Purchase 50 mg naltrexone free shipping
There is a revival of interest in using maggots of nonmyiasis species to remove necrotic tissue from wounds medications removed by dialysis 50mg naltrexone mastercard, their secretions also preventing bacterial contamination. Cutaneous larval migrans is characterized by itchy inflammatory hookworm larvae trails Human hookworms (the nematodes Ancylostoma and Necator) invade the body through the skin, the infective larvae burrowing in to the dermis and then migrating via the blood to eventually reach the intestine. Invasion may cause dermatitis (known as ground itch) and this becomes more severe upon repeated infection. Humans, however, can also be invaded by the larvae of the cat and dog species of Ancylostoma. Infection is acquired when exposed skin comes in to contact with soil that has been contaminated by animals carrying the adult worms in their intestines. Eggs in the faeces hatch to produce the infective larvae, which remain viable for prolonged periods. As the human host is foreign for these species, the larvae fail to escape from the dermis after invasion, and may live for some time, migrating parallel to the skin and leaving intensely itchy sinuous inflammatory trails (creeping eruption), which are easily visible at the surface. Certain ticks, lice and mites live on blood or tissue fluids from humans Some feed non-selectively on humans, the normal hosts being animals; other species are human specific. Prolonged feeding, as practiced by ticks, may leave painful lesions in the skin, which can become secondarily infected. Species such as lice and scabies mites, which spend the greater part or the whole of their lives on the human body, can cause severe skin conditions when populations accumulate. Good personal hygiene prevents infestation; use of insecticidal creams, lotions, shampoos and powders containing malathion or carbaryl helps to clear the insects directly. The scabies mite has a more intimate contact with the human host than lice, living its whole life in burrows within the skin. The female lays eggs in to these burrows, and so the area of infection can spread to cover large areas of the body from the original site, which is usually on the hands or wrists. Infection causes a characteristic rash with itching, and secondary infections may follow scratching. Very heavy infections may develop in immunocompromised individuals or in people who are unable to care adequately for themselves. Under these conditions, there is extensive thickening and crusting of the skin (Norwegian scabies). Treatment with permethrin or malathion is recommended; benzyl benzoate can also be used on unbroken skin but is less effective. Oral ivermectin may be required in addition to topical therapy for Norwegian scabies. The skin rash has a characteristic distribution in many infectious diseases, but with the exception of zoster, the reason for this is unknown. The distribution as well as the nature of the lesion can be important in diagnosis. This is because human skin is naked and is a turbulent, highly reactive tissue in which immune and inflammatory events are clearly visible. Rashes cause discomfort and may be painful but they may be very helpful for the clinician who needs to make a diagnosis. The veterinarian is less privileged because the skin of most other mammals is largely covered with fur, and skin lesions generally involve hairless areas such as udders, scrotums, ears, prepuces, teats, noses or paws, which have the human properties of thickness, sensitivity and vascular reactivity. They are highly adapted to human skin and mucosa and are ancient associates of our species; therefore, for most of the time they cause little or no disease. Papillomaviruses are generally transmitted by direct contact, but they are stable and can also be spread indirectly. For instance, plantar warts can be acquired from contaminated floors or from the non-slip surfaces at the edges of swimming pools, and in a given individual warts can be spread from one site to another by shaving. Papillomavirus infections are associated with cancer of the cervix, vulva, penis, rectum, head, and neck Human papillomavirus infections are associated with nearly 4% of all cancers. The association between genital warts and cancer of the cervix, vulva, penis and rectum is referred to in Chapter 17. Warts may undergo malignant change (squamous cell carcinomas) in nearly 30% of these patients, usually in sun-exposed sites. Papillomavirus infects cells in the basal layers of skin or mucosa and are tissue tropic After entering the body via surface abrasions, the virus infects cells in the basal layers of the skin or mucosa. Virus replication is slow and is critically dependent on the differentiation of host cells. There is marked proliferation of prickle cells, and vacuolated cells are present in the more superficial layers. Immune responses eventually bring virus replication under control and, several months after infection, the wart regresses. Diagnosis of papillomavirus infection is clinical and there are many treatments Wart viruses cannot be cultivated in the laboratory, and serologic tests are mainly of epidemiological, rather than diagnostic, use. Many treatments have been used for warts, some of them doubtless seeming effective because skin warts eventually disappear without treatment. Treatments of skin warts include the application of karyolytic agents such as salicylic acid and destruction of wart tissue by cryotherapy, freezing with dry ice (solid carbon dioxide) or with liquid nitrogen. Genital intraepithelial lesions, especially cervical, can lead to malignant disease, and treatment to eliminate the infection may involve laser therapy, loop excision, and surgery. Immunomodulating and antiviral agents such as imiquimod and topical cidofovir, respectively, have been used in certain clinical settings. It only infects humans and is spread by contact, or in the case of genital lesions, by sexual intercourse. Orf is a papulovesicular lesion caused by a poxvirus Orf (contagious pustular dermatitis) is an uncommon infection of the epidermis and is acquired by direct contact with infected sheep or goats. They cause a wide variety of clinical syndromes, the basic lesion being an intraepithelial vesicle, from which the virus is shed. Infection is usually transmitted from the saliva or cold sores of other individuals and frequently by kissing. During the primary infection, virus particles enter sensory nerve endings in the lesion and are transported to the dorsal root (trigeminal) ganglion, where they initiate latent infection in sensory neurones (see Ch. The latent virus remains in the sensory ganglion for life, and under certain circumstances can reactivate and spread down sensory nerves to cause cold sores at the site of the original infection. A sensory prodrome in the affected area which may include feeling pins and needles, pain, burning, and itching precedes the appearance of the lesion and is due to virus activity in sensory neurones. Less commonly, when the ophthalmic branch of the trigeminal ganglion is involved, the lesion is a dendritic ulcer of the cornea. Large amounts of virus are shed in the cold sore, which scabs over and heals over the course of about 1 week. In both herpes simplex virus and varicella-zoster virus infections the virus in mucocutaneous nerve endings travels up the axon to reach the sensory neurones, where it becomes latent. Recurrences are due to reactivation of the virus within the neurone to become infectious followed by passage of virus down the axon to mucocutaneous site(s) and local spread and replication to form clinical lesion(s). Recurrent herpetic eruptions have been successfully treated with low doses of aciclovir given twice daily for 6 to 12 months, at which time treatment can be stopped and the frequency of recurrent infection reassessed. Alternative antivirals such as ganciclovir, foscarnet or cidofovir may be used when antiviral resistance is being considered. Infection is by inhalation of droplets from respiratory secretions and saliva, or by direct contact from skin lesions. Immunity develops and prevents reinfection (a second attack of varicella), but the virus persists in the body, and later in life, after reactivation, causes zoster (shingles). Nearly all humans in resource-rich countries are infected during childhood, but there are many areas of the world where the incidence of chickenpox in children is low. In the skin, it takes a day or two longer, and it is at this stage, when the characteristic varicella vesicles appear in a centripetal distribution, that a clinical diagnosis can be made.
