Order proventil 100 mcg with mastercard
If an inflammatory mass is present asthma x-ray in children order proventil 100 mcg line, one should avoid surgery and undergo conservative treatment instead. Prevention and Outcomes Prevention of appendicitis is not normally feasible; however, prompt recognition of symptoms and appropriate intervention can significantly reduce the morbidity associated with this disease. Arenaviridae Category: Pathogen Transmission route: Direct contact, inhalation Definition the arenaviridae family comprises highly infectious, virulent, zoonotic, viral pathogens that are transmitted to humans by rodents. Each arenavirus is associated with a specific host that is native to its geographical region. These branches represent the geographical origin and its subsequent evolutionary pathway to its current locale. The virus particles are spherical with an average diameter of 110 to 130 nanometers (nm) and are enveloped in a lipid membrane. They virions bead off from the host cells, giving off a grainy or sandlike appearance, hence the name "arena," meaning "sand" in Latin. The Old World or Lassa virus derives from the rodent family Muridae, subfamily Muridnae, for which viruses including Lassa and lymphocyte choriomeningitis were derived. The New World or Tacaribe virus comes from rats, bats, and mice of the family Muridae, subfamily Sigmodontinae. These viruses include Amapari, Guanarito, Junin, Latino, Machupo, Sabia, Tacaribe, and Whitewater Arroyo. Three of the New World viruses are found in the southwestern regions of the United States; Tacaribe is found in Trinidad. Agricultural areas, barns, homes (especially poorly maintained ones), and dry savannas are especially vulnerable to epidemics. Other areas of possible infection are laboratories that use mice or rodents and homes with pet mice, rats, or hamsters. Secondary and nosocomial infections are especially problematic for Lassa and Machupo viruses. Pathogenicity and Clinical Significance Arenaviruses are considered highly infectious, virulent pathogens. Five of these, Lassa, Junin, Machupo, Guanarito, and Sabia, are known to cause severe hemorrhagic syndromes and have led to regional epidemics. Lymphocytic choriomeningitis causes an acute central nervous system disease that can lead to congenital malformation. Other viruses are virulent to humans but have caused limited, nonlethal, and nonepidemic cases only or have been grown only in the laboratory. Since then, it has spread throughout West Africa and, because of widespread international travel, has appeared throughout the world. A reported 100,000 to300,000casesoccureachyear,with5,000deathsin West Africa alone. In addition to the expected transmission routes, persons in this area consume rodents, leading to infection caused by ingestion. Pregnant women are especially at risk, and they risk miscarriage caused by infection at a rate of 75 percent. The incubation time for Lassa fever is seven to eighteen days, after which the infected person has a fever, is weak, and has general malaise. The next stage of the illness involves vascular permeability, such as facial edema and pleural effusions; if a patient reaches this stage of the illness, the prognosis becomes poor. Rapid Salem Health deterioration follows, with pulmonary edema, shock, seizures, and coma. Another significant feature of this illness is sensineural deafness in up to 15 percent of patients. The South American hemorrhagic fevers (Argentine hemorrhagic fever, Guanarito, Machupo, Junin, and Sabia) are usually found in agricultural areas or in hot, dry landscapes, such as the Argentine pampas. Incubationisoneto two weeks, after which the patient experiences fever, malaise, mild neurological symptoms, and vascular damage. After three to four days, the fever may dissipate, but it can return two to four days later with a severe headache and meningitis. Lymphocytic choriomeningitis can cause severe damage to the central nervous system, including hydrocephalus and chorioretinitis. Some success has been found, however, with the use of ribavirin, a nucleoside analogue that has shown to help reduce morbidity and mortality in Lassa, Machupo, and Junin infections. Ribavirin must be given early in the course of the infection to target the viral life cycle. In general, patients with a lower viral load tend to have lower morbidity and mortality rates. Army Medical Research Institute of Infectious Diseases has taken a special interest in the South American hemorrhagic viruses as potential biological warfare agents. Details new antiviral strategies and includes comprehensive explanations of the pathogenicity of the most virulent arenaviruses. An overview of the history of arenaviruses, including their coevolution with rodent species. A detailed look at arenaviruses and hemorrhagic fevers, highlighting the vascular damage they cause. This phylum consists of invertebrates (animals that lack a backbone) that manifest bilateral symmetry (in which both halves of the body are identical), an exoskeleton (an external skeleton), a segmented body (a body divided into sections), and jointed legs. The most diverse category in the Arthropoda phylum is class Insecta, which includes some wellknown disease carriers: mosquitoes, ticks, and flies. Rarely are these diseases caused by the arthropod itself; rather, they are typically caused by pathogenic bacteria, viruses, and protozoa that are carried by a vector. Any arthropod that carries disease-causing microbes is called a vector or carrier. Causes Pathogenic microbes that move from an infected host to a healthy host through insect bites include bacteria, viruses, protozoa, and helminths. Examples of insect-borne illnesses that are caused by bacteria include Lyme disease, plague, and tularemia. Common insect-borne diseases that are of viral origin include West Nile encephalitis, Chikungunya, yellow fever, and dengue fever. Sometimes the vector simply offers a means of mechanical transfer from one point to another, such as when a housefly picks up a pathogen from a garbage bin and then deposits the pathogen on food that is consumed by humans. Thus, in this case the vector serves as an intermediate host required to complete the life cycle of the pathogenic protozoan Plasmodium. Risk Factors Persons who are not native to high-risk regions of the world, namely tropical regions, are considered most at risk because they have no common knowledge of these illnesses and have not become immune to secondary infections. Symptoms Symptoms depend on the disease origin (bacterial, viral, protozoan, or helminthic). Lyme disease is the most common tickborne disease in the United States and is caused by a corkscrew-shaped bacterium called Borrelia burgdorferi. Early symptoms of Lyme disease include one or more of the following: a characteristic skin rash called erythema migrans, tiredness, headache, chills, muscle and joint pain, and inflammation of the lymph glands. Another bacteria-caused arthropod-borne disease is plague, one of the most ancient diseases known to affect humans (an epidemic of the fourteenth century wiped out about one-third of the human population). Bubonic plague produces symptoms such as high fever, headache, chills, and painful swollen lymph nodes (also known as buboes). Pneumonic plague symptoms include fever, headache, and pneumonia-like symptoms such as shortness of breath, cough, chest pain, and blood in the sputum. Tularemia, another disease of bacterial origin, produces signs and symptoms based on the portal (path) Salem Health of entry of the pathogen. The most common form of tularemia is spread by tick or deer fly bites and produces high fever accompanied by skin ulcers and inflammation (pain and swelling) of the lymph nodes. If left untreated, the infection can become more severe and cause pneumonia-like symptoms such as chest pain, cough, and difficulty in breathing.
