Generic extra super avana 260mg fast delivery
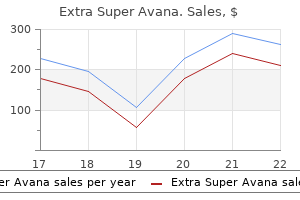
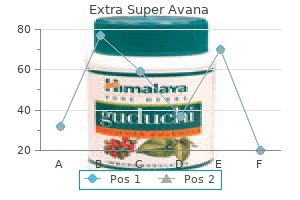
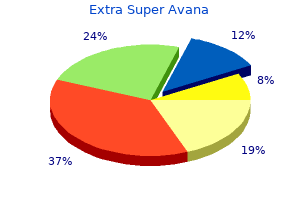
Peripheral blood smear should be reviewed systematically for blasts impotence yoga poses buy extra super avana in united states online, blast equivalents, other abnormal cells, and dysplasia (all hematopoietic lineages). Immunophenotyping Immunophenotyping by flow cytometric analysis remains the mainstay of diagnosis. Based on cytogenetics, three risk groups have been identified for treatment risk stratification and the 5-year survival rates for those with favorable, intermediate-risk, and poor-risk cytogenetics are 65%, 41%, and 14%, respectively. Aside from the cytogenetics and molecular risk factors, response to therapy is one of the strongest predictor of outcome. Specific molecular genetics, if available, should also be performed on bone marrow blasts. Several of these mutations having prognostic importance are described in recent clinical trials. These patients should be treated in well-equipped pediatric oncology centers, on pediatric protocols. The treatment should be risk-adapted, to improve outcome and to minimize the morbidity and mortality associated with the therapy. Special attention should be given to supportive care such as prevention and treatment of tumor lysis syndrome, hyperleukocytosis, and infection complications. Therapeutic approaches have continued to emerge from several well-designed trials by various cooperative groups. The adequate prophylaxis usually consists of four to five doses of intrathecal chemotherapy with either cytarabine or methotrexate or a combination of these two with hydrocortisone given concurrently with systemic chemotherapy. Systemic Disorders Induction Therapy the primary goal of induction therapy is to achieve a significant reduction of leukemia burden, i. The standard induction therapy consists of a combination of cytarabine and an anthracycline in a 7 + 3 strategy. That is, cytarabine (typically 100 mg/m2/day) administered by continuous infusion over 7 days with an anthracycline (daunorubicin 4560 mg/m2 given on days 13). Several strategies have been tried to achieve further intensification of this regimen, such as increasing the dose of cytarabine, prolonging the time of administration or early administration of subsequent courses of therapy. Certain anthracyclines (idarubicin and mitoxantrone) are favored for their perceived greater antileukemic effect and/or lower cardiotoxicity, but no anthracycline agent has been demonstrated to be superior. Addition of a third drug to the 7 + 3 regimen has not been shown to be beneficial. Supportive Care and Control of Infections the treatment is intensive and prolonged neutropenia is common with virtually all courses of therapy. With high-dose Ara-C regimens, there is a particular increase in -streptococcal infection. Prompt initiation of antibiotics directed at both gramnegative bacilli and gram-positive -streptococci is crucial in salvaging the patients-a common regimen is to initiate therapy with cefepime and vancomycin. In some recent trials, prophylactic cefepime/ciprofloxacin drastically reduced death from -streptococcal infections. The risks for treatment-related morbidity and mortality remain high from unrelated donors with less than perfect match. For low-risk patients, two to five courses of combination chemotherapy with high-dose cytarabine, anthracycline with or without the addition of a third drug such as etoposide or 6-thioguanine are used to consolidate and maintain remission. Maintenance Therapy the benefit of maintenance therapy in children when tested in randomized trials has shown controversial results. Many new agents with diverse putative mechanisms of action are currently entering clinical trials for adults Table 3). It is characterized by the presence of a balanced reciprocal translocation between the long arms of chromosomes 15 and 17 [t(15;17)(q22;q21)] which is seen in 98% of cases. It causes a block in differentiation and accumulation of abnormal promyelocytes in bone marrow. The targeted immunotherapy agents such as gemtuzumab ozogamicin and clofarabine along with newer chemotherapeutics as mentioned in Table 3 have shown some activity in clinical trials. The standard induction therapy consists of a combination of cytarabine and an anthracycline in a 7 + 3 strategy and remains as effective as any other induction regimen. Consolidation therapy is risk based but usually consists of two to three cycles of high-dose cytarabine. Single-agent arsenic trioxide in the treatment of newly diagnosed acute promyelocytic leukemia: long-term follow-up data. Biology, risk stratification, and therapy of pediatric acute leukemias: an update. The Ph1 chromosome is formed in a reciprocal balanced translocation between the long arms of chromosomes 9 and 22. An appropriately planned diagnostic evaluation aids in planning of an optimal therapy and follow-up. This is most commonly diagnosed in the older adolescents in the pediatric age range. The clinical features, lab findings and cytogenetics in each phase are summarized in Table 1. Meningeal leukemia this is a rare complication seen in blast transformation and may present with cranial nerve palsies and papilledema. Hyperleukocytosis the leukostatic complications due to high leukocyte count are especially seen in brain, lung, retina and penis. Hence children with symptomatic hyperleukocytosis might require immediate treatment with drugs or leukapheresis. Thrombocytosis this may be associated with thromboembolic or hemorrhagic complications. Hydroxyurea is a ribonucleoside diphosphate reductase inhibitor and started at 2550 mg/m2/day and adjusted as per hematologic response. The recommended starting dose is 340 mg/m2 once daily (available as 100 mg and 400 mg tablets). Tablets may be dispersed in water or apple juice using 50 mL for 100 mg and 200 mL for 400 mg tablet. Blast Crisis Start imatinib at 500 mg/m2 or dasatinib at the dose of 80 mg/ m2/day in two divided doses. Imatinib dose escalation applied as a strategy in children who do not show the expected response and in advanced phases has shown some benefit. A progression-free survival of 98% at the end of 2 years has been achieved in children. Hyperleukocytosis should be treated by cytotoxic drugs- hydroxyurea and if needed, leukapheresis. Treatment of priapism includes analgesia, hydration, application of warm compresses, and initiation of chemotherapy. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Chronic myelogenous leukemia is a chronic hematopoietic stem cell disorder characterized by myeloid hyperplasia of bone marrow. Chronic myelogenous leukemia is characterized by three phases: (1) chronic phase, (2) accelerated phase and (3) blast phase. The typical diagnostic findings of a peripheral smear in chronic phase consist of myeloid cells in all stages of maturation, few blasts with basophilia. A child in chronic phase can present in tumor lysis, hyperleukocytosis, priapism or thrombocytosis. These regions are site for tumor suppressor genes and have a definite role in hematopoiesis. The bone marrow has less than 20% blasts and may have normal, hypo- or hypercellularity. Myelodysplastic syndrome disorders have a tendency to transform into leukemias mostly myeloid leukemias, and hence are referred as preleukemias. This lack of understanding was because of poor understanding of the biologic mechanisms of the disease, rarity of the disease, lack of uniform diagnostic criteria and use of adult criteria for classification and prognostic system. The classification systems are based on clinical examination, findings of peripheral smears, cytogenetics and bone marrow histology.
