Discount avanafil 50 mg with amex
These measurements determine the dimensions of the graft material erectile dysfunction doctor visit discount 200mg avanafil with amex, which is trimmed to size. The previously placed pelvic sidewall sutures are then brought out to the corresponding locations on the graft. It is useful to leave the sutures long until after cystoscopy confirms patency of the ureters. The vaginal wall is judiciously trimmed, if needed, and closed with a 2-0 absorbable suture. Anterior Polypropylene Mesh Results Nicita (1998) described the use of polypropylene mesh for the treatment of anterior vaginal wall prolapse (see Table 124. He sutured the mesh to the anterior aspect of the arcus tendineus fascia pelvis on each side using 3-0 Prolene sutures. The only patient that developed dyspareunia had vaginal mesh extrusion (exposure), and this was managed with mesh trimming and vaginal closure. Several subsequent studies using polypropylene mesh reported variable success ranging from 76% to 98% (de Tayrac et al. The lateral extensions of the mesh were placed in contact with the arcus tendineus fascia pelvis and anchored with a transobturator approach. After a mean follow-up of 18 months, the authors reported an anatomic success rate of 97. In a subsequent series with 87 women and with 24 months of follow-up, de Tayrac again used Gynemesh and found that 77 women (88. Capio needle driver used to facilitate suture placement in the arcus tendineus fascia pelvis. No statistical difference in outcomes was noted with either objective or subjective measures. After 3 years of follow-up, the addition of the polypropylene mesh to the anterior repair did statistically decrease the risk of recurrent stage 2 or greater anterior prolapse. Recurrence was noted in 14 of 105 women in the mesh group versus 40 of 97 women in the group with no graft (P < 0. However, there was no statistically significant difference in symptomatic outcomes (pelvic pressure, vaginal bulge, or difficulty with bladder emptying) between the groups. Polypropylene mesh is anchored to the sacrouterine ligament at the bladder base, laterally to the obturator fascia, and distal to the bladder neck using 2-0 polyglactin suture. Additional prolapse surgery was not more common in the anterior colporrhaphy group, and no differences in QoL data or de novo dyspareunia were identified. These finding as well as an increased awareness of the severity of complications of using vaginal mesh for prolapse has led to the near abolition of the use of transvaginal mesh patch interposition or mesh kits. Alteration of the vaginal axis with compensatory prolapse in an untreated compartment has been well reported. Development of apical and or posterior prolapse (stage 2 or greater) after an anterior repair with mesh was seen in 46% of 150 women (Withagen et al. Pooled analysis of two studies that reported de novo prolapse after anterior repair (Nieminen et al. Anterior Repair With Cadaveric Fascia Results Cadaveric fascia lata with or without pubovaginal sling has shown efficacy rates of 81% to 100% for the treatment of anterior vaginal wall prolapse (Frederick and Leach, 2005; Groutz et al. The addition of the fascia lata patch to the anterior repair did not statistically decrease the risk of recurrent prolapse (P = 0. Cadaveric dermis has been used in the treatment of anterior compartment prolapse with efficacy of 42% to 84% at 2 years of follow-up (Behnia-Willison et al. In a retrospective review of 70 patients, 61 (87%) had no cystocele recurrence after a mean follow-up Chapter 124 Vaginal and Abdominal Reconstructive Surgery for Pelvic Organ Prolapse 2787 Biologics Versus Mesh Results Natale et al. No difference in subjective cure was noted; however, a better impact of surgery on sexual function was reported in the porcine group. Mesh repairs had the lowest anatomic failure rate (18%), followed by porcine (46%, P = 0. Subjective improvement in prolapse and voiding scores were similar, and composite failure was no different among groups (4% mesh, 12% porcine, 13% colporrhaphy). Mesh-Related Complications Vaginal exposure (extrusion) has been reported in anterior compartment prolapse repair with most materials. In 21 trials on mesh-augmented repairs summarized in a Cochrane review, the mean mesh extrusion rate was 11. Reoperation rates for prolapse, QoL measures, and de novo dyspareunia were no different in women undergoing native tissue repair versus mesh repair (Maher et al. Three pairs of delayed absorbable sutures are inserted into the arcus tendineus fasciae pelvis and into the porcine dermis patch. One patient had superficial vaginal wound separation, which was treated with conservative measures. After 1 year of follow-up, the women randomized to receive the Pelvicol graft failed 7% of the time compared with the 19% failure rate in those women who underwent the anterior colporrhaphy alone (P = 0. One patient who received the Pelvicol graft had vaginal extrusion of the material 1 month after surgery. There were no differences between the 2 groups in the incidence of postoperative dyspareunia. Handel compared two different grafts (polypropylene mesh [n = 25] and porcine dermis [n = 56]) versus traditional anterior colporrhaphy with suture alone (n = 18) (Handel et al. For patients undergoing repair with a graft, it was anchored to the levator fascia bilaterally and to the uterosacral-cardinal ligament complex apically. Both operations significantly improved QoL without differences noted between the groups. The retropubic space is entered through either a low midline or transverse incision. The site of normal vaginal attachment on the pelvic sidewall from the interior aspect of the superior pubic ramus to the ischial spine is then identified. These sutures are then placed in the appropriate location in the lateral wall of the vagina. Care is taken to avoid paravaginal veins, which commonly course through this area. Elevating the vagina to its normal anatomic position to localize suture placement site may facilitate vaginal suture placement. After the sutures are tied, cystoscopy must be performed to confirm ureteral patency and the absence of intravesical sutures. Paravaginal defect repair as viewed from the retropubic space: approximation of the pubocervical fascia medially to the arcus tendineus fascia pelvis laterally with 2-0 braided nonabsorbable suture. Note the vertical orientation of the vaginal vessels in relation to the transverse orientation of the bladder vessels. Inset shows suture being passed beneath the vaginal vessels to ensure generous purchase of pubocervical fascia and control of hemostasis. In a retrospective study of 233 patients with follow-up spanning 2 to 8 years, Richardson et al. Of these patients, 53 (23%) had previously undergone 1 or more anterior vaginal wall prolapse repairs. Colombo found that Burch colposuspension increased the functional urethral length and pressure-transmission ratio in the proximal urethra, whereas the abdominal paravaginal repair did not. With a mean follow-up of 17 months, 4 patients (8%) had recurrent cystocele, 3 patients developed vault prolapse, and 1 patient developed an enterocele. Interestingly no anatomic failure occurred after 38 months, inferring that site-specific repair by either route has curative potential. The results from 45 women found no statistical difference between the abdominal (N = 20) and vaginal (N = 20) approaches, but they had to abandon the laparoscopic (N = 5) approach because of the lack of improvement in prolapse stage (Hosni et al. Fluoroscopic imaging of the bladder demonstrating a large cystocele before (A) and after (B) Valsalva maneuver was performed. They also noted that none of the women had urethral obstruction after pessary placement.
