Zenegra 100mg on line
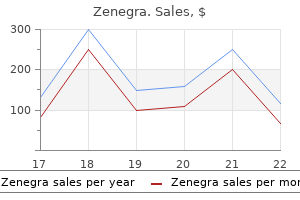
Causes Postural or orthostatic proteinuria should be ruled out in children by performing a first morning urine protein/creatinine ratio (0 erectile dysfunction treatment viagra generic zenegra 100 mg line. Fixed or nonorthostatic proteinuria requires complete evaluation, sometimes including a renal biopsy. Endothelial Layer Endothelium comprises the innermost layer of the glomerular capillary and remains in direct contact with circulating plasma and the cellular constituents of blood. The body of the glomerular endothelial cell rests within the hilum of the capillary loop, in close proximity to mesangial cells. A thin layer of endothelial cytoplasm extends from the endothelial cell and envelops the inner aspect of the capillary lumen. The endothelial surface layer, composed of glycocalyx and plasma components, may indeed be important as a barrier. Glomerular capillaries possess hydraulic conductivity (permeability) that permits passage of large volumes of ultrafiltrate and small solutes. Simultaneously, these capillaries also exhibit selective permeability that actively restricts passage of albumin (3800 kDa) and other larger molecules. From a functional perspective, and given our current state of knowledge, the three layers seem to be equally important in the macromolecular transport. Clearly, more needs to be learned about endothelial functions and their role in glomerular capillary macromolecular transport. The adjacent foot processes do not come in direct contact with each other and are separated by an approximately 40-nm-wide space known as the filtration slit. Although some shedding of podocytes into the urinary space and excretion in urine is normal, this process can be accelerated by injury and disease states. Urinary loss of podocytes (or podocyturia) can result in a permanent and irreplaceable quantitative deficit of podocytes in the glomeruli (podocytopenia). The nature of glomerular capillary selective permeability (permselectivity) has been a matter of considerable debate. Based on experimental data and mathematical modeling, glomerular permselectivity has been attributed to (1) molecular size, (2) molecular charge, and (3) molecular configuration. Podocytes are thought to be involved in the pathogenesis of a range of diseases, such as minimal change disease, focal segmental glomerulosclerosis, other types of glomerulonephritic and diabetic nephropathy. Genetics of proteinuria: an overview of gene mutations associated with nonsyndromic proteinuric glomerulopathies. The first clue about the role of anionic charges in proteinuria was the observation in normal rats that clearance of albumin was significantly lower than that of neutral tracer molecules of dextran of the equal molecular size. Findings that Ficoll may actually not be as tightly configured in solution as previously thought has put the role of molecular configuration into question. However, normal urinary protein excretion under physiologic circumstances in an adult is less than 150 mg/24 h, a finding suggesting that renal tubules reabsorb most of the filtered albumin. This inference has been drawn from the fractional clearance of dextran and Ficoll (Sigma-Aldrich, St. Dextran is a complex branched polysaccharide, a polymer of glucopyranose, with an elongated or sausage-shaped molecular structure. Ficoll, in contrast, is a highly branched, polysaccharide-epichlorohydrin complexed molecule with a globular shape. The albumin molecules in the tubular lumen bind to the cubilinmegalin receptor complex. The next step involves acidification of the vesicles, a step facilitated by the chloride channel-5 (ClC-5). This is an important step for albumin to be dissociated from the megalin-cubilin complex and for megalin to be recycled. Cubilin is a 460-kDa protein that does not have a transmembrane domain and remains anchored to the brush-border membrane by attaching itself to megalin. Cubilin binds to the albumin molecule, which along with megalin is internalized as an endocytosis vesicle. Proteinuria is also well known to be an independent risk factor for increased mortality and renal disease progression in both type 1 and type 2 diabetes mellitus. Proinflammatory chemokines Proteinuric states are characterized by an excessive synthesis of a variety of proinflammatory cytokines and chemokines by the tubular cells. The resident fibroblast population, along with its circulating population recruited by various proinflammatory cytokines and complement components, results in the formation of myofibroblasts. Activation of complement Complement, as a mediator of injury in proteinuria, has been investigated since the 1980s. Glomerular proteinuria is detectable by urine dipsticks and can be quantified by usual techniques discussed below. Proteinuria seen in such clinical circumstances is referred to as tubular proteinuria. Three markers commonly used as indicators of tubular proteinuria in clinical practice are 2-microglobulin, 1-microglobulin, and retinol binding protein. Overflow proteinuria this is the least common type of proteinuria found in children. Monoclonal gammopathies characterized by high plasma concentrations of monoclonal immunoglobulin fractions in the serum lead these proteins to appear in the glomerular ultrafiltrate. Once proximal tubular reabsorption capacity of these filtered plasma proteins is exceeded, they begin appear in urine. Bence-Jones protein, seen in multiple myeloma and other B-cell lymphomas, is an example of such overflow proteinuria. Bence-Jones protein was originally detected by heat precipitation methodology, but immunoelectrophoresis is now generally used to detect the monoclonal (M peaks) urinary protein excretion. Concentrated urine may give a positive reading even when the daily protein excretion is normal, whereas dilute urine may result in a negative, or only slightly positive reading even in the presence of elevated daily protein excretion. Twenty-four-hour collection of urine and the urine protein/creatinine ratio are other, more precise methods to quantify proteinuria. A family history of any renal disease must be ascertained to determine whether inherited disorders, such as Alport syndrome, need to be considered. Dipstick (semiquantitative) 24 hour urine collection Urine protein/urine creatinine ratio Physical examination the purpose of physical examination is to establish blood pressure, evidence of edema, and any clinical manifestations of rash or joint involvement that may indicate vasculitis or collagen-vascular diseases. The respiratory system, including the sinuses, should be examined for any evidence of clinical disease, sinusitis, or polyps, as seen in Wegener granulomatosis (now reclassified as granulomatosis with polyangiitis). Some investigators have estimated it to be as high as 50% to 60% of children with proteinuria. Consequently, the purpose of investigations in evaluating a patient with proteinuria is to determine whether any renal disease exists. The recommendation of the expert panel of Pediatric Nephrologists constituted by the National Kidney Foundation provides a framework for evaluation of proteinuria in children. Several case reports have implicated nutcracker phenomenon, or compression of the left renal vein by the aorta and another adjoining vessel, such as the superior mesenteric artery or vertebral artery. The principle of the test is to document proteinuria in the upright posture and its absence in recumbent posture. One can obtain differential timed urine collection of 12 h each: while the patient is recumbent and during upright posture. Alternately, a spot urine collection is obtained after 8 to 10 h of flat overnight rest (first morning void after waking up), and another sample is requested later in the day after 4 to 6 h of ambulation. None of these patients had evidence of renal disease or worsening of their proteinuria. In a 10-year follow-up of 46 Air Force recruits, all were found to have normal renal function, and proteinuria was persistent in 49% cases. The diagnosis of orthostatic proteinuria was confirmed, and the patient was reassured. The primary care physician had evaluated the patient extensively and had obtained normal data, except in the 24-h urine protein evaluation.
