Buy discount tastylia line
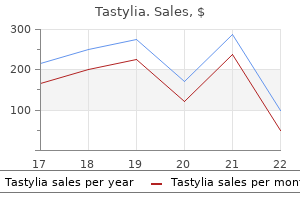
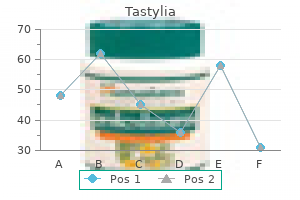
This small portable device can be used in multiple exam rooms and requires minimal training for use treatment jokes purchase tastylia 10 mg on line. It is recommended that if one has Type 2 diabetes and is using diabetes medications and insulin, one should perhaps test three or four times a day. In the case of Type 2 diabetes, using medications, and having trouble achieving good control, testing two or four times a day is recommended. If one has Type 2 diabetes and managing with diet/exercise only, there is no specific recommendation. Many people like to do a "fasting test" when they wake up, as a gauge to start the day. If they are concerned about meal planning, they may opt to do a "preprandial" and "postprandial" test (before the meal and 2 h after), so as to do a "before-and-after" comparison. Unfortunately, health insurance companies often cover only one or two test strips a day for people with Type 2 diabetes, and this may not be sufficient. However, in some cases, insurance companies will cover more strips if a physician writes a prescription for more strips. Health authorities generally endorse frequent monitoring regardless of type of diabetes, or method of treatment, but one study reported finding little value in monitoring for people with Type 2 diabetes who are not taking insulin (Farmer, Wade, French et al. Very high blood glucose in the early morning may be due to the release of certain hormones in the middle of the night. The body can make counter-regulatory hormones that work against the action of insulin. These hormones, including glucagon, epinephrine, growth hormone, and cortisol, raise blood glucose levels when needed by signaling the liver to release more glucose and by inhibiting glucose utilization throughout the body. There is a surge in the amount of growth hormone the body releases in the middle of the night, followed by a surge in cortisol that effectively drives up glucose production in the liver. In people with Type 2 diabetes, whose liver may not respond to insulin well enough to stop glucose production, changes in glucose metabolism during sleep can have a profound effect on morning blood glucose levels. Then, the body sometimes reacts by releasing counter-regulatory hormones, such as glucagon and epinephrine, to signal the liver to convert its stores of glycogen into glucose, raising blood glucose levels. This can result in a period of high blood sugar following an episode of hypoglycemia. The Somogyi effect is most likely to occur following an episode of nighttime hypoglycemia resulting in high blood sugar levels in the morning. People who wake up with high blood sugar should check their blood glucose levels in the middle of the night. If their blood sugar level is falling, or low, at that time, they should alert their healthcare provider with a view to implementing strategies of increasing food intake or lowering insulin dose in the evening. Some people with diabetes monitor 1 h after the start of meals in an effort to find their peak blood sugar level and then work to prevent spikes above certain levels. The after-meal blood sugar goals for nonpregnant adults published by major diabetes organizations now specify that the levels should be measured 2 h after the start of a meal. As of 2015, American Association of Clinical Endocrinologists guidelines call for the tightest control, with 2-h readings below 140 mg/dL (Handelsman, Bloomgarden, Grunberger et al. In any case, these two conditions are strongly linked and the combination is especially hazardous to health. The aim of a study published in the Journal of Hypertension was to determine whether there exists a gender-specific association between blood pressure levels and incident Type 2 diabetes mellitus in a representative population sample. The data were collected from several thousand men and women aged 25 to 74 years, who participated in one of the three Monitoring Trends and Determinants on Cardiovascular Diseases Augsburg (Germany) surveys between 1984 and 1995, and who were free of diabetes at baseline. Compared to individuals with normal blood pressure, the hazard ratios of incident diabetes were associated with an optimal blood pressure and high normal blood pressure, and hypertension were 0. A study titled "Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis" appeared in the Journal of the American Medical Association in 2015. The investigators reported that each 10 mmHg of lower systolic blood pressure was associated with a significantly lower risk of mortality; absolute risk reduction in events per 1000 patient-years and cardiovascular events; and absolute risk reduction in coronary heart disease, stroke, and retinopathy. The authors concluded that in patients with Type 2 diabetes, lowering blood pressure is associated with decreased mortality and other clinical outcomes, with lower risk reduction observed among those with baseline blood pressure of 140 mmHg