Discount zocor 40mg on line
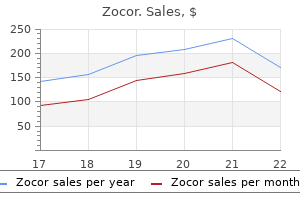
Indications for hospitalization include infants younger than 1 month of age and cholesterol ratio calculator nz generic zocor 10 mg, according to some, younger than 2 or even 6 months of age, toxic presentation or dehydration, intolerance to Antibiotic Selection If a urine Gram stain was obtained, the results may help guide initial empiric antibiotic choice while awaiting urine culture results. Uropathogen prevalence and resistance rates also vary by gender and visit setting as well as by previous exposure to antibiotics, so these factors must be considered when choosing empiric antibiotic therapy. Gram-positive bacterial uropathogens include Staphylococcus saprophyticus, Enterococcus, and, rarely, Staphylococcus aureus. Neonates and young infants should be covered for Enterococcus species when choosing empiric antibiotics because the incidence of infections with this uropathogen is higher in early infancy than at a later age (Beetz and Westenfelder, 2011). Enterococcus is frequently sensitive to ampicillin and first-generation cephalosporins. A combination of ampicillin and a third-generation cephalosporin or aminoglycoside is considered a safe empiric choice for neonates and young infants receiving parenteral therapy. Most uropathogens are susceptible to narrow-spectrum antibiotic agents such as first-generation cephalosporins and nitrofurantoin. Nitrofurantoin has also been associated with increased risk of hemolytic anemia in infants less than 3 months of age and should not be used in this population. Broad-spectrum antibiotics include broad-spectrum penicillins (antipseudomonal penicillins and -lactamase/-lactam inhibitor combination penicillins), macrolides, fluoroquinolones, second-, third-, or fourth-generation cephalosporins, lincosamides, and carbapenems. Although fluoroquinolones are highly effective against most uropathogens, bacterial resistance has increased as a result of widespread use. Fluoroquinolones should not be a first-line choice but should be reserved for those with suspected or proven resistant uropathogens such as Pseudomonas aeruginosa. In addition, the safety of quinolones in children has been questioned and is under investigation (Bradley et al. Routinely repeating a urine culture in children treated with an antibiotic based on previous urine culture susceptibilities is not necessary (Currie et al. In boys younger than 1 year of age, 18% develop a recurrent infection, usually within the following year. If the initial infection is in a boy more than 1 year of age, his risk of a reinfection increases to 32%. A similar trend is noted in girls less than and greater than 1 year of age who have a recurrence risk of 26% and 40%, respectively (Winberg et al. Infrequent voiding and urinary retention, or high pressures as may occur with dysfunctional voiding or obstructive uropathies, may compromise the local immunity of the bladder. This relates to the fact that the fecal flora frequently becomes resistant to the treatment antibiotic. In general, the risk of resistance appears to be about three times greater after treatment with antibiotics. The ideal antibiotic for prophylaxis would be effective against most uropathogens, be easily administered and tolerated without significant side effects, have high urinary concentrations and low serum concentrations, and make little impact on indigenous bacterial flora and bacterial resistance (Beetz and Westenfelder, 2011). The dosage is usually one-fourth the normal dose, and in toilet-trained children, it is routinely administered shortly before going to sleep in hopes of increasing the duration of antibiotic within the urinary bladder. Nitrofurantoin produces minimal effect on the fecal flora, and resistance rates have remained relatively low, making it an effective prophylactic antibiotic. This deficiency is found in about 10% of AfricanAmericans, Sardinians, non-Ashkenazi Jews, Greeks, Eti Turks, and Thais. Many unanswered questions exist regarding not only which patients benefit from prophylactic antibiotics but also the best therapeutic regimen. The ideal dosing and schedule, as well as the use of alternating antibiotics, remain to be defined. Patient noncompliance with a prescribed daily antibiotic is common (Daschner and Marget, 1975). After the acute inflammatory phase, the ultimate scar involves a loss of tissue that is reflected on radiographic imaging as thinning of the renal parenchyma over the calyces. It can be difficult or impossible to distinguish scar from regions of congenital dysplasia by radiographic imaging, although patients with a small kidney and diffusely decreased isotope uptake and decreased differential renal function are often considered to have renal dysplasia. Prompt antimicrobial treatment decreases the chance of permanent renal damage, as does the elimination of any subsequent episode of pyelonephritis (Oh et al. The use of anti-inflammatory agents to minimize renal injury and scar during the acute phase of pyelonephritis is under investigation (Huang et al. Anorectal and lower urinary tract function are interrelated, and constipation is often associated with bladder dysfunction. Reported frequency of constipation associated with pediatric bladder dysfunction ranges from 30% to 88% (Burgers et al. Detailed information regarding treatment of pediatric bladder and bowel dysfunction is reviewed in Chapters 30 and 36. In general, the initial conservative therapeutic measures for treating the child with bladder dysfunction include voiding behavior modification with timed voiding schedules and treatment of constipation, if present (Allen et al. In patients who fail conservative treatment, directed therapy is focused toward improving the specific cause of bladder dysfunction. Targeted interventions may include pharmacologic therapy, biofeedback, electrical stimulation therapy, surgery, clean intermittent catheterization, or a combination of these therapies (Malm-Buatsi et al. Symptoms are often vague and nonspecific and may include fever, abdominal or flank pain or mass, and more nonspecific symptoms including weight loss and failure to thrive. Imaging may demonstrate a masslike lesion with focal or diffuse renal involvement as well as perinephric extension (Cooper and Turner, 1997; Eastham et al. This may be mistaken for a malignancy and requires a high index of suspicion (Inouye et al. Technically, these operative cases can be extremely difficult because the process may extend beyond the kidney, distorting and destroying normal anatomy as it involves and encases surrounding structures, including the psoas muscle and, at times, even the great vessels (Loffroy et al. This seems to be true in particular if at birth the children had normal kidneys that were unaffected by significant renal dysplasia. This rate is consistent with that found in the prospective International Reflux Study in Children (Smellie et al. Two other studies with follow-up of 22 and 41 years demonstrated an increased prevalence of hypertension of 29% and 35%, respectively, in patients with scars, suggesting that scars are a risk factor for the development of hypertension (Bailey et al. It has also been demonstrated that during first pregnancies, hypertension was significantly more common in women with severe renal scarring (Martinell et al. Children with significant bilateral renal scars or reduction of renal function warrant long-term follow-up for assessment of hypertension, renal function, and proteinuria. A historical cohort study demonstrated that with long-term follow-up 140 of 18,592 (0. In one neonatal intensive care unit, funguria increased 10-fold throughout a 10-year period (Kossoff et al. Predisposing factors in children include antibiotic use, prematurity, intravenous and umbilical artery catheterization, parental nutrition, and an immunocompromised state (Keller et al. The urinary tract may serve as a portal of entry and as a site of disseminated fungal infection. In children with disseminated candidiasis, the kidney is the most commonly involved organ (Keller et al. It is important to recognize the infections caused by Torulopsis glabrata because these are commonly resistant to fluconazole (Kauffman et al. Fungal bezoars may also form in the renal pelvis and potentially create urinary obstruction in these children (Bartone et al. For this reason, renal ultrasound may be beneficial in evaluating these patients, especially if the funguria is persistent. Urinary alkalization and oral antifungal therapy may occasionally dissolve some fungal balls, but if the child is suffering from renal obstruction, percutaneous or surgical removal of these fungus balls is necessary. Percutaneous drainage may also be needed so that local antifungal therapy can be administered. In these individuals, local and systemic amphotericin B and/or oral fluconazole may be useful for treatment. If the fungal balls are shown to persist, endoscopic or open surgical removal may be necessary. The timing of treatment of asymptomatic funguria that are related to indwelling urethral catheters continues to be debated. In individuals with funguria secondary to these foreign bodies, progression to disseminated candidemia is rare (Kauffman et al. Stopping antibiotic therapy, changing or removing urethral catheters, and urinary alkalinization may be helpful in some cases, but these do not always clear the fungus from the urine. Prospective studies with intravesical amphotericin B bladder irrigation and oral fluconazole show that both may clear the funguria (Gubbins et al.