Avanafil 200 mg on-line
A retrograde urethrogram demonstrates filling of the rectum in this patient who was seen several years after brachytherapy with fecaluria enlarged prostate erectile dysfunction treatment order avanafil 200 mg with mastercard. Fistulae caused by Crohn disease are complex, and management should be individualized (Cools et al. Digital rectal examination often permits palpation of the fistula tract along the anterior rectal wall. Cystoscopy and sigmoidoscopy visualize the fistula tract in the majority of cases and provide a mechanism for biopsy. In patients with a history of pelvic malignancy, biopsy of the fistula is suggested to evaluate for a local recurrence of the tumor (Shin et al. Lateral projections may be necessary to visualize small fistulae, because contrast in the rectum or urethra can sometimes obscure extremely thin fistulous tracts (Karsten et al. Additional procedures may be needed to bring about a satisfactory result in these patients; this is an important issue to discuss in preoperative patient counseling. After prostate cancer treatment 201 patients underwent rectourethral fistula repair. In the ablation group 84% of patients underwent bowel diversion before rectourethral fistula repair compared with 65% in the prostatectomy group. Concomitant bladder neck contracture or urethral stricture developed in 26% of patients in the ablation group and in 14% in the prostatectomy group. The ultimate success rate of fistula repair in the energy ablation and radical prostatectomy groups was 87% and 99% with 92% overall success (Harris et al. Urinary drainage consisted of urethral catheter in all patients and suprapubic catheter in 14 (47%). Spontaneous healing was achieved in 14 patients (47%): 8 (27%) without fecal diversion and 6 (20%) after fecal diversion. The majority of operated patients underwent transanal or transperineal flap (endorectal, dartos, or gracilis) successfully. Algorithm-based treatment approach for rectourethral fistula is useful in the management of this rare condition. Selective fecal diversion is possible, and majority of patients who require definitive intervention can be treated with a transanal or transperineal approach. The rate of permanent stoma is low, but long-term urinary dysfunction is frequent (Keller et al. An interposition flap or graft was placed in 91% and 92% of the 2 groups, respectively. Postoperatively the rates of urinary incontinence and complications were higher in the energy ablation group at 35% and 25% versus 16% and 11%, respectively. Spontaneous healing was achieved in 14 patients (47%): 8 (27%) without fecal diversion, and 6 (20%) after fecal diversion. Only 2 patients (7%) required an abdominal approach (positive oncologic margins or nonfunctioning bladder). Fifteen out of the 20 patients (75%) who underwent fecal diversion had stoma closure with an overall permanent stoma rate of 17%. The controversy surrounding the staged repair centers on the issue of whether to perform fecal diversion at all, or whether to perform it before or at the time of repair of the urinary tract. This is considered the standard conservative approach and, in combination with an indwelling urethral catheter, permits a trial of spontaneous healing of the fistula without open manipulation of the urinary tract. In support of the single-stage repair, a successful one-stage approach limits the potential morbidity and cost of multiple procedures that, by design, accompany the staged repair. Staged repairs may be considered in cases of large fistulae, those associated with radiation therapy, uncontrolled local or systemic infection, immunocompromised states, or inadequate bowel preparation at the time of definitive repair. Tissue interposition flaps, predominantly gracilis muscle, were used in 72% of repairs. Most high-volume centers (25 patients) performed transperineal repairs with tissue flaps in 100% of cases. Regardless of complexity, Urinary Tract Fistulae 2957 rectourethral fistulas have an initial closure rate approaching 90% when the transperineal approach is used. Permanent fecal and/or urinary diversion should be a last resort in patients with devastated, nonfunctional fecal and urinary systems. The York-Mason procedure is a transrectal, transsphincteric approach that has been found to be effective and to have low morbidity. However, in patients with small, nonirradiated fistulae, a single-stage approach can be used, provided that a vigorous bowel preparation and broad-spectrum antibiotics are used (Renschler and Middleton, 2003). For repair of the urinary tract, the patient is placed prone on the operating room table in the jackknife position. A full-thickness incision through the posterior anus and dorsal rectal wall is performed and deepened down to the level of the coccyx through the external anal sphincter. Later in the procedure during closure, careful anatomic reapproximation of the layers of the external anal sphincter is necessary to avoid the devastating complication of anal incontinence postoperatively. The anorectal incision as described provides excellent exposure of the fistula in the anterior rectal wall. The fistula tract is excised, and the anterior rectal wall is mobilized circumferentially around the fistula margins. Closure of the incision is performed by reapproximating the posterior rectal wall and then sequentially closing the layers of the anal sphincter in an anatomic fashion. In the largest series of patients undergoing the York-Mason procedure, Renschler and Middleton (2003) reported a successful repair in 22 of 24 patients. One of the two failures was subsequently repaired with another York-Mason procedure. No serious complications were reported, and no patient developed anal incontinence or anal stenosis. The major disadvantage to this approach is the relatively poor exposure and lack of maneuverability within the operative field. Anatomically, this is a familiar approach for many urologists and has the added advantage of local access to a variety of potential interpositional flaps. Excellent results have been obtained with the perineal approach in combination with an interpositional flap, including gracilis muscle (Choi et al. The principal advantage of this technique is the availability of greater omentum for an interpositional flap. Potential disadvantages include the morbidity and prolonged postoperative convalescence associated with a laparotomy incision, poor exposure of the operative field (with limited maneuverability in the deep pelvis), and the risk of urinary and fecal incontinence. These fistulae may be large and are associated with considerable induration, fibrosis, and ischemia for a variable distance around the fistula, limiting reconstructive options. Treatment of renovascular fistulae is contingent on the presentation, cause, and hemodynamic stability of the patient. Patients with severe hemorrhage on removal of the nephrostomy tube can be temporized in some instances by replacing the tube, or, in large mature tracts, by placing a Foley catheter to tamponade the bleeding. In patients with ongoing bleeding, transcatheter angiographic embolization of the lacerated vessel is recommended. Even repeat arteriographic treatment can be necessary in case of persistent bleeding, which can be caused by missed pseudoaneurysm and the recanalization of the embolized vessels or new renal vascular lesion. The lesion may be missed during the initial arteriography because of arterial spasm. Progressive deterioration of the injured vessel integrity could be the other possibility (Zhaohui et al. Occasionally, flank exploration is necessary with partial or simple nephrectomy to control hemorrhage. Patients who had irradiated rectourethral fistulas required significantly more complex operations, likely contributing to the higher morbidity, mortality, and lower fistula closure rate (Hanna et al. In another group of 45 patients, those with prior radiation/ablation were significantly more likely to require permanent colostomy (25 of 29 [86%] vs. Urinary reconstruction may not be possible in some of these cases, necessitating urinary diversion (Faris et al. Most reported ureterovascular fistulae are ureteroiliac artery fistulae, although ureteroiliac vein fistulae have been reported as well (Teuton et al. Ureteroaortic fistulae (and perigraft fistulae) are rare and have a high mortality (Deem et al. Most cases of ureteroarterial fistulae are reported in patients with a prior history of vascular disease, radiation therapy, and/ or pelvic surgery, especially in the setting of indwelling ureteral stents (Aslam et al.
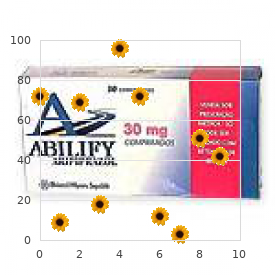
| Comparative prices of Avanafil | ||
| # | Retailer | Average price |
| 1 | 7-Eleven | 458 |
| 2 | Target | 732 |
| 3 | Rite Aid | 785 |
| 4 | IKEA North America | 620 |
| 5 | Defense Commissary Agy. | 471 |
| 6 | Nordstrom | 940 |
| 7 | O'Reilly Automotive | 245 |
| 8 | Army Air Force Exchange | 427 |
| 9 | QVC | 394 |
Order avanafil with paypal
It is important to note that erectile dysfunction journal order avanafil 100mg amex, despite effective healing of the urethra after mesh removal, eventual incontinence and inadequate symptom resolution may occur (Kowalik et al. Long-term follow-up and additional treatment options are warranted in this population. During surgical intervention for slings that perforate into the urethra, we prefer an inverted-U incision because this allows for excellent exposure of the proximal urethra, bladder neck, and endopelvic fascia. Likewise, this incision provides a vaginal epithelial flap that avoids overlapping suture lines, theoretically decreasing the risk for a fistula. The distal portion of the inverted U should be distal to the site of the urethral perforation, and the proximal portions of the U should extend to the level of the bladder neck in most cases. We will frequently use a Martius labial fat pad flap to further prevent fistula formation. Mesh excision is typically carried out to the level of the pubic bone or ischiopubic rami. This type of excision leaves behind the arms of the mesh that tunnel into the retropubic space or obturator fossa. It is not typically necessary to enter these spaces because the mesh at this location is no longer under tension and is far from the urethra. The majority of intravesical mesh perforations are most likely the result of an unrecognized cystotomy or placement of the mesh within the urinary bladder at the time of surgery. True migration of the mesh across the seromuscular wall of the bladder into the lumen is much less likely, and this underscores the importance of performing a complete and thorough cystoscopic examination of the bladder with adequate hydrodistention to minimize this complication. We have found that the trocar may sometimes telescope the bladder wall during insertion and obscure visible bladder perforation. Imaging modalities such as computed tomography scans and cystography may help in difficult cases but are not a substitute for cystoscopic examination. She initially had mesh on the left side of the bladder, then 6 months later had sling material on the right side of the bladder. She underwent a successful transurethral, transvaginal, and suprapubic mesh resection. Different techniques and surgical approaches have been advocated with varying levels of invasiveness, complexity, and success. For small areas of mesh perforation, the literature supports endoscopic excision with scissors or ablation with the holmium laser as an appropriate initial step. In 14 women with intravesical mesh, Oh and Ryu (2009) transurethrally resected the mesh deep into the perivesical fat. The women had dysuria, hematuria, pelvic pain, and urgency preoperatively, and six women had stone encasing the mesh at the time of transurethral excision. In a case report, Jorion (2002) excised the mesh endoscopically using an offset nephroscope transurethrally and a 5-mm laparoscopic trocar placed suprapubically. Laparoscopic grasping forceps were used to grasp the mesh, and endoscopic shears excised the mesh flush with the bladder mucosa, allowing for easy mesh removal. Cystoscopy at 1 month revealed healed mucosa, and the woman was continent and symptom-free. In another report, the mesh was initially cut endoscopically, but because of an adherent calculus, the mesh could not be extracted endoscopically (Tsivian et al. Therefore, a suprapubic approach was required to remove the stone and intravesical mesh. Since stones frequently form on the intravesical portions of the sling, Irer et al. We reserve endoscopic (holmium laser) management of intravesical mesh perforation for very small areas of perforation in select patients. If endoscopic excision is attempted and fails, removal of perforated bladder mesh can be removed through a transvaginal or retropubic approach. For slings that perforate into the bladder at or below the