Order extra super avana line
Some congenital malformations syndromes such as Smith-Lemli-Opitz syndrome short term erectile dysfunction causes purchase extra super avana mastercard, Miller-Dieker syndrome, Rubinstein-Taybi syndrome, etc. Exposure to environmental factors such as ionizing radiation, therapeutic drugs, intrauterine infections such as cytomegalovirus are known to cause certain types of brain malformations. Brain malformations have been estimated to occur with an incidence of approximately 3. The incidence and prevalence of the individual brain malformation is described under the specific malformations below. Classification of malformations of brain on embryological and anatomical basis is easy to understand and follow Table 1). Classification systems based on underlying molecular or genetic defects are too complex and beyond the scope of this chapter. The age of onset varies from birth (in some cases may be intrauterine) to adulthood depending upon the severity and complexity of the brain malformations. Neonatal seizures including refractory epileptic encephalopathies, hypotonia, feeding or breathing difficulties tend to be the earliest manifestations. During infancy and early childhood, developmental delay, seizures, including infantile spasms, partial seizures and other refractory epilepsy syndromes such as Lennox-Gestaut syndrome may unmask the underlying brain malformations. Intellectual disability, developmental language disorders, specific learning difficulties, behavioral disability, epilepsy, motor difficulties secondary to spasticity, ataxia, weakness or movement disorder become evident as the children grow old. Although all these function deficits are not specific for brain malformations, certain phenotypical characteristics may point to a specific brain malformation. For example, occurrence of infantile spasms in a female infant with retinal lacunae points to Aicardi syndrome. Brain malformations are also increasingly being diagnosed during routine or dedicated prenatal ultrasonographic examinations. Signs and symptoms that are relatively specific for certain brain malformations are discussed under individual malformations of the brain. Soon three flexures (bends) make their appearance-the mesencephalic flexure at the midbrain level, the cervical flexure at the junction of hindbrain with spinal cord and the pontine flexure in the hindbrain. Neuroimaging with magnetic resonance provides anatomical diagnosis of specific malformation in most of the cases with its ability to see brain in various planes, though further evaluation especially genetic may sometimes be required to reach a final diagnosis and for genetic counseling. Drugs are also sometimes needed to treat spasticity, sialorrhea and movement disorders. Physical, occupational and speech therapy are generally required as patients frequently manifest cerebral palsy, speech and swallowing difficulties. Orthopedic, neurosurgical, ophthalmological consultations are needed in appropriate cases. Genetic diagnosis and counseling is important where such facilities are available. Risk of recurrence and possibility of prenatal diagnosis should be communicated to prevent the birth of another affected child after the diagnosis of brain malformation in an index case. Severe and diffuse malformations tend to have grave prognosis for development, seizure control, and survival. It occurs in 1 in 250 pregnancies but only in 1 in 10,000 live births as majority of the affected fetuses do not survive till delivery. In addition to nonseparation of the cerebral hemispheres, there is variable degree of nonseparation of hypothalamic, thalamic, lentiform and caudate nuclei. The alobar holoprosencephaly is the most severe, showing almost complete absence of separation of the cerebral hemispheres with characteristic midline single ventricle (a crescent-shaped monoventricle) which may communicate with a dorsal cyst. The corpus callosum, falx cerebri and interhemispheric fissure are absent as are the olfactory bulbs and tracts. As an accompaniment, corpus callosum shows absence of genu and body and only splenium is present posteriorly. The frontal horns of lateral ventricle are absent and only occipital horns and trigones are present. Septum pellucidum is absent and third ventricle tends to be small due to partial separation of deep gray nuclei. Rudimentary frontal horns may be present and only genu of corpus callosum is absent. In the midline interhemispheric variant (syntelencephaly), cerebral hemispheres show lack of separation across the midline affecting the posterior frontal and parietal lobes with absent corpus callosum in the corresponding region. Anterior frontal lobes, basal forebrain and occipital lobes are normally separated. With the advent of advanced neuroimaging techniques, milder forms are being increasingly recognized. Maternal diabetes, fetal exposure to alcohol and retinoic acid have the strongest association. Other reported risk factors such as hypocholesteremia, viruses, toxins and medications have also been reported. Facial midline abnormalities include hypotelorism, flattened nasal bridge, median cleft lip and palate, or a single median maxillary central incisor. Cyclopia, with the presence of a single median eye and a proboscis, can be present. Patients tend to have microcephaly in the absence of hydrocephalus which may complicate the clinical course in some children. Endocrinopathies are common due to hypothalamic involvement and especially frequent is the diabetes insipidus. Growth hormone deficiency, hypocortisolism, and hypoparathyroidism may be seen less commonly. Special attention need to be paid to the feeding and swallowing dysfunction to prevent malnutrition and may require gastrostomy tube. Diabetes insipidus and other endocrinopathies need early detection and intervention. Causes of death include aspiration pneumonia, severe dehydration from diabetes insipidus and rarely intractable epilepsy. In familial cases where causative gene has been identified, prenatal diagnosis is through genetic testing by means of amniocentesis or chorionic villous biopsy. Systemic Disorders Agenesis of Corpus Callosum Corpus callosum is the largest white matter tract in the brain connecting the two cerebral hemispheres and providing the pathway for communication between them. It develops between the 8th week and 14th week of fetal life and the axons that traverse it connect the homotopic regions of the cerebral hemispheres. It can occur as an isolated entity or more commonly associated with other malformations of brain or cortical development. Some patients have abnormalities in organ systems outside central nervous system commonly affecting renal, musculoskeletal or ophthalmological structures and defining specific genetic/ malformation syndromes. Clinically, the children may come to attention at birth manifesting hypoglycemia secondary to pituitary insufficiency, and are found to have microphallus, undescended testes, and midline birth defects such as cleft lip or palate. Many patients have addition brain malformations which may account for occurrence of seizures, developmental delay or cerebral palsy in the affected children. Particular attention needs to be given to endocrinological evaluation, treatment and monitoring. Chiari 1 malformation this anomaly refers to the downward displacement of cerebral tonsils of at least 35 mm through foramen magnum into the spinal canal. The reasons for downward herniations are not clear through several theories such as traction by tethered cord, and small posterior fossa has been proposed. Clinically, patients may be entirely asymptomatic coming to attention through neuroimaging done for some other purposes. Those who are symptomatic frequently manifest posterior headache that is increased with Valsalva maneuvers. Compression of brainstem and spinal cord may occur manifesting with long tract signs such as spasticity, hyper-reflexia, urinary incontinence, ataxia or sensory changes. Presentation may be complicated by the development of syringomyelia in some patients. Treatment where indicated is surgical decompression of the posterior fossa and duraplasty.