Cheap zenegra online
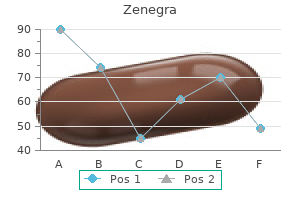
Vasodilators such as nitric oxide appear to decrease afferent arteriolar resistance preferentially so that erectile dysfunction injections australia order on line zenegra, at least at lower levels of renin-angiotensin activity, filtration is increased even in the presence of decreased renal blood flow. Higher levels of renin production constrict both the afferent and efferent vessels sufficiently that glomerular filtration is decreased. Thus, tubuloglomerular feedback regulates glomerular filtration to maintain a balance between glomerular filtration and tubular reabsorption. Other regulators of glomerular flow include vasoconstrictors such as norepinephrine; vasodilators such as histamine, certain prostaglandins, and bradykinin; and molecules that may directly affect K f, such as antidiuretic hormone. Renal nerve activity has a complex effect on whole organ kidney perfusion and may affect levels of angiotensin activity. However, it does not appear to affect glomerular filtration as strongly as the renin-angiotensin system,24 and it may influence natriuresis more by altering peritubular blood flow and tubular sodium reabsorption. Red and green boxes represent sites of arteriolar smooth muscle where resistance is applied to afferent and efferent arterioles. Box size is proportional to vasoconstrictor tone Brackets show the drop in hydrostatic pressure across the capillary, a major determinant of filtration. In the case of protein, the concentration 160 Physiology of glomerular filtration Normal rats 1. Clearance of molecules at each given size is shown with respect to the clearance of inulin as an indicator of glomerular filtration rate. Note that cations have facilitated clearance at any molecular size, whereas anions have decreased clearance. Permselectivity of the glomerular capillary wall: facilitated filtration of circulating polycations. Diffusion accounts for the clearance of large molecules, most commonly when plasma protein concentrations are elevated or filtration equilibrium is reached, as is the case in dehydration. Conversely, convection involves the movement of solute along with flow; it sometimes is referred to as "solvent drag. Albumin, which is filtered less than would be anticipated from its size, is a prolate ellipsoid (cigar shaped) and is unlikely to be distensible. The glycocalyx and the coating of the cells comprising the glomerular filter are negatively charged. Several additional factors may influence the passage of macromolecules through the glomerular filter. If the filter has properties of a porous structure, size considerations will be affected by shape and distensibility of the cleared molecule. As molecules approach the size where steric hindrance may affect filtration, the macromolecule may strike the edge of a pore in the filter. The larger the molecule, the more likely it is to strike the filter rather than going through the opening. Cell biology of the glomerulus / Physiologic feedback regulating filtration 161 in clearance of albumin. Briefly, the main cause is likely to be the disruption of podocyte structural integrity. Loss of charge selectivity may be a maintenance factor for increased clearance of negatively charged molecules in the presence of foot process effacement. The capillary endothelium, like all endothelial cells, produces proteins that regulate coagulation and inflammation. The loss of the podocyte permits such distention to bring the denuded basement membrane into contact with the Bowman capsule. This contact leads to synechia formation and the extrusion of vascular content directly into the interstitial space, an event implicated by many investigators in the pathogenesis of glomerulosclerosis. The mesangial cell has been described as a pericyte,44 similar to the Ito cells in the liver. Communication among the primary cells of the glomerulus represents an important component of glomerular biology. Additional fibroblasts are likely recruited to the glomerulus from the tubulointerstitium during disease. It is now thought that these cells, when dedifferentiated, are capable of migrating onto the mesangial stalk to establish or reconstitute the podocyte population. Even a minor disruption of the normal function of these cells can have significant consequences for kidney function and, by extension, total body physiology. The derangements that result are considered more extensively in other chapters of this book. Resolved: Capillary endothelium is a major contributor to the glomerular filtration barrier. Glomerular endothelial cells and podocytes jointly synthesize laminin-1 and -11 chains. Comparison of heparan sulfate proteoglycans from equine and human glomerular basement membranes. Early increase of chondroitin sulfate glycosaminoglycan in the glomerular basement membrane of rats with diabetic glomerulopathy. Immunocytochemical study of glomerular permeability to anionic, neutral and cationic albumins. The intrarenal renin-angiotensin system: From physiology to the pathobiology of hypertension and kidney disease. Cyclooxygenase-2 modulates afferent arteriolar responses to increases in pressure. Role of the renal nerves in modulating renin release during pressure reduction at the feline kidney. Imaging of the porous ultrastructure of the glomerular epithelial filtration slit. Role of the coagulation/fibrinolysis system in fibrin-associated glomerular injury. Participation of glomerular endothelial cells in the capillary repair of glomerulonephritis. Tracking the fate of glomerular epithelial cells in vivo using serial multiphoton imaging in new mouse models with fluorescent lineage tags. Nephrin regulates lamellipodia formation by assembling a protein complex that includes Ship2, filamin and lamellipodin. Hyperglycemia induces Toll like receptor 4 expression and activity in mouse mesangial cells: Relevance to diabetic nephropathy. Differential expression of functional Fc-receptors and additional immune complex receptors on mouse kidney cells. The podocyte is a differentiated cell that provides a static barrier to filtration. Which of the following does not increase macromolecular clearance by the glomerulus Fenestration of the glomerular endothelium is maintained in part by production of a. The normal homeostatic mechanisms that preserve a constant milieu interior will be presented. The pathophysiology of disturbances in sodium (Na+) composition will be discussed to provide a better understanding of common clinical problems encountered in pediatrics. Salient differences in Na+ handling between the adult and neonatal kidney will also presented. As a neonate, 70% of our weight is water, and the fraction of our body weight that is water decreases as we age. Adipose tissue has only 10% water content compared to most organs, which contain 70% to 80% water, and thus excess fat reduces the percentage of body weight that is water. The intracellular compartment comprises 60% of our total body water, with the extracellular compartment making up approximately 40%.