trigone, we prefer an inverted-U incision similar to the aforementioned management of urethral perforation because this allows for exposure of the proximal urethra, bladder neck, and endopelvic fascia. Furthermore, this incision provides a vaginal epithelial flap that avoids overlapping suture lines, theoretically decreasing the risk for fistula. Similar to the management of urethral perforations, we do not excise the entire sling as long as it is no longer under tension and is well away from the bladder. For slings that perforate the bladder dome or other areas of the bladder not accessible from a transvaginal approach, we remove the mesh transabdominally. The sling can usually easily be seen entering the bladder in the retropubic space. Although not always necessary, opening the bladder in the midline usually aids with closure and identification of the exact area of bladder perforation. In general, reconstruction should involve nonoverlapping suture lines and may benefit from interposition of tissue such as a labial fat pad, greater omentum, peritoneum, or autologous fascial sling. The bladder was closed with absorbable suture, and catheter drainage was maintained postoperatively. One woman was managed with periurethral collagen injection, and two underwent pelvic floor muscle training and estrogen. There are several reported cases of successful laparoscopic removal of intravesical mesh after retropubic sling placement. The authors have also had success with an intraperitoneal robotic-assisted approach in women with bladder dome or posterior wall perforation. Thigh and groin pain appear to be more commonly associated with the transobturator approach. A randomized controlled study from Finland revealed that 16% of women in the transobturator (in-to-out) group had groin pain compared with only 1. The authors hypothesized that the cause of the pain was either subclinical hematoma or a transient neuropathic phenomenon. Roth (2007) found that steroids and local anesthetic were effective for pain relief with no side effects in three women with persistent groin pain 3 months postoperatively. Wound-related complications include minor superficial cutaneous infections and pelvic abscesses. Connolly (2004) reported a case of necrotizing fasciitis in an obese, diabetic woman that resolved after intensive resuscitation. It is interesting to note that a review of necrotizing fasciitis in gynecologic surgery found that obesity (88%), hypertension (65%), and diabetes (47%) were all risk factors for postoperative fasciitis (Gallup et al. The sling was easily removed through a vaginal incision, and mesh cultures were positive for Bacteroides fragilis. Abscesses and adductor myositis have also Chapter 125 been reported, manifesting as leg pain, difficulty ambulating, and cellulitis (DeSouza et al. Initial conservative management was successful in most women, with four women with persistent or severe pain treated with a combination of steroid and local anesthetic injections. Two women developed recurrent pain and had significant pain relief after sling excision. In the case of retropubic mesh, this involves an abdominal and vaginal incision, and in the case of transobturator mesh, this involves incisions in the medial thigh and vagina. For the complete excision of transobturator mesh, we typically consult an orthopedic surgeon to aid with lateral dissection of the sling. Five of the eight women were cured of their pain after a median follow-up of 8 months. Based on anecdotal experience after removing hundreds of chronically obstructive slings, we have found that obstructive slings are most likely to be found close to the bladder neck. In addition, we have found that progression of anterior and apical prolapse can cause a nonobstructive sling to become obstructive 10 years or more after placement of the sling. If the diagnosis of sling obstruction is in doubt, urodynamics can be performed to provide confirmation (Levin et al. The most common symptoms of obstruction are an inability to void (urinary retention), incomplete emptying, and de novo urgency and frequency. The urinary storage symptoms and pain become more prevalent over weeks to months as the bladder attempts to adjust to the obstruction. The optimal evaluation for women with postoperative voiding dysfunction is poorly defined in the literature. The decision to perform urethrolysis or sling incision is usually based on a clear temporal relationship between onset of symptoms and the surgical procedure. However, it appears that the temporal relationship correlating symptoms with an antecedent surgical procedure should be the primary criterion in selecting women for sling-release procedures. Cystoscopy is useful to rule out bladder pathology, urethral mesh perforation, and a hypersuspended bladder neck.
Cheap avanafil 50mg line
Tibaek S impotence in men over 50 generic avanafil 50 mg online, Gard G, Klarskov P, et al: Are activity limitations associated with lower urinary tract symptoms in stroke patients Whittle J: How can rates of prostate-specific antigen screening be reduced in men aged 80 and older Although most fistulae in patients in the industrialized world are iatrogenic, they may also occur as a result of congenital anomalies, malignancy, inflammation and infection, radiation therapy, iatrogenic (surgical) or external tissue trauma, ischemia, parturition, and a variety of other processes. The continuous leakage of urine and/or fecal material can have a devastating effect on the quality of life of the patient. Except for a palliative setting, the active treatment of fistulae is always warranted. Although some types of urinary fistulae heal with conservative management, surgery is usually necessary for a definitive repair. These should be approached on a case-by-case basis, because repair may involve some innovative and even improvisational maneuvers in the operating room. The surgeon should be familiar with a variety of approaches and techniques, because one approach will not be optimal for all patients with a given type of urinary fistula. Ensuring adequate nutrition is integral to surgical healing in general but is especially important in the setting of a urinary fistula. Not uncommonly, the catabolic processes contributing to the lack of healing, which may have been a contributing factor in the initial fistula formation, are often ongoing. This is especially relevant in fistulae related to radiation therapy or in debilitated patients. Medicolegal Aspects Acquired urinary fistulae in the industrialized world are almost universally unexpected and may result in a great deal of inconvenience, discomfort, and physical disability for the affected individual. They are most often acquired as a result of a medical or surgical intervention for an unrelated problem, and, consequently, considerable emotional and psychological distress often accompany the diagnosis and subsequent treatment. Often medicolegal issues occur with a high risk for litigation (Thomas and Williams, 2000). Nevertheless, minimizing patient discomfort, maintaining a positive and honest patient-physician relationship while providing constant reassurance, and, finally, and perhaps most important, pursuing expeditious and successful treatment of the fistula most often result in a mutually satisfying long-term outcome. Notably, after the initial early diagnosis of a urinary fistula, which results in external urinary leakage, immediate management or control of the urinary leakage is vital. Addressing this quickly will reduce skin breakdown and related complications, as well as alleviate much of the psychological distress. The judicious use of catheters, pads, skin care, and odor control products and appliances can be very helpful in this regard. These simple measures can often deflect the anger of an otherwise very disaffected patient, thereby reducing the potential for further aggravating an already difficult medical and, possibly, litigious situation. Careful planning and execution of gynecologic or cancer surgery and/or radiotherapy reduce the risk of iatrogenic fistula formation, although there is little research on the impact of preventive measures on this type of fistulae. The risk factors for obstructed labor are well known: illiteracy, low economic status, and short stature (<150 cm) (Kasamba et al. The finding of a persistent fistula after presumably definitive treatment may suggest the existence of other contributing host factors, such as malignancy, nutritional issues, the possibility of an unrecognized foreign body, tissue ischemia, or surgical factors such as inadequate postoperative urinary drainage, persistent distal urinary obstruction, or technical problems with the surgery (Arrowsmith et al. Preparation and Optimization of Patient Prevention of urinary fistulae is, of course, paramount; however, nutrition, infection, and malignancy are important considerations not only when assessing a patient for the risk of creation of a fistula during any given intervention but also during an evaluation for the repair of an existing urinary fistula. Although the majority of urinary fistulae in the industrialized world occur in healthy, well-nourished individuals, a nutritional assessment may be an important factor in some patients with fistulae, such as those patients with malignancies. The first surgical repair was described in 1663 by Hendrik von Roonhuyse denuding the fistula margins and then approximating them with sharpened stiff swan quills (Margolis and Mercer, 1994). As resources increase within these countries, the number of obstetric fistulae seems to decrease, but those of iatrogenic fistulae seem to increase (Tebeu et al. Voiding cystourethrogram demonstrates filling of the vagina (arrows) with voiding as a result of a posthysterectomy vesicovaginal fistula. The technique was subsequently modified as a partial colpocleisis by Latzko (1942) and the more commonly used dissection and repair in layers or "flap-splitting" technique (variously attributed to Hayward, Collis, and Lawson Tait) (Wall, 2005). The studies included data from West Africa, Bangladesh, Turkey, Jordan, Ethiopia, Egypt, and India. The major risk factors for both appear to be age at first marriage, short stature, pregnancy with a male child rather than a female child, failure to attend antenatal care, low socioeconomic status, low social class, lack of employment, and illiteracy. The affected individuals, commonly young teens, are often ostracized and shunned by family and friends and become permanent outcasts in society. The time of onset of labor is rarely recorded, and reports from delivery locations may disregard the fact that the woman has labored at home for days before attending the delivery location. The ureteral catheters have been passed through the urethra and delineate the ureteric orifices before repair. Digital examination confirms rectovaginal and vesicovaginal fistulae in this patient. The mean duration of the fistula was 4 years, and the entire care process took up to 2. Health system causes such as poor quality obstetric care, staff unaccountability, late referral, and poor nursing standards are prevalent in sub-Saharan Africa and rural areas of Pakistan and other parts of Asia (Jokhio et al. This ritual practice involves using a knife to incise the anterior vagina as a treatment for a variety of conditions, including infertility, dyspareunia, dysuria, and back pain. The remainder are related to general surgical procedures in the pelvis, anterior colporrhaphy or cystocele repair, anti-incontinence surgery, or other urologic procedures. Overall, the risk of pelvic organ fistula after hysterectomy has been reported to be between 0. It is important to recognize that most urinary tract injuries do not result in a fistula. The relative proportions of the types of urinary fistula have changed with urethral fistulae having increased, whereas ureteral, bladder and/or urethral fistulae have decreased. At the Zekai Tahir Burak center in Turkey, 25,998 gynecologic and obstetric operations were performed over a 3-year period. If unrecognized intraoperatively, a pelvic urinoma may develop and ultimately drain out through the vaginal cuff. Tissue ischemia and then necrosis promote fibrosis and induration, finally resulting in an epithelial or mucosal lining of the tract and the development of a fistula tract. The degree of bladder injury appears to be a major factor in iatrogenic fistula formation. The bladder lacerations occurred during the hysterectomy portion of the surgery in 61% of cases and during the additional procedures in 39% (Mathevet et al. Most fistulae occurred as a consequence of caesarean section, surgical intervention, or hysterectomy for ruptured uterus (Raassen et al. The rate of urogenital fistulae associated with simple abdominal hysterectomy for benign disease is often described as being approximately 1 in 1000.
