Cheap ventolin 100mcg free shipping
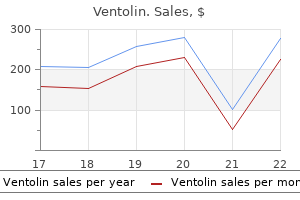
Entrapment in this region may be a consequence of chronic degenerative change asthma definition vintage discount 100mcg ventolin fast delivery, but may also occur as a complication of breast surgery or shoulder surgery. Some authorities have interpreted distal plexus entrapments as an impingement at the pectoralis minor and so have advocated resection of the pectoralis minor muscle, usually from an anterior deltopectoral groove or an axillary approach. A related problem that has been difficult to document properly in the past is axillary nerve entrapment. Unfortunately, this set of findings is sometimes mistaken for the consequence of a "rotator cuff tear," leading to unnecessary and unsuccessful rotator cuff surgery. If the pathology can be confirmed, it is often possible to treat the axillary nerve entrapment with a transaxillary neuroplasty, which is a relatively small procedure with rapid postoperative recovery. A, Finger localization is used to identify the location on the skin of optimal image slice and entry point for access (arrow). B-D, A titanium Lufkin needle (arrows in B, C, and D) is advanced to a position adjacent to the area of the axillary nerve, which was hyperintense on the neurography study. Imaging in the open scanner is by fast low-angle shot (Flash) T1-weighted sequences, which take about 10 seconds to acquire. The needle causes minimal artifact and appears as a black signal void in the image. When an autoimmune neuritis is suspected, a full immunologic work-up should be carried out. Treatment with immune-suppressant medications such as montelukast, cyclosporine, or etanercept can prove to be necessary in individual cases in which an autoimmune neuritis becomes the leading diagnosis. Operations such as supraclavicular scalenectomy or transaxillary neuroplasty are less invasive and may have lower surgical risks than transaxillary first rib resection. A-C, Image findings in patients with painless pure motor weakness of hand intrinsic muscles with no sensory findings (Gilliatt-Sumner hand). There is hyperintensity and swelling in the elements of the lower trunk without mechanical deformation or other evidence of mechanical entrapment (arrows). Surgical treatment is unlikely to be effective, and an inflammatory or vascular etiology is suspected. Note hyperintensity without any increase in caliber or any distortion in the course of the brachial plexus elements. A, In the coronal image, the arrow indicates a darkened area caused by the injectate within the anterior scalene muscle. B, In the axial image, the titanium needle is seen passing into the anterior scalene muscle. The injectate has expanded the muscle; however, the failure of injectate to flow into the more posterior portions of the muscle suggests fibrosis within the muscle. A, the titanium needle is advanced into the anterior aspect of the anterior scalene muscle (arrows). B, Injectate has been deposited in the anterolateral portion of the anterior scalene muscle (arrow) and the needle has been advanced to the deep surface of the muscle. C, the needle has been repositioned to advance into the deep aspect of the middle scalene muscle (arrows). D, Hypointense signal demonstrates the deposition of injectate within the deep portion of the middle scalene muscle (arrow). It is immediately posterior to the internal jugular vein and carotid artery, but also immediately anterior to the brachial plexus. Optimal effect requires that the needle be centrally placed in the muscle while medication is slowly injected, allowing it to spread along the longitudinal extent of the muscle. If the anesthetic injected is limited to the scalene muscle, then this will have no effect on cervical spinal pathology. However, it can completely relieve the pain symptoms of a scalene syndrome in the short term, often resulting in permanent relief without any requirement for surgery. It is also possible to accomplish this injection reliably with ultrasound33 or computed tomographic guidance. The role of the hyaluronidase is twofold: it is capable of dissolving hyaluronate polymer scarring that commonly entraps nerves, and is also capable of improving the distribution of an injected medication beyond the immediate site of introduction. Distal plexus and axillary nerve entrapments can also be resolved in many cases with hyaluronidase. Bupivacaine has some mild myotoxicity,57-59 so that there is an effect similar to that of botulinum toxin that can lead to muscle relaxation persisting beyond the duration of the usual anesthetic effect on nerves. A detailed discussion of surgical methods for transaxillary first rib resection, supraclavicular approach for scalene resection, and axillary approach for neuroplasty of the distal brachial plexus is available in the online version of this chapter at ExpertConsult. Studies of image diagnosis outcomes and formal outcome studies are also discussed. Recurrence rates are low overall and should not be considered as a reason to avoid neuroplasty surgery. Magnetic resonance neurography for the evaluation of peripheral nerve, brachial plexus, and nerve root disorders. Selective botulinum chemodenervation of the scalene muscles for treatment of neurogenic thoracic outlet syndrome. Magnetic resonance neurography- surgical correlation of neurologic thoracic outlet syndrome. Considerable outcome data are available showing that surgical treatments are highly effective for the patient when compared with the benchmark provided by analogous assessments of the efficacy of spine treatments for spinal conditions. This is similar only to the situation in piriformis muscle syndromes affecting the nerve elements in the sciatic notch (see Chapter 251). Surgical neuroplasty procedures have the principal advantage of allowing for fine manipulation around the nerve elements under close direct vision in a limited field of view. However, as long as there is uncertainty about the actual location of the neurogenic pain generator, this sort of targeted approach bears the risk of missing the actual pathology. Consequently, successful identification of the specific location of the pathology is a critical step to safe, effective surgical management. First rib resection is undoubtedly the best treatment for entrapment of the midplexus between the first rib and clavicle. Comparative analysis of neuroplasty versus first rib resection for scalene syndromes ideally should consider long-term outcome and note the complications associated with first rib resection, such as major nerve laceration, lung puncture, chyle duct leakage, and worsening of the condition from incomplete bone resection,8,65 as well as high rates of early recurrence after rib resection. A, the patient can be prepped and draped with the arm outstretched to prepare for the axillary second incision. During the first, supraclavicular portion of the operation, the arm is then adducted. The arm is in a clear fluoroscopy drape so that the hand and arm can be examined during nerve stimulation if necessary. B, the exposure after removal of the anterior scalene muscle as well as removal of middle scalene components that cross the lower trunk: the upper trunk (ut) is at the lateral margin, the internal jugular (ij) is at the medial margin, and the subclavian artery (sca) forms the inferior margin of the exposure. Also note the middle trunk (mt), lower trunk (lt), and transverse cervical artery (tca). The incision begins 2 cm from the midline and extends laterally for no more than 4 to 5 cm. If the incision extends further lateral to this, it is likely that small supraclavicular cutaneous nerve branches will be cut, producing numbness on the chest below the incision, a minor but annoying postoperative problem. The best cosmetic result can be obtained if the incision curves to follow the valley of a skin line and stays well above the clavicle. The surgeon should keep in mind that the position of the skin over the clavicle varies with head and neck position, so the chosen skin line should be close to 2 cm above the level of the clavicle. After the initial incision, the platysma is cut parallel to the skin incision and blunt dissection is used to create an exposure between the sternal and clavicular heads of the sternocleidomastoid muscles. The medial surface of the scalene fat pad is then carefully mobilized off of the jugular vein. Ideally the medial retractor blade protects and retracts the internal jugular vein, the inferior retractor blade retracts and protects the chylous and lymphatic structures and other traversing small vessels, and the superior blade protects and retracts the nerve to the omohyoid muscle. As dissection through the fat pad proceeds, electrodiagnostic stimulation is used to search for the location of the phrenic nerve where it lies on the surface of the anterior scalene Neuroplasty Approaches There are two important approaches for lysis of adhesions in the brachial plexus: supraclavicular and transaxillary. The supraclavicular approach provides good access to all neurological components proximal to the clavicle, whereas the transaxillary approach is useful for entrapments occurring between the clavicle and the point of entrance of the neurovascular bundle into the arm at the axilla.