Cheap 50 mg naltrexone overnight delivery
Biologic meshes are extremely expensive comparatively but do deter visceral adhesions to the abdominal wall symptoms stiff neck cheap naltrexone 50 mg overnight delivery. Soma small studies with bioprosthetics have found a relatively low number of complications and no recurrences. Other data suggests that they are of no comparative benefit although no prospective randomized trials have been performed. Nonetheless, biologic mash minimizes the risk of complications such as adhesions and enterocutanaous fistulae which can have devastating consequences. Autologous reinforcement of the abdominal wall has also been employed with the use of autologous tensor fascia lata grafts. This is of added morbidity and has not been shown to be of additional benefit with recurrence rates of up to 29%. Bridging of the abdominal wall defect may be necessary when release of the rectus abdominis does not allow for muscular opposition. As stated previously, this can be accomplished with an open book repair or with mesh. When bridging with mash is decided upon, the repair should begin in the standard component separation technique. The general consensus is that the biologic mesh or "neodermis" is placed in the retrorectus plane with 3 to 5 em of overlap with the muscle. Care should be employed as to not strangulate the epigastric vessels rendering the muscle ischemic. Unfortunately, the intercostal nerves may be incorporated in this closure technique and impair the innervations to the muscle. Thera exists no consensus on the utility of mesh used in conjunction with the standard repair. Intuitively, posterior or deep placement wound allow for buttressing of the mesh against the anterior surface of the coelomic cavity which would hold this intimately against the abdominal wall facilitating its incorporation and neovascularization. Other sources demonstrate significant decrease in recurrence when placed as an overlay with small studies boasting zero recurrences. Gastric decompression is achieved with a nasal gastric tuba to minimize abdominal distention during the immediate postoperative period as ileus will often result. Of equal importance, this helps to minimize wrenching and emesis, which can damage the reconstruction. Chapter 29 Components Separation 325 A urinary catheter is usually placed intraoperatively and continued postoperatively. This allows for accurate assessment of urine output and volume resuscitation status. Secondly, this can provide important data in bladder pressures and thus intraabdominal pressures to assess for potential abdominal compartment syndrome. Drains have not been demonstrated to prevent seroma formation, although they should be considered in patients especially with large flaps and those with exposed biologic mesh as this is known accumulate periprosthetic fluid. External abdominal support is achieved by an abdominal binder to provide abdominal wall support while the repair is approaching a plateau in the healing process at approximately 6 weeks. This can be left longer in patients who are of higher suspected risk of recurrence such as obese individuals or smokers. Again, there is no prospective evidence demonstrating decreased rate of seroma formation with binder usage. From an intuitive stance, a binder should assist in minimization of dead space and shifting or shearing of the tissues during the healing process. Complications associated with component separation can be classified in to major and minor subdivisions and commonly include recurrence, infection, seroma, necrosis, and wound dehiscence fistulae formation. De Vries Reilingh has compiled the results of over 460 patients who underwent component separation at several institutions and including various modifications of the originally described technique. Although wound complications are high, this can be accounted for on several levels. This compromises the vascularity to the skin itself which can result in skin edge necrosis and healing problems along the midline. The potential space under the skin or fasciocutaneous flaps is expansive and allows a large area for both hematoma and seroma to form, especially in patients with onlay biologic mesh. This is not necessarily the incidence in more conventional forms of herniorrhaphy with open techniques and laparoscopic approaches. There is likely a bias in comparing the complication rates of herniorrhaphy versus the component separation techniques as these patients have large hernias that have often failed other forms of repair. The patients undergoing component separations are sometimes not amendable to any other forms of repair as there is loss of the skin overlying the visceral contents in the case of trauma laparotomies and grafting of the enteric contents. An important point of consideration is that in the elective setting, the mortality of this reconstructive technique is extremely low. Hernia recurrence is a major consideration of this technique and has been scrutinized over the past two decades (Table 29. Ewart evaluated the results of abdominal wall reconstruction in 60 consecutive patients utilizing standard component separation technique, mesh repair, tensor fascia lata flaps, or latissimus dorsi flaps. Only one (9%) of the patients in the component separation group had a recurrence and those with primary repair or mesh repair had recurrences of 14% and 27%, respectively. He found that the most common factors influencing recurrence were patient factors such as poor tissue integrity and increased intraabdominal pressure and technical errors. Increased risk of recurrence was found in patients who had colostomy or fistula takedown at the time of hamiorrhaphy. Obesity is associated with these complications, but was not found to be statistically significant. This repair technique as opposed to mesh repair alone provides relatively uniform dynamic support to the abdomen and thus minimizes areas of intrinsic weakness of the abdominal wall and reduces recurrence. The release of the rectus abdominis via the conventional component separation technique and various modifications allows for a tension-free closure of the abdomen and has been found to endure over time. This has opened a new chapter in how surgeons think about reconstructing the abdominal wall and is becoming the standard of care for reconstructing the massive ventral harnia. Many variations of this original technique have resulted to allow for closure of larger defects. The beauty of component separation is that this provides autologous dynamic support to the abdominal wall and thus optimizes its original integrity and minimizes the risk and complications and necessity of mesh repair. This has been proven to be a safe and eHective technique for abdominal wall reconstruction. Early results of midline hernia repair using a minimally invasive component separation technique. The vascular territories of the superior epigastric and deep inferior epigutric systems. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of indsiOilel hemia. Incisionel hsmia in:re-opened abdominal incisions: an overlooked risk factor, Br J Surg. Utilization of human cadaveric acellular dermis for abdominel hsmia:reconstruction. Successful closu:rs of abdominel well hemias using the components separation techniques. The vascular anatomy of the rectus abdominfs musculocutaneous flaps based on the deep superior epigastric system. Unacceptable results of the Mayo p:rocedure for:repair of abdominel inci8ional hernias. Recalcitrant abdominal wall Herniu: long term superiority of autologous tissue repair. The vucular anatomy of the lower anterior abdominal wall: a microdissection study on the deep inferior epigastric vessels and the perforator branches. Multilayer reconstruction of abdominal wall defects with acellular dermal autograft (AiloDerm) and component separation. Rarely, however, there is a n99d for more complex reconstructive options which are described in this chapter.