Generic extra super avana 260mg line
Malar rash can appear as a blush or a maculopapular eruption with associated scaling and usually is not pruritic erectile dysfunction medication for high blood pressure extra super avana 260mg visa. Discoid lupus, named after its coin shape, is an erythematous rash that primarily affects the face, ears, and scalp, although the upper extremities, upper chest and back may be affected. The central area may be hypopigmented, whereas the active border may appear hyperpigmented. The lesions may heal with a scar or atrophy, and discoid patches on the scalp may result in a scarring alopecia if the hair follicles are damaged. Severe ulcerating lesions may signify more significant disease activity in other organs, whereas the appearance or reappearance of a malar rash often heralds a disease flare. The affected area becomes pale and painful, then cyanotic, and on rewarming, erythematous. There may be an associated tingling or burning sensation, especially during the rewarming, erythematous phase. For the purpose of identifying patients in clinical studies, a person shall be said to have systemic lupus erythematosus if any 4 or more of the 11 criteria are present, serially or simultaneously, during any interval of observation. Clinical and laboratory characteristics and long-term outcome of pediatric systemic lupus erythematosus: a longitudinal study. Renal involvement manifests as proteinuria, microscopic hematuria, hypertension, or elevated blood urea nitrogen and creatinine level. Because class and severity of the renal disease guides treatment, biopsy results play a major role in determining therapy. A renal biopsy with histologic, immunofluorescent, and electron of antiphospholipid antibodies. Arthritis presents as symmetrical involvement of both the large and small joints, primarily involving the knees, wrists, ankles, and fingers. The affected joints usually have only mild to moderate joint effusions; however, significant joint-line tenderness and painfully reduced range of movement may be present. This class does not require specific treatment and generally has a good prognosis. This class of renal disease is considered very mild, but there is always a risk of progression. Nephrotic syndrome, hypertension, and abnormal blood urea nitrogen and creatinine levels may be prevalent. The most significant lesions associated are widespread subendothelial immune deposits and proliferation of the mesangial cells. Membranous nephritis (Class V) occurs in 1020% of patients who have renal disease. Flares can be frequently detected by increasing proteinuria before the recurrence of constitutional symptoms like fever, weight loss, increasing hair loss and oral ulcers. A few isolated subepithelial or subendothelial deposits may be visible by immunofluorescence or electron microscopy, but not by light microscopy. A segmental lesion is defined as a glomerular lesion that involves less than half of the glomerular tuft. This class includes cases with diffuse wire loop deposits but with little or no glomerular proliferation. The classification of glomerulonephritis in systemic lupus erythematosus revisited. In 1999, 2754 Systemic Disorders the American College of Rheumatology classified neuropsychiatric involvement into 19 separate disease entities Table 4). Characteristically, the hallucinations have features of an organic psychosis, including visual or tactile hallucinations. Decreased concentration and cognitive dysfunction, psychosis, seizures, transverse myelitis, central nervous system vasculitis, or stroke are the other most common neuropsychiatric manifestations. When present, cerebrovascular disease usually involves the microcirculation, and therefore angiographic studies are usually normal except in the presence of a stroke. Both lymphopenia and granulocytopenia can be present, but lymphopenia is more common. Lymphopenia is a sensitive marker of general disease activity and does not require specific therapy. The clinical spectrum includes pleuritis, pneumonitis, infectious pneumonia, pulmonary hemorrhage, pulmonary hypertension, and pneumothorax. Uncommon manifestations are diaphragm involvement (including shrinking lung syndrome), vasculitis and pulmonary embolus. Severity of pulmonary involvement ranges from asymptomatic abnormalities of pulmonary function tests to severe life-threatening pulmonary hemorrhage. Hematologic Involvement Anemia, thrombocytopenia, and leukopenia are seen in 5075% of patients. The Coombs test is positive in approximately 3040% of patients, but only less than 10% of patients have overt hemolysis. Cardiac Involvement Symptomatic pericarditis with pericardial effusion is the most common cardiac manifestation, occurring in approximately 15 25% of patients; up to 68% of patients have echocardiographic abnormalities consistent with pericarditis. Less commonly, endocarditis or myocarditis or valvular disease occurs and rarely ischemic heart disease may result secondary to coronary artery vasculitis. Valvular heart disease may be associated with the presence of antiphospholipid antibodies and noninfective or Libman-Sacks endocarditis. Table 4 Nomenclature and case definitions for neuropsychiatric lupus syndromes Central nervous system · Asepticmeningitis · Cerebrovasculardisease · Demyelinatingsyndrome · eadache(includingmigraineand H benign intracranial hypertension) · ovementdisorder(chorea) M · Myelopathy · Seizuredisorders · Acuteconfusionalstate(<1%) · Anxietydisorder · Cognitivedysfunction(5580%) · Mooddisorder(1457%) · Psychosis(08%) Peripheral nervous system · cuteinflammatory A demyelinating polyradiculoneuropathy (GuillainBarrй syndrome) · Autonomicdisorder · ononeuropathy(single/ M multiplex) · Myastheniagravis · Cranialneuropathy · Plexopathy · Polyneuropathy Gastrointestinal and Liver Disease Gastrointestinal involvement occurs in 2040% of patients. Abdominal pain can result from peritoneal inflammation (serositis), vasculitis, pancreatitis, malabsorption, pseudoobstruction, paralytic ileus, or direct bowel wall involvement (enteritis). Lupus enteropathy may present as acute ischemic enteritis or a protein losing enteropathy. Bowel wall inflammation presenting as cramping abdominal pain and diarrhea can reflect enteritis or may be secondary to a mesenteric vasculitis or thrombosis. Pancreatitis is uncommon, with an overall incidence of less than 5%, and may reflect active disease, an infectious complication, or be secondary to drug therapy like steroids or azathioprine. Hepatomegaly occurs in 4050% of patients and up to 25% have abnormal liver function tests. Markedly elevated liver function Reproduced from the American College of Rheumatology. Irregular menses frequently are related to active disease and usually resolve when the disease is controlled. Mothers should be started on dexamethasone as soon as a fetus is identified as having heart block to decrease maternal antibodies and inflammation of the conducting system and to delay the onset of fibrosis. Juvenile systemic lupus erythematosus: review of clinical features and management. Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Pattern of neuropsychiatric manifestations and outcome in juvenile systemic lupus erythematosus. Systemic lupus erythematosus is a periodic disease hence frequently leading to delay in diagnosis. Gastrointestinal disease, significant liver involvement, myositis, and myocarditis are rare in children. Malar or butterfly rash is the most common cutaneous manifestation and hallmark of the disease. Isolated discoid lupus erythematosus without systemic involvement is rarely seen in the pediatric age group. A true lupus headache is refractory to standard analgesic treatment requiring narcotic analgesia. Measurement of autoantibodies in pediatric-onset systemic lupus erythematosus and their relationship 2756 Chapter 46. In the remaining few, it is generally felt that faulty dilution technique or method of detection are the culprits. These patients may develop higher morbidity due to recurrent thrombotic tendencies, renal and neuropsychiatric complications and pregnancy related complications. Lupus anticoagulant, anticardiolipin antibodies and b2-glycoprotein antibodies are forms of antiphospholipid antibodies that can be tested.