Buy ventolin discount
However asthma treatment prednisone buy ventolin 100mcg without prescription, because the side effects from unrestricted delivery of radiation to large volumes of normal tissue would be catastrophic, a balance must be struck between efficacy and toxicity and achieve a "therapeutic window. Radiation tolerance, in turn, is a function of multiple factors including total dose, dose per fraction, frequency of administration, volume of tissue irradiated, anatomic site, tissue type, comorbid conditions such as hypertension and diabetes, preexisting functional deficits, the underlying host genetic milieu, and (controversially) chronobiologic variables. The "radioablative" effect is a combination of tumor cell killing and vascular obliteration engendered by the single high dose of radiation. Fractionation of the radiation dose, in contrast, provides a means of augmenting the dose while attempting to limit detrimental effects on adjacent normal tissue by taking advantage of inherent repair differences between normal and neoplastic tissue, as well as allowing tumor exposure to radiation at various phases of sensitivity and oxygenation status. The fractionated approach also allows reoxygenation of hypoxic tumor regions between fractions, providing improved efficacy through oxygen fixation of radiation damage. Composite radiation isodose distribution for a left parieto-occipital glioblastoma multiforme treated with three-dimensional conformal radiation therapy. Posteroanterior, lateral, and vertex beams are shown; the orange line represents the 60-Gy dose region. The abnormal T2 region is defined by the red line; the red-shaded region is T2 plus 2-cm expansion (initial treatment volume). The contrast-enhancing region is defined by the light blue line; the yellow-shaded region represents T1 plus 2. Early research confirmed the benefit of three-dimensional treatment planning in terms of the ability to reduce the volume of brain receiving full-dose treatment by 30% with non-axial techniques when compared with conventional parallel-opposed orientations. This approach results in highly shaped radiation dose distributions especially evident in concave or convex target volumes, which is of significance when tumors are in close proximity to the optic apparatus, vestibulocochlear structures, hypothalamic-pituitary axis, hippocampus, and brainstem. Bony landmarks for the intracranial contents include the calvaria, cribriform plate, and bases of the middle and posterior cranial fossae. Inadequate attention to bony anatomic landmarks and appropriate margins as defined earlier can lead to regional underdosing, and isolated relapses within the inferior frontal lobes, especially near the cribriform plate, or within the posterior fossa have been reported. Cataract development and injury to the lacrimal gland appear to be minimized by appropriate design. An additional advantage in the cranium, because of its spheroidal geometry, is access to numerous beam entry points, which allows improved dose conformality. This delay is primarily to allow tissue and wound healing, particularly at the skin surface. The lavender-shaded region represents the target volume surrounded by labeled isodose lines. Charged Particles Charged-particle radiation is a specific type of external beam radiation that delivers charged particles (most commonly protons) rather than photons. Charged particles have the inherent advantage of depositing most of the dose at a specific depth within a very narrow range that depends on the initial energy, thus avoiding the typical exit dose present in photon therapy. Avoidance of the exit dose can decrease the integral radiation dose significantly. Conventional proton therapy, referred to as double scatter, as used for the coverage of larger volumes, typically requires the proton beams to be modified by passive range modulators to disperse the Bragg peak and broaden deposition of the dose, which therefore results in an increase in dose within the entry path of the beam. More modern techniques, such as pencil beam scanning, allow for significant reduction of unnecessary radiation dose both in the entry beam paths and in the lateral directions, thereby considerably minimizing integral dose, and more important, complex targets can be treated with much greater ease. Therefore, although this form of radiation is biologically more effective in terms of tumor cytotoxicity, the repair of sublethal damage in normal tissue is simultaneously diminished, and therefore there is risk that the therapeutic window might actually become smaller if adequate measures are not undertaken to dramatically diminish the dose to and volume of normal tissue irradiated. MedicalManagement Older data from the 1970s suggest that the median survival time of untreated patients with brain metastases was approximately 1 month. As a consequence, measures to decrease vasogenic edema are commonly used in the initial management of patients with metastatic brain tumors, and they provide relief of symptoms in most patients. These trials were primarily conducted in the 1970s and focused on identifying the appropriate schedule and dose. As a consequence, this schedule has become the most commonly used fractionation scheme for patients with brain metastases treated in the United States over the past few decades. In contrast, metastatic tumors to the brain are a commonly encountered clinical situation, and patients have even poorer outcomes than those with primary brain tumors. Brain Metastases the exact incidence of brain metastases remains unclear because of coding issues in cancer databases. Estimated rates depend on whether the incidence is calculated from autopsy data, clinical studies, tumor registries, hospital records, or other sources. Less commonly, primary tumors of the gastrointestinal tract and genitourinary system, lymphomas, sarcomas, and prostate cancer also metastasize to the brain. In terms of diseasespecific risk, melanoma has the greatest likelihood of metastasizing to the brain. The overall incidence of brain metastases is probably increasing because of the combination of better diagnostic techniques and small gains in systemic therapy. Improved systemic therapeutic options have altered the conventional disease course such that patients with primary cancers live longer. With longer survival, asymptomatic micrometastatic disease in the brain is more likely to become overt, thereby increasing the incidence. Furthermore, the brain has traditionally been thought to represent a sanctuary site by not permitting penetration of most cytotoxic chemotherapeutic agents when the blood-brain barrier is intact. Effective eradication of systemic micrometastatic disease therefore introduces the possibility of having brain-only metastatic disease remaining, which is then expressed clinically over time. Dose-ResponseRelationship There appears to be a dose-response relationship between radiation dose and local control. This trial demonstrated a significant advantage in survival and neurological improvement with higher doses, thus suggesting that intracranial disease control is related to dose and that such control actually translates into neurological improvement and a survival advantage. The matching procedure produced equivalent groups of patients and showed a significant dose effect, with 30 Gy resulting in a local response rate of 50% versus 77% for doses in the 40- to 60-Gy range. In this analysis, although local control improved from 50% to 77% by escalating the radiation dose (P =. The lack of a distinct survival advantage was a consequence of competing causes of mortality in patients with brain metastases and confirmed that local control will improve survival only in patients who are not experiencing simultaneous systemic progression. It is clear that a significant proportion of patients with brain metastases succumb to systemic disease, and therefore enhancing control of intracranial diseases is unlikely to provide a survival benefit to this group of patients. In clinical trials, whether prospective or retrospective, in which a significant majority of patients harbor considerable systemic disease that will dictate the outcome, improvement in survival from more aggressive intracranial local control is unlikely to be demonstrated. However, in clinical situations in which patient selection identifies individuals who are less likely to rapidly succumb to systemic progression and patients who are at risk for dying of intracranial disease, local control of brain metastases becomes critical. Two such randomized trials by Vecht and associates31,32 and Patchell and colleagues33 have validated this paradigm by showing improved survival in the surgical arms. This analysis suggested that patients with brain metastases could be broadly categorized into three classes with different outcomes. Even so, about one third of patients had extracranial progression by 6 months and about two thirds did by 2 years, with death as a competing risk. In a four-arm trial evaluating misonidazole, no significant survival advantage was noted. In a preplanned partition by geographic region, North American patients, in whom treatment was more prompt, were found to have a statistically significant prolongation of time to neurological progression from 8. All these patients had received at least part of their radiation course at greater than 3 Gy per fraction, a hypofractionated approach that would not fall under the current standard of care in North America. A similar series involving an overlapping patient cohort from the same institution identified rates of radiation-induced dementia of 1. Furthermore, communicating hydrocephalus was thought to contribute to the dementia, and 3 of 4 patients who underwent shunting showed symptomatic improvement. Prospective data evaluating neurocognitive function, however, have shown a more complex picture, with baseline detriment in neurocognitive function created from a confluence of factors, including the presence of brain metastases, neurosurgical interventions, chemotherapy, and other neurotoxic therapies such as steroids and anticonvulsants. This is a very frustrating experience because adequate doses of radiation cannot be delivered without significant risk to these patients. Aggressive, primary treatment interventions to provide durable local control is obviously preferable to being backed into this unfortunate situation of recurrent intracranial disease with limited treatment options. Although survival expectations are lower in patients with advanced age, benefit still seems to be derived from aggressive treatment in patients with adequate performance status. Increasingly, histopathologic distinctions are being superseded by molecular and genetic characterizations, which will take on increasing importance as the prognostic value and the ability to target these aberrations is further developed. Nevertheless, the clinical data that are available to direct management and elucidate the role of radiation are based on more traditional histopathologic features, except for anaplastic oligodendroglioma, where with the recent recognition that co-deletion of 1p19q is both a predictive and prognostic variable has led to its routine incorporation in the treatment selection strategy. Malignant or high-grade gliomas are rapidly growing tumors that tend to diffusely infiltrate the brain parenchyma, thus typically preventing complete microscopic surgical excision.
