Buy trimethoprim online pills
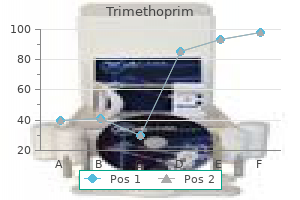
Avoid use in patients with: severe renal impairment (aluminum- and sodiumcontaining products); heart failure or high blood pressure (sodium-containing products) virus 912 discount trimethoprim 480mg with visa. Adverse effects include: diarrhea (magnesium preparations) and constipation (aluminum preparations). Bismuthcontaining products are also used to relieve upset stomach symptoms (indigestion, heartburn, nausea, gas, belching). Loperamide Avoid use in: children <12 years of age; patients with bloody or black stools. Adverse effects include: abdominal pain, nausea, constipation, drowsiness, dizziness, and dry mouth. Avoid use: in children <2 years of age (clotrimazole, miconazole, tolnaftate) or children <12 years of age (butenafine, terbinafine). Avoid use: in children <12 years of age; if patient has lower abdominal, back, or shoulder pain, or fever, chills, nausea, vomiting, or foulsmelling vaginal discharge; in combination with tampons, douches, spermicides, or other vaginal products. Adverse effects include: vaginal itching, burning, vaginal soreness, and swelling. Antitussives Dextromethorphan (Delsym, Robitussin Cough, Vicks 44) Temporary relief of cough due to minor throat and bronchial irritation with the common cold or inhaled irritants. Use with caution in patients with a chronic cough that occurs with smoking, asthma, and emphysema and in patients with cough with production of mucus. Adverse effects include: confusion, excitement, irritability, nervousness, and serotonin syndrome (uncommon). Temporarily relieves nasal congestion due to the common cold, hay fever, or other upper respiratory allergies. Use with caution in patients with: heart disease; high blood pressure; thyroid disease; diabetes; trouble urinating due to an enlarged prostate. Use with caution in patients with heart disease; high blood pressure; diabetes; thyroid disease; trouble urinating due to an enlarged prostate gland. Adverse effects include: arrhythmias, tachycardia, high blood pressure, anxiety, headache, dizziness, tremor, and insomnia. Patients taking oral contraceptives regularly should also use backup contraception, such as condom, until next period cycle starts. Emergency contraceptive Levonorgestrel (Plan B One-Step) To prevent pregnancy following unprotected intercourse or possible contraceptive failure. Adverse effects include: heavier menstrual bleeding, nausea, lower abdominal pain, fatigue, headache, dizziness, and breast tenderness. Expectorants Guaifenesin (Mucinex) Used to help loosen phlegm (mucus) and thin bronchial secretions to make cough more productive. Laxatives Bulk formers Polycarbophil, psyllium, and methylcellulose preparations (Citrucel, Fibercon, Metamucil) Temporary relief of occasional constipation and irregularity. Stimulants Adverse effects include: stomach discomfort, rectal burning, and mild cramps. Use with caution in patients on a sodium-restricted diet; in patients with kidney disease. All laxatives Use with caution in patients with a sudden change in bowel habits that persist for 2 weeks; in patients with abdominal pain, nausea, or vomiting. Treatment of overactive bladder for women with symptoms of urge incontinence and urinary urgency and frequency for at least 3 months. Avoid use in: men; women <18 years of age; patients with symptoms of a urinary tract infection (pain or burning when urinating, blood in urine, unexplained lower back pain, urine that is cloudy or foul smelling). Adverse effects include: sleepiness, dizziness, confusion, dry mouth, constipation, and blurred vision. Avoid use: if allergic to ragweed; in children <2 years of age; near the eyes; inside the nose, mouth, or vagina; on lice in eyebrows or eyelashes. Warnings Avoid use in: children <12 years of age; combination with alcohol, other antihistamines, or sedatives; individuals with angle-closure glaucoma; men with trouble urinating due to an enlarged prostate gland. Avoid use in: children <18 years of age; women who are pregnant or breastfeeding; individuals with temporomandibular joint disease (gum only); individuals with allergies to adhesive tape (patch only). Use patch with caution in patients with a history of dermatologic conditions (eczema, psoriasis, ectopic dermatitis). Gum Adverse effects include: jaw soreness, hiccups, dyspepsia, throat and mouth irritation, nausea, vomiting, lightheadedness. Lozenge Adverse effects include: mouth irritation, nausea, hiccups, cough, heartburn, headache, sore throat, dizziness. Transdermal patch Adverse effects include: local skin reactions (erythema, itching, burning), headache, and sleep disturbances (insomnia, abnormal/vivid dreams). Select the product that is simplest in formulation; in general, single-ingredient products are preferred. Combination products may contain effective doses of some ingredients and subtherapeutic doses of others. Furthermore, there may be differing durations of action among the ingredients, and there is always a possibility that the clinician or patient is unaware of the presence of certain active ingredients in the product. Many products with the same brand name contain different ingredients that are labeled for different uses. For example, multiple products (with different active ingredients) carry the Allegra name, including Allegra Allergy (fexofenadine), Allegra-D (fexofenadine and pseudoephedrine), and Allegra Anti-Itch Cream (allantoin and diphenhydramine). For children, the dose, dosage form, and palatability of the product are prime considerations. These agents should be avoided or used cautiously by patients with type 1 diabetes and patients with hypertension, angina, or hyperthyroidism. Cimetidine, an H2 antagonist, is a well-known inhibitor of hepatic drug metabolism and can increase the blood levels and toxicity of agents such as phenytoin, theophylline, and warfarin. A prime example is rhinitis medicamentosa or "rebound rhinitis," a condition that manifests as nasal congestion without rhinorrhea, associated with the regular use of topical decongestant nasal sprays for more than 3 days. The improper and long-term use of some antacids (eg, aluminum hydroxide) may cause constipation and even impaction in the elderly, as well as hypophosphatemia. Long-term laxative use can result in abdominal cramping and fluid and electrolyte disturbances. A condition known as laxative abuse syndrome is often observed in women with anorexia nervosa. The long-term use of analgesics containing caffeine may trigger rebound headaches upon discontinuation. Antihistamine Sneezing Runny nose Itchy, watery eyes Itchy throat Active ingredient (in each tablet) Purpose Uses temporarily relieves these symptoms due to hay fever or other upper respiratory allergies: Warnings Ask a doctor before use if you have Glaucoma A breathing problem such as emphysema or chronic bronchitis Trouble urinating due to an enlarged prostate gland Ask a doctor or pharmacist before use if you are taking tranquilizers or sedatives When using this product You may get drowsy Avoid alcoholic drinks Alcohol, sedatives, and tranquilizers may increase drowsiness Be careful when driving a motor vehicle or operating machinery Excitability may occur, especially in children If pregnant or breast-feeding, ask a health professional before use. In case of overdose, get medical help or contact a Poison Control Center right away. The label must contain, in the following order: active ingredient(s), including the amount in each dosage unit; purpose of product (pharmacologic action); use(s) for product (indication); specific warnings, including when the product should not be used and pregnancy information; when the patient should seek care of a health care provider; side effects and substances or activities to avoid; dosage instructions (when, how, and how often to take medication); and inactive ingredients. Additional requirements include, but are not limited to , the following: type size must be large enough to be easily read, >6-point font type for information in drug facts section; bullets must be solid square or circle 5-point type; and directions in table format for dosage instructions when presented for three or more age groups or populations. Antihistamines may cause sedation or drowsiness, especially when taken concurrently with sedative-hypnotics, tranquilizers, alcohol, or other central nervous system depressants. She also takes over-the-counter ibuprofen for occasional knee pain and a multivitamin supplement once daily. She has heard good things about natural products and asks you if taking a garlic supplement daily could help to bring her blood pressure and cholesterol under control. Are there any supplements that could increase bleeding risk if taken with ibuprofen The medical use of plants in their natural and unprocessed form undoubtedly began when the first intelligent animals noticed that certain food plants altered particular body functions. Since the literature surrounding dietary supplements is evolving, reputable evidence-based resources should be used to evaluate claims and guide treatment decisions. The recommendations in this database are limited by the quality of the existing research and the quality of the dietary supplement used at the time of the report.
