Discount tadalafil 2.5mg free shipping
Conversely erectile dysfunction gene therapy treatment purchase tadalafil pills in toronto, in a glaucoma patient who has undergone cataract surgery, progression may be masked in evaluation by this method. The software presents an eventbased method that is based on the pattern deviation plot and, therefore, adjusts for the potential confounding effects of diffuse loss of sensitivity from media opacities. Detection of new or progressing visual field defects is performed by comparison to the baseline; therefore, it is critical to have reliable baseline examinations. Often, the patient experiences a learning effect, and the second visual field may show substantial improvement over the first. The software automatically selects the first 2 available examinations as the baseline tests. However, one can easily override this selection to a more suitable time-point (eg, change in therapy after progression), or to avoid initial learning effects (which could reduce the sensitivity to detect progression). It identifies points that show change greater than the expected variability (at the 95% significance level), as determined by previous studies with stable glaucoma patients. If significant change is detected in at least 3 points and repeated in the same points in 2 consecutive follow-up tests, the software will flag the last examination as Possible Progression. A number of points in the inferonasal region show repeatable significant change (blackfilled triangles). The Octopus perimeter also provides a comprehensive statistical package (EyeSuite) for evaluation of visual field progression. In addition, the software provides an analysis of progression by individual test points (pointwise linear regression) and by clusters, where test locations are combined according to nerve fiber bundle patterns. Structure and function correlations It is important to correlate changes in the visual field with those in the optic nerve head. If such correlation is lacking, the ophthalmologist should consider other causes of vision loss, such as ischemic optic neuropathy, demyelinating or other neurologic disease, or pituitary tumor. It should be noted, however, that progressive visual field loss may sometimes be seen in the absence of optic nerve head changes and vice versa. Conversely, in cases of more severe disease, progressive visual field losses tend to occur despite lack of detectable structural change. This apparent disagreement may be explained by the different characteristics of the tests, including scaling, variability, and presence of floor/ceiling effects. Therefore, follow-up of glaucoma patients should be performed using both structural and functional assessments. The structure and function relationship in glaucoma: implications for detection of progression and measurement of rates of change. Perimetric tests are also subjective examinations and therefore responses may vary on repeat testing, or during the same test, reducing the ability to confidently detect genuine early abnormalities. Other tests measuring the integrity of the visual field include contrast sensitivity perimetry, flicker sensitivity, microperimetry, visually evoked cortical potential, and multifocal electroretinography. However, these tests are not commonly employed in the evaluation of patients with glaucoma. Predicting progression of glaucoma from rates of frequency doubling technology perimetry change. Other Tests for Selected Patients Several other tests may be helpful in selected patients. The test employs shorter-wavelength sound waves than does conventional ocular ultrasonography, limiting penetration through the sclera but increasing the resolution. Other factors that may contribute to disease susceptibility include corneal hysteresis, low ocular perfusion pressure, low cerebrospinal fluid pressure, abnormalities of axonal or ganglion cell metabolism, and disorders of the extracellular matrix of the lamina cribrosa. Patients may seem relatively asymptomatic until the later stages of the disease, when central vision is affected. Careful periodic evaluation of the optic nerve and visual field testing are essential in the management of glaucoma. Stereophotographic documentation of the optic nerve or computerized imaging of the optic nerve or retinal nerve fiber layer aids the detection of subtle changes over time. Visual field loss should correlate with the appearance of the optic nerve; significant discrepancies between the pattern of visual field loss and optic nerve appearance warrant additional investigation, as noted in Chapter 3. Fluctuation of intraocular pressure and glaucoma progression in the early manifest glaucoma trial. Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Older age the Baltimore Eye Survey found that the prevalence of glaucoma increases dramatically with age, particularly among individuals of African descent, whose prevalence exceeded 11% in those older than 80 years. Therefore, older age appears to be an independent risk factor for the development and progression of glaucoma. In addition, glaucoma is more likely to be diagnosed in black patients at a younger age and at a more advanced stage than it is in white patients. As mentioned previously, black patients have thinner corneas on average than white patients. Evaluation of the optic nerve head is particularly challenging in highly myopic eyes that have tilted discs or posterior staphylomas. Also, the myopic refractive error may cause minification of the optic nerve, further complicating accurate optic nerve assessment. Myopia-related retinal degeneration or anomalies can cause visual field abnormalities that are difficult to distinguish from those caused by glaucoma. In addition, patients who are highly myopic may have difficulty performing accurately on visual field tests, making interpretation of visual field abnormalities more challenging. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Associated Disorders Diabetes mellitus There is controversy as to whether diabetes mellitus is a risk factor for glaucoma. However, the Framingham Study, the Baltimore Eye Survey, the Barbados Eye Study, and a revised analysis of the Rotterdam Study did not find a significant association. Furthermore, the Rotterdam Study and the Barbados Eye Study, which were large longitudinal population-based studies, did not identify diabetes as a risk factor for the development of glaucoma. However, the cohort of diabetic patients was skewed, because the presence of retinopathy was an exclusion criterion for this study. Hypertension the Baltimore Eye Survey found that systemic hypertension was associated with a lower risk of glaucoma in younger (<65 years) subjects and a higher risk of glaucoma in older subjects. The hypothesis is that younger individuals with high blood pressure may have better perfusion of the optic nerve, but as these patients age, their chronic hypertension may have adverse effects on the microcirculation of the optic nerve and increase its susceptibility to glaucomatous optic neuropathy. Conversely, in the Barbados Eye Study, the relative risk of developing glaucoma among subjects with systemic hypertension was less than 1. The overtreatment of systemic hypertension may contribute to glaucoma progression in some cases (eg, normal-tension glaucoma) and should be monitored. Other associated conditions Sleep apnea, thyroid disorders, hypercholesterolemia, migraine headaches, low cerebrospinal fluid pressure, corneal hysteresis, and Raynaud phenomenon have variously been identified in some studies as potential risk factors for the development of glaucoma. The patients at greatest risk of blindness are those who present with visual field loss at the time of diagnosis. For patients with decreased visual function, a referral to a vision rehabilitation specialist should be considered. These specialists can help improve visual function by optimizing lighting, enhancing contrast, reducing glare, and providing adaptations to enhance activities of daily living. Orientation and mobility specialists can be consulted and vision substitution strategies (eg, talking books, watches) utilized to improve daily function and quality of life for these patients. Accordingly, many authorities believe the terms normal-tension glaucoma and low-tension glaucoma should be abandoned. Correlation of asymmetric damage with asymmetric intraocular pressure in normal-tension glaucoma (low-tension glaucoma). Differential Diagnosis Normal-tension glaucoma can be mimicked by many conditions, as summarized in Table 4-2. Patients with myopia may have anomalous optic nerve heads or myopia-related visual field defects that often make it difficult to diagnose glaucoma or monitor for glaucomatous progression. Visual field defects consistent with glaucoma have been noted after a decrease in blood pressure following a hypotensive crisis; however, these defects do not progress once the underlying condition is stable.
