Buy generic ceftin 500mg online
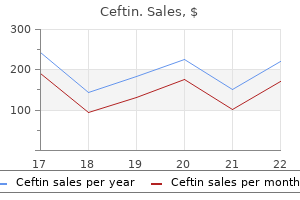
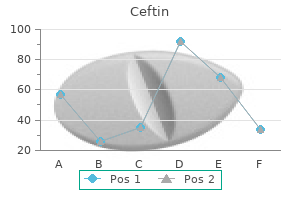
Patients may be assessed for weight-bearing after 1 hour under direct supervision antibiotics that cover mrsa buy discount ceftin 250mg online, and limits to ambulation may be determined by patient pain and degree of underlying bone destruction. Serious toxicities occurred in three patients (5%), including solitary cases of local pain, neuropathic pain, and foot drop. Pain relief was durable through the 24-week follow-up period in 80% of the patients who reported excellent pain relief at the immediate postablation time point. Furthermore, eight of eight patients who were prescribed opioid analgesics prior to the procedure reduced their doses following cryoablation. A low attenuation ice ball surrounds the tip of one of two cryoprobes early (B) and late (C) during treatment of the tumor. Cementoplasty was performed to add structural support to this important weight-bearing region. No significant complication occurred, although two patients terminated treatment prematurely due to sonication-related pain. A small study of five patients by Hierholzer and colleagues54 found cementoplasty alone to significantly reduce pain from skeletal metastases, including three patients with tumors in nonaxial skeletal locations. Ethanol Ablation In a series of 27 painful bone metastases treated in 25 patients with one to three doses of 3 to 25 mL of 95% ethanol, Gangi and colleagues45 reported complete pain relief in 3 patients, 75% reduction in analgesics in 10 patients, 25% to 50% reduction in 5 patients, and minimal or no relief in 7 patients as measured 24 to 48 hours following the procedure. One serious complication occurred, specifically weakness after treatment of a vertebral metastasis extending into the brachial plexus. The risks during device placement are similar to other percutaneous needle insertion procedures, allowing for the relatively large caliber of bone access needles or drills. Thermal damage to the normal structures described previously may result in nerve dysfunction, bowel or bladder perforation, infection, skin burns, or tumor/fistula formation. These complications are minimized through measures to displace or insulate critical structures as well as intraprocedural monitoring with imaging and thermocouples. Cementoplasty Cementoplasty may be performed as solitary treatment or in combination with ablative therapy in the treatment of painful metastatic disease involving bone. Small pneumothorax during cryoablation of T2 vertebral body metastasis from renal cell carcinoma in a 51-year-old man required smallcaliber chest tube drainage overnight. Active contrast extravasation (arrow) into a moderate-sized prevesical hematoma immediately following cryoablation of a pubic body metastasis from papillary thyroid carcinoma in a 59-year-old man. Femoral neuropathy in a 58-year-old woman resulted from cryoablation of a psoas muscle metastasis from melanoma during which the ice ball encompassed the femoral nerve (arrow). Cement extravasation following combined ablation and cementoplasty of a painful periacetabular metastasis from renal cell carcinoma in a 71-year-old man. Percutaneous thermal and chemical ablative therapies can effectively treat these metastases in carefully selected patients. Cementoplasty is a useful adjunct in treating lesions at risk for pathologic fracture caused by axial loading and may even have direct analgesic effects when used alone. Several adjunctive techniques allow safe treatment of metastases even in relative proximity to normal critical structures. Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. Delay in progression of bone metastases in breast cancer patients treated with intravenous pamidronate: results from a multinational randomized controlled trial. A randomized, controlled trial of intravenous clodronate in patients with metastatic bone disease and pain. Effect of oral clodronate on metastatic bone pain: a double-blind, placebo-controlled study. The palliation of symptomatic osseous metastases: final results of the Study by the Radiation Therapy Oncology Group. A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bone metastases. Pain relief and quality of life following radiotherapy for bone metastases: a randomised trial of two fractionation schedules. A randomized trial of three single-dose radiation therapy regimens in the treatment of metastatic bone pain. Prospective randomised trial of single and multifraction radiotherapy schedules in the treatment of painful bony metastases. Radiofrequency ablation of spinal tumors: temperature distribution in the spinal canal. Image-guided ablation of painful metastatic bone tumors: a new and effective approach to a difficult problem. Percutaneous radiofrequency ablation of painful osseous metastases: a multicenter American College of Radiology Imaging Network trial. Percutaneous radiofrequency ablation with a multiple-electrode switching-generator system. Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences Image-guided percutaneous thermal ablation for the palliative treatment of chest wall masses. Lethal isotherms of cryoablation in a phantom study: effects of heat load, probe size, and number. Percutaneous imageguided radiofrequency ablation of painful metastases involving bone: a multicenter study. Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Radiofrequency ablation of bone metastases induces long-lasting palliation in patients with untreatable cancer. Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. Combined cementoplasty and radiofrequency ablation in the treatment of painful neoplastic lesions of bone. Combined radiofrequency thermal ablation and percutaneous cementoplasty treatment of a pathologic fracture. Radiofrequency ablation therapy combined with cementoplasty for painful bone metastases: initial experience. Percutaneous osteoplasty as a treatment for painful malignant bone lesions of the pelvis and femur. Such treatment has been used mostly as salvage therapy after failure of standard of care systemic therapies. Additionally, this treatment is also being considered because response rates remain largely positive even in situations when the same drug that was used systemically and failed to elicit any kind of response is used intra-arterially. The goal of such therapies in first line, typically referred to as induction therapy, is to obtain the highest response as early as possible in the disease to downstage a nonsurgical candidate to a surgical candidate. At the time of diagnosis 20% are present and 30% to 50% will appear later in the course of the disease. Even if surgery is the best treatment option for liver metastases, it will be possible in only 20% of patients. Consequently, it is not surprising that systemic chemotherapy is the dominant form of therapy for patients with liver metastases. The advantage of such an intra-arterial approach is directly related to the first-pass extraction of the drug by the liver and inversely proportional to the body clearance of the drug. As a result, a permanent and easy access route had to be obtained using a port linked to an intra-arterial catheter. Furthermore, a femoral access will most often be needed for endovascular flow remodeling, even if the indwelling catheter is inserted through the axillary arterial route. Second, those arteries not providing flow to the liver (such as those feeding the stomach, duodenum, or pancreas) that arise between the perfusion hole in the catheter and the liver must be permanently occluded to avoid toxicity resulting from extrahepatic drug perfusion. In clinical practice, the gastroduodenal artery and the right gastric artery are the more frequent arteries requiring endovascular occlusion because it is rarely possible to place the perfusion hole of the catheter downstream of these two arteries. Occlusion of the right gastric artery is considered to be critically important to minimize toxicity from the infused drug to the liver as discussed in the results section. First, it is sometimes difficult to visualize the right gastric artery on hepatic artery angiography; second, it can arise from several places between the common hepatic artery and the distal part of the left branch of the hepatic artery. When its origin cannot be seen on the hepatic artery angiogram, it is often useful to perform selective angiography of the left gastric artery.