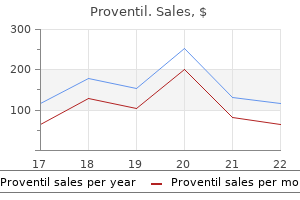
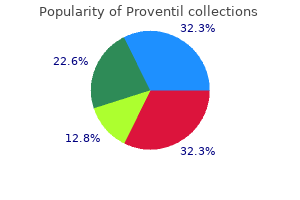
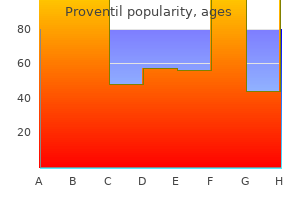
100mcg proventil otc
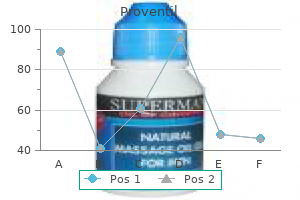
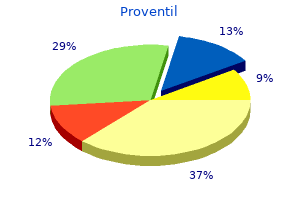
Congenital uterine anomalies are often identified during the investigation of infertile women asthma nos definition buy proventil 100 mcg mastercard, but they are rarely a cause of infertility; more frequently they are associated with pregnancy loss. An additional feature of conventional ultrasound units is Doppler imaging, which, for example, can assist in distinguishing adenomyomas from leiomyomas (Chapter 8). When potentially clinically relevant uterine anomalies are identified or suggested, additional imaging techniques are typically suggested to confirm and characterize the lesions. It can also be performed during the initial sonographic examination of the patient. These techniques are described in detail in Chapter 8, and will not be dealt with in detail here. Hysteroscopy Hysteroscopy provides direct visualization of the cervical canal and the endometrial cavity and allows access for the performance of surgical procedures such as adhesiolysis, metroplasty, myomectomy, and polypectomy. Initially described as "a technique looking for an indication," the impact of hysteroscopy in our specialty has been radical. This came about when hysteroscopy started to be used as a surgical access route into the uterus. This revolutionized and greatly simplified many procedures that previously required a laparotomy and a hysterotomy to access the uterine cavity and significantly reduced their morbidity. The use of local anesthetic techniques, in conjunction with the development of smaller caliber operative hysteroscopic systems that provide excellent vision, now allows most of these procedures to be performed in an office environment with an awake and engaged patient. Hysteroscopy and hysteroscopic procedures are discussed in Chapters 7, 29, 32, 34, and 35. Diagnostic evaluation techniques 385 Assessment of tubal and peritoneal factors Tubal and peritoneal factors are important causes of female infertility. Contrast imaging techniques principally designed to evaluate fallopian tube patency, together with laparoscopy, are the principal techniques for the evaluation of tubo-peritoneal causes of infertility. Other currently employed techniques include hystero-salpingo-contrastsonography (HyCoSy) and transvaginal hydro-laparoscopy (hydro-culdoscopy, fertiloscopy). In many centers, HyCoSy has become the primary assessment of choice because of reduced discomfort, the lack of radiation exposure, and the ability to perform the test by a well-trained gynecologist in an office setting35 (Chapter 8). Hysterosalpingography Hysterosalpingography is a radiologic contrast study of the cervical canal, endometrial cavity, and fallopian tubes. Such timing also avoids radiation exposure to the oocyte that will resume meiosis after the luteinizing hormone surge. Films are taken at appropriate phases of the procedure and when abnormal findings are encountered. In certain cases, a true lateral film may be necessary to determine such features as the position of the uterus, the location of intrauterine lesions, and the course and configuration of the tubes. When water-soluble media are used, the patient is reexamined fluoroscopically, and an additional film is taken 10 to 20 minutes after removal of the cannula. This examination and imaging may yield information about the external contour of the internal genitalia, the shape of the ovarian fossa, and presence of periadnexal adhesions. We recommend a 1979 book by Musset, describing hysterosalpingography, which is a classic and still valid today. This contrast material is eliminated within 30 minutes and does not cause pelvic granuloma formation, which has been reported after the use of oil-soluble media. Hysterosalpingography can provide valuable information about the uterus and oviducts. The cannula has been placed first in the right and then the left cervix to obtain this composite image. It is also not as sensitive for the detection of intracavitary abnormalities such as polyps and leiomyomas and has relatively little utility in evaluating adenomyosis. The use of selective salpingography in the others revealed tubal patency in one or both tubes in 131 of 318. The remaining 187 women were submitted to tubal cannulation; this procedure was successful, in one or both tubes, in 145 and failed in 42. It may simply be due to tubal spasm, which may be reduced by premedication and the use of gentle technique. Other causes include a mucous plug, synechiae, or more important lesions (obliterative fibrosis, salpingitis isthmica nodosa, endometriosis, or prior surgery), as outlined in Chapter 19. Endometriosis is encountered less frequently, usually when the tube is distally occluded, including post fimbriectomy. Rarely, signs specific to tuberculosis may be observed in what appears as a tube with a shortened ampullary segment. In some instances, the occlusion is incomplete and a small opening remains; this is termed phimosis of the distal tubal ostium. Salpingography provides information regarding the intratubal architecture, which is predictive of the prognosis of conception. Salpingography is a poor predictor of periadnexal adhesions, although not infrequently they prevent the dissemination of the contrast material, which remains confined. However, edema, hemorrhage, and anatomic distortion may not permit adequate evaluation. Selective salpingography the technique of selective salpingography is the injection of contrast medium directly into the uterine tubal ostium. This is achieved with the use of a special radiopaque cannula inserted through the cervix and guided toward the uterine cornu through the ostium, whereupon the contrast material is injected. The increased pressure generated by the direct injection helps to overcome obstructions 390 Infertility Hysterosalpingography: Abnormalities of the fallopian tube. Appearance Simple obstruction Comments May be due to tubal spasm, presence of mucous plug, synechia, or lesions. Tubal cannulation Cannulation of the fallopian tube from within the endometrial cavity requires the use of a special flexible guide wire and narrow-gauge cannula. This cannulation system is introduced through the larger cannula used for selective salpingography. These techniques are useful in differentiating "true" from "false" cornual occlusion. The therapeutic benefits of this approach have been shown for apparent cornual spasm, obstructions caused by amorphous material (tubal plugs), and tubal synechiae in the region of the uterine tubal ostium. It is doubtful that these techniques have a real therapeutic effect on occlusions owing to obliterative fibrosis, chronic follicular salpingitis, salpingitis isthmica nodosa, or endometriosis. Hysterosalpingography: extensive endometriosis of the left tube (arrows) with milder disease on the right in a patient with prior excision of the distal tubal segments for permanent