins of the complement system, namely C1-inhibitor and factors H and I, have also been described. C1-inhibitor deficiency is the most well characterized; it is inherited in an autosomal dominant manner and is associated with hereditary angioedema. Mutations in the gene coding for C1-inhibitor result in either an absent or a non-functional protein. C1-inhibitor deficiency may be acquired secondary to a range of lymphoproliferative conditions, including chronic lymphocytic leukaemia and multiple myeloma. In addition to disease-causing mutations, genetic polymorphisms have been described for many complement components. Typical symptoms of the disease, and less common ones Recurrent infections Patients with inherited complement defects have an increased susceptibility to pyogenic infections. Properdin deficiency and defects in the components of the terminal lytic pathway are particularly associated with an increased susceptibility to neisserial infections, indicating the importance of the cytolytic property of the terminal membrane attack complex in host defence against Neisseria. Aetiology of the disease Genetic defects are described for nearly all the components of the complement system. Most of the defects in the classical complement pathway are inherited as autosomal recessive traits. Natural history and complications of the disease Natural history of infections in complement disorders, and their complications the most common presentation of patients with complement deficiencies is an increased susceptibility to recurrent infections by encapsulated bacteria, particularly Neisseria meningitides (Table 299. Homozygous C3 deficiency is also associated with increased susceptibility to Streptococcus pneumoniae and Haemophilus influenza sino-pulmonary infections and meningitis. While the majority of the infections occur in childhood, there is a reduction in frequency and severity of infections as the adaptive immune response matures. Bridge between innate and adaptive Complement antibody responses Enhance immunological memory Waste disposal Clearance of immune complexes and apoptotic cells C1q Covalently bound fragments of C3 C3b and C4b C3 receptors on B-cells C3 receptors on antigen-presenting cells of these components in clearing immune complexes and apoptotic debris. Deficiency of C1-inhibitor leads to inappropriate generation of bradykinin, with resultant increased vascular permeability. Patients with C1-complex or C4 deficiency present early in life, and both sexes may be equally affected. Factor H deficiency is also associated with membranoproliferative glomerulonephritis or dense deposition disease, predominantly in children. Demographics of the disease Defects and deficiencies of complement components are rare, but are being increasingly recognized and reported.
Purchase 20 mg vivanza free shipping
There may also be convergent downward gaze (the patient looks at the tip of their nose) impotence bicycle seat order generic vivanza from india. Progressive deterioration of the conscious level points to a growing haematoma, and sudden posturing and coma indicate bleeding into the lateral or third ventricle. Primary prevention All patients should have their cardiovascular risk assessed on a regular basis. Dietary measures should be used for all patients, and pharmacological therapies added as needed. Niacin, fibrates, and statins can all be used, although statins have been shown to be most effective. Diabetes High-vascular-risk individuals should be screened for diabetes, and treatment instigated accordingly. Antiplatelets are no longer considered adequate for prevention of cardioembolic stroke. There is strong evidence that dose-adjusted warfarin reduces the risk of stroke occurrence by approximately two-thirds, with only a slight increase in bleeding risk. The most common reasons for not prescribing warfarin are a high perceived risk of bleeding, and difficulties maintaining an international normalized ratio in the therapeutic range. Large clinical trials have demonstrated that these agents have effects that are broadly similar to those of warfarin, with a consistent reduction in intracranial haemorrhage risk. Their key advantage is their fixed dosing regimen with no requirement for anticoagulation monitoring. However, they are contraindicated in patients with a creatinine clearance less than 15 ml/min, and the current absence of an established antidote or rapid-reversal agent is considered a disadvantage. Other relevant codes G45 Transient ischaemic attack, including transient global amnesia I69 Sequelae of cerebrovascular disease Z82. Following this, lifestyle modifications and medical therapies should be instigated as appropriate. Dietary measures associated with stroke risk reduction include reduced total fat and cholesterol intake; increased consumption of fruits, vegetables, and fish oils; and reduced salt intake. Alcohol should be taken in moderation, with the weekly intake not exceeding 14 units per week. Exercise has a significant association with reduction in relative stroke risk, and the effect is even greater with strenuous activity. Patients should therefore be encouraged to take at least 30 minutes of exercise at least five times per week, or whatever they can achieve if they have limited mobility. Anticoagulant therapy Outside the context of atrial fibrillation, anticoagulation is also recommended as primary prevention for various other patients who are at high risk of cardioembolic stroke. This includes patients who are at high risk of thromboembolism following acute myocardial infarction, particularly a large anterior myocardial infarction; patients with left ventricular aneurysm or thrombus; and patients with paroxysmal tachyarrhythmias, chronic heart failure, or a history of thromboembolic events. Anticoagulation is also indicated for patients with mechanical prosthetic heart valves or rheumatic mitral valve disease. Hypertension this is the most common risk factor for stroke, and is extremely treatable. Adults over 40, and those with other vascular risk factors, should therefore be screened regularly for raised blood pressure. A clinic systolic blood pressure of >180 mm Hg or higher or clinic diastolic blood pressure of >110 mm Hg indicates severe hypertension. Antihypertensive drug treatment should be offered to all people aged under 80 who have Stage 1 hypertension and target organ damage, established cardiovascular disease, renal disease, diabetes, or a 10-year cardiovascular risk equivalent to 20% or greater and to people of any age with Stage 2 or severe hypertension. Current treatment targets are a clinic blood pressure <140/90 mm Hg in people aged under 80, and <150/90 mm Hg in people aged 80 and over. Blood-pressure variability may be as important as average levels in predisposing to stroke risk, and further research is needed in this area. Antiplatelet agents Antiplatelet agents provide no net benefit in the primary prevention of stroke, although they are widely accepted for secondary prevention. Secondary prevention While primary prevention of stroke is essential, it can be difficult to apply, as the population at risk is ill defined. Effective secondary prevention has the potential to reduce stroke risk by a half to two-thirds. The preventative strategies for long-term stroke prevention can be classified into three main categories: lifestyle modifications, medical therapies, and surgical intervention for carotid disease. Lifestyle