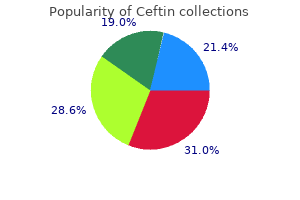
Buy 250mg ceftin with mastercard
The combined study groups demonstrated a duplex restenosis rate of 24% with a mean lesion length of over 10 cm antimicrobial infection purchase generic ceftin online. Both groups experienced functional outcome improvement as well with significantly improved treadmill study in 88% of patients. A retrospective study of mid-length lesions (mean >10 cm) with duplex follow-up appears to show an approximately 40% restenosis rate at 2 years. This potential use stemmed from the successful utilization of these devices for the treatment of aneurysmal disease. The early covering materials, such as Dacron, seem to elicit a significant inflammatory response with associated poor patency and high thrombosis rates. Complete neointimal formation has been documented although for long-segment disease, this process may take many months. The tibial outflow status and treatment were significantly different between these two groups. Interestingly, even with the concern of covering potential collaterals, no difference was seen at 1 or 3-year follow-up. For lesions over 15 cm stent fractures were common in the bare nitinol stent groups whereas rare in the stent-graft group. Two randomized trial publications using balloon catheters coated with paclitaxel demonstrated encouraging results when compared to uncoated balloons. In a second study, 87 patients were randomized to bare balloon versus paclitaxel-coated balloon, and in mean lesion lengths ranging from 5. Many trials using different drug and coating technologies are currently being planned. These investigations may result in a significant alteration in treatment strategies for patients with femoropopliteal artery disease. In the first trial the addition of the sirolimus to a self-expanding nitinol stent using a polymer base demonstrated early but not sustained significant benefit possibly due to problematic drug elution rates and better-than-expected results with bare nitinol stents. Early procedural failure may be related to lack of periprocedural anticoagulation or patient-specific coagulation abnormalities. Early technical issues that may lead to failure include suboptimal lesion dilation, stent-graft oversizing leading to material redundancy, and unrecognized proximal or distal dissection. Appropriate sizing of balloons, stents, and stent-grafts and covering all dilated areas with stents or stent-grafts may minimize these failures. An intermediate time for procedural failure (6 to 24 months) is most commonly caused by excessive intimal hyperplasia at the site of intervention. Bare metal stents typically restenoses diffusely, whereas stent-grafts more commonly restenosed at the leading edge. Late failure is most often secondary to progression of proximal or distal vascular occlusive disease. Although some profess that the main reason to refrain from stenting is the ease of re-treatment after angioplasty or atherectomy, one must remember that restenosis is a multifaceted process. This process includes recoil, intimal hyperplasia, and, most importantly, vascular atresia. In-stent restenosis can be especially difficult to treat, however, because of the dense nature of the intimal hyperplasia. To date treatment of in-stent restenosis with plain balloon angioplasty, cutting balloon angioplasty, and cryoplasty have not demonstrated efficacy. It is hoped that drug-coated balloons or drug-coated stents may improve the current results. Further in the future bioabsorbable stents have started to demonstrate early efficacy in the coronary vascular bed. This large, randomized, multicenter, international trial demonstrated 1- and 2-year primary patency rates of over 80% as well as a 3-year freedom from repeat revascularization rate of 83%. This represents a 50% reduction in restenosis over both balloon angioplasty and bare metal stents. The common femoral artery is typically large enough for even the larger sheaths available and usually offers a readily compressible site for postprocedure homeostasis. When utilizing retrograde vascular access for contralateral procedures the choice of sheath is important. Previous aortobi-iliac or bifemoral bypass may make it difficult or impossible to utilize the contralateral femoral access due to the severity of the bifurcation angulation. Utilization of Plexiglas protection, placed over the head of the patient, may allow for a simplified working field. Antegrade access may be very problematic and occasionally unfeasible in the obese patient. This approach is usually reserved for total occlusions that have not been able to be traversed from a more cephalad approach. The popliteal artery lies deep in the popliteal space with a vein that lies posterior and slightly lateral. The artery should be entered above the joint line to decrease the chance of bleeding into the joint space. Popliteal hematomas are often very symptomatic and the development of compartment syndrome is a significant consideration. After definition of the anatomic landmarks on fluoroscopy, the vessel is effectively located for needle entry by utilizing duplex ultrasound or a Doppler probe. If a more cephalad sheath is in place, angiography or "road mapping" may also define the vessel. With the recent development of effective reentry type and total occlusion devices, the need for popliteal access has diminished considerably. Although possibly more important for stent-grafts, inflow is important for any endovascular femoropopliteal procedure. Status of distal runoff vessels has been shown to affect the durability of endovascular procedures. Intervention with 2- to 3-vessel distal runoff is associated with significant improvement in patency compared to patients with 0- to 1-vessel runoff. Special attention to oral antiplatelet therapy may be beneficial, although comparative data are lacking. The objective is to create a subintimal dissection plane proximal to occlusion, through the subintimal space, and then reenter into the true lumen at the distal portion of the lesion. The theory behind utilizing the subintimal channel is that it is free from endothelium and atheroma that can invite thrombus and neointimal hyperplasia to accumulate. The first category of devices is designed to stay in the true vessel lumen, whereas the second category of devices is generally thought of as reentry devices. Use of the reentry devices allows for successful crossing of all but the most heavily calcified lesions. Before deciding on the optimal invasive approach, the etiology of the femoropopliteal occlusion should be evaluated. The differential diagnosis most commonly includes atherosclerotic thrombosis, embolization, aneurysmal thrombosis, and, more rarely, arterial entrapment, adventitial cystic disease, and traumatic dissection. Atherosclerotic occlusions typically include an eccentric plaque that generally starts on the back wall. Collateral flow around the occlusion may lead the operator to overestimate the occlusion length. Prior to gaining vascular access the operator should evaluate which major side branches or collaterals should optimally not be compromised. The preferable access and wire direction as well as evaluating the extent of disease at the reentry segment should then be completed. If the arterial vessel at the site of reconstitution has little disease then the wire will typically reenter spontaneously; however, if there is significant disease then reentry will be more problematic. Angioplasty has been the cornerstone of therapy but randomized trials have demonstrated superiority of both stents and stentgrafts. However, patency of bare metal stents and stent-grafts is still suboptimal and techniques of successfully treating restenosis have yet to be defined. Other, more niche techniques have been successfully utilized but currently there are no randomized data to allow us to compare to angioplasty or stents. Facing the diabetes epidemic-mandatory reporting of glycosylated hemoglobin values in New York City.