contraception. The right tube is occluded immediately adjacent to the lesion (arrow), which demonstrates the progressive nature of the lesion. Both tubes are dilated and occluded distally (hydrosalpinx), although some contrast material escaped into the peritoneal cavity (d) with the increased pressure. In view of the finding of bipolar (distal and proximal) disease; reconstructive surgery is not recommended. The intramural segments have been opacified (arrows) and appear normal, as does the uterus. With further injection of contrast material, increased tubal distention, and pressure, some contrast material escaped into the peritoneal cavity (d) through a crack on the distal end of the left tube. Both tubes exhibit prominent ampullary folds (arrows), which is a good prognostic sign. After distention of the right ampullary segment, contrast material slowly escapes from a small distal opening (arrow) into the peritoneal cavity (d). In the event endoscopy is to be undertaken next, the surgeon will be prepared to use the endoscopic procedure for both confirmation and treatment of the lesion(s). The uterus is of normal size (u); the left hydrosalpinx is quite large and is confined to the pelvis (h). The right tube forms a very large mass that extends high into the abdominal cavity (gh). In addition to extensive fundal synechiae, there is massive intravasation of the contrast material (i). The right tube is occluded in the proximal ampullary region, which demonstrates significant intratubal adhesions (arrows). The right tube, which is almost completely opacified, has dilated and constricted sections and terminates in the shape of a Maltese cross, a pathognomonic sign for tuberculosis. Both tubes appear rigid; only the proximal portions of the tubes are opacified until the proximal ampulla, distal to which the contrast material produces the so-called "cotton wool" image (arrows).
100mcg proventil with amex
Seventy-two hours of mild hypothermia after cardiac arrest is associated with a lowered inflammatory response during rewarming in a prospective observational study asthma 2014 movie soundtrack proventil 100mcg. Impact of intraoperative temperature and humidity on healing of intestinal anastomoses. Autologous peritoneal mesothelial cell implant in rabbits and peritoneal dialysis patients. Stimulation of mesothelial cell proliferation by exudate macrophages enhances serosal wound healing in a murine model. The potential of mesothelial cells in tissue engineering and regenerative medicine applications. Stem cells isolated from adult rat muscle differentiate across all three dermal lineages. Short course dexamethasone treatment following injury inhibits bleomycin induced fibrosis in rats. Hepatocyte growth factor prevents peritoneal fibrosis in an animal model of encapsulating peritoneal sclerosis. Adenoviral-mediated gene expression of hepatocyte growth factor prevents postoperative peritoneal adhesion in a rat model. Inhibition of thrombin-activated fibrinolysis inhibitor decreases postoperative adhesion. The preventive effect of dexmedetomidine against postoperative intra-abdominal adhesions in rats. Evaluation of vitamin C and vitamin E for prevention of postoperative adhesion: a rat uterine horn model study. The comparison of the effects of ellagic acid and diclofenac sodium on intra-abdominal adhesion: An in vivo study in the rat model. Biodegradable and thermosensitive micelles inhibit ischemia-induced postoperative peritoneal adhesion. Oxidative stress in the pelvic cavity and its role in the pathogenesis of endometriosis. With modern intrauterine surgical techniques, intrauterine adhesions have become increasingly recognized as a postoperative complication. For a non-gravid uterus, causes include the use of surgical hysteroscopy for resection or destruction of endometrium, myomas, polyps, and uterine septae; curettage for endometrial hyperplasia; surgery that includes opening of the uterine cavity; and infections such as genital tuberculosis or schistosomiasis. The development of intrauterine adhesions may be an anticipated consequence of various modalities of intrauterine surgery. For example, an endometrial ablation has the specific purpose of destroying the basal layer of the endometrium to cause amenorrhea. Introduction Adhesions or synechiae within the endometrial cavity can have a profound impact on fertility. They are most commonly related to postabortal or postpartum instrumentation of the recently gravid uterus, but there exist several other circumstances that predispose to their formation. Understanding the pathogenesis of such synechiae is the first step to understanding primary prevention of such adhesions, as well as their diagnosis. Asherman, described the frequency, etiology, and symptoms of intrauterine adhesions. In his series, he defined two entities: traumatic intrauterine adhesions and stenosis of the internal cervical os. The stroma is largely substituted with fibrous tissue and the glands are replaced by inactive cubo-columnar endometrial epithelium. The functional and basal layers are indistinguishable, with the functional layer replaced by an epithelial monolayer unresponsive to hormonal stimulation and fibrotic synechiae forming across the cavity. Gestational changes make the myometrium softer and therefore more susceptible to the traumatic effect of curettage or other intrauterine procedures. The comparatively low estrogen status during and after pregnancy has a negative impact on the regeneration of the endometrium. In some women, the intrauterine trauma may lead to changes in vascularization and resulting hypoxia, and this extensive vascular damage results in endometrial atrophy and fibrosis. Genital tuberculosis was first reported in 1956, and endometrial tuberculosis remains endemic in some developing countries. Absence of enough normal endometrial tissue to support development of the placenta. Defective vascularization at the level of the denuded endometrium inhibiting effective implantation, leading to an occlusion of blood supply to the early embryo. None of these systems are universally accepted or validated, making comparisons between them difficult. Hysterosalpingography has the advantages of providing an outline of the areas of occlusion or filling defects as well as a simultaneous assessment of the cornual region, tubal contours, and tubal patency. In severe intrauterine adhesions, the endometrial cavity is completely distorted and narrowed, and both tubes may be occluded. In a large-scale review describing clinical presentations, amenorrhea was reported by 1102/2981 (37%) and light uterine bleeding in 924/2981 (31%) of women. Moderate Fibromuscular adhesions are characteristically thick but may be covered by endometrium and can bleed when divided Type 3 Type 2 Multiple small adhesions Stenosis of internal in the internal ostium ostium, causing almost isthmic region complete occlusion without concomitant corporal adhesions One-fourth to three fourths of cavity involved. Type 5 Type 4 Supra isthmic diaphragm Atresia of the internal