and higher (Emdin, Rahimi, Neal et al. The standard blood pressure target currently recommended is less than 130/80 mmHg for the general population of people with elevated blood pressure. However, another study published in Cochrane Database of Systematic Reviews, concerning blood pressure targets for people with Type 2 diabetes, aimed to determine whether achieving targets lower than the standard target will reduce mortality and morbidity in those with elevated blood pressure and diabetes. The authors concluded that at the present time, evidence from randomized trials does not support blood pressure targets lower than the standard targets in people with elevated blood pressure and diabetes (Arguedas, Leiva, and Wright. When selecting a blood pressure monitor, it is essential to determine that the cuff fits the arm. It is also recommended that the home user bring the instrument to the next appointment with a healthcare provider to calibrate it with a conventional aneroid sphygmomanometer. The arm with the cuff should be supported on a flat surface (such as a table) with the upper part of the arm at heart level. An illustration of blood pressure self-measurement positioning with a self-inflatable cuff can be found online. If the monitor has built-in memory to store readings, it can be taken to the next appointment with a healthcare provider. Also, several studies have shown that it is normal to have blood pressure variation between the right and the left arm: A difference of 10 mmHg, or less, is considered normal and is not a cause for concern. In November 2017, health authorities lowered the cutoff range to 130/80, as noted above. Diabetic retinopathy was classified as nondiabetic retinopathy, nonproliferative diabetic retinopathy, and proliferative diabetic retinopathy stages. It can be done at home and, while it may not be quite as accurate as if it were done in the office of a healthcare provider, if sufficient care is taken, it may be quite adequate. First, the person lies down for about 10 min to equalize the effect of gravity on blood pressure in the arms and legs. Then, a blood pressure cuff is used to measure blood pressure in the arms and at the ankles. Inflation is allowed to cycle, and when it ends, the blood pressure reading is recorded. The higher of two systolic readings of the left and right arm brachial artery is generally used in the assessment. In participants with an abnormal automatic index, correlations with Doppler indexes were good in both legs. In terms of detecting an abnormal index in a routine preventive examination, the automatic method had good sensitivity (92%), specificity (98%), positive predictive value (86%), negative predictive value (99%), and accuracy (97%) compared with the Doppler method. Good results were obtained in participants with an abnormal index with regard to agreement and concordance with the Doppler method (Benchimol, Pillois, Benchimol et al. There are, however, concerns about the trustworthiness of the index in certain clinical conditions where, for instance, there may be significant hardening of the arteries, and in some cases, in On the Importance of Monitoring Blood Sugar and Other "Vital Signs" 159 diabetes. As previously noted, there is a strong link between Type 2 diabetes and atherosclerosis, and there is a strong link also between both atherosclerosis and Type 2 diabetes, and systemic inflammation. This is also known as the albumin-tocreatinine ratio test or the urine albumin test. Microalbuminuria is a subtle increase in the urinary excretion of the protein albumin that cannot be detected by a conventional assay. In diabetes, microalbuminuria is an early sign of diabetic kidney disease: the normal urinary albumin is less than 30 mg per 24 h, and 300 mg or more of urinary albumin per day is considered gross albuminuria. According to a report in the journal Diabetes Care, albuminuria has also been shown to predict cardiovascular outcomes in diabetic populations and that reducing it leads to reduced risk of adverse kidney and cardiovascular events (Basi, Fesler, Mimran et al. Postprandial lipidemia has come to the forefront as a result of more recent studies showing that nonfasting triglycerides predict the onset of arteriosclerotic cardiovascular disease better than fasting measurements do. Also, postprandial particle markers such as apolipoprotein B-48 (apo B-48) makes it easier and simpler to examine the postprandial phenomenon. The diabetic patients without vascular disease had apo B-48 concentrations similar to that of the controls. The prevalence of elevated serum cholesterol is not increased in patients with diabetes, but mortality from coronary heart disease increases exponentially as a function of serum cholesterol levels. The aim of a study of dyslipidemia reported in the Indian Journal of Pharmaceutical Science was to determine the lipid profile of Type 2 diabetic and age-/gender-matched healthy participants, and its association to fasting plasma glucose in clinically diagnosed diabetic participants.