Discount zocor 20mg otc
In more recent years cholesterol test chemist zocor 10mg free shipping, commercially available devices (such as the Peristeen transanal irrigation system or the cone-shaped enema tip) have gained some popularity because they provide a more streamlined and patient-friendly way to administer the enemas. The procedure reliably evacuates the descending and rectosigmoid colon in most patients with a variety of defecation disorders (Christensen and Krogh, 2010). Despite a high success rate and growing acceptance, use has been affected by costs and some difficulty with self-administration (Alhazmi et al. This option is a reasonable first step in potential surgical patients, because it may delay or avoid the need for more invasive interventions or provide evidence that regular washouts lead to improvement before committing to antegrade enemas. Favorable outcomes appear to decrease again after puberty (Christison-Lagay et al. This may reflect the impact of changes in body habitus associated with transferring issues in those with neurologic conditions, combined attempts at independence with less caregiver support, and compliance issues with the washout regimen. Just like any other catheterizing protocol, understanding and reinforcing information to the patient and her or his caregivers are essential. It cannot be overemphasized how important ongoing detailed counseling and continued support, pre- and postoperatively (ideally provided by a well-trained dedicated member of the team, such as a nurse practitioner), are to ensure adequate and continued motivation, without which the procedure is set for failure. Operative Technique Although preoperative bowel preparation may facilitate the initiation of postoperative enemas, an aggressive cleanout is not necessary for the purpose of performing the procedure. Appropriate prophylactic antibiotics are always administered perioperatively and may be adjusted based on any concurrent urinary tract reconstruction. In such cases (often spina bifida patients with prior abdominal incisions and ventriculoperitoneal shunts), a large incision is avoided. Because the tendency is to maintain the appendix in situ, this is achieved by wrapping it with the cecal wall, an adaptation that follows the principle of the Nissen fundoplication (Koyle et al. Other issues that may be considered include the presence, length, and quality of the appendix; need and timing of urinary tract reconstruction; patient age and potential intellectual capacity, as well as dexterity, ambulatory status, and body habitus. Patients with a neuropathic bowel and anorectal malformations seem to fare better than those with chronic idiopathic constipation (Curry et al. Nevertheless, with increasing experience, modest success rates appear to be improving (Curry et al. Age at operation is also important, with failures more commonly seen in younger patients irrespective of the diagnosis (Curry et al. Note location of cecum and appendix (arrow) close to the liver in a child with spinal dysraphism. The colon can also be sutured to the posterior aspect of the anterior abdominal wall to ensure that the catheterizable conduit is not lying free in the peritoneal cavity, preventing kinking and difficulties with catheterization. If the appendix is not suitable to be split or is absent, alternative options must be considered. Some advocate this option as the procedure of choice when the appendix is not available (Sugarman et al. Another option worthy of consideration is the use of either a cecostomy tube (C-tube or cecal button). Creation of access with a colon flap (A), tubularized and subsequently imbricated (B). Granulation tissue (black arrows) and leakage (white arrow) around cecostomy tube. The tube can also be placed open or under laparoscopic guidance at the time of concomitant appendicovesicostomy (Lorenzo et al. The decision between left or right access may be a difficult one and can be settled by temporarily placing a cecostomy or percutaneous colostomy tube. If equivalent or better on the right, then the in situ appendix is the simpler option. Enema Regimen Although protocols differ, the first enema is commonly administered via the indwelling catheter or percutaneously placed tube after the postoperative ileus resolves, followed by a progressive escalation titrated to the desired effect. Considering individual patient needs and variable response, there is much "trial and error" involved. One of the most important points, especially in the early weeks and months after surgery, is to advise patients not to expect immediate success, because early disappointment can lead to frustration and failure. In fact, many children may not achieve a steady state or a reliable enema routine for a period of up to 6 months (Curry et al. Patients may also experience a degree of rectal leakage within the first few hours after the washout, but this does not appear to be a long-term problem. Although the washout regimen is established outside the hospital, it is vital to maintain regular contact with the nurse specialist who helps manage the process. Enema protocols differ among centers, and patients and families frequently modify them to suit their own particular needs. Initially, daily washouts with 20 mL/kg of solution are encouraged, but once the patient is comfortable with the process and a routine has been established, they may attempt to decrease frequency to alternate days. The time of day that the enema is administered is patient dependent, although most families prefer to give the enema during the early evening hours, after dinner. This time is chosen to allow a sufficient interval to achieve the desired result before bedtime. Rarely, others learn that twice-daily cleanouts are necessary and adjust their frequency accordingly. Because patients have to sit on the toilet for a long time, buttock pressure sores may develop, a complication that can be minimized with the use of padded toilet seats. Although uncommon, and depending on the solution used, water intoxication and/or electrolyte abnormalities may occur (Hunter et al. Changes and experimentation should only be done under supervision to minimize this risk. Once a steady state is achieved, there is little benefit from dramatically interfering or modifying the regimen. Contrast enema study in a child with long-standing constipation demonstrating redundant colon without associated anatomic abnormalities or radiologic evidence of Hirschprung disease. This issue can lead to frustration, failure, and abandonment of the irrigations (Griffiths and Malone, 1995). In an attempt to rectify this problem, some have advocated placing the conduit in the left colon, rather than the cecum (Ellison et al. By doing so, the length of bowel that has to be washed through is reduced and theoretically so is the time taken for successful enema completion. Presence of a large amount of fecal material in the distal colon and rectum (white arrows). This patient became impacted while doing infrequent antegrade enemas through a cecostomy access (black arrow). Attempts at clearing this fecal load with antegrade flushes only led to abdominal pain, lack of tolerance, and poor response. Improvement was achieved with disimpaction and retrograde enemas followed by diligent, regular antegrade flushes to achieve complete washout. In the majority of patients, this is a transient phenomenon that subsides during the first 3 months. Warming the solution, lowering additive concentration, reducing the rate of the infusion, adding sodium chloride, or using an antispasmodic before the enema can be tried in these cases. These patients may require occasional retrograde cleanouts or be candidates for re-positioning the location of the access channel in the colon (cecum vs. This large national series reported an overall full and partial success rate of 79%, with complication rates that were lower than in earlier historical series. Standardized tools have been employed to reflect improvements in quality of life (Shankar et al. Nonvalidated questionnaires have shown high satisfaction rates, with a majority of respondents recommending the procedure to others with intractable defecation disorders (Hoekstra et al. Stomal complications and difficulty catheterizing the conduits remain the most important postoperative problems (Barqawi et al. This enables the patient to evacuate the colon at regular intervals, avoiding impaction and reducing fecal incontinence.