Buy tadalafil 5mg low cost
Intervention Results the operation was performed at L4-L5 in 69 patients erectile dysfunction after radiation treatment for prostate cancer discount tadalafil 5mg fast delivery, at L3-L4 in 6 patients, and at L5-S1 in 1 patient. Of the 68 consecutive patients with 2-year follow-up, 55 were women and 13 were men. Thirty-five patients were randomized to the instrumentation group, while 33 were randomized to the noninstrumented cohort. The clinical outcome was excellent (patient resumed unrestricted activity and had near complete relief of pain in the back, lower limbs, or both) or good (occasional discomfort in the back or lower limbs, necessitating occasional non-narcotic medication) in 76% of the patients in whom instrumentation was placed and 85% of those in whom no instrumentation was used (p = 0. However, only 45% of the noninstrumented cases revealed arthrodesis at 2 years after surgery (p = 0. Preoperative angular motion, spondylolisthesis, and sagittal motion did not significantly contribute to pseudarthrosis. There were no new peripheral neurologic deficits observed after surgery in either group. Two patients (one in each group) required a decompressive laminectomy at an adjacent level. One patient had hardware removed due to persistent low back pain; solid fusion was observed. One patient in the noninstrumented group experienced low back pain in the setting of pseudarthrosis and subsequently underwent an instrumented fusion. One patient in the instrumented group experienced recurrent stenosis and pseudarthrosis developed, requiring a second decompression and instrumented arthrodesis. The 2-year follow-up is relatively short and may not accurately capture the long-term differences among clinical outcomes in those with a successful fusion compared to those in which a pseudarthrosis was present. Although no clinical differences were observed at 2 years postoperatively, longer-term follow-up may be necessary to evaluate the role of successful fusion in the clinical outcomes. Historically, the methods of evaluating a fusion mass have varied in the literature. Using radiographs to determine fusion status has traditionally been difficult; the current study evaluated fusion mass on radiographs as critically as possible; however, this method may factor into the low reported fusion rate in noninstrumented cases, which is contrary to their high clinical success rate. Relevant Studies Some surgeons have reported clinical success after decompression alone for spinal stenosis in the setting of degenerative spondylolisthesis. This landmark study revealed that patients who underwent an arthrodesis with the decompression experienced significant improvements in clinical outcome compared to those that did not undergo arthrodesis. Similar findings were described in a meta-analysis of operative treatments in degenerative spondylolisthesis by Mardjetko et al. The successful rate of fusion with rigid pedicle fixation had been previously described in studies evaluating multiple degenerative spinal conditions. Although the fusion rates were markedly increased in the instrumented group, there was no significant difference in clinical outcome between the two groups despite the high percentage of pseudarthrosis present in the noninstrumented cohort. These results were in agreement with the landmark findings by Herkowitz and Kurz,2 and were thought to be related to the development of a fibrous fusion that provided sufficient structural support to prevent progressive spondylolisthesis. In an effort to determine the long-term influence of pseudarthrosis on the clinical outcomes, Kornblum et al. Long-term clinical outcome was excellent or good in 86% of the patients with solid arthrodesis but in only 56% of patients who developed a pseudarthrosis (p = 0. Following these landmark studies, the standard teaching has been decompression and fusion for patients presenting with symptomatic degenerative spondylolisthesis; sometimes however, the patient may similarly benefit from decompression alone or motion-preserving alternatives. Satisfactory clinical outcomes have been achieved with an isolated decompression in selected patients, avoiding the additional risks and costs of instrumentation and spinal fusion. Thus, less invasive, motion-preserving alternatives have been introduced to provide neural decompression and stabilization. The Graf, Dynesys, and Coflex systems have all showed promising clinical outcomes with 2- to 5-year follow-up data similar to patients who have received fusions with or without instrumentation. An essential component of the surgical intervention may rest in the ability to classify instability within degenerative spondylolisthesis. However, there is no current, widely accepted algorithm designed to provide surgeons with a decision-making model that would allow them to tailor their surgical treatment to patients presenting with a variety of symptoms, radiographic findings, and observed pathology in the setting of degenerative spondylolisthesis. Minimum 5-year results of degenerative spondylolisthesis treated with decompression and instrumented posterior fusion. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective study comparing decompression with decompression and intertransverse process arthrodesis. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective long-term study comparing fusion and pseudarthrosis. Radiographic predictors of delayed instability following decompression without fusion for degenerative grade I lumbar spondylolisthesis. Cost-utility of lumbar decompression with or without fusion for patients with symptomatic degenerative lumbar spondylolisthesis. Can low-grade spondylolisthesis be effectively treated by either coflex interlaminar stabilization or laminectomy and posterior spinal fusion Prospective study of surgical treatment of degenerative spondylolisthesis: Comparison between decompression alone and decompression with Graf system stabilization. Wilson Research Question/Objective Degenerative spondylolisthesis is a common cause of spinal stenosis, causing walking disability and leg pain in older adults. Previous studies have demonstrated the utility of surgical management in relieving these symptoms, but they have not clearly shown which surgical option is superior, although most surgeons in the United States opt for decompression with fusion in this scenario. The hypothesis of this randomized control study was that laminectomy plus fusion would result in greater physical healthrelated outcomes and lesser disability scores than laminectomy alone. Study Design A randomized control study was conducted, and patients from five centers were assessed for eligibility from March 2002 through August 2009. Sample Size In total, 130 patients were identified as eligible, 40 declined to participate, and 44 declined to undergo randomization and were included in the observation group. Sixty-six patients underwent randomization, 35 were randomized into laminectomy, and 31 were randomized into laminectomy plus fusion. Follow-Up Initial clinical assessments were performed during routine outpatient visits at 1. Exclusion criteria included lumbar instability, defined as motion >3 mm at the listhesis level on flexionextension radiographs or as judged by the enrolling surgeon based on history of mechanical back pain with axial loading of spine. Intervention or Treatment Received Patients in the laminectomy alone treatment arm received complete laminectomy with partial removal of the medial facet joint at the single level of spondylolisthesis. Patients in the laminectomy plus fusion treatment arm received the above treatment as well as implantation of pedicle screws, titanium alloy rods across the level of listhesis, and bone graft harvested from the iliac crest. Results There were no statistically significant between-group differences in baseline characteristics. According to a random-intercept logistic-regression model, the predicted rate of a minimal clinically important difference of 5 points at the 2-year follow-up was 91. Over the course of 4 years, the laminectomy-alone group had a 34% rate of reoperation, all for subsequent clinical instability at the index level as assessed by the primary surgeon, compared to 14% in the laminectomy-plus-fusion group, all done at an adjacent lumbar level for disc herniation or clinical instability. Surgical complications, blood loss, length of stay, and length of procedure were all significantly greater in the laminectomy-plus-fusion group than in the laminectomyalone group. Study Limitations As noted in the manuscript, there were some differences between the original trial registration and the final protocol, which may have some implications on internal validity. It was also specified that follow-up would continue through 5 years, and that a hospital-cost analysis would be conducted. Additionally, 14% of randomized participants were lost to follow-up at the 2-year mark, and 30% were lost at the 4-year mark. Last, less-invasive decompression strategies, such as unilateral laminotomies, and other fusion strategies, including minimally invasive techniques, use of bone-graft extenders or bone morphogenetic protein, or interbody fusion techniques, have become more popular over the time course of the study. These newer surgical options raise the question of generalizability of this study. Wilson Research Question/Objective Lumbar spinal stenosis is the most common indication for spinal surgery, and studies have shown that surgical treatment in selected patients is more successful than conservative measures.
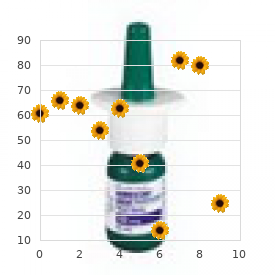
| Comparative prices of Tadalafil | ||
| # | Retailer | Average price |
| 1 | Ross Stores | 803 |
| 2 | Aldi | 642 |
| 3 | Family Dollar | 885 |
| 4 | Walgreen | 111 |
| 5 | AutoZone | 703 |
| 6 | Amazon.com | 511 |
Cheap 10mg tadalafil with mastercard
Epithelial erosions rarely develop effexor xr impotence purchase tadalafil 20mg overnight delivery, but a severe decrease in vision typically occurs between 10 and 30 years of age. There are 3 variants of macular dystrophy, and they are distinguished based on biochemical differences. Errors occur in the synthesis of keratan sulfate and in the activity of specific sulfotransferases involved in the sulfation of the keratan sulfate lactose aminoglycan side chain. Typically, the cornea is thin with dense opacities that occur more posteriorly in the periphery. This test can help in the diagnosis of macular dystrophy, even in preclinical forms and carriers. Pathologically, the opacities are accumulations of unesterified and esterified cholesterol and phospholipids. In the normal process of embedding tissue in paraffin, cholesterol and other fatty substances are dissolved; therefore, fresh tissue should be submitted to the pathologist for special lipid stains. Electron microscopy shows abnormal accumulation of lipid and dissolved cholesterol in the corneal epithelium, in the Bowman layer, and throughout the stroma. Confocal microscopy reveals disruption of the basal epithelial/subepithelial nerve plexus, with highly reflective intracellular and extracellular deposits. The diagnosis is usually made by the second or third decade of life, although it may be further delayed in patients who have the crystalline form of the disease. Central subepithelial crystals are seen in only 50% of patients and do not involve the epithelium. A fasting lipid profile should be done to detect possible hyperlipoproteinemia or hyperlipidemia. Patients with abnormal serum lipid levels are managed with dietary changes and/or medication, but the progression of the corneal dystrophy is unaltered. Visual morbidity in thirty-four families with Schnyder crystalline corneal dystrophy (an American Ophthalmological Society thesis). On electron microscopy, the collagen fibril diameter