Buy labetalol without a prescription
Taking aging into consideration blood pressure in spanish generic labetalol 100mg with amex, a study on effects of moderate running training on postischemic recovery of contractile function and coronary perfusion in senescent myocardium has been done, and the beneficial effect of exercise on the elderly was clearly shown [115]. Both in vitro and in vivo studies validate the cardioprotective effect of exercise training [116,117]. Atherosclerosis Both carotid atherosclerosis and coronary atherosclerosis could be prevented and improved by exercise training [120,121]. Apolipoprotein E knockout mouse has been widely used as a model for inducing atherosclerosis. In women with abdominal obesity, a combination of aerobic and resistance exercises may be preferable to a single exercise mode for the same purpose [136]. Cardiomyopathy (Diabetic Cardiomyopathy, Dilated Cardiomyopathy, Cardiac Fibrosis) Diabetes is considered as one of the major causes of cardiomyopathy. A cluster of common features has been recognized in diabetic cardiomyopathy, including early decreased diastolic compliance, left ventricular hypertrophy and increased interstitial fibrosis [137]. Both directly and indirectly, exercise training is effective in preventing and treating diabetic-caused cardiac dysfunction. It has been established that enhancement of nonoxidative glucose pathway, lipotoxicity, mitochondrial disturbances, increased activity of reactive oxygen species, impaired endogenous antioxidant capacity, and altered calcium handling play significant roles in diabetic hearts. An 11% increase of peak oxygen uptake was found in diabetic heart after exercise intervention [139]. Dilated cardiomyopathy involves enlargement of cardiac chambers, meaning its ability to stretch becomes weaker. Exercise regimen in this might be tailored since exercise capacity is closely related to autonomic modulation and right ventricular dysfunction [145]. More evidence will be necessary to determine the exercise regimen on this group of patients. Cardiac fibrotic remodeling can result from normal aging or pathological stimuli such as ischemia, necrosis, and longterm high blood pressure. Targeting Smad3 signaling, miR-29b could hinder cardiac fibrotic progress either induced by hypertension [148] or post-infarct cardiac remodeling [149]. In heart tissue of a model of early ovarian hormone deprivation, physical training was found to prevent increase in fibrosis and promote an increase in the cardiac contractile response [153]. Emerging evidence supports that exercise training has enormous benefits in improving cardiac function and decreasing premature mortality [156]. Exercise training is the most cost-effective way to prevent cardiovascular related disease. In addition, other tools-drugs, patient education, behavioral, and psychological management-must be employed as well [157,158]. By learning all these mechanisms, we are looking forward to the possibility of "exercise in pills" and individualized cardiac rehab based on more detailed biophysiological markers. Competing Financial Interests the authors declare no competing financial interests. Modeling future cardiovascular disease mortality in the United States: national trends and racial and ethnic disparities. Recent advancements in understanding endogenous heart regeneration-insights from adult zebrafish and neonatal mice. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Exercise protects the cardiovascular system: effects beyond traditional risk factors. Phosphoinositide 3-kinase (p110alpha) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. New molecular mechanisms for cardiovascular disease: cardiac hypertrophy and cell-volume regulation. Phosphoinositide dependent protein kinase 1 is required for exercise-induced cardiac hypertrophy but not the associated mitochondrial adaptations. Regional effects of voluntary exercise on cell size and contraction-frequency responses in rat cardiac myocytes. Molecular basis of physiological heart growth: fundamental concepts and new players. Features of cardiomyocyte proliferation and its potential for cardiac regeneration. Periostin induces proliferation of differentiated cardiomyocytes and promotes cardiac repair. Physical exercise affects slow cycling cells in the rat heart and reveals a new potential niche area in the atrioventricular junction. Cardiac repair with a novel population of mesenchymal stem cells resident in the human heart. Exercise training provides cardioprotection against ischemia-reperfusion induced apoptosis in young and old animals. Partial persistence of exercise-induced myocardial angiogenesis following 4-week detraining in the rat. Insulin-like growth factor I is essential for postnatal growth in response to growth hormone. The insulin-like growth factor 1 receptor induces physiological heart growth via the phosphoinositide 3-kinase (p110alpha) pathway. Insulin-like growth factor I receptor signaling is required for exercise-induced cardiac hypertrophy. Protective effects of exercise and phosphoinositide 3-kinase (p110alpha) signaling in dilated and hypertrophic cardiomyopathy. The protective effects of exercise and phosphoinositide 3-kinase (p110alpha) in the failing heart. Role of gp130-mediated signalling pathways in the heart and its impact on potential therapeutic aspects. Deletion of Interleukin-6 attenuates pressure overload-induced left ventricular hypertrophy and dysfunction. Signal transducer and activator of transcription 3 in the heart transduces not only a hypertrophic signal but a protective signal against doxorubicin-induced cardiomyopathy. Ventricular ErbB2/ErbB4 activation and downstream signaling in pacing-induced heart failure. Neuregulin1/ErbB4 signaling induces cardiomyocyte proliferation and repair of heart injury. Exercise training activates neuregulin 1/ErbB signaling and promotes cardiac repair in a rat myocardial infarction model. The role of neuregulin/ErbB2/ErbB4 signaling in the heart with special focus on effects on cardiomyocyte proliferation. Cardiac endothelial cells regulate reactive oxygen species-induced cardiomyocyte apoptosis through neuregulin-1beta/erbB4 signaling. Exercise-Based Cardiovascular Therapeutics: From Cellular to Molecular Mechanisms Chapter 7 95 [71] Ren J, et al. Nitric oxide synthase inhibition abolishes exercise-mediated protection against isoproterenol-induced cardiac hypertrophy in female mice. Exercise protects against myocardial ischemia-reperfusion injury via stimulation of beta(3)-adrenergic receptors and increased nitric oxide signaling: role of nitrite and nitrosothiols. Neuronal nitric oxide synthase is indispensable for the cardiac adaptive effects of exercise. Exercise training improves functional sympatholysis in spontaneously hypertensive rats through a nitric oxide-dependent mechanism. Training-induced increase in nitric oxide metabolites in chronic heart failure and coronary artery disease: an extra benefit of waterbased exercises Exercise training modulates cytokines activity in coronary heart disease patients. Exercise-induced reduction in myocardial infarct size after coronary artery occlusion in the rat. Prior exercise training improves the outcome of acute myocardial infarction in the rat.