ostium with causing complete concomitant corporal separation of the main adhesions cavity from its lower segment More than three-fourths of cavity involved. With amenorrhea American Fertility Society18 Adhesions in one-quarter to three-quarters of uterine cavity involved; ostial areas and upper fundus only partially occluded. Fibromuscular adhesions that are characteristically thick, still covered by endometrium that may bleed on division, partially or totally occluding the uterine cavity. More than three-quarters of uterine cavity agglutinated; ostial areas and upper cavity occluded. Valle and Sciarra28 Filmy adhesions in less than one-quarter of uterine cavity involved; thin or filmy adhesions. Filmy adhesions composed of basal endometrium producing partial or complete uterine cavity occlusion. Composed of connective tissue with no endometrial lining and likely to bleed upon division, partially or totally occluding the uterine cavity. Diagnosis 301 302 Pathogenesis, pathology, and clinical significance of intrauterine adhesions Grade 1 2 2A 3 3A 3B 4 Extent of intrauterine adhesions Thin or filmy adhesions easily ruptured by hysteroscope sheath alone. In such instances, hysteroscopic treatment is likely to be successful, and the patient can expect to resume normal postoperative menstrual function. Direct visualization of the cervical canal and endometrial cavity accurately confirms the presence, extent, and degree of adhesions and can be used to estimate the quality of the endometrium. Studies report that for 50% of women with "missed" abortion, spontaneous, and complete evacuation within 2 weeks without substantial morbidity occurs, making this an attractive management option. It is important to balance overzealous curettage and the resulting trauma to the basalis of the endometriumc against incomplete removal of any retained and potentially adhesiogenic placental remnants that may induce fibroblast activity and collagen formation before endometrial regeneration occurs. Targeted intrauterine pregnancy tissue removal using a hysteroscopic tissue removal device might reduce the risk of adhesion recurrence, offering some advantage to women with a predisposition to recurrent Asherman syndrome42 (see Chapter 31). Fertility is substantially altered in this group, with live birth reported in only 33. Where there is doubt whether echogenic material in the cavity is simply retained blood clot, color Doppler sonography might discriminate between this and vascular retained products. While conservative management is the best way of primary prevention for this group, it is not always possible. Hysteroscopic guidance for removal of retained products is less traumatic than blind curettage,45,46 and there are emerging data that hysteroscopic morcellation techniques might prevent the formation of adhesions in the uterine cavity. The use of postoperative adjunctive estrogen therapy is an example of this controversy. Protocols may use estrogen alone or sequentially with a progestin for 2 to 3 cycles, and there exists a protocol utilizing 2. From a prospective study, a trimmed Foley catheter was placed into the endometrial cavity after hysteroscopy in 32 women compared with 18 controls. The Foley was inflated and left in situ for a week before removal, and a follow-up hysteroscopy demonstrated a significantly greater rate of adhesion formation in the control group: (7/32 [22%]) of women in the Foley group vs. More recently, chemical barriers such as hyaluronic acid have been used to physically separate the uterine walls. Secondary prevention after postpartum procedures Postoperative estrogen therapy has been the prime met hod of stimulating rapid endometrial regeneration. Treatment of human endometrium with estrogen therapy is postulated to upregulate angiogenic growth factors and potentiate endothelial cell proliferation, ultimately leading to enhanced normal endometrial growth.
Discount 100mcg proventil with visa
The signs and symptoms of dislocation include pain on movement of the joint asthma treatment by fish cheap 100mcg proventil fast delivery, the need to support the dislocated arm with the intact hand and distortion of the joint. Glenohumeral ligaments Comments Anatomical: the ligaments of the shoulder joint, which is a ball and socket joint, are the coracohumeral, the glenohumeral, the transverse humeral and the capsular ligaments. Physiological: the coracohumeral, the glenohumeral and the transverse humeral ligaments keep the shoulder joint stable and in place. In cases of repeated dislocations associated with stretching of the tendons, it becomes unstable and may need surgical attention. A lesion of the rotator cuff causes severe pain in the shoulder and reduces joint mobility. It may take a long time to recover its mobility, ranging from a few months to a few years. Trochlea Capsular ligament Synovial membrane Articular cartilage Ulna Radius Proximal radioulnar joint Capitulum Humerus Comments Anatomical: the elbow joint is a hinge joint formed by the articulation of three bones, the humerus (the trochlea and the capitulum), the ulna and the radius. The proximal radioulnar joint and the elbow joint are kept in place by a strong capsule and an extracapsular structure made up of anterior, posterior, medial and lateral ligaments. The biceps and the brachialis are responsible for flexion of the forearm and the triceps is responsible for its extension. Its diagnostic features include pain in the arm, swelling and a visible distortion of the joint contour. The complication to be avoided is a posttraumatic loss of mobility associated with incomplete extension of the elbow. Olecranon Ulna Proximal radioulnar joint Annular ligament Radius Comments Anatomical: the proximal radioulnar joint is the articulation of the head of the radius with the radial notch of the ulna. It is surrounded by a strong capsule and a strong extracapsular ligament, the annular ligament. Pronation depends on the action of the pronator quadratus and the pronator teres and supination depends on the action of the biceps and the supinator muscle. Coronoid fossa Coronoid process Trochlear notch Ulna Olecranon Trochlea Olecranon fossa Humerus Comments Anatomical: At the upper end of the ulna, a hook-like cavity lodges the trochlea at the lower end of the humerus at an angle of 10 degrees anteriorly. The coronoid process of the ulna lies in the anterior aspect of the arm, near the proximal end of the ulna, in continuity with the olecranon. Physiological: the movements at the elbow are flexion and extension and those at the proximal radioulnar joint are pronation and supination. The coronoid process maintains the stability of the elbow joint and prevents its dislocation. Ulna Articular disc of white fibrocartilage Synovial membrane Lunate Pisiform Triquetrum Hamate Capitate Proximal ends of the metacarpals Trapezoid Trapezium Scaphoid Capsular ligament Articular cartilage Distal radioulnar joint Radius Comments Anatomical: the wrist (radiocarpal) joint is an ellipsoid joint formed by the radius, the scaphoid, the