Generic valacyclovir 500mg on-line
Anticonvulsant therapy Magnesium sulphate can be used to control an eclamptic fit (up to 8 g) hiv infection symptoms after one year purchase valacyclovir overnight. An eclamptic fit is usually self-limiting, and prolonged fitting warrants a brain scan to rule out other pathology, such as an intracerebral bleed [E]. If an eclamptic fit occurs, magnesium sulphate is the prophylaxis of choice, as demonstrated by the Eclampsia Trial [B]. Magnesium sulphate acts as a membrane stabilizer and vasodilator and reduces intracerebral ischaemia. In cases of oliguria, care must be taken, as magnesium sulphate is renally excreted. Toxicity is detected by the absence of patellar reflexes, but ultimately respiratory arrest and muscle paralysis or cardiac arrest will occur. However, the Magpie Trial evaluated magnesium sulphate versus placebo in women with pre-eclampsia and demonstrated a clear benefit of prophylactic therapy [A]. Magnesium sulphate halved the risk of eclampsia and probably reduced the risk of maternal death. There did not appear to be any substantive harmful short-term effects to either the mother or baby. It is plausible that active assessment of cardiovascular risk up to six months postpartum may lead to earlier identification of cardiovascular risk and the potential for lifestyle modification. Both maternal and fetal morbidity and mortality are more likely to occur with early-onset disease. Despite the many tests being investigated, pre-eclampsia cannot be accurately predicted. An abnormal uterine artery Doppler at 20 weeks will increase risk approximately six-fold in both high- and low-risk women. Cerebral haemorrhage and adult respiratory distress are common causes of death in pre-eclampsia; therefore acute management focuses on controlling blood pressure and restricting fluid intake. The use of anti-hypertensive therapy in moderately hypertensive women demonstrates a significant reduction in severe hypertension only; there are no other proven additional benefits. Low-dose aspirin in pregnancy results in a small (10 per cent), but significant reduction in pre-eclampsia; there is an associated reduction in preterm delivery. Magnesium sulphate is the anticonvulsant of choice following an eclamptic fit, resulting in fewer fits and less maternal morbidity compared to diazepam and phenytoin. Can 24-hour ambulatory blood pressure measurement predict the development of hypertension in primigravidae Assessment of uterine arterial notching as a screening test for adverse pregnancy outcome. Antiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient data. Antenatal complications: maternal Chapter 8 Medication in pregnancy Clare L Tower prescription of high-dose folic acid groups at particular risk. Second, it allows drugs with potentially terotogenic effects to be changed to a safer alternative. Furthermore, it allows the opportunity to discuss particular risks and concerns, of both the medical problem itself and the medications that will be prescribed during pregnancy. Thus, women may suddenly stop drugs in early pregnancy that may have a significant impact on their own health. Discussions in the pre-conception period will prevent such non-compliance in early pregnancy of important medications, such as antiepileptics or immunosuppressants. Candidates would be expected to have a good understanding of the prescribing principles used when treating pregnant women, maternal and fetal side effects, and drug exposure to infants during breastfeeding. Many pregnant women require medication for specific pregnancy and non-pregnancy related conditions. Therefore, a broad understanding of the impact of pregnancy on drug pharmacokinetics (drug handling) and pharmacodynamics (drug actions) is required. Furthermore, the large majority of drugs cross the placenta, and some drugs have significant fetal effects. For this reason, most drugs are not licensed for use in pregnancy, thus prescribing in pregnancy often lies outside licensed indications. A detailed discussion of prescribing for particular disorders during pregnancy can be found in the relevant sections of this book. However, studies have demonstrated that pregnancy has no measurable affect on drug bioavailability via these mechanisms. It is beneficial for many of these women to be seen pre-conceptually for several reasons. First, it allows optimization of therapy such that pregnancy can be commenced with the lowest achievable risks. Typical examples of this include optimization of glycaemic control in diabetic women and the the volume of distribution is defined as the volume in which an amount of drug would need to be distributed to produce a particular blood concentration. Therefore, for drugs which are highly bound in the tissues, such as basic drugs like amphetamine, the volume of distribution is large, but the plasma concentration is low. For acidic drugs, such as warfarin, which are highly protein bound, the volume of distribution is relatively low, but the plasma concentration high. Therefore, the volume of distribution is dependent upon plasma volume, tissue volume, the amount of binding of a drug in the tissues and to plasma proteins. Pregnancy Effects of pregnancy on pharmacokinetics and pharmacodynamics 193 causes an increase in plasma volume that reaches a peak at around 32 weeks gestation. Therefore, pregnancy results in an increase in volume of distribution (due to increased plasma volume) and an increase in the fraction of a drug that is unbound, or active, in the plasma (due to a fall in plasma proteins). Thus, measurements of total drug concentration, which are used for medications such as phenytoin and sodium valproate, underestimate the corresponding unbound or active concentrations. This may result in prescribing higher doses than necessary, which is particularly important as the teratogenicity of both these drugs is reported in registries to be dose dependent [D]. Although the liver smooth endoplasmic reticulum is the main site of enzymatic metabolism, virtually all cells have the ability to metabolize drugs to some degree, with other main sites being the epithelial cells of the gut, kidney, lung and skin. Not only does pregnancy alter the activity of these enzymes, but it also varies with gestation, drug interactions (for examples, enzyme inducers) and genotype. Enzymes demonstrating increased activity will result in reduced plasma levels of a drug, requiring an increase in dose and vice versa. Thus, variation of drug metabolism with pregnancy is complex, and although the majority of enzymes increase in activity, some decrease. The overall effect is further compounded by genetic variation and the effect of plasma volume and plasma proteins described above. This should be considered when prescribing in pregnancy, and since there are so many unknown factors, clinicians must be guided by the overall clinical effect of a drug. Renal clearance Pregnancy causes an increase in renal blood flow and glomerular filtration rate of more than 50 per cent, which can have a significant effect on drugs that are predominantly excreted by the kidneys. Thus, the clearance of betalactam antibiotics, such as penicillins and cephalosporins, is increased during pregnancy [C]. Although there may be lower plasma levels as a result, levels in urine may be higher, which may be a desired effect for treating urinary tract infections. Low molecular weight heparins, such as dalteparin and enoxaparin, also demonstrate increased renal clearance during pregnancy, which may require dose adjustments [C]. Transfer of drugs across the placenta can occur by passive transfer, active transport, facilitated diffusion, phagocytosis and pinocytosis. Therefore, small, un-ionized lipid-soluble drugs Antenatal complications: maternal 194 Medication in pregnancy are able to cross at the fastest rate. This can be influenced by the degree of plasma protein binding and by placental metabolism. Drugs with a molecular weight <500 Da, which is the large majority, are able to cross the placenta by passive diffusion. Heparin (both unfractionated and low molecular weight) is the most well-known drug that is unable to cross the placenta due to its high molecular weight of between 3000 and 5000 Da, depending on the preparation.
