0.2mg tamsulosin
This drug has a low immunogenic potential man health xchange tamsulosin 0.2mg for sale, and it shows little cross-reactivity with antibodies induced by other -lactams. Gram (+) bacilli Listeria monocytogenes Gram () cocci Neisseria gonorrhoeae** Neisseria meningitidis **including penicillinaseproducing strains Gram () rods Acinetobacter species Citrobacter species Enterobacter species Escherichia coli Gardnerella vaginalis Haemophilus influenzae Klebsiella species Proteus species Providencia species Pseudomonas aeruginosa Salmonella species Serratia species Anaerobic organisms Clostridium species Peptococcus species Peptostreptococcus species Propionibacterium species Bacteroides species Fusobacterium species V. Instead, they bind to and inactivate -lactamases, thereby protecting the antibiotics that are normally substrates for these enzymes. With the emergence of resistant strains, it is important to curtail the increase in vancomycin-resistant bacteria (for example, Enterococcus faecium and Enterococcus faecalis) by restricting the use of vancomycin to the treatment of serious infections caused by -lactam resistant, gram-positive microorganisms or gram-positive infections in patients who have a serious allergy to the -lactams. Serum drug concentrations (troughs) are commonly measured to monitor and adjust dosages for safety and efficacy. Vancomycin is not absorbed after oral administration, so the use of the oral formulation is limited to the treatment of severe antibioticassociated C. Daptomycin is indicated for the treatment of complicated skin and skin structure infections and bacteremia caused by S. Moreover, telavancin exhibits an additional mechanism of action similar to that of daptomycin, which involves disruption of the bacterial cell membrane due to the presence of a lipophilic side chain moiety. It is an alternative to vancomycin, daptomycin, and linezolid, in treating complicated skin and skin structure infections caused by Spirochetes Mycoplasma Chlamydia **Oral vancomycin only for C. It is also an agent of last choice for hospital-acquired and ventilator-associated bacterial pneumonia when alternative treatments are not suitable. Due to its unique structure and mechanism of action, cross resistance with other antimicrobial agents is unlikely. Fosfomycin is rapidly absorbed after oral administration and distributes well to the kidneys, bladder, and prostate. It maintains high concentrations in the urine over several days, allowing for a one-time dose for the treatment of urinary tract infections. They have a detergent-like effect that disrupts cell membrane integrity, leading to leakage of cellular components and ultimately cell death. Polymyxins are concentration-dependent bactericidal agents with activity against most clinically important gram-negative bacteria, including P. However, alterations in the cell membrane lipid polysaccharides allow many species of Proteus and Serratia to be intrinsically resistant. Only two forms of polymyxin are in clinical use today, polymyxin B and colistin (polymyxin E). The use of these drugs has been limited for a long time, due to the increased risk of nephrotoxicity and neurotoxicity (for example, slurred speech, muscle weakness) when used systemically. However, with the increase in gram-negative resistance, they have seen a resurgence in use and are now commonly used as salvage therapy for patients with multidrug-resistant infections. Careful dosing and monitoring of adverse effects are important to maximize the safety and efficacy of these agents. Which of the following would be the most appropriate treatment option for oncedaily outpatient intravenous therapy? Myalgias and rhabdomyolysis have been reported with daptomycin therapy and require patient education and monitoring. Which of the following regimens is most appropriate for empiric coverage of methicillinresistant Staphylococcus aureus and Pseudomonas aeruginosa in this patient? He is taken to the operating room for surgery, and postsurgical cultures reveal Escherichia coli and Bacteroides fragilis, susceptibilities pending. Based on the severity of the allergic reaction, aztreonam is the choice of all the -lactams. Although cross-reactivity with cephalosporins and carbapenems is low, the risk rarely outweighs the benefit in these cases. No antibiotic resistance has been reported, and it remains the drug of choice unless the patient has a severe allergic reaction. Which of the following agents is the best choice for the treatment of meningitis in this patient? A 76-year-old male with hospital-acquired pneumonia also receiving amiodarone for atrial fibrillation. Based on symptoms and a urinalysis, she is diagnosed with a urinary tract infection. Which of the following is an appropriate oral option to treat the urinary tract infection in this patient? Option D is not an appropriate choice because the patient has baseline renal dysfunction and telavancin should be avoided unless benefit outweighs the risk. Option C is the best choice in this case since it is approved for skin and skin structure infections, and the patient has no apparent contraindication. Option A and C are incorrect because enterococci are inherently resistant to all cephalosporins. Bacterial ribosomes differ structurally from mammalian cytoplasmic ribosomes and are composed of 30S and 50S subunits (mammalian ribosomes have 40S and 60S subunits). In general, selectivity for bacterial ribosomes minimizes potential adverse consequences encountered with the disruption of protein synthesis in mammalian host cells. However, high concentrations of drugs such as chloramphenicol or the tetracyclines may cause toxic effects as a result of interaction with mitochondrial mammalian ribosomes, since the structure of mitochondrial ribosomes more closely resembles bacterial ribosomes. Substitutions on these rings alter the individual pharmacokinetics and spectrum of antimicrobial activity. Mechanism of action Tetracyclines enter susceptible organisms via passive diffusion and also by an energy-dependent transport protein mechanism unique to the bacterial inner cytoplasmic membrane. They are commonly used in the treatment of acne and Chlamydia infections (doxycycline). Resistance the most commonly encountered naturally occurring resistance to tetracyclines is an efflux pump that expels drug out of the cell, thus preventing intracellular accumulation. The organism multiplies in the gastrointestinal tract, where it secretes an enterotoxin that produces diarrhea. Treatment includes doxycycline, which reduces the number of intestinal vibrios, and uid replacement. Infection results in skin lesions, headache, and fever, followed by meningoencephalitis and, eventually, arthritis. It causes nongonococcal urethritis, pelvic in ammatory disease, and lymphogranuloma venereum. Response to tetracyclines is prompt if the drug is started early in the disease process. Resistance to one tetracycline does not confer universal resistance to all tetracyclines. Distribution: the tetracyclines concentrate well in the bile, liver, kidney, gingival fluid, and skin. Moreover, they bind to tissues undergoing calcification (for example, teeth and bones) or to tumors that have a high calcium content. Minocycline also achieves high levels in saliva and tears, rendering it useful in eradicating the meningococcal carrier state. Protein Synthesis Inhibitors cross the placental barrier and concentrate in fetal bones and dentition. Tetracycline is primarily eliminated unchanged in the urine, whereas minocycline undergoes hepatic metabolism and is eliminated to a lesser extent via the kidney. In renally compromised patients, doxycycline is preferred, as it is primarily eliminated via the bile into the feces. Effects on calcified tissues: Deposition in the bone and primary dentition occurs during the calcification process in growing children. This may cause discoloration and hypoplasia of teeth and a temporary stunting of growth. Hepatotoxicity: Rarely hepatotoxicity may occur with high doses, particularly in pregnant women and those with preexisting hepatic dysfunction or renal impairment. Phototoxicity: Severe sunburn may occur in patients receiving a tetracycline who are exposed to sun or ultraviolet rays. Vestibular dysfunction: Dizziness, vertigo, and tinnitus may occur particularly with minocycline, which concentrates in the endolymph of the ear and affects function. Pseudotumor cerebri: Benign, intracranial hypertension characterized by headache and blurred vision may occur rarely in adults. Although discontinuation of the drug reverses this condition, it is not clear whether permanent sequelae may occur. Contraindications: the tetracyclines should not be used in pregnant or breast-feeding women or in children less than 8 years of age. It is indicated for the treatment of complicated skin and soft tissue infections, as well as complicated intra-abdominal infections.
