Purchase super p-force without a prescription
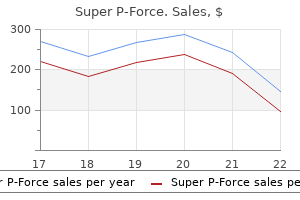
Accordingly erectile dysfunction pills uk buy super p-force american express, a more complex exponential equation that accounts for concurrent drug administration and drug elimination is required to describe the change in concentration. In neonates, who often have relatively slow rates of drug elimination, only a small fraction of drug is eliminated during the time of infusion of most drugs, and such adjustments can usually be omitted. Accordingly, a simpler and clinically applicable equation, such as Equation 12, may be used to estimate pharmacokinetic parameters. Armed with this insight, the clinician can make adjustments to drug therapy that achieve a desired level of drug exposure and ultimately drug effect for the patient. For aminoglycoside antibiotics, the ability to measure drug concentration levels is part of standard clinical analytical capability in most institutions so that information can be provided to the clinician to adjust dosage in a timely manner. The need for individual adjustment exists because of the variability among individual patients. This variability is due to the range of demographic, anatomic, physiologic, genetic, and biochemical differences among patients that ultimately impacts the pharmacokinetic parameters and influences the concentration profile of a drug at the site of action after a dose is administered. Population pharmacokinetics estimates the impact of these various differences on pharmacokinetic parameters to provide clinicians with a means to adjust dosage before starting therapy. By estimating the variability as a separate parameter, factors that contribute to variability can be measured and are referred to as patient covariates. Other typical covariates that can impact pharmacokinetic parameters are factors such as age, body weight or body mass index, genetic variants in drug-metabolizing enzymes, and presence of concomitant disease in a patient. These covariates can be particularly important for adjusting pediatric dosing requirements based on those recommended for adults. This occurs most often the liver (especially for drugs metabolized by cytochrome P450 3A4). When this occurs, the amount of parent drug reaching the systemic circulation is only a small fraction of the dose administered. After an intravenous dose of medication infused peripherally, drug enters either the inferior or superior vena caval circulation, returns to the heart, and enters the systemic circulation before perfusing the liver, which receives 25% of the cardiac output. Drugs that undergo almost complete hepatic or intestinal metabolism before reaching the systemic circulation are described as having a high hepatic or intestinal intrinsic clearance. Some drugs used in the care of newborns that exhibit moderate to significant firstpass presystemic clearance are midazolam,10 morphine,11 and propranolol. For drugs administered intermittently, peak and trough concentrations at steady state are the same after each dose. For drugs administered by continous infusion, serum concentrations will be constant. Constant serum concentrations, however, do not define equilibrium between compartments, because distribution between tissues and circulation may still be occurring. The time to reach steady state is dependent only on the elimination rate constant and therefore half-life. If a drug is administered repeatedly at a fixed dosing interval, the time to reach greater than 90% of steady state is four or more half-lives as shown in Table 19-1. During long-term drug treatment, dose adjustments should be made when concentrations are close to steady state and generally not more often than every three half-lives unless organ dysfunction is altering the half-life or Vd or concentration-related toxicity occurs. Chapter19-PrinciplesofPharmacokinetics 205 when dosing is adjusted linearly based on body weight. If a drug has only been studied in a population where the body weight changes are a fraction of the range that occur in the population at large, the impact of the covariate may not be accurately described for populations outside the body weight range that was studied. This occurs often when drugs are studied in relatively healthy adults and dosing is extrapolated to very young or very old patients. If the adjustment is a linear scaling based on weight or age, it can result in underdosing for young patients and overdosing for old patients. This equation can be rewritten in terms of volume of distribution and clearance by substituting for the elimination rate constant, K = Cl / Vd. Suppose we conduct a study with six children where drug concentrations are measured in the circulation over a 12-hour period after starting the infusion. The drug concentration rises in each subject to a steady-state concentration level, which differs among the six children. Using population pharmacokinetic modeling, an estimate of the average value for clearance and elimination rate constant can be determined that produces the population-average concentration profile for this group of children. Individual estimates of the two pharmacokinetic parameters Cl and Vd for each of the six subjects are determined along with the population variability for these parameters. The residual error is the difference between the measured concentrations and the populationaverage concentration profile. When the residual error is plotted against a covariate of interest, it should distribute randomly about the line of zero. If this difference plot instead shows a trend in the data that is not equally distributed about the zero line, it suggests that it might be important to incorporate the covariate into the model to reduce the model prediction residual error. As can be seen, when the residual error is plotted against body weight, the data are evenly distributed about the line for zero error, but the plot for creatinine clearance shows a decreasing trend with increasing creatinine clearance. Because the residual error plot shows a trend or "structure" versus the creatinine clearance, it indicates that creatinine clearance is likely an important covariate to include in the model. By plotting the individual subject parameter estimates against a covariate of interest (in this case drug clearance, because creatinine clearance is likely to be directly related to it), an understanding of the relationship between the covariate and model parameter emerges that indicates how it should be included in the model. Therefore the model would be updated to include creatinine clearance as a linear scale factor for drug clearance. Because these residual errors show a strong linear relationship that increases with increasing creatinine clearance, it strongly supports the need to incorporate creatinine clearance into themodelequations. This would represent the range of offset of the actual clearance values from the line. An advantage to using the population approach is that the sampling times and the number of samples for the different children in the trial does not have to be the same. In essence, because the population approach is fitting the relationship to all the data at the same time, if one subject is missing a sample point, the method uses information from the other samples to infer the likely shape of the curve for the individual. Another advantage is that the population approach identifies important variables that influence pharmacokinetics to guide dosing in a specific population. The covariate of creatinine clearance shows a linear relationship against the total clearance value. Any remaining residual variability that represents random noise in the concentration versus time relationship is given by epsilon. Note that the and define the variation in the parameter values between and within an individual. The actual parameter is assumed to have a mean value of zero for the overall population relationship with nonzero value for the variance. Basic principles of pharmacokinetics are built on the physiologic and pathologic changes encountered in developing and sick newborns. When combined with Monte Carlo simulation, these techniques describe ranges of drug concentrations that are likely to be achieved with specific dosages in specific neonatal populations. Using variations among patients that are known and those that are not, these techniques provide useful guidance to dosing and drug concentrations that are likely to be achieved in neonatal pharmacotherapy. When applied to drug concentrations measured during therapeutic drug monitoring, they help guide dosage adjustments to achieve therapeutic goals and avoid toxicity. Borchard U: Pharmacokinetics of beta-adrenoceptor blocking agents: clinical significance of hepatic and/or renal clearance. This set of relationships can then be used to adjust dosing for a patient based directly on the individual covariates and can improve dosing when it is not feasible to measure concentrations during therapy. It can also provide a means to understand the relationship between adults and children for drugs that have been studied in both groups. These averages and their variation can be used to estimate an anticipated range of outcomes, such as the serum concentration, using a mathematical approach termed Monte Carlo simulation. With this technique, a random combination of a variable, such as the average clearance, and its variation among patients are combined to calculate the concentration after a drug dose. This is then repeated hundreds to thousands of times to calculate a range of likely concentrations that will be produced by a particular dosage. The rapid developmental change in physiology among neonates lends itself to analysis by Monte Carlo simulations to understand the range of possible drug concentrations that are likely to be produced when pharmacokinetic parameters change with maturation or organ dysfunction. This allows prospective selection of optimal dosages based on defined patient covariates.
Syndromes
- The skin over the shins does not thicken, as it sometimes does in people who have Graves disease.
- Cushing syndrome
- Nausea
- Needing to move, restlessness
- Stopping smoking can help prevent tumors of the head and neck or lungs, which can lead to hoarseness.