Trimethoprim 480 mg line
These fistulas are the only high-flow and high-pressure lesions in the classification due to the direct connection between artery and sinus antibiotics sinus infection purchase genuine trimethoprim on line. All other fistulas are low flow secondary to their indirect fistulous connections with internal and external branches. Type D fistulas exist between branches of the internal and external carotid arteries and the cavernous sinus. Type A fistulas rarely undergo spontaneous resolution secondary to the high-flow and high-pressure nature of the fistulous connection. When left untreated, a majority of patients will develop progressive visual loss and aggressive neurologic symptoms. Concerning angiographic features, such as cortical venous reflux, represent an indication for treatment because of the increased likelihood of intracranial hemorrhage. Spittau and colleagues provided the most clinically useful classification based on the pattern of venous drainage. Variability in the anatomic location of occurrence, individual lesion angioarchitecture, and presenting symptomatology make accurate classification of lesions a vital step in preparing a treatment plan. The classification systems discussed here simplify these lesions by selecting the key features that are most likely to influence a particular mode of intervention. Effect of presenting hemorrhage on outcome after microsurgical resection of brain arteriovenous malformations. Treatment of arteriovenous malformations of the brain with combined embolization and stereotactic radiosurgery: results after 1 and 2 years. The efficacy of particulate embolization combined with stereotactic radiosurgery for treatment of large arteriovenous malformations of the brain. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Postembolization neurological deficits in cerebral arteriovenous malformations: stratification by arteriovenous malformation grade. A proposed grading system for endovascular treatment of cerebral arteriovenous malformations: Buffalo score. Linear accelerator radiosurgery of cerebral arteriovenous malformations: an update. Linac radiosurgery for cerebral arteriovenous malformations: results in 169 patients. Interim report on the radiosurgical treatment of cerebral arteriovenous malformations. Cerebral arteriovenous malformations: the value of radiologic parameters in predicting response to radiosurgery. Stereotactic linac-based radiosurgery in the treatment of cerebral arteriovenous malformations located deep, involving corpus callosum, motor cortex, or brainstem. Grading venous restrictive disease in patients with dural arteriovenous fistulas of the transverse/sigmoid sinus. Spontaneous carotid-cavernous fistulas: clinical, radiological, and therapeutic considerations. Endovascular treatment of intracranial dural arteriovenous fistulas with spinal perimedullary venous drainage. Dural arteriovenous fistulas of the posterior fossa draining into subarachnoid veins. Myelopathy due to intracranial dural arteriovenous fistulas draining intrathecally into spinal medullary veins. Spontaneous occlusion of a bilateral caroticocavernous fistula studied by serial angiography. Dural arteriovenous fistulas of the hypoglossal canal: systematic review on imaging anatomy, clinical findings, and endovascular management. Hypoglossal canal dural arteriovenous fistula: incidence and the relationship between symptoms and drainage pattern. Characteristics, diagnosis and treatment of hypoglossal canal dural arteriovenous fistula: report of nine cases. Microsurgical resection of these lesions is the most definitive strategy for occlusion but requires immense surgical prowess and endurance. This serves as a basis for preoperative surgical planning and determination of appropriate endovascular preoperative interventions. The next fundamental step involves a surgical approach with a wide operative field providing optimal working angles for the nidal disconnection, and unanticipated maneuvers are potentially necessary if complications are encountered. Feeding arteries must then be sequentially dissected, occluded, and disconnected from the nidus. Identifying and disconnecting the arterial feeding vessels involves perinidal circumdissection with immense importance reliant on preserving the dominant draining veins. Following circumdissection and occlusion of the feeding arteries, the dominant draining veins are disconnected to complete the nidal resection. These lesions provide an immense surgical challenge hindering intraoperative efficiency. Therefore, the surgeon must have knowledge of time-saving and decision-making maneuvers to provide an efficient strategy for the resection. Keywords: microsurgical, dissection, angioarchitecture, nidus, circumdissection, efficiency, fundamental, craniotomy 13. Therefore, neurosurgeons must be aware of the indications for therapy and selection of an appropriate mode of treatment. Large and/or complex lesions are often best managed with observation,8,9 but large malformations can be made more amendable to radiotherapy or microsurgical excision by the use of preoperative embolization. Key Points Understand the unique three-dimensional anatomic distribution of the arteriovenous malformation prior to attempting excision. Plan a generous exposure utilizing wide arachnoid dissection and gravity retraction to facilitate optimal working angles for the more tedious steps of excision. Feeding arteries must be located and appropriately sacrificed using microclips, bipolar cautery, or both. The exposure of the arteriovenous malformation nidus should proceed in a circumferential manner until the apex is visible, augmented by intraoperative navigation to ensure correct pial incision and transparenchymal trajectory. The surgeon must protect the dominant draining vein until the feeding arteries are sacrificed; if the vein is injured prior to sacrifice of the feeding arteries, the surgeon must control the venous bleeding without occluding the vein and focus on eliminating the feeding arteries. Timely removal of the arteriovenous malformation is the best method to control the bleeding. Out of these modalities, the catheter angiogram provides the most valuable information regarding nidus hemodynamics and angioarchitecture. Routine preoperative arterial pedicle embolization for augmentation of feeder devascularization can be performed based on surgeon preference. The enhanced flow through deep parenchymal feeders poses a greater intraoperative risk for hemorrhage during disconnection and these feeders are commonly inaccessible for embolization. Therefore, selective embolization of those feeders that are relatively inaccessible early in microsurgical dissection is reasonable. A preoperative discussion between the microsurgeon and interventionalist is warranted before embolization is undertaken. When planning patient positioning concerning the operative trajectory, the need for optimal working angles, maximizing exposure of feeding arteries, and minimizing risk to the major draining veins should be considered. The major pitfalls encountered with patient positioning include failure to maximize gravity retraction and forgoing the use of free surfaces while attempting to access the lesion. The failure to maximize gravity retraction on the brain results in the need for use of aggressive fixed retraction, which increases cortical injury risk and, potentially, morbidity. The superior and posterior margins of the nidus are obscured by the presence of embolic material. By endovascularly obliterating the major cortical pedicles, increased flow within parenchymal perforators is encouraged due to being the path of least resistance for hemodynamic flow. This enhanced flow increases the risk of hemorrhage from these vessels, which already pose a significant surgical challenge. It is paramount to avoid penetrating the dura while drilling to create the craniotomy; therefore, a greater number of burr holes as well as making short passes with the craniotome decreases the risk for injury to the underlying engorged draining veins.
Diseases
- Diaphragmatic hernia upper limb defects
- Syndactyly type 5
- Leukemia subleukemic
- Parsonage-Turner syndrome
- Keratosis palmoplantaris with corneal dystrophy
- Congenital rubella
- Van der Woude syndrome 2
- Wildervanck syndrome
Cheap trimethoprim express
The decision about positioning is usually straightforward with the head turned in such a way that lesion is in the most superior part of the exposure antibiotic z pack purchase trimethoprim 960mg overnight delivery. Lesions on the orbital surface generally warrant a lateral exposure if they are far from the midline, allowing for a lateral subfrontal view. Orbital surface lesions with a more medial presentation are usually best accessed from the anterior subfrontal view, making a head neutral with significant extension the position of choice. Lesions of the frontal lobe presenting to the interhemispheric fissure present several reasonable choices for positioning. One is a head neutral position with an interhemispheric approach and gentle retraction of the frontal lobe ipsilateral to the lesion from medial to lateral. This works well, particularly if the lesion is relatively superficial in the interhemispheric fissure. Another clever approach to a lesion presenting to the interhemispheric fissure is to place the patient lateral with the lesion side down. In this position, gravity naturally pulls the lesion-side brain down, giving a more natural medial-to-lateral retraction of the brain. Depending on how anterior and medially they present, they also have feeding from the anterior temporal artery and the anterior choroidal artery. Lesions that are more posterior can also recruit posterior cerebral artery feeding. It is important to keep this vasculature in mind when deciding what position to use. A true lateral position or supine with the head rotated the appropriate amount usually works well for this approach. First, it is best if the lesion is in the center of the brain exposed by the bone flap. Next, the position must facilitate access to the proximal feeding vessels and allow visualization of the draining veins. The veins, which in general cannot be sacrificed until the majority or all of the arterial input has been taken, can tether the mass of the nidus. Finally, the patient must be positioned in such a way that the surgeon is reasonably comfortable during the procedure. Long surgeries with the surgeon in some contorted position make for a long, painful day and lead to rushing and careless mistakes. Lesions with more anterior extension can be positioned supine with the head turned. For progressively more posterior lesions, it may be more comfortable to have the patient either in a semi-sitting position or prone. In the superficial frontal lobe, especially in the superior, middle, and inferior frontal gyrus, arterial supply is from anterior Dumont et al. Sitting and semi-sitting have the advantage of allowing pooled blood to run off during surgery, facilitating visualization and maximizing the effectiveness of the bipolar. The disadvantage is the added time it takes to position properly and the added risk of hypotension and air embolism. More posterior lesions are exposed via a horseshoe-shaped flap with the lesion in the center. Lesions that present to the interhemispheric fissure can be exposed via a bicoronal incision. First, care must be used in placing the cranial fixation device such as the Mayfield head holder. Either the pins can get in the way of the exposure or they can be placed too far from the equator of the head allowing the head to slip. Even if the head holder shifts subtly during the case, the resulting movement can make the skin closure difficult. Occasionally, someone may have to crawl under the blood drapes to remove the fixed head holder and switch to a horseshoe-type holder in order to complete the closure. When dissection within the interhemispheric fissure is needed, the sagittal sinus must be exposed. There are many options for this but the safest alternative is to place multiple