Cheap generic tamsulosin uk
Induction is the time from administration of a potent anesthetic to development of effective anesthesia mens health 012013 chomikuj purchase generic tamsulosin line. Recovery is the time from discontinuation of anesthetic until consciousness and protective reflexes return. Recovery is essentially the reverse of induction and depends on how fast the anesthetic diffuses from the brain. Maintenance of anesthesia After administering the anesthetic, vital signs and response to stimuli are monitored continuously to balance the amount of drug inhaled and/or infused with the depth of anesthesia. Maintenance is commonly provided with volatile anesthetics, which offer good control over the depth of anesthesia. Opioids such as fentanyl are used for analgesia along with inhalation agents, because the latter are not good analgesics. Recovery Postoperatively, the anesthetic admixture is withdrawn, and the patient is monitored for return of consciousness. Redistribution from the site of action (rather than metabolism of the drug) underlies recovery. If neuromuscular blockers have not been fully metabolized, reversal agents may be used. The patient is monitored to assure full recovery, with normal physiologic functions (spontaneous respiration, acceptable blood pressure and heart rate, intact reflexes, and no delayed reactions such as respiratory depression). Stage I-Analgesia: Loss of pain sensation results from interference with sensory transmission in the spinothalamic tract. A rise and irregularity in blood pressure and respiration occur, as well as a risk of laryngospasm. Regular respiration and relaxation of skeletal muscles with eventual loss of spontaneous movement occur. To minimize waste, potent inhaled agents are delivered in a recirculation system containing absorbents that remove carbon dioxide and allow rebreathing of the agent. Common features of inhalation anesthetics Modern inhalation anesthetics are nonflammable, nonexplosive agents, including nitrous oxide and volatile, halogenated hydrocarbons. They cause bronchodilation but also decrease both spontaneous ventilation and hypoxic pulmonary vasoconstriction (increased pulmonary vascular resistance in poorly aerated regions of the lungs, redirecting blood flow to more oxygenated regions). Movement of these agents from the lungs to various body compartments depends upon their solubility in blood and tissues, as well as on blood flow. The more lipid soluble an anesthetic, the lower the concentration needed to produce anesthesia and, thus, the higher the potency. Uptake and distribution of inhalation anesthetics the principal objective of inhalation anesthesia is a constant and optimal brain partial pressure (Pbr) of inhaled anesthetic (partial pressure equilibrium between alveoli [Palv] and brain [Pbr]). The partial pressure of an anesthetic gas at the origin of the respiratory pathway is the driving force moving the anesthetic into the alveolar space and, thence, into the blood (Pa), which delivers the drug to the brain and other body compartments. Because gases move from one body compartment to another according to partial pressure gradients, steady state is achieved when the partial pressure in each of these 175 Halothane Iso urane Sevo urane Des urane Nitrous oxide 0 0. Alveolar wash-in: this refers to replacement of normal lung gases with the inspired anesthetic mixture. The time required for this process is directly proportional to the functional residual capacity of the lung (volume of gas remaining in the lungs at the end of a normal expiration) and inversely proportional to ventilatory rate. As the partial pressure builds within the lung, anesthetic transfer from the lung begins. For inhaled anesthetics, think of the blood as a pharmacologically inactive reservoir. Drugs with low versus high solubility in blood differ in their speed of induction of anesthesia. When an anesthetic gas with low blood solubility such as nitrous oxide diffuses from the alveoli into the circulation, little anesthetic dissolves in the blood. Therefore, equilibrium between inhaled anesthetic and arterial blood occurs rapidly, and relatively few additional molecules of anesthetic are required to raise arterial anesthetic partial pressure. In contrast, anesthetic gases with high blood solubility, such as halothane, dissolve more completely in the blood, and greater amounts of anesthetic and longer periods of time are required to raise blood partial pressure. This results in increased times of induction and recovery and slower changes in depth of anesthesia in response to changes in the concentration. The solubility in blood is ranked as follows: halothane > isoflurane > sevoflurane > nitrous oxide > desflurane. It therefore takes longer for the gas to reach equilibrium between the alveoli and the site of action in the brain. Again, for inhaled anesthetics, think of the blood as a pharmacologically inactive reservoir. Alveolar-to-venous partial pressure gradient of anesthetic: this is the driving force of anesthetic delivery. For all practical purposes, pulmonary end-capillary anesthetic partial pressure may be considered equal to alveolar anesthetic partial pressure if the patient does not have severe lung diffusion disease. The arterial circulation distributes the anesthetic to various tissues, and the pressure gradient drives free anesthetic gas into tissues. As venous circulation returns blood depleted of anesthetic to the lung, more gas moves into the blood from the lung according to the partial pressure difference. The greater the difference in anesthetic concentration between alveolar (arterial) and venous blood, the higher the uptake and the slower the induction. Over time, the partial pressure in venous blood closely approximates that in the inspired mixture, and no further net anesthetic uptake from the lung occurs. Effect of different tissue types on anesthetic uptake: the time required for a particular tissue to achieve steady state with the partial pressure of an anesthetic gas in the inspired mixture is inversely proportional to the blood flow to that tissue (greater flow results in a more rapidly achieved steady state). It is also directly proportional to the capacity of that tissue to store anesthetic (a larger capacity results in a longer time required to achieve steady state). Brain, heart, liver, kidney, and endocrine glands: these highly perfused tissues rapidly attain steady state with the partial pressure of anesthetic in the blood. Skeletal muscles: these are poorly perfused during anesthesia and have a large volume, which prolongs the time required to achieve steady state. However, potent volatile anesthetics are very lipid soluble, so fat has a large capacity to store them. Slow delivery to a high-capacity compartment prolongs the time required to achieve steady state in fat tissue. Bone, ligaments, and cartilage: these are poorly perfused and have a relatively low capacity to store anesthetic. Therefore, these tissues have minimal impact on the time course of anesthetic distribution in the body. Washout: When an inhalation anesthetic is discontinued, the body becomes the "source" that drives the anesthetic back into the alveolar space. The same factors that influence attainment of steady state with an inspired anesthetic determine the time course of its clearance from the body. Mechanism of action No specific receptor has been identified as the locus of general anesthetic action. The fact that chemically unrelated compounds produce anesthesia argues against the existence of a single receptor. Anesthetics It appears that a variety of molecular mechanisms may contribute to the activity of general anesthetics. For example, the activity of the inhibitory glycine receptors in the spinal motor neurons is increased. In addition, inhalation anesthetics block excitatory postsynaptic currents of nicotinic receptors. The mechanism by which anesthetics perform these modulatory roles is not fully understood. Halothane Halothane is the prototype to which newer inhalation anesthetics are compared. Due to adverse effects and the availability of other anesthetics with fewer complications, halothane has been replaced in most countries. Therapeutic uses: Halothane is a potent anesthetic but a relatively weak analgesic. Thus, it is usually coadministered with nitrous oxide, opioids, or local anesthetics.
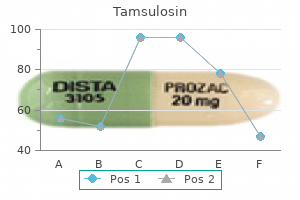
| Comparative prices of Tamsulosin | ||
| # | Retailer | Average price |
| 1 | Wegman's Food Markets | 131 |
| 2 | Verizon Wireless | 141 |
| 3 | Burger King Holdings | 982 |
| 4 | Williams-Sonoma | 623 |
| 5 | Dollar General | 297 |
0.2 mg tamsulosin with visa
Determining antimicrobial susceptibility of infective organisms After a pathogen is cultured prostate cancer 44 order tamsulosin 0.4mg fast delivery, its susceptibility to specific antibiotics serves as a guide in choosing antimicrobial therapy. Some pathogens, such as Streptococcus pyogenes and Neisseria meningitidis, usually have predictable susceptibility patterns to certain antibiotics. In contrast, most gram-negative bacilli, enterococci, and staphylococcal species often show unpredictable susceptibility patterns and require susceptibility testing to determine appropriate antimicrobial therapy. Bacteriostatic versus bactericidal drugs: Antimicrobial drugs are classified as either bacteriostatic or bactericidal. Selection of Antimicrobial Agents (or urine) levels achievable in the patient, thus limiting the spread of infection until the immune system attacks, immobilizes, and eliminates the pathogen. If the drug is removed before the immune system has scavenged the organisms, enough viable organisms may remain to begin a second cycle of infection. Because of their more aggressive antimicrobial action, bactericidal agents are often the drugs of choice in seriously ill and immunocompromised patients. Note that viable organisms remain even in the presence of the bacteriostatic drug. In contrast, addition of a bactericidal agent kills bacteria, and the total number of viable organisms decreases. Although practical, this classification may be too simplistic because it is possible for an antibiotic to be bacteriostatic for one organism and bactericidal for another. For example, linezolid is bacteriostatic against Staphylococcus aureus and enterococci but is bactericidal against most strains of S. This serves as a quantitative measure of in vitro susceptibility and is commonly used in practice to streamline therapy. Effect of the site of infection on therapy: the bloodbrain barrier Adequate levels of an antibiotic must reach the site of infection for the invading microorganisms to be effectively eradicated. Of particular significance are the capillaries in the brain, which help to create and maintain the bloodbrain barrier. Lipid solubility of the drug: the lipid solubility of a drug is a major determinant of its ability to penetrate into the brain. Principles of Antimicrobial Therapy antibiotics, such as penicillin, are ionized at physiologic pH and have low solubility in lipids. They therefore have limited penetration through the intact bloodbrain barrier under normal circumstances. Molecular weight of the drug: A compound with a low molecular weight has an enhanced ability to cross the bloodbrain barrier, whereas compounds with a high molecular weight (for example, vancomycin) penetrate poorly, even in the presence of meningeal inflammation. In women, pregnancy or breast-feeding also affects selection of the antimicrobial agent. Immune system: Elimination of infecting organisms from the body depends on an intact immune system, and the host defense system must ultimately eliminate the invading organisms. Renal dysfunction: Poor kidney function may cause accumulation of certain antibiotics. Serum creatinine levels are frequently used as an index of renal function for adjustment of drug regimens. However, direct monitoring of serum levels of some antibiotics (for example, vancomycin, aminoglycosides) is preferred to identify maximum and/or minimum values to prevent potential toxicities. Thus, elderly patients are particularly vulnerable to accumulation of drugs eliminated by the kidneys. Hepatic dysfunction: Antibiotics that are concentrated or eliminated by the liver (for example, erythromycin and doxycycline) must be used with caution when treating patients with liver dysfunction. Poor perfusion: Decreased circulation to an anatomic area, such as the lower limbs of a diabetic patient, reduces the amount of antibiotic that reaches that area, making these infections difficult to treat. Age: Renal or hepatic elimination processes are often poorly developed in newborns, making neonates particularly vulnerable to the toxic effects of chloramphenicol and sulfonamides. Young children should not be treated with tetracyclines or quinolones, which affect bone growth and joints, respectively. Elderly patients may have decreased renal or liver function, which may alter the pharmacokinetics of certain antibiotics. Pregnancy and lactation: Many antibiotics cross the placental barrier or enter the nursing infant via the breast