Generic 100mg labetalol fast delivery
In diffusion-limited exchange blood pressure chart keep track discount labetalol 100mg with mastercard, raising the blood flow causes relatively little increase in solute exchange because the blood is already spending too little time in the capillary to unload its solute fully. An increase in blood flow can also trigger an increase in permeability the preceding section describes the purely passive, biophysical effect of blood flow on solute exchange. However, recent work indicates that blood flow can also induce active increases in endothelial permeability to lipophobic solutes. This is described in the next section because it is one of several ways in which the body adjusts the rate of solute transfer to meet increased demand during exercise. However, if the supply artery is narrowed by atheroma, solute delivery is restricted and transfer may lag behind the increased demand. In patients with coronary artery disease, this results in exercise-induced angina, while in patients with femoral artery disease it results in calf pain during exercise (intermittent claudication). Typical values for glucose in skeletal muscle capillaries are ~5 at rest, because blood flow is low in resting muscle, and <1 during exercise, because blood flow is raised. Additional factors include an increase in the O2 diffusion velocity through muscle myoglobin as intracellular O2 partial pressure falls, and in the case of small lipophobic solutes such as glucose, probably an increase in capillary permeability with flow. The number of muscle fibres supplied by one capillary, and hence the radius of the Krogh cylinder, depends on the anatomical capillary density and the fraction that is well perfused at any moment in time. The injection of visible particles or dyes has shown that, in resting skeletal muscle, half to three quarters of the capillaries are not perfused, or are perfused only sluggishly, at any one moment because the terminal arterioles supplying them are in the constricted phase of their vasomotion cycle (Section 10. In resting skeletal muscle (top), contraction of terminal arteriole 2 arrests the perfusion of one capillary module (dashed lines). Each perfused capillary must therefore supply a broad cylinder of muscle (Krogh cylinder). When exercise commences (bottom), metabolic vasodilatation dilates terrK minal arteriole 2, leading to perfusion of the previously closed-off capillarReduced ies. This improves the homogeneity distance for of O2 supply, increases the perfused di usion capillary surface area, reduces the radius of each Krogh cylinder and thus reduces the maximum diffusion distance rK. During exercise the terminal arterioles are dilated by metabolites released by the contracting muscle fibres (Section 13. This increases the number of well-perfused capillaries, a process termed capillary recruitment. These changes improve the uniformity of the O2 supply; that is, they reduce the heterogeneity present in resting muscle (Section 10. The metabolic hyperaemia increases the rate of delivery of O2 and glucose and prevents the transcapillary exchange from becoming flowlimited. Metabolites such as glucose are diffusion-limited at the high flows that occur during exercise, so solute transfer is not limited by solute delivery rate. Increased metabolic consumption steepens the concentration gradient the increased metabolic rate of an active tissue lowers the tissue concentration of glucose and O2, and therefore increases the concentration difference between the capillary blood and the tissue. For example, the mean concentration difference for glucose across the capillary wall is estimated to increase from ~0. The increased concentration difference, coupled with the shortening of diffusion distance by capillary Endothelial permeability increases in response to flow Recent measurements of K+, Na+, urea and fluorescein exchange show that an increase in blood flow not only increases the delivery of solute to the capillaries but also triggers a rapid rise in capillary permeability. The flow-mediated rise in permeability involves an active endothelial response mediated by nitric oxide. The raised permeability helps to explain the large increase in transcapillary glucose flux into exercising muscle. To draw together the various concepts introduced in this chapter, let us finish with two specific examples of how solute flux is increased to meet an increase in demand. Diffusion, not fluid filtration, accounts for most of the transcapillary transport of glucose and other small metabolites. During 25 min of cycling, the glucose consumption of leg muscles is proportional to the exercise intensity. Arterial plasma glucose itself is kept constant through increased glucose production by the liver and other tissues. The factors that increase the transfer of blood glucose to the exercising muscle fibres are brought together in Table 10. Capillary recruitment reduces the radius of the Krogh cylinder and hence the diffusion distance x. Increased blood flow delivers glucose faster to the capillary and prevents a major fall in the mean intracapillary plasma concentration, thereby avoiding flow limitation of exchange. As the glycogen store is depleted, blood glucose extraction (Ca - Cv)/Ca increases. When muscle glycogen is depleted prior to exercise, glucose extraction is increased (dashed lines with blue circles). Note that the O2 demand of the exercising muscle, 5 mL O2/min, exceeds the total resting arterial supply, 1 mL O2/min. If blood flow did not increase, the O2 content of the blood would approach zero soon after it entered the capillary (dotted-dashed line). A, arterial end of exchange microvessels (strictly, the terminal arteriole); V, venous end of exchange system. During exercise, capillary recruitment occurs, as described previously for glucose. This raises the surface area available for exchange and reduces the diffusion distance. If flow did not increase, O2 exchange would become severely flow-limited, since a moderately exercising muscle consumes more O2 per minute than its total resting arterial supply. An additional factor that speeds up O2 transport in exercising muscle is the partial deoxygenation of the myoglobin that is present at up to 7 g/kg in the sarcoplasm of red muscle. Solutes such as O2 and glucose diffuse rapidly across the capillary wall down concentration gradients. Water, by contrast, flows slowly across the wall down a pressure gradient across the intercellular cleft and fenestrae. A porous membrane, such as the capillary wall, limits the area available for diffusion and restricts the intrapore diffusivity. The intercellular space is small, so permeation is much slower than for lipid-soluble molecules. The pores are the tiny spaces between the polymers of the endocapillary coat, the glycocalyx. Solute extraction E is the fraction of the arterial solute that is extracted by the tissue during capillary transit. E = (Ca - Cv)/ Ca, where Ca and Cv are the arterial and venous plasma concentrations. The effect of increased blood flow depends on whether solute exchange is flow-limited, diffusion-limited or intermediate. Such exchange is flow-limited; raising the blood flow increases the exchange rate proportionately, as with O2 uptake by pulmonary capillaries. Protein interactions at endothelial junctions and signaling mechanisms regulating endothelial permeability. Skeletal muscle capillary function: contemporary observations and novel hypotheses. A three-pathway pore model describes extensive transport data from mammalian microvascular beds and frog microvessels. Capillary diffusion distances: their importance for cardiac and skeletal muscle performance. Filtration, diffusion and molecular sieving through peripheral capillary membranes; a contribution to the pore theory of capillary permeability.