- Loss of vision
- Testing of side vision (visual field examination)
Order super p-force mastercard
The World Health Organization strongly warns against the use of combination oral contraceptives (progesterone + estrogen) by breast-feeding mothers until the baby is 6 months old erectile dysfunction natural remedies at walmart buy super p-force 160 mg without prescription. Careful monitoring of the infant, including laboratory measurement of drug levels, can further reduce the risk of breast-feeding on these medications. These drugs target specific proteins, such as tumor necrosis factor, while leaving others untouched. However, several researchers have postulated that monoclonal antibody drugs might exhibit limited absorption via the immunoglobulin G-transporting neonatal Fc receptor that is expressed in intestinal cells of adults and fetuses. A small group of these medications antagonize the action of endothelial growth factor. Receptors for this hormone are expressed on the cells of the intestinal lining, leading to the potential for adverse effects without systemic absorption. Natalizumab is an unusually long-lasting antibody requiring around 24 weeks to reach a steady-state level in the maternal blood. A recent breast milk study of natalizumab demonstrated that, over the first 12 weeks of administration, drug levels in the milk rose to five times the level detected after the first injection. Data on the extended monitoring of this drug after 12 weeks have not been published, but the implication is that drug levels in the milk may continue to rise, possibly to the point of being hazardous. A brief breast-feeding interruption of 12 hours should suffice to limit exposure in the milk, even in the most extreme case. These drugs are designed to have potent local effects but minimal to no absorption into the plasma. However, significant drug levels are measurable following the use of high-potency topical steroids over a large body surface. A risk versus benefit assessment may be required if breast-feeding is to continue under these circumstances. Milk levels are typically in the picogram range due to the large molecular weight (16 to 27 kDa) of these drugs. The most conservative and reasonable approach is to withhold breast-feeding for 7 half-lives after the last dose is given. As with the tyrosine kinase inhibitors just discussed, breast-feeding cessation for 7 half-lives effectively eliminates the risk to the infant. If a combination of chemotherapeutic agents is used, the period of breast-feeding cessation should be based on the agent with the longest half-life. Both azathioprine and tacrolimus transfer into milk at very low levels, and postmarketing surveillance for these drugs has so far not identified any serious adverse effects or increase in infection rates among infants exposed through breast milk. Satisfactory studies have not been published for the remainder of the drugs in this class. There is rarely satisfactory literature published on the safety of an herb in breast-feeding women, and practically never on combination herbal products. Relevant information about the effectiveness of an herb is more likely to be available. The decision whether or not to take a supplement should include information about both risks and benefits. These substances are not radioactive themselves, but rather they block or absorb radiation in order to highlight different areas of the body. These products are specifically designed to target certain tissue compartments and do not leak into other areas. Iodinated and gadolinium-based agents in particular exhibit less than 1% excretion via breast milk and less than 1% oral bioavailability in the infant. The American College of Radiologists has issued guidelines stating that these products are compatible with breast-feeding without restriction. Live attenuated viral strains from vaccines have been detected in breast milk but none has been successfully cultured. If it is absolutely necessary, then the mother should be advised to avoid breast-feeding for 2 weeks after vaccination. At least 80% of those vaccinated develop neutralizing antibodies by 10 days and 99% develop them by 28 days. The tendency of a substance to cross the blood-brain barrier is highly correlated with its ability to cross the lactocyte barrier and appear in the milk. No reliable threshold of toxicity in infants has been established for any drug of abuse. However, the more relevant question of whether a woman who uses these drugs should breastfeed needs to be evaluated on a case-by-case basis. The physiologic and psychologic benefits of breast-feeding may still outweigh the detriments of incidental drug exposure. Issues of drug interactions, contaminants, and addiction all complicate this judgment. Infants may have positive results on drug screens for extended periods of time, even in the absence of observable effects. Sometimes, the radioisotope is used by itself, but more often it is attached to a "carrier" compound that helps target the organ of interest and speed up elimination of the radioactivity from the body. Each formulation will have two separate half-lives: the biologic half-life that is defined by how quickly the compound is eliminated from the body and the radioactive half-life that measures how quickly the radioactive atom decays into a more stable isotope. These two factors have no influence on each other, but both contribute to the effective reduction of radiation in the patient. The former is mitigated by breast-feeding cessation, and the latter by restrictions on close contact between mother and child. The Nuclear Regulatory Commission issues guidelines for various radiopharmaceuticals with the intent of delivering an effective dose of less than 1 mSv of radiation (1 mSv = 100 mrem) to the infant for each procedure. Very low doses of radioactive iodine tracers may be compatible with breast-feeding if the affected milk is discarded or stored for an appropriate period of time. Studies have demonstrated a linear relationship between smoking rates in the mother, nicotine levels in the milk, and urine cotinine levels in the breast-fed infant. Dopamine antagonists can function as galactagogues by encouraging the release of prolactin from the pituitary. The standard oral dose of 10 to 15 mg three times per day can be as much as tripled for maximum effect. Other problems include extrapyramidal symptoms, gastric cramping, and tardive dyskinesia. Some mothers also experience a rebound drop in milk production if they discontinue the drug without weaning slowly. Heroin may also transfer directly into breast milk alongside all of its metabolites. As with other opiates, tolerance follows from chronic use, and addicts may end up using extraordinarily large doses. Heavily dependent users should be advised against breast-feeding, and their infants should be transitioned to formula. Methadone is a potent and very long-acting opiate analgesic used primarily to prevent withdrawal in opiate addicts. Estimates vary significantly regarding the degree of cocaine contamination in the breast milk, ranging from 1% to 10% of the maternal dose. Breast milk is likely free of cocaine after 24 hours, but infants can become drug-screen-positive as a result of ingesting these metabolites. There are no high-quality human studies on the transfer of illicit hallucinogens into breast milk. The signs and symptoms of hallucinogen intoxication have not been described in patients whose sole exposure was through breast milk. Nonetheless, these drugs are all predicted to enter the milk avidly and mothers abusing these substances should not breast-feed. Although many of these plants do contain biologically active compounds, their efficacy in increasing milk production is doubtful. High-volume milk production depends on frequent and complete emptying of the ducts. This situation can usually be reversed by nondrug means, but some women will require a galactagogue to maintain adequate milk output.
Generic super p-force 160 mg visa
This canal is simultaneously being divided into right and left channels by the fusion of the enlarging superior and inferior endocardial cushions erectile dysfunction diabetes super p-force 160mg. The opening between right and left sides of the common atrium, now partially divided by the growing septum primum, is called the foramen (or osteum) primum. Soon the lower edges of the septum primum fuse with the endocardial cushions, and further growth of both the septum and the cushions closes the foramen primum. Before it closes completely, however, several perforations appear in the superior portion of the septum primum. Thus communication between the right and left atrial cavities is maintained during this complex morphogenetic process. Another septum (the septum secundum) begins to form at about the time the foramen secundum becomes well defined. Further growth produces a thick membrane, but the oval opening in this membrane persists as the foramen ovale. This arrangement of two parallel septa (septum primum and septum secundum) with offset holes (septum secundum and foramen ovale) produces a flap valve between the two atria, ensuring unidirectional flow of blood from right to left. Fusion of the endocardial cushions (composed of cardiac mesenchyme) forms the septum intermedium. This structure not only divides the atrioventricular canal into right and left portions but also acts as a central attachment point and reference center for several septation events, as already described. The cushion tissue of the septum intermedium contributes to the formation of the membranous portion of the interventricular septum, as well as to the development of the atrioventricular valves and the fibrous cardiac skeleton. Even though the heart is enlarging while septation proceeds, the dimensions in this central region around the septum intermedium remain constant. A significant enlargement in this region at this time could lead to congenital heart defects. Partitioning of the ventricle is accomplished primarily by fusion of trabeculae, which form a muscular interventricular septum. Ventricular septation is completed by formation of the membranous portion of the septum from an outgrowth of endocardial cushion tissue. This morphogenetic process occurs simultaneously with division of the proximal outflow area. Initially, no direct communication is present between the right atrium and the right ventricle. Remodeling activities in the inner curvature of the heart create this communication by mechanisms which are still obscure. The proximal portion of the outflow tract is subdivided into the conus and truncus regions, both of which are divided into left and right halves by ridges of endocardial cushion tissue called the conotruncal or bulbar ridges. Septation of the conus region results in the formation of an outflow segment for each ventricle, whereas in the truncus region distinct aortic and pulmonary valves develop. A portion of the conal septum extends down and attaches to the muscular interventricular septum, partially closing the interventricular foramen. Complete closure of the foramen is accomplished by downgrowth of cushion tissue from the septum intermedium. In