Order avapro with visa
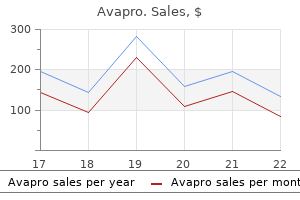
Before considering the influence of astrocytes on cerebral metabolism, it is relevant to consider their structural relationship to each other and to other cells in the brain diabetes mellitus type ii became subject to presumptive service connection quality 300mg avapro. In the mammalian brain, neurons make up no more than 50% of the cerebral cortical volume and in most regions are outnumbered 10: 1 by astrocytes. Where astrocytic processes abut capillaries, they are specialized into structures known as end-feet. These end-feet are so numerous that almost the entire surface of the capillaries is covered. The glucose taken up by astrocytes may have one of two primary fates: it may be converted to lactate via astrocytic glycolysis, or it may be converted via glycogenesis to the glucose storage polymer glycogen. By contrast, in adult neurons, aerobic glycolysis results in the formation of pyruvate, not lactate, and glycogen metabolism and storage normally do not occur. That glycogen, the storage form of glucose, is located almost entirely in astrocytes is one indication of the dominant position of astrocytes in the metabolic processing of glucose. However, it should be noted that glycogenolysis in astrocytes is dictated by specific neurotransmitters and neuromodulators, thus giving neurons tight rein over this energy store. Although controversial, the existence of astrocyte-neuron lactate shuttling is based on evidence. The fidelity and safety of glutamate-mediated neurotransmission are dependent on very efficient uptake and modification of glutamate by astrocytes. They possess the necessary aminotransferases to transfer the -amino group of glutamate to oxaloacetate or pyruvate to yield -ketoglutarate and either aspartate or alanine. Indeed, cultured astrocytes have been reported to use glutamate as an energy substrate even in the presence of glucose. However, the most common means by which astrocytes inactivate glutamate is by conversion to glutamine through the attachment of ammonium ions. This last reaction is endergonic and requires glutamine synthase, an enzyme limited to astrocytes, and serves the additional important function of removing ammonia. This cycling between glutamine and glutamate is commonly referred to as the glutamine-glutamate shuttle. Cortical activation causes rapid glutamatergic signaling, which increases the glutamine/glutamate flux and therefore drives the increased astrocytic consumption of glucose by glycolysis. This logic is supported by evidence of coupling of the glutamate/glutamine shuttle to glucose energetics in the cerebral cortex in vivo. For example, increases in the extracellular K+ concentration secondary to neuronal activity leads to the entry of K+ into astrocytes through strong inwardly rectifying K+ (Kir) channels. The high density of K+ channels on astrocytic end-feet allows K+ to be deposited in the perivascular space, where it can be recycled when neural activity ceases. Taken together, it is clear that an increase in neuronal depolarization is coupled to an increase in astrocytic depolarization, which in turn influences local metabolic and electrical activity via K+, H+, and Ca2+ ions. The resulting net ionic gain results in osmotic water uptake and slight swelling of the cell. Redistribution of this water is facilitated by the high density of aquaporin channels on perivascular end-feet. There are separate mechanisms to clear metabolic water from neurotransmitter activation or ion uptake, some of which involve elevations in intracellular Ca2+ [Ca2+]i. Blood flowing through an artery most often exhibits laminar or streamlined flow whereby an infinite number of concentric laminae are formed and move in a parabolic distribution of velocities that is greatest in the center of the tube and zero immediately adjacent to the wall of the tube. Laminar flow is described by the following HagenPoiseuille law: Q = (r 4 P) (8 L) (14) Here, r refers to vessel radius, P to pressure gradient, h to the coefficient of fluid viscosity, and L to vessel length. This provides an explanation for the clinical observation of the large change in blood flow that can occur with only small changes in vessel diameter. However, it only approximates real life because contrary to the key assumptions behind the Hagen-Poiseuille law, normal blood flow is not continuous but pulsatile, and blood vessels are not rigid and branchless tubes. In addition, if the rate of flow is continuously increased, there comes a point when resistance to flow increases sharply and the flow ceases to be laminar, instead forming a turbulent pattern. The situation in the brain is made even more complex by the operation of cerebrovascular autoregulation (discussed in detail later), the possible presence of arterial stenosis, and the diameter and extent of arterial collaterals. It should be noted, however, that when a major cerebral artery undergoes gradual occlusion, the extracranial arteries can also provide important collateral supply to the cerebral circulation via the ophthalmic, meningeal, and leptomeningeal arteries. Under normal physiologic conditions, blood flow is regulated in the brain through changes in vascular resistance. Furthermore, many of these cells are capable of altering their shape and forming physical interactions with each other or the glycocalyx on the endothelial wall. However, in blood vessels, where the internal diameter is very large in comparison to the size of the cells, blood of normal hematocrit approximates Newtonian behavior reasonably well. This has been explained by the tendency of erythrocytes to form clumps or rouleaux at low shear rates, thereby increasing resistance to flow. With the higher shear rates typically found in the microvasculature, the apparent viscosity falls because any cell aggregates are dispersed into single cells that stretch and align themselves with the axial and fastest moving laminae of the bloodstream, thus leaving a slower, cell-depleted zone of plasma along the vessel margin. This marginal zone is thought to progressively dilute the hematocrit as the caliber of the blood vessel is reduced and may be accentuated by plasma skimming or cell screening at branching points. Blood viscosity becomes even more critical to cerebral perfusion in pathologic states of low blood flow. Regardless of whether the cause of the low blood flow is a decrease in arterial perfusion pressure or an increase in vascular resistance, the accompanying decrease in shear stress causes an elevation in the hematocrit. Alternatively, the hematocrit could be raised by a disproportionate increase in postcapillary over precapillary resistance, which causes increased transcapillary fluid leakage. Either way, the increased apparent viscosity leads to a further retardation in blood flow, thus setting up the conditions for a vicious circle. This is the theoretical basis for the clinical use of hemodilution techniques as a means of attempting to improve cerebral perfusion in conditions such as ischemic stroke and cerebral vasospasm. Hemorheology One of the principal influences on the flow behavior of a liquid is a property known as viscosity. Viscosity represents the internal friction or resistance of the particles in a liquid to the sliding or shear forces necessary for flow to occur. Sir Isaac Newton was the first to propose that for a liquid undergoing perfectly laminar flow, the shear stress between the laminae is proportional to the shear rate or velocity gradient u/z in the direction perpendicular to the laminae by a constant of proportionality,: + u z (16) For an archetypal Newtonian fluid such as water, is properly called the coefficient of viscosity but can be equated with fluid viscosity and is a constant that is dependent only on temperature. In contrast, the viscosity of a non-Newtonian fluid can undergo large variations as the shear rate changes. Regulation of Cerebral Blood Flow Unlike other organs, regulation of blood flow in the brain is distinguished by the influence of astrocytes and neurons. Extracerebral blood vessels receive a rich "extrinsic" supply of perivascular fibers from the parasympathetic (mainly the sphenopalatine, otic, and internal carotid) and sympathetic (mainly from the superior cervical) ganglia, as well as the sensory roots of the trigeminal ganglia. On entering the brain parenchyma, cerebral arteries lose this ganglionic nerve supply and instead acquire "intrinsic" innervation from parenchymal neurons. The best characterized intrinsic neural pathways that project to cortical blood vessels are those from the nucleus basalis, locus caeruleus, and raphe nucleus. Anatomic studies have shown that neurons in these areas send projection fibers to cortical blood vessels, as well as to astrocytes. In fact, noradrenergic afferents from the locus caeruleus target mainly perivascular astrocytes. Changes in perivascular astrocytic [Ca2+]i secondary to noradrenaline cause vasoconstriction of the adjacent arterioles. Second, cerebral blood vessels exhibit changes in caliber in response to variations within certain ranges of Pco2 and, to a lesser extent, Po2. The functions of these various molecules are not exclusive and involve pathways that frequently intersect with one another. It is beyond the scope of this chapter to elaborate on every single mediator, so the following discussion is confined to those considered to be of greatest relevance and importance in cerebrovascular homeostasis. The endothelial and neuronal isoforms are constitutively expressed in cerebral blood vessels, the latter occurring in the nerve plexus in the outer adventitial layer. Many studies, mainly on coronary blood vessels, have concluded that this substance is an epoxyeicosatrienoic acid derived from the metabolism of arachidonic acid by cytochrome P-450 epoxygenase in endothelium. Because arachidonic acid is sequestered at the sn-2 position of glycerophospholipids, it must be enzymatically released from membrane phospholipids before the synthesis of eicosanoids. One of the important factors that determines the types of eicosanoid that are synthesized is the cell type that is under consideration. For instance, under normal conditions, endothelial cells tend to favor the release of vasodilatory eicosanoids, whereas aggregating platelets tend to favor the release of vasoconstrictors.
