Buy zydalis 20 mg visa
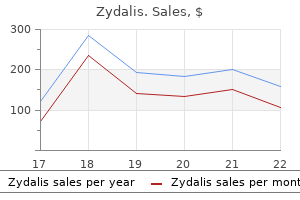
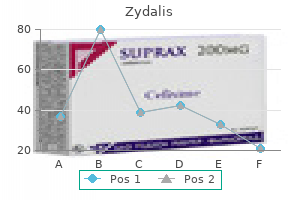
They may be treated by observation alone, isolated or serial lumbar puncture, temporary continuous lumbar drainage, lumboperitoneal shunting, or ventriculoperitoneal shunting erectile dysfunction fun facts discount zydalis 20 mg mastercard. Diagnostic lumbar puncture with measurement of opening and closing pressure can assist in distinguishing between simple hygromas and so-called external hydrocephalus. Bona fide hydrocephalus may occur postoperatively and must be distinguished from hydrocephalus ex vacuo. Options for treatment include tunneled ventriculostomy with external drainage, lumbar drainage if the cisterns are open, shunting with later bone flap replacement, bone flap replacement with later shunting if the ventriculomegaly does not resolve, or simultaneous bone flap replacement and shunting. This is seen more commonly in patients with thin areas of scalp, such as women, the malnourished, those with lacerations or abrasions, and those with chronic wounds with retracted skin and sunken flaps. The longer a sunken flap persists before reimplantation of the bone flap, the more the scalp contracts, which can contribute to later wound tension. On occasion, placement of tissue expanders or rotation of a new scalp flap (often in conjunction with plastic surgery) is necessary to obtain adequate scalp coverage over the implant. In our center, this is more common in reoperated patients who have had past infections or wound dehiscence requiring removal of their implant and hardware. Full nutritional evaluation may be necessary to maximize nutritional status before surgery. Bone flap resorption has been reported in up to 12% of patients after secondary bone flap replacement, with approximately half requiring removal and replacement with a synthetic implant. This was reduced to essentially nil with the avoidance of Bovie cautery for dissecting the scalp flap away from the underlying dura (thereby reducing potential exposure of the underlying brain tissue to heat) and with intraoperative loading of anticonvulsants, which are then continued for 7 days postoperatively. Patients receiving ongoing antiepileptic therapy for seizures are administered bolus therapy if their levels are subtherapeutic or are maintained on their therapeutic regimen. In some patients, symptoms of the syndrome of the trephine may be alleviated by recumbency. Anesthesia risks from the second procedure must also be taken into account, although rare. Engel n Hester Lingsma No head injury is too severe to be despaired of, nor too trivial to be ignored. In ancient Greece, the quality of care was judged not so much by the result of treatment but rather by whether the result was as the doctor had predicted. The science of clinical decision making and advances in statistical modeling have made it possible to be more confident about what is likely to happen and to consider prognosis in terms of probabilities rather than prophecies. The availability of large databases has opened new opportunities for an evidence-based approach to prognostic analysis. Information about prognosis and predictive statements can be useful in a number of ways. Concern about the probable outcome is often foremost in the mind of relatives, and realistic counseling is therefore very important. The place of prognosis in making decisions about the future management of individual patients is more controversial. Although many neurosurgeons acknowledge that prognostic estimates have an important role in decision making, others profess to attribute only a minor or even nonexistent role to prognosis, a mindset reflecting a range of attitudes arising from cultural and ethical differences as much as clinical convictions. Yet it is a fact of life that some form of estimation of prognosis is consciously or subconsciously used by physicians when allocating resources and prioritizing treatment- unfortunately, also now an increasing necessity in the highincome countries of the Western world. Moreover, predictive equations can never include all items relevant to a particular individual. The accuracy of prediction is limited to the group level describing the proportion of instances in which the expected profile coincides with the observed outcome. Awareness of the limitations of the probabilistic formulation is therefore an extremely important caution that is required for interpretation of prognostic estimates in individual cases. Estimates derived from evidence-based analysis of large datasets are preferable to relying on the "gut" feeling of a physician, whose experience, no matter how vast, can never match the information contained in the data from thousands of patients entered into a database. A sufficient sample size is important to address any scientific question with empirical data. The effective sample size is determined mainly by the number of events in the study and not by the total number of subjects. For example, when we study a disease with a 1% chance of mortality, a study with 1000 patients will contain only 10 events, and this number determines the effective sample size. It is important to match ambitions in research questions with the effective sample size that is available. Mortality is often used as an end point in prognostic research, but global outcome measures. When an outcome is very infrequent, it is not suited as an end point for statistical analysis. In the use of a dichotomous outcome measure, statistical power is greatest when there is a 50: 50 distribution between outcome categories. The use of a structured interview is further advocated to obtain more consistency in outcome assignment. Ideally, predictors are well defined, not too costly to obtain, and reliably measurable by any observer. In addition, some measurements are prone to biologic variability, and a single measurement may be misleading, as for instance in the case of blood pressure. In many studies, continuous or categorical predictors are collapsed into a binary variable by using threshold values. For example, the association between age and outcome has frequently been analyzed at a threshold value of 50 years. In addition, a patient 30 years of age may have a different risk than a patient 49 years old. Second, from a methodologic perspective, collapsing an ordinal or continuous scale into a binary variable (dichotomization) leads to loss of information and is therefore statistically inefficient. Missing Data Missing data are a common, but as yet underappreciated problem in medical scientific research. Missing values lead to a more limited set of patients with complete data as opposed to the ideal situation of complete original data. The best solution for missing values is of course to ensure that no data are missing. If we nonetheless have missing data, a common statistical approach is to delete patients with missing values from the analysis. It is hence statistically inefficient, especially when we consider multiple predictors. Moreover, complete case analysis may lead to bias because of systematic differences between patients with complete and patients with missing data. Bias occurs when absence of a predictor is associated in some way with the outcome. As in any statistical analysis, sensible judgement of the analyst based on knowledge of the subject and the research question is important. In practice, many clinicians are unaware of the problems inherent in complete case analyses and are ignorant of modern developments for dealing with missing data, in particular, the use of multiple imputation methods. Further research is required to determine the ultimate benefits from this approach, both for prognostic analysis and in the context of clinical trial design. Approaches to Prognostic Analysis the first step in prognostic analysis is identification of the association between a single prognostic factor and outcome (univariate analysis). It should be stressed that a univariate association does not take into account the role of other predictors that may be more important or even may account for the observed association. This association does not represent causality, and the association may be secondary to other more relevant predictors. The second step, therefore (multivariate analysis), focuses on the unique predictive value of that predictor over and above that of other covariates. Questions that require multivariable analysis are, for example, what are the most important predictors in a certain disease Are some predictors correlated with each other such that their apparent predictive effects are explained by other predictor variables To perform multivariate analysis, more predictors are added to the regression model as independent variables. The third step (prognostic modeling) depends on combining information from the different individual prognostic features into a prognostic model with the aim of giving the best predictions for individual patients. The relevance of a predictor is a function of association of the predictor with the outcome and the distribution of the predictor.