burr holes on either side of the sinus, strip the dura of the sinus away from the bone flap, and then carefully complete the cutting of the bone immediately over the sinus. Fortunately, the dura of the sinus is very thick; unfortunately, the sinus can be arterialized and the normally easily controlled transosseous venous bleeding can be arterialized and difficult to control. Working under the bone edge, especially if there is any problem in controlling intraoperative bleeding, can lead to serious problems. The transosseous venous channels can be a source of important bleeding while turning the craniotomy as they can be arterialized. This step should be never underestimated and should be preferentially done under the microscope. It is easy to lose the benefits of a generous craniotomy by minimizing the extent of dura opening. The dura can be stellated into as many parts as necessary to maximize the opening. Not infrequently, especially near the venous sinuses, a large arterialized vein will enter the dura and then travel within the dura to reach the sinus. At the end of the case, if the vein is arterialized, the vein along with the portion of dura left to protect it can be sacrificed. Lesions of the anterior, superior, and middle temporal gyrus can be exposed via a standard pterional approach. If the lesion is also in the inferior temporal gyrus, it is useful to do an interfacial dissection of the temporal fascia. This extended exposure is mandatory for middle cranial fossa presenting lesions in which a subtemporal look is necessary. If the lesion is anterior, such as in the uncus, the lesion may be immediately visualized with minimal frontal or temporal lobe retraction. If the lesion is more posterior, in and around the sylvian fissure, it may be necessary to split the fissure for optimal exposure. During the exposure therefore, it is necessary to make the exposure sufficiently large to identify the distal vessel. Deep lesions of the temporal lobe are more complex and are beyond the scope of this chapter. Lesions of the convexity can be treated using a pterional-type exposure 122 Dumont et al. Surgical Approaches and Nuances for Lobar Arteriovenous Malformations arterialized sinus with care. The safest way to accomplish this is with multiple burr holes on both sides of the sinus. Similarly, although less often than frontally, important arterialized or nonarterialized veins may travel through the dura on their way to the sinus. The occipital lobe, especially in the region of the interhemispheric fissure, should be considered eloquent because of the visual pathways and the visual cortex. Care must be taken not only to avoid injury to the surrounding brain during resection, but also in utilizing retraction. Prolonged retraction of the occipital lobe from medial to lateral to work in the interhemispheric fissure frequently results in a visual field deficit, which may not always be reversible. Placing the patient in the lateral position with the lesion-side down is one way to try to minimize retraction injury. The risks of embolization are not insignificant, and our own institutional data identified a 7. An individualized approach to this adjunct will help minimize the risks and ensure that only those who will truly benefit from embolization are treated. Preoperative embolization is not the same as preradiosurgical embolization or embolization used alone with an intent to cure or treat a high-risk feature. Embolization can also be used to treat flow-related aneurysms that will not be easily accessible during the resection. Careful study of the Onyx cast after embolization can also help to orient the surgeon during the resection and facilitate microsurgical manipulation of the lesion. For larger lesions, the embolization is best performed in stages in order to avoid sudden hemodynamic shifts that could predispose to normal perfusion pressure breakthrough. We generally prefer a 2-day interval, or longer, between embolization sessions in order to give the local cerebral circulation a chance to adjust to the increased flow.
Buy trimethoprim 960mg without prescription
Vital signs-Careful evaluation of vital signs (blood pressure antibiotics horses generic trimethoprim 480mg visa, pulse, respirations, and temperature) is essential in all toxicologic emergencies. Hypertension and tachycardia are typical with amphetamines, cocaine, and antimuscarinic (anticholinergic) drugs. Hypotension and bradycardia are characteristic features of overdose with calcium channel blockers, blockers, clonidine, and sedative hypnotics. Hypotension with tachycardia is common with tricyclic antidepressants, trazodone, quetiapine, vasodilators, and agonists. Rapid respirations are typical of salicylates, carbon monoxide, and other toxins that produce metabolic acidosis or cellular asphyxia. Hyperthermia may be associated with sympathomimetics, anticholinergics, salicylates, and drugs producing seizures or muscular rigidity. Constriction of the pupils (miosis) is typical of opioids, clonidine, phenothiazines, and cholinesterase inhibitors (eg, organophosphate insecticides), and deep coma due to sedative drugs. Horizontal nystagmus is characteristic of intoxication with phenytoin, alcohol, barbiturates, and other sedative drugs. The presence of both vertical and horizontal nystagmus is strongly suggestive of phencyclidine poisoning. Mouth-The mouth may show signs of burns due to corrosive substances, or soot from smoke inhalation. Poisoning due to cyanide can be recognized by some examiners as an odor like bitter almonds. Skin-The skin often appears flushed, hot, and dry in poisoning with atropine and other antimuscarinics. Excessive sweating occurs with organophosphates, nicotine, and sympathomimetic drugs. First, the airway should be cleared of vomitus or any other obstruction and an oral airway or endotracheal tube inserted if needed. For many patients, simple positioning in the lateral, left-side-down position is sufficient to move the flaccid tongue out of the airway. Breathing should be assessed by observation and pulse oximetry and, if in doubt, by measuring arterial blood gases. Patients with respiratory insufficiency should be intubated and mechanically ventilated. The circulation should be assessed by continuous monitoring of pulse rate, blood pressure, urinary output, and evaluation of peripheral perfusion. An intravenous line should be placed and blood drawn for serum glucose and other routine determinations. At this point, every patient with altered mental status should receive a challenge with concentrated dextrose, unless a rapid bedside blood glucose test demonstrates that the patient is not hypoglycemic. Hypoglycemic patients may appear to be intoxicated, and there is no rapid and reliable way to distinguish them from poisoned patients. It is useful to remember that these drugs cause death primarily by respiratory depression; therefore, if airway and breathing assistance have already been instituted, naloxone may not be necessary. Larger doses of naloxone may be needed for patients with overdose involving propoxyphene, codeine, and some other opioids. The benzodiazepine antagonist flumazenil (see Chapter 22) may be of value in patients with suspected benzodiazepine overdose, but it should not be used if there is a history of tricyclic antidepressant overdose or a seizure disorder, as it can induce convulsions in such patients. This includes gathering any available history and performing a toxicologically oriented physical examination. Other causes of coma or seizures such as head trauma, meningitis, or metabolic abnormalities should be sought and treated. Icterus may suggest hepatic necrosis due to acetaminophen or Amanita phalloides mushroom poisoning. Abdomen-Abdominal examination may reveal ileus, which is typical of poisoning with antimuscarinic, opioid, and sedative drugs. Hyperactive bowel sounds, abdominal cramping, and diarrhea are common in poisoning with organophosphates, iron, arsenic, theophylline, A phalloides, and A muscaria. Focal seizures or motor deficits suggest a structural lesion (eg, intracranial hemorrhage due to trauma) rather than toxic or metabolic encephalopathy. Nystagmus, dysarthria, and ataxia are typical of phenytoin, carbamazepine, alcohol, and other sedative intoxication. Twitching and muscular hyperactivity are common with atropine and other anticholinergic agents, and cocaine and other sympathomimetic drugs. Muscular rigidity can be caused by haloperidol and other antipsychotic agents, and by strychnine or by tetanus. Generalized hypertonicity of muscles and lower extremity clonus are typical of serotonin syndrome. Seizures are often caused by overdose with antidepressants (especially tricyclic antidepressants and bupropion [as in the case study]), cocaine, amphetamines, theophylline, isoniazid, and diphenhydramine. Alterations in the serum potassium level are hazardous because they can result in cardiac arrhythmias. Drugs that may cause hyperkalemia despite normal renal function include potassium itself, blockers, digitalis glycosides, potassium-sparing diuretics, and fluoride. Drugs associated with hypokalemia include barium, agonists, caffeine, theophylline, and thiazide and loop diuretics. Renal Function Tests Some toxins have direct nephrotoxic effects; in other cases, renal failure is due to shock or myoglobinuria. Blood urea nitrogen and creatinine levels should be measured and urinalysis performed. Arterial Blood Gases Hypoventilation results in an elevated Pco2 (hypercapnia) and a low Po2 (hypoxia). The Po2 may also be low in a patient with aspiration pneumonia or drug-induced pulmonary edema. Poor tissue oxygenation due to hypoxia, hypotension, or cyanide poisoning will result in metabolic acidosis. The Po2 measures only oxygen dissolved in the plasma and not total blood oxygen content or oxyhemoglobin saturation and may appear normal in patients with severe carbon monoxide poisoning. Pulse oximetry may also give falsely normal results in carbon monoxide intoxication. A larger than expected anion gap is caused by the presence of unmeasured anions (lactate, etc) accompanying metabolic acidosis. This may occur with numerous conditions, such as diabetic ketoacidosis, renal failure, or shock-induced lactic acidosis. Drugs that may induce an elevated anion gap metabolic acidosis Substances that are often associated with an abnormal osmol gap include acetone, ethanol, ethylene glycol, isopropyl alcohol, methanol, and propylene glycol. Decontamination C Decontamination procedures should be undertaken simultaneously with initial stabilization, diagnostic assessment, and laboratory evaluation. Skin Contaminated clothing should be completely removed and double-bagged to prevent illness in health care providers and for possible laboratory analysis. Gastrointestinal Tract Controversy remains regarding the efficacy of gastrointestinal decontamination, especially when treatment is initiated more than 1 hour after ingestion. For most ingestions, clinical toxicologists recommend simple administration of activated charcoal to bind ingested poisons in the gut before they can be absorbed (as in the case study). In unusual circumstances, gastric lavage or whole bowel irrigation may also be used. Hypoxemia due to carbon monoxide poisoning may result in ischemic changes on the electrocardiogram. Imaging Findings A plain film of the abdomen may be useful because some tablets, particularly iron and potassium, may be radiopaque. Chest radiographs may reveal aspiration pneumonia, hydrocarbon pneumonia, or pulmonary edema. Hemodialysis may be indicated depending on the severity of poisoning or the blood concentration: Carbamazepine Ethylene glycol Lithium Methanol Metformin Phenobarbital Salicylate Theophylline Valproic acid Hemodialysis is ineffective or is not useful: Amphetamines Antidepressants Antipsychotic drugs Benzodiazepines Calcium channel blockers Digoxin Metoprolol and propranolol Opioids 1 Toxicology Screening Tests It is a common misconception that a toxicology "screen" is the best way to diagnose and manage an acute poisoning.