Order labetalol 100 mg without a prescription
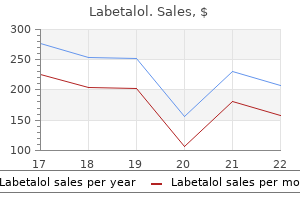
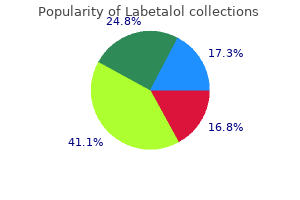
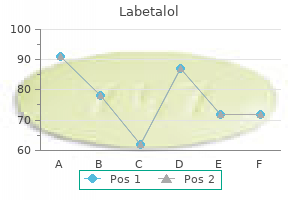
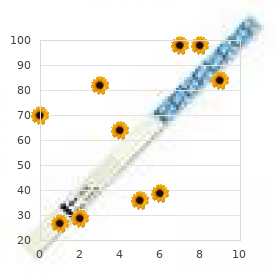
P-values in the table for the remaining dependent variables reflect that of the overall model fit arrhythmia chapter 1 generic labetalol 100mg on-line. Solid line is the model goodness-of-fit line for the regression, whereas the upper and lower dotted lines are 95% confidence limits of the model goodness-of-fit line. In applying these advanced models to describe cardiac hemodynamics, it is noteworthy that changes in systemic arterial pressure are accounted for in series with the magnitude of flow or volume exiting the heart, which can be directly interpreted as the perfusion pressure-generating capability of the heart. This maldistribution or "stealing" of blood flow away from locomotor muscles contributes to early recruitment of nonoxidative pathways for energy production within locomotor muscles setting forth rapid cascading changes intramuscularly. Again, we acknowledged that there are other noninvasive techniques for assessing exercise cardiac hemodynamics aside from those methods mentioned in this chapter. Therefore, to emphasize that in the absence of availability of resources dedicated to performing invasive "gold" standard cardiac hemodynamic evaluation while also minimizing unnecessary patient risk, the strongest alternative method for assessing exercise cardiac pumping capability is the inert gas uptake technique. Forecasting the impact of heart failure in the united states a policy statement from the american heart association. Outcome of heart failure with preserved ejection fraction in a population-based study. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Longterm prognostic impact of therapeutic strategies in patients with idiopathic dilated cardiomyopathy: changing mortality over the last 30 years. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. Diastolic heart failure-abnormalities in active relaxation and passive stiffness of the left ventricle. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Randomized, controlled trial of long-term moderate exercise training in chronic heart failure effects on functional capacity, quality of life, and clinical outcome. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Four-year efficacy of cardiac resynchronization therapy on exercise tolerance and disease progression: the importance of performing atrioventricular junction ablation in patients with atrial fibrillation. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. Reduced rate of alveolar-capillary recruitment and fall of pulmonary diffusing capacity during exercise in patients with heart failure. Influence of cardiomegaly on disordered breathing during exercise in chronic heart failure. Influence of locomotor muscle afferent inhibition on the ventilatory response to exercise in heart failure. Relation between hemodynamic and ventilatory responses in determining exercise capacity in severe congestive heart failure. Determinants of variable exercise performance among patients with severe left ventricular dysfunction. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Cardiopulmonary exercise testing in the clinical and prognostic assessment of diastolic heart failure. Exercise oscillatory breathing in diastolic heart failure: prevalence and prognostic insights. Absence of exercise capacity improvement after exercise training program a strong prognostic factor in patients with chronic heart failure. Prognostic significance and measurement of exercise-derived hemodynamic variables in patients with heart failure. Peak cardiac power output, measured noninvasively, is a powerful predictor of outcome in chronic heart failure. How do different indicators of cardiac pump function impact upon the long-term prognosis of patients with chronic heart failure Peak exercise cardiac power output; a direct indicator of cardiac function strongly predictive of prognosis in chronic heart failure. Comparison and relation of indirect and direct dynamic indexes of cardiac pumping capacity in chronic heart failure. A non-invasively determined surrogate of cardiac power ("circulatory power") at peak exercise is a powerful prognostic factor in chronic heart failure. Correlates and prognostic implication of exercise capacity in chronic congestive heart failure. Clinical correlates and prognostic significance of the ventilatory response to exercise in chronic heart failure. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Coupling of hemodynamic measurements with oxygen consumption during exercise does not improve risk stratification in patients with heart failure. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Lack of correlation between exercise capacity and indexes of resting left-ventricular performance in heart-failure. Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. Failure of dobutamine to increase exercise capacity despite hemodynamic improvement in severe chronic heart failure. Acute inotropic stimulation with dopamine in severe congestive heart failure: beneficial hemodynamic effect at rest but not during maximal exercise. Relationship of exercise capacity to resting left ventricular performance and basal plasma norepinephrine levels in patients with congestive heart failure. Exertional fatigue due to skeletal muscle dysfunction in patients with heart failure. Exercise intolerance in patients with chronic heart failure: role of impaired nutritive flow to skeletal muscle. Ventilatory response to exercise improves risk stratification in patients with chronic heart failure and intermediate functional capacity. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. Bostan: the Criteria Committee of the New York Heart Association; Little, Brown & Company; 1994. Prevalence and prognostic significance of heart failure stages application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. Comparison between New York Heart Association classification and peak oxygen consumption in the assessment of functional status and prognosis in patients with mild to moderate chronic congestive heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. Dissociation between peak exercise oxygen consumption and hemodynamic dysfunction in potential heart transplant candidates. Relation between chemosensitivity and the ventilatory response to exercise in chronic heart failure. Impaired skeletal muscle nutritive flow during exercise in patients with congestive heart failure: role of cardiac pump dysfunction as determined by the effect of dobutamine. Factors determining symptoms in heart failure: comparison of fast and slow exercise tests. Characterization of the circulatory response to maximal upright exercise in normal subjects and patients with heart disease. Incremental prognostic value of exercise hemodynamic variables in chronic congestive heart failure secondary to coronary artery disease or to dilated cardiomyopathy.

Buy labetalol american express
The latter elicits a metabolic vasodilatation heart attack 3964 order 100 mg labetalol, which overcomes the concomitant adrenergic receptor-mediated vasoconstriction. Thus, sympathetic activity normally raises rather than reduces myocardial blood flow. The increase can precede exercise (feed forward), before the more powerful metabolic hyperaemia is triggered. Ischaemic vasodilatation, downstream from a coronary artery stenosis, helps to maintain the restig coronary flow in angina patients (Concept box 15. Also, ischaemic vasodilatation at the margins of an infarct helps to limit its extent. In aortic valve stenosis, the high resistance to ejection further increases the systolic stress within the left ventricle wall, especially during exercise. Human coronary arteries are functional end arteries prone to atheroma Coronary arteries are a common site for atheroma (atherosclerosis). Briefly, atheroma is a cholesterol-rich, subintimal plaque that narrows the coronary artery lumen, limiting blood flow and causing ischaemic pain (angina) during exercise. Atheroma may also trigger arterial thrombosis (the formation of an organized blood clot), which blocks a coronary artery and causes myocardial infarction. The narrowing of even one branch of a coronary artery is serious because human coronary arteries are functional end arteries, that is, they have ineffective anastomoses. Special problems Systole obstructs coronary blood flow About two-thirds of the coronary arterial system is intramural, that is, inside the myocardium. Acute ischaemic incidents (infarction, arrhythmia) are around nine times more common during strenuous exercise than at rest. This is attributed to catecholaminetriggered arrhythmias, rupture of atheromatous plaques by mechanical stress and increased blood coagulability in exercise. Nevertheless, the risk of developing symptomatic ischaemic heart disease is about halved in fit compared with unfit humans. Arterio-arterial anastomoses Atheromatous plaque obstructing ow Acute coronary obstruction by a thrombus causes myocardial infarction (a heart attack) the sudden obstruction of an atheromatous coronary artery by plaque rupture and thrombosis is the most common cause of death in the West (see Section 9. Here, the accumulation of interstitial K+, H+, adenosine and other factors stimulates nociceptors (Section 16. This causes a band of crushing chest pain, often radiating into the arms and neck. Residual coronary blood flow is often so low that myocytes begin to die after a few hours (necrosis). Treatment includes: supplementary O2; morphine, to reduce the pain and the pro-arrhythmogenic sympathetic activity; low-dose aspirin, together with a second antiplatelet agent (such as clopidogrel, prasugrel or ticagrelor; see Section 9. Even severe atheromatous stenosis of the artery, if it develops slowly, may have little effect on flow during rest, because the rise in proximal resistance is offset by a fall in distal resistance. Acute ligation of a major canine coronary artery reduces myocardial perfusion less severely, to ~16%. However, during exercise the fixed resistance of the stenosed artery prevents flow from increasing sufficiently to meet the increase in myocardial O2 demand. Even if the distal resistance vessels undergo maximal metabolic and ischaemic vasodilatation, the proximal stenosis now dominates the total resistance to flow; for a worked example, see Concept box 15. Therefore, exercise precipitates local myocardial ischaemia, leading to nociceptor activation and a crushing chest pain, reversible on rest, called angina pectoris. If a healthy coronary artery has a resistance of 1 unit and coronary resistance vessels have a resistance of 19 units, the total resistance is 20 units. R =19 R =1 (coronary artery) (rest of vessels) Total resistance = 20 During exercise, metabolic vasodilatation of the myocardial resistance vessels reduces their resistance, for example, to four units. R=4 R=1 Total resistance =5 (4x flow) Consider a severely stenosed coronary artery, of resistance 10 units, in a resting individual. Distal arteriogenesis and dilatation reduces the distal coronary resistance from 19 to , say, 10 units. R = 10 R = 10 atheroma Total resistance = 20 When the patient exercises, the reserve dilatation of coronary resistance vessels reduces the distal resistance further, for example, to three units. This fails to meet the increased O2 demand, leading to ischaemia and angina during exercise. R=3 R = 10 Total resistance = 13 Other triggers for angina include mental stress and cold. Mental stress increases coronary sympathetic vasomotor activity, leading to the contraction of atheromatous coronary arteries. As the eminent anatomist John Hunter