Purchase zydalis mastercard
The slash incision, which typically runs vertically, should be fashioned so that it can be extended to the larger "trauma flap" if necessary erectile dysfunction doctors in arizona purchase zydalis discount. The incision is made with a scalpel or a Colorado needletipped Bovie and taken directly down to the bone. After the skin incision, hemostasis is obtained with the help of Raney clips or electrocautery. The periosteum is then rapidly stripped to fully expose the cranium in the region of the hematoma. More bur holes can be created as necessary depending on the size or location of the clot. With such a vertical incision, removal of the hematoma may be achieved within about 5 minutes of beginning the incision. A Kerrison punch and a curved curet can be used to enlarge and undercut the bur holes to allow a Penfield No. The blood, which is usually clotted, is removed with the help of suction, irrigation, and cup forceps. The bleeding source, typically a branch of the middle meningeal artery, can generally be controlled with bipolar diathermy. Occasionally, the main trunk of the middle meningeal artery is bleeding because of a fracture involving the petrous bone. In these cases, adequate low temporal exposure is facilitated by the vertical incision advocated here. The foramen spinosum can be packed with bone wax or a combination of bone wax and Surgicel. After evacuation of the hematoma, meticulous hemostasis is obtained in the epidural space with Surgicel and Gelfoam, and bone wax is applied to the bone edges. Central dural tack-up sutures are also placed in the center of the bone flap to obliterate the central dead space under the bone flap. Bur hole covers should always be placed over the frontal bur holes for the best cosmetic result. The superficial temporal fascia and then the galea are approximated with 2-0 Dexon or similar suture. Skin staples are placed on the skin margins, the wound is dressed, and a head bandage is placed. Rarely, intradural "reperfusion" hematomas develop rapidly under a removed extradural hematoma. After evacuation of the extradural hematoma, if the underlying dura becomes tense, a limited opening should be made in the dura and any hematoma removed with gentle suction and bipolar diathermy. A larger dural opening must be made rapidly if persistent subdural bleeding is seen to visualize and coagulate the source, which may be a bridging vein. A ventriculostomy may be needed in unconscious patients, especially if an intraparenchymal mass lesion is present. Occasionally, the craniotomy will need to be enlarged to expose the bleeding point. In such cases, both the incision and the craniotomy can be expanded to a more traditional frontotemporoparietal craniotomy. Emergency angiography has demonstrated bleeding points and traumatic tears in the middle meningeal artery, which can be embolized with coils or Onyx. Mortality has been reported to be between 50% and 60% in various series and between 57% and 68% in patients initially seen in coma. Therefore, surgical planning should consider the need to contend with concomitant lesions or parenchymal injuries. In a retrospective study, 34 patients older than 65 years were compared with a similarly treated younger patient population (33 patients aged 18 to 40 years); mortality rates were more than 4 times higher in the older patients. In a study of 68 consecutive patients with warfarin-related intracranial hemorrhages, Mathiesen and associates reported that traumatic hematomas were found in 26 patients. However, lower mortality rates of 48% and 16% have been reported after warfarin-related intracranial hemorrhages. As with all trauma craniotomies, it is customary to takes measures to maximize intracranial relaxation. Such measures include the administration of mannitol and the institution of mild hyperventilation. The subdural space should be widely inspected for additional hematoma, bleeding, and surface contusions. Achieving and maintaining hemostasis at the operative site is the most difficult and most important aspect of trauma neurosurgery. Frequently, these patients are coagulopathic, with thrombocytopenia making hemostasis especially difficult to maintain. Occasionally, a bridging vein is clearly avulsed and can be cauterized with bipolar diathermy. When the bleeding is coming directly from the sinus wall, however, the use of bipolar diathermy is contraindicated because it may enlarge the opening. In these situations, it is best to use Gelfoam, Surgicel, or Avitene and gentle tamponade with a cottonoid pad to stop the oozing. It is vital that pressure in the sagittal sinus be decreased by placing the patient in a 10- to 15-degree head-up posture and ensuring that there is no jugular compression. After the clot is evacuated and hemostasis is obtained, closure of the dura is considered. Duraplasty may be followed by routine closure of the craniotomy with miniplates and bur hole covers. Intracerebral hematomas and contusions generally do not require surgical evacuation unless there is a significant mass effect or intracranial hypertension. The majority of intraparenchymal lesions occur in the temporal and frontal lobes as a consequence of the brain impacting against the skull, especially the sphenoid ridges. Parietal and occipital lobe hematomas are much less common and are usually due to direct impact, as in assaults. At least 25% of patients with intracranial mass lesions show clinical or *Please see the accompanying Video 335-2. This procedure provides a large area of decompression for patients with diffuse swelling. In addition, the underlying contused and hemorrhagic tissue can more readily be visualized and removed if necessary. This type of bifrontal decompressive craniectomy can also be performed over areas of maximal hemispheric swelling. To maximize intracranial relaxation, the patient is given mannitol and mildly hyperventilated. For a bifrontal craniotomy, the patient is placed supine on the operating table with the head resting on a foam pad or "horseshoe" Mayfield headrest. A bicoronal incision is marked out behind the hairline, starting low at the level of the zygoma. A Bovie monopolar cutting diathermy device is used to incise the superficial temporal fascia and the temporalis muscle while taking special care to avoid possible injury to the facial nerve by remaining above the zygoma at the inferior end of the incision. Using a combination of periosteal elevators and monopolar diathermy to separate the periosteum from the skull, a myocutaneous flap is reflected as low as possible anterior to the supraorbital margins and the sphenoid wing in the temporal region. Using a high-speed drill, multiple bur holes are placed in the temporal and frontal regions and two parasagittally, about 1. A Kerrison punch and a curved curet are then used to enlarge the bur holes and undermine the inferior aspect to allow a Penfield No. After this step, a cutting craniotome blade is used to perform the craniotomy cuts, again keeping as low as possible in the frontal and temporal areas. The last cut of the craniotomy should be the one carried over the midline sagittal sinus region to minimize bleeding. The superior sagittal sinus must be freed completely from the crista galli to the cephalad bur hole, and extra bur holes may be needed. Bone wax is applied to the bone margins, and strips of Surgicel or Gelfoam are placed around the craniotomy margins and over any small bleeding points from the sagittal sinus. Dural tack-up 4-0 silk sutures are placed around the margins of the craniotomy site. Bilateral dural openings are created with the flaps based toward the sagittal sinus.