modifications All patients should be educated regarding the same lifestyle modifications as recommended for primary prevention. Dyslipidaemia Although hypercholesterolaemia is a weaker risk factor for stroke than for heart disease, trials have shown a clear positive effect of cholesterol-lowering therapy on the incidence of ischaemic stroke. Long-term dual antiplatelet therapy with aspirin and clopidogrel is not routinely used for stroke prevention. While prolonged use is associated with a reduction in ischaemic stroke, this is offset by an increased risk of major bleeding. There is some evidence for shortterm use in those with significant symptomatic carotid atherosclerotic disease which is not amenable to surgery, and those at high risk of subsequent stroke. Anticoagulation should be initiated unless contraindicated in patients with cardioembolic stroke, after a suitable interval to avoid increasing the risk of early haemorrhagic transformation of cerebral infarcts. For patients aged 55 or over, and African or Caribbean patients of any age, antihypertensive treatment should typically be initiated with a long-acting dihydropyridine calcium channel blocker or a thiazide-like diuretic. Beta blockers are not routinely recommended as a first line antihypertensive therapy for stroke prevention unless there are associated comorbidities. Thereafter, treatment should be monitored frequently and increased as necessary to achieve the target blood pressure as quickly as is tolerated and safe in primary care. Patients who do not achieve the target blood pressure should be referred for a specialist opinion. If these criteria are satisfied, the diagnosis of stroke will be correct in 95% of cases. Clinical assessment should then seek to establish what the mechanism of stroke is and where the lesion is, with a focused history and examination. This is a clinical evaluation instrument, with documented validity and reliability, and is used to assess the severity of a stroke and its likely prognosis. It is highly accurate for identifying acute intra-cerebral haemorrhage, which is present within minutes of onset and seen as hyperattenuation, but Glycaemic control the general recommendation for the Hb A1c target level after a stroke is <7%, although a more stringent target of <6% may be considered in the early management of diabetes. More aggressive Hb A1c targets are not advised in the long-term management of glycaemic control, particularly in patients with high cardiovascular risk, as such targets are associated with increased mortality. The diagnosis of stroke is predominantly clinical and, once stroke is suspected, the initial assessment should first to seek to establish 772 Box 227. Changes indicative of acute ischaemia include focal hypoattenuation, which is very specific and predictive for irreversible ischaemia, and oedema without hypoattenuation, in which case the tissue is potentially salvageable. Typically, multiparametric sequences are obtained, including diffusion-weighted imaging, T1- and T2-weighted sequences, angiography, and fluid-attenuated inversion recovery. The advantage of this is that the extent of the lesion and the stroke mechanism can be clarified very early on. All stroke patients should be treated in a stroke unit, as there is strong evidence that this significantly reduces death, dependency, and the need for institutional care. The gold standard is to admit patients with stroke directly to a stroke unit and continue care there until discharge. Other diagnoses that should be considered aside from stroke While the diagnosis of acute ischaemic stroke is often straightforward, there are several important stroke mimics (see Box 227. These should be considered in the differential diagnosis, and care taken to exclude them as appropriate. Homeostasis Oxygen Patients should receive oxygen therapy if they are hypoxaemic (oxygen saturations <95%), as hypoxaemia can worsen cerebral ischaemia. However, the routine use of supplemental oxygen in patients who are not hypoxaemic is not currently recommended.
Generic vivanza 20 mg on-line
High intakes of red and processed meats have been linked with colorectal cancer erectile dysfunction beta blockers generic 20 mg vivanza amex, although this does not appear to be due to high intakes of protein per se. Athletes, keen to increase muscle mass, may consume 3 g of protein per kilogram of body weight from food and a further 1 g of protein per kilogram of body weight from supplements. These levels are not harmful in the short term, but it is unknown what impact, if any, they have on chronic diseases later in life. Protein intakes at this level result in increased oxidation of amino acids rather than increased synthesis of muscle, making them ineffective for the purpose used. People cite barriers such as disliking vegetables and fruit, not being confident in preparing vegetables, lack of time, and lack of availability. Poor diets, and types of fat An unsaturated fat is a fat or fatty acid in which there are one or more double bonds in the fatty acid chain. A fat molecule is monounsaturated if it contains one double bond, and polyunsaturated if it contains more than one double bond. Unsaturated fatty acids show geometric isomerism: the doubly bonded carbon atoms either have their attached hydrogens on the same side (cis) or have them on opposite sides (trans). Cis fatty acids are bent and cannot stack easily, so they have a lower melting point. The main sources are meat and dairy products; this fact perhaps explains why the traditional Northern European, American, and Australian diets are associated with a higher risk of coronary heart disease. They may promote inflammation, having been associated with increased levels of interleukin 6 and C-reactive protein. Diets high in deep-fried fast foods, manufactured baked goods, sweets, and savoury snack foods may be high in trans fats. In northern India, the consumption of vanaspati, made from vegetable oil and containing over 40% trans fats, can be as high as 20 g per person per day; its use is widespread in food manufacturing and street foods. In recent years, legislation, voluntary changes by food manufacturers, and better food labelling has reduced the amount of trans fats used in many countries. Ideally, saturated fats should make up less than 10% of total energy intake and should be replaced with monounsaturated fats such as rapeseed or olive oil. High-fat dairy produce should be replaced with low-fat dairy; consumption of fatty meats should be kept low; and it is recommended that people aim to eat between one and two portions of fish each week, with one of these being a portion of oily fish. Vitamin and mineral deficiencies Micronutrients (vitamins and minerals) are nutrients that are needed in small quantities throughout life. They are necessary for a wide range of processes, including immunity; brain and nervous system development; cognitive processes; skeletal and muscular growth and function; gastrointestinal function; and vision. Deficiencies lead to specific illnesses as well as an increased susceptibility to infection, delayed recovery, and reduced response to vaccination. Also important is the treatment of illnesses that result in nutrient deficiencies, such as diarrhoea, malaria, and worms. However, some 500 000 children become blind annually due to xerophthalmia (vitamin A deficiency), and half of pregnant women worldwide are anaemic (half due to iron deficiency), with