the distal outflow tract (the aortic sac), a wedge of mesenchyme (the aorticopulmonary septum) develops between the fourth and sixth aortic arches. This mesenchyme (thought to be of neural crest origin78) grows downward and then penetrates and fuses with the conotruncal ridges. Blood cells are formed from those angioblasts remaining in the lumen, as well as by cell division and budding from the primitive endothelial lining. Growth and fusion of the isolated hollow blood islands result in the formation of tubes, and the tubes fuse to form long interconnected channels. Lateral buds from tubes and channels also may extend the developing vasculature into adjacent areas. This sequence, based on observations of sectioned embryos, constitutes the basic template for how vessels form. Little is known concerning how the intricate pattern of anastomosing vessels is established in the early embryo. Skeletal muscle forms from paraxial mesoderm, whereas cardiac muscle is a derivative of splanchnic mesoderm. It seems likely, however, that all mesenchyme, whether derived from mesoderm or from neural crest (as in head mesenchyme), has the potential to form vascular smooth muscle. E-H,Formationofaportion of a primitive vascular network by fusion of blood islands. Coelom Myotome Sclerotome and spread out deep to the embryonic skin, where they form the musculature. Various morphologic processes, including fusion, tangential splitting of layers, reorientation of muscle fibers, and formation of tendon intersections, are responsible for the final morphologic form of the named muscles. The musculature of the limb is also derived from the myotome portion of the somites. These myoblasts migrate into the elongating limb buds and arrange themselves into dorsal and ventral muscle masses, which later become subdivided into the definitive limb muscles. CardiacMuscle smooth muscles of the iris and the myoepithelial cells that surround sweat glands and mammary glands are thought to be of neural crest origin. SkeletalMuscle Cardiac muscle develops from splanchnic mesoderm adjacent to the pericardial or transverse portion of the intraembryonic coelom. Myocardial precursor cells undergo mass migration and do not fuse to form myotubes. Rather, the myoblasts differentiate as discrete cells, with closely applied end-to-end junctions, which persist as the adult intercalated disk. They form a layer around the endothelial tube of the heart, which eventually becomes the myocardial or muscular wall of the heart. SmoothMuscle Mesenchyme cells that are to develop into skeletal muscle elongate and lose their multiple processes. These myotubes start producing actin and myosin myofilaments, which increases girth. The skeletal muscles of the head and neck develop from paraxial mesoderm represented by somitomeres in the early embryo. Somites themselves are interesting structures-serially repeated paired blocks of condensed (closely packed) paraxial mesoderm cells. Approximately 44 pairs of somites eventually develop in humans, beginning between day 19 and day 21. Chondroblasts aggregate, condense, and begin to produce collagen fibers and ground substance. In the embryo, bone tissue is formed in either of two distinct ways, depending on the site and type of bone growth. The first is de novo bone formation, in which mesoderm cells (or, in the case of some skull bones, neural crest cells) first condense (pack) into sheets or membranes. Cells in these sheets then differentiate into osteoblasts, which secrete prebone or osteoid. Osteoid is the extracellular matrix onto which hydroxyapatite crystals (a unique calcium phosphate mineral) form. Once the mineral is present and integrated into the collagen of the matrix, the tissue is considered to be bone. This type of bone formation is called Chapter3-BasicEmbryology 35 intramembranous ossification because the osteogenesis occurs within these sheets or membranes of condensed mesenchyme. The second manner in which bone forms in the embryo is called endochondral ossification. As implied by the name, bone forms in this case only in sites where preexisting cartilage models are found. Rather, bone replaces the preexisting cartilage model in a sequence of steps, as follows. Cartilage cells hypertrophy and calcify in an area where bone is to form-that is, they become large and undergo metabolic changes, which lead to infiltration of the surrounding cartilage extracellular matrix with insoluble calcium salts. In this way, the cartilage cells become partitioned from their surroundings by an environment that is presumed to cut off their supply of oxygen and nutrients, and they die.
Order super p-force 160mg online
Regulatory T cell clones induced by oral tolerance: suppression of autoimmune encephalomyelitis erectile dysfunction from diabetes order super p-force 160 mg mastercard. Regulatory T cells expressing interleukin 10 develop from Foxp3+ and Foxp3- precursor cells in the absence of interleukin 10. Suppression of autoimmune inflammation of the central nervous system by interleukin 10 secreted by interleukin 27-stimulated T cells. A dominant function for interleukin 27 in generating interleukin10-producing anti-inflammatory cells. Antigen-specific inhibition of effector T cell function in humans after injection of immature dendritic cells. Identification of a previously unknown antigen-specific regulatory T cells and its mechanism of suppression. Double-negative regulatory T cells induce allotolerance when expanded after allogeneic haematopoietic stem cell transplantation. In vitro-expanded antigen-specific regulatory T cells suppress autoimmune diabetes. Induction of foxp3+ regulatory T cells in the periphery of T cell receptor transgenic mice tolerized to transplants. In vivo prevention of transplant arteriosclerosis by ex vivo-expanded human regulatory T cells. Infusion of ex vivo expanded T regulatory cells in aduslts transplanted with umbilical cord blood: safety profile and detection kinetics. Ly-1+2- suppressor T cells downregulate the generation of Ly-1-2+ effector T cells. A consequence of removing L3T4+ suppressor T cells from a host generating predominantly Lyt-2+ T cell-mediated immunity. Concomitant tumor immunity to a poorly immunogenic melanoma is prevented by regulatory T cells. Cutting edge: regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Infected site-restricted Foxp3+ natural regulatory T cells are specific for microbial antigens. Pathogen-specific T regulatory 1 cells induced in the respiratory tract by a bacterial molecule that stimulates interleukin 10 production by dendritic cells: a novel strategy for evasion of protective T helper type 1 responses by Bordetella pertussis. Pathogen-specific regulatory T cells delay the arrival of effector T cells in the lung during early tuberculosis. Coordination of early protective immunity to viral infection by regulatory T cells. Generation and large-scale expansion of human inducible regulatory T cells that suppress graftverus-host disease. Lymphocyte-filled villi: comparison with other lymphoid aggregations in the mucosa of the human small intestine. The development of intestinal lymphoid tissues at the interface of self and microbiota. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Regulation of C-type lectin antimicrobial activity by a flexible N-terminal prosegment. Gammadelta intraepithelial lymphocytes are essential mediators of host-microbial homeostasis at the intestinal mucosal surface. Nod2-dependent regulation of innate and adaptive immunity in the intestinal tract. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. The genome of Akkermansia muciniphila, a dedicated intestinal mucin degrader, and its use in exploring intestinal metagenomes. Quantitative relationships of monomeric and polymeric immunoglobulin A, immunoglobulin M, and other proteins in serum, bile, and saliva. Anti-inflammatory role for intracellular dimeric immunoglobulin a by neutralization of lipopolysaccharide in epithelial cells. Entry route of Salmonella typhimurium directs the type of induced immune response. Secretory IgA-mediated neutralization of Shigella flexneri prevents intestinal tissue destruction by down-regulating inflammatory circuits. Mice carrying a knock-in mutation of Aicda resulting in a defect in somatic hypermutation have impaired gut homeostasis and compromised mucosal defense. Early appearance of "natural" mucosal IgA responses and germinal centers in suckling mice developing in the absence of maternal antibodies. Immunoglobulins in intact, immunized, and contaminated axenic mice: study of serum IgA. Use of axenic animals in studying the adaptation of mammals to their commensal intestinal microbiota. Commensal enteric bacteria engender a self-limiting humoral mucosal immune response while permanently colonizing the gut. Identification of multiple isolated lymphoid follicles on the antimesenteric wall of the mouse small intestine. Requirement for lymphoid tissue-inducer cells in isolated follicle formation and T cell-independent immunoglobulin A generation in the gut. Regulation of humoral and cellular gut immunity by lamina propria dendritic cells expressing Toll-like receptor 5. Novel functions of the polymeric Ig receptor: well beyond transport of immunoglobulins. Secretory IgA possesses intrinsic modulatory properties stimulating mucosal and systemic immune responses. The sensing of environmental stimuli by follicular dendritic cells promotes immunoglobulin A generation in the gut. Transforming growth factor beta specifically enhances IgA production by lipopolysaccharide-stimulated murine B lymphocytes. Smad3 and Smad4 mediate transforming growth factor-beta1-induced IgA expression in murine B lymphocytes. The microbiota mediates pathogen clearance from the gut lumen after non-typhoidal Salmonella diarrhea. Protective efficacy of IgA monoclonal antibodies to O and H antigens in a mouse model of intranasal challenge with Salmonella enterica serotype Enteritidis. Reversible microbial colonization of germfree mice reveals the dynamics of IgA immune responses. Differences in intraepithelial lymphocyte T cell subsets isolated from murine small versus large intestine. Evidence for regional specialization and extrathymic T cell maturation in the human gut epithelium. Complexity of the mouse gut T cell immune system: identification of two distinct natural killer T cell intraepithelial lineages. Thymic selection determines gammadelta T cell effector fate: antigen-naive cells make interleukin-17 and antigen-experienced cells make interferon gamma. Exogenous stimuli maintain intraepithelial lymphocytes via aryl hydrocarbon receptor activation. T-cell alpha beta + and gamma delta + deficient mice display abnormal but distinct phenotypes toward a natural, widespread infection of the intestinal epithelium. Gut-derived intraepithelial lymphocytes induce long term immunity against Toxoplasma gondii. Induction of a rapid and strong antigenspecific intraepithelial lymphocyte response during oral Encephalitozoon cuniculi infection. Gammadelta T cells play a protective role during infection with Nippostrongylus brasiliensis by promoting goblet cell function in the small intestine.