Buy discount zocor 40 mg line
A variety of solid renal masses commonly seen in children include congenital mesoblastic nephroma cholesterol urine test discount 5mg zocor free shipping, neuroblastoma, Wilms Tumor, clear cell sarcoma, rhabdoid tumors, solitary multilocular cyst, metanephric adenoma, renal cell carcinoma, and angiomyolipoma. A full description of individual presentations of each renal tumor, of their natural history and management is found in Chapter 53. A 6-year-old male patient presenting with abdominal pain, elevated erythrocyte sedimentation rate and C-reactive protein, and inability to stand erect. Dimercaptosuccinic acid renal scans (A and B) demonstrating areas of photopenia with preservation of the renal contour consistent with acute pyelonephritis. The patient on the left (A) demonstrates formation of a renal scar, which can be differentiated from the acute lesion because of loss of the renal contour. It is certainly better than sonography at detecting and quantifying stone burden, however, it has been shown that this increased accuracy is seldom clinically impactful (Passerotti et al. When performed, it is imperative to obtain adequately timed images to thoroughly visualize the urinary tract. Frequently, in the rush to evaluate trauma patients, postintravenous enhanced images are obtained during the "arterial phase" when only the renal cortex is enhanced. Although this provides information regarding renal cortical contusion or laceration, injuries to the renal collecting system or ureter may not be seen. A strict protocol should be followed to ensure accurate and reproducible results (Conway and Maizels, 1992; Majd, 1989; Shulkin et al. The region of background subtraction should be similarly tightly drawn, being careful to include regions adjacent to the kidney and within the confines of the body. Intravenous furosemide (1 mg/kg) is given when the dilated collecting system is determined to be maximally filled and not before. Differential renal function, washout curves, and washout half-times can then be computer-generated; however, additional features might be helpful in predicting natural history (Shalaby-Rana et al. Thus, management decisions should be made based on patient age, renal function, diuresis half-life, curve shape, and upright clearance. The clinician should be sure to review the actual drainage images, regions of interest used, and curves as any variation in technique can lead to misleading results. Reduction in renal blood flow as a result of increased intrapelvic pressure is suggested by the finding of cortical retention of tracer (akin to an obstructed nephrogram on an intravenous pyelogram). The importance of controlling for patient hydration is apparent in this diuresis renogram being used to evaluate hydronephrosis in a young child after bilateral pyeloplasties. Despite fluid resuscitation with 375 mL, only 30 mL of urine were drained through the urethral catheter. Cortical transit through both kidneys was observed to be poor, as well as drainage from both collecting systems. Diuresis-induced drainage half-lives were improved for both kidneys, on the left side. Furosemide is administered 30 minutes after administration of radiotracer with a diuresis half-life being calculated from the time when the tracer rather than when the furosemide is administered. After 30 minutes of diuresis, equal amounts of tracer has cleared from both collecting systems: 65% (right) and 64% (left). The dilated right collecting system appears to drain well initially but demonstrates a prolonged half-life on repeat renography at 2 years of age (B). Chapter 24 09/20/2007 10/08/2007 Pre- lasix Pediatric Urogenital Imaging 423 50% 50% A 01/25/2008 49% 51% B 04/14/2008 C 51. Ultrasound scan shows mild right hydronephrosis in a 7-year-old male patient with right upper quadrant pain. The test is performed by intravenous injection of 99mTc-pertechnetate followed by dynamic and static gamma images of the pelvis. Similar to renal scintigraphy, photon-deficient areas represent poor blood flow as in torsion, and photon-hyperdense areas can represent inflammation as in epididymitis. In experienced centers, this technique can be very sensitive and specific (up to 100%) and potentially perform better than sonography in the setting of the acute scrotum (Flores et al. However, its lack of availability, invasiveness, and radiation exposure limit its widespread adoption over sonography. Perhaps the most appropriate use is in cases that are equivocal by examination and sonography, but only if potentially testicle-saving surgery is not unreasonably delayed (Kodali et al. However, it lacks the anatomic resolution of the collecting system and urethra, still requires urethral catheterization, and is still a nonphysiologic measurement. A few minutes later, the patient developed right flank pain, and there was gradual accumulation of the tracer in the right kidney (rising second part of the curve) (A). The renal cortex is well preserved as cortico-medullary differentiation is present and there is no sonographic evidence of renal cortical cysts. The diuresis curve demonstrates no drainage, and instead, reflects continuous accumulation of tracer in the right collecting system. Radionuclide cystography examples of mild (A), moderate (B), and severe (C) vesicoureteral reflux. Simi S, Ballardin M, Casella M, et al: Is the genotoxic effect of magnetic resonance negligible Piscitelli A, Galiano R, Serrao F, et al: Which cystography in the diagnosis and grading of vesicoureteral reflux Polish Society of Pediatric Nephrology: [Polish Society of Pediatric Nephrology recommendations for the management of children with urinary tract infection], 2015.