is approximately half the normal size in all lamellae. Abnormal lamellar layers consisting of thin filaments arranged in an electron-lucent ground substance separate the lamellae of normal appearance. The course is nonprogressive or slowly progressive, with moderate to severe vision loss. Congenital stromal dystrophy of the cornea caused by a mutation in the decorin gene. Transmission electron microscopy shows membrane-based inclusions with delicate granular material. Confocal microscopy shows an accumulation of pathologic material in stromal cells and inclusions in the basal nerves. Fleck corneal dystrophy is a nonprogressive condition that may be congenital or may present early in the first decade of life. The epithelium, Bowman layer, Descemet membrane, and endothelium are not involved. Fleck dystrophy may be associated with decreased corneal sensation, limbal dermoid, keratoconus, central cloudy dystrophy, punctate cortical lens changes, pseudoxanthoma elasticum, or atopy. On electron microscopy, there is disorganization of the posterior stromal lamellae. On confocal microscopy, there are microfolds and a hyperreflective layer in the posterior stroma. B, Slit-lamp photograph shows a diffusely thin, flat cornea with a posterior stromal opacity. Focal endothelial abnormalities, a prominent Schwalbe line, fine iris processes, pupillary remnant, iridocorneal adhesions, corectopia, pseudopolycoria, and anterior stromal tags have been noted. On electron microscopy, there are membrane-bound intracellular vacuoles containing electron-dense material suggestive of secondary lysosomes, and there are inclusions consistent with lipofuscin-like lipoprotein, suggesting a degenerative process. Primary dysfunction of the endothelial cells manifests as increased corneal swelling and deposition of collagen and extracellular matrix in the Descemet membrane, which is thickened. It is not clear whether the reduction in the posterior nonbanded zone and the increase in thickness of the abnormal posterior collagenous layer are primary effects of endothelial dysfunction or are secondary to chronic corneal edema. Cornea guttata is first evident centrally and then spreads toward the periphery (stage 1). As the disease progresses, the Descemet membrane may become thickened, and stromal edema may worsen, causing epithelial bullae and bullous keratopathy (stage 3). Subepithelial fibrosis, scarring, and peripheral superficial vascularization secondary to chronic edema occur in end-stage disease (stage 4). Fuchs dystrophy usually presents in the fourth decade of life or later (except in the case of the early-onset variant, which may present as early as the first decade of life). Symptoms are rare before 50 years of age and are related to the edema, which causes a decrease in vision, contrast sensitivity, and/or glare. Symptoms are often worse upon awakening because of decreased surface evaporation during sleep. Cornea guttae are seen with indirect illumination over the iris and with the red reflex. In advanced cases, anterior stromal puncture, placement of amniotic membrane, or a conjunctival flap may be considered to relieve pain, but restoration of vision requires a corneal transplant. In one recent case series, removal of a relatively small area of abnormal Descemet membrane and endothelium (descemetorhexis) resulted in mitosis of normal endothelial cells from the periphery, leading to resolution of the edema and improvement in vision. In advanced cases where there has been anterior corneal scarring, a full-thickness procedure may still be indicated. The prognosis for graft survival is good, especially if the procedure is done before vascularization occurs. Specular microscopy may be helpful in the initial evaluation of Fuchs dystrophy and in following the clinical course for loss of corneal endothelial cells; however, it is not necessary in the presence of diffuse confluent guttae. Endothelial cell counts less than 1000/mm2, morning increase in corneal thickness, or the presence of epithelial edema suggests that the cornea may decompensate following intraocular surgery (see Chapter 2); thus, appropriate precautionary measures should be taken. Treatment of Fuchs endothelial dystrophy by Descemet stripping without endothelial keratoplasty. Opinion is divided on the value of relying on specular microscopy alone in making the diagnosis. Confocal microscopy reveals vesicular lesions and railroad track, bandlike dark areas with irregular edges. Anterior stromal puncture can be used to induce focal subepithelial fibrosis in cases of localized swelling. With more severe disease, keratoplasty may be required and, if present, glaucoma must be managed. If peripheral anterior synechiae, glaucoma, or both are present preoperatively, the prognosis for successful corneal transplant is reduced. A, Broad, oblique view shows clusters of endothelial vesicles, which are commonly seen. Stromal thickening with severe disorganization and disruption of the lamellar pattern is evident. This dystrophy is a congenital, usually nonprogressive condition with asymmetric corneal clouding and edema that ranges from a diffuse haze to a ground-glass appearance; focal gray spots are occasionally seen. Multiple chromosomal loci for keratoconus have been reported, but the identification of specific genes remains elusive. Clinically unaffected first-degree relatives have a higher chance of showing subclinical topographic abnormalities associated with keratoconus than does the general population. There is a slight female preponderance, and the incidence is higher in South Asia and the Middle East. Genetic predisposition and environmental risk factors such as eye rubbing, inflammation, atopy, hard contact lens wear, and oxidative stress all play a role in the onset and progression of keratoconus. Onset occurs during puberty, and the progression rate is greatest in young people. Keratoconus can be associated with ocular diseases such as vernal keratoconjunctivitis, Leber tapetoretinal degeneration, retinitis pigmentosa, and floppy eyelids.
Order tadalafil canada
However erectile dysfunction doctors rochester ny buy tadalafil discount, because of its logistic and practical limitations, its clinical role in acute stroke is limited. Meanwhile, other incremental refinements in the def inition of the ischemic penumbra are likely, including measurement of biochemical thresholds with spectros copy, and imaging of a "molecular penumbra" by means of measuring gene markers of protein expression [1]. Although early studies suggested that various magnetic resonance imaging techniques such as perfusion and diffusionweighted imaging could differentiate between penumbra and infarct, more recent studies have shown that this may be an oversimplification. Computed tomography perfusion oxygen free radicals, releasing cytotoxic enzymes, alter ing vasomotor reactivity, and increasing cytokine and chemoattractant release [76]. However, the empirical evidence suggests that the benefits of reperfusion are greater than the hazards (Sections 13. In the ischemic penumbra that surrounds the anoxic core, cells can be rescued by rapid reperfusion. Contrastenhanced computed tomography may be able to delineate infarcted and penumbral tissue in acute stroke. Reperfusion and brain damage Reperfusion within the revival times of ischemic tissues may salvage cells and aid recovery (by restoring oxygen and nutrient delivery to ischemic brain tissue). However, it may also be detrimental, causing socalled "reperfu sion injury" due to the resupply of glucose (which may increase lactic acidosis), oxygen (which may trigger pro duction of injurious free radicals), water, and osmotic equivalents (which may exacerbate vasogenic edema), and bloodborne cells (such as neutrophils), which may exacerbate ischemic damage [74, 75]. Rescue of the penumbra, either by restoration of blood supply or by interruption of the adverse metabolic or neurochemical cascade, is the basis of acute stroke therapy. This causes an increase in extracellular K+ as well as an influx of Na+, Cl-, and Ca2+ into the cells. The ini tial increase in extracellular K+ may spread, triggering depolarization of neurons and reversal of the amino acid transporters. In these conditions, both voltageoperated and receptoroperated calcium channels are recruited, thus provoking an elevation of free cytosolic Ca2+. The depolarized presynaptic neurons release the neurotrans mitter glutamate into the synaptic cleft. Reuptake of glu tamate is impaired, leading to an increase in extracellular concentration of the excitatory amino acid glutamate. Upon their activa tion, these open their associated ion channel to allow the influx of Ca2+ and Na+ ions [2, 84]. Glutamateevoked Na+ increase in astrocytes evokes the transmission of intercellular Na+ and Ca2+ metabolic waves and an increase in uptake of glucose [85]. Under physiological conditions, calcium ions (Ca2+) govern a multitude of cellular processes, including cell growth, differentiation, and synaptic activity. Consequently, there are energydependent homeostatic mechanisms to maintain a low intracellular Ca2+ concentration (about 100 times lower than its extracellular concentration) so that Ca2+ signals remain spatially and temporally localized. In excitotoxicity, the excessive synaptic release of glutamate which leads to excessive influx of Ca2+, together with any Ca2+ release from intracellular compartments, can overwhelm Ca2+ regulatory mechanisms and this leads to dysregulation of Ca2+ homeostasis, and ultimately to cell damage and death. The cell damage associated with a nonphysiological unreg ulated rise in intracellular cytoplasmic Ca2+ is caused mainly by changes in total calcium influx [6]. Mitochondrial injury is associated with failure of mitochondrial functions such as oxidative phosphorylation, and release of reactive oxygen species (see later) [6, 84]. Mitochondrial calcium accumulation and oxidative stress can then trigger the assembly (opening) of a highconductance pore in the inner mitochondrial membrane. In addition, the augmented intracellular Ca2+ enhances the increase in extracellular glutamate, thus propagating excitotoxicity [84]. Although Ca2+ disregulation is para mount to neurodegeneration, the exact mechanism by which Ca2+ ions actually mediate excitotoxicity is less clear [2]. One hypothesis suggests that Ca2+dependent neurotoxicity occurs following the activation of distinct signaling cascades downstream from key points of Ca2+ entry at synapses, and that triggers of these cascades are physically colocalized with specific glutamate receptors [2]. Calcium influx leads to elevated intracellular and intramitochondrial Ca2+ concentrations and lethal meta bolic derangements, which include calciumdependent activation of intracellular enzyme systems, failure of oxidative phosphorylation, and the generation of free radicals that further compromise cells by attacking proteins, lipids, and nucleic acids. Oxidative stress (production of free radicals) and lipids, particularly the fatty acid component of membrane phospholipids, producing changes in the flu idity and permeability of the cellular membranes (lipid peroxidation) [80, 84]. In addition, the conver sion of xanthine dehydrogenase to xanthine oxidase pro motes the cellular formation of toxic oxygen free radicals such as the superoxide anion, which further breaks down membrane, cytoskeletal, and nuclear structures. Apoptosis A free radical is any atom, group of atoms, or molecule with an unpaired electron in its outermost orbital [80]. Free radicals are produced in small quantities by normal cellular processes in all aerobic cells. For example, "leaks" in mitochondrial electron transport allow oxygen to accept single electrons, forming superoxide (O2-). They can react with and damage proteins, nucleic acids, lipids, and other classes of