50mg naltrexone overnight delivery
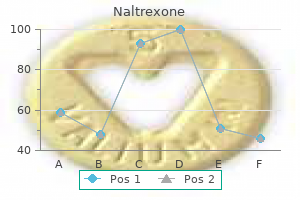
Specifically medicine 4h2 discount generic naltrexone canada, symptoms are aggravated by sudden turns or cutting movements, propulsive skating movements in hockey, and kicking in soccer or football. Importantly, the pain limits sudden accelerating movements which can be the difference in success and failure for high level athletic performance. Other symptoms that may be associated include pain with coughing or sneezing and adductor symptoms. The onset is often insidious with no clear precipitating event and fails to resolve with conservative management. Other findings may include a dilated external ring, a palpable gap over the inguinal canal, and pain with resisted trunk rotation. Plain pelvis x-rays may be useful for screening hip and bony pelvis abnormalities. The floor is examined supine and durign a sit-up for areas of weakness and tendemess. The athlete is asked to rotate the shoulder toward the opposite hip against resistance. Shown is edema in the parasymphyseal region of ttle pubis and secondary cleft sign (sm~ws) indicating aponeurotic lesion associated with this condi1ion. In addition, the examination findings should corroborate the location of maximum pain and tenderness as consistent with a sports hernia condition, and other diagnoses should be excluded by examination and imaging. One study by Ekstrand compared surgery versus various non-operative conservative treatment regimens in 66 soccer players with chronic groin pain. All athletes had groin pain for more than 3 months and only the surgical group showed substantial and statistically significant improvement. Pathophysiologic Mechanisms the surgical approach to the treatment of sports hernia type pubalgia should be based on an understanding of the pathophysiology and mechanisms involved in this condition. An imbalance in muscle strength across the pelvis may lead to increased stress across the pubis and chronic pubalgia type pain. There may be a tear or weakening of the rectus muscle at its insertion site on the pubis. Attenuated external oblique with translucency of the central portion of the aponeurosis distally lsrrows). The external oblique has already been opened 1hrough 1he external ring 10 expose 1he spermatic cord. These latter mechanisms have led some groups to recommend routine or liberal resection of one or more of these nerves during surgical repair. It should be noted that these mechanisms are not mutually exclusive of each other and may co-exist in a given athlete. Laparoscopic mesh repair the primary pelvic floor repair that has been employed by Meyers is a sutured repair that is focused on attachment and realignment of the lower rectus with the pubis. Meyers often accompanies this repair with a partial adductor release in which multiple tiny incisions are made in to the tendinous insertion site near the pubis to decompress the adductor compartment. The Muschawek minimal repair technique involves primary repair of the posterior inguinal fioor. Two overlapping rows of suture are used to imbricate tha defect and in order to stabilize the posterior wall and reduce tension on the rectus abdominis. In addition, a genital neurectomy is performed if there is tension on the nerve or bulging that compresses the genital nerve. This is analogous to a Lichtenstein type repair and typically utilizes lightweight polypropylene mesh. In addition to the repair of the posterior fioor, anchoring sutures are placed in the lateral rectus to further stabilize that side of the abdominal attachment. An ilioinguinal neurectomy is performed if the nerve is entrapped in a slit in the external oblique away from the external ring or if it would potentially be tethered by the mesh in order to eliminate it as a source of postoperative pain. In addition, ilioinguinal and/or iliohypogastric neurectomies are frequently performed in their athletes. In one study of 55 athletes with chronic groin pain, occult hernias were identified laparoscopically in 20 (36%). This repair is the same technically as standard laparoscopic transabdominal preperitoneal or total extraperitoneal inguinal hernia repair with broad mesh coverage of the entire floor, particularly the area of the medial O. Our group has utilized a stepwise program that is focused on both core abdominal strengthening and stabilization as well as attention to lower body strength, O. In particular, strengthening and stretching exercises involving the adductor muscle group are an important component to this. In general, the first 7 to 10 days after repair the athlete is limited to normal activities of daily living and walking. From that point on, activity is increased progressively and sequentially beginning with light jogging, stationary biking, and progression to core and lower body exercises. Finally, sport-specific activity is initiated until the athlete is ready for physical contact and return to play. Muschawek has advocated an accelerated path for return to sport in athletes undergoing! The mesh covers the entire inguinal floor including posterior rectus sheath and its insertion on the pubis. Such an approach has allowed return to play as early as 3 to 4 weeks after the procedure. In the majority of cases, repairs are typically done in the off-season for sport and so a more conservative timetable for return to play is generally utilized. In our experience, return to play is feasible within 5 to 8 weeks after repair in most individuals but may take longer in selected athletes who have significant adductor or other associated injuries. Operations were performed in 5,218 athletes out of a total of 8,490 individuals who were evaluated (61. Twentysix different variations of repairs and 121 different combinations of procedures were carried out. Most repairs involved a primary pelvic floor repair as described above in conjunction with different types of release procedures. Complications were reported in approximately 1% of athletes and included hematomas that required reoperation in 0. Muschawek reported results in a prospective evaluation of 129 athletes treated from 2008 to 2009. Ninety-six percent of athletes had resumed training by 4 weeks after repair and a full return to pre-injury sports activity had occurred in 75. In our experience over 90% of repairs have been done under local anesthesia as an outpatient procedure. Successful return to athletic competition was seen in 91% of athletes at a mean follow-up interval of 13. The most common reason for failure in our experience had been ongoing adductor symptoms that resulted in subsequent adductor release procedures in 5 individuals. A3 a result, we have begun to carry out a partial adductor release similar to that reported by Meyers in highly selected athletes with predominately adductor pathology. Whether an open or laparoscopic approach should be utilized must be dictated by the experience of the surgeon. Since the laparoscopic repair will be transperitoneal, it is essential to know if there is likely to be extensive adhesions or adhesions at the umbilical level which might jeopardize the safety of the repair. This means that the surgeon must know what is going to be done if confronted by the unexpected. There must be a plan that allows the procedure to be converted to an open anterior repair if needed. Finally, the surgeon must have a plan in place for closing the peritoneum or covering the mesh repair if re-peritonealization is impossible. The monitor is positioned at the foot of the table and is angled so that the screen is facing the surgeon. The assistant surgeon or scrub nurse, if acting as the assistant, stands opposite the surgeon. The scrub table is placed across the legs so that both the surgeon and nurse can reach the instruments. Patient Prep Although it has been shown that the routine use of a foley catheter increases the risk of retention, if the surgeon thinks that the procedure will be prolonged a catheter can be placed. The entire abdomen should be prepped so that the position of the trocars can be varied if necessary. The groin on the side of the hernia is shaved and prepped in case the procedure must be converted to open.