Generic zocor 5mg with mastercard
Postnatally cholesterol levels uk normal range buy zocor online, a catheter will not pass into the bladder, and a narrowed penile urethra with a membrane at the level of the membranous/prostatic urethra can be seen on cystoscopy. Prenatal ultrasound scan demonstrating "keyhole" sign indicative of lower urinary tract obstruction. Transverse ultrasound image of the bladder demonstrating marked thickening of the urinary bladder after decompression and associated bilateral distal ureteral dilation. Equally, the neonatal team should be advised of the likely concentrating defect inherent with these disease processes that may be exacerbated with a postobstructive diuresis. A repeat ultrasound scan should be obtained to serve as a baseline for maximal decompression following intervention. Debate exists as to whether this disease represents a severe obstruction that occurs on the continuum very early prenatally. However, recently the utility of this approach has been challenged, although long-term outcome data are not available. Voiding cystourethrogram demonstrating a dilated posterior urethra consistent with the diagnosis of posterior urethral valves. The more lethal form occurs in association with microcolon-intestinal hypoperistalsis syndrome. Most children will require urinary diversion with vesicostomy or intermittent catheterization. Recommendations for Lower Urinary Tract Obstruction A baseline renal/bladder ultrasound scan should be performed and used as a guide after an interval of decompression. The period of recommended bladder decompression will vary depending on the timing of the serum creatinine nadir. Serial ultrasonography is used to follow involution of cyst and assure normalcy and expected compensatory hypertrophy in the contralateral kidney. Recommendations for Multicystic Dysplastic Kidney A postnatal renal/bladder ultrasound scan should be performed in the early postnatal period to confirm the prenatal findings. In the setting of a functional solitary kidney, blood pressure measurement, assessment of proteinuria, and the consideration of yearly ultrasonography should be pursued through puberty to monitor for hyperfiltration injury that may occur with compensatory hypertrophy. Of note, the consideration for serial imaging is not evidence based but in part designed to ensure consistent follow-up for this population that may be at increased risk for renal disease in adulthood. Complete involution of the affected cystic kidney should occur over this interval, and persistent cystic kidneys with a solid component may be considered for surgical removal. Duplication Anomalies/Ureterocele/Ectopic Ureter the prenatal identification of duplication anomalies typically occurs as a result of the obstruction of the upper pole moiety that follow the Meyer-Weigert rule. Dilation of the upper pole ureter can be seen and differentiated from the lower pole. A duplication anomaly should also be suspected in the setting of ureteral dilation that is greater than associated renal pelvis dilation. On occasion, prenatal ultrasonography may detect a cystic mass within the bladder that is more easily identified on postnatal bladder ultrasonography, which differentiates a ureterocele from an ectopic ureter. This may be difficult at times when the ureterocele opening is ectopic within the bladder neck (Chertin et al. Ureterocele disproportion is a rare condition in which a large ureterocele is identified on bladder ultrasonography with minimal upper urinary tract dilation (Share and Lebowitz, 1989). Postnatal ultrasonography should guide the clinician toward the correct diagnosis in most cases. A ureterocele can be differentiated from an ectopic ureter based on the thickness of the cystic wall within the bladder. Initial management may involve puncture of the ureterocele, but this approach is not absolute. However, recent practice patterns appear to support an elective role as first-line therapy despite the creation of reflux (Chertin et al. Furthermore, some centers have supported a "watchful waiting" approach (Direnna and Leonard, 2006). The primary objective for treatment of duplex systems with ureterocele or ectopic ureter should be directed at preservation of the lower pole moiety. In brief, the upper pole approach may involve nephron sparing or ablative methods, both of which have recently gained popularity with a minimally invasive approach (Mason et al. The decision with regard to preservation of the upper pole is left to the discretion of the physician, as neither practice is evidence based. Long-term data confirm that most patients with an ectopic ureter can be managed with upper tract surgery alone (De Caluwe et al. However, this does allow for appropriate identification to aid in prenatal counseling and more importantly afford the opportunity for patients to seek a center of excellence to discuss the anticipated postnatal course. The distinction between bladder and cloacal exstrophy has a profound impact on the natural history of the disease shared by caregivers and providers. Cystoscopic appearance of bladder outlet obstruction caused by ball-valving ureterocele. Prenatally, bladder exstrophy is hallmarked by a nonvisualized bladder, abnormal genitalia, protruding mass (exstrophic bladder) inferior to a low-lying umbilicus, and widened pubic diastasis and has been reported to be detected in 50% of patients with the diagnosis (Wiesel et al. As opposed to cloacal exstrophy, the vertebral spine, kidneys, and the remainder of fetal survey is expected to be normal (Gearhart et al. Bladder exstrophy represents a midline anterior wall defect that affects the bladder and genitalia but should allow for otherwise development free from major organ system dysfunction, as seen with cloacal exstrophy. A postnatal ultrasound scan should be performed shortly after birth with specific attention toward evaluation of the urinary bladder. Renal scintigraphy may play a role Recommendations for Bladder Exstrophy Postnatally, bladder exstrophy does not represent an emergent condition. In addition to the aforementioned prenatal findings for bladder exstrophy complex, the addition of omphalocele and/or renal, vertebral, or limb anomalies may be encountered (Robin et al. They found a persistent cloacal membrane in 3 of 22 patients and developed major and minor criteria for classifying the findings (Table 22. Decisions for surgical intervention will be dictated by the extent of organ system involvement. Although prenatal treatment appears safe for the mother and fetus, the long-term impact has not been well defined and the needless exposure to 7 of 8 patients may not be justified. Cloacal Malformation Cloacal malformation or persistent cloaca is rare and occurs 1 in 50,000 births. This condition only occurs in females and is a result of the arrest in development of the urorectal membrane and urogenital sinus that creates direct communication among the rectum, vagina, and urinary tract. One may also see a dilated vagina or uterus, and on occasion this may have a bifid character caused by a uterus didelphys. The proposed mechanism of urinary ascites is retrograde flow of urine through the uterus and fallopian tubes into the peritoneum, which may lead to oligohydramnios, but this will vary depending on the degree of gastrointestinal obstruction. Equally, an association with tracheo-esophageal fistula may be seen and should be considered in the presence of polyhydramnios. The delivery of patients with the potential diagnosis of cloacal malformation should be elective and inclusive of all necessary neonatal, pediatric surgical, and pediatric urologic care providers. The accuracy of prenatal imaging to diagnose this condition varies because of its rarity such that the clinician should have a heightened level of suspicion when the fetal ultrasound scan is suggestive of a persistent cloaca. Postnatal Treatment of Congenital Adrenal Hyperplasia Postnatally, the immediate concern for electrolyte imbalance should be raised. In parallel to electrolyte stabilization, a concerted effort should be made to obtain a final diagnosis, which includes measurement of serum 17-hydroxyprogesterone and genetic testing. As mentioned earlier, early prenatal diagnosis allows the ability for caregivers to consider pursuing consultation at centers of excellence that provide fetal surgical intervention. To assess the benefit of prenatal closure of myelomeningocele, a multicenter randomized trial comparing prenatal closure versus postnatal closure was published in 2011. The most significant complications included preterm labor and uterine dehiscence (Adzick et al. Specific to urology outcomes, prenatal closure did not improve urodynamic parameters or decrease the need for clean intermittent catheterization or urinary reconstruction (Clayton and Brock, 2018). It is divided into classical, which is subdivided into salt-wasting (75%) and simple virilizing (25%) variants, and nonclassical, which has more benign course of disease. The condition will clinically affect 1 of 8 in those potentially affected because males will not demonstrate ambiguity (Nimkarn et al.