Purchase trimethoprim line
Sample error infection home remedy 960 mg trimethoprim, eg, obtaining cultures after antimicrobial agents have been administered, inadequate volume or quantity of specimen obtained, or contamination of specimens sent for culture 2. Noncultivable or slow-growing organisms (Histoplasma capsulatum, Bartonella or Brucella species), in which cultures are often discarded before sufficient growth has occurred for detection 3. Not recognizing the need for special media or isolation techniques (eg, charcoal yeast extract agar for isolation of Legionella species, shell-vial tissue culture system for rapid isolation of cytomegalovirus) Even in the setting of a classic infectious disease for which isolation techniques have been established for decades (eg, pneumococcal pneumonia, pulmonary tuberculosis, streptococcal pharyngitis), the sensitivity of the culture technique may be inadequate to identify all cases of the disease. Cultures of specimens taken from infected sites should eventually become sterile or demonstrate eradication of the pathogen and are useful for documenting recurrence or relapse. Followup cultures may also be useful for detecting superinfections or the development of resistance. The duration of definitive therapy required for cure depends on the pathogen, the site of infection, and host factors (immunocompromised patients generally require longer courses of treatment). Precise data on duration of therapy exist for some infections (eg, streptococcal pharyngitis, syphilis, gonorrhea, tuberculosis, and cryptococcal meningitis). Minimizing duration of antimicrobial therapy for specific infections is an intervention that may help prevent the development of antimicrobial resistance. For many infections, a combined medical-surgical approach may be required for clinical cure. First-generation cephalosporins: cefazolin for parenteral administration; cefadroxil or cephalexin for oral administration. Second-generation cephalosporins: cefuroxime for parenteral administration; cefaclor, cefuroxime axetil, cefprozil for oral administration. Third-generation cephalosporins: ceftazidime, cefotaxime, ceftriaxone for parenteral administration; cefixime, cefpodoxime, ceftibuten, cefdinir, cefditoren for oral administration. Gemifloxacin, levofloxacin, and moxifloxacin have excellent activity against pneumococci. Generally, streptomycin and gentamicin are used to treat infections with Gram-positive organisms, whereas gentamicin, tobramycin, and amikacin are used to treat infections with Gram-negatives. Regimens that have been reported to be efficacious include nitrofurantoin (for urinary tract infection); potential regimens for bacteremia include daptomycin, linezolid, and dalfopristin/quinupristin. When meningitis with penicillin-resistant pneumococcus is suspected, empiric therapy with this regimen is recommended. Quinolones used to treat pneumonococcal infections include levofloxacin, moxifloxacin, and gemifloxacin. Adjunctive immunomodulatory drugs such as drotrecogin-alfa can also be considered for patients with severe sepsis. Errors in susceptibility testing are rare, but the original results should be confirmed by repeat testing. Drug dosing and absorption should be scrutinized and tested directly using serum measurements, pill counting, or directly observed therapy. For example, are adequate numbers of granulocytes present and is undiagnosed immunodeficiency, malignancy, or malnutrition present Finally, culture and susceptibility testing should be repeated to determine whether superinfection has occurred with another organism or whether the original pathogen has developed drug resistance. Pharmacodynamic factors include pathogen susceptibility testing, drug bactericidal versus bacteriostatic activity, drug synergism, antagonism, and postantibiotic effects. Together with pharmacokinetics, pharmacodynamic information permits the selection of optimal antimicrobial dosage regimens. For drugs whose killing action is concentration-dependent, the rate and extent of killing increase with increasing drug concentrations. Concentration-dependent killing is one of the pharmacodynamic factors responsible for the efficacy of once-daily dosing of aminoglycosides. Proposed mechanisms include (1) slow recovery after reversible nonlethal damage to cell structures; (2) persistence of the drug at a binding site or within the periplasmic space; and (3) the need to synthesize new enzymes before growth can resume. For agents that are primarily bacteriostatic, inhibitory drug concentrations are much lower than bactericidal drug concentrations. In general, cell wall-active agents are bactericidal, and drugs that inhibit protein synthesis are bacteriostatic. The classification of antibacterial agents as bactericidal or bacteriostatic has limitations. Some agents that are considered to be bacteriostatic may be bactericidal against selected organisms. On the other hand, enterococci are inhibited but not killed by vancomycin, penicillin, or ampicillin used as single agents. Bacteriostatic and bactericidal agents are equivalent for the treatment of most infectious diseases in immunocompetent hosts. Bactericidal agents should be selected over bacteriostatic ones in circumstances in which local or systemic host defenses are impaired. Bactericidal agents are required for treatment of endocarditis and other endovascular infections, meningitis, and infections in neutropenic cancer patients. Failure to reduce antimicrobial agent dosage in such patients may cause toxic effects. Conversely, patients with burns, cystic fibrosis, or trauma may have increased dosage requirements for selected agents. The pharmacokinetics of antimicrobials is also altered in the elderly (see Chapter 60), in neonates (see Chapter 59), and in pregnancy. Drug Concentrations in Body Fluids Most antimicrobial agents are well distributed to most body tissues and fluids. In most cases, oral therapy with these drugs is equally effective, is less costly, and results in fewer complications than parenteral therapy. The intravenous route is preferred in the following situations: (1) for critically ill patients; (2) for patients with bacterial meningitis or endocarditis; (3) for patients with nausea, vomiting, gastrectomy, ileus, or diseases that may impair oral absorption; and (4) when giving antimicrobials that are poorly absorbed following oral administration. Monitoring Serum Concentrations of Antimicrobial Agents For most antimicrobial agents, the relation between dose and therapeutic outcome is well established, and serum concentration monitoring is unnecessary for these drugs. To justify routine serum concentration monitoring, it should be established (1) that a direct relationship exists between drug concentrations and efficacy or toxicity; (2) that substantial interpatient variability exists in serum concentrations on standard doses; (3) that a small difference exists between therapeutic and toxic serum concentrations; (4) that the clinical efficacy or toxicity of the drug is delayed or difficult to measure; and (5) that an accurate assay is available. In clinical practice, serum concentration monitoring is routinely performed on patients receiving aminoglycosides or vancomycin. Flucytosine serum concentration monitoring has been shown to reduce toxicity when doses are adjusted to maintain peak concentrations below 100 mcg/mL. Conditions That Alter Antimicrobial Pharmacokinetics Various diseases and physiologic states alter the pharmacokinetics of antimicrobial agents. Although indications for combination therapy exist, antimicrobial combinations are often overused in clinical practice. The unnecessary use of antimicrobial combinations increases toxicity and costs and may occasionally result in reduced efficacy due to antagonism of one drug by another. Antimicrobial combinations should be selected for one or more of the following reasons: 1. To treat polymicrobial infections (such as intra-abdominal abscesses, which typically are due to a combination of anaerobic and aerobic Gram-negative organisms, and enterococci). The antimicrobial combination chosen should cover the most common known or suspected pathogens but need not cover all possible pathogens. The availability of antimicrobials with excellent polymicrobial coverage (eg, -lactamase inhibitor combinations or carbapenems) may reduce the need for combination therapy in the setting of polymicrobial infections. The value of combination therapy in this setting has been clearly demonstrated for tuberculosis. To decrease dose-related toxicity by using reduced doses of one or more components of the drug regimen. This use of antimicrobial combinations is discussed in the paragraphs that follow. However, for some infections there are no effective alternatives to the drug of choice. For example, in patients with neurosyphilis who have a history of anaphylaxis to penicillin, it is necessary to perform skin testing and desensitization to penicillin.
