Sulfasalazine 500 mg overnight delivery
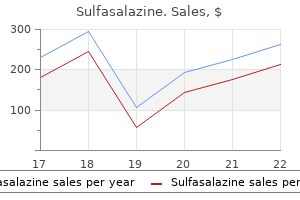
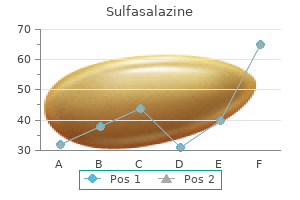
There is no evidence to support routine screening of patients taking tamoxifen at standard doses pain diagnosis and treatment center pittsfield ma purchase sulfasalazine with mastercard. Ancillary Testing Clinical Features Patients develop white, glistening crystals in the inner plexiform layer and nerve fiber layer. With high doses, patients may lose vision due to direct retinal toxicity as well as macular edema and optic neuropathy. Optical coherence tomography also demonstrates the cystoid spaces as well as photoreceptor disruption. With extended use, renal failure ensues due to the oxalate deposition in the kidney. Both flecked retina and crystalline retinopathy have been reported in primary disease. It is a naturally occurring carotenoid also used to treat vitiligo and disorders involving photosensitivity. It also can be found in common foods and has been suggested to be toxic with large dietary ingestion. Optic nerve head edema may be present, and these patients can have significant visual loss. Permanent vision loss may be due to the optic nerve disease, as patients with only retinopathy had improvement in both symptoms and signs. Alone or in combination with ribavirin, interferon is now the standard of care for treatment of hepatitis C. An ischemic retinopathy can develop in patients taking interferon, in some cases causing serious visual decline. Many of the descriptions of interferon retinopathy are in the Japanese language literature. Subsequently, corroborating reports have described ischemic retinopathy in both cancer treatment and hepatitis C treatment. Common side effects, such as flushing, rise in uric acid levels, and gastritis have curtailed its use in exchange for other cholesterol reducing medications. Electroretinography shows a decrease in the amplitude of the b-wave under both scotopic and photopic conditions. The edema rapidly improves after discontinuation of niacin with resolution and improvement in vision commonly within 2 weeks. In two of the well documented cases, the patients received more than 40 g total of clofazimine. Optical coherence tomography does, however, demonstrate cystoid spaces in the outer plexiform layer. Minor disruptions in the blood-ocular barrier may cause leakage too slow for fluoroscein angiography, but still result in edema. Excessive levels of iron can lead to cardiac failure; so the treatment is often life-saving. The most common predisposing factor is repetitive blood transfusions in patients with thalassemia or aplastic anemia. Patients with renal failure and high aluminum levels are also sometimes treated with deferoxamine. It is currently under increased study for use in multidrug resistant tuberculosis as well as systemic or discoid lupus erythematosus. It also causes brownish discoloration of the conjunctiva, tears, and thin superficial lines in the cornea. All of the patients died within months of the detection of the retinopathy and there was no pathologic specimen obtained. After receiving multiple transfusions, the patient developed hemosiderosis treated with deferoxamine. Haimovici also reported patients with peripapillary, papillomacular, and paramacular changes similar to those described above. Gonzalez and co-workers reported two patients treated with deferoxamine who presented with vitelliform lesions. When methanol is ingested, an anion gap metabolic acidosis occurs with acute renal failure. Fomepizole is a competitive alcohol dehydrogenase inhibitor with demonstrated efficacy in methanol poisoning. It is the active ingredient in tonic water, which was used by sailors as a malaria prophylactic. While vision may return, patients may be left with permanent, severe visual field constriction. During the acute phase, the retinal arterioles can be normal with mild venous distention. Within weeks to months, the arterioles become severely constricted and the optic nerve becomes atrophic. At least two teams of investigators have suggested that deferoxamine may increase the transport of copper, out of cells and raise the extracellular concentration of copper. A model of deferoxamine toxicity in the albino rat demonstrated increased toxicity with light and oxygen exposure. It may be a direct effect of the drug or a secondary effect from chelation of divalent metal ions. One study in albino rats showed a reduction in toxicity as measured by electrophysiology when it was conjugated with hydroxyethyl starch. Any patient treated with deferoxamine should be carefully monitored for visual changes. Although a dose dependent toxicity was found in one study, no dose response or risk factors for retinopathy were found in another. Inhalation and skin contact can also induce 2220 Retinal Toxicity of Systemic Medications Visual field changes can be asymptomatic, and, in children, accurate peripheral visual testing can be dfficult. Miyata M, Imai H, Ishikawa S, et al: Changes in human electroretinography associated with thioridazine administration. Oshika T: Ocular adverse effects of neuropsychiatric agents: incidence and management. Easterbrook M: the sensitivity of Amsler grid testing in early chloroquine retinopathy. Easterbrook M, Trope G: Value of Humphrey perimetry in the detection of early chloroquine retinopathy. Duncker G, Schmiederer M, Bredehorn T: Chloroquine-induced lipidosis in the rat retina: a functional and morphological study. Duncker G, Bredehorn T: Chloroquineinduced lipidosis in the rat retina: functional and morphological changes after withdrawal of the drug. Harnois C, Samson J, Malenfant M, et al: Canthaxanthine retinopathy: anatomic and functional reversibility. Harnois C, Cortin P, Samson J, et al: Static perimetry in canthaxanthin maculopathy. Functional and morphological alterations of the rabbit retina after 11 months dietary carotenoid application. Functional and morphological alterations of the rabbit retina after acute canthaxanthin application with small unilamellar phospholipid liposomes. Kawano T, Shegehira M, Uto H, et al: Retinal complications during interferon therapy for chronic hepatitis C. Esmaeli B, Koller C, Papadopoulos N, Romaguera J: Interferon-induced retinopathy in asymptomatic cancer patients. Tokai R, Ikeda T, Miyaura T, et al: Interferon-associated retinopathy and cystoid macular edema. Kiratli H, Irkee M: Presumed interferonassociated bilateral macular arterial branch obstruction.