Buy 260mg extra super avana
Generally erectile dysfunction video buy cheap extra super avana 260mg online, a 13 months course is sufficient, provided no further seizures have occurred. Else, it is to be repeated after 24 weeks of initiation of medical therapy to document the change in size of abscess and resolution. Surgical Treatment Neurosurgeon should be involved early in the course of therapy. The choice of surgical procedure has not been found critical in deciding the outcome of the case and should depend upon the surgical expertise available and the hemodynamic status of the child. Deep-seated abscess, small abscess and those involving eloquent cortical regions are preferably drained using stereotactic aspiration and aspiration via craniotomy or craniectomy or excision is performed in superficial abscess or abscess located in the posterior fossa. Management of Brain Abscess in an Immunocompromised Child Apart from the typical bacterial organisms, Mycobacterium tuberculosis and fungal organisms such as Aspergillus, Nocardia, Candida and Mucor are the common causes of brain abscess. Empirical therapy should be avoided in immunocompromised patients and every effort should be made in establishing a microbiological diagnosis. With advent of newer neuroimaging modalities, antibiotic therapy, the mortality has reduced from 3060% in the preimaging era to 325%. Rupture of abscess into the ventricles and posterior fossa location are associated with rapid deterioration and a very high mortality rate. Common neurological sequelae are delayed onset seizures (commonly seen with frontal lobe abscess), mental retardation and focal neurological deficits. Brain abscess is a focal intraparenchymal pus collection with microorganism seeding occurring from contiguous, hematogenous or direct inoculation. Brain abscess associated with hematogenous spread are often multiple in number and generally located in the distribution of middle cerebral artery. The most common microorganisms causing brain abscess in children worldwide are aerobic and anaerobic streptococci. The causative organism usually depends upon immune status of the child and source of primary infection. Magnetic resonance imaging of brain with gadolinium is the imaging modality of choice for diagnosing brain abscess. Lumbar puncture is contraindicated in brain abscess with significant mass effect due to risk of sudden herniation and collapse. Successful treatment of brain abscess requires prompt and appropriate antimicrobial therapy combined with surgical drainage in most cases. Broad-spectrum antibiotic cover until culture reports are available should be empirically initiated. Duration of antibiotic treatment should be at least 46 weeks in surgically drained abscess and 68 weeks in surgically untreated cases. Consensus document on controversial issues for the treatment of infections of the central nervous system: Bacterial brain abscesses. Clinical and microbiologic features guiding treatment recommendations for brain abscesses in children. Microbiological spectrum of brain abscess at a tertiary care hospital in South India: 24-year data and review. The study of etiologic and demographic characteristics of intracranial brain abscess: a consecutive case series study from Pakistan. Brain abscess: management and outcome analysis of a computed tomography era experience with 973 patients. Brain abscess in children: epidemiology, predisposing factors and management in the modern medicine era. Demyelination or loss of myelin of the white matter which is a key feature of these disorders can be either primary or secondary. The secondary demyelinating disorders result from infectious, ischemic, metabolic or hereditary disorder. The etiology of primary demyelinating disorders is unclear but thought to be multifactorial. These conditions can be monophasic, relapsing remitting or progressive and can have a highly localized or diffuse involvement of the central nervous system. The prognostic and therapeutic implications necessitate a proper diagnostic classification of these disorders at onset. The International Pediatric Multiple Sclerosis Study Group has proposed consensus definitions for demyelinating disorders in children to aid in standardization of diagnosis, investigations and further research. This chapter discusses the consensus definitions, different clinical phenotypes, differential diagnoses, diagnostic evaluation and approach to classification, management and outcome of primary inflammatory demyelinating disorders of the central nervous system in children. The antigenic trigger activates the T-cells which cross the blood-brain barrier and react against myelin epitopes. Multifocal and diffuse lesions are found in gray matter, white matter and spinal cord. Children may present with multifocal neurological signs such as hemiparesis, paraparesis, unilateral or bilateral pyramidal signs, cranial nerve deficits, ataxia, visual loss due to optic neuritis, seizures, slow or slurred speech or aphasia and sensory symptoms. Respiratory failure secondary to brainstem involvement or severely impaired consciousness can occur. Different patterns of contrast enhancement can be present and include open ring and nodular enhancement. Spinal fluid examination is mandatory in a child who presents with acute neurological deficit. Cerebrospinal fluid findings are usually abnormal showing a moderate pleocytosis with elevated protein content. The incidence of acquired demyelinating diseases in population-based studies range between 0. Prevalence is expected to be high in resource poor settings because of the proposed role of antecedent infections in the etiology of acute demyelinating disorders. Treatment Treatment of acute inflammatory demyelinating disease requires that other possible diagnoses, especially infectious, neoplastic and metabolic disorders are carefully excluded. The mainstay of acute therapy for all inflammatory demyelinating central nervous system disorders are corticosteroids. Intravenous steroids are required to shorten the acute inflammatory process and hasten recovery. Duration of taper less than 3 weeks has been associated with an increased risk of relapse. The infectious agents serve as an antigenic trigger which Prognosis Acute disseminated encephalomyelitis is a monophasic illness. No encephalopathy (no alteration in consciousness or behavior that cannot be explained by fever) 4. The 2010 Revised McDonald criteria for dissemination in time can be satisfied by the emergence of new T2 lesions (with or without enhancement) on serial scans or can be met on a single baseline scan if there exists simultaneous presence of a clinically silent gadolinium-enhancing lesion and a nonenhancing lesion. Factors associated with a decreased relapse include age less than 10 years of age, encephalopathy, postinfectious presentation, isolated transverse myelitis, meningism or seizures. Comparison of clinical and magnetic imaging features between acute disseminated encephalomyelitis and multiple sclerosis is given in Table 2. Studies have shown that in children vaccinated after the first episode of demyelination neither tetanus nor hepatitis B vaccination increased the risk of conversion. Clinical Features Diagnosis of multiple sclerosis is defined by recurrent attacks of inflammatory demyelination. Presenting features include motor deficits, sensory dysfunction, brainstem symptoms, optic neuritis and ataxia. Most patients in the adolescent age group experience the second attack of demyelination within 1 year, whereas children below 10 years have a longer attack interval. Even though the course is most often relapsing remitting in the beginning, patients develop permanent physical disability, spasticity, tremor, or bladder dysfunction over time. Etiopathogenesis Environmental factors have been implicated in the susceptibility of children to multiple sclerosis. Three important factors are: (1) vitamin D deficiency; (2) viral infections, particularly Epstein-Barr virus, herpes virus and varicella zoster; (3) exposure to cigarette smoke. The scale quantifies disability in five functional systems namely pyramidal, cerebellar, brainstem, sensory, bowel and bladder, visual, cerebral and others. There are no biologic markers that can distinguish multiple sclerosis from other demyelinating disorders. Intrathecal oligoclonal bands in the cerebrospinal fluid detected by isoelectric focusing are a feature of multiple sclerosis. Neurophysiological testing such as visual and auditory evoked potentials is also of diagnostic importance in detecting subclinical evidence of demyelination. Treatment All acute relapses of multiple sclerosis should be treated by intravenous corticosteroids.
