Purchase kamagra effervescent online pills
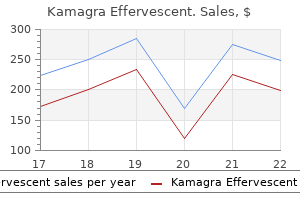
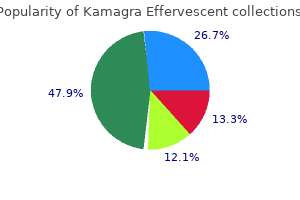
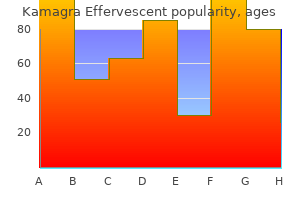
Diseases of the heart erectile dysfunction caused by anabolic steroids buy kamagra effervescent from india, PericarDium, anD Pulmonary Vasculature BeD Groups 2 to 5 Pulmonary Hypertension 65. It is a tonic state punctuated by periods of phasic activity during which autonomic and cardiac functions are erratic. Sympathetic neural activity decreases and parasympathetic tone predominates, which decreases the arterial baroreceptor set point, heart rate, blood pressure, cardiac output, and systemic vascular resistance. Because of the predominance of parasympathetic neural tone, it is not unusual for healthy individuals to have sinus bradycardia, marked sinus arrhythmia, sinus pauses, or first-degree and type I second-degree atrioventricular block during sleep. The supine position makes airway collapse more likely because of posterior displacement of the tongue, soft palate, and mandible. Sedative-hypnotic medications or alcohol may compound these effects and increase the risk for obstructive apnea. Apneas terminate because of transient arousal to a lighter sleep stage, as can be demonstrated with electroencephalographic recordings, but may not result in subjective awakening or awareness. Chemoreceptors are activated by the hypoxemia and hypercapnia of apnea and elicit postapneic hyperventilation, which also contributes to arousal. During apnea, as hypoxemia worsens, peripheral sympathetic activity increases markedly and blood pressure rises acutely. In some individuals, peripheral sympathetic overactivity may be accompanied by cardiac parasympathetic activation, which results in peripheral vasoconstriction and bradycardia. These mechanisms may be manifested clinically by lack of the usual dip in nocturnal blood pressure, drug-resistant hypertension (see Chapters 43 and 44), automatic tachycardias driven by sympathetic activity, and profound nocturnal bradycardias caused by cardiac vagal activity. Common nocturnal arrhythmias, such as marked sinus arrhythmia and second-degree atrioventricular block (Mobitz type I), are exacerbated, and higher-degree conduction abnormalities, such as long sinus pauses and advanced atrioventricular block, may occur transiently (see Chapters 34 and 37). In conjunction with structural heart disease or heart failure, this may have prognostic implications. Inspiratory effort against a collapsed airway during obstructive apnea generates marked negative intrathoracic pressure, which itself causes acute cardiac structural and hemodynamic effects. Its principal feature is upper airway occlusion, which causes partial or complete cessation of air flow. This causes hypoxia and strenuous ventilatory efforts, followed by transient arousal and restoration of airway patency and air flow. In symptomatic individuals, the condition is called obstructive sleep apnea syndrome. Obstructive apnea is defined as the absence of air flow for at least 10 seconds in the presence of active ventilatory efforts, as reflected by thoracoabdominal movements. Obstructive hypopnea is defined as a decrease of more than 50% in thoracoabdominal movements for at least 10 seconds associated with a decrease of greater than 4% in oxygen saturation. This increases venous return to the right side of the heart, produces ventricular interdependence, decreases left ventricular compliance and filling, and results in decreased cardiac output. When coupled with heightened peripheral sympathetic activity, these changes can directly increase cardiac afterload and detrimentally affect left ventricular systolic function. These changes, together with oscillations in sympathetic and parasympathetic tone, may promote the initiation of atrial fibrillation during sleep. The severity of the nocturnal oxygen desaturation was associated with the magnitude of this risk independently of other risk factors for atrial fibrillation, including obesity, hypertension, and heart failure. Data from the Sleep Heart Health Study of more than 6000 subjects suggest that nocturnal desaturation of 4% or greater is independently 1. Its principal defect is an instability in ventilatory control, which results in oscillations in the arterial partial pressure of carbon dioxide (Paco2) above and below the apneic threshold and consequent periodic hyperpnea and apnea. Ventilation is controlled by feedback loops that integrate information from multiple sources. Control of ventilation becomes unstable when a phase delay exists between the input (chemosensors) and responses (ventilatory muscles) in these feedback loops and also when the gain of these feedback loops is increased so that a small input produces an exaggerated response. Increased chemosensitivity chronically decreases Paco2 closer to the apneic threshold. In addition, stimulation of pulmonary irritant mechanoreceptors by increased left ventricular filling pressure and pulmonary edema causes hyperventilation beyond what is necessary to normalize Paco2. This hyperpnea leads to hypocapnia beyond the apneic threshold, and the central efferents to the ventilatory muscles become suppressed, thus resulting in apnea. In heart failure, this may be exacerbated by the prolonged lung-to-periphery circulation time, which is inversely proportional to cardiac output. During apnea, the declining Pao2 and rising Paco2 ultimately initiate breathing, which may or may not be followed by an arousal. The repetitive episodes of hypoxemia can have detrimental effects on myocardial oxygen supply, ventricular performance, and electrical stability. Heart rate and blood pressure increase gradually with the rate of ventilation and peak with hyperpnea. The mechanisms of the elevated heart rate and blood pressure are not directly related to hypoxemia or sympathetic activity but instead are directly related to the periodic breathing itself and are even manifested during periodic breathing in the awake state. Indeed, increasing evidence suggests that daytime periodic breathing is itself associated with poor outcomes in heart failure patients. It is possible that this is partly due to the associated increase in sympathetic activity, which is a known prognostic factor in heart failure. Other symptoms may include nightly gasping or choking episodes, nighttime or morning headaches, morning dry mouth or sore throat, gastroesophageal acid reflux, and nocturia. Certain cranial features, such to its widespread acceptance by individual patients. Treatment of obesity by lifestyle modification is to identify its appropriate role. In the interim, optimization of heart failure management should remain the principal goal. These are options for patients with specific craniofacial characteristics amenable to each specific approach. Provocative pilot studies have suggested that renal sympathetic denervation may potentially attenuate the severity of sleep apnea, but further studies are needed. This resets the resting hypocapnic state of heart failure further from the apneic threshold. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). McArdle N, Hillman D, Beilin L, Watts G: Metabolic risk factors for vascular disease in obstructive sleep apnea: A matched controlled study. Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, et al: Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea, a randomized trial. Zeidan-Shwiri T, Aronson D, Atalla K, et al: Circadian pattern life-threatening ventricular arrhythmia in patients with sleep-disordered breathing and implantable cardioverterdefibrillators. Bitter T, Westerheide N, Prinz C: Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Oldenburg O, Lamp B, Faber L, et al: Sleep-disordered breathing in patients with symptomatic heart failure. Sahlin C, Sandberg O, Gustafson Y, et al: Obstructive sleep apnea is a risk factor for death in patients with stroke: A 10-year follow-up. Witkowski A, Prejbisz A, Florczak E, et al: Effects of renal sympathetic denervation on blood pressure, sleep apnea course, and glycemic control in patients with resistant hypertension and sleep apnea. Global trends are similar, with the worldwide population older than 65 years projected to increase to 973 million, or 12%, in 2030 and to constitute approximately 20% of the population in 2050. More than 80% of all deaths attributable to cardiovascular disease occur in people older than 65 years, with approximately 60% of deaths in those older than 75 years. An important point is that cardiovascular disease in older people is not seen in isolation. Eighty percent of older Americans have at least one chronic medical condition, and half have at least two. It is not as well recognized that changes in the prevalence of these diseases occur with aging from 65 to 100 years. In particular, diabetes prevalence decreases, whereas anemia, arthritis, cancer, and dementia increase in prevalence. Dementia that impairs memory, decisionmaking ability, orientation to physical surroundings, and language is estimated to be present in 13% of community-dwelling white persons older than 65 years and is more prevalent in women than in men and African-American and Hispanic populations. Cardiovascular disease is both the most frequent diagnosis and the leading cause of death among both men and women older than 65 years. The profile of these common cardiovascular diseases differs in older patients from that in younger patients.