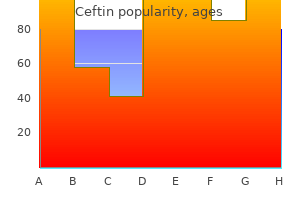
Purchase ceftin 250mg free shipping
When measuring velocity of an angular object antibiotics make acne better cheap ceftin 500 mg overnight delivery, such as blood flow through a blood vessel, the angle between the transducer and the direction of flow needs to be incorporated into the formula: fd = 2ft*cos *v/c = the angle between the ultrasound beam and the direction of flow the measuring angle should be 60 degrees or less due to several factors: 1. At an angle below 60 degrees the ultrasound beam scatter from the vessel walls increases, making it less efficient. Angles above 60 degrees are not recommended because small errors in angle measurement may result in large errors in velocity estimation due to the dependency on the cosine in the equation. Practically, an angle of 60 degrees is used most often because it is the easiest to accomplish and most reproducible between observers. Duplex ultrasound offers a combination of two-dimensional gray scale imaging of vascular structures, color-coding of blood flow, and Doppler-derived velocity and direction. Correct clinical interpretation and use of ultrasound technology mandates first understanding its basic principles. Ultrasound utilizes the reflection of high-frequency sound waves from various structures to create a two-dimensional image of these structures (this is called B-mode, or brightness mode). The Doppler effect is used to measure movement in a sampled volume, such as that of blood flow. Measuring Velocity-The Doppler Effect When sound waves reflect off a moving object, the frequency of the reflected wave is deferent than that of the transmitted one. In audible terms, this phenomenon may be encountered while observing a moving car passing by a stationary observer. As the car nears and then passes, the pitch (or rather, frequency) of its engine sound seems to change. This change is known as the Doppler shift frequency: Ultrasound Technology Medical ultrasound transducers emit high-frequency sound waves that are produced by piezoelectric materials. When subjected to electric currents, piezoelectric materials (crystals) vibrate at a rate that corresponds to the electric current frequency. Higherfrequency transducers tend to produce a more defined image, whereas lower-frequency transducers penetrate deeper into tissue while sacrificing image quality. Sound waves need to travel to the selected tissue and back before a new pulse can be triggered; otherwise two pulses will overlap. Spectral waveform analysis-Blood flowing through a blood vessel has a velocity but also a mass. The more the number of blood cells flowing through a measured area, the stronger the signal amplitude picked up by the detector. As opposed to spectral waveform analysis, color flow is an imaging tool that presents frequency shift estimates (as opposed to accurate measurements) in real time and in color. Flow direction and velocity are depicted as color hue and intensity, typically on a spectrum of red and blue. Modern duplex ultrasound equipment, however, allows the technologist to alter the color "map. Differentiation from other nonvascular causes of limb pain may be difficult to determine. Indications for noninvasive lower extremity testing include, but are not limited to , lower extremity discomfort with exertion, lower extremity ischemic rest pain, the presence of ischemic ulcerations or gangrene, absent pulses on physical examination, digital ischemia, and assessment of wound healing potential. As arterial narrowing progresses, there is a decrease in systolic blood pressure distal to the site of stenosis. Measurement of the pressure drop will allow assessment of the presence and severity of arterial disease. A sensing unit (such as a continuous wave Doppler or plethysmograph) is placed distal to the cuff. Then, as pressure in the cuff is gradually deflated, the point at which arterial blood flow is resumed is noted as the systolic blood pressure at that level. This is most often, but not exclusively, the case in elderly patients and those with diabetes mellitus or advanced chronic kidney disease. Exercise Testing Exercise prompts an increase in demand for arterial flow to the lower extremities. A standard protocol for treadmill testing is 5 minutes in duration at a speed of 2 mph and 12% incline. While patients walk they are asked to report onset of symptoms of leg pain, chest pain, shortness of breath, or fatigue. The number of repetitions at the first onset of pain and the total number of repetitions should be recorded. A major limitation of heel-raise exercise in relation to treadmill exercise is lack of reproducibility. In patients who cannot perform exercise, such as those who cannot stand or walk, and for those patients with other comorbidities, such as congestive heart failure or chronic pulmonary disease, reactive hyperemia testing is an alternative to exercise testing. Limb cuffs are inflated on the thighs at suprasystolic pressure for a maximum of 3 to 5 minutes, resulting in distal ischemia. After releasing the cuffs, reactive hyperemia confers reduced resistance to blood flow with vasodilation of the arteries distal to the occlusive cuff, similar to that achieved with exercise. Reactive hyperemia is considered a difficult test for patients largely because of discomfort. Segmental pressures are performed by applying blood pressure cuffs to several locations along the lower extremities (upper thigh, lower thigh, calf, ankle, foot and digit). Each segment is compared to the contralateral segment, the ipsilateral adjacent segments, and the higher of the two brachial pressures. A reduction in pressure greater than 20 mm Hg from one level to the next distal segment, or compared to the contralateral similar segment, is considered significant. Blood pressure cuffs are inflated to obliterate venous, but not arterial, flow, commonly to a level of approximately 65 mmHg. It is used to assess patients with moderate to severe intermittent claudication and to follow patients after surgery and endovascular therapy. Dampened signals may be obtained proximal to an obstruction but also distal to it. Collaterals surrounding a total occlusion may resemble flow distal to an occlusion because they are low resistance. Most vein graft restenosis occurs during the first 6 to 12 months postoperatively25 with an estimated 60% primary patency at 5 years. The addition of end-diastolic velocities greater than 100 cm/second suggest greater than 75% stenosis. Although it can locate areas of stenosis, in cases of multiple stenosis it may be difficult to determine the hemodynamically significance of the distal stenosis. The sensitivity and specificity for detecting occlusion were even higher (90% and 96% to 100%, respectively). The same criteria that have been described for lower extremity arterial stenosis may be used. Provocative Testing for Vasospasm Cold challenge testing assesses the ability of the digital vascular bed to respond to cold stimuli and recovery. Digital blood flow is assessed before, during, and after exposure to cold stimuli. Cold challenge test is reproducible and is often used in patients with suspicion of secondary Raynaud phenomenon. Some use the digital-brachial index, whereas others claim digital pressures are unreliable. The method allows single digit flow quantification, enabling mapping of pathology to the distribution of particular vascular beds, such as in the case of the hypothenar hammer syndrome. It is commonly used to diagnose and follow patients with extracranial internal carotid disease in native arteries as well as after surgery and stent deployment. Measurement acquisition can be performed manually or with automated edge detection software programs while the operator holds the transducer at the correct location. The subclavian artery and vein, along with the brachial plexus, traverse through the thoracic outlet. If the Doppler spectral waveform morphology is parvus et tardus bilaterally, this suggests critical aortic stenosis or impaired cardiac output. Therefore, native artery velocity criteria tend to overestimate the degree of stenosis in stented arteries. It is characterized by posterior circulation symptoms of diplopia, ataxia, and vertigo.