Quality 200mg avanafil
The patient may be at greater ease with an enterostomal therapist to express concerns about forms of urinary diversion best erectile dysfunction doctors nyc generic 100 mg avanafil otc, so consultation with such a therapist may be extremely helpful. Certain patients may not be able to comprehend the strict flushing, irrigation, and catheterization regimens that must be followed after continent urinary diversion or may lack the motor skills to independently perform self-care. Patients with multiple sclerosis, quadriplegic individuals, and very frail or mentally impaired patients will at some point in their lives require family or visiting nurses for basic care and are therefore viewed as poor candidates for any form of continent diversion. Indeed, these patients may also require assistance with external appliances, but the degree of time and expertise required is much less burdensome on the care provider and the health care system. On the contrary, continent catheterizable diversion requires continuous attention and may limit patient and family options when determining long-term care needs. Therefore the site for a potential external stoma should be selected with care before the operation. In general, the location must be free from fat creases in the standing and sitting positions, and it should not be close to the umbilicus or prior abdominal scars that may interfere with proper adherence of an external appliance. In general, the stoma should be brought through the right (or left) lower quadrant of the abdomen on a line extending from the umbilicus to the anterior superior iliac spine. The stoma should be as far lateral from the midline as possible, but the site selected should ensure that the bowel segment comprising the stoma traverses the rectus muscle. The selected site for the stoma should be marked with an X scratched onto the anterior abdominal wall. Marking the stoma site with ink should be avoided because it may be washed away during the antiseptic preparation of the skin. The surgeon undertaking continent urinary diversion should be familiar with more than one type of continent urinary diversion technique. Although it is uncommon to have to abandon a given bowel segment for the reservoir, it is not uncommon to have to modify the antireflux or continence mechanism. In these circumstances, it is essential that the surgeon be able to select an alternate form of continent diversion from what was originally intended. Renal and hepatic function must be reviewed carefully in the patient selected for continent diversion (Mills and Studer, 1999). The reabsorption and recirculation of urinary constituents and other metabolites require that liver function be normal. Renal function should be determined preoperatively, and if borderline, creatinine clearance should be measured. A minimal level of at least 60 mL/ min should be documented before the patient is deemed an appropriate candidate for continent diversion. In the case of unilateral or bilateral hydronephrosis, the upper urinary tract(s) should be decompressed with ureteral stenting or percutaneous nephrostomy, with subsequent reevaluation of renal function before consideration for a continent diversion. Procedures that require the use of the colon should always be preceded by a colonoscopic assessment of the entire large intestine. Performing only a sigmoidoscopy for a procedure that will use only this segment of the large bowel is insufficient because disease proximal to the resected segment may leave the patient with short colon syndrome. The preoperative assessment of the colon is not mandatory but remains prudent if continent urinary diversion using small intestine is planned. Most patients undergoing radical cystectomy can be admitted to the hospital on the day of surgery. In most institutions a mechanical bowel preparation is employed on the day before surgery, in addition to oral metronidazole (500 mg) the night before. However, in addition to general surgery literature, several nonrandomized urologic studies have called into question the usefulness of preoperative bowel preparation for urinary diversion using small bowel (Large et al. These require a midline incision, skirting the umbilicus to the side opposite the selected stoma site. The incision for a right colon pouch usually extends from the pubis to a point midway between the umbilicus and the xiphoid. The cranial extent of the incision is governed by the hepatic flexure, which must be divided to obtain sufficient colonic length and to allow for the right colon to easily fold on itself. The incision for procedures using only the ileum may only extend to just below the umbilicus, but the length of the incision should be tailored to the patient and will vary. The cystectomy procedure is covered elsewhere in this text, and only those points germane to continent diversion are covered here. After abdominal exploration, the ureters are isolated, transected, and transposed to an appropriate place for subsequent diversion. The right retroperitoneum is first opened over the iliac artery to expose the right ureter. In the typical circumstance of conduit diversion, the right ureter is transected below the common iliac artery. For all continent diversions, both ureters are transected as low as possible and shortened to the appropriate length once the final anatomy has been determined. The sigmoid colon is freed from its lateral peritoneal attachments by incising along the line of Toldt. A wide tunnel is created by blunt finger dissection ventral to the aorta and common iliac arteries and caudal to the inferior mesenteric artery. This affords left ureteral access to the previously exposed right retroperitoneum. In cases of uroepithelial malignancy, it is prudent to evaluate the margin status of the most distal portion of both ureters using frozen-section analysis. In situations in which substantial ureteral length is removed to obtain negative surgical margins, extension of the afferent limb mechanism may be necessary to allow tension-free ureteral intestinal anastomoses. In carrying out bowel surgery for continent urinary diversions, stapling is the preferred method for division of Cutaneous Continent Urinary Diversion 3207 the bowel segment as well as for reconstruction of bowel continuity. This technique shortens operative times greatly and affords safe and reliable bowel anastomosis. Suturing is not necessary with the exception of placing two silk Lembert sutures at the apex of side-to-side stapled bowel anastomoses to prevent tension on the staple line. To avoid stone formation on the stapled proximal bowel segments, oversewing the stapled end of the conduit with absorbable material isolates the metal staple line from urinary contact within the lumen. To construct a nonappendiceal continent urinary diversion stoma, a skin button matching the diameter of the structure to be used in the diversion is resected. Cutaneous tissues are separated down to the level of the anterior rectus fascia, where a circle of similar diameter is excised from this fascia, or alternatively the fascia is incised in a cruciate fashion. In carrying out this maneuver, the surgeon must ensure the fascia and skin are properly aligned to avoid angulation. Rectus muscle fibers are separated bluntly, and an instrument is passed through the posterior fascia and peritoneum. Alternatively, the appendix lends itself to an umbilical stoma (Bissada, 1993; Gerharz et al. These stents drain urine externally, ensuring that urine is safely diverted beyond any anastomotic site during the early healing period. The distal end hole allows for the passage of a straight wire through the stent, which decreases the likelihood of anastomotic trauma at the time of stent removal. The bulb suction should be opened before removal to prevent inadvertent creation of a hernia at the site. In obese patients, those with tissues of poor quality, or nutritionally depleted patients, through-and-through stay sutures can also be used. Ureteral stents should always be brought through separate abdominal incisions, sutured to the anterior abdominal wall, and directed into separate drainage bags for monitoring of urine output. Even at this early stage it is important to ensure adequate drainage of the reservoir to prevent pouch rupture should the ureteral stents be displaced. In the case of limited pouch access such as with an appendiceal stoma, a large (approximately 28 Fr) Malecot tube should be placed directly into the reservoir and secured to the skin. The reservoir is sutured to the abdominal wall to prevent urine leakage into the peritoneal cavity when the tube is removed. This maneuver also helps to prevent migration and angulation of the reservoir, which could result in incontinence or catheterization difficulties. First, the variations of ureterosigmoidostomy such as ileocecal sigmoidostomy, rectal bladder, and the sigmoid hemi-Kock operation with proximal colonic intussusception allow for excretion of urine by means of evacuation. Second is the large category of continent diversions requiring clean intermittent catheterization of the constructed pouch for urine drainage at standard intervals. The concept of refashioning bowel so that it serves as a urinary reservoir rather than a conduit has become universally accepted.
Syndromes
- Anti-nausea medication
- Embryonal carcinoma
- Collapse
- Seizures
- Hepatocellular carcinoma (hepatitis B virus)
- Surgical removal of burned skin (skin debridement)
- Coughing, wheezing, trouble breathing, or an asthma attack.