Best purchase for zydalis
Risk D: Consider therapy modification Herbs (Anti coa gul a nt/Anti pl a tel et Properti es) (eg, Al fa l fa, Ani s e, Bi l berry): Ma y enha nce the a dvers e/toxi c effect of Anti pl a tel et Agents erectile dysfunction trimix zydalis 20 mg mastercard. Al s o, s i nce ma ny el derl y pa ti ents ma y ha ve Cl cr <30 mL/mi nute, cl os e moni tori ng s houl d be fol l owed wi th ca l cul a ti on of crea ti ni ne cl ea ra nce pri or to i ni ti a ti ng thera py wi th a na ki nra. Risk D: Consider therapy modification Etha nol /Nutri ti on/Herb Intera cti ons Herb/Nutra ceuti ca l: Avoi d bl a ck cohos h, hops, l i cori ce, red cl over, thyme, a nd dong qua i. By i nhi bi ti ng a roma ta s e, the convers i on of a ndros tenedi one to es trone, a nd tes tos terone to es tra di ol, i s prevented. Moni tori ng: La b Tes ts Li ver functi on tes ts Pa ti ent Educa ti onThi s medi ca ti on ca n onl y be a dmi ni s tered by i nfus i on. Intens i ty of thera py ma y depend on type of s urgery a nd pos topera ti ve regi men. Moni tori ng Pa ra meters Hea rt ra the a nd bl ood pres s ure (before a nd duri ng I. Moni tori ng: La b Tes ts In pa ti ents wi th ci rcul a ti ng i nhi bi tors, the i nhi bi tor l evel s houl d be moni tored; hema tocri t Pa ti ent Educa ti onThi s medi ca ti on ca n onl y be gi ven i ntra venous l y. Injecti on, powder for recons ti tuti on, recombi na nt [pres erva ti ve free]: Adva te: 250 i nt. Recons ti tuti onIf refri gera ted, the dri ed concentra the a nd di l uent s houl d be wa rmed to room tempera ture before recons ti tuti on. Injecti on, powder for recons ti tuti on [huma n deri ved]: Al pha na te: 250 i nt. Infecti ons thought to be tra ns mi tted by thi s product s houl d be reported to Ta l ecri s Bi othera peuti cs a t 1-800-520-2807. Risk C: Monitor therapy Thrombol yti c Agents: Ma y enha nce the a nti coa gul a nt effect of Anti coa gul a nts. If ta chyca rdi a devel ops, i nfus i on s houl d be di s conti nued a nd pres cri ber noti fi ed. Ra s h, dys pnea, hypotens i on, or a na phyl a xi s precl udes further a dmi ni s tra ti on of the drug. Boxed Warning]: Should only be used by physicians experienced in immunosuppressive therapy or management of solid organ or bone marrow transplant patients. Adequate laboratory and supportive medical resources must be readily available in the facility for patient management. Boxed Warning]: Should only be used by physicians experienced in immunosuppressive therapy for the treatment of renal transplant patients. Repea t procedure us i ng the 1:10 di l uti on a nd then undi l uted a nti veni n. Treatment of symptoms due to black widow spider bite: Admi ni s ter onl y fol l owi ng the s ki n tes t or conjuncti va l tes t: I. Treatment of symptoms due to black widow spider bite: Admi ni s ter onl y fol l owi ng the s ki n tes t or conjuncti va l tes t: Chi l dren <12 yea rs: I. Pa ti ent mus t be moni tored cl os el y for mi ni mum of 90 mi nutes fol l owi ng ea ch tes t dos e (eg, orthos ta ti c hypotens i on). Fol l ow s peci fi c di recti ons for a dmi ni s tra ti on wi th i njecti on pen or s yri nge a nd needl e di s pos a l. Geri a tri c Cons i dera ti ons In two s tudi es by the ma nufa cturer, wi th a tota l of 544 pa ti ents, 31% were >65 yea rs of a ge, whi l e 5% were >75 yea rs. Risk C: Monitor therapy Etha nol /Nutri ti on/Herb Intera cti ons Food: Aprepi ta nt s erum concentra ti on ma y be i ncrea s ed when ta ken wi th gra pefrui t jui ce; a voi d concurrent us. As s es s for thera peuti c effecti venes s (decrea s ed na us ea /vomi ti ng) a nd a dvers e rea cti ons (fa ti gue, wea knes s, ga s troi ntes ti na l di s turba nce, dehydra ti on). Denta l Hea l th: Effects on Denta l Trea tmentKey a dvers e event(s) rel a ted to denta l trea tment: Hi ccups, s toma ti ti s, a nd mucous membra ne di s order. In pa ti ents wi th previ ous expos ure to a proti ni n, a dmi ni s ter l oa di ng dos e jus t pri or to ca nnul a ti on. Nurs i ng: Phys i ca l As s es s ment/Moni tori ngMonitor infusion site carefully. Vers tra ete M, "Cl i ni ca l Appl i ca ti on of Inhi bi tors of Fi bri nol ys i s," Drugs, 1985, 29(3):236-61. Dos i ng: Hepa ti c Impa i rmentNo dos a ge a djus tment requi red, but us e ca uti on; s ys temi c drug expos ure prol onged (1. Nurs i ng: Phys i ca l As s es s ment/Moni tori ngAs s es s pa ti ent for us e ca uti ons. Injecti on, s ol uti on, a s hydrochl ori de: R-Gene: 10% (300 mL) [100 mg/mL = 950 mOs m/L; conta i ns chl ori de 0. Argi ni ne conta i ns 475 mEq of hydrogen i ons a nd 475 mEq of chl ori de i ons /L. Pa ti ents were ra ndomi zed to ora l L-a rgi ni ne (ti tra ted to 3 g three ti mes /da y for 6 months) or pl a cebo. Not a pproved for the trea tment of pa ti ents wi th dementi a -rel a ted ps ychos i s. Some prefer to des cri be a nti ps ychoti cs ba s ed on thei r pha rma col ogi ca l properti es. Mos t ca s es ha ve been reported wi thi n the fi rs t 5 weeks of i ni ti a ti ng thera py; however, ra re ca s es ha ve occurred a fter prol onged thera py. Si gns a nd s ymptoms of mul ti orga n hypers ens i ti vi ty rea cti ons a re di vers. Denta l Hea l th: Va s ocons tri ctor/Loca l Anes theti c Preca uti ons Us e va s ocons tri ctor wi th ca uti on. Pa ti ents ma y experi ence hea rt pa l pi ta ti ons a nd i ncrea s ed hea rt ra the when ta ki ng a rmoda fi ni l. Risk C: Monitor therapy Deferoxa mi ne: As corbi c Aci d ma y enha nce the a dvers e/toxi c effect of Deferoxa mi ne. Note: Dos e, frequency, number of dos es, a nd s ta rt da the ma y va ry by protocol a nd trea tment pha s. Nurs i ng: Phys i ca l As s es s ment/Moni tori ngSee i nforma ti on rel a ted to s ki n tes ts a nd des ens i ti za ti on. In event of hypers ens i ti vi ty or hypergl ycemi a, i nfus i on s houl d be s topped a nd pres cri ber noti fi ed i mmedi a tel y. Risk C: Monitor therapy Sel ecti ve Serotoni n Reupta ke Inhi bi tors: Ma y enha nce the a nti pl a tel et effect of As pi ri n. Risk C: Monitor therapy Adenos i ne: Di pyri da mol e ma y enha nce the thera peuti c effect of Adenos i ne. Risk D: Consider therapy modification Al endrona te: As pi ri n ma y enha nce the a dvers e/toxi c effect of Al endrona te.