Cheap zocor 5 mg with amex
Although the advent of endourology and minimally invasive surgery has played an unprecedented role in minimizing morbidity cholesterol medication and kidney disease generic zocor 10 mg free shipping, it has also introduced newly described and reported periprocedural complicating events. Training in urology has also witnessed another paradigm shift, from the era of classic surgical mentoring to the current use of simulators and virtual reality surgery. Learning curves of complex surgical procedures such as open radical prostatectomy once estimated to be around 100 to 1000 cases have dropped to 40 cases with robotic-assisted surgery. Surprisingly, complication rates have not followed the same trend, and some authors associate this with the increased number of young surgeons progressing through their learning curves. There has been a dramatic increase in the use of minimally invasive procedures in the surgical management of urologic disease. These include the wide range of modern endoscopic and endourologic procedures and the use of laparoscopic and robotic surgical techniques. As such, surgical training has also evolved with a dramatic decrease in the exposure to major open surgery in the average urologic training program. Today, major index and common urologic oncologic and reconstructive procedures are performed in a minimally invasive fashion. Although the new generation of surgeons are better trained in minimally invasive techniques, the principles for the treatment of major complications remains the same. Increased incidence of complications was associated with several factors, such as procedure complexity (laparoscopic partial nephrectomy and cystectomy), length of surgery greater than 4 hours, and serum creatinine greater than 1. Several studies have shown that complications increase up to ninefold with procedure complexity and decrease fourfold with surgeon experience. However, there is a unique set of complications related to pneumoperitoneum and access, for example. A high index of suspicion is necessary intraoperatively and postoperatively to detect and treat these complications in an expeditious and safe manner. Although technology has changed the actual performance of operations, it has also led to the development of minimally invasive means to treat surgical complications. These include interventional radiologic techniques and, in many instances, minimally invasive laparoscopic and/or robotic approaches to treat complications. Many recently graduated surgeons come to face challenging situations and complications that were not encountered during their training with an obvious lack of specific management guidelines. Robotic simulators of operative complications or animal models might come into play once again to bridge this gap in training. As expected, there is a wide array of physiologic, medical, and surgical complications associated with different urologic procedures. Complications are even more specific to laparoscopic and minimally invasive surgery, which is being increasingly utilized in urologic practice. Physiologic complications such as arrhythmias, more specifically bradycardia resulting from gas extension of the peritoneum, can occur. These physiologic effects are discussed elsewhere in this book in the chapters on laparoscopy. Positioning, access, vascular, urologic, bowel, and visceral complications can occur. As such, procedure-specific complications, especially those associated with endourologic procedures, are not covered here and are addressed elsewhere in this book in the chapters that specifically address each particular procedure. Hence, this chapter will focus on various general complications of common major urologic procedures. It will also attempt to propose strategies to deal with and more importantly to avoid different complex scenarios. The stratification of this system depends on the severity of the complication and the invasiveness of the intervention required to manage it. The utilization of the Clavien-Dindo grading scale has increased over the past several years in urologic practice from 21% in 2010 to 50% in 2012 (Mitrapoulos, 2017, Yoon et al. This system was not designed for urologic surgery, but its use has been validated, and it has proven to be simple, reproducible, and applicable to our specialty (Rassweiler et al. The Clavien-Dindo system is classically based on management of a complication rather than its severity or morbidity. It also does not differentiate between early and late postoperative complications or address intraoperative complication reporting, and it may not be suitable for pediatric urology. Despite this, it is the most commonly used tool and allows for objective reporting of postoperative complications. In fact, the interobserver agreement rate was reported to be as high as 89%, even in nebulous clinical scenarios when it was evaluated a few years after its early use (Clavien et al. In urology, this grading system has been the subject of procedurespecific assessments. Many groups have since evaluated the utility of the Clavien-Dindo grading system in different urologic procedures such as laparoscopic or open radical nephrectomy and robotic prostatectomy. The Clavien classification serves its purpose in evaluating outcomes in academic and teaching centers. Utilizing this scheme, as an instrument in outcomes, there is an 80% observed concordance in surgical outcomes among postgraduate trainees and attending urologists (Elkoushy et al. Requiring pharmacologic treatment with drugs other than such allowed for grade I complications. There are seven grades, and some subdivisions of some grades allow pooling of the rare and severe complications. In the future, similar to different treatment guidelines, surgeons may have to define procedural guidelines. This will include optimal operational performance including a standardization of all surgical steps and adverse occurrences that can be considered as surgical errors. This would encourage analysis of the individual performance of a surgeon according to intraobserver and interobserver perceived errors. It is evident that grading systems such as the Clavien system are only one correct and necessary step in this direction. Permanent neurologic impairment is very rare, as spontaneous recovery often results with minor positional trauma. For the sake of discussion, we describe common positional nerve injuries and intraoperative nerve injuries. Positional Nerve Injury Positioning injuries are usually the result of compression injury during prolonged operative times with or without adequate padding and support. Insufficient padding and cushioning of pressure points contribute greatly to neuromuscular injuries, especially in obese patients. The clinical presentation is in the immediate postoperative period affecting the area of sensory and motor supply of the damaged nerve. Sensory loss, paresthesias, or motor deficit results depending on the affected nerve territory. In the lithotomy and modified lithotomy positions, the posterior tibial nerve can be injured as a result of compression of the posterior knee against the stirrups, resulting in weak plantarflexion. This can be associated with sensory loss in the sole and lateral aspect of the foot and posterior calf paresthesia. The peroneal nerve can also can be compressed against the stirrups as it courses laterally around the fibular neck with resultant foot drop and foot eversion weakness. Excess traction of the legs and compression against stirrups are also associated with injuries to the pudendal nerve resulting in variable perineal sensory loss and rarely incontinence. The peroneal nerve is also at risk in the lateral position, as excess pressure on the dependent leg without adequate padding can be the mechanism of injury. Excessive pressure on the leg against the operative table results in ipsilateral foot drop. Although the obturator nerve is most at risk during pelvic surgery, positional injury to this nerve has been described with hyperflexion of the thigh at the hip joint in exaggerated lithotomy positions causing motor weakness in thigh adduction. Inadequate cushioning and padding is very often the reason for sciatic nerve injury.