anaemia being associated with 20% of maternal deaths. It has been proposed that this is due to the formation of mutagenic N-nitroso compounds during the preservation of the meat, and to haem-induced carcinogenesis. However, high consumption of preserved meat products has also been linked to a generally poorer diet containing low levels of fruit and vegetables, and high levels of refined carbohydrates and alcohol. High consumption of red meat has been strongly associated with colorectal cancer and less strongly associated with stomach cancer. Heavy metals from cookware may contaminate food, although it is not known how this impacts upon the burden of disease worldwide. Lead can leach from glazed earthenware into leben, a traditional Tunisian acidified milk drink, and can contaminate food when unheated spices are ground in earthenware pots in Mexico. Low vegetable and fruit consumption Low fruit and vegetable consumption is estimated to contribute to 2. This represents a minimum amount and is of particular importance for reducing the risks of developing cardiovascular disease, diabetes, and obesity, as well as avoiding micronutrient deficiencies. Attempts have been made to quantify the protective effects of increased fruit and vegetable intake on health: an increment of one serving per day is associated with a 6% reduction in ischaemic stroke and a 4% lower risk of fatal ischaemic heart disease. Fruits and vegetables are high in fibre, vitamins, phytonutrients, and potassium and low in energy. The health benefits from increased consumption of fruits and vegetables seem to be due to the foods as a whole rather than to individual nutrients. The term is also used to refer to cheap, highly processed, ready-to-eat or takeaway foods that are energy dense, high in fat and salt/sugar, and low in fibre and contain few micronutrients. In 95% of cases, it is due to the impact of an obesogenic lifestyle (overconsumption of energy and/or insufficient energy expenditure) on a variable background of genetic susceptibility. The remaining cases are caused by certain drugs, specific endocrine diseases, and monogenic syndromes (see Box 336. Obesity is most prevalent in Westernized countries, with up to one-third of adults being affected, but it is rapidly increasing in the developing world. Most countries are showing a steady rise in the prevalence of overweight and obesity. Socially, obesity is still associated with undesirable stigma, and this affects all aspects of life. Over the last 50 years, many surveys and reports have found that obese children perform less well and are more likely to be placed into remedial classes at school; obese adolescents, especially young overweight women, have lower acceptance rates for universities and receive less financial support from home; and obese adults are subjected to a higher percentages of prejudice in their employment and are often perceived as lacking in self-control and drive. Obesity has also been shown to impinge on personal relationships as well as marriage prospects. Cost of obesity to society the cost to society of obesity is huge, with it accounting for 6% of direct health expenditure in Europe. Obesity has also been implicated in several malignancies and in chronic renal failure. Psychiatric diseases associated with obesity include anxiety, depression, bipolar disease, and two distinct eating disorders: binge eating disorder and night-eating syndrome. With permission from the World Health Organization 1150 (A) Prevalence of overweight*, ages 18+, 2016 (age standardized estimate) Male Prevalence (%) <20. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. Smoking cessation Many smokers are reluctant to stop smoking for fear of weight gain. Weight gain mostly occurs within the first 2 months of smoke cessation and is due to increased energy intake, reduced metabolic rate, and reduced physical activity. Prevention strategies should be considered to lessen the possibility of weight gain after smoking cessation. Exercise should be recommended, as it reducing craving and withdrawal symptoms and halves weight gain. Greater benefits are seen when it is used as part of a cognitive behavioural smoking cessation programme. Bupropion, an atypical antidepressant, may be considered as a supplement to help patient minimize weight gain after smoking cessation, although the evidence of its effectiveness is not robust. Nicotine replacement therapy is commonly given as part of the cessation programme and can be very effective in limiting weight gain. However, on withdrawal of nicotine replacement, the patients can gain as much weight as those who were not on the replacement. Physical inactivity further increases this risk of dying early, with the combination of physical inactivity and obesity thought to account for 30% of all premature deaths worldwide. Pregnancy There is substantial evidence that obesity in pregnancy contribute to increased morbidity and mortality for both mothers and babies. Prior to pregnancy, obese women should be provided with information about the possible complications of obesity, and encouraged to lose weight before conception. Diet, exercise, and behavioural therapy again should comprise the first-line therapy. If pharmacological therapy is required, then metformin and orlistat can be safely used.
Purchase 20 mg vivanza with amex
Conditions which increase the risk of other forms of aspergillus disease include preexisting structural lung disease (bronchiectasis/previous tuberculosis) leading to a chronic necrotizing aspergillosis erectile dysfunction treatment home cheap 20 mg vivanza with visa, and/or aspergilloma. Aspergillus infection Definition of aspergillosis Aspergillosis is classically divided into invasive, saprophytic, and allergic disease. Invasive aspergillosis typically enters via the respiratory tract, sinuses, or skin, and can reach other tissues via direct extension or haematogenous spread. Microbiological evidence (direct/indirect tests, not meeting proven diagnostic criteria) Natural history of aspergillosis, and complications of the disease Invasive aspergillosis is almost universally fatal if it is not identified and if appropriate treatment is not commenced early. The initial presentation is normally with pulmonary disease, which can progress to haemorrhagic infarction and necrotizing pneumonia. Recent improvements in survival have been due to alterations in the levels of immunosuppression used for transplantation, increased awareness of the disease, use of prophylaxis, and early empirical treatment. Approach to diagnosing aspergillosis There is a high index of suspicion of aspergillosis in patients who are potentially at risk of the disease. Other diagnoses that should be considered aside from aspergillosis Other diagnoses that should be considered aside from aspergillosis are other causes of pneumonia, including bacterial community and 1086 nosocomial organisms. Pulmonary emboli and adult respiratory distress syndrome can also present with similar symptoms in critically ill patients. Typical symptoms of candidiasis, and less common symptoms Typical symptoms depend on the site of infection. In mucocutaneous disease, classical white plaques are seen on the hard palate; dysphagia and odynophagia are the hallmarks of oesophageal candidiasis. Invasive candidiasis normally presents as fever and/or sepsis syndrome with no obvious source. Some patients, particularly those who are neutropenic, can present