Syndromes
- If you are seeking treatment of drug abuse for yourself or a family member
- Vaginal bleeding
- Hematoma (blood accumulating under the skin)
- Children 10 years and older, and adults (including seniors): 60 - 100 beats per minute
- Disseminated intravascular coagulation (DIC)
- If the amount of zinc or tin swallowed is low, recovery should occur within approximately 6 hours.
- Secondary syphilis occurs about 2-8 weeks after the first sores form. About 33% of those who do not have their primary syphilis treated will develop this second stage. These symptoms will often also go away without treatment and again, the bacteria become dormant (inactive) in your system. For more specific information about this type of syphilis, see secondary syphilis.
Generic 960 mg trimethoprim amex
The renal excretion of active drug can also be affected by concurrent drug therapy infection 4 weeks after surgery purchase 480mg trimethoprim visa. The renal excretion of drugs that are weak acids or weak bases may be influenced by other drugs that affect urinary pH. This is due to changes in ionization of the object drug, as described in Chapter 1 under Ionization of Weak Acids and Weak Bases; the Henderson-Hasselbalch Equation. For some drugs, active secretion into the renal tubules is an important elimination pathway. P-glycoprotein, organic anion transporters, and organic cation transporters are involved in active tubular secretion of some drugs, and inhibition of these transporters can inhibit renal elimination with attendant increase in serum drug concentrations. Many drugs are partially eliminated by P-glycoprotein, including digoxin, cyclosporine, dabigatran, colchicine, daunorubicin, and tacrolimus. The plasma concentration of these drugs can be increased by inhibitors of P-glycoprotein including amiodarone, clarithromycin, erythromycin, ketoconazole, ritonavir, and quinidine. In theory, drugs acting on the same receptor or process are usually additive, eg, benzodiazepines plus barbiturates, until the receptor is saturated or the effect is maximal. However, two drugs competing for the same binding site may result in less than an additive effect. Drugs acting on different receptors or sequential processes may be synergistic, eg, nitrates plus sildenafil or sulfonamides plus trimethoprim. Conversely, drugs with opposing pharmacologic effects may reduce the response to one or both drugs. Pharmacodynamic drug interactions are relatively common in clinical practice, but adverse effects can usually be minimized if one understands the pharmacology of the drugs involved. In this way, the interactions can be anticipated and appropriate counter-measures taken. For example, concurrent administration of two nephrotoxic drugs can produce kidney damage, even though the dose of either drug alone may be insufficient to produce toxicity. Furthermore, some drugs can enhance the organ toxicity of another drug, even though the enhancing drug has no intrinsic toxic effect on that organ. Hukkanen J: Induction of cytochrome P450 enzymes: A view on human in vivo findings. Meng Q, Lin K: Pharmacokinetic interactions between herbal medicines and prescribed drugs: Focus on drug metabolic enzymes and transporters. Pelkonen O et al: Inhibition and induction of human cytochrome P450 enzymes: Current status. Zakeri-Milani P, Valzadeh H: Intestinal transporters: Enhanced absorption through P-glycoprotein-related drug interactions. The two drugs may or may not act on the same receptor to Appendix: Vaccines, Immune Globulins, & Other Complex Biologic Products Harry W. Maddix, PharmD Vaccines and related biologic products constitute an important group of agents that bridge the disciplines of microbiology, infectious diseases, immunology, and immunopharmacology. The reader who requires more complete information is referred to the sources listed at the end of this appendix. From a practical standpoint, only immunoglobulins have been used for passive immunization, because passive administration of cellular components of the immune system has been technically difficult and associated with graft-versus-host reactions. Products of the cellular immune system (eg, interferons) have also been used in the therapy of a wide variety of hematologic and infectious diseases (see Chapter 55). Passive immunization with antibodies may be accomplished with either animal or human immunoglobulins in varying degrees of purity. These may contain relatively high titers of antibodies directed against a specific antigen or, as is true for pooled immune globulin, may simply contain antibodies found in most of the population. Passive immunization is useful for (1) individuals unable to form antibodies (eg, congenital agammaglobulinemia); (2) prevention of disease when time does not permit active immunization (eg, postexposure); (3) for treatment of certain diseases normally prevented by immunization (eg, tetanus); and (4) for treatment of conditions for which active immunization is unavailable or impractical (eg, snakebite). The injections may be moderately painful, and rarely a sterile abscess may occur at the injection site. Desirable features of the ideal immunogen include complete prevention of disease, prevention of the carrier state, production of prolonged immunity with a minimum of immunizations, absence of toxicity, and suitability for mass immunization (eg, cheap and easy to administer). Active immunization is generally preferable to passive immunization-in most cases because higher antibody levels are sustained for longer periods of time, requiring less frequent immunization, and in some cases because of the development of concurrent cell-mediated immunity. However, active immunization requires time to develop and is therefore generally inactive at the time of a specific exposure (eg, for parenteral exposure to hepatitis B, concurrent hepatitis B IgG [passive antibodies] and active immunization are given to prevent illness). Adults with immunocompromising conditions, asplenia, cerebrospinal fluid leaks, or cochlear implants 3. Previously unvaccinated adults at increased risk for occupational or travel exposure to polioviruses 1. Postexposure prophylaxis (administer with rabies immune globulin in previously unvaccinated individuals) Rabies Inactivated virus Rotavirus Live virus None Every 10 years For all infants 1. Persons past their 13th birthday without a history of varicella infection or immunization 3. Influenza vaccine should be administered annually to children aged 6 months to 18 years. Conventional immune globulin contains aggregates of IgG; it will cause severe reactions if given intravenously. However, if the passively administered antibodies are derived from animal sera, hypersensitivity reactions ranging from anaphylaxis to serum sickness may occur. Highly purified immunoglobulins, especially from rodents or lagomorphs, are the least likely to cause reactions. To avoid anaphylactic reactions, tests for hypersensitivity to the animal serum must be performed. If an alternative preparation is not available and administration of the specific antibody is deemed essential, desensitization can be carried out. Consequently, much smaller doses of human antibody can be administered to provide therapeutic concentrations for several weeks. Prophylaxis to decrease the risk of infection, interstitial pneumonia, and acute graft-versus-host disease in adults undergoing bone marrow transplantation. For the treatment of patients <1 year of age with infant botulism caused by toxin type A or B. The availability of hepatitis A vaccine has greatly reduced the need for preexposure prophylaxis. Patients >40 years should receive hepatitis A vaccine in addition to immune globulin for postexposure prophylaxis Postexposure prophylaxis in nonimmune persons following percutaneous, mucosal, sexual, or perinatal exposure. Postexposure prophylaxis (within 6 days after exposure) in nonimmune contacts of acute cases.