Syndromes
- Serum phosphorus
- Chronic inflammatory disease (e.g., rheumatoid arthritis, SLE)
- Bleeding, infection, and pain at the injection site
- Maternal (mitochondrial) inheritance
- Medicines, including blood pressure medications (especially beta-blockers), heart medications (such as digoxin), some peptic ulcer medications, sleeping pills, and antidepressants
- Camphorated oil
- Procedures to reduce feeling in the nerve (such as nerve ablation using radiofrequency, heat, balloon compression, or injection of chemicals)
- Inability to urinate
- Use heat or ice on the breast
- Injury to the head and face (swelling, blood, or a deformity can cause choking)
Safe kamagra effervescent 100 mg
Balance training such as Tai Chi and exercises aimed at improving strength and endurance diminish fall rates erectile dysfunction and high blood pressure generic kamagra effervescent 100mg on line. Behavioral intervention for the development of fear of falling after such events can be effective and is strongly encouraged (Dukyoo et al. Further useful interventions in the long term include vitamin D substitution (>800 international units/day), improvement of vision with cataract surgery (Foss et al. However, none of these measures abolish the risk of falling, and even well-intended interventions may be associated with an increased fall risk. Unexpectedly, this was shown in some patients who received new prescription eyeglass lenses (Campbell et al. Use of walkers is associated with the highest fall risk, raising the question whether these ubiquitous devices have inherent design flaws that are contributory (Stevens et al. Moderate benefit on fall rates and cost-effectiveness of interventional programs has been demonstrated (Hektoen et al. The efficacy of interventional programs could potentially be improved by increased involvement of falling elderly, ongoing program participation, and regular home visits. Advances like these, along with screening of elderly persons for fall risk and preventive program enrollment, may eventually diminish the burden of this epidemic. Unfortunately, with middle-aged women and the elderly, the cause may be merely a function of gender or age. Patients with fixed motor or sensory impairments must be advised honestly about their almost unavoidable tendency to fall. Environmental adjustments, participation in fall prevention programs, and use of protective devices can reduce the frequency of falls and related injuries. Endovascular management of symptomatic cerebral malperfusion due to carotid dissection after type A aortic dissection repair. Selfreported falls and fall related injuries among persons aged > 65 years-United States, 2006. Transcallosal diffusion tensor abnormalities in predominant gait disorder parkinsonism. Infarct hemisphere and noninfarcted brain volumes affect locomotor performance following stroke. Descriptive analysis of fatal falls of older adults in a Midwestern county in the year 2005. Multifactorial intervention to reduce falls in older people at high risk of recurrent falls. Falls and health status in elderly women following second eye cataract surgery: a randomized controlled trial. Prevalence and characteristics of traumatic intracranial hemorrhage in elderly fallers presenting to the emergency department without focal findings. The relationship between fear of falling to spatiotemporal gait parameters measured by an instrumented treadmill in people with multiple sclerosis. Anterior cerebral artery infarction: stroke mechanism and clinical imaging study in 100 patients. Modifiable cardiovascular risk factors and axial motor impairments in Parkinson Disease. Forward-backward postural protective stepping responses in young and elderly adults. Peripheral vestibular dysfunction is prevalent in older adults experiencing multiple non-syncopal falls versus age-matched non-fallers: a pilot study. Falling is not just for older women: support for pre-emptive prevention intervention before 60. A case of pial arteriovenous fistula with giant venous aneurysm and multiple varices treated with coil embolization. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta analysis. Secondary intracranial hemorrhage after mild head injury in patients with low-dose acetylsalicylate acid prophylaxis. A spatiotemporal analysis of gait freezing and the impact of pedunculopontine nucleus stimulation. Practice parameter: Assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Predictors of falls and fractures in bradykinetic rigid syndromes: a retrospective study. Sensory loss and walking speed related factors for gait alterations in patients with peripheral neuropathy. Increased gait variability is associated with the history of falls in patients with cerebellar ataxia. The epidemiology of trauma-related mortality in the United States from 2002 to 2010. Home-based exercise program and fall-risk reduction in older adults with multiple sclerosis: phase 1 randomized controlled trial. Age differences in energy absorption in the upper extremity during a descent movement: implications for arresting a fall. Unintentional fall injuries associated with walkers and canes in older adults treated in U. A commentary on clinical assessment, changes across the life course, functional implications and future interventions. Manual therapy for the cervical spine and reported adverse effects: a survey of Irish manipulative physiotherapists. The syndrome of delirium can be a physiological consequence of a medical condition or stem from a primary neurological cause. Delirium is by far the most common behavioral disorder in a medical-surgical setting. The consequences of delirium are serious: they include prolonged hospitalizations, increased mortality, high rates of discharges to other institutions, severe impact on caregivers and spouses, and between $143 billion and $152 billion annually in direct healthcare costs in the United States (Kerr et al, 2013; Leslie and Inouye, 2011). Bonhoeffer, in his classification of organic behavioral disorders, established that delirium is associated with clouding of consciousness. Despite this long history, physicians, nurses, and other clinicians often fail to diagnose delirium (Wong et al. Healthcare providers often miss this syndrome more from lack of recognition than misdiagnosis. The elderly in particular may have a "quieter," more subtle presentation of delirium that may evade detection. Clinicians must take care to distinguish delirium from dementia, the other common disorder of cognitive functioning. Delirium is acute in onset (usually hours to a few days) whereas dementia is chronic (usually insidious in onset and progressive). The definition of delirium must emphasize an acute behavioral decompensation with fluctuating attention, regardless of etiology or the presence of baseline cognitive deficits or dementia. Complicating this distinction is the fact that underlying dementia is a major risk factor for delirium. Arousal, a basic prerequisite for attention, indicates responsiveness or excitability into action. Consciousness, a product of arousal, means clarity of awareness of the environment. In general, awareness, attention, and cognition fluctuate over the course of a day. Furthermore, delirious patients have disorganized thinking and an altered level of consciousness, perceptual disturbances, disturbance of the sleep/wake cycle, increased or decreased psychomotor activity, disorientation, and memory impairment. Other cognitive, behavioral, and emotional disturbances may also occur as part of the spectrum of delirium. Gross swings in attention and awareness, arousal, or both occur unpredictably and irregularly and become worse at night. Because of potential lucid intervals, medical personnel may be misled by patients who exhibit improved attention and awareness unless these patients are evaluated over time.
Discount kamagra effervescent 100 mg fast delivery
In one study of nasopharyngeal cancer patients receiving radiotherapy who developed impairment in olfactory function new erectile dysfunction drugs 2014 order kamagra effervescent with paypal, decreased olfactory bulb volume was noted (Veyseller et al. Sudden smell loss alerts the practitioner to head trauma, ischemia, infection, or a psychiatric condition. Gradual smell loss can be a marker for the development of a progressive obstructive lesion, cumulative drug effects, or simply presbyosmia or presbygeusia. While losses secondary to head trauma are most commonly abrupt, in some cases the loss appears over time or only becomes apparent to the patient after a long interval. Blood serum tests may be helpful in identifying conditions such as diabetes, infection, heavy metal exposure, nutritional deficiency. Medical or surgical interventions are available for most patients with obstructive or inflammatory disorders. For example, in cases of rhinosinusitis, an oral taper of prednisone can initially be used to quell general inflammation followed by topical administration of the nasal spray or drops in the inverted head position, such as the Moffett position (Canciani and Mastella, 1988). Candidiasis or other oral infections can be quelled with topical antifungal and antibiotic treatments. Some salty or bitter dysgeusias respond to chlorohexidine mouth wash, possibly as a result of its strong positive charge (Wang et al. Patients with excessive oral dryness, including dryness due to medications, often benefit from the use of mints, lozenges, or sugarless gum, as well as oral pilocarpine or artificial saliva. Medications that induce distortions of smell or taste can often be discontinued and other types of medications or modes of therapy substituted, although reversal of the dysfunction may take months (Doty et al. Antioxidants, such as alpha-lipoic acid, may be effectual in some cases of hyposmia, hypogeusia, dysosmia, dysgeusia, and burning mouth syndrome (Hummel et al. Despite being widely mentioned in the medical literature, zinc and vitamin A therapies unlikely benefit olfactory disturbances except when frank deficiencies are present, although both of these agents may improve taste dysfunction secondary to hepatic deficiencies (Deems et al. Studies reporting positive effects of theophylline, acupuncture, and transcranial magnetic stimulation are not convincing and generally lack appropriate control groups. Donepezil (an acetylcholinesterase inhibitor) has been reported to improve both cognitive and odor identification scores in patients with Alzheimer disease (Velayudhan and Lovestone, 2009). It is of interest that repeated exposure to odorants may, in fact, increase sensitivity to them in both animals and humans, providing a rationale for therapies in which multiple odors are smelled before and after going to bed (Hummel et al. In one study, patients with post-infectious and posttraumatic olfactory impairment were put through 16 weeks of "training" of smelling four separate odorants, which resulted in an increase in function for both groups (Konstantinidis et al. Importantly, spontaneous recovery over time occurs in some instances, providing hope to at least some patients. A determination of all the medications that the patient was taking before and at the time of symptom onset is important, as are comorbid medical conditions potentially associated with taste and smell impairment, such as renal failure, liver disease, hypothyroidism, diabetes, and dementia. Delayed puberty in association with anosmia (with or without midline craniofacial abnormalities, deafness, and renal anomalies) suggests the possibility of Kallmann syndrome. Recollection of epistaxis, discharge (clear, purulent or bloody), nasal obstruction, allergies, and somatic symptoms, including headache or irritation, have potential localizing value. The possibility of malingering should be considered, particularly if litigation is involved. However, normal agerelated function returned in only 11% of the anosmic and 23% of the hyposmic patients. The amount of dysfunction present at the time of presentation, not etiology, was the best predictor of prognosis. An important but overlooked element of therapy comes from chemosensory testing itself. Confirmation or lack of conformation of loss is beneficial to patients, particularly ones who come to believe they may be "crazy" as a result of unsupportive medical providers or family members. It is extremely therapeutic for an older person to become aware that, while his or her smell function is not what it used to be, it still falls above the average of his or her peer group. It is unfortunate that many such patients are simply told by their physician they are getting old and nothing can be done for them, often exacerbating or leading to depression and decreased self-esteem. Cell proliferation and migration in the anterior forebrain, with special reference to persisting neurogenesis in the olfactory bulb. Olfactory dysfunction in patients with narcolepsy with cataplexy is restored by intranasal Orexin A (Hypocretin-1). Localization of orexins and their receptors in the rat olfactory system: possible modulation of olfactory perception by a neuropeptide synthetized centrally or locally. Clinical manifestations of olfactory and gustatory disorders associated with hepatic and renal disease. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Coming to your senses: detecting taste and smell alterations in chemotherapy patients. Functional heterogeneity in human olfactory cortex: an event-related functional magnetic resonance imaging study. Use of olfactory training in post-traumatic and postinfectious olfactory dysfunction. Morphology of the mammalian olfactory epithelium: form, fine structure, function, and pathology. Smell identification test as a treatment response marker in patients with Alzheimer disease receiving donepezil. Impact of recurrent head trauma on olfactory function in boxers: a matched pairs analysis. Olfactory bulb volume and olfactory function after radiotherapy in patients with nasopharyngeal cancer. Therefore, clinicians are well advised to spend most of their time interviewing the patient. History-taking for head and face pain is similar to that for other presenting complaints, but several specific aspects should be addressed. Usually one begins by asking the patient to describe their symptoms or, alternatively, simply by asking how they can be helped. Once the patient has had an opportunity to speak, directed but open-ended questions (see Box 20. It is valuable to establish this information at the beginning of the interview so each type of pain can be carefully delineated. A headache of recent onset obviously has many possible causes, including the new onset of either a benign or serious condition. In general, the more recent the onset of headache, the more worrisome the possible cause. The "worst ever" headache, an increasingly severe headache, or change for the worse in an existing headache pattern all raise the possibility of an intracranial lesion. If no underlying cause is discovered despite expedited, thorough investigation, a diagnosis of primary thunderclap headache can be considered. Onset of a new headache in patients older than 50 years raises suspicion of an intracranial lesion. A history of antecedent head or neck injury should be sought; even a relatively minor injury can be associated with subsequent development of epidural, subdural, subarachnoid, or intraparenchymal hemorrhage and post-traumatic dissection of the carotid or vertebral arteries (Debette and Leys, 2009). However, post-traumatic headaches can occur following head injury in the absence of any demonstrable pathology. Headache is an exceedingly common symptom that affects virtually everyone at some time in their life. Headache is one of the most common reasons for outpatient healthcare visits in the United States. The primary headache disorders do not have an underlying structural cause, but all the primary headache disorders can be stimulated by secondary conditions. The diagnosis of head and face pain depends on three elements: the history, neurological and general examinations, and appropriate investigations, if needed. Chronic migraine is defined as headache occurring on 15 days per month for 3 months which has the features of migraine headache on 8 days per month. Chronic migraine usually develops in individuals with a history of episodic migraine headaches. Some patients with apparent medication overuse do not improve after drug withdrawal. Episodic cluster headaches typically occur daily for several weeks or months and are followed by a lengthy headache-free interval. Chronic cluster headaches occur at least every other day for more than 1 year or with remissions lasting < 1 month. If there is no regular periodicity, it is useful to inquire about the longest and shortest periods of freedom between headaches.
Kamagra effervescent 100mg mastercard
All unnecessary medications that increase the risk of falls erectile dysfunction vacuum pump medicare purchase kamagra effervescent 100mg, especially sedatives, antihypertensives, and hypnotics, should be discontinued. High-risk behavior such as the use of ladders and moving about at low levels of illumination is discouraged, and women are advised to wear sturdy lowheeled shoes. Patients are distractible, and stimuli may gain attention indiscriminately, trivial ones often getting more attention than important ones. All components of attention are disturbed, including selectivity, sustainability, processing capacity, ease of mobilization, monitoring of the environment, and the ability to shift attention when necessary. Although many of the same illnesses result in a spectrum of disturbances from mild inattention to coma, delirium is not the same as disturbance of arousal. The disturbance develops over a short period of time (usually hours to a few days), represents a change from baseline attention and awareness, and tends to fluctuate in severity during the course of a day. The disturbances in Citeria A and C are not better explained by another pre-existing, established, or evolving neurocognitive disorder and do not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal. Specify whether: Substanceintoxicationdelirium: this diagnosis should be made isntaed of substance intoxication when the symptoms in Criteria A and C predominate in the clinical picture and when they are sufficiently severe to warrant clinical attention. If a mild substance use disorder is comorbid with the substance intoxication delirium, the 4th position character is "1," and the clinician should record "mild [substance] use disorder," before the substance intoxication delirium. If a moderate or severe substance use disorder is comorbid with the substance intoxication delirium, the 4th position character is "2,"and the clinician should record "moderate [substance] use disorder" or "severe [substance] use disorder," depending on the severity of the comorbid substance use disorder. Medication-induceddelirium: this diagnosis applies when the sympotoms in Criteria A and C arise as a side effect of a medication taken as prescribed. If the medication is a sedative, hypnotic, or anxiolytic taken as prescribed, the code is F13. If the medication is an amphetamine-type or other stimulant taken as prescribed, the code is F15. The other medical condition should also be coded and listed separately immediately before the delirium due to another medical condition. Note that the etiological medical condition both appears as a separate code that precedes the delirium code and is substituted into the delirium due to another medical condition rubric. Specify if: Hyperactive: the individual has a hyperactive level of psychomotor activity that may be accompanied by mood lability, agitation, and/or refusal to cooperate with medical care. Hypoactive: the individual has a hypoactive level of psychomotor activity that may be accompanied by sluggishness and lethargy that approaches stupor. Mixedlevelofactivity: the individual has a normal level of psychomotor activity even though attention and awareness are disturbed. There are multiple intrusions of competing thoughts and sensations, and patients are unable to order symbols, carry out sequenced activity, and organize goal-directed behavior. Speech shifts from subject to subject and is rambling, tangential, and circumlocutory, with hesitations, repetitions, and perseverations. Decreased relevance of the speech content and decreased reading comprehension are characteristic of delirium. Confused speech is further characterized by an abnormal rate, frequent dysarthria, and nonaphasic misnaming, particularly of words related to stress or illness, such as those referable to hospitalization. They are most common in the visual sphere and are often vivid, three-dimensional, and in full color. Hallucinations are generally unpleasant, and some patients attempt to fight them or run away with fear. Some hallucinatory experiences may be release phenomena, with intrusions of dreams or visual imagery into wakefulness. DisturbedSleep/WakeCycle Disruption of the day/night cycle causes excessive daytime drowsiness and reversal of the normal diurnal rhythm. Nocturnal peregrinations can result in a serious problem when the delirious patient, partially clothed in a hospital gown, has to be retrieved from the hospital lobby or from the street in the middle of the night. This is one of the least specific symptoms and also occurs in dementia, depression, and other behavioral conditions. In delirium, however, disruption of circadian sleep cycles may result in rapid eye movement or dream-state overflow into waking. AlteredLevelofConsciousness Consciousness, or clarity of awareness, may be disturbed. In hyperalert patients, the extreme arousal does not preclude attentional deficits because patients are indiscriminate in their alertness, are easily distracted by irrelevant stimuli, and cannot sustain attention. The two extremes of consciousness may overlap or alternate in the same patient or may occur from the same causative factor. AlteredPsychomotorActivity There are three subtypes of delirium, based on changes in psychomotor activity. The hyperactive subtype is usually hyperalert and agitated, and has prominent overactivity of the autonomic nervous system. Moreover, the hyperactive type is more likely to have delusions and perceptual disorders such as hallucinations. About half of patients with delirium manifest elements of both subtypes, called mixed subtype, alternating between hyperactive and hypoactive. Only about 15% are PerceptualDisturbances the most common perceptual disturbance is decreased perceptions per unit of time; patients miss things that are going on around them. In addition to the patients being younger, the hyperactive subtype has more drug-related causes, a shorter hospital stay, and a better prognosis. Patients are disoriented first to time of day, followed by other aspects of time, and then to place. Disorientation is one of the most common findings in delirium but is not specific for delirium; it occurs in dementia and amnesia as well. Among patients with delirium, recent memory is disrupted in large part by the decreased registration caused by attentional problems. In delirium, reduplicative paramnesia, a specific memoryrelated disorder, results from decreased integration of recent observations with past memories. In a form of reduplicative paramnesia known as Capgras syndrome, however, a familiar person is mistakenly thought to be an unfamiliar impostor. Higher visual-processing deficits include difficulties in visual object recognition, environmental orientation, and organization of drawings and other constructions. Spelling and syntax are also disturbed, with spelling errors particularly involving consonants, small grammatical words (prepositions and conjunctions), and the last letters of words. Writing is easily disrupted in these disorders, possibly because it depends on multiple components and is the least used language function. Delirium is the final common pathway of many pathophysiological disturbances that reduce or alter cerebral oxidative metabolism. These metabolic changes result in diffuse impairment in multiple neuronal pathways and systems. Dysfunction of the anterior cingulate cortex is involved in disturbances of the management of attention (Reischies et al. Other areas include the bilateral or right prefrontal cortex in attentional maintenance and executive control, the temporoparietal junction region in disengaging and shifting attention, the thalamus in engaging attention, and the upper brainstem structures in moving the focus of attention. The thalamic nuclei are uniquely positioned to screen incoming sensory information, and small lesions in the thalamus may cause delirium. In addition, there is evidence that the right hemisphere is dominant for attention. Cortical blood flow studies suggest that right hemisphere cortical areas and their limbic connections are the "attentional gate" for sensory input through feedback to the reticular nucleus of the thalamus. Another explanation for delirium is alterations in neurotransmitters, particularly a cholinergic-dopaminergic imbalance. Delusions, like hallucinations, are probably release phenomena and are generally fleeting, changing, and readily affected by sensory input. Some patients exhibit facetious humor and playful behavior, lack of concern about their illness, poor insight, impaired judgment, and confabulation. Dysphoric (unpleasant) emotional states are the more common, and emotions are not sustained. Up to half of elderly delirious patients display symptoms of depression with low mood, loss of interests, fatigue, decreased appetite and sleep, and other feelings related to depression.