with a disseminated papulonodular rash, which is a sign of disseminated disease. Other non-specific pulmonary signs include consolidation, infarcts, and cavitation. Increasing availability of galactomannan antigen testing provides a useful adjunct to diagnosis of invasive aspergillosis. False positives occur with concomitant use of piperacillin/tazobactam, and there is cross-reactivity with other fungal species. Identification of fungal elements in sputum, bronchoalveolar lavage fluid, and sinus aspirate can also indicate invasive aspergillus disease. Others at a higher risk include those who have had broad-spectrum antibiotics, or who have total parenteral nutrition, recent gastrointestinal surgery, haemodialysis, or indwelling vascular catheters. Natural history and complications of candidiasis Untreated candidaemia has a high mortality. Candidaemia which is not detected early can result in dissemination to other tissues, leading to endophthalmitis, endocarditis, bone and joint involvement, and meningitis. Chronic mucocutaneous candidiasis can be a sign of underlying immunosuppression, and should prompt further investigation. Depending on the cause, it does not normally affect mortality, but can cause considerable morbidity and distress to patients. Bronchoscopy is useful, not only to obtain samples for culture and histology, but also to look for typical macroscopic appearances of tracheobronchitis. Approach to diagnosing candidiasis There is a high index of suspicion of candidiasis in patients who are potentially at risk of this disease. Ophthalmoscopy should be performed in all patients with suspected or proven candidaemia. Prognosis of aspergillosis, and how to estimate it Invasive aspergillosis can rapidly be fatal. Improved outcomes at 6 weeks are reported in those not having myeloablative treatments, and those not requiring invasive ventilation or renal support. Other diagnoses that should be considered aside from candidiasis Other diagnoses that should be considered aside from candidiasis are other causes of fever in neutropenic patients, including bacteria (community and nosocomial organisms. Treatment of aspergillosis and its effectiveness First-line treatment for invasive aspergillosis is normally with voriconazole, which is superior to liposomal amphotericin B. Newer agents such as caspofungin and other echinocandins can be used as salvage therapy. Oral itraconazole has been used particularly in chronic cavitatory pulmonary aspergillosis. Aspergillomas do not respond to antifungal medication and may require surgical resection. Candida infection Definition of candidiasis Candidiasis can be divided into mucocutaneous disease, focal infection in specific organs, or fungaemia/invasive disease. Acceptable diagnostic alternatives to the gold-standard test for candidiasis Identification of Candida spp. Infection is normally due to invasion by these commensal organisms, rather than new infection. Other relevant investigations for candidiasis Histological findings consistent with candidiasis, such as hyphae and pseudohyphae in tissue samples, can help with diagnosis. However, there is no role at present for serological assays in the diagnosis of candidiasis, although tests are in development. Worse outcomes are associated with delayed commencement of therapy and inadequate antifungal regimens. Up to 40% of patients who survive the initial illness have significant neurological complications such as hydrocephalus, blindness, and cognitive impairment. Treatment of candidiasis and its effectiveness Empirical treatment for candidaemia/invasive candidiasis is with an echinocandin agent such as caspofungin. Fluconazole can be considered for non-neutropenic patients who are not critically ill and who are not considered to be at high risk for fluconazole resistance. Liposomal amphotericin B is an alternative in the case of intolerance or lack of availability of other treatments. Best practice is to remove all invasive venous catheters and to treat for a minimum of 14 days after blood culture clearance. Oral step down to fluconazole can be considered once the patient is clinically stable but should be managed in consultation with an infection specialist. For oesophageal candidiasis, oral fluconazole or amphotericin are the first choice, although echinocandins may be used. A single dose of fluconazole is normally sufficient for uncomplicated vaginal candidiasis. Approach to diagnosing cryptococcosis There is a high index of suspicion in patients who are potentially at risk of invasive cryptococcosis. Pulmonary cryptococcosis can easily be confused with pneumocystis pneumonia or other causes of pneumonia in the immunocompromised host. Skin manifestations of cryptococcosis can easily be mistaken for malignancy, molluscum contagiosum, or invasive yeast infections other than cryptococcosis, such as histoplasmosis or talaromycosis (penicilliosis). Cryptococcal infection Definition of cryptococcosis Cryptococcosis, also known as cryptococcus disease, is caused by dissemination of Cryptococcus spp. Serum tests are positive in >99% of patients with disseminated invasive cryptococcosis. The clinical disease pattern caused by these organisms is similar, and laboratories do not normally speciate further than Cryptococcus spp. When a lumbar puncture is performed, there is generally a marked increase in opening pressure with mild increase in protein, lymphocytosis (although the white-cell count can be normal), and low glucose ratio. Typical symptoms of cryptococcosis, and less common symptoms the primary route of infection is via inhalation and subsequent haematogenous dissemination. Focal neurological signs are a sign of late disease and should prompt rapid investigation and treatment. Pulmonary disease can vary from asymptomatic infection, to typical pneumonic symptoms, to disease patterns which can mimic pneumocystis pneumonia. Cutaneous manifestations of disseminated disease are relatively common, with pustular, nodular, umbilicated, or ulcerated lesions. Cryptococcal infection can also disseminate to other organs, including the long bones, the liver, the kidneys, and the spleen.
Purchase vivanza 20 mg line
Sputum production causes of erectile dysfunction in your 20s order vivanza 20 mg line, dyspnoea, haemoptysis, chest pain, and weight loss are variably reported; systemic feature become more prominent as the disease progresses. The clinical features may resemble those of concurrent chronic lung disease, and radiological changes may be equally nonspecific. Environmental contamination of clinical specimens yielding false positive results is common, and even repeatedly positive sputum culture may occur in the absence of progressive clinical or radiological features. As for Mycobacterium tuberculosis infection, macrophages are key to an effective host immune response. Resident macrophages phagocytose the invading mycobacteria, but then require stimulation with interferon gamma and other cytokines to activate intracellular killing mechanisms and eradicate the infection. Generally, medical therapy with combinations of antimicrobial agents is used and continued for at least 12 months after achieving negative sputum cultures. These patients should be observed closely with repeated sputum cultures and appropriate interval lung imaging. For patients with disease predominantly localized to one lung, there is a role for resectional surgery in the circumstances of inadequate response