Order trimethoprim 480 mg online
These drug reactions are manifested as skin eruptions virus 20 deviantart gallery buy discount trimethoprim online, edema, anaphylactoid reactions, glomerulonephritis, fever, and eosinophilia. Drug reactions mediated by immune responses can have several different mechanisms. IgE is fixed to tissue mast cells and blood basophils, and after interaction with antigen the cells release potent mediators. These allergic responses involve IgG or IgM in which the antibody becomes fixed to a host cell, which is then subject to complementdependent lysis or to antibody-dependent cellular cytotoxicity. In some drug reactions, several of these hypersensitivity responses may occur simultaneously. Some adverse reactions to drugs may be mistakenly classified as allergic or immune when they are actually genetic deficiency states or are idiosyncratic and not mediated by immune mechanisms (eg, hemolysis due to primaquine in glucose-6-phosphate dehydrogenase deficiency, or aplastic anemia caused by chloramphenicol). When this happens, the immune system detects the drug-hapten conjugate as "modified self" and responds by generating IgE antibodies specific for the drug-hapten. It is not known why some patients mount an IgE response to a drug while others mount IgG responses. Fixation of the IgE antibody to high-affinity Fc receptors (FcRs) on blood basophils or their tissue equivalent (mast cells) sets the stage for an acute allergic reaction. The most important sites for mast cell distribution are skin, nasal epithelium, lung, and gastrointestinal tract. When the offending drug is reintroduced into the body, it binds and cross-links basophil and mast cell-surface IgE to signal release of the mediators (eg, histamine, leukotrienes; see Chapters 16 and 18) from granules. Other vasoactive substances such as kinins may also be generated during histamine release. These mediators initiate immediate vascular smooth muscle relaxation, increased vascular permeability, hypotension, edema, and bronchoconstriction. Several agents directed toward the inhibition of leukotrienes may be useful in acute allergic and inflammatory disorders (see Chapter 20). Desensitization to Drugs When reasonable alternatives are not available, certain drugs (eg, penicillin, insulin) must be used for life-threatening illnesses even in the presence of known allergic sensitivity. In such cases, desensitization (also called hyposensitization) can sometimes be accomplished by starting with very small doses of the drug and gradually increasing the dose over a period of hours or days to the full therapeutic range (see Chapter 43). This practice is hazardous and must be performed under direct medical supervision with epinephrine available for immediate injection, as anaphylaxis may occur before desensitization has been achieved. It is thought that slow and progressive administration of the drug gradually binds all available IgE on mast cells, triggering a gradual release of granules. Once all of the IgE on the mast cell surfaces has been bound and the cells have been degranulated, therapeutic doses of the offending drug may be given with minimal further immune reaction. Examples include systemic lupus erythematosus following hydralazine or procainamide therapy, "lupoid hepatitis" due to cathartic sensitivity, autoimmune hemolytic anemia resulting from methyldopa administration, thrombocytopenic purpura due to quinidine, and agranulocytosis due to a variety of drugs. In these drug-induced autoimmune states, IgG antibodies bind to drug-modified tissue and are destroyed by the complement system or by phagocytic cells with Fc receptors. Fortunately, autoimmune reactions to drugs usually subside within several months after the offending drug is withdrawn. Immunosuppressive therapy is warranted only when the autoimmune response is unusually severe. Drug Treatment of Immediate Allergy One can test an individual for possible sensitivity to a drug by a simple scratch test, ie, by applying an extremely dilute solution of the drug to the skin and making a scratch with the tip of a needle. However, skin tests may be negative in spite of IgE hypersensitivity to a hapten or to a metabolic product of the drug, especially if the patient is taking steroids or antihistamines. Drugs that modify allergic responses act at several links in this chain of events. In the efferent limb of the allergic response, isoproterenol, epinephrine, and theophylline reduce the release of mediators from mast cells and basophils and produce bronchodilation. Epinephrine opposes histamine; it relaxes bronchiolar smooth muscle and contracts vascular muscle, relieving both bronchospasm and hypotension. As noted in Chapter 8, epinephrine is the drug of choice in anaphylactic reactions. The antihistamines competitively inhibit histamine, which would otherwise produce bronchoconstriction and increased capillary permeability in end organs. The clinical features of serum sickness include urticarial and erythematous skin eruptions, arthralgia or arthritis, lymphadenopathy, glomerulonephritis, peripheral edema, and fever. The mechanism of tissue injury is immune complex formation and deposition on basement membranes (eg, lung, kidney), followed by complement activation and infiltration of leukocytes, causing tissue destruction. Glucocorticoids are useful in attenuating severe serum sickness reactions to drugs. In severe cases plasmapheresis can be used to remove the offending drug and immune complexes from circulation. The sulfonamides, penicillin, thiouracil, anticonvulsants, and iodides all have been implicated in the initiation of hypersensitivity angiitis. Erythema multiforme is a relatively mild vasculitic skin disorder that may be secondary to drug hypersensitivity. Stevens-Johnson syndrome is probably a more severe form of this hypersensitivity reaction and consists of erythema multiforme, arthritis, nephritis, central nervous system abnormalities, and myocarditis. Administration of nonhuman monoclonal or polyclonal antibodies such as rattlesnake antivenom may cause serum sickness. Like other drug hypersensitivities, the drug may chemically react with host tissue to create a new antigen. Upon first exposure to the allergen (drug), antigen-presenting cells stimulate a T-cell response specific for that allergen. Upon second and all subsequent exposures, tissue-derived antigen-presenting cells that come in contact with the new antigen (allergen-modified host protein) secrete chemokines and cytokines that attract memory T cells to the site of allergen re-exposure. Lymphocytes and antigen-presenting cells such as macrophages accumulate at the site, causing induration, erythema, and swelling. Immunosuppressive Agents Capron A et al: Intra-cellular immunosuppressive drug monitoring: A step forward towards better therapeutic efficacy after organ transplantation Wolf M et al: Peripheral administration of antithymocyte globulins: A review of current literature. Rheumatology 2016;55:775 Cantini F et al: Tailored first-line biologic therapy in patient with rheumatoid arthritis, spondyloarthritis, and psoriatic arthritis. Macy E: Practical management of patients with a history of immediate hypersensitivity to common non-beta-lactam drugs. Immunodeficiency Diseases Sriaroon P, Ballow M: Immunoglobulin replacement therapy for primary immunodeficiency. Acute graft-vs-host disease is the process of donor T cells attacking host recipient tissues (including skin), despite ongoing immunosuppressive therapy such as tacrolimus. She is comatose, tachypneic (25 breaths per minute), and tachycardic (150 bpm), but she appears flushed, and fingertip pulse oximetry is normal (97%) breathing room air. Questioning of her parents reveals that they are homeless and have been living in their car (a small van). The nights have been cold, and they have used a small charcoal burner to keep warm inside the vehicle. The occupational-environmental toxicologist is primarily concerned with adverse effects in humans resulting from exposure to chemicals encountered at work or in the general environment. In clinical practice, the occupational-environmental toxicologist must identify and treat the adverse health effects of these * the author thanks the late Gabriel L. In addition, the trained occupational-environmental toxicologist will be called upon to assess and identify hazards associated with chemicals used in the workplace or introduced into the human environment. Occupational and environmental toxicology cases present unusually complex problems. Occupational and environmental exposure is rarely limited to a single type of molecule. Most workplace or environmental materials are compounds or mixtures, and the ingredients are often poorly described in the documentation that is available for physician review. Because many of these illnesses have long latency periods before they become manifest, it is often a matter of detective work, when patients finally present with disease, to ascertain past exposure and relate it to present clinical effect. Monitoring of exposure concentrations both in the workplace and in the general environment has become more common, but it is far from widespread, and so it is often very difficult to establish the extent of exposure, its duration, and its dose rate when this information is critical to the identification of the toxic disorder and its management.
Order discount trimethoprim line
Calcium hydroxylapatite (Radiesse) for correction of the midand lower face: Consensus recommendations antibiotics for sinus infection not helping trimethoprim 960mg line. Advances in facial rejuvenation: Botulinum toxin type A, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Treatment of forehead/glabellar rhytide complex with combination botulinum toxin A and hyaluronic acid versus botulinum toxin A injection alone: A split-face, rater-blinded, randomized control trial. Advances in facial rejuvenation: Botulinum toxin type a, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxina and hyaluronic acid dermal fillers (24-mg/mL smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxina and hyaluronic acid dermal fillers (24-mg/mL smooth, cohesive gel) alone and in combination for lower facial rejuvenation: Satisfaction and patient-reported outcomes. New collagen formation after dermal remodeling with an intense pulsed light source. Rejuvenation of photoaged skin: 5 year results with intense pulsed light of the face, neck, and chest. The effect of botulinum toxin type a on full-face intense pulsed light treatment: A randomized, double-blind, split-face study. Current concepts in nonablative radiofrequency rejuvenation of the lower face and neck. Multicenter study of noninvasive radiofrequency for periorbital tissue tightening. Improvement of neck and cheek laxity with a nonablative radiofrequency device: A lifting experience. Monopolar radiofrequency facial tightening: A retrospective analysis of efficacy and safety in over 600 treatments. Results of a survey of 5,700 patient monopolar radiofrequency facial skin tightening treatments: Assessment of a low-energy multiple-pass technique leading to a clinical end point algorithm. Ultrasound tightening of facial and neck skin: A rater-blinded prospective cohort study. Noninvasive lifting of arm, thigh, and knee skin with transcutaneous intense focused ultrasound. The true mandate of the cosmetic physician, however, when dealing with the feminine form, is to strive beyond rejuvenation into the realm of beauty maximization. Contrary to the common requests of patients to eliminate unsightly lines, affecting facial beauty goes far beyond wrinkles and furrows. Creating the best rather than a different version of the patient requires a comprehensive approach to restore lost volume, smooth contours, and enhance facial features naturally2 (see Chapter 7). Although truly the domain of autologous fat and pharmaceutically available "dermal" fillers, botulinum-based neuromodulators can also play a significant role in optimizing beauty by generating ideal proportions. It is therefore incumbent upon injection specialists to have a deep understanding of beauty and the goals necessary to achieve a pleasing result. This article will focus on the artistic use of botulinum toxin to enhance facial beauty beyond the obvious indication of diminishing unsightly wrinkles. True facial beauty arouses the senses to an emotional level of pleasure and evokes in the perceiver a high degree of attraction. Perception of beauty is innate, as borne out by numerous studies confirming that newborn infants prefer attractive faces. Furthermore, in modern day culture there exists a "beauty premium" and a "plainness penalty"- attractive individuals are more likely to be hired, promoted, and to earn higher salaries than unattractive individuals. Is it possible that our brains act like supercomputers, mathematically assessing beauty Our attraction to beauty may in part be hard-wired into our "computer" brains and based on how closely we subconsciously recognize Phi proportions. This may explain why across the world, regardless of their origin, most people seem to have similar subjective ideas of what constitutes an attractive face. Racial variations of skin color and diverse features then provide for an endless spectrum of Phi beauty that is unique for each