Purchase 100mg kamagra effervescent
Significant or progressive electrocardiographic abnormalities despite a lack of symptoms is an indication for consideration for prophylactic pacing impotence forums effective 100mg kamagra effervescent. Anesthesia in patients with myotonic dystrophy increases both the risk of respiratory failure and arrhythmias. In patients presenting with wide complex tachycardia, cardiac electrophysiologic study with particular evaluation for bundle branch reentry tachycardia should be done. Implantable cardioverterdefibrillators are being increasingly used in patients with myotonic dystrophies. The course of neuromuscular abnormalities in the myotonic dystrophies is variable. Respiratory failure from progressive muscle dysfunction is the most common cause of death. Some patients, however, are only minimally limited by weakness up to the age of 60 to 70 years. Sudden death can reduce survival in patients with the myotonic dystrophies including those minimally symptomatic from a neuromuscular status. Decisions regarding prophylactic cardiac devices need to be made with full consideration of all aspects for the care of the myotonic patient. Arrows demarcate expected size and shape of the branching atrioventricular bundle. At cardiac electrophysiologic study, the most common abnormality found is a prolonged His-ventricular (H-V) interval. Conduction system disease can progress to symptomatic atrioventricular block and necessitate pacemaker implantation. The prevalence of permanent cardiac pacing in patients with myotonic dystrophy type 1 varies widely between studies based on referral patterns and the indications used for implant. Updated practice guidelines have recognized that asymptomatic conduction abnormalities in neuromuscular diseases such as myotonic dystrophy may warrant special consideration for pacing. Therapy with right bundle branch or fascicular radiofrequency ablation can be curative. Up to one third of deaths in myotonic dystrophy type 1 are sudden; presumably, most are due to arrhythmias. Distal conduction disease producing atrioventricular block can result in the lack of an appropriate escape rhythm and asystole or bradycardia-mediated ventricular fibrillation. Sudden death can occur in myotonic dystrophy type 1 despite pacing, implicating ventricular arrhythmias. Nonarrhythmia causes of sudden death, probably acute respiratory issues, play some role. Emery-Dreifuss muscular dystrophy is a rare inherited disorder in which skeletal muscle symptoms are often mild but with cardiac involvement that is both common and serious. The disease is classically inherited in an X-linked recessive fashion but there is heterogeneity with families that fit an X-linked dominant, autosomal dominant and autosomal recessive inheritance pattern. Mutations in genes found on chromosome 1 encoding two other nuclear membrane proteins, lamins A and C, have been identified as being responsible for a variety of other disorders with a phenotypic expression similar to X-linked Emery-Dreifuss muscular dystrophy. Mutations in the tail regions of lamins A and C are responsible for the majority of cases of autosomal dominant Emery-Dreifuss muscular dystrophy with a phenotype of both cardiac and skeletal muscle involvement. Mutations in the rod domain of the lamin A/C gene primarily cause isolated cardiac disease including dilated cardiomyopathy, conduction system degeneration, and atrial and ventricular arrhythmias. The disorder has been labeled "benign X-linked muscular dystrophy" to differentiate the slowly progressive muscular weakness from that of Duchenne muscular dystrophy. In the autosomal dominant and recessive inheritance of Emery-Dreifuss muscular dystrophy, a more variable phenotypic expression and penetrance typically are observed. A mutation in the lamin A/C gene also is responsible for an autosomal dominantly-inherited familial partial lipodystrophy characterized by marked loss of subcutaneous fat, diabetes, hypertriglyceridemia, and cardiac abnormalities. Cardiovascular Manifestations Arrhythmias and dilated cardiomyopathy are the major manifestation of cardiac disease in Emery-Dreifuss muscular dystrophy and its associated disorders. In X-linked recessive Emery-Dreifuss muscular dystrophy abnormalities in impulse generation and conduction are common. The atria appear to be involved earlier than the ventricles, with atrial fibrillation and atrial flutter, or more classically, permanent atrial standstill and junctional bradycardia. Abnormalities in impulse generation or conduction are present in virtually all patients by age 35 to 40 years, and requirement for pacing is typical. Ventricular arrhythmias including sustained ventricular tachycardia and ventricular fibrillation occur. Although arrhythmias are the most common presentation of cardiac involvement in X-linked recessive Emery-Dreifuss muscular dystrophy, a dilated cardiomyopathy can rarely develop. The dilated cardiomyopathy is more common in patients in whom survival has been improved with cardiac device implantation. Patients with disorders caused by lamin A and C mutations typically present at 20 to 40 years of age with cardiac conduction disease, atrial fibrillation, and dilated cardiomyopathy. Progression of a cardiomyopathy to the extent that heart transplantation is required has been described. Implantable cardioverter-defibrillators are the appropriate cardiac device for a majority of patients. A monomorphic ventricular tachycardia is induced with atrial-ventricular (A-V) dissociation and His association, consistent with bundle branch reentry tachycardia. Prophylactic placement of an implantable cardioverter-defibrillator is advocated in patients with Emery-Dreifuss muscular dystrophy and its associated disorders if significant electrocardiographic conduction disease is present and pacing is being considered. In a large observational European series, risk factors for sudden death and appropriate implantable cardioverter-defibrillator therapy included nonsustained ventricular tachycardia, left ventricular ejection fraction less than 45% at presentation, male sex, and lamin A or C nonmissense mutations. Patients with left ventricular dysfunction should benefit from pharmacologic therapy but data on this issue are limited. Female carriers of X-linked recessive Emery-Dreifuss muscular dystrophy develop conduction disease, and electrocardiographic monitoring on a routine basis is appropriate. An autosomal recessive or sporadic limb-girdle muscular dystrophy associated with a progressive dilated cardiomyopathy is caused by mutations affecting the function of the dystrophin-glycoprotein complex, including sarcoglycan and fukutin-related proteins (subtypes 2C to 2F and 2I, respectively). The sarcoglycans complex with dystrophin-associated glycoproteins to counteract mechanical stress associated with contraction. Fukutin-related proteins affect glycosylation of a dystrophin-associated glycoprotein. An autosomal recessive limb-girdle muscular dystrophy associated with a variable onset of a dilated cardiomyopathy is caused by a mutation in a sarcolemmal repair protein termed dysferlin (subtype 2B). Other subtypes of limbgirdle muscular dystrophy are not commonly associated with cardiac or arrhythmia abnormalities. Clinical Presentation the onset of muscle weakness is variable but usually occurs before age 30. The recessive disorders tend to cause earlier and more severe weakness than the dominant disorders. Patients commonly present with complaints of difficulty with walking or running secondary to pelvic girdle involvement. As the disease progresses, involvement of the shoulder muscles and then more distal muscles occurs, with sparing of facial involvement. The limb-girdle muscular dystrophies are a group of disorders with a limb-shoulder and pelvic girdle distribution of weakness, but with otherwise heterogeneous inheritance and genetic cause. Genes involved include those encoding dystrophin-associated glycoproteins, sarcomeric proteins, sarcolemma proteins, nuclear membrane proteins, and cellular enzymes. An autosomal dominant limb-girdle muscular dystrophy (subtype 1B) with a high prevalence of arrhythmias and a late dilated cardiomyopathy is caused by mutations encoding lamin A/C, as in Emery-Dreifuss muscular dystrophy. Cardiovascular Manifestations As with many of the features of the limb-girdle muscular dystrophies, heterogeneity in the presence and degree of cardiac involvement is usual. The limb-girdle muscular dystrophies types 2C to 2F, termed sarcoglyconopathies, manifest with a dilated cardiomyopathy. Cardiomyopathy is most common in the subtype 2E and least common in the subtype 2D. A severe cardiomyopathy, including presentation with heart failure in childhood, can occur. Limb-girdle muscular dystrophy type 2I, caused by mutations in fukutin-related proteins, is associated with a dilated cardiomyopathy.