Generic tastylia 10mg with visa
Mechanistic investigations of the 1-deoxy-D-xylulose 5-phosphate reductoisomerase treatment integrity cheap tastylia 10mg amex. Study of 1-deoxy-D-xylulose-5-phosphate reductoisomerase: Synthesis and evaluation of fluorinated substrate analogues. The chemical mechanism of D-1-deoxyxylulose-5-phosphate reductoisomerase from Escherichia coli. Mechanistic studies with 2-C-methyl-D-erythritol 4-phosphate synthase from Escherichia coli. Stereochemistry of the reduction step mediated by recombinant 1-deoxy-D-xylulose 5-phosphate isomeroreductase. Stereochemical course of the reduction step in the formation of 2-C-methylerythritol from the terpene precursor 1-deoxyxylulose in higher plants. Synthesis of (3R,4S)-3,4-dihydroxy-5-oxohexylphosphonic acid, an isosteric analogue of 1-deoxy-D-xylulose 5-phosphate, the substrate of the 1-deoxy-D-xylulose 5-phosphate reducto-isomerase. Synthesis and evaluation of 1-deoxy-D-xylulose 5-phosphate analogues as chelation-based inhibitors of methylerythritol phosphate synthase. Substrate analogs for the investigation of deoxyxylulose 5-phosphate reductoisomerase inhibition: synthesis and evaluation. Synthesis and antimalarial evaluation of prodrugs of novel fosmidomycin analogues. Short-course regimens of artesunate-fosmidomycin in treatment of uncomplicated Plasmodium falciparum malaria. Fosmidomycin plus clindomycin for treatment of pediatric patients aged 1 to 14 years with Plasmodium falciparum malaria. Fosmidomycin-clindamycin for Plasmodium falciparum infections in African children. Inadequate efficacy of a new formulation of fosmidomycin-clindamycin combination in Mozambican children less than three years old with uncomplicated Plasmodium falciparum malaria. Randomized controlled trial of fosmiomycin-clindamycin versus sulfadoxine-pyrimethamine in the treatment of Plasmodium falciparum malaria. Assessment of the pharmacokinetics and dynamics of two combination regimens of fosmidomycin-clindamycin in patients with acute uncomplicated falciparum malaria. Pharmacokinetics and pharmacodynamics of fosmidomycin monotherapy and combination therapy with clindamycin in the treatment of multidrug resistant falciparum malaria. Efficacy and safety of fosmidomycin-piperaquine as nonartemisinin-based combination therapy for uncomplicated falciparum malaria: a single-arm-age de-escalation proof-of-concept study in Gabon. Arylmethyl substituted derivatives of fosmidomycin: synthesis and antimalarial activity. Apicoplast isoprenoid precursor synthesis and the molecular basis of fosmidomycin resistance in Toxoplasma gondiii. Fosmidomycin uptake into Plasmodium and Babesiainfected erythrocytes is facilitated by parasite-induced new permeability pathways. Structural basis of fosmidomycin action revealed by the complex with 2-C-methyl-D-erythritol 4-phosphate synthase (IspC). Structures of Mycobacterium tuberculosis 1-deoxy-D-xylulose-5-phosphate reductoisomerase provide new insights into catalysis. Crystallographic structures of two biphosphonate: 1-Deoxyxylulose5-phosphate reductoisomerase complexes. Design, synthesis, and X-ray crystallographic studies of -aryl substituted fosmidomycin analogues as inhibitors of Mycobacterium tuberculosis 1-deoxyD-xylulose 5-phosphate reductoisomerase. Binding modes of reverse fosmidomycin analogs toward the antimalarial target IspC. Synthesis and biological evaluation of cyclopropyl analogues of fosmidomycin as potent Plasmodium falciparum growth inhibitors. Novel deoxyxylulosephosphate-reductoisomerase inhibitors: fosmidomycin derivatives with spacious acyl residues. A fragment-based approach to understanding inhibition of 1-deoxy-D-xylulose-5-phosphate reductoisomerase. Isoprenoid biosynthesis as a target for antibacterial and antiparasitic drugs: phosphonohydroxamic acids as inhibitors of deoxyxylulose phosphate. Coordination chemistry based approach to lipophilic inhibitors of 1-deoxy-D-xylulose-5-phosphate reductoisomerase. Synthesis of -aryl-substituted and conformationally restricted fosmidomycin analogues as promising antimalarials. Isoprenoid biosynthesis via the methylerythritol phosphate pathways: Structural variations around phosphonate anchor and spacer of fosmidomycin, a potent inhibitor of deoxyxylulose phosphate reductoisomerase. Synthesis of -substituted fosmidomycin analogues as highly potent Plasmodium falciparum growth inhibitors. Synthesis and antiplasmodial activity of highly active reverse analogues of the antimalarial drug candidate fosmidomycin. Synthesis and antimalarial activity of N-benzylated (N-arylcarbamoyl)alkylphosphonic acid derivatives. Synthetic fosmidomycin analogues with altered chelating moieties do not inhibit 1-deoxy-D-xylulose 5-phosphate reductoisomerase or Plasmodium falciparum growth in