260 mg extra super avana fast delivery
Most authors recommend a 46 weeks intravenous antibiotic therapy for surgically drained bacterial abscess and a 68 weeks therapy when medical therapy is solely offered erectile dysfunction at the age of 21 generic 260 mg extra super avana with amex. Immunocompromised children may require a longer duration with additional cover for atypical organisms. Cerebritis may require a shorter duration compared to a fully encapsulated abscess. Role of Oral Antibiotics No data is available to recommend or refute oral antibiotic therapy. However, oral drugs often fail to penetrate blood-brain barrier and do not achieve the minimal inhibitory concentration for most of the microorganisms within the abscess. They are however indicated in children with signs of impending herniation secondary to mass effect caused by massive perilesional edema. The duration of antiepileptics depends upon the imaging and electroencephalographic findings. A second pulse of methyl prednisolone may be necessary in children with severe symptoms not responding sufficiently to the first course of corticosteroids. The available literature on the use of interferon and glatiramer acetate in pediatric patients is restricted to tolerability data in isolated small case series or case reports. This is due to the brief subclinical phase, immaturity of myelin system, and immunologic immaturity. In addition children may differ in their innate capacity for myelin repair leading to fundamental differences in the appearance of white matter lesions. Despite the dramatic appearance of the lesions, resolution of the initial lesions may be seen. Clinical Features Neuromyelitis optica is an inflammatory disease of the central nervous system that preferentially affects the optic nerves and spinal cord. Neuromyelitis optica spectrum is now recognized to typically evolve as a relapsing disorder and include patients with unilateral optic neuritis and myelitis occurring weeks or even years apart. A variety of extraneurological manifestations such as intractable vomiting, anorexia and weight loss have also been described as the presenting manifestation of these patients. These symptoms are attributed to the highly specific involvement of certain brain regions such as hypothalamus and medullary centers in these patients. Magnetic resonance imaging may show signal intensity changes in the optic nerve with gadolinium enhancement. When occur, they are not oval or ovoid or perpendicularly located as in lesions of multiple sclerosis, but tend to be punctate small round dots. A cloud-like enhancement defined as multiple patchy enhancements with blurred margins in adjacent regions in contrast to the isolated spotty enhancement seen in multiple sclerosis may also help differentiating neuromyelitis optica from multiple sclerosis on imaging. Cerebrospinal fluid examination includes a marked elevation in white cell count (often polymorphonuclear) in addition to elevated protein. In contrast to multiple sclerosis, only a small percentage of the patients show presence of oligoclonal bands. Seropositive patients tend to have relapsing remitting course and the long-term prognosis is poor. Plasmapheresis should be initiated if a severe attack does not respond promptly to corticosteroids. This is especially important in cases of ascending cervical myelitis because 2346 system site such as optic neuritis, transverse myelitis, brainstem, cerebellar or hemispheric lesions. Optic neuritis is defined by acute or subacute visual loss, restricted visual fields and pain with ocular movement. A brief description of the clinical features and diagnostic evaluation in patients with acute transverse myelitis is given below. If the clinical features are characterized by signs and symptoms attributable to more than one central nervous system sites, the event is referred as polyfocal. The event should not include encephalopathy, though in brainstem syndromes encephalopathy may be present. The classification is purely based on clinical features rather than magnetic resonance imaging findings. It is typically preceded by a mild illness in the 3 weeks prior to symptom onset, as reported in 50100% of patients. The criteria for diagnosing transverse myelitis include sensory, motor, or bladder or bowel dysfunction attributable to the spinal cord, with progression to nadir in less than 21 days from onset. Initial evaluation should include a gadolinium-enhanced magnetic resonance imaging of the spine to exclude a compressive myelopathy. Magnetic resonance imaging usually shows hyperintense signal changes on T2W sequences. Lesions of acute transverse myelitis in children are typically longitudinal, may demonstrate enhancement and are centrally located. If there is no evidence of a compressive lesion, a lumbar puncture should be performed. Other investigations recommended include parainfectious markers like virological serology. If there are features to suggest a systemic inflammatory disorder, autoimmune screening and serum angiotensin-converting enzyme levels are indicated. High-dose corticosteroids have shown to have beneficial effect and hasten recovery. In tropical countries, infections of the central nervous system should be an important diagnostic consideration due to the therapeutic implications. When there is complete ring enhancement of the lesions the differential diagnoses include brain abscess, tuberculoma and toxoplasmosis. When there is contrast enhancement, primary or secondary lymphoma also should be considered. Mutifocal discrete white matter lesions also may suggest primary or secondary central nervous system vasculitic disorders and noninfectious granulomatous disorders like neurosarcoidosis. Inherited disorders to be considered are leukodystrophies and mitochondrial disorders, especially when there is a progressive course. All patients should be evaluated with neuroimaging preferably magnetic resonance imaging and cerebrospinal fluid testing. Magnetic resonance imaging of the brain and spinal cord with and without gadolinium should be obtained in all children with an initial demyelinating event. The work-up should also include cerebrospinal fluid studies including cell count with differential, total protein, IgG index, evidence of oligoclonal bands. In addition to the routine testing, cerebrospinal fluid should be sent for infectious screening and virological studies, especially when the clinical features suggest an underlying infectious process. Neurophysiological testing such as visual evoked potentials, somatosensory evoked potentials and brainstem auditory evoked potentials is of additional diagnostic value. Evoked potential studies aid in localization of lesions and confirm organic basis for clinically ambiguous symptoms. Furthermore, evoked potential studies can identify clinically silent lesions, thereby providing objective support for dissemination in space in children with suspected multiple sclerosis. A broad approach to diagnosis and classification in children with demyelinating disorders are shown in Flow chart 1. Differential Diagnosis the differential diagnoses for a child who presents with an acute neurological deficit and white matter lesions on neuroimaging is wide. Contrast enhancement may suggest an infectious, inflammatory or granulomatous disorder. Most often neuroimaging is the first available investigation and a critical look at the magnetic resonance image helps in formulating the differential diagnosis. The features to be looked are size and nature of the lesions (multifocal discrete, confluent or diffuse), topographical distribution of the lesion (predominantly white matter, basal ganglia, thalamus, brainstem, cerebellum) pattern of contrast enhancement (complete ring/ open ring/patchy/diffuse enhancement). Central nervous system inflammatory demyelinating disorders comprise a group of disorders with heterogenous clinical manifestations. Early and correct diagnostic categorization in these children has prognostic and therapeutic implications. Multiple sclerosis and acute disseminated encephalomyelitis diagnosed in children after long-term follow-up: comparison of presenting features. Clinical, environmental, and genetic determinants of multiple sclerosis in children with acute demyelination: a prospective national cohort study. Consensus definitions proposed for pediatric multiple sclerosis and related disorders.