once remarked in relation to his own stress-induced angina, "My life is at the mercy of any rascal who chooses to annoy me"; Hunter indeed died during a stressful medical committee meeting. Severe cold can likewise trigger a reflex sympathetic constriction of ischaemic coronary vessels, triggering angina or exacerbating exercise-induced angina. Stable angina is exercise-induced angina that is predictable for a given level of exercise. Crescendo angina is exercise-induced angina occurring at progressively lower levels of exertion. This usually leads to unstable angina occurring at rest with minimal increase in cardiac metabolic demand and is likely to progress to a myocardial infarction. It is caused by an episode of coronary artery vasospasm, that is, intense, prolonged contraction of the artery. Thus, variant angina is precipitated by reduced myocardial O2 supply, whereas exercise-induced angina is precipitated by increased myocardial O2 demand. Variant angina is usually treated with vasodilators such as dihydropyridine Ca 2+ channel blockers. Another rare cause of extreme coronary artery vasoconstriction arises from conditions associated with sudden and excessive adrenergic drive, such as severe emotional trauma (stress-related cardiomyopathy/broken heart syndrome), phaeochromocytoma, subarachnoid haemorrhage or overdose with drugs such as amphetamines or cocaine. The dramatic surge in plasma catecholamines is thought to result in direct myocyte stunning and toxicity combined with small vessel vasoconstriction, which leads to a deterioration in cardiac contractile ability and potentially cardiogenic shock. An unusual pattern of contractile dysfunction in the heart often occurs where the left ventricular base contracts while the apex balloons. The pattern of wall motion abnormalities seen may be related to the distribution of adrenergic receptors in the myocardium and vasculature. Conduit artery relaxation reduces the pulse wave velocity, which delays the wave reflection (1. Nitrodilators may also dilate coronary collateral vessels that bypass the stenosis. Still image of a left ventriculogram in the right anterior oblique view taken at peak contraction demonstrating apical ballooning. This was accompanied by posterolateral segment akinesis in the left anterior oblique view. Treatment with aspirin and another antiplatelet drug is required until the stent becomes endothelialized to prevent thrombosis occurring on the stent. This is usually for 1 month for a bare-metal stent, and 1 year for a drug-eluting stent because the endothelialization process is slowed due to antiproliferative medication. Functional adaptations High O2 extraction (>60% at rest) Metabolic vasodilatation dominates regulation Good autoregulation Vascular 2 adrenergic receptors, so adrenaline causes vasodilatation 15. Special tasks During exercise, the muscle circulation must increase the O2 and glucose delivery to match the increase in work, that is, blood flow must be coupled to exercise intensity. During open heart surgery, a stenosed length of artery is bypassed from the ascending aorta with a segment of saphenous vein or radial artery, or an internal mammary artery (typically on the left) is dissected and rerouted beyond the coronary artery stenosis. The number of capillaries per muscle fibre increases in proportion to the mitochondria per fibre. The arterial vessels likewise adapt to conduct a staggering maximal blood flow of 400 mL/min/100 g in endurancetrained muscles. Assessment of human coronary circulation Coronary sinus thermodilution measures coronary blood flow quantitatively, as described in Chapter 7 (Section 7. Coronary angiography is used to locate atheromatous obstructions, often as a guide to vascular surgery. A gamma-emitting isotope such as thallium or technetium is infused into the circulation and its appearance in myocardium is imaged by a gamma-camera at rest and following exercise.
Labetalol 100mg on line
Initial lymphatics lack smooth muscle in most tissues hypertension foods to eat order 100mg labetalol, so extrinsic pumping is needed here. Because the initial lymphatics are in series with the muscular lymphatics, both intrinsic and extrinsic propulsion are necessary overall. Extrinsic propulsion Flow in the non-contractile lymph vessels is induced by tissue movements, which intermittently compress the lymphatics, for example, skeletal muscle contractions, intestinal peristalsis, pulsation of adjacent arteries. Extrinsic propulsion accounts for the large increase in lymph flow from the leg of an anaesthetized animal when the leg is cycled passively. Successive regions, comprising one or more lymphangia, behave like mini-hearts linked in 208 11. Each region has longitudinally running pacemaker cells, that trigger local action potentials in the circumferentially orientated smooth muscle, leading to rhythmic contractions. The smooth muscle action potentials are generated by L-type Ca 2+ channels and fast Na+ channels. As in the cardiac ventricle, a diastolic filling phase, with the distal valve open and the proximal valve closed, is followed by an isovolumetric contraction phase (all valves closed), then an ejection phase (proximal valve open; ejection fraction ~25%) and an isovolumetric relaxation phase (all valves closed). Lymphatic contraction is regulated by filling pressure, sympathetic nerves and vasoactive agents Lymphatic contractile frequency, and to a lesser degree stroke volume, are increased by distension. In this way, a lymphatic segment can increase its output in response to an increased input from a more distal segment. Large lymphatics are innervated by an outer plexus of sympathetic noradrenergic fibres and an inner plexus of peptidergic fibres. Sympathetic activity and circulating adrenaline both increase contractile frequency. The dashed loop shows increased contractility and ejection fraction after