Order 40 mg zocor mastercard
Continence can be achieved with appropriate reconstruction and the use of intermittent catheterization cholesterol deficiency generic zocor 40 mg overnight delivery. Despite the extensive malformations noted, many patients have lived fruitful lives. In our experience, the median age at which children are continent for urine is 11 years old (Maruf et al. The choice between a catheterizable urethra and an abdominal stoma depends on the adequacy of the urethra and bladder outlet, interest and dexterity of the child, and orthopedic status regarding the spine, hip joints, braces, and ambulation. A more recent evaluation of a large cohort of children with cloacal exstrophy (Suson et al. It must be stressed that although broad management strategies can be suggested, the management of patients with cloacal exstrophy must be individualized to maximize functional outcomes. The factor most likely to lead to long-term disability is the level of the neurologic defect. Early aggressive evaluation and management of the neurologic issues with long-term close follow-up to evaluate for signs of cord tethering are critical to make sure that function can be preserved (McLaughlin et al. When neurologic issues are minimal or absent, bowel pull-through and voided continence would be ideal. Using a six-point scoring system to determine bowel and bladder continence (6 = best; 0 = worst), they evaluated 12 patients who had been managed over time. They had 7 patients with a continence score of 1 (colostomy and incontinent bladder) and only 1 patient who had a score of 5 (enema program and a continent bladder), attesting to the difficulties presented with surgical reconstruction. If patients with terminal ileostomy were aggressively managed with hyperalimentation, growth characteristics in the two groups were very similar. As noted earlier, bowel reconstructive techniques have permitted most children to avoid the long-term debility associated with short gut syndrome. Attempts at phallic reconstruction in the past had minimal success because of the diminutive nature of the corpora in boys and the wide pubic separation. Modern reconstructive surgical techniques may allow some boys to have complete phallic reconstruction performed with forearm or other grafts. Fertility appears to be universally compromised in boys, but girls have normal fertility, and pregnancy has been reported. Girls have higher degrees of cervical prolapse when compared with their counterparts with bladder exstrophy. Baumgartner T, Jayman J, Friedlander D, et al: the role of pelvic and lower limb immobilization in classic bladder exstrophy: an institutional study of three mainstay techniques. Bolduc S, Capolicchio G, Upadhyay J, et al: the fate of the upper urinary tract in exstrophy, J Urol 168:2579, 2002. Caione P, Kapoza N, Lais A, et al: Female genito-urethroplasty and submucosal periurethral collagen injections as adjunctive procedures for continence in the exstrophy-epispadias complex, Br J Urol 71:350, 1993a. Caione P, Lais A, Dejenaro N, et al: Glutaraldehyde cross linked bovine collagen in the exstrophy-epispadias complex, J Urol 150:631, 1993b. Fishel-Bartal M, Perlman S, Messing B, et al: Early diagnosis of bladder exstrophy: quantitative assessment of a low-inserted umbilical cord, J Ultrasound Med 2017. Chandra S, Sharma A, Bharga S: Covered exstrophy with incomplete duplication of the bladder, Pediatr Surg Int 15:422, 1999. Chitrit Y, Zorn B, Filidori M, et al: Cloacal exstrophy in monozygotic twins detected through antenatal ultrasound scanning, J Clin Ultrasound 21:339, 1993. Gobet R, Weber D, Renzulli P, et al: Long-term follow up (37-69 years) of patients with bladder exstrophy treated with ureterosigmoidostomy: uronephrological outcome, J Pediatr Urol 5:190, 2009. Goyal A, Fishwick J, Hurrell R, et al: Antenatal diagnosis of bladder/cloacal exstrophy: challenges and possible solutions, J Pediatr Urol 8:140, 2012. Halachmi S, Farhat W, Konen O, et al: Pelvic floor magnetic resonance imaging after neonatal single stage reconstruction in male patients with classic bladder exstrophy, J Urol 170:1505, 2003. Hamada H, Pakano K, Shinah H, et al: New ultrasonographic criterion for the prenatal diagnosis of cloacal exstrophy: elephant trunk-like image, J Urol 162:2123, 1999. Honeck P, Kienle P, Huck N, et al: Adenocarcinoma in continent anal urinary diversion: is a sigma rectum pouch a surgical option after failed ureterosigmoidostomy Kasprenski M, Maruf M, Jayman J, et al: Penile disassembly in exstrophy: time to reevaluate Kasprenski M, Yang Z, Maruf M, et al: Terminal markers of urothelial differentiation: a comparison of newborn and delayed bladder exstrophy closures to controls, 2018b. Meizner I, Bar-Ziv J: In utero prenatal ultrasonic diagnosis of a rare case of cloacal exstrophy, J Clin Ultrasound 13:500, 1985. Mildenberger H, Lkuth D, Dziuba M: Embryology of bladder exstrophy, J Pediatr Surg 23:116, 1988. Mirk M, Calisti A, Feleni A: Prenatal sonographic diagnosis of bladder exstrophy, J Ultrasound Med 5:291, 1986. Lais A, Paolocci N, Ferro N, et al: Morphometric analysis of smooth muscle in the exstrophy-epispadias complex, J Urol 156:819, 1996. Lottmann H, Melin Y, Lombrail P, et al: Reconstruction of bladder exstrophy: retrospective study of 57 patients with evaluation of factors in favor of acquisition of continence, Ann Urol 32:233, 1998. Pettersson L, Tranberg J, Abrahamsson K, et al: Half century of follow up after ureterosigmoidostomy performed in early childhood, J Urol 189:1870, 2013. Qi L, Wang M, Yagnik G, et al: Candidate gene association study implicates p63 in the etiology of nonsyndromic bladder-exstrophy-epispadias complex, Birth Defects Res A Clin Mol Teratol 2013 (in press). In Operative surgery: paediatric surgery, ed 4, Edinburgh, 1989, Butterworths, p 620. Rosch W, Christl A, Strauss B, et al: Comparison of preoperative innervation pattern and post reconstructive urodynamics in the exstrophy-epispadias complex, Urol Int 59:6, 1997. Siffel C, Correa A, Amar E, et al: An epidemiologic study from the International Clearinghouse for Birth Defects Surveillance and Research, and an overview of the literature, Am J Med Genet C Semin Med Genet 157:321, 2011. Tourchi A, Jayman J, Zhaoyong F, et al: Multivariate analyses of the factors affecting success in cloacal exstrophy primary closure, 2017. Wittmeyer V, Aubry E, Liard-Zmuda A, et al: Quality of life in adults with bladder exstrophy-epispadias complex, J Urol 184:2389, 2010.