Generic ventolin 100 mcg on line
A asthma treatment homeopathy discount ventolin 100mcg overnight delivery, the plexus image extends from axilla to axilla, although this image does not follow the plexus into the proximal part of the arm. The patient had bilateral arm and hand pain with different sets of symptoms on the right and left; magnetic resonance imaging of the cervical spine yielded negative findings; and no wrist or elbow entrapment was observed on electrodiagnostic studies. This image demonstrates an exaggerated sinusoidal course (asterisk) on the right side where the plexus passes below the clavicle and over the first rib. The left side of the image shows a very different configuration at the same location (double asterisk), with some focal narrowing of the upper trunk. B, the image in A is produced by an experienced technician or physician manipulating the positions of the "X" marks until the plexus elements come into view: a process called curved reformatting. The resulting trace line documents posterior deviation of the plexus (double asterisk), which is at the location of the scalene muscle. A1 to A4, Series of oblique coronal imaging sections, each showing portions of the exiting cervical spinal nerves and proximal brachial plexus. Isolated segments of nerve elements appear at various locations, and some are difficult to identify reliably. B, An overlay maximum intensity projection, made possible because the nerves are among the brightest elements in the image. It is easy to match the dorsal root ganglia (d) with the cervical spinal nerves because of the appearance of physical continuity. Nerve hyperintensity (h) associated with motor symptoms is readily appreciated in the right C6 cervical spinal nerve because all the other elements are of obvious lower intensity. Downward distortion of the right C7 and C8 cervical spinal nerves (s) by an enlarged scalene muscle is also evident because of the assembled view of the entire proximal plexus bilaterally. By using multiplanar reformatting techniques dynamically in this way, the surgeon can directly explore the nerve anatomy rather than relying on a few preprinted outputs. Indeed, limitations in the quality of diagnostic techniques have led to ongoing disagreement about the very existence of this class of nerve entrapment syndromes. In part, these problems arise because of the difficulty in placing diagnostic electrodes for electrophysiologic studies in this region. These findings can indicate entrapment or adhesions, as well as posttraumatic effects. With time after injury or repair, the development of traumatic neuromas is readily appreciated. In patients with hereditary neuropathies, disordered distribution of interfascicular lipid can be detected. Elements of the brachial plexus appear bright and swollen but demonstrate no distinct evidence of impingement. The full length of the foraminal impingement can easily be appreciated on a neurographic image. Some types of nerve abnormality associated with lumbar spine disease are well distal to the foramen but also significantly proximal to the sciatic notch. These are very difficult to access either by injection or by physical examination. Distortion of the course of the tibial nerve by pseudoaneurysm in the popliteal fossa. The patient experienced a severe tibial nerve neuropathy immediately after knee arthroscopy. The image demonstrates that the nerve was intact but flattened and distorted by a pseudoaneurysm of the tibial artery caused by the endoscope. Imaging of the complete course of the L4 spinal nerve as it progresses into the femoral nerve has made it possible to search for abnormalities along the intra-abdominal and intrapelvic course that previously were almost impossible to diagnose. It is very reliable for demonstrating the presence of a split nerve/split muscle configuration in the setting of a possible piriformis syndrome. Reliable identification of anatomic variants of the sciatic nerve now plays a critical role in improving the safety of surgery for the release of pelvic sciatic nerve entrapment. Image of the dorsal ramus of a lumbar nerve demonstrates the degree of detail that can be achieved under optimal conditions. Varying degrees of severity of brachial plexus entrapment in patients with thoracic outlet syndrome. A, Linear brachial plexus with a short segment of mild irritative changes near the lateral border of the scalene triangle (arrow). B, Evidence of more restrictive fibrosis associated with narrowing and brightening of elements of the brachial plexus near the scalene border (arrow). D, Severe multiple-element abnormality with narrowed and swollen segments and marked hyperintensity (arrow). E, Linear normal plexus with isolated focal impingement of the C5 spinal nerve (arrow) just proximal to the scalene triangle. F, Fibrous band causing sharp downward distortion of the middle and lower trunk proximal to the scalene triangle (right arrow), with a second sharp upward distortion (left arrow) of the lower trunk near the insertion of the scalene muscle at the first rib. G, Moderate restrictive impingement of the brachial plexus at the scalene triangle causing generalized distortion of the course of the plexus (arrow) with a short segment of focal hyperintensity. H, Severe pain, numbness, and weakness caused by progressive thoracic outlet syndrome, manifested as multiple points of sharp distortion of the course of the nerve (arrows) with edema and hyperintensity affecting multiple elements of the brachial plexus. For instance, median nerve entrapment in the distal part of the forearm can lead to failure of treatment if only the flexor retinaculum is addressed. Electrodiagnostic studies can yield misleading results if they are performed under the assumption that abnormalities in certain regions. However, both images are from the same individual and were obtained at the same location in the wrist; they differ only in that one is in a position of flexion and one in extension of the wrist. In a series of patients with clinically and electrodiagnostically confirmed carpal tunnel syndrome, electromyography revealed that although most had compressive lesions, some demonstrated only nerve adhesion with loss of normal mobility of the nerve on flexion and extension of the wrist. From the points of view of electrodiagnosis and surgical treatment, there is little difference between adhesive and compressive carpal tunnel syndrome. Both entities produce similar clinical and diagnostic pictures and respond to the same surgical treatment. However, from the point of view of imaging, it is important to appreciate that patients may have moderate to severe carpal tunnel symptoms with no evidence of nerve compression if adhesion is present. Clinically, this demonstration is of potentially greater importance because in many cases it is possible to demonstrate with imaging that a nerve is not gliding normally across a joint. Restriction of movement of a nerve can cause repeated trauma to the nerve, as well as symptoms of pain exacerbated by extremes of motion or by assuming particular postures or limb positions. The right side (A) demonstrates an S-shaped course passing under the clavicle and over the first rib (arrows), whereas the elements of the brachial plexus on the left side (B) travel along a comparatively straight course (arrow). Lumbar neurography for evaluation of sciatica of nondisk origin caused by entrapment of the lumbar spinal nerve in the distal foramen. A, Normal anatomy of the L3, L4, and proximal L5 nerve roots and lumbar spinal nerves as they exit the spine and travel in essentially linear manner. B, Exiting right L5 nerve root (asterisk) in a 65-year-old woman with persistent right L5 radiculopathy after two spine operations. The course of the exiting root is distorted, and both focal narrowing and a region of L5 spinal nerve hyperintensity (arrow) are apparent. C, Myelogram of the same patient obtained just before magnetic resonance neurography. The L5 root abnormality (asterisk) is too distal to be appreciated on the myelogram, and the study was read as showing a normal L5 root with no impingement. After neurographic diagnosis, the patient underwent distal foraminotomy, which provided excellent lasting relief of the radiculopathy. The nerve is flattened and hyperintense and has expanded to more than twice its normal diameter. This is a postoperative result that occurred when only one of the two bipartite elements of the piriformis muscle was released in a patient with a split nerve and split muscle. Differential retraction of the cut piriformis segment in relation to the intact segment caused a severe mechanical impingement syndrome. After axonotmesis, recovery may require several months, but there are few reliable means of distinguishing this situation from neurotmesis, in which no recovery can be expected without surgical intervention. B, the right and left L5 spinal nerves (arrows) on the anterior surface of the sacrum are compared in the T1-weighted image with the massive swelling of the left spinal nerve. C and D, Matched T1-weighted (C) and T2-weighted fat saturation (D) images showing the extent of swelling (arrows).