- Pain or feeling of fullness below the ribs
- Injury to the voice box (larynx), thyroid gland, or esophagus
Order avanafil overnight
An incision is made in the midline from 2 cm above the umbilicus to just above the level of the pubis (B) erectile dysfunction doctor in karachi best avanafil 100 mg. This is carried in a cephalad direction to the level of the vas deferens in men and the round ligament in women. The peritoneum is incised lateral to the medial umbilical ligaments bilaterally to the level of the internal inguinal rings at which point the vas deferentia in men and the round ligaments in women will be identified and are divided. Attention is then turned to the bowel mobilization to achieve adequate exposure of the great vessels and the ureters. On the right side the white line of Toldt is incised and carried around the cecum where then the posterior peritoneum is incised to allow mobilization of the root of the small bowel mesentery. On the left side the white line of Toldt is likewise incised, and a window is created below the sigmoid colon mesentery to communicate with the right-sided posterior peritoneotomy. With the aid of a retractor such as a Bookwalter, exposure is maximized and the bowel retracted cephalad. Communication with the anesthesiologist at this point is vital to ensure that inadvertent compression of the vena cava has not occurred. A moistened laparotomy pad or pads should be placed behind retractor blades to protect the abdominal contents. After adequate exposure is achieved, the bilateral ureters are dissected free from their attachments beginning a few centimeters above where they cross the iliac arteries to the level of the detrusor hiatus. The obliterated umbilical artery should be ligated and divided before completing the ureteral dissection; this aids in maximizing ureteral length. The ureter is then controlled with either suture ties or suture ligature and divided. Although controversial, the distal ureteral margin can be sent for frozen section analysis to evaluate for the presence of urothelial carcinoma. Although studies have shown a correlation between findings of carcinoma in the ureteral margin and subsequent upper tract recurrence (Schumacher et al. According to surgeon preference, temporary ureteral catheters directed off the surgical field can be used to maintain urinary flow during the remainder of the procedure, or the ureters can be temporarily ligated to avoid spillage of urine into the operative field. Although further extension cephalad to include the preaortic packet to the level of the inferior mesenteric artery has been studied in bladder cancer, none have demonstrated any additional staging information beyond a dissection from the common iliac arteries distally (Bochner et al. Surgical quality as measured by nodal yield has demonstrated a survival benefit in bladder cancer. Later an examination of 1260 patients in the Surveillance, Epidemiology, and End Results data set with lymph node metastatic bladder cancer showed that overall survival improved from a median of 13 months if 1 to 5 nodes were removed to 23 months if 10 or more were removed (Wright et al. If there is a large tumor at the base of the bladder, care must be observed to ensure an adequate margin of resection at this point. The rectum is dissected free with either blunt dissection or sharp dissection in the midline and is carried to the level of the prostate, at which point Denonvilliers fascia is encountered and incised. In cases of advanced disease, previous pelvic radiation, or reactive fibrosis from previous resection or intravesical chemotherapy, difficulty in developing this plane may be encountered. In such instances blunt dissection should not be performed, because this may cause inadvertent injury to the rectum. Instead, under direct visualization, sharp dissection should be performed with care taken to maintain rectal integrity. If a rectal injury is encountered, primary repair with or without flap coverage and/or bowel diversion should be performed (Kozminski et al. Care should be taken, however, if sealing instruments are used: the heat they generate can transmit and may injure the rectum if in close proximity. After completion of the posterior dissection, the urethra should be palpable, and at this point attention can be turned to the anterior dissection in a fashion similar to a radical prostatectomy. The endopelvic fascia overlying the levator muscles is incised sharply, allowing for identification of the confluence between the urethra and the dorsal venous complex. If continent ileal neobladder urinary diversion is planned, adequate urethral length must be maintained and a frozen section analysis of the urethral margin performed. In a study of 436 patients who underwent eight cutaneous or orthotopic diversions, urethral recurrence occurred in 7. In addition, the study demonstrated that patients with an orthotopic diversion were at lower risk of urethral recurrence (4% vs. In another study of 118 male patients after radical cystectomy, no patients with a negative intraoperative urethral frozen section had a urethral recurrence at 10 years of follow-up (Lebret et al. A large study examining the usefulness of preoperative prostatic urethral biopsy in predicting final urethral margin status demonstrated poor correlation (68%), but very high negative predictive value (100%) if the intraoperative frozen section was negative (Kassouf et al. We therefore recommend that in the presence of a positive urethral margin, orthotopic neobladder should not be performed and the patient should be made aware of this possibility during preoperative counseling. The role of preservation of the neurovascular bundles, unlike in radical prostatectomy, remains controversial in radical cystectomy. In a report of erectile dysfunction in sexually active men treated with radical cystectomy, Zippe et al. There is, however, concern because of the high rate of occult prostate cancers in radical cystectomy specimens. Despite this, in highly selected patients, excellent local control can be maintained. In a study of 100 patients without evidence of prostate cancer preoperatively and negative frozen section at surgery, only 5 (5%) developed local recurrence, although distant metastasis did develop in 31 patients (Vallancien et al. Among men who underwent nerve sparing, age, similar to the radical prostatectomy series, is a strong predictor of functional recovery with a drop from 62% potency for men aged 40 to 49 years to 20% for those 70 to 79 years (Schoenberg et al. In addition, in their report of 101 patients only 5 (5%) suffered a local recurrence; however, caution should be noted as one was a patient with pT2 disease. The risks and benefits of nerve sparing should be judged according to preoperative sexual function and disease burden. Additional efforts have been used to improve sexual functional outcomes, including subtotal resection of the prostate. Described techniques include leaving the prostate in its entirety or sparing the prostatic capsule and/or the seminal vesicles. These approaches have largely been studied in the context of orthotopic neobladder urinary diversion. Compared with men, women are seen initially with more advanced disease (Kluth et al. For this reason, anterior pelvic exenteration remains the gold standard of therapy. As discussed later, however, in patients with low-stage disease (cT1 and cT2) in whom orthotopic neobladder is considered, vaginal and urethral sparing is necessary. As described earlier, the initial steps for bowel mobilization, anterior bladder mobilization, and ureteral dissection are the same in men and in women with the exception of the gonadal vessels. In female patients the ovarian vessels should be identified during the bowel mobilization and ligated with a 2-0 silk suture distally, and a 2-0 silk suture ligature and a tie proximally, and then divided. After gaining entry to the vaginal canal, the surgeon easily can control the lateral and posterior vascular pedicles to the bladder. Care should be taken to ensure that sufficient vaginal mucosa is maintained above the urethral meatus to allow for closure of the vaginal defect in subsequent steps. Because of the vascular nature of the female pelvis and the sinusoidal nature of the vascular pedicles as they pass over the lateral vaginal wall, care is needed to ensure hemostasis. The posterior vaginal flap is then closed to the corresponding mucosae of the introitus in a clamshell fashion to maintain vaginal girth at the cost of some vaginal length. Bothersome drainage of peritoneal fluid will result if the vaginal closure is not watertight, and an interrupted closure is preferred. A vaginal packing is then placed with the dual purpose of distending the vagina and providing tamponade to any residual vaginal wall hemorrhage (particularly useful if vaginal sparing is performed; discussed later) and aids in the identification of unrecognized defects in the closure. In the absence of bladder neck involvement and the presence of low-stage disease (cT2), orthotopic neobladder can be considered. This necessitates urethral sparing with adequate length proximal to the striated sphincter and anterior vaginal wall sparing to provide support to the neobladder. As described previously, the lateral vascular pedicles are intimate with the lateral wall of the vagina, and to control these vessels properly they must be separated from the vagina before ligation. A vaginal packing during this step can aid in defining the plane of separation between the bladder and the anterior vaginal wall in the midline. After development the dissection plane between the posterior bladder and the anterior vagina is extended laterally, separating the lateral vascular pedicles from the lateral vaginal wall. To ensure that an adequate bladder margin is maintained, the vessels should not be divided until the midpoint of the lateral vaginal wall, in the anterior posterior plane, has been reached.