Diseases
- Thies Reis syndrome
- Pacman dysplasia
- Cardioskeletal myopathy-neutropenia
- Neurofibroma
- Gorlin Chaudhry Moss syndrome
- Torsades de pointes
- Chromosome Chromosome 1
- Hemangioblastoma
Buy generic valacyclovir on-line
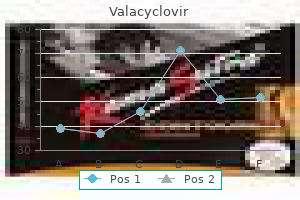
Although the mass appears circumscribed on the routine views (A antivirus scan generic 500 mg valacyclovir,C), the spot compression image (E) demonstrates that the mass has ill-defined margins. Although the margins are generally well defined, there is mild irregularity of the contour of the mass (arrowheads). There is a large partially enhancing solid mass in the left neck, which extends to the clavicle. Mammographically, these masses are superficial, circumscribed, oval or lobulated masses. Case report: squamous cell carcinoma of the skin metastasizing to the breast-imaging findings. Besides papillary carcinoma, the papillary subtype of ductal carcinoma in situ has been reported to present as a complex cystic mass. There is increased density associated with the posterior deep margin of the right implant (arrows). Subglandular implants generally obscure more breast parenchyma than subpectoral implants. To improve visualization of the parenchyma, Eklund or implant-displaced views should be routinely done in patients with implants. Although we always perform implant-displaced views, these views are not shown in this book unless they provide specific information for the case. This sequence is excellent for identifying free silicone due to extracapsular rupture. If water saturation is added to the T2 sequence, then silicone will be brighter than water. The silicone is easily identified either as free silicone or between the layers of the fibrous capsule and the shell of the prosthesis. Unfortunately, silicone injections resulted in painful hardening of the breast, sloughing of skin, granulomatous hepatitis, and pulmonary embolism. The superior edge of the implant demonstrates a contour deformity that corresponds to the mammographic abnormality. Both contour deformities and implant folds are normal findings of an intact implant. Herniation is when an intact implant shell is extruded through the fibrous capsule. Capsular herniation is distinguished from a contour bulge by identifying bunching of the implant at the location of the ruptured capsule. Screening mammography in 350 women with breast implants: prevalence and findings of implant complications. The implant (I) wall is intact, but there is a thin fluid collection (F) outside the implant. About 20% of all types of implants demonstrate at least a small amount of calcification. In a few cases, heavy calcification has been associated with severe capsular contracture, which has been labeled the Krakatau syndrome. This syndrome is named after the famous volcano in Indonesia because when this abnormal implant is removed, the breast exhibits a craterlike depression. The Krakatau syndrome; a late complication of retroglandular mammary augmentation. The elastomer shell is a semiporous membrane that allows silicone to flow into the surrounding tissues without rupture of the shell. The most common migration of free silicone is to the upper outer or upper medial soft tissues. Rarely, silicone will migrate to the breast or axilla from a distal injection site, such as the arm. Unilateral axillary adenopathy secondary to a silicone wrist implant: report of a case detected at screening mammography. There are oval densities with calcifications in the areas of the previous implants. Usually the fibrous capsule surrounding the implants is removed with the implants. After partial mastectomy for breast cancer, the woman noticed that her left breast is larger than her right, and there is a new thickening in the lumpectomy site. The breast sonogram was performed before the mammograms to investigate the palpable abnormality in the lumpectomy scar. The palpable thickening corresponds sonographically to a deformed, collapsed implant. Intracapsular failure involves rupture of the implant elastomer shell without rupture of the surrounding fibrous capsule. With intracapsular rupture, the liquid contents of the implant are contained within the fibrous capsule. Extracapsular failure is when both the implant elastomer shell and the fibrous capsule have been ruptured. As a result of this type of rupture, the internal contents of the implant (silicone or water) are extruded outside the capsule into the surrounding tissues. The advantages of saline are that they have a lower reported incidence of contracture and that leakage from the implant is undesirable but harmless. One article reviewing the literature found that mammography has a sensitivity of 28. The life span of silicone gel breast implants and a comparison of mammography, ultrasonography, and magnetic resonance imaging in detecting implant rupture: a meta-analysis. Radiographic diagnosis of breast implant rupture: current status and comparison of techniques. The right implant is filled with hypoechoic fluid and exhibits multiple echogenic lines within it. The hypoechoic band (R) next to the implant shell (arrows) is acoustic reverberation artifact. A review of over 1000 silicone gel implants found that the median life span for those implants was 16. The most reliable sign of rupture is identification of multiple horizontal, straight, or curvilinear lines ("stepladder" sign) within the silicone gel. Another important sonographic sign of rupture is the presence of "echodense noise" (snowstorm appearance), which indicates free silicone. This image illustrates mild collapse of the implant shell with silicone on both sides of the collapsing walls. Two mild or indirect signs of intracapsular rupture are the "keyhole" sign (arrow) and the "noose" sign (arrowhead). This image demonstrates more small areas (arrows) where the implant shell has separated from the fibrous capsule.
Buy discount valacyclovir 1000 mg on line
These factors interact to cause descent of the presenting part antivirus software for mac cheap valacyclovir 500 mg without prescription, and expulsion of the fetus. Through the use of oxytocin, the frequency, intensity and duration of the contractions can be augmented. However, there are limits to the maximum effect that may be achieved, especially when the potential for inducing iatrogenic fetal compromise is taken into consideration. There is also little evidence to show that the outcome of labour, in terms of successful vaginal delivery, can be improved when the uterine activity is normal. There are groups of women who are more likely to have a dysfunctional labour than others, for example the obese, those of advanced maternal age, those with diabetes, multiple pregnancy, etc. While the mechanisms underlying the alterations in normal physiology is not yet fully understood within each of these groups, changes in myometrial activity, dysfunction of the gap junctions between cells and changes in the interaction between fetal and maternal factors undoubtedly play an important role. During this period, women may experience painful contractions and need a great deal of support. However, it is important that unnecessary interventions to accelerate labour are not implemented at this point, as clinical studies have demonstrated that oxytocin augmentation during this phase does not result in an increase in the vaginal delivery rate, but rather a 10-fold increase in the incidence of caesarean delivery and a 3-fold increase in low Apgar scores [B]. In place of active intervention, careful explanation and the provision of adequate analgesia may be all that is required before the cervical changes complete and the active phase of labour is entered. Any decision to augment in the latent phase should be based on medical or obstetric indications. In such an event, management along the lines consistent with an induction of labour may be the most appropriate, although the risks of uterine hyperstimulation may be increased. This affects up to 26 per cent of nulliparae and 8 per cent of multiparae and, whereas no single aetiology is responsible for all cases, 70 per cent of nulliparae and 80 per cent of multiparae will respond to oxytocin. This observation suggests that poor/inco-ordinate uterine activity is a significant factor, although an improvement in the rate of cervical dilatation does not necessarily correlate with an improved outcome in terms of vaginal delivery. Primary dysfunctional labour may culminate in an obstructed labour and is associated with higher rates of maternal infection, uterine rupture and postpartum