lunate and the triquetrum. An articular disc of white fibrocartilage lies between the ulna and the cavity of the joint. Physiological: the movements at the wrist include flexion, extension, abduction and adduction. Ulna Ulnar collateral ligament Proximal ends of the metacarpal bones Radial collateral ligament Anterior radiocarpal ligament Radius Comments Anatomical: the anterior, lateral and medial radiocarpal ligaments keep the wrist joint and the distal radioulnar joint in place. Physiological: the movements of the wrist include flexion, extension, abduction (radial flexion), adduction (ulnar flexion) and circumduction. The ranges of flexion and adduction of the hand are greater than those of extension and abduction, respectively. Circumduction of the hand is the result of a combination of flexion, adduction, extension and abduction. The blood supply to the wrist depends on the palmar carpal arteries and veins, and its nerve supply comes from the radial, ulnar and medial nerves. Clinical: Pain caused or exacerbated by movement and associated with swelling suggests a sprain of the wrist, with or without a ligamentous rupture. In rheumatoid arthritis, the wrist and the joints of the hand are almost constantly painful. Scaphoid Trapezium Flexor retinaculum Synovial sheath (in blue) Median nerve Hamate Pisiform Tendons of flexor muscles (in white) Comments Anatomical: the carpal tunnel is the space bounded by the distal row of carpal bones (the hamate and the trapezium) and in which the flexor retinaculum, the tendons of the flexor muscles of the fingers and the median nerve are lodged. There are many synovial joints in the hand, and they are located between the constituent bones-for example, between the carpal bones, the carpal bones and the metacarpals, the metacarpals and the proximal phalanges. Physiological: the synovial fluid inside the synovial sheath prevents the tendons from rubbing against the bones. The movements of the fingers include flexion, extension, abduction, adduction and circumduction. The joints of the fingers, being of the hinge variety, allow only flexion and extension to occur. Clinical: the thumb is the most mobile finger because of its ellipsoid joints and can touch every other finger and the palm of the hand. Pain in the hand, paraesthesia and pins and needles in the fingers occurring at night, as well as loss of motor function, support the diagnosis of carpal tunnel syndrome, which affects mostly the first three fingers and is due to compression of the median nerve along its passage. Acetabulum of the hip bone Articular cartilage Acetabular labrum Synovial membrane Capsular ligament Femur Acetabular labrum Ligament of head of femur Comments Anatomical: the hip joint is a ball and socket joint between two bones, the hip bone and the femur. The acetabular labrum is a fibrocartilaginous ring, attached to the hip bone and that delimits the articular cavity in the hip bone. Physiological: the acetabular labrum plays a crucial role by controlling the range and types of movement in the joint-flexion, extension, abduction, adduction, rotation and circumduction-and maintaining its stability. Clinical: Pain in the inguinal region on walking and difficulty in performing some movements of flexion and rotation suggest osteoarthritis of the hip joint. It is due to the natural course of ageing of the joint and is associated with progressive thinning of the articular cartilage, the distorting effect of direct contact between the exposed surfaces of the bones and, occasionally, the development of an intraarticular effusion. Ilium Iliofemoral ligament Pubofemoral ligament Femur Ischium Pubis Comments Anatomical: the extraarticular ligaments of the hip joint are the iliofemoral, the pubofemoral and the ischiofemoral ligaments. Physiological: the hip joint is kept in place by the ligaments and by the periarticular muscles. Clinical: the signs and symptoms of hip dislocation include pain in the groin, distortion of the joint contour, abnormal orientation of the lower limb, asymmetry between the right and left hip joints and, possibly, some shortening of the affected limb. One must also look for secondary complications, such as a bone fracture, damage to the femoral artery and skin lacerations. Acetabulum Capsular ligament (cut) Ligament of the head of the femur Acetabular labrum Comments Anatomical: the acetabular labrum is a fibrocartilaginous ring attached to the hip bone. Physiological: the ligament of the head of femur helps maintain the stability of the joint. Clinical: Rupture of the ligament of the head of femur can damage the accompanying artery and lead to necrosis of the femoral head. Capsular ligament Synovial ligament Menisci (semilunar cartilages) Tibia Cruciate ligament Articular cartilage Femur Comments Anatomical: the knee joint is a hinge joint made up of three articulating bones-the femur, the tibia and the patella. Because the femur and the tibia do not fit together perfectly, the space between them is filled by the semilunar cartilages or the menisci, which are mobile and malleable fibrocartilaginous discs that rest on the tibial condyles and the intraarticular fat pads. The synovial membrane does not coat the menisci but covers the cruciate ligaments, which cross each other and attach the femur to the tibia. Physiological: the menisci bridge the gap between the femoral condyles and the tibial articular surface, stabilise and lubricate the joint and absorb the weight of the body and shocks. Clinical: When the shape of the menisci can adapt to the positions of the articulating bones during movements, the joint is stable. A pain on its own or that is associated with joint swelling suggests a meniscal lesion. Pain on movement made worse by a cracking sound, knee instability and a haemorrhagic effusion in the joint (haemarthrosis) suggest a severe sprain of the knee. Tubercle Anterior cruciate ligament Medial meniscus Posterior cruciate ligament Lateral meniscus Comments Anatomical: There are two cruciate ligaments, one anterior and the other posterior. The medial and lateral menisci are mobile and malleable fibrocartilaginous discs on top of the tibial condyles. Physiological: the menisci act as stabilisers, shock absorbers and distributors of stresses and lubricants by controlling the absorption and secretion of synovial fluid in the joint. The cruciate ligaments prevent forward displacement and excessive rotation in the joint. Being a hinge joint, it can perform only flexion and extension, with movements along only one axis. Clinical: A rupture or tear of a cruciate ligament can be partial or complete and affect one or both of these ligaments in the same knee. The anterior cruciate is most often involved as a result of a sudden change of direction in running or jumping, for example. Fibula Lateral malleolus Synovial membrane Talus Capsular ligament Medial malleolus Articular cartilage Tibia Comments Anatomical: the ankle joint is a hinge joint formed by the distal ends of the tibia and the fibula, the medial and lateral malleoli and the talus.