molecules such as the extracellular matrix glycosaminoglycans. The sulfurcontaining amino acids and the polyunsaturated fatty acids (found in high concentrations in the brain) are particularly vulnerable. Fortunately, cells possess appro priate defense mechanisms in the form of free radical scavengers and enzymes which metabolize free radicals or their precursors. During severe brain ischemia, insufficient oxygen is available to accept electrons passed along the mitochon drial electron transport chain, leading to eventual reduc tion ("electron saturation") of the components of this system. Like other free radicals, the free radicals that are elevated in cerebral ischemia react with and damage proteins, nucleic acids, Apoptosis is a mode of programmed cell death in which the cell synthesizes proteins and plays an active role in its own demise. For example, during normal human embryonic development, apoptosis results in the loss of the inter digital webs required for normal formation of the fingers and toes. The normal turnover of cells in the intestinal villi is also apoptotic, as is the turnover of nor mal lymphocytes. Indeed, inhibition of the apoptotic death of lymphocytes may lead to Bcell lymphoma. Although necrosis is the predominant mechanism of cell death after stroke (mediated by excitotoxicity, as described earlier), growing evidence indicates that hypoxic/ischemic cell death also continues to some extent hours to days after the onset of ischemia, particularly within the periinfarct zone or ischemic penumbra, by apoptosis as a consequence of a genetically regulated program that allows cells to die with minimal inflammation or release of genetic material. Active caspases kill cells by cleaving critical cell repair and home ostatic proteins as well as cytoskeletal proteins [82]. In other words, they dismantle multiple cell processes in the 602 13 Specific treatment of acute ischemic stroke cytoplasm and nucleus to promote cell death by suicidal mechanisms resembling apoptosis [81]. Necrosis may proceed by analogous programmed path ways recently revealed in the nematode Caenorhabditis elegans [90]. However, treatment with matrix metalloproteinase inhibitors has not been shown to protect the brain. Indeed, a recent study suggested that such inhibitors might contribute to brain damage [94, 95]. Inflammation Although the original model of excitotoxicity empha sizes calcium influx through glutamate receptorcoupled ion channels, ionic imbalance (and cell death) may also proceed via other routes [81]. Acidosis Acidosis arises as a result of energy deprivation by sus tained tissue ischemia. It may contribute to tissue dam age and prevent or retard recovery during reoxygenation by several mechanisms: activation of novel classes of acidsensing ion channels that further perturb sodium and calcium homeostasis [91], and inhibition of mito chondrial respiration and lactate oxidation [4, 5]. After an initial transient hyperemia (up to 200% of baseline), cortical spreading depression exacerbates cellular injury and augments tissue damage by causing profound oligemia that persists for up to three days, thereby imposing an energy burden of reestablishing ionic equilibrium in hypoxic tissue [93]. Proteolysis of the neurovascular matrix by plasminogen activator and metalloproteinases is believed to be linked with hemorrhagic transformation of the brain Periinfarct depolarization Cerebral ischemia triggers an inflammatory reaction, by means of an active gene expression, within hours to days that may last up to several months [76, 96]. Several mediators are released or activated, such as adhesion molecules, proteolytic enzymes belonging to the family of metalloproteinases (including matrix met alloproteinases), and inflammatory cytokines [98, 99]. The result is infiltration of leukocytes into the brain parenchyma, and the activation of resident microglial and astroglial cells [98, 99]. The effects of inflammation are both detrimental (for example, exacerbation of edema) and potentially beneficial. Cell death occurs by a necrotic pathway characterized by either ischemic cell change or edematous cell change. The four major stages of cell death the cell death process has four major stages [78]: 1) the first stage is the induction stage, which includes several changes initiated by ischemia and reperfusion that are very likely to play major roles in cell death.
Purchase tadalafil
Examination of biological relatives who have accompanied the patient to the office may be revealing sudden erectile dysfunction causes buy discount tadalafil line, and genetic testing of the patient or affected family members may also be helpful. Gray patches, pseudocysts, and/or fine lines in the corneal epithelium are noted on examination and are best seen by using a broad oblique slit-lamp beam or with retroillumination. The bleb pattern (Bron) resembles pebbled glass and is best seen with retroillumination. Symptoms are typically related to recurrent epithelial erosions and/or blurred vision, ghosting, or monocular diplopia, and while more common in patients older than 30 years, they can occur at any age. Symptoms of recurrent erosions typically occur in the morning; however, discomfort in the morning may also occur in patients with nighttime lagophthalmos. Both eyes must be examined because evidence of the dystrophy may be found in the uninvolved eye. Unilateral dystrophic changes may be related to focal trauma rather than a dystrophy. In some cases, clinical findings may mimic corneal intraepithelial dysplasia; therefore, consideration should be given to submitting removed material for histologic study. The epithelial cells contain an electron-dense accumulation of fibrogranular material surrounded by tangles of cytoplasmic filaments ("peculiar substance"). There are frequent mitoses and a thickened basement membrane with projections into the basal epithelium; the basal epithelial cells have increased levels of glycogen. On confocal microscopy, hyporeflective areas ranging from 40 to 150 m in diameter are seen in the basal epithelium and contain potential reflective spots. Tiny intraepithelial vesicles are seen-most easily with retroillumination-extending to the limbus. Symptoms are usually limited to mild ocular irritation and a slight decrease in vision. The Stocker-Holt variant, which maps to a different gene, may have an earlier onset and demonstrate more severe signs and symptoms. Retroillumination shows sectorial, densely crowded, clear microcysts in a feathery shape. On immunohistochemistry, there is scattered staining on Ki67 without evidence of increased mitotic activity. In Meesmann dystrophy, such band-shaped, feathery lesions do not exist, and the corneal involvement is more diffuse. Also, the intraepithelial cysts of Meesmann dystrophy are not as densely crowded as in Lisch dystrophy but are isolated, with clear spaces between the cysts. Lisch corneal dystrophy is genetically distinct from Meesmann corneal dystrophy and maps to xp22. Treatment of Lisch corneal dystrophy with photorefractive keratectomy and mitomycin C. Disruption of epithelial tight junctions leads to abnormally high epithelial permeability. Confocal microscopy shows irregular, elongated epithelial cells with large accumulations of brightly reflective material noted within or beneath the epithelium and within the anterior stroma. Amyloid deposition is noted in the basal epithelial layer on transmission electron microscopy. There is a significant decrease in vision, with photophobia, irritation, and tearing, as well as progression of protruding subepithelial lesions. Soft contact lenses are effective in reducing the abnormal epithelial permeability to decrease recurrences. A spectrum of clinical manifestations of gelatinous drop-like corneal dystrophy in Japan. A, Confocal microscopy reveals highly reflective material without shadows in the basal epithelium. Symptoms often begin in the first or second decade of life with painful recurrent epithelial erosions. Anterior scarring and associated surface irregularity both contribute to reduced vision. The Bowman layer is replaced with fibrocellular material in a pathognomonic wavy, "sawtoothed" pattern. On confocal microscopy, distinct deposits are found in the epithelium and Bowman layer. B, Anterior segment optical coherence tomography shows typical hyperreflective deposits in the characteristic sawtoothed configuration at the level of the Bowman layer. C, Subepithelial reticular (honeycomb) opacities of Thiel-Behnke corneal dystrophy. Epithelial atrophy and disruption, with degeneration of basal epithelial cells, and focal thinning or absence of the Bowman layer increase progressively with age. An eosinophilic layer develops between the epithelial basement membrane and Bowman layer, with stromal deposition of the amyloid substance distorting the corneal lamellar architecture. Amyloid stains rose to orange-red with Congo red dye and metachromatically with crystal violet dye (Table 7-4). It exhibits dichroism (shift from red-orange to apple green in response to a single rotating polarizing filter) and birefringence. The spectrum of corneal changes is broad, and the classic branching lattice lines may not be present in all cases. Subtle refractile lines, central and subepithelial ovoid white dots, and diffuse anterior stromal haze appear early in life and, in a corneal graft, these may be the first signs of recurrence. These lines start centrally and superficially and spread centrifugally, becoming deeper. The stroma can take on a "groundglass" appearance, but the peripheral cornea typically remains clear. Epithelial erosions recur often and may occur as early as the first decade of life. Stromal haze and epithelial surface irregularity may decrease vision, typically in the fourth decade. Familial amyloidosis with lattice corneal changes (formerly lattice corneal dystrophy type 2) is no longer considered a dystrophy (see Chapter 8). An electron-dense material made up of rod-shaped bodies immersed in an amorphous matrix is seen on electron microscopy. Histochemically, the deposits are noncollagenous protein that may derive from the corneal epithelium and/or keratocytes. The lesions are separated by clear spaces early in the disease process but later become more confluent. The dystrophy is slowly progressive, with most patients maintaining good vision and visual acuity, and only rarely dropping to 20/200 after age 50 years. Recurrent erosions occur and vision decreases as the opacities become more confluent. Recurrent erosions may be treated with therapeutic contact lenses and superficial keratectomy. The disease may recur in the graft after several years, presenting as fine subepithelial opacities anteriorly and peripherally in contrast to the original presentation. Laser refractive surgery should be avoided in patients with granular dystrophy because of the risk of haze. The deposits appear as rod-shaped bodies on electron microscopy; randomly aligned fibrils of amyloid are also seen. Stellate-shaped opacities with intervening clear spaces can be seen in direct illumination (left) and in retroillumination (right). Determination of treatment strategies for granular corneal dystrophy type 2 using Fourier-domain optical coherence tomography. They accumulate in the endoplasmic reticulum and not in lysosomal vacuoles, as seen in systemic mucopolysaccharidoses. On confocal microscopy, blurred accumulations of light-reflective material are seen in the anterior corneal stroma. Unlike most corneal dystrophies, it has an autosomal recessive inheritance, involves the entire corneal stroma and periphery, and may involve the corneal endothelium. Patients with macular dystrophy initially show superficial, irregular, whitish, flecklike opacities that evolve into focal, gray-white, superficial stromal opacities with intervening haze.