a haemorrhage. Lymph nodes absorb some lymph: postnodal versus prenodal lymph the concentration of plasma proteins in postnodal lymph from the legs of dogs and sheep is up to twice that in the prenodal lymph, due mainly to the absorption of water by nodal blood capillaries. Therefore, postnodal lymph composition is unrepresentative of interstitial fluid composition, and postnodal lymph flow underestimates capillary filtration rate. However, the exact proportion of afferent lymph that is absorbed in human lymph nodes is unknown, and probably depends on posture, since capillary pressure in the nodes must increase with dependency. This increases their filtration rate, especially in the most dependent (lowermost) tissues. The foot, for example, swells at a rate of ~30 mL/h, driving people to unlace their shoes during long-haul flights or long films. The latter increased from 25 mmHg to 29 mmHg in university students over an 8-h period of sitting in lectures, reading, etc. These changes would be considerably worse, were it not for the following attenuating mechanisms. Hepatic lymph is particularly rich in plasma protein, due to the discontinuities in the hepatic capillary endothelium. The intestine makes the second greatest contribution to total lymph flow, especially after a meal. The limbs contribute a variable quantity of lymph, depending on exercise intensity. Dependent vasoconstriction is a local reaction, mediated by the myogenic response (Section 13. This attenuates filtration in these vessels, which have a higher Lp than arterial capillaries. Reduced capillary filtration capacity the contraction of some terminal arterioles may stop flow completely through capillary modules for short periods, thereby reducing the capillary filtration capacity. Exercise causes muscle swelling and a fall in plasma volume People working out at the gym notice that intensively exercised skeletal muscles becomes swollen and tense. Likewise, rockclimbers, for reasons not unconnected with their well-being, become keenly aware of swollen, pumped forearm muscles during steep, fingery climbs. The causes are as follows: Increased interstitial osmolarity is the main cause of the acute swelling. The increased crystalloid osmotic pressure is exerted across endothelial aquaporin channels, which are strongly expressed in the continuous capillaries of muscle. Although aquaporin conductance is low, the increase in interstitial osmotic suction is large, so capillary filtration rate increases substantially. Since aquaporins are water-only channels, the Na+Cl- concentration rises in the venous blood of active muscle. In addition, muscle sarcoplasm osmolarity increases during exercise, due to phosphocreatine breakdown and lactate formation. During prolonged heavy exercise involving multiple, large muscle groups, such as strenuous cycling, net muscle volume can increase by up to 1100 mL and plasma volume falls by ~600 mL (20%). The relative preservation of plasma volume is brought about by a compensatory absorption of interstitial fluid from the non-exercising tissues into the plasma compartment. The oedema is not usually detected until interstitial volume has doubled, which corresponds to ~10% limb swelling. Pulmonary oedema is often secondary to left ventricular failure, which raises left ventricular filling pressure and hence pulmonary venous pressure (Section 18. The congested, oedematous lungs are difficult to inflate, causing dyspnoea (difficulty in breathing). In the most severe cases the interstitial oedema spills over into the alveolar spaces, impairing O2 exchange, with potentially fatal consequences. Causes of oedema Oedema develops when capillary filtration rate exceeds lymphatic drainage rate for a sufficient period. The key relation is: Tissue swelling rate = Capillary filtration rate - Lymphatic drainage rate From this relation we see that oedema can result from a raised capillary filtration rate and/or a low lymph drainage rate. The oedema fluid again has a low protein 211 Circulation of fluid between plasma, interstitium and lymph (L) (P) (mg/mL) Prefemoral lymph n=4 74 80 60 40 20 0 0. This progressively lowered the plasma protein concentration P (top of white bars). Two of the safety factors against oedema are seen operating here: the dilution of interstitial protein (reducing extravascular colloid osmotic pressure, i); and increased lymphatic drainage rate. The hypoproteinaemia can be caused by: malnutrition (inadequate protein intake); intestinal disease (malabsorption and protein loss); nephrotic syndrome (albumin leakage into urine, >20 g/ day, due to a breakdown of the glomerular ultrafilter); hepatic failure (failure to synthesize albumin, fibrinogen, - and -globulins). The attendant fibrosis raises portal vein pressure, and hence intra-abdominal capillary pressures. The most common cause of lymphoedema worldwide is filariasis, a nematode worm infestation transmitted by mosquitoes. The nematodes impair lymphatic function in the limbs and scrotum, causing a gross lymphoedema associated with hyperkeratotic, elephant-like skin (elephantiasis). The hydraulic conductance Lp and protein permeability Pprotein increase and the protein reflection coefficient falls. This buffering mechanism is most effective in tissues with normally high extravascular protein concentrations, such as the lung (i 18 mmHg). If Pi is normally -2 mmHg and clinical oedema becomes apparent at around +1 mmHg, the change in Pi provides a safety margin of 3 mmHg. In oedematous interstitium, by contrast, large volumes of capillary filtrate can accumulate with little further rise in the opposing pressure Pi. However, once oedema develops, interstitial compliance becomes very large, so there is little further rise in the supra-atmospheric pressure. The dashed lines indicate that lymph flow reaches a limit in stationary tissue, but perhaps not in moved limbs.