milk. Although the concentration of an antibiotic in breast milk is usually low, the total dose to the infant may be sufficient to produce detrimental effects. Risk factors for multidrug-resistant organisms: Infections with multidrug-resistant pathogens need broader antibiotic coverage when initiating empiric therapy. Common risk factors for infection with these pathogens include prior antimicrobial therapy in the preceding 90 days, hospitalization for greater than 2 days within the preceding 90 days, current hospitalization exceeding 5 days, high frequency of resistance in the community or local hospital unit (assessed using hospital antibiograms), and immunosuppressive diseases and/or therapies. Safety of the agent Antibiotics such as the penicillins are among the least toxic of all drugs because they interfere with a site or function unique to the growth of microorganisms. Cost of therapy Often several drugs may show similar efficacy in treating an infection but vary widely in cost. Although choice of therapy usually centers on the site of infection, severity of the illness, and ability to take oral medications, it is also important to consider the cost of the medication. In hospitalized patients requiring intravenous therapy initially, the switch to oral agents should occur as soon as possible. Utilizing these properties to optimize antibiotic dosing regimens can improve clinical outcomes and possibly decrease the development of resistance. This effect is sometimes called concentration-independent or time-dependent killing. In this chapter, the list is used to illustrate the spectra of bacteria for which a particular class of antibiotics is therapeutically effective. Narrow-spectrum antibiotics Chemotherapeutic agents acting only on a single or a limited group of microorganisms are said to have a narrow spectrum. Administration of broadspectrum antibiotics can drastically alter the nature of the normal bacterial flora and precipitate a superinfection due to organisms such as Clostridium difficile, the growth of which is normally kept in check by the presence of other colonizing microorganisms. This strategy reduces the possibility of superinfections, decreases the emergence of resistant organisms, and minimizes toxicity. Advantages of drug combinations Certain combinations of antibiotics, such as -lactams and aminoglycosides, show synergism; that is, the combination is more effective than either of the drugs used separately. Because such synergism among antimicrobial agents is rare, multiple drugs used in combination are only indicated in special situations (for example, when an infection is of unknown origin or in the treatment of enterococcal endocarditis). Principles of Antimicrobial Therapy agent that is bactericidal may result in the first drug interfering with the action of the second. For example, bacteriostatic tetracycline drugs may interfere with the bactericidal effects of penicillins and cephalosporins. Another concern is the risk of selection pressure and the development of antibiotic resistance by giving unnecessary combination therapy. Genetic alterations leading to drug resistance Acquired antibiotic resistance requires the temporary or permanent gain or alteration of bacterial genetic information. Drug resistance due to altered targets Drug resistance due to decreased accumulation Permeability Aminoglycosides Chloramphenicol Clindamycin Fluoroquinolones b-Lactams Macrolides Rifampin Sulfonamides Tetracycline Trimethoprim Vancomycin Tetracycline b-Lactams enter gramnegative cells through porin channels. However, resistant organisms may also have altered porin channels through which cephalosporins do not pass. Tetracycline Tetracycline was e ective against gynecologic infection due to Bacteroides, but now these organisms are resistant due to the presence of plasmidmediated protein that promotes e ux of the drug. Neisseria gonorrhoeae is now largely resistant to penicillin because of penicillinase activity. Decreased accumulation: Decreased uptake or increased efflux of an antibiotic can confer resistance because the drug is unable to attain access to the site of its action in sufficient concentrations to injure or kill the organism. Also, the presence of an efflux pump can limit levels of a drug in an organism, as seen with tetracyclines. Enzymatic inactivation: the ability to destroy or inactivate the antimicrobial agent can also confer resistance on microorganisms. Examples of antibiotic-inactivating enzymes include 1) -lactamases ("penicillinases") that hydrolytically inactivate the -lactam ring of penicillins, cephalosporins, and related drugs; 2) acetyltransferases that transfer an acetyl group to the antibiotic, inactivating chloramphenicol or aminoglycosides; and 3) esterases that hydrolyze the lactone ring of macrolides. Because the indiscriminate use of antimicrobial agents can result in bacterial resistance and superinfection, prophylactic use is restricted to clinical situations in which the benefits outweigh the potential risks. The duration of prophylaxis should be closely observed to prevent the unnecessary development of antibiotic resistance. Hypersensitivity Hypersensitivity or immune reactions to antimicrobial drugs or their metabolic products frequently occur. For example, the penicillins, despite their almost absolute selective microbial toxicity, can cause serious hypersensitivity problems, ranging from urticaria (hives) to anaphylactic 4 Treatment prior to most surgical procedures can decrease the incidence of infection afterwards. E ective prophylaxis is directed against the most likely organism, not eradication of every potential pathogen.
Discount tamsulosin
Duration of therapy is dependent on the rate of replacement of healthy skin and nails mens health 042013 purchase cheapest tamsulosin. Ultrafine crystalline preparations are absorbed adequately from the gastrointestinal tract, and absorption is enhanced by high-fat meals. Adverse effects are rare after oral administration, but nausea and vomiting occasionally occur. The topical imidazoles have a variety of uses, including tinea corporis, tinea cruris, tinea pedis, and oropharyngeal and vulvovaginal candidiasis. Oral ketoconazole has historically been used for the treatment of systemic fungal infections but is rarely used today due to the risk for severe liver injury, adrenal insufficiency, and adverse drug interactions. Tinea pedis, tinea corporis, tinea cruris, cutaneous candidiasis, and tinea versicolor may be treated with the 0. Amphotericin B is the best choice since nephrotoxicity is commonly associated with this medication. Although the dose of fluconazole must be adjusted for renal insufficiency, it is not associated with causing nephrotoxicity. She has a history of breast cancer, which was diagnosed 3 months ago, and has been treated with chemotherapy. Her chest x-ray shows possible pneumonia, and respiratory cultures are positive for Aspergillus fumigatus. Fluconazole, flucytosine, and ketoconazole do not have reliable in vitro activity and are therefore not recommended. There is a black box warning that warns against the use of itraconazole in patients with evidence of ventricular dysfunction, including patients with heart failure. The patient complains of thickening of the nail of the right big toe and a change in color (yellow). Which of the following is the most appropriate choice for treating this infection? Terbinafine is better tolerated, requires a shorter duration of therapy, and is more effective than either itraconazole or griseofulvin. Therefore, protozoal diseases are less easily treated than bacterial infections, and many of the antiprotozoal drugs cause serious toxic effects in the host, particularly on cells showing high metabolic activity. In the United States, drugs for some protozoal infections may be obtained by contacting the Centers for Disease Control and Prevention. The disease can be acute or chronic, with varying degrees of illness, from no symptoms to mild diarrhea to fulminating dysentery. Therapy is indicated for acutely ill patients and asymptomatic carriers, since dormant E. For example, luminal amebicides act on the parasite in the lumen of the bowel, whereas systemic amebicides are effective against amebas in the intestinal wall and liver. Mixed amebicides are effective against both the luminal and systemic forms of the disease, although luminal concentrations are too low for single-drug treatment. Mechanism of action: Amebas possess ferredoxin-like, low-redox-potential, electron transport proteins that participate in metabolic electron removal reactions. Pharmacokinetics: Metronidazole is completely and rapidly absorbed after oral administration. Resistance: Resistance to metronidazole is not a therapeutic problem for amebiasis, although strains of trichomonads resistant to the drug have been reported. Tinidazole is as effective as metronidazole, with a shorter course of treatment, but it is more expensive. Adverse effects of iodoquinol include rash, diarrhea, and dose-related peripheral neuropathy, including a rare optic neuritis. Paromomycin is directly amebicidal and also exerts its antiamebic actions by reducing the population of intestinal flora. Systemic amebicides these drugs are useful for treating liver abscesses and intestinal wall infections caused by amebas. It eliminates trophozoites in liver abscesses, but it is not useful in treating luminal amebiasis. Intramuscular injection is the preferred route, since it is an irritant when taken orally. The use of this ipecac alkaloid is limited by its toxicity, and it has largely been replaced by metronidazole. Adverse effects include pain at the site of injection, nausea, cardiotoxicity (arrhythmias and congestive heart failure), neuromuscular weakness, dizziness, and rash. Plasmodium falciparum is the most dangerous species, causing an acute, rapidly fulminating disease that is characterized by persistent high fever, orthostatic hypotension, and massive erythrocytosis (an abnormal elevation in the number of red blood cells accompanied by swollen, reddish limbs). Plasmodium malariae is common to many tropical regions, but Plasmodium ovale is rarely encountered. Resistance acquired by the mosquito to insecticides, and by the parasite to drugs, has led to new therapeutic challenges, particularly in the treatment of P. Female mosquito Infected mosquito Liver cell 2 Sporozoites migrate to the liver, where they form merozoites. Gametocytes Merozoites 6 Red blood cell Trophozoite Some merozoites become gametocytes. Infection can also result from use of a bloodcontaminated needle 3 Merozoites are released and invade red blood cells. These are released when the red blood cell ruptures, and they can infect other red blood cells. Drugs e ective against erythrocytic form: Artemisinin Atovaquone/proguanil Chloroquine Quinine Me oquine Pyrimethamine 4 In the red blood cell, the merozoite becomes a trophozoite. Pharmacokinetics: Primaquine is well absorbed after oral administration and is not concentrated in tissues. Chloroquine Chloroquine is a synthetic 4-aminoquinoline that has been the mainstay of antimalarial therapy, and it is the drug of choice in the 552 43. To protect itself, the parasite polymerizes the heme to hemozoin (a pigment), which is sequestered in the food vacuole. The increased pH and the accumulation of heme result in oxidative damage to the phospholipid membranes, leading to lysis of both the parasite and the red blood cell. Pharmacokinetics: Chloroquine is rapidly and completely absorbed following oral administration. The drug has a very large volume of distribution and concentrates in erythrocytes, liver, spleen, kidney, lung, and melanin-containing tissues, and leukocytes. The accumulation of heme results in lysis of both the parasite and the red blood cell. Chloroquine should be used cautiously in patients with hepatic dysfunction, severe gastrointestinal problems, or neurologic disorders. Resistance: Resistance has become a serious medical problem throughout Africa, Asia, and most areas of Central and South America. Common adverse effects include nausea, vomiting, abdominal pain, headache, diarrhea, anorexia, and dizziness. It has a long half-life (20 days) because of enterohepatic circulation and its concentration in various tissues. The drug undergoes extensive metabolism and is primarily excreted via the bile into the feces. It is reserved for severe infestations and for chloroquine-resistant malarial strains. Antiprotozoal Drugs Quinine is usually administered in combination with doxycycline, tetracycline, or clindamycin. The major adverse effect of quinine is cinchonism, a syndrome causing nausea, vomiting, tinnitus, and vertigo. Drug interactions include potentiation of neuromuscular-blocking agents and elevation of digoxin levels if taken concurrently. Resistance to this combination has developed, so it is usually administered with other agents, such as artemisinin derivatives. Pyrimethamine in combination with sulfadiazine is also used against Toxoplasma gondii. If megaloblastic anemia occurs with pyrimethamine treatment, it may be reversed with leucovorin.