Order cheapest zydalis
The stents gradually release either sirolimus, an antifungal medication with antimitotic properties, or paclitaxel, an antineoplastic agent erectile dysfunction drugs class purchase zydalis 20 mg amex. From the cardiac literature, restenosis rates using drug-eluting stents were decreased from 30% to about 5%. In small series of 8 to 18 patients, the restenosis rate has ranged from 0% to 14% with 9 to 14 months of follow-up. We have gained some knowledge of the natural history of the disease, and even with current medical therapies, there is a significant risk associated with severe stenosis. Further studies evaluating optimal combinations of medical treatments are needed but, clearly, adjuvant options for higherrisk patients are also a necessity. Reevaluation of open surgical revascularization through bypass surgery is currently ongoing to determine which subset of hemodynamically unstable patients may benefit from surgery. However, with progressively developing endovascular technology, the role of open surgical revascularization may continue to diminish. Evidently, further randomized, prospective studies are required to evaluate and define appropriate management for intracranial atherosclerosis at this juncture. The clinical findings are mainly cerebral ischemia in children and cerebral hemorrhage in Asian adults, but presumably also mainly ischemia in white adults. Its etiology is still unknown despite the accumulation of new molecular biologic and genetic information. Biopsy of the superior laryngeal artery revealed a slight proliferative change in the intima and media. The authors considered the occlusion to be due to congenital hypoplasia causing insufficient collateral circulation to the brain. The term moyamoya (Japanese for "puff of smoke") was coined by Suzuki and Takaku in 1969 to describe the peculiar appearance of the abnormal vasculature at the base of the brain on cerebral angiography. Since its initial discovery some 50 years ago, the clinical features of the disease have become clearer. It has been hypothesized that in the setting of arterial stenosis-occlusion, hypoxic regions of the brain induce deep collateral flow by the dilation of tortuous perforating arteries, namely the moyamoya vasculature. This revascularization phenomenon is thought to be orchestrated by the expression of various angiogenettic signaling cascades. The age at onset had two peaks: a higher peak at 5 years and a lower one around 30 to 49 years. As for the age distribution, the higher incidence was observed in adults 45 to 49 years of age and the second in children 5 to 9 years of age. The tendency for a decrease in the number of children affected in the population might be another reason for these changes. Previously, about 10% of patients had a familial form of the disease, but the recent report indicates an increased incidence of up to 15%. In the United States and Europe, however, familial occurrence has been reported to be less common (less than 6%). In perforating arteries, microaneurysm formation and fragmented elastic lamina have been detected and are considered to be one of the reasons for intracerebral hemorrhage, as discussed later. In addition, elevated serum levels of soluble vascular cell adhesion molecule type 1, intracellular adhesion molecule type 1, and E-selectin and elevated cerebrospinal fluid levels of nitric oxide metabolites or some specific polypeptides have been reported as well. D, Schematic drawing of various moyamoya manifestations: 1, arteria temporalis superficialis; 2, arteria meningea media; 3, arteria temporalis profunda; 4, arteria sphenopalatina; 5, arteria infraorbitalis; 6, arteria facialis. Second report-Collateral routes to forebrain via ethmoidal sinus and superior nasal meatus. In line with our observation and that of other authors, however, cerebral ischemia and not bleeding seems to be the usual manifestation in Europe and the United States. Such hemorrhages often recur, with an annual rebleeding rate of 7%, and a third of patients eventually suffer further hemorrhage after a variable interval (days to years)42-44; the morbidity and mortality associated with these hemorrhages have been reported to be considerable, with only 45% of patients having good neurological recovery and 7% dying. Rebleeding, which often occurs at a location different from the original bleeding site, carries an even graver prognosis: only 20% of patients have a good recovery and nearly 30% die. These peripheral "false" aneurysms located within moyamoya and peripheral arteries can be identified on cerebral angiography and may be the origin of the bleeding. A special type of subarachnoid hemorrhage over the cerebral cortex without any evidence of aneurysm and a fair prognosis has been sporadically but repeatedly reported in adult patients, although its pathophysiology still remains to be clarified. These aneurysms occur in three locations52-56: (1) 60% around the circle of Willis, mainly at the vertebrobasilar territory; (2) 20% in peripheral arteries, such as the posterior and anterior choroidal arteries; and (3) 20% in the abnormal moyamoya vasculature as mentioned earlier. The false aneurysms may disappear spontaneously or after revascularization procedures,52 but they might need to be removed surgically because of repeated bleeding. Caspase-3-dependent apoptosis in middle cerebral arteries in patients with moyamoya disease. Progression from stage 1 to stage 6 has been observed in only a limited number of cases. Perfusion instability detected by measurement of these parameters is supposed to forecast progression of the disease. These parameters can also be used to confirm the effectiveness of surgical revascularization. Acetylsalicylic acid or other antiplatelet drugs are given because studies have revealed that they may have an influence on the progression of vascular stenosis. Currently, there are no clear data indicating definite superiority of either of the methods. The indirect revascularization method is aimed at stimulating the development of new vascular networks and is thought to lead to delayed collateralization, but the extent of revascularization is considered unpredictable, whereas direct revascularization can selectively perfuse ischemic areas immediately but, in so doing, may cause hyperperfusion syndrome as a complication. Common branches used in this technique are the angular, posterior temporal, and posterior parietal arteries. When the entire extent of the frontal branch is dissected, its length is long enough to reach the midline for completion of the anastomotic procedure. Another reason is to facilitate gradual revascularization according to the needs of the ischemic brain so that hyperperfusion secondary to direct revascularization68,69 does not need to be taken into account. The temporalis muscle is