Buy discount super p-force 160mg online
A large number of secondary fetal and perinatal outcomes were also assessed in the metaanalysis venogenic erectile dysfunction treatment buy discount super p-force 160 mg online, but no significant effects were seen. The ratios of total tocopherol (in mg) to total fat (in g) present in newborns and adults are similar. Studies of the tocopherol content of platelets, white blood cells, and buccal mucosal cells have also provided important data, but data are fewer because of greater assay complexity and difficulty in obtaining an adequate sample size. Breast milk feedings result in a rapid increase in blood and tissue content of vitamin E, with a peak in platelet tocopherol concentration at age 6 months, which is about the time when other foods, less rich in -tocopherol, are added to the diet. Liver tocopherol concentrations reported in these twostudies(datacombinedinfigure)wereingoodagreement. Such data, as well as the fact that content of -tocopherol secreted in breast milk decreases over the course of lactation stages, being highest in colostrum, suggest that transport mechanisms are complex and may differ over time. Parity, nutritional status, socioeconomic status, and habitual dietary intake of vitamin E appear to have little effect on the levels of -tocopherol in breast milk. This could have significance for the rapidly growing fetus and newborn, especially under conditions of marginal maternal nutrition. Nonetheless, there remains a question about how much -tocopherol, as opposed to -tocopherol, is advisable in the feedings of infants whose natural food is colostrum and breast milk, both of which are rich in -tocopherol. Bieri and Evarts estimated that -tocopherol, when present in a diet sufficient in -tocopherol but at a / ratio of 2 to 3: 1, may account for as much as 20% of the total vitamin E activity of the diet. Analyses were carried out after 8 hours for percentage of hemolysis and concentrations of -tocopherol, -tocopherolquinone, and malonyldialdehyde. Additional studies similarly showed significant correlation of maternal and newborn plasma vitamin E levels without consideration of plasma lipid content. Therefore physiologic characteristics as well as tocopherol concentration determine functional adequacy of vitamin E at the tissue level. Membranes of the brain and retina, especially during fetal life and early infancy, have high lipid content and an even higher complement of highly unsaturated fatty acids, particularly docosahexaenoic acid. This is true during fetal life, labor and delivery, and the perinatal and newborn period because hypoxic or ischemic episodes followed by reoxygenation result in excessive production of oxidant radicals regardless of initial oxygen tensions. Almost all of these infants have been exposed to episodes of hypoxia and hyperoxia, periods of pulmonary and gastrointestinal dysfunction, repeated systemic infection, and weeks of suboptimal nutrition before reaching a postmenstrual age that approaches term. Tragically, the deaths of 38 preterm infants were associated with intravenous administration of daily tocopheryl acetate at doses of 25 to 100 mg/kg/day, although whether the deaths were related directly to tocopherol or other constituents in the solution is not known. By itself, this tocopherol is metabolically inert until it is made more pharmacologically available for human metabolism. The actual absolute dosage provided to neonates often varies unless adjusted for body weight. Thus the vitamin and polysorbate intake could vary if administration is dependent on rate of total parenteral infusion. One or more of these inert constituents of intravenous vitamin E may lead to progressive intralobular cholestasis, inflammation of hepatic venules, and extensive sinusoidal veno-occlusion by fibrosis, as previously described and attributed to E-Ferol,148 and possibly to vitamin E acetate and polysorbate. Based on neonatal tocopherol metabolism studies, vitamin E provided as an alcohol may be a better choice. Enteral absorption of vitamin E appears to be sufficient to rapidly increase serum tocopherol levels. The importance of tissue -tocopherol status during the perinatal period likely has important implications beyond the neonatal period. A study of children with cystic fibrosis (at risk for fat-soluble vitamin deficiency) diagnosed by newborn screening compared with standard clinical methods linked vitamin E deficiency in infancy with later cognitive outcome. There is also strong advocacy for vitamin E as a nutritional therapeutic intervention in children with certain neurodevelopmental deficiencies because neuronal oxidative stress and deficiencies in antioxidant defenses likely contribute to these conditions. With supraphysiologic intakes, there is concern that vitamin E, under certain circumstances, might promote proinflammatory reactions at the fetomaternal interface. Investigators are now in general agreement that the importance of vitamin E for reproduction is underestimated and misunderstood if only its antioxidant properties are considered. Furthermore, emerging evidence regarding the importance of tocopherol forms other than -tocopherol, in particular -tocopherol, and the roles of tocotrienols as antioxidants and antiinflammatory molecules need to be expanded into the perinatal population. Rahal A, Kumar A, Singh V, et al: Oxidative stress, prooxidants, and antioxidants: the interplay. Valko M, Leibfritz D, Moncol J, et al: Free radicals and antioxidants in normal physiological functions and human disease. Menon R: Oxidative stress damage as a detrimental factor in preterm birth pathology. Boscoboinik D, Szewczyk A, Azzi A: Alpha-tocopherol (vitamin E) regulates vascular smooth muscle cell proliferation and protein kinase C activity. Ogihara T, Kitagawa M, Miki M, et al: Susceptibility of neonatal lipoproteins to oxidative stress. Ricciarelli R, Tasinato A, Clement S, et al: Alpha-tocopherol specifically inactivates cellular protein kinase C alpha by changing its phosphorylation state. Vanderpas J, Vertongen F: Erythrocyte vitamin E is oxidized at a lower peroxide concentration in neonates than in adults. In de Duve C, Hayaishi O, editors: Proceedings of the international symposium on tocopherol, oxygen, and biomembranes, Amsterdam, 1978, Elsevier Scientific. Serbinova E, Kagan V, Han D, et al: Free radical recycling and intramembrane mobility in the antioxidant properties of alpha-tocopherol and alphatocotrienol. Ahsan H, Ahad A, Iqbal J, et al: Pharmacological potential of tocotrienols: a review. Biopotencies of all eight stereoisomers, individually or in mixtures, as determined by rat resorption-gestation tests. Jansson L, Lindroth M, Tyopponen J: Intestinal absorption of vitamin E in low birth weight infants. Hosomi A, Arita M, Sato Y, et al: Affinity for alpha-tocopherol transfer protein as a determinant of the biological activities of vitamin E analogs. Sato Y, Hagiwara K, Arai H, et al: Purification and characterization of the alpha-tocopherol transfer protein from rat liver. Cohn W, Kuhn H: the role of the low density lipoprotein receptor for alphatocopherol delivery to tissues. Fahraeus L, Larsson-Cohn U, Wallentin L: Plasma lipoproteins including high density lipoprotein subfractions during normal pregnancy. Mino M, Nagamatu M: An evaluation of nutritional status of vitamin E in pregnant women with respect to red blood cell tocopherol level. Mino M, Nakagawa S, Tamai H, et al: Clinical evaluation of red blood cell tocopherol. Cindrova-Davies T, Spasic-Boskovic O, Jauniaux E, et al: Nuclear factor-kappa B, p38, and stress-activated protein kinase mitogen-activated protein kinase signaling pathways regulate proinflammatory cytokines and apoptosis in human placental explants in response to oxidative stress: effects of antioxidant vitamins. Cohen-Kerem R, Koren G: Antioxidants and fetal protection against ethanol teratogenicity. Jauniaux E, Cindrova-Davies T, Johns J, et al: Distribution and transfer pathways of antioxidant molecules inside the first trimester human gestational sac. Jishage K, Tachibe T, Ito T, et al: Vitamin E is essential for mouse placentation but not for embryonic development itself. Zaken V, Kohen R, Ornoy A: Vitamins C and E improve rat embryonic antioxidant defense mechanism in diabetic culture medium. Ferencz A, Orvos H, Hermesz E: Major differences in the levels of redox status and antioxidant defence markers in the erythrocytes of pre- and full-term neonates with intrauterine growth restriction. Poston L: Intrauterine vascular development: programming effects of nutrition on vascular function in the new born and adult. Inan C, Kilic I, Kilinc K, et al: the effect of high dose antenatal vitamin E on hypoxia-induced changes in newborn rats. Iwasa H, Aono T, Fukuzawa K: Protective effect of vitamin E on fetal distress induced by ischemia of the uteroplacental system in pregnant rats. Yoshioka T, Motoyama H, Yamasaki F, et al: Protective effect of vitamin E against lipoperoxides in developing rats. Viana M, Castro M, Barbas C, et al: Effect of different doses of vitamin E on the incidence of malformations in pregnant diabetic rats. Boskovic R, Gargaun L, Oren D, et al: Pregnancy outcome following high doses of Vitamin E supplementation.