Discount 0.4mg tamsulosin otc
Most cases occur from disruption of an atherosclerotic lesion prostate function purpose purchase 0.4 mg tamsulosin overnight delivery, followed by platelet activation of the coagulation cascade and vasoconstriction. These agents help to balance the cardiac oxygen supply and demand equation by affecting blood pressure, venous return, heart rate, and contractility. All calcium channel blockers are, therefore, arteriolar vasodilators that cause a decrease in smooth muscle tone and vascular resistance. Verapamil has greater negative inotropic effects than amlodipine, but it is a weaker vasodilator. Nondihydropyridine calcium channel blockers can worsen heart failure due to their negative inotropic effect, and their use should be avoided in this population. Nitrates such as nitroglycerin cause dilation of the large veins, which reduces preload (venous return to the heart) and, therefore, reduces the work of the heart. Pharmacokinetics 2 min 25 min Key: Onset of action Duration of action Nitroglycerin Sublingual tablet or spray Oral, sustained release 35 min 48 hr Transdermal 30 min 1012 hr Isosorbide dinitrate Sublingual 5 min 1 hr Nitrates differ in their onset of action and rate of elimination. For prompt relief of an angina attack precipitated by exercise or emotional stress, sublingual (or spray form) nitroglycerin is the drug of choice. All patients suffering from angina should have nitroglycerin on hand to treat acute angina attacks. Therefore, it is commonly administered via the sublingual or transdermal route (patch or ointment), thereby avoiding the hepatic first-pass effect. Phosphodiesterase type 5 inhibitors such as sildenafil potentiate the action of the nitrates. Tolerance to the actions of nitrates develops rapidly as the blood vessels become desensitized to vasodilation. Tolerance can be overcome by providing a daily "nitrate-free interval" to restore sensitivity to the drug. This interval of 10 to 12 hours is usually taken at night because demand on the heart is decreased at that time. Therefore, the nitrate-free interval in these patients should occur in the late afternoon. It is indicated for the treatment of chronic angina and may be used alone or in combination with other traditional therapies. The other answers refer to angina (with varying levels of severity) caused by atherosclerosis. One sublingual nitroglycerin tablet always relieves his symptoms, but this medication gives him an awful headache every time he takes it. The nitroglycerin spray would also be expected to cause headache, so this is not the best choice. Ranolazine is not indicated for immediate relief of an angina attack, nor is it a first-line option. The other options will not provide prompt relief of angina and should not be used to treat an acute attack. He is adherent to a maximized dose of -blocker with a low heart rate and low blood pressure. Ranolazine can be used when other agents are maximized, especially when blood pressure is well controlled. He was continued on his previous home medications (diltiazem, enalapril, and nitroglycerin), and atenolol was added at discharge. He has only had a few sporadic episodes of stable angina that are relieved with nitroglycerin or rest. Nondihydropyridine calcium channel blockers such as diltiazem should be avoided in patients with heart failure with reduced ejection fraction. Patients should be treated with one of three -blockers approved for heart failure with reduced ejection fraction (bisoprolol, metoprolol succinate, or carvedilol). It sounds like his angina symptoms are well managed with his current therapy so adding isosorbide mononitrate would not be necessary. Continue once-daily administration of isosorbide mononitrate but advise the patient to take this medication in the evening. Advise continuation of isosorbide mononitrate twice daily for full 24-hour coverage of anginal symptoms. Switch to isosorbide dinitrate, as this has a longer duration of action than the mononitrate. Switch to nitroglycerin patch for consistent drug delivery and advise him to wear the patch around the clock. It is important to maintain a nitrate-free period to prevent the development of tolerance to nitrate therapy. The nitroglycerin patch should be taken off for 10 to 12 hours daily to allow for nitrate-free interval. Anticoagulants and Antiplatelet Agents Katherine Vogel Anderson and Patrick Cogan I. Bleeding disorders involving the failure of hemostasis are less common than thromboembolic diseases. Both thrombi and emboli are dangerous, because they may occlude blood vessels and deprive tissues of oxygen and nutrients. Venous thrombosis typically involves a clot that is rich in fibrin, with fewer platelets than are observed with arterial clots. The next step involves the formation of a plateletfibrin plug at the site of the puncture. Anticoagulants and Antiplatelet Agents formation, except that the triggering stimulus is a pathologic condition in the vascular system, rather than external physical trauma. Chemical mediators synthesized by endothelial cells: Chemical mediators, such as prostacyclin and nitric oxide, are synthesized by intact endothelial cells and act as inhibitors of platelet aggregation. This prevents platelet activation and the subsequent release of platelet aggregation agents. Damaged endothelial cells synthesize less prostacyclin than healthy cells, resulting in lower prostacyclin levels. Roles of thrombin, thromboxanes, and collagen: the platelet membrane also contains receptors that can bind thrombin, thromboxanes, and exposed collagen. In the intact, normal vessel, circulating levels of thrombin and thromboxane are low, and the intact endothelium covers the collagen in the subendothelial layers. The corresponding platelet receptors are, thus, unoccupied, and as a result, platelet activation and aggregation are not Prostacyclin Nitric oxide Endothelial cells 2 Healthy, intact endothelium releases prostacyclin into plasma. This triggers a complex series of chemical reactions, resulting in platelet activation. Platelet activation Receptors on the surface of the adhering platelets are activated by the collagen of the underlying connective tissue. These receptors function as sensors that are activated by the signals sent from the adhering platelets. Fibrinolysis During clot formation, the fibrinolytic pathway is locally activated. Because these agents have different mechanisms of actions, synergistic or additive effects may be achieved when agents from different classes are combined. This shifts the balance of chemical mediators to favor the antiaggregatory effects of prostacyclin, thereby preventing platelet aggregation. The inhibitory effect is rapid, and aspirin-induced suppression of thromboxane A2 and the resulting suppression of platelet aggregation last for the life of the platelet, which is approximately 7 to 10 days. Aspirin is the only antiplatelet agent that irreversibly inhibits platelet function. Pharmacokinetics: When given orally, aspirin is absorbed by passive diffusion and quickly hydrolyzed to salicylic acid in the liver. Salicylic acid is further metabolized in the liver, and some is excreted unchanged in the urine. Adverse effects: Higher doses of aspirin increase drug-related toxicities as well as the probability that aspirin may also inhibit prostacyclin production. Ibuprofen, if taken within the 2 hours prior to aspirin, can obstruct the access of aspirin to the serine residue and, thereby, antagonize platelet inhibition by aspirin. Therefore, immediate release aspirin should be taken at least 60 minutes before or at least 8 hours after ibuprofen. The maximum inhibition of platelet aggregation is achieved in 1 to 3 hours with ticagrelor, 2 to 4 hours with prasugrel, 3 to 4 days with ticlopidine, and 3 to 5 days with clopidogrel. Pharmacokinetics: these agents require loading doses for quicker antiplatelet effect.