Buy sulfasalazine 500 mg cheap
Cases of conjunctival perforation resulting in persistent leak have been described neck pain treatment options buy discount sulfasalazine 500mg on line. The suture is placed by passing the needle from just behind the limbus beside the scleral flap to emerge from the corneal groove. The needle is passed back into the corneal groove, through the partialthickness scleral flap and emerges from the posterior third of the flap. Adjustable sutures A recent development in scleral flap suture technique was an adjustable suture which allows trans-conjunctival adjustment of tension postoperatively using specially designed forceps with smooth edges (DuckworthandKent. Adjustable suture forceps with special fine smooth tips for transconjunctival suture adjustment without tearing conjunctiva. It can be manually cut and removed with appropriate blade and scissors, or alternatively a special punch can be used. Transconjunctival loosening of adjustable sutures without sudden fall in intraocular pressure. An anterior incision reduces the risk of iris incarceration and bleeding from the iris root or ciliary body. This has led to a reduction in cystic areas within the bleb from 90% to 29% as well as the rate for blebitis and endophthalmitis. Punch sclerostomy A punch sclerostomy is the method of choice, and many punches are available. An infusion can be placed to maintain a continuous intraocular pressure particularly in high-risk patients 4. Manual block removal If a blade and scissors are used it is difficult to cut a sclerostomy much smaller than 3 1. The rest of the block is dissected posteriorly to full-depth, using a blade or Vannas scissors to cut the base. Anterior segment infusion to maintain intraocular pressure and gauge opening pressure of sclerostomy. Inserted with an oblique paracentesis in a phakic eye to minimize any risk to lens. Glaucoma Filtration Surgery; Indications, Techniques and Complications applied to the block during dissection preventing damage to the iris and underlying structures. Scleral flap sutures are tighted/loosened accordingly and extra sutures placed as needed. The iris can be made to present through the sclerostomy without intraocular manipulation using an infusion, reducing iris trauma and the need for an assistant. Therefore great attention has been focused on reproducible water-tight closure technique. Traditional closure used single interrupted suture at the ends of conjunctival incision, newer techniques include the use of lateral purse-string sutures, interrupted horizontal mattress sutures78 or a suture with corneal grooves. Absorbable suture is preferred for patient comfort and ease of management despite the theoretical increase in inflammation. Mydriatics/cycloplegics such as atropine 1% may be used although with advanced techniques this is now less common. Iris presenting through small sclerostomy with gentle pressure on back edge when infusion used. Corneal groove creation (five grooves) for closure of fornix based conjunctival flap to minimize leakage and suture discomfort. Topical Antibiotics Patients usually receive antibiotics for ~4 weeks postoperatively. The placement of a paraffin gauze dressing (Jelonet), eye pad followed by shield ensure closure and offers extra protection. The aim is to achieve good lid closure and prevent any corneal epithelial breakdown, which can be slow to heal postoperatively, causing subsequent postoperative treatment (steroids) and bleb manipulation delays. Topical NonSteroidal Antiinflammatory Drugs these may be useful in selected patients at high risk of failure but their efficacy is not proven. The keys to successful postoperative bleb management are early recognition of a failing bleb, dedicated surgeon time and correct selection and timing of the various intervention options. Oral or Intravenous Steroids Systemic steroids are not used routinely due to their potentially dangerous side-effects. Steroids (prednisolone acetate 1%) are prescribed 2 hourly for the first 2 weeks with subsequent dosing adjusted according to bleb morphology. Most patients receive a reducing dose of topical steroids for ~8 weeks postoperatively. A flat bleb may result from tight scleral flap sutures and digital pressure through the upper lid is exerted as posterior as possible to the scleral flap under direct slit-lamp visualization until a good bleb forms. The absence of a wound leak is a prerequisite to successful bleb massage and it is essential to avoid an iatrogenic wound leak which delays further bleb manipulation. One or more sutures are sequentially removed/lysed between 1 and 4 weeks postoperatively. Excessive needling should be avoided due to the risk of hypotony and the associated complications such as suprachoroidal hemorrhage. Fortunately, this scenario is less common as subscleral flap needling is a high-risk procedure and direct visualization of the needle tip may not be possible. This is important in a soft eye due to the increased risk of intraocular tracking. This is achieved by puncturing and/or loosening scar tissue in the region of the filtration bleb. The patient is asked to look down using an assistant or speculum to retract the upper lid. The bleb is approached with a 29G needle via a very posterior superior fornix entry. Multiple stabs toward the scleral flap are made until a clear increase in bleb size is achieved. Management If the scleral flap is damaged during construction/dissection, further surgery should continue at a new site with undamaged sclera. In severe damage where the sclerostomy cannot be secured, an autologous or donor scleral patch, or processed pericardium may be sewn onto the operation site to regain globe integrity. Prevention the preoperative use of topical apraclonidine 1% or adrenaline significantly reduces tissue vascularity and bleeding, improving visualization and control of the operative field. In nanophthalmic eyes, scleral decompression may be required before intraocular entry. Similarly, postoperative suprachoroidal hemorrhage is prevented by prevention of hypotony. Management If a conjunctival tear occurs without adjuvant antifibrotic, it can be repaired by a simple purse-string vicryl suture on a vascular needle. The use of topical apraclonidine 1% or adrenaline at time of surgery effectively reduces tissue vascularity. Management Gentle wet-field diathermy (either bipolar or unipolar) can be used to control bleeding. Scleral Flap Damage Damage to the scleral flap including tearing or buttonhole can occur during flap construction (before sclerostomy) or after sclerostomy. Note iridolenticular instability preoperatively and consider alternative procedure. Aqueous leakage decreases bleb height and leads to increased subconjunctival fibrosis and failure. Careful conjunctival edge protection during antifibrotic application and the use of a noncrushing clamp. Management Small wound leaks are often self-limiting especially in the presence of an elevated bleb with good posterior aqueous drainage. Significant leaks with hypotony and choroidal effusions are best managed by wound resuturing. Pre- and postoperative hypotony and systemic hypotension, all of which may compromise an already damaged optic nerve should be avoided. Patients should seek ophthalmological attention immediately if they develop a purulent discharge.