vitro. Acyloxybenzyl and alkoxyalkyl prodrugs of a fosmidomycin surrogate as antimalarial and antitubercular agents. Amino acid based prodrugs of a fosmidomycin surrogate as antimalarial and antitubercular agents. Effects of bisphosphonates on the growth of Entamoeba histolytica and Plasmodium species in vitro and in vivo. Bisphosphonates inhibit the growth of Trypanosoma brucei, Trypanosoma cruzi, Leishmania donovani, Toxoplasma gondii, and Plasmodium falciparum: a potential route to chemotherapy. Plasmodium IspD (2-C-methyl-D-erythritol 4-phosphate cytidyltransferase), an essential and druggable antimalarial target. Structure of 4-diphosphocytidyl-2-C-methylerythritol synthetase involved in mevalonate-independent isoprenoid biosynthesis. A second target of the antimalarial and antibacterial agent fosmidomycin revealed by cellular metabolic profiling. Antiapicoplast and gametocytocidal screening to identify the mechanisms of action of compounds within the malaria box. Synthesis and evaluation of fluoroalkyl phosphonyl analogues of 2-C-methylerythritol phosphate as substrates and inhibitors of IspD from human pathogens. Nonphosphate inhibitors of IspE protein, a kinase in the nonmevalonate pathway for isoprenoid biosynthesis and a potential target for antimalarial therapy. Identification of 1,3-diiminoisoindoline carbohydrazides as potential antimalarial candidates. Thiazolpyrimidine inhibitors of 2-methylerythritol 2,4-cyclodiphosphate synthase (IspF) from Mycobacterium tuberculosis and Plasmodium falciparum. Aryl bis-sulfonamide inhibitors of IspF from Arabidopsis thaliana and Plasmodium falciparum. Recombinant expression and biochemical characterization of the unique elongating -ketoacyl-acyl carrier protein synthase involved in fatty acid biosynthesis of Plasmodium falciparum using natural and artificial substrates. Lipid synthesis in protozoan parasites: a comparison between kinetoplastids and apicomplexans. Nuclear-encoded proteins target to the plastid in Toxoplasma gondii and Plasmodium falciparum. Cofactor-induced conformational rearrangements establish a catalytically competent active site and a proton relay conduit in FabG. Inhibition of Plasmodium falciparum fatty acid biosynthesis: Evaluation of FabG, FabZ, and FabI as drug targets for flavonoids. Crystal structure of dimeric FabZ of Plasmodium falciparum reveals conformational switching to active hexamers by peptide flips. Packing and loop-structure variation in non-isomorphous crystals of FabZ from Plasmodium falciparum. Identification, characterization, and inhibition of Plasmodium falciparum -hydroxy-acyl carrier protein dehydratase (FabZ). Structural elucidation of the specificity of the antibacterial agent triclosan for malarial enoyl acyl carrier protein reductase.
Buy tastylia online pills
Evaluation of the topical anti-inflammatory activity of ginger dry extracts from solutions and plasters 9 medications that can cause heartburn tastylia 20 mg for sale. The effect of ginger powder supplementation on insulin resistance and glycemic indices in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trial. Effect of ginger powder supplementation on nitric oxide and C-reactive protein in elderly knee osteoarthritis patients: a 12-week double-blind randomized placebo-controlled clinical trial. Nagao T, Meguro S, Hase T, Otsuka K, Komikado M, Tokimitsu I, Yamamoto T, and K Yamamoto. A catechin-rich beverage improves obesity and blood glucose control in patients with type 2 diabetes. Standardized capsule of Camellia sinensis lowers cardiovascular risk factors in a randomized, double-blind, placebo-controlled study. Hypoglycemic and antidiabetic effect of Pleurotus sajor-caju aqueous extract in normal and streptozotocin-induced diabetic rats. Protection against the diabetogenic effect of feeding tert-butylhydroquinone to rats prior to the administration of streptozotocin. Dietary reference intakes: vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Final report on the safety assessment of capsicum annuum extract, capsicum annuum fruit extract, capsicum annuum resin, capsicum annuum fruit powder, capsicum frutescens fruit, capsicum frutescens fruit extract, capsicum frutescens resin, and capsaicin. Anti-proliferative and potential anti-diabetic effects of phenolic-rich extracts from edible marine algae. In vitro and cellular antioxidant activities of seaweed extracts prepared from five brown seaweeds harvested in spring from the west coast of Ireland. Inhibitory effect of polyphenol-rich extracts of jute leaf (Corchorus olitorius) on key enzyme linked to type 2 diabetes (-amylase and -glucosidase) and hypertension (angiotensin I converting) in vitro. Organic nitrates and nitrate resistance in diabetes: the role of vascular dysfunction and oxidative stress with emphasis on antioxidant properties of pentaerithrityl tetranitrate. Ambivalent role of gallated catechins in glucose tolerance in humans: a novel insight into non-absorbable gallated catechinderived inhibitors of glucose absorption. Hibiscus sabdariffa Linnaeus (Malvaceae), curcumin and resveratrol as alternative medicinal agents against metabolic syndrome. Influence of betalin-rich extracts on reduction of discomfort associated with osteoarthritis. Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. Relative inhibition of lipid peroxidation, cyclooxygenase enzymes, and human tumor cell proliferation by natural food colors. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Does elevated arginase activity contribute to diabetes-induced endothelial dysfunction The Journal of Federation of American Societies for Experimental Biology, 20 (Meeting Abstract Supplement): A1125. Rumpler W, Seale J, Clevidence B, Judd J, Wiley E, Yamamoto S, Komatsu T, Sawaki T, Ishikura Y, and K Hosoda. Effects of green tea consumption on inflammation, insulin resistance and pulse wave velocity in type 2 diabetes patients. Linkage of inflammation and oxidative stress via release of glutathionylated peroxiredoxin-2, which acts as a danger signal. Comparative effects of beta-carotene and fucoxanthin on retinol deficiency induced oxidative stress in rats. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. The effect of ginger (Zingiber officinale) on glycemic markers in patients with type 2 diabetes. Acute myocardial infarction and coronary vasospasm associated with the ingestion of cayenne pepper pills in a 25-year-old male. Effect of oral curcumin administration on serum peroxides and cholesterol levels in human volunteers. Anti-inflammatory effects of red pepper (Capsicum baccatum) on carrageenan- and antigen-induced inflammation. Total phenolic contents, chelating capacities, and radical-scavenging properties of black peppercorn, nutmeg, rosehip, cinnamon and oregano leaf. Effect of turmeric and curcumin on oxidative stress and antioxidant enzymes in streptozotocin-induced diabetic rat. Endothelial dysfunction in diabetes mellitus: molecular mechanisms and clinical implications. Betanin attenuates oxidative stress and inflammatory reaction in kidney of paraquat-treated rat. Increased resistance to oxidation of betalain-enriched human low density lipoproteins. Sugar beet fiber in formula diet reduces postprandial blood glucose, serum insulin and serum hydroxyproline. Tian C, Ye X, Zhang R, Long J, Ren W, Ding S, Liao D, Jin X, Wu H, Xu S, and C Ying. Green tea polyphenols as an anti-oxidant and antiinflammatory agent for cardiovascular protection. Cinnamon supplementation does not improve glycemic control in postmenopausal type 2 diabetes patients. Inactivation of lipoxygenase and cyclooxygenase by natural betalains and semi-synthetic analogues. Molecular and physiologic actions of insulin related to production of nitric oxide in vascular endothelium. Effects of a beetroot juice with high neobetanin content on the early-phase insulin response in healthy volunteers. Relationship among habitual tea consumption, percent body fat, and body fat distribution. Antidiabetic and antioxidant activities of eight medicinal mushroom species from China. Yuan G, Zhou L, Tang J, Yang Y, Gu W, Li F, Hong J, Gu Y, Li X, Ning G, and M Chen. Effects of heating, aerial exposure and illumination on stability of fucoxanthin in canola oil. In vitro effects of beetroot juice and chips on oxidative metabolism and apoptosis in neutrophils from obese individuals. It is native to northern China where it was widely cultivated to feed the "worms" that are used in the production of silk. The "silkworm" is actually the larva of the domesticated silk moth, Bombyx mori (see Section 5. The tree is generally known as the Chinese mulberry (Sang Ye-), although it is now widely cultivated in North America, Mexico, Argentina, Australia, and Central Asia. The journal Archives of Pharmacal Research reports that nine flavonoids have been isolated from the leaves of M. The journal European Food Research and Technology reported on the total phenolic content, phenolic acids, radical scavenging activity, and antiproliferative properties of different parts of mulberry (M. The highest phenolic content was found in methanol extracts of mulberry root, followed by leaves, branches, and fruit (Chon, Kim, Park et al. The root bark of the mulberry contains stilbenoids (resveratrol is a stilbenoid) that have antimicrobial, cytotoxic, anti-inflammatory, and lipid-lowering properties (Chan, Lye, and Wong. Moralbanone, along with seven known compounds, kuwanon S, mulberroside C, cyclomorusin, eudraflavone B hydroperoxide, oxydihydromorusin, leachianone G, and -acetyl-amyrin were isolated from the root bark of M.