Syndromes
- Improve symptoms
- Blood clots in the legs or lungs
- Cancerous changes called leiomyosarcoma (rare)
- Barbiturates
- ALT test
- Sinus bradycardia -- slow heart rates from the natural pacemaker of the heart
- Cervical cancer
Order 0.4 mg tamsulosin
The scope of this chapter this chapter reviews some of the evidence that has accumulated prostate cancer screening guidelines discount tamsulosin 0.2 mg without prescription, since the publication of the previous edition, on the economic impact of diabetes and on the cost effectiveness of interventions. It aims to provide clinicians and health policy makers with information on the economic impact of diabetes and an indication of how diabetes management and service development should evolve in relation to economic considerations. It does not claim to be a systematic review in the sense used, for example, by the Cochrane Collaboration but recently published studies have been selected if they are considered to contribute significantly to these aims. Given the need to restrict its length, the chapter cannot claim to be a comprehensive review of this burgeoning field. Two literature searches (details available on request) were employed for this chapter. The remainder of the chapter is divided into two broad areas: studies of the economic impact of diabetes; and studies of the cost effectiveness or cost utility of interventions. Reasons for this were expounded by Songer and Barcelу [2] in the previous (third) edition of this textbook. However, the overwhelming majority of this evidence relates to developed (high-income) countries. The economic impact of diabetes Estimates of costs-from different perspectives Fundamental to the quantification of the economic impact of any condition is the question of viewpoint, that is, when costs are being identified, is this from the point of view of the individual with the condition, that of the family, the health system, society as a whole, or a combination of these? These data are estimates of healthcare expenditures by country which include spending by health systems as well as by individuals or families living with diabetes. The proportions attributable to systems on the one hand and to individuals on the other will vary from country to country according to the funding arrangements for the delivery of care. Using formulae first put forward by Jцnsson [4], the method used requires knowledge of the prevalence of diabetes, the total healthcare budget of each country, and an assumption of the ratio of the total cost of medical care for people with diabetes compared to the cost of care for people without diabetes -the "diabetes cost ratio" (R). These formulae enable the calculation of the total cost of care for people with diabetes. Initial estimates of these costs [5] and the most recent estimates [3] have assumed likely lower and upper bounds of R of 2 and 3. As will be emphasized later, this average figure conceals gross disparities in the resources available for diabetes care in different countries (and, quite plausibly, within countries). An estimated 20% of global diabetes expenditure is attributable to low- and middle-income countries in which 80% of people with diabetes live [3]. Estimating diabetes healthcare expenditure using such formulae is a "top-down" approach, that is, calculating expenditures on individuals using epidemiologic and financial data from populations. In most populations, hospital admission is the main driver of expenditures and it has long been known that, although the absolute incidence of hospital admission is greatest in the elderly, the greatest relative difference in admissions between individuals with diabetes and those without is seen in the young. In the former category were the costs of screening and testing (for diagnosis and retinopathy), those attributable to treatment and management of diabetes itself, and those attributed to treating its complications. Included in the indirect cost total were estimates for loss of productivity due to premature mortality, informal care, sickness absence (absenteeism) from work, and the potential loss of productivity among people with diabetes who remain at work (so called "presenteeism" [7]). Thus, even though the economic impact of diabetes on healthcare is high, its impact outside the realm of healthcare is higher still. This finding in the literature is common though not universal (see, for example, reference [8]). Though not often costed in any detail, these aspects of care have long been known to be significant. The authors are clear that the methods for estimating the costs of presenteeism are in their infancy [6]. Nevertheless, these estimates are bound to be contentious since they imply that people with diabetes in work are considerably less productive than they should be, because of their diabetes. Within the direct care category, the proportional contributions of the subcategories do not change greatly. However, within the indirect cost category, the proportional contributions of premature mortality costs are expected to fall (which is gratifying) whereas those of informal caring are expected to rise-which is more concerning. As might be expected, costs rise in all categories, driven by higher prevalences, higher treatment costs, and higher costs of complications. The total cost of diabetes (direct and indirect, type 1 and type 2) is predicted to rise by 68% on its 2010/2011 total while the rise for type 1 and type 2 separately are 121% and 63%, respectively [6]. The predicted increases in direct and indirect costs are roughly equal whereas the predicted increase of indirect costs for type 1 is, in proportional terms, the largest of all. The authors comment that "any improvements in the way diabetes is treated that lead to better glycemic control and fewer complications could have a significant impact on these costs, but this remains to be assessed. These changes and concomitant improvements in morbidities such as visual and renal impairment will need to be taken into account in revisions of models such as that of Hex et al. Interviews with participants, data from hospital billing departments, medical records departments, and government sources are being used in a combination of bottom-up and top-down approaches to calculate direct medical costs, direct nonmedical costs and indirect costs from different viewpoints-patients and their families, health system, insurers, and the wider society. This and other ongoing studies as yet unpublished may well confirm that the diabetes cost ratio, at least in some populations, is significantly greater than the 3 previously taken as the likely upper limit. The evidence base for the costs of diabetes in countries other than the Americas, western Europe and Australasia is growing (see, for example, data from India [12,13], Ethiopia [14], and Iran [15]). Drivers of direct costs Given that hospital admission for diabetes is an important driver of healthcare expenditures and that the bulk of hospital admissions of people with diabetes are for the treatment of complications, it follows that the presence of complications will be a potent influence on healthcare costs. The presence of microvascular complications alone increased the per person costs by a factor of 1. The presence of both types of complications increased costs specific to hospitalization by 5. When individuals and families pay the cost of care themselves the economic impact of diabetes can be particularly savage when much or most of it is borne by individuals or families. A larger share of healthcare expenditure for the condition is shouldered by individuals living in low- and middle-income countries when compared with those living in high-income countries [3]. In Latin America, for example, 4060% of the cost of medical care for people with diabetes is out-of-pocket. At least one study from India [21] has reported an increase over time in the extent to which families living with diabetes have to use their own income to fund diabetes care. Information from a sample of patients attending hospital clinics and general practitioners in urban and rural areas of seven states in India in 2005 showed that families in urban areas spent, on average, 10% of their income funding the care of a diabetic member while, for families in rural areas, the figure was 17%. Compared with a previous, similar study carried out in 1998 [22] and after accounting for inflation, the proportion of family income devoted to diabetes care had increased by 113%. In both studies, poorer families contributed larger proportions of their income than did the wealthier families and the secular increase was most marked in the poorest families increasing from 24. Perhaps surprisingly, they found that coverage by any type of health insurance was higher (90%) in the group with diabetes than in those without (81%). More adults aged 1864 years with diabetes had Medicare coverage compared to those without (14% vs. Those within this age group who had diabetes were more likely to have more than one source of insurance coverage (13% vs. Songer [24] had commented earlier that 15% of families with one or more children reported difficulty in obtaining health insurance coverage because of pre-existing illness clauses. Some of the consequences, at least in the process of care although not in outcome, of non- and under-insurance are detailed by DeVoe et al. The need for individuals and families in some populations to contribute towards the costs of care is exacerbated by curtailment in earning power as a result of diabetes. With greater than 10 years diabetes duration and controlling for confounders, men with diabetes in employment and with upper secondary education were 4. Songer [26] speculates that "with renewed enthusiasm for the long-term health of individuals after the diagnosis of diabetes [in more recent cohorts of patients], there is hope regarding the potential for full and productive employment. The former, Australian, study concentrated on the economic consequences of taking early retirement as a result of diabetes. The consequences were twofold: loss of income as a result of not being in employment, and reduced accumulated savings to finance their retirement as a result of their diabetes. The burden of caring resulted in loss of earnings and significant levels of strain in the carers, as well as loss of earnings and significantly poorer health-related quality of life in the individuals being cared for. The consequences of less-than-optimum therapy the efficient use of resources is a topic for the next section of this chapter. The consequences of less than optimum therapy are, however, a useful link between descriptive economic studies and analytical studies such as cost-effectiveness and cost-utility analyses. Several large studies have commented on what they consider to be less-than-optimal care. For example, the DiabCare Asia study audited the quality of care in 11 countries in 1998 and 2003 [32] and concluded, from the examination of the records of over 20,000 patients in the first and 15,500 in the second study, that the level of blood glucose control was, in their view, unsatisfactory (mean HbA1c 8% and mean fasting blood glucose 9 mmol L-1). In the Bangladesh component of DiabCare Asia [33], similar conclusions were drawn with a mean HbA1c (amongst 1952 patients) of 8. It is now an accepted tenet of diabetes care that poor metabolic control (not only of blood glucose but also blood pressure and lipids) is associated with an increased likelihood of the development of complications.