to drug therapy, infection with resistant organisms, or the development of significant local complications. Hepatosplenomegaly and lymphadenopathy are often evident on imaging, if not detectable on clinical examination. Laboratory tests reveal non-specific abnormalities, including anaemia, leucopaenia, and elevated alkaline phosphatase levels. The possibility of multiple concurrent infectious pathologies should always be remembered, as the affected patients are usually highly immunocompromised. Following the completion of treatment, secondary prophylaxis with either azithromycin or clarithromycin should be continued until adequate immune reconstitution has occurred. The typical clinical presentation of non-tender, unilateral lymphadenopathy with minimal systemic symptoms is largely indistinguishable from that of tuberculous lymphadenitis which is the main differential diagnosis. A definitive diagnosis may be made on mycobacterial culture, but results are delayed by several weeks and, frequently, no organism is cultured. Antimycobacterial chemotherapy is usually reserved for recurrent disease or cases where surgical excision is impossible or incomplete. It is most commonly due to Mycobacterium fortuitum, Mycobacterium abscessus, Mycobacterium chelonae, Mycobacterium marinum, and Mycobacterium ulcerans (Table 311. Deeper inoculation of mycobacteria may occur through accidental trauma or surgery and may result in tenosynovitis, arthritis, or osteomyelitis. Surgical debridement may be indicated for extensive disease, abscess formation, or circumstances where adequate drug therapy is difficult. Leprosy Definition and aetiology of leprosy Leprosy is a chronic granulomatous infection of the skin and peripheral nerves caused by the intracellular bacillus Mycobacterium leprae. It is characterized by anaesthetic skin lesions and peripheral neuropathy with nerve thickening. Left untreated, affected individuals may develop disfiguring and disabling deformities as a result of repeated trauma and secondary infection of anaesthetic areas. Following the introduction of multidrug treatment, the global prevalence of leprosy has fallen dramatically from an estimated 12 million registered cases in 1985 to fewer than 200 000 at the start of 2011. However, disease transmission continues to occur at substantial levels in some countries. Lesions are generally macular, poorly defined, and widely and symmetrically distributed. Histological examination demonstrates diffuse infiltration of the deeper dermis with foamy macrophages laden with bacilli but few granulomata. Moving from tuberculoid towards lepromatous disease, there is a reduction in the cellular immune response and a corresponding increase in the bacillary load and the number of skin lesions present. Histological examination reveals small granulomata that become more diffuse on progression towards lepromatous disease. The skin lesions of intermediate forms are highly variable and may be macular, papulonodular, plaque-like, or geographic. Persistent disability resulting from nerve damage adds to the global burden of disease and means that leprosy remains a leading cause of neurological disability in developing countries. Natural history of leprosy the means of transmission and natural history of Mycobacterium leprae infection are not completely understood. Individuals with lepromatous disease produce minute particles laden with bacilli that are presumed to be the vehicle of airborne person-to-person transmission. Bacilli are taken up via the upper respiratory tract mucosa and then demonstrate a specific tropism for Schwann cells and macrophages, to establish a slowly replicating intracellular infection. The emergence of mycobacterial antigens from infected cells induces a specific host immune response, which may result in a chronic inflammatory process affecting the skin and peripheral nerves. Nerve involvement in leprosy Peripheral nerve involvement in leprosy is extremely common. Sensory nerve dysfunction usually predominates, characterized by anaesthetic skin lesions. Motor and autonomic nerves may also be affected, resulting in weakness and reduced sweating, respectively. Affected nerves are usually thickened and palpable but, occasionally, significant nerve dysfunction occurs in the absence of obvious inflammation. Typical symptoms of leprosy, and less common symptoms the cardinal diagnostic features of leprosy are summarized in Box 311. The nature of the host cell-mediated immune response determines the clinical manifestations of leprosy. Eye involvement in leprosy Blindness is a relatively common complication of leprosy. Motor and sensory damage lead to impaired eye closure and reduced corneal sensation, predisposing to corneal ulceration, repeated trauma, and secondary cataract formation. Reactional states in leprosy the immune response in leprosy is dynamic, and spontaneous fluctuations can result in rapid alterations in clinical status. Type 1 (reversal) reactions follow spontaneous increases in T-cell reactivity and are characterized by inflammation of skin lesions and acute neuritis, often associated with rapid deterioration in nerve function. Inflammation must be rapidly controlled in order to prevent permanent nerve damage. Type 1 reactions occur in onethird of individuals with borderline disease and may be evident at presentation. Erythema nodosum leprosum (Type 2) reaction is an acute onset systemic disorder with multiple organ involvement that typically occurs in individuals with multibacillary disease. It arises as a result of extravascular deposition of immune complexes and consequent complement and neutrophil activation. Typical features include fever, painful skin nodules, uveitis, arthritis, and dactylitis. Approach to diagnosing leprosy In an endemic area, leprosy should be considered in any patient presenting with peripheral neuropathy or persistent skin lesions. Histological diagnosis is the gold-standard test, with the presence of neural inflammation distinguishing leprosy from other granulomatous disorders. Microscopy of slit-skin smears for bacilli is useful for identifying infectious patients and to monitor the response to treatment, but is of little value in diagnosis since it is negative in many patients with leprosy. Management of reactional states in leprosy Reactional states require urgent assessment and treatment in order to prevent permanent nerve dysfunction. Decompressive surgery is occasionally used to relieve mechanical obstruction caused by nerve oedema if nerve dysfunction persists despite medical treatment. Similarly, high-dose corticosteroids are initially used to treat erythema nodosum leprosum reactions but alternative agents such as thalidomide may be required to achieve sustained control. Reactions may continue to occur for years after successful antimicrobial therapy, and patients must be educated about the possibility and nature of reactions and the need to contact their physician immediately if symptoms arise. Hence, a detailed neurological assessment should be performed at each clinical encounter. If neuropathy occurs, prevention of secondary tissue damage is the primary objective. Patients should be educated to avoid activities that put neuropathic areas at risk, provided with appropriate orthotics, and advised to undertake regular self-examination. Secondarily infected tissues require prompt antibiotic treatment and possibly surgical debridement to minimize tissue damage.