Purchase sulfasalazine 500mg with mastercard
One group had bilateral vision with light perception to counting fingers pain treatment machine purchase sulfasalazine 500 mg on-line, and another group had 20/200 to 20/400 vision. Calculation of Time Trade-off How many more years does participant expect to live The inability to recognize a friend or loved one would also increase feelings of social isolation and impact functioning. In particular, among the participants who had no prior laser treatment in the affected eye, 60/447 (13%) were classified as having either doubtful or definite anxiety, and 57/447 (12%) as having doubtful or definite depression, using the Hospital Anxiety and Depression Scale. If the boundaries are not well-demarcated, or if one is not certain if the lesion extends under the foveal center, or if the lesion is so close to the foveal center that the treating ophthalmologist believes the scotoma from treatment will outweigh any benefits of treatment, then one could manage the lesion as if its location were subfoveal as described below. Dashed line indicates eyes assigned randomly at entry to no treatment; solid line, eyes assigned at entry to laser treatment. From Macular Photocoagulation Study Group: Argon laser photocoagulation for neovascular maculopathy after five years. By 3 years, 63% of the eyes assigned to no treatment and 45% of the eyes assigned to treatment had severe visual loss. The relative risk of losing 6 lines or more of visual acuity from baseline among untreated eyes (n = 117) compared with laser-treated eyes (n = 119) was 1. About 75% of all these recurrences occurred by the end of the first year after treatment. An additional 17% of all the recurrences occurred between 1 and 2 years of follow-up. At the end of the third year of follow-up, the average visual acuity of the treated eyes with no recurrence was 20/50 and that of the treated eyes with recurrence was 20/250. The investigators believed that fluorescein leakage within this time might represent persistence of neovascularization. However, one could consider using the term recurrence whenever the following conditions apply: (1) leakage is seen at the periphery of a laser-treated area and (2) one has previously documented unequivocal lack of peripheral leakage after treatment. A persistence could be defined as leakage at the periphery of the laser-treated area without any prior unequivocal documentation of lack of peripheral leakage on prior fluorescein angiograms. Topical anesthesia usually is sufficient if one is careful to ensure that neither ocular motility nor patient discomfort will compromise the success of treatment by preventing the ophthalmologist from delivering laser of sufficient intensity and duration of exposure to produce a uniform white treatment burn. This is especially true when small amounts of undertreatment may allow persistence of neovascularization93,94 or small amounts of overtreatment might obliterate foveal structures unnecessarily. Thus, no visible wavelength appears to have a significant advantage over other wavelengths. There is no evidence to suggest that this technique compromises the effectiveness of treatment. Certain subgroups in the various trials had different treatment benefits, which should be considered when determining whether treatment would be beneficial for a particular patient. Rather, the subgroup analysis data should serve as a guideline when trying to decide whether treatment should be recommended to a particular individual. For instance, in the krypton trial of juxtafoveal lesions,89 patients who were normotensive had a marked treatment benefit. Patients who had evidence of hypertension, either by elevated systolic or diastolic blood pressures or by the use of antihypertensive medications, had no treatment benefit. From Macular Photocoagulation Study Group: Persistent and recurrent neovascularization after krypton laser photocoagulation for neovascular lesions of ocular histoplasmosis. The desired endpoint for the intensity of the laser lesion is to create a uniformly relatively white lesion. This laser is no longer recommended for treatment within the macular region because macular xanthophyll pigment directly absorbs the blue light of the argon blue-green laser, thereby inducing thermal damage to the inner retina. None of the findings from the subfoveal trials suggests a reason to favor either the argon green or the krypton red wavelength. Evaluation of photocoagulation treatment can be determined by placing the treatment drawing (c) under the pretreatment drawing (a) on a lightbox. Slight extension of treatment should have little effect on the visual acuity, since the treatment in these situations will not affect central foveal photoreceptors. In step 2, immediately after treatment, a posttreatment photograph (digitally) or Polaroid (film) is taken. In step 3, the treatment drawing from step 2 is placed on a light box, and the pretreatment drawing from step 1 is placed over this, superimposing the landmark vessels, or superimposed by digital image software. If so, then one determines if the patient has had presumed recent disease progression in this eye. Presumed recent disease progression includes any of the following: blood associated with the lesion, visual acuity loss within the past 3 months, or growth of the lesion on fluorescein angiography within the last 3 months. In the absence of presumed recent disease progression for a subfoveal lesion with a minimally classic or occult with no classic lesion composition, careful follow-up, perhaps at 3 week, and then 6 week, and 3 month, intervals is indicated to watch for progression to a predominantly classic lesion (see below) or development of presumed recent disease progression. Side effects that occurred more frequently in the ranibizumab arms than in the control group at 1 year included mild to moderate conjunctival hemorrhage, eye pain, and vitreous floaters. Uveitis and endophthalmitis occurred in fewer than 1% of patients in the ranibizumab and control groups. Serious nonocular adverse events occurred essentially as frequently among ranibizumab-treated patients as among controls. This randomized, double-masked, active treatment-controlled study compared safety and efficacy of 0. Results from this study showed that 94% (132/140) of ranibizumab-treated patients assigned to 0. In addition, ranibizumab-treated patients were more likely to improve 10 or more points in ratings of dependency on others because of vision than were sham injection patients. Since then, additional reports have appeared in the literature presenting safety evaluations of the drug when injected into the vitreous of rabbits,109 immunofluorescent studies suggesting the ability of bevacizumab to penetrate the retina,109 and evidence of potential clinical efficacy. The strength of evidence to support use of bevacizumab is weaker, based on case series and anecdotal reports. It is unknown at this time if intravitreal bevacizumab is almost as good, better, or worse than ranibizumab for reducing the risk of visual acuity loss and increasing the chance of visual acuity gain. However, the evidence may be strong enough to warrant consideration of bevacizumab when ranibizumab is not available to a patients because of regulatory limitations. Patients received an infusion of bevacizumab (5 mg/kg) at baseline, followed by one or two additional doses at 2 week intervals. No serious ocular or systemic adverse events were identified during safety assessments, which were performed at all visits. The only treatment-related adverse event was a treatable, reversible, mild elevation of systolic blood pressure (+12 mm Hg; P=. As compared to 164 (55%) of 296 patients in the control group, 206 (70%) of 294 patients treated with 0. However, because the results were far different from that obtained with ranibizumab, most ophthalmologists would not consider the use of pegaptanib over ranibizumab at this time. This conclusion should be evaluated with caution, however, as based on these small numbers, the confidence intervals surrounding the estimated percentage values are likely to be rather wide. With respect to safety, the risk of endophthalmitis in any invasive ocular procedure may be minimized with proper aseptic technique, the use of a lid speculum, careful postinjection monitoring, and educating patients about which postinjection symptoms to report to the physician. Bevacizumab is not manufactured with the strict particulate matter limits that are required for ocular drugs, such as ranibizumab, nor does it contain preservatives. Additional data are needed to determine if bevacizumab results in similar efficacy and safety to warrant its use when ranibizumab is available. When ranibizumab is not available because of regulatory limitations or cost, bevacizumab might be considered. In one study of Medicare enrollees in a nationwide managed-care system, one third of English-speaking patients, and more than one half of Spanish-speaking patients, exhibited either marginal or inadequate health literacy, and thus were unable to understand consent forms or medicine labels. In addition, health literacy tended to decline with age, with inadequate health literacy exhibited in only 15. If an ophthalmologist uses the same level of language with all patients, there is a risk, therefore, that a substantial minority of patients will be unable to comply with treatment plans. This, in turn, can lead to patient disappointment and ophthalmologist frustration, since a treatment would likely be more effective if the patient were compliant with instructions.