Generic avanafil 200mg otc
Anatomic failures were higher in the open group compared with the minimally invasive group (24 erectile dysfunction in diabetes ppt order avanafil pills in toronto. Compared with women who underwent minimally invasive sacrocolpopexy, women undergoing open sacrocolpopexy had a higher operative blood loss (188 vs. Chapter 124 Vaginal and Abdominal Reconstructive Surgery for Pelvic Organ Prolapse 2809 longer hospital stay (2. In a comparison of traditional and robotic sacrocolpopexy, robotic cases had fewer anatomic failures (5. The primary outcome was total operative time from incision to closure, but secondary outcomes included postoperative pain, functional activity, bowel and bladder symptoms, QoL, anatomic vaginal support, and cost from a health care perspective. Total operative time was significantly longer in the robotic group (227 +/-47 versus 162 +/-47 min; P < 0. Although pain scores were not significantly different on postoperative day 1, the robotic group reported more pain at rest and with normal activities at several points during the 6-week postoperative period. The authors thought the increase in pain was due to manipulation and fascial closure of the right paracolic gutter accessory port; they have since changed the port size to an 8-mm port. At 6- and 12-month follow-up, anatomic and QoL outcomes did not differ between the two groups (see Table 124. Perioperative complications, including visceral injury and mesh erosion, did not differ significantly between these groups (Antosh et al. Long-term success and complication data from well-designed studies for sacrocolpopexy are limited. Follow-up ranged from 1 to 28 months with median (interquartile range) follow-up time for each group: uterosacral colpopexy, 6. The interesting aspect of this study, however, was that the authors were able to extrapolate long-term outcomes. Mean operative time significantly decreased from 196 to 162 min when comparing the first 15 versus the last 30 cases. Mean operative time decreased from 222 min during the first 10 cases to 183 for the next 10 cases. The cost of minimally invasive prolapse surgery has been compared with open, vaginal, laparoscopic, and robotic procedures. Surgical costs can be calculated in several different ways; consequently, comparison of cost data can be difficult (Tarr and Paraiso, 2015). The cost analysis did not account for the initial robot purchase or yearly maintenance (Paraiso et al. Vaginal procedures do have high success rates with low operation rates and may be the procedure of choice for many older women. The 2016 Cochrane review concluded that there was no evidence of any difference for any of the primary outcomes between different types of apical vaginal native tissue repairs. In addition, they noted that regarding uterine preservation, sacrospinous hysteropexy was not inferior to vaginal hysterectomy with uterosacral suspension for the treatment of apical uterovaginal prolapse. Colpocleisis Colpocleisis is an obliterative procedure used in the treatment of post-hysterectomy vaginal vault prolapse or significant uterovaginal prolapse. The total colpocleisis is performed in patients who have undergone hysterectomy and refers to removal of the vaginal epithelium to approximately 2 to 3 cm from the urethral meatus with complete closure. This procedure involves creating lateral channels to allow potential uterine drainage. Advantages of the colpocleisis procedures are shorter operative time, ability to use regional anesthesia or local anesthesia with sedation, minimal complications, minimal recurrence, and decreased recuperative time (Cespedes et al. In those whose uterus is to be left in situ, preoperative evaluation should include a Papanicolaou smear, pelvic sonogram, and endometrial biopsy if indicated. Performance of hysterectomy at the time of colpocleisis eliminates the risk of developing cervical or endometrial cancer and eliminates the risk of developing pyometra, which is a serious complication of partial colpocleisis when the channels become obstructed (Shayya et al. However, most patients selected for colpocleisis are older with significant comorbidities that make a concomitant hysterectomy undesirable. The cervix is grasped with a tenaculum, and a rectangular segment of vaginal epithelium is marked anteriorly and posteriorly. The excision of the vaginal epithelium will extend 3 cm from the urethral meatus to 3 cm from the cervix (Cespedes et al. It is important to leave sufficient vaginal epithelium laterally to allow creation of the lateral channels to facilitate drainage. It is optional to place a 14-Fr Red Robinson catheter or a vessel loop along the vaginal sidewalls to assist in forming the channels. A high perineorrhaphy (levator myorrhaphy) is important to narrow the introitus and prevent recurrence. For both techniques, success depends on the amount of vaginal tissue sutured together. This creates a septum of support, which is enhanced by bringing the levator muscles together along with the perineorrhaphy. Several authors have reported that it is unnecessary to open the enterocele sac if one is present, because the repair will close the potential space in which the bowel may protrude (DeLancey and Morley, 1997; Karin Glavind and Kempf, 2005). If the enterocele sac cannot be reduced, then purse-string absorbable sutures incorporating the sac and the uterosacral remnants can be used to reduce the sac (Cespedes, 2001). DeLancey and Morley (1997) reported on 33 women who underwent colpocleisis over a 20-year period. She was treated with repeat colpocleisis and had a good response 1 year after the second colpocleisis. All but one patient expressly denied regret over the decision to have an operation that precludes the ability to have intercourse; however, one "accepted" her sexual inactivity. Many indicated relief of the discomfort associated with the prolapse and were positive about the outcome of the operation. Patients were followed by examination and phone survey, which appraised satisfaction and regret. In a multicenter, prospective study designed to study the effect of colpocleisis on pelvic support, symptoms, QoL, morbidity, and postoperative satisfaction, FitzGerald et al. Urinary frequency and urgency were the most bothersome symptoms reported in 33% of patients. Good anatomic results were noted in 107 patients with 101 reporting a relief of symptoms. There was no reported regret regarding the ability to engage in sexual intercourse. In a retrospective series of more than 300 women, the anatomic success rate was 98. Of 4776 colpocleisis procedures, 43% done on women older than 80 years, the mean length of stay was 2. This multicenter trial confirmed the results of earlier studies, which demonstrated improved body image, improved pelvic floor symptoms, low levels of regret, and high levels of satisfaction (Crisp et al. Urinary incontinence after colpocleisis may occur and has been attributed to several mechanisms. Successive rows of sutures are placed until the apical prolapse is completely reduced. A high perineorrhaphy is performed by removing a triangular segment of the vaginal epithelium. The fibromuscular tissues of the perineal body are approximated in the midline with absorbable sutures to narrow the introitus. Indigo carmine is administered, and a cystoscopy is carried out to confirm ureteral patency. The dissection is carried laterally and continued to the posterior lateral sulcus. Usually the enterocele reduces easily, and no further treatment is necessary (Cespedes et al. At this point, the colpocleisis is carried out starting at the leading edge of the prolapse. These progressive purse-string sutures are carried out until the prolapse is adequately reduced. Alternatively, the prolapse may be reduced as described for the partial colpocleisis by placing transverse rows of interrupted sutures. The remainder of the procedure is carried out as described for the partial colpocleisis.
Avanafil 200 mg without prescription
A 4-Fr ureteral catheter traverses the fistula tract in this endoscopic photograph causes of erectile dysfunction and premature ejaculation purchase 50mg avanafil with visa. Immature fistulae may appear as areas of localized bullous edema without distinct ostia. Cystourethroscopy can confirm the presence of the fistula but also may reveal the size of the tract, the presence of collateral fistulae, and the location of the ureteric orifices in relation to the fistula. In the setting of a prior history of pelvic malignancy, a biopsy of the fistula is often done to evaluate for the possibility of a recurrent malignancy. This type of requirement would usually mitigate against a completely transvaginal attempt at repair. Cross-sectional imaging may also be helpful in assessing for recurrent malignant disease in those with such a history. During voiding, care should be taken to exclude vaginal voiding or reflux of contrast from the introital region cephalad into the vagina, which would produce a falsely positive image. In some instances, a cystogram can also permit an assessment of bladder capacity (important in the setting of prior radiotherapy), cystocele, bladder neck competence, and vesicoureteral reflux, any of which may have an impact on operative repair. Ultrasound examination has also been used as diagnostic tool but remains user dependent (Volkmer et al. The fistulous connection is between the bladder anteriorly and the vagina posteriorly. The contrast agent is seen opacifying and outlining the vagina, superimposed on the bladder. Likewise, testing potassium levels will show higher levels compared with serum levels. However, in the setting of a prior history of radiation or radical pelvic surgery. Classification of Fistulae An ideal fistula classification system should correlate with the outcome and prognosis of the eventual fistula treatment. The Waaldijk and Goh classifications are the only ones that have been used to document sufficient numbers of obstetric fistula patients. The Waaldijk classification assesses mainly the extent of the urethral involvement and whether the injury to the urethra is circumferential. Similarly, the Goh classification looks at three of the four proven variables known to affect the outcome for obstetric fistula repair: the location of the fistula (assessing the extent of urethral involvement), the size of the fistula, and the amount of scarring (including whether or not it is circumferential) (Browning, 2006; Goh, 2004; Goh et al. There has been one comparative study showing that the Goh system is superior to the Waaldijk in terms of predicting closure (Capes et al. Bladder catheterization may temporize some of these effects until definitive repair is undertaken but often will not completely eradicate leakage, especially in those with a large fistula or those with significant detrusor overactivity. Furthermore, catheterization may provoke additional irritation and pelvic pain and is a constant reminder to the patient of an iatrogenic insult. Before epithelialization is complete, an abnormal communication between viscera will tend to close spontaneously, provided that the natural outflow is unobstructed. In this approach, a small cautery electrode is passed into the fistula tract endoscopically as far as possible. The electrode is slowly withdrawn from the tract with the electrode set on coagulation. Also, laser welding has been tried with success in a small series of women with fistula smaller than 3 mm (Dogra and Saini, 2011). This approach may also devitalize adjacent tissues, thereby compromising their future use as flaps. The fibrin sealant may be injected directly into the fistula tract after fulguration as described earlier. In general, these conservative measures are useful for small, oblique fistulae (usually less than 2 to 3 mm in diameter), in patients who are agreeable to this course of therapy. Few studies described catheter drainage in large fistulae, although it seemed that those of less than 1 cm diameter were most likely to heal spontaneously. The time between the insult and institution of drainage in cases of nonsurgical closure varied widely, although in most cases this was less than 3 weeks. Similarly, the duration of catheterization before the initiation of conservative treatment was deemed to have been unsuccessful and varied considerably, making true estimates of the effectiveness of this approach impossible; generally this varied between 10 days and 3 months. Reported success rates varied between 0 and 100% (but 5 series had a sample size of 1), although in several series it was difficult to determine how many women had attempted conservative management. In large series of obstetric fistulae in which a consistent approach to conservative management has been applied, spontaneous healing has been reported in up to 28% of cases (Waaldijk, 1994, 1997, 2004). In one series of urogenital fistulae of varying causes, spontaneous closure was seen in 19 of 238 or 8. Patients with small epithelialized fistulae may benefit from a minimally invasive treatment involving disruption of the epithelial layer of the fistula tract. Previous failed attempts at repair produce scarring and anatomic distortion and may compromise potential reconstructive flaps. Longer periods of time, up to 6 to 12 months, have been advocated for radiation-induced fistulae, which are often associated with severe obliterative endarteritis and reduced tissue vascularity. In this setting, reduced inflammation and edema permit easier identification of tissue planes (and therefore flap development), less bleeding, and less tension on the reapproximated suture lines. There is no consensus in the literature as to the definition of "early" in this context, with different studies either failing to specify at all, or giving a broad range of definition. The enthusiasm for delayed management has waned, and, in general, uncomplicated postgynecologic urinary fistulae may be repaired as soon as they are identified and confirmed, thereby minimizing patient discomfort and anguish (Blaivas et al. Early repair can be considered within 2 to 3 weeks after the occurrence of the fistula. If that time window has passed, a waiting period of 2 to 3 months is considered to be safe. Another potential reason to delay repair is to treat ongoing infection or inflammation at the level of the vaginal cuff. Periodic reexamination of the vaginal tissues can be performed every 1 to 2 weeks, and definitive repair scheduled when suitable pliability is noted (Carr and Webster, 1996). A vaginal approach can be attempted as soon as 2 to 3 weeks after the initial injury, if conservative therapy fails. The vaginal tissues are usually relatively undisturbed from the prior causative surgery, especially if the surgery was transabdominal. Each approach has merits depending on the particular circumstances of the fistula, and excellent outcomes can be expected with both approaches (Table 129. Next to factors such as size, location, and the need for adjunctive procedures often influence the choice of approach, also the experience of the operating surgeon must be taken into account. There are no randomized studies comparing abdominal and vaginal approaches, although there are recent retrospective studies comparing vagina and abdominal approaches. Fistula located high at the vaginal cuff may be difficult to expose transvaginally. Reimplantation may not be necessary even if fistula tract is located near ureteric orifice. Therefore a vaginal approach is to be recommended or referral to a skilled vaginal surgeon should be offered. In patients with a small-capacity or poorly compliant bladder (often secondary to radiation) requiring augmentation cystoplasty, an abdominal approach is indicated, because both procedures can be performed using the same incision. Currently the open abdominal approach is often being replaced by laparoscopic or robotic repairs (see later). There is some evidence that estrogen supplementation may improve spontaneous closure of fistulae (Goh et al. Perioperative antibiotics are administered, according to the existing American Urological Association or European Association of Urology guidelines on vaginal surgery. Treatment of existing infection based on preoperative urine culture is potentially beneficial in preventing bacteremia during surgery. Patients should be specifically queried regarding sexual function and dyspareunia occurring before the onset of the event that resulted in the fistula. Furthermore, adjuvant procedures that may alter vaginal appearance or function, such as the harvesting of a Martius fibrofatty labial flap or an episiotomy, should be carefully discussed with the patient in advance, especially regarding sexual function, although the impact on sexuality of the Martius flap is limited (Malde et al.
