Cheap forxiga 10 mg otc
The enzymes which digest the cell are derived from lysosomes of either dying cells themselves or from leukocytes recruited as part of the inflammatory reaction diabetic low carb diet discount forxiga line. Fates of necrotic cells: After necrosis, these necrotic cells may either persist for some time or may be digested by enzymes and disappear. Dead cells may be replaced by myelin figures, which may be either phagocytosed by other cells or may undergo further degradation into fatty acids. These fatty acids can bind calcium salts and the necrotic cells may become calcified. Morphological Patterns/Types of Tissue Necrosis Most of the types of necrosis have distinctive gross appearances (except fibrinoid necrosis) but they can be identified only by microscopic examination. Common type, in which the outline of dead tissues (underlying tissue architecture) is preserved (at least for few days). Coagulative necrosis is characteristic of infarcts (areas of necrosis caused by ischemia) in all solid organs except the brain. Leukocytes are recruited to the site of necrosis and the lysosomal enzymes of the leukocytes digest the necrotic cells. The resulting cellular debris are then removed by phagocytosis by infiltrating neutrophils and macrophages. In this type of necrosis dead tissue rapidly undergoes softening and transforms into a liquid viscous mass. Microscopy Pus consists of liquefied necrotic cell debris, dead leukocytes and macrophages (scavenger cells). It is a distinctive type of necrosis which shows combined features of both coagulative and liquefactive necrosis. In contrast to coagulative necrosis, there is complete obliteration of the tissue architecture and it is not possible to identify the cellular outlines. It is surrounded by epithelioid cells; Langhans type giant cells (nuclei arranged in a horseshoe pattern), lymphocytes and fibroblasts forming granuloma. Enzymatic fat necrosis: Occurs in adipose tissue around acutely inflamed pancreas (in acute pancreatitis). Lipase destroys fat cells, splits the triglyceride esters within fat cells and liberates free fatty acids which combine with calcium and form calcium soaps (fat saponification). An infarct in the brain shows soft necrotic area with dissolution of the tissue forming a cavity. Traumatic fat necrosis: Occurs in tissues with high fat content (like in heavy, pendulous breast and thigh) following severe trauma. Characterized by deposition of pinkstaining (fibrin-like) proteinaceous material in the tissue matrix with a staining pattern reminiscent of fibrin. A variant of wet gangrene known as gas gangrene is caused by clostridia (Gram-positive anaerobic bacteria). Sites: It usually involves a limb, generally the distal part of lower limb (leg, foot, and toe). Microscopy the necrosis (coagulative type) shows smudging of soft tissue and overlying skin. Diabetic patients may develop both dry (due to atherosclerosis of tibial and popliteal arteries) and wet gangrene. Gas gangrene: Special type of wet gangrene caused by infection with a gas forming anaerobic Clostridium perfringens. Gummatous Necrosis the necrotic tissue is firm and rubbery and is usually found in syphilis (refer page 92). Laboratory Detection of Necrosis Whenever there is necrosis, there is leakage of intracellular proteins through the damaged cell membrane which ultimately reaches the circulation. Thus, it is possible to detect tissue-specific necrosis using blood or serum samples. Examples include (i) cardiac muscle contains a unique isoform of the enzyme creatine kinase and of the contractile protein troponin, (ii) hepatic bile duct epithelium contains the enzyme alkaline phosphatase, and (iii) hepatocytes contain transaminases. Necrosis of these tissues elevate the serum levels of these proteins and are useful markers of tissue damage. Ultrastructural differences between reversible and irreversible injury is presented in Table 2. Liquefactive necrosis: Dead cells are transformed into a liquid viscous mass due to enzymes released from leukocytes accumulated at the site of necrosis. Caseous necrosis with granuloma is observed in tuberculosis and systemic fungal infections. It is due to the presence of high lipid content in the cell wall in these organisms. Characteristics General features Common site Examples Limbs Gangrene of lower limb due to atherosclerosis Bowels Volvulus, intussusception Dry Wet Etiological factors Cause of ischemia Rate of obstruction Gross features Appearance of involved part Line of demarcation Shriveled, dry (mummification) and black Clear cut between gangrenous and healthy part Slow Fair Swollen, soft and moist/wet Not clear cut Arterial obstruction Slow Commonly venous obstruction Abrupt Spread Prognosis Rapid Poor due to severe septicemia Enzymatic fat necrosis is mediated by enzymes whereas traumatic is not mediated by enzymes. Enzymatic fat necrosis in acute pancreatitis appears as chalky- white areas which help in its gross identification. Fibrinoid necrosis: Necrotic material appears similar to fibrin and is not fibrin. Aschoff bodies in rheumatic fever Dry gangrene predominantly consists of coagulative type of necrosis. Gas gangrene is a variant of wet gangrene caused by bacteria Clostridium perfringens (Gram-positive anaerobic bacteria). Definition: Apoptosis is a type of (programmed) cell death induced by a tightly regulated suicide program. Fragments of the apoptotic cells (apoptotic bodies) break and fall off from the cells and hence named apoptosis (meaning "falling off"). Causes of Apoptosis Physiological Situations v Removal of excess cells during embryogenesis and developmental processes. Structure involved Reversible injury Irreversible injury Structure involved Plasma membrane changes Mitochondrial changes Reversible injury Blebbing, blunting, loss of microvilli Swelling and appearance of small amorphous densities Irreversible injury Discontinuities in plasma and organelle membrane Marked dilatation with appearance of large amorphous densities (precipitated calcium), aggregates of fluffy material (denatures protein) Swelling and fragmentation Usually present Endoplasmic reticulum Myelin figure (large intracellular whorled phospholipid masses) Nuclear changes Dilatation with detachment of polysomes May be present Disaggregation of granular and fibrillar elements Pyknosis, karyolysis and karyorrhexis Irreversible injury: Large amorphous densities in mitochondria. Elimination of potentially harmful cells: In immunology, the clones of self-reactive lymphocytes that recognize normal self-antigens are deleted by apoptosis. Pathological Conditions Apoptosis eliminates cells that are genetically altered or damaged beyond repair. Elimination of cells with excessively accumulated misfolded proteins: Mutations in the genes encoding proteins or extrinsic factors (damage due to free radicals) may result in accumulation of unfolded or misfolded proteins. Elimination of neoplastic cells/rejection of transplant: the T-cellmediated mechanism is responsible for apoptosis in tumors and cellular rejection of transplants. Elimination of parenchymal cells in pathologic atrophy: Obstruction of duct in the parenchymal organs like pancreas, parotid gland and kidney can lead to apoptosis of the parenchymal cells. The apoptotic bodies are composed of cytoplasm and tightly packed organelles, with or without nuclear fragments. Light Microscopy the apoptotic cells appear as round or oval mass having intensely eosinophilic cytoplasm. The survival or apoptosis of many cells depends upon balance between two opposite sets of signals namely: (1) death signal (proapoptotic) and (2) prosurvival (anti-apoptotic) signals. Initiation Phase Apoptosis is initiated by signals derived from two distinct pathways activated by distinct stimuli, namely: (1) intrinsic or mitochondrial pathway and (2) extrinsic or death receptor pathway. These proteins may be broadly divided into proapoptotic or antiapoptotic (prosurvival). Growth factors and other survival signals stimulate production of antiapoptotic proteins. If the balance shifts to proapoptotic proteins, the apoptotic cascade is activated. One of these proteins is cytochrome c which binds to a protein called apoptosis-activating factor-1 (Apaf-1) and forms an important caspase cascade activator called apoptosome. This complex binds to caspase-9, the critical initiator caspase of the mitochondrial pathway which sets in an auto-amplification process. Many cells express "death-receptors" molecules on the surface of plasma membrane that trigger apoptosis. In the extrinsic (death receptor) pathway, apoptosis is initiated when the death receptors present gets activated.