Order ceftin 500mg visa
When large vessels are transected virus guard ceftin 500 mg otc, the gelfoam may be swept into the retroperitoneum. In patients with pseudoaneurysms or arteriovenous fistulas, where a precise embolization may be desirable, coils are the embolic material of choice. In contrast to gelfoam pledgets, which are injected in a relatively uncontrolled manner, coils can be pushed through the catheter with a floppy wire and deposited in a more deliberate fashion. While the patient was resuscitated, a selective superior gluteal artery angiogram was performed showing extravasation from multiple sites. A variety of coil sizes and shapes are available for both standard selective and superselective microcatheters. In most cases, however, coils are not the primary embolization material in hemodynamically unstable patients because of the time needed for careful placement and occasional incomplete vascular occlusion. Balloon occlusion techniques may also be useful when hemorrhage is discovered from a vessel that cannot be safely embolized, such as the common or external iliac arteries. The balloon remains inflated while a stent-graft is deployed or the patient is transferred to the operating room for open repair. These occlusions may represent thrombosed arterial transections or areas of spasm. Differentiation is impossible from the diagnostic angiograms because both lesions appear as abrupt arterial cutoffs. Probing of the occlusion with a guide wire is ill advised because of the risk of converting an intact but spastic artery into a perforated vessel. This may be technically difficult if only a short stump of the vessel remains patent. In this instance, placement of a coil is preferred to the less-controlled injection of gelfoam pledgets. An alternative management strategy in hemodynamically stable patients is to follow transfusion requirements without embolization with prompt return to the angiographic suite for evidence of resumed bleeding (transfusion of more than 4 to 6 units of packed red cells in fewer than 24 hours). Patients who are not embolized should be monitored carefully because the rate of clot lysis is unpredictable. If extravasation was visualized with only selective injections, these should be repeated. Bilateral internal iliac angiograms should be performed if extravasation was from a midline vessel. When embolization in the pelvis is complete but the patient remains hemodynamically unstable, angiographic evaluation of the abdomen or thorax for another source of bleeding may be warranted. Concerns regarding contrast material, such as renal failure, are legitimate but should never prevent the procedure. Patients who undergo angiography for diagnosis and treatment of pelvic bleeding are dying. Nontarget embolization is an important procedure-specific complication of pelvic embolization. Fortunately, the most common site of nontarget embolization is another branch of the internal iliac artery. This is usually of little clinical consequence because the bladder, rectum, and pelvic soft tissues have multiple sources of blood supply, including the opposite internal iliac artery and sources originating outside the anatomic boundaries of the pelvis. As long as the embolic material is of appropriate size and composition, ischemic complications are rare. Emboli that lodge in the profunda femoris artery or other muscular branches are usually clinically silent unless these are sources of collateral supply to the lower limb. Impotence in men and inability to achieve pregnancy in women may be perceived as potential complications of embolization by referring physicians. Before the widespread application of percutaneous embolization in pelvic trauma, impotence was closely linked to urethral injury with an incidence of 30% to 50%. No studies prove that pelvic embolization in trauma does not cause impotence in men or infertility in women, however. These concerns should be weighed against the immediate needs of an exsanguinating patient. Early intervention in hemodynamically unstable patients with pelvic fractures is essential to reduce the morbidity of the injury. Embolization can be quickly and safely performed using widely available embolic materials. Angiography is likely to continue to have an important role in the management of pelvic trauma. The cause of death in fractures of the pelvis: with a note on treatment by ligation of the hypogastric (internal iliac) artery. Early management of the trauma patient with pelvic fracture: a medical perspective. Diagnosis and control of posttraumatic pelvic hemorrhage: transcatheter angiographic embolization techniques. Transcatheter embolization of autologous clot in the management of bleeding associated with fractures of the pelvis. Percutaneous transcatheter embolization for massive bleeding from pelvic fractures. A prospective study on the safety and efficacy of angiographic embolization for pelvic and visceral injuries. The role of arterial embolization in controlling pelvic fracture haemorrhage: a systematic review of the literature. Hemorrhage associated with pelvic fractures: causes, diagnosis, and emergent management. Diagnostic arteriography and therapeutic transcatheter embolization for post-traumatic pelvic hemorrhage. Current management of pelvic fractures: a combined surgical-angiographic approach to hemorrhage. Pelvic fracture from major blunt trauma: outcome is determined by associated injuries. Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilization and external fixation. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Postmortem angiography and dissection of the hypogastric artery in pelvic fractures. Delayed, exsanguinating pelvic hemorrhage after blunt trauma without bony fracture: case report. Ligature of the internal iliac artery for massive haemorrhage complicating fracture of the pelvis. The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. Mortality after successful transcatheter arterial embolization in patients with unstable pelvic fractures: rate of blood transfusion as a predictive factor. Associated aortic rupture-pelvic fracture: an alert for orthopedic and general surgeons. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. Traumatic rupture of the superior gluteal artery, without fracture of the pelvis, causing compartment syndrome of the buttock. Profound hypotension in blunt trauma associated with superior gluteal artery rupture without pelvic fracture. External iliac artery and lumbosacral plexus injury secondary to open book fracture of the pelvis: report of a case. Angiographic embolization of bilateral internal iliac arteries to control life-threatening hemorrhage after blunt trauma to the pelvis. Percutaneous balloon catheterization: a technique for the control of arterial hemorrhage caused by pelvic trauma. Stent graft treatment of an external iliac artery injury associated with pelvic fracture. Prompt and accurate diagnosis is vital to minimize these adverse effects when traumatic injuries to vascular structures are suspected.