Cheap 260mg extra super avana fast delivery
Patients with confirmed hypertension should be evaluated carefully to identify the underlying etiology erectile dysfunction age young buy cheapest extra super avana, determine comorbidities and detect target-organ damage. Therapeutic lifestyle modification should be advised in all hypertensive children. Pharmacologic therapy is required in those with secondary hypertension, stage 2 or symptomatic hypertension and in the presence of end-organ damage. Since there is no consensus on the first-line antihypertensive agent, medications should be prescribed rationally based on the underlying cause and risk of side effects. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. The initial urinary stream washes away distal urethral organisms and should be discarded. Cleaning of the vulva in prepubescent girls or the meatus in boys is not necessary. Early morning urine samples harbor greater bacterial counts but are less amenable to outpatient practice. In neonates and infants particularly girls, the best technique for obtaining an uncontaminated specimen is suprapubic aspiration from the bladder. It can be performed safely using a 21-gauge needle, 12 cm above the pubic symphysis. Occasionally parents may succeed in collecting a clean-catch sample in a male infant. Bag specimens have unacceptably high contamination rate, even with thorough cleaning of the prepuce or the perineum and are not recommended. Use of diapers or absorptive pads for collecting urine for culture is not recommended. In children with indwelling catheters, urine can be aspirated from the catheter using a sterile needle and syringe. Obtaining appropriate urine specimen is difficult in patients with ureterostomy or vesicostomy. Catheterization of the stoma under asepsis is recommended and the culture result should be interpreted as any catheter specimen. If delay of more than 2 hours is anticipated, the specimen can be stored in a refrigerator at 4єC for up to 72 hours before plating. This would preserve the white cell count and prevent growth of contaminating bacteria. Organisms such as Klebsiella, Proteus, Enterobacter, Staphylococcus and Streptococcus faecalis are identified in immunocompromised hosts, patients with prolonged urinary catheterization and in nosocomial settings. Infection with Candida may be seen in preterm infants, immunocompromised children and following prolonged antibiotic therapy. Ascending infection from the urethra to bladder and the kidneys is common in older children. Direct extension of infection can occur in the presence of fistulas from vagina or intestines to the urinary tract. Irrational antibiotic therapy may lead to fecal recolonization with virulent bacteria thereby predisposing to bacteriuria by disrupting the normal periurethral flora. However, a major drawback of urine culture is the time-delay between collection of the specimen and identification of bacterial growth. Nitrate reductase It is based on reduction of nitrate to nitrite by nitrate reductase enzyme present in most coliforms. The sensitivity of nitrite test is low in infants who void frequently and have short bladder incubation time. Sometimes the child may present with recurrent fever, diarrhea, vomiting, abdominal pain and poor weight gain. Urinary symptoms such as burning, urgency, frequency, flank pain, turbid urine, intermittent voiding dysfunction and a recent onset of enuresis are seen in older children. It is difficult to predict based on symptoms whether a child has localized cystitis or pyelonephritis. The choice of antibiotic should be guided by the most likely organism and its local susceptibility pattern. A third-generation cephalosporin (cefotaxime or ceftriaxone) is preferred Table 3). Usually a single antimicrobial should be used in community-acquired infections and combinations should be reserved for critical cases. Oral cefixime is as efficacious as parenteral therapy in children with suspected acute pyelonephritis. Intravenous therapy with single daily dose of aminoglycoside has also been found to be safe and effective. Once the result of antimicrobial sensitivity is available, treatment may be modified accordingly. When the clinical condition improves and the child is accepting by mouth, oral antibiotics may be started. Systemic Disorders whom the preputial bacteria may reduce nitrite and give a falsepositive result. Leukocyte esterase A chloroacetate stain reacts with the enzyme leukocyte esterase found in neutrophil granules. It is more accurate than microscopy because enzyme activity is still retained when white cells have disintegrated. Detection of bacteriuria Microscopy of uncentrifuged, unstained urine will detect more than 104 bacteria/mL of urine. The presence of a single bacterium in a centrifuged or a Gram stained fresh urine specimen has a high sensitivity and specificity for predicting a positive urine culture. Urine Culture On culture, the bacterial count is important to differentiate true infection from contamination by periurethral flora. The cut-off figures for significant bacteriuria vary with the method of urine collection Table 2). A urine culture should be repeated in case of mixed growth suggestive of contamination. Nonspecific markers of inflammation such as leukocytosis, raised C-reactive protein do not provide confirmatory evidence of pyelonephritis. Even under effective therapy, proven with repeat urine cultures, fever may persist for up to 3 days. Failure to respond to therapy may be due to presence of resistant pathogens, complicating factors, or noncompliance. Ultrasonography should be performed early if the expected clinical response is not observed. Routinely a urine culture to document response to therapy is not necessary and should be repeated only if the patient fails to respond to the therapy. It is a noninvasive test that can demonstrate the size the shape of the kidneys such as solitary or dysplastic kidney, horseshoe kidney and the presence of ureterocele. The procedure requires intravesical administration of an echo-enhancing agent (air-filled microbubbles) through transurethral catheterization. It is characterized by decreased radiotracer uptake caused by cortical ischemia and tubular dysfunction during acute infection. Only a few well-designed studies have tested the value of these imaging protocols. It is presumed that most vulnerable children would have already developed scars in infancy. Milder reflux that may be missed by this approach, is assumed to not to be contributing to renal scarring. Medications used for prophylaxis Table 3) are usually given as single bedtime dose. The ideal antibiotic for prophylaxis should have a broad spectrum of action and achieve a high urinary concentration with minimal alteration of the bowel flora. Nitrofurantoin and cotrimoxazole are the most commonly used drug for long-term prophylaxis.