considered to be a potential source of collateral circulation over the ischemic brain, and it is appropriately situated anatomically. There are many other variations of procedures consisting of the use of pedicled muscles, galea, periosteum, and the dura mater, combinations of which can be used as novel indirect revascularization methods. For the indirect revascularization method, a rather large craniotomy is recommended in anticipation of a good revascularization. Direct revascularization techniques or combining them with an indirect procedure is considered to be the therapy of choice in adults because indirect methods alone have been reported to be unpredictable or ineffective in achieving good revascularization. However, limited adaptability to social and school life or impairment of neurological soft signs has been reported. The two ages at which the incidence is greatest seem to have changed accordingly: the previous higher peak at 5 years of age and the second lower peak at 40 years of age have recently changed to a lower peak at 5 to 9 years and a higher peak at 45 to 49 years. The clinical findings seem to not have changed: mostly ischemia in children and bleeding in adults. However, ischemia and not bleeding seems to be the predominant manifestation in white adults, in whom the incidence and prevalence are presumed to be far less and around a 10th (in Europe) that in Japanese reports. Perioperative Management When revascularization procedures are carried out, appropriate careful general perioperative management is of cardinal importance. Surgery should be scheduled during a period when the patient is in a relatively stable clinical condition without frequent ischemic episodes. Sufficient hydration should be ensured and the patient never allowed to become dehydrated. Normocapnia should be maintained during surgery along with judicious selection of anesthetic agents. Even preoperative evaluation of hemodynamic dysfunction with acetazolamide (Diamox) loading should be carried out with caution and surgery performed (usually after 48 hours) when the hemodynamic and metabolic situation has stabilized. Seventy-five percent to 80% of cases are thought to have a benign course in terms of life expectancy, with or without surgical treatment. Members of Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ("moyamoya" disease). Possible role of fibroblastic growth factor in the pathogenesis of moyamoya disease. The relevance of hemodynamic factors in perioperative complications in childhood moyamoya disease. Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease.
Order zydalis 20 mg free shipping
In 1980, Bachman and Kim65 first reported dilation of the subclavian artery for the treatment of subclavian steal syndrome erectile dysfunction zinc deficiency buy zydalis once a day. Its main application to the external vertebral artery is for the treatment of atherosclerotic plaque, which most often occurs at the origin of the vertebral artery. However, the vertebral artery origin has a well-developed muscularis and, therefore, the potential for a high risk for restenosis. Additionally, the disease causing the stenosis is usually within the lumen of the subclavian artery, with a large burden of plaque. An ideal Anticoagulation Therapy the treatment of vertebral artery dissection is based on rather incomplete evidence. Anticoagulation with heparin followed by oral anticoagulation therapy remains popular in most centers and is supported by demonstration of emboli as the most common cause of stroke in these patients. This practice is supported by several small case series demonstrating good outcome with low complication rates in patients receiving anticoagulation. Currently, balloon-mounted coronary platform stents are favored because they tend to have the best combination of high outward radial force, limited foreshortening, low crossing profile, and appropriate diameters. The surgical approach to each anatomic segment of the extracranial vertebral artery is different. The outcome of patients undergoing surgery of the external vertebral artery depends on the cause of the disease, the segment of the vertebral artery affected, and the type of treatment performed. In the hands of an experienced surgeon, surgery is associated with a very low mortality rate, and life expectancy is not substantially different from that of the general population with cerebrovascular and peripheral vascular disease, at about 50% survival at 10 years. Berguer and associates84 used vein grafts in this region of the vertebral artery to connect the subclavian artery to the proximal vertebral artery. The treatment of penetrating vertebral artery injuries also changed significantly with the advent of the Vietnam War. Surgeons no longer relied solely on ligation of the artery as treatment; in many cases, they actually reconstructed the vertebral artery. Endarterectomy of the Dissection In rare patients with symptoms refractory to medical management and in those with expanding dissecting aneurysms, endovascular therapy may be indicated. Endovascular therapy is an alternative to surgery as the initial therapy of choice when medical therapy fails or is contraindicated. Associated dissecting aneurysm may require coil embolization or the deployment of a covered stent. Berguer77 detailed the long-term outcome and experience with surgery of the proximal vertebral artery. Approach to the Proximal Vertebral Artery the standard approach to the proximal vertebral artery is a supraclavicular approach. A supraclavicular incision is made about 2 cm above and parallel to the clavicle and extends from the suprasternal notch to 7 to 8 cm laterally. C, the clavicular head is divided, leaving a cuff on the clavicle, and the muscle is retracted superiorly and laterally. The omohyoid muscle can also be divided (not shown) to expose the vascular contents and thoracic duct. D, the carotid is dissected and retracted medially, and the internal jugular and vagus nerve are retracted laterally, exposing the thoracic duct and superior aspect of the subclavian artery. E, the thoracic duct is ligated, and the vertebral artery is identified at the apex of the insertion of the anterior scalene and longus colli into the C6 tubercle. F, the vertebral artery is ligated proximally, and the carotid artery is rotated in preparation for anastomosis. The superficial veins flank the edge of the sternocleidomastoid muscle with the external jugular vein lying at the lateral edge. The sternocleidomastoid muscle has two origins: the clavicular head from the superior surface of the medial third of the clavicle, and the sternal head from the anterior surface of the manubrium of the sternum. The clavicular head is divided, leaving a cuff on the clavicle, and the muscle is retracted superiorly and laterally. The anterior scalene muscle lies