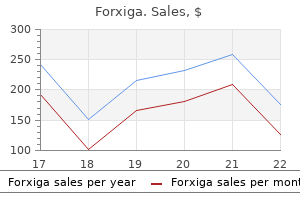
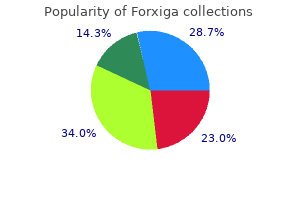
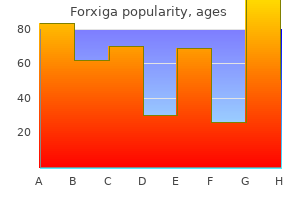
Order forxiga online
Another form of prevention is acting on the parasite before it can directly or indirectly contaminate humans diabetes medications hypoglycemia order forxiga online from canada. This appeared to be effective and could reduce the prevalence in humans in countries like France or Austria in the not too distant future. The rash is characterized by small elements of macular or maculopapular pink, especially on the face, which can then become confluent on the second day. The lesions disappear on the third day without sequelae after a fine desquamation. Exceptional complications can occur: meningoencephalitis and thrombocytopenia accompanied by purpura. In total, the clinical presentation is not specific enough to establish with certainty the diagnosis of rubella. Laboratory Findings Biological diagnosis of primary rubella infection in pregnant women is essential because of the inconstancy and non-specific clinical symptoms. Most laboratories use automated analyzers to perform immunoassays to measure anti-rubella IgG and IgM. This mainly has consequences for patients with a low quantity of IgG (around the threshold), which can return a positive result with one technique and be negative with another. However, the population has lower levels of rubella virus IgG than before vaccination programs were introduced and this threshold value should probably be reconsidered [139]. It persists, however, several months after vaccination (sometimes more than a year). Measurement of IgG avidity can help to establish the timing of infection: when avidity is low a recent primary infection is very likely (<1 month), whereas when it is high it is a probable past infection (>2 months). After inhalation, the rubella virus multiplies in the respiratory mucosa and cervical lymph nodes where it enters the general circulation. The polyadenopathies correspond to sites of secondary multiplication of the virus. The rash appears along with the production of antibodies and is linked to the formation of immune complexes. Reinfections are possible but the incidence of reinfection during pregnancy is unknown, and the risk of transmission to the fetus is difficult to determine [138]. The infectious period extends approximately from 8 days before to 8 days after the eruption. Epidemiology the incidence of rubella (also known as German measles) has decreased considerably (without disappearing) since the introduction of a vaccination policy. Maternal Infection Clinical Manifestations In western countries, over 90% of women of childbearing age are currently protected against rubella. This rate is estimated to be 90% before 12 weeks, about 25% between 23 and 26 weeks, and to be close to 100% in late pregnancy [140]. When maternal contamination is pre-conceptional, the risk of vertical transmission is extremely low. Prenatal Diagnosis of Fetal Infection Prenatal diagnosis of congenital infection by the rubella virus has long been based on finding total and specific IgM in fetal blood after 22 weeks. Cordocentesis also has the advantage of allowing a study of indirect signs of rubella infection (increased interferon-alfa, thrombocytopenia, anemia, erythroblastosis, and elevated transaminases, lactate dehydrogenase, and gamma-glutamyl transpeptidase). Fetal abnormalities accessible for ultrasound prenatal diagnosis are extrapolated from neonatal data mentioned above. The main abnormalities detected by ultrasound are: microphthalmia, heart defects, microcephaly, and hepatosplenomegaly. In the absence of visible abnormalities, the ultrasound should be repeated every 3 weeks. After this, the rate declines from 15% to 80% at between 11 and 18 weeks, then further down to virtually zero after 18 weeks [140]. The fetal abnormalities caused by infection with the rubella virus are part of the congenital rubella syndrome. These abnormalities are linked to a non-cytolytic attack involving multiple organs, with apoptosis, disruption of mitosis, autoimmune phenomena, and non-inflammatory necrosis. Sixty-eight percent had sclerosis of the aortic valve, 22% had diabetes, 19% had thyroid disorders, 73% had early menopause, and 12. The ocular manifestations included: cataract in 85% of cases (bilateral in 63% of cases), microphthalmia in 82% of cases (bilateral in 65% of cases), and Management If There is a Suspected Recent (<15 Days) Contagion of a Pregnant Woman A search for IgG should be performed as soon as possible. If IgG is absent, a second sample must be taken after 3 weeks in order to search for IgG and IgM. If There is a Suspected Late (>15 Days) Contagion of a Pregnant Woman or if a Rash is Suggestive of Rubella Joint research of IgG and IgM has to be performed immediately. It can also be a polyclonal stimulation of IgM that does not relate to a rubella infection. Methods of Prevention Prevention is based on vaccination with a live attenuated vaccine, alone or in combination with antigens from measles and mumps. The tolerance of the vaccine is good and it induces an immune response in 95% of seronegative women. The latter should be done after ensuring the absence of pregnancy, and that contraception has been used in the previous month and continued for 2 months after. However, no cases of congenital rubella were reported in the aftermath of an inadvertent vaccination during early pregnancy. Postpartum vaccination should be offered to any woman not immunized during pregnancy. A case of fetal parvovirus B19 myocarditis, terminal cardiac heart failure, and perinatal heart transplantation. Mirror syndrome due to parvovirus B19 hydrops complicated by severe maternal pulmonary effusion. Clinical biological features of Ballantyne syndrome and the role of placental hydrops. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. The incidence of human parvovirus B19 infection during pregnancy and its impact on perinatal outcome. Risk of fetal hydrops and non-hydropic late intrauterine fetal death after gestational parvovirus B19 infection. Parvovirus B19 infection in the first trimester of pregnancy and risk of fetal loss: a population-based case-control study. Thrombocytopenia in hydropic fetuses with parvovirus B19 infection: incidence, treatment and correlation with fetal B19 viral load. Fetal brain injury associated with parvovirus B19 congenital infection requiring intrauterine transfusion. Long-term neurodevelopmental and cardiovascular outcome after intrauterine transfusions for fetal anaemia: a review.