Common Oleander (Oleander). Kamagra Effervescent.
- Dosing considerations for Oleander.
- What is Oleander?
- Heart problems, asthma, seizures, cancer, menstrual problems, skin problems, warts, and many other conditions. It also has been used as a poison.
- How does Oleander work?
- Are there safety concerns?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96768
Order kamagra effervescent online
A minimum 5-day course of parenteral anticoagulation is recommended to ensure that the levels of prothrombin have fallen into the therapeutic range with warfarin erectile dysfunction doctors northern virginia buy kamagra effervescent with paypal. Because warfarin has a narrow therapeutic window, frequent monitoring of coagulation is essential to ensure that the anticoagulant response is therapeutic. Although a recent study has raised the possibility that testing every 12 weeks may be sufficient in such patients, these results require confirmation in a large number of patients. Like all anticoagulants, the major side effect of warfarin is bleeding; a rare complication is skin necrosis. Warfarin crosses the placenta and can cause fetal abnormalities, so it should not be used during pregnancy. Bleeding complications may be mild, such as epistaxis or hematuria, or more severe, such as retroperitoneal or gastrointestinal bleeding. If the patient is at high risk for bleeding, sublingual vitamin K can be administered. For life-threatening bleeding or if patients cannot tolerate the volume load, prothrombin complex concentrates can be used. Those with gastrointestinal bleeding often have underlying peptic ulcer disease or a tumor. A rare complication of warfarin, skin necrosis usually occurs 2 to 5 days after initiation of therapy. Well-demarcated erythematous lesions form on the thighs, buttocks, breasts, or toes. Examination of skin biopsy specimens taken from the borders of these lesions reveals thrombi in the microvasculature. Warfarin-induced skin necrosis occurs in patients with congenital or acquired deficiencies of protein C or protein S. The resultant procoagulant state triggers thrombosis that is localized to the microvasculature of fatty tissues for unknown reasons. Treatment involves discontinuation of warfarin and reversal with vitamin K, if needed. Because of the potential for skin necrosis, patients with known protein C or protein S deficiency require overlapping treatment with a parenteral anticoagulant when initiating warfarin therapy. The fetal abnormalities include a characteristic embryopathy, which consists of nasal hypoplasia and stippled epiphyses. The risk for embryopathy is highest with warfarin administration in the first trimester of pregnancy. Central nervous system CardiovasCular disease and disorders of other organs 1829 abnormalities can also occur with exposure to warfarin at any time during pregnancy. Finally, maternal administration of warfarin produces an anticoagulant effect in the fetus that can cause bleeding. This is of particular concern at delivery, when trauma to the head during passage through the birth canal can lead to intracranial bleeding. Because of these potential problems, warfarin is contraindicated in pregnancy, particularly in the first and third trimesters. Observational studies have suggested that patients with thrombosis complicating antiphospholipid syndrome require higher-intensity warfarin regimens to prevent recurrent thromboembolic events, an approach that increases the risk for bleeding. There is no need to stop warfarin treatment before procedures associated with a low risk for bleeding, including dental cleaning, simple dental extraction, cataract surgery, or skin biopsy. Dosing For prevention of stroke in patients with nonvalvular atrial fibrillation, 82 rivaroxaban is given at a dosage of 20 mg once daily with a reduction to 15 mg once daily in patients with a creatinine clearance of 15 to 49 mL/min, dabigatran is given at a dosage of 150 mg twice daily with a reduction to 75 mg twice daily in those with a creatinine clearance of 15 to 30 mL/min, and apixaban is given at a dosage of 5 mg twice daily with a reduction to 2. For this indication, patients must first receive a minimum of a 5-day course of a parenteral anticoagulant before starting dabigatran at a dosage of 150 mg twice daily. This all-oral regimen was shown to be as effective as conventional anticoagulant therapy for the treatment of patients with deep vein thrombosis and/or pulmonary embolism but was associated with a 69% reduction in major bleeding. Hemostasis, Thrombosis, Fibrinolysis, and Cardiovascular Disease Direct Oral Anticoagulants (See also Chapters 52, 53, and 73) Newer, direct oral anticoagulants that target thrombin or factor Xa are now available as alternatives to warfarin. These drugs have a rapid onset of action and half-lives that permit once- or twice-daily administration. Designed to produce a predictable level of anticoagulation, the new oral agents are more convenient to administer than warfarin because they are given in fixed doses without routine monitoring of coagulation. Monitoring Although administered without routine monitoring, in some situations determination of the anticoagulant activity of the new oral anticoagulants can be helpful,94 including assessment of adherence, detection of accumulation or overdose, identification of bleeding mechanisms, and determination of activity before surgery or intervention. Although the new agents are associated with less intracranial bleeding than warfarin is, the risk for gastrointestinal bleeding is higher with dabigatran and rivaroxaban than with warfarin. Dyspepsia occurs in up to 10% of patients treated with dabigatran; this problem improves with time and can be minimized by taking the drug with food. Periprocedural Management Like warfarin, use of the new oral anticoagulants must be stopped before procedures associated with a moderate or high risk for bleeding. Assessment of residual anticoagulant activity before high-risk procedures is prudent. Management of Bleeding None None None the new oral anticoagulants have no specific antidotes. Coagulation testing will determine the extent of anticoagulation, and renal function should be assessed so that the half-life of the drug can be calculated. Timing of the last dose of anticoagulant is important, and oral activated charcoal may help prevent absorption of drug administered in the past 4 to 6 hours. Dialysis removes dabigatran from the circulation in patients with renal impairment; it does not remove rivaroxaban or apixaban because unlike dabigatran, they are highly protein bound. Consequently, these agents are contraindicated in pregnancy, and when used by women of childbearing potential, appropriate contraception is important. Fibrin degradation Fibrinogen degradation Ongoing Investigations Although the safety of the new oral anticoagulants has been questioned, postmarketing surveillance data are reassuring. A humanized mouse monoclonal antibody fragment against dabigatran is under development as an antidote for dabigatran,98 and a recombinant variant of factor Xa is being developed as an antidote for oral factor Xa inhibitors. The fibrin specificity of plasminogen activators reflects their capacity to distinguish between fibrin-bound and circulating plasminogen, which depends on their affinity for fibrin. Plasminogen activators with high affinity for fibrin preferentially activate fibrin-bound plasminogen. Fibrin-bound plasmin, which is protected from inactivation by alpha2-antiplasmin, degrades fibrin to yield soluble fibrin degradation products. In contrast, plasminogen activators with little or no affinity for fibrin do not distinguish between fibrin-bound and circulating plasminogen. Activation of circulating plasminogen results in systemic plasminemia and subsequent degradation of fibrinogen and other clotting factors. All these agents act by converting the proenzyme, plasminogen, to plasmin, the active enzyme. Plasminogen activators that preferentially activate fibrin-bound plasminogen are fibrin specific. In contrast, nonspecific plasminogen activators do not discriminate between fibrin-bound and circulating plasminogen. Alteplase and its derivatives are fibrin-specific plasminogen activators, whereas streptokinase, anistreplase, and urokinase are nonspecific agents. Streptokinase binds to plasminogen and induces a conformational change in plasminogen that exposes its active site. The streptokinase/plasmin(ogen) complex then serves as the activator of additional plasminogen molecules. Streptokinase Unlike other plasminogen activators, streptokinase is not an enzyme and does not directly convert plasminogen to plasmin.