individual. To paraphrase Hungerford, "beauty may actually reside in the Phi (eye) of the beholder". Injection therapy restores youth by softening aging lines, reestablishing fullness of features, and smoothing contours with gradual transitions. However, creative use of botulinum toxin and fillers will also offer the opportunity to enhance attractiveness by pursuing ideal proportions. Individual ideal facial proportions can be obtained with the aid of a golden mean caliper-a tool for dynamically measuring the Phi ratio. The Beautiful Temple and Botulinum Toxin Aesthetic injectors focusing purely on the presence of unsightly lines and creases often overlook the contribution of forehead and temple contour to overall beauty. An overly concave temple can detract from facial attractiveness, and signify a stigma of advancing age. Similarly, excess convexity in a female temple can portend a masculine look and distort the beautiful facial oval (or heart shape) preferred by most cultures. Facial width from the medial canthus to the ipsilateral cheek prominence should normally not exceed Phi (1. Deposition of botulinum toxin into the temporalis muscle within its fossa can reduce upper facial bulkiness and provide the initial subtle concavity to the gentle S-shaped Ogee curve of the feminine form. The temporalis muscle consists of superficial and deep parts that originate from the temporal bone and fascia in the temporal fossa of the parietal bone. Furthermore, although maximal clench is diminished,17 no detrimental effect on chewing has been observed, as the masseter and pterygoid muscles remain the principle contributors to mastication. As such, the superior portion of the muscle is firmly adherent to the underlying bone and devoid of interposing fascia. The periosteum and deep fascia of the forehead (galea aponeurotica) as they traverse the upper face under the frontalis muscle cannot continue under the temporalis muscle and as such lie over the muscle as the deep and superficial temporal fascia respectively. This anatomical oddity, of a deep fascia lying on the surface of the muscle which bears its name, provides a resistant plane that is appreciably felt when penetrating the region with a needle. Overlying this fascia in the posterior leaves of the superficial temporal fascia are the superficial temporal vessels (arteries and veins) and specifically the frontal ramus of the superficial temporal artery. Located in the depth of the muscle are the anterior and posterior deep temporal arteries (branches of the internal maxillary artery, second division), the middle temporal artery (connecting the deep and superficial arterial system), and the prominent middle temporal vein approximately 2 cm above the zygomatic arch. Prudent technique would require aspiration before injection of toxin into the temporal muscle to minimize the possibility of intravascular washout limiting the clinical result. Post-injection pressure for several minutes, regardless of the appearance of blood through the puncture site, will diminish the possibility of delayed unsightly bruising. The Beautiful Glabella and Botulinum Toxin Subtle differences in glabellar appearance have a profound effect on beauty and youthfulness. Aging skin changes and actinic exposure lead to the appearance of lines, creases, and dyschromias compounded with tissue atrophy and volume loss. This is to be distinguished from an elevated eyebrow resulting from increased frontalis activity as compensation for an upper eyelid partial levator dehiscence. A beautiful glabella is not just about the absence of static or dynamic frown lines. The glabellar complex consists of the interweaving of two superficial gliding muscles, the frontalis (elevator) and the procerus (depressor); and two deep brow depressor muscles, the paired corrugator and depressor supercilii. The glabellar confluence of elevator and depressors is somewhat stratified as the frontalis blends superficially with the deeper depressors. Delineation of each specific muscle within the central glabellar complex is clinically impossible; however, for practical purposes, function is stratified in that the elevator fibers of the frontalis remain sandwiched between the more superficial procerus fibers and the deeper corrugator/depressor fibers. Varying the height and depth of toxin deposition according to the muscle action being targeted can alter the resting position of the medial brow. Phi harmony in the upper face dictates that the medial brows begin in a vertical line above the medial canthii at a height of 0. This technique is indicated when medial eyebrow position is too high and superior medial orbital hollowing is present to accommodate the potentially redundant skin that may occur as a result of treatment.
Cheap 960mg trimethoprim mastercard
Adverse effects include nausea iv antibiotics for sinus infection buy trimethoprim 480 mg, diarrhea, stomatitis, and peripheral neuropathy with prolonged use. Metronidazole has a disulfiram-like effect, and patients should be instructed to avoid alcohol. Although teratogenic in some animals, metronidazole has not been associated with this effect in humans. A structurally similar agent, tinidazole, is a once-daily drug approved for treatment of trichomonas infection, giardiasis, amebiasis, and bacterial vaginosis. When administered orally, systemic absorption is negligible but fecal concentrations are high. It is as effective as oral vancomycin and may be associated with lower rates of relapsing disease. Strains with high-level resistance have caused hospitalassociated outbreaks of staphylococcal infection and colonization. Although higher rates of resistance are encountered with extensive use of mupirocin, most staphylococcal isolates are still susceptible. Mupirocin is indicated for topical treatment of minor skin infections, such as impetigo (see Chapter 61). Topical application over large open areas, such as pressure ulcers or surgical wounds, is an important factor leading to emergence of mupirocin-resistant strains and is not recommended. Mupirocin temporarily eliminates S aureus nasal carriage by patients or health care workers, but results are mixed with respect to its ability to prevent subsequent staphylococcal infection. Patients most likely to benefit from decolonization are those undergoing orthopedic or cardiothoracic procedures. Owing to their significant toxicity with systemic administration (especially nephrotoxicity), polymyxins were, until recently, largely restricted to topical use. Ointments containing polymyxin B, 5000 units/g, in mixtures with bacitracin or neomycin (or both) are commonly applied to infected superficial skin lesions. Emergence of strains of Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacteriaceae that are resistant to all other agents has renewed interest in polymyxins as parenteral agents for salvage therapy of infections caused by these organisms. Typical doses of rifaximin range from 200 mg to 550 mg administered orally twice to three times daily depending on the indication. Unlike other rifamycins, rifaximin is not thought to be associated with cytochrome-P450-mediated drug interactions due to its limited absorption. Mupirocin is active against Gram-positive cocci, including methicillin-susceptible and methicillin-resistant strains of Nitrofurantoin At therapeutic doses, nitrofurantoin is bactericidal for many Gram-positive and Gram-negative bacteria; however, P aeruginosa and many strains of Proteus are inherently resistant. Antibacterial activity appears to correlate with rapid intracellular conversion of nitrofurantoin to highly reactive intermediates by bacterial reductases. It is not known which of the multiple actions of nitrofurantoin is primarily responsible for its bactericidal activity. There is no cross-resistance between nitrofurantoin and other antimicrobial agents, and resistance emerges slowly. As resistance to trimethoprim-sulfamethoxazole and fluoroquinolones has become more common in Escherichia coli, nitrofurantoin has become an important alternative oral agent for treatment of uncomplicated urinary tract infection. It is metabolized and excreted so rapidly that no systemic antibacterial action is achieved. The drug is excreted into the urine by both glomerular filtration and tubular secretion. In renal failure, urine levels are insufficient for antibacterial action, but high blood levels may cause toxicity. Nitrofurantoin is contraindicated in patients with significant renal insufficiency. Traditional recommendations are to avoid use in patients with creatinine clearance <60 mL/min; however, some data suggest short-term nitrofurantoin treatment is acceptable in patients with creatinine clearance >30 mL/min. The dosage for urinary tract infection in adults is 100 mg orally taken four times daily. Macrocrystalline nitrofurantoin, which has slower dissolution and absorption than nitrofurantoin monohydrate, constitutes 25%. The remaining 75% is nitrofurantoin monohydrate contained in a powder blend, which, upon exposure to gastric and intestinal fluids, forms a gel matrix that releases nitrofurantoin over time. A single daily dose of nitrofurantoin, 100 mg, can prevent recurrent urinary tract infections in some women. Neuropathies and pulmonary toxicities may occur, particularly with prolonged use or in patients with renal impairment. Hemolytic anemia can occur in patients with glucose-6-phosphate dehydrogenase deficiency. Rashes, pulmonary infiltration and fibrosis, and other hypersensitivity reactions have been reported. Methenamine mandelate, 1 g four times daily, or methenamine hippurate, 1 g twice daily by mouth (in children age 6 to 12 years, 500 mg four times daily or twice daily, respectively), is used only as a urinary antiseptic to prevent, not treat, symptomatic urinary tract infection. Sulfonamides should not be given at the same time because they may form an insoluble compound with the formaldehyde released by methenamine. Persons taking methenamine mandelate may exhibit falsely elevated tests for catecholamine metabolites. Antiseptics are disinfecting chemical agents with sufficiently low toxicity for host cells that they can be used directly on skin, mucous membranes, or wounds. Sterilants kill both vegetative cells and spores when applied to materials for appropriate times and temperatures. Disinfection prevents infection by reducing the number of potentially infective organisms by killing, removing, or diluting them. Often a combination of agents is used, eg, water and moderate heat over time (pasteurization); ethylene oxide and moist heat (a sterilant); or addition of disinfectant to a detergent. Prevention of infection also can be achieved by washing, which dilutes the potentially infectious organism. Hand hygiene is probably the most important means of preventing transmission of infectious agents from person to person or from regions of high microbial load, eg, mouth, nose, or gut, to potential sites of infection. Evaluation of effectiveness of antiseptics, disinfectants, and sterilants, although seemingly simple in principle, is very complex. Factors in any evaluation include the intrinsic resistance of the microorganism, the number of microorganisms present, mixed populations of organisms, amount of organic material present (eg, blood, feces, tissue), concentration and stability of disinfectant or sterilant, time and temperature of exposure, pH, and hydration and binding of the agent to surfaces. Users of antiseptics, disinfectants, and sterilants need to consider their short-term and long-term toxicity because they may have general biocidal activity and may accumulate in the Methenamine Mandelate & Methenamine Hippurate Methenamine mandelate is the salt of mandelic acid and methenamine and possesses properties of both of these urinary antiseptics. Oral mandelic acid or hippuric acid is absorbed and excreted unchanged in the urine. Disinfectants and antiseptics may also become contaminated by resistant microorganisms-eg, spores, P aeruginosa, or Serratia marcescens-and actually transmit infection. Cleansing of wounds with soap and water may be less damaging than the application of antiseptics. Some of the chemical classes of antiseptics, disinfectants, and sterilants are described briefly in the text that follows. The reader is referred to the general references for descriptions of physical disinfection and sterilization methods. They are not used as sterilants because they are not sporicidal, do not penetrate protein-containing organic material, and may not be active against hydrophilic viruses. Their skin-drying effect can be alleviated by addition of emollients to the formulation. Alcohol-based hand rubs are ineffective against spores of C difficile, and handwashing with soap and water is required for decontamination after caring for a patient with infection from this organism. They must be allowed to evaporate before cautery, electrosurgery, or laser surgery. Therefore, instruments such as tonometers that have been disinfected in alcohol should be rinsed with sterile water, or the alcohol should be allowed to evaporate before they are used. Water-soluble chlorhexidine digluconate is used in waterbased formulations as an antiseptic. It is active against vegetative bacteria and mycobacteria and has variable activity against fungi and viruses.