Buy 50mg naltrexone with mastercard
The drains are removed after 10 to 14 days or when the output decreases to <30 cc/day medicine youkai watch discount 50mg naltrexone overnight delivery. The use of elastic abdominal binders might help in decreasing the incidence of seromas and improving postoperative discomfort. Complications such as seromas, nap necrosis, hematomas, and wound infections are reported in up to 67% of cases. It is well established that local wound complications contribute to hernia recurrence. Due to usually extensive bowel manipulation, postoperative ileus is reported in about 30% of cases. Cardiac and pulmonary complications can manifest in an isolated form or as part of postoperative abdominal compartment syndrome. The best timing for hernia repair in this patient population remains controversial. Although laparoscopic hernia repair has been safely performed in morbidly obese patients, longer operative times and postoperative stay in addition to higher recurrence and overall complication mtes have to be expected. In addition-if the procedure has to be converted to open-mtes of parioperative complications and recurrence increase sign:ifi. This is due largely to the multiple risk factors common in morbidly obese patients, including medical co-morbidities, increased intraabdominal pressure, larger hernia defects, increase l:ikel:ihood of previous failed repairs, and intraoperative d:illiculties that result in longer operative times. Since medical weight loss has been shown to be largely ineffective, a surgical weight loss procedure should be considered. In the setting of clean-contaminated barlatrlc procedures, associated high recurrence rates can be explained by the limited choice of repair (primary or biologic mash). It is our approach whenever feasible to offer weight loss surgery prior to hernia repair in the absence of symptoms warranting more urgent repair. In cases where the hernia must be reduced in order to complate the barlatric procedure, a form of repair has to be implemented to avoid incarceration during the subsequent weight loss period. The choice of repair is guided by the size of the defect Small (2 em or less) umbilical defects can be repaired primarily, whereas larger defects require the use of biologic mesh, preferably underlay for reinforcement and not to bridge the defect We do not advocate the use of a synthetic material in the sat. One last option consists of prophylactic mesh insertion at the time of bariatric surgery. On the basis of these findings and the fact that the majority of the bariatric procedures are conducted laparoscopically, we do not advocate for prophylactic hernia repair with mash. Loss of Domain the presence of a hernia containing a l&~ga amount of viscera can result in the development of a "second" abdominal cavity. The chronic changes that occur in the mesentery, venous and lymphatic returns, subcutaneous and epidermidis, contribute to the irreducibility of the hernia. Over lime, the progressive contraction of the abdominal muscles reduces the capacity of the abdominal cavity, resulting in loss of domain. Although often a prosthetic mesh of adequate size can overcome the loss of domain, the risk of developing abdominal compartment syndrome, wound breakdown, and mesh exposure is quite significant. Additional methods used to overcome loss of domain include tissue expanders, debulking (of both omentum and bowel), and component separation techniques. Whenever an extensive component separation is not sufficient to obtain abdominal wall closure, a bridging mesh has to be utilized. Due to the high incidence of wound complications in such a scenario, the choice may be limited to the use of biologic graft even with the known limitations of utilizing such material to bridge rather than to reinforce an autologous repair. During the preoperative assessment, the finding of loss of domain is usually obvious. An additional approach that has been wall described is the progressive preoperative distention of the abdominal cavity (progressive preoperative pneumoperitoneum). DiHerent technical variations have been described, but in general this approach consists of insuftlaling air or nitrous oxide via a peritoneal dialysis catheter or similar intraperitoneal access catheter over the course of 1 to 2 weeks. The progressive nature of abdominal distention is done to avoid the possible acute complicatiom of abdominal compartment syndrome that might develop with one-stage rapair. Once adequate abdominal expamion is obtained, a repair with prosthetic mesh or component separation with biologic mesh reinforcement will follow. A thorough knowledge of the different synthetic and biologic mesh characteristics can guide selection that best fits the clinical scenario. Usa of newer lmga-poralightwaight meshes in clean-contaminated fields remainsin spite of several reports on their safety-controversial. Certainly, in the presence of the heavily contaminated and infected field, the choice of repair is limited to a primary repair, staged procedure or the use of a biologic mesh. Although biologic meshes generally give adequate results in contaminated fields when used as reinforcement, their performance in infected fields remains uncertain. Finally, in case of mash infection, selective non-operative treatment might be attempted when systemic and local factors allow. Use of biological meshes for abdominal wall reconstruction in highly contaminated ilelds. Repair of giant midline abdominal wall hernias: "components separation technique" versus prosthetic repair: interim analysis of a randomized controlled trial. Acellular dermal allograft for ventral hernia repair in the compromised surgical ileld. Endoscopically assisted "components separation" for closure of abdominsl wall defects. Mesh graft infection following abdominal hernia repair: risk factor evaluation and strategies of mesh graft preservation. There are several clinical instances, which seem to identify certain hernia repairs as "complex. Hernias that involve contaminated wounds such as ostomies, enterocutaneous fistulas, or prior superficial or deep space infections. Hernias are associated with morbidly obese and the sequelae of the metabolic syndrome (see Table 28. Hernias, in these patient populations, are considered complex because their infection rates, recurrence rates, and overall complication rates are higher when compared to hernias in patients without these risk factors. Regardless of the source or timing of contamination, the most common organisms responsible for prosthetic mesh infection are gram-positive species specifically Staphylococcus aureus. Once a biofilm occurs on the surface of a prosthetic mesh, the ability to eradicate the infection is essentially zero necessitating the need for reoperation and mesh explanation. The undamaged and properly functioning abdominal wall yields a platform that supports pulmonary, digestive, and urologic function as well the locomotion of the thoraco-abdominal musculature. The net effect of a damaged and weakened abdominal musculature is the imbalance of intraabdominal and abdominal wall pressures leading to a hernia defect. In the undamaged abdominal wall, muscles contract isometrically to counter intraabdominal forces causing an equilibration of pressures. In the damaged abdominal wall, the muscles contract isotonically leading to a non-uniform of forces that have the net effect of progressively expanding the abdominal wall defect. In casas where hernia defects are small-lass than 10 em-patching a defect with mash may be adequate; but in complex hernias that are large, have severely weakened tissues, and/or are prone to recurrence or infection, what is required is to restore the abdominal musculature to its proper position and function. The literature suggests that recurrence rates ara significantly lower with the routine usa of mash as compared to tissue only repairs; paradoxically, the risk of infection is significantly higher in those patients treated with mesh due to the presence of a foreign body. The incidence of infection in mash hernia repair in clean-contaminated and contaminated casas can be as high as 40%. Other factors like steroid usa, smoking, and prolonged operative times further increase the risk of infection. Until recently, the true risk of morbidity associated with the contaminated abdominal wall was unclear. Again there is some data that suggests that augmenting that repair with mesh improves the outcomes but there are no long-term and randomized studies to confirm this. Military surgeons like their civilian counterpart have increasing employed abdominal wall reconstruction techniques to definitely manage these complex cases. Fortunately, 67% of the cohort successfully underwent early delayed abdominal closure via a silo technique where gortex mesh was placed and sequentially tightened over weeks until fascial closure was obtained. In cases where the primary closure was not possible patients underwent abdominal wall reconstruction supplemented with early on prosthetic (62%) and later biologic mesh (31 %). Abdominal Wall Reconstruction Techniques 1vo major techniques exist to reconstruct complex abdominal wall defects.