Purchase kamagra effervescent 100mg mastercard
Patients in the intervention group were more than twice as likely as control patients to receive thromboprophylaxis at discharge (22 www.erectile dysfunction treatment trusted 100 mg kamagra effervescent. Betrixaban has a longer half-life (23 hours) and undergoes much less renal clearance (only 17%) compared with other novel oral anticoagulants. ExtendedOut-of-HospitalProphylaxis inMedicalPatients References Overview and Molecular Pathophysiology 1. Casazza F, Becattini C, Bongarzoni A, et al: Clinical features and short term outcomes of patients with acute pulmonary embolism. Park B, Messina L, Dargon P, et al: Recent trends in clinical outcomes and resource utilization for pulmonary embolism in the United States: Findings from the nationwide inpatient sample. Fanikos J, Piazza G, Zayaruzny M, et al: Long-term complications of medical patients with hospital-acquired venous thromboembolism. Inflammation activates platelets, which play a central role in releasing microparticles that accelerate the thrombotic process. Technological advances in imaging have progressed so far that we now face a new 20. Guanella R, Ducruet T, Johri M, et al: Economic burden and cost determinants of deep vein thrombosis during 2 years following diagnosis: A prospective evaluation. Decousus H, Quere I, Presles E, et al: Superficial venous thrombosis and venous thromboembolism: A large, prospective epidemiologic study. Decousus H, Prandoni P, Mismetti P, et al: Fondaparinux for the treatment of superficial-vein thrombosis in the legs. Blondon M, Righini M, Bounameaux H, et al: Fondaparinux for isolated superficial vein thrombosis of the legs: A cost-effectiveness analysis. Moores L, Aujesky D, Jimenez D, et al: Pulmonary embolism severity index and troponin testing for the selection of low-risk patients with acute symptomatic pulmonary embolism. Heneghan C, Ward A, Perera R, et al: Self-monitoring of oral anticoagulation: Systematic review and meta-analysis of individual patient data. Sconce E, Avery P, Wynne H, et al: Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Siegal D, Yudin J, Kaatz S, et al: Periprocedural heparin bridging in patients receiving vitamin K antagonists: Systematic review and meta-analysis of bleeding and thromboembolic rates. Miesbach W, Seifried E: New direct oral anticoagulants-current therapeutic options and treatment recommendations for bleeding complications. Diseases of the heart, PericarDium, anD Pulmonary Vasculature BeD Epidemiology 33. Ageno W, Becattini C, Brighton T, et al: Cardiovascular risk factors and venous thromboembolism: A meta-analysis. Dentali F, Ageno W, Rancan E, et al: Seasonal and monthly variability in the incidence of venous thromboembolism. Parkin L, Sweetland S, Balkwill A, et al: Body mass index, surgery, and risk of venous thromboembolism in middle-aged women: A cohort study. Zoller B, Li X, Sundquist J, et al: Age- and gender-specific familial risks for venous thromboembolism: A nationwide epidemiological study based on hospitalizations in Sweden. Tang Y, Sampson B, Pack S, et al: Ethnic differences in out-of-hospital fatal pulmonary embolism. Zoller B, Li X, Sundquist J, et al: Risk of pulmonary embolism in patients with autoimmune disorders: A nationwide follow-up study from Sweden. Mantha S, Karp R, Raghavan V, et al: Assessing the risk of venous thromboembolic events in women taking progestin-only contraception: A meta-analysis. Chandra D, Parisini E, Mozaffarian D: Meta-analysis: Travel and risk for venous thromboembolism. Corral J, Roldan V, Vicente V: Deep venous thrombosis or pulmonary embolism and factor V Leiden: Enigma or paradox Bounameaux H, Perrier A, Righini M: Diagnosis of venous thromboembolism: An update. Optimal Duration and Selection of Anticoagulants Anticoagulation for Acute Pulmonary Embolism 67. Prandoni P, Noventa F, Ghirarduzzi A, et al: the risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. Douketis J, Tosetto A, Marcucci M, et al: Risk of recurrence after venous thromboembolism in men and women: Patient level meta-analysis. Becattini C, Agnelli G, Schenone A, et al: Aspirin for preventing the recurrence of venous thromboembolism. Meyer G, Vicant E, Danays T, et al: Fibrinolysis for patients with intermediate-risk pulmonary embolism. Fukuda I, Taniguchi S, Fukui K, et al: Improved outcome of surgical pulmonary embolectomy by aggressive intervention for critically ill patients. Kataoka M, Inami T, Hayashida K, et al: Percutaneous transluminal pulmonary angioplasty for the treatment of chronic thromboembolic pulmonary hypertension. Barbar S, Noventa F, Rossetto V, et al: A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. Indeed, a number of recent important discoveries have improved our understanding of the disease, helped guide patient management, and laid foundations for future research. The term pulmonary hypertension refers to the presence of high pulmonary vascular pressure and can be the end result of a variety of different underlying disorders. Each pulmonary artery accompanies the appropriate-generation bronchus and divides with it down to the level of the respiratory bronchiole. Elastic arteries are conducting vessels that are highly distensible at low transmural pressure. As the arteries decrease in size, the number of elastic laminae decreases and smooth muscle increases. The intima of the pulmonary arteries consists of a single layer of endothelial cells and their basement membrane. The adventitia is composed of dense connective tissue in direct continuity with the peribronchial connective tissue sheath. The alveolar capillaries are lined with a continuous layer of endothelium resting on a continuous basement membrane and focally connected to scattered pericytes located beneath the basement membrane. Within the respiratory units, the pulmonary arteries and arterioles are centrally located and give rise to precapillary arterioles, from which a network of capillaries radiates into the alveolar walls. The alveolar capillaries collect at the periphery of the acini and then drain into venules located in the interlobular and interlobar septa. The bronchial arteries ramify into a capillary network drained by bronchial veins; some empty into the pulmonary veins and the remainder into the systemic venous bed. The bronchial circulation therefore constitutes a physiologic right-to-left shunt. The distal pulmonary arteries may be affected by medial hypertrophy and intimal fibrosis. A variable degree of destruction of the vascular bed in emphysematous or fibrotic areas may also be present. Hematologic disorders: chronic hemolytic anemias, myeloproliferative disorders, splenectomy 5. Systemic disorders: sarcoidosis, pulmonary Langerhans cell histiocytosis, lymphangioleiomyomatosis, neurofibromatosis, vasculitis 5. Metabolic disorders: glycogen storage disease, Gaucher disease, thyroid disorders 5. Many of these abnormalities both elevate vascular tone and promote vascular remodeling and therefore represent logical pharmacologic targets. These thrombi may completely occlude the lumen or form different grades of stenosis, webs, and bands. Collateral vessels from the systemic circulation (from bronchial, costal, diaphragmatic, and coronary arteries) can grow and at least partially perfuse the areas distal to complete obstructions. All mutations, either in a homozygous or compound-heterozygous state, disrupted function of the gene.