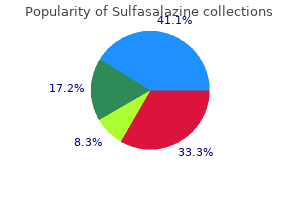
| Comparative prices of Sulfasalazine | ||
| # | Retailer | Average price |
| 1 | Ace Hardware | 936 |
| 2 | The Home Depot | 114 |
| 3 | QVC | 443 |
| 4 | RadioShack | 255 |
| 5 | Subway | 952 |
| 6 | Walgreen | 306 |
| 7 | Sports Authority | 577 |
| 8 | AT&T Wireless | 919 |
Order 500mg sulfasalazine overnight delivery
Direct ophthalmoscopy has the distinct advantage that all features of the angle are in their normal spatial relationship to the observer pain management treatment cheap 500 mg sulfasalazine with amex. A broad panoramic view of the contours of the angle is obtained with great flexibility in viewing angle and lighting. For direct surgical intervention in the angle, the direct view is the only practical approach. Several specialized surgical lenses have been designed to allow simultaneous instrumentation and viewing of the angle. With experience, this is usually not a problem, but the initiate to gonioscopy will find this more challenging than the direct view afforded by the Koeppe lens. Because the mirrored lens can be used at the slit lamp, all the advantages of the slit lamp become advantages of the technique, i. The slit lamp affords stable and well-focused illumination coupled with high-magnification optics. Slit lamp-based gonioscopy also has the advantage of being directly compatible with slit lamp-based lasers. One extremely useful variation of indirect gonioscopy is a four-mirror lens with a small central region of contact. Because the curve of the lens closely matches the anterior surface of the cornea, no special gonioscopic fluids are used, and the normal tear film provides an optical coupling of the lens to the cornea. This makes the examination convenient and causes less blurring of vision than when gonioscopy is performed using viscous contact fluids. But the special utility of these lenses relates to their small (~5 mm), central, and relatively flat area of contact with the cornea. Because the area of contact is small and central, gentle posterior pressure on the lens will indent the central cornea, displacing aqueous fluid and deepening the periphery of the anterior chamber. This particular maneuver can be helpful in assessing the degree of synechial closure of an extremely narrow angle. Frequently, an angle will appear so narrow that usual gonioscopic techniques do not make clear whether the angle is actually closed by synechiae or is merely extremely narrow, or even touching, but without synechiae formation. By gentle indention of the central cornea with the four-mirror lens, the chamber can be transiently deepened in the periphery, and this differentiation can be made. The most widely recognized use for gonioscopy is in the differentiation between narrow-angle glaucoma and open-angle glaucoma. All patients with elevated pressures should have gonioscopy to make this important differentiation. Different systems for grading the narrowness of the angle have been developed in an attempt to help the clinician define the appearance of the angle in concrete terms and make some reasonable prediction of the threat of angle closure. A grade 0 angle is considered closed and allows no view of any of the angle structures. Spaeth9 suggested a somewhat more complex grading system that includes a capability for recording not only the angle between iris and cornea but also an estimate of the height of iris insertion and of the general shape of the iris contour. Such variations serve to emphasize the difficulty of reducing the variability of angle appearances to a single numerical value. Although it may be useful to sort out gonioscopic appearances initially on the basis of four or five angle grades, the duty of the gonioscopist does not stop there. Features such as the peripheral iris contour, the distribution of pigmentation, and consistency of appearance from one region to the next, all demand careful attention. Thus, rather than rely on numerical grades, the gonioscopist should consider using descriptive language to document angle appearance. It is really not possible to produce a simple and short list of gonioscopic findings that will separate normality from pathology. There are some discrete and obvious findings that will be evident if only looked for. These would include foreign bodies in the angle, large peripheral synechiae, and proliferation of new vessels. Many other findings are more subtle and will be evident only to the observer who has an extensive grounding in the appearance and variations of the normal angle. For this reason, gonioscopy should be performed frequently, not only in patients for whom it is absolutely essential but also in a fair number of normal individuals in order to build an internal sense of the clinical appearance of the chamber angle. If the examiner has not observed a number of normal infant angles (which can be done. Only by being comfortable and proficient with the technique of gonioscopy will the practitioner achieve full benefit of its ability to contribute to the care of glaucoma. Examination of the nerve is helpful in making the initial diagnosis, in setting a goal for treatment, and in monitoring the success of therapy. Clinically visible damage to the nerve head may take the form of relatively discrete focal damage or a more generalized, diffuse loss of axons. The major vessels of the retina travel within the optic nerve into the eye, whereas within the eye they travel on or near the surface of the nerve head and nerve fiber layer. Because the nerves are packed together at the nerve before spreading out over the retina, the neural rim is usually elevated somewhat above the level of the retina, and gentle curves in the vessel paths, as they cross the neural rim, reflect this. The normal optic disk is slightly oval, with the greatest dimension in the vertical. The size of the cup rather directly reflects the ratio between the size of the disk and the number of nerve fibers. In normals, the number of nerve fibers is not highly variable, whereas disk area may vary four to five times. Therefore, most of the variability in size of the normal cup reflects the size of the optic disk; larger disks have large cups, small disks, small cups. Generalized diffuse loss of axons produces a uniform enlargement of the cup; focal loss of axons produces localized enlargement of the cup. The whole proposition may also be stated in terms of the neural rim, which is perhaps more meaningful because it is the neural rim that contains the functional tissue. From that perspective, generalized loss produces a rather uniform narrowing of the neural rim, whereas focal loss produces focal narrowing of the rim. A large circular cup may be a sign of glaucoma (populations of glaucoma patients generally have larger optic nerve cups and smaller neural rim areas than do normal controls), but it may also be a normal variant. However, on a single look, cup size by itself is not highly specific for glaucoma. A single look at circular cups can be more specific if there is inequality between the two eyes of a patient. The problem of identifying pathologic damage in a circular cup is far simpler if a change occurs over time. Although a slow, age-related loss of axons probably occurs normally, such progression is not detectable by usual clinical means. Therefore, clinical detection of any change is highly suggestive of an uncontrolled pathologic process. The two most likely foci for early selective damage are the superior and inferior poles of the nerve, with the inferior pole at somewhat greater risk than the superior. Early loss of neural tissue at the poles leads to a shape change in the optic cup from circular to oval resulting from vertical elongation of the cup. Selective loss at one or both poles may lead to a focal narrowing of the neural rim, sometimes referred to as a polar notch. As cupping progresses, the vertical cup elongation seen with moderate degrees of damage may begin to revert to a circular shape as the horizontal dimension of the cup expands because of increasing loss of temporal and then nasal axons. Usually, a small group of nasal axons survives in the late stages of damage, subserving a small island of vision in the temporal field.