Heal-All (Figwort). Super P-Force.
- How does Figwort work?
- Are there any interactions with medications?
- What is Figwort?
- Dosing considerations for Figwort.
- Are there safety concerns?
- Eczema, itching, psoriasis, and hemorrhoids.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96455
Discount super p-force
Neutrophils are not normally present in amniotic fluid; these cells are recruited into the amniotic compartment in the course of intraamniotic infection erectile dysfunction caused by medications generic 160 mg super p-force visa, and their origin is predominantly fetal. The clinical manifestations of this involvement can include respiratory distress syndrome, suspected or proven neonatal sepsis, pneumonia, bronchopulmonary dysplasia, intraventricular hemorrhage, periventricular leukomalacia, necrotizing enterocolitis, thymus involution, and dermatitis. Splenic hyperplasia, as reported in these experiments, contrasts with that observed in humans487; however, the latter may reflect the end-stage disease associated with perinatal death. Because intraamniotic infection may have a chronic course, the laboratories of Jobe and Newnham have explored the potential role of repeated injections of intraamniotic bacterial endotoxin in fetal sheep. In neonates, thymic involution correlates with the duration of acute illness and with the percentage of lymphocytes in the peripheral blood. These effects were observed as early as 5 hours after exposure to endotoxin and documented for 5 to 7 days. Preterm neonates exposed to intraamniotic infection and/or inflammation have activation of both the innate immune system373,478,507 and the adaptive immune system. Activation of T cells (members of the adaptive limb of the immune response) has been observed in term and preterm infants born to mothers with clinical chorioamnionitis. We need to interpret observations derived from animal models by taking into account the differences between the naturally occurring infection in humans and the specific experimental conditions used to elicit intraamniotic inflammation. The latter would be more meaningful in studying the fetal response to microorganisms. The laboratories of Jobe, Newnham, Gravett, and Novy have reported and are investigating the fetal immune response using such models. The short-term and longterm consequences of congenital fetal dermatitis remain to be determined. Amniotic fluid has natural antimicrobial properties (at least, in part, attributed to defensins). It is also possible that oligohydramnios may be the result of a redistribution of blood flow away from the kidneys occurring during the host response to microbial products. In cases of overwhelming fetal sepsis, myocardial depression can lead to fetal death. This probably contributes to the increased vulnerability of preterm neonates exposed to intraamniotic infection/ inflammation. This has been demonstrated by color Doppler ultrasound imaging in which influx and efflux of amniotic fluid can be visualized. Meconium can be detected in the alveoli in cases of fetal death, suggesting that under certain circumstances amniotic fluid can reach the alveoli. Tracheobronchial fluid obtained through an endotracheal tube placed shortly after birth often shows the presence of white blood cells and microorganisms in patients with intraamniotic infection. Moreover, congenital pneumonia is observed in a fraction of infants with intraamniotic infection. Subsequently, the laboratories of Jobe and Newnham systematically studied endotoxin-induced fetal lung injury in sheep and rhesus macaques. Subsequently, Nelson and Ellenberg,166 using data from the Collaborative Perinatal Project, showed that among low-birth-weight infants chorioamnionitis was associated with an incidence of cerebral palsy increasing from 12 to 39 per 1000 live births. Dammann and Leviton589 proposed that intraamniotic infection leads to a fetal inflammatory response, which, in turn, contributes to adverse outcomes such as preterm labor and delivery, intraventricular hemorrhage, white matter damage, and neurodevelopment disability (mainly cerebral palsy). These cytokines promote the passage of microbial products and other cytokines into the brain by increasing the permeability of the blood-brain barrier. This increase in permeability is, at least in part, dependent on cyclic guanosine monophosphate and nitric oxide. It is noteworthy that some studies have not demonstrated an association between histologic chorioamnionitis and cerebral palsy in preterm neonates. However, exposed neonates have evidence of microglial activation, astrogliosis, neuronal damage, and the clinical manifestations of cerebral palsy. A fundamental question with clinical importance is the identification of the infant exposed to intraamniotic inflammation/infection who has neuroinflammation from the infant who does not. Studies with positron emission tomography indicate that microglial activation can be detected shortly after birth; therefore, the molecular diagnosis of neuroinflammation is possible. The administration of stem cells can also have powerful effects,656-661 suggesting that a combination of regenerative medicine and nanotechnology can be used to treat congenital neuroinflammation and prevent long-term disability. This effect on the bowel can be demonstrated for 14 days after exposure to the inflammatory insults after Ureaplasma parvum inoculation. Systemic inflammation can affect multiple fetal organ systems and predispose to short-term and long-term complications. Two of the long-term complications are bronchopulmonary dysplasia and cerebral palsy. Recent observations suggest that the modulation of the maternal and fetal inflammatory response during pregnancy may have considerable importance for understanding the mechanisms of disease of preterm labor and fetal injury. This has substantial potential for the diagnosis, treatment, and prevention of long-term handicap related to congenital infections. This article has been substantially changed from that published in earlier editions of this book. In particular, we gratefully acknowledge the intellectual contributions of Maria-Teresa Gervasi and Tinnakorn Chaiworapongsa. Espinoza J, Erez O, Romero R: Preconceptional antibiotic treatment to prevent preterm birth in women with a previous preterm delivery. Adlerberth I, Lindberg E, Aberg N, et al: Reduced enterobacterial and increased staphylococcal colonization of the infantile bowel: an effect of hygienic lifestyle Prevalence, microbiology, and clinical significance of intraamniotic infection in women with preterm labor and intact membranes. Romero R, Gomez R, Chaiworapongsa T, et al: the role of infection in preterm labour and delivery. Romero R, Espinoza J, Chaiworapongsa T, Kalache K: Infection and prematurity and the role of preventive strategies. Romero R, Quintero R, Nores J, et al: Amniotic fluid white blood cell count: a rapid and simple test to diagnose microbial invasion of the amniotic cavity and predict preterm delivery. Vousden N, Chandiramani M, Seed P, Shennan A: Interleukin-6 bedside testing in women at high risk of preterm birth. Kacerovsky M, Musilova I, Stepan M, et al: Detection of intraamniotic inflammation in fresh and processed amniotic fluid samples with the interleukin-6 point of care test. Romero R, Miranda J, Chaemsaithong P, et al: Sterile and microbial-associated intra-amniotic inflammation in preterm prelabor rupture of membranes. Romero R, Miranda J, Chaiworapongsa T, et al: Sterile intra-amniotic inflammation in asymptomatic patients with a sonographic short cervix: prevalence and clinical significance. Romero R, Espinoza J, Mazor M: Can endometrial infection/inflammation explain implantation failure, spontaneous abortion, and preterm birth after in vitro fertilization Kacerovsky M, Musilova I, Hornychova H, et al: Bedside assessment of amniotic fluid interleukin-6 in preterm prelabor rupture of membranes. Romero R, Miranda J, Chaiworapongsa T, et al: A novel molecular microbiologic technique for the rapid diagnosis of microbial invasion of the amniotic cavity and intra-amniotic infection in preterm labor with intact membranes. Romero R, Miranda J, Chaiworapongsa T, et al: Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Russell P: Inflammatory lesions of the human placenta: Clinical significance of acute chorioamnionitis. Pacora P, Chaiworapongsa T, Maymon E, et al: Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. Olding L: Value of placentitis as a sign of intrauterine infection in human subjects. Holzman C, Lin X, Senagore P, Chung H: Histologic chorioamnionitis and preterm delivery. Lee J, Romero R, Xu Y, et al: A signature of maternal anti-fetal rejection in spontaneous preterm birth: chronic chorioamnionitis, anti-human leukocyte antigen antibodies, and C4d. Lee J, Romero R, Chaiworapongsa T, et al: Characterization of the fetal blood transcriptome and proteome in maternal anti-fetal rejection: evidence of a distinct and novel type of human fetal systemic inflammatory response. In Milunsky A, editor: Genetic disorders of the fetus, New York, 1986, Plenum, p 571. Prevalence, microbiology, and clinical significance of intraamniotic infection in twin gestations with preterm labor. Altshuler G, Hyde S: Clinicopathologic considerations of fusobacteria chorioamnionitis.