Discount 100mg kamagra effervescent mastercard
Few clinical trials have assessed the efficacy of antidepressant medications in patients with epilepsy erectile dysfunction causes std cheap kamagra effervescent 100 mg otc. Older antidepressants and the antidepressant bupropion have been associated with increased seizures and should be avoided. Prueter and Norra (2005) suggest that citalopram and sertraline be considered first-line antidepressant medications in epilepsy because of their limited interactions with antiepileptic medication. Conversion disorder Medication-induced conditions Reprinted with permission from Marsh, L. Individuals with comorbid anxiety and depressive disorders report lower quality of life than individuals with either disorder alone (Kanner et al. Common anxiety disorders include agoraphobia, generalized anxiety disorder, and social phobia. Care must be taken to distinguish between panic attacks and fear occurring in the context of a seizure ("ictal fear"). Rates of depression vary as a function of the sample assessed (clinical samples report higher rates of depression than population samples) and the measures used to diagnose depression. Depression often goes undiagnosed in patients with epilepsy, because symptoms of depression may be viewed as a normal reaction to illness. However, accurate diagnosis of depression is critical because depression is associated with poorer quality of life, under-employment, and family dysfunction (Ettinger et al. Interestingly, presurgical depression is associated with poorer postsurgical seizure outcomes (Metternich et al. The suicide rate in epilepsy is two or more times greater than in the general population (Stefanello et al. Risk factors for suicide include history of self-harm, family history of suicide, stressful life situations, poor morale, stigma, and psychiatric disorders. Individuals with comorbid anxiety and depression are at greater risk for suicidal ideation than individuals with only one syndrome (Stefanello et al. Psychosocial stressors, genetic disposition, and neuropathology may play Psychosis the association between epilepsy and psychosis has been debated throughout the past century. Individuals with epilepsy onset before age 20 years, duration of illness greater than 10 years, history of complex partial seizures, and temporal lobe epilepsy are at increased risk of psychotic disturbances. Postictal psychosis most commonly develops after many years of epilepsy (Devinsky, 2003). Episodes of postictal psychosis are short in duration, lasting from a few hours to a few months. In interictal psychosis, episodes of psychosis are not temporally tied to seizure onset and typically last for more than 6 months. Aggression the relationship between epilepsy and aggression remains controversial. Early research suggested that the prevalence of aggression in epilepsy ranged from 4. Rates of aggression are believed to be higher in individuals with temporal lobe epilepsy. Results vary owing to the definition of aggression used and the method of group selection. Hippocampal sclerosis is less common in individuals with epilepsy and aggression (Tebartz van Elst et al. A subgroup of individuals with epilepsy and aggression have significant amygdala atrophy (Tebartz van Elst, 2002). Stroke Neuropsychiatric disorders after stroke are common and distressing to patients and their families but often go undertreated. The most common neuropsychiatric outcomes of stroke are depression, anxiety, fatigue, and apathy, which each occur in at least 30% of patients and have substantial overlap. Neuropsychiatric complications of stroke are challenging to manage and require more research (Hackett et al. Interestingly, rates appear to be similar for individuals in early, middle, and late stages following stroke. Depression after a stroke is associated with age, time since stroke, cognitive impairment, and social support. Significantly higher rates (5 to 6 times more likely) of post-stroke depression have been reported among individuals with a premorbid diagnosis of depression (Ried et al. Depression is associated with longer hospital stays, suggesting that it affects rehabilitation efforts. Depression is associated with poorer recovery of activities of daily living and increased morbidity. The presence of executive dysfunction with or without co-occurring depressive symptoms may be the strongest predictor of morbidity following stroke (Melkas et al. Studies assessing the relationship between disability and depression in stroke patients have been equivocal. Depression is associated with poorer quality of life in individuals who have had a stroke, even when neurological symptoms and disability are held constant. The relationship between depression and lesion location has been the focus of significant research and controversy. Early research by Robinson and Price showed that left anterior lesions were associated with increased rates and severity of depression. Lesions nearer the left frontal pole or left caudate nucleus were associated with increased rates of depression. More recent review articles have not supported a relationship between lesion location and depression in post-stroke patients (Bhogal et al. Of note, there is significant heterogeneity in previous studies, particularly between different sample sources. Depression is associated with leftsided lesions in studies using hospital samples, whereas depression is associated with right-sided lesions in community samples (Bhogal et al. Poststroke depression is associated with left-sided lesions in individuals in the first month following stroke (Bhogal et al. Other differences in previous research, such as method of depression diagnosis, may contribute to the mixed results. Few studies have assessed the effectiveness of various treatments for depression in these patients. A recent review suggests that there is no clear evidence that standard antidepressant medications are effective in the treatment of poststroke depression (Hackett et al. Although such interventions may not lead to effective cessation of depressive disorders, they may result in overall reductions in depressive severity. One study suggests that nortriptyline was more effective in the treatment of depression than either placebo or fluoxetine (Robinson et al. In this study, response to treatment with nortriptyline was associated with improvement in cognitive and functional abilities. This improvement in cognition and functional abilities following reduction in depressive symptoms has not always been replicated (Hackett et al. Between 11% and 35% of individuals experience emotional incontinence after stroke (Parvizi et al. Emotional incontinence is associated with lesions of the brainstem and cerebellar region (see Parvizi et al. Note: Adjusted for age, sex, marital status, socioeconomic status, alcohol abuse, and quality of life. Aggression Reports have suggested that individuals have difficulty controlling aggression and anger following a stroke. Inability to control anger or aggression was associated with increased motor dysfunction and dysarthria. There is some evidence that lesions in the area supplied by the subcortical middle cerebral artery are associated with inability to control anger. Poststroke irritability and aggression are associated with lesions nearer to the frontal pole. Fluoxetine has been shown to successfully reduce levels of post-stroke anger (Choi-Kwon et al. Similarly, reductions in irritability and aggression have been associated with reductions in depression following pharmacological intervention (Chan et al. Many behavioral changes such as increased disinhibition are associated with dysfunction within the frontal cortex.
Safe 100mg kamagra effervescent
When compared with men impotence vasectomy kamagra effervescent 100mg on line, women with atrial fibrillation have a higher risk for stroke and are less likely to receive anticoagulation and ablation procedures. Current guidelines encourage at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise per week. Women are advised to sustain aerobic activities for at least 10 minutes during each exercise session. Resistance and strengthening exercises at least 2 days per week are also recommended for all women. The guidelines advise that women should not smoke and should avoid environmental tobacco smoke. If a high-risk woman has an indication for but is intolerant of aspirin therapy, clopidogrel should be substituted. Aspirin is useful for primary prevention in women 65 years or older (81 mg daily or 100 mg every other day) if blood pressure is controlled to reduce the risk for ischemic stroke. It may be reasonable to consider aspirin therapy in women younger than 65 years for prevention of ischemic stroke if they have high risk for stroke. This algorithm includes specific recommendations for prevention of stroke in women with atrial fibrillation (see also Chapter 38). This intervention also improves quality of life and medication compliance and reduces morbidity and mortality. Heart disease and stroke statistics-2014 update: A report from the American Heart Association. National Research Council: Exploring the Biological Contributions to Human Health: Does Sex Matter Huxley R, Barzi F, Woodward M: Excess risk of fatal coronary heart disease associated with diabetes in men and women: Meta-analysis of 37 prospective cohort studies. Hemingway H, McCallum A, Shipley M, et al: Incidence and prognostic implications of stable angina pectoris among women and men. Tsuchihashi K, Ueshima K, Uchida T, et al: Transient left ventricular apical ballooning without coronary artery stenosis: A novel heart syndrome mimicking acute myocardial infarction. Regitz-Zagrosek V, Petrov G, Lehmkuhl E, et al: Heart transplantation in women with dilated cardiomyopathy. Most women with cardiovascular disease can have a pregnancy with proper care, but a careful pre-pregnancy evaluation is mandatory. Cardiac disease may sometimes be manifested for the first time in pregnancy because the hemodynamic changes may compromise a limited cardiac reserve. An understanding of the normal findings on cardiac examination in a pregnant patient is therefore important. For those physicians counseling patients with cardiac disease about the potential risks of a pregnancy, a comprehensive knowledge of the underlying defect as well as of the hemodynamic changes that pregnancy will impose is imperative. With the declining incidence of rheumatic heart disease in Western countries, maternal cardiac disease is now predominantly congenital in origin, although at present the leading causes of maternal death are acquired disease, with myocardial infarction, aortic dissection, and cardiomyopathy recognized as the major clinical syndromes. Such patients should be seen in a high-risk pregnancy unit for evaluation including a clinical examination, electrocardiogram, and chest radiograph. An echocardiogram facilitates a detailed evaluation of myocardial function, valvular disease, and pulmonary artery pressures. In patients with congenital heart disease, their perception of normal activity may be skewed, and an exercise test is helpful in delineating their true functional aerobic capacity. In general, patients who cannot achieve more than 70% of their predicted functional aerobic capacity are unlikely to tolerate a pregnancy safely. A careful discussion of the maternal and fetal risks, and of whether or not these risks might change with time or treatment, is indicated. The possibility that pregnancy might cause irreversible hemodynamic deterioration should be considered, as well as the difficult issue of the long-term outlook for the mother. If the woman is going to pursue a pregnancy, a strategy should be outlined regarding the frequency of follow-up evaluation by the cardiologist, and a plan should be put in place for obstetric and cardiovascular management during the pregnancy as well as during labor and delivery. Worrisome predictors of maternal cardiac events include (1) prior cardiac event. Some series, for example, include only patients with congenital heart disease9; others include patients with acquired heart disease, and so-called high-risk patients, such as those with clinically significant pulmonary hypertension or a dilated aorta, may not be identified and are underrepresented. Accordingly, these "predictors" should be used only as a guide, and each case should be considered individually. During pregnancy, a multidisciplinary team approach is recommended, with close collaboration with the obstetrician, so that the mode, timing, and location of delivery can be planned. During pregnancy, fetal growth is monitored by the obstetric team, and for the woman with congenital heart disease, a fetal cardiac echocardiogram is offered at approximately 22 to 26 weeks of pregnancy to determine whether a congenital cardiac anomaly is present. The plasma volume approaches 50% above baseline by the second trimester and then virtually plateaus until delivery. By contrast, with a cesarean section, approximately 800 mL of blood often is lost, which may pose a more significant hemodynamic burden to the parturient. After delivery of the baby, an abrupt increase in venous return occurs, in part because of autotransfusion from the uterus but also because the baby no longer compresses the inferior vena cava. In addition, autotransfusion of blood continues in the 24 to 72 hours after delivery, and this is when pulmonary edema may occur. All of these abrupt changes mandate that for the high-risk patient with cardiac disease, a multidisciplinary approach during labor and delivery be used. The cardiologist and the obstetrician should work with the anesthesiologist to determine the safest mode of delivery. This increased plasma volume is followed by a slightly lesser rise in red cell mass, which results in the relative anemia of pregnancy. Uterine blood flow increases with placental growth, and an accompanying fall in peripheral resistance may result in a slight fall in blood pressure, which also begins in the first trimester. The venous pressure in the lower extremities rises, causing pedal edema in approximately 80% of healthy pregnant women. The adaptive changes of a normal pregnancy result in an increase in cardiac output, which by the end of the second trimester approaches 30% to 50% above baseline. For most patients with cardiac disease, a vaginal delivery is feasible and preferable; a cesarean section is indicated only for obstetric reasons. An important exception to this rule is that of the patient who is anticoagulated with warfarin, because the baby also is anticoagulated and thus at increased risk for intracranial hemorrhage from the stress of vaginal delivery. In addition, cesarean section also may be considered in patients who have a dilated unstable aorta. With these high-risk scenarios, delivery should take place in a center where expertise is available to monitor the hemodynamic changes of labor and delivery and to intervene when necessary. If vaginal delivery is elected, fetal and maternal electrocardiographic monitoring should be performed. Delivery can be accomplished with the mother in the left lateral position so that the fetus does not compress the inferior vena cava, thereby maintaining venous return. For those patients with tenuous hemodynamics, SwanGanz catheterization before onset of active labor facilitates optimization of the hemodynamics and should be continued for at least 24 hours after delivery, when pulmonary edema commonly occurs. No universal consensus has yet emerged regarding the administration of antibiotic prophylaxis at the time of delivery for patients with lesions vulnerable to infective endocarditis. Because bacteremia may occur even during an uncomplicated delivery, antibiotic prophylaxis remains optional for patients most vulnerable to the deleterious effects of endocarditis-that is, those with cyanotic heart disease and prosthetic valves. Because of the altered hemodynamics during pregnancy, the physical examination findings in a healthy pregnant woman reflect such changes and may mimic those in cardiac disease. By the middle of the second trimester, the jugular venous pressure may be elevated, with brisk descents, because of the volume overload and reduced peripheral resistance. The apical impulse is more prominent, and on auscultation, the first sound may appear loud. Commonly, an ejection systolic murmur can be heard at the left sternal edge, never more than grade 3/6 in intensity, which relates to increased flow through the left or right ventricular outflow tract. The second sound also may appear accentuated, and these combined auscultatory features may suggest an atrial septal defect or pulmonary hypertension. Continuous murmurs also may be heard, as either a cervical venous hum or a mammary souffle. If any findings on the physical examination are suggestive of cardiac disease, transthoracic echocardiography should be performed. This investigation facilitates the evaluation of ventricular size and function, valvular heart disease, and any these hemodynamic changes may be problematic for the mother with cardiac disease.