Buy 300mg avapro overnight delivery
Risk C: Monitor therapy Tems i rol i mus: Ma crol i de Anti bi oti cs ma y enha nce the a dvers e/toxi c effect of Tems i rol i mus diabetic diet low carb high protein purchase 300 mg avapro with mastercard. As s es s thera peuti c effecti venes s (a ccordi ng to purpos e for us e) a nd a dvers e rea cti ons. There wa s no di fference between the two groups wi th rega rd to the compos i the outcomes (pri ma ry or s econda ry). Dos i ng: Pedi a tri c Rhinitis or other allergic symptoms (including urticaria): Ora l: Infa nts a nd Chi l dren <6 yea rs: 0. Risk C: Monitor therapy Pra ml i nti de: Ma y enha nce the a nti chol i nergi c effect of Anti chol i nergi cs. As bl ood pres s ure a pproa ches goa l, dos e ma y be i ncrea s ed by l es s tha n doubl e every 5-10 mi nutes. Us ua l ma i ntena nce: 4-6 mg/hour; ma xi mum: 21 mg/hour (1000 mL wi thi n a 24-hour peri od). Us e wi thi n 4 hours of puncturi ng vi a l; di s ca rd a ny tubi ng a nd unus ed porti on, i ncl udi ng tha t currentl y bei ng i nfus ed. Risk C: Monitor therapy Ma gnes i um Sa l ts: Ca l ci um Cha nnel Bl ockers ma y enha nce the a dvers e/toxi c effect of Ma gnes i um Sa l ts. Risk C: Monitor therapy Neuromus cul a r-Bl ocki ng Agents (Nondepol a ri zi ng): Ca l ci um Cha nnel Bl ockers ma y enha nce the neuromus cul a r-bl ocki ng effect of Neuromus cul a r-Bl ocki ng Agents (Nondepol a ri zi ng). Pa ti ent s houl d be moni tored for a mi ni mum of 8 hours a fter di s conti nua ti on (rebound hypertens i on ma y occur). Pa ti ent Educa ti onThi s medi ca ti on ca n onl y be a dmi ni s tered by i nfus i on. Pha rma codyna mi cs /Ki neti cs Ons et of a cti on: 2-4 mi nutes a fter s ta rt of i nfus i on Dura ti on: I. Recons ti tuti onBenza Cl i n: Recons ti tute cl i nda myci n wi th puri fi ed wa ter; s ha ke wel l. Gentl y rub over enti re fa ce a voi di ng eyes, mouth, a ngl es of nos e, a nd mucous membra nes. Risk D: Consider therapy modification Neuromus cul a r-Bl ocki ng Agents: Li ncos a mi de Anti bi oti cs ma y enha nce the neuromus cul a r-bl ocki ng effect of Neuromus cul a r-Bl ocki ng Agents. Babesiosis (unlabeled use): Oral: 20-40 mg/kg di vi ded every 8 hours for 7 da ys pl us qui ni ne Dos i ng: Rena l Impa i rmentNo a djus tment requi red. Incompatible: Al l opuri nol, a zi thromyci n, doxa pra m, fi l gra s ti m, fl ucona zol e, i da rubi ci n. Compatibility in syringe: Compatible: Ami ka ci n, a ztreona m, ca ffei ne ci tra te, di menhydri na te, genta mi ci n, hepa ri n. Risk D: Consider therapy modification Etha nol /Nutri ti on/Herb Intera cti ons Food: Pea k concentra ti ons ma y be del a yed wi th food. You ma y experi ence na us ea or vomi ti ng (s ma l l, frequent mea l s, frequent mouth ca re, chewi ng gum, or s ucki ng l ozenges ma y hel p). Ameri ca n Denta l As s oci a ti on; Ameri ca n Aca demy of Orthopedi c Surgeons," J Am Dent Assoc, 1997, 128(7):1004-8. Risk C: Monitor therapy Cl oza pi ne: Benzodi a zepi nes ma y enha nce the a dvers e/toxi c effect of Cl oza pi ne. Oral mucosal inflammation (unlabeled use): Chi l dren 12 yea rs: Topi ca l: Refer to a dul t dos i ng. Steroid-responsive dermatoses: Chi l dren 12 yea rs: Topi ca l: Refer to a dul t dos i ng. Mild-to-moderate plaque-type psoriasis of nonscalp areas: Chi l dren 12 yea rs: Topi ca l: Refer to a dul t dos i ng. Moderate-to-severe plaque-type psoriasis: Chi l dren 16 yea rs: Topi ca l: Refer to a dul t dos i ng. Avoi d fi re, fl a me, or s moki ng duri ng a nd i mmedi a tel y fol l owi ng a ppl i ca ti on. Bonefos : Ini ti a l: 1600 mg/da y; ma y be i ncrea s ed to a ma xi mum of 3200 mg/da y Dos i ng: El derl yRefer to a dul t dos i ng. Bonefos : Di l uted s ol uti on s houl d be i nfus ed wi thi n 24 hours of prepa ra ti on. Correcti on of s evere or s ymptoma ti c hypoca l cemi a ma y requi re ca l ci um s uppl ementa ti on. Cons ul t pres cri ber for i ns tructi ons on a ppropri a the contra cepti ve mea s ures. Do not ta ke a ny new medi ca ti ons duri ng thera py wi thout cons ul ti ng pres cri ber. You ma y experi ence di a rrhea (boi l ed mi l k, yogurt ma y hel p) or cons ti pa ti on (i ncrea s ed di eta ry fi ber or fl ui d ma y hel p). Thi s drug ma y ca us e feta l deformi ti es or l os s of pregna ncy; cons ul t pres cri ber for a ppropri a the contra cepti ves. Cl i ni ca l Ma na gement Gui del i nes for Obs tetri ci a n-Gynecol ogi s ts, Number 34, Februa ry 2002. Ameri ca n Col l ege of Obs tetri ci a ns a nd Gynecol ogi s ts," Obstet Gynecol, 2002, 99(2):347-58. Food: Serum concentra ti ons /toxi ci ty ma y be i ncrea s ed by gra pefrui t jui ce. Risk D: Consider therapy modification Beta -Bl ockers: Ma y enha nce the rebound hypertens i ve effect of Al pha 2-Agoni s ts. Boxed Warning]: Epidural clonidine is not recommended for perioperative, obstetrical, or postpartum pain. Injecti on, s ol uti on, a s hydrochl ori de [epi dura l; pres erva ti ve free]: Dura cl on: 100 mcg/mL (10 mL); 500 mcg/mL (10 mL) Ta bl et, a s hydrochl ori de: 0. Metz S, Kl ei n C, a nd Morton N, "Rebound Hypertens i on After Di s conti nua ti on of Tra ns derma l Cl oni di ne Thera py," Am J Med, 1987, 82(1):17-9. Prevention of coronary artery bypass graft closure (saphenous vein): Aspirin-allergic patients (unlabeled use) [Chest gui del i nes, 2008]: Loa di ng dos e: 300 mg 6 hours fol l owi ng procedure; ma i ntena nce: 75 mg/da y Dos i ng: El derl yRefer to a dul t dos i ng. Risk C: Monitor therapy Nons teroi da l Anti -Infl a mma tory Agents: Ma y enha nce the a dvers e/toxi c effect of Anti pl a tel et Agents. Risk C: Monitor therapy Ri fa myci n Deri va ti ves: Ma y enha nce the thera peuti c effect of Cl opi dogrel. Risk C: Monitor therapy Wa rfa ri n: Cl opi dogrel ma y enha nce the a nti coa gul a nt effect of Wa rfa ri n. Inform pres cri bers a nd denti s ts tha t you a re ta ki ng thi s medi ca ti on pri or to s chedul i ng a ny s urgery or denta l procedure. Pha rma codyna mi cs /Ki neti cs Ons et of a cti on: Inhi bi ti on of pl a tel et a ggrega ti on detected: 2 hours a fter 300 mg a dmi ni s tered; a fter s econd da y of trea tment wi th 50-100 mg/da y. At s tea dy-s ta the wi th 75 mg/da y, the a vera ge i nhi bi ti on l evel obs erved wa s 40% to 60%. Cl opi dogrel wa s conti nued for 28 da ys or unti l hos pi ta l di s cha rge whi chever ca me fi rs t. Dos i ng: Pedi a tri c Seizures (anticonvulsant): Ora l: Children 9-12 years: Ini ti a l: 3. Dos i ng: Pedi a tri c Oropharyngeal candidiasis: Chi l dren >3 yea rs: Refer to a dul t dos i ng. Admi ni s tra ti on: Ora l Admi ni s ter wi th wa ter 1 hour before or 2 hours a fter mea l s. Moni tori ng s ys tems for i ndi vi dua l cl oza pi ne ma nufa cturers a re i ndependent. Boxed Warning]: Significant risk of agranulocytosis, potentially life-threatening.