Purchase online super p-force
Ultrasound or ultrasound plus maternal serum alpha fetoprotein can be used to screen for open neural tube defects in multiple gestations erectile dysfunction electric pump buy super p-force toronto, as the concentration of maternal serum alpha fetoprotein is proportional to the number of fetuses. The upper limit for a twin pregnancy is approximately twice that for a singleton pregnancy (~4. Genetic amniocentesis is typically performed in the mid second trimester; earlier amniocentesis should be avoided as it can lead to increased rates of pregnancy loss, leakage of fluid, and fetal talipes equinovarus. Patients should be counseled that the amniocentesis loss rate is likely elevated above the baseline risk of loss for twin pregnancies. A 2012 review by Vink and colleagues49 demonstrated a pooled procedure-related loss rate at less than 24 weeks of 3. When studies using a control group were analyzed, the pooled odds ratio for total pregnancy loss among cases was 1. Multiple gestations have an increased incidence of structural anomalies, including cardiovascular anomalies. To date, no large series have evaluated the sonographic detection rate of malformations in twin gestations. The 2012 American College of Radiology Appropriateness Criteria recommend anatomic survey between 18 and 20 weeks, with follow-up scans as needed to clarify suboptimal visualization of any structures. Part of this increased risk results from preterm labor and delivery, and a portion of this risk is secondary to complications inherent to multiple gestations. Serial ultrasound imaging is the best method for evaluating fetal growth in a multiple pregnancy, and the biometric parameters used to assess singletons are accurate in multiples. Although individual growth curves for twins and triplets have been described, singleton weight standards are generally used for assessing weight in twins and higher-order multiples. In twins, each fetus grows at the same rate as for singletons up to approximately 32 weeks of gestation. After approximately 32 weeks, the combined weight gain in twins is the same as in a singleton at the same gestational age. In higher-order multiple pregnancies, this weight difference seems to become evident at even earlier gestational ages. Pregnancies complicated by multiple gestations should be monitored serially for growth with ultrasound imaging. Although one fetus may develop differently (but normally) from the other in terms of size, most fetuses in multifetal pregnancies grow concordantly. Nonetheless, in most cases, the smaller twin will have a birth weight less than the tenth percentile. Growth discordancy is the difference in sonographically estimated fetal weight expressed as a percentage in relation to the larger twin, and a 20% difference is generally considered to be clinically significant. Discordantly grown twins are likelier to be associated with adverse neonatal outcomes such as low and very low birth weight, neonatal oxygen requirement, neonatal care unit admission, hyperbilirubinemia, and stillbirth. For example, velamentous umbilical cord insertion- umbilical cord insertion directly into the membranes-occurs 9 to 10 times more frequently in twins than in singletons and 25 to 50 times more frequently in triplets than in singletons. A 13-fold increase in birth weight discordancy has been noted in monoamniotic twins with a velamentous umbilical cord insertion. Dizygotic twins are distinct individuals that exhibit genetically different growth patterns. It is not surprising, therefore, that these twins may have divergent birth weights. Nonetheless, several pathologic conditions result in discordant weight gain in these fetuses, including in utero crowding, unequal sharing of the placenta, and the combination of a normal fetus with an anomalous fetus. In addition to growth discordancy, multiple gestations are associated with increased risk for intrauterine growth restriction. Uteroplacental insufficiency is thought to be the main cause of growth restriction in multiple gestations. Because the risk for neurologic injury to the surviving twin may be as high as 25% if intracardiac potassium chloride injection is used, selective umbilical cord occlusion is the approach for monochorionic twins complicated by discordant anomalies and growth anomalies. The current abates blood flow in the umbilical cord and causes asystole in the targeted fetus. It is currently the procedure of choice for many institutions but there is no consensus on the optimal management for these cases. Most co-twin deaths occurred within 2 weeks, and the overall rate of neonatal death was 4%. Preterm premature rupture of membranes occurred in 22% of cases, and preterm delivery occurred in 33% of cases. Neonatal morbidity related to neurologic abnormalities and/or prematurity occurred in 7% of survivors. The routine use of ultrasound monitoring has shown that early fetal wastage is common in multiple gestations. In patients with twin gestations scanned before 7 weeks, up to 27% will have spontaneous reduction of one sac by 12 weeks. Explanations include physiologic resorption, misinterpretation of artifact, and sonographic error. Although this phenomenon may be associated with first-trimester bleeding/spotting and with abnormalities in maternal analytes in first-trimester screening, it has not been associated with adverse pregnancy outcomes. The chorionicity and gestational age of the pregnancy dictates the management options. In patients with dichorionic twins or trichorionic triplets, options include expectant management, termination of the entire pregnancy, or selective reduction by intracardiac potassium chloride injection. In these pregnancies, the circulation between the fetuses is not shared, so the death of one fetus is an independent event. Intracardiac injection of potassium chloride is used to cause asystole in the targeted fetus. Nonetheless, there are patients who may opt for expectant management, especially if the anomaly is not expected to have a favorable outcome, because selective termination can be associated with a slightly increased risk for miscarriage and preterm delivery. Selective termination of a monochorionic pregnancy is more complicated because vascular anastomoses in the placenta allow intrafetal transfusion. If one twin dies in utero, blood may be shunted to that twin, causing extreme hypotension in the surviving twin. Lee and colleagues67 showed that monochorionic diamniotic twins had a higher rate of stillbirth than dichorionic diamniotic pairs overall and at each gestational age after 24 weeks. No amniotic membrane is visualized in a same-sex twin pregnancy with one placental mass. The diagnosis of monoamniotic twins can be confirmed by observing umbilical cord entanglement on ultrasound imaging. In a study by House and colleagues,72 22 patients were managed at a tertiary care center over a 10-year period. Management included close fetal surveillance with daily testing starting at 24 to 26 weeks of gestation. Antenatal corticosteroids were routinely used, and elective delivery was performed at 34 to 35 weeks, provided that the results of testing were reassuring. Nevertheless, monoamniotic twins were likelier to be born prematurely and had more respiratory problems compared with monochorionic diamniotic and dichorionic diamniotic twins. Although vaginal delivery is not contraindicated, it should be undertaken with caution. If the diagnosis is suspected early in the first trimester, a follow-up scan is needed for confirmation, because an incorrect diagnosis is possible at early gestational ages. Conjoined twins may be joined at various anatomic locations and are classified on the basis of the location of the union. The ventral unions make up 87% of cases and include cephalopagus (11%), thoracopagus (19%), omphalopagus (18%), ischiopagus (11%), and parapagus (pelvis and variable trunk) (28%). The less frequent dorsal unions make up 13% of cases and include craniopagus (5%), rachiopagus (vertebral column) (2%), and pygopagus (sacrum) (6%). Depending on the type of conjoined twin and the gestational age, this procedure can be performed by dilatation and curettage, dilatation and evacuation, induction, or hysterotomy. If expectant management is desired, care should be transferred to a referral center. Generally, delivery should be performed by cesarean delivery as near to term as possible, with a multidisciplinary team approach. Vaginal delivery is possible in selected cases of extreme prematurity or if survival is improbable. Successful separation of the twins depends on the degree of organ and vascular sharing between the two fetuses.