haemorrhage [C]. Prolonged latent phase During the latent phase, changes occur in the ground substance glycoprotein, collagen content and hydration state of the cervix, which result in the remodelling and effacement that may be observed during this period. Friedman described the latent phase as lasting up to 20 hours in nulliparae (median 8. It is important to note that in up to 40 per cent of women, progress will improve by simply improving maternal hydration; the provision of one-to-one care or a professional maternal companion if this is not already provided; 368 Poor progress in labour a longer period of time to allow labour to progress; mobilization; augmentation with oxytocin; delivery by caesarean section. Secondary arrest Secondary arrest affects approximately 6 per cent of nulliparae and 2 per cent of multiparae, and may be defined as a cessation of cervical dilatation following a normal period of active-phase dilatation. It should also be acknowledged that, up to the stage of arrest, the uterine activity has been sufficient to produce a normal response in terms of cervical effacement and dilatation. Nevertheless, in one series of patients with secondary arrest, 60 per cent of nulliparae and 70 per cent of multiparae demonstrated an improvement in progress with oxytocin. However, the caesarean section rate was ten times greater in the treatment arm than in the uncomplicated cohort. Cephalo-pelvic disproportion cannot usually be properly diagnosed until the latter stages of labour, and it is in these cases that particular care must be taken. Secondary arrest in the second stage of labour the second stage of labour is the period from full cervical dilatation to delivery of the fetus, and is a continuum in the process of labour and not a static phase. It may also be divided into pelvic and perineal stages, representing the differences between full dilatation with the head high and the overwhelming sensation a patient feels when the presenting part is deep in the pelvis and exerting pressure on the rectum. The second stage may also lengthen when an epidural is present, an effect contributed to by relaxation of the pelvic floor and failure of the Ferguson reflex. As long as the fetal condition remains satisfactory, in the nullipara, an oxytocin infusion in combination with the provision of additional time for the co-ordination of maternal efforts with uterine activity can reduce the incidence of instrumental vaginal deliveries. Pain relief and its effects on labour are discussed in Chapter 30, Obstetric anaesthesia. It is important that before augmentation is considered, pain relief is discussed with the patient. Although there is a transient reduction in contraction frequency after epidural analgesia is commenced, this usually resolves spontaneously and with careful management should not impact on the first stage of labour [A]. It is important to recognize that although epidural analgesia is associated with an increase in the rate of instrumental vaginal delivery, there is no evidence of an increased risk of delivery by caesarean section [A]. Secondary arrest in the decelerative phase Friedman observed that delay during the decelerative phase on a partogram, between cervical dilatations of 7 and 10 cm, was associated with an increased risk of failure to respond to oxytocin augmentation and difficulty in procuring a successful instrumental vaginal delivery. The provision of one-to-one care One-to-one care is the single most effective intervention to improve outcomes, both maternal and fetal, in labour. The carer does not have to be a midwife, but should not Variable decelerations and a rising baseline are common in obstructed labour. Where fetal scalp sampling reveals a When to augment labour 369 be the husband/partner (although of course his/her presence may be welcomed). Continuous support is also associated with a slight reduction in the overall length of labour [A]. Although in the mobile epidural group, women were encouraged to walk, there was no difference in the length of labour, need for augmentation or type of delivery between the two groups [B]. Amniotomy Amniotomy has traditionally been practised to shorten the length of labour. Meta-analysis of the trials incorporating routine early amniotomy into the management of spontaneous labour shows that amniotomy is not associated with statistically significant reduction in duration of the first stage in nulliparous or multiparous women. Given that the reduction in length of labour is not large and not significant and that there is a potential for increase in the need for caesarean section, it has been suggested that amniotomy should be reserved for women with abnormal progress in labour. Despite widespread use in clinical practice, there is a huge paucity of evidence to demonstrate that the use of oxytocin to augment labour improves either the maternal or fetal outcomes. This is in part due to ethical committees not giving permission for a placebo arm, or poor trial recruitment in the presence of a placebo arm. Although this trial did show that mothers randomized to oxytocin had higher satisfaction scores than those in the control arm, the numbers were too small to draw decisive conclusions. However, early intervention was noted to shorten labour considerably with a trend towards a reduction in the number of operative vaginal deliveries required. Augmentation of labour in multiparae is one of the greatest contributing factors to uterine rupture. It is reasonable not to augment and to allow labour to continue at a slower rate, but in all cases all other factors, such as maternal support and hydration, must be optimized. This vague definition reflects the wide variations in clinical practice currently in operation. Inefficient uterine activity is a failure of the uterus to function in a way that results in normal progression of labour. Inco-ordinate uterine activity does not need to be specifically addressed if progress in labour is normal. However, it will not be appropriate to leave all women this long, and decisions must be taken in the context of full clinical assessment. Between 8 per cent of multiparae and 22 per cent of nulliparae will fail to respond to oxytocin and require delivery by caesarean section, although the majority of patients will deliver vaginally within this time with few risks of intrapartum injury [C]. It is important to recognize that as fetal compromise may result from augmentation of the forces, continuous monitoring of the fetus should be employed. The Royal College of Obstetricians and Gynaecologists audit standards suggest that caesarean section should not be performed for poor progress in nulliparae before a trial of oxytocin. However, it should be realized that this recommendation is not based on any evidence from randomized trials and situations exist in which this advice should not be followed. Once commenced, oxytocin should be titrated to provide a contraction frequency of four or five in 10 minutes, with each contraction lasting approximately 40 seconds. Such a regimen has been shown to be compatible with normal progress in labour (>1 cm/hour) with minimal adverse sequelae, as long as the appropriate action is taken if signs of maternal or fetal compromise develop. The frequency and duration of contractions may be assessed by either internal or external tocography; uterine tone and quantification of uterine activity can only be measured by internal tocography. Advocates of intrauterine pressure monitoring claim that uterine hyperstimulation can be identified earlier and, in patients with a previous caesarean section scar, that dehiscence can be diagnosed more promptly with a consequent improvement in neonatal outcome. However, a prospective randomized study failed to show an improvement in the obstetric outcome when an intrauterine pressure catheter was employed in an augmented labour when compared with an external tocograph [B]. They observed that an oxytocin infusion in conjunction with a strict diagnosis of labour, early amniotomy and oneto-one care resulted in a marked reduction in the rate of interventional deliveries. The Dublin team made every effort to ensure that it is understood that this strategy was not applicable to multiparae, though this message is often forgotten in other units. Active management is a package encompassing antenatal classes, one-to-one care, a strict diagnosis of labour, early amniotomy and oxytocin for slow progress and frequent vaginal assessment. The low rates of caesarean section achieved in Dublin has not been matched in other units.