Cheap kamagra effervescent online mastercard
Organization around the physical findings is efficient because very specific neurological localization erectile dysfunction 26 order kamagra effervescent 100mg on line, which limits the diagnostic alternatives, often is possible. The long tracts of the nervous system traverse the entire brainstem in the longitudinal (rostrocaudal) plane, whereas cranial nerve nuclei and their respective cranial nerves originate and exit at distinct levels of the brainstem. This arrangement allows for exquisite localization of function based on the findings of the neurological examination. The chapter begins with a discussion of the brainstem ocular motor syndromes, followed by descriptions of miscellaneous brainstem, brainstem stroke, and thalamic syndromes. Vertical gaze ophthalmo- plegia is an example of a brainstem syndrome in which the objective physical findings dictate the diagnostic approach to the problem. Symptoms of vertical gaze ophthalmoplegia, when present, are relatively nonspecific and usually occur in patients who have difficulty looking down, as required for reading, eating from a table, and walking down a flight of stairs. The neurological examination discloses associated signs of the disorders listed in the differential diagnosis (see Box 21. The syndrome of combined vertical gaze ophthalmoplegia is diagnosed when the ocular findings occur in isolation from long-tract signs. With combined vertical gaze ophthalmoplegia, vertical saccades and pursuit are lost. The Bell phenomenon (reflex movement of the eyes up and out in response to forced eye closure) often is absent and skew deviation (vertical misalignment of the eyes) may occur. Isolated combined vertical gaze ophthalmoplegia usually is due to infarction of the rostral dorsal midbrain. When onset is gradual instead of abrupt or if the patient is young, other disorders should be considered (see Box 21. For Whipple disease, oculomasticatory myorhythmia, which consists of pendular converging and diverging eye oscillations with synchronous jaw oscillations, is pathognomonic. Care should be taken not to overlook lesions inferior to the floor of the third ventricle. Smallbowel biopsy should be considered if Whipple disease is a possible diagnosis. UpgazeParesis(DorsalMidbrainor ParinaudSyndrome) Another brainstem syndrome that can occur without symptoms is the dorsal midbrain syndrome. When symptoms do occur, the patient reports difficulty looking up and may have blurred distant vision caused by accommodative spasm. The location of the lesion causing the upgaze paresis of the dorsal midbrain syndrome is the posterior commissure and its interstitial nucleus (Leigh and Zee, 2006). The presence of the full syndrome implies a lesion of the dorsal midbrain (including the posterior commissure), bilateral lesions of the pretectal region, or a large unilateral tegmental lesion. Other than the mild upgaze limitation that can occur with aging, which is caused by involutional changes in the orbital connective tissues (Chaudhuri and Demer, 2013), the most common cause of loss of upgaze is a tumor in the pineal region. Forced ductions (see Chapter 18) may be performed by grasping anesthetized conjunctiva with forceps and moving the globe through its range of motion; the presence of restriction of movement with forced ductions implies a lesion within the orbit. In children and adolescents, pineal region tumors or obstructive hydrocephalus are usually the cause. Symptoms, when they occur, are related to difficulty in reading, eating, and walking down stairs. Neurological examination reveals loss of downward pursuit and saccades, although pursuit may sometimes be spared. The vertical oculocephalic maneuver may be normal or may disclose gaze limitation. Convergence may be lost, and gazeevoked upbeat nystagmus may be present on upward gaze. In young patients, forced ductions should be performed to assess for congenital restrictive downgaze limitation. Lesions may be detected in the rostral mesodiencephalic junction inferior to the floor of the third ventricle. When diplopia is present, it can be due to medial rectus paresis (horizontal diplopia) or skew deviation (vertical diplopia). Gazeevoked vertical nystagmus (usually on upgaze) and skew deviation may be present with the higher eye on the side of the lesion. Skew deviation is a pure vertical ocular misalignment that is not due to a cranial nerve palsy, orbital lesion, or strabismus but is caused by unilateral or asymmetrical damage to the otolith-ocular pathways (Zwergal et al. Internuclear ophthalmoplegia, discussed further in Chapter 44, may be a false localizing sign. Less common causes include trauma, herniation, infections, tumor, vasculitis, and surgical procedures. Limitation or slowing of adduction initially is formulated simply as an adduction deficit. With bilateral lesions, loss or limitation of horizontal saccades and (usually) pursuit in both directions is characteristic. In the acute phase, transient vertical gaze paresis and vertical nystagmus or upgaze paresis can also be seen. In the chronic phase, vertical eye movements are full, although nystagmus may be noted on upgaze. The explanation for gaze palsy occurring with a nuclear lesion is given later in the chapter (see Syndromes Involving Ocular Motor Nuclei). The diagnostic formulation varies with age, rapidity of onset, and associated clinical findings. For patients with an acute onset who are older than 50 years of age, stroke is a likely cause. Global paralysis of gaze rarely occurs in isolation, however, and signs and symptoms of involvement of other local structures usually are present. The location of the lesion is the frontopontine tract for saccades, and the parieto-occipito-pontine tract for pursuit, where they converge at the subthalamic and upper midbrain level (Thurtell and Halmagyi, 2008). The diagnostic formulation usually is focused on extraaxial (cranial nerve, neuromuscular junction, or muscle) pathology, because a brainstem lesion rarely causes isolated complete ophthalmoplegia. HorizontalGazeParesis Although there are no common symptoms of horizontal gaze paresis, this condition seldom occurs in isolation. Because supranuclear gaze pareses are conjugate by definition, diplopia does not occur. ThirdCranialNerveNucleus the common manifestations of third cranial nerve nucleus lesions are diplopia and ptosis. The signs present on the side of the lesion are weakness of the inferior and medial recti and the inferior oblique muscles. Upgaze limitation is present in both eyes because the superior rectus subnucleus is contralateral, and the axons from this subnucleus cross within the nuclear complex. Once the proper localization has been made, the diagnostic formulation is straightforward. SixthCranialNerveNucleus the sixth cranial nerve nucleus has two populations of neurons. Accordingly, a lesion of the sixth cranial nerve nucleus causes ipsilateral horizontal gaze palsy. On examination, a conjugate horizontal gaze paresis is present, which cannot be overcome by the oculocephalic maneuver or caloric stimulation. A peripheral seventh cranial nerve palsy usually accompanies a lesion of the sixth cranial nerve nucleus. When botulism is suspected, electromyography with repetitive nerve stimulation and serum or stool assay for botulinum toxin should be performed. The common symptoms are diplopia, oscillopsia (the illusion that objects or scenes are oscillating), and blurred vision. Associated findings include skew deviation and gaze-evoked nystagmus on upgaze or lateral gaze. Acutely, there may be an exotropia (one eye deviated outward) in primary position.