Purchase super p-force on line amex
Interleukin-13 induces a hypersecretory ion transport phenotype in human bronchial epithelial cells erectile dysfunction vitamin shoppe buy super p-force 160mg with visa. Differential regulation of nitric oxide synthase-2 and arginase-1 by type 1/type 2 cytokines in vivo: granulomatous pathology is shaped by the pattern of L-arginine metabolism. Interleukin-13 induces tissue fibrosis by selectively stimulating and activating transforming growth factor beta(1). Interleukin-4- and interleukin-13enhanced transforming growth factor-beta2 production in cultured human bronchial epithelial cells is attenuated by interferon-gamma. Differential monocyte chemoattractant protein-1 and chemokine receptor 2 expression by murine lung fibroblasts derived from Th1- and Th2-type pulmonary granuloma models. Interleukin-13 stimulates the proliferation of lung myofibroblasts via a signal transducer and activator of transcription-6-dependent mechanism: a possible mechanism for the development of airway fibrosis in asthma. Leukotrienes mediate murine bronchopulmonary hyperreactivity, inflammation, and part of mucosal metaplasia and tissue injury induced by recombinant murine interleukin-13. Direct effects of interleukin-13 on epithelial cells cause airway hyperreactivity and mucus overproduction in asthma. Effect of different penicillin derivatives on complement components in human serum. Blackley and the development of hay fever as a disease of civilization in the nineteenth century. A second study of the behaviour and fate of skin homografts in rabbits; a report to the War Wounds Committee of the Medical Research Council. Role of persistence of antigen and indirect recognition in the maintenance of tolerance to renal allografts. Characterization of a clonal assay and determination of the size of clones derived from single precursors. Quantifying the frequency of alloreactive T cells in vivo: new answers to an old question. Limiting dilution analysis of alloreactive T-cell status and distribution during allograft rejection. The role of peptides in T cell alloreactivity is determined by self-major histocompatibility complex molecules. The crystal structures of K(bm1) and K(bm8) reveal that subtle changes in the peptide environment impact thermostability and alloreactivity. Alloreactive cytotoxic T lymphocytes focus on specific major histocompatibility complex-bound peptides. Induction of minor alloantigen-specific T cell subsets in vivo: recognition of processed antigen by helper but not by cytotoxic T cell precursors. Cross-priming for a secondary cytotoxic response to minor H antigens with H-2 congenic cells which do not cross-react in the cytotoxic assay. Identification of classical minor histocompatibility antigen as cell-derived peptide. Cellular peptide composition governed by major histocompatibility complex class I molecules. Feasibility of immunotherapy of relapsed leukemia with ex vivogenerated cytotoxic T lymphocytes specific for hematopoietic systemrestricted minor histocompatibility antigens. Identification of a graft versus host disease-associated human minor histocompatibility antigen. The immunogenicity of a new human minor histocompatibility antigen results from differential antigen processing. Differences that matter: major cytotoxic T cell-stimulating minor histocompatibility antigens. The relevance of minor histocompatibility antigens in solid organ transplantation. Role of perforin-mediated cell apoptosis in murine models of infusion-induced bone marrow failure. Decreased immunogenicity of a transplantation antigen in hosts sensitized to other isoantigens of its cellular vehicle. Antigen competition in cytotoxic T cell response to minor histocompatibility antigens. The preferential cytolytic T lymphocyte resonse to immunodominant minor histocompatibility antigen peptides. Immunodominance of H60 is caused by an abnormally high precursor T cell pool directed against its unique minor histocompatibility antigen peptide. Immunodominance in the graft-vs-host disease T cell response to minor histocompatibility antigens. In vitro cell-mediated immune responses to the male specific (H-Y) antigen in mice. Responsiveness to H-Y antigen, Ir gene complementation, and target cell specificity. Rejection of bone-marrow graft by recipient-derived cytotoxic T lymphocytes against minor histocompatibility antigens. Rapid identification of clinical relevant minor histocompatibility antigens via genome-wide zygosity-genotype correlation analysis. Expression and presentation of endogenous mouse mammary tumor virus superantigens by thymic and splenic dendritic cells and B cells. The failure of skin grafting to break tolerance to class I disparate renal allografts in miniature swine despite inducing marked anti-donor cellular immunity. Cytotoxic T-lymphocytedefined human minor histocompatibility antigens with a restricted tissue distribution. The histological distribution of the blood group substances in man as disclosed by immunofluorescence. Removal of IgM anti-endothelial antibodies results in prolonged cardiac xenograft survival. Evidence for a similar or common mechanism for natural killer activity and resistance to hemopoietic grafts. The problem of anti-pig antibodies in pig-to-primate xenografting: current and novel methods of depletion and/or suppression of production of anti-pig antibodies. Mechanism of the xenogeneic hyperacute rejection reaction and its modification due to actively and passively produced enhancement [in German]. Relationship of platelets, blood coagulation, and fibrinolysis to hyperacute rejection of renal xenografts. Clinical criteria for evaluating first set, accelerated, and white graft rejection in human skin homografts. Intact pig pancreatic islet function in the presence of human xenoreactive natural antibody binding and complement activation. Role of antibodyindependent complement activation in rejection of porcine bone marrow cells in mice. Pathologic features of acute renal allograft rejection associated with donor-specific antibody, analysis using the Banff grading schema. Accomodation of vascularized xenografts: Expression of "protective genes" by donor endothelial cells in a host Th2 cytokine environment. Human monocytes activate porcine endothelial cells, resulting in increased E-selectin, interleukin-8, monocyte chemotactic protein-1, and plasminogen activator inhibitor-type-1 expression. Disordered regulation of coagulation and platelet activation in xenotransplantation. Anti-L3T4 in vivo prevents alloantibody formation after skin grafting without prolonging graft survival. T-cell subsets, bm mutants, and the mechanisms of allogeneic skin graft rejection. Demonstration and characterization of Ia-positive dendritic cells in the interstitial connective tissues of rat heart and other tissues, but not brain. Dendritic cells as a tool to induce transplantation tolerance: obstacles and opportunities. Immunologic "ignorance" of vascularized organ transplants in the absence of secondary lymphoid tissue. Protective long-term antibody memory by antigendriven and T help-dependent differentiation of long-lived memory B cells to short-lived plasma cells independent of secondary lymphoid organs. In vivo dynamics of regulatory T-cell trafficking and survival predict effective strategies to control graft-versus-host disease following allogeneic transplantation. In vivo analyses of early events in acute graft-versus-host disease reveal sequential infiltration of T-cell subsets. The role of vascular endothelium in the afferent pathway as suggested by alymphatic homotransplantation.
Buy super p-force 160mg without prescription
Adoptive transfer of minor histocompatibility antigen-specific T lymphocytes eradicates leukemia cells without causing graft-versus-host disease erectile dysfunction pills amazon generic 160 mg super p-force amex. Evidence for allelic specificity of mixed leukocyte reaction and for both direct and indirect pathways of recognition. Production of alpha-1,3-galactosyltransferase knockout pigs by nuclear transfer cloning. Production of alpha-1, 3-galactosyltransferase null pigs by means of nuclear transfer with fibroblasts bearing loss of heterozygosity mutations. Heart transplantation in baboons using alpha1,3-galactosyltransferase gene-knockout pigs as donors: initial experience. Marked prolongation of porcine renal xenograft survival in baboons through the use of alpha1, 3-galactosyltransferase gene-knockout donors and the cotransplantation of vascularized thymic tissue. Long-term discordant xenogeneic (porcine-to-primate) bone marrow engraftment in a monkey treated with porcine-specific growth factors. Bone marrow transplantation from alpha1,3-galactosyltransferase gene-knockout pigs in baboons. Xenogeneic thymokidney and thymic tissue transplantation in a pig-to-baboon model: I. Search for cross-species transmission of porcine endogenous retrovirus in patients treated with living pig tissue. No association of kidney graft loss with human leukocyte antigen antibodies detected exclusively by sensitive Luminex single-antigen testing: a Collaborative Transplant Study report. Effect of the proteasome inhibitor bortezomib on humoral immunity in two presensitized renal transplant candidates. Molecular signatures of urinary cells distinguish acute rejection of renal allografts from urinary tract infection. Search for common antigenicities among twentyfive sarcomas induced by methylcholanthrene. A systematic analysis of experimental immunotherapies on tumors differing in size and duration of growth. Studies on the basis for diversity and time of appearance of antigens in chemically induced tumors. A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. A mutated intron sequence codes for an antigenic peptide recognized by cytolytic T lymphocytes on a human melanoma. Chemical carcinogen mechanisms of action and implications for testing methodology. Nonrandom escape of tumor cells from immune lysis due to intraclonal fluctuations in antigen expression. Stochastic state transitions give rise to phenotypic equilibrium in populations of cancer cells. Reflections on the implications of multistage carcinogenesis for the nature of neoplasia. Synergy between T-cell immunity and inhibition of paracrine stimulation causes tumor rejection. Antigenic cancer cells that escape immune destruction are stimulated by host cells. An experimental comparison of transplanted tumor and a transplanted normal tissue capable of growth. Stroma is critical for preventing or permitting immunological destruction of antigenic cancer cells. Robustness, scalability, and integration of a wound-response gene expression signature in predicting breast cancer survival. Gene expression signature of fibroblast serum response predicts human cancer progression: similarities between tumors and wounds. Renal damage progresses despite improvement of renal function after relief of unilateral ureteral obstruction in adult rats. Characterization of renal interstitial fibroblast-specific protein 1/S100A4positive cells in healthy and inflamed rodent kidneys. Fibroblastspecific protein 1 identifies an inflammatory subpopulation of macrophages in the liver. Microscopical Researches into the Accordance in the Structure and Growth of Animals and Plants. Lectures on Surgical Pathology Delivered at the Royal College of Surgeons of England, London. Fibroblast procollagen production rates in vitro based on [3H]hydroxyproline production and procollagen hydroxyproline specific activity. Different tumor microenvironments contain functionally distinct subsets of macrophages derived from Ly6C(high) monocytes. Myeloid-derived suppressor cells: more mechanisms for inhibiting antitumor immunity. Genetically tagging endothelial cells in vivo: bone marrow-derived cells do not contribute to tumor endothelium. Minimal contribution of marrowderived endothelial precursors to tumor vasculature. Bone marrow-derived circulating endothelial precursors do not contribute to vascular endothelium and are not needed for tumor growth. An autoradiographic study of inhibition of cellular proliferation by local x-irradiation. Origin of fibroblasts in experimental healing wounds: autoradiographic studies using tritiated thymidine. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Presence of human circulating progenitor cells for cancer stromal fibroblasts in the blood of lung cancer patients. Effect of differences in cancer cells and tumor growth sites on recruiting bone marrow-derived endothelial cells and myofibroblasts in cancer-induced stroma. Endothelial progenitor cells are cellular hubs essential for neoangiogenesis of certain aggressive adenocarcinomas and metastatic transition but not adenomas. Cancer immunotherapy and preclinical studies: why we are not wasting our time with animal experiments. Immune surveillance against a solid tumor fails because of immunological ignorance. Stereotypical chronic lymphocytic leukemia B-cell receptors recognize survival promoting antigens on stromal cells. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Proinflammatory mediators and genetic background in oncogene mediated tumor progression. Oncoprotein signaling mediates tumorspecific inflammation and enhances tumor progression. Up-regulation of matrix metalloproteinase-9 in T lymphocytes of mammary tumor bearers: role of vascular endothelial growth factor. Interleukin-2 production by tumor cells bypasses T helper function in the generation of an antitumor response. Retroviral vector-mediated gamma-interferon gene transfer into tumor cells generates potent and long lasting antitumor immunity. Retroviral interleukin 5 gene transfer into interleukin 5-dependent growing cell lines results in autocrine growth and tumorigenicity. Long-term inhibition of tumor growth by tumor necrosis factor in the absence of cachexia or T-cell immunity. Granulocyte colonystimulating factor gene transfer suppresses tumorigenicity of a murine adenocarcinoma in vivo. Tumor suppression after tumor cell-targeted tumor necrosis factor alpha gene transfer. Reciprocal functional modulation of the activation of T lymphocytes and fibroblasts derived from human solid tumors. Plasticity in tumor-promoting inflammation: impairment of macrophage recruitment evokes a compensatory neutrophil response. Refractoriness to antivascular endothelial growth factor treatment: role of myeloid cells.