Purchase generic naltrexone on-line
To prevent sexual transmission symptoms stomach cancer 50mg naltrexone otc, mucosal immunity is needed, and this is likely to come from a mucosally administered vaccine. Worldwide, the cervical and vaginal mucosa are the major portals but the rectal mucosa is the more common route in North America and Europe. A T-cell vaccine would need to induce a long-lasting mucosal immune response that includes mucosal neutralizing IgA and IgG antibody and T-cell responses. Hepatitis B virus is often transmitted sexually Hepatitis B virus is detectable in semen, saliva and vaginal secretions. Hepatitis C is less commonly transmitted sexually; < 5% of long-term sexual partners are infected. The crab louse is well adapted for life in the genital region, clinging tightly to the pubic hairs (see Ch. It takes up to 10 blood feeds a day and this causes itching at the site of the bites. Patients may have evidence of scabies elsewhere on the body, with burrows between the fingers or toes. Anal intercourse allows the transfer of microorganisms from penis to rectal mucosa or to anal and perianal regions. Gonococcal or papillomavirus lesions, for instance, may occur in any of these sites. These include salmonellae, shigellae, hepatitis A virus, Giardia intestinalis and Entamoeba histolytica (see Ch. Except for hepatitis and human papillomavirus there are no vaccines for these infections, but antimicrobial chemotherapy is often available. Transmission depends upon human behaviour, which is notoriously difficult to influence. Long intervals between the onset of infectiousness and disease increase the chances of transmission. These may be confined to the gastrointestinal tract or are initiated in the gut before spreading to other parts of the body. In this chapter, we consider the important bacterial causes of diarrheal disease and summarize the other bacterial causes of food-associated infection and food poisoning. Viral and parasitic causes of diarrheal disease are discussed, as well as infections acquired via the gastrointestinal tract and causing disease in other body systems, including typhoid and paratyphoid fevers, listeriosis and some forms of viral hepatitis. For clarity, all types of viral hepatitis are included in this chapter, despite the fact that some are transmitted by other routes of infection. Infections of the liver can also result in liver abscesses, and several parasitic infections cause liver disease. Peritonitis and intra-abdominal abscesses can arise from seeding of the abdominal cavity by organisms from the gastrointestinal tract. Several different terms are used to describe infections of the gastrointestinal tract; those in common use are shown in Box 22. A wide range of microbial pathogens is capable of infecting the gastrointestinal tract, and the important bacterial and viral pathogens are listed in Table 22. For an infection to occur, the pathogen must be ingested in sufficient numbers or possess attributes to elude the host defences of the upper gastrointestinal tract and reach the intestine. Here they remain localized and cause disease as a result of multiplication and/or toxin production, or they may invade through the intestinal mucosa to reach the lymphatics or the bloodstream. The damaging effects resulting from infection of the gastrointestinal tract are summarized in Box 22. Diarrhea without blood and pus is usually the result of enterotoxin production, whereas the presence of blood and/or pus cells in the faeces indicates an invasive infection with mucosal destruction. True food poisoning occurs after consumption of food containing toxins, which may be chemical. The organisms may be destroyed during food preparation, but the toxin is unaffected, consumed and acts within hours. In food-associated infections, the food may simply act as a vehicle for the pathogen. Campylobacter) or provide conditions in which the pathogen can multiply to produce numbers large enough to cause disease. Some are found in both humans and animals, while others are strictly human parasites. Diarrhea is the result of an increase in fluid and electrolyte loss in to the gut lumen, leading to the production of unformed or liquid faeces and can be thought of as the method by which the host forcibly expels the pathogen (and in doing so, aids its dissemination). However, diarrhea also occurs in many non-infectious conditions, and an infectious cause should not be assumed. In the resource-rich world, it remains a very common complaint, but is usually mild and self-limiting except in the very young, the elderly and immunocompromised patients. However, such infections can be acquired by travellers to these areas and imported in to their home countries. Many cases of diarrheal disease are not diagnosed, either because they are mild and self-limiting and the patient does not seek medical attention, or because medical and laboratory facilities are unavailable, particularly in resource-poor countries. It is generally impossible to distinguish on clinical grounds between infections caused by the different pathogens. This is especially important in outbreaks, because of the need to instigate appropriate epidemiologic investigations and control measures. There may be associated vomiting, Bacterial causes of diarrhea Escherichia coli E. Some strains are important members of the normal gut flora in humans and animals (see Ch. In order to spread to a new host, pathogens are excreted in large numbers in the faeces and must survive in the environment for long enough to infect another person directly or indirectly through contaminated food or fluids. However, greater insight in to mechanisms of pathogenicity has led to specific group designations: enteropathogenic E. Hepatitis A, enteric fevers Perforation of mucosal epithelium after infection, surgery or accidental trauma. Infection of the gastrointestinal tract can cause damage locally or at distant sites. Strains that cause diarrheal disease do so by several distinct pathogenic mechanisms and differ in their epidemiology (Table 22. There is a range of pathogenic mechanisms within the species, resulting in more or less invasive disease. Verotoxin receptors have been identified on renal epithelium and may account for kidney involvement. Their role in diarrheal disease, especially in young children, is incompletely understood and somewhat controversial, with some studies reporting no association. More than 50 people died and the likely vehicle was sprouted beans imported from the Middle East. These organisms act in the small intestine to cause persistent diarrhea, especially in children in resource-poor countries. To simplify discussion and comparison, past convention has been to replace this species name with the serotype designation. While technically incorrect (the serotype is not a species), this practice is helpful when discussing interrelationships between different isolates. This convention is thus followed here to maintain continuity with other scientific literature. There is a large animal reservoir of infection, which is transmitted to humans via contaminated food, especially poultry and dairy products. Salmonella infection is also transmitted from person to person, and secondary spread can therefore occur, for example, within a family after one member has become infected after consuming contaminated food. The bacteria migrate to the lamina propria layer of the ileocaecal region, where their multiplication stimulates an inflammatory response, which both confines the infection to the gastrointestinal tract and mediates the release of prostaglandins. The organisms are not contained within the gastrointestinal tract, but invade the body to cause septicaemia; consequently, many organs become seeded with salmonellae, sometimes leading to osteomyelitis, pneumonia or meningitis.