Purchase ceftin paypal
Plan to puncture the skin 1 to 3 cm below this mark at a 45-degree cephalad angulation antibiotics buy online ceftin 250 mg on-line. Fluoroscope the result to make sure puncture has been made correctly; if not, remove the needle and guide wire and try again. Prophylactic hemodialysis and hemofiltration have not been validated as effective strategies. Fenoldopam, dopamine, calcium channel blockers, atrial natriuretic peptide, and L-arginine have not been shown to be effective. Use of furosemide, mannitol, or an endothelin receptor antagonist is potentially detrimental. Does the stenosis affect the main renal artery, an accessory renal artery, or branch vessels Each feature will affect the way we approach endovascular treatment and the prognosis. Most of these involve the renal artery ostium, which is the junction between the renal artery and the aorta. These stenoses are thought to be caused by aortic thickening and plaque that narrows the renal artery lumen like a curtain. Stents are commonly used to treat these lesions to prevent the curtain from reoccluding the ostium following balloon angioplasty. The truncal or nonostial portion of the main renal artery responds to balloon angioplasty in a manner similar to stenoses in other peripheral arteries of similar size. Intimal fibroplasias, about 10%, which may occur in an ostial location presents as a focal or long smooth narrowing caused by replacement of adventitial fibrous tissue with dense collagen that is difficult to treat effectively by balloon angioplasty and may require the use of a cutting balloon or stent. It is imperative that the interventionist reviews and uses this information to plan and implement the procedure. Is the renal artery oriented at a right angle from the aorta or in a cephalad or caudad direction Is the aortorenal artery angle so acute that an approach from the arm might be better Most renal arteries do not arise at a horizontal angle from the axial plane of the aorta; in fact 93% of right renal arteries arise anterior-lateral and the 52% of left renal arteries posterior-lateral to this plane. Most interventionists prefer to work from a right femoral artery access, but this is not always the optimal approach. Advancing a balloon or stent into a renal artery with an acute inferior angulation can be very difficult from a contralateral femoral puncture. I prefer to perform a renal intervention from an ipsilateral femoral puncture so that my guide catheter is stabilized against the contralateral aortic wall. Stents should be avoided in nonostial stenoses and in arteries less than 5 mm in diameter. It is more important for the interventionist to be able to use one system safely and effectively, to know when he or she has reached the limits of his or her ability, and to avoid major complications-especially those caused by neglect and stupidity. Always keep the tip of the guide wire in the fluoroscopic field and pay attention to it. If the end of the wire begins to buckle (accordion), it means that the tip is wedged against a plaque, beneath the intima or in a small branch vessel, and that a perforation or intimal dissection is in the near future. The arterial access site should be planned after review of all available noninvasive imaging procedures (see the above discussion). This means that you should cross the lumen of the stenosis parallel to its axis with a soft guide wire. Think of it as trying to advance the guide wire through the stenosis without touching its walls. To do this you would have to have the axis of the catheter guiding the wire in perfect alignment with the stenosis. Stay within safe limits of contrast dosage and accept the fact that the safe dose is frequently less than you would suspect. Make sure that you are attempting to treat a hemodynamically significant stenosis; otherwise you will be exposing the patient to risk without the chance of reward. Pressure measurements are required on stenoses narrowing the lumen diameter by 50% to 75%; most of us can accurately judge a greater degree of stenosis and pressure measurements are not required in these lesions, although they are useful compared to completion pressures to determine benefit. This said, I have had one case in which there was no gradient across a 75% in-stent stenosis that was being treated for a second time. I assume this was because of adequate retroperitoneal collateral blood supply or high resistance in the distal vascular bed, possibly related to atheroembolism. My advice is to terminate the procedure and seek medical or surgical consultation for alternative therapy. This is especially important during procedures on pediatric patients and young females. Perform an aortogram only if information is needed that is not available from the noninvasive images. Record images as rapidly as possible on your equipment; frequently, view of the origin of the renal artery is obstructed by aortic branches after the first several frames. Alter the angulation or catheter position if necessary to observe the renal artery origin in profile. Form reverse curve catheters below the aortic arch, that is, in the contralateral iliac, celiac, or mesenteric arteries or in the aorta using the Cope technique. Introduce the catheter or guiding system chosen to cross the stenosis over a soft, straight guide wire (usually a Benson guide wire). Advance 2 to 3 cm of the guide wire beyond the catheter tip so that it prevents the tip from scoring the endothelium as it moves along the aortic wall; that is, position the tip of the reverse curve catheter about 1 cm below the expected origin of the renal artery and remove the guide wire. Push the catheter superiorly, expecting the tip to make a quick lateral movement as it enters the renal artery ostium. If blood can be aspirated, confirm the catheter tip position by injecting a small amount of contrast. When treating ostial stenoses, the stent should protrude at least 2 mm into the aorta. It is not necessary to flare its aortic margin, but it may make it easier to re-catheterize in the event of in-stent restenosis. Special care must be taken not to damage branch vessels when treating an adjacent truncal stenosis; the branch can be ruptured or dissected if too large a balloon is used. The geometry of more than two unequally sized balloons can be calculated using the Gaylord algorithm. I feel that they are of special benefit in the obese, the elderly, and patients with chronic back pain who are unlikely to keep their leg straight during recovery. A guide catheter or guide sheath is then advanced to the renal artery ostium and a magnified angiogram recorded to determine vessel size and the degree of stenosis. Delayed washout or stasis of contrast indicates inadequate treatment of the stenosis, dissection, or peripheral embolization. Guide catheter with a Bentson guide wire placed in the aorta above the renal artery. The guide catheter is pulled inferiorly until the renal orifice is located and the stenosis crossed with a guide wire. The "no touch" technique accomplishes this by placing a soft guide wire cephalad through the catheter tip, which reduces its wall contact. Contrast injected through a Touhey-Borst adapter will confirm that the tip is adjacent to the renal artery lumen after which a 0. Never remove the guide wire before you are absolutely sure that the stenosis has been completely and optimally treated. It would be foolish to remove the guide wire from the renal artery to use it to place a pigtail catheter in the aorta for a flush aortogram and then discover that the stenosis has not been adequately treated or that a flow-limiting dissection has occurred. I recommend performing the completion arteriogram through the guide catheter or guide sheath with the image tube angled to view the vessel origin in tangent. Acute renal failure and worsening of chronic renal failure are most often related to contrast agents. Their treatment is detailed in an excellent review in emedicine and will not be repeated here. Treatment associated with combined therapy consisting of plasma exchange and low-to-intermediate-dose corticosteroid therapy has been shown to be effective in some cases of renal cholesterol embolism.