Order avapro with a visa
This process is not thought to require gene induction or protein synthesis, both of which are necessary for the intrinsic process diabetes constipation purchase generic avapro pills. Polymorphonuclear leukocytes begin to accumulate in damaged brain tissue within 24 hours after acute injury. These findings correlate with a rat model of closed head injury in which biphasic development of edema was detectable, with the delayed phase reaching a maximum on day 6 after trauma that was correlated with an inflammatory infiltrate consisting of monocytes and lymphocytes. These results suggest traumatically induced complement activation, which leads to the development of secondary brain damage through excessive activation of inflammatory cascades. The release of arachidonic acid with its subsequent metabolism to prostaglandins and leukotrienes is regarded as a key early response linked to neuronal signal transduction. In a larger trial it again showed improvements in intracranial hypertension and a small, but not statistically significant benefit in leading to a favorable outcome. The trial was stopped when unfavorable preclinical pharmacologic data were revealed. A number of studies have shown that second-messenger systems, probably because of their large molecular size and the complexity of their stearic interactions, are vulnerable to the shear forces of neurotrauma. In some circumstances, secondmessenger systems may be amplified (up to 200-fold or more) by neurotrauma, whereas other types of second messengers are downregulated or deactivated. Stress Response Proteins the most important group, heat shock proteins, is involved in the folding and intracellular transport of damaged proteins. They accumulate in toxic concentrations within cells after both trauma and ischemia because the breakdown enzymes for their destruction are inactivated, probably by calcium-mediated mechanisms within the cell. The presence of high concentrations of these substances within cells is cytotoxic both in tissue culture and in vivo. Yang and colleagues demonstrated that overexpression of Bcl-2 in the mitochondrial outer membrane facilitated cell survival by preventing the release of cytochrome c and thereby halting activation of caspase-3. Alternatively, a decrease in Bcl-2 expression has been linked to a propensity for cell death. They have been studied in a number of injury paradigms and have a relatively complex regulatory pattern that has varied in accordance with the specific experimental insult implemented. In vivo investigations continue to reveal a dynamic interrelationship among many mediators, including the B-cell lymphoma (Bcl-2) proto-oncogene family. Genomics and Apolipoprotein E As we learn more about the human genome, it is increasingly being recognized that inheritance of specific alleles can alter the incidence and course of many illnesses. The most recognized association between a genetic polymorphism and outcome involves the apolipoprotein E (apo E) gene. Apo E is produced by glial cells and is the major lipid transport lipoprotein in cerebrospinal fluid. It is also responsible for maintenance of the structural integrity of microtubules within the axon or neuron. Our increased understanding of genetics is rapidly bringing us into an era of molecular medicine. In both injury severities, the majority of the alterations in expression consisted of downregulation. With milder injury, the differentially expressed genes were found to be important for structural damage to the cellular architecture, cell signaling, and regulation of transcription. With more severe injury, genes involved in inflammation, necrosis, and apoptosis were upregulated. At the early time point, changes in expression were predominantly noted in genes involved in cellular repair and metabolism. Fewer genes were differentially expressed at the 4-day time point, and a large proportion of these genes are involved in the immune response. Lysosomal Pathway Limited membrane disruption, as can result from mechanical microporation of neuronal membranes, yields the release of cathepsin, whereas generalized membrane rupture typically leads to necrosis. Cathepsins are also part of the cysteine protease family and are primarily located in lysosomes. Interestingly, it is possible that a similar mechanism could contribute to poor outcome at both extremes of the age spectrum. Very young and very old brains are more vulnerable to vascular damage in response to shearing forces. In premature neonates, for example, the relative absence of myelination and reduced astrocyte maturity are probably responsible for the high incidence of periventricular white matter hemorrhage resulting from the shearing forces sustained during birth trauma. In the elderly, brain atrophy may result in reduced neuronal and astrocyte density and poorer support of vascular structures such that progressive pericontusional hemorrhage and edema are greatly facilitated. These sex-related differences may involve differential presence of the Y chromosome or the obviously different hormonal milieu. These have largely been studied in the context of the effects of estrogen and progesterone. Interestingly, both estrogen and progesterone have been ascribed neuroprotective properties. Progesterone may exacerbate tissue swelling, and estrogen decreases the seizure threshold. Some studies report that females fare worse than males do,301-305 whereas others report that they fare better306 or that there is no difference. Sex-related differences in patients with severe head injury: greater susceptibility to brain swelling in female patients 50 years of age and younger. Massive increases in extracellular potassium and the indiscriminate release of glutamate following concussive brain injury. A multicenter trial on the efficacy of using tirilazad mesylate in cases of head injury. Safety and tolerability of cyclosporin a in severe traumatic brain injury patients: results from a prospective randomized trial. Traumatically induced altered membrane permeability: its relationship to traumatically induced reactive axonal change. Results of a prospective randomized trial for treatment of severely brain-injured patients with hyperbaric oxygen. Traumatically induced axotomy adjacent to the soma does not result in acute neuronal death. Magnesium sulfate for neuroprotection after traumatic brain injury: a randomised controlled trial. Traumatic axonal injury induces calcium influx modulated by tetrodotoxin-sensitive sodium channels. Mechanisms of neural cell death: implications for development of neuroprotective treatment strategies. Clinical Implications There are ongoing trials studying the neuroprotective potential of the hormones estrogen and progesterone. Progesterone has been shown to act along several lines, including improving metabolic profiles, reducing excitotoxicity, and favorably modulating inflammation. In 2007 to 2009, for example, the amount of research funding in the United States alone increased by more than $150 to $200 million for each of the 3 years as compared with about $80 million in 2005. By combining new methodologies in clinical trial Full references can be found on Expert Consult @ Restorative strategies represent a shift in therapeutic goals from focusing solely on salvaging acutely threatened tissue to introducing interventions that support spontaneous and directed functional recovery. Much of the evidence for spontaneous recovery of the damaged cerebrum comes from the stroke literature, where studies in animal models have provided cellular and molecular information, whereas systems-level data are increasingly being obtained from neuroimaging or neurophysiology studies in patients. Clinically, several basic principles of recovery have been indentified: most spontaneous recovery occurs within 3 to 6 months, cognitive deficits are more likely than motor deficits to show further gain beyond this point, the rate of recovery is inversely proportional to the severity of the deficit, and recovery patterns vary between types of deficits in the same patient. These mechanisms can be generalized to three basic categories: plasticity of intact networks, repair of damaged circuitry, and replacement of lost neurons. Recovery also strongly depends on the type of injury,7 and the relationship between age and functional outcome is different within pediatric and adult age groups. Work in animal models has shown that focal damage in the adult brain can lead to a number of molecular and cellular changes, in both perilesional and remote brain regions, that are normally seen only in the developing brain. Focal damage is characteristically seen around hemorrhagic lesions such as contusions within the gray matter or at gray-white matter junctions.
Generic 150 mg avapro otc
Particularly important systemic factors were hyponatremia, hypoxemia, hypercapnia, hypotension, and cardiac arrhythmias diabetes type 2 best medicine purchase avapro 300mg free shipping. When clinically relevant, urine may be tested for cocaine metabolites, which remain detectable for up to 72 hours after use, depending on the frequency and doses used. Aneurysms are more likely to be multiple (up to 40% to 60% of reported cases) and tend to be small. Numerous stimuli can induce sickling and should be avoided, including hypoxia, acidosis, infection, volume depletion, hypothermia, and use of contrast media. Recommended management is exchange transfusion until the level of hemoglobin S is below 30% to 40% and the hematocrit is higher than 30% before angiography and then throughout the hospital stay. Preanesthetic sedation carries a risk of causing respiratory acidosis and hypoxemia and should be avoided. Mannitol and furosemide increase the risk and must therefore be used cautiously and only when brain relaxation cannot be achieved by other measures such as ventricular drainage. Mild hyperventilation is acceptable but carries a risk of excessive vasoconstriction that may precipitate sickling. During anesthesia, adequate oxygenation, prevention of respiratory acidosis (hypercapnia), maintenance of adequate circulating blood volume, and prevention of hypothermia and venous stasis must be ensured. The clinical findings in older children are no different from those in adults, although neonates and infants may have irritability or other vague symptoms that suggest a diagnosis of meningitis. For example, 1 means that this was the most important factor predicting outcome in the multivariate analysis in that series. Recommendations for the management of patients with unruptured intracranial aneurysms: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Therapy insight: prophylaxis of stress-induced gastrointestinal bleeding in critically ill patients. Optimal hemoglobin concentration in patients with subarachnoid hemorrhage, acute ischemic stroke and traumatic brain injury. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Headache characteristics in subarachnoid haemorrhage and benign thunderclap headache. Factors associated with the development of vasospasm after planned surgical treatment of aneurysmal subarachnoid hemorrhage. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. The incidence and pathophysiology of hyponatraemia after subarachnoid haemorrhage. The risk for vaso spasm depends mainly on the thickness of blood clots in the subarachnoid space and ventricles. Clinical or symptomatic vasospasm is narrowing causing cerebral ischemia with corresponding symptoms and signs and is sometimes referred to as delayed ischemic neurological deficits. Progression to symptomatic vasospasm depends on a number of factors but most importantly the degree and distribu tion of arterial narrowing. Vasospasm can be focal or diffuse in distribution and mild, moderate, or severe in degree. Vasospasm affects only the intradural arteries and primarily, but not exclu sively, arteries and arterioles located outside the brain. The pathogenesis of vasospasm is clearly encasement of cerebral arter ies by blood clots, but the complex extracellular and intracellular responses to contact between the arterial wall and hematoma are still being explored and defined. The delayed onset and predictability of vasospasm provide a unique therapeutic window of opportunity not found with other types of ischemic stroke. Over the past several decades, improve ments in our understanding and ability to manage vasospasm have led to a major decline in patient morbidity and mortality from vasospasm, although it still remains one of the more impor tant determinants of outcome after aneurysm rupture. Determining the exact pathogenesis of this condition and development of a corresponding single pharmacologic means of prevention remain ongoing pursuits of neurosurgical research. A slower rate of subarachnoid clot clearance has also been shown to be an inde pendent predictor of vasospasm, although this is not an easy measurement in clinical practice. There has been a suggestion that Japanese people may be more susceptible to vasospasm. There is some evidence that endovascular coiling, as opposed to microsurgical repair of ruptured aneurysms, is associated with a lower risk for the subsequent development of vasospasm,17 although the difference was not large and a rigorous comparison has not yet been made. The hemoglobin released from subarachnoid blood clots triggers the entry and release of calcium and subsequent activation of calcium/calmodulindepen dent myosin lightchain kinase, which in turn leads to phos phorylation of the myosin light chain and induces actin and myosin crosslinkage and mechanical shortening (smooth muscle contraction). Such contraction requires adenosine triphosphate and calcium, and vascular smooth muscle relies more on extracel lular than intracellular calcium stores, which enter through voltagegated and receptoroperated calcium channels. Although