Buy super p-force 160 mg line
For instance erectile dysfunction treatment london discount super p-force 160mg online, mycophenolic acid, propofol, and 4-methylumbelliferone are metabolized to a greater extent by kidneys than by liver. In neonatal intensive care units, drugs are often administered to patients requiring very complex care. Life-threatening illnesses produce remarkable variation in pharmacokinetic behavior. Adjustment in drug dosage in the face of a changing disease is critical to avoid toxicity. This section addresses the issue of diseases as it applies to drug disposition in the newborn. Similarly, the presence of congenital heart defects or preferential perfusion of the pulmonary or the systemic vasculature will have an impact on pharmaceutical targets. A significant decrease in cardiac output or oxygen delivery can result in adverse effects on liver function and consequently diminish drug metabolism and clearance. In newborns with congestive heart failure, elevated plasma levels of digoxin have been observed, suggesting decreased drug clearance. Under these circumstances, drugs for which the kidneys represent the primary route of elimination. Reduction in tubular function can significantly affect the elimination of compounds that depend on tubular reabsorption or secretion, such as penicillins and furosemide. In addition, changes in plasma and urine pH can alter the excretion of ionized drugs, especially weak acids and weak bases. The development of uremia may be associated with changes in the cardiac output, liver function, and permeability of blood-brain barrier, all of which can further disturb drug disposition. The clinical significance of drug accumulation depends on whether the unexcreted products are pharmacologically active or toxic. Nomograms have been developed to allow modification of drug dosage in patients with renal failure. However, most nomograms primarily apply to adult and not infant patients, and must thus be used with caution. Pulmonary hypertension, pulmonary hypoplasia, and pulmonary hemorrhage are common in the newborn period and can impact drug delivery via the inhaled route. Furthermore, pulmonary hypertension may lead to a concurrent decrease in systemic cardiac output, with all its consequences on kidney and liver drug-handling capacities. Therapeutic hypothermia has been increasingly used in preterm newborns with perinatal asphyxia as a neuroprotective treatment. Asphyxia and separately hypothermia have profound effects on drug metabolism, clearance, and distribution. Newborns with asphyxia often have acute kidney injury with oliguria, liver failure, and cardiac insufficiency. Yet, given the breadth of severity of asphyxia, its effects on renal and hepatic clearance tend to be variable and are rarely predictable. Hypothermia per se can impact blood composition, circulatory hemodynamics, enzymatic processes, and regional perfusion. For instance, distribution of pancuronium, midazolam, gentamicin, and morphine was found to be unchanged or diminished by hypothermia. Hepatic insufficiency can affect drug elimination by (1) reducing plasma protein binding, (2) decreasing liver blood flow, and (3) disturbing intrinsic biotransformation reactions. A decrease in plasma protein concentration influences the disposition of drugs extensively bound to proteins. Drugs belonging to the first group exhibit a more uniform change in drug elimination during hepatic failure. This results from inconsistent qualitative and quantitative changes in liver enzyme activity in the presence of liver disease of variable severity. Furthermore, there are gestational and postnatal age-dependent changes in the expression of metabolizing enzymes. Expression follows three patterns: high expression during fetal compared with postnatal life, constant levels in the fetal and the postnatal periods, and activation of enzymes in the postnatal life. Because of the marked variability in the severity of liver dysfunction, it is difficult to formulate rules for dosage modification. Marked changes in pharmacokinetics (as noted with renal insufficiency) are generally not observed in liver failure. The consequences of concurrent disease on the pharmacokinetics and pharmacodynamics of drugs are irrefutably complex. An accurate prediction of drug disposition in the face of interacting, intricate, individual variables is virtually impossible. The relative paucity of information on drug pharmacokinetics in infants with cardiac, renal, and hepatic dysfunction and the often changing and transient nature of these disorders render careful clinical observations and appropriate therapeutic monitoring imperative under these circumstances. The concentration of a drug in the blood enables one to monitor the dose-response relationship and to predict its pharmacokinetics. A compartment is not necessarily a defined physiologic or anatomic site but is considered one of many tissues that exhibit similar affinity for a drug. The factors that determine the movement of a drug in and out of compartments are those that affect distribution. In this model, it is assumed that following drug administration, immediate equilibration of drug concentration is achieved in all major tissues. First-order kinetics apply to this model, meaning that the rate of changes in the amount of drug in the body is a constant fraction of the amount of drug present at the time. The rate of disappearance of a drug concentration using first-order kinetics can be expressed as: dC dt = -kC [18-9] where C = concentration of the drug, and k = first-order elimination rate constant, expressed in units of time-1. Integration of this equation yields the drug concentration at time t: log C = - kt 2. Table 18-4 ComparativePlasmaHalf-Livesof MiscellaneousDrugsinNewborns andAdults Plasma Half-Life (hr) Newborn Acetaminophen Phenylbutazone Indomethacin Meperidine Phenytoin Carbamazepine Phenobarbital Caffeine Theophylline Chloramphenicol Salicylates Digoxin 3. In newborns, because the elimination rate is decreased for many drugs, the half-life is often prolonged compared with that in the adult (Table 18-4). Thus Dss is also equal to the rate of drug elimination during the dosing interval. The -phase represents the distribution phase, and the -phase is the elimination phase. It can easily be appreciated that the time required to attain steady-state drug concentrations is equal to approximately 5 halflives, when first-order rates of absorption, distribution, and elimination are in process. The first part of the curve with its sharper slope, the phase, represents the distribution of drug to highly perfused areas, including the blood. With time and depending on the affinity of the drug for certain tissues, the agent distributes to the peripheral compartment or compartments. Usually, the half-life of drugs that distribute according to 2-compartment model is determined during the phase. To apply kinetic analysis of a multicompartment model, one assumes that all rate processes for the passage of drug from one compartment to another exhibit first-order kinetics. Therefore the plasma level-time curve for a drug that follows a multicompartment model is described by the summation of several firstorder rate processes. By substituting C with Css min and C0 with Css max, the following equation is obtained: log Css min - log Css max = - kt 2. Total clearance gives an indication of drug elimination from the central compartment without reference to the mechanism of this process. Clearance by the kidneys is called renal clearance, and that by all other organs is referred to as nonrenal clearance. The same factors that determine renal and hepatic elimination of drugs affect drug clearance. In contrast to a firstorder process, in which the fraction of drug eliminated is constant, in zero-order kinetics the elimination rate itself is constant. Consequently, the zero-order half-life is not constant but is proportional to the initial amount or concentration of the drug: t 12 = 0. Many drugs exhibit zeroorder kinetics with elevated concentrations, and as these decline first-order kinetics prevail.