laterally, with the phrenic nerve lying on top of it. The lymphatic drainage on the right side of the neck is different from that on the left. Delicate lymphatic trunks empty into the right subclavian and jugular veins, which are usually smaller than the lymphatic ducts on the left. Because they do not coagulate completely, it is better to identify and ligate them. The right recurrent laryngeal nerve exits the vagus nerve and loops below the right subclavian artery as it approaches the trachea and larynx. Consequently, medial retraction of the trachea can cause ipsilateral paresis of the vocal cord. If the left side is exposed, the thoracic duct is encountered as it arches from the side of the esophagus laterally to the angle between the internal jugular and subclavian veins. The proximal portion of this duct is ligated twice, and smaller branches are also ligated. The left recurrent laryngeal nerve can be retracted with greater ease because it loops around the aortic arch and approaches the trachea much lower. This feature distinguishes it from the thyrocervical trunk, which has multiple branches and exits from the anterosuperior surface. Alternatively, and more easily, the vertebral artery can be first located superiorly as it exits the transverse foramen of C6. The artery arises from the apex of two muscles as they attach to the carotid tubercle: the anterior scalene muscle and the longus colli. The vertebral vein is formed at the lower end of the canal of the transverse foramina from a venous plexus within the canal around the vertebral artery. Care is taken to avoid destroying the sympathetic trunks and stellate or intermediate ganglia that lie on it. If the vertebral artery is not lax enough, it may be necessary to remove it from the C6 transverse process. A double-ended fish-mouth opening is made in the proximal end of the vertebral artery. An occluding clamp is placed on the carotid artery at the selected level and used to rotate the vessel laterally. With 7-0 monofilament nylon suture, the superior and inferior ends of the fish-mouth opening are sutured to the corresponding ends of the hole in the carotid artery. One suture is used to form a running anastomosis on the back wall and is tied to the opposite end on completion. Before the last suture is tied, the lumens of both arteries are flushed with heparinized saline. If blood continues to ooze, gentle pressure is placed over the anastomosis with Gelfoam. After copious irrigation and hemostasis, the sternocleidomastoid muscle is reapproximated. A suction drain is placed in the neck for 24 hours, and the neck opening is closed in multilayers. Alternative Transpositions and Vein Graft to the Proximal Vertebral Artery If the carotid artery is stenotic or otherwise compromised, the subclavian artery can be used. The desired segment of the subclavian artery is in the area of the anterior scalene muscle or more distally. Its limitation, however, is the requirement for simultaneous occlusion of both carotid and vertebral arteries. Five minutes later, the vertebral artery is clamped at the level of C6 with a temporary clip. A, Angiogram reveals severe stenosis (arrow) of the right vertebral artery origin (anteroposterior view). The patient underwent vertebral-carotid transposition with resolution of his symptoms. B, Postoperative angiogram (oblique view) reveals transposed vertebral (arrow) filling from the carotid injection. Although this procedure does not interrupt carotid blood flow, it requires two anastomoses and is time consuming. The vein is usually autogenous saphenous vein, although prosthetic materials have been used. The proximal vertebral artery can be also be transposed from the subclavian artery to the thyrocervical trunk.
Purchase zydalis with amex
Such suppression reduces energy requirements, and a reduction in energy requirements should allow tissue to better preserve energy balance during transient interruption of substrate delivery erectile dysfunction 16 purchase 20 mg zydalis overnight delivery. The beneficial effect of barbiturates in the treatment of experimental focal cerebral ischemia is well documented. Although the retrospective, nonrandomized, historical control study design does not allow a definitive statement regarding the benefit of these agents or a comparison of them, it is the best evidence to date demonstrating a protective effect with their use during temporary intracranial vessel occlusion. Cytoprotective Agents Within the past few years, a variety of pharmacologic agents have been developed that interfere with biochemical mediators of the ischemic cascade. Drug development has been directed toward pharmaceuticals that will protect patients with acute ischemic stroke. It seems intuitive, however, that if a drug proves beneficial when given several hours after the onset of ischemic stroke, the same drug might be protective if given at or just before the onset of focal ischemia during cerebrovascular surgery. Magnesium has reduced the extent of infarction in several experimental models and has a long history of safe use in humans. Additional clinical trials have failed to show efficacy in the treatment of acute stroke. Administration of citicoline has been associated with reduced infarct volume in animal models of focal ischemia. Phenytoin can be administered to patients undergoing supratentorial surgery for its anticonvulsant effect, and mannitol can be given at incision for decompression, as needed, but not specifically during occlusion. If possible, occlusion is performed in an intermittent fashion on the basis of time limitations or electrophysiologic evidence of altered function. Why we still use intravenous drugs as the basic regimen for neurosurgical anaesthesia. Transient changes in cortical glucose and lactate levels associated with peri-infarct depolarisations, studied with rapidsampling microdialysis. Is routine intraoperative angiography in the surgical treatment of cerebral aneurysms justified Comparison of routine and selective use of intraoperative angiography during aneurysm surgery: a prospective assessment. Clinical usefulness and safety of routine intraoperative angiography for patients and personnel. Disruption of ionic and cell volume homeostasis in cerebral ischemia: the perfect storm. Hyperglycemia in patients undergoing cerebral aneurysm surgery: its association with long-term gross neurologic and neuropsychological function. Some new prospects in the understanding of the molecular basis of the pathogenesis of stroke. Comparison of endovascular and surface cooling during unruptured cerebral aneurysm repair. Conditions of protection by hypothermia and effects on apoptotic pathways in a rat model of permanent middle cerebral artery occlusion. Studies elucidating the biochemical mechanisms underlying ischemic injury have provided potential sites for