Generic tastylia 20mg free shipping
Because glucagon has actions opposite to those of insulin medicine 6 clinic proven tastylia 20 mg, it therefore functions to maintain plasma glucose levels between meals. However, unlike insulin, glucagon action is probably mostly in the liver, with limited effects in other tissues. It stimulates liver amino acid uptake, gluconeogenesis, and glucose release, and inhibits glycolysis and fatty acid synthesis. In general, actions of glucagon are mediated by increased phosphorylation of existing enzymes. Prolonged stimulation by glucagon may have some effects on gene transcription, usually in the opposite direction from that of insulin. It is released from the -cells (delta-cells) under control of the same stimuli that result in insulin release and that act primarily as a regulator of insulin release, preventing insulin levels from rising too rapidly. It may also have an endocrine role as an inhibitor of nutrient absorption in the gut. As one rises, it inhibits the release of the other, Chronic Hyperglycemia-A Primer 13 and vice versa: Simply put, glucagon promotes serum glucose, whereas insulin inhibits it. First, our pancreas produces less insulin as we age: the journal Seminars in Nephrology reported the following (we paraphrase): As we age, we experience increased incidence of hypertension, Type 2 diabetes, and coronary heart disease. However, it is not known whether this dysfunction is an inevitable consequence of "biological aging," or the result of environmental or lifestyle variables such as obesity, or physical inactivity common in the aging. All of these modifiable factors have been shown to cause increased insulin resistance, and they are risk factors for development of metabolic syndrome. Insulin secretion, on the other hand, declines with age even after adjustments for differences in adiposity, fat distribution, and physical activity. This may be responsible for the glucose intolerance in the aging even after improvements have been made in their lifestyle factors (Muller, Elahi, Tobin et al. The ratio of insulin secretion to insulin resistance is termed the disposition index. Insulin response is estimated as the change in insulin divided by the change in glucose from 0 to 30 min: It is a measure of the sensitivity to glucose of the -cells in the pancreas (Lorenzo, Wagenknecht, Rewers et al. The relation between -cell responsivity and insulin sensitivity is assumed to be constant (Cobelli, Toffolo, Man et al. In a normal individual, impaired insulin sensitivity increases pancreatic -cell responsivity, whereas in someone with impaired tolerance, this does not occur. This tells us that in Type 2 diabetes, insulin secretion cannot keep up with declining insulin sensitivity (Cobelli, Toffolo, Man et al. Actually, there is a disconnect: A report in the journal Diabetologia informs us that glucagon suppression by both elevated blood sugar and elevated serum insulin is not different in young and older people; the metabolic clearance rate of glucagon is similar in young and older individuals or participants, but liver sensitivity to increments in plasma glucagon is increased in older people (Gosmanov, Adair Gosmanov, Gerich 2011; Simonson, and DeFronzo. So far as can be determined, the term "pancreas" first appears in the works of Rufus of Ephesus, a first-century Greek doctor, who was probably the first to use this term to refer to this organ. However, no function was attributed to the pancreas, and he believed that the pancreas was only an extension of the digestive system. In pre-Elizabethan English, "wonderful" was akin to "surprising" rather than "enjoyable. In 1889, they surgically removed the pancreas of dogs and discovered serendipitously that they had induced the body wasting process of diabetes. It was Minkowski who performed the operation and made the crucial link to recognize that the symptoms of the treated dogs were due to diabetes. Thus, they were able to conclude that the pancreas contained regulators of blood sugar. The disease, diabetes mellitus, results from a failure of the body to produce or to respond properly to the hormone insulin, thus resulting in abnormal metabolism of carbohydrates, and elevated levels of glucose in the blood and in urine. Type 2 diabetes begins with insulin resistance, a condition where body cells fail to respond properly to insulin. With the progress of the diseases, there may eventually also be a lack of insulin. This results in abnormally high blood glucose concentrations, and generalized body wasting. The destruction of -cells is less pronounced than in Type 1 diabetes and, instead, there is an accumulation of aggregates of certain proteins, amyloid, in the pancreatic islets that become folded into a shape that allows many to stick together, forming fibrils. Type 2 diabetes is characterized by high rates of secretion of glucagon into the blood, the rates unaffected by, and unresponsive to , the concentration of glucose in the blood. Glucagon is a hormone, produced by -cells of the pancreas that raises the concentration of glucose in the bloodstream. History Footnote 2: Paul Langerhans, Frederick Grant Banting, and Charles Herbert Best In 1869, Paul Langerhans published "Contributions to microscopic anatomy of the pancreas. Oskar Minkowski and Josef von Mering had shown that removing the pancreas of a dog caused it to develop diabetes. Subsequently, Eugene Lindsay Opie found that there were morphological changes in pancreatic islet cells of patients who died of diabetes. He suspected that pancreatic islets are the source of a hormone that