Buy discount zenegra on line
The Oxford classification of IgA nephropathy: Pathology definitions erectile dysfunction medicine in homeopathy buy zenegra on line amex, correlations, and reproducibility. The Oxford classification of IgA nephropathy: Rationale, clinicopathological correlations, and classification. Prognostic indicators in children with IgA nephropathy: Report of the Southwest Pediatric Nephrology Study Group. IgA nephropathy in children: Significance of glomerular basement membrane deposition of IgA. Histological differences in new-onset IgA nephropathy between children and adults. The Oxford IgA nephropathy clinicopathological classification is valid for children as well as adults. Defective galactosylation and clearance of IgA1 molecules as a possible etiopathogenic factor in IgA nephropathy. Galactose-deficient IgA1 in sera of IgA nephropathy patients is present in complexes with IgG. Autoantibodies targeting galactose-deficient IgA1 associate with progression of IgA nephropathy. Circulating immune complexes in IgA nephropathy consist of IgA1 with galactose-deficient hinge region and antiglycan antibodies. Interactions of human mesangial cells with IgA and IgA-containing immune complexes. IgA1containing immune complexes in IgA nephropathy differentially affect proliferation of mesangial cells. Aberrantly glycosylated IgA molecules downregulate the synthesis and secretion of vascular endothelial growth factor in human mesangial cells. Familial clustering of IgA nephropathy: Further evidence in an Italian population. IgA nephropathy, the most common cause of glomerulonephritis, is linked to 6q22-23. Aberrant IgA1 glycosylation is inherited in familial and sporadic IgA nephropathy. Galactose-deficient IgA1 in African Americans with IgA nephropathy: Serum levels and heritability. Patients with IgA nephropathy have increased serum galactosedeficient IgA1 levels. Aberrant galactosylation of IgA1 is involved in the genetic susceptibility of Chinese patients with IgA nephropathy. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Evidence-based assessment of treatment options for children with IgA nephropathies. Role for specific complement phenotypes and deficiencies in the clinical expression of IgA nephropathy. Long-term prognosis and prognostic indices of IgA nephropathy in juvenile and in adult Japanese. Clinicopathological features and the prognosis of IgA nephropathy in Japanese children on long-term observation. Long-term outcome 19 years after childhood IgA nephritis: A retrospective cohort study. Anaphylactoid purpura: Characteristics of 16 patients who progressed to renal failure. Long-term renal survival and related risk factors in patients with IgA nephropathy: Results from a cohort of 1155 cases in a Chinese adult population. Prognostic factors in mesangial IgA glomerulonephritis: An extensive study with univariate and multivariate analyses. Prognostic indicators of IgA nephropathy in the Chinese: Clinical and pathological perspectives. Natural history of immunoglobulin A nephropathy and predictive factors of prognosis: A long-term follow up of 204 cases in China. Risk stratification for progression of IgA nephropathy using a decision tree induction algorithm. A novel simpler histological classification for renal survival in IgA nephropathy: A retrospective study. Predictors of outcome in paediatric IgA nephropathy with regard to clinical and histopathological variables (Oxford classification). Clinical trial to evaluate omega-3 fatty acids and alternate day prednisone in patients with IgA nephropathy: Report from the Southwest Pediatric Nephrology Study Group. Which of the following histopathologic features is not included as a part of the Oxford classification The increased incidence of IgA nephropathy in Asian countries such as Japan may be due to all of the following, except: a. An aggressive approach by pediatric nephrologists in these countries for performing renal biopsies in children with isolated microscopic hematuria or low levels of proteinuria d. Dominant or codominant deposition of immunoglobulin A, mainly in the glomerular mesangium b. The formation of nephritogenic circulating immune complexes containing galactose-deficient IgA1 and antiglycan antibody d. Serum galactose-deficient IgA1 level is elevated in approximately 75% patients with IgA nephropathy; this is a heritable trait. In the United States, the percentage of children who have gross hematuria at the time of presentation with IgA nephropathy is approximately: a. Examination of cortical renal tissue obtained via kidney biopsy A normal urinalysis may eventually be seen in what percentage of pediatric patients diagnosed with IgA nephropathy Serial measurements of urinary protein excretion averaged over 6 month intervals after renal biopsy b. The mainstay of treatment for persistent proteinuria in the setting of IgA nephropathy is: a. Indeed, although these criteria seem distinct, in real life the clinical forms are often incomplete or changing during the course of the disorder, complicating a precise separation of the two entities and their evaluation and treatment. This verotoxin was subsequently found to be a member of a family of toxins first identified with Shigella and known as Shiga toxin (Stx).