Syndromes
- Restlessness, irritability
- Rapid heart rate
- Congenital torticollis
- You have symptoms with the canker sore such as fever, diarrhea, headache, or skin rash.
- Shortness of breath
- Narcolepsy
Order discount tadalafil on line
Following surgery patients were kept at bedrest in the hospital erectile dysfunction treatment boots buy tadalafil online, without a brace, for 2 months postoperatively. This study was a landmark report because it provided a stillused surgical approach/technique for L5-S1 isthmic spondylolisthesis in a time of noninstrumented fusions. The primary advantage of this surgical technique in the 1960s and 1970s was preservation of midline structures to prevent further slippage and to decrease blood loss, with a high fusion rate. However, several decades later the Wiltse approach has shown benefit in preventing approach-related muscle atrophy. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: A technique and feasibility study. First, the authors aimed to expand on their prior work1,2 detailing the anterior approach to the cervical spine for intervertebral disc removal and fusion. Finally, the authors wanted to share detailed results for the first 14 patients in whom the procedure was employed. In addition to these main objectives, they shared details regarding their procedure for localization of the operative level and postoperative protocol. Prior to utilizing the procedure on humans, the authors employed eight dogs to demonstrate safety and feasibility. Study Design Retrospective review of patients who underwent anterior removal of cervical intervertebral discs and fusion. Sample Size Fourteen patients between the ages of 25 and 50 years (average 38 years). Follow-Up At the time of publication, follow-up ranged from 15 to 36 months (average 24 months). Inclusion/Exclusion Criteria Operative intervention was indicated in patients whose pain and disability failed to improve with conservative modalities. The authors acknowledged that posterior laminectomy is often effective in the setting of posterior osteophytes and/or acute disc protrusions. To relieve nerve-root compression in the foramen, removal of the articular facet, in addition to laminectomy, may be required. This procedure, especially when employed bilaterally, can lead to cervical instability. Furthermore, removal of a degenerated but nonprolapsed cervical disc is not feasible via the posterior approach. As such, the authors state that disc removal and fusion of the cervical spine is indicated in patients whose symptoms are due to osteoarthritic spurs impinging on nerve roots in the intervertebral foramina, especially if their symptoms are bilateral or caused by disc degeneration or subluxation. Thirteen patients had clinical symptoms of cervical nerve root irritation or compression. Ten of these patients had intervertebral-disc degeneration with accompanying osteophyte formation on imaging. Three patients had disc degeneration alone without visible osteophyte formation or significant disc space narrowing. One patient had cervical subluxation with long-tract signs due to spinal cord involvement. Intervention or Treatment Received Prior to the operative intervention, the authors utilized clinical and radiographic findings to identify the correct operative levels. The authors preferred intranasal intubation in an effort to avoid the neck extension required to achieve mouth intubation. At the time, placing 20 pounds of cervical traction prior to incision was common practice at Johns Hopkins Hospital. The authors utilized an 8 to 10 cm transverse incision left of the midline and about three fingerbreadths above the clavicle. The sternocleidomastoid muscle was retracted laterally, while the strap muscles were retracted medially and inferiorly. Next, the carotid sheath was identified with subsequent palpation of the carotid pulse. A vertical incision was then made through the paratracheal fascia medial and parallel to the carotid artery. Using their fingers, the authors spread the areolar soft tissue between the central structures (thyroid, esophagus, trachea) and the carotid sheath laterally. After careful placement of retractors, the authors identified the midline of the underlying bony structures and made a vertical incision in the prevertebral fascia. After placing a spinal needle in the suspected disc space, a lateral radiograph was obtained to confirm the intervertebral level. Large anterior osteophytes were partially removed to allow access to the disc space, but an effort was made to preserve the superior and inferior cortical bone edges, enabling the bone graft to be posteriorly countersunk. In this series, the exposed intervertebral space accepted a block of bone 10 to 15 mm high, 10 to 15 mm wide, and 10 to 15 mm deep. Using an osteotome, vertical cuts, 2 cm deep, roughly 2 cm apart were made at the top of the crest. The horseshoe-shaped piece of bone consisted of cancellous bone surrounded by three sides of cortical bone. The bone graft was trimmed and positioned inside the intervertebral space such that the cancellous top and bottom surfaces were in contact with the previously exposed cancellous surfaces of the endplates. After widening the intervertebral space, the bone graft was tapped into position and countersunk. Immobilization of the neck was not utilized immediately following soft tissue closure. Six patients had the surgery performed at two levels, and the remaining seven patients had a single-level procedure. The intervertebral disc between the fifth and sixth cervical vertebrae was most commonly removed (11), followed by the disc between the sixth and seventh cervical vertebrae (7). Results Fusion was defined as a visible bone bridge between two vertebral bodies on imaging as well as an absence of motion between the vertebral bodies during dynamic radiographs. Of the 22 intervertebral discs operated on, 18 eventually showed a bone bridge and 21 lacked motion (three fibrous unions). Nine patients were considered to have an excellent result: all preoperative symptoms relieved. One patient had a poor initial result: symptoms unchanged from preoperative status. The authors observed that neck and occipital pain was often relieved immediately after surgery. Of note, this patient had a similar complication following previous thyroid surgery, which was attributed to sensitivity to intubation tubing. It is important to note that the patient who initially had a poor result was eventually reclassified as fair following an additional procedure. After fusion of the previous operative levels was noted 10 months postoperatively, she underwent multiple bilateral posterior foraminotomies and partial facetectomies, a procedure that would have resulted in instability in the absence of anterior fusion. Following the second procedure, she experienced symptom relief and was able to return to work part time. However, given the uncertainty and technical difficulty associated with such a new procedure, the authors likely opted for a small initial patient series. Average patient follow-up was 24 months, which allowed for reasonable monitoring of postoperative pain and function. In 1955, Robinson and Smith first described the procedure for cervical intervertebral disc removal and fusion via the anterior approach. The authors provided some conceptual support for this new procedure and early clinical data regarding eight patients. The surgical exposure was practiced on dogs prior to the first human procedure in 1954. Their surgical exposure was derived from a method used to expose esophageal diverticula. In the year after devising the operative technique, Cloward operated on 47 patients, achieving excellent clinical results. Of the 47 patients he operated on, 42 had complete resolution of their preoperative symptoms.