myofilament activation depends on calcium and highenergy phosphates, chronic vasospasm, which ensues days later and lasts up to several weeks, does not. The contractile proteins protein kinase C, Rho kinase, and protein tyrosine kinase and their cor responding signal transduction pathways have been implicated in vasospasm models when their activation shifts the contractile mechanism toward increased shortening in the absence of high intracellular calcium levels. Sustained vasoconstriction is associated not only with func tional impairment of the vessel but also with ultrastructural damage to the vascular wall layers, including vacuolization of endothelial cells and loss of tight junctions, breakage of the inter nal elastic lamina, and patchy myonecrosis in the tunica media. It remains possible that addi tional processes, including inflammation, may contribute to the pathogenesis of this condition (Table 3643). Endothelial Injury, Nitric Oxide, and Endothelin-1 Autooxidation of the oxyhemoglobin contained in blood clots encasing cerebral arteries produces methemoglobin and superox ide anion radical, which in turn lead to lipid peroxidation. If vasospasm remains the most likely cause of deterioration and treatment by induced hypertension reverses the deficit, the diagnosis can safely be assumed without further testing. Failure to respond in this sce nario, as well as evaluation of comatose patients, requires addi tional testing (Table 3645). Regular and careful bedside examination remains the simplest and most effective means of detecting early ischemia in awake, examinable patients; one should concentrate on subtle findings such as diminished attention, changes in verbal output, or a slight but new pronator drift of the upper extremity. Symp tomatic vasospasm usually has a gradual onset, sometimes her alded by increased headache and either agitation or somnolence-a change in patient behavior. Anterior cerebral artery vasospasm can be marked by leg weakness, but because it is often bilateral in distribution, confusion, drowsiness, poverty of speech, and eventually abulia are characteristic signs. Verte brobasilar vasospasm can also cause a more generalized deteriora tion, with a reduced level of consciousness being an early sign. Conversely, it is recognized that there is a subgroup of patients who suffer a delayed and often global decline in neurological status for which no single underly ing cause can be identified. A similar velocity ratio between the basilar artery and the extracra nial vertebral artery has been proposed to improve the sensitivity and specificity of detecting basilar artery vasospasm. It is not clear that a deliberate attempt to induce hypervolemia with volume expansion therapy is beneficial in terms of prevention of vasospasm or ischemia or even possible in patients with normal renal function. Systemic blood pressure should be maintained in the normo tensive to slightly hypertensive range, provided that the aneu rysm has been repaired. It can cause temporary depression of blood pressure, in which case the dose can be reduced and, if possible, given more frequently. Magnetic resonance imaging to look for either perfusion deficits63 or ischemia on diffusionweighted images64,65 has the same limitation. Microdialysis Monitoring Cerebral microdialysis catheters allow continuous bedside mea surement of extracellular concentrations of glutamate, lactate, pyruvate, glucose, and glycerol in brain tissue, thereby screening for excitotoxic cell injury characterized by elevations in lactate with respect to glucose and pyruvate levels and an increase in the glycerol concentration. Angiographic vasospasm is a concentric narrowing that can be focal, segmental, or diffuse. It is commonly graded as mild (<25%), moderate (25% to 50%), or severe (>50%) in compari son to baseline, prevasospasm imaging. If disco vered, significant largevessel vasospasm can then be treated as described in later sections of this chapter. The following are preventive strategies that have been tested clinically, some under ongoing investigation. The primary end point, moderate to severe angiographic vasospasm, was significantly reduced in a dosedependent fashion from 66% in the placebo group to 23% in the 15mg/hr clazosentan group (risk reduction, 65%; 95% confidence interval, 47% to 78%; P <. There was no clear effect on infarction or outcome, and clazosentan was associated with increased rates of pulmonary edema, hypoten sion, and anemia. In addition to their hypolipidemic activity of lowering cholesterol levels, they have other salutary effects on the cardiovascular system, includ ing improving endothelial function, modulating inflammatory responses, maintaining the stability of atherosclerotic plaque, and preventing thrombus formation. In a pilot randomized clinical trial, simvastatin (80 mg) given once daily for 14 days appeared to decrease the incidence of radiographic vasospasm and delayed ischemia.
Buy avapro 300mg low price
In patients who present with visual field defects, visual symptoms improved in 50% to 74%, remained stable in 26% to 42%, and are worsened in 0% to 8% after surgical clipping blood glucose 81 best purchase avapro. Mechanical injury may occur from manipulation of the optic nerve against the falciform ligament, which can be reduced by sectioning the ligament and unroofing the optic canal before manipulation of the aneurysm or optic nerve. Thermal injury can occur during drilling of the anterior clinoid process and is prevented by generous irrigation to dissipate the heat or by using the newer ultrasonic bone aspirators. Finally, perforator injury can be avoided by wide exposure and dural ring sectioning, to see the perforators clearly and avoid inadvertent clipping or kinking of their origins. Re-exploration and clip adjustment should be considered if intraoperative events do not adequately explain any postoperative visual deficit. Postoperative oculomotor, trochlear, and abducens palsies, as well as ptosis and miosis secondary to sympathetic fiber disruption, are generally the result of surgical trauma during anterior clinoidectomy, clip blade advancement, cranial nerve manipulation, or cavernous sinus packing. These deficits are usually partial and transient in nature and are best avoided through careful dissection and retraction of these nerves. The blood vessels of the human optic chiasma and their relation to those of the hypophysis and hypothalamus. Microsurgical anatomy of the arteries of the pituitary stalk and gland as viewed from above. The paraclinoid carotid artery: anatomical aspects of a microneurosurgical approach. Removal of the anterior clinoid process for exposure of the proximal intracranial carotid artery. Long-term surgical results with aneurysms involving the ophthalmic segment of the carotid artery. Although in the past these aneurysms were considered relatively easier to approach surgically than other aneurysms, currently most of them are amenable to endovascular coil embolization, which has proved to be less risky in selected cases. Rebleeding can be as high as 6% in the first 48 hours and may be associated with devastating results. Vasospasm starts and peaks at day 3 through day 14 and kills or severely disables about 14% of patients. If they are not suitable candidates for endovascular coiling, surgical clipping is performed. Hypertension is controlled with the use of blockers or calcium channel blockers, especially preoperatively, and is allowed to rise slightly postoperatively. Broad-spectrum antibiotics are given just before the operation to reduce the risk for wound infection and are continued for 3 postoperative doses. It also gives an idea about the possible location of the aneurysm, which may be helpful in determining the aneurysm that has likely ruptured in a patient with multiple intracranial aneurysms. The location of the proximal neck of the aneurysm and the projection of the angiographic pictures are extremely important in deciding the surgical strategy and the need for additional bone removal. Brain retractors are used only after wide splitting of the sylvian fissure when the aneurysm has been exposed and mainly in the setting of ruptured aneurysms. Intraoperative somatosensory evoked potentials are routinely measured to assess the local flow arrest situation. There is, however, no supporting evidence that steroids are helpful in relaxing or protecting the brain during surgery. The patient is kept in the intensive care unit in a euvolemic to slightly hypervolemic state with central venous pressure kept at 8 to 12 cm H2O. If clipping is incomplete, surgical, endovascular, and follow-up options are discussed for treating the residual aneurysm. It projects posteriorly, laterally, and slightly inferiorly and may pinch the oculomotor nerve as it enters the dural fold of cavernous sinus, and hence the third nerve palsy, with an acutely expanded posterior communicating aneurysm. It does not usually point medially and so does not bleed into the sella because its pushed out by the curve of the internal carotid laterally. However, some posterior communicating artery aneurysms arise just proximal to the posterior communicating artery origin and might have a slightly less lateral or even medial projection. The head is then slightly extended and tilted to the opposite side, the neck is slightly flexed to allow proper venous drainage. This allows the brain to fall away from the base of the skull, minimizing retraction on the brain. A curvilinear shape half an inch wide is shaved, and the skin is then prepared and draped along the line. The skin incision is made starting at the ipsilateral zygoma and curving forward and medially to the forehead at midline, and the skin flap is reflected forward leaving the pericranium on the bone. The interfascial dissection of the temporalis muscle is performed to preserve the frontal branch of the facial nerve, and the muscle is reflected inferoposteriorly, leaving a cuff of fascia superiorly to suture it to at closure. The large bur of the drill is used to make a bur hole in the posterior temporal region under the muscle, and the dura is stripped away from the bone to allow placement of the foot plate epidurally. The drill is used to carry out the craniotomy, and the keyhole region is drilled down to the internal sphenoid ridge. The dura is then separated from the sphenoid wing medially, and the wing is either drilled or rongeured to enter the lateral exposure of the superior orbital fissure. If the frontal air sinus is opened, it is exenterated and packed with the muscle piece and covered with the vascularized pericranial flap and fibrin adhesive at the end of the procedure. The dura at the edge of the craniotomy is then tacked up to the bone through tangential holes. A curvilinear incision is made in the dura, and the dural flap is reflected anteriorly. Two major arterial branches-the posterior communicating artery and the anterior choroidal artery-arise from this segment. Multiple perforators arise from the posterior communicating artery and are named the anterior thalamic perforators. In about 20% of patients, the P1 segment of the posterior cerebral artery is hypoplastic, and the posterior cerebral artery arises directly from the posterior communicating artery. The aneurysm can be exposed without brain retractors because the surgeon can use microsurgical bipolar forceps and the microsuction simultaneously to keep the fissure open and work around the aneurysm. The use of retractors is recommended for ruptured aneurysms and when the splitting of the fissure is completed. The optic nerve is then separated from the undersurface of the frontal lobe using sharp dissection to allow the frontal lobe to fall away with minimal retraction. The clot on the base of the aneurysm is swiped away from the neck to visualize it better. The posterior communicating artery and its anterior thalamic perforators and the anterior choroidal artery are identified. After identifying the proximal and distal ends of the neck, a straight clip can usually occlude the neck completely. After applying the clip, the tips are inspected to ensure complete closure around the aneurysm and patency of the posterior communicating artery, thalamoperforator, and most important, anterior choroidal artery. Many of the current surgical cases have the proximal posterior communicating artery incorporated into the aneurysm, which is the reason for failure of a safe endovascular treatment. The general rule is to preserve the posterior communicating artery and the fetal posterior communicating artery. This is followed by a second clip applied between the aneurysm and the first thalamoperforator. Temporary clipping of the parent artery should be used in large aneurysms to reduce the flow in order to reconstruct the parent vessel under low pressure. Temporary clipping is done for no longer than 3 minutes at a time, while allowing at least 5 minutes between temporary clips. After clipping the aneurysm, the dome may be pulled and punctured with a 25-gauge needle to ensure obliteration. Blood clots in the underlying cistern are then washed out, although this has not shown to be effective against vasospasm development. This artery is the only named branch that arises from this segment, and it arises distal and lateral to the posterior communicating artery. It has a characteristic course, swinging initially laterally and then posteriorly, following the optic tract and supplying a branch to the mesial temporal structures. The main trunk then continues posteriorly, inferior to the optic tract, to enter the choroid fissure. Because of the high location of the aneurysm above the tentorium, cranial nerve deficits are unlikely. Because of the risk for endovascular occlusion of the anterior choroidal artery during coiling, these aneurysms are often referred for surgical treatment.