Order tamsulosin
This is not an allergic reaction androgen hormone production discount 0.4mg tamsulosin, and the patient can be rechallenged; however, the patient might be at risk for developing C. The cell wall is composed of a polymer called peptidoglycan that consists of glycan units joined to each other by peptide cross-links. To be maximally effective, inhibitors of cell wall synthesis require actively proliferating microorganisms. The most important members of this group of drugs are the -lactam antibiotics (named after the -lactam ring that is essential to their activity), vancomycin, and daptomycin. The nature of this side chain affects the antimicrobial spectrum, stability to stomach acid, crosshypersensitivity, and susceptibility to bacterial degradative enzymes (-lactamases). Mechanism of action the penicillins interfere with the last step of bacterial cell wall synthesis (transpeptidation or cross-linkage), resulting in exposure of the osmotically less stable membrane. Cell lysis can then occur, either through osmotic pressure or through the activation of autolysins. Penicillins are only effective against rapidly growing organisms that synthesize a peptidoglycan cell wall. Consequently, they are inactive against organisms devoid of this structure, such as mycobacteria, protozoa, fungi, and viruses. Penicillin-binding proteins: Penicillins also inactivate numerous proteins on the bacterial cell membrane. Cell Wall Inhibitors prevent cell wall synthesis but also lead to morphologic changes or lysis of susceptible bacteria. Penicillins inhibit this transpeptidase-catalyzed reaction, thus hindering the formation of cross-links essential for cell wall integrity. Production of autolysins: Many bacteria, particularly the grampositive cocci, produce degradative enzymes (autolysins) that participate in the normal remodeling of the bacterial cell wall. In the presence of a penicillin, the degradative action of the autolysins proceeds in the absence of cell wall synthesis. Thus, the antibacterial effect of a penicillin is the result of both inhibition of cell wall synthesis and destruction of the existing cell wall by autolysins. However, gram-negative bacteria have proteins inserted in the lipopolysaccharide layer that act as water-filled channels (called porins) to permit transmembrane entry. Natural penicillins: Natural penicillins (penicillin G and penicillin V) are obtained from fermentations of the fungus Penicillium chrysogenum. Semisynthetic penicillins, such as amoxicillin and ampicillin (also known as aminopenicillins), are created by chemically attaching different R groups to the 6-aminopenicillanic acid nucleus. Penicillins are susceptible to inactivation by -lactamases (penicillinases) that are produced by the resistant bacteria. Despite widespread use and increase in resistance to many types of bacteria, penicillin remains the drug of choice for the treatment of gas gangrene (Clostridium perfringens) and syphilis (Treponema pallidum). Penicillin V has a similar spectrum to that of penicillin G, but it is not used for treatment of bacteremia because of its poor oral absorption. Penicillin V is more acid stable than penicillin G and is often employed orally in the treatment of infections. Penicillinase-producing strains are treated using ceftriaxone, with azithromycin or spectinomycin as a backup. Infection often occurs in an institutional setting in individuals who are ill from other causes. Resistance to penicillin G has greatly increased worldwide due to mutations in one or more of the bacterial penicillinbinding proteins. A single treatment with penicillin is curative for primary and secondary syphilis. Resistance to these antibiotics is now a major clinical problem because of inactivation by plasmid-mediated penicillinases. Antimicrobial spectrum of ampicillin Gram (+) cocci Enterococci Gram (+) bacilli Listeria monocytogenes Gram () cocci Gram () rods Escherichia coli Haemophilus in uenzae Proteus mirabilis Salmonella typhi Anaerobic organisms Spirochetes Mycoplasma Chlamydia Other B. They are effective against many gram-negative bacilli, but not against Klebsiella because of its constitutive penicillinase. Formulation of ticarcillin or piperacillin with clavulanic acid or tazobactam, respectively, extends the antimicrobial spectrum of these antibiotics to include penicillinase-producing organisms (for example, most Enterobacteriaceae and Bacteroides species). Resistance Natural resistance to the penicillins occurs in organisms that either lack a peptidoglycan cell wall (for example, Mycoplasma pneumoniae) or have cell walls that are impermeable to the drugs. Acquired resistance to the penicillins by plasmid-mediated -lactamases has become a significant clinical problem. Multiplication of resistant strains leads to increased dissemination of the resistance genes. By obtaining resistance plasmids, bacteria may acquire one or more of the following properties, thus allowing survival in the presence of -lactam antibiotics. They are the major cause of resistance to the penicillins and are an increasing problem. Some of the -lactam antibiotics are poor substrates for -lactamases and resist hydrolysis, thus retaining their activity against -lactamaseproducing organisms. The presence of an efflux pump can also reduce the amount of intracellular drug (for example, Klebsiella pneumoniae). Administration: the route of administration of a -lactam antibiotic is determined by the stability of the drug to gastric acid and by the severity of the infection. Penicillin V, amoxicillin, and dicloxacillin are available only as oral preparations. They are slowly absorbed into the circulation and persist at low levels over a long time period. Absorption: Most of the penicillins are incompletely absorbed after oral administration, and they reach the intestine in sufficient amounts to affect the composition of the intestinal flora. Food decreases the absorption of all the penicillinase-resistant penicillins because as gastric emptying time increases, the drugs are destroyed by stomach acid. Metabolism: Host metabolism of the -lactam antibiotics is usually insignificant, but some metabolism of penicillin G may occur in patients with impaired renal function. Excretion: the primary route of excretion is through the organic acid (tubular) secretory system of the kidney as well as by glomerular filtration. They are primarily metabolized in the liver and do not require dose adjustment for renal insufficiency. Adverse reactions Penicillins are among the safest drugs, and blood levels are not monitored. Hypersensitivity: Approximately 5% percent of patients have some kind of reaction, ranging from rashes to angioedema (marked swelling of the lips, tongue, and periorbital area) and anaphylaxis. Cell Wall Inhibitors To determine whether treatment with a -lactam is safe when an allergy is noted, patient history regarding severity of previous reaction is essential. Diarrhea: Diarrhea is a common problem that is caused by a disruption of the normal balance of intestinal microorganisms. It occurs to a greater extent with those agents that are incompletely absorbed and have an extended antibacterial spectrum. Nephritis: Penicillins, particularly methicillin, have the potential to cause acute interstitial nephritis. Neurotoxicity: the penicillins are irritating to neuronal tissue, and they can provoke seizures if injected intrathecally or if very high blood levels are reached. Hematologic toxicities: Decreased coagulation may be observed with high doses of piperacillin, ticarcillin, and nafcillin (and, to some extent, with penicillin G). Cytopenias have been associated with therapy of greater than 2 weeks, and therefore, blood counts should be monitored weekly for such patients. Cephalosporins have the same mode of action as penicillins, and they are affected by the same resistance mechanisms. First generation: the first-generation cephalosporins act as penicillin G substitutes. Second generation: the second-generation cephalosporins display greater activity against three additional gram-negative organisms: H. They are the only cephalosporins commercially available with appreciable activity against gram-negative anaerobic bacteria. However, neither drug is first line because of the increasing prevalence of resistance among B. Third generation: these cephalosporins have assumed an important role in the treatment of infectious diseases.
Buy tamsulosin 0.2mg fast delivery
This formulation is equivalent to mycophenolate mofetil in the prevention of acute rejection episodes in kidney transplant recipients mens health 100 order tamsulosin cheap. Hybridomas are produced by fusing mouse antibody-producing cells with tumor cells. Hybrid cells are selected and cloned, and the antibody specificity of the clones is determined. Clones of interest can be cultured in large quantities to produce clinically useful amounts of the desired antibody. The polyclonal antibodies, although relatively inexpensive to produce, are variable and less specific, which is in contrast to monoclonal antibodies, which are homogeneous and specific. Antithymocyte globulins Antithymocyte globulins are polyclonal antibodies that are primarily used at the time of transplantation to prevent early allograft rejection along with other immunosuppressive agents. They may also be used to treat severe rejection episodes or corticosteroid-resistant acute rejection. The antibodies bind to the surface of circulating T lymphocytes, which then undergo various reactions, such as complementmediated destruction, antibody-dependent cytotoxicity, apoptosis, and opsonization. The antibody-bound cells are phagocytosed in the liver and spleen, resulting in lymphopenia and impaired T-cell responses. The antibodies are slowly infused intravenously, and their half-life extends from 3 to 9 days. Because the humoral antibody mechanism remains active, antibodies can be formed against these foreign proteins. Corticosteroids antibody approved for clinical use in 1986, indicated for the treatment of corticosteroid-resistant acute rejection of kidney, heart, and liver allografts. The drug has been discontinued from the market due to the availability of newer biologic drugs with similar efficacy and fewer side effects. Basiliximab the antigenicity and short serum half-life of the murine monoclonal antibody have been averted by replacing most of the murine amino acid sequences with human ones by genetic engineering. Usually, two doses of this drug are administered-the first at 2 hours prior to transplantation and the second at 4 days after the surgery. For transplantation, the most common agents are prednisone and methylprednisolone, whereas prednisone and prednisolone are used for autoimmune conditions. In addition, they are effective against a wide variety of autoimmune conditions, including refractory rheumatoid arthritis, systemic lupus erythematosus, temporal arthritis, and asthma. The exact mechanism responsible for the immunosuppressive action of the corticosteroids is unclear. For example, they are diabetogenic and can cause hypercholesterolemia, cataracts, osteoporosis, and hypertension with prolonged use. Sirolimus is used prophylactically with cyclosporine to prevent renal rejection but is less effective when an episode is occurring. Furthermore, the combination of cyclosporine and sirolimus is more nephrotoxic than cyclosporine alone. Immunosuppressive drug regimens should work synergistically at different places in the T-cell activation cascade. Additionally, cyclosporine and tacrolimus are both extremely nephrotoxic and when used together would cause harm to the patients. Prednisone can affect not only T-cell proliferation but also that of B cells and is, therefore, nonspecific. Mycophenolate mofetil exerts its immunosuppressive action by inhibiting inosine monophosphate dehydrogenase, thus depriving the cells of guanosine, a key component of nucleic acids. Homer and Aristotle described the poison arrow; Socrates was executed with poison hemlock; Cleopatra used an African Cobra to commit suicide; lead poisoning may have helped bring down the Roman Empire; Marilyn Monroe, Elvis Presley, and actor Heath Ledger all fatally overdosed on prescription medication. Once in the body, some of the common targets of toxicity include the central nervous system, the lungs, the kidney, the heart, the liver, the blood, and even the intricate acid/ base and electrolyte balance of the body. An understanding of the varied mechanisms of toxicity helps to provide an explanation for the clinical manifestations and a basis for the approach to treatment. This chapter provides an overview of the emergent management of the poisoned patient. In addition, a brief review of some of the more common and interesting toxins, their mechanisms, clinical presentations, and clinical management is presented. Airway, breathing, and circulation are assessed and addressed initially, along with any other immediately lifethreatening toxic effect (for example, profound increases or decreases in blood pressure, heart rate, breathing, or body temperature, or any dangerous dysrhythmias). Acid/base and electrolyte disturbances, along with an acetaminophen and salicylate blood level, can be further assessed as laboratory results are obtained. Clinical Toxicology for administration of the "coma cocktail" as possibly diagnostic and therapeutic. The "coma cocktail" consists of intravenous dextrose to treat hypoglycemia, a possible toxicological cause of altered mental status, along with naloxone to treat possible opioid or clonidine toxicity, and thiamine for ethanol-induced Wernicke encephalopathy. Decontamination Once the patient is stabilized, the