Buy tadalafil line
There were no restrictions on duration of symptoms or prior nonoperative management erectile dysfunction and diabetes discount 5 mg tadalafil with visa. Patients received surgical decompression of the cervical spinal cord combined with instrumented fusion. The method of decompression was determined by the attending surgeon and was either an anterior, posterior, or circumferential approach. The number of vertebral segments decompressed and fused were determined by the surgeon as well. Intervention Results Patient age at presentation differed significantly among the severity groups. The mean age at presentation was higher for patients with severe disease and decreased for patients with moderate and mild disease. As expected, preoperative outcomes were progressively more favorable, from severe to moderate to mild disease. Also, the number of vertebral levels decompressed differed significantly among the groups, with more extensive decompressions performed in patients with severe disease compared to those with mild or moderate disease. There were no differences among the severity groups with respect to sex, smoking status, and preoperative duration of symptoms. The complication rate did not differ among severity groups, and the most common complication was dysphagia in the early postoperative setting in 3. Indications for revision surgery included neck hematoma, deep wound infection, and graft malposition. Three patients had worsening myelopathy immediate postop; two of the three improved to baseline at 1-year follow-up. The authors mention that, from an ethical standpoint, not to operate on patients with myelopathy would not be feasible. Also, from a logistical standpoint, if a randomized controlled trial were implemented, the crossover rate from the nonoperative arm to the operative arm would undermine the randomized study design. Finally, the operations performed did not have a standardized surgical protocol and were performed by different surgeons at 12 institutions. The authors found that, based on univariate analyses, the probability of achieving a score of >16 decreased with the presence of certain symptoms, including gait dysfunction, certain clinical signs such as lower limb spasticity, positive smoking status, higher comorbidity score, more severe preoperative myelopathy, and older age. Those patients undergoing a two-stage surgery and those with longer operative durations also had a greater risk of perioperative complications. A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: Analysis of an international prospective multicenter data set of 757 subjects. A systematic review of clinical and surgical predictors of complications following surgery for degenerative cervical myelopathy. Chapter Radiographic and Pathologic Features of Spinal Involvement in Diffuse Idiopathic Skeletal Hyperostosis* Resnick D, Niwayama G. Cervical, thoracic, and lumbar radiographs of patients identified with patterns consistent with the disease were reviewed. Gross and microscopic pathology findings were described from dissection of cadaveric spines in patients with and without radiographic findings consistent with the disease. Thoracic and lumbar vertebral column from 215 cadavers were chosen at random during postmortem examination. Criteria included (a) presence of "flowing" calcification along the anterolateral aspects of at least four contiguous vertebrae, (b) relative preservation of disc height in involved areas and the absence of extensive radiographic changes of "degenerative" disc disease, and (c) absence of apophyseal or sacroiliac ankylosis. The most common radiographic abnormalities were found in the thoracic spine (96%), specifically the seventh to tenth thoracic vertebrae. They describe a consistent pattern of flowing ossification along the anterolateral aspect of the vertebral bodies, between 1 and 20 mm thick, with underlying linear radiolucency separating ossification from vertebrae. An asymmetric pattern and predilection for the right side of the thoracic spine was seen. An overall "bumpy" appearance results from increased and more anterior deposition across disc spaces between involved vertebrae. Lumbar abnormalities were thick, up to 20 mm, and most commonly occurred along the third lumbar vertebrae. Cervical abnormalities also demonstrated flowing anterior ossification between 11 and 22 mm thick, occurring most commonly on the fifth and sixth cervical vertebrae. Progression of ossification was seen in all spine segments, beginning at the anterior vertebral body and gradually elongating across adjacent disc spaces. In advanced cases, underlying linear radiolucency disappeared with merging of anterior ossification and underlying sclerotic vertebral body. Radiographic and pathologic examination of the spine was performed on all 25 cadavers. Selection of radiographs was based on previously reported patterns of ossification that differed from known pathologies, such as ankylosing spondylitis and degenerative disc disease. Oppenheimer first described this entity as spondylitis ossificans ligamentosa in 1942, based on radiographic ossification of spinal ligaments in the absence of intervertebral disc or apophyseal involvement. Demonstrates anterior nonmarginal syndesmophytes from the third to seventh cervical vertebrae. Calcification and ossification of vertebral ligaments (spondylitis ossificans ligamentosa): Roentgen study of pathogenesis and clinical significance. A controlled study of diffuse idiopathic skeletal hyperostosis: Clinical features and functional status. Diffuse idiopathic skeletal hyperostosis may give the typical postural abnormalities of advanced ankylosing spondylitis. An Research Question/Objective the role of arthrodesis and fixation in the surgical management of degenerative spondylolisthesis with spinal stenosis in the lumbar spine has been the topic of much research over the past several decades. Previous studies had demonstrated improved clinical outcomes if arthrodesis was performed with decompression at the level of listhesis. Subsequent studies advocating for the addition of spinal instrumentation to enhance arthrodesis showed improved fusion rates, but the effect on clinical outcome remained uncertain. The goal of this study was to determine whether the addition of pedicle screw instrumentation would improve the fusion rate and clinical outcome of patients undergoing posterolateral fusion after decompression for spinal stenosis in the setting of degenerative spondylolisthesis. Study Design this was a prospective randomized study that evaluated the impact of adding transpedicular fixation on patient outcomes in the surgical management of spinal stenosis with degenerative spondylolisthesis. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Sample Size Seventy-six consecutive patients with symptomatic spinal stenosis associated with degenerative spondylolisthesis at a single institution. Decompressive laminectomy and singlelevel bilateral intertransverse process arthrodesis with or without transpedicular instrumentation. The aim of this study was to investigate whether fusion surgery as an adjunct to decompression surgery resulted in better clinical outcomes than decompression alone in patients with lumbar spinal stenosis, with or without degenerative spondylolisthesis. Patients with symptomatic lumbar stenosis were recruited from October 2006 through June 2012 from seven Swedish hospitals. Prior to randomization, patients were assessed for degenerative spondylolisthesis, defined as the presence of anterolisthesis of one vertebral body of 3 mm in relation to the vertebra below. Sample Size Three hundred fifty-eight patients were assessed for eligibility, and 247 patients underwent randomization. One hundred twenty-three patients, including 67 with degenerative spondylolisthesis, were assigned to the decompression-with-fusion group, and 124 patients, including 68 with degenerative spondylolisthesis, were assigned to the decompression-alone group. Follow-Up Surveys were sent to participants before surgery and at 1, 2, and 5 years postoperatively. Exclusion criteria were spondylolysis, degenerative lumbar scoliosis, history of previous surgery for lumbar spinal stenosis or instability, stenosis not caused by degenerative change, stenosis caused by herniated disc, other spinal conditions. Intervention or Treatment Received Patients in the decompression-alone group received decompression surgery, whereas patients in the decompressionwith-fusion group received decompression with fusion. There were no significant differences between the two groups in any of the preoperative variables. Among patients with preoperative degenerative spondylolisthesis, the mean degree of vertebral slip was 7. There were also no significant differences between the two groups in the secondary functional, pain, and quality-of-life measures (Table 32. The decompression-with-fusion group had significantly greater operative time and amount of bleeding.