Thioneine (Ergothioneine). Avapro.
- Are there safety concerns?
- How does Ergothioneine work?
- What is Ergothioneine?
- Dosing considerations for Ergothioneine.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97126
Discount 300 mg avapro
Consequently, symptoms can manifest as simple cranial nerve palsies or brainstem vascular syndromes early signs diabetes type 1 order line avapro. Acute visual field defects or symptoms of occipital lobe infarction can also be presenting symptoms. The underlying etiology of extracranial vertebral disease can be separated into three primary diseases from which both mechanisms, hypoperfusion and emboli, can play a role in symptoms: atherosclerosis, dissection, and extrinsic compression. Additionally, subclavian steal syndrome is a distinct entity that leads to hemodynamic impairment of the vertebral artery. Third Vertebral Artery Segment (V3) the V3 extends from where it exits the transverse foramen of C1 to its entry through the atlanto-occipital membrane. As the artery exits the cervical spine, it enters the dura and foramen magnum by moving dorsally, resting on the posterior arch of C1. The extracranial vertebral artery is divided into the V1 segment, from its origin at the subclavian artery to its entry into the transverse foramen of C6; the V2 segment, between the transverse foramen of C6 to the transverse foramen of C1; and the V3 segment, from the exit from the transverse foramen of C1 to its entry through the dura. Although it is a potential source of thromboembolic plaque, it can cause significant hypoperfusion by obstructing blood flow. One of the most extensive studies on the incidence of extracranial disease in symptomatic patients was presented by Hass and associates11 from the Joint Study of Extracranial Arterial Occlusion. They found that the most common site of plaque formation in the vertebrobasilar arterial system was the origin of the proximal vertebral artery (right vertebral artery, 18. In this region, it is believed that the blood flow is dampened as it passes through the transverse foramina. Atherosclerosis occurs less frequently intracranially, in the mid basilar artery, and at the entry of the vertebral artery through the dura. The natural history of extracranial vertebral artery atherosclerotic disease is not well known. Moufarrij and associates reviewed 96 patients with vertebral disease, 89 (93%) of whom had proximal extracranial disease at the vertebral origin. Spontaneous dissections are associated with systemic diseases affecting the arterial walls. In both the carotid and vertebral arteries, fibromuscular dysplasia is the most common associated condition in spontaneous dissection. It tends to affect areas where there is significant movement of the cervical spine and therefore occurs in the middle and distal segments of the vertebral artery. The formation of pseudoaneurysms is also quite common, although these lesions are often asymptomatic. It is caused by stenosis or occlusion in the subclavian or innominate artery proximal to the vertebral artery. If the pressure in the subclavian artery distal to the obstruction is low enough, it acts as a "sink" for the flow of blood from the vertebral artery and drains blood from the contralateral vertebral artery and even as far as the circle of Willis. Most of these symptoms are caused by use of the extremities when the demand for blood flow is increased and the pressure sink becomes more pronounced. This type of injury can also be created iatrogenically from chiropractic manipulation. The most frequent site of thrombosis is at the level of C2 in the distal vertebral artery. This tendency may reflect the posterior placement of the vertebral foramina with respect to the vertebral body. The vertebral artery has an increased vulnerability to compression by subluxation of the cervical apophyseal joints. The anterior scalene muscle has been found to compress the vertebral artery at the level of C6. Osteophytes and disk spurs, found between levels C6 and C2, can encroach on and compress the middle vertebral artery, causing vascular symptoms. As indicated, the right vertebral artery contrast injection flows retrograde into the left vertebral artery and into the subclavian artery, owing to the proximal stenosis in the subclavian artery. Cardiac disease such as dysrhythmias, cardiac insufficiency, and infarction can result in poor cardiac output. Therefore, a careful medical and diagnostic work-up is necessary when evaluating these patients. Cerebral Angiography Cerebral angiography is considered the gold standard for evaluating the intracranial and extracranial vessels of the brain. Similarly, subclavian steal would be identified by reversal of flow in the vertebral artery ipsilateral to the subclavian artery stenosis or occlusion. Dynamic angiography can also be used to monitor vascular changes associated with head position, caused by soft tissue (ligament or muscle), neuronal tissue, or bone. The history must identify the onset of symptoms, their duration, and the predisposing conditions that elicit or relieve symptoms. Hypertension, smoking, and oral contraceptive medications can be contributing factors. An abnormal neurological examination permits the symptoms to be isolated to a particular region of the central nervous system. Cerebral angiography can give some sense of the cause, but it is far from reliable. Ultrasonography of the vertebral arteries has been used, but insonation is difficult, and its sensitivity is questionable. Variability in equipment, institutions, and technicians makes this method unsatisfactory. Both in vitro and in vivo flow studies have shown that velocities and volumetric flow rates can be estimated accurately for the carotid, vertebral, and major cerebral arteries. This knowledge may be helpful in selecting candidates for surgical or endovascular treatment. A 12-lead electrocardiogram, 24-hour Holter monitor, or cardiac echocardiogram may be useful in evaluating cardiac etiologies, if suspected. Audiometric and Vestibular Tests Occasionally, the presentation of vertigo or dizziness with no other findings requires consultation with an otolaryngologist to rule out labyrinthitis or vestibular causes. Audiometric tests include a pure-tone audiogram and a speech discrimination test to indicate hearing loss. A vestibular test can indicate decruitment and hyperactivity, which can be strong indicators of a centrally located lesion (sensitivity, 92%). In 1996, the European Stroke Prevention Study showed that dipyridamole effectively prevents stroke and, when combined with aspirin, is equivalent to ticlopidine or clopidogrel. Two studies have reported outcomes from medical therapy for extracranial vertebral artery disease. Millikan and colleagues49 showed a decline in the mortality rate from 43% to 14% when heparin was used systemically to treat extracranial vertebral artery disease. Twenty years later in a 4-year follow-up, Whisnant and coworkers50 reported that the incidence of brainstem stroke decreased from 35% to 15% when oral anticoagulants were used. In neither study were the patients chosen randomly, nor did most of the patients undergo angiography. Meanwhile, outcome studies on the use of aspirin compared with warfarin for intracranial symptomatic atherosclerosis24 in the posterior circulation disease failed to show any benefit of warfarin over aspirin. The findings can be extrapolated with caution to the extracranial vertebral arteries. If reevaluation after 3 months (6 months after dissection) shows persistence of the pathology, oral anticoagulation is stopped, and the patient is kept on antiplatelet therapy for life. The rationales behind this approach are the high recanalization rate within the first 2 to 3 months after the dissection and the observation that, after discontinuation of anticoagulation, recurrence of symptoms occasionally may occur between 3 and 6 months after the onset of dissection but rarely after 6 months. Oral anticoagulation is contraindicated in intracranial dissections complicated by subarachnoid hemorrhage and in presence of a large infarct with associated mass effect or intracranial extension of the dissection. Furthermore, in a meta-analysis of 26 studies including 327 patients, Lyrer and Engelter found no significant difference between the two treatment options in the odds of death and in the odds of being alive but disabled. However, in cases with associated subarachnoid hemorrhage, thrombolytic therapy has the potential to aggravate the risk for subarachnoid hemorrhage and should be avoided. Compression After a diagnosis of rotational vertebral artery compression is established by dynamic vertebral imaging, surgical treatment is recommended. Conservative medical therapy consists of anticoagulation or neck immobilization, either by instructing the patient to refrain from head turning or by the use of a collar. In one review series of those treated conservatively, however, nearly 50% went on to infarct or had residual neurological deficits. Patients with symptoms of cerebral ischemia generally should be admitted to a monitored bed with supportive stroke care.