Jojoba. Naltrexone.
- What is Jojoba?
- Dosing considerations for Jojoba.
- Acne, psoriasis, sunburn, chapped skin, hair loss, and other uses.
- Are there safety concerns?
- How does Jojoba work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96612
Buy naltrexone 50 mg without prescription
After seeding the surface of an agar plate with the organism to be typed treatment nausea naltrexone 50 mg without a prescription, suspensions of different phages are dropped on to the surface and the plate incubated. Phages that are able to lyse the strain will produce zones of clearing of the bacterial lawn. The patterns of lysis obtained with the same set of bacteriophages on different isolates of Staph. Specialized typing techniques Serotyping distinguishes between strains, using specific antisera this classic technique distinguishes between strains by a difference in their antigenic structure, which is recognized by reaction with specific antisera. However, serotyping requires the production and maintenance of appropriate banks of reagents. Therefore, this approach, when employed, is usually restricted to reference laboratories. Different Gram-negative rods may acquire the same plasmids by conjugation between different species. However, this method has also been used to map the spread of antibiotic resistance plasmids among hospital pathogens. However, as with serotyping, phage typing requires a reference laboratory for the production, maintenance and testing of the standard phage suspensions and has thus generally fallen out of favour. However, discrimination between strains of the same species may be less because of the conserved nature of the target sequences. Isolates in the first two patients are highly related (although slightly different in patient 2). However, several studies have shown that this method is especially prone to artefact and inter- and intra-laboratory variation. While a comparison of total chromosomal sequences is not a practical option, analysis of a subset of nucleotide sequences is the basis for what one could consider fourth-generation molecular epidemiology. Thus, recent years have seen a variety of sequence-based approaches to assessing microbial relatedness. However, issues related to the choice of epidemiologically relevant sequences, method of analysis, data output, and interpretation continue to be explored and optimized, a process being greatly facilitated by current developments in microbial whole genome sequencing. Molecular techniques for epidemiologic fingerprinting have many advantages Although molecular techniques may require expertise and equipment, they have several advantages. They can be extremely precise, can be performed rapidly, do not involve handling infectious organisms and can be used to type all of the relevant isolates. Disposable second layers of clothing were also used, for example outer gloves, a gown and hand and foot covering. These are investigated mostly by detecting virus in samples from symptomatic patients and then, depending on the clinical setting, collecting samples from asymptomatic patients when deciding whom to include in a cohort from whom isolates can be obtained. In general, only identification of the microbe as a virus is required in outbreaks of viral gastroenteritis, as the management is the same for all the viral causes of gastroenteritis. However, in this setting it is important from an epidemiologic perspective to identify the cause of the outbreak. Surveillance is critical to monitor any changes in the virus as these alterations to parts of its genome may result in the virus evading detection as the primers used in the diagnostic test may no longer match the complementary sequence of the template. In addition, for those viruses for which we have a vaccine, it is important to know which strains are circulating currently to ensure a good antigenic match with the vaccine strains. In an outbreak of respiratory infection, identification and typing of the virus is important not only for epidemiological purposes but also for issues of treatment and prophylaxis. Molecular detection and typing methodologies such as sequencing may be required, usually for epidemiologic purposes rather than direct management of patients. However, in a setting such as postoperative acute hepatitis B infection, an intensive investigation will be carried out covering the possible routes of transmission. This may include investigating blood products, healthcare workers who were involved in exposure-prone procedures, other patients on the operating list, sexual contacts, and other risk activities involving potentially blood-contaminated needles. Once the potential sources have been identified, serologic tests may be carried out to seek evidence of current, recent or past hepatitis B infection. Genome detection methods and sequencing of blood samples from the individual with acute hepatitis B, as well as the potential source or sources, will help to confirm the transmission event or events. Sterilization and disinfection are often talked about by microbiologists in relation to the production of sterile culture media and other laboratory activities, but it must be stressed that the concept of sterility is central to almost all areas of medical practice. An understanding of the rationale of sterilization and disinfection will aid intelligent use of the range of sterile equipment (from needles to prostheses) and techniques (from surgery to handwashing) employed in medical practice. Sterilization is achieved by physical or chemical means, either by the removal of organisms from an object or by killing the organisms in situ, sometimes leaving toxic breakdown products (pyrogens) in the object. Corrective / Preventive measures Once tracking is complete, corrective and preventive measures can be introduced Typing of the aetiologic agent responsible for the outbreak and knowledge of its characteristics and mode of transmission allow preventive measures to be taken. What these include depends to a great extent on the pathogen involved, but all must aim to improve basic hygiene, from more effective handwashing and improved general cleaning to more effectively regulated sterilization of equipment. Hygiene is a crucial factor since agents of nosocomial infection can be spread between patients by hospital staff. As noted earlier, awareness of the risks of being exposed to blood-borne virus infections in a hospital setting is Antiseptics are used to reduce the number of viable organisms on the skin Antiseptics are a particular group of disinfectants. Some act differentially, destroying the transient flora but leaving untouched the normal skin flora deep in the skin pores and hair follicles. It is impossible to sterilize the skin, but thorough washing with antiseptic soaps can reduce the numbers of organisms on the surface considerably and therefore reduce contact spread of infection (see above). However, the resident bacteria in the hair follicles and ducts of sweat glands can recolonize the skin surface within hours. In other words, a low bioburden is a prerequisite for cost-effective sterilization. If a population of microbes is exposed to a sterilizing technique, and the number of survivors, expressed as a logarithm, is plotted against time, the slope of the graph defines the death rate. These lines may be sigmoid or have shoulders, indicating that individual cells respond slightly differently, some being killed more easily than others. In the case of bacteria, the physiologic state of the organisms influences the scrub disinfectant. In addition, bacteria may be carried transiently on the skin surface and may be transmitted from a contaminated source to a susceptible patient. Careful handwashing with soap and water removes the transient flora and some of the superficial resident flora. Scrubbing the hands with disinfectants removes more of the resident flora, but the skin surface is recolonized within hours from the normal flora deep in the skin pores. It does not affect spores, but is effective against intracellular organisms such as Brucella and mycobacteria and many viruses. Since the beginning of recorded history, various other techniques have been used to prevent the multiplication of microorganisms, such as drying and salting of food. The detailed mechanisms of the death process of microorganisms may vary with the sterilizing technique used, but the net effect is similar in that essential cell constituents (nucleic acids or proteins) are inactivated. The D value is the time required to reduce the population by 90% at a specified temperature. Bacillus stearothermophilus spores are used as biologic indicators of effective heat sterilization by including filter paper strips carrying a standard number of spores in to the autoclave cycle. However, the spores of some bacterial species, especially soil organisms, are able to withstand this temperature. The safety margin is reduced in the presence of large numbers of organisms because there is a greater probability of more heat-resistant individuals existing in a large population; hence, the importance of cleaning instruments, whenever possible, before sterilization. Moist heat in an autoclave is used to sterilize surgical instruments and dressings and heat-resistant pharmaceuticals. A method for the sterilization of heat-sensitive instruments such as endoscopes uses a combination of lowtemperature (subatmospheric) steam and formaldehyde. All of these processes need to be carried out in a suitable pressure vessel and are therefore usually available in the hospital central sterile supply department.