Buy extra super avana on line amex
Mostly diagnosis is made by radioimaging erectile dysfunction jokes purchase cheap extra super avana online, but a stereotactic diagnostic biopsy can help in establishing accurate diagnosis. Fever, headache, and radiating root pain accompanied by myelopathy are the features of acute form. Chronic variety is usually localized to a few segments and presents with progressive spinal cord compression. Treatment of tuberculous hydrocephalus depends on the level of the cerebrospinal fluid obstruction. Spinal cord and nerve roots are surrounded by the inflammatory exudates but not infiltrated by exudates. Neuronal injury occurs by direct compression and ischemia caused by small vessels involvement with periarteritis. Clinical features of involvement of spinal cord or nerve root or both may be present. Myelography shows characteristic findings in the form of poor flow of contrast material with multiple irregular filling defects, cyst formation and sometimes spinal block. Systematic review and meta-analysis of the current evidence on the duration of protection by bacillus Calmette-Guйrin vaccination against tuberculosis. Some cause epidemics, some are sporadic infections and a few are endemic to certain regions. In the developing world, vector breeding is facilitated due to poor environmental hygiene; and this, concurrent with the poor host immunity and vaccination coverage, make encephalitis a significant public health issue. There were outbreaks of Chandipura virus in Andhra Pradesh in 2003; in Gujarat in 2004; in Nagpur in 2005 and 2007 and sporadic cases from 2005 to 2006 in Andhra Pradesh. Nipah virus encephalitis epidemics were reported in 2001 and 2007 from West Bengal. In acute viral encephalitis, a remarkable pathological finding is the infiltration of mononuclear inflammatory cells in the Virchow-Robin spaces and in the meninges around the wall of vessels (perivascular cuffing). With further disease progression, astrocytosis proliferation and hypertrophy of microglial cells with formation of microglial aggregates (microglial nodules) and neuronophagia (clusters of microglial cells surrounding a dead neuron) become prominent histopathological findings. The virus traverses mucous membranes and then travels by retrograde axonal transport to the trigeminal ganglion, where it remains dormant. There is periodic activation and anterograde axonal transport to allow viral shedding and infection of new hosts. Japanese B encephalitis Soon after the mosquito inoculates a patient, there is viral multiplication in the skin; this results in viremia and later invasion of the nervous system. Inflammatory demyelinating diseases like acute disseminated encephalomyelitis, acute renal failure, hepatic failure, intoxication with drugs or poisons, Reye syndrome, autoimmune encephalitis, and cortical venous thrombosis may be considered as differential diagnoses depending upon the clinical scenario. The onset of the illness, any other associated medical illness, telltale evidence of other illness like an odor, rashes or signs of trauma should be picked up. The constellation of presenting symptoms, the course of illness and the findings on examination should be analyzed systematically to arrive at a diagnosis and to plan investigations. If the patient with encephalitis has concomitant myocarditis, pleurodynia, herpangina or hemorrhagic conjunctivitis an enterovirus should be suspected. Signs of hemorrhage may also be seen with Dengue virus, Yellow fever virus and Rift Valley fever virus. Fever abates in 23 weeks when the involuntary movements become more obvious and occur in the form of choreoathetosis or ballism. Presence of movement disorders, orofacial dyskinesias, seizures that are resistant to treatment and a subacute onset should point to an autoimmune encephalitis and the appropriate investigations should be planned. The latter is most common and in arthropod-borne infections is associated with alterations of the blood-brain barrier. Rabies virus may reach the brain by inhalation when a person enters a cave infested with infected bats or inhalation from aerosols in the laboratory. Following the bite, the Rabies virus which has an affinity for nicotinic receptors invades the muscle. It is not known for certain whether the virus invades the muscle spindles or the motor end plates; or whether the superficial sensory nerve endings are invaded. Postviral encephalomyelitis refers to a demyelinating illness occurring within 2 weeks of the rash and consists of altered mental status, seizures, and focal neurological deficits. Measles inclusion body encephalitis presents with dementia, behavioral abnormalities, myoclonus, seizures and even coma. Gradually there will be affection of the pyramidal and extrapyramidal tracts with macular pigmentary degeneration. Rabies encephalitis often has to be distinguished from demyelination after rabies vaccine given as postexposure prophylaxis. The features that help one to distinguish rabies encephalitis from postvaccinial demyelination would include presence of hydrophobia or/and aerophobia, autonomic features like salivation, and rapid progression which favor rabies. A careful search should be made for the skin lesions of dengue, chikungunya, herpes zoster and hand foot and mouth disease. Hypertension in the child with altered sensorium would open up another set of diagnoses to pursue. If the patient has psychiatric symptoms, intractable seizures and new onset movement disorders with coma or if the patient has telltale evidence of an ongoing malignancy; antibodies to N-methyl-D-aspartate receptor and voltage-gated potassium channels should be checked. If the child with encephalitis has associated atypical pneumonia, Mycoplasma and Chlamydia serology and cold agglutinins in serum should be sought. Diagnostic investigations for immunocompromised patients with altered consciousness are given in Box 2. Stereotactic Brain Biopsy Stereotactic brain biopsy may be considered in cases where no diagnosis has been reached and if the patient is deteriorating. If there is no focal lesion, the biopsy is taken from the nondominant frontal lobe. An experienced neurosurgeon and an experienced histopathologist are prerequisites for a brain biopsy. When the etiology is not clear, other microbiological investigations must be obtained. These are also required in epidemic situations, where the etiology has not been established. The local health authorities must be informed, and a microbiologist should be consulted when taking the samples. These samples include urine, throat swab, nasopharyngeal aspirate, serum (acute, and convalescent after 2 weeks) and swab from vesicles or rash, if present. Magnetic Resonance Imaging Magnetic resonance imaging (including diffusion weighted imaging should be done in all patients, ideally within 24 hours if not within 48 hours). Magnetic resonance spectroscopy, positron emission tomography and single-photon emission computed tomography are not indicated in suspected viral encephalitis. Supportive care assumes great importance in the management of viral encephalitis with immediate attention to the airway, breathing and circulation. Seizures should be managed with timely recognition and treatment of nonconvulsive seizures. Ventilatory support, oxygenation and management of shock and syndrome of inappropriate antidiuretic hormone secretion should be instituted whenever necessary. In areas endemic for malaria, empirical treatment for the same is started until a definite other diagnosis is established or malaria is ruled out. Doxycycline should also be initiated if the chances for a rickettsial or ehrlichial infection are high. Intravenous macrolides are included in the regime if there is suspicion of Mycoplasma pneumoniae encephalitis. Nutrition of the child should be supervised; the feeding tube, urinary catheter and tracheostomy should be tended carefully. Sessions with the psychologist, physiotherapist, occupational and speech therapist should be begun early. Incomplete surveillance in many affected areas gives a false idea about the mortality. In order to ensure that no case is missed, it is mandatory to report cases of acute encephalitic syndrome. Children with suspected viral encephalitis are often inadequately investigated and managed. Treatable differential diagnoses should always be considered during the evaluation of a patient with acute encephalitis syndrome. If bacterial meningitis cannot be ruled out or until it is ruled out, patient should receive treatment for pyogenic meningitis. In case of suspicion of rickettsial or ehrlichial infection, doxycycline should be given.