prevents diabetes. Edward Albert Sharpey-Schafer, a British physiologist, called this hormone insulin. In 1921, Frederick Grant Banting and Charles Herbert Best began experiments that led to the discovery of the function of insulin: They initially extracted it from dog and other animal pancreas and found that the extract lowered glucose levels in dogs that had induced diabetes. Eventually, a successful method of extraction was developed that enabled large amounts of highly purified insulin to be obtained from ox pancreas, and this made it possible for a clinical study to commence in January 1922. The study was a great success and confirmed the effectiveness of insulin in treating diabetes. In 1922, Banting, Best, and Collip, the latter purified the extract, were granted patent rights for producing insulin, and they sold those rights to the University of Toronto for one dollar. In 1923, Frederick Grant Banting and John James Rickard Macleod, in whose laboratory insulin was first extracted, were awarded the Nobel Prize and Banting gave half of his prize money to Best, while Macleod gave half of his to Collip. In fact, intravenous infusion of glucose would elicit a smaller rise in insulin release than would oral administration of an equivalent amount of glucose. The increase in insulin levels caused by actually eating food is thought to be due to gastrointestinal peptide hormones released in response to food absorption and they potentiate the glucose effect on insulin release. Consuming a meal rich in carbohydrate causes insulin levels to rise and glucagon levels to fall. The decrease of glucagon is due to inhibition of its release by insulin and to the elevation in plasma glucose. Glucagon levels also rise because glucagon release is likewise stimulated by amino acids. Were the release of insulin caused by amino acids unopposed by a corresponding increase in release of glucagon, it would result in hypoglycemia because little glucose is being made available. Because the pancreas has intestinal peptide hormones that respond to the types of nutrients in the meal, it can regulate the disposal of the nutrients without an undue change in plasma glucose. It would be difficult to attain this adjustment in pancreatic hormone release by the injections of insulin, and that is part of the problem faced by individuals with Type 1 diabetes. Hence, insulin and glucagon work synergistically to keep blood glucose concentrations normal. The muscle plays an important role in absorbing about 80% to 95% of sudden increases in plasma glucose levels, such as those observed during a rich carbohydrate meal. During exercise, the muscle becomes more sensitive to insulin action and therefore retains the ability to import glucose from circulation despite the exercise-induced reduction in insulin levels. It is reported that barely 39% of adults with diabetes are physically active compared with 58% of nondiabetic American adults (Morrato, Hill, Wyatt et al. Thus, for most people with Type 2 diabetes, exercise is recommended for diabetes management and can be undertaken safely and effectively. Structured interventions combining physical activity and modest weight loss have been shown to lower the risk of Type 2 diabetes by up to 58% in high-risk populations.
Cheap tastylia 20 mg with mastercard
In the treated patients medications recalled by the fda generic tastylia 20 mg fast delivery, the cellular surface thiol status in peripheral blood lymphocytes was restored. The authors concluded that silimarin reduces blood glucose levels by mechanisms that are independent of insulin production (Huseini, Larijani, Heshmat et al. The aim of a study published in the journal Clinical Pharmacology was to determine the benefits in Type 2 diabetes of adding a P-glycoprotein antagonist (silymarin), to a product containing Berberis aristata extract. Patients with Type 2 diabetes with suboptimal glycemic control were treated with diet, hypoglycemic drugs, and, in cases of concomitant alterations of the lipid profile, hypolipidemic agents. The patients received an add-on therapy consisting of either a standardized extract of B. The investigators concluded that the combination of berberine plus silymarin proved to be more effective than berberine alone in reducing HbA1c, when administered at the same dose, and in the form of standardized extracts, to Type 2 diabetic patients (Di Pierro, Putignano, Villanova et al. Type 2 diabetes patients 25 to 50 years old, and on stable medication, were recruited from the Iranian Diabetes Society and endocrinology clinics in East Azarbayjan (Tabriz, Iran). They were assigned to two groups: Patients in the silymarin treatment group received 140 mg, three times daily of dried extracts of S. All patients completed the study and did not report any adverse effects or symptoms from the silymarin supplementation. According to a report in the journal Antioxidants (Basel, Switzerland), silymarin contains flavonolignans (as noted earlier in this chapter, silybin is the major one). In many cases, the antioxidant properties of silymarin are considered the basis of its protective actions. Direct scavenging of free radicals and chelating free Fe++ and Cu++, mainly effective in the gut 2. Maintaining an optimal redox balance in the cell by activating a range of antioxidant enzymes and nonenzymatic antioxidants, mainly via Nrf2 activation, probably the main driving force of the antioxidant action of silymarin 4. Activating vitagenes, responsible for synthesis of protective molecules, including heat shock proteins, thioredoxin, and sirtuins 6. There were two