Buy generic valacyclovir online
Finally antiviral y retroviral generic 1000 mg valacyclovir with visa, if palpating the quadrant is not helpful, palpating the comparable area in the opposite breast is helpful. Commonly, the parenchymal pattern of patients is symmetric, so the physical exam is also symmetric. Sonographic Technique and Cross-Correlation with Mammography corresponding contralateral quadrant, you can detect abnormal asymmetries. This technique is particularly useful with malignancies that are commonly difficult to feel, such as lobular carcinoma. There are several problems with using external anatomical landmarks for locating mammographic abnormalities: (1) mammographic estimation of location is not accurate and may be difficult to determine if the abnormality is only on one view, (2) the change in patient position between the mammogram and the ultrasound commonly results in changes in the relative position of internal breast structures compared with external landmarks, and (3) the external breast position of a handheld transducer does not correlate with a specific internal imaging position. Estimating location on a mammogram is commonly inaccurate, as the standard mammographic views are the craniocaudal (horizontal) and mediolateral oblique views. The greatest source of error is related to the mediolateral oblique view because this view is not oriented 90 degrees to the craniocaudal view. Even if the location of a lesion is accurately identified by the mammogram, its relative position may change when the patient changes position for the ultrasound. Usually the mammogram is performed with the patient in the upright position, and the ultrasound is performed with the patient in the supine position. Because the breast is a flexible structure, it changes its shape from one position to the other. In the upright position, the position of the breast drops due to gravity, whereas in the supine position, the breast flattens against the chest wall. Compared with other external landmarks, the nipple may be lower in the upright position compared with the supine position. Therefore, a lesion above the nipple in the upright position may shift to the same level as the nipple in the supine position. For example, a 10:00 lesion in the upright position may become a 9:00 lesion in the supine position. Finally, the external position of the handheld transducer does not necessarily correlate with the internal position of the lesion. Even if a linear transducer is used, the examiner commonly uses a variety of angles and hand pressures to optimally visualize the abnormality. Even slight angulation will produce a discrepancy between the position of the sonographic transducer and the actual position of the lesion. Furthermore, transducer pressure may cause the lesion to shift position relative to the nipple. Both of these factors may produce a discrepancy between the mammographic position and the sonographic position. Because external landmarks are not reliable in crosscorrelating mammographic/sonographic abnormalities, you should use internal landmarks. However, you must use a technique that addresses the problems listed earlier: 19 Cross-Correlation of Sonographic and Mammographic Image To accurately, efficiently, and confidently identify a mammographic abnormality sonographically, the technician who performs the breast sonographic examination should be familiar with mammographic imaging. Furthermore, the ultrasound examiner should be able to review the mammogram and identify internal landmarks that can be cross-correlated with the ultrasound. Finally, by confirming the mammographic landmarks sonographically, the examiner should be able to pinpoint the location of the mammographic abnormality in the breast with ultrasound and consequently be able to explain the etiology of the puzzling mammographic finding. Unfortunately, sometimes the ultrasound examiner does not attempt to closely cross-correlate anatomically the ultrasound examination with the mammogram. Some examiners do not attempt to correlate the exams because they do not routinely interpret mammograms and are uncomfortable reviewing mammograms. However, more common reasons for lack of close cross-correlation include the following: (1) the sonographic image has a small field of view compared with the mammographic global field of view. Therefore, the position of a breast mass for these exams appears extremely different. Furthermore, some individuals have a right breast that exhibits a pattern different from the left breast. For these reasons, ultrasound examiners commonly ignore internal breast anatomical landmarks and estimate the location of the mammographic abnormality using external landmarks. These quadrants are defined by drawing a horizontal and a vertical line through the nipple. The quadrants label four 20 Sonographic Technique and Cross-Correlation with Mammography (1) limited sonographic field of view compared with mammography, (2) differences between mammographic and sonographic patient position and technical orientation, and (3) nonuniformity of breast anatomy both between individuals and within the same individual. By using internal breast anatomical landmarks, you immediately address the first two problems. If you identify location by the internal anatomy of an organ, then relating the position of a focal abnormality from the limited sonographic field of view to a wide field of view modality is not a problem. Furthermore, unlike external landmarks, internal landmarks do not shift with body position. Furthermore, this process of anatomical cross-correlation would not be different even if the patient were lying prone because, unlike external landmarks, internal anatomical landmarks do not change relative to each other. Even though internal landmarks solve the problems of limited sonographic field of view and positional changes, many examiners are inhibited from using internal breast landmarks, as there is great anatomical variation between different breasts. However, whenever you perform a breast sonogram to identify a mammographic abnormality, you should always have the corresponding mammogram. If you are able to cross-correlate mammographic structures with sonographic structures, then you may use the mammogram as a sonographic guide to locating the lesion. Therefore, ideally sonographic examiners should be able to sonographically interpret the mammographic image. To systematically cross-correlate sonography with mammography, you should be familiar with normal breast anatomy. There are mainly seven sonographically different structures in the breast and chest wall of the average normal 45-year-old woman. Subcutaneous fatty layer: this structure lies under the skin and appears as an anterior hypoechoic layer of tissue, which tends to thicken at the periphery of the breast and is more prominent in the medial portion of the breast. Superficial fascia: the superficial and deep layers of the fascia envelop the breast. The superficial layer is an undulating hyperechoic line within the subcutaneous fat that parallels the skin. The deep layer is a hyperechoic line within the retromammary fat that parallels the anterior chest wall muscles. Glandular tissue: Normal glandular tissue consists of hyperechoic glandular lobes that are in a radial arrangement around the nipple. Each lobe is in the shape of a prolate ellipse and is surrounded anteriorly by the subcutaneous fat and posteriorly by the retromammary fat. Within the lobes, main ducts originate from the nipple and end in a series of terminal duct lobular units. Anterior chest wall muscles: this layer is formed by the pectoralis minor and major muscles and appears as a hypoechoic solid layer posterior to the retromammary fat. Chest wall: this structure consists of ribs connected by intercostal muscles and covered on the deep surface by the pleura. Most of these anatomical structures are also generally identifiable mammographically. Rules of Cross-Correlation Once you are familiar with normal sonographic and mammographic breast anatomy, you will be able to anatomically cross-correlate the two modalities. If you are not familiar with cross-correlation of these modalities, you should not be intimidated by the task of cross-correlating sonographic and mammographic structures. The first rule is that the background breast tissue appearance is similar on the two modalities. This means that normal fibroglandular parenchyma is white (or dense) on mammography and white (or hyperechoic) on sonography. Furthermore, fat appears dark (or lucent) on mammography and dark (or hypoechoic) on sonography. The main exception to this rule is the presence of dilated ducts that are sonographically dark (hypoechoic) and mammographically white (dense). When the breast tissue is filled with dilated ducts, such as in ductal ectasias, the breast tissue appears white (dense) on mammography but has numerous linear dark structures (dilated ducts) on sonography. When you are aware of the appearance of breast tissue with the two modalities, then when you review a mammogram you should be able to predict the sonographic appearance of the breast. For example, a mammographically fatty, lucent breast will be sonographically hypoechoic. Conversely, a mammographically dense breast usually sonographically exhibits diffusely hyperechoic fibroglandular parenchyma.
Linum Usitatissimum (Flaxseed). Valacyclovir.
- Relieving mild menopausal symptoms.
- Osteoporosis.
- Are there any interactions with medications?
- Prostate cancer, diverticulitis, irritable bowel syndrome (IBS), constipation, stomach upset, bladder inflammation, lung cancer, breast cancer, skin irritation, attention deficit-hyperactivity disorder (ADHD), and other conditions.