Proventil 100 mcg sale
However even at laparotomy asthma definition biweekly effective proventil 100mcg, it is very difficult to perform a complete ovarian cystectomy, as it is often difficult to see whether or not ovariolysis is satisfactory or if part of the ovary and/or cyst remains on the broad ligament. Therefore, in this situation, which is commonly encountered in patients previously treated for endometriosis and with assisted reproductive technologies, the best approach may be conservative management with close ultrasound monitoring until the end of the pregnancy, and surgical treatment considered within 2 to 3 months of delivery. Patients with a persistent adnexal mass and no previous surgical history are best operated upon early during the second trimester of pregnancy. There are no trials comparing laparoscopic and laparotomic surgery for the treatment of ovarian masses during pregnancy. Samples of peritoneal fluid and peritoneal washings are collected for cytologic examination. Then the paracolic gutters, diaphragm, omentum, the entire peritoneal cavity, and ovaries are scrutinized, looking for signs of malignancy. The ovaries may often be inspected before mobilization of the adnexal mass, because when the laparoscope is inserted above the uterine fundus, it is often possible to inspect the pelvic peritoneum without the intrauterine manipulator. The laparoscope is slowly moved behind the uterus, and there is often some space laterally between the adnexa and the pelvic sidewall making it possible to inspect the peritoneum and part of the ovarian surface. The second circumstance occurs when the adnexal mass is in the posterior cul-de-sac, hidden behind the uterus. In the first situation, it is important to grasp the adnexa before puncture of the cyst to avoid the mass "disappearing" after drainage into the posterior cul-de-sac. Adnexal masses may be hidden behind the uterus, but in this case, the left ovarian mass is located anteriorly and easily accessible for surgical dissection. This process may be optimized by tilting the table laterally toward the contralateral side, an approach that will shift the uterus to the opposite side, thereby creating a space that facilitates mobilization of the adnexa. Simultaneous vaginal examination and manipulation may also be helpful, pushing the adnexal mass higher in the peritoneal cavity. When the mass cannot be seen laparoscopically, a laparotomy is probably the best choice because access to the mass will not be easy. In our experience, it is generally possible to see and to treat the mass using a laparoscopic approach except in patients with severe pelvic adhesions. Management of the mass When the mass is visible, the surgical management is similar to that used in non-pregnant patients. The key point is to always grasp the adnexa to prevent it falling back behind the uterus before the end of the procedure. Indeed, mobilization of the adnexa is the most traumatic part of the procedure for both the adnexa and the uterus, and it is important to do it only once. Techniques used for ovarian cystectomy by the authors have been described previously and are also described in Chapter 41. Then hydrodissection may be performed through this small incision, which is enlarged carefully. The plane is identified as atraumatically as possible with some combination of scissors, continued hydrodissection, and appropriate grasping and dissecting forceps such as the curved and tapered "Maryland" design. The best cleavage plane is to be found when the surface of the cyst is white or yellow, without any red tissue. The risk and impact of inadvertent rupture of the cyst can be reduced by several measures. The surgeon should perform the dissection without grasping or pushing the cyst, avoiding the use of instruments applied perpendicularly the surface of the cyst, and keeping the active instruments as parallel as possible to the cyst surface. The instruments should always be moved in a direction that is away from the cyst, and the surgeon should perform the dissection in a patient and careful fashion until the structure is separated from the ovary. Prior to removal from the peritoneal cavity, it is often useful to aspirate the cyst contents while in the specimen bag to facilitate extraction. In our department, this technique has been successful in about 50% of the cases, whatever the experience of the surgeon. To treat large teratomas, greater than 7 cm in diameter, a careful puncture is made, and aspiration is performed using a 10-mm diameter suction system, after the mass is placed inside a laparoscopic specimen removal bag. If spillage occurs, aspiration and extensive lavage should be performed as quickly as possible. This usually is done following removal of the laparoscopic port; it is typically useful to aspirate the cyst contents to facilitate removal through the small laparoscopic incision. Then the cyst and the ovary are grasped through the peritoneum, which is incised while pulling the ovary against the abdominal wall, thus facilitating extraction of the ovary. The cyst and the ovary should be grasped close to the puncture site to minimize spillage. Thereafter drainage of the cyst is completed and the ovary is extracted through the 3-cm abdominal incision. The ovary is released into the peritoneal cavity without any suture, and the abdominal wall is closed. The increased uterine volume typically increases the distance between the origin of the ovarian vessels and the abdominal incision. Therefore, this method should be reserved for very large masses, which are generally accompanied by very long ligaments. The site of the minilaparotomy should be individualized, considering the length of the ligament. If the traction applied on the ligament is too strong, the adnexal vessels may be torn, necessitating a laparotomy to control the bleeding. A cap is also available (shown above) that facilitates repositioning of a laparoscopic port. When performing adnexal surgery during pregnancy, three efficient grasping forceps should be available, since one is always used to prevent the ovary from falling behind the uterus. The cleavage plane should always be exposed as clearly as possible by coupling meticulous technique with proactive hemostasis. When pulling the forceps in opposite directions to dissect the cyst from the ovary, short and slow movements must be used and the position of the forceps on the cyst wall and on the remaining ovarian tissue adjusted often enough to obtain ideal exposure of the plane. The dissection is performed, the cyst wall is on the left side of the picture, the correct dissection plane shown in the upper part of the photo while a suboptimal dissection plane is visible in the lower aspect of the dissection-it is more red in color. The scissors are used to incise the ovarian cortex down to the level of the capsule of the ovarian cyst. The best plane will be found by improving the exposure of the cleavage plane using two tenacious grasping forceps. Adnexal torsion It is essential to stress, particularly for general gynecologists, that treatment of adnexal torsion is a surgical emergency,28 even if the acute pelvic pain may be effectively relieved using oral drugs. A late diagnosis will increase the risk of adnexal necrosis, of spontaneous abortion, and/ or of premature labor. The cyst wall is inspected, looking for solid projections; the cleavage plane is visible (arrows). Adnexal mass occurring with intrauterine pregnancy: report of fifty-four patients requiring laparotomy for definitive management. Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. Outcome in laparoscopic management of persistent adnexal mass during the second trimester of pregnancy. Arterial to end-tidal carbon dioxide pressure difference during laparoscopic surgery in pregnancy. Laparoscopic management of a ruptured benign dermoid cyst during advanced pregnancy. Adnexal masses in pregnancy: a review of 130 cases undergoing surgical management. Laparoscopy versus laparotomy in the management of adnexal masses during pregnancy. It can be performed vaginally, or abdominally via laparotomy, or laparoscopically. Due to a trend toward late childbearing, fertility preservation has become a major issue in young patients with gynecological cancer. One in 51 women will be diagnosed with cancer by age 39 and one in 19 women by age 49. Fertility-sparing treatments have been successfully attempted in selected cases of cervical, endometrial, and ovarian cancer. Therefore, the gynecologist should be familiar with fertility-preserving options in patients with gynecological malignancies.