Discount ventolin 100mcg online
Reported operative results were generally satisfying: recovery of elbow flexion (M3) was obtained in 100% of the cases with avulsion of C5-C640 asthma symptoms sneezing discount 100mcg ventolin visa,41 and in 70% with avulsion of C5-C6-C7. A precondition of performance of this transfer is good strength of the triceps, which is no less than M4. The anterior branch of the axillary nerve is dissected proximally into the quadrilateral space and cut. The nerve to the long head of the triceps is divided at its entrance into the muscle and transferred to the divided anterior branch of the axillary nerve. Postoperatively, the strength of C7 musculature can be weaker by M1 grade than that before surgery, but it recovers significantly over a period of 6 months. This is because musculature generally classed as C7 can actually be innervated considerably by the lower trunk. In a series of 40 patients who had received direct coaptation of the phrenic nerve to the anterior division of the upper trunk for restoration of elbow flexion, 82. In the past, the hypoglossal nerve has been used for nerve transfer reconstruction of brachial plexus palsy. In a report of 14 patients who had undergone this transfer, by a nerve graft with mean length of 15 cm in adults and 7. This possibility arises because the supinator is supplied by C5 and C6 fibers running in the deep branch of the radial nerve, in distinction to the C7-dominated bulk of radial nerve components. In a report of obturator nerve transfer to the femoral nerve, a patient with femoral nerve palsy, which was caused by removal of a tumor involving the lumbar plexus, obtained M4 strength of the quadriceps and could walk nearly normally. It is indicated mainly for brachial plexus root avulsion when the proximal stump of the spinal nerve is not salvageable. It can also be applied for lengthy nerve defects when regenerating axons after nerve grafting have to progress over a long distance to reach the target. Nerve transfer cannot generally replace thorough exploration of nerve lesions, however, because the proximal stump of the injured nerve usually provides a more abundant source of axons and repair with the original nerve will require a less extensive postoperative cortical functional reorganization. Contralateral C7 transfer for treatment of brachial plexus root avulsions in children: a report of 12 cases. Intratemporal facial nerve transfer with direct coaptation to the hypoglossal nerve. Clinical application of ipsilateral C7 nerve root transfer for treatment of C5 and C6 avulsion of brachial plexus. Anatomic study of the intercostal nerve transfer to the suprascapular nerve and a case report. Evaluation of intercostal to musculocutaneous nerve transfer in reconstructive brachial plexus surgery. Suprascapular nerve reconstruction in 118 cases of adult posttraumatic brachial plexus. Different functional reorganization of motor cortex after transfer of the contralateral C7 to different recipient nerves in young rats with total brachial plexus root avulsion. Nerve transfer surgery for adult brachial plexus injury: A 10-year experience at Louisiana State University. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part 1: an anatomic feasibility study. Long thoracic nerve neurotization for restoration of shoulder function in C5-7 brachial plexus preganglionic injuries: case report. Sensory recovery of the hand with intercostal nerve transfer following complete avulsion of the brachial plexus. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a Meta-analysis of the English literature. Results of intercostal nerve transfer to the musculocutaneous nerve in brachial plexus birth palsy. Intercostal nerve transfer of the musculocutaneous nerve in avulsed brachial plexus injuries: evaluation of 66 patients. Spinal accessory neurotization for restoration of elbow flexion in avulsion injuries of the brachial plexus. Posterior approach for both spinal accessory nerve to suprascapular nerve and triceps branch to axillary nerve for upper plexus injuries. The dorsal approach to the suprascapular nerve in neuromuscular reanimation for obstetric brachial plexus lesions. Surgical treatment for total root avulsion type brachial plexus injuries by neurotization: A prospective comparison study between total and hemicontralateral C7 nerve root transfer. The influence of interrupting the relationship between dorsal ganglion and ulnar nerve on treatment outcome of contralateral C7 nerve root transfer: an experimental study. Hemicontralateral C7 transfer to median nerve in the treatment of root avulsion brachial plexus injury. Hemi-contralateral C7 transfer in traumatic brachial plexus injuries: outcomes and complications. Selective contralateral C7 transfer in posttraumatic brachial plexus injuries: A report of 56 cases. Minimum 4-year follow-up on contralateral C7 nerve transfers for brachial plexus injuries. The prespinal route in contralateral C7 nerve root transfer for brachial plexus avulsion injuries. Contralateral C7 nerve transfer with direct coaptation to restore lower trunk function after traumatic brachial plexus avulsion. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomic study and repot of four cases. Total ipsilateral C7 root neurotization to the upper trunk for isolated C5-C6 avulsion in obstetrical brachial plexus palsy: a preliminary technical report. Effect of ipsilateral C7 nerve root transfer on restoration of rat upper trunk muscle and nerve function after brachial plexus root avulsion. Medial pectoral nerve to axillary nerve neurotization following traumatic brachial plexus injuries: indications and clinical out-comes. Reanimation of elbow extension with medial pectoral nerve transfer in partial injuries to the brachial plexus. The anatomy of the pectoral nerves and their significance in brachial plexus reconstruction. Intercostal and pectoral nerve transfers to re-innervate the biceps muscle in obstetric brachial plexus lesions. Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: evaluation of 99 patients with various nerve transfers. Initial report on the limited value of hypoglossal nerve transfer to treat brachial plexus root avulsion. Transfer of supinator motor branches to the posterior interosseous nerve to reconstruct thumb and finger extension in tetraplegia: case report. Sulaiman the incidence and prevalence of peripheral nerve injuries after extremity trauma are relatively low, with reported rates of 1. Management of acute nerve injuries has improved significantly since the 1970s, but surgical management is still performed only at major medical centers, where there are specialists trained in the management of patients with complex nerve injuries, especially brachial plexus injuries. Hence, even for patients living in major metropolitan cities in the United States, it is still often necessary to travel to a different city or state to reach the closest centers where their injuries can be treated. Neurosurgeons, by virtue of their training, can master microsurgical repair of injured nerves, but most neurosurgeons are not exposed to comprehensive management of patients with complex nerve injuries, including initial evaluation, surgical planning and knowledge of anatomy, and the intraoperative decision-making process. This chapter reviews critical steps in the management of patients that have sustained acute nerve injuries. Once a diagnosis of nerve injury has been made, overall management, including timing of surgery, is determined by the nature of the injury (open versus closed), acuity of the injury (early versus delayed presentation), and findings on clinical, electrodiagnostic, and imaging studies. They divided the injuries into three groups according to the degree of forces exerted per surface area of the injured nerves and the complexity of the injury. Type A nerve injuries, generally caused by medium- to high-energy forces are applied directly or indirectly to nerves, include nerve transection, contusion, stretch, traction, and avulsion nerve injuries.
Buy generic ventolin 100mcg
Axial asthma treatment of albuterol q2 q1 buy ventolin no prescription, sagittal, and coronal thoracic spine computed tomography scan reveals a thoracic intradural extramedullary ventral meningioma. Similarly, a series by Selch and coworkers retrospectively reviewed 25 nerve sheath tumors. Tumor size remained stable in 18 cases, and 7 (28%) demonstrated more than 2-mm reduction in tumor size. The authors surmised that symptom resolution might require a prescribed dose of more than 12 Gy. Despite the encouraging results, longer follow-up is required to establish the ultimate efficacy of radiosurgery for benign intradural extramedullary tumors. Kondziolka and colleagues reported the local relapse rate after radiosurgery for vestibular schwannomas increased over the first 3 years of follow-up. Long-term follow-up is required before concluding that radiosurgery is as efficacious as microsurgical resection for the treatment of benign spinal tumors. More information is needed to understand the tolerance of the spinal cord to radiosurgery. Treatment of hemangioblastomas in von Hippel-Lindau disease with linear accelerator-based radiosurgery. Stereotactic radiosurgery yields long-term control for benign intradural, extramedullary spinal tumors. Initial clinical experience with image-guided linear accelerator-based spinal radiosurgery for treatment of benign nerve sheath tumors. Image-guided radiosurgery for spinal tumors: methods, accuracy and patient intrafraction motion. Multisession CyberKnife radiosurgery for intramedullary spinal cord arteriovenous malformations. Radiosurgery using the Cyberknife for benign spinal tumors: Korea Cancer Center Hospital experience. International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Arteriovenous malformations of the spinal cord: clinical, anatomical, and therapeutic consideration: a series of 150 patients. Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Clustering of features of von HippelLindau syndrome: evidence for a complex genetic locus. The long-term results of Gamma Knife radiosurgery for hemangioblastomas of the brain. Treatment of hemangioblastomas in von Hippel-Lindau disease with linear acceleratorbased radiosurgery. Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Spinal cord and intraduralextraparenchymal spinal tumors: current best care practices and strategies. Risk factors for neurological complications after acoustic neurinoma radiosurgery: refinement from further experiences. Resnick Perhaps no other subspecialty in the field of neurosurgery has advanced as rapidly since the early 2000s as the evaluation and management of spine disorders. Once a smaller, complementary aspect of neurosurgical practice involving intracranial pathologic conditions, the management of the spectrum of spine disorders has now become the largest component of most neurosurgical practices. Surgical procedures for the treatment of spinal cord tumors, traumatic spinal cord/column injury, infections of the spine, spinal stenosis, and disk herniation have been routinely performed by neurosurgeons since the 1960s and remain a substantial portion of clinical practice. Since 2000, the scope of spine disorders routinely managed by neurosurgeons has markedly expanded to encompass the entire spectrum of spine disease, including conditions such as primary tumors of the spinal axis and pediatric and adulthood spine deformity. Advanced minimally invasive techniques are now routinely performed by neurosurgeons. The editors of the "Spine" section of Youmans and Winn Neurological Surgery, 7th edition, have endeavored to comprehensively present the accumulated knowledge of the field of spine surgery. Some of the chapters detail subject areas generated from the synthesis of much peer-reviewed literature, produced from multiple randomized clinical trials. Other newer but potentially influential subject areas have much more limited foundations in current published literature but are authored by recognized leaders in the field who have described how new technology or surgical techniques compare with more standard treatments. For each chapter, we asked world-renowned leaders in the field of spine surgery to detail their accumulated experience, including their recommendations on evaluation, surgical decision making, and surgical techniques. Each author provided an annotated list of influential articles for each subject area. Our section focuses on the entire spectrum of diseases of the spinal cord and the vertebral column in adults and consists of 63 chapters organized into 10 parts that address the following topics: basic science, approach to the patient, degenerative diseases, infections, tumors, inflammation, congenital abnormalities, trauma, deformities, and surgical techniques. Pediatric spine diseases and their management are covered separately (see Chapters 229 to 239). Chapter 276 is a review of the scientific basis of disk degeneration and regeneration. The latter process appears to provide a rationale for new future treatment options. Chapter 277 is concerned with the pathophysiologic mechanisms and treatment of spinal cord injury. Chapter 278 is a discussion of the fundamentals of electrophysiologic monitoring and also provides a comprehensive review of clinical monitoring. Part 1 closes with Chapter 279 on the important topic of bone metabolism and osteoporosis. Part 2, "Approach to the Patient," contains thorough and comprehensive chapters addressing the essential clinical topics: the differential diagnosis of spine diseases, surgical and nonsurgical management of pain, and complication avoidance in spine surgery. Part 3, "Degenerative Diseases of the Spine," consists of six chapters that focus on evaluation and treatment of degenerative diseases. Topics include cervical disk herniation; ossification of the posterior longitudinal ligament; thoracic disc herniation; lumbar disk disease; stenosis in the cervical, thoracic, and lumbar spine; and lumbar spondylolisthesis. Part 4, "Infection of the Spine," contains three chapters on discitis and epidural abscess, osteomyelitis, and fungal and tubercular infections. Part 5, "Tumors of the Spine," consists of five chapters that expansively review the assessment and treatment of benign tumors of the axial skeleton; primary malignant tumors of the axial skeleton; benign tumors of the intradural and extradural neural elements; metastatic spine lesions; and malignant primary spine tumors. Part 6, "Inflammatory Diseases of the Spine," consists of two chapters on topics that frequently are part of the differential diagnosis of neck and lumbar pain: rheumatoid arthritis and ankylosing spondylitis (and diffuse idiopathic skeletal hypertrophy). Part 7, "Congenital Anomalies of the Spine," is concerned with adults and contains three chapters that extensively cover the following topics: congenital malformations of the thoracic and lumbar spine, tethered cord syndrome, and syringomyelia. Similar topics in pediatric patients are found elsewhere in this book (Chapters 229-233, 237, and 238). Part 8, "Spinal Trauma," contains nine chapters in which all aspects of trauma to the spinal cord and axial skeleton are systematically reviewed. Topics include assessment and classification of spine instability; medical management of spinal cord injury; classification and treatment of O-C1 injuries; C2 fractures and instability; evaluation, classification, and treatment of cervical injuries; treatment of cervicothoracic junction injuries; transient quadriparesis and athletic injuries of the cervical spine; evaluation, classification, and treatment of thoracolumbar injuries; and evaluation and treatment of osteoporotic fractures. From this part, the student will acquire scientific building blocks, whereas the practitioner will gain greater understanding of the rationale for approach and treatment. Chapter 273 is a thorough review of the anatomy of the spinal cord and vertebral column; Chapter 274 is a complementary chapter on spine imaging. Part 10, "Techniques for Spinal Procedures," is the largest part of this section and contains 16 chapters that expansively and comprehensively review surgical techniques and operations for the spine. Chapter 320 covers bone graft options, including bone graft substitutes and bone graft harvesting. Chapters 321 and 322 are on cervical and lumbar arthroplasty, and Chapter 323 is on nucleoplasty and posterior dynamic stabilization systems. A block of chapters is dedicated to instrumentation involving the occipital region, C1, and C2; the anterior cervical region; the posterior subaxial and cervicothoracic regions; the anterior thoracic region; the anterior and lateral lumbar region; and the posterior thoracic and lumbar regions (with historical overview). Chapter 330 concludes this block with a discussion of posterior, transforaminal, and anterior lumbar interbody fusion. A comprehensive overview is then presented in Chapter 331, on the principles and clinical applications of image-guided navigation of the spine. Chapter 333 is a general overview on spine osteotomies as they apply throughout the spine. The final two chapters of this section concentrate on two important topics: indications and techniques for revision spine surgery (Chapter 334) and minimally invasive techniques in treating degenerative disease (Chapter 335).
Stinktree (Tree Of Heaven). Ventolin.
- How does Tree Of Heaven work?
- Are there safety concerns?
- What is Tree Of Heaven?
- Dosing considerations for Tree Of Heaven.
- Diarrhea, menstrual disorders, asthma, cramps, epilepsy, fast heart rate, gonorrhea, malaria, tapeworms, or use as a tonic.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96679
Cheap 100 mcg ventolin otc
In the case of sacral dumbbell tumors asthmatic bronchitis 39 buy ventolin 100mcg with amex, extended lateral bone removal may be limited because the sacroiliac lateral articulation cannot be taken down without significant risk of sacroiliac instability. In cases in which presacral extension occurs, a separate anterior retroperitoneal approach is required with the assistance of a colorectal surgeon. The location in respect to the spinal cord dictates the approach and the amount of bone removal needed for a safe resection. Anteriorly located tumors are common; however, most of the time debulking and a gross total resection are feasible from a posterior standard laminectomy. Usually meningiomas have an en plaque involvement of the dura, and the exact amount of dura that needs to be resected for a complete free margin is difficult to determine. Given the relatively benign course of most spinal meningiomas and the long time to recurrence (some series have demonstrated an average of 9 to 15 years), the decision to resect or cauterize the dural attachment is usually influenced by the feasibility of dural reconstitution. Approach depends on the level of the tumor as well as its location within the spinal canal (dorsal, lateral, ventral) and surgeon preference. In the case of ventrally situated tumors, anterior approaches can be performed in the cervical spine and are unnecessary in the lumbar spine, where intradural nerve roots can be retracted without concern. Anterior approaches are particularly complicated in the thoracic region; upper thoracic lesions may be accessed through a trap-door approach or parascapular extrapleural approach. For the remainder of thoracic lesions, however, extracavitary or retropleural approaches are employed if a traditional posterior midline approach is not suitable. In the lumbar spine, posterior or posterolateral approaches are generally sufficient, with lateral retroperitoneal approaches rarely needed for what is an entirely intradural pathology. Nevertheless, posterior approaches are the most commonly utilized for spinal meningiomas. A durotomy is fashioned-guided by the use of intraoperative ultrasound-so that rostral and caudal poles of the tumor surface are visualized. In the case of tumors with a dorsal dural base, an ellipsoid durotomy can be fashioned to resect the dural base. An arachnoid plane exists between the spinal cord and tumor capsule and can be exploited for small tumors. Larger tumors with even minor spinal cord compression should be addressed first with internal debulking using an ultrasonic aspirator, thus relieving cord compression and facilitating visualization of tumor margins. When manipulating the tumor capsule, traction should always be applied away from the spinal cord. Cautery of the dural base, if accessible, prior to tumor debulking may reduce intraoperative bleeding. In the case of meningiomas, surgeons are often presented with the dilemma of how to manage the dural base. For dorsally situated lesions, excision of the dural base and reconstructive duraplasty are straightforward. Lateral and anterior meningiomas, however, may have dural bases that cannot be resected or, if resection is feasible, dural reconstruction is not. A, Sagittal T1-weighted magnetic resonance imaging with contrast shows an intramedullary enhancing mass at T12-L1 and L2. B, Sagittal T2-weighted image demonstrating significant displacement of the cauda equina at the L1-L2 level. These lesions can be managed almost exclusively through posterior midline approaches, with subperiosteal dissection, bone removal, and dural opening as previously described. Myxopapillary ependymomas tend to be solid fleshy tumors amenable to en bloc resection. Paragangliomas, however, can be very vascular and more adherent to surrounding nerves. Next, the filum is identified and tested with a neurostimulator in similar fashion to a standard tethered cord release. Sometimes, tumors are too friable and fall apart with even the most gentle manipulation. In other instances, the tumor may be too large to deliver from the thecal sac without dangerous traction on the surrounding nerve roots, or functional roots may be intimately involved. Once resection is completed, the dura should be closed with a running suture in watertight fashion. Generally, patients are kept on intravenous antibiotics while a lumbar drain is in place. Leaks may be addressed with oversewing, but formal operative repair is required for persistent drainage. Postoperative imaging invariably shows a small pseudomeningocele that may resolve. For multiply recurrent spinal meningiomas or meningiomas with atypical or malignant histology, radiation doses of 50 to 54 Gy in 1. For spinal myxopapillary ependymoma, however, adjuvant radiotherapy has a more defined role. Adjuvant radiotherapy following surgery has been associated with significantly improved local control at 10 years (86% versus 46%) and progression-free survival at 10 years (75% versus 37%) regardless of whether resection was total or subtotal. Sonneland and associates reported on a series of 31 paragangliomas addressed surgically, with all 26 successful en bloc resections remaining disease free. Their benign histology makes surgical resection the ideal therapy to achieve long-term tumor control and even cure, but their intimate relationship with critical neural structures makes achieving this goal a challenge. With appropriate planning and consideration of the unique challenges associated with each tumor type, the successful management of these lesions can be achieved and is quite rewarding. Complete resection of intracranial meningiomas, as described by Simpson, is commonly accepted to be associated with superior local control rates, and the same principle is applicable to the spine. Long-term outcome after removal of spinal schwannoma: a clinicopathological study of 187 cases. Management of spinal meningiomas: surgical results and a review of the literature. Intraspinal meningiomas: review of 54 cases with discussion of poor prognosis factors and modern therapeutic management. Surgery of spinal nerve sheath tumors with special reference to neurofibromatosis. Surgical management of dumbbell and paraspinal tumors of the thoracic and lumbar spine. Paraganglioma of the cauda equina region: clinicopathologic study of 31 cases with special reference to immunocytology and infrastructure. Spinal meningioma: relationship between histological subtypes and surgical outcome Primary intraspinal neoplasms in Norway, 1955 to 1986: a population-based survey of 467 patients. Management of patients with schwannomatosis: report of six cases and review of the literature. A distinctive, heritable tumor with special associations, including cardiac myxoma and the Cushing syndrome. Intracranial retrograde dissemination in filum terminale myxopapillary ependymomas. Multi-modality neurophysiological monitoring during surgery for adult tethered cord syndrome. Multimodality intraoperative neurophysiologic monitoring findings during surgery for adult tethered cord syndrome: analysis of a series of 44 patients with long-term follow-up. Neurophysiological monitoring for safe surgical tethered cord syndrome release in adults. The transcondylar approach to extradural nonneoplastic lesions of the craniovertebral junction. Midline ventral intradural schwannoma of the cervical spinal cord resected via anterior corpectomy with reconstruction: technical case report and review of the literature. Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. Combined posterior and posterolateral one-stage removal of a giant cervical dumbbell schwannoma. Endoscope-assisted posterior approach for the resection of ventral intradural spinal cord tumors: report of two cases.
Syndromes
- Name of the product (ingredients and strengths, if known)
- Do not scratch the ears or insert cotton swabs or other objects in the ears.
- Certain types of moles (atypical or dysplastic) or multiple birthmarks
- Frequent urination
- Spine
- Some poisons
- Have a fever.
- Poorly developed middle section of the face
- Iron deficiency anemia
Generic 100 mcg ventolin overnight delivery
In cases of significant facet joint hypertrophy asthma symptoms in child purchase ventolin 100mcg with visa, the medial part of the inferior articular process of the proximal vertebra is resected; this exposes the superior articular process of the distal vertebra and often facilitates the lateral decompression. With severe bony stenosis of the lateral recess, excision of the medial border of the superior articular process of the distal vertebra may be necessary to finish the decompression of the lateral recess. The medial border of the pedicle is a good anatomic landmark for sufficient lateral decompression. At this stage, the lateral border of the dural sac is visualized, and the decompression can be finalized with undercutting of the roof of the neural foramen. Identification and preservation of the pars interarticularis is important to prevent iatrogenic fractures of this structure. Before wound closure, adequate hemostasis is ensured by diathermy, bone wax, or hemostatic sponges. Paraspinal muscles are approximated in the midline, and the subcutaneous tissue and skin are closed. The use of closed suction drainage after decompression remains at the discretion of the individual surgeon; two randomized controlled trials have not shown significant differences in rates of postoperative surgical site infection, hematoma, or neurological deficit, regardless of whether suction drains were used. Surgical Technique: Bilateral Decompression through Bilateral or Unilateral Laminotomy. In bilateral laminotomy technique, the spinous process and the supraspinous and interspinous ligaments are preserved. The paraspinal muscles are elevated from the spinous processes and the laminae bilaterally, and each side is decompressed separately under microscopy. Starting from one side, both the proximal and distal laminae are resected so that the attachments of the ligamentum flavum are detached. A, Drawing showing bilateral decompression and opening of lateral recess with preservation of the articular facets. Changing the angle of the microscope enables the surgeon to excise the whole ligament. If necessary, decompression is finalized by undercutting resection of the facet joint and neural foramen. In this technique, the initial (ipsilateral) side is decompressed in a manner similar to the bilateral laminotomy technique. The paraspinal muscles need to be retracted from this side only; the posterior anatomy of the contralateral side is preserved. To facilitate the ipsilateral decompression, the spinous process on this side can be thinned out by a high-speed bur. After decompression of the ipsilateral side, the contralateral side is visualized by angling of the microscope and tilting of the operating table. For exposure of the contralateral ligamentum flavum and the facet joint, the base of the spinous process and the inner layer of the contralateral lamina are resected with either a curved chisel or a diamond bur. The ligamentum flavum and the medial facet joint can then be resected piece by piece with a Kerrison rongeur until the contralateral pedicle and lateral border of the dural sac are identified. By changing the angle of the microscope, the surgeon can perform complete decompression of the contralateral side down to the neural foramen over the top of the dural sac. Microendoscopic decompression, a modification of the unilateral approach, combines the microsurgical technique described previously with a tubular retractor system and endoscopy. It provides the added benefit of minimal damage to the ipsilateral paraspinal musculature. With the unilateral technique, an approach from the more symptomatic side is recommended. If symptoms are bilateral and similar, approaching from the left side may be more convenient for a right-handed surgeon. Two successive levels may be decompressed through the same approach, but for any further successive levels, an approach from the opposite side should be considered. Facet joint resection on the ipsilateral side tends to be greater than on the contralateral side, especially at the upper lumbar levels, because the ipsilateral recess may be difficult to decompress without more extensive facet joint removal. Postoperative imaging studies have shown 73% to 83% facet joint preservation on the ipsilateral side compared with 95% to 97% on the contralateral side. Moreover, maneuvering the instruments through the working channel involves a steep learning curve. Without conventional threedimensional vision, it is also more difficult to assess the eventual extent of the decompression. In three randomized controlled trials,118-120 extensive supervised exercise programs or supervised physical therapy programs using mixed techniques did not improve surgical outcomes compared with "treatment as usual" or advice simply to "keep active" after surgery. However, a meta-analysis of these three studies suggested that active postoperative rehabilitation is more effective than usual care for function and for back and leg pain, although not clinically significantly so for pain. A, Drawing showing bilateral decompression by different sides (right side on L5-S1, left side on L4-5). B, Postoperative radiograph showing the areas of decompression at L3-4 (white arrow) and L4-5 (black arrow). Up to 2 years later, the patients who underwent surgery demonstrated less leg pain than did the patients who received conservative treatment,125 but at the 6-year follow-up, no difference between the groups was reported. In conclusion, the efficacy of surgical treatment slowly decreased after the 2-year follow-up, but at 6 years it was still superior for functional status, as measured by the Oswestry Disability Index. Significant crossover in both randomized arms makes intention-to-treat analysis difficult. The authors of a systematic review concluded that current evidence consistently favors decompressive surgery over conservative treatment for improvements in pain, disability, and quality of life, although not for walking ability. Significant improvement in back pain has been reported after decompression without fusion,125-127 possibly as a result of improved lumbar posture and facet joint denervation with surgical trauma. Overall patient satisfaction was significantly superior after bilateral laminotomy; 2. Rajasekaran and colleagues130 compared decompression through splitting of the lumbar spinous process with conventional midline decompression in a randomized trial of 51 patients. They found no significant differences in functional outcome, back pain, leg pain, or neurogenic claudication at a mean 14. Furthermore, no difference in clinical results at 2 years was noted in another randomized trial in which conventional microsurgical decompression (in 100 patients) was compared with full-endoscopic interlaminar decompression (in 92 patients). The effect of age on postoperative outcome remains controversial; some studies suggest that older age, even in the presence of common comorbidities, is not predictive of surgical outcome,89,135-137 whereas other studies report an association between older age and postoperative symptom severity. Shorter symptom duration (of <1 year84 or 2 years140) has been reported to increase the probability of a successful outcome. Two thirds of patients with preoperative resting numbness complain of postoperative residual leg pain and numbness 2 years after surgery. Multilevel surgery is not associated with an increased risk of a symptomatic postoperative epidural hematoma. Early diagnosis and immediate surgical decompression of the hematoma are prerequisites for a successful outcome. Preoperative risk factors for facet cyst formation include instability, asymmetrical disk degeneration, and sagittal imbalance. Interspinous process devices have been used either as standalone implants or in augmenting conventional decompression procedures. However, the reoperation rate during the first postoperative year reached 29% (38% with two-level procedures) with the interspinous process device in contrast to 8% with a conventional decompression. At 2-year follow-up, they reported comparable clinical outcomes and reoperation rates (10. Surgical treatment with a stand-alone interspinous process device is associated with fewer medical complications than is traditional decompression, but the risk of needing early revision surgery is substantially greater. Postoperative magnetic resonance image showing an epidural hematoma compressing the dural sac. Indirect decompression with the use of interspinous process devices (C, white arrows). They are associated with increased frequency and severity of facet joint osteoarthritis, as well as degenerative changes of the ligamentum flavum. Concomitant instrumented fusion has been suggested for younger patients and in cases of mobile degenerative spondylolisthesis or minor degenerative changes at the affected level. Moreover, symptoms of cervical spinal cord compression may emerge postoperatively as a result of prolonged neck extension during lumbar surgery.
Cheap ventolin 100 mcg visa
Although the patient may not notice subtle sensory loss in the torso extrinsic asthma medical definition buy discount ventolin 100 mcg online, proximal limbs, or feet, even smalls patches of sensory loss in the face or hands are readily described. The patient may relate a complete loss of sensation (anesthesia), or an alteration-either a decrease (hypesthesia) or increase (hyperesthesia) in sensation. Patients with significant autonomic nerve impairment may report a perception of numbness in locations where intact somatic nerves lead to normal objective sensory thresholds. Other patients may report dysesthesias or paresthesias, such as tingling, electric shock sensations, or pins and needles. The evolution of sensory loss is sought, particularly to ascertain whether recovery is occurring. Motor Deficit the location and severity of muscle weakness are key features of the history. Most patients describe their deficit in terms of general movements, their impact on activities of daily living, and changes with coordination. For example, a patient with a severe groinlevel femoral nerve injury with complete denervation of quadriceps may simply give the impression that the leg feels weak overall and has a limp. Questions directed to how the patient performs on stairs or gets up from a sitting or squatting position will lead to improved understanding of the nature of the functional deficit. Any consequences on occupational and recreational performance should also be discussed. In a similar manner, further questioning may provide insight into the evolution of the deficit. For instance, patients with complete peroneal nerve injuries should be questioned about any dorsiflexion of the toes or foot while supine. An obvious scenario is the infant with a plexus injury, when information provided by the parents is particularly helpful. Pertinent information related to the spontaneous range of motion and the relative strength of various muscle groups should be questioned. A full exposure of the affected limb, as well as of the contralateral normal limb used as a reference, is recommended. The examination should be performed in a consistent and reproducible fashion so as not to overlook findings, starting from the proximal aspect of the limb and systematically working distally. When it becomes apparent that a single peripheral nerve is affected, confirming a normal examination of adjacent motor and sensory nerves is important. With proximal upper extremity nerve palsies, the examiner should always assess the parascapular and shoulder girdle muscles before proceeding more distally to the arm and hand. Again, it is extremely important to compare the affected side with the normal side so that the examination may be sensitive enough to identify subtle palsies in otherwise strong patients. In the lower extremity, the previous principles entail examining both the anterior and the posterior aspects of the patient, up to and including the gluteal region and hip joint. In assessing muscle strength, an attempt is made to discriminate gross limb movement from specific muscles action because the latter provides for more precise lesion localization. For example, lateral abduction of the shoulder within the first 30 degrees is mostly produced by the supraspinatus, the next 60 degrees by the deltoid (up to about 90 degrees of abduction), and above 90 degrees by medial rotation of the scapula. The examiner must keep in mind, however, that these (and other) cutoff points are variable, with transitions between muscles often being gradual and dynamic. Finally, the examiner needs to be aware of substitutive movements that the patient learns and adapts to overcome deficits. The inexperienced clinician may confuse these for recovery of muscle function when, in fact, there is none. For example, a patient with a complete deltoid palsy may be able to laterally abduct the shoulder to 90 degrees by using a combination of strong supraspinatus contraction and rotation of the scapula (contraction of the pectoralis and coracobrachialis may also play a role). Careful visualization of shoulder mechanics from above and behind, with concurrent palpation of the deltoid, will allow the examiner to make an accurate assessment. Orthopedic Assessment Orthopedic assessment remains an important, albeit often forgotten, part of the neuromuscular examination. After the initial inspection of the patient, the affected limb and joints should be palpated and tested for first passive and then active range of motion. In the empty can test, the patient abducts the affected arm with elbow extended and wrist pronated, as if pouring out a can of soda. The examiner then pushes down on the extended arm and the patient tries to resist. If pain is elicited on the ipsilateral side anteriorly, it is suggestive of a hip joint disorder on the same side. In appropriate patients, plain radiographs of the affected joints should be performed during the initial diagnostic work-up to exclude osseous injuries. When a significant musculoskeletal abnormality is suspected, a referral to an orthopedic specialist may be advisable. Inspection the examination always begins with a visual assessment of the affected limb or bodily region in comparison with the normal side. Previous scars and past surgeries should be questioned, especially those that may be related to the nerve injured. Baseline photographs may be useful for long-term follow-up and assessment of treatment efficacy. For example, consider the patient with an upper (with or without middle trunk) brachial plexus injury. Another example is a humeral-level radial nerve injury that produces a typical wrist and finger drop when the patient holds the arms outstretched in front. Ulnar claw hand (hyperextension of the Motor Examination Motor testing is perhaps the most objective and reproducible aspect of the neuromuscular examination. Adhering to the principles outlined earlier, the examiner compares the involved versus normal extremity with respect to bulk, tone, and strength. Strength is rated using the British Medical Research Council system (Table 245-1). B, Right humeral level radial nerve palsy causing wrist and finger drops (arrowhead). C, Right sciatic palsy with atrophy of leg muscles and flail right foot (arrowhead). Autonomic abnormalities, including erythema, alopecia, and swelling, are present in the right leg. However, as the lesion becomes better localized, a more focused motor examination can be used to isolate the lesion to a single nerve, or even within a segment of the nerve. This is accomplished by testing sequential muscles innervated by the nerve in question as well as by confirming the normal examination of a nearby nerve. Complicated injuries to the brachial plexus and lumbosacral plexus often require a comprehensive strength assessment of all regional muscles to provide the best localization. When testing a muscle, it is important to both inspect movement and palpate the muscle being examined. This allows detection of even trace contractions, which may not even result in movement. For example, having the patient supine while testing for lateral abduction of the shoulder will eliminate gravity when testing supraspinatus and deltoid muscles. Similarly, the supine patient can rest the arm on the chest wall and then be asked to flex the hand toward the head, thus allowing the elbow flexors to contract with the effects of gravity minimized. Variable strength over a reduced range of motion is common when patients partially recover. When possible, an accurate assessment of muscle bulk using a tape measure should be performed. In doing this, the examiner should first mark the extremity from a fixed bony landmark to compare comparable areas on the affected and unaffected limbs during serial examinations. Instead, the pulp of the distal fingers touch because the flexor pollicis longus and flexor digitorum profundus to the index finger are weak. The previously mentioned ulnar claw hand occurs when the patient is asked to actively open the hand and is a hallmark of ulnar nerve injury. Conversely, median nerve injury produces the benedictine hand in which the index and middle finger fail to properly flex when the patient is instructed to make a fist. Even the previously described classical neurological findings require careful examination to localize the lesion. An upper motor neuron lesion affecting the pyramidal tract, a cord lesion affecting the L5 motor neuron pool, a spinal lesion interfering with L5 outflow, and peripheral lesions affecting the L5 nerve root, lumbosacral trunk, peroneal division of the sciatic nerve, and peroneal nerve itself may all result in footdrop.
Buy ventolin 100 mcg line
The same group performed a follow-up study in 2000 in patients with a minimum of 10 years of follow-up asthma meaning buy generic ventolin from india. Eighty-four patients (76%) out of 110 without neurological symptoms at initial presentation remained neurologically stable. However, 29 (83%) of the patients who had had neurological symptoms at initial presentation had experienced clinical deterioration during the 10 years. The pain is most typically mechanical in nature, worsening with extension of the lumbar spine. Radicular pain can be caused by direct nerve root compression in the lateral recesses, with the L5 nerve root most commonly affected. This pain is usually described as a shooting pain radiating down the posterolateral thigh to the lateral shin and to the dorsum of the foot. In addition to lateral recess stenosis, significantly compression of the neural foramina themselves can occur. This may lead to L4 radiculopathy, because L4-L5 is the most frequently affected level. This pain is usually described as radiating down the anterolateral thigh, over the knee, and to the medial shin and medial malleolus. In contradistinction, neurogenic claudication tends to have a more inconsistent distribution. The pain and paresthesias are typically described as involving the anterior thighs, often bilaterally. These symptoms fit well with the anatomic changes noted on flexion-extension of the back. A cadaveric study showed significant decreases in both spinal canal area and foraminal size with extension, and their expansion with flexion. The differential diagnosis for patients presenting with these symptoms should include vascular claudication as well as hip and sacroiliac joint disorders. It is most common at the L4-L5 level, unlike other forms of spondylolisthesis, which are more common at L5-S1. Current theories for this finding include greater ligamentous laxity and hormonal effects in women. A history of significant trauma or personal history of malignancy (or signs and symptoms of malignancy) may increase the suspicion of traumatic or pathologic etiologies. Specific focus should be placed on distributions of any potential sensory loss as well as any weakness or loss of deep tendon reflexes in the lower extremities. Weakness of the extensor hallucis longus is typical for a severe L5 radiculopathy, and weakness in dorsiflexion for a severe L4 radiculopathy. A study looking at asymptomatic individuals showed that 90% had between 1 mm and 3 mm of translation. Significant sagittal imbalance, high pelvic tilt (>20 degrees), or lumbar lordosis to pelvic incidence mismatch (>10 degrees) may necessitate treatment beyond management of just the spondylolisthesis. Care should be taken in the prescription of these medications, especially in the elderly. Radiographic predictors of outcome, including degree of slip (by Meyerding criteria), disk height, and mobility, were also analyzed in this study. Among all three groups, surgically treated patients had better outcomes than nonoperatively treated patients. Regarding patients who did not undergo surgery, those who had grade 1 slips and those who had hypermobility (on the basis of flexion-extension radiographs) tended to have better outcomes with treatment. Two early randomized trials demonstrated favorable results (as defined in each study) in patients who underwent fusion in comparison with decompression alone. If symptoms are persistent after a short trial of medications, a course of physical therapy can be useful. Epidural steroid injections can potentially deliver short-term benefit; there is likely no significant long-term benefit. Goals of conservative care should be to provide pain relief and maintain normal activities of daily living. However, many studies demonstrated worsened clinical results in the setting of pseudoarthrosis, and thus, many methods of spinal instrumentation have been developed to achieve higher rates of fusion. Half were assigned to an observational cohort (patient-selected surgery versus nonoperative therapy) and the other half to a randomization cohort. Two separate analyses were conducted, one being as-treated, and the other being intent-to-treat. Final analysis showed that patients who underwent surgery appeared to have statistically significant better outcomes. A follow-up study in 2013 by Pearson and associates26 looked at differences in treatment effect using subgroup analysis. All subgroups with more than 50 patients were noted to improve significantly with surgery. Although these interventions along with the engineering of spinal instrumentation systems continue to be refined, a number of commonly employed techniques are described here. As mentioned previously, the implementation of spinal instrumentation must balance the benefits of increased stability with the added surgical risk and cost. This allows the surgeon to attain "360-degree fusion," thus optimizing stability across a mobile segment of the spinal column. B, Postoperative lateral radiograph after L4-L5 laminectomy and posterolateral fusion. Major drawbacks include risks to vascular and autonomic structures lying in front of the lumbosacral spinal column, including intraabdominal contents, iliac vessels, and the prevertebral sympathetic plexus (which may induce retrograde ejaculation in male patients). Lateral lumbar interbody fusion, which has also been described, involves a lateral, retroperitoneal approach to the spinal column. This approach spares the abdominal contents and bypasses risk to iliac vessels and sympathetic nerves. Retroperitoneal contents are at greatest risk with this approach, including the ureter, psoas muscle, genitofemoral nerve, and the rest of the lumbar plexus. The exiting nerve root may also cross the targeted disk space, but intraoperative stimulation can be helpful in guiding dissection. This maneuver allows a thorough discectomy and bilateral placement of interbody cages. The pars interarticularis is not violated with this technique, and a circumferential fusion can be accomplished through a single posterior approach. A main concern with this approach is the amount of medial retraction necessary to visualize the disk space and implant interbody grafts, which can result in increased rates of postoperative nerve root injury or cauda equina/conus medullaris syndrome. This step allows removal of the inferior articular facet from the cranial vertebra and generous expansion of the neural foramen. Along with removal of part of the superior articulating facet from the caudal vertebra, the disk space and traversing nerve root can be easily visualized. The discectomy and interbody graft placement can thus be accomplished with minimal manipulation of the nerve root. There is a large body of literature comparing the various techniques for lumbar fusion. With refinement of the preceding techniques for lumbar instrumented fusion and innovation in surgical systems for exposure and visualization, many of the described approaches are now performed using "minimally invasive" strategies. B, Postoperative sagittal and coronal reformatted computed tomography views demonstrating significant reduction after placement of a large interbody cage via a minimally invasive transpsoas approach. C, Postoperative lateral radiograph demonstrating the laterally placed interbody cage and posterior percutaneous instrumentation. A differentially threaded axial rod is used to distract the vertebral bodies as well as provide stabilization. Angling the tubular retractor often enables central canal decompression to reach the contralateral foramen by undercutting of the lamina and ligamentum in addition to the interbody fusion. These minimally invasive approaches are often more reliant on intraoperative fluoroscopy, exposing the patient and surgeon to more radiation. However, blood loss and perioperative morbidity are often decreased with minimally invasive techniques.