Purchase cheap extra super avana
Dietary phosphate is absorbed through the small intestine impotence husband buy extra super avana amex, predominantly in the jejunum. To maintain balance, the amount of phosphate absorbed in the intestine is similar to Systemic Disorders the amount excreted in the urine. Children with chronic kidney disease have growth retardation, bone deformities and anemia. Hypophosphatasia is characterized by disordered mineralization of bones secondary to deficient tissue nonspecific alkaline phosphatase activity, resulting from loss of function mutations in the liver/bone/kidney alkaline phosphatase gene. Deformities noted in the childhood variant include enlarged joints, dolichocephaly, short stature and waddling gait. Signs of intracranial hypertension, failure to thrive, fractures and bone pain are common. Radiographs show widespread demineralization and rachitic changes at ends of metaphysis. Low serum levels of alkaline phosphatase and increased urinary phosphoethanolamine support the diagnosis. High levels of fluorine are reported in drinking water from Seemandhra, Telangana, Gujarat and Rajasthan. Features of hypophosphatemic rickets include bowing of legs, muscle weakness, bone pain and short stature. Clinical findings are limited to legs and findings like rachitic rosary and wrist widening are usually absent. Urine is analyzed for calcium, phosphate and creatinine on timed and spot specimens. Serum concentrations of phosphate (P) depend on intestinal absorption, renal elimination and release from bone. The use of multiple daily doses is advised as serum phosphate levels return to low baseline values within a few hours of phosphate supplementation. Flow chart 1 Diagnostic approach to refractory rickets In addition, an active form of vitamin D (12 µg/day alfacalcidol or 0. The dose of vitamin D analog is increased during periods of increased growth velocity and decreased after healing of rickets; the dose is titrated to achieve normal levels of alkaline phosphatase, improve bowing and growth velocity, while avoiding hypercalciuria. Optimal therapy is indicated by the resolution of bone pains (within a few weeks), return to normal of levels of alkaline phosphatase (within a few months), increase in growth velocity (in a year) and straightening of legs (in 34 years). Persistence of leg bowing persists despite optimal treatment requires consideration of surgery, preferably beyond growing age. Improvement in serum calcium occurs within days, radiologic improvement within 23 months while the rickets heals by 910 months. Phosphate supplements are not required if correction of serum calcium results in improvement in secondary hyperparathyroidism that causes hypophosphatemia. The requirement of alkali typically decreases from 58 mEq/kg/day in infancy to 34 mEq/kg/day in childhood and 12 mEq/kg/day in adults. Compliance is hindered by the need for multiple daily doses and bitter taste of the citrate solution; palatability is improved by mixing it with water or juice. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Cinacalcet as adjunctive therapy for hereditary 1,25-dihydroxyvitamin D-resistant rickets. Vitamin D refractory rickets is a clinical syndrome where there is lack of bone mineralization despite adequate therapy with vitamin D. Clinical signs of refractory rickets include growth failure, bony deformities, bone pain, muscle weakness, polyuria, polydipsia and dental caries. There is a paucity of data about the longterm sequelae of persistent hypertension in children, but it is known that children with hypertension have evidence of end-organ damage and are at risk of hypertension into adulthood. The widespread adoption of National High Blood Pressure Education Program Fourth Report has led to uniformity in classification and management of hypertension. The incidence of primary hypertension is estimated to be 120% and rising among children and young adults. The use of the former is discouraged due to the environmental toxicity of mercury. The oscillometric devices measure mean arterial pressure and then use algorithms to calculate systolic and diastolic blood pressure. Advantages of these instruments are their ease of use (especially in infants and younger children and in intensive care setting), no environmental hazard and minimization of observer bias. The disadvantages are that the algorithms used by companies are proprietary and differ among devices; this can result in variations and lack of comparability. Blood pressure values exceeding the 90th centile by oscillometric method should be confirmed by an auscultatory technique. Systemic Disorders Ambulatory Blood Pressure Monitoring Blood pressure demonstrates a circadian rhythm and is affected by sleep/wake cycle and activity. A portable device records systolic and diastolic blood pressure every 2030 min over 24 hours. Parents or child are instructed to maintain a diary with record of the time of sleeping and time of waking and any activity. The mean blood pressure during the day and night and over 24 hours as well the degree to which blood pressure exceeds the upper limit of normal over a time period (blood pressure load > 25% is considered abnormal) are calculated. Absent or reduced dipping (< 10%) is seen in children with chronic kidney disease. This allowed correlation of high blood pressure in adults with the adverse events thus making it possible to have relevant cut-off measurements. As mentioned previously, there is a paucity of long-term studies looking at effects of pediatric hypertension and hence definitions are just based on normative distribution of systolic and diastolic blood pressure in healthy children Table 1). This table includes the 50th, 90th, 95th and 99th percentiles by gender, age and height. Measurement of Blood Pressure Blood pressure should be measured routinely, at least annually, in all children older than 3 years who seek medical consultation. Children below 3 years with any of the following risk factors should also be screened for hypertension: (1) history of prematurity, very low birthweight babies, or other neonatal complications requiring intensive care; (2) congenital heart disease (repaired or unrepaired); (3) recurrent urinary tract infections, hematuria, or proteinuria; (4) known renal disease or urologic malformation; (5) family history of congenital renal disease; (6) solid organ transplantation; (7) malignancy or bone marrow transplant; (8) treatment with drugs known to raise blood pressure; (9) other illnesses associated with hypertension. Secondary causes are likely in a younger child and in presence of stage 2 hypertension. Renal parenchymal causes account for 75% and renovascular causes for 10% of secondary hypertension Table 2). Renal parenchymal disease includes conditions like acute or chronic glomerulonephritis, reflux nephropathy and obstructive uropathy. Renovascular disease may occur due to renal artery stenosis, renal artery thrombosis or Takayasu aortoarteritis. Endocrine causes include pheochromocytoma, neuroblastoma, primary hyperaldosteronism, Cushing syndrome Method of Measurement and Devices Various measurement devices are available. The auscultatory method is preferred, and performed using either the mercury or aneroid Table 1 Staging of pediatric hypertension Normal blood pressure Prehypertension Stage 1 hypertension Stage 2 hypertension White coat hypertension Definition Average systolic or diastolic blood pressure < 90th percentile Average systolic or diastolic blood pressure 90th to 95th percentile, or blood pressure > 120/80 mm Hg Average systolic or diastolic blood pressure 95th to 99th percentile plus 5 mm Hg Average systolic or diastolic blood pressure > 99th percentile plus 5 mm Hg Blood pressure > 95th centile when measured in clinic setting but < 90th centile when measured outside clinic environment. This appears to be a prehypertensive condition with risk of ventricular hypertrophy and progression to sustained hypertension Blood pressure normal in clinic setting but in hypertensive range when measured outside clinic environment as detected on ambulatory blood pressure monitoring. This condition is considered more serious than white coat hypertension Raised blood pressure without end-organ damage or symptoms, such as headache, nausea or blurred vision Raised blood pressure along with presence of end-organ damage, such as encephalopathy, seizures, congestive heart failure, acute kidney injury, papilledema or pulmonary edema Masked hypertension Hypertensive urgency Hypertensive emergency Note that normative data is based on age, height and gender. Definitions are based on blood pressure taken on greater than or equal to three separate occasions. The addition of 5 mm Hg to define stage 2 hypertension is to allow for interobserver differences. Blood pressure tables are applicable for children aged 1 year and older, and should be used when measuring blood pressure by auscultatory method. Primary hypertension is a diagnosis of exclusion when no etiology is identified after careful evaluation. Reflux nephropathy Micturating cystourethrogram, dimercaptosuccinic acid scintigraphy. These conditions should be suspected when there is strong family history, severe and difficult to control hypertension, and presence of electrolyte and acid-base abnormalities. Clinical history taking and examination Table 3) for the underlying etiology should be focused on detecting secondary causes.