Discount trimethoprim online amex
Properties and use of botulinum toxin and other microbial neurotoxins in medicine antibiotics loss of taste discount 480mg trimethoprim free shipping. A randomized pilot study comparing the action halos of two commercial preparations of botulinum toxin type A. Assay of diffusion of different botulinum neurotoxin type a formulations injected in the mouse leg. Impact of postreconstitution room temperature storage on the efficacy of incobotulinumtoxinA treatment of dynamic lateral canthus lines. Sensitive and quantitative detection of botulinum neurotoxin in neurons derived from mouse embryonic stem cells. Novel application of human neurons derived from induced pluripotent stem cells for highly sensitive botulinum neurotoxin detection. Botulinum toxin type A treatment to the upper face: Retrospective analysis of daily practice. A prospective, split-face, randomized, double-blind study comparing onabotulinumtoxinA to 12. Botulinum toxin type A and other botulinum toxin serotypes: A comparative review of biochemical and pharmacological actions. Neurotoxin gene clusters in Clostridium botulinum type A strains: Sequence comparison and evolutionary implications. Biochemical, functional and potency characteristics of type A botulinum toxin in clinical use. Subunit stoichiometry of the Clostridium botulinum type A neurotoxin complex determined using denaturing capillary electrophoresis. Content of botulinum neurotoxin in Botox/Vistabel, Dysport/Azzalure, and Xeomin/Bocouture. Using translational medicine to understand clinical differences between botulinum toxin formulations. Biophysical characterization of the stability of the 150-kilodalton botulinum toxin, the nontoxic component, and the 900-kilodalton botulinum toxin complex species. Molecular basis for disruption of E-cadherin adhesion by botulinum neurotoxin A complex. A new botulinum toxin type A free of complexing proteins for treatment of cervical dystonia. Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. Noninferiority of incobotulinumtoxinA, free from complexing proteins, compared 34. Onset and duration of effect of incobotulinumtoxinA, onabotulinumtoxinA, and abobotulinumtoxinA in the treatment of glabellar frown lines: A randomized, double-blind study. Clinical equivalence of conventional OnabotulinumtoxinA (900 kD) and IncobotulinumtoxinA (neurotoxin free from complexing proteins-150 kD): 2012 multidisciplinary French consensus in aesthetics. Consensus recommendations on the aesthetic usage of botulinum toxin type A in Asians. IncobotulinumtoxinA in aesthetics: Russian multidisciplinary expert consensus recommendations. Conversion ratio between Dysport and Botox in clinical practice: An overview of available evidence. Full profile of the continuous antigenic regions of the H-chain of botulinum neurotoxin A. Localization of the sites and characterization of the mechanisms by which anti-light chain antibodies neutralize the actions of the botulinum holotoxin. Comparison of efficacy and immunogenicity of original versus current botulinum toxin in cervical dystonia. Antibody-induced failure of botulinum toxin type A therapy in a patient with masseteric hypertrophy. Antibody-induced secondary treatment failure in a patient treated with botulinum toxin type A for glabellar frown lines. Neutralizing antibodies to botulinum neurotoxin type A in aesthetic medicine: Five case reports. Clinical resistance to three types of botulinum toxin type A in aesthetic medicine. Botulinum A toxin therapy: Neutralizing and nonneutralizing antibodies-therapeutic consequences. Type A botulinum neurotoxin complex proteins differentially modulate host response of neuronal cells. Comparative antigenicity of three preparations on botulinum neurotoxin A in the rabbit. Immunological characterization of the subunits of type A botulinum neurotoxin and different components of its associated proteins. New formulation of Botox: Complete antibody-induced treatment failure in cervical dystonia. Neutralizing antibodies in dystonic patients who still respond well to botulinum toxin type A. Neutralizing antibodies and secondary therapy failure after treatment with botulinum toxin type A: Much ado about nothing Formation of neutralizing antibodies in patients receiving botulinum toxin type A for treatment of poststroke spasticity: A pooled-data analysis of three clinical trials. Prevalence of neutralising antibodies in patients treated with botulinum toxin type A for spasticity. Very early reduction in efficacy of botulinum toxin therapy for cervical dystonia in patients with subsequent secondary treatment failure: A retrospective analysis. IncobotulinumtoxinA (Xeomin) can produce antibody-induced therapy failure in a patient pretreated with abobotulinumtoxinA (Dysport). Clinical presentation and management of antibodyinduced failure of botulinum toxin therapy. Five-year experience with incobotulinumtoxinA (Xeomin): the first botulinum toxin drug free of complexing proteins. Prospective analysis of neutralising antibody titres in secondary non-responders under continuous treatment with a botulinumtoxin type A preparation free of complexing proteins-a single cohort 4-year follow-up study. All of these agents are administered by injection and therefore have the potential to cause needle anxiety and injection site reactions such as erythema, bruising, discomfort, tenderness, pain, and infection. The ionic charge imparted to the target molecule allows the drug to be driven into the skin as indifferent ions are pulled from the skin by the indifferent electrode to complete the circuit. However, few molecules are amenable to being delivered by iontophoresis, especially lipophilic molecules. Although it has been reported to be successful with botulinum toxin, 5,6 iontophoretic delivery lacks targeting and delivery specificity, is often painful, and is heavily influenced by time and by drug concentration. As a result, many macromolecules (including insulin, antibodies, and growth hormone) still need to be administered by injection. The stratum corneum and upper layers of the epidermis are essentially a multilayered arrangement of the mature and differentiated horny cells of the epidermis that are interwoven with a lipid matrix that itself has a lamellar structure. Passage through the stratum corneum is less likely to be successful for highly ionic and/or aqueous molecules than lipophilic molecules, and it is also less efficient for larger molecules than smaller molecules. Furthermore, the process is heavily influenced by time and by the concentration of the relevant molecule. Most attempts to enhance transepidermal delivery by manipulating drug structure have been rudimentary from a biochemical standpoint-because, for example, conjugating a drug to a carrier can compromise its activity and permeation enhancers may disrupt protein linkages and tertiary structures vital to the biological activity of a protein. Iontophoresis has also been explored as an alternative mechanism for drug delivery. The toxin forms a complex with the peptides, with the protein transduction domains directed outward where they are free to attach to cell surfaces. The peptide-covered toxin is absorbed through cell membranes, crosses the cytoplasm to the cell membrane on the other side, and passes out and into the next cell. This is an active energy transport system and is not specific to botulinum toxin-it is a variant of induced macropinocytosis where the cell takes a "drink" of the surrounding media and conveys it out to the other side without harming the cell or the cell membrane. Once the complex has traversed the cell, it moves through the next cell, and the next, until it exits the epidermis on the dermal side. An additional important clinical finding was that, even though noninvasive treatments do not generally provide sufficient efficacy to treat severe hyperhidrosis, subjects with profound hyperhidrosis at baseline experienced an excellent reduction in sweating. Adverse events were generally mild, localized, and transient, with the most common treatment-related adverse events being erythema or pain at the application site and folliculitis. Treatment-emergent adverse events were generally mild and transient and none of the studies revealed any safety signals of clinical relevance.