Purchase zenegra in united states online
Changing trends of histopathology in childhood nephrotic syndrome in western Saudi Arabia erectile dysfunction what to do order generic zenegra. The increasing incidence of initial steroid resistance in childhood nephrotic syndrome. Is focal segmental glomerulosclerosis increasing in patients with nephrotic syndrome Nephrotic syndrome in African children: Lack of evidence for "tropical nephrotic syndrome" Quartan malarial nephrotic syndrome: Collaborative clinicopathological study in Nigerian children. Age and ethnicity affect the risk and outcome of focal segmental glomerulosclerosis. Racial differences in the incidence and renal outcome of idiopathic focal segmental glomerulosclerosis in children. Nephrotic syndrome: Vasoconstriction and hypervolemic types indicated by renin-sodium profiling. Pathophysiology of edema formation in children with nephrotic syndrome not due to minimal change disease. Effects of hypoproteinemia on renal hemodynamics, arterial pressure, and fluid volume. Role of plasma vasopressin in the impairment of water excretion in nephrotic syndrome. Blood volume, colloid osmotic pressure and F-cell ratio in children with the nephrotic syndrome. Lowered tissue-fluid oncotic pressure protects the blood volume in the nephrotic syndrome. Interstitial fluid volume, plasma volume and colloid osmotic pressure in patients with nephrotic syndrome. Evidence that some mechanism other than the renin system causes sodium retention in nephrotic syndrome. Role for intrarenal mechanisms in the impaired salt excretion of experimental nephrotic syndrome. Proteolytic processing of the epithelial sodium channel gamma subunit has a dominant role in channel activation. A critique of the overfill hypothesis of sodium and water retention in the nephrotic syndrome. Treatment of severe edema in children with nephrotic syndrome with diuretics alone: A prospective study. Reversible membranous nephropathy associated with the use of nonsteroidal anti-inflammatory drugs. Costeffectiveness of latent tuberculosis screening before steroid therapy for idiopathic nephrotic syndrome in children. Congenital nephrotic syndrome: Evolution of medical management and results of renal transplantation. Statin therapy improves brachial artery endothelial function in nephrotic syndrome. Insulin resistance, dyslipidaemia, inflammation and endothelial function in nephrotic syndrome. The role of I and B in peritonitis associated with the nephrotic syndrome of childhood. Decreased serum factor B concentration associated with decreased opsonization of Escherichia coli in the idiopathic nephrotic syndrome. Assessment of serum factor B, serum opsonins, granulocyte chemotaxis, and infection in nephrotic syndrome of children. Serum hemolytic factor D values in children with steroidresponsive idiopathic nephrotic syndrome. Serum immunoglobulins in the nephrotic syndrome: A possible cause of minimal-change nephrotic syndrome. Comparison of incidence of invasive Streptococcus pneumoniae disease among children before and after introduction of conjugated pneumococcal vaccine. Occurrence of infection among children with nephrotic syndrome during hospitalizations. Primary peritonitis in children with nephrotic syndrome: Results of a 5-year multicenter study. Serious infections due to penicillin-resistant Streptococcus pneumoniae in two children with nephrotic syndrome. Reversible renal failure in hypertensive idiopathic nephrotics treated with captopril. Angiotensin converting enzyme inhibitors for reduction of proteinuria in children with steroid-resistant nephrotic syndrome. Pathophysiology of edema and acute renal failure in idiopathic nephrotic syndrome. Vitamin D metabolites and calcium metabolism in patients with nephrotic syndrome and normal renal function. Osteomalacia and hyperparathyroid bone disease in patients with nephrotic syndrome. The hyperlipidemia of the nephrotic syndrome: Relation to plasma albumin concentration, oncotic pressure, and viscosity. Effects of infusions of serum albumin on serum lipids and lipoproteins in nephrosis. Hyperlipidaemia in untreated nephrotic syndrome, increased production or decreased removal Changes in serum lipoprotein(a) levels in children with corticosensitive nephrotic syndrome. Acute myocardial infarction in a young boy with nephrotic syndrome: A case report and review of the literature. Persistence of serum lipid abnormalities in children with idiopathic nephrotic syndrome. The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Subclinical cardiovascular disease and its association with risk factors in children with steroid-resistant nephrotic syndrome. Hyperlipidaemia, diet and simvastatin therapy in steroid-resistant nephrotic syndrome of childhood. Management of hyperlipidemia in children with refractory nephrotic syndrome: the effect of statin therapy. The reversal of intussusception associated with nephrotic syndrome by infusion of albumin. Mechanism of furosemide resistance in analbuminemic rats and hypoalbuminemic patients. Efficacy of metolazone and furosemide in children with furosemide-resistant edema. Angiotensin converting enzyme inhibition ameliorates glomerular filtration of macromolecules and water and lessens glomerular injury in the rat. Effect of fosinopril in children with steroid-resistant idiopathic nephrotic syndrome. Combined renin angiotensin blockade in childhood steroid-resistant nephrotic syndrome. Blood pressure in children with minimal change nephrotic syndrome during oedema and after steroid therapy: the influence of familial essential hypertension. Nephrotic state as a risk factor for developing posterior reversible encephalopathy syndrome in paediatric patients with nephrotic syndrome. Varicella-zoster virus infections in immunocompromised patients: A single centre 6-years analysis. Simultaneous sequencing of 24 genes associated with steroid-resistant nephrotic syndrome.