assessment for decontamination can occur. Several substances do not adsorb to activated charcoal (for example, lead and other heavy metals, iron, lithium, potassium, and alcohols), limiting the use of activated charcoal unless there are coingested products. Hemodialysis: the elimination of some medications/toxins may be enhanced by hemodialysis if certain properties are met: low protein binding, small volume of distribution, small molecular weight, and water solubility of the toxin. Some examples of medications or substances that can be removed with hemodialysis include methanol, ethylene glycol, salicylates, theophylline, phenobarbital, and lithium. Urinary alkalinization: Alkalinization of the urine enhances the elimination of salicylates or phenobarbital. Increasing the urine pH with intravenous sodium bicarbonate transforms the drug into an ionized form that prevents reabsorption, thereby trapping it in the urine to be eliminated by the kidney. Multiple-dose activated charcoal: Multiple-dose activated charcoal therapy enhances the elimination of certain drugs (for example, theophylline, phenobarbital, digoxin, carbamazepine, valproic acid) by creating a gradient across the lumen of the gut. Medications traverse from areas of high concentration to low concentration, promoting medication already absorbed to cross back into the gut to be adsorbed by the activated charcoal present. In addition, activated charcoal blocks the reabsorption of medications that undergo enterohepatic recirculation (such as phenytoin), by adsorbing the substance to the activated charcoal. Acetaminophen Acetaminophen produces toxicity when its usual metabolic pathways become saturated. However, in overdose, the glutathione is depleted, leaving the metabolite to produce toxicity. Clinical Toxicology nomogram is helpful for acute acetaminophen ingestions when levels can be obtained between 4 and 24 hours postingestion. Methanol (wood alcohol) and ethylene glycol: Methanol is found in such products as windshield washer fluid and model airplane fuel. However, methanol and ethylene glycol are oxidized to toxic products: formic acid in the case of methanol and glycolic, glyoxylic, and oxalic acids in the case of ethylene glycol. If untreated, methanol ingestion may produce blindness, metabolic acidosis, seizures, and coma. Ethylene glycol ingestion may lead to renal failure, hypocalcemia, metabolic acidosis, and heart failure. Isopropanol (rubbing alcohol, isopropyl alcohol): this secondary alcohol is metabolized to acetone via alcohol dehydrogenase. Carbon monoxide Carbon monoxide is a colorless, odorless, and tasteless gas, which is impossible for individuals to detect without a carbon monoxide detector. It is a natural by-product of the combustion of carbonaceous materials, and common sources of this gas include automobiles, poorly vented furnaces, fireplaces, wood-burning stoves, kerosene space heaters, house fires, and charcoal grills. Following inhalation, carbon monoxide rapidly binds to hemoglobin to produce carboxyhemoglobin. The binding affinity of carbon monoxide to hemoglobin is 230 to 270 times greater than that of oxygen. Consequently, even low concentrations of carbon monoxide in the air can produce significant levels of carboxyhemoglobin. Carbon monoxide toxicity can occur following the inhalation or ingestion of methylene chloride found in paint strippers also. Once absorbed, methylene chloride is metabolized by the liver to carbon monoxide through the cytochrome P450 pathway. The symptoms of carbon monoxide intoxication are consistent with hypoxia, with the brain and heart showing the greatest sensitivity. Symptoms include headache, dyspnea, lethargy, confusion, and drowsiness, whereas higher exposure levels can lead to seizures, coma, and death. Select Pharmaceutical and Occupational Toxicities carbon monoxidepoisoned patient includes prompt removal from the source of carbon monoxide and institution of 100% oxygen by nonrebreathing face mask or endotracheal tube.
Tamsulosin 0.2mg discount
High-calorie diets are commonly high in saturated animal fat mens health workouts effective tamsulosin 0.4 mg, which via increased gastrointestinal absorption may accelerate diabetic complications. It is also thought that obesity-induced neuropathy can be improved by dietary restriction of fat intake, relevant to diabetic individuals who are obese (Chapter 41). The most obvious effects of decreasing saturated fat intake would be on glycemic control where improved insulin sensitivity and secretion could influence end-organ function at sites of microvascular disease. Other compelling evidence of the role of overconsumption of saturated fats in progressive diabetic complications comes from studies using lipid lowering therapies such as statins and fibrates. There is, however, ongoing controversy as to whether restriction of dietary fat intake has beneficial effects on microvascular disease in diabetes. Statins are thought to have broad-ranging benefits in diabetic individuals, while fibrates have shown inconsistent results with a number of pleiotropic effects such as anti-inflammatory actions, in addition to improving flowmediated dilatation. Statins have also been shown to have anti-inflammatory effects [23], which are postulated to be due to their capacity to limit the production of isoprenoids which are key downstream mediators of the inflammatory response. In other experimental models, there is also some rationale for the use of fenofibrates and statins to treat microvascular complications. As seen in nondiabetic individuals, regular moderate exercise can improve a number of risk factors relevant to the development of microvascular complications and may be an effective nonpharmacologic approach if compliance issues could be overcome [25]. Adipokines Adipose tissue is highly secretory, releasing a number of factors which are modulated in response to hyperglycemia and viewed to influence diabetic complications. These adipokines include adiponectin, which is thought to reduce oxidative stress. Circulating adiponectin is also predictive of progressive kidney, retinal, and cardiovascular complications in diabetes. In contrast, however, increases in circulating adiponectin concentrations have also been shown to correlate with vascular complications in T1 diabetic individuals. In rodent models, elevating adiponectin concentrations attenuates, while prevention of the interaction of adiponectin with its receptors, worsens kidney disease in diabetes [19]. Intravitreal leptin concentrations are increased in individuals with proliferative diabetic retinopathy, while leptin has been shown to stimulate ischemia-induced retinal neovascularization [26]. In addition, deletion of the leptin receptor in mice also results in autonomic neuropathy. Systemically, elevations in leptin concentrations are associated with renal disease and infusion of exogenous leptin leads to renal disease in various experimental models [1]. This could be partly because leptin has been reported to be pro-inflammatory, albeit in other contexts. However, it is unclear as to why leptin has specific effects at sites of diabetic complications which appear independent of its profound effects on appetite. Protein modifications and turnover One of the most complex processes that occur within cells is the folding of proteins, where stoichiometry dictates the final structure aided by posttranslational modifications such as advanced glycation, glycosylation, and phosphorylation. Indeed, changes in the functional properties of proteins are postulated as major contributors to chronic diseases including diabetic complications, which share the pathologic feature of aggregated misfolded protein deposits. This suggests the exciting possibility that "protein-misfolding" may present a common target for therapeutic intervention in diabetic complications [27]. Autophagy Autophagy is a cellular process that recycles amino acids during times of need, including starvation and metabolic disorders such as diabetes [28]. Therefore, changes in autophagy could facilitate the use of inappropriate fuels for energy production. In diabetic microvascular disease, the study of autophagy is a relatively recent area of research. These studies suggest that changes in autophagy may contribute to structural and functional decline at sites of diabetic complications via disruption of cellular "spring cleaning" of damaged proteins. Posttranslational modifications of proteins Enzymatic glycosylation Glycosylation is a critical enzymatic posttranslational modification resulting in the addition of glycans onto proteins, lipids, and other organic molecules. Advanced glycation Advanced glycation of free amino groups on proteins and amino acids is a nonenzymatic posttranslational modification first discovered in food chemistry more than 100 years ago by the physician Louise Camille Maillard [32]. This reaction is influenced by many factors and is as heterogeneous as the complex biochemical reactions by which these advanced glycated products can be formed. Physiologically, advanced glycation is postulated as an evolutionary pathway for labeling of senescent cellular amino acids for their recognition and ultimate turnover but it is likely that this is an over-simplistic view of these complex modifications. Indeed, recent evidence has shown that advanced glycation may modulate insulin secretion [33] and signaling [34,35], although the ultimate influence of this particular action on diabetic complications is yet to be determined. In addition, advanced glycation is thought to stabilize extracellular matrix proteins via cross-linking. It is therefore likely that these posttranslational modifications have other as yet undiscovered physiologic roles. In diabetes, not only do long-lived proteins become more heavily modified but short-lived proteins are also altered by advanced glycation. The consequences of excessive modification of proteins by advanced glycation are numerous. This has been shown under pathologic conditions to excessively cross-link the matrix resulting in stiffening and slow turnover rates. Intracellularly, advanced glycation can directly alter trafficking and protein function. Therefore, approaches that increase the activity of glyoxalase-1 or decrease the accumulation of methylglyoxal may also be worth considering as therapeutic targets in diabetic microvascular complications. This is a highly relevant finding since nephrin is strongly implicated in the pathogenesis of proteinuria including in the diabetic setting with nephrin gene deletion, nephrin gene mutations, and acquired nephrin deficiency as seen in diabetes with all these alterations in nephrin associated with increased proteinuria. Gp91phox has a number of tissue specific homologues which include Nox-5 (humans only), Nox-1, and Nox-3. These include Nox-4, originally identified in renal tissues, which is a unique subunit in that it does not require the other subunits to generate O2 -. Although originally discovered in the cytosol, Nox-4 has been recently discovered in the mitochondria. Nitric oxide synthase Nitric oxide is produced frequently as a cellular signaling molecule by numerous cell populations. Mitochondrial sources the excess generation of superoxide (O2 -) by dysfunctional mitochondria has been postulated as an early event in diabetic complications [47]. Under physiologic conditions, about 1% of oxygen is only partially reduced to O2 -, instead of fully to water. However, there has never been substantiation of this phenomenon in in vivo models of diabetes. Despite this, there are a number of studies demonstrating mitochondrial functional abnormalities at sites of diabetic complications [12]. This is part of the therapeutic rationale for the use of antioxidants which may target the mitochondrial production of superoxide to treat diabetic complications. Idebenone is an antioxidant with preferential mitochondrial uptake by organs such as neurons, kidney, and cardiac tissues. Administration of exogenous Coenzyme Q has shown therapeutic benefits in animal models of diabetic complications [49,50]. There are numerous other important cellular antioxidants, such as glutathione and numerous vitamins [12]. It is well appreciated that there are changes in the expression and activity of antioxidant enzymes at sites of diabetic microvascular disease [12]. Catalase overexpression is, however, protective in experimental models of type 2 diabetic nephropathy. Modulating antioxidant activity as a potential therapy for diabetic complications remains disappointing in clinical trials, however, despite some benefits of agents such as -lipoic acid on pain and muscle weakness in diabetic polyneuropathy [1]. Inflammatory cell infiltration Phagocytic cells such as monocytes and macrophages are often the first infiltrating cells that arrive at sites of diabetic complications [57,58] in response to chemotactic molecules. A number of rodent studies have suggested a causal role for monocytes and macrophages in the development of diabetic complications [59]. These changes in cytoskeletal rearrangement are also likely to be important for other cell types affected by diabetes. Inflammation An intact acute inflammatory cascade is critical for innate immunity, and is triggered in response to a real or perceived threat to tissue homeostasis. Although the innate immune response is relatively nonspecific, adaptive immunity allows the human body to recognize and remember pathogens resulting in the capacity for an enhanced inflammatory response upon subsequent exposure to the same pathogen. Acute inflammation is a tightly regulated cascade of factors such as pro-inflammatory cytokines.
Buy 0.2 mg tamsulosin overnight delivery
The receptors coupled to the second messenger system are known as metabotropic receptors prostate cancer blood in urine buy discount tamsulosin 0.2 mg on line. Responses in the somatic motor neurons are generally slower than in the autonomic nervous system. Somatic motor neurons innervate skeletal muscles (not smooth muscle) and have no ganglia. Also, the responses in the somatic motor nervous system are faster compared to the responses in the autonomic nervous system due to the lack of ganglia in the former. When a person is in the "fight-or-flight" mode, as in the case of a bear attack, the sympathetic system will be activated. Activation of the sympathetic system causes an increase in heart rate and blood pressure and a decrease (not increase) in gastric motility. It also causes dilation (not constriction) of the pupil and inhibition of lacrimation. Activation of the parasympathetic system causes a reduction in heart rate, constriction of the pupil, an increase in gastric motility and salivation, and contraction of the bladder muscle. Therefore, inhibition of the parasympathetic system causes an increase in heart rate, dilation of the pupil, a decrease in gastric motility, dry mouth, and relaxation of detrusor muscles. Acetylcholine is the neurotransmitter in the cholinergic system, and it activates both muscarinic and nicotinic cholinergic receptors, not adrenergic receptors. Activation of the sympathetic system causes an increase in blood pressure (not a drop in blood pressure) due to vasoconstriction and stimulation of the heart. The parasympathetic division is involved in accommodation of near vision, movement of food, and urination. The postganglionic fibers of the parasympathetic division are long compared to those of the sympathetic nervous system. Neurotransmitter release is triggered by the arrival of action potentials in the postsynaptic cell. Intracellular calcium levels drop in the neuron before the neurotransmitter is released. The parasympathetic nervous system maintains essential bodily functions, such as vision, movement of food, and urination. It uses acetylcholine, not norepinephrine, as a neurotransmitter, and it discharges as discrete fibers that are activated separately. The postganglionic fibers of the parasympathetic system are short compared to those of the sympathetic division. When an action potential arrives in the presynaptic neuron, calcium enters the presynaptic neuron and the calcium levels increase in the neuron before the neurotransmitter is released. Activation of 1 receptors causes mydriasis, vasoconstriction, and an increase in blood pressure. Activation of 1 receptors increases heart rate, contractility of the heart, and blood pressure. Activation of 2 receptors causes dilation of bronchioles and relaxation of skeletal muscle vessels. Thus, inhibition of these receptors will cause vasorelaxation (1 blockade), reduction in heart rate (1 blockade), reduction in contractility of the heart (1 blockade), reduction in blood pressure, bronchoconstriction (2 blockade), and constriction of blood vessels supplying skeletal muscles (2 blockade). When there is a sudden drop in blood pressure, the baroreceptors send signals to the brain, and the brain activates the sympathetic system (not the parasympathetic system) to restore blood pressure to normal values. Neurotransmitters generally bind to the membrane receptors on the postsynaptic effector cells and cause cellular effects. These types of receptors that are coupled to second messenger systems are known as metabotropic receptors. These types of receptors that activate ion channels directly are known as ionotropic receptors. Synthesis of acetylcholine: Choline is transported from the extracellular fluid into the cytoplasm of the cholinergic neuron by an energy-dependent carrier system that cotransports sodium and can be inhibited by the drug hemicholinium. Release of acetylcholine: When an action potential propagated by voltage-sensitive sodium channels arrives at a nerve ending, voltage-sensitive calcium channels on the presynaptic membrane open, causing an increase in the concentration of intracellular calcium. Elevated calcium levels promote the fusion of synaptic vesicles with the cell membrane and the release of their contents into the synaptic space. Binding to a receptor leads to a biologic response within the cell, such as the initiation of a nerve impulse in a postganglionic fiber or activation of specific enzymes in effector cells, as mediated by second messenger molecules. Recycling of choline: Choline may be recaptured by a sodiumcoupled, high-affinity uptake system that transports the molecule back into the neuron. Muscarinic receptors Muscarinic receptors belong to the class of G proteincoupled receptors (metabotropic receptors). Locations of muscarinic receptors: these receptors are found on ganglia of the peripheral nervous system and on the autonomic effector organs, such as the heart, smooth muscle, brain, and exocrine glands. Diacylglycerol activates protein kinase C, an enzyme that phosphorylates numerous proteins within the cell. Muscarinic agonists: Pilocarpine is an example of a nonselective muscarinic agonist used in clinical practice to treat xerostomia and glaucoma. Direct-Acting Cholinergic Agonists agonists and antagonists that are directed against specific receptor subtypes. The nicotinic receptor is composed of five subunits, and it functions as a ligand-gated ion channel. The more therapeutically useful drugs (pilocarpine and bethanechol) preferentially bind to muscarinic receptors and are sometimes referred to as muscarinic agents. Nitric oxide then diffuses to vascular smooth muscle cells to stimulate protein kinase G production, leading to hyperpolarization and smooth muscle relaxation via phosphodiesterase-3 inhibition. It lacks nicotinic actions (due to the addition of the methyl group) but does have strong muscarinic activity. Actions: Bethanechol directly stimulates muscarinic receptors, causing increased intestinal motility and tone. Therapeutic applications: In urologic treatment, bethanechol is used to stimulate the atonic bladder, particularly in postpartum or postoperative, nonobstructive urinary retention. These include sweating, salivation, flushing, decreased blood pressure, nausea, abdominal pain, diarrhea, and bronchospasm. Therapeutic uses: Because of its high potency, receptor nonselectivity, and relatively long duration of action, carbachol is rarely used therapeutically except in the eye as a miotic agent to treat glaucoma by causing pupillary contraction and a decrease in intraocular pressure. Adverse effects: At doses used ophthalmologically, little or no side effects occur due to lack of systemic penetration (quaternary amine). Actions: Applied topically to the eye, pilocarpine produces rapid miosis and contraction of the ciliary muscle. The drug is beneficial in promoting salivation in patients with xerostomia resulting from irradiation of the head and neck. Sjцgren syndrome, which is characterized by dry mouth and lack of tears, is treated with oral pilocarpine tablets and cevimeline, a cholinergic drug that also has the drawback of being nonspecific. Therapeutic use in glaucoma: Pilocarpine is used to treat glaucoma and is the drug of choice for emergency lowering of intraocular pressure of both open-angle and angle-closure glaucoma. Pilocarpine is extremely effective in opening the trabecular meshwork around the Schlemm canal, causing an immediate drop in intraocular pressure as a result of the increased drainage of aqueous humor. Adverse effects: Pilocarpine can cause blurred vision, night blindness, and brow ache. The effects are similar to those produced by consumption of mushrooms of the genus Inocybe. Parenteral atropine, at doses that can cross the bloodbrain barrier, is administered to counteract the toxicity of pilocarpine. It is located both pre- and postsynaptically in the nerve terminal where it is membrane bound. It is rapidly absorbed and has a short duration of action of 10 to 20 minutes due to rapid renal elimination. Intravenous injection of edrophonium leads to a rapid increase in muscle strength. Care must be taken, because excess drug may provoke a cholinergic crisis (atropine is the antidote).