Cheap vivanza 20 mg amex
The risk of bone fracture is slightly increased in patients with osteopenia and considerably increased in those with osteoporosis erectile dysfunction drugs at walgreens order 20 mg vivanza visa. It can also be used to screen for cancer in patients with dermatomyositis and polymyositis. It is also used to screen for pulmonary hypertension complicating diseases such as systemic sclerosis. It has genetic, constitutional, and environmental risk factors and presents a spectrum of clinical phenotypes and outcomes. Less common symptoms are mechanical locking and rapid progression of hip (less commonly, knee) symptoms. A variety of insults may trigger the need to repair, and often this slow but efficient process compensates for the insults, resulting in an anatomically remodelled but functioning asymptomatic joint. Risk factors vary according to joint site, and differ according to development and progression. In those that worsen, clinical progression is variable but is usually only slowly progressive and the transition from mild to severe typically takes many years. The pain is characteristically worse on usage/movement and is relieved by rest, typically being worst at the end of the day and best in the morning. Restricted activity and function often reflects pain severity but may be the presenting symptom, even in the absence of marked pain. The severity of pain and functional impairment are greatly influenced by psychosocial factors (anxiety, depression), daily activity requirements, and the presence of comorbidity. The exception is thumb-base involvement (first carpometacarpal joint and trapezioscaphoid joint), which sometimes progresses to require surgery. The presence of predominantly soft tissue rather than bony swelling and high inflammatory markers in the blood are more suggestive of inflammatory arthritis. The gait is typically an antalgic limp, with less time spent weight bearing on the arthritic side. Examination may reveal restricted flexion/extension, coarse crepitus, joint-line tenderness (with or without periarticular tenderness, especially over the upper medial tibia region), and small-to-moderate knee effusions. Apatite-associated destructive arthritis Apatite-associated destructive arthritis occurs in elderly women, is almost totally confined to the hips, shoulders (Milwaukee shoulder), and knees, and has a poor outcome. It causes intermittent pain and stiffness and is well localized to the involved joints; it commonly starts around menopause but becomes less symptomatic once nodes are fully developed. Typical end-stage deformity is lateral (ulnar/radial) deviation without instability. Generally, imaging and special investigations are not required, as they do not confirm the clinical diagnosis or alter decision-making. If there is diagnostic uncertainty in a patient with significant or progressive symptoms in a large joint, then imaging. National Guideline Centre (2014) Osteoarthritis: Care and management in adults, Clinical guideline 177. However, they have potential for serious toxicity from gut bleeding/perforation, renal impairment, cardiovascular safety, and drug interactions. Suitable patients who fail to respond to conservative measures should be referred for a surgical opinion. Evidence for their efficacy is based on uncontrolled, observational studies and several large cohort studies, but also on a wealth of expert and patient experience. Over 95% of joint replacements continue to function well into the second decade after surgery, and most provide lifelong, pain-free function. However, around one in five patients are not satisfied with their replacement, and a minority obtains little or no pain relief following this procedure. Importantly, referral should be made before there is prolonged and established functional limitation and severe pain, since these often compromise a good outcome from surgery. Steroid injection is therefore best reserved to obtain temporary control of moderate-to-severe pain, for example to enable a patient to participate in a special event such as a holiday or wedding. Reduction of adverse biomechanical measures Reduction of adverse biomechanical measures, such as via pacing of activities, use of appropriate footwear. It is characterized by inflammation of the synovium with consequent cartilage and bone destruction. They are generally associated with longstanding disease, being relatively rare at presentation. It typically follows a relapsing and remitting course, with patients experiencing less symptomatic periods followed by disease flares. Untreated, the presence of persistent joint synovial inflammation damages the underlying cartilage and bone resulting in joint deformity. Inflammation of the synovial lining of tendon sheaths can result in tendon damage and rupture. Septic arthritis is a serious complication with a high mortality, and diagnosis requires a high degree of clinical suspicion. It affects all ethnic groups, although an increased prevalence has been found in certain Native American populations. Cytokine and cell-contact-dependent interactions drive the persistence of inflammation, with fibroblasts playing a central role in leukocyte retention and survival. Rheumatoid nodules (present here over the right middle finger proximal interphalangeal joint) and fixed deformity (present here at the right little finger proximal interphalangeal joint) are unusual in early disease. This in turn may result in impingement of the spinal cord (cervical myelopathy), presenting a neurosurgical emergency. It appears to be on the decline, with the current incidence estimated at two to three patients per million per year. Typical features include fever, weight loss, cutaneous ulceration, and mononeuritis multiplex. Other diagnoses that should be considered Non-inflammatory conditions such as osteoarthritis can present with polyarthralgia (pain in five or more joints), but significant synovitis and protracted early morning stiffness are uncommon. Reactive arthritis is usually oligoarticular and asymmetric and often affects the large joints of the lower limbs. Episodes of arthritis are usually monoarticular (the great toe is most commonly affected) and begin suddenly, often overnight. Occasionally, gout can present in an oligo- or polyarticular manner and this can cause particular diagnostic confusion. Pseudogout is caused by the deposition of calcium pyrophosphate dihydrate crystals into joints. The presentation of pseudogout is similar to that of gout, although the knees and wrists are most commonly affected. The duration of the symptoms is important; their presence for at least 6 weeks is predictive of the development of persistent inflammation. Synovial fluid analysis Synovial fluid analysis should be carried out if the diagnosis is uncertain and fluid is available, particularly if a septic arthritis is suspected. A cell count on the fluid can identify if the process is inflammatory (>1000 white blood cells/mm3), and polarized microscopy allows the identification of crystals. The most commonly affected joints are the hips and the shoulders, although more distal joints such as the knees and ankles can be involved. Imaging Plain radiographs Plain radiographs of the hands and feet should usually be performed in patients with a symmetrical inflammatory arthritis. The latter usually occurs after several years of the disease; however erosions are occasionally evident within the first year of symptoms, and the initial radiographs serve as a baseline for comparison with future films. Ultrasound There is increasing interest in the ability of ultrasound to detect and quantify synovitis and to detect early erosive change not evident on plain radiographs. Ultrasound detection of synovitis in clinically uninvolved joints may be useful in identifying patients who present with joint pain and features suggestive of inflammation. Bone marrow oedema (which may precede erosive change) and early erosions can also be visualized.