Proven labetalol 100 mg
Oseltamivir and the risk of influenza-related complications hypertension bp proven labetalol 100mg, hospitalisation in patients with diabetes. Oseltamivir and oseltamivir carboxylate pharmacokinetics in obese adults: dose modification for weight is not necessary. Experience with oseltamivir in the control of a nursing home influenza B outbreak. Use of antiviral drugs to reduce household transmission of pandemic (H1N1) 2009, United Kingdom. Long-term use of oseltamivir for the prophylaxis of influenza in a vaccinated frail older population. An open-label crossover study to evaluate potential pharmacokinetic interactions between oral oseltamivir and intravenous zanamivir in healthy Thai adults. Thrombocytopenia from combination treatment with oseltamivir and probenecid: case report, MedWatch data summary, and review of the literature. The pharmacokinetics and tolerability of oseltamivir suspension in patients on haemodialysis and continuous ambulatory peritoneal dialysis. Selection of oseltamivir resistance mutation N294S in humans with influenza A H5N1. Outcomes of infants exposed to oseltamivir or zanamivir in utero during pandemic (H1N1) 2009. Clinical benefits with oseltamivir in treating influenza in adult populations: results of a pooled and subgroup analysis. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. Protective measures and human antibody response during an avian influenza H7N3 outbreak in poultry in British Columbia, Canada. Effects of the combination of favipiravir (T-705) and oseltamivir on influenza A virus infection in mice. Effects of double combinations of amantadine, oseltamivir and ribavirin on influenza A(H5N1) virus infections in cell culture and in mice. Activities of oseltamivir and ribavirin used alone and in combination against infections in mice with recent isolates of influenza A(H1N1) and B viruses. Lack of effect of moderate hepatic impairment on the pharmacokinetics of oral oseltamivir and its metabolite oseltamivir carboxylate. Lack of pharmacokinetic interaction between the oral anti-influenza neuraminidase inhibitor prodrug oseltamivir and antacids. Oseltamivir pharmacokinetics and clinical experience in neonates and infants during an outbreak of H1N1 influenza A virus infection in a neonatal intensive care unit. Lower clinical effectiveness of oseltamivir against influenza B contrasted with influenza A infection in children. A community cluster of influenza A(H1N1)pdm09 virus exhibiting cross-resistance to oseltamivir and peramivir in Japan, November to December 2013. Safety of neuraminidase inhibitors against novel influenza A(H1N1) in pregnant and breastfeeding women. In vitro activity of favipiravir and neuraminidase inhibitor combinations against oseltamivir-sensitive and oseltamivir-resistant pandemic influenza A(H1N1) virus. Effectiveness of personal protective equipment and oseltamivir prophylaxis during avian influenza A(H7N7) epidemic, the Netherlands, 2003. Post-marketing assessment of neuropsychiatric adverse events in influenza patients treated with oseltamivir: an updated review. Assessment of neuropsychiatric adverse effects in influenza patients treated with oseltamivir: a comprehensive review. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial. Role of combination antiviral therapy in pandemic influenza and stockpiling implications. Outcomes and susceptibility to neuraminidase inhibitors in individuals infected with different influenza B lineages: the Influenza Resistance Information Study. Detection of the rapid emergence of the H275Y mutation associated with oseltamivir resistance in severe pandemic influenza virus A/H1N1 09 infections. Oseltamivir (Tamiflu) and its potential for use in the event of an influenza pandemic. Prolonged shedding of multidrug-resistant influenza A virus in an immunocompromised patient. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. Writing Committee (Writing Committee of the Second World Health Organization Consultation on Clinical Aspects of Human Infection with Avian Influenza (H5N1) Virus) et al. Infant outcomes among pregnant women who used oseltamivir for treatment of influenza during the H1N1 pandemic. Neuraminidase inhibitorresistant influenza viruses may differ substantially in fitness and transmissibility. Neuraminidase inhibitorresistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficacy and pathogenicity in vitro and in vivo. Oral oseltamivir is effective in the treatment of acute influenza in a vaccinated population. Paper presented at the European Congress of Clinical Microbiology and Infectious Diseases, Stockholm, Sweden. Oral oseltamivir is effective in the treatment of acute influenza in a vaccinated program. Its chemical name is (1S,2S,3R, 4R)-3-[(1S)-1-(acetyla-mino)-2-ethylbutyl]-4-[(aminoiminomethyl) amino]-2-hydroxy-cyclo-pentanecarboxylic acid (trihydrate) and its molecular formula is C15H34N4O7 (trihydrate). Its oral bioavailability is low, so that the development of peramivir as a treatment for patients with influenza has focused on its efficacy and safety as a parenteral agent administered by either intramuscular or intravenous injection. It is efficacious as a single-dose, intravenous treatment for adults with uncomplicated influenza. Therefore, it may be possible to treat an infection caused by an influenza strain resistant to the latter two drugs with this agent. Peramivir was first approved in 2010 in Japan for treatment of influenza A or B infection as a single dose of 300 mg infused intravenously over 15 minutes. For patients at high risk of complications of influenza, a single dose of 600 mg was approved and multiple daily doses were an option depending on the condition of the patients. Peramivir, oseltamivir, and zanamivir are all potent inhibitors of avian influenza A viruses, including H5N1, H7N7, H7N9, and H9N2 strains that cause disease in humans (Govorkova et al. In mice with lethal, induced disseminated infection caused by H5N1 and H9N2 viruses with similar susceptibility to peramivir and oseltamivir in vitro, both drugs were equally efficacious when given orally prophylactically beginning 4 hours before intranasal virus challenge or as treatment, up to 60 hours after virus inoculation. Survival rates and virus concentration in lung and brain were not different among drugs, and virus strains recovered after treatment remained drug susceptible (Govorkova et al. However, at least in the case of influenza B infection, the reduced susceptibility of influenza B viruses to oseltamivir in vitro appears to be associated with reduced clinical benefit compared with treatment of influenza A virus infection (Kawai et al. Data have been reported on peramivir-resistant influenza viruses generated by serial passage in cell culture in the presence of the drug (Smee et al. However, other mutations confer variable degrees of cross-resistance among oseltamivir, peramivir, and zanamivir. Reduced virulence in mice with experimental infection caused by a peramivir-resistant mutant (Smee et al. Peramivir-resistant influenza A N1 and N2 virus mutants generated by reverse genetics exhibit variable degrees of cross-resistance to oseltamivir and zanamivir and variably altered virulence in mice (Abed et al. Peramivir-resistant viruses have not been isolated from treated mice with experimental influenza infection (Sidwell et al.