Generic 250 mg ceftin with mastercard
These patients should undergo urgent (<24 hours) repair barring other serious concomitant nonaortic injuries tween 80 antimicrobial purchase ceftin in united states online, or immediate repair after other injuries have been treated or stabilized, but at the latest prior to hospital discharge. As mentioned previously, expectant management with follow-up imaging is appropriate. These endografts have been tested and approved for safety and efficacy in clinical trials for thoracic aneurysmal disease. The currently available thoracic endograft sizes mostly reflect the larger aortic diameters that would be typically encountered in an older cohort with degenerative aneurysms. The aortic diameters are relatively smaller in the younger subset of trauma patients. Excessive oversizing has been implicated with endoleak, device infolding, endograft collapse, and even death from acute aortic occlusion. Anatomic Considerations There are several fundamental differences in the anatomic morphology between patients with atherosclerotic thoracic aortic aneurysm and traumatic aortic injuries that may have an impact on the choice of endograft devices and deployment techniques. We have not yet encountered any patients who required such proximal access because of vessel size, however. The soft distensible nature of these arteries with a very short indwelling time for the sheaths has allowed rather uniform femoral access in the cases we have treated. A rapid decision must be made whether to cover the subclavian artery or not and whether a prophylactic carotid-subclavian bypass is required. Those decisions follow established criteria with aneurysmal disease, namely, the need to maintain forward vertebrobasilar flow through at least one vertebral artery. The standard 2 cm landing zone also may not be necessary in all these cases with relatively healthy aortas that are not usually completely severed circumferentially. As such, we currently do not believe that subclavian coverage is needed in most patients and have only used it in five of ours and mostly earlier in our experience. We currently attempt to reach only the distal ostium of the left subclavian artery, which facilitates the procedure and decreases the problem of poor apposition to the lesser curve of the arch. The distal landing zone, on the other hand, is usually not a critical factor because the long segment of the normal descending thoracic aorta is more than sufficient to permit proper device fixation. These devices may not reach the site of injury from a femoral access due to the short delivery system, necessitating either use of a longer makeshift delivery system or access through a more proximal site, typically the distal external iliac artery that can be exposed under the inguinal ligament. Such an intercalating construction allows slightly improved conformation to the arch but at the same time introduces multiple junctions with a potential for a type 3 endoleak. Systemic Anticoagulation the decision to administer systemic anticoagulation must be individualized based on the balance of the perceived risks of bleeding in a particular organ system versus the thromboembolic complications. The safety of systemic anticoagulation using heparin during endovascular repair in a multitrauma patient with a closed head injury or abdominal solid organ injury is a controversial issue. A minority opinion was expressed that heparin may not be necessary because most of these cases can be performed relatively rapidly and the risk of a thrombotic event is likely small if performed via a percutaneous approach. We believe that this technique may allow a more rapid endograft delivery and repair in a hemodynamically unstable patient. These include concomitant brachial artery access, femoral artery guide wire placement, controlled hypotension, and transient asystole induced pharmacologically or by rapid ventricular pacing. Device-related late complications include endoleak, stent-graft collapse, physiologic coarctation of the aorta, stentgraft migration, dynamic obstruction of the left subclavian artery or left common carotid artery, erosion through the aortic wall, and aortoenteric fistula. The most common indications for secondary interventions were endoleak (50, 60%), stent-graft collapse (9, 11%), intraoperative rupture (2, 2%), iliac artery injury (1, 1%), and penetration of metal stent (1, 1%); the remaining 20 (25%) were described as device-related failures that required secondary intervention. Of the 50 endoleaks reported in literature, only 15 were specifically described as type 1 endoleak, and the rest were nonspecified. One was treated with coil embolization, two resolved spontaneously, five required open conversion, and five required placement of additional cuffs. Unreliable cooperation of an agitated trauma patient and the presence of concomitant injuries, however, may make local anesthesia less favorable. We use local anesthesia in these cases very selectively and only in patients where airway management is not a major problem. Regional anesthesia may not be practical in the trauma setting, therefore favoring the use of general anesthesia. Obstruction of the left subclavian artery and left common carotid artery has been shown to occur when the ostium is partially obstructed. These can be treated by additional stent placement in the left subclavian artery or the left common carotid artery or by carotid-subclavian or right carotid-carotid bypass surgery. In a younger fit patient, conversion to open repair with stent-graft explanation may be a more durable option. One of the five patients underwent endograft removal and reconstruction using a rifampin-impregnated Dacron graft. The remaining four patients were treated medically; one patient survived and was placed in hospice care, two died of rupture of the mycotic aneurysm, and one died of multiorgan system failure. The above-mentioned findings underscore the importance of lifelong follow-up for the early diagnosis and treatment of such potentially fatal complications. Direct blows to the abdomen, falls from height, and explosions are responsible for the rest of the cases. Thoracolumbar spine fractures and seat-belt injuries are associated with high risk for blunt aortic injuries of the abdominal aorta. The clinical presentation depends on the mechanism of the injury, the specific type of injury, the presence of free intraperitoneal hemorrhage or retroperitoneal hematoma, the time lag since the injury, and the presence of other associated injuries. Of the patients presenting to a trauma room, about 28% have nonrecordable blood pressure and 21% undergo emergency resuscitative thoracotomy. Blunt injuries may often be missed on initial examination or even during the initial hospitalization, unless they are associated with significant bleeding or early ischemic changes. Mesenteric, renal, or extremity ischemia can occur depending on the location of the injury. It is reported that in 33% of patients with blunt aortic trauma, the diagnosis may be made months to years from the initial injury. In a review of 302 abdominal vascular injuries, the aorta was involved in 63 cases (21%) followed by inferior vena caval injuries (25%). In hemodynamically stable patients with gunshot wounds, radiographic evaluation of the chest and abdomen might assist in the operative planning or in diagnosing associated extra-abdominal injuries. Endovascular treatment of selected traumatic vascular injuries is particularly promising for restoring luminal continuity, closing aortocaval fistulas, and excluding pseudoaneurysms. Others have similarly reported on the efficacy of endovascular repair in the setting of blunt trauma to infrarenal abdominal aorta. For injuries of the visceral aorta, a left thoracotomy and cross clamping of the aorta is sometimes necessary. After control of the hemorrhage the associated intra-abdominal injuries are addressed. Lateral aortorrhaphy is possible in some cases due to the relative healthy aorta and limited injury in the trauma population. In patients with high-velocity missiles the extent of the injury may not be fully appreciated by visual inspection and care must be taken not to leave behind devitalized tissue. In these and other extensive aortic wall injuries a prosthetic graft repair may be needed. In cases where enteric spillage is encountered it is recommended that the spillage be controlled and the peritoneum be washed out prior to the use of a prosthetic graft. Although suboptimal, several reports do not consider the presence of enteric spillage a contraindication for the use of a prosthetic graft for aortic repair in trauma. Pre- and postaortography (C) document successful exclusion of the pseudoaneurysm after endovascular aortic repair with a bifurcated stent-graft. The reported incidence of aortic injury after such spinal instrumentations is less than 0. Mechanism of Injury Penetration of a malpositioned pedicle screw can cause penetrating injury to the aorta at the time of operation. Studies have shown that actual pedicle screw penetration of the aorta is not necessary to cause delayed iatrogenic aortic injury. Mere impingement on the aorta by the fixation screw can lead to aortic wall weakening and the potential for eventual erosion as the aorta continues to pulsate and cause repeated trauma with every heartbeat. Proximity of the screw tip to the aortic wall has been reported in 2% to 12% of iatrogenic aortic injuries. Acute aortic perforation results in hemorrhage, leading to either hemodynamic instability in case of free rupture or rapid hematoma formation, or both. Iatrogenic aortoiliac trauma can also lead to pseudoaneurysm or aortocaval fistula formation. Iatrogenic Aortic Injuries During Laparoscopic Procedures Retroperitoneal vascular injuries resulting from trocar placement during gynecologic and general surgery operations have an incidence of approximately 0.