Trusted sulfasalazine 500mg
Effectiveness and complications of longterm therapy [German with English abstract] pain treatment spa cheap 500 mg sulfasalazine amex. Clinicopathologic reports, case reports, and small case series: Intravitreal antivirals in the management of patients with aquired immunodeficiency syndrome with progressive outer retinal necrosis. Kohno T, Uchida H, Inomata H: Ocular manifestations of adult T-cell leukemia/ lymphoma. Matsuo T, Nakayama T, Koyama T, et al: Cytological and immunological study of the aqueous humor in acute retinal necrosis syndrome. Matsuo T, Nakayama T, Koyama T, et al: Mild type acute retinal necrosis syndrome involving both eyes at three-year interval. Immunen I, Laatikainen L, Linnanvuori K: Acute retinal necrosis syndrome treated with vitrectomy and intravenous acyclovir. Kumano Y, Manabe J, Hamamoto M, et al: Detection of varicella-zoster virus genome having a Pst1 site in the ocular sample from a patient with acute retinal necrosis. Sado K, Kimura T, Hotta Y, et al: Acute retinal necrosis syndrome associated with herpes simplex keratitis. Perry C, Wagstaff A: Famciclovir: a review of its pharmacologic properties and therapeutic efficacy in herpesvirus infections. Perry C, Faulds D: Valaciclovir: a review of its antiviral activity pharmacokinetic properties, and therapeutic efficacy in herpesvirus infections. Tamesis Syphilis is a sexually transmitted, chronic, systemic infection caused by the spirochete Treponema pallidum. Primary infection is followed by an incubation period of ~3 weeks, usually succeeded by the appearance of a primary skin or mucous membrane lesion, the chancre. Symptoms of this stage (fever, malaise, headache, generalized lymph node enlargement, and rash) generally appear within a few weeks or, at most, a few months after the primary chancre has disappeared. Individuals with historic or serologic evidence of syphilis but with no clinical manifestations by definition have latent syphilis. Approximately one-third of untreated cases will progress to tertiary syphilis, with syphilitic inflammatory lesions of the heart, aorta, brain, kidney, bone, eye, or skin. The primary mode of transmission is through sexual intercourse, but transmission during oral sexual practices may also occur. Transmission after blood transfusions is, in essence, unheard of in civilized societies today because of the screening of blood and blood products for transfusion. One study based on a placebocontrolled trial of antibiotic efficacy in aborting syphilis in known contacts, however, suggested a 30% incidence of transmission with a single sexual encounter. Infant deaths resulting from syphilis and new admissions of patients with syphilitic psychoses have fallen 99% since 1940 in the United States, and the total number of cases of late and latent syphilis has fallen 98% since 1943. A decrease of 98% in the number of congenital syphilitic cases has occurred since 1941. A smaller rise occurred between 1971 and 1980, which can be accounted for primarily by the increasing incidence of syphilis in the homosexual community. By 1988, there were 40 275 new cases of primary and secondary syphilis reported in the United States. That number had fallen to 16 500 in the 1995 Summary of Notifiable Diseases, and to 7980 in 2004. This organism is a thin, spiral-shaped parasite for whom the only known natural host is Homo sapiens. The origins are unknown, and several hypotheses exist regarding the development of syphilis in humans. Two main theories, one tracing the development from the tropics and the other tracing the development from native Americans, are most commonly espoused. The first clear descriptions of clinical evidence of syphilis were recorded at the end of the fifteenth century, when a pandemic known as the Great Pox, as distinguished from smallpox, swept over Europe and Asia. The disease became known as the French disease among Italians and the Italian disease among the French. It supposedly received its present name from a poem written in 1530 by Fracastoro about an infected shepherd named Sifilis. Note the sector of the retina, beginning at the disk and extending superiorly, with infiltrate retinitis and associated retinal vasculitis. The number of individuals in at-risk groups then gradually increases, eventually providing enough numbers for the next major outbreak. In the decade from 1970 to 1980 in a large referral uveitis practice, Schlaegel and Kao estimated that only 1. If this test had not been used in their investigations, three-fourths of their syphilitic iritis cases would have gone undiagnosed. This point is reemphasized as a result of an experience with 25 of 1020 new uveitis referral cases seen between 1 Jan 1983, and 30 Jan 1989. All had total resolution of their uveitis with systemic intravenous penicillin therapy at doses adequate for neurosyphilis. Although some authors have stated that ocular manifestations of syphilis are more likely to arise in the secondary stage of acquired syphilis, it is emphasized that in almost every instance in a referral practice, the patients have had latent syphilis with no clinical manifestations prompting a suspicion of this disease. In addition, although the older literature divided syphilitic iritis into three types according to iris features, that in only one of the cases showed an iris pathologic condition that prompted a specific suspicion for syphilis. Inflammatory cells may accumulate in the vitreous body to varying degrees (including nearly to the point of vitreal opacification) in syphilitic panuveitis or posterior uveitis. It may be difficult to evaluate the choroid and retina in such instances, but if and when the retina can be seen, sectors or foci of active choroiditis will usually be found. Indeed, a healthy dictum for all ophthalmologists to follow would be that any patient with iritis and papillitis should be considered to have syphilis unless proved otherwise. Multifocal chorioretinal lesions, now healed, with scarring in a patient with previous active syphilis with multifocal choroiditis. Note the swelling of the optic nerve and the hazy view of the nerve secondary to the associated inflammatory cells in the vitreous anterior to the disc. Untreated, this stromal keratitis is frequently accompanied by stromal neovascularization. Syphilitic interstitial keratitis may be diffuse and generalized, or it may be localized. The keratitis may be subtle, and in the photophobic patient with minimal circumlimbal injection, patience and practice are required to discover the subtle, diffuse patina of tiny, tan inflammatory cells in the affected area of the corneal stroma. An associated iritis with or without keratic precipitates may develop, and peripheral corneal neovascularization may ensue. Untreated, the keratitis may progress to involve the entire cornea, with progressive neovascularization of the stroma, enormous photophobia, and discomfort and decreased visual acuity for the patient. In congenital syphilitic keratitis, both eyes are affected, either simultaneously or sequentially, in more than 75% of patients. Sector interstitial keratitis and luetic, old, inactive sector interstitial keratitis with stromal scarring in the inferonasal quadrant in a patient with previously treated syphilis. Luetic sector interstitial keratitis with ghost vessels in the deep corneal stroma (extremely difficult to capture on film and reproduce). Direct techniques include the darkfield examination, in which exudate from a suspected syphilitic lesion is examined by microscopy with a darkfield technique. The antibody will stick to syphilitic organisms in the exudate or specimen and will be seen by the characteristic apple-green fluorescence when the specimen is examined under the fluorescence microscope. Indirect techniques depend on serologic studies, including Treponema-specific and nontreponemal tests. This test is typically positive in patients with active syphilis and negative in patients with successfully treated syphilis. This test will remain positive for life, regardless of whether the patient has been treated. Spirochetes (arrow) in the cornea, as demonstrated by silver stain, after penetrating keratoplasty in a patient with secondary syphilis and active interstitial keratitis. An acute febrile reaction frequently accompanied by headache, myalgia and other flu-like symptoms occurs within the first 24 h after any therapy for syphilis and may induce early labor or cause fetal distress in pregnant women. Clinical suspicion and penicillin therapeutic trials have been enlightening in these instances. It is as yet unclear whether this therapeutic approach is sufficient therapy in most patients with neurosyphilis, and little to no experience exists with these treatment regimens in patients with ocular syphilis.