Buy generic vivanza online
Simple advice includes wearing loose soft clothing impotence genetic buy generic vivanza, keeping cool, and avoiding alcohol because of its vasodilatory effects. In patients with uncontrolled disease, addition of oral H2 antihistamines or leukotriene-receptor antagonists have been advocated but evidence for their effectiveness is limited. Corticosteroids, while effective for acute disease control, should be avoided for long-term treatment because of their adverse effects. Low-salicylate or additive(pseudoallergen)-free diets have been advocated for chronic ordinary urticaria and may help a minority of individuals. In atypical cases, a skin biopsy can be helpful, especially to exclude urticarial vasculitis. Provocative testing can be carried out for inducible urticaria, for example the ice cube test for cold urticaria, and solar simulator exposure for solar urticaria. Other relevant investigations For inducible urticaria, no specific tests are required, with the exception of cold-urticaria, where underlying viral infections and coagulopathy should be excluded. Definition of the disease the immunobullous disorders are a group of diseases in which pathogenic autoantibodies bind to target antigens either in intraepidermal desmosomes (intercellular adhesion junctions) or in part of the basement membrane zone, resulting in loss of adhesion, and blister formation. The immunobullous disorders can be categorized by the level of blister formation (see Table 252. Aetiology of the disease the autoantibodies in patients with these disorders play a pathogenic role in inducing blister formation. The target antigens for many of these conditions have now been identified (see Table 252. Typical symptoms of the disease, and less common symptoms Pemphigus vulgaris and pemphigus foliaceus Pemphigus vulgaris usually presents with painful erosions of the oral mucosa. Over 50% of patients also have cutaneous involvement with widespread flaccid blisters and erosions. The nasal and genital mucosae, the conjunctivae, and the oesophagus may also be involved. Pemphigus foliaceus tends to be less severe than pemphigus vulgaris with a more insidious onset. Patients present with crusted, scaly lesions affecting the face, scalp, and upper trunk. It has an equal sex distribution and affects all races, but pemphigus vulgaris is commonest in those of Jewish ancestry. Bullous pemphigoid Bullous pemphigoid is a chronic, blistering disease affecting elderly people, usually with onset after the age of 60. Studies have found a higher frequency of neurological conditions such as multiple sclerosis in patients with bullous pemphigoid. Bullous pemphigoid Bullous pemphigoid often presents with a prodrome of pruritus (may last for months), followed by development of urticated papules and plaques, and then tense bullae, on either erythematous or normal skin. Blisters most frequently appear on the central abdomen and limbs, often favouring the flexures. The onset of linear IgA disease in adults may be insidious, but is usually abrupt. The trunk is always involved, but the limbs, face, and scalp are also commonly affected. All patients have an underlying gluten-sensitive enteropathy, but this may be asymptomatic. This is related to disease severity, dose of prednisolone used for treatment, and comorbidities. Bullous pemphigoid is a chronic, self-limiting disease with exacerbations and remissions. There is also an increased mortality rate in elderly patients, probably related to side effects from steroids and immunosuppressive agents. In contrast, dermatitis herpetiformis is usually a lifelong condition and spontaneous remissions are rare (up to 10%). In all these disorders, possible complications of cutaneous blistering may occur, such as secondary bacterial infections and scarring. Oral involvement can lead to severe pain and subsequent restriction of dietary intake and poor oral hygiene. A sample of perilesional, uninvolved skin should also be taken for direct immunofluorescence to look for deposition of immunoglobulins/complement. Acceptable diagnostic alternatives to the gold standard Indirect immunofluorescence is performed on serum or blister fluid and detects circulating immunoglobulins/complement. If a skin biopsy is not appropriate in a particular patient, this test will aid with diagnosis, depending on the pattern and type of immunoglobulin/complement deposition. Treatment and its effectiveness the general principle of treating immunobullous disease is to make the patient comfortable with the lowest dose of immunosuppression required. Most morbidity and mortality is from treatment rather than the disease and this has to be weighed up when making management decisions. In some patients, disease can be managed with superpotent topical steroids in combination with anti-inflammatory agents, such as a tetracycline, erythromycin, or nicotinamide. When control is established, steroids should be tapered very slowly to avoid relapse. In those patients with more resistant disease and who are unable to come off steroids, an additional immunosuppressive agent, such as azathioprine or mycophenolate mofetil, is added. Pemphigus is often more challenging to treat and therefore more frequently requires the addition of azathioprine or mycophenolate mofetil. Oral disease should be managed with good oral hygiene, topical antiseptics, and topical steroids (sprays/gels/mouthwashes). Treatment of dermatitis herpetiformis is usually with a combination of dapsone and a gluten-free diet. Pruritus is relieved within a couple of days of commencing dapsone, but the lesions will rapidly return if it is stopped. Haemolysis and methaemoglobinaemia are present in virtually all patients on dapsone, although these are usually tolerable. Patients on a strict gluten-free diet may be able to reduce their dapsone dose or stop it completely. Sulfapyridine is used as an alternative in those patients who are unable to tolerate dapsone. Approach to diagnosing the disease the clinician should take a history, including a detailed enquiry about the blisters, time course, any preceding itch or rash, previous episodes, and areas affected. A past medical history, a detailed drug history, a family history, and a systems enquiry including any gastrointestinal symptoms should be recorded (dermatitis herpetiformis). This should be followed by a thorough examination of the skin, hair, nails, and mucous membranes; look for blisters, excoriations, erosions, and evidence of scarring and/or secondary infection. Other diagnoses that should be considered the differential diagnosis for these conditions includes all causes of immunobullous disorders as well as other causes of blistering such as bullous impetigo and bullous erythema multiforme. Patients who have pemphigus but who only have oral involvement should have aphthous ulcers, herpes, mucous membrane pemphigoid, lichen planus, and erythema multiforme excluded. In the non-bullous phase of bullous pemphigoid, conditions such as eczema, scabies, and drug reactions should be considered. Bullous drug reactions, as well as drug-induced pemphigus/bullous pemphigoid should be considered. An incisional skin biopsy should be taken through an intact blister for histopathology. The level of the split (subcorneal, intra-epidermal or suprabasal) will help indicate possible diagnoses. The inflammatory infiltrate should 858 Any patient with a suspected immunobullous disorder should be referred to dermatology for specialist investigation and treatment, although long-term management is often with a multidisciplinary team. Other bullous disorders Mucous membrane pemphigoid Mucous membrane pemphigoid is a rare, chronic blistering disease which usually affects middle-aged or elderly people. It is predominantly a mucosal disease, most frequently affecting oral and conjunctival mucosa. Patients should be managed by a multidisciplinary team, including ophthalmologists and oral surgeons. Oral and topical corticosteroids in combination with azathioprine or mycophenolate mofetil are used.