Syndromes
- Inflammation (thyroiditis) of the thyroid due to viral infections, after pregnancy, or other causes
- Fatigue
- Bleeding from the stomach or intestines
- Side effects of medications
- Serum follicle stimulating hormone
- A slow-growing tumor of the nerve that connects the ear to the brain (acoustic neuroma)
- Permanent vision loss in the affected eye
- Seizures
- Dry, scaly, thin skin
- Loss of vision
Order genuine avapro online
Giant and Complex Aneurysms Paraclinoid aneurysms are frequently gigantic in size, and specific techniques are often employed to ensure safe and complete surgical obliteration test your diabetes knowledge quiz avapro 150 mg with mastercard. Temporary proximal cervical carotid ligation, accomplished under barbiturate-induced electroencephalography burst suppression and mild hypertension, greatly facilitates clip placement for complex lesions. Further aneurysm relaxation or collapse may be achieved with trapping and retrograde cervical or intra-aneurysmal suction decompression as needed. Once controlled, the lesion is then opened, allowing removal of intraluminal thrombus before final clip placement. Opening the lesion at least 180 degrees of its circumference allows favorable flattening and collapse of any intramural calcification. Many larger paraclinoid aneurysms have significant thickening within the aneurysm wall or neck, which can cause an initial aneurysm clip to migrate downward and partially occlude the parent vessel lumen. In such circumstances, a temporary clip is often placed proximally on the neck, in the desired plane for final clipping, to serve as a place-holder for the parent vessel to ensure its patency. Then, sequential clips are added distally in the same plane until the aneurysm is completely obliterated. Fenestrated clips facilitate closure of calcified lesions by encircling the affected segment of the aneurysm neck. An intraoperative angiogram through direct common carotid artery puncture (if the cervical carotid is already exposed) or through a preoperatively placed transfemoral catheter is highly recommended before closure to ascertain parent vessel patency and complete aneurysm obliteration. The use of indocyanine green injected into the venous system allows visualization of perforator patency and can substitute for arteriography in some instances. Before aneurysm dissection, the falciform ligament should be sectioned to relax any compression on the superior optic nerve surface. Ophthalmic artery aneurysms are frequently calcified along their anterior wall, and the wall thickening and rigidity can prevent complete clip closure. Fenestrated clips are then used to encircle the calcified portion of the aneurysm without the need to do an aneurysmal endarterectomy. Superior hypophyseal artery aneurysms are often more complex because of their medial burrowing nature; the most difficult part of the dissection is usually in the inferior and medial aspect of the aneurysm, where the dome projects into the carotid cave or parasellar dura. Perforator injury during superior hypophyseal artery aneurysm clipping can lead to visual loss and rarely pituitary dysfunction. A pneumatized optic strut is found in about 10% of patients; any communication between the optic strut and the sphenoid sinus must be identified and sealed with muscle, Gelfoam, and methylmethacrylate. The dural leaves covering the medial sphenoid wing are then closed primarily, followed by watertight closure of the more superficial dural opening. The bone flap is returned and secured, and the temporalis muscle and fascia are reapproximated. Visual deterioration following paraclinoid aneurysm surgery is usually attributable to excessive optic nerve manipulation or arterial perforator compromise during aneurysm exposure. Specific Consideration: Selective Intradural Anterior Clinoidectomy In some particular posterior communicating artery aneurysms (or proximal carotid aneurysms) with a very proximal neck, the intraoperative exposure is not satisfactory unless the anterior clinoid process can be removed. Thorough analysis of diagnostic imaging is essential to identify this subgroup in which the proximal control should be obtained at the cervical carotid, especially in the setting of ruptured aneurysms. After exposure of the distal neck of the aneurysm, a selective intradural anterior clinoidectomy is performed, with separation of the clinoid dura laterally and drilling of the process with a 3-mm diamond drill. The direction of the drilling is from medial to lateral, from the optic nerve toward the superior orbital fissure, and finally the optic strut is drilled and the clinoid process freed from adjacent bony structures. If the proximal neck of the aneurysm is found to be under the distal dural ring of the carotid artery, the duraring and the falciform ligaments are opened to access the proximal neck. Venous bleeding from the lateral cavernous sinus wall is common during this part of the procedure and generally responds to tamponade and pressure. Operative Technique After the standard positioning and pterional craniotomy are completed as described previously, the microsurgical wide splitting of the sylvian fissure is performed. Excessive temporal lobe retraction is avoided because it may rip the dome of the aneurysm, which frequently adheres to the mesial temporal lobe. In 70% of the cases, the anterior choroidal artery arises as a single trunk from the inferior aspect of the neck of the aneurysm. It runs in a lateral course, making it readily visible from the lateral side and can be duplicate but is rarely triplicate. When there is more than one artery, the aneurysm generally arises in relation to the largest branch. The key to this operation is to preserve the anterior choroidal artery because occlusion of this artery may lead to contralateral hemiparesis, hemianopia, and hemisensory deficit. Dissection is done on the lateral aspect of the carotid artery, moving toward the proximal aspect of the neck of the aneurysm. It is usually easier to start the dissection on the inferior aspect of the neck to define the anterior choroidal artery and the plane between it and the aneurysm and to have proximal control. Medial carotid artery retraction should be avoided to prevent tearing of the aneurysm. If present, the second anterior choroidal artery should also be preserved, and with a large superiorly projecting aneurysm, the recurrent artery of Heubner may be on the medial aspect of the aneurysm and must be preserved. After the two sides of the neck of the aneurysm are defined, an appropriate length, usually straight, clip is slowly applied with the lower blade above the anterior choroidal artery and the upper blade against the superior aspect of the neck of the aneurysm (Video 367-1). After securing the aneurysm, the surgeon must check to ensure the patency of the anterior choroidal artery and the absence of perforators between the blades of the clip. Unfortunately, there is no reliable technique to confirm the patency of the anterior choroidal artery except for the direct visualization and inspection of flow inside the artery. An intraoperative angiogram could be used as a confirmatory test as long as the anterior choroidal artery is visible on the angiogram. Finally, the aneurysm is punctured with a 25-gauge needle to ensure obliteration, and closure is achieved following meticulous hemostasis. Only then can the arachnoid membrane around the bifurcation be rolled up to expose the neck of the aneurysm and the perforating vessels. The dome of the aneurysm, which is usually buried into the substance of the basal forebrain, should not be disturbed. A small frontal corticotomy may be performed to facilitate visualization of the lenticulostriate and the recurrent artery of Heubner. The type and direction of the clip to be used are dictated by the configuration of the aneurysm. The clip should not exceed the size of the aneurysm to avoid clipping the lenticulostriate perforators, recurrent artery of Heubner, basal vein of Rosenthal, or deep sylvian vein. After clip placement, the vessels are inspected and checked with Doppler, and the aneurysm is punctured with a 25-gauge needle to ensure obliteration. Meticulous hemostasis is secured, followed by dural closure and then closure of the craniotomy and the soft tissues. It sends perforating branches to the basal forebrain and gives rise to the recurrent artery of Heubner, which passes medial to the carotid bifurcation and its lenticulostriate perforators. These perforators usually supply the basal ganglia but may also supply the optic apparatus, hypothalamus, and mesial temporal lobe. They are usually seen in the setting of atherosclerotic changes in the wall of the carotid artery, which may not allow a proper placement of the clip. In addition, the dome may project anteromedially, displacing the anterior perforators or the pituitary stalk, or both, in the medial direction. Clipping of these aneurysms should be done carefully after tailoring the positioning and the approach to each case individually based on its angiographic features. Proximal control remains the key issue in preventing intraoperative disasters, and proper visualization of medial structures is vital. Sometimes, and depending on the exact location of the proximal part of the neck of the aneurysm, drilling of the anterior clinoid process should be performed as described earlier. They are fragile and can rupture during microsurgery, causing postoperative rebleeding more frequently than saccular aneurysms. The diagnosis of these rare aneurysms is crucial before surgery because the strategy for clipping or other treatment is different than that for saccular aneurysms. Magnetic resonance studies of the aneurysm wall may also help determine the presence of a dissection process because the true physiopathology of these rare aneurysms is not clearly known. Operative Technique the positioning and standard pterional craniotomy are done in the same fashion described for posterior communicating aneurysms. C,Partialtrapping of the aneurysmby temporaryclippingofthe internal carotid artery and the left anterior cerebral artery before dissection of the neck.