Sulfasalazine 500mg cheap
Heterochromia of the affected eye is not a constant feature and is not required for diagnosis pain treatment center lexington safe sulfasalazine 500 mg. Infection secondary to toxoplasmosis, rubella or herpes simplex virus have been implicated as possible triggers. Although typically presenting as a unilateral condition, up to 13% of patients have bilateral disease. The incidence varies from 6% to 59% with the higher incidence seen with longer follow-up. Typically patients seek medical attention only when vision becomes blurred by cataract formation. Granulomas consist of small islands of macrophages, epithelioid cells, giant cells, and a surrounding rim of lymphocytes. The diagnosis is based on the sequelae of granulomatous inflammation in more than one organ with compatible radiologic and immunologic findings and by carefully excluding other granulomatous diseases or known causes of local granulomatous reactions. Glaucoma Approximately 11% of patients with sarcoidosis developed glaucoma as a complication of anterior uveitis. Usually, the glaucoma is secondary to obstruction of trabecular meshwork by inflammatory debris, precipitates or nodules. Other uveitic complications include cataract, cystoid macular edema,126 choroiditis,127 corneal band keratopathy and visual loss. Glaucoma associated with sarcoid uveitis is managed using the same principles as previously described. Signs and Symptoms Ocular findings include anterior uveitis (most common, 35% of cases), posterior uveitis (25% of cases)119 (includes chorioretinitis, retinal periphlebitis, and optic disk inflammation), occasionally involvement of lacrimal glands and rarely eyelid swelling. The course of ocular involvement does not necessarily parallel the systemic disease. Small grayish white balls of inflammatory cells (snowballs) in vitreous with string of pearl-type vitreous opacities can be seen in intermediate uveitis. Funduscopic examination can reveal characteristics of posterior uveitis mentioned above. Symptoms usually last from hours to a few weeks with recurrence occurring at monthly or yearly intervals. Patients can experience several self-limited attacks and then subside or relapse into chronic form of glaucoma. Chandler and Grant were the first to describe an uncommon cause of open-angle glaucoma secondary to idiopathic inflammatory precipitates on the trabecular meshwork. Some patients will eventually develop other inflammatory disorders such as sarcoidosis, ankylosing spondylitis, rheumatic arthritis, episcleritis, glaucomatocyclitic crisis, or chronic uveitis. The affected eyes appear white and quiet with minimal inflammatory precipitates on the cornea. However, continued prophylactic use of topical antiglaucoma medications may be used if the frequency of episodes is believed to be frequent and asymptomatic, or if optic nerve and/or visual field changes are present from multiple attacks. Apraclonidine has been shown to be effective during acute attacks146; thus more selective alpha-2 agonists are likely both effective and safe. Oral indomethacin may be effective because prostaglandins have been implicated in the disease. It is assumed that the glaucoma is secondary to underlying inflammation of the trabecular meshwork. The glaucoma is typically unresponsive to classic antiglaucoma therapy but shows an excellent response to topical corticosteroid therapy which is given hourly initially and gradually tapered down. Examples include sarcoidosis and glaucomatocyclitic crisis in which the signs and symptoms have been discussed elsewhere. Large trabecular precipitates have also been noted in patients within one month after argon laser trabeculoplasty. Therefore, routine gonioscopy should be considered for all patients after laser treatment. The onset of the disease typically occurs before 16 years of age and lasts more than 6 months. It is postulated to be a chronic inflammation caused by the release of cytokines from macrophages and T-cell invasion which evoke synoviocyte proliferation. It is a diagnosis of exclusion and is clinically categorized into three sub-types. Occasionally, red eye, decreased vision, unequal pupils, ocular pain and headaches may be present in older children. The period of highest risk for the development of uveitis is within 4 years of onset of the arthritis with the average latency period of 18 months from the diagnosis of the arthritis. Late sequelae of rheumatoid uveitis are band keratopathy, cataract formation, glaucoma,158,162 macular edema and rarely chorioretinitis. The mean interval between the onset of uveitis and the diagnosis of glaucoma is ~9 years. Inflammatory infiltrate, mainly by plasma cells, can result in trabeculitis and steroids therapy may lead to steroidinduced open-angle glaucoma. Management Topical steroids with topical mydriatic/cycloplegic drops are the mainstay of treatment. There is currently no useful virus culture available for the diagnosis of viral anterior segment disease. The uveitis is usually unilateral and can cause sectoral atrophy of the iris without previously associated with keratitis. Infection of the cornea includes superficial epithelial keratitis in which slit-lamp examination reveals typical corneal vesicles, dendritic ulcers, and geographic ulcers. Stromal or disciform keratitis is characterized by stromal infiltrate, ulceration, and necrosis. A variety of topical antiviral agents such as idoxuridine, vidarabine, and trifluridine are currently available to treat herpes simplex. Filtration surgery could be indicated in a refractory case; laser trabeculoplasty should be avoided. The patient had undergone iridectomies for angle-closure glaucoma before the development of herpes zoster. Herpes zoster ophthalmicus typically involves the infection of the trigeminal nerve and is caused by reactivation of latent varicella virus. Approximately 11% of the patients with systemic herpes zoster developed herpes zoster ophthalmicus. Mucopurulent conjunctivitis and episcleritis (sectoral or diffuse) can also be observed. Corneal sensation is decreased or irreversibly lost if stromal keratitis is involved and may lead to neurotrophic ulcers. Signs and Symptoms With anterior uveitis, the involved eye may presents with blurred vision, photophobia, ciliary injection, iris edema, and miosis. Antiviral therapy may include systemic acyclovir to reduce viral replication and prevent uveitis in early course of the disease. Generally these antiviral medications are effective if administration begins within 72 h of the appearance of the skin lesions. The treatment of the secondary glaucoma is the same as discussed above with medical therapy followed by surgery if indicated. The disease is caused by the transmission of Traponema pallidum from mother to fetus in utero. The cornea is edematous, opaque and vascularized in its deep layers which gives the pinkish color of the cornea and is termed the salmon patch of Hutchinson.