Buy 50mg naltrexone amex
Every infection is a race between microbial replication and spread and the mobilization of host responses medications gout buy generic naltrexone 50 mg on-line. Microorganisms can infect in four main ways, depending upon whether host defences are intact or impaired. It is sometimes difficult to incriminate a specific microbe as the cause of a disease. A biologic response gradient causes a spectrum that can range from an asymptomatic to a lethal infection. To establish themselves on or in the host, microorganisms must either attach to , or penetrate, one of these body surfaces. The outer surface, covered by skin or fur, protects and isolates the body from the outside world, forming a dry, horny, relatively impermeable outer layer. Elsewhere, however, there has to be more intimate contact and exchange with the outside world. Therefore, in the alimentary, respiratory and urogenital tracts, where food is absorbed, gases exchanged and urine and sexual products released, respectively, the lining consists of one or more layers of living cells. In the eye, the skin is replaced by a transparent layer of living cells, the conjunctiva. Well-developed cleansing and defence mechanisms are present at all these body surfaces, and entry of microorganisms always has to occur in the face of these natural mechanisms. Successful microorganisms therefore possess efficient mechanisms for attaching to , and often traversing, these body surfaces. These receptor molecules, of which there may be more than one, are not present for the benefit of the virus or other infectious agent; they have specific functions in the life of the cell. Very occasionally, the receptor molecule is present only in certain cells, which are then uniquely susceptible to infection. In these cases, the presence of the receptor molecule determines microbial tropism and accounts for the distinctive pattern of infection. Receptors are therefore critical determinants of cell susceptibility, not only at the body surface, but in all tissues. After binding to the susceptible cell, the microorganism can multiply at the surface (mycoplasma, Bordetella pertussis) or enter the cell and infect it (viruses, chlamydia; see Ch. They are either shed in large numbers in secretions and excretions or are available in the blood for uptake, for example by blood-sucking arthropods or needles. Skin bacteria may enter hair follicles or sebaceous glands to cause styes and boils, or teat canals to cause staphylococcal mastitis. Several types of fungi (the dermatophytes) infect the nonliving keratinous structures (stratum corneum, hair, nails) produced by the skin. When the latter is very slow, as in the case of nails, the infection is more likely to become chronic. Even a small break in the skin can be a portal of entry if virulent microorganisms such as streptococci, water-borne leptospira or blood-borne hepatitis B virus are present at the site. A few microbes, such as leptospira or the larvae of Ancylostoma and Schistosoma, are able to traverse the unbroken skin by their own activity. It is kept clean by the continuous flushing action of tears, aided every few seconds by the windscreen wiper action of the eyelids. Therefore, the microorganisms that infect the normal conjunctiva (chlamydia, gonococci) must have efficient attachment mechanisms (see Ch. Interference with local defences due to decreased lacrimal gland secretion or conjunctival or eyelid damage allows even non-specialist microorganisms to establish themselves. Contaminated fingers, flies, or towels carry infectious material to the conjunctiva, examples including herpes simplex virus infections leading to keratoconjunctivitis or chlamydial infection resulting in trachoma. Antimicrobial substances in tears, including lysozyme, an enzyme, and certain peptides have a defensive role. Biting arthropods Biting arthropods such as mosquitoes, ticks, fleas and sandflies (see Ch. The arthropod transmits the infection and is an essential part of the life cycle of the microorganism. Sometimes the transmission is mechanical, the microorganism contaminating the mouth parts without multiplying in the arthropod. In most cases, however, the infectious agent multiplies in the arthropod and, as a result of millions of years of adaptation, causes little or no damage to that host. After an incubation period, it appears in the saliva or faeces and is transmitted during a blood feed. Efficient cleansing mechanisms (see Chs 18 and 19) deal with these constantly inhaled particles. In the upper or lower respiratory tract, inhaled microorganisms, like other particles, will be trapped in mucus, carried to the back of the throat by ciliary action, and swallowed. Those that invade the normal healthy respiratory tract have developed specific mechanisms to avoid this fate. Specific molecules on the organism (often called adhesins) bind to receptor molecules on the susceptible cell. Inhibiting ciliary activity is another way of interfering with cleansing mechanisms. Avoiding destruction by alveolar macrophages Inhaled microorganisms reaching the alveoli encounter alveolar macrophages, which remove foreign particles and keep the air spaces clean. Most microorganisms are destroyed by these macrophages, but one or two pathogens have learnt either to avoid phagocytosis or to avoid destruction after phagocytosis. Tubercle bacilli, for instance, survive in the macrophages, and respiratory tuberculosis is thought to be initiated in this way. The vital role of macrophages in antimicrobial defences is dealt with more thoroughly in Chapter 14. Alveolar macrophages are damaged following inhalation of toxic asbestos particles and certain dusts, and this leads to increased susceptibility to respiratory tuberculosis. Under normal circumstances, multiplication of resident bacteria is counterbalanced by their continuous passage to the exterior with the rest of the intestinal contents. They will then avoid being carried straight down the alimentary canal to be excreted with the rest of the intestinal contents. The concentration of microorganisms in faeces depends on the balance between the production and removal of bacteria in the intestine. Electron micrograph of thin section from organ culture of guinea pig trachea 1 h after addition of the virus. Infection sometimes involves more than mere adhesion to the luminal surface of intestinal epithelial cells. Shigella flexneri, for example, can only enter these cells from the basal surface. Initial entry occurs after uptake by M cells, and the bacteria then invade local macrophages. This gives rise to an inflammatory response with an influx of polymorphs, which in turn causes some disruption of the epithelial barrier. Non-motile microorganisms, in contrast, rely on random and passive transport in the mucus layer. As might be expected, microorganisms that infect by the intestinal route are often capable of surviving in the presence of acid, proteolytic enzymes and bile. All organisms infecting by the intestinal route must run the gauntlet of acid in the stomach. The fact that tubercle bacilli resist acid conditions favours the establishment of intestinal tuberculosis, but most bacteria are acid sensitive and prefer slightly alkaline conditions. The minimum disease-producing dose was 108 bacteria without bicarbonate and 104 bacteria with bicarbonate.