Cheap tadalafil 2.5mg without prescription
Risk factors for bleb-related endophthalmitis include blepharitis or conjunctivitis impotence statistics purchase tadalafil with paypal, ocular trauma, nasolacrimal duct obstruction, contact lens use, chronic bleb leak, male sex, and young age. Trabeculectomy performed at the inferior limbus is associated with an unacceptably high risk of bleb-related endophthalmitis. Patients may present with blebitis, which is characterized by mucopurulent infiltrate within the bleb, localized conjunctival hyperemia, and minimal intraocular inflammation (A). Bleb-related endophthalmitis (B) is characterized by diffuse bulbar conjunctival hyperemia, purulent material within the bleb, and anterior chamber cellular reaction; it is also sometimes characterized by hypopyon formation and marked vitritis. Aqueous leakage from a filtering bleb may occur as an early or late complication of surgery. Early-onset bleb leaks are usually related to ineffective wound closure or a conjunctival buttonhole. Late-onset leaks occur more frequently after full-thickness procedures such as posterior lip sclerectomy or after use of antifibrotic drugs. Clinical manifestations of hypotony maculopathy include decreased vision, hypotony, optic nerve and retinal edema, and radial folds of the macula. Choroidal effusions are more likely to occur in elderly patients because of increased scleral rigidity, which occurs with age and does not allow sclera to buckle under low pressure. Suprachoroidal fluid can be drained through one or more posterior full-thickness sclerotomies overlying the area of effusion, as the anterior chamber is deepened through a paracentesis. Numerous techniques have been described for managing bleb leaks, including the use of an oversize contact lens, aqueous suppressants, suture, tissue glue, autologous blood injection, and oral antibiotics from the tetracycline family. Excision of the bleb, in combination with a conjunctival graft or conjunctival advancement with or without a scleral graft, is also possible. If there is undue tension during closure, conjunctival relaxing incisions and a pedicle conjunctival flap can be created to help closure. Risk factors for bleb failure include anterior segment neovascularization, black race, aphakia, prior failed filtering procedures, uveitis, prior cataract surgery, prior vitreoretinal surgery, and young age. In eyes that do not respond to this initial therapy, transconjunctival needle revision may restore aqueous flow. Contact lenses may be difficult to fit in the presence of a filtering bleb, or the lens may ride against the bleb, causing discomfort and increasing the risk of infection. Several options can be considered for the patient who has myopia, requires a trabeculectomy, and prefers not to or cannot wear spectacles. Clear lens extraction (either before, after, or combined with trabeculectomy) is controversial. In some circumstances, hard or soft contact lens use under close supervision may be considered after trabeculectomy. Contact lens use is more often feasible in patients after tube shunt implantation than after trabeculectomy. When an initial filtering procedure is not adequate to control the glaucoma and resumption of medical therapy is not successful, revision of original surgery, a second filtering surgery at a new site, tube shunt implantation, or possibly cyclodestructive procedures may be indicated. Incidence of late-onset blebrelated complications following trabeculectomy with mitomycin. Outcomes of bleb excision and conjunctival advancement for leaking or hypotonous eyes after glaucoma filtering surgery. Combined Cataract and Trabeculectomy Both cataract and glaucoma are conditions that are more prevalent with age. It is not surprising that many patients with glaucoma eventually develop cataracts either naturally or as a result of glaucoma therapy. However, cataract surgery as a treatment of open-angle glaucoma is a topic of debate. For patients in whom glaucoma is the greatest immediate threat to vision, trabeculectomy alone is usually performed first. Several clinical challenges are common in patients with coexisting cataract and glaucoma. Medical therapy for glaucoma may create chronic miosis, and the surgeon must deal with a small pupil. The anterior chamber can be very shallow in eyes with angle closure, making cataract surgery technically difficult. In patients with pseudoexfoliation syndrome, zonular support of the lens is often fragile, and vitreous loss is therefore more common in such complicated eyes. As with all surgery, the risks, benefits, and alternatives should be discussed with the patient. Trabeculectomy may be combined with phacoemulsification, which is performed through the superior trabeculectomy incision or through a temporal clear corneal incision. As no violation of conjunctiva or sclera occurs with this procedure, standard trabeculectomy can be performed later when dictated by independent indications. The effect of phacoemulsification and combined phaco/glaucoma procedures on the intraocular pressure in open-angle glaucoma. When pupillary block is associated with a visually significant cataract, lens extraction might be considered as a primary procedure to relieve pupillary block. However, laser iridotomy can be considered as a first step to stop acute pupillary block, so that cataract surgery may be performed more safely at a later time. Phacoemulsification and goniosynechialysis in the management of unresponsive primary angle closure. Reduction in intraocular pressure after cataract extraction: the Ocular Hypertension Treatment Study. Tube Shunt Implantation There are many different types of devices that aid angle filtration by shunting aqueous to a site away from the limbus, such as the equatorial subconjunctival space. Tube shunt implantation generally involves placing a tube in the anterior chamber, in the ciliary sulcus, 214 Glaucoma or through the pars plana into the vitreous cavity. The tube is connected to an extraocular plate, which is attached to the sclera in the equatorial region of the globe, between the extraocular muscles, and in some cases tucked under the muscles; some devices employ 2 plates. Aqueous flows out through the tube and into the subconjunctival space in the region of the extraocular plate. Tube shunts can be broadly categorized as nonvalved devices, which have no flow restrictor, or valved devices, which have a flow restrictor (Table 8-2). In eyes with an existing encircling band placed for retinal detachment, a Schocket procedure can be performed. In this procedure, a silicone tube is passed from the anterior chamber and threaded into the capsule surrounding a previously placed scleral buckle (Video 8-3). Indications the devices mentioned and similar types of implants have generally been reserved for difficult glaucoma cases in which trabeculectomy has failed or is likely to fail. The 5-year follow-up Table 8-2 Tube Shunts Single Plate Surface area, mm2 Height profile, mm Plate material Flow restrictor Pediatric surface area, mm2 No 55 133 1. However, when the factors that precipitated the initial failure cannot be modified, or when it is not technically possible to repeat the trabeculectomy, implantation of a tube shunt may be the procedure of choice. In certain types of uveitis (eg, young patients with juvenile idiopathic arthritis), the success rate of trabeculectomy is low and tube shunt implantation is often the primary surgical treatment. When a complete vitrectomy has been performed, the tube can be placed through the pars plana. Many surgeons use tube shunts as a primary procedure in uncontrolled aphakic glaucoma. Special attention should be paid to any vitreous in an aphakic eye, as vitreous may occlude the tube. The use of a soft contact lens over a trabeculectomy bleb is a risk factor for bleb trauma and subsequent infection. The use of a soft contact lens following tube shunt implantation is not without risk, however, as the conjunctiva overlying the tube is more prone to erosion with contact lens use. Borderline corneal endothelial function is a relative contraindication for anterior chamber placement of a tube. Techniques Although tube shunts differ in design, the basic techniques for implantation are similar. Subsequent tube shunts can be placed in any quadrant, but the inferonasal quadrant tends to be used next for larger plate models, while the superonasal quadrant is used for smaller plate models.
Discount tadalafil 2.5 mg free shipping
With all topical ocular hypotensive medications doctor for erectile dysfunction in chennai 5 mg tadalafil otc, pregnant and breastfeeding patients should be advised to perform nasolacrimal occlusion during eyedrop instillation. In general, it is prudent to minimize the use of medications in pregnant women whenever possible. The clinician may want to consider laser trabeculoplasty or other surgical intervention in cases in which the benefits outweigh the potential risks. Use of Glaucoma Medications in Elderly Patients There are specific considerations regarding the use of glaucoma medications in elderly patients. First, elderly patients generally have greater difficulty instilling their medications than do younger patients; consequently, their adherence to the treatment regimen may be affected. Instillation difficulties may be due to tremor, poor coordination, or a comorbidity such as arthritis. Adherence will also be affected in an elderly patient with reduced mental capacity or poor memory and a complicated drug regimen, especially because this individual is most likely already taking multiple systemic medications for other ailments. Second, elderly persons have a greater susceptibility to the systemic adverse effects of glaucoma medications. The incidence and severity of systemic adverse effects may be higher with b-blockers and a2-adrenergic agonists in these patients. For example, it has been shown that a significant proportion of asymptomatic elderly patients suffer a significant, but reversible, reduction in pulmonary function with the use of b-blockers. Avoiding unsuspected respiratory side-effects of topical timolol with cardioselective or sympathomimetic agents. The use of lower-cost generic medications has been shown to improve patient adherence to medication regimens. Patient Adherence to a Medication Regimen Glaucoma medications are effective only if patients use them. The first step in improving patient adherence to a medication regimen is patient education. If patients understand the disease and the nature and benefits of treatment, adherence is increased; it is also enhanced when patients are aware of the possible adverse effects of a medication. The ophthalmologist must make sure that the patient understands the treatment regimen. If the patient requires multiple medications and doses, it may be helpful to coordinate administration with daily events, such as meals or brushing teeth. Finally, as mentioned previously, proper instillation of eyedrops, by the patient or someone else, is essential and should be confirmed by the ophthalmologist. Surgical treatment for glaucoma is usually undertaken when medical therapy is not appropriate, not tolerated, not effective, or not properly used by a particular patient, and the glaucoma remains uncontrolled with either documented progressive damage or a high risk of further damage. Laser surgery is used as primary, adjunctive, or prophylactic treatment in various types of glaucoma. The clinician must exercise caution when recommending incisional surgery because potential adverse effects (infections, hypotony, cataracts) can result in vision loss. However, this finding did not translate to better visual field stabilization on average because subjects who received initial surgical treatment had a higher risk of cataract in the long term. However, the 9-year follow-up data showed that initial surgery led to less visual field progression than did initial medical therapy in subjects with advanced visual field loss at baseline, whereas subjects with diabetes mellitus had more visual field loss over time if treated initially with surgery. Surgical treatment can be accelerated in patients with advanced visual field loss at presentation. Each of the many possible procedures is appropriate in specific conditions and clinical situations. Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Visual field progression in the Collaborative Initial Glaucoma Treatment Study the impact of treatment and other baseline factors. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Particular attention must be paid to visual field examination, gonioscopy, and optic nerve evaluation; the trabecular meshwork must be visible on gonioscopy. The degree of pigmentation in the angle determines the power setting: the more pigmented the trabecular meshwork, the less energy required. If a large bubble appears, the power is reduced and titrated to achieve the proper effect. The adjunctive use of topical apraclonidine or brimonidine has been shown to blunt postoperative pressure elevation. Additional laser treatment may be helpful in some patients, especially if the entire angle has not been treated previously. Also, the effect after re-treatment may not be as long lasting as that of the first treatment. Selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with open-angle glaucoma: a systematic review and metaanalysis. For example, the diagnosis of plateau iris syndrome is confirmed only when a patent iridotomy fails to change the peripheral iris configuration and relieve angle closure. Contraindications A laser iridotomy is not recommended in the case of a completely flat anterior chamber because of the risk of corneal endothelial damage. Angle closure from mechanisms other than pupillary block also does not require iridotomy (ie, neovascular glaucoma and iridocorneal endothelial syndrome). An eye with active rubeosis iridis may bleed and develop a large hyphema following laser iridotomy. Laser iridotomy or surgical iridectomy breaks the pupillary block and results in opening of the entire peripheral angle (bottom) if no permanent peripheral anterior synechiae are present. Preoperative considerations In acute angle closure, performing laser iridotomy is often difficult due to the cloudy cornea, shallow chamber, and engorged iris that are present in this condition. Corneal edema may be improved prior to laser iridotomy by pretreatment with topical glycerin. In prophylactic iridotomies, pretreatment with pilocarpine may be helpful by stretching and thinning the iris. The patient should be asked about anticoagulants, as their use increases the risk of hyphema. The argon laser alone can be used for performing iridotomy in most eyes, but very dark and very light irides present technical challenges. There are variations in technique, and iris color dictates which technique is chosen. Often, compression of the eye with the laser lens will provide a tamponade for the vessel, thereby slowing bleeding until coagulation can occur. In rare cases when this does not work, it may be helpful to use an argon laser to coagulate the vessel. Topical corticosteroids are usually prescribed for 1 week, longer if necessary, as prophylaxis against inflammation. The effects of iridotomy size and position on symptoms following laser peripheral iridotomy. Dysphotopsia after temporal versus superior laser peripheral iridotomy: a prospective randomized paired eye trial. Laser Gonioplasty, or Peripheral Iridoplasty Indications Gonioplasty, or iridoplasty, is a technique to deepen the angle. It is primarily used in persistent appositional angle-closure glaucoma after successful iridotomy in cases of plateau iris syndrome, nanophthalmos, and lens-related angle-closure. It is also used in cases of acute angle closure in which a shallow chamber precludes iridotomy.