Order labetalol paypal
This rise is exacerbated by a reflex sympathetic peripheral venoconstriction arteria humeral profunda order 100mg labetalol overnight delivery, as noted earlier. The true filling pressure is the difference between the internal and external pressures, or transmural pressure (trans = across; mural = wall). The external pressure on the heart is the subatmospheric intrathoracic pressure, namely -5 cmH2O at end-expiration and -10 cmH2O at end-inspiration. However, at the same time, the expansion of the lungs during inspiration increases the pulmonary blood pool, which temporarily reduces the return of blood to the left ventricle. This is the reason why murmurs associated with right-sided heart valves become louder on inspiration, while those associated with left-sided heart valves become louder during expiration. The reduction in left ventricular output is partly offset by sinus arrhythmia, the tachycardia associated with inspiration (Section 5. Coughing, and other forms of forced expiration, such as the Valsalva manoeuvre (Section 17. The resulting fall in ventricular filling and cardiac output contributes to the dizziness associated with a severe bout of coughing. An increase in cardiac pumping reduces filling pressure the heart is a pump; that is, it removes blood from the venous system and transfers it into the arterial system. Pericardial effusions and constrictive pericarditis both raise the pressure around the heart. This impairs ventricular filling and can reduce the cardiac output severely, requiring surgical intervention. Under steady-state conditions, the venous return is simply the cardiac output observed in veins, rather than arteries. Imagine a right ventricular output that is merely 1% greater than the left ventricular output. In heavy exercise, with outputs around 25 L/ min, catastrophic congestion would build up within minutes. Conversely, a sustained excess of left ventricular output would quickly drain the pulmonary vessels dry. If right ventricular output begins to exceed left ventricular output, the increase in pulmonary blood volume raises the pressure in the pulmonary veins, which increases the filling of the left ventricle. The opposite happens if left ventricular output transiently exceeds right ventricular output. On standing up, the right output is less than the left output for a few beats, due to venous pooling. Also, as noted earlier, the different effects of respiration on right and left outputs cause a regular, alternating imbalance, synchronous with the respiratory cycle. Cardiac output must equal venous return in the steady state, so where the two lines cross is the steady state (open red circle). In the steady state in vivo, the cardiac output and venous return must be equal, and this happens at only one point on the plot, namely where the two curves cross. In cardiac failure, the output curve (Starling curve) is depressed by a fall in contractility. At the same time, there is a rise in mean circulatory pressure, due to sympathetic peripheral venoconstriction and renal fluid retention. These are the characteristic features of moderate ventricular failure (Chapter 18). This consideration is particularly important in failing hearts, which become very dilated and have an abnormally large radius. Consequently, a smaller component of the wall tension is angled towards the cavity, generating less pressure. The curvature of the ventricle wall thus determines how effectively the active wall tension is converted into intraventricular pressure. In other words, afterload depends on chamber radius, as well as arterial pressure. Since the radius of the chamber falls as ejection proceeds, afterload falls too, facilitating the late phase of ejection; in other words, ejection gets easier as it proceeds. However, this is not so in the grossly dilated, failing heart (in the following section; see also Section 6. The enddiastolic pressure itself is often referred to , inaccurately, as the preload. Afterload is the force per unit cross-sectional area (stress) that opposes the shortening of an isotonically contracting muscle strip. It can be adjusted in vitro by making a muscle pick up a weight as it begins to shorten. Starling, in his Law of the Heart Said the output was greater if, right at the start, the cardiac fibres were stretched a bit more, So their force of contraction would be more than before. Contractions grow weaker and stroke volume drops, Depressing blood pressure; so down the guard flops. But when the heart reaches a much larger size, this leads to heart failure, and often demise. Your patient is dying of decompensations, So reduce his blood volume or call his relations. Reduction of cardiac distension is an important therapeutic goal in heart failure because it improves the conversion of contractile force into intraventricular pressure. Distension is usually reduced by lowering the cardiac filling pressure, using diuretics to reduce plasma volume. Overall, a high arterial pressure has an adverse effect, depressing the output in the short term and leading to ventricular hypertrophy and eventually cardiac failure in the long term. In the intact heart, the afterload is often increased by a rise in arterial pressure and this reduces shortening during systole. This raises pulmonary vascular resistance, pulmonary arterial pressure and right ventricular afterload. The increased afterload causes a sharp fall in right ventricular output and the patient may collapse. For any pump operating at a fixed power, be it the heart or a laboratory roller pump, the maximum stroke volume occurs at zero outflow pressure. If the contractile energy is reduced by heart failure, the pump function curve is shifted downwards (point W to point 3). Since the resistance of the peripheral circulation is a major determinant of mean arterial pressure, it also affects stroke volume. This is put to practical use in the treatment of heart failure; the stroke volume of a failing heart can be improved by lowering the peripheral resistance, using vasodilator drugs. The contractility of the ventricle increases, and this enables the ventricle to maintain the stroke volume from a lower, near-normal end-diastolic volume. These act in an autocrine/ paracrine fashion to increase the myocyte Ca 2+ store and Ca 2+ transient. Activation of the Na+/H+ exchanger raises the intracellular Na+, which slows the expulsion of Ca 2+ by the Na+/Ca 2+ exchanger.