Purchase 500mg sulfasalazine
Systemic Findings No systemic orofacial chest pain treatment guidelines buy generic sulfasalazine 500mg on line, skeletal, or auditory abnormalities have been documented. Ocular Findings Clinical findings are numerous and include refractive errors, usually myopia that progresses slightly with age but also some hyperopia and astigmatism. Extensive fibrillar degeneration of the vitreous with or without vitreous bands and strands over the retinal periphery are nearly universal. Sheathing of the retinal vessels is common, and the vessels often become attenuated in the periphery. Peripheral retinal abnormalities include minute, shiny crystalline-like deposits resembling snowflakes. White with pressure is a common Ancillary Testing Visual-field defects correspond to the peripheral retinal pigment epithelial atrophy and include arcuate scotomas and ring scotomas that may lead to central fixation loss. Electroretinography demonstrates diffuse photoreceptor dysfunction with preservation but severe reduction of both rod and cone responses. Some patients are asymptomatic until age 40 years when nuclear cataracts become Heredofamilial Vitreoretinopathies finding in the peripheral retina. Peripheral radial perivascular degeneration may also be observed in a minority of patients. Typical circumferential lattice peripheral retinal degeneration has not been reported. Ancillary Testing Elevated dark adaptation and reduced scotopic b-wave amplitude with dim white light are seen in most snowflake subjects. Many patients become symptomatic in mid-life when nuclear cataracts become visually significant. Retinal detachment may cause vision loss, necessitating vitreoretinal surgical techniques. Management Genetic counseling may be important for snowflake patients and families. The genetic and clinical evidence thus suggests that snowflake vitreoretinal degeneration is a entity distinct from other heredofamilial vitreoretinal dystrophies. First described in 1898, juvenile hereditary retinoschisis has been shown to be transmitted in an x-linked fashion with 100% penetrance80,81 but variable expressivity. Despite its X-linked transmission pattern, juvenile hereditary retinoschisis has been observed in females with consanguineous parents. Ocular Findings the primary clinical feature of juvenile hereditary retinoschisis is foveal retinoschisis. The macular pigmentation may become mottled and, in later stages, may resemble atrophic age-related macular degeneration. Peripheral retinoschisis is variably elevated and usually does not extend posteriorly past the arcades. Avascular or vascular vitreous veils may occur, probably representing various combinations of retinoschisis and large inner layer holes. This cell type spans much of the retinal thickness, and loss of its integrity has been postulated to explain the characteristic structural defects and functional deficits. Ancillary Testing Color vision testing often yields a mild red-green dyschromatopsia. These electroretinographic findings are characteristic and may conclusively establish the diagnosis, even in young children. Later in the disease after secondary photoreceptor dysfunction, both a-waves and b-waves may be subnormal. The electrooculogram is fairly normal until disease is very advanced, when it becomes subnormal. Fluorescein angiography demonstrates typical findings that may be very useful in establishing a diagnosis. No staining or leakage of fluorescein dye occurs, differentiating juvenile hereditary retinoschisis from causes of cystoid macular edema. Histopathologic studies have demonstrated splitting of the retina in the superficial retina, the inner limiting membrane, and nerve fiber layer. Vision may remain stable during young adulthood but usually worsens slowly with advancing age. Retinal detachment and vitreous hemorrhage represent two of the most serious complications of juvenile hereditary retinoschisis. Juvenile hereditary retinoschisis is high in the differential diagnosis of vitreous hemorrhage in male children. Retinal detachment may occur when holes develop in both the outer and the inner retinal layers. A diagnosis may be established by utilizing diagnostic photocoagulation through the elevated retina; the presence of an attached outer retinal layer will give rise to a white chorioretinal burn. Laser photocoagulation and other attempts to flatten retinoschisis cavities have failed to demonstrate any benefit and have led to retinal detachments. Occasionally, posterior retinal breaks or vitreous hemorrhage necessitates the use of vitrectomy techniques to achieve internal tamponade and retinal reattachment. Molecular Genetics of Juvenile Hereditary Retinoschisis Linkage analysis results reveal that the gene for juvenile hereditary retinoschisis localizes to the short arm of the X chromosome in the region Xp22. Since carriers of juvenile hereditary retinoschisis are asymptomatic, carrier detection is of considerable value. Availability of highly polymorphic genetic markers now permits detection of the carrier state with a theoretical reliability of at least 94. Note the disproportionate loss in the amplitude of the b-wave as compared with the a-wave in the tracing taken with a high luminance white light flash stimulus. Wide-angle fundus photograph shows peripheral retinal degenerative changes including chorioretinal atrophy, pigment clumping, and retinoschisis (arrows). The peripheral retinoschisis may extend posteriorly, at times connecting to macular lesions. Macular retinoschisis has a cystoid appearance and may resemble that associated with juvenile hereditary retinoschisis. A fibrillar appearance of the condensed vitreous posterior to the lens has been noted. Clinical Course Individuals are often identified in the first decade of life when they are noted to have poor central vision and nyctalopia. Surgical intervention has been associated with poor outcomes, although the use of vitreous microsurgical techniques has improved surgical outcomes. Ancillary Testing Electrophysiologic testing is of particular benefit in diagnosis of this condition owing to unique characteristics among vitreoretinal dystrophies. The electroretinogram demonstrates markedly reduced or completely absent a-wave and b-wave amplitudes. If present, photopic and scotopic responses are similar, indicating an apparent absence of detectable rod activity. Ancillary Testing In enhanced S-cone syndrome, unique electroretinographic findings are present and are mediated mainly by S (blue) cones. Also, the electroretinogram obtained under conditions of bright white light stimulation is similar to that obtained with dark adaptation even though the 30-Hz flicker response is markedly diminished. Molecular analysis of patients with these conditions will likely elucidate answers to these questions. Systemic Findings No systemic associations, including skeletal, facial, or joint abnormalities, have been reported. Ancillary Testing the electroretinogram shows normal to slightly reduced rod and cone function. Fluorescein angiography may show widespread, severe leakage in the posterior pole, sometimes with cystoid macular edema. Peripherally, there is blockage of choroidal fluorescence by deposited pigment on a background of window defect.