- Improving kidney function in people with lupus.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96952
Buy generic valacyclovir pills
Tracheal or oesophageal intubation can be confirmed immediately hiv infection rates louisiana buy valacyclovir 500mg lowest price, with complete accuracy. Ranitidine diminishes gastric acid secretion; sodium citrate neutralizes acid already in the stomach. Ranitidine 150 mg should be prescribed for 2 hours before an elective operation and administered 8-hourly to all women in labour with risk factors for caesarean section. The risk of aspiration of gastric contents is not confined to general anaesthesia: protective laryngeal reflexes may be obtunded in the event of an excessively high regional block. A crystalloid fluid preload has become recognized as an ineffective means of preventing hypotension after spinal injection. Its short intravascular half-life prevents a sustained increase in cardiac output before sympathetic blockade develops. They increase cardiac output and prevent hypotension more reliably than crystalloid. However, all colloids incur a risk of anaphylaxis, and concern has been raised that the further increase in cardiac output from autotransfusion of blood as the uterus contracts after delivery might precipitate circulatory overload. The progressively gravid uterus causes increasing vena caval compression, epidural venous engorgement and consequent displacement of the dura and reduced subarachnoid space volume. Postural manoeuvres after intrathecal injection, such as moving from right to left lateral or flexing the knees and thighs, promote cephalad spread of the injectate by influencing vertebral canal blood volume. Loss of light touch sensation to T5 is a better predictor of pain-free caesarean section under (opioid-free) spinal anaesthesia than loss of cold sensation. Light touch sensation is ascertained by asking if the woman has any appreciation of ethyl chloride dripped on to skin. The extent of the block and modality of testing should be recorded in case a subsequent claim of intraoperative pain has to be defended. The obstetrician must clarify with the anaesthetist that it is appropriate to start surgery. Relief of aortocaval compression by swift delivery of the baby will be required urgently. Obstetricians should not, therefore, leave the theatre suite during induction of spinal anaesthesia. Opioids the addition of intrathecal fentanyl, diamorphine or morphine can reduce the incidence of intraoperative visceral pain, although fentanyl does not contribute significantly to post-operative analgesia. Reports of respiratory depression after intrathecal doses of opioids in obstetric practice are conspicuous by their absence. Level of injection Magnetic resonance imaging has shown that the conus medullaris of the spinal cord extends below the level of the body of L1 in 20 per cent of patients. Vasopressors Ephedrine (alpha and beta sympathomimetic) was regarded as the vasopressor of choice in obstetrics for decades. Persisting reservations about the effects of alpha-agonists on uteroplacental blood flow were founded on studies of Columbian ewes, which did not undergo regional anaesthesia. Increased fetal metabolic rate secondary to ephedrine-induced betaadrenergic stimulation may be the explanation. Infusions of phenylephrine, compared with ephedrine, are associated with improved maternal haemodynamic control and less nausea and vomiting [B]. In one study, loss of 396 Obstetric anaesthesia and analgesia widely regarded as the vasopressor of choice at caesarean section and should mitigate the slight fetal acidosis that was observed in a meta-analysis of spinals compared with epidurals or general anaesthetics. Judicious fluid boluses and small increments of either ephedrine or phenylephrine will correct hypotension. Pre-emptive infusions of vasopressor are best avoided to avoid arterial pressure overshoot. Epidural anaesthesia Few elective caesarean sections are now performed under epidural anaesthesia, because the quality of anaesthesia is generally poorer than that afforded by subarachnoid block. The rate of conversion to general anaesthesia for epidurals is consistently greater than that for spinals. De novo epidural anaesthesia is still favoured by some when gradual establishment of block is desired to minimize hypotension. In severe pre-eclampsia, postoperative infusion of epidural bupivacaine/fentanyl in a high-dependency area will confer optimal analgesia and contribute to blood pressure control. A South African study demonstrated that women who were fully conscious and co-operative after an eclamptic seizure could safely undergo caesarean section under epidural anaesthesia. If analgesia in labour has been poor, it is unlikely that anaesthesia for caesarean section will be satisfactory. The floor of the triangle is composed, from superficial to deep, of the fascial extensions of external oblique, internal oblique, and transversus abdominis, respectively, and the peritoneum. The needle is inserted through the triangle, using the loss-of-resistance technique. The needle is shown in the transversus abdominis plane, and the fascial layers have separated as a result of the injection of local anesthetic Anaesthesia for caesarean section 397 of analgesia for labour to surgical anaesthesia for caesarean section takes around 20 minutes. In contrast to single-shot spinal anaesthesia, abrupt changes in blood pressure are unusual. Good communication among midwives, obstetricians and anaesthetists should make general anaesthesia for the woman with a working epidural a rarity. Even in the event of cord prolapse, traditionally managed without question by general anaesthesia, there might be time for an epidural top-up, provided upward displacement of the presenting part is effective in avoiding cord compression. However, the initial spinal anaesthetic block precludes ascertainment of correct positioning of the epidural catheter. Anterior placenta praevia in a woman over 35 who has undergone previous caesarean sections suggests a particularly high risk of placenta accreta and massive haemorrhage. An important distinction must be made between women with the potential for major intraoperative haemorrhage (as in placenta praevia) but who are normovolaemic. Pregnant women can compensate for significant blood loss by vasoconstriction, which will be abolished by regional anaesthesia. Any woman who has bled and is pale and tachycardic is not suitable for regional anaesthesia, regardless of the blood pressure. Regional anaesthesia might be ideal for advanced placement of uterine artery balloons immediately before caesarean section, but totally inappropriate for interventional radiological management of haemorrhage. Good communication between the anaesthetist and obstetrician is vital in these cases, and the safety of the mother must always remain of paramount importance. If the history or evaluation of the airway suggests that tracheal intubation might be difficult, awake fibre-optic intubation should be considered. A multicentre comparison of continuous intrathecal labour analgesia versus continuous epidural labour analgesia was published in 2008, powered to detect a >1 per cent incidence of neurological complications related to use of the intrathecal catheter [B]. In the event of anaphylaxis, adrenaline (epinephrine) is likely to improve rather than reduce utero-placental blood flow. Rapid operative delivery while the anaesthetist administers pharmacological treatment will aid maternal resuscitation. Depth of anaesthesia the regimen of thiopental, succinylcholine and intubation has remained standard and largely unchanged since it superseded ether by facemask 50 years ago, and has permitted a lighter plane of inhalational general anaesthesia. If uterine hyperstimulation has been contributory to fetal compromise, uterine relaxation conferred by a volatile agent might be therapeutic. In contrast, a maternal stress response to excessively light general anaesthesia Placenta praevia and antepartum haemorrhage Regional anaesthesia has been associated with reduced estimated blood loss and transfusion requirements at caesarean section with placenta praevia. Although the evidence is not high level, the commonly held obstetric view that placenta praevia mandates general anaesthesia is not supported. Individual risk factors must be considered First stage of labour 398 Obstetric anaesthesia and analgesia will be to the detriment of uteroplacental blood flow. With inhalational agent monitoring now universally available, the risk of awareness in obstetric anaesthesia should have been consigned to history.
Cheap 1000mg valacyclovir visa
General anaesthesia is indicated for the majority of caesarean sections where there is immediate threat to the life of the mother or fetus and a regional technique is absolutely contraindicated or has failed hiv infection no symptoms generic 1000mg valacyclovir overnight delivery. The principal risks of general anaesthesia are airway problems, aspiration of gastric contents and anaphylaxis. Ranitidine should be prescribed for women in labour with risk factors for caesarean section. Placenta praevia does not necessarily dictate general anaesthesia for caesarean section. Regional anaesthesia is inappropriate for women with signs of significant haemorrhage. Prescribing intramuscular opioids for labour analgesia in consultant-led First stage of labour 400 Obstetric anaesthesia and analgesia 7. Effect of low-dose versus traditional epidural techniques on mode of delivery: a randomised controlled trial. Ambulation in labour and delivery mode: a randomised controlled trial of high-dose vs mobile epidural analgesia. The risk of caesarean delivery with neuraxial analgesia given early versus late in labor. Assessment of a modified four-category classification of urgency of caesarean section. In: Confidential Enquiry into Stillbirths and Deaths in Infancy, 7th Annual Report. A randomised double-blinded comparison of phenylephrine and ephedrine infusion combinations to maintain blood pressure during spinal anesthesia for caesarean delivery: the effects on fetal acid-base status and hemodynamic control. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: a randomised controlled trial. Epidural compared with general anaesthesia for caesarean delivery in conscious women with eclampsia. A randomized, double-masked, multicenter comparison of the safety of continous intrathecal labor analgesia using a 28-gauge catheter versus continuous epidural labor analgesia. A prospective study of awareness and recall associated with general anaesthesia for caesarean section. It was not until much later that intervention with a good outcome for both mother and baby became possible. Consequently, a dramatic rethink of all midwifery and obstetric management is being called for, mainly by those outside the profession. Unfortunately, both clinical and ultrasonographic estimations of fetal size are prone to inaccuracy (especially in large term infants), and many unnecessary inductions of labour and caesarean deliveries are performed as a consequence. Currently, there is no evidence to support induction of labour for suspected fetal macrosomia in the non-diabetic woman (see Chapter 25, Induction of labour). Maternal request Traditionally, caesarean sections have been reserved for situations guided by standard clinical indications. The arguments surrounding this area are complex and combine ethical dilemmas, the fetal and maternal risks of vaginal and surgical deliveries and the financial consequences of permitting such a preference. During the antenatal period, the dialogue between patients and their doctors has increased over recent years. Changing Childbirth enshrined in practice the principle of total involvement of the pregnant woman in her own care. However, if these risks are fully explained to the woman, she should be allowed to accept one set of risks over the other. Several studies have reported an increase in the incidence of instrumental Morbidity and mortality 403 is the sole reason, care should be taken to explore the request and a second opinion can be sought. Other indications, such as multi-fetal pregnancy, abruptio placenta, placenta praevia, fetal disease and maternal disease, are less common. The Confidential Enquiries enable the risks associated with each method of delivery to be analysed. A comparison of fatality rates can be useful, but it is preferable to restrict the analysis to direct deaths, as many women whose deaths were classified as indirect had pre-existing illness. Direct deaths are specifically those that result from obstetric complications of the pregnant state, from interventions, omissions or incorrect treatment, or from a chain of events that occur after any of the above. It can be seen that the case fatality rate for all caesarean sections is at least five times that for vaginal delivery, and for emergency caesarean delivery this may be 12 times greater. The factors to be weighed when determining the recommended mode of delivery depend on the balance between the desires of the mother, the risks of a repeat operation, the risks to her child of labour, and the risk of labour on the strength of the old scar (see Chapter 26, Management of previous caesarean section). The level of information discussed must be commensurate with the urgency of the procedure, and a commonsense approach is needed. Although it is often difficult to impart complete and thorough information when caesarean sections are performed as emergency procedures, mothers must understand what is being planned and why. It is important to remember that no adult may give consent for another (although it is good practice to keep relatives fully informed). Full documentation of the recommendation and its refusal is mandatory, but no healthcare provider can force a competent adult to undergo surgery against her will. One must always respect the wishes of the patient and her cultural and religious beliefs, no matter how challenging the consequences appear. In an elective or unhurried atmosphere, where there is significant doubt about capacity to consent, two medical opinions are required to over-ride patient wishes. It is advised, though not mandatory, that one of these should be obtained from a psychiatrist. The national consent forms require both the risks and benefits to be discussed with patients and recorded on the consent form. It is suggested that the top copy of the form should be offered to the patient, although in some situations this may not be appropriate. Although it is usual to obtain written consent, it is important to remember that verbal consent is equally valid and in an emergency situation may be more appropriate. Common medical practice is to highlight risks but not benefits, but it is important to remember that the operation is being offered because of the perceived benefits, which in many cases are both maternal and fetal. Although this approach may improve patient comfort post-operatively and reduce the incidence of over-distension of the bladder (a complication of regional anaesthesia), such a policy runs the risk of introducing an iatrogenic urinary tract infection. A left lateral tilt minimizes compression of the maternal inferior vena cava and reduces the incidence of hypotension (with its consequent reductions in placental perfusion). Plastic adhesive drapes may prove more effective than standard drapes in the prevention of wound infections. The choice of incision and closure should be individualized to the characteristics of the woman and the circumstances demanding operative intervention. The transverse incision has the advantages of improved cosmetic results, decreased inter-operative and postoperative analgesic requirements and thus less pulmonary compromise and superior wound strength postpartum. Haeri demonstrated no difference between the two incisions when comparing overall operative time, post-operative haemoglobins of <10 g/dL, or post-operative febrile morbidity [D]. The Pfannenstiel incision the skin and subcutaneous tissues are incised using a transverse curvilinear incision at a level of two fingerbreadths above the symphysis pubis, extending from and to points lateral to the lateral margins of the abdominal rectus muscles. The subcutaneous tissues are separated by blunt dissection and the rectus sheath is incised transversely along the middle 2 cm. This incision is then extended with scissors or blunt dissection before the fascial sheath is separated from the underlying muscle.
Generic valacyclovir 1000mg free shipping
Rarely lifespan with hiv infection order valacyclovir line, there can be systemic involvement with this reactivation, involving multiple visceral inflammation. In both manifestations, the clinical presentation of the disease is classical enough to make a confident diagnosis clinically. The non-pregnant adult needs to be more closely monitored, with evidence of any systemic symptoms needing prompt evaluation and treatment by a specialist medical team. In relation to pregnancy effective up to 10 days after contact, but does not absolutely preclude development of the disease [E]. The risk of infection following contact with shingles in a non-exposed area is remote. If shingles is disseminated, in an exposed area or in an immunocompromised individual, then the risk is greater. Clinicians should be aware of the excess morbidity associated with varicella infection in adults, including pneumonia, hepatitis, encephalitis and occasionally mortality. Varicella zoster virus immunoglobulin is of no benefit once chickenpox has developed. Hospital assessment and intravenous acyclovir are required for those patients with varicella pneumonia, those over 36 weeks gestation and patients with clinical deterioration after day 6 of the rash [E]. A neonatologist is required to be involved should the disease onset coincide with the delivery period. The risk of developing secondary complications is increased in cigarette smokers and in patients with chronic lung disease, immunosuppression and prolonged courses of steroids. Intrapartum Delivery during the viraemic period can be hazardous to both the mother and baby. Delaying delivery decreases the maternal complications of bleeding, thrombocytopenia and disseminated intravascular coagulation. It also allows time for transfer of protective antibodies from the mother to the fetus, thus decreasing the incidence of varicella of the newborn, which has high associated morbidity and mortality [E]. If there is no positive history, pregnant women should be advised about avoidance of contact with chickenpox or shingles and to contact healthcare personnel immediately if exposure occurs. Similar advice should be proferred to an immunocompromised person exposed to shingles. Admission to hospital and intravenous acyclovir should be considered if the woman is 36 weeks gestation, has any signs of varicella pneumonia or has any clinical deterioration. Ideally, delivery should be delayed until 7 days after the onset of the maternal illness. However, IgM levels rise with reactivation and cannot therefore be used as a marker for first infection. In relation to pregnancy There are no implications from a maternal health point of view. Cytomegalovirus Epidemiology and aetiology Transmission can be horizontal via direct human-tohuman contact and with sexual activity. The lungs, liver, kidney and salivary glands are the most commonly affected organs. Presentation and diagnosis the predominant symptoms are fever, malaise, sore throat and headache. These rashes typically occur in 90 per cent of patients who have been treated with ampicillin for their sore throat. In the majority of cases, this is a self-limiting illness, but it can run a protracted course with the patient feeling debilitated for several months. Presentation and diagnosis In healthy adults, the presentation is indistinguishable from infectious mononucleosis. Haemolytic anaemia, thrombocytopenia and deranged liver function tests may be present. The varied manifestations include encephalitis, retinitis, pneumonitis and involvement of the gastrointestinal tract. Togaviruses 165 In relation to pregnancy There are no special features involving the pregnant woman and no known effects of vertical transmission. Malaise and fever are the common clinical features, with conjunctivitis and lymphadenopathy (particularly postauricular and suboccipital). The classical rash is a pink/ red macular type, starting on the forehead and spreading to the trunk and limbs. Rare complications are secondary pulmonary bacterial infection, arthralgia, encephalitis and haemorrhagic manifestations due to thrombocytopenia. The diagnosis is usually clinical but can be confirmed by culturing the virus from urine, nasopharynx or cerebrospinal fluid. Epidemiology and aetiology Aerosol droplets and exchange of bodily fluids transmit this virus. The rash is less prominent but more widespread, involving the face, trunk and extremities. Those patients with hereditary blood dyscrasias, for example sickle cell anaemia, are susceptible to aplastic crises. Serological testing is required for diagnosis as the clinical presentation is similar to that of a number of viral syndromes. In relation to pregnancy Management In healthy individuals this is normally a self-limiting illness, with no specific therapy being warranted. In relation to pregnancy Spontaneous abortion and intrauterine fetal death have been associated with parvovirus B19 infection. All pregnant women presenting with a non-vesicular rash compatible with a viral infection should be investigated for rubella and parvovirus B19 infection [E]. When serology shows potential for early infection with parvovirus B19, the patient should be referred to a fetal medicine unit capable of fetal blood sampling and intravascular transfusion [E]. Rubella infection in pregnancy does not confer increased risk to the mother; it is the devastating teratogenic effects of this virus that are of concern (see Chapter 13, Fetal infections). Human Ig can decrease the symptoms of the disease, but does not prevent the teratogenicity. All susceptible women who are receiving healthcare should ideally have their serological state tested. Opportunistic testing for this can be performed, for example family planning clinics and infertility investigation. It is recommended that pregnancy should be avoided for one month after the vaccine is administered. Antenatal complications: maternal Antepartum the routine booking bloods taken in the antenatal period include serological testing for the presence of rubella antibodies. If not immune, the patient should be counselled about avoidance of any affected people. All pregnant women presenting with a non-vesicular rash compatible with a viral infection should be investigated for rubella and parvovirus B19 infection, irrespective of a prior history of rubella vaccination or previous positive rubella antibody tests [E]. Fetal infection the implications to the fetus of rubella infections are discussed in Chapter 13, Fetal infections. Risk factors are frequent unprotected sexual intercourse with different partners and intravenous drug abuse. This acute febrile illness is associated with high morbidity and mortality, particularly in developing countries. A maculopapular rash then occurs, initially on the face, then spreading to the rest of the body. Complications include otitis media, bacterial pneumonia, myocarditis, hepatitis and encephalomyelitis. Rarely used serological tests include a haemagglutination inhibition antibody that is present by the onset of the rash and remains positive for life.