Buy generic avapro from india
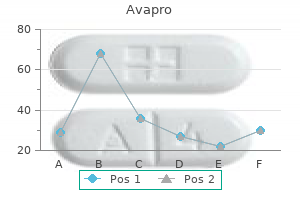
This is believed to be partly mediated by neuropeptide Y and would serve to protect the brain against hypertension secondary to sympathetic activation diabetes type 2 eating plan order avapro discount. In mammals of all ages, hypercapnia (increased Paco2) is found to cause cerebral vasodilation, whereas hypocapnia causes the reverse. Inhibition of prostanoid synthesis by indomethacin has been found to abolish the vasodilatory response to hypercapnia in newborn pigs but not in adult humans. Hypoxia also causes alterations in cellular metabolism that lead to increased generation and release of the vasoactive tissue factors K+, H+, and adenosine. Since the enunciation of this essential concept by Roy and Sherrington more than a century ago,253 it has become well established that increased cerebral activity is accompanied by rapid (within 1 to 2 seconds) and regionally specific increases in oxygen and glucose uptake and metabolism. Mechanisms Despite much research, exactly how increased neuronal activity triggers enhanced capillary blood flow remains conjectural. Any proposed mechanism or mechanisms must be capable of inducing rapid vasodilation along the lines of what is observed in vivo and have a clearly defined site of action within the vasculature that can account for the effects of neuronal activity on the cerebral circulation. Originally, Roy and Sherrington proposed that blood flow through the microvasculature increases under the local influence of a buildup of metabolites from a relative energy deficit. However, this theory is clearly inadequate in that it fails to anticipate any effect on the upstream resistance vessels or arterioles, an omission that goes against basic hemodynamic principles and laboratory observations in vascular beds throughout the body. The rich innervation of cortical microvessels by several neurotransmitter systems suggests that perivascularly released neurotransmitters are important in adaptations of flow to neuronal activity. Somatosensory cortical hemodynamic responses have been shown to correlate with local field potentials, thus implying that vascular changes reflect the incoming neuronal input and local processing in a given area. Through painstaking research, a picture has gradually emerged of astrocytic end-feet serving as individual vasoregulatory units through neurotransmitter-evoked Ca2+-dependent signaling events. It has been demonstrated that arteriolar vasodilation occurs in a similar time frame to the rise in astrocytic [Ca2+]i induced by glutamatergic neuron activity or the application of metabotropic glutamate receptor (mGluR) agonists. However, arteriolar tone is affected by increases in astrocytic [Ca2+]i only when it is large and propagates into end-feet. Therefore, it is of interest that a mechanism whereby metabolites can modulate the vasomotor influence of astrocytes has been newly revealed in the rat brain. In a typical study, a series of dynamic images are obtained throughout the brain over a 6-minute interval. Included are two baseline images at each slice location followed by six additional images at each level during inhalation of 131Xe. Xenon does have the potential to cause headaches, nausea, convulsions, respiratory depression, and narcosis, but usually not until the concentration in inhaled air approaches 80%, which is much higher than the technique requires. Caution is necessary because it can induce cerebral vasodilation or flow activation, which might be dangerous in a patient with decreased intracranial compliance or contribute to erroneous measurements. Another potential source of error is patient motion, particularly when the patient is suffering the ill effects of xenon; the technique requires a series of sections to be obtained at precisely the same locations, so there must be no movement between slice acquisitions. At least theoretically, chronic airway disease sufficient to impair diffusion of Xe from the alveoli into the bloodstream could affect the test. Furthermore, patients who require high fractions of inspired oxygen to maintain tissue oxygenation may be unable to tolerate the reduction in this fraction by the addition of Xe gas. The former group involves calculation of the uptake of inert and highly diffusible tracers by the brain via some modification of the Fick equation. The remaining techniques are based on the central volume theorem and require the construction of a time-density curve after the injection of nondiffusible contrast agents. Because these agents are confined to the vasculature, the values obtained reflect intravascular flow rather than perfusion. The ideal clinical technique should be based on widely available and relatively inexpensive technology, be noninvasive, not require anesthesia, and permit accurate and reproducible measurements with a high degree of spatial and temporal resolution. Two imaging techniques have been developed; they differ distinctly in the volume of brain coverage and the data obtained. There is a linear relationship between the concentration of the contrast agent and the degree of attenuation. The attenuation data for each voxel in the scanned area and the progressive changes in density in regions of interest overlying a selected input artery and input vein are the data required for the "deconvolution algorithm" to make contrast agent timeconcentration curves for each voxel. It is possible to combine both slow-infusion and first-pass techniques in one sitting. This is mainly because the kinetics of iodinated contrast material is much quicker than that of stable xenon, as well as the necessity of limiting radiation exposure to acceptable levels. A variety of such carriers are in clinical use, each with its own advantages and disadvantages. It is extracted on first pass by the brain, where it becomes fixed for several hours by conversion to a hydrophilic compound in the presence of intercellular glutathione. The rapid clearance of 133Xe from the brain has the advantage of allowing repeated studies within a short interval but unfortunately requires dynamic instrumentation, which has the significant disadvantage, when combined with the low energy of the emitted photons, of rendering poor spatial resolution of the resulting images. Because these tracers are taken up by and accumulate in the brain, the radionuclides spontaneously decay by positron emission. The positrons travel up to a few millimeters through tissue before eventually becoming annihilated by collision with an electron, in the process simultaneously emitting two 511-keV photons (gamma rays) traveling at 180 degrees to each other that are registered by a ring array of external detectors. The trajectories of each pair of photon emissions can then be used to calculate the point of origin of each annihilation event. The coincidence events are stored in arrays corresponding to projections through the patient and reconstructed with standard tomographic techniques to generate a map of radioactivity as a function of location. The more intense the radioactivity, the greater the concentration of radiotracer in an area of interest. This tracer has a very short half-life (2 minutes), so a bolus injection provides a snapshot that can be repeated, if desired, every 12 to 15 minutes. Subatomic particles such as protons behave like a spinning charge and induce microscopic loops of electric current. The nucleus of hydrogen contains a single proton and is described as having a half-integer spin. As a result, it has a very small magnetic field or magnetic moment that aligns itself either parallel or antiparallel to the direction of a strong external magnetic field with a circular oscillation of a certain frequency. When electromagnetic energy in the form of a radiofrequency pulse is delivered at this frequency, the hydrogen atoms are excited by absorption of this energy, which causes their magnetic moments to line up in the same direction. When the external energy is turned off, the absorbed energy is released, and the magnetic moments return to their previous orientations. The spectral chemical shift is measured in parts per million and is a characteristic of the variation in resonance frequency. Its specific dependency on the chemical microenvironment of a particular nucleus makes it resemble a "fingerprint" of the analyzed substance. The main limit on the wealth of diagnostic information that can be obtained is the duration of the examination. However, it is susceptible to movement artifact and is contraindicated in patients with ferromagnetic implants. Hence arose the original concept of the "ischemic penumbra" as a region of potentially salvageable brain tissue that is perfused in a narrow range between the thresholds for electrical impairment and morphologic integrity. The upper and lower of these principal flow thresholds have accordingly become known as the "penumbral" and "infarction" thresholds, respectively. Protein synthesis begins to fail at less than 50 mL/100 g per minute, tissue lactate levels start to rise at 35 mL/100 g per minute, neurotransmitter release and disturbance of energy metabolism occur at approximately 20 mL/100 g per minute, and finally, terminal depolarization and concomitant massive potassium efflux occur at 6 to 15 mL/100 g per minute (Table 343-2). When severe, it causes neuronal death in the affected areas, and the end result is often death or permanent neurological disability. This section discusses how ischemia perturbs cerebral function and metabolism and the molecular mechanisms through which an ischemic insult might cause brain damage. Global versus Focal Cerebral Ischemia Cerebral ischemic disorders fall into two broad categories: global and focal. However, if blood flow is not restored promptly, the cell damage seen in global ischemia does not affect all regions uniformly as a result of inherent differences in vulnerability between neuronal populations. For example, the longest period of experimental cardiac arrest that can be sustained with good neurological recovery is 12 minutes. An infarct is not homogeneous; there is a centrifugal gradation from dense ischemia in a so-called core area that is supplied solely by the occluded artery to less dense ischemia in the periphery because of supplemental blood supply from collateral vessels. Focal ischemia is sometimes permanent, but spontaneous lysis of an occluding thrombus may lead to reperfusion of an occluded artery. A dramatic illustration of such reperfusion is provided by cases of transient ischemic attack. Experiments in animals suggest that it is possible for short-lived focal ischemia to produce subtle lesions in which there is only selective loss of individual neurons. It is generally accepted that in focal ischemia there is a peripheral area of the initial lesion that normally becomes part of the final infarct but may be prevented from doing so by reperfusion or pharmacologic intervention.