Ceftin 500 mg otc
Because this study used mean survival rather than median survival treatment for uti keflex ceftin 250mg low price, a direct comparison with other studies in the literature is difficult. The drug-eluting properties of these microspheres allow prolonged and controlled release of the chemotherapeutic agent into the tumor bed, thereby achieving greater drug concentration within the tumor and minimizing systemic toxicity. Despite the small sample sizes, there were impressive response rates, and overall outcomes ranged between 13 and 30 months. In this cohort, patients who had previously received systemic chemotherapy were compared with historical controls who were treated with chemotherapy alone. Radioembolization with Ytrium-90 Microspheres Traditionally, whole-liver external-beam radiation therapy hashad limited use in the treatment of primary liver cancers because the liver parenchyma is radiation sensitiveand is unable to tolerate the radiation dose required to achievetumoricidal effects. Radioembolization delivers small radioactive (yttrium-90) particles deeply within the tumor bed. Factors associated with improved survival included good performance status and peripheral tumor type. The most common clinical toxicities were fatigue (64%) and selflimiting abdominal pain (40%) (Table 14. In patients who are not candidates for surgical resection due to poor liver function or prohibitive comorbidities, thermal ablation initially appears to be a good option. The greater understanding of the pathophysiology, its risk factors, genotypes, phenotypes, and recent formulation of its own staging system hopefully will allow clinicians greater tools to improve the outcomes of a dismal disease. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Clinicopathological factors predicting outcome after resection of massforming intrahepatic cholangiocarcinoma. Intrahepatic cholangiocarcinoma arising in cirrhotic liver frequently expressed p63-positive basal/stem-cell phenotype. Peripheral cholangiocarcinoma (cholangiocellular carcinoma): clinical features, diagnosis and treatment. A new staging system for massforming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Chemotherapy in advanced biliary tract carcinoma: a pooled analysis of clinical trials. Arterial chemoinfusion therapy through an implanted port system for patients with unresectable intrahepatic cholangiocarcinoma-initial experience. Chemoembolization of intrahepatic cholangiocarcinoma with cisplatinum, doxorubicin, mitomycin C, ethiodol, and polyvinyl alcohol: a 2-center study. Initial experience from a combination of systemic and regional chemotherapy in the treatment of patients with nonresectable cholangiocarcinoma in the liver. Transcatheter arterial chemoembolization or chemoinfusion for unresectable intrahepatic cholangiocarcinoma: clinical efficacy and factors influencing outcomes. Hepatic intraarterial chemotherapy with gemcitabine in patients with unresectable cholangiocarcinomas and liver metastases of pancreatic cancer: a clinical study on maximum tolerable dose and treatment efficacy. Hepatic arterial infusion of mitomycin C with degradable starch microspheres for unresectable intrahepatic cholangiocarcinoma. New intra-arterial drug delivery system for the treatment of liver cancer: pre-clinical assessment in a rabbit model of liver cancer. Precision hepatic arterial irinotecan therapy in the treatment of unresectable intrahepatic cholangiocellular 44. Treatment of unresectable cholangiocarcinoma using yttrium-90 microspheres: results from a pilot study. Yttrium-90 radiotherapy for unresectable intrahepatic cholangiocarcinoma: a preliminary assessment of this novel treatment option. Radiofrequency ablation of intrahepatic cholangiocarcinoma: preliminary experience. Sonography-guided percutaneous microwave ablation of intrahepatic primary cholangiocarcinoma. Since then, improved diagnostic imaging techniques, significant developments in interventional radiology, and the results of clinical trials have revolutionized and clearly defined the role of percutaneous biliary interventions. The majority of strictures of the mid and lower common bile ducts, which are mainly caused by carcinoma of the head of the pancreas, can be drained effectively by the endoscopic approach. It is advocated by some surgeons in certain circumstances before curative resection, however, as a method of correcting metabolic derangements produced by biliary obstruction prior to surgery. Either internal/external biliary drainage catheters or more plastic stents are inserted 2 to 6 weeks prior to elective surgery. Most patients with malignant obstructive jaundice caused by carcinoma of the gallbladder, carcinoma of the pancreas, and cholangiocarcinoma present with advanced disease2,3 and only 20% to 30% of such tumors are resectable at the time of diagnosis. One of the important goals of preoperative imaging is establishing whether there is vascular invasion by a tumor at the hepatic hilum. Previously, angiography was used to identify the vascular anatomy prior to surgery in carcinoma gallbladder7 and hilar cholangiocarcinoma. To manage infectious complications of biliary obstruction, such as cholangitis and sepsis 2. To relieve obstructive jaundice when an endoscopic retrograde approach fails or is not indicated 3. Preoperative decompression and stent placement to assist in surgical manipulation (controversial) 4. To gain access to the biliary system to perform other bile duct interventions, such as biopsy, stent placement, and transhepatic brachytherapy for cholangiocarcinoma Three-dimensional reconstructions can be produced successfully by taking advantage of the negative contrast effect of lowattenuation bile in the dilated ducts relative to the adjacent enhanced liver13 and can determine the level and cause of biliary obstruction. Ductal dilatation, strictures, and anatomic variation are well depicted by this technique and this ability makes this modality well suited for planning the optimal therapeutic approach for patients with biliary obstruction. Cytologic study is positive in roughly 50% of the patients with cholangiocarcinoma, although the reported sensitivity varies widely. Vitamin K, fresh frozen plasma, and platelets (as needed) should be administered to correct any coagulopathy. Liver function tests: Serum bilirubin and alkaline phosphatase levels should be checked to obtain baseline values (an elevated alkaline phosphatase level, even in the setting of a near-normal bilirubin indicates a low-grade obstruction). Baseline renal function: Blood urea and creatinine should be checked, especially before administering preprocedure nephrotoxic antibiotics. Informed Consent the procedure should be explained completely to the patient, outlining the risks with specific attention to sepsis and bleeding. The spectrum of antibiotic coverage must include both gram-positive and gram-negative organisms. Escherichia coli is the most common organism involved; enterococci, klebsiella species, and Streptococcus viridans are other frequently observed organisms. Antibiotic therapy should be modified according to the results of positive bile or blood cultures. Intercostal blocks have also been used and in some cases general anaesthetic is required. Skin Preparation It is best to prepare a wide area, which will permit access to the biliary system from the left and right sides, as needed. A 22-gauge needle is inserted into the liver immediately anterior to the midaxillary line and advanced horizontally to the lateral Sedation/Analgesia Biliary procedures are most often performed under conscious sedation (midazolam and fentanyl) with liberal infiltration of local anesthetic at the site and up to the capsule of the liver. Bacterial contamination usually occurs when an isolated ductal system is accessed. As a consequence of this contamination, it is often impossible to withdraw drainage even if the drainage is not required clinically. Thus a patient could be left with a permanent, unwanted, and potentially problematic drainage catheter. Inthese patients, drainage is often ineffective in relieving symptoms and can therefore be avoided. Dilated ducts are located by withdrawing the needle and injecting contrast medium or aspirating until bile is obtained. The aspiration method has the advantage of avoiding a large stain of parenchymal contrast if several passes are required.