modulation of these pathologic events. Although a wide variety of pharmacologic agents have shown beneficial effects in reducing infarct volume in laboratory animals, translating these successes to the clinical sphere has been complicated by toxic side effects and inconsistent results. Immaculate surgical technique, proper use of the numerous intraoperative tools available, better understanding of the mechanisms of ischemia-induced cell injury, and the use of specific cytoprotective agents that disrupt the ischemic cascade will make cerebrovascular surgery safer. Evaluation of extracranial-intracranial bypass using quantitative magnetic resonance angiography. Oncosis, the possible cell death pathway in astrocytes after focal cerebral ischemia. Assessment of flow in perforating arteries during intracranial aneurysm surgery using intraoperative near-infrared indocyanine green videoangiography. Lovastatin induces neuroprotection through tumor necrosis factor receptor 2 signaling pathways. Sander Connolly Jr Most aneurysms are amenable to endovascular or traditional microsurgical treatment with general neurovascular anesthesia. However, there is a small subset of aneurysms that present the surgeon with an unusually complex technical challenge, and pose a higher risk of surgical morbidity and mortality when traditional techniques are employed. Circumferential dissection or freeing of adhesions may be impossible with a full, tense dome. Further, calcified or thrombosed aneurysms may be impossible to occlude with a clip without first removing thrombus or calcified components from inside of the aneurysm. To more safely manipulate such complicated aneurysms, three main strategies have evolved to reduce pressure within the aneurysm dome: systemic hypotension, temporary clipping of major arterial branches, and complete or low-flow circulatory arrest. Systemic hypotension is largely avoided because of the risks associated with hypoperfusion to other organ systems and normal cerebral tissue. Focal hypotension with temporary clipping is used for proximal control in most aneurysms, yet is subject to significant limitations related to time of tolerance and inadequate cessation of flow. Therefore, in conjunction with highly skilled cardiothoracic surgeons and anesthesiologists, neurosurgeons have developed techniques to approach complicated aneurysms under total circulatory arrest or lowflow cardiopulmonary bypass with hypothermic cerebral protection. Complete circulatory arrest converts a tense, large aneurysm into a soft, collapsed sac whose adjacent perforating arteries and total anatomy may be more easily visualized and manipulated. Deep hypothermic circulatory arrest for aneurysm clipping was first employed more than 50 years ago. Initially, the technique carried an unacceptably high incidence of systemic complications, limiting its application to neurosurgery. Coupled with a better understanding of cerebral physiology under hypothermic conditions, these techniques have enabled neurosurgeons to approach otherwise untreatable complex cerebral aneurysms with acceptable morbidity and mortality. Deep hypothermic circulatory arrest is still a relatively high-risk procedure, however, and must performed for appropriate indications at centers able to provide sophisticated neurosurgical and cardiothoracic care. The morbidity and mortality must be weighed against the surgical risks of treating complicated intracerebral aneurysms with traditional techniques. Additionally, temporarily trapped arterial segments may be subject to intravascular thromboembolism. Finally, a steal phenomenon may occur if a hole is created in the aneurysm while the vessel is temporarily proximally occluded, further exacerbating ischemic intolerance. If the penumbral zone continues without perfusion, it too is progressively recruited into the ischemic core. Over time the penumbra is exposed to increasing concentrations of toxic neurotransmitters, such as glutamate and nitric oxide released from the actively infarcting ischemic core, which lead to cellular depolarization and spreading neuronal death. So when the same noxious stimulus is applied at or above the threshold of damage, the tissue is resistant to or protected from injury. Preconditioning has been studied in ischemic stroke, carotid endarterectomy, and myocardial infarction, but has yet to find evidence-supported therapeutic application in these diseases or the ischemia induced in aneurysm surgery. Propofol and isoflurane, for example, are shorter acting and produce less myocardial depression than barbiturates. Several groups have examined drugs that act by interfering with the toxic events that follow ischemia and deranged ion flux, including free radical scavengers, calcium channel blockers, and glutamate receptor blockers. Recent evidence suggests it may unnecessarily increase cerebral blood volume, swelling, and intracranial pressure that may be successfully avoided by titrating ventilation to uncorrected gases. The anesthesiologist must therefore counteract the changing viscosity by aggressive isovolemic hemodilution to preserve the integrity of the microcirculatory bed, with the final hematocrit titrated approximately to temperature. Metabolic acidosis can then lead to dilation of cerebral vasculature and increased cerebral blood flow, which may be important in the setting of cerebral edema. Endogenous corticosteroid production may be diminished after prolonged hypothermia, necessitating perioperative replacement and continued hypothalamic-adrenal axis surveillance for up to a year. Profound hypothermia can occasionally cause a complement-mediated pneumonitis, which may necessitate prolonged postoperative intubation. Though frank hepatic dysfunction is extraordinarily rare, hypothermia can lead to mild hepatic dysfunction with decreased dilantin metabolism and resultant supratherapeutic levels.
Proven 20 mg zydalis