Generic naltrexone 50 mg otc
The fascia at the umbilicus is closed with absorbable suture medicine 44 159 buy naltrexone 50mg otc, followed by closure of the skin incision. The surgeon typically stands on the right side of the patient, however, sides may be alternated during the procedure to facilitate reduction of hernia contents or mesh placement. Technique the hernia is first assessed, measuring the size and palpating the boarders. Entry in to the peritoneum is either accomplished under visual control or through an optical trocar, depending on whether or not a single port access device is used or 2 to 3 trocars through one incision is used. The multi-port access generally uses one 10 mm port and either one or two 5 mm ports through separate fascial incisions. The peritoneum is accessed by using a musclesplitting technique and the single access port device is placed and the abdomen insufilated. Bower and Love describe the use of a Veress needle in the left upper quadrant of the abdomen to provide insufll. The procedure is carried out in the same fashion as the standard laparoscopic method. At the end of the procedure, port(s) are removed and the fascial defects are closed with absorbable suture followed by skin closure. Requirements for discharge are recovery from general anesthetic, able to tolerate clear liquids, and able to tolerate pain with oral medication. Prolonged operative time, organ injury or suspicion of organ injury, bleeding, or perioperative anesthetic complications would be indications for inpatient admission. The literature for all types of single site or single port hernia procedures showed few conversions to the standard laparoscopic methods and no conversions to an open method. Postoperative complications were minor and were able to be corrected without any further surgery. Generally, patient follow-up appointments have ranged from 2 weeks up to 24 months. Patients have been monitored for recurrence at the primary site as well as access site hernias. As advancements are made in laparoscopic surgery, newer methods are explored to provide improvements to the procedure as a whole. Due to the novelty of this procedure, only a small amount of research with short-term outcomes is available. Questions have been posed as to whether or not this technique is superior to standard laparoscopic methods. Some surgeons dispute this thought, as they believe the incision needed for the single access port device is larger than what is needed for the standard laparoscopic approach. Ultimately, there are issues with this technique that need to be further evaluated. There is also a necessity for more long-term randomized controlled studies in accessing recurrences of primary hernias as well as access site hernias. Single-port laparoscopic totally extraperitoneal inguinal hernia repair with the TriPort system: initial experience. Single-incision laparoscopic surgery for total axtraperito- ~ neal repair of inguinal harnie. First, unlike most other laparoscopic procedures, we approach ventral hernias from the opposite direction, and oftentimes in apposition to our field of view. We find ourselves looking "up" instead of down, and "at" ourselves instead of "ahead" of ourselves. Thus, we may need to manipulate mesh and tackers in reverse when the camera is coming from the contralateral side. Aside from the difficulties of adhesiolysis being performed laparoscopically, these two factors alone can be challenging to most surgeons who may otherwise be very adept at other laparoscopic procedures. In addition, when we repair a ventral hernia, we are exposing the patient to the very same problem we are addressing. Further, the application of the reduced port techniques and single port access surgery should be applied with the same thought process as multiport laparoscopy. When undertaking the practice of laparoscopic ventral hernia repair, these factors play an important role in moving forward. Both as hurdles we must overcome, as well as potential learning points from which we can improve the technique and outcomes when positioned correctly. Attention to a new approach as well as the potential for subsequent hernia formation at the port site must remain in the forefront. However, if a laparoscopic repair is going to proceed, then the single port access technique is a viable alternative. All patients for ventral hernia repair can be considered to have the procedure performed laparoscopically, but both science and common sense will dictate which patients are appropriate candidates for this approach. Oftentimes, patients will be prepared for a laparoscopic approach and repair, but intraoperative findings or conditions may dictate an open procedure needs to be performed. In this light, a surgeon performing laparoscopic hernia surgery should also be well versed in all open repair techniques, meshes, and reconstructive procedures. The most important contraindication would be lack of familiarity with single port access surgery. Clearly you have to decide at what level of skill you can proceed with the hernia repair through decreasing number of port sites. This allowed us to repair small hernias and ultimately we graduated to much larger hernia repairs. However, as you move forward with single port access, the most important contraindication will be your level of skill with this new procedure. As you develop your technical skills, single port access ventral hernia repair can be offered to the patients with small and large hernias as well as multiple or complex defects. Again, the most important aspect is safety and it should always be remembered to add another port site or trocar whenever necessary to maintain a safe operative procedure. Each of these hernias can be repaired easily and oftentimes with success, serving as a bridge to larger and more complex hernias. Just as is taught with single port access cholecystectomy and colectomy surgery, the "step-down" approach is a gradual transition from multipart to single port surgery. In fact, as the developers of single port access surgery, the author began the road to reduced port surgery with the introduction of the "two-port, one-stitch" technique for ventral hernia repair. Not only does it make for an easier transition, but it also allows for a better chance at success at each level, encouraging the surgeon to move to the next level. In our experience, as reported initially in our first series, we have repaired not only primary defects but also recurrent hernias. We had been able to apply this technique to multiple defects as well as small to large defects. In addition, we have been able to apply the repairs with prior mesh repairs that need a new sublay mesh. Multiple defects Multiply recurrent hernias Lateral hernias Long midline incision hernias Complicated hernias Complex hernias the contraindications for single port ventral hernia repair are the same as for multipart ventral hernia repair. Any medical contraindication that would disallow the application of carbon dioxide or the implantation of mesh would also be a contraindication in these patients. We need to plan the surgery before we arrive in the operating room, so we are ready to handle all possibilities. Conversion from single port access to reduced port surgery to multipart laparoscopy to open surgery is not a complication, but rather a natural progression in the "safe" approach to ventral hernia repair. The planning for these patients is somewhat different With most laparoscopies we can generally enter through the umbilicus. However, most patients generally have a midline scar through which the hernia has occurred. A surgical procedure in a particular quadrant of the abdomen would make that a quadrant we would want to avoid. In some instances, the initial port site may need to be just to the left of the xyphoid process. If permanent tacks were used, this could help delineate the size and position of the mesh that has been placed in the past, which may help with the decision on the size of the mesh you will be placing. Another important aspect of recurrent ventral hernias we have found is to obtain a copy of the prior operative reports. These operative reports will certainly help in planning whether or not you will need to remove or replace mesh. In simple hernias, you can oftentimes avoid placement of a Foley catheter if the patient has just urinated and you are going to be entering high in the abdomen or lateral where the bladder would not be positioned.