Purchase cheap avanafil on-line
The bowel should be fixed to the body wall near the site of the ureteral implantation so that the ureters do not angulate erectile dysfunction and prostate cancer proven 200mg avanafil. The complication rate for this technique is relatively low, although the follow-up is also relatively short. Initial reports suggested that it carried with it an 87% incidence of maintaining an antireflux valve with a 5% incidence of stricture and a 2% incidence of leak (Schwaiboldetal. The ureter is brought in the proximal sulcus transmurally and anchored to the serosa externally. The ureter is sutured by the technique of either Bricker or Wallace (as described earlier) to the end of the bowel, and the bowel is used to make a one-way valve. Unlike with individual ureterointestinal antirefluxing anastomosis, when these valves fail or stenose, both kidneys are affected. Three basic types of antireflux mechanisms commonly used with the bowel are ileocecal intussusception, ileoileal intussusception, and ileal nipple valve placed into colon. Serosal surfaces of the afferent limbs adjacent to the mesentery are sutured together with silk sutures. The antimesenteric borders of the apposed bowel segments are opened, thus making a trough. Thus the ileum should not be transected less than 13cm from the ileocecal junction. The ileal serosa is scarified either by multiple cross-incisions with a knife or with the electrocauteryunit. The intussuscepted ileum is secured to the cecal wall with 3-0 silk sutures placed circumferentially 2 mm apart. The valve has a moderate tendency to fail because the intussusception has a significant chance of reduction. In one series, the antireflux mechanism remained intact in 55% of the patients during the long term(HensleandBurbige,1985). The cecum is opened along a taenia, and the ileum is intussuscepted over the catheter under direct vision. Where the intussusception lies adjacent to the cecal wall, mucosa of the intussuscepted ileum and the cecal mucosa adjacent to it are incised down to muscle. Long-termfollow-up in eight patients reveals maintenance of the antireflux valve in seven withthemodifiedtechnique(Friedmanetal. Intheirseries,82%ofpatients maintained valve competence; however, there was a 20% incidence of stone formation (Wiesner et al. The mucosa of the intussuscepted segment is incised, and the mucosa of the cecum adjacent to it is also incised. The serosa of the ileum is secured to the serosa of the cecum with interrupted 3-0 silk sutures placed circumferentially (not depicted). The gastrointestinal stapler without the knife or the linear stapler, from which the distal five to eight staples have been removed, is used to secure the intussusception in place; three rows with the gastrointestinal stapler or four rows with the linear stapler are placed in quadrants. It is for this reason that the distal staples are removed from the staple cartridge before it is placed in the stapler and before the intussusception is stapled. With the cautery unit, the mucosa of the intussusception is incised along its length. The muscularis of both is exposed and sewn together with interrupted 3-0 chromic suture. The distal serosa is then sutured proximally to the serosa of the intussuscepted segment circumferentially with 3-0 nonabsorbable sutures. This is meant to secure the intussusception and to prevent its reduction with failure of the antireflux mechanism. Because the intussuscepted nipple valve as an antireflux mechanism has resulted in a 10% complication rate (5% stone formation on the exposed staples, 4% stenosis, and 1% prolapse) (Stein et al. One such modification has been described by the University of Southern California group. An 8- to 10-cm isolated segment of ileum is tapered distally and laid between two segments of small bowel in which their serosal walls adjacent to the mesentery are sutured together. The apposed bowel is opened along its antimesenteric border; lateral flaps are constructed adjacent to the segment and closed over its anterior aspect, thus making a serosal trough in which 4 cm of the segment of tapered ileum is positioned (Stein and Skinner, 2003). The concept is that as pressure in the pouch increases, the walls of the tapered nipple valve are compressed, thus preventing reflux. Thedistal6cmofserosais scarified by multiple cross-striations and then turned back on itself to form a nipple. The long-term success rate for this type of valve is unknown but is comparable to tunneled anastomoses (Osman et al. The ileum distally is opened within 2 to 3 cm of the rent in the mesentery; a 5-cm length of ileum is intussuscepted and secured by placement of staples in quadrants. The ileal mucosa is incised adjacent to an incision in the intussuscepted segment, and the two muscle coats are sutured together with interrupted 3-0 chromic suture. The serosa of the intussuscepted segment is sutured circumferentially to the base of the ileum, into which the proximal segment is intussuscepted with interrupted silk suture. Complications of Ureterointestinal Anastomoses the complications that occur with ureterointestinal anastomoses include leakage, stricture, reflux in those anastomoses that were performed to prevent reflux, and pyelonephritis. In a review of the various types of procedures, it appears that of the colonic antirefluxing procedures, the Pagano technique offers the lowest incidence of stricture with an acceptable incidence of reflux. With respect to small bowel antireflux procedures, the Le Duc procedure and the ureterointestinal serosal apposition procedure seem to offer the lowest incidence of stricture with the highest success rates in preventing reflux. With respect to stricture formation and leakage, it appears the Wallace technique has the best results (Kouba et al. The distal end of ileum is opened along its antimesenteric border to within 2 to 3 cm of the cleared mesentery to provide adequate exposure and direct visualization of the intussuscepted segment. A Babcock clamp is placed into the lumen of the bowel, and a portion of bowel wall is grasped by invaginating it into the clamp with a finger. The ileal segment is intussuscepted by pulling on the Babcock clamp with gentle constant traction. If there is resistance, the mesentery is usually too bulky, and it must be defatted carefully before another attempt to intussuscept Urinary Fistula Urinary fistulas typically occur within the first 7 to 10 days postoperatively with an incidence of 3% to 9% (see Table 139. Self-expanding metal alloy stents (Wallstents, Schneider, Zurich, Switzerland) showed more promising results in a small trial of nonmalignant ureterointestinal strictures withsuccessfultreatmentof10/10stricturesatamedianfollowup of 22 months; one patient developed a stone on the stent (Palascak et al. Pyelonephritis Acute pyelonephritis occurs both in the early postoperative period and during the long term. These complications cause considerable morbidity and, in fact, are associated with significant mortality. In one series of intestinal segments in the urinary tract, 8 of 178 patients died of sepsis (Schmidt etal. That these complications may result in delayed mortality is indicated by the fact that 2 of 115 children and 3 of 127 adults died of septic complications 5 to 14 years after intestinal diversion (Pitts and Muecke, 1979). When sepsis is associated with decreasing renal function and uremia, the morbidity and mortality are markedly increased. Although the mortality rate may be somewhat lower in the current age of antibiotics, the rise of multidrug-resistant organisms poses a significant threat in both the short and long term in patients undergoing urinary diversion. The table is derived from composite reports in the literature in which specific anastomoses were described and from which the data could be accurately analyzed. Because of these two requirements, it is not possible to comment, for example, on the incidences of reflux or leakage among various anastomotic types inclusively. These complications can be minimized by adherence to the principles of ureterointestinal surgery discussed earlier. Approximately 8 cm of mesentery are cleared from the distal end of the ileum, and the serosa is scarified and then turned back on itself to form a nipple of approximately 4 cm in length. The incidence of urinary intestinal leak is markedly reduced by the use of soft Silastic stents (Mattei etal. A urinary intestinal leak may cause periureteral fibrosis and scarring with subsequent stricture formation. Stricture In general, the antirefluxing techniques have a higher incidence of stricture. Patients are at risk for ureterointestinal strictures for the life of the anastomosis and must be observed on a scheduled periodic basis.