Buy ceftin 500mg on line
Transjugular liver biopsy results in the transplanted liver: comparison of two surgical hepatic venous anastomotic configurations in 269 consecutive biopsies over a 14-year period infection cheap 500 mg ceftin with visa. At our institution, we have also performed transvenous liver biopsy in post-piggyback technique liver transplant patients from a right-side common femoral vein approach. When using this approach, one must be cognizant of the increased risk of pneumothorax when obtaining the biopsy specimen. Additionally, the patient must be of normal-to-smaller stature due to the length of the biopsy cannula and needle provided in the biopsy set. The transplant centers using only the percutaneous approach advocate correcting the coagulopathy, draining the ascites,69 and leaving the fascia of the incision open for easier access. Contribution of transjugular liver biopsy in patients with the clinical presentation of acute liver failure. Transjugular liver biopsy-indications, adequacy, quality of specimens, and complications- a systematic review. Transjugular liver biopsy: a prospective study in 43 patients with the Quick-Core biopsy needle. Large-needle biopsy versus thin-needle biopsy in diagnostic pathology of liver diseases. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. Transjugular liver biopsy: how good is it for accurate histological interpretation Low-dose midazolam sedation: an option for patients undergoing serial hepatic venous pressure measurements. Percutaneous liver biopsy with plugging of needle track: a safe method for use in patients with impaired coagulation. A comparison of transjugular and plugged-percutaneous liver biopsy in patients with impaired coagulation. A comparison of transjugular and pluggedpercutaneous liver biopsy in patients with contraindications to ordinary percutaneous liver biopsy and an "in-house" protocol for selecting the procedure of choice. Hepatic venous pressure gradient identifies patients at risk for severe hepatitis C recurrence after liver transplantation. Emergency transjugular liver biopsies in post-liver-transplant patients: technical success and utility. Hepatic venography, manometric studies and transjugular liver biopsy in the follow-up of liver transplant patients. The role of transjugular liver biopsy in fulminant liver failure: relation to other prognostic indicators. Transjugular liver biopsy is a safe and effective intervention to guide management for patients with a congenital bleeding disorder infected with hepatitis C. A Canadian multicenter retrospective study evaluating transjugular liver biopsy in patients with congenital bleeding disorders and hepatitis C: is it safe and useful Interest of transjugular liver biopsy in adult patients with heamophilia or other congenital bleeding disorders infected with hepatitis C virus. Transjugular liver biopsy is safe and diagnostic for patients with congenital bleeding disorders and hepatitis C infection. Complications following percutaneous liver biopsy: a multicentre retrospective study on 68,276 biopsies. Complications associated with percutaneous needle biopsy of the liver when one, two or three specimens are taken. Transjugular liver biopsy: modified Ross transseptal needle versus Quick-Core biopsy needle. Orthotopic liver transplantation for acute and subacute hepatic failure in adults. The importance of percutaneous liver biopsy in the management of the liver transplant recipient. Complications of liver biopsy in liver transplant patients: increased sepsis associated with choledochojejunostomy. Transjugular intrahepatic portosystemic shunts in the management of Budd-Chiari syndrome in the liver transplant patient with intractable ascites: anatomic considerations. Choice of surgical technique influences perioperative outcomes in liver transplantation. Transjugular liver biopsy: prospective evaluation of the angle formed between the hepatic veins and the vena cava main axis and the modification of a semi-automated biopsy device in cases of an unfavorable angle. Use of a stiff guidewire in transjugular liver biopsy in patients with a pronounced angle of the suprahepatic veins. A new technique of side to side caval anastomosis during orthotopic hepatic transplantation without inferior vena cava occlusion. Thus, gastric variceal bleeding is not sufficiently controlled by medical treatment alone or it is often more difficult to control by endoscopic intervention than bleeding from esophageal varices. Because gastric variceal bleeding remains a therapeutic challenge, a transcatheter treatment of retrograde approach has been developed. The isolated gastric varices form in a large portosystemic shunt between the gastric veins and the left inferior phrenic vein in the bare area of the stomach. They are mainly supplied from the left gastric vein and/or the posterior gastric vein but less frequently from the short gastric vein. They can be introduced through a 6 French guiding catheter or 4 French sheath over a 0. Risk factors for gastric variceal bleeding include the presence of red color sign, enlarging variceal size, and impaired liver function. Recently, sclerosing foams using polidocanol or sodium tetradecyl sulfate have been applied. Hypovolemic shock should be stabilized first by conservative treatment and balloon tamponade. Periodic endoscopic screening is important because the bleeding is not always predictable. Double coaxial balloon catheter system: a 9 French guiding catheter with a 20-mm balloon and a 5 French coaxial catheter with a 10-mm balloon. By angiography, the superior mesenteric and celiac arteriograms are useful to grasp the whole portal venous system. Image reconstruction with multiplanar reformation, maximum intensity protection, or volume-rendering technique allows three-dimensional analysis. Size and shape of balloon catheters are determined based on the diameter and configuration of the estimated access route veins. A transjugular approach may allow deeper balloon insertion and reduce patient discomfort when the balloon inflation is planned until the next day. A power injector should not be used to avoid variceal rupture caused by forceful pressure. The volume of sclerosing agent is estimated according to the contrast volume to fill the varices. The balloon is kept inflated until adequate blood flow stasis of the varices is obtained. First, coil or glue embolization is necessary to occlude large or high-flow collateral veins. Gentle manipulation to insert the microcatheter is mandatory to avoid vessel perforation. If the microcatheter reaches the varices, intravariceal glue injection can be performed and coils are deployed in the draining vein to avoid glue migration. Following microcoil embolization of the collateral vein (arrows), the varices were sufficiently filled with 5% eoi under balloon occlusion. Even without its escape into the collateral veins, the sclerosing agent does not always stagnate in the entire varices. Balloon-occluded venography shows collateral drainage into the inferior phrenic vein (arrow) without filling the gastric varices. With the inferior phrenic vein occluded with another 10-mm balloon catheter (arrow), 18 mL of 5% eoi was injected from the balloon catheter in the Gr shunt.