Generic zocor 10mg mastercard
With hypercalciuria cholesterol ratio hdl ldl order zocor us, salt restriction will reduce urinary calcium losses by promoting reabsorption of sodium and calcium. Avoiding excessive protein intake to reduce the acid load is also recommended in recurrent stone formers. A thiazide diuretic can be used in the normocalcemic hypercalciuric patient to increase distal tubular reabsorption of calcium. For primary hyperoxaluria, the goal of therapy is to decrease oxalate production, increase urine calcium oxalate solubility, and decrease crystal deposition in the kidney. Potassium citrate, orthophosphate, or magnesium citrate formulations are used to decrease urinary calcium oxalate supersaturation. In individuals with hypocitraturia, a diet rich in fruits and vegetables, and/or supplemental potassium citrate is recommended. Sodium citrate should be avoided because the excess salt may increase hypercalciuria. If stone formation continues despite high fluid intake and alkalinization of the urine, D-penicillamine or tiopronin can also be used. In hyperuricosuria, allopurinol, alkalinization of urine, and avoidance of protein excess are recommended. Struvite calculi often require surgical removal and prolonged treatment with antibiotics. For children who present with acute renal colic, analgesia and adequate hydration with appropriate monitoring of fluid and electrolyte status are the mainstays of therapy. Radiologic evaluation should be performed, and in the setting of urinary obstruction, infection, acute kidney injury, or incontrollable pain, urologic intervention may be needed. For small ureteral stones (< 10 mm), management with observation with or without medical expulsive therapy is recommended. The choice of intervention is typically guided by stone size, composition, and location. Complete removal is important in children as residual small fragments are associated with regrowth and adverse outcomes. Medical expulsive therapy with an -blocker has been successful in the management of small ureteral stones. Percutaneous nephrolithotomy is the recommended treatment for large renal pelvic or caliceal stones (>20 mm). Ureteroscopy is increasingly becoming a first-line procedure of choice, Urologic Aspects of Pediatric Nephrology 351 especially for distal ureteral stones greater than 10 mm. Open surgery is usually reserved for very young children with complex stones, children with orthopedic issues that limit positioning, or those who have failed primary therapy. Urolithiasis has a high rate of recurrence, especially if an underlying metabolic disorder exists. Prevention with appropriate medical therapy and high fluid intake should be encouraged to limit morbidity. The estimated prevalence of hypertension in children is much lower than the prevalence seen in the adult population; however, data suggests the increase in the prevalence in hypertension seen in the pediatric population in recent years is closely linked to increasing obesity rates in children (Din-Dzietham et al. Weight-related disorders such as hypertension are now increasingly common in pediatric patients and are likely to account for the rise in the prevalence of hypertension from 2. An accurate measurement of blood pressure is essential to the diagnosis of hypertension (National High Blood Pressure Education Program, 2004). Systolic blood pressure is defined by the first Korotkoff sound, with the disappearance of the Korotkoff sounds defining diastolic blood pressure. As accurate auscultatory measurement of blood pressure is often difficult in infants and young children, the use of automated (oscillometric) blood pressure measurement devices is now widespread; however it should be noted that pediatric normative blood pressure data is based on auscultatory and not oscillometric standards. A recent clinical practice guidelines for management of hypertension in children and adolescents (Flynn et al. A major focus of this report was improving the recognition of hypertension by simplifying the initial screening blood pressure table. The blood pressure classification scheme has also been revised to align the classification system for adolescents with the absolute blood pressure values used in adult blood pressures guidelines (Redwine et al. The term prehypertension has been abandoned and replaced with elevated blood pressures to be consistent with the adult guidelines. Staging of hypertension is useful in determining which children require more immediate attention for diagnostic evaluation and management. Echocardiograms are no longer recommended as part of the initial screening of patients with confirmed hypertension. However, baseline echocardiography is now recommended at the initiation of pharmacologic therapy for all patients regardless of the etiology of their hypertension. For patients with stage 1 hypertension or those with primary (essential) hypertension without end-organ damage, therapeutic lifestyle changes are the initial intervention of choice (Lurbe et al. However, like all behavioral interventions, the long-term success of therapeutic lifestyle changes requires engagement not only of the patient, but of family members as well. Pharmacologic therapy should be considered in patients with primary (essential) hypertension who do not have improvement in their blood pressure after a trial of therapeutic lifestyle changes, or in patients with stage 2 hypertension, evidence of end-organ damage, symptomatic hypertension, or secondary hypertension (Flynn and Daniels, 2006). Unlike adult hypertension guidelines, there are no data or evidence-based guidelines regarding which drug to select when initiating pharmacologic therapy. Rather than standardized approaches to pharmacologic therapy, most practitioners individualize therapy with the underlying renal, cardiac, or endocrine conditions guiding the choice of the initial agent. Adverse effects of each agent and available formulations need to be considered, because many standard adult hypertensive medications are not available in liquid formulations or are in fixed ratios that are not suitable for the pediatric population. Once therapy is initiated, blood pressure should be monitored closely, including laboratory monitoring, both for efficacy of the antihypertensive medication and for potential side effects. Based on data suggesting that end-organ damage is present in patients with blood pressures greater than the 90th percentile but less than the 95th end-organ damage from hypertension. Two other clinically relevant designations for severity of hypertension are important: (1) hypertensive emergency, when a patient has end-organ injury such as encephalopathy, pulmonary edema, or cerebral hemorrhage or clinical symptoms like blurred vision, headache, or nausea, which can be associated with severely elevated blood pressure; and (2) hypertensive urgency, when blood pressure is severely elevated without clear evidence of end-organ involvement or overt symptoms. It also should be recognized that not every child with elevated blood pressure readings in the office setting has true hypertension. Up to one-fourth of such patients have normal blood pressures outside of the office setting and are classified as having "white coat" hypertension. The causes of hypertension are classified as either primary (essential) or secondary when a specific etiology is identified. Historically, secondary causes of hypertension have been thought to predominate in the pediatric population (Vehaskari, 2009). In infants younger than 1 year of age, the majority of cases are caused by either coarctation of the aorta or renovascular disease. In school-age children, the dominant secondary causes of hypertension are renal parenchymal diseases including reflux nephropathy. Malignancy-associated hypertension, primarily with Wilms tumor and nephroblastoma, typically presents in infancy and early childhood, and pheochromocytoma is seen more frequently in the adolescent population. Secondary causes of hypertension should still be sought in adolescents, however, this population, much like adults, is far more likely to have primary (essential) hypertension. Although hypertension is becoming more common in children, the differential diagnosis of childhood hypertension is quite broad. Features from the history, the physical, the age of the patient, and even the blood pressure values themselves can narrow the diagnostic focus. A secondary cause for hypertension should always be sought in infants younger than 1 year of age, and secondary causes should also be investigated thoroughly in preadolescent children as renal disease is the most common secondary cause of hypertension in this age group. Ideally blood pressure measurements should be obtained in both upper extremities and in at least one lower extremity. The physical examination should focus on identifying signs of underlying disorders that are associated with hypertension. Although there is substantial data in the adult population regarding the sensitivity and specificity of these biomarkers, and although there are emerging pediatric data, these biomarkers have not yet entered widespread clinical use, and the application of the data from adult studies is challenging in the pediatric population. Common complications include hyponatremia caused by excessive free water retention, hypernatremia from sodium administration, hyperkalemia caused by reduction in glomerular filtration and tubular potassium secretion, anion gap metabolic acidosis secondary to impaired renal hydrogen ion excretion and concurrent impairment of bicarbonate reabsorption and regeneration, hyperphosphatemia caused by reduced renal excretion, and hypocalcemia secondary to increased serum phosphate and impaired vitamin D metabolism. However, there is a clear association between excessive fluid accumulation and adverse outcomes in the pediatric population. Fluid intake should therefore be limited to match output including insensible fluid loss with replacement of output. If patients are fluid overloaded, then urine output should not be replaced, and diuretics are likely indicated. Adequate calories should be provided that meet maintenance requirements and to limit or prevent excessive catabolism. Hemodialysis provides the most efficient and rapid correction of fluid and electrolyte disturbances; however hemodialysis can be poorly tolerated in patients with hemodynamic instability.