Valacyclovir 1000mg free shipping
Regimens vary (although there is an increasing trend towards regional protocols) hiv infection symptoms in pregnancy order generic valacyclovir from india, for example: Labour ward management of pre-eclampsia A set protocol should be followed when a women has severe pre-eclampsia [E]. Typical entry criteria for such a protocol would be:14 Labetolol: bolus of 20 mg i. Colloid should be infused prior to treatment if the baby is undelivered, to protect the uteroplacental circulation and prevent hypotension and fetal distress [E]. Antenatal complications: maternal eclampsia, or severe hypertension (>170/110 mmHg) with + or >1 g/24 hours proteinuria, or hypertension (>140/90 mmHg) with ++ or >3 g/24 hours proteinuria with an additional complication such Fluid management As women with pre-eclampsia can have a reduced intravascular volume, leaky capillary membranes and low albumin levels, they are prone to pulmonary oedema. Renal failure is a rare complication of pre-eclampsia that usually follows 190 Pre-eclampsia and non-proteinuric pregnancy-induced hypertension acute blood loss, when there has been inadequate transfusion, or as a result of profound hypotension. Oliguria without a rising serum urea or creatinine is a manifestation of severe pre-eclampsia and not of incipient renal failure. Administration of intravenous fluid in response to oliguria must be performed with caution [E]. Most protocols limit fluid intake (in the form of intravenous crystalloid) to approximately 1 mL/kg per hour [E]. In a well-perfused women, oliguria (<400 mL/24 hours) requires no treatment per se. If the creatinine or potassium rises, haemodialysis or haemofiltration may be necessary, and the advice of a renal physician should be sought. The administration of diuretics temporarily improves urine output, but further decreases the circulating volume and exacerbates electrolyte disturbances; frusemide should only be given if there are signs of pulmonary oedema [E]. In particularly difficult cases, pulmonary artery catheterization should be considered. Anaesthesia A general anaesthetic can be dangerous, as endotracheal intubation can cause severe hypertension. Regional blockade is the preferred method of analgesia for labour and of anaesthesia for operative deliveries [E], but a coagulopathy must be excluded. Care must be taken to avoid arterial hypotension (particularly following postpartum haemorrhage) in view of the vasoconstriction and reduced intravascular volume. A low threshold for central invasive monitoring is necessary in women who require a caesarean section [E]. Postpartum care As a third of eclamptic fits occur postpartum, intensive monitoring is required, usually for 48 hours after delivery. Although eclampsia has been reported beyond this time, it is unlikely to be associated with serious morbidity. In addition to blood pressure and urine testing, tests of renal and liver function should be instigated; residual disease may merit referral to a physician. Underlying predispositions to pre-eclampsia, such as an inherited thrombophilia or antiphospholipid syndrome, should be excluded (multiparous women are more likely to have an underlying cause). The postnatal visit is also an excellent opportunity to discuss complications of the pregnancy and the planned management of any future pregnancy. While it is generally considered that facilitated diffusion, phagocytosis and pinocytosis play little significant role in drug transfer, there is growing interest in placental active transport, utilizing energy-requiring drug transporters. All these transporters work against a concentration gradient, and several have now been described within the placenta. Within this period, each structure has a period of maximal vulnerability, and usually, the earlier the insult the more severe the resulting malformation. However, some structures that have initially formed during embryogenensis are still vulnerable to effects in the fetal period of development (9 weeks to term). However, encephalocoeles have been described post-closure during the fetal period. The classic and most famous example of this is thalidomide, which was introduced as an anti-emetic in the 1950s and was subsequently withdrawn when it was found to cause phocomelia. Lactation the principles of drug transfer from the maternal circulation into breast milk are the same as those across any membrane, and thus will depend on the lipophilic properties, degree of ionization and plasma protein binding of the drug. The amount of drug that the infant is exposed to will be dependent upon volume of milk ingested, maternal plasma levels and infant excretion (which probably varies with age and is less with increasing immaturity). Plasma protein binding has been shown to have a significant impact on levels in breast milk. Drugs which are highly protein bound result in less infant exposure via breast milk. Measurable infant levels were only found for drugs with less than 70 per cent plasma protein binding. Placental drug metabolism There is growing evidence that the placenta expresses many of the enzymes able to metabolize drugs. However, it is known that, for some enzymes it varies with gestation, and the activity of many is altered by alcohol and cigarette smoking. Drugs that undergo metabolism in the placenta include steroids, such as dexamethasone, and alcohol. For example, transplacental passage of antiarrhythmic drugs has been used to treat fetal supraventricular tachycardias since the first report in 1980. Co-administration of other anti-arrhythmic drugs has been suggested to improve success by modifying P-glycoprotein transport of digoxin. In general, use of the lowest number of drugs (monotherapy where possible) and the lowest effective dose is recommended, remembering the effects of pregnancy on plasma levels of a drug [E]. For obvious reasons, this is in no way exhaustive and more detailed discussions can be found in the literature referenced at the end of this chapter, or in the relevant sections of this book. Teratogenicity A teratogen is an agent that is able to permanently alter the development, growth, structure or function of a developing embryo or fetus. The period of organogenesis (embryonic Effects of pregnancy on pharmacokinetics and pharmacodynamics 195 Table 8. Stop if oligohydramnios [D,E] Nifedipine may demonstrate increased clearance in third trimester [D] Teratogenic in first trimester. Renal and cardiac problems in late gestation [D,E] Considered compatible Anti-hypertensives Optimize blood pressure control Beta-blockers associated with fetal growth restriction (less so with labetalol). Intravenous doses should be given with fetal monitoring Usually stop as may adversely effect placental development. Studies ongoing Present in breast milk (except nifedipine, which is >90% protein bound). Tooth discolouration [D,E] Only small amounts cross placenta, but has been associated with bone/cartilage problems. Association with reduced fetal weight [C] Fetal liver lacks enzyme to convert to active metabolite (6-mercaptopurine) Unknown levels in breast milk, but usually considered safe Low concentrations of metabolites in breast milk. Fluoxetine crosses placenta, but not considered teratogen [D,E] Cardiovascular malformations, floppy infant, neonatal arrhythmias, hypoglycaemia, thyroid dysfunction [D] Found in breast milk. Some suggest reducing/stopping just prior to delivery [D,E] Anti-epileptics Sodium valproate Optimize treatment on lowest dose, avoid if possible Total concentrations fall, but more so than the unbound concentrations. Neonatal serum levels <10% of maternal levels [D,E] Carbamezepine Obtain control on lowest dose possible Obtain control on lowest dose possible Probably safe in breastfeeding [D,E] Phenytoin Total concentrations fall, but more so than the unbound concentrations. Considered safe [D,E] Lamotrigine Obtain control on lowest dose possible Crosses placenta, limited data as newer drug [D,E] Low transfer in breast milk, therefore considered safe [D,E] Anti-coagulants Warfarin Discuss risks, and make plan for pregnancy. May be safe to use heparin as alternative throughout pregnancy, but for women with metal valves this may not provide sufficient anti-coagulation [E] Teratogen. Does not cross placenta due Increased renal clearance, to molecular size may require increased dose.