Purchase generic proventil line
Alkalinization increases urothelial penetration and may increase effectiveness asthma jobs buy cheap proventil online, but it also increases systemic absorption and potential toxicity. Common side effects are dysuria, urethral irritation, and bladder pain or burning. The differential diagnosis includes recurrent vaginitis, non-provoked vulvodynia, provoked vestibulodynia, pelvic congestion syndrome, and pelvic floor tension myalgia. There sometimes is a history of long bicycle rides, episodes of prolonged sitting, or pelvic trauma immediately preceding the onset of symptoms. Also, reconstructive pelvic surgery can damage the nerve from compression, scar tissue formation, or direct impingement. Symptoms can include hyperesthesia, allodynia, paresthesias, burning or stabbing pain, sensations of incomplete voiding or inability to void normally, overactive bladder, dyspareunia, bowel dysfunction, sensation of a mass in the rectum, and pain with defecation or dyschezia. The pudendal nerve arises from the sacral plexus (S2S4) and then splits into the anorectal, perineal, and clitoral branches. Image-guided pudendal nerve blocks directed at these locations can be both diagnostic and therapeutic. If the pain is relieved after injections (local anesthetic with or without steroids), then most likely the source of the pain has been identified. Pain relief may take 1 to 2 months for maximum benefit and should last at least several months. Medical management with a tricyclic antidepressant or gabapentin is often helpful. Other treatment options include pelvic floor physical therapy, pregabalin, oral muscle relaxants, and local muscle relaxants (vaginal diazepam and rectal belladonna and opium suppositories). For example, there is evidence from brain imaging studies of morphologic and functional changes associated with chronic pain syndromes. However, it is important to recognize that trying to determine whether chronic pain is "physical" (neurological) or "mental" (psychological) is not useful; somatogenic and psychogenic labels need not be, and most often are not, mutually exclusive. Trying to make such a distinction about pain is not useful in designing treatment, nor is it consistent with the current biologic understanding of pain. It is important when managing chronic pain that all of these aspects of pain, not just the pain level, be addressed. The patient needs to recognize that pain relief is important but is only one aspect of managing chronic pain. And she must realize that repeated disease-specific treatments, such as multiple, annual surgeries for endometriosis, are not effective. Currently available treatments reduce pain levels by an average of only about 30%. Management is complex and multimodal, and rarely will the gynecologic surgeon be the sole practitioner in treating chronic pain. The major treatment options for chronic pain are: (1) pharmacological, (2) psychological or behavioral, (3) physical therapy, (4) interventional, (5) neuromodulation or neuroablation, and (6) surgical. Surgical interventions are generally disease-specific treatments, exemplified by excision of endometriosis or hysterectomy for adenomyosis. However, for many patients, this approach is inadequate, and treatment of the ongoing symptom of chronic or persistent pain is needed. Treatment of pain is based on the concept that when pain is chronic or persistent, the pain itself can become an illness, i. A thorough evaluation with pain-directed history and physical examination, with surgical interventions reserved for those with clear diagnoses amenable to surgery, is crucial to providing care that helps rather than hurts. Realizing the likelihood of multiple diagnoses and the potential of chronic pain as a diagnosis is important to providing such care. Prevalence and incidence of chronic pelvic pain in primary care: evidence from a national general practice database. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Prevalence and correlates of three types of pelvic pain in a nationally representative sample of Australian women. Use of the Short-Form McGill Pain Questionnaire as a diagnostic tool in women with chronic pelvic pain. How neuroimaging studies have challenged us to rethink: is chronic pain a disease How reliable is a self-administered questionnaire in detecting sexual abuse: a retrospective study in patients with pelvic-floor complaints and a review of literature. Emotional, physical, and sexual abuse in patients visiting gynaecology clinics: a Nordic cross-sectional study. Relaxin is not related to symptomgiving pelvic girdle relaxation in pregnant women. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: a systematic review. Stenosis of the external cervical os: an association with endometriosis in women with chronic pelvic pain. Two cases of supernumerary ovary and one of accessory ovary, with an analysis of previously reported cases. The efficacy of laparoscopic surgical treatment of ovarian remnant and ovarian retention syndromes. Conservative management of corpus luteum haemorrhage in patients on anticoagulation: a report of three cases and review of literature. Oral desipramine and topical lidocaine for vulvodynia: a randomized controlled trial. A randomized comparison of group cognitive-behavioral therapy, surface electromyographic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Surgical and behavioral treatments for vestibulodynia: twoand-one-half year follow-up and predictors of outcome. Follow-up report on a randomized controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal to moderate endometriosis. Influence of endometriosis on pain behaviors and muscle hyperalgesia induced by a ureteral calculosis in female rats. Surgical treatment of endometriosis: a 7-year followup on the requirement for further surgery. Predictors of chronic pelvic pain in an urban population of women with symptoms and signs of pelvic inflammatory disease. Multicystic mesothelioma: an analysis of pathologic findings and biologic behavior in 37 cases. A randomized controlled trial of medroxyprogesterone acetate and psychotherapy for the treatment of pelvic congestion. A randomized controlled trial of goserelin and medroxyprogesterone acetate in the treatment of pelvic congestion. Embolisation of symptomatic pelvic veins in women presenting with non-saphenous varicose veins of pelvic origin-three-year follow-up. Bilateral laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndrome. Understanding multisymptom presentations in chronic pelvic pain: the inter-relationships between the viscera and myofascial pelvic floor dysfunction. The pelvis and beyond: musculoskeletal tender points in women with chronic pelvic pain. A randomized, controlled study comparing a lidocaine patch, a placebo patch, and anesthetic injection for treatment of trigger points in patients with myofascial pain syndrome: evaluation of pain and somatic pain thresholds. Botulinum toxin A versus bupivacaine trigger point injections for the treatment of myofascial pain syndrome: a randomised double blind crossover study.