Cheap sulfasalazine 500mg amex
Inflammation in the form of flare and cells in the anterior chamber may be present pain treatment lexington ky buy generic sulfasalazine canada. The presumed mechanism of this pressure rise is acute inflammation of the trabecular meshwork with a corresponding reduction in the facility of outflow. This pressure rise is typically self-limited, and improvement may be hastened by a short course of topical antiinflammatory agents. It has been hypothesized by some that angle recession is only a marker for significant injury and that the late development of glaucoma may correlate better with the amount of trabecular disruption observed acutely. Cho et al compared the clinical characteristics of 18 patients with very poor visual outcome after nonperforating hyphema to 166 patients with better visual outcome after nonperforating hyphema. The presence of posterior segment injuries, anterior segment injuries, poor initial visual acuity, glaucoma, vitreous hemorrhage and eyelid laceration were all associated with long term poor visual outcome. They include contusion of the outflow apparatus, physical disruption of the meshwork, and plugging of the meshwork with red blood cells. Acute pressure elevation may pose a threat to vision as a result of optic nerve damage or corneal staining. In a prospective study of 137 patients with traumatic hyphema, Read and Goldberg5 found that optic atrophy tended to occur with pressures at or greater than 35 mmHg and durations varying from 5 to 14 days. Patients with either sickle-cell disease or trait are susceptible to these complications. Carbonic anhydrase inhibitors may increase sickling as a result of systemic acidosis. Since methazolamide theoretically causes less systemic acidosis than does acetazolamide, methazolamide may be a safer choice in this clinical situation. Carbonic anhydrase inhibitors or osmotic agents may increase hemoconcentration and viscosity in an already compromised ocular microvasculature. Acetazolamide can increase ascorbate in the aqueous, and this may worsen the sickling process. Epinephrine agents may further compromise blood flow as a result of vasoconstriction. The successful use of intracameral tissue plasminogen activator in a sickle cell patient with traumatic hyphema and acute glaucoma has been reported. Rebleeding into the anterior chamber after an initial hyphema can be a potentially devastating complication. Aminocaproic acid has been shown to decrease the rate of rebleeding in some patients. The treatment of acute pressure elevation as a result of hyphema entails the use of conventional pharmacologic agents to control pressure elevation, with the exception of miotic agents. Cycloplegic agents and topical steroids are often used as well for the associated traumatic iritis. Many surgical procedures have been reported, including anterior chamber washout,15 clot expression,16 delivery of the clot with a cryoprobe,17 automated hyphemectomy,18 and ultrasonic emulsification and aspiration. This glaucoma may result from any of several mechanisms that are dealt with later in this chapter. Initial treatment consists of a topical b-blocker as well as oral carbonic anhydrase inhibitors and a systemic hyperosmotic agent, if needed. Miotics should be avoided because they may cause further shallowing of the anterior chamber. High-dose oral steroids are recommended by some individuals who believe that steroids will stabilize the choroidal vessels. This is in contrast to acids, which more often produce an injury that is self-limited as a result of tissue coagulation. Glaucoma is more often associated with alkali burns, and thus this section is restricted to alkali burns. It was not until the 1960s that pressure elevation was documented acutely following an alkali burn. The nature of the acute pressure rise was studied in rabbits by Chiang and associates,27 who demonstrated a dicrotic pressure rise after the application of sodium hydroxide. There was an immediate pressure rise of 40 mmHg, followed by a gradual decline in pressure to 20 mmHg above normal in 10 min. A second, gradual pressure rise then occurred, reaching 40 mmHg above normal at 1 h. Paterson and Pfister28 set out to determine the exact mechanisms of these pressure rises in rabbits. They believed that shrinkage of the outer coats of the eye was the major cause of the initial pressure spike. Lid contraction and extraocular muscle spasm were not significant factors in raising the pressure. Prostaglandin release with inflammation was implicated as the major factor in the second hypertensive phase. In addition to the conventional therapies directed at the anterior segment consequences of an alkali burn, treatment of any pressure elevation is important. This includes topical b-blocker therapy, oral carbonic anhydrase inhibitors, and systemic hyperosmotic agents as needed. Topical epinephrine has been effective in blunting the second hypertensive phase in experimental animal models. This is generally considered to be a result of ongoing inflammation with secondary peripheral anterior synechiae. The treatment of this late-onset glaucoma would include conventional medical and surgical therapies addressed at this underlying mechanism of chronic angle closure. Drainage of blood from the suprachoroidal space may be warranted in certain situations. Generally, it is advisable to wait for several days if possible before draining the blood because this allows time for the blood to be fully sequestered in the suprachoroidal space. Chronic synechial closure of the angle may be a long-term sequela of massive suprachoroidal hemorrhage. This may require later intervention in the form of medical therapy, laser iridoplasty (gonioplasty), surgical goniosynechialysis, conventional filtration surgery, or a cycloablative procedure, depending on the individual circumstances. In 1962, Wolff and Zimmerman31 tied together the pathologic entity of angle recession and the clinical phenomenon of unilateral chronic glaucoma following trauma. Blanton32 observed a bimodal pattern, with glaucoma occurring either within the first year or after 10 years. The inner circular muscle of the ciliary muscle may be atrophied, giving the ciliary body band a broad and more fusiform appearance. The clinical presentation of glaucoma secondary to angle recession is variable and depends somewhat on the time of presentation relative to the initial injury. More often, angle-recession glaucoma presents years after the initial event as a chronic unilateral glaucoma. In a pathologic review of 100 eyes enucleated for unilateral glaucoma, Miles and Boniuk39 found 11 eyes with angle deformity as the principal cause for the glaucoma. Eight of these 11 patients gave a history of previous trauma to the eye ranging from 6 months to 24 years before the onset of glaucoma. In a population-based survey Salmon et al performed gonioscopy on 987 inhabitants of a small South African village. They found a cumulative lifetime prevalence of angle recession in the community of 14. Examination can often reveal asymmetry of anterior chamber depth between the two eyes, with the involved eye having a greater chamber depth. There are often associated findings of ocular trauma, such as tears in the iris sphincter or root.