Order line zenegra
The efficacy of preoperative hydration strategies was demonstrated by a meta-analysis of 20 randomized controlled trials that investigated the renoprotective effects of perioperative hemodynamic optimization among 4220 adult surgical patients who were undergoing elective or emergency procedures erectile dysfunction bangalore doctor zenegra 100mg mastercard. Mannitol Experimental studies suggest that mannitol may be protective by causing diuresis (which minimizes intratubular cast formation) and by acting as a free radical scavenger (thereby minimizing cell injury). Loop diuretics Furosemide induces forced diuresis, and it also reduces active sodium chloride (NaCl) transport in the thick ascending limb of the loop of Henle; the ensuing decrease in energy requirement may protect the tubule cells in the presence of a decrease in energy delivery. If urine output does not improve after restoration of intravascular volume, more invasive monitoring may be required to guide further therapy. Fenoldopam this is a potent, short-acting, selective dopamine A-1 receptor agonist that increases renal blood flow and decreases systemic vascular resistance. Based on the underlying cause, comorbid conditions, and possible previous therapy, the child may be hypovolemic, euvolemic, or hypervolemic. Accurate initial assessment, and careful follow-up with accurate records of fluid input and output as well as body weights, physical examinations, and additional invasive monitoring as needed, will guide the appropriate fluid therapy. Commonly used fluids are crystalloid solutions, such as normal saline (10 to 20 mL/kg given over 30 min, repeated twice as needed, monitoring vital signs for appropriate responses). Conversely, a child with signs of fluid overload may require immediate fluid removal or fluid restriction. Furosemide-induced diuresis can simplify fluid, electrolyte, and nutritional management. The renoprotective effects of these agents have been evaluated primarily in trials of adults undergoing cardiac surgical procedures and with congestive heart failure. Although initial data seemed promising, more recent evidence from large randomized trials failed to show a clinic benefit from these agents. Care should be taken to avoid hypotension from overzealous diuretic therapy because that can increase the risk of nonrecovery of kidney function or death. Once euvolemia has been established, the clinician must pay careful attention to ongoing fluid losses (insensible water loss of approximately 300 to 500 mL/m2/day in addition to replacement of urine and gastrointestinal losses) and gains (fluids, medications, and nutrition administered). Insensible water losses are higher in febrile children and lower in ventilated children with decreased respiratory losses. In patients with fluid overload, the achievement of negative balance may require replacement of less than the total urine output. In general, electrolyte disturbances are asymptomatic and require a high index of suspicion and routine monitoring for early detection. Sodium intake should be restricted to 2 to 3 mEq/kg/day, to prevent sodium and fluid retention with resultant hypertension. Ongoing therapy in such patients can be guided by monitoring of plasma and urinary electrolytes. The management of hyperkalemia depends on the onset and severity and is outlined in Table 30. This therapy requires several hours of contact with the colonic mucosa to be effective. In addition, patients with hyperkalemia who continue to have some urine output may benefit from the kaliuresis induced by intravenous administration of loop diuretics such as furosemide, but care should be exercised to avoid fluid depletion and hypotension. In addition to ion exchange resin, such patients should receive calcium gluconate on an emergency basis to counteract the effects of hyperkalemia on the myocardium. Uptake of potassium by cells can be stimulated by infusion of glucose and insulin (in the absence of significant fluid overload), the -agonist albuterol by nebulizer, or intravenous sodium bicarbonate. Administration of sodium bicarbonate should be initiated only in life-threatening situations in which respiratory compensation is inadequate, or the acidosis is contributing to worsening hyperkalemia. In cases of severe or progressive acidosis following shock, serious infections, or other hypercatabolic states, supplemental bicarbonate may be required to correct and maintain arterial pH to more than 7. Adequate calories to account for maintenance requirements and supplemental calories to combat excessive catabolism should be administered. Infants should receive at least 120 Kcal/kg/day, and older children should be administered at least 150% of maintenance caloric intake. If adequate protein and calorie nutrition cannot be achieved because of fluid restriction, renal replacement therapy should be instituted early in the course of the illness. Where possible, treatment should be modified empirically according to systemic druglevel targets. The choice of dialysis modality depends on the clinical status of the patient, the expertise of the physician, and the availability of appropriate resources. It has been reported that approximately half of patients with reduced renal clearance receive drug doses that are 2. The volume of distribution of hydrophilic agents can increase as a result of fluid overload and decreased binding of the drug to serum proteins, and drug doses must be adjusted to account for these changes. To ensure efficacy and prevent toxicity, therapeutic drug monitoring is highly recommended. However, in the absence of drug monitoring (as is the case for most Prognosis and outcome / Congenital heart disease 591 especially useful in the presence of hemodynamic instability and multiorgan dysfunction because it allows for gentle, continuous management of fluid overload. Therefore, extracorporeal circuit volumes that comprise more than 10% to 15% of patient blood volume should be primed with whole blood to prevent hypotension and anemia. Because the prime volume is not discarded, it is important to not reinfuse the blood into the patient at the end of the treatment, to prevent volume overload and hypertension. Survival was lowest in patients with liver disease or transplant (31%), pulmonary disease or transplant (45%), and bone marrow transplant (45%). In a multicenter pooled analysis of 3476 children with hemolytic-uremic syndrome who were followed up for a mean of 4. With no improvement in blood pressure, he was transferred to the intensive care unit. He remained hypotensive and required multiple additional fluid boluses and vasopressors. By the next morning, the initial blood culture results returned positive for Gram-positive cocci in clusters. By the second day, the patient developed oliguria and peripheral and pulmonary edema, and he needed mechanical ventilation. His weight was now 25 kg, and the total fluid intake and output were very imbalanced (6 L in and 1 L out). A kidney ultrasound scan done at the bedside showed bilaterally enlarged and echogenic kidneys, with no hydronephrosis. The blood culture returned positive for methicillin-resistant Staphylococcus aureus. At the time of renal consultation, it was quite obvious that the child in Clinical Vignette 30. However, translational research efforts in humans have yielded disappointing results. Third, the absence of shrunken kidneys on ultrasound makes chronic kidney disease less likely, and the absence of hydronephrosis eliminates obstruction. This child already satisfies the indications for initiation of renal replacement therapy. Second, his high fluid requirements (for nutrition, vasopressor drips, antibiotics, crystalloids and colloids, and blood products) are likely to continue. Given his tenuous clinical condition, the treatment of choice would be continuous renal replacement therapy. In addition, adequate nutrition should be provided (by total parenteral nutrition), potassium intake should be restricted, and additional nephrotoxin use should be avoided. His short-term prognosis remains guarded and depends on the efficacy of renal and other supportive care. He will require long-term follow-up because he is at risk for developing chronic kidney disease in the future. Acute renal failure in critically ill patients: A multinational, multicenter study. Worsening renal function in children hospitalized with decompensated heart failure: Evidence for a pediatric cardiorenal syndrome Demographic characteristics of pediatric continuous renal replacement therapy: A report of the prospective pediatric continuous renal replacement therapy registry. Childhood acute renal failure: 22-year experience in a university hospital in southern Thailand. Temporal relationship and predictive value of urinary acute kidney injury biomarkers after pediatric cardiopulmonary bypass.
Purchase zenegra 100mg without prescription
The American Academy of Neurology recently updated the 1995 American Academy of Neurology guideline for the diagnosis of brain death in patients older than 18 years (Wijdicks et al erectile dysfunction treatment pills purchase cheapest zenegra. Available estimates indicate that >50% of families provide consent for organ donation (Sheehy et al. This gap can be reduced by separating the communication of brain death from the discussion of organ donation (von Pohle, 1996), improving the identification of potential donors (Cloutier et al. Programs that incorporate an in-house presence of the coordinator from the organ procurement agency can be effective in achieving these goals (Salim et al. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Use of intensive care at the end of life in the United States: an epidemiologic study. Applicability and relevance of models that predict short term outcome after intracerebral hemorrhage. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Dealing with conflict in caring for the seriously ill: "it was just out of the question". Predictive value of Glasgow Coma Scale after brain trauma: change in trend over the past ten years. However, physicians require time for a clearer prognosis to emerge and families require time to fully understand the illness and its implications. Hospitals and care teams should be prepared to provide this time to the populations they serve. Withdrawal of support in intracerebral hemorrhage may lead to selffulfilling prophecies. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Technical appendix from Vital Statistics of the United States, National Vital Statistics System, mortality, 2001. Work Table 307: deaths from 39 selected causes by place of death, status of decedent when death occurred in hospital or medical center, and age: United States, 2011. Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Brain death diagnoses and evaluation of the number of potential organ donors in Quebec hospitals. Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. Withdrawal of lifesustaining therapy in injured patients: variations between trauma centers and nontrauma centers. Predicting decline and survival in severe acute brain injury: the fourth trajectory. Factors associated with withdrawal of mechanical ventilation in a neurology/neurosurgery intensive care unit. Who, why and when: stroke care unit patients seen by a palliative care service within a large metropolitan teaching hospital. Outcome prediction in mechanically ventilated neurologic patients by junior neurointensivists. Relationship of national institutes of health stroke scale to 30-day mortality in Medicare beneficiaries with acute ischemic stroke. Validation of an acute ischemic stroke model: does diffusion-weighted imaging lesion volume offer a clinically significant improvement in prediction of outcome Hyperglycemia and clinical outcome in aneurysmal subarachnoid hemorrhage: a meta-analysis. Outcome prediction for individual intensive care patients: useful, misused, or abused Organ donor potential and performance: size and nature of the organ donor shortfall. Outcomes, preferences for resuscitation, and physician-patient communication among patients with metastatic colorectal cancer. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. What matters most in end-of-life care: perceptions of seriously ill patients and their family members. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Discussing prognosis with patients and their families near the end of life: impact on satisfaction with end-of-life care. Failure to engage hospitalized elderly patients and their families in advance care planning. Reasons for dissatisfaction: a survey of relatives of intensive care patients who died. Power and limitations of daily prognostications of death in the medical intensive care unit. The power of compassion: truth-telling among American doctors in the care of dying patients. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Outcomes for surgical and endovascular management of intracranial aneurysms using a comprehensive grading system. Goal setting, prognosticating, surrogate decision making: Primer of Palliative Care. Rate of use and determinants of withdrawal of care among patients with subarachnoid hemorrhage in the United States. Do-notresuscitate orders, quality of care, and outcomes in veterans with acute ischemic stroke. Determination of neurologic prognosis and clinical decision making in adult patients with severe traumatic brain injury: a survey of Canadian intensivists, neurosurgeons, and neurologists. Interobserver agreement and predictive value for outcome of two rating scales for the amount of extravasated blood after aneurysmal subarachnoid haemorrhage. Withdrawal of life-sustaining treatment in a mixed intensive care unit: most common in patients with catastropic brain injury. End-of-life decisions: a cohort study of the withdrawal of all active treatment in intensive care units in the United Kingdom. Racial differences in mortality among patients with acute ischemic stroke: an observational study. Early care limitations independently predict mortality after intracerebral hemorrhage. Improving end-of-life communication and decision making: the development of a conceptual framework and quality indicators. Communication of the cancer diagnosis to pediatric patients: impact on long-term adjustment. Risk score for in-hospital ischemic stroke mortality derived and validated within the Get With the Guidelines-Stroke Program. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Waiting lists continue to grow across the world despite remarkable advances in the transplantation process, from the creation of public engagement campaigns to the development of critical pathways for the timely identification, referral, approach, and treatment of the potential organ donor. The pathophysiology of dying triggers systemic changes that are intimately related to organ viability. The intensive care management of the potential organ donor optimizes organ function and improves the donation yield, representing a significant step in reducing the mismatch between organ supply and demand.
Discount zenegra 100 mg visa
The Glasgow Coma Score is a predictor of good outcome in cardiac arrest patients treated with therapeutic hypothermia erectile dysfunction medication shots zenegra 100 mg without prescription. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Predictive factors of outcome and hemorrhage after acute ischemic stroke treated by mechanical thrombectomy with a stent-retriever. Quantitative rates of brain glucose metabolism distinguish minimally conscious from vegetative state patients. Continuous electroencephalographic monitoring in critically ill patients: indications, limitations, and strategies. Is magnetic resonance spectroscopy superior to conventional diagnostic tools in hypoxic-ischemic encephalopathy Quantitative analysis of the loss of distinction between gray and white matter in comatose patients after cardiac arrest. Radiologicalpathological correlation of diffusion tensor and magnetization transfer imaging in a closed head traumatic brain injury model. Progression of auditory discrimination based on neural decoding predicts awakening from coma. Prediction of awakening from hypothermic post anoxic coma based on auditory discrimination. Admission interleukin-6 is associated with post resuscitation organ dysfunction and predicts long-term neurological outcome after out-of-hospital ventricular fibrillation. Default network connectivity reflects the level of consciousness in non-communicative brain-damaged patients. A quantitative analysis of head injury using T2*-weighted 395 gradient-echo imaging. Anoxic-ischemic encephalopathy: clinical and electrophysiological associations with outcome. Predictors of outcome in traumatic brain injury: new insight using receiver operating curve indices and Bayesian network analysis. All rights reserved Chapter 22 Family discussions on life-sustaining interventions in neurocritical care 1 2 M. Life-sustaining interventions may include intubation and mechanical ventilation, artificial nutrition and hydration, antibiotic treatment, brain surgery, or vasoactive support. A large part of care in the neurosciences intensive care unit is discussion of proportionality of care. This chapter provides a stepwise approach to hold these conferences and discusses ways to do it effectively. Family discussions with the care team are essential to help relieve anxiety and prepare for the withdrawal of care and the dying process (Truog et al. Families have identified communication with healthcare providers and decision making about goals of care as high priorities for improving end-of-life care in Canada (Heyland et al. Decision making about goals of care can be defined as an end-of-life communication and the decision-making process between a clinician and a patient (or a surrogate decision maker if the patient is incapable) in an institutional setting to establish a plan of care. This process includes deciding whether to use life-sustaining treatments (Sinuff et al. There is noteworthy inconsistency in reported mortality and decisions to withdraw care which results in variances in early de-escalation of life-sustaining treatment (MacKenzie et al. Stroke patients seen by palliative care specialists are more functionally impaired, less likely to have decision-making capacity, and more likely to die in hospital (Holloway et al. Compared with nonstroke patients receiving palliative care consultations, stroke patients are more often referred to palliative care for end-of-life and de-escalation of life-sustaining treatment decisions (Holloway et al. In acute ischemic stroke patients treated with thrombolytics, withdrawal of care was instituted in 3. Early deaths are common in stroke, and most occur as a result of brain death or in the setting of de-escalation of life-sustaining interventions when prognosis for recovery is believed to be poor; (Shepardson et al. In addition, like patients, surrogates are often overly optimistic in predicting how well their patient will do over time (Zier et al. Surrogate decision makers consistently overestimated the chances of survival of their patients, even when clinicians offered minimal chance for recovery. In one study, when told, "It is very unlikely that your patient will survive," the median chance of survival reported by 80 surrogates was still above 30%. When the chance of survival was quantified specifically by the provider to be 5%, the chance of survival assigned by surrogates was a significantly higher median value of 15%, with a maximum value of 40% (Zier et al. It is important for physicians to recognize some of these limitations inherent in the use of surrogate decision makers. Patients should make their wishes known as much as possible, so that designated surrogates can be best prepared should their services be needed. Data suggest that physicians often do not talk to patients and families about their options, risks, and benefits (Levinson et al. Studies have demonstrated that communication between physicians and surrogate decision makers is often poor (Malacrida et al. Another study suggested that 33% of family members had symptoms of posttraumatic stress disorder and also reported that family members had a higher burden of symptoms if they were involved in making decisions about de-escalation of life-sustaining interventions and end-of-life care (Azoulay et al. These effects can be lessened by clinician communication and behaviors (Lautrette et al. Family or patient demographics such as age; race and ethnicity; education level; gender; and patient comorbidities were not associated with family member satisfaction in end-of-life decision making (Gries et al. Members of the care team should approach communication with decision makers thoughtfully. In one study, specific communication strategies were associated with increased satisfaction and included: assurances of comfort, providing written information, support for shared decision making, expressions of empathy, specific patient care measures like extubation before death, and family presence at time of death (Hinkle et al. Prognostic disclosure during withdrawal-of-care discussions is associated with increased satisfaction with decision making (Heyland et al. Doubt and uncertainty about the prognosis may result in vague recommendations from the physician about end-of-life decisions (Christakis and Asch, 1993; Christakis and Iwashyna, 1998) and family members could lose trust in the physician and this could also lead to worse family satisfaction in decision making (Reynolds et al. The broad scope of family discussions is complex and the multifaceted needs of patients and their families require an interdisciplinary team of health professionals, including physicians, nurses, therapists, pharmacists, spiritual care providers, social workers, and others. The members of the care team should strive to develop a trusting relationship with the patients and their families. The first meeting should focus on developing a trust and working on a model of care, balancing hope for the best with preparing for the worst (Back et al. The family and healthcare team must simultaneously prepare for survival or decline to death (Lynn, 1997). This allows the providers to determine the extent of the family knowledge and their expectations. The second goal is for the providers to provide intelligible information in accordance with the family needs and desires. The third goal is to support the family by helping them cope with the emotional impact of the present circumstances. The final goal is to cultivate a strategy in the form of a treatment plan with the participation of the family. Proactive and periodic meetings with the family may help increase family satisfaction and decision making (Epstein and Street, 2011). Family members vary as to how much information they wish to know and how active they wish to be in the decision-making process, with some decision makers preferring physicians to take more responsibility for decisions (Heyland et al. Members of the healthcare team should be aware of the burden that surrogate decision makers carry, and tailor their communication styles to their needs and frequently reassure the family members that they have the support of the healthcare team (Curtis and White, 2008). The complexity of the interaction can sometimes create serious miscommunications (Taylor, 1988; Lind et al. In addition to the verbal component of disclosing the bad news, it necessitates other skills: responding to family emotional reactions, involving the family in decision making, dealing with the expectation for cure, the involvement of multiple family members, and the dilemma of how to give hope when a poor outcome is likely. Physicians and other members of the healthcare team can minimize the complexity and risks associated with conveying unfavorable information by understanding the process involved and applying standardized principles of communication and counseling. But the skill to engage realistically with the family, to listen empathically, and to join with them in their suffering helps construct a respectful and effective partnership between the provider team and the family.
Cheap 100 mg zenegra visa
Although the patient has good urine output erectile dysfunction in diabetes patients purchase zenegra with american express, the intensive fellow wants a nephrology consult. Clinical evaluation and interpretation of these complex functions can be categorized into tests for glomerular functions, tubular functions, and hormonal functions (Table 4. Clinicians use broad sets of evaluation tools to judge renal function in adults and children. Dynamic radiologic tests, such as radionuclide renal scans, to evaluate renal perfusion and excretion functions are equally important in evaluation of renal functions. This chapter discusses the pathophysiology, test methodology, and interpretation of clinically useful renal function tests. The pores between the foot processes are slit pores, which are covered by a thin membrane called a slit diaphragm. The anionic heparan sulfate proteoglycans serve to form the charge barrier to the filtration of anionic macromolecules. This action permits the kidney to maintain homeostasis by excreting the daily solute load derived from dietary intake, but preserving the larger proteins. Along the glomerular capillary tuft, a portion of the glomerular filtrate is ultrafiltered into the Bowman space (urinary space). This ultrafiltrate is processed by the renal tubules and collecting duct and eventually leaves the kidney as urine. The LpS in the glomerular capillary is 50 to 100 times that of a muscle capillary, and the capillary hydraulic pressure (and mean gradient favoring filtration [Pgc - Pbs - p]) is much greater in the glomerulus than in a muscle capillary. The plasma oncotic pressure (p) rises in response to the ultrafiltration of protein-free fluid. After the filtration of 20% of the nephron plasma flow, filtration equilibrium is normally achieved. Further filtration at the same plasma flow does not occur because the plasma oncotic pressure equals the hydraulic pressure, and there is no net ultrafiltration pressure. They partially restrict the filtration of albumin Glomerular filtration rate / Clinical assessment of glomerular filtration rate 47 (mean radius, 3. The endothelial cells do not contribute to size selectivity because the endothelial fenestrae are relatively wide open and do not begin to restrict the passage of macromolecules with a radius of less than approximately 40 nm. Modeling of the glomerular filtration barrier suggests that the major portion of the capillary wall functions as an isoporous membrane, but a very small fraction of the filtrate passes through larger pores. The renal clearance of a substance x (Cx) is calculated as follows: Permeability of the glomerular capillaries is 50 to 100 times greater than that of capillaries in muscles, thus allowing for filtration to occur. Starling forces in the glomerular capillary favor ultrafiltration up to the limit of 20% of nephron plasma flow. Both size selectivity and charge selectivity appear to be important in preventing macromolecular transport. Inulin clearance, considered the "gold standard," is seldom performed in clinical circumstances. Inulin is freely filtered and not protein bound, and is not reabsorbed, secreted or metabolized by the kidney. Under current practice, the insertion of a bladder catheter for renal functional measurement alone is not justifiable, and therefore urine collections are obtained every 20 to 30 min, as dictated by the urge of the patient to urinate. In this case, urine flow is maintained high by providing an initial oral fluid load of 500 to 800 mL water/m2 and replacing urine output with intake of water (mL for mL). First, some children may not be toilet trained and are unable to provide accurate collections of timed urine. Technical difficulties encountered in performing inulin infusions, reaching a steady state of inulin distribution, and accurately measuring inulin concentrations in plasma are added concerns. In addition, the inulin assay is not very specific, and it can be potentially hazardous (boiling acid reagents). These problems have rendered the standard inulin clearance impractical for use in children. Therefore, it is possible to determine the plasma clearance by infusing the substance at a constant rate until a steady state is achieved. Glomerular filtration rate / Clinical assessment of glomerular filtration rate 49 this constant infusion technique has used inulin, although other markers, especially radionuclide tagged tracers, also can be used (discussed later). After equilibration of the marker in its distribution space, the excretion rate equals the infusion rate. The renal clearance of the molecule can then be calculated from the rate of infusion and the concentration in plasma. The relative constancy of Cr production and its urinary excretion in the steady state helps one analyze for completeness of the collection. On the day of the test, the child is asked to void and empty the bladder in the morning (7 a. All urine voided in the next 24 h is collected in the container as part of this collection. The volume of urine is noted accurately, and the urine is analyzed for Cr concentration. Urinary Cr excretion (Cr index) should generally exceed 15 to 20 mg/kg/day in children older than 3 years of age and is 20% higher than that for pubertal adolescent boys. Nevertheless, daily variation in urinary Cr excretion results in a standard deviation of 10% to 15%. In addition, Cr concentration is affected, to a small extent, by dietary intake of meat, exercise, and pyrexia. More importantly, it is well known that Cr is secreted by the renal tubules; this secretory component accounts for approximately 10% of the urinary Cr excretion in normal individuals. Creatinine was measured using a modification of the Technicon Autoanalyzer Jaffe assay. Plasma creatinine and urea concentration in children: normal values for age and sex. The urinary excretion of Cr is determined by muscle catabolism and is hence an index of muscle mass. It is eliminated from the body exclusively by the kidneys, primarily by glomerular filtration, but also to a small extent by tubular secretion. Glomerular filtration rate / Clinical assessment of glomerular filtration rate 51 from serum Cr and some parameter of body habitus. This formula is also based on the relationship that Cr clearance is reciprocally proportional to serum Cr. The newer generation of autoanalyzers determine serum Cr enzymatically, using the creatinase methods. Although the enzymatic Cr method appears to agree with "true" Cr obtained from the Jaffe reaction after Fuller earth absorption, some manufacturers use calibration factors (bias) to produce Jaffe-comparable results. This bias is not linear and therefore is unlikely to improve the accuracy of serum Cr determination in children. Without the bias, the enzymatic Cr generally runs 10% to 20% lower than those measured by the Jaffe method. This formula has limited utility in pediatrics because of the inaccuracies in children 8 years old or younger. Serum cystatin C during 30 postnatal days is dependent on the postconceptional age in neonates. Serum Cys-C levels are high in full-term neonates and gradually decline in the first 4 months of life. Serum Cys-C levels are even higher in preterm infants and appear to be inversely influenced by gestational age (Table 4. Beyond the first year, the constancy of Cys-C is relatively stable and is largely independent of muscle mass, gender, body composition, and age. Because Glomerular filtration rate / Clinical assessment of glomerular filtration rate 53 Table 4. Reference ranges for plasma cystatin C and creatinine measurements in premature infants, neonates, and older children. Initially, the concentration falls rapidly but at a progressively diminishing rate because of diffusion of the marker in its distribution volume as well as its renal excretion. Thereafter, the slope of the decline of plasma concentration reflects predominately its renal excretion rate.