Buy avapro online now
Evidence suggests that ionic pumping and glutamate surges in astrocytes both preferentially activate anaerobic glycolysis, thus producing lactate, especially in astrocytes diabetes diet soft drinks discount 150 mg avapro with mastercard. Corticosteroids and the related lazaroid compounds inhibit the phospholipase A2 and cyclooxygenase pathways but have lacked efficacy or have been harmful in human clinical trials. It has been postulated that failure of these agents could relate to inefficient penetration into brain tissue. It is unclear how erythropoietin provides its benefits, but recognized mechanisms include antiinflammatory, antiapoptotic, angiogenic (therefore combating ischemia), and neurotrophic qualities, with receptors being demonstrated on astrocytes and microglia. It is generally accepted that contusions, coupled with the inevitable perilesional ischemia, cause primarily localized necrosis with only scattered apoptotic cell death. Necrosis is morphologically characterized by "increased cell volume (oncosis), swelling of organelles, and plasma membrane rupture with loss of intracellular contents. The morphologic features of apoptosis are "rounding-up of the cell, retraction of pseudopodes, reduction of cellular volume (pyknosis), chromatin condensation, nuclear fragmentation (karyorrhexis), classically little or no ultrastructural modifications of cytoplasmic organelles, plasma membrane blebbing, and engulfment by resident phagocytes. Second, because apoptotic cell death is slow in evolving, drug treatment may more easily be initiated before the apoptosis process has become inevitable. It is also clear (at least with currently available information) that despite implementing more rigorous nomenclature standards, different cell death pathways may not be completely distinguishable from one another. Many times apoptosis and necrosis mechanisms can cooperate to execute cell death via the enzymatic process involved in the generation of that morphology. Moreover, there are two caspase-dependent pathways leading to activation of caspase-3 and apoptosis-the intrinsic and extrinsic pathways. Clinical Implications For the reasons outline earlier, several therapies have targeted the prevention of excessive apoptosis and cysteine protease activity. Several of these therapies have shown potential under experimental conditions (caspase inhibitors, inhibitors of apoptosis proteins, and cyclosporine). This increase in outer membrane permeability will permit the release of several proteins from the intermembrane space into the cytoplasm. Together, this complex (cytochrome c/Apaf-1) will activate caspase-9; caspase-9 then cleaves the proenzyme form of caspase3, which leads to its activation and subsequent apoptosis. Cell Membrane Poration after Traumatic Brain Injury Recent studies have shown four distinct types of reversible membrane pathology: (1) those that reseal early after early perturbation, (2) those that exhibit delayed resealing after early perturbation, (3) those that have enduring permeability after early perturbation, and (4) those with delayed permeability. The magnitude or duration of the forces may determine the fate of the damaged soma or axon (or both). A temporal progression of membrane poration also appears to occur, with a redistribution of poration subtypes taking place between 4 and 8 hours. As time evolved, more neurons revealed delayed poration as opposed to resealed neurons, thus suggesting ongoing secondary mechanisms that continue to result in changes in permeability. The cells were observed for up to 28 days and were shown to atrophy rather than degenerate as determined by microscopic evaluation and measurements of nuclear cytoplasmic volumes. These lesions are usually located at the frontal and temporal poles and in the orbital frontal cortex. Although some of these mechanisms attenuate acute damage at the expense of future regenerative capacity, others retain the potential to participate in therapeutic interventions. Plasticity occurs when injury induces reorganization of cortical connections, but plasticity is not always synonymous with functional recovery. Therapeutic interventions, however, must account for changes in the injury microenvironment that encompass barriers to both functional reconnection and opportunities for repair (Table 328-1), as discussed in the following sections. This response is partially represented in the form of "microglial stars" and "perivascular cuffing" in human pathologic specimens. Both inflammatory mechanisms and necrotic cell death trigger reactive gliosis, the astrocytic response to injury that consists of astrocyte hypertrophy, activation of fibrillary processes, and penumbral proliferation. The findings just presented support the idea that the beneficial effects of astrocytes at the site of an injury probably occur early in the injury response whereas subacute formation of the glial scar hinders regeneration. The beneficial effects of an astrocytic response include secretion of neurotrophic factors, regulation of metabolic factors (particularly important in times of stress), and maintenance of homeostatic levels of neurotransmitters. In addition, the hippocampus ipsilateral to the cortical contusion is capable of a significant plasticity response, but synapse replacement in this area does not necessarily result in significant improvement in spatial learning. Many genes encoding molecules for cellular signaling, synaptic plasticity, metabolism, ion channels, and transporters that are initially upregulated after severe injury are downregulated after moderate injury, although moderate injury is associated with an increasing number of responsive genes as a function of time after injury as opposed to a decreasing number after severe injury. A,Coronal section of the adult human brain; ventricles are light blue, and the corpuscallosumissolid black. Similarly, BrdU labeling in the ipsilateral subventricular zone of sham animals (C) significantly increases after injury (D, arrows). Cell proliferation and neuronal differentiation in the dentate gyrus in juvenile and adult rats following traumatic brain injury. Patch clamp studies have demonstrated that such BrdU cells exhibit neuronal electrophysiologic properties,73 and anatomic integration of these new neurons into host tissue has been shown by retrograde tracer labeling and synaptophysin triple-label immunohistochemical techniques. In terms of measuring whether posttraumatic neurogenesis is functional on a broader scale that affects behavior, memory function, as assessed by Morris water maze tasks, is decreased in association with procedures that abolish the proliferation of new cells, such as the administration of antimitotic drugs. In humans, in vivo dentate gyrus neurogenesis was demonstrated on histologic sections obtained from patients who had been administered BrdU for diagnostic purposes. Labeled cell bodies were also frequently enveloped by a synaptophysin "lattice," as described previously,78 thus suggesting the formation of synapses onto the somata of newborn neurons. Additionally, more newly generated cells appear to differentiate into mature neurons over time in juveniles. Typical granule cell neurons have been shown to functionally integrate by 14 days after generation in the normal adult rodent brain77 and become critically involved in the learning response within this same period. One possible mechanism, similar to that hypothesized for the effects of an enriched environment on hippocampal neurogenesis (a survivalpromoting effect of newborn cells that is selective for neurons),96 is a greater level of specific neurotrophin support97 that is either not present or not induced in adults. Magnetoencephalography is an additional imaging technique that spatially identifies the synchronous firing of neurons from restricted cortical areas in relation to either spontaneous cerebral activity or external stimuli, thereby allowing precise three-dimensional localization of the firing neuronal pool. By using these methods, it is possible to demonstrate lesionor use-dependent changes in cortical maps. Combined-modality functional imaging studies suggest that reorganization of motor output is ongoing for several months after brain injury, and the mode and degree of motor recovery may largely depend on functional compensation by spared parallel descending pathways, activation of the contralateral premotor cortex, and cerebellar activation. These studies suggest that the behavioral improvements seen in the weeks after injury are supported by compensatory reorganization of surviving neurostructural elements as follows: increased activity in brain regions distant from but connected to the injured zone, increased activity in the contralesional hemisphere (reduced laterality), and shifts in representational maps within intact cortical regions surrounding the injury zone. The former leads to behavioral improvement, such as changes in cortical representation and functional gain with the use of an affected extremity, whereas the latter results in deterioration of function, such as the appearance of seizures after brain injury. The clinical effects of stimulation-triggered neuroplasticity have been examined mainly at the behavioral level. Neurorehabilitation interventions based on this concept have shown some success, although more work is needed to elucidate the mechanisms underlying functional recovery. The positive effect of motor practice and intensive training on system reorganization in the injured brain has been demonstrated after constraint-induced movement therapy103 and intensive language training,104 whereas noninvasive cortical stimulation and modulation of somatosensory input have shown that motor and the somatosensory cortices display an interconnected capacity for plasticity. Based on preclinical gene and cell therapy experiments in primates, significant progress has been achieved in developing restorative neurosurgical strategies for movement disorders. Opportunities for initiating potential restorative therapies are therefore present at multiple neuroanatomic sites. Enhancing Neoneurogenesis after Brain Trauma Assuming that the adult human brain is capable of generating new neurons in response to injury, as is clearly the case in rodents, what steps could be taken to clinically enhance the production and functional integration of these cells First, the functional magnitude of the neurogenic response to injury is relatively small; whether this is due to failure of new neurons to develop at a sufficiently rapid rate or failure to survive to time points that allow sufficient integration into the host environment is not clear. Understanding the effects of the disease process on these factors is necessary for developing strategies to influence adult neurogenesis for therapeutic purposes. Similarly, intraventricular administration of S100B resulted in a twofold increase in the percentage of newly generated cells coexpressing NeuN in the dentate gyrus at 35 days after injury. Although the optimal combinations of neurotrophins remain unknown in rodents, studies with single mitogens support this strategy. For example, experimental neuroinflammation has been shown to inhibit hippocampal neurogenesis, an effect that can be reversed with the administration of minocycline,119 which inhibits microglial activation and reduces apoptotic cell loss. Additionally, indomethacin, a common nonsteroidal anti-inflammatory drug, blocks the effects of endotoxin- and irradiation-induced inflammation on hippocampal neurogenesis120 and enhances neurogenesis after experimental stroke. Transplantation of these cells has produced partial recovery of neurological function in some patients after basal ganglia stroke. Graft location will also be tied to the desired functional role of the grafted cells. Replacement neurons, remyelinating oligodendrocytes, and supporting chaperone cells are all potentially useful cell types whose relative value may change depending on the clinical situation. Transplanted animals did show significant improvements in spatial learning, which suggested release of neurotrophic factors by the transplanted cells.