reported events of nausea and headache, but these appeared to be unrelated to silymarin administration (Hawke, Schrieber, Soule et al. In another study, patients with chronic hepatitis C received 600 and 1200 mg/day silimarin treatment for 12 weeks. The patients reported symptoms from the gastrointestinal tract; two patients reported headache/dizziness, and one reported pruritus (Gordon, Hobbs, Bowden et al. Generally, silymarin is considered safe, even at doses as high as 13 g/day, with no interactions (at least at low concentrations, such as 10 M) with chemotherapeutic agents like vincristine or l-asparaginase. Additional studies of the safety of this botanical in diverse patient populations can be found in Kazazis, Evangelopoulos, Kollas et al. Selected Botanicals and Plant Products That Lower Blood Glucose (Continued) 281 10. It is found in the roots, rhizomes, stems, and bark of various plants including Hydrastis canadensis (goldenseal), Coptis chinensis (Coptis or goldenthread), Berberis aquifolium (Oregon grape), B. Berberine extracts and decoctions have demonstrated significant antimicrobial activity against a variety of organisms including bacteria, viruses, fungi, protozoans, helminths, and chlamydia. This report reviews the efficacy and safety of berberine in the treatment of Type 2 diabetes, hyperlipidemia, and hypertension, based on meta-analysis of available clinical data. There was no statistically significant difference between berberine and prescription oral hypoglycemic agents. An animal model study published in the American Journal of Physiology-Endocrinology and Metabolism aimed to determine the mechanism of action for berberine in vivo and in vitro. Berberine increased insulin sensitivity after 5 weeks of administration to dietary obese rats. An increase in glycolysis was observed with an increase in lactic acid production. Berberine showed no cytotoxicity, and it protected the plasma membrane in L6 myotubes in cell culture. Berberine reduces blood glucose by a number of mechanisms, for example, by reducing glucose release from glycolysis in the liver and by lowering fasting glucose, fasting insulin, and postprandial glucose. Here are further reports: A study published in the Journal of Clinical Endocrinology and Metabolism aimed to determine the efficacy and safety of berberine in the treatment of Type 2 diabetic patients with dyslipidemia. The authors concluded that berberine is effective and safe in the treatment of Type 2 diabetes and dyslipidemia (Zhang, Li, Zou et al. The journal Metabolism reported a study that aimed to determine the efficacy and safety of berberine in the treatment of Type 2 diabetic patients. One group of adult participants with newly diagnosed Type 2 diabetes was given berberine, whereas the other was given metformin (0. The hypoglycemic effect of berberine was found to be similar to that of metformin. Significant decreases observed in the berberine group were reductions in HbA1c from 9. In a second study, adult participants with poorly controlled Type 2 diabetes were given supplementary berberine in a 3-month trial. The investigators concluded that this pilot study found berberine to be a potent oral hypoglycemic agent with beneficial effects on lipid metabolism (Yin, Xing, and Ye. A report in the journal Metabolism concluded that "Berberine lowers blood glucose in type 2 diabetes patients through increasing insulin receptor expression. In the berberine-treated patients, the percentages of peripheral blood lymphocytes that express the insulin receptor gene (InsR) were significantly elevated as a result of the therapy. Liver function was improved greatly in these patients, as evidenced by meaningful reduction of the elevated liver enzymes. Selected Botanicals and Plant Products That Lower Blood Glucose (Continued) 283 the investigators confirmed the activity of berberine on the insulin receptor gene in humans and its relationship to the glucose-lowering effect, and concluded that berberine is, therefore, an ideal medicine for patients with Type 2 diabetes and that its mode of action differs from that of metformin and rosiglitazone (Zhang, Wei, Xue et al. Berberine in the treatment of Type 2 diabetes mellitus: a systemic review and meta-analysis. A study published in the European Journal of Endocrinology aimed to compare the effects of berberine to those of metformin on the metabolic features of women with polycystic ovary syndrome. One clinical source reported in the journal Metabolism that berberine 500 mg twice daily for 3 months is effective in treating diabetes (Yin, Xing, and Ye. As with most herbs, it is better to take berberine in multiple doses spread throughout the day. In one study, newborn infants exposed to berberine had elevations of bilirubin to such an extent that kernicterus developed. Kernicterus is a very rare type of brain damage that occurs in newborns with severe jaundice. If left untreated, the bilirubin can then become deposited in the brain, where it causes long-term damage. The molar displacing effect of berberine was found in vitro to be about 10-fold that of phenylbutazone, a known potent displacer of bilirubin, and about 100-fold that of papaverine, a berberine-type alkaloid. The chronic intraperitoneal administration of berberine (10 and 20 g/g) to adult rats (mixed breed of Wistar and Sprague-Dawley), once daily for 1 week, resulted in a significant decrease in mean bilirubin serum protein binding due to an in vivo displacement effect, and a persistent elevation in steadystate serum concentrations of unbound and total bilirubin, possibly due to inