Buy cheap tadapox on-line
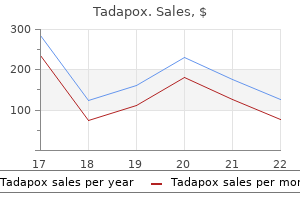
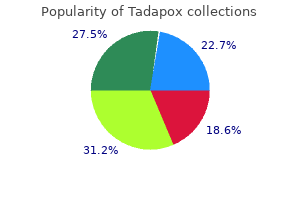
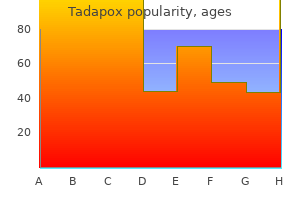
In a report of 31 patients with craniocervical dislocation erectile dysfunction causes alcohol cheap tadapox 80 mg mastercard, 23 survived with treatment by occipitocervical fusion;6 improved neurologic function was seen in 5 patients, 9 had no change, and 9 remained neurologically intact. Patientreported outcomes showed persistent functional disabilities in survivors, but low levels of chronic pain. Atlas Fractures Atlas fractures are common injuries, occurring in 10% of all cervical spine fractures. Atlas fractures occur in combination with axis fractures in approximately 20% of patients. However, review of long-term outcomes showed poorer quality of life after an atlas fracture, which was independent of the treatment given. Radiographs should be scrutinized for displacement of the lateral masses, which is seen best on the open-mouth view. D, Displaced lateral mass fracture (arrows) of the atlas with transverse ligament avulsion. Outward displacement of the lateral masses results in loss of craniocervical and atlantoaxial motion and, rarely, cranial migration of the dens into the foramen magnum. The possibility of lateral mass screw fixation to maintain alignment is appealing because it results in osteosynthesis without fusion. Several techniques are possible, including posterior, transoral, transnasal, and transcervical. One study reviewed 22 patients treated with posterior fixation at 2-year follow-up. In unstable bursttype fractures, the transverse ligament is disrupted and may not adequately heal despite direct fixation of the atlas ring, resulting in delayed C1-C2 instability. Most commonly, this occurs following fractures, including odontoid, atlas, and occipital condyle fractures, as well as injuries to the transverse ligament. These injuries result in an increase in the atlanto-dens interval and have a poor prognosis for healing. Isolated transverse ligament injuries are best treated surgically with atlantoaxial fusion. In children, a trial of nonsurgical treatment by reduction and immobilization is recommended. Illustrations demonstrates atlantoaxial rotatory instability classification, with the direction of rotation (arrows). This type of instability is associated with both transverse ligament and alar ligament insufficiency. Three injury types are considered: traumatic spondylolisthesis of the axis, odontoid fractures, and C2 body fractures. In addition, axis fractures occur frequently in combination with atlas and other cervical spine injuries. Traumatic Spondylolisthesis of the Axis Traumatic spondylolisthesis of the axis is a common fracture and has many variants. Initially described as a pars interarticularis fracture secondary to judicial hangings, traumatic spondylolisthesis occurs more frequently from hyperextension mechanisms. This injury is a traumatic separation of the anterior elements from the posterior elements. Classically, fractures occur in the pars interarticularis, but many variations are present. Other fracture locations include the pedicles, posterior vertebral bodies, and laminae. The fractures may not be symmetric between the sides, implying an oblique vector mechanism. Recently, small case series have focused on various surgical techniques: anterior C2-C3 fusion with plate, osteosynthesis fixation with a C2 pedicle screw, C2-C3 fixation using pedicle screws, and posterior C1-C3 fusion. In one report of 23 patients treated with primary fixation, all experienced healing. Pedicle screw fixation across the fracture combined with C3 pedicle or lateral mass screws has been shown to be safe and effective. The treatment requires open reduction; the facet dislocations cannot be reduced with closed traction because of the pars interarticularis fractures. Treatment of the traumatic spondylolisthesis component of this injury can be nonsurgical or by using pedicular fixation. Odontoid Fractures Classification the classic Anderson and Alonzo system provides excellent prognostication and defines treatment pathways. Odontoid fractures in geriatric patients are associated with erosive atlantoaxial arthrosis, which weakens the dens, and thus are considered insufficiency fractures. Treatment All treatment decisions are based on low-quality evidence because a Cochrane systematic review could not identify any studies with criteria of high-enough quality on which to base treatment decisions for any fracture type. At 64-month follow-up, 92% had bony healing, 4% had fibrous pseudarthrosis, and 4% had unstable pseudarthrosis. Patients had mild to moderate symptoms of pain, functional disability, and psychologic disturbance based on healthrelated quality of life. The odontoid screw provides the advantage of stability to allow healing without loss of atlantoaxial motion. A systematic review of odontoid screw fixation reported a 10% nonunion rate, a 10% rate of revision surgery, and a 10% incidence of persistent dysphagia. One biomechanical study found no difference when comparing fixation with one versus two screws;46 another study reported higher fusion rates in a clinical series using two screws. The Magerl C1-C2 transarticular fixation and C1 lateral mass screws with C2 pedicle screws are the most common methods. Fusion rates are higher with the posterior technique compared with the anterior odontoid screws, but comparisons of clinical outcomes are lacking. Combined Atlas and Axis Injuries Combined atlas and axis injuries are common, occurring in 25% of injuries in the upper cervical spine and 3% to 4% of all cervical injuries. The latter is reserved for those patients who cannot be managed nonsurgically or who have substantial displacement of the axis. The surgical procedure needs to be individualized depending on fracture morphology and can include Magerl transarticular screws, the Harms technique, or occipitocervical fusion. Fractures in Geriatric Patients Odontoid fractures in elderly patients are reaching epidemic proportions and are recognized as resulting in high rates of morbidity, mortality, and poor quality of life. Increasingly, odontoid fractures are being recognized as insufficiency fractures, with erosive disease contributing to fracture in more than 50% of patients. One study reported that nonsurgical care was associated with nonunion in 20% of patients compared with only 5% in surgically treated patients. Treatment failure, either death or worsening of disability, occurred in more than 50% of patients and in both treatment groups. One study reported that patients in whom nonunion developed after nonsurgical treatment had similar outcomes to those who experienced union. A 2013 study found that surgically treated patients had improved health-related outcomes and lower mortality than nonsurgically treated patients. Axis Body Fractures Fractures of the axis body are a heterogeneous group of injuries that are usually stable and have a good prognosis. A systematic review classified these injuries by orientation of the fracture planes. Lower Cervical Spine Injuries Classification Many classification systems for lower cervical spine injuries have been described based on presumed mechanism and morphologic characteristics. Recent advances focus on quantification of stability, modern imaging, and better predictive models to aid decision making for treatment. Allen and Ferguson Classification the Allen and Ferguson system is a mechanistic classification with the major patterns of compressive flexion, vertical compression, distractive flexion, compressive extension, distractive extension, and lateral flexion. Disruption of each column is graded on a scale of 0 to 5 and the sum of scores ranges from 0 to 20, with a sum greater than 7 generally requiring surgical treatment. Cervical Spine Instability the classic definition of spinal instability is "the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain. Checklists have been proposed, incorporating the variables of anterior or posterior column injury, translation, excessive angulation, distraction, and neurologic injury, but these have not shown substantial clinical use or validity. Long-term goals are to maximize neurologic recovery while providing lasting stability to the injured segment. In addition to avoidance of further complications, the number of treated levels should be minimized, as should postoperative immobilization. Although algorithms may assist in the decision-making process, optimal treatment depends not only on neurologic status, the severity of injury, and the injury type, but also on concomitant injuries, comorbidities, and other patient-specific factors.
Amygdalin (Apricot Kernel). Tadapox.
- How does Apricot Kernel work?
- Cancer. Apricot kernel and the active chemical amygdaline or Laetrile is not effective for treating cancer.
- What is Apricot Kernel?
- Dosing considerations for Apricot Kernel.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97133
80 mg tadapox mastercard
The uncinate processes form an important landmark for the lateral extent of anterior decompression procedures erectile dysfunction pink guy cheap tadapox line. Posteriorly, the cervical vertebrae are characterized by bifid spinous processes and large lateral masses, but not the elongated transverse processes found in the thoracic and lumbar regions. Lateral mass instrumentation is most commonly used for posterior fixation from C3 through C6 because of its technical ease and safety. The starting point for C7 pedicle screw instrumentation is the upper outer quadrant of the lateral mass. A laminoforaminotomy to palpate the pedicle may improve the accuracy and safety of this procedure. Thoracic Spine Several unique anatomic characteristics are important to understand when assessing and treating thoracic spinal pathology. This articulation adds to the inherent stability of the thoracic spine and is thought to be a major contributing factor to the decreased frequency of degenerative pathology in the thoracic region compared with the cervical and lumbar regions. The thoracic facet joints are oriented in the coronal plane to allow for axial rotation. The ratio of the canal to the spinal cord is relatively small in the thoracic spine, which increases the risk of neurologic injury even with small amounts of canal incursion. Close study of thoracic anatomy is mandatory before instrumentation in this region, and alternative techniques should be considered. Such techniques involve the use of hooks, translaminar screws, or an in-out-in trajectory in which the screw intentionally breaches the lateral pedicle wall and abuts the rib head for added stability. Thoracic pedicles have been shown to expand in diameter to accommodate larger screws placed to maximize pullout strength. Progressing cranially to the midthoracic spine, the starting point shifts to a more medial and cephalad position. Alternatively, the funnel and slide techniques can be used to identify the cancellous bone found within the pedicle in contrast to the cortical bone found on the anterior margin of the transverse process. The anatomic technique, with the screw angled caudally in line with the true pedicle anatomy, allows for placement of a longer screw but necessitates the use of a polyaxial screw, which can limit the success of deformity correction. The straightforward approach with the screw angled in line with the end plate, as opposed to the pedicle, has gained popularity because it allows placement of a fixed-angle screw to obtain more powerful deformity correction. The aorta lies on the left anterolateral aspect of the vertebrae and follows the spine caudally, dividing into the common iliac arteries at or around the L4-L5 disk level. The distance from the margin of the vertebrae to the aorta decreases from the cephalad to caudad thoracic spine (4. The aorta is located more posterolateral and closer to the vertebrae at the levels above the apex of the curve. Below the apex of the curve, the aorta is located closer to the midline, which increases the risk of injury at the thoracolumbar junction in patients with Lenke type 1 curves. The use of navigation systems to improve the accuracy of pedicle screw placement is especially useful in the thoracic spine because the margin for error is small. This technique can restore disk height (which in turn provides indirect decompression of the neuroforamen and spinal canal), restores segmental lordosis, and improves spinal alignment. The large surface area within the disk and the compressive environment also provide a favorable setting for bony fusion. The interbody space can be accessed with a variety of approaches, including posterolateral, anterior, or lateral. In the sagittal plane, the cage makes maximal contact with the end plates at all four corners of the interbody device, minimizing the risk for cage migration. Regardless of the approach used, an understanding of the anatomy and biomechanics of the vertebral end plates is essential for the success of the procedure. The bony end plate lies between a layer of hyaline cartilage adjacent to the intervertebral disk and the trabecular bone of the vertebral body. The strength and stiffness of the lumbar end plates increase in the more caudal vertebrae. Within an individual end plate, both strength and stiffness increase from the center to the periphery of the plate. Overall strength and stiffness of end plates decrease by up to 30% and 46%, respectively, at higher grades of disk degeneration, with the most substantial changes in the periphery of the end plates. The motion segments above L4 and those in older patients are especially vulnerable to motion segment degeneration. Careful assessment of end plate morphology and the degree of degeneration are important for decreasing interbody cage subsidence and migration rates. Instrumentation Transpedicular screw fixation from an open posterior approach has become the standard technique for lumbar spine instrumentation because it provides increased strength and stiffness from three-column vertebral fixation. Cortical bone of the pars interarticularis and a medial-to-lateral trajectory can be used to obtain fixation while reducing the exposure required for instrumentation compared with a traditional trajectory. The starting point for the screws in a cortical bone trajectory is 2 to 3 mm medial to the lateral border of the pars interarticularis and caudal to the facet joint. This can preserve innervation to the multifidus muscle and decrease intraoperative blood loss. The cortical bone trajectory also can minimize disruption of the facet joint immediately cranial to the fusion level. This trajectory can be used for all lumbar vertebrae; however, caution should be used at higher levels because the pars interarticularis becomes thinner and the pedicle diameter is smaller, which substantially increases the technical difficulty of screw placement and theoretically increases the risk of pars fracture or inadvertent cortical perforation. Techniques using facet and translaminar screws were originally described decades ago; however, the use of these techniques in posterior fixation has recently received renewed attention. Although facet and translaminar screws do not provide rigidity equivalent to that of pedicle screws, successful outcomes have been reported when these alternative screw techniques were used as adjuncts in anterior interbody fusion. The addition of pelvic fixation overcomes this challenge by placing fixation across the center of rotation of the pelvis and out of the plane of the remainder of the instrumentation. Initially, the Galveston technique involved the placement of an L-shaped rod between the tables of the ilium. Classic iliac fixation uses a starting point in or just medial to the posterior superior iliac spine. Although this technique is relatively straightforward, it requires lateral connectors to join to the medial pedicle screw construct. A more medial starting point on the posterior superior iliac spine can reduce implant prominence but makes connection of the remainder of the construct more difficult. In this S2-alar-iliac technique, the screw tulips are aligned with the remainder of the construct and are unlikely to be symptomatically prominent; however, because the screws cross the sacroiliac joint, irritation or degeneration of the sacroiliac joint can result. Recent evidence suggests that the technique is associated with a lower revision rate. This understanding has implications in the diagnosis and treatment of spinal pathology and is essential knowledge for any surgeon treating patients with common and often debilitating spinal disorders and injuries. Key Study Points A detailed knowledge of spine anatomy is a prerequisite for safe and effective nonsurgical and surgical treatment of patients with spine pathology. Growing evidence exists that the health and function of the multifidus muscles has an effect on clinical function in the lumbar spine. The freehand technique for thoracic pedicle screw instrumentation is safe and effective. In patients with spine deformity, the relationship of the great vessels to the spine may be altered. The morphology and degenerative state of the vertebral end plate is an important consideration when applying interbody instrumentation. Increasing evidence supports the safety and efficacy of the cortical bone screw trajectory and S2-alar-iliac fixation. A review on the development and classification of vertebral bony anomalies is presented. No change in the multifidus cross-sectional area or facet deterioration was reported. The cross-sectional area and fat content of paraspinal musculature in patients with chronic recurrent and acute low back pain was examined. The most consistent finding was paraspinal muscle atrophy (specifically in the multifidus) in patients with chronic low back pain.
Buy tadapox australia
For patients with substantial cord compression erectile dysfunction what doctor purchase 80mg tadapox fast delivery, a slight flexion alignment is initially preferred. If fusion is to be performed, it is important to restore lordosis after decompression but before final implant tightening. Surgical Steps the spinous processes of C2 and C7 are marked, and correct levels are identified using fluoroscopy. The skin and subcutaneous tissue can be infiltrated with a 1:500,000 epinephrine solution to help with hemostasis. The dissection is then deepened, keeping strictly within the median raphe to avoid bleeding and muscle damage. After the spinous process is reached, further dissection is performed subperiosteally from distal to proximal using electrocautery; self-retaining retractors are then placed bilaterally. Depending on the pathology treated, a laminectomy is performed in a piecemeal or en bloc fashion. Specific Instructions: Laminoplasty When performing a laminoplasty, patient positioning, skin incision, and lamina exposure are like those of the conventional posterior approach, but care should be taken to preserve the C2 and C7 attachments. Preservation of the C2 and C7 muscle attachments theoretically reduces loss of lordosis and neck pain caused by mechanical instability after laminoplasty. Posterior Minimally Invasive Foraminotomy the minimally invasive approach to the cervical spine has been shown to reduce the length of hospital stays and postoperative pain medication requirements. This approach is mainly useful in treating radiculopathy secondary to lateral disk herniation without instability and kyphotic deformity. A prone position with a slight reverse Trendelenburg position can reduce bleeding. When small incisions are planned, fluoroscopy is relatively more important for identification and confirmation of the target level before the incision is made. Surgical Steps A 3-cm midline skin incision is placed with the target disk level as the center. The superficial dissection is continued through the midline until the cervical fascia is encountered, which is divided longitudinally in the midline to expose the tips of the spinous process. Further dissection is performed subperiosteally elevating the paraspinal musculature from the lamina, spinous process, and facet joint using a Cobb elevator and electrocautery. At this stage, a self-retaining or handheld retractor is placed to reflect paraspinal muscles from the target interlaminar area. A high-speed burr is used to remove the caudal edge of the upper lamina and the medial third of the facet. This resection may be completed with a small Kerrison rongeur, but no more than half of the facet should be resected. Microscope magnification and protection of the nerve root with a small Penfield retractor is suggested. Bleeding from the perineural venous plexus can usually be controlled with hemostatic agents and cottonoid packing. The shaded region of the lamina, facet region, pedicle, and vertebral body can be completely resected if a tumor or infection is present. This approach is indicated in the treatment of tumors, infections, spine fractures, and spine dislocations. Intraoperative fluoroscopy or plain radiography is used to locate the intended surgical level. A posterior vertical midline incision is made, and the thoracolumbar fascia is divided in the midline. Total laminectomies of the affected levels are performed using a high-speed burr or Kerrison rongeurs. After the posterolateral decompression is completed, the disks corresponding to the upper and lower corpectomy levels are removed. The corpectomy is performed using curets, rongeurs, and osteotomes from the posterolateral corner through a transpedicular approach. The exiting nerve root often is transected to improve exposure; however, the T12 and T1 roots should be preserved whenever possible because of the potential for more important radicular sequelae. The posterior longitudinal ligament can be resected if needed, and the completeness of the corpectomy can be judged by direct visualization of the anterior longitudinal ligament. Care should be taken to preserve the bony end plates at the upper and lower levels of the corpectomy to avoid subsidence and enhance graft incorporation. Advantages the advantages of the posterolateral transpedicular approach include circumferential decompression of the spinal cord and stabilization through a single skin incision. This approach obviates the need for single-lung ventilation and the lateral decubitus positioning required for standard anterior thoracic approaches. Minimally Invasive Thoracotomy Minimally invasive thoracotomy uses a smaller incision and generally smaller retractors compared with traditional open transthoracic exposures. Generally, a 5- to 6-cm skin incision is used to reach the anterior and lateral surface of the T5-T10 vertebral bodies. Surgical Steps Minimally invasive thoracotomy is performed with the patient placed in the right lateral decubitus position and under general anesthesia. Because this procedure requires single-lung ventilation, a double-lumen endotracheal tube is used. The intended spinal level is identified by counting the ribs and is confirmed with fluoroscopy. The serratus anterior muscle is separated along the direction of its fibers to expose the underlying rib and intercostal space. If the affected level is above T7, the ventral edge of the latissimus dorsi is retracted or incised. The anesthesiologist generally reduces inspiration volume before the pleural incision to avoid inadvertent injury to the lung. Self-retaining rib retractors enable clear visualization of the lateral aspect of the spine. A spinal needle is inserted into the disk space and radiography is used to confirm the target spinal level. With this approach, the anterolateral circumference of the thoracic vertebra can be visualized. Segmental vessels can be ligated or clipped and cut if vertebral body access is needed. A radiolucent sponge is placed anterior to the spine to protect the aorta during the remainder of the surgical procedure. However, there is a substantial learning curve among surgeons not familiar with transthoracic approaches and those unaccustomed to working without the assistance of a thoracic surgeon. Posterior Midline Approach to the Thoracolumbar Spine the posterior midline approach is perhaps the most common approach used by spine surgeons in routine practice. This approach provides direct visualization of the spinous process, laminae, pars interarticularis, facet joints, transverse process, and pedicles. It can be used to perform diskectomy, direct decompression, osteotomies, and posterior interbody fusion and to place pedicle screws and cortical screws. Patient Position the posterior midline approach is performed with the patient prone on a spinal frame, with the abdomen hanging freely to decrease blood loss. Fluoroscopy can be used to mark the target level before the skin incision is made. The skin and subcutaneous tissue are infiltrated with 1:500,000 epinephrine, which may help in hemostasis. Surgical Steps A midline skin incision corresponding to the target vertebrae is performed, and further dissection down the midline is accomplished using electrocautery to reach thoracolumbar fascia, which are incised in line with the skin incision. Cerebellar or Gelpi retractors are used to help maintain sufficient tissue tension during exposure. The tendinous attachments of muscles over the spinous process are released, followed by subperiosteal exposure of the lamina of interest using a Cobb elevator. This procedure can be performed unilaterally or bilaterally, depending on surgical indications. At this point in the procedure, the paraspinal muscles can be held laterally with self-retaining retractors.
Tadapox 80mg overnight delivery
Thus injections for erectile dysfunction video cheap tadapox 80 mg online, spinal column stability exists if gravity and the alar ligaments, which project laterally and slightly cranially from the dens to the anterior-medial edge of the foramen magnum, and the tectorial membrane ligaments hold the occipital condyles downward. The tectorial membrane, which is the thickened continuation of the posterior longitudinal ligament spanning between the dens and the foramen magnum, is the other essential restraining ligament. The atlas is a ring-like structure with large lateral masses connected by a short anterior arch and a longer posterior arch. The posterior arch is notched on its superior surface by the vertebral artery, which can be considered a weak location where fractures can occur. The inferior surface of the atlantal lateral masses is semiconvex and located directly above a similar facet articulation of the axis. These articulations have no bony stability to allow gliding and rotation needed for atlantoaxial rotation. Most conspicuous is the dens or odontoid process, which projects in a cranial direction behind the atlantal anterior arch. Forward translation is prevented by the transverse ligament and secondarily by the alar ligaments. Biomechanically, the atlas acts as a bushing while the stabilizing ligaments extend from the axis to the occiput. This structure thickens horizontally, creating the transverse ligament that spans behind the dens and attaches to tubercles on the atlas. The transverse ligament prevents anterior atlantoaxial subluxation by maintaining the dens in apposition to the atlantal anterior arch. The anterior atlantal ligament extends from the posterior aspect of the atlantal anterior arch to the ventral aspect of the dens. Subaxial Anatomy the subaxial cervical vertebrae have similar morphology, although they become larger caudally. Short, obliquely oriented pedicles connect the vertebral body to the lateral masses. The lateral masses are rhomboid shaped when viewed laterally and square shaped when viewed dorsally. The upward and downward projections of the lateral masses are the superior and inferior facets, respectively. Posteriorly, the lateral masses are connected by thin lamina that thickens in the midline. The anulus fibrosus has a strong collagenous structure and is important for stability. Two-paired synovial facet joints are oriented upward and help prevent anterior translation. The anterior and posterior longitudinal ligaments are broad and these ligaments are located on the anterior and posterior vertebral bodies, respectively. The nuchal ligaments are the ligamentum nuchae, which strongly attach to the external occipital protuberance, C2, C7, and T1, and the supraspinatus and interspinous ligaments. Occipital Condyle Fractures Occipital condyle fractures occur in 1% to 3% of patients with blunt craniocervical trauma; in patients with an initial Glasgow Coma Scale score of 3 to 6, the incidence is reported as high as 4. Impaired consciousness limits physical examination, but abnormalities in cranial nerve function suggest occipital condyle fractures. The critical determination of stability is based on displacement between the occipital condyles and C1 lateral masses. Treatment with a halo vest may be considered for patients with less severe injuries. A study of 31 patients with occipital condyle fracture with a 27-month follow-up found low levels of disabilities, but 21% of patients had moderate or severe disability. Another study reported similar results in 28 patients with nondisplaced fractures treated nonsurgically. This injury continues to be difficult to diagnose, and failure to make a diagnosis results in neurologic injury or death. Classification Injuries are traditionally classified by direction, which is not clinically helpful because the direction of displacement simply reflects the head position relative to the thoracic spine. Patients are immobilized with a collar, and transportation within the hospital should be limited. In displaced craniocervical injuries, reduction and stabilization may be achieved with a halo vest. Definitive Treatment For displaced injuries, occipitocervical fusion is recommended. A systematic review found that neurologic worsening developed in only 1 patient of 29 treated with early surgery; of 12 patients treated nonsurgically, treatment was successful in 5 and neurologic injury or inability to achieve stability occurred in 7 patients. The use of the halo vest is limited because of poor patient acceptance and its limited effectiveness in the lower cervical spine. Most patients with stable injuries are treated with a hard collar or cervicothoracic orthosis; it is recommended that these devices be applied by a certified orthotist. In cognitively impaired patients, the risk of decubitus ulceration is present; therefore, skin checks should be performed frequently. After orthosis application, the patient can be mobilized and an upright radiograph obtained, which is essential to confirm the efficacy of nonsurgical management. Displacement, angulation, development of increased pain, or any neurologic change indicates treatment failure and may require surgical treatment, which occurs in approximately 5% to 10% of patients. Education of the patient and family is essential to ensure proper brace management. Geriatric patients may have dysphagia when in an orthosis with aspiration risk, and a swallow consultation should be obtained before feeding. Because activities of daily living may be compromised, an occupational therapy consultation is recommended. The double arrows show that there is symmetric spread between the spinous processes indicating the absence of posterior ligamentous injury. Type A0 injuries have no bony injury such as a central cord syndrome or have isolated process fractures. Isolated lamina fractures are uncommon and have fracture lines medial to the facet but lateral to the spinous process. Ventral displacement into the spinal canal with associated neurologic deficit has been described. Spinous process fractures may be avulsion injuries of the lower cervical or upper thoracic levels from the pull of the supraspinous ligament58 or a result of impaction occurring during hyperextension. However, there may be associated posterior ligamentous disruption; therefore, vigilance is required to ensure maintenance of alignment with orthotic treatment. Transverse process fractures are defined as a fracture of any portion of the transverse process and can extend into the foramen transversarium. Type A1 injuries are compression fractures involving a single end plate; type A2 fractures involve both end plates. Type A fractures associated with flexion-distraction injuries are classified as type B injuries. Type A1 and A2 fractures are uncommon in the cervical spine and usually are secondary to low-energy trauma in the presence of osteoporosis. The spinal cord is compressed and edema is seen within the ventral aspect of the spinal cord. C, Lateral fluoroscopic view obtained after C5 corpectomy and plate reconstruction. D, Lateral radiograph shows excellent realignment following anterior corpectomy with strut grafting and application of an anterior plate. Type A3 and A4 burst fractures without posterior osteoligamentous involvement occur as a result of axial loading and are associated with the risk of neurologic injury. In the absence of substantial retropulsion or neurologic injury, they may be managed in a rigid orthosis with close radiographic follow-up. If neurologic injury is present, surgical treatment with anterior corpectomy, strut grafting, and plating should be performed. Type B Injuries Type B1 injuries are distraction injuries through the posterior bony structures.
Discount 80 mg tadapox fast delivery
Mesodermal elements such as cartilage impotence your 20s purchase generic tadapox canada, bony spicules, teeth, adipose tissue, and muscle may be prominent features. Mucinous-appearing intratumoral cysts are common and are often lined with respiratory or gastrointestinal epithelium (20-30). The size of a mature teratoma varies from relatively small pineal lesions to huge holocranial lesions with massive extracranial extension into the orbit, face, ears, and oral cavity. Hypodense fatattenuation tissue surrounds a densely calcified component that grossly resembles a tooth. A lobulated mixed signal intensity component is present in the posterior 3rd ventricle. Neoplasms, Cysts, and Tumor-Like Lesions 628 Teratoma With Malignant Transformation Teratomas with malignant transformation generally arise from immature teratomas and contain somatic-type cancers such as rhabdomyosarcoma or undifferentiated sarcoma. Other Germ Cell Neoplasms Germinomas are by far the most common of the germ cell neoplasms. These include yolk sac (endodermal sinus) tumor, embryonal carcinoma, choriocarcinoma, and mixed germ cell tumor. Differentiating intracranial germ cell neoplasms on the basis of imaging studies alone is problematic. Many express different oncoproteins, so immunohistochemical profiling is an essential part of diagnosis. Yolk sac tumors are composed of primitive epithelial cells in a loose, variably cellular myxoid matrix. Embryonal carcinoma is another tumor that contains large, anaplastic epithelioid cells that are arranged in sheets, cords, and nests. Imaging findings are nonspecific and may be indistinguishable from germinoma (20-36). Note that the mass fills most of the left lateral ventricle, extends across the midline into the right lateral ventricle, and inferiorly through the foramen of Monro into the third ventricle. Neoplasms, Cysts, and Tumor-Like Lesions 630 Choriocarcinoma Most choriocarcinomas develop within or outside the uterus following a gestational event ("gestational" choriocarcinoma). Nongestational choriocarcinomas can arise from germ cells in gonadal or extragonadal midline locations. They are composed of mononucleated trophoblastic cells admixed with large multinucleated syncytiotrophoblastic cells. Primary glial neoplasms such as astrocytoma (including glioblastoma) (20-38) and oligodendroglioma (20-39) can occur within the pineal gland itself as can melanoma arising from pineal melanocytes (20-40). Metastases from extracranial sources also occasionally present as pineal masses (20-41). In general, imaging findings with intrinsic pineal gland masses are nonspecific and do not permit differentiation between the broad spectrum of histologic types, so biopsy is necessary to guide patient management. A general approach to evaluating pineal region masses is delineated in the box below. Mixed germ cell tumor with germinomatous and mature teratomatous elements was found at surgery. No systemic source could be identified, so this is a presumed primary melanoma of the pineal gland. The most common of these tumors are the embryonal neoplasms, a heterogeneous group of primitive neoplasms with protean histopathologic manifestations. The rapidly evolving molecular classification of brain tumors has fundamentally changed the understanding of embryonal neoplasms. In the 2016 World Health Organization schema, the classification of the largest group of embryonal neoplasms-medulloblastoma-was revised to reflect both recognized histopathologic variants and clinically relevant molecular subgroups. Embryonal neoplasms other than medulloblastomas have also undergone substantial changes. They exhibit highly cellular sheets and lobules of uniform small round "blue cells" with neuroblastic (Homer-Wright) rosettes and perivascular pseudorosettes. Desmoplastic/Nodular Medulloblastoma and Medulloblastoma With Extensive Nodularity. This variant is characterized by abundant islands of reticulin fibers interspersed in a background of less differentiated small round blue cells (21-2). Large anaplastic-appearing cells with nuclear pleomorphism, high mitotic activity, and abundant apoptosis are characteristic (21-3). Glistening, translucent "sugar icing" metastases coat cerebellum; "drop" metastases along spinal cord, cauda equina. Neoplasms, Cysts, and Tumor-Like Lesions 638 (21-6A) Autopsy specimen from an adult shows desmoplastic medulloblastoma as a firm, fibrous-appearing, somewhat lobular and laterally located mass in the cerebellar hemisphere. Large cell/anaplastic variants do occur but are uncommon, whereas desmoplastic histology is rare. They are located within the fourth ventricle and focally infiltrate the dorsal brainstem and vermis. Dense sheets of uniform cells with round or oval hyperchromatic pleomorphic nuclei surrounded by scanty cytoplasm are the typical appearance ("small round blue cell tumor") (21-1A). Neuroblastic (Homer-Wright) rosettes-radial arrangements of tumor cells around fibrillary processes-are found in 40% of cases (21-1B). In one-third of children younger than 3 years, the diagnosis is made only after life-threatening signs of intracranial hypertension appear. If dense tentorial or falcine calcifications are present, the patient should be evaluated for basal cell nevus (Gorlin) syndrome. Enhancement patterns show striking variation, ranging from minimal to patchy to marked. Obstructive hydrocephalus and a small focus of calcification in the mass are present. Note subtle pial enhancement along the tectum, in the hemispheric sulci, and coating the spinal cord. Note mass effect on the 4th ventricle and ill-defined hypointensities in the right cerebellar hemisphere and vermis. Occasionally a diffusely infiltrating medulloblastoma presents without a dominant enhancing mass. Increasing head circumference and signs of elevated intracranial pressure are common. Headache, nausea, vomiting, and visual disturbances are typical presenting symptoms. Necrosis and intratumoral hemorrhages are common, as are dystrophic calcifications. All sequences exhibit heterogeneous signal intensity with T1 shortening (21-15A) and T2* blooming secondary to intratumoral hemorrhage. Heterogeneous enhancement with solid and rim enhancement is typical (21-17) (21-18). It is the most common extracranial solid cancer in childhood and the most common overall cancer of infants. Multiple bilateral lesions involving both the inner and outer tables of the skull are typical. Linear hypointensities that represent the "hair on end" bony spicules can sometimes be identified within the strongly enhancing masses (21-20). Note the striking orbital spiculated periostitis with adjacent soft tissue masses. The modified Kadish classification is used for staging and recognizes four stages: stage A, tumors that are localized to Esthesioneuroblastoma Terminology. Embryonal Neoplasms the nasal cavity; stage B, nasal cavity and paranasal sinuses; stage C, orbital and intracranial extension; stage D, cervical and distant metastases. Nodal and/or distant metastases to lung, bone, and liver develop in 10-30% of patients. A "dumbbell" shape-the upper portion in the anterior cranial fossa and the lower portion in the nose with the narrowest aspect at the cribriform plate-is seen with large masses (21-22). The lesion extends superiorly into the anterior cranial fossa and laterally into the right orbit. Nodes harboring metastatic disease are predominantly solid and demonstrate avid contrast enhancement.
80 mg tadapox free shipping
Blood products and melanin contain metal ions including iron erectile dysfunction drugs prices buy tadapox online pills, copper, manganese, and zinc. Nearly 75% of melanoma metastases have either T1 hyperintensity or demonstrate susceptibility effect; 25% demonstrate both. Virtually all nonhemorrhagic metastases enhance following contrast administration (27-15B) (27-18D). Patterns vary from solid, uniform enhancement to nodular, "cyst + nodule," and ring-like lesions (27-21) (27-22). Actively bleeding metastatic adenocarcinoma, unknown primary, was found at surgery. The second has central necrosis, and the infundibular metastasis is isointense with white matter. The necrotic metastasis shows a "cyst + nodule" configuration, whereas the smaller hemorrhagic metastasis shows a tiny ring of enhancement. Metastases and Paraneoplastic Syndromes 845 (27-22) A 63y man presented with severe headaches and papilledema. The conspicuity of metastases can be increased on T1 C+ scans with fat suppression and magnetization transfer sequences. The use of double- and even triple-dose contrast-enhanced scans has been reported to increase sensitivity but is not in standard use. However, lipid signal is also common in many cellular processes, including inflammation and necrosis. Their use may permit early detection of micrometastases before lesions become apparent on standard gadolinium-enhanced sequences. Differential Diagnosis the differential diagnosis of parenchymal metastases varies with imaging findings. The major differential diagnosis for punctate and ring-enhancing metastases is abscess. No matter what the imaging findings are, a solitary cerebellar mass in a middle-aged or older adult should be considered a metastasis until proven otherwise! Even with a "cyst + nodule" appearance, which is classic for hemangioblastoma, metastasis should still be at the top of the differential diagnosis list. Both metastases and multiple embolic infarcts share a predilection for arterial "border zones" and the gray-white matter interfaces. Hemorrhagic metastases generally show disordered evolution of blood products and an incomplete hemosiderin rim. Skull and Dural Metastases Terminology the term "skull" refers both to the calvaria and to the skull base. As one cannot distinguish neoplastic involvement of the periosteal versus meningeal dural layers, we refer to these layers collectively as the "dura. Calvarial and skull base metastases can occur either with or without dural involvement. In contrast, dural metastases without coexisting calvarial lesions are less common. Solitary or multiple focal lesions involve the skull, dura (and underlying arachnoid), or both. A less common pattern is diffuse neoplastic dura-arachnoid thickening, seen as a curvilinear layer of tumor that follows the inner table of the calvaria. Complete evaluation requires both soft tissue and bone algorithm reconstructions of the imaging data (2724). Scans with soft tissue reconstruction obscure skull lesions, which may be invisible unless bone algorithms are utilized (27-25). Soft tissue scans viewed with bone windows do not provide sufficient detail for adequate assessment. Large dural metastases displace the brain inward, buckling the gray-white matter interface medially. Hypodensities in the underlying brain suggest parenchymal invasion or venous ischemia. A few osseous metastases-mostly those from prostate and treated breast cancer-can be blastic and sclerotic. The most common finding is a focal soft tissue mass centered on the diploic space. Hyperintense fat in the diploic space provides excellent, naturally occurring demarcation from skull metastases. Metastases replace hyperintense yellow marrow and appear as hypointense infiltrating foci (27-27). Dural metastases thicken the dura-arachnoid and are typically iso- or hypointense to underlying cortex (27-28) (27-29). Hyperintensity in the underlying brain is present in half of all cases and suggests either tumor invasion along the perivascular spaces or compromise of venous drainage. Nearly 70% of dural metastases are accompanied by metastases in the overlying skull (27-31). Most dural metastases enhance strongly, appearing as biconvex masses centered along the adjacent diploic space. Edema indicates infiltration along the perivascular spaces into the brain parenchyma. Most metastases-especially those from renal cell carcinoma-are hypervascular (27-32). Differential Diagnosis the differential diagnosis of skull and dura-arachnoid metastases depends on which compartment is involved and whether solitary or multiple lesions are present. The major differential diagnoses for skull metastases are surgical defects and normal structures. A surgical defect such as a burr hole or craniotomy can be distinguished from a metastasis by clinical history and the presence of defects in the overlying scalp. Venous lakes, vascular grooves, arachnoid granulations, and sometimes even sutures can mimic calvarial metastases. Normal structures are typically well corticated, and the underlying dura is normal. Skull base osteomyelitis is a rare but life-threatening infection that can resemble diffuse skull base metastases. The major differential diagnosis for solitary or multifocal dura-arachnoid metastases is meningioma. Metastases, especially from breast cancer, can be virtually indistinguishable from solitary or multiple meningiomas on the basis of imaging studies alone. Metastases and Paraneoplastic Syndromes the differential diagnosis of diffuse dura-arachnoid thickening is much broader. Nonneoplastic pachymeningopathies such as meningitis, chronic subdural hematoma, and intracranial hypotension can all cause diffuse duraarachnoid thickening. Metastatic dural thickening is generally-although not invariably-more "lumpy-bumpy" (27-28) (27-29). Recent advances in therapeutic management have been achieved, so early diagnosis is critical for optimal treatment. Terminology the anatomic term "leptomeninges" refers to both the arachnoid and the pia. Arachnoid metastases are almost always secondary to dura involvement and look quite different (27-34). Other synonyms include meningeal carcinomatosis, neoplastic meningitis, and carcinomatous meningitis. Although uncommon, leptomeningeal dissemination of melanoma carries an especially dire prognosis. Sulcal-cisternal enhancement, especially at the base of the brain, can be seen in some cases (27-37A). If tumor has extended from the pia into the perivascular spaces, underlying brain parenchyma may show hyperintense vasogenic edema. Neoplasms, Cysts, and Tumor-Like Lesions 852 Postcontrast T1 scans show meningitis-like findings. Smooth or nodular enhancement seems to coat the brain surface, filling the sulci (27-38C) and sometimes almost the entire subarachnoid space including the thecal sac (27-39). Cranial nerve thickening with linear, nodular, or focal mass-like enhancement may occur with or without disseminated disease (27-51) (2752). Tiny enhancing miliary nodules or linear enhancing foci in the cortex and subcortical white matter indicate extension along the penetrating perivascular spaces.
Syndromes
- Tall height
- Dried fruits
- Increased heart rate
- Nausea and vomiting
- Keep the person warm and comfortable. Loosen tight clothing.
- Check water temperature in a bath before placing a child in it.
- Change in blood pressure
- Disseminated intravascular coagulation
Buy tadapox 80 mg overnight delivery
The initial management of disk herniation in athletes is similar to that for the general population for management of axial pain and isolated root compression erectile dysfunction pump prescription buy generic tadapox canada. Effacement of the spinal cord can be managed nonsurgically, but repeat imaging should be performed to exclude cord compression in symptomatically improved athletes before they return to sports activities. Certain procedures may preclude a safe return to play; however, this consideration should not encourage the surgeon to perform a procedure with a decreased likelihood of clinical success. Musculoligamentous Injuries Muscular and ligamentous injuries are common sports-related injuries. Ligamentous sprain or muscular strain can occur after aggressive bending or rotational injuries to the neck. Pain may not be immediate; instead, it may manifest over the 24-hour period after injury. Tenderness is typically seen on palpation, and range of motion may be limited by patient guarding. If necessary, a collar should be used until ligamentous injury is definitively ruled out. Active range of motion and strengthening exercises can be initiated as pain improves. Athletes should be asymptomatic and display normal strength and range of motion before resuming sports-related activities. Return to Play No major sporting association has adopted a policy specifically regarding return to play after cervical injury. The decision regarding return to play is complex because of the heterogeneity of the involved pathoanatomy. Although some guidelines on return to play have been offered (Table 2), no high-level evidence exists to support the recommendations. The basic prerequisites for return to play include normal strength, pain-free range of motion, spinal stability, and adequate canal space for the spinal cord. The Torg ratio, or spinal canal diameter relative to vertebral body diameter, can be calculated based on measurements obtained from a lateral radiograph. The Torg ratio is helpful in determining whether an athlete has cervical stenosis. Subsequent studies suggest that the Torg ratio may have inadequate predictive value for determining future injury. Athletes with mild or moderate stenosis and no findings of parenchymal injury, whose symptoms resolve quickly, may be considered relatively contraindicated to return to contact sports. The final decision regarding return to play should consider the degree of stenosis and the propensity for injury during the intended sports activity. Athletes who undergo one- or two-level instrumented fusion of the subaxial spine and who demonstrate radiographically confirmed fusion are relatively contraindicated for return to play. These athletes must demonstrate full painless range of motion before return to play can be considered. Several studies have indicated that professional American football players and baseball players can return to their sport at or near their preoperative performance level. Occipitocervical and atlantoaxial fusion, whether postoperative or congenital (Klippel-Feil syndrome), also are considered absolute contraindications to return to contact sports. Thoracic and Lumbar Injuries Thoracic Injury Compared with injuries to the cervical and lumbar spine in athletes, thoracic spine injuries are relatively uncommon because of the increased biomechanical support provided by the ribs, sternum, and costal cartilage with associated ligamentous structures (Table 3). However, thoracic spine injuries tend to be missed and are associated with the potential for catastrophic outcomes if not identified and managed. The transitional cervicothoracic and thoracolumbar zones are especially vulnerable to unstable injury patterns. Thoracic spine injuries can involve concomitant rib fractures, pneumothorax, or visceral injuries, and the Advanced Trauma Life Support protocol should always be observed in the acute setting. A complete neurologic examination is necessary, including assessment of motor and sensory function, rectal examination, assessment of deep tendon reflexes, and assessment for the bulbocavernosus reflex. Table 2 Musculoligamentous injuries occur as a result of overuse in sports such as rowing, golf, and throwing sports, but they also occur as a result of acute, higher-energy injuries. Injections can be useful in managing refractory injuries but are generally not indicated. Thoracic disk herniations resulting from sports injuries are considerably less common than disk herniations in the cervical or lumbar spine,36 and typically occur in the lower one-third of the thoracic spine. Compression fractures, burst fractures, and fracture-dislocations in the thoracic spine secondary to sports injuries are uncommon. Management of these uncommon injuries is similar to that of injuries resulting from other mechanisms. Table 3 Lumbar Injury Low Back Pain in Athletes Low back pain is common in the general population, presenting in most adults at some point in their lifetime. Pain with extension often is associated with spondylolysis and posterior facet injuries, whereas pain with flexion is often discogenic. A thorough neurologic examination is required, and a history of any loss of bowel or bladder function should prompt urgent imaging to rule out compression of the cauda equina. Fracture Lumbar spine fractures in the athlete can be broadly characterized as minor fractures occurring with lower-energy trauma or repetitive activity, or as major fractures capable of causing substantial instability or neurologic deficit. Return to play is guided by resolution of symptoms and a progressive rehabilitation program involving sport-specific activity and restoration of full painless range of motion. Major fractures, which occur primarily in collision sports such as skiing or snowboarding, include burst fractures, fracturedislocations, and other potentially unstable three-column injuries. Isolated facet fractures are generally managed with a brace if the fracture is unilateral and no associated vertebral body fracture is present. Surgical management may prevent return to play at an elite level, but few data exist to guide treatment. Spondylolysis and Spondylolisthesis Spondylolysis, or defects of the pars interarticularis, is common in young athletes and has been reported in up to 47% of young athletes who have low back pain. Patients often experience low back pain that is worse with extension and that may be unilateral. Associated neurologic deficits are rare, unless a higher grade of spondylolisthesis is present, typically in the L5 distribution. Although oblique radiographic views were historically recommended to increase visualization of the pars, this practice has become less common because of the increased radiation and low sensitivity. Surgery may be considered for athletes who have recurrent symptoms after bracing, pain lasting at least 6 months, pain that precludes return to sport, or progressive spondylolisthesis (greater than 50% slip). Return to play is possible at 6 to 12 months postoperatively, but patients should be counseled that lumbar fusion may be a career-ending treatment. Lumbar Disk Herniation Lumbar disk herniation is most common in athletes younger than 35 years and those who participate in sports with repetitive flexion and compression movements, such as football, wrestling, hockey, tennis, and golf. Patients commonly report prodromal low back pain followed by radicular pain that is sometimes accompanied by a neurologic deficit. The overall prognosis of patients who have lumbar disk herniation is favorable, with one large study of 342 professional athletes reporting that athletes successfully returned to play 82% of the time. Epidural corticosteroid injections may help speed recovery; however, data to support this treatment are limited. Surgical management generally consists of laminotomy and disk fragment excision, although several studies have found approximately equivalent return-to-play rates after surgical management (mean, 80%) compared with nonsurgical management. Among elite athletes, time to recovery after lumbar diskectomy ranges from 3 to 9 months, with a mean 3 to 5 years of career length postoperatively. As previously noted, return-to-play rates for athletes undergoing surgical treatment of lumbar disk herniation are high and are comparable to those in athletes undergoing nonsurgical treatment. A successful return-to-play rate of 80% was reported in a study of adolescent athletes who underwent nonsurgical treatment for lumbar spondylolysis. In general, up to 12 months of rehabilitation may be required for select patients who are able to return to play after lumbar fusion. Summary Spine injuries in athletes can range from minor sprains and strains to catastrophic spinal cord injury. Team physicians and consultants should develop a comprehensive management protocol to address on-the-field injuries. The ability to return to play varies because of the heterogeneity of involved pathoanatomy and the consequences of necessary treatments. The risk for further injury after return to play should be the primary consideration in the decision-making process. Key Study Points Team physicians should develop a checklist and a comprehensive algorithm for management of on-the-field spine injuries in advance of game day. Stingers and burners involve a unilateral upper extremity, and symptoms are usually self-limited.
Buy tadapox no prescription
Diseases that specifically affect the putamen or globi pallidi in a bilaterally symmetric pattern have a somewhat different pathoetiologic spectrum erectile dysfunction drugs in canada discount 80mg tadapox overnight delivery. Additional information such as patient age and specific imaging characteristics can also help establish a reasonable differential diagnosis. In the subsequent chapters in this part, we consider toxic and metabolic disorders by diagnosis. Entities within each differential diagnosis are categorized as common, less common, and rare but important. Vascular disease, hypoxic-ischemic insults, and common metabolic disorders, such as chronic liver failure, are the most frequent causes of abnormality. Putamen Lesions In general, the putamina are less commonly affected than either the globi pallidi or thalami. Acute hypertensive bleeds are usually unilateral although T2* scans often disclose evidence of prior hemorrhages. However, there are some lesions that predominantly or almost exclusively involve the putamina. Most cause bilateral symmetric abnormalities on imaging studies (29-21) (29-22) (29-23). As with the symmetric basal ganglia lesions discussed previously, bilateral thalamic lesions tend to be toxic, metabolic, vascular, infectious, or hypoxic-ischemic (29-24) (29-25) (29-26) (29-27) (29-28) (29-29). The most common and rare but important causes of bithalamic lesions in children and adults are shown in the boxes on the next page. The anatomy and physiology of the brain dopaminergic system are briefly reviewed, as is the anatomy essential to evaluating preand postoperative deep brain stimulation. Understanding the different stages of brain formation and normal progression of myelination is essential to diagnosing inherited metabolic disorders. At the opposite end of the age spectrum, volume is normally lost in some parts of the brain, while other areas remain relatively intact. Abnormal mineral deposition in the basal ganglia can be a clue to degenerative and metabolic disorders. Understanding what is normal heavy metal deposition in different decades is a prerequisite to diagnosing these abnormalities on imaging studies. Dementia and Brain Degeneration Once an understanding of the normal aging brain is established, we discuss the pathology and imaging manifestations of dementia. Some agents are deliberately injected, inhaled, or ingested, whereas others are accidentally encountered or administered in a controlled medical setting. Some toxins accumulate slowly, so their clinical manifestations are subtle and onset insidious. Adulterated drugs are common, and contaminants may have additional adverse effects on their own. Presentation may also be confounded by "polydrug" abuse and secondary effects such as hypoxia that mask the underlying pathology. Acute effects on chronic underlying disease in abusers also contributes to the difficulty in sorting out which clinical and imaging findings can be attributed to specific drugs. Abnormalities in the deep gray nuclei (basal ganglia, thalamus) with varying white matter involvement are suggestive of toxicmetabolic causes. In this article, we first focus on the most common types of toxic encephalopathies, beginning with the acute and long-term effects of alcohol on the brain followed by a discussion of drug abuse. Inhaled toxins (such as carbon monoxide and cyanide) and heavy metal poisoning are then considered. Excessive alcohol consumption can result in chronic brain changes as well as acute, life-threatening neurologic disorders. Comorbid diseases such as malnutrition with vitamin deficiencies may lead to Wernicke encephalopathy. Altered serum osmolarity associated with alcohol abuse can cause acute demyelinating disorders. We begin our discussion of alcohol and the brain by briefly considering the acute effects of alcohol poisoning. We then consider chronic alcoholic encephalopathy before turning to other complications of alcohol abuse, including alcoholinduced demyelination syndromes and Wernicke encephalopathy. Binge drinkers represent a model for endophenotypic risk factors for alcohol misuse and early exposure to repeated binge cycles. Seizure-induced changes in the cortex, with gyral hyperintensity and diffusion restriction, may also be associated. Acute Alcohol Poisoning Etiology the acute effects of binge drinking are striking. Cellular swelling, life-threatening cytotoxic cerebral edema, and nonconvulsive status epilepticus may ensue (30-1). Acute alcohol poisoning is a complication of binge drinking and is most common in adolescents and young adults. The adolescent brain is also undergoing structural maturation and has a unique sensitivity to alcohol. Adolescent binge drinking Chronic Alcoholic Encephalopathy the long-term adverse effects of ethanol on the brain are much more common than those of acute alcohol poisoning. Chronic alcohol-related brain damage can be divided into primary and secondary effects. Toxic Encephalopathy 921 (30-3) Sagittal graphic shows generalized and superior vermian atrophy and corpus callosum necrosis related to alcoholic toxicity. Mammillary body and periaqueductal gray necrosis is seen with Wernicke encephalopathy. Chronic or harmful alchohol use leads to neurochemical, structural, and morphologic neuroplastic changes. Other direct effects include the toxicity of acetaldehyde and related lipid peroxidation products, which can bind to brain tissue and initiate upregulation and expression of inflammatory factors. The resultant membrane injury, neuronal loss, and reduction of white matter volume reflect the indirect effects of alcohol neurotoxicity. Repeated binge drinking damages the cortical and subcortical microstructure of the brain. Disturbed dendritic complexity occurs in areas of the prefrontal and parietal regions that mediate reward-related motivation. The folia of the rostral vermis and anterosuperior aspects of the cerebellar hemispheres are atrophic, separated by widened interfolial sulci. Purkinje cell loss in the cerebellum, together with patchy loss of granular cells and molecular layer atrophy, reflects the alcohol-induced cerebellar degeneration. A characteristic pattern of progressive brain volume loss is seen with chronic alcoholic encephalopathy. Initially, the superior vermis atrophies and the cerebellar fissures become prominent (30-4) (30-5) (306). In later stages, the frontal white matter becomes involved, reflected by widened sulci and enlarged lateral ventricles. Brain volume loss, especially in the prefrontal cortex, is common as is more focal atrophy of the superior vermis. The cerebral hemispheres also appear moderately atrophic with prominent superficial sulci. Toxic Encephalopathy (30-8) Autopsy specimens are from a patient with Wernicke encephalopathy. The inset below the pathologic section shows normal mammillary bodies for comparison. Malnutrition secondary to hyperemesis gravidarum (pregnancy-related vomiting), eating disorders, or bariatric surgery with drastically reduced thiamine intake is typical. Toxicity is likely mediated through its metabolite chloroacetaldehyde, which may impair thiamine function. Thiamine is required to maintain membrane integrity and osmotic gradients across cell membranes. Inadequate thiamine results in lactic acidosis with intra- and extracellular edema.
Buy 80 mg tadapox fast delivery
At 1-year follow-up erectile dysfunction medication south africa buy generic tadapox 80mg on-line, both neckspecific exercise groups did better with less disability and less pain, but no difference was noted between them. At 2-year follow-up, both neck-specific exercise groups had less disability, but improvements in pain were not significant. This study of comprehensive exercise versus advice showed no difference between groups at each data point up to 12 months. The authors of this systematic review reported that multimodal care may be beneficial for patients with early or recalcitrant symptoms after whiplash-associated disorders or associated disorders with neck pain. Acute management includes the airway and respiration, cardiovascular resuscitation, spinal shock, and bowel and bladder function. After medical, surgical, and vertebral stability are achieved, the patient is typically transferred from the surgical intensive care unit; rehabilitation then begins, with a focus on maximizing functional independence with therapy and education. Issues to be addressed include impaired mobility and self-care; respiratory dysfunction; autonomic dysreflexia; venous thromboembolism; risk of pressure ulcers; pain; neurogenic bowel and bladder conditions; sexual dysfunction; and other secondary conditions, which may include spasticity, heterotopic ossification, syrinx, nerve entrapment/compression, osteoporosis, abnormalities of carbohydrate and lipid metabolism, and a myriad of (preventable) causes of early death. Keywords: complete and incomplete spinal cord injuries; neurogenic bladder; neurogenic bowel; neuropathic pain; paraplegia; tetraplegia Dr. Gittler or an immediate family member serves as a board member, owner, officer, or committee member of the American Academy of Physical Medicine and Rehabilitation. Motor vehicle crashes are the leading cause of injury, followed by falls, violently acquired injuries (primarily gunshot wounds), and sports injuries (with diving remaining the most common sport associated with spinal injury). The most frequent neurologic category is incomplete tetraplegia (45%), followed by incomplete paraplegia (21%). Damage begins at the moment of primary injury when the cord itself is damaged, either directly or as a result of bone fragments or disk material. Within minutes, subsequent swelling within the spinal canal increases pressure on the cord and may cut blood flow to spinal cord tissue. During spinal shock, the entire spinal cord below the level of injury becomes temporarily disabled, with loss of all reflexes in addition to paralysis and loss of sensation. The cascade of biochemical and cellular events kills neurons, destroys myelin, and triggers an inflammatory immune response, which is the beginning of the secondary injury process. An incomplete injury means that the ability of the spinal cord to convey messages to or from the brain is not completely lost. In a complete injury, there is no communication from the brain and spinal cord to parts of the body below the level of the injury. Tetraplegia refers to impairment or loss of motor and/or sensory function in the cervical segments of the spinal cord. Paraplegia refers to impairment or loss of motor and/or sensory function in the thoracic, lumbar, or sacral segments of the spinal cord. The term paraplegia also is used in referring to cauda equina and conus medullaris injuries. The terms tetraparesis and paraparesis should not be used because they are imprecise. An accurate clinical examination will result in an appropriate diagnosis, can predict recovery, can frame rehabilitation and health care planning, and is essential for research. The examination should be performed within 72 hours of injury unless factors, including sedation for ventilation, intoxication, severe pain, psychiatric disorder, or head injury, preclude an examination. The level of an injury and the completeness or incompleteness of an injury guide the rehabilitation goals and expected functional outcome. The Consortium for Spinal Cord Medicine, funded by the Paralyzed Veterans of America, has created a series of evidence-based clinical practice guidelines (and companion consumer guides) that have been graded for scientific strength and methodology. Research is focused on the following four key principles: neurologic protection, regeneration, cell replacement, and retraining central nervous system circuits and plasticity. In animal models and limited human studies, hypothermia has been shown to reduce damage to susceptible neurons in the primary injury site, reduce damage to microvasculature, and improve functional outcome. Several approaches exist for repairing damaged axons through remyelination and new growth, including anti-inflammatory drugs, which inhibit amino acid toxicity and cell death that occurs after initial injury. Nogo-A is a monoclonal antibody that blocks proteins that inhibit the sprouting and regeneration of axons after spinal injury. Nasal olfactory cells have been shown to promote axonal regeneration and remyelination at the injury site. Rats with transected spinal cords retain the ability to walk with intense step and gait training on a treadmill. Other animal models have used a combination of spinal cord stimulation and neurotransmitters such as serotonin. Interdisciplinary Inpatient Rehabilitation Comprehensive rehabilitation services should include a highly specialized interdisciplinary approach that addresses medical, physiologic, functional, psychological, and social issues. Members of the team should strive to prevent the medical complications that affect activities of daily living and functional mobility. The team should formulate comprehensive discharge plans and arrange for the patient to receive lifelong follow-up to promote optimal health. In addition, weight-bearing restrictions and precautions may require that the individual delay comprehensive interdisciplinary rehabilitation. This controversy is largely the result of concern about perispinal bleeding related to anticoagulant prophylaxis. Vena cava filters are placed when there is contraindication to anticoagulation, major bleeding complications, and recurrent embolism while the patient is receiving adequate therapy. The neurologic level of injury has a substantial effect on the function of the respiratory system. Paralysis of abdominal muscles results in an ineffective cough and impaired clearance of airway secretions. During acute injury, the forced vital capacity of patients with tetraplegia is markedly reduced, with a predicted forced vital capacity of 30%, which improves substantially by 5 weeks and continues to improve until 5 months after injury. Discussions of electric phrenic pacing and noninvasive ventilation have been documented in the literature. This condition may result in increased bladder pressure and incomplete bladder emptying, which can lead to vesicoureteral reflux, hydronephrosis, and subsequent renal failure. Intermittent catheterization is the preferred bladder management technique after an acute injury. To maintain bladder pressures, patients may require pharmacologic management, including anticholinergic agents to relax the detrusor, alpha-blockers to lower outlet resistance, and intravesical botulinum toxin injection to relax the smooth muscle. Although patients are at a high risk for urinary tract infection, they more commonly have bacterial colonization. In addition to pyuria, a urinary tract infection also includes fever and constitutional symptoms. In addition, epididymitis and orchitis occur frequently in male patients with chronic indwelling catheters. Other options may include a suprapubic catheter or a continent stoma that can be catheterized. Although electrical stimulation of the sacral roots is an effective alternative for micturition on demand, there is a risk of abolishing reflex erection and ejaculation. Scheduled bowel care after the period of spinal shock should include determination of premorbid patterns of bowel function. Scheduling a bowel program for after a meal takes advantage of the gastrocolic reflex. Information on the neurogenic bowel is available from the Consortium for Spinal Cord Medicine. These erections are mediated by a reflex arc exclusively in the sacral spinal cord. Tactile input passes through the pudendal nerve that accompanies the motor fibers; the efferent limb consists of preganglionic axons that travel via the pelvic nerve to the pelvic plexus to the penis, which can then result in an erection. These erections are "mentally induced" directions, which are initiated by various afferent stimuli generated or received by the brain. The brain receives afferent sensory inputs, and descending pathways from the brain control outflow from the thoracolumbar sympathetic and sacral parasympathetic plexuses to the penis. Although the dominant autonomic input for tumescence is parasympathetic, whereas the input for flaccidity is sympathetic, other complicating factors are involved. Synergistic autonomic pathways compensate for each other between various neurotransmitters, including noradrenaline, acetylcholine, and nitric oxide.
Purchase tadapox in india
Brace wear was successful in preventing progression to a surgical-magnitude curve in 75% of patients compared with 42% of patients in the observation group erectile dysfunction kegel generic tadapox 80mg online. Patients who were at Risser stage 0 were found to be at risk for requiring surgery despite compliant brace wear. Romano M, Minozzi S, Zaina F, et al: Exercises for adolescent idiopathic scoliosis: A Cochrane systematic review. A lack of high-quality evidence precluded a recommendation for using scoliosis-specific exercises. Patients in the Schroth exercise group had greater improvement in the Biering-Sorensen score than the patients receiving standard care alone (32. At 6 months, the self-image and pain domains improved in the Schroth group and declined in the standard care group. Proposed guidelines for distal fusion levels were based on the location of the neutral vertebra. Wang Y, Fei Q, Qiu G, et al: Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis: A prospective study. Patients in the accelerated pathway group had a 48% shorter length of stay than those in the traditional pathway group. Hahn F, Zbinden R, Min K: Late implant infections caused by Propionibacterium acnes in scoliosis surgery. The risk factors for infection were revision surgery, performance of spinal fusion, and the use of spine implants. Impaired trunk balance and the strength of trunk muscles are important factors in the pathomechanism of scoliosis. The specific characteristics of each neuromuscular disorder determine the efficacy of nonsurgical management, the indications for surgery, the time of intervention, and the expected postoperative complications. Segmental posterior spinal fusion has been an effective definitive treatment for neuromuscular scoliosis, and the role of growth-modulating devices in younger children has been recently reported. In general, the complication rate is higher in patients with neuromuscular conditions than in children and adolescents who have scoliosis and no comorbidities. Despite advances in scoliosis surgery and an improved understanding of underlying neuromuscular mechanisms in many disorders, further research is needed to provide optimal orthopaedic care for children with neuromuscular disorders and scoliosis. Keywords: cerebral palsy; Duchenne muscular dystrophy; neuromuscular scoliosis; Rett syndrome; spinal muscular atrophy Dr. Sponseller or an immediate family member has received royalties from Globus Medical and DePuy; serves as a paid consultant to DePuy; has received research or institutional support from DePuy; and serves as a board member, owner, officer, or committee member of the Scoliosis Research Society. Abousamra nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this chapter. Introduction Neuromuscular scoliosis describes a heterogeneous group of disorders. Cerebral Palsy Prevalence Cerebral palsy is the most common cause of neuromuscular scoliosis. Posterior fusion is performed with anchors consisting of pedicle screws, tapes, or wires at key levels, including the apex. Correction may be produced by distraction, compression, and cantilever bending of the spine. Intraoperative monitoring of somatosensory-evoked potentials and transcranial electric motor-evoked potentials has been recommended, even for patients with severe motor deficits, to ensure that movement, sensation, and bladder function remain intact. Descending neurogenic motor potentials may provide motor data in patients whose motor cortex is difficult to stimulate. The LuqueGalveston procedure as well as pedicle screw instrumentation have been effective in correcting scoliosis deformity with a low complication rate. Correction of pelvic obliquity also was found to be similar in patients treated using unit rod instrumentation, iliac screws, or sacral alar iliac screws. Pedicle screw density consisting of more than 50% of the fixation construct is superior to a low density construct (consisting of <50% of the pedicle screw construct). Studies have acknowledged the increased cost of pedicle screw constructs compared with unit rod instrumentation. Growth-modulating techniques have been effective in correcting scoliosis and pelvic obliquity and delaying definitive fusion in young children with cerebral palsy and severe scoliosis; however, deep wound infections have been a common surgical complications with a rate of approximately 30%. When indicated, preoperative training with noninvasive positive-pressure ventilation has been shown to be effective in improving respiratory outcomes and reducing the incidence of respiratory complications. This subclassification has been associated with increased risk of postoperative complications as well as a decreased health-related quality of life. Rett Syndrome Prevalence and Nonsurgical Treatment Scoliosis is the most common orthopaedic condition seen in children with Rett syndrome. Myelomeningocele Prevalence and Nonsurgical Treatment Scoliosis has been reported in up to 80% of children with myelomeningocele and increases in frequency in patients with higher spinal lesions. Scoliosis magnitude, as defined by the Cobb angle, is not considered a good indicator of sitting imbalance, has been weakly related to restrictive lung function in children with myelomeningocele, and has no established relationship with physical function or self-perception. Sitting balance by itself has been related to better overall quality of life and physical function, and ambulatory status has not been related to quality of life and self-perception. If a ventriculoperitoneal shunt is in place, shunt function should be assessed prior to surgery. Considerations Recent efforts have been made to decrease the high rate of pseudarthrosis and implant failure, reported after spinal fusion in patients with myelomeningocele. The orthopaedic surgeon should consider the need for a plastic surgery consultation if muscle and skin coverage pose problems. In addition to careful preoperative planning, these findings have led to the recent conclusions that although spinal fusion in patients with myelomeningocele corrects the coronal deformity and halts scoliosis progression, it has a high complication rate and no clear effect on healthrelated quality of life. Because it frequently leads to nonhealing skin erosions, surgical correction is indicated. Considerations Segmental instrumentation using sublaminar wires or pedicle screws has been effective in providing good correction and stability. Outcomes A high rate of postoperative complications has been reported for patients with Duchenne muscular dystrophy. Summary Scoliosis is a common orthopaedic deformity in children with neuromuscular disorders. The differences in pathophysiology between these disorders and the variations in the neurologic level of involvement impose different risk factors that play an important role in guiding treatment. Although many children need surgery and spinal fusion as a definitive treatment for scoliosis, a specific multidisciplinary management approach in the context of each disorder would likely lead to improved postoperative outcomes. Further research in this field is needed to determine optimal orthopaedic care for children with neuromuscular disorders and scoliosis. Key Study Points Posterior spinal fusion with segmental instrumentation is the most appropriate method of fixation for most children with neuromuscular scoliosis. A high postoperative complication rate is seen after spinal fusion in patients with neuromuscular scoliosis. Growth-modulating techniques have been recently investigated and are effective for managing severe neuromuscular scoliosis that develops in the first decade of life. Steroid therapy is effective in decreasing the need for scoliosis surgery in children with Duchenne muscular dystrophy. This literature review of neuromuscular scoliosis showed that growing rods are effective in correcting scoliosis for this population. Patients with neuromuscular disorders have a high rate of surgical site infection. Canavese F, Rousset M, Le Gledic B, Samba A, Dimeglio A: Surgical advances in the treatment of neuromuscular scoliosis. This literature review of neuromuscular scoliosis reported that the likelihood and severity of scoliosis increases with the degree of neuromuscular involvement. Although neuromuscular scoliosis can be well corrected with different constructs, there is a high rate of associated complications. The author of this book chapter reported that spinal deformity in neuromuscular disorders results from a lack of muscular control and muscular weakness. Although there are similarities between neuromuscular disorders, each disorder is unique, and looking at neuromuscular scoliosis as a single condition underestimates the consideration needed to establish a treatment plan.