Discount avanafil online amex
The arcades anastomose one with another and give off straight vessels erectile dysfunction specialists order avanafil 200 mg online, which enter the bowel and form an anastomotic network within the bowel wall. It has been shown experimentally that up to 15 cm of small bowel can survive laterally to a straight vessel. Thus, theoretically, the mesentery could be cleared from the small bowel for a length of 15 cm without necrosis of the end. In general, however, it is unwise to assume that more than 8 cm of small bowel will survive away from a straight vessel. When segments of jejunum or ileum are isolated, the mesentery should be transected in such a way that the isolated intestinal segment receives its blood supply from an arcade supplied by a palpable artery of substance that courses through the base of the mesenteric pedicle. Two portions of the small bowel may lie within the confines of the pelvis and, as such, may be exposed to pelvic irradiation and pelvic disease: the last 2 inches of the terminal ileum, which is often fixed in the pelvis by ligamentous attachments, and the 5 feet of small bowel beginning approximately 6 feet from the ligament of Treitz, the mesentery of which is the longest of the entire small bowel. In a postirradiated patient, one should try to avoid use of these two segments of the small intestine in any reconstructive procedure. The stomach, jejunum, and rectum are also used in reconstructive procedures, although less commonly. Successfully performing surgical mobilization of these structures and reconstructing them for their new function requires a thorough knowledge of the surgical anatomy, vascular supply, and metabolic function of each portion of the intestinal tract. Three branches of the celiac axis give rise to the majority of the arterial supply of the stomach. The left gastric (coronary) artery arises directly from the celiac axis and supplies the lesser curvature. The hepatic artery, after arising from the celiac axis, gives off the right gastric artery, which also supplies the lesser curve of the stomach, and the gastroduodenal artery, which supplies the antrum and duodenum before giving off the right gastroepiploic artery. The splenic artery originates from the celiac axis and gives off the vasa brevia (short gastrics), which supply the fundus and cardia, and the left gastroepiploic artery. The right gastroepiploic artery meets with the left gastroepiploic artery; thus both supply collateral flow to the greater curve of the stomach. By use of the gastroepiploic vessels, a pedicle of stomach may be mobilized as far as the pelvis. The blood supply for these segments is based on either the left or right gastroepiploic artery, depending on the portion of stomach used. On occasion, the left gastroepiploic artery is atretic at some point in its course and does not provide an adequate blood supply. When a wedge of fundus is used, it should not include a significant portion of the antrum and should never extend to the pylorus or all the way to the lesser curve of the stomach. When the blood supply is based on the left gastroepiploic artery, the short gastric vessels that course from the gastroepiploic artery to the stomach are ligated along the greater curvature proximal to the pedicle to the origin of the gastroepiploic artery. The omentum is left attached to the gastroepiploic vessels and helps secure and support them. It may be necessary for proper pedicle mobility to detach the omentum from the colon along the avascular plane located at the point of its attachment to the transverse colon. If an antrectomy is performed, Colon the large bowel is divided into the cecum, ascending colon, transverse colon, left colon, sigmoid colon, and rectum. Portions of the large bowel are fixed or retroperitoneal, and other segments lie free within the peritoneal cavity. The cecum, on rare occasion, may lie free within the abdominal cavity and therefore may have great mobility. Two accessory peritoneal bands bind the cecum and distal ileum to the retroperitoneum and lateral abdominal wall. One band arises from the distal ileum, attaches to the cecum, and is fixed to the retroperitoneum. A second band arises from the cecum and fixes the cecum 3160 Chapter 139 Use of Intestinal Segments in Urinary Diversion 3161 Left gastric a. The remainder of the ascending colon is fixed to the right posterior abdominal wall at the level of the hepatic flexure, at which point the hepatocolic ligament secures this portion of the colon to the liver. The transverse colon lies free within the abdominal cavity and is fixed in the left upper quadrant at the splenic flexure by the phrenocolic ligament. The descending colon is fixed to the lateral abdominal wall; however, the sigmoid colon may or may not lie free within the abdominal cavity. The major arteries supplying the colon and rectum include the ileocolic, right colic, middle colic, left colic, sigmoid, superior hemorrhoidal, middle hemorrhoidal, and inferior hemorrhoidal arteries. These arteries anastomose with one another to form the arc of Drummond and allow considerable leeway in mobilizing the colon. The middle colic artery arises from the first portion of the superior mesenteric artery and typically ascends the transverse mesocolon to the right of midline. The right colic artery usually arises just below the middle colic artery from the superior mesenteric artery and courses to the right colon. In some cases, the right colic artery may arise from the ileocolic artery or directly from the middle colic artery. If the right colic artery arises from the ileocolic artery, mobilization of a distal ascending colon segment is more likely to be brought easily into the deep pelvis. On occasion-particularly if the right colic artery originates from the middle colic artery-it is necessary to divide the right colic artery at its origin to mobilize the distal portion of the ascending colon to the pelvis. The ileocolic artery is the terminal portion of the superior mesenteric artery and supplies the last 6 inches of ileum and ascending colon. The left colic artery arises from the inferior mesenteric artery, and then the inferior mesenteric artery gives off four to six sigmoid branches, the last of which becomes the superior hemorrhoidal artery. This anastomoses with the middle hemorrhoidal artery, a branch of the internal iliac artery, which, in turn, anastomoses with the inferior hemorrhoidal artery, the terminal branch of the internal pudendal artery. The middle sacral artery, which originates directly from the aorta, may supply the posterior aspect of the rectum. Watershed areas are regions of the colon that receive dual blood supply from the most distal branches of two larger arteries. Because of the small diameter of these distal branches, watershed areas are particularly vulnerable to ischemia in the setting of hypotension or thromboembolic event. Although anastomoses in these locations usually heal well provided the principles of proper technique are followed, if possible it is wise to select an area for the anastomosis to one side of these points, where the feeding arteries have a larger diameter. The ascending colon is mobilized first by transecting the cecal and distal ileal fibrous attachments to the lateral abdominal wall and retroperitoneum as described earlier and then by detaching it from the lateral abdominal wall along the avascular line of Toldt. The transverse colon is mobilized by dividing the gastrocolic omentum (along the avascular plane of its attachment to the colon), the hepatocolic ligament (which may have some small vessels coursing through it), and the phrenocolic ligament. The descending colon is mobilized, much like the right colon, by incision of the avascular line of Toldt lateral to the colon. Further mobility is gained by isolating a pedicle of the intestinal segment on the basis of one of the major arterial vessels described earlier. The advantages of the stomach over other intestinal segments for urinary intestinal diversion are that it is less permeable to urinary solutes, it has a net excretion of chloride and protons rather than a net absorption of them, and it produces less mucus. When it is used in urinary reconstruction, electrolyte imbalance rarely ensues in patients with normal renal function, although hypochloremic metabolic alkalosis has been described. The incidence of bacteriuria has been reported to be as lowas25%,muchlessthanthe60%to80%incidencereportedfor ileal and colon segments. However, more recent data suggest that there is no difference in bacteriuria among any of the segments. The urine, which usually has a pH of 6 to 7, does not typically result in an increased incidence of peristomal skin problems. Authors have also noted that in bladder augmentation patients, there is little difference in urinary pH between gastric and ileal augmentations. Serum gastrin levels are usually normal or minimally elevated, depending on what portion of the stomach is used and how much (Adams etal. Experimentally, antral exclusion may result in elevated circulating gastrin levels, leading to intestinal ulcerative problems in the postoperative period (Tiffanyetal. Rarely, severe ulcerative complications have occurred in cases in which stomach has been used for urinary reconstruction (Reinberg et al. Long-term histamine (H2 receptor) antagonists or proton-pump inhibitors should be considered for these patients. Early complications of the use of portions of the stomach for reconstruction include gastric retention caused by atony of the stomach or edema of the anastomosis; hemorrhage, most commonly originating from the anastomotic site; hiccups secondary to gastric distention; pancreatitis as a consequence of intraoperative injury; and duodenal leakage. Delayed complications include dumping syndrome, steatorrhea, small stomach syndrome, increased intestinal transit time, bilious vomiting, afferent loop syndrome, hypoproteinemia, and megaloblastic or iron deficiency anemia. Gastroduodenal and gastroureteral leaks have also been reported, occasionally resulting inafataloutcome(Leong,1978).