Discount 2.5mg tadalafil fast delivery
Straws are available with a nonreturn valve if the patient cannot suck using a conventional one because of facial weakness erectile dysfunction recreational drugs buy discount tadalafil online, but has an intact swallow fasteners [439]. If patients still cannot dress themselves, then care assistants or a member of the family will be needed to help. A hemiplegic patient may be independent eating sandwiches but dependent for eating a steak. Some of the more common feeding problems and the aids that can help are shown in Table 11. Cognitive and visuospatial problems may put patients and others living in the same building in danger from lacerations, burns, fires, gas poisoning, explosions, and flooding. Again, problems are easily identified by talking to or observing the patient in the kitchen. An occupational therapist may be able to teach patients alternative methods of performing certain tasks and for many with physical rather than cognitive problems there is a large variety of kitchen aids available to help with specific difficulties (Table 11. Patients with cognitive problems may be helped by things such as electric kettles which turn themselves off and gas detection systems which interrupt the supply automatically, but for those with severe cognitive problems it may be necessary to ban them from the kitchen or to remove cookers. Where patients cannot prepare food for themselves, it is obviously important to ensure delivery of prepared meals to their homes, or to have a care assistant who can prepare meals. One year after a firsteverinalifetime stroke, about 20% of surviving patients need some help from another person to feed (see Table 11. Dependency in feeding is one of the most demeaning problems because of its associations with infancy. Impaired function of the arm and hand is the most common cause, although problems with sitting balance, facial weakness, and visuospatial and sensory function may all be important as well. Most problems can be identified simply by talking to the patient and/or carer, but often it is useful for a trained observer, usually an occupational therapist, to assess the patient. For instance, it is important that any dentures are in good working order and in the mouth rather than in a glass of water on the bedside table. Also that the patient is sitting at a table on a chair of appropriate height and that the knife is sharp. Solutions Cannot open cans with one functional hand Cannot open bottles with one functional hand Cannot cut up or peel ingredients with one functional hand Wallmounted (electric) tin opener A bottle or jar stabilizer to fix the bottles to work surface A plate or board with spikes on which to impale the item to be cut 11. This section will address some of the social factors that are often of greatest concern to patients and their carers. Some patients with complex or worsening disability may not, if admitted to hospital, be able to return to their own home. Some stroke units have predischarge apartments in the hospital which allow the team and the patient to assess under supervision how well the patient copes. Thus, if one is going to avoid unnecessary delays in hospital, one has to make a decision before the patient has achieved their optimal functional status. After all, given unlimited funds, it is almost always possible to maintain even the most severely disabled patient at home. The final decision is often a result of negotiation between the patient, carer, and team members. For instance, patients with visuospatial or cognitive problems may not appreciate the likely problems which will face their carers after discharge. For these sorts of reasons it is not always possible to fulfil the wishes of both patient and carer. Options for alternative accommodation, and the availability of support in the community, vary from place to place, country to country, and from time to time. In general, a range of accommodation is needed offering a variety of levels of support and supervision to meet the needs of individual patients. Estmates of the proportion who return to work have varied widely due mainly to methodological factors [441]. It is also likely that the local arrangements for paying sickness benefit will influence whether patients return to work, and the timing of their return. Of course, many patients who are approaching retirement age may not want to return to work anyway. This may involve one or more visits home with the patient and any carer to establish exactly what the practical problems are. If a short visit is not enough, then home visits (with the potential for "round the clock" supervision) for a few days and nights can be useful to predict how the patient and carer will cope in the longer term. Some employers have occupational health departments which can provide further specialist advice on their own specific regulations covering return to work, and on any alterations to the working environment or the job itself which would facilitate this. They are often under the misconception that patients should rest after a stroke and that physical activity will bring on another stroke [443]. This misconception may have made them rule out, inappropriately, the possibility of return to work. Many patients and their carers are under the misconception that exercise, hard work, or stress will bring on another stroke. Prolonged immobility on longhaul flights with the attendant risk of venous thromboembolism, and the effect of altitude (most commercial airplanes are pressurized to a level equivalent to an altitude of about 7000 feet) on the brain, are two issues that need to be considered. In all patients, but especially those who have had an ischemic stroke associated with a patent foramen ovale, it may be wise to emphasize simple measures to reduce the risk of venous thromboembolism, such as adequate hydration and avoiding prolonged immobility [448]. In giving advice one also needs to take into account: Patients may require specific occupational therapy to improve the physical skills required for particular jobs, and/or retraining to change employment. And they may find that although they can perform the physical aspects of their work, their concentration may be impaired. In many countries, special schemes are available to provide employment for disabled people. Many patients who have a stroke while on holiday are repatriated by air within a week or two without apparent illeffects. But after stroke, libido, coital frequency, and satisfaction are reduced among both patients and their partners [449]. This reduction in activity is due to both physical and psychosocial factors, the latter probably being of greater importance (Table 11. Reduced sexual activity may contribute to a worsening emotional relationship with their partner. A patient and their partner may believe that reduced satisfaction with their sexual relationship is an inevitable consequence of stroke. Although we often feel embarrassed about talking to people about these aspects of their lives, it is important that sexual problems are discussed. The psychological problems contributing to sexual dysfunction are often the most difficult to sort out. Sometimes patients and their partners simply need to be reassured that sexual activity, like any other physical activity, will not precipitate Twothirds of stroke patients are retired from employment. Restriction in leisure activities may be the result of physical or cognitive impairments but may also be caused by psychological factors and even fear that an activity may bring on a further stroke. Many disabled stroke patients are unable to continue with their normal leisure activities and do not take up new ones that are within their abilities [444]. Reduction in leisure activities will exacerbate social isolation, lower mood, and adversely affect relationships with carers. The level of social activities, including leisure, can be measured using the Frenchay Activities Index; however, the Nottingham Leisure Questionnaire has been developed specifically for this purpose [445, 446]. Source: Photographs by Renzo Mazzolini for the Chest Heart and Stroke Association, Scotland. Verbal information may usefully be supplemented by leaflets supplied by charities and patient organizations, which include advice for patients and carers. We encourage patients to resume sexual activity as soon as they wish after a stroke. One exception might be a patient with a recent rupture of an aneurysm which has not for some reason been coiled or clipped. One might imagine that the increase in blood pressure associated with orgasm could cause a rebleed. Unfortunately, a stroke can put tremendous strains on a relationship that are more difficult to manage.