Zocor 5mg otc
Ileocecal Valve Use of the ileocecal valve as a continence mechanism began with Gilchrist et al cholesterol foods good cheap zocor 40 mg without a prescription. In general, a short segment of terminal ileum, whether imbricated or tailored, is used as an efferent limb. This segment should be kept as short and straight as possible to facilitate easy intermittent catheterization. Continence is based on the imbricated ileocecal valve, not the length of the efferent limb. The imbrication is usually secured with interrupted, permanent sutures, involving the very distal ileum and ileocecal valve, and the imbrication is carried onto the cecum. Besides the appendix, this continence mechanism is perhaps the simplest and has the shortest learning curve to achieve reliable results. Continence rates have been reported as high as 95% with preservation of normal upper tracts (Hensle and Ring, 1991; Kaefer et al. Initial incision may be made to one side to form a shorter limb for implantation in the bladder and a longer one to be brought through the abdominal wall. They noted a very low incidence of detrimental effect on gastrointestinal function in a select group of patients with neurogenic dysfunction. Urine from the reservoir and generated pressure is allowed to enter a sleeve of ileum around the catheterizable channel. Compression of the inner tube theoretically provides continence, and early experience was encouraging. Initial continence rates approached 75% and then 90% with a single revision (Benchekroun et al. Others have been unable to duplicate Continent Vesicostomy Yachia (1997) described creation of a bladder tube fashioned from a wide flap of the anterior bladder wall. An attempt to provide a continence mechanism was fashioned by weaving the bladder tube through the rectus muscle for compression and continence. Continence in their small, short-term series was reported to be 100%, but this has not been duplicated. A rectangular flap in continuity with the bladder is tubularized over a 14-Fr to 16-Fr catheter. The bladder is plicated around the proximal 3 cm of the tube using nonabsorbable suture to create a type of nipple similar to gastric fundoplication. Macedo and Srougi (2000) described a similar continence mechanism created at the time of initial augmentation. Their technique is potentially appealing for patients requiring augmentation and having no appendix because of the simplicity; however, continence is based on a type of nipple valve that historically has been difficult to keep fixed. Casale (1991) has described a form of continent vesicostomy in which the continence mechanism is based on a flap valve created from a tubularized strip of bladder mucosa. Parallel incisions 3 cm apart are made into the anterior bladder and used to create a long rectangular flap. The abdominal wall should be measured to ensure that the strip is long enough to reach the skin without tension. The muscle portion is left broad to come around without tension and provide good blood supply. The edges of this strip are mobilized until it can be tubularized along its entire length. It may be beneficial to mobilize only one edge over to the other side to avoid overlapping suture lines. Casale (1991) originally incised the mucosa transversely at the end of the intravesical strip to be tubularized; Rink et al. The bladder mucosa from either side of the channel is then mobilized and closed over the mucosal tube to create a flap valve. More extensive mobilization of the side opposite that mobilized for the inner tube allows closure without overlapping suture lines, which may help avoid fistula formation and incontinence. It does tend to stricture if not catheterized regularly-more so than other catheterizable channels (Cain et al. Stomal stenosis remains a significant problem for 45% in the experience at Indiana University (Cain et al. Skin flaps and avoidance of tension to reach the skin may minimize this risk but do not eliminate it. Advantages include avoidance of an intraperitoneal procedure and bowel anastomosis; the appendix can be reserved for use with enemas. It does use some bladder and decrease capacity, which may not be appropriate for many patients. Lower Urinary Tract Reconstruction in Children 711 however, new hydronephrosis was reported (Abd-El-Gawad et al. The incidence of complications after continent diversion will undoubtedly increase with longer follow-up. These patients will be subject to the same complications seen with bladder augmentation. All of those complications, including infection, hydronephrosis, calculi, spontaneous perforation, and tumor, have been reported after continent diversion in adults if not in children. Because more intestine is usually required in continent diversion than bladder augmentation, the incidence of complications may ultimately be higher than with simple augmentation. Already, serum changes of increased chloride, decreased bicarbonate, and acidosis have been noted in some patients after continent diversion (Allen et al. The most common complication in pediatric continent diversion thus far has been stomal stenosis. Stenosis occurs more commonly at the umbilicus with use of appendix compared with tapered ileal segments (Fichtner et al. Various skin flaps may be placed into the terminal end of the appendix or intestinal segment to lower the rate of stenosis, but they do not eliminate stenosis (Kajbafzadeh et al. This technique only allows for bladder drainage, either intermittent or continuous, depending on whether the drainage adaptor is in place (Lopes and Lorenzo, 2016). Although these buttons can be placed percutaneously under cystoscopic guidance as a primary approach, we have found it helpful to initially place a suprapubic tube to allow for an established tract. The button can then be placed with or without a guidewire in the outpatient setting. Results With Pediatric Continent Diversion the most challenging aspect of continent diversion in children remains construction of an efferent limb that provides reliable continence and easy catheterization (Ardelt et al. The appendix is simple to use, suitable for most children, and associated with very good continence rates. If the appendix is not present or is to be used for antegrade colonic enemas, tapered intestinal segments provide a nice alternative. Nipple valves are the most complex continence mechanism and therefore have a longer learning curve. Continence rates approaching 85% can be expected with stapled nipple valves (Benson and Olsson, 1998; Kaefer et al. With use of the other efferent limbs, continence rates above 90% and approaching 95% have been reported in children (Ardelt et al, 2012; Duckett and Snyder, 1986; Hensle and Ring, 1991; Kaefer et al. With proper patient selection and appropriately performed continent diversion, postoperative hydronephrosis in children is rare and is not increased when compared with conduit diversion (Stein et al. In cases of catheterization not being performed reliably, Transitional Care Considerations As children with spina bifida and other similar conditions age, the need for adult care of pediatric urologic problems has grown in concert. This patient care need has led to the emergence of a new field of urologist, the transitional urologist, the detail of which will be covered in greater degree elsewhere in this book. However, when considering transitional care associated with patients who have undergone lower urinary tract reconstruction, certain factors must be considered. The bladder is then closed with absorbable suture, incorporating the bladder tube with the initial sutures to prevent kinking. One study from Husmann (2017) draws attention to the various causes of morbidity and mortality in a contemporary population of patients after lower urinary tract reconstruction. In this report of 385 patients with a history of bladder augmentation, significant long-term complications include spontaneous bladder rupture in 3% of patients with rupture leading to death in 1 patient. Factors that contributed to bladder rupture include substance abuse, mental/physical deficits, and noncompliance with catheterization. In another report by Husmann from 2016, the author further Chapter 37 highlights the scrutiny needed in transition patients who have been augmented. Reporting on the same population of patients as the 2017 article, the study finds that 240 mL of saline bladder irrigation daily was highly effective in reducing bladder calculi in the postaugmented patient. Furthermore, the article draws attention to a population of 80 patients undergoing bladder augmentation and concomitant bladder neck procedures.