Best purchase vivanza
After taking the initial step of considering vitamin deficiency impotence under 40 buy cheap vivanza 20 mg, it would be good, if possible, to confirm any deficiency with simple blood tests. Deficiencies in fat-soluble vitamins Vitamin A deficiency Most people associate vitamin A deficiency with night blindness. However, less severe depletion leading to increased vulnerability to gastrointestinal and respiratory infections and measles is common, with good evidence that oral vitamin A supplementation can reduce mortality by around 50%. Vitamin D deficiency Severe vitamin D deficiency leads to osteomalacia in adults, who may present with fractures but more commonly suffer from pelvic bone pain, muscle aches, and general weakness. Many cells within the body exhibit vitamin D receptors and hence there must be many functions of this vitamin that are still poorly understood. At least 16 types of cancer, including breast, colon, ovary, and prostate cancer, have been linked to vitamin D deficiency due to poor sunlight exposure. Deficiency occurs as a result of overt fat malabsorption and malnutrition, chronic kidney disease, or poor sunlight exposure. Modern life at high latitudes may not provide enough skin exposure to sunlight to permit full functional levels. Deficiency due to malabsorption can lead to neuropathy, myopathy, and compromised immunity. Other diagnoses that should be considered the differential diagnoses of the many vitamin deficiency syndromes are extremely broad and overlap with each other, as the associated symptoms and signs are generally fairly non-specific. Vitamin K deficiency Deficiency in vitamin K is unusual, as this vitamin is produced by gut flora. Overdosage can lead to difficulty in achieving therapeutic effectiveness with warfarin. Treatment and its effectiveness Vitamin deficiencies should be treated in the wider context of dealing with malnutrition. General principles include ensuring generous micronutrient and vitamin supplementation during early feeding while avoiding excess provision of micronutrients that might encourage microbial growth or increase free radical damage. Additional specific vitamin supplements should be given to patients with overt deficiency states. Giving single vitamin supplements to malnourished individuals can pose potential problems, both from direct toxicity of the vitamin itself. A prime example of Acceptable diagnostic alternatives to the gold standard Acceptable diagnostic alternatives to the gold-standard tests for vitamin deficiency are shown in Table 333. Other relevant investigations Other relevant investigations for vitamin deficiency are shown in Table 333. We would therefore recommend that, since there are only limited means of determining which vitamin levels are compromised, a balanced preparation of all vitamins and micronutrients should be administered in suspected cases of deficiency. Care should be taken when prescribing, however, as some oral multivitamin preparations lack some vitamins and trace elements and, currently, there are no complete liquid vitamin preparations. Some specific examples of patients for whom supplementation is essential are patients at risk of refeeding syndrome, patients suffering with alcoholic liver disease, patients who are elderly, and patients with non-healing wounds; in these cases, vitamin B1 (thiamine) and multivitamin supplements should be provided. In general, total provision should be both balanced and supra normal in order to meet normal maintenance needs, possible raised demands of illness, and correction of depletion. Safe Upper Levels for Vitamins and Minerals: Report of the Expert Group on Vitamins and Minerals, 2003. The stress response is characterized by activation of the sympathetic nervous system, with concomitant increases in circulating catecholamines and increased secretion of pituitary hormones. Adrenocorticotropic hormone stimulates the release of cortisol, promoting protein catabolism as well as lipolysis and gluconeogenesis. Additionally, injury and sepsis are associated with the release of cytokines such as tumour necrosis factor alpha, interleukin 1, and interleukin-6. The net effect of critical illness is an increased energy requirement coupled with a loss of total body protein. If critical illness is prolonged, the adaptive stress response may become maladaptive, in essence exerting a parasitic effect leaching away structural proteins, (typically around 17% of muscle mass is lost after about 3 weeks) and impairing host immunity. This may be manifested by diaphragmatic weakness and prolonged ventilator weaning; impaired wound healing; and an increased propensity to infection. Primarily, therapy should be directed towards the underlying illness, as nutritional support per se will not reverse the stress response and its sequelae. Nonetheless, adequate nutritional support in the early stages of critical illness may attenuate protein catabolism and its adverse effects. Burns, polytrauma, and septic shock are characterized by an enhanced hypermetabolic response and an increased energy expenditure, compared to other types of critical illness. As recovery occurs, the metabolic response to the illness converts from a catabolic to an anabolic phase, which is associated with an increase of fat and protein stores, and weight gain. Moreover, as activities such as spontaneous breathing and mobilization increase, energy expenditure increases further and should be accounted for when calculating nutritional requirements. While underfeeding is obviously undesirable, gross overfeeding can cause hyperglycaemia, hepatic steatosis, and immune dysfunction, as well as increase carbon dioxide production and contribute to respiratory failure. Indirect calorimetry devices allow non-invasive measurement of respiratory gas exchange, from which the energy expenditure can be calculated. Although indirect calorimetry can reduce incidences of overand underfeeding by providing accurate measurements of energy expenditure, there are a number of potential sources of error when using this technique. In critically ill patients, steady state conditions are easily disturbed by intercurrent illness such as seizures or sepsis; pain; anxiety; catecholamine use; altered ventilation; airway leaks; and increased inspired oxygen concentrations. Over the course of the day, measurements of energy expenditure may vary by as much as 23%. Predictive equations can also be utilized to estimate energy expenditure in the critically ill. Such equations are frequently inaccurate in critically ill patients, often overestimating caloric requirements. Amino acids released during protein catabolism are largely recycled, so the minimal daily protein requirement for adults is only about 20 g/day. During critical illness, this value varies, depending on the stage and severity of the illness, but is unlikely to be in excess of 80 g/day. Detecting malnutrition in the critically ill Malnutrition can be defined as a pathological state resulting from a relative or absolute deficiency in one or more essential nutrients. Malnutrition is associated with increased mortality and morbidity, and it is essential to screen all acutely ill patients for this condition. In Step 4, the scores obtained for the three steps are added together to provide a final score indicating the overall risk of malnutrition. This score then dictates the nutritional management plan, which is determined in Step 5. The majority of critically ill patients screened in this way have been shown to be at high risk of malnutrition and require nutritional support. Glutamine Glutamine is the most abundant non-essential amino acid in the body; it becomes conditionally dependent. Moreover, as a nucleotide precursor, it is intimately connected to protein synthesis. Consequently, glutamine is essential for preserving normal intestinal mucosal structure and function and may prevent translocation of harmful bacteria and bacterial products. There is moderate evidence that glutamine reduces infection rates and days of mechanical ventilation in critically ill patients but it seems to have minimal or no effect on length of intensive care stay or risk of death. Nutritional delivery in the critically ill Nutrition can be administered directly into the gastrointestinal tract, as enteral nutrition, or given intravenously, as parenteral nutrition. In critically ill patients, there is a paucity of evidence that clearly demonstrates the superiority of enteral nutrition over parenteral nutrition. Indeed, because of gastrointestinal intolerance, it is frequently difficult to administer the prescribed amount of feed by the enteral route. Moreover, the increased rates of infection that have been historically described as being associated with parenteral nutrition may actually have been related to the under-treatment of hyperglycaemia, or excess lipid administration.