Purchase genuine proventil line
The tubal lumen (arrow) is completely obliterated by dense collagenous connective tissue (Hematoxylin and eosin stain) asthma treatment devices discount proventil 100 mcg online. This prompted the assumption that the mechanical arrest of ovum transport may lead to nidation within a pseudo gland. These post-electrosurgically induced lesions lack the feature of (reactive) muscular hypertrophy and have been coined endosalpingoblastosis as opposed to endosalpingiosis. Since both uterine and tubal features may be found in the same specimen, their origin is postulated to be from pluripotent coelomic stem cells. Diagnosis the mainstays of diagnosis are the distinctive radiologic and laparoscopic appearances. With transcervical injection of a dye solution, characteristic diverticula may become visible. Note the fusiform shape of the cornua (C) and the intravasation of the blue dye solution in the superficial vessels of the fundus. Continuing hormonal stimulation produces a steady progression of the tubal lesion as well as ovarian cyst formation. The absence of muscular hypertrophy in the animal model could implicate a cofactor, possibly inflammation in humans. The evidence supporting this view is circumstantial, based predominantly on historical, histological, serological, and radiological evidence of associated inflammation or infection. Of all the current pathological conditions of the oviduct, this disease warrants the most research. Distal tubal disease and occlusion the degree of damage to the pelvis may range from a few filmy peritubal adhesions with tubal patency to a "frozen pelvis" and an occluded distal oviduct. The anatomical distortion may be categorized as peritubal, occlusive tubal, and ciliary. If the fallopian tube is freely mobile with space between the tube, ovary, and pelvic sidewall, and the adhesions are easily transected, then the prospects for restoration of tubal function are reasonable. If the adhesive process has fused the tube to the ovary, usually with dense adhesions, then the probability of successful correction is diminished. If the ovary and/or oviduct have fused additionally to the pelvic sidewall, often with loss of ovarian volume, then the prospects for effective repair are guarded (Chapter 27). The tube is distended with blue dye solution which is visible through the adhesion. Ascending genital tract infection 279 some studies suggest that reversal of sterilization helps restore both body image and self-esteem (Chapter 39). However, in our experience, it is an unusual cause unless it is complicated by rupture and its sequelae. The peak incidence of the disease is between ages 14 and 24 and so affects the female during reproductive life. There have been conflicting reports in the literature regarding the prevalence of infertility in the patients. Furthermore, most studies pertain to heterogenous groups of women who may or may not have active disease or medical therapy or bowel surgery. One of these was approved by the American Fertility Society, currently the American Society of Reproductive Medicine. This rate is much lower when the tubal epithelium is greatly affected, and higher when mildly affected. Scarring, limited tubo-ovarian mobility, reduced ovarian surface, and compromised ovulatory function may compound the abnormal transport. Delay in retrieval or transport of the cumulus complex may result in blastocyst formation within the oviduct and an ectopic implantation. Sterilization reversal Female sterilization by surgical occlusion of the fallopian tubes is the most widely used contraceptive method worldwide, accounting for 10% to 40% of contraceptive methods. In the United States of America, 20% of sterilized women seek a reversal, but less than half of these will actually undergo reversal of sterilization. The blood supply to the cyst may be compromised with consequent inflammatory adhesion of the ischemic cyst to adjacent pelvic structures. Accessory tubal ostia An ampullary ostium on a tissue stalk may or may not communicate with the tubal lumen. Coelomic invagination has been postulated as the causative mechanism for accessory ostia and multiple lumina. The presence of a rudimentary or noncommunicating uterine horn may be misdiagnosed as an occluded proximal tube. Only a web of mesosalpingeal tissue links the terminus of the occluded ampulla with the isolated fimbrial tissue (Chapter 27). Prefimbrial phimosis Prefimbrial phimosis may be a partial expression of the process that leads to ampullary atresia. This appears to be an intermediate degree of stenosis between a normal distal ampulla and ampullary atresia. Abdominal ovaries In this rare condition, the infundibulopelvic ligaments are short, and the ovarian ligaments are commensurately longer. Elongated fallopian tubes On occasion, a fallopian tube can be significantly elongated. This does not impair function, provided there has been no damage to the tube and the fimbrial-ovarian special relationship is normal. In this woman, the ovaries were located at the pelvic brim, superior to the normal location. Although the initial oviductal infection is mucosal; thereafter, the muscularis and serosa are involved. Tuberculosis has a proclivity to infect tubal mucosal epithelium (as it does the endometrium) by hematogenous spread. At first the disease is a microscopic infection secondary to a primary focus (usually respiratory). It then may progress to become nodular, albeit with preservation of fimbria, or adhesive with distortion of the adnexa. In the exudative form of tuberculosis, salpingitis-caseated granulomata can coalesce to simulate a pyosalpinx. The contrast material that has escaped from the distal end of the fallopian tube surrounds the cyst (arrow). The extensive tubal damage caused by this disease is such that tubal repair cannot yield functional fallopian tubes. A A Tubal polyps Tubal polyps are usually located within the intramural segment, and less often in the isthmus. They consist of polypoid functional endometrial tissue anchored on a stalk that extends from the cornual endometrium. They are often bilateral with a single polyp at each site and range from a few millimeters to over a centimeter in size. Short segments of rigid proximal tubes (arrows) with distal enlargement and intrauterine adhesions (A). Endometriosis and the development of tuboperitoneal fistulas after tubal ligation. Tubal lesions subsequent to sterilization and their relation to fertility after attempts at reversal. The limited clinical usefulness of taking a history in the evaluation of women with tubal factor infertility. Lower genital tract infection and endometritis: insight into subclinical pelvic inflammatory disease. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Factors predicting upper genital tract inflammation among women with lower genital tract infection. The accuracy of serum chlamydial antibodies in the diagnosis of tubal pathology: a meta-analysis.