Order valacyclovir 500mg free shipping
The odds-ratio of producing infants below the tenth centile of weight for gestational age (compared with nondrinkers) for women consuming alcohol hiv infection of the brain order 1000mg valacyclovir, but less than one unit per day, is 1. Its vasoconstrictive properties are thought to cause abnormal implantation, hypertensive episodes and abruption. Down-regulation of beta-adrenoreceptors in the myometrium may lead to increased uterine irritability and predispose to preterm labour. Amphetamines and ecstasy may have similar effects, although there are much less data. Studies of cocaine use in pregnancy have confirmed the increased risk of preterm labour and abruption; however, these are often lost when confounders (alcohol use and smoking) have been accounted for. Antenatal complications: maternal Substituting methadone for heroin has a beneficial effect on prenatal growth, but this may have more to do with increased levels of antenatal care than the action of the heroin itself (see below). The vasoconstrictive properties of cocaine suggest it should cause prenatal growth restriction. This results from the acute withdrawal of transplacental opioid which occurs at the delivery of a baby born to an opiate-abusing mother. The onset of the syndrome is normally within 24 hours of birth if the opiate used was short acting. Mothers willing to participate in longitudinal studies may be more highly motivated, and superior parenting skills in co-operative families may make the effects of the substance abuse appear less significant. The literature is confusing and does not offer clear guidance, perhaps because of the aetiological difficulties discussed above. Opiates Opiate use in pregnancy is indeed associated with poor developmental outcomes for the offspring; however, it seems that confounding factors are most likely to be responsible, rather than the drug itself. Results of child development tests have been found to be lower at one and two years of age by some researchers. However, a clear harmful effect of opioids themselves on child development is not strongly suggested by the literature. Alcohol, cocaine and amphetamines have a less marked effect on neonatal behaviour, if any effect at all. Rare events such as neonatal hypertension, arrhythmias and necrotizing enterocolitis are said to be more common in the offspring of cocaine users, although the confounding effects of prematurity are difficult to separate. Amphetamine-exposed newborns occasionally demonstrate hyperactivity, poor feeding and disrupted sleep patterns. Greater irritability, tremors and startle responses have been reported, but a well-controlled Jamaican study8 has suggested that once again the postnatal environment is more important than drug exposure per se. In fact, neonatal scores were found to be higher in the offspring of heavy marijuana users. In rural Jamaican society, these women tend to be wealthier and more highly educated. Benzodiazepines may cause neonatal respiratory depression, reduced tone and poor feeding. Cocaine Head circumference is inversely related to cocaine exposure during pregnancy. Along with the reported association with serious fetal/neonatal intracranial pathology, it is unsurprising that cocaine itself is thought to be directly damaging to neurodevelopment, with or without confounding social factors. Indeed, neurophysiological testing of such children suggests reduced numbers of oligodendrocytes and impaired myelination. Closer examination of the data on neurodevelopmental outcome has challenged this view, and the two sides of the debate are difficult to reconcile. The meta-analysis performed by Frank and colleagues9 selected 36 prospective and blinded studies in which polydrug use was uncommon. After controlling for confounding factors, there was no significant overall association between prenatal cocaine exposure and cognition, language and motor skills, behaviour, attention, affect or neurophysiology, up to six years of age [C]. Independent of any direct actions of the drug, pregnancy and neurodevelopmental outcomes are nevertheless poor and will only improve with better access to healthcare and social support. Because of this, they may present needing help only at the time of a social, domestic or medical crisis. All those caring for pregnant women should be vigilant for substance abuse and take the opportunity to institute specialized antenatal care whenever presentation occurs. Enquiry about illicit substance use should be routinely made of all pregnant women in a matter-of-fact way. Covert urine testing may confirm substance abuse, but be careful when disclosing this information source, as it may be seen as underhand and untrustworthy and may damage the fragile relationship between the woman and the healthcare services. Exchanging needles or moving to non-intravenous modes of delivery would be examples of harm reduction. Reducing alcohol and tobacco consumption and establishing methadone maintenance are particularly important aims in pregnancy. Antenatal care Significant improvements in pregnancy outcome are achieved by regular antenatal care, which should be tailored to the individual. It aims initially to promote a change in the nature of the drug taking, to stabilize lifestyles and reduce criminal behaviour. Stopping drug abuse Type of drug(s) used, when, how often, how much and mode of administration. Are there specific psychological or health problems leading to , or a consequence of, the drug abuse Users are provided with a regular but limited supply, which offers the opportunity to remove themselves from the criminal high-risk behaviours often necessary to fund a street habit and which carry such risk to the pregnancy. Having to attend regularly to obtain prescriptions allows close antenatal surveillance and healthcare. Use of both methadone and heroin carries a 6-fold increase in neonatal mortality risk. Anecdotal evidence recommends that this should occur in the second trimester, as leaving it until later risks preterm labour [E]. The greater risk of withdrawal during pregnancy is a subsequent relapse of illegal narcotic use. This is considered to carry the greatest risk of fetal harm, and withdrawal during pregnancy should only be attempted in highly motivated women with a stable, supportive and drug-free environment to which they can return. Without an incentive, it may be very difficult to gain the trust and co-operation of pregnant users who fear reprisals for their substance abuse. Most programmes choose to treat the pregnant, alcohol-dependent woman with short-acting barbiturates or benzodiazepines. Chlordiazepoxide and other benzodiazepines, such as diazepam and barbiturates, are valuable for symptomatic treatment during medical withdrawal from alcohol. Women who conceive while taking this drug should receive counselling before deciding to continue the pregnancy. Epidural analgesia may prove most effective if opioid receptors are already saturated by the illegal opiate. Those women who have undergone supervised withdrawal from opiates during the pregnancy should avoid systemic opiates in labour. In cocaine users, ephedrine may be less effective at reversing hypotension secondary to regional analgesia. Postnatal care Above all, the new mother should be supported in her first few days, as any new parent should be. Intrapartum care Labour may be the first time a pregnant substance abuser presents to medical services. If the baby seems well, it should be transferred to the postnatal ward with the mother. Methadone withdrawal may take a little longer, but will usually have begun by 4 days (the minimum time period that women are advised to stay in hospital). If the infant is demonstrating withdrawal symptoms, it will need special care facilities. Infant weaning should occur gradually; fortunately the quantities of opiates reaching breast milk are small. Drug misuse by a parent does not necessarily equate with child neglect or abuse, and automatic child abuse registration will only discourage women from seeking antenatal care. Social services should be informed of the delivery and decisions made about the levels of support needed to ensure child safety.