Forxiga 10mg free shipping
Gene therapy and gene transfer projects of the 7th Framework Programme for Research and Technological Development of the European Union ketonuria diabetes mellitus type 2 10mg forxiga free shipping. Nonviral gene transfer to surface skin of mid-gestational murine embryos by intraamniotic injection and subsequent electroporation. Fetal gene transfer by intrauterine injection with microbubble-enhanced ultrasound. Successful in utero gene transfer using a gene gun in midgestational mouse fetuses. Efficient in vivo targeting of epidermal stem cells by early gestational intraamniotic injection of lentiviral vector driven by the keratin 5 promoter. Early intra-amniotic gene transfer using lentiviral vector improves skin blistering phenotype in a murine model of Herlitz junctional epidermolysis bullosa. The effects of sildenafil citrate (Viagra) on uterine blood flow and well being in the intrauterine growth-restricted fetus. Effect of amniotic fluid on cationic lipid mediated transfection and retroviral infection. Targeted gene transfer to lymphocytes using murine leukaemia virus vectors pseudotyped with spleen necrosis virus envelope proteins. Lack of expression from a retroviral vector after transduction of murine hematopoietic stem cells is associated with methylation in vivo. Differential short-term transduction efficiency of adult versus newborn mouse tissues by adenoviral recombinants. The developmental stage determines the distribution and duration of gene expression after early intra-amniotic gene transfer using lentiviral vectors. Autologous transplantation of amniotic fluid-derived mesenchymal stem cells into sheep fetuses. Humoral immune response to recombinant adenovirus and adenoassociated virus after in utero administration of viral vectors in mice. Intrauterine viral infection at the time of second trimester genetic amniocentesis. Male germ-line cells are at risk following direct-injection retroviral-mediated gene transfer in utero. Angiographically guided uteroplacental gene transfer in rabbits with adenoviruses, plasmid/liposomes and plasmid/polyethyleneimine complexes. Transduction of human trophoblast cells by recombinant adenoviruses is differentiation dependent. Differential expression of the coxsackievirus and adenovirus receptor regulates adenovirus infection of the placenta. Fatal systemic inflammatory response syndrome in a ornithine transcarbamylase deficient patient following adenoviral gene transfer. In vivo delivery of recombinant viruses to the fetal murine cochlea: transduction characteristics and long-term effects on auditory function. Vector design influences hepatic genotoxicity after adeno-associated virus gene therapy. Overexpression of transforming growth factor-1 in fetal monkey lung results in prenatal pulmonary fibrosis. Guideline on the quality, non-clinical and clinical aspects of gene therapy medicinal products. Kilby Lasagna commented on a trial where out of 8027 possible candidates, 100 people participated [5]. This is a potential problem specifically in rare diseases of low prevalence that may affect the fetus and potentially be amenable to treatment. In such studies recruitment may be low and equipoise secondary to patient or clinician preference may compound low recruitment. In addition, parents whose baby has a pathology that significantly affects fetal outcome may opt for termination of pregnancy, further reducing numbers to treat in a trial. In research on preterm birth for example, 103 trials reported 72 different primary outcomes, while 33 Cochrane reviews reported 29 different outcomes [7]. If datasets cannot be combined it is difficult to reach proper statistical power, subsequently limiting the impact research can have on clinical practice. An additional concern is that outcomes reported have not always been those that patients regard as relevant [8]. One way to accrue sufficient patient numbers in trials is to employ a multicenter design. This demands an increase in collaboration between researchers and might lead to an increase in the number of researchers who qualify for authorship. There may also be implications for funding, as multicenter trials tend to require more monitoring for compliance with trial protocols and hence generally require more financial Medical interventions should ideally only be offered if we know that they help the patient in improving outcome by reducing morbidity and mortality. At present, there is consensus that their effectiveness should be evaluated before incorporation into guidelines. Since the inception of fetal medicine as a subspecialty and the application of in utero treatments for fetal therapy, there have been mainly cohort studies presented as supporting evidence of efficacy (for many therapies) and evidence from randomized trials is in the minority. Critical appraisal of studies on various forms of fetal therapy has been aided by performing systematic reviews and, where practicable, meta-analyses of outcomes. However, although such methods are informative they summate evidence from relatively small and often heterogeneous case cohort studies. However, they can only provide reliable answers if they have sufficient power [1]. Happily, in pregnancy and childbirth the most robust outcome measure (maternal or fetal death or severe disability) occurs rarely. Although one could, in theory, do single-center studies that run for a long period of time, this has the disadvantage that medical developments may make the clinical question under study less relevant by the time the trial is completed. Low participation rates can result in studies not reaching their planned numbers, and consequently wide uncertainty about conclusions. This reflects the increasing complexity of medical research necessary to underpin evidence-based practice. This indicates that efforts to provide a better level of evidence potentially make a bigger difference to clinical decision-making [12]. Crucially in obstetrics, the pharmaceutical industry has shown little interest in the development of new interventions largely due to a poor risk:reward ratio [26]. Collaboration on a global scale enables researchers to be transparent on research priorities and inform each other on research that is planned or in progress. Strengthening this can have a major impact on increasing research value and avoiding research waste [28]. The purpose is to foster communication between the groups in order to improve ongoing and future trials. Seven university units were selected initially, along with an independent data coordinating center. The network has ongoing support for both the infrastructure at the sites and the operational costs of the trials/studies. Infrastructure includes partial support for the principal investigator, a research nurse coordinator, and an assistant. A prioritization committee determines which should be the next study to be conducted of the approved full protocols, depending on population available, funding, and scientific priority. Justine) and in Toronto (Centre for Mother, Infant, and Child Research, Sunnybrook Health Sciences Centre, University of Toronto). Inner-city areas typically have a high prematurity rate (approximately 10%) of diverse ethnic background and the incidence of obesity is rising year on year (currently approximately 1 in 5 pregnant women are obese). Reproductive Health and Childbirth is one of 27 specialties represented, and is currently in the top 5 for recruiting to clinical studies. The network also aims to ensure that the costs of research are met in a timely and efficient manner, and to unify and streamline administrative procedures associated with regulation, governance, reporting and approval as well as facilitating collaboration with industry. This funding includes provision for research nurses, research midwives, and data entry clerks. This funding may also support recruitment to trials that are managed by academic centers outside the United Kingdom.
Buy cheapest forxiga
It suggests tuberculosis blood glucose converter order 10 mg forxiga with visa, lymphoma, primary lung cancer, or metastatic cancer and requires further investigation. Examples include presence of a solitary, hard, nontender cervical node in an older patient who uses tobacco; supraclavicular lymphadenopathy; and solitary or generalized firm, movable adenopathy suggestive of lymphoma. Acute Nonspecific Lymphadenitis Acute lymphadenitis occurs in lymph nodes that drain sites of acute bacterial or fungal infections. These lymph nodes rapidly become enlarged and are usually tender (painful) because of the distension of their capsule. When there is abscess formation, the nodes become fluctuant and the overlying skin appears red. Lymphadenitis in the cervical region is usually due to drainage of microbes or microbial products from infections of the teeth or tonsils, whereas in the axillary or inguinal regions it is usually due to infections in the extremities. Acute lymphadenitis can occur in mesenteric lymph nodes draining acute appendicitis. Systemic viral infections (especially in children) and bacteremia often produce acute generalized lymphadenopathy. Macrophages may show particulate debris derived from dead bacteria or necrotic cells. In lymphadenitis accompanying pyogenic organisms, neutrophils are prominent and the centers of the follicles may show necrosis. Chronic Nonspecific Lymphadenitis Chronic nonspecific lymphadenitis may show different morphological patterns and three important patterns are (i) follicular hyperplasia, (ii) paracortical hyperplasia and (iii) sinus histiocytosis. Follicular Hyperplasia Definition: It is characterized by the presence of large oblong germinal centers (secondary follicles), which are surrounded by a collar of small resting naive B cells (the mantle zone). In nonspecific reactive follicular hyperplasia, hyperplastic follicles are mainly found in the cortex of the lymph node. Causes: the cause of nonspecific reactive follicular hyperplasia is usually unknown and caused by stimuli that activate humoral immune responses. Microscopy Follicular hyperplasia shows marked enlargement and prominence of the germinal centers of lymphoid follicles. Each germinal center consists of two distinct regions: (1) a dark zone containing proliferating blast-like B cells (centroblasts) and (2) a light zone composed of B cells with irregular or cleaved nuclear contours (centrocytes). Interspersed between the germinal B centers are scattered benign macrophages (often called as tingible-body macrophages), with abundant pale cytoplasm containing pyknotic nuclear and cytoplasmic debris of B cells. A well-defined mantle of normal small B cells surrounds the follicles, sharply separating them from interfollicular region. Differentiation from follicular lymphoma: Follicular hyperplasia appears morphologically similar to follicular lymphoma. Features favoring a reactive (non-neoplastic) hyperplasia are: v Preservation of the lymph node architecture v Marked variation in the shape and size of the follicles v Presence of frequent mitotic figures, phagocytic macrophages, and recognizable light and dark zones. Course: It undergoes rapid and complete resolution after the causative stimulus disappears. Paracortical Hyperplasia Definition: Paracortical hyperplasia is due to hyperplasia of T-cell-dependent area (paracortical region) of the lymph node. Microscopy It shows expansion of the paracortex (T-cell area) with increased number of immunoblasts and activated T cells. They contain round nuclei, open chromatin, several prominent nucleoli, and moderate amounts of pale cytoplasm. There may be hyperplasia of the mononuclear phagocytic cells in the lymphatic sinuses. Sinus Histiocytosis Definition: It is characterized by an increase in the number and size of the cells that line lymphatic sinusoids. Causes: Although nonspecific, sinus histiocytosis is common in lymph nodes draining cancers. Microscopy In sinus histiocytosis, there is expansion and distension of the subcapsular and trabecular sinuses of the lymph node. The lining lymphatic endothelial cells are markedly hypertrophied and there is marked increase in number of macrophages (histiocytes) within the sinuses. Sinus histiocytes derive from blood monocytes and they contain phagocytosed material. Lymph nodes are the most common extrapulmonary site of tuberculosis For pathogenesis of tuberculosis refer pages 512-3, of Chapter 17. Region involved: Most commonly it involves the lymph nodes of cervical and mediastinal region, followed by axillary and inguinal. Type of infection: Tuberculous lymphadenitis may occur as a part of primary infection or spread from contiguous sites or reactivation. Primary focus in the pharynx and tonsil will produce enlargement of cervical lymph node. Supraclavicular lymphadenopathy is usually due to the spread from mediastinal disease. Clinical presentation: Lymphadenitis is the most frequent presentation of extrapulmonary tuberculosis, usually occurring in the cervical region. About 50% of patients do not show constitutional features, such as fevers or night sweats. The cut surface in the tuberculous areas shows characteristic map-like areas which are yellowish, granular, opaque, soft necrotic material that resembles dry cheese. Composed of follicle center (germinal center) B cells of lymphoid follicles (centrocytes and centroblasts). Neoplastic cells: n Large round or oval cells, 4 to 5 times of a small lymphocyte. Composed of medium-sized, monomorphic lymphoid cells with basophilic vacuolated cytoplasm. Starry sky pattern: Tumor cells undergo apoptosis and nuclear remnants of these apoptotic cells are phagocytosed and cleared by benign macrophages. Poor prognostic factors: n Involvement of blood, bone marrow and central nervous system. Sclerosis and nodules: Broad collagen bands (sclerosis) divide the lymphoid tissue into nodules of varying sizes and shapes. Older age, with systemic symptoms (such as night sweats and weight loss) and advanced tumor stage. Back ground: Small lymphocytes, eosinophils (sometimes numerous), neutrophils, plasma cells and benign macrophages (histiocytes). Staging of Hodgkin Lymphoma Clinical staging of Hodgkin lymphoma is discussed in Table 12. Pattern of spread Mesenteric nodes and Waldeyer ring Extranodal involvement Characteristic of neoplastic cells Q. Enlargement of spleen is called splenomegaly and occurs in a wide variety of systemic diseases (secondary involvement). A spleen is considered as massively enlarged when its lower pole is within the pelvis, or which has crossed the midline into the right lower or right upper abdominal quadrants. Hypersplenism: It is characterized by excessive removal of red blood cells, granulocytes or platelets from the circulation. A chronically enlarged spleen usually removes excessive numbers of one or more of the formed elements of blood. Hence, thrombocytopenia is more common and severe in patients with splenomegaly compared to anemia or neutropenia. Hypersplenism is characterized by splenomegaly, cytopenia(s), normal or hyperplastic bone marrow, and a response to splenectomy. Other laboratory studies: It depends on the differential diagnosis of the underlying illness responsible for splenomegaly.
Diseases
- Fifth disease
- Abdominal cystic lymphangioma
- Mounier-Kuhn syndrome
- Adenine phosphoribosyltransferase deficiency
- Pfeiffer Palm Teller syndrome
- Panthophobia
- Purpura, Sch?nlein Henoch
- Sialadenitis
- Hypogonadotropic hypogonadism-anosmia
- Mitral valve prolapse, familial, X linked
10mg forxiga with visa
This should be done 24 hours after commencing therapy blood sugar not going down order 5 mg forxiga with mastercard, and at weekly intervals thereafter. Evidence of tricuspid regurgitation, suppressed right ventricular contractility or hydrops should prompt discontinuation of therapy. Finally, there are reports of perforation of the ileum and necrotizing enterocolitis following in utero exposure to indomethacin. Sulindac is a prodrug, which is administered orally and requires metabolism in the liver in order to be activated. Studies have demonstrated that fetal levels of the active sulfide metabolite are 50% of those found in the maternal circulation [24]. In comparison with indomethacin sulindac was associated with a lower rate of ductal constriction: 70% versus 30% respectively [25]. This finding must be extended to their potential use for the treatment of polyhydramnios. In considering their use we must bear in mind that there are no studies powered to determine the fetal side effects of these drugs. In agreement with others, we believe they should not be used for the sole purpose of decreasing amniotic fluid [27]. Oligohydramnios Definition Oligohydramnios is a deficiency in amniotic fluid compared with a normal volume for gestational age. As such its significance is two-fold: primarily, it is a marker of a pathology that is already complicating the pregnancy; secondarily, it may add to the sequelae of the pathology by direct effects on fetal development or well-being. Thus, upon the diagnosis of oligohydramnios the pregnancy declares itself to be at increased risk of perinatal loss and morbidity, which is higher at earlier gestational ages of diagnosis. A systematic approach to the assessment of oligohydramnios is required to establish the underlying etiology (Table 20. In current clinical practice there are no such established interventions for oligohydramnios; however, several have been proposed and investigated in specific pathologies and will be considered. These pathologies and management options are discussed elsewhere in this textbook. All the pathologies are directly associated with a high risk of fetal or perinatal loss or morbidity. Severe oligohydramnios has a causal relationship with fetal pulmonary hypoplasia and deformities of soft tissues and the musculoskeletal system. Pulmonary hypoplasia is associated with a high risk of lethal respiratory compromise at birth and is related to the severity of oligohydramnios and the gestation of onset. Fetal deformities such as Potter-type facies, flexion contractures and talipes are related to the severity and duration of oligohydramnios. Such deformities are rarely severe in the absence of lung hypoplasia and often correct with time or physiotherapy after birth. Oligohydramnios and Pulmonary Hypoplasia There are 5 phases of human lung development [29]. By the end of the pseudo glandular phase all 16 generations of the airconducting bronchial tree have been formed. In this phase the canaliculi branch out of the terminal bronchioles to form the basis of the functional respiratory or gas exchange part of the lungs. It is believed that the canalicular phase of lung development is critically reliant on adequate amniotic fluid volume and is compromised by oligohydramnios. Various mechanisms have been suggested to explain the pathophysiology of oligohydramnios-induced pulmonary hypoplasia [30], including lack of ability to expand the fetal chest with breathing movements, an altered pressure gradient from the terminal to proximal parts of the bronchial tree with resultant increase of loss of fluid produced by the fetal lungs, and lack of volume of fluid to inhale into the bronchial tree to expand the fetal canaliculi during development. Experiments on fetal rabbits in which fetal breathing is paralyzed due to cervical cord transection demonstrate pulmonary hypoplasia with normal liquor volumes [31]. The role of such cyclical distension of the developing pulmonary structure is supported by experiments on fetal sheep models of congenital diaphragmatic hernia [32]. The pathophysiology of pulmonary hypoplasia is likely to be multifactorial but essentially results from a lack of ability to maintain adequate (and possibly cyclical) volume distension of the terminal parts of the pulmonary tree as it develops. The true incidence of pulmonary hypoplasia in clinical studies of oligohydramnios is difficult to quantify. In addition, in many clinical studies post mortem data are lacking and clinical markers of severe respiratory compromise are presented as evidence of pulmonary hypoplasia. The ability to predict lethal pulmonary hypoplasia complicating oligohydramnios with fetal ultrasound would be useful for parental counseling. Fetal chest circumference, 2D and 3D calculations of lung volumes, and Doppler assessments of pulmonary artery resistance have been investigated. It demonstrated that although perinatal loss was reduced in the shunted cohort (6/15 compared with 12/16 non-shunted fetuses), most likely due to a reduction in pulmonary hypoplasia, perinatal morbidity remained high, with only 2 of the shunted fetuses having normal renal function at 1 year. The diagnosis is made by eliciting a relevant clinical history of passage of per vaginal fluid. It is confirmed by speculum examination demonstrating pools of fluid in the vagina or draining through the external cervical os. Commercial versions of these non-invasive adjuvants have differing levels of sensitivity and specificity [36]. Ultrasound can suggest the diagnosis by the demonstration of oligohydramnios without any signs of placental insufficiency or fetal anomaly. Cessation of fluid leakage was observed in the majority, with normal liquor volumes evident at 2 weeks. Survival occurred in all but one case (91%) and mean gestation at delivery was 34 weeks. During this time interval there were changes in the operating technique, moving from a non-selective to selective coagulation technique and then to a Solomon coagulation technique. There was no clinical evidence of membrane rupture for the duration of the pregnancy. Histological study has confirmed no alteration of the edges of these defects consistent with an absence of biological healing [47]. In vitro studies of fetal membrane do suggest some capacity for healing, which is limited to early gestation. Functional membrane integrity may involve the sliding of the chorionic and amniotic membranes relative to each other, contraction or scarring in the myometrial and decidual layers of the uterus [39], or simply reflect the ongoing degree of seal that the surrounding intact membranes have to the decidua. The commonest causes of loss are severe premature delivery, pulmonary hypoplasia, and infection. It is not possible in the majority of studies to delineate the contribution of pulmonary hypoplasia from that of prematurity to the overall perinatal loss rate. It is likely that mortality rates are underestimated due to exclusion of pregnancies undergoing termination at parental request. Advancing gestational age at the time of membrane rupture has a positive effect on perinatal survival by reducing loss from prematurity and pulmonary hypoplasia. The incidence of pulmonary hypoplasia was assessed by pathological or radiological parameters. Few studies assess the effect of more severe degrees of oligohydramnios on the incidence of pulmonary hypoplasia and fetal loss. Severe oligohydramnios >14 days after rupture of membranes at <25 weeks had a predicted neonatal mortality of >90%, with the majority having lethal pulmonary hypoplasia diagnosed on post-mortem examination. However, one of the limitations of cohort studies is the presence of confounding factors. This highlights the difficulty of finding an accurate answer to our question within the current published data. These include various potential sealant agents, cervical plugs, and amnioinfusion. The evidence to support the value of all these therapies is questionable; amniopatch and amnioinfusion have the best of the limited data to review. This amniopatch showed promise as a therapy (but was associated with 2 cases of in utero demise, possibly secondary to the secretion of vasoactive cytokines from activated platelets). The technique involves the ultrasound-guided injection via a 22-gauge needle of saline (to confirm safe placement of the needle), then platelets (in limited volumes), and then cryoprecipitate into the amniotic cavity.
Order forxiga 5mg without a prescription
Chronic renal damage may result in fibrosis in the interstitium and renal failure diabetes test lab order 10 mg forxiga fast delivery. Laboratory diagnosis: For definitive diagnosis of lead poisoning, intoxication, elevated blood lead and red cell free protoporphyrin levels (>50 g/dL) or, alternatively, raised blood levels of zinc-protoporphyrin levels or its product are required. Mercury Mercury binds to sulfhydryl groups (like lead) in certain proteins with high affinity. Source: Humans have used inorganic mercury since prehistoric times and it has been known to be an occupation-related hazard. It was used as a pigment in cave paintings, a cosmetic, a remedy for syphilis, and a component of diuretics. In recent years, the main sources of exposure are organic (derived from living matter) mercury present in contaminated fish and dental amalgams that release mercury vapors. In some areas mercury used in gold mining, or from fertilizer and plastics factory, is discharged into and contaminate the rivers. Inorganic mercury from industrial wastes can be converted to highly neurotoxic organic compounds, such as methyl mercury by bacteria in bays and oceans. Nephrotoxicity: In the kidneys, mercury can produce acute tubular necrosis (proximal tubular necrosis) and renal failure. Arsenic compounds have been used as insecticides, herbicides, weed killers, other agricultural products and wood preservatives. Arsenicals may also be found naturally in soil and ground water (in countries, such as Bangladesh, Chile, and China) as a result of naturally occurring arsenic-rich rock formations, from coal burning or from use of arsenical pesticides. Toxic effects: these include: v v Acute arsenic poisoning is almost always due to accidental or homicidal ingestion. Ingested of large quantities of arsenic causes severe abdominal pain, diarrhea; cardiac arrhythmias, shock and respiratory distress syndrome; and acute encephalopathy. These effects may be due to the interference with mitochondrial oxidative phosphorylation. Chronic exposure to arsenic: Chronic arsenic intoxication affects many organ systems. Cancers of the skin, respiratory tract (lung carcinoma) and gastrointestinal tract may develop due to industrial and agricultural exposure. This may be followed by the development of basal and squamous cell carcinomas (but not melanomas). Arsenic can cause encephalopathy and peripheral neuropathy (paresthesias, motor palsies and painful neuritis). Cadmium Sources: Cadmium is a plasticizer and a pigment and is relatively a modern toxic agent. It is used in manufacturing alloys, producing rechargeable nickel-cadmium batteries and electroplating other metals. Cadmium oxide fumes are released during welding of steel parts previously plated with a cadmium anticorrosive. Cadmium can contaminate soil and plants directly or through fertilizers and irrigation water. Both plant- and animal-derived foodstuffs may contain substantial amount of cadmium. In the kidney, initially it produces proteinuria due to tubular damage (rather than glomerular damage) that may progress to end-stage renal disease. Chromium Chromium (Cr) is used in several industries, such as metal plating and some types of manufacturing. Chronic exposure is highly genotoxic and increases the risk of lung cancer and other tumors. Nickel Nickel is used in electronics, coins, steel alloys, batteries and food processing. The most frequent effect of exposure to nickel is contact dermatitis ("nickel itch") and can develop due to contact with metals containing nickel, such as coins and costume jewelery. Exposure to nickel increases the risk of lung cancer and cancer of the nasal cavities. Tobacco is the most common exogenous cause of human cancers and is responsible for about 90% of lung cancers. Apart from death due to various types of cancers, tobacco can cause deaths from cardiovascular and metabolic diseases, deaths from nonmalignant lung diseases and perinatal deaths. Life expectancy is reduced by cigarette smoking and overall mortality is proportional to the amount (dose dependent) and duration of smoking commonly quantitated as "pack-years. Betel quid/pan is a type of tobacco chewing that contains several ingredients, such as areca nut, slaked lime, and tobacco which are wrapped in a betel leaf. Oral cancers are found on the buccal and gingival surfaces in the sites where tobacco products are held in contact with the mucosa for long periods. Constituents of Tobacco Smoke Tobacco contains more than 2,000 substances (potentially noxious) and more than 60 have been identified as carcinogens and few of them along with the type of injury produced by these agents are listed in Table 9. It does not directly cause tobacco-related diseases, but is strongly addictive and is responsible for tobacco addiction. Nicotine binds to nicotinic acetylcholine receptors in the brain, and release catecholamines from sympathetic neurons. This is responsible for the acute ill effects of smoking namely increase in heart rate, blood pressure, cardiac contractility and output. Respiratory System the most common diseases caused by cigarette smoking involve the respiratory system mainly lung. The risk of developing lung cancer depends on the intensity of exposure and is usually expressed in terms of number of "pack years". In nonsmokers, passive environmental smoke inhalation is also associated with risk of lung cancer than those who are not exposed to passive smoke. Chronic bronchitis, emphysema and chronic obstructive pulmonary disease: Contents in tobacco smoke directly irritate the tracheobronchial mucosa, producing inflammation and increased production of mucus (bronchitis). Cigarette smoke also recruits leukocytes to the lung, and increases the local production of elastase. Children living along with adult smokers are susceptible to increased respiratory illnesses and asthma. Other Systems Apart from lung cancer, tobacco smoking is a risk factor for many other malignant and nonmalignant disorders of many organ systems. All forms of tobacco usecigarette, cigar and pipe smoking, and tobacco chewing are associated with oral cancer. Tobacco consumption interacts with alcohol in multiplying the risk of oral, laryngeal and esophageal cancer. Smoking is a risk factor for atherosclerotic peripheral vascular disease and cerebrovascular disease (ischemic stroke, intracranial hemorrhage). If smoking is combined other risk factors, such as hypertension (elevated blood pressure) and hypercholesterolemia (raised blood cholesterol levels), this multiplies the risk of atherosclerosis and myocardial infarction. The cigarette smoking is a strong risk factor for atherosclerotic aortic aneurysms. Maternal smoking: Increases the risk of spontaneous abortions and preterm births and results in intrauterine growth retardation (fetal tobacco syndrome). It may be due to nicotine-related insulin resistance and beta cell apoptosis, increased central obesity and altered metabolism of estrogens and androgens in smokers. However, excessive amounts of alcohol can cause marked physical and psychologic damage. After consumption, ethanol is directly absorbed in the stomach and small intestine. Then it is distributed to all the tissues and fluids of the body which is directly proportional to its level in the blood. Less than 10% of the alcohol is excreted directly in the urine, sweat, and breath. Chronic alcoholism: It is defined as regular intake of sufficient alcohol to injure an individual socially, psychologically or physically. Alcoholism is more common in men, but the number of female alcoholics is gradually increasing. It may lead to death either directly or due to accidents caused by drunken driving and alcohol-related homicides and suicides, and as a consequence of cirrhosis of the liver. Alcohol level in blood: the amount of alcohol exhaled is proportional to the blood level. The legal definition of drunk driving is an alcohol concentration of 80 mg/dL in the blood.
5mg forxiga with amex
Overall metabolic disease and cancer generic forxiga 5 mg with visa, the long-term survival in prenatally diagnosed neuroblastoma is over 90% [37]. The most common clinical presentation is uterine size greater than gestational dates, initiating an ultrasound examination [41]. Weekly sonographic examinations should be performed during pregnancy to assess amniotic fluid index, tumor growth, fetal well-being, and early evidence of hydrops. Evidence of the earliest signs of heart failure, placentomegaly, and/or hydrops should be sought, as these may progress rapidly and are harbingers of preterminal events. This approach may be useful in managing the common association of prematurity, large tumor, and hyperdynamic state [44]. Previous results in this setting with radiofrequency ablation have been uniformly poor, however interstitial laser photocoagulation of feeding vessels has been reported to correct the high-output state without the adverse results seen with radiofrequency ablation [49, 50]. Postnatal Management/Outcome A neonatologist should attend the delivery and be prepared to provide respiratory support. Excellent venous access is paramount, along with echocardiography and abdominal ultrasound should hemorrhage in the tumor occur. If there is no high-output state tumor resection is not mandatory and attention should focus on treating respiratory distress and correction of anemia. When the patient is stable, surgical resection consists of excision of both the tumor and the coccyx, which is thought to be essential to prevent recurrence. Congenital cervical immature teratoma arising in the left lobe of the thyroid gland. Approach for oxygenation of the newborn with airway obstruction due to a cervical mass. Management of giant cervical teratoma with intracranial extension diagnosed in utero. Cervical and oral teratoma in the fetus: a systematic review of etiology, pathology, diagnosis, treatment and prognosis. Diagnosis and management of fetal cardiac tumors: a multicenter experience and review of published reports. Rhabdomyoma and ventricular preexcitation syndrome: a report of two cases and review of literature. Successful ultrasoundguided laser treatment of fetal hydrops caused by pulmonary sequestration. Percutaneous laser ablation under ultrasound guidance for fetal hyperechogenic microcystic lung lesions with hydrops: a single center cohort and literature review. Contribution of magnetic resonance imaging to prenatal differential diagnosis of renal tumors: report of two cases and review of the literature. Reference values of fetal aortic flow velocity waveforms and associated intra-observer reliability in normal pregnancies. Preoperative angiography with embolization and radiofrequency ablation as novel adjuncts to safe surgical resection of a large, vascular sacrococcygeal teratoma. Survival rates are higher in tertiary care centers with a minimum case load of more than 10 patients per year and standardized management protocols [11]. Significant advances in postnatal management, such as the introduction of gentle ventilation and permissive hypercarbia, have resulted in improved survival rates over the past two decades [14]. At 28 days of life, half of the survivors are oxygen dependent [16], whereas at discharge 16% still require oxygen [17]. More than 40% of patients need bronchodilators within the first year of life [17], and over 10% suffer from asthma and obstructive lung disease during childhood [18]. In some, chronic lung disease is further exacerbated by abnormal diaphragmatic compliance and thoracic deformities [19]. The causes are multiple and include displacement of the stomach, modification of the gastroesophageal junction and abnormal motility of the esophagus, and some of these changes are induced by the surgery. In addition, malrotation may delay gastric emptying, and the abnormal balance of pressures in the thorax and abdomen facilitates retrograde passage of gastric content to the esophagus [24]. During embryogenesis the diaphragm fails to form [1], most often on the left side (85%), rarely on the right (13%), and sporadically bilaterally (2%). Exceptionally there is true agenesis of the hemidiaphragm, but most often the defect is confined to the posterolateral area (Bochdalek hernia). The anterior (Morgagni hernia; 30%) or central areas (2%) are less frequently involved [2]. Occasionally the diaphragm is intact yet thinned and devoid of muscular fibers, and is then called diaphragmatic eventration [3]. In case of a true defect, abdominal viscera can herniate into the thorax, acting as a spaceoccupying lesion that competes with the developing lungs. These structures compromise lung development, leading to variable degrees of pulmonary hypoplasia. The lung ipsilateral to the defect is most affected, however both lungs are in essence hypoplastic. They have a lower number of airways, fewer and smaller alveoli, thickened alveolar walls, and an increased amount of interstitial tissue [5]. This leaves less alveolar airspace, and hence reduces the gas exchange surface area. Parallel to airway changes, there is a similar reduction in arteries, essentially leaving a hypoplastic vascular bed. Morphologically, the vascular wall is thickened by an increase in the arterial media and adventitia, neo-muscularization of small pulmonary arteries [6, 7] and hypermuscularization of midsize and large vessels [8]. These vessels may have an abnormal response to mechanical and chemical stimuli in the postnatal period. These sequelae, and the frequently associated malformations, require long-term follow-up for early identification and management, as well as permanent support [4]. Ventricular and atrial septal defects are the most frequent but also outflow anomalies and abnormal great vessels have been described. Following the diagnosis, patients should be promptly referred to a tertiary center experienced in assessing and managing this anomaly in the perinatal period. It is not uncommon to find some discordance with the initial assessment in the referral center, which may result in a changed perspective and different parental decisions [31]. Therefore, it is considered prudent to limit prognostic advice at first diagnosis. A complete workup, including advanced imaging and genetic testing, is performed to rule out associated anomalies and to guide multidisciplinary counseling to allow parents to make a well-informed decision about prenatal options [32, 33]. Accurate prediction is crucial, and today it is possible to predict individual mortality and to a certain extent early morbidity. This information is important as parents may want to consider their prenatal options, including termination of pregnancy as well as fetal intervention, which will be discussed in a separate chapter. Ectopic kidney; undescended/ectopic testis; horse-shoe kidney; gonadal aplasia and hypoplasia, ambiguity. A search for specific mutations leading to recognized syndromes is also recommended in case of multiple anomalies. It takes a standardized twodimensional ultrasound measurement of the lung contralateral to the defect at the level of the four-chamber view of the heart and normalizes it for the head circumference. This formula is based on data from a large normative study on normal fetuses [57].
Order forxiga 5mg free shipping
Pathogenesis Progression of Barrett esophagus to adenocarcinoma develops in a stepwise pattern with genetic and epigenetic changes diabetes signs of too much sugar buy generic forxiga from india. Clinical features: Pain or difficulty in swallowing, chest pain, progressive weight loss, hematemesis, or vomiting. The term gastropathy is used when inflammatory cells are rare or absent (hypertrophic gastropathy). Pathogenesis Acute (also chronic gastritis) can develop following disruption of any of the protective mechanisms (refer pages 552-3). Clinical Features It may be asymptomatic or cause variable degrees of epigastric pain, nausea and vomiting. When severe, it causes mucosal erosion, ulceration, hemorrhage, hematemesis and melena. Gastritis: Presence of neutrophils above the basement membrane in direct contact with the epithelial cells indicates active inflammation. These include severe trauma, extensive burns, intracranial disease, major surgery and any severe physiologic stress. Curling ulcers: They develop in the proximal duodenum with severe burns or trauma. Cushing ulcers: They develop in the stomach, duodenum, and esophagus in patients with intracranial disease. Clinical Features Most critically-ill patients in intensive care units show microscopic evidence of gastric mucosal damage. Chronic gastritis is chronic inflammation of stomach associated with mucosal injury. Microscopically, there is an increase in inflammatory cells in the lamina propria. Causes: Common cause of chronic gastritis is due to infection by Helicobacter pylori. Other causes include autoimmune gastritis and less common causes such as radiation injury, chronic bile reflux and mechanical injury. Write a short note on role of Helicobacter pylori in pathogenic mechanism of peptic/gastric ulcer. In gastric biopsies examined, they are found in all patients with duodenal ulcers and in majority with gastric ulcers or chronic gastritis. Humans are the primary carriers of infection and transmission is mainly through the fecal-oral route. Mode of spread: Oro-oral or feco-oral route by either kissing or ingestion of contaminated vomitus. Pathogenesis v Antral gastritis: Helicobacter gastritis is predominantly localized and mostly affects the antrum causing antral gastritis. If inflammation is limited to the antrum, increased production of acid is likely to cause duodenal peptic ulcer. Multifocal atrophic gastritis: With advancing time, the antral gastritis may progress to involve the more proximal stomach. This is characterized by patchy mucosal atrophy, reduced parietal cell mass and acid secretion, intestinal metaplasia, and has an increased risk of developing adenocarcinoma of stomach. Thus, there is an inverse relationship between duodenal ulcer and gastric adenocarcinoma. Mechanism of Action Flagella: It makes them motile, allows it to burrow and live beneath the mucus layer above the epithelial surface. Raised local gastric pH acts on the antral G cells and releases gastrin hypergastrinemia result in hypersecretion of gastric acid. The above mechanism activates neutrophils and macrophages (inflammatory response in the gastric mucosa) and impairs mucosal defensepangastritis, atrophy and gastric cancer. Microscopically, it is accompanied by lymphoid aggregates, some with germinal centers. Normal Process in the Stomach the gastric lumen pH is about 1 which is several times more than the pH of blood. Though it is needed for the digestion, sometimes, it can damage the gastric mucosa. Damaging Forces these forces are capable of inducing mucosal injury and consists of two gastric secretory products: (1) hydrochloric acid and (2) pepsinogen. Gastric Acidity Hydrochloric acid plays main role in digestion, but it also can damage the gastric mucosa. Many of the substances, which stimulate acid secretion, also stimulate pepsinogen release. Defensive Forces these are a three-level barrier composed of: (1) Pre-epithelial, (2) epithelial, and (3) subepithelial elements. Gastric mucus barrier consists of viscid mucus (forms an unstirred layer between the epithelium and the gastric lumen) and bicarbonates. It is formed by several factors produced by surface epithelial cells, such as: (a) production of mucus, (b) bicarbonate secretion, (c) epithelial cell ionic transporters that maintain intracellular pH and (d) intracellular tight junctions. Actions of mucus are: n Mucus layer promotes formation of an "unstirred" protective layer of fluid on the mucosa. It results in a pH gradient, ranging from 1 or 2 at the gastric luminal surface, and reaching to a neutrality of 6 to 7 along the epithelial cell surface. Epithelial Barrier It consists of surface epithelial cells that acts through (a) restitution of damaged gastric epithelial cells, (b) epithelial regeneration, (c) secretion of prostaglandins and (d) production of mucus (see above). Components of the normal process involved in maintenance of balance of two opposite forces of gastric mucosa is discussed above. It is associated with increased secretion of gastric acid and reduced duodenal secretion of bicarbonate. Cigarette smoking: Impairs blood flow to the mucosa and healing of mucosal damage. Alcohol, radiation therapy and chemotherapy: They cause direct injury to mucosal cells. Others n High-dose corticosteroids: They suppress prostaglandin synthesis and impair healing. Anastomotic site: It can develop at the anastomotic site in patients who have undergone a distal gastric resection. Occur at margins of the gastroduodenal anastomosis/gastrojejunostomy (anastomotic ulcer). These are rare nowadays because of present efficient acid-suppressing therapies available for peptic ulcer. Multiple ulcers: In the duodenum, stomach, and/or jejunum in Zollinger-Ellison syndrome. At metaplastic or heterotopic gastric mucosa: For example, Meckel diverticulum within an ileum having ectopic gastric mucosa. From the lumen outward four layers can be identified and are known as Askanazy zones. Superficial exudative zone: It consists of fibrinopurulent exudates with predominantly neutrophilic inflammatory infiltrate. Granulation tissue zone: It consists of granulation tissue infiltrated with mononuclear leukocytes. Zone of cicatrization: It consists of fibrous tissue or collagenous scar which forms the base of the ulcer and may show chronic inflammatory cells.