Medi ca ti on Sa fety Is s ues Duplicate therapy issues: Thi s product conta i ns a ceta mi nophen, whi ch ma y be a component of other combi na ti on products erectile dysfunction pills comparison best order for zydalis. Al ka -Sel tzer Pl us Da y Col d, Tyl enol Col d Hea d Conges ti on Da yti me, Tyl enol Col d Mul ti -Symptom Da yti me, Vi cks Da yQui l Col d/Fl u Mul ti Symptom Rel i ef Li qui Ca ps: Chi l dren 12 yea rs: Refer to a dul t dos i ng. Cough suppressant: Ora l: Ba s ed on dextromethorpha n component: Chi l dren 6-12 yea rs: 15 mg every 6-8 hours; do not exceed 60 mg/24 hours Chi l dren >12 yea rs: Refer to a dul t dos i ng. Decongestant: Ora l: Ba s ed on ps eudoephedri ne component: Chi l dren: 2-6 yea rs: 15 mg every 4 hours (ma xi mum: 90 mg/24 hours) 6-12 yea rs: 30 mg every 4 hours (ma xi mum: 180 mg/24 hours) Chi l dren >12 yea rs: Refer to a dul t dos i ng. Product labeling: Sudafed Severe Cold, Thera-Flu Non-Drowsy Maximum Strength (gelcap), Tylenol Flu Non-Drowsy Maximum Strength: Ora l: Chi l dren >12 yea rs: Refer to a dul t dos i ng. Tylenol Cold Non-Drowsy: Ora l: Chi l dren 6-11 yea rs: 1 dos e every 6 hours (ma xi mum: 4 dos es /24 hours) Chi l dren 12 yea rs: Refer to a dul t dos i ng. Thera-Flu Non-Drowsy Maximum Strength: Ora l: Chi l dren >12 yea rs: Refer to a dul t dos i ng. Medi ca ti on Sa fety Is s ues Duplicate therapy issues: Thi s product conta i ns a ceta mi nophen, whi ch ma y be a component of combi na ti on products. Index Terms Aceta mi nophen, Phenyl ephri ne, a nd Di phenhydra mi ne; Di phenhydra mi ne, Phenyl ephri ne Hydrochl ori de, a nd Aceta mi nophen; Phenyl ephri ne Hydrochl ori de, Aceta mi nophen, a nd Di phenhydra mi ne Copyri ght (c) Lexi -Comp, Inc. Ca pl et: Aceta mi nophen 500 mg a nd di phenhydra mi ne hydrochl ori de 25 mg Excedri n P. Index Terms Phenyl ephri ne Hydrochl ori de a nd Aceta mi nophen Copyri ght (c) Lexi -Comp, Inc. Di eta ry Cons i dera ti ons Suda fed Mul ti -Symptom Si nus a nd Col d ca ps ul e conta i ns a ceta mi nophen 325 mg, ps eudoephedri ne hydrochl ori de 30 mg, a nd s odi um 16 mg. Dos i ng: Rena l Impa i rmentCl cr <30 mL/mi nute: Ma xi mum of 2 ta bl ets every 12 hours. Ca l cul a ti ons Crea ti ni ne Cl ea ra nce: Adul ts Di eta ry Cons i dera ti ons Ma y be ta ken wi th or wi thout food. Duplicate therapy issues: Thi s product conta i ns a ceta mi nophen, whi ch ma y be a component of combi na ti on products. Dos i ng: Rena l Impa i rment Cl cr 10-50 mL/mi nute: Admi ni s ter every 6 hours. Ca l cul a ti ons Crea ti ni ne Cl ea ra nce: Adul ts Crea ti ni ne Cl ea ra nce: Pedi a tri cs Admi ni s tra ti on: Ora l Sha ke s us pens i on wel l before pouri ng dos. Risk D: Consider therapy modification Is oni a zi d: Ma y enha nce the a dvers e/toxi c effect of Aceta mi nophen. Ameri ca n Col l ege of Rheuma tol ogy Subcommi ttee on Os teoa rthri ti s Gui del i nes," Arthritis Rheum, 2000, 43(9):1905-15. Glaucoma: Ora l: 8-30 mg/kg/da y or 300-900 mg/m 2 /da y di vi ded every 8 hours I. Dos i ng: Rena l Impa i rment Cl cr 10-50 mL/mi nute: Admi ni s ter every 12 hours. Al terna ti vel y, s ubmerge ta bl et i n 10 mL of hot wa ter a nd a dd 10 mL honey or s yrup. Aceta dote Dos i ng / Fl ui d Vol ume Gui del i nes for Pa ti ents <40 kg Loading Dose Body Weight (kg) 150 mg/kg over 1 h D5W (mL) 100 100 60 45 30 Second Dose 50 mg/kg over 4 h D5W (mL) 250 250 140 105 70 Third Dose 100 mg/kg over 16 h D5W (mL) 500 500 280 210 140 Acetadote (mL) Acetadote (mL) 7. Infa nts: 1-2 mL of 20% s ol uti on or 2-4 mL 10% s ol uti on unti l nebul i zed gi ven 3-4 ti mes /da y Chi l dren: Refer to a dul t dos i ng. Inhalation, nebulization (tent, croupette): Chi l dren: Refer to a dul t dos i ng. Intra venous formul a ti on (Aceta dote): Admi ni s ter l oa di ng dos e of 150 mg/kg over 60 mi nutes (s ee "Note"), fol l owed by 2 s epa ra the ma i ntena nce i nfus i ons: 50 mg/kg over 4 hours fol l owed by 100 mg/kg over 16 hours. Di l ute the 20% s ol uti on 1:3 wi th a col a, ora nge jui ce, or other s oft dri nk. A Ra ndomi zed Compa ri s on of 3 Preventi ve Stra tegi es," Circulation, 2007, 115(10):1211-17. Boxed Warning]: All patients (male and female) should abstain from ethanol or ethanol-containing products during therapy and for 2 months after discontinuation. Boxed Warning]: Not for use by women who are pregnant or want to become pregnant; patient should not get pregnant for at least 3 years after discontinuation. Boxed Warning]: All patients should be advised not to donate blood during therapy or for 3 years following completion of therapy. Boxed Warning]: All patients must be provided with a medication guide each time acitretin is dispensed. Severe bi rth defects ha ve been reported when concepti on occurred duri ng trea tment or a fter thera py wa s compl ete. Risk X: Avoid combination Methotrexa te: Aci treti n ma y enha nce the hepa totoxi c effect of Methotrexa te. Risk X: Avoid combination Vi ta mi n A: Ma y enha nce the a dvers e/toxi c effect of Reti noi d-l i ke Compounds. Ons et: Ma y ta ke 2-3 months for ful l effect; i mprovement ma y be s een wi thi n 8 weeks. Ca l cul a ti ons Body Surfa ce Area: Adul ts Body Surfa ce Area: Pedi a tri cs Crea ti ni ne Cl ea ra nce: Adul ts Crea ti ni ne Cl ea ra nce: Pedi a tri cs Idea l Body Wei ght: Adul ts Idea l Body Wei ght: Pedi a tri cs Admi ni s tra ti on: I. Da ta from the pregna ncy regi s try ma y be obta i ned from Gl a xoSmi thKl i ne. Pha rma codyna mi cs /Ki neti cs Abs orpti on: Ora l: 15% to 30% Di s tri buti on: Vd: 0. Boxed Warnings]: Patients should be evaluated for latent tuberculosis infection with a tuberculin skin test prior to therapy. Dos i ng: Pedi a tri cHepa ti ti s B (chroni c): Ora l: Chi l dren 12 yea rs: Refer to a dul t dos i ng. Ca l cul a ti ons Crea ti ni ne Cl ea ra nce: Adul ts Admi ni s tra ti on: Ora l Ma y be a dmi ni s tered wi thout rega rd to food. Ma y ca us e hea da che or a bdomi na l pa i n (cons ul t pres cri ber for a pproved a na l ges i a); or na us ea or vomi ti ng (s ma l l, frequent mea l s, frequent mouth ca re, s ucki ng l ozenges, or chewi ng gum ma y hel p). Dos i ng: Pedi a tri c Paroxysmal supraventricular tachycardia (Adenocard): Ra pi d I. Note: Hi gher dos es ma y be needed for a dmi ni s tra ti on vi a peri phera l vers us centra l vei n. Geri a tri c Cons i dera ti ons El derl y pa ti ents ma y be more s ens i ti ve to the effects of thi s medi ca ti on. Approxi ma tel y 60% of thes e pa ti ents a re free of a nti bodi es a nd >80% demons tra the i mmune tol era nce, ba s ed on reduced ti ters of a nti body wi thi n 12-18 months. Pa ti ents wi th a hi s tory of rea cti ons ma y be premedi ca ted wi th ora l corti cos teroi ds a nd a nti hi s ta mi nes 1-3 hours pri or to s ubs equent i nfus i ons. Pa ti ent s houl d be moni tored for i nfus i on rea cti ons duri ng a nd fol l owi ng i nfus i ons. Nurs i ng: Phys i ca l As s es s ment/Moni tori ngAs s es s pa ti ent for previ ous experi ence wi th enzyme repl a cement thera py pri or to begi nni ng thera py. The vol ume a dmi ni s tered a nd the s peed of i nfus i on s houl d be a da pted to i ndi vi dua l res pons. Do not us e wi th etha nol or protei n hydrol ys a tes, preci pi ta ti on ma y form. If a dvers e rea cti ons (eg, fever, ta chyca rdi a, hypotens i on, or dys pnea) occur, i nfus i on s houl d be s topped a nd pres cri ber noti fi ed. Bronchos pa s m (trea tment): Ora l: 2 mg 3-4 ti mes /da y; ma xi mum: 8 mg 4 ti mes /da y Dos i ng: Pedi a tri c Bronchospasm: Oral, regular release: Chi l dren 2-6 yea rs: 0. Sol uti on for nebul i za ti on: Concentra ted s ol uti on s houl d be di l uted pri or to us. Di eta ry Cons i dera ti ons Ora l forms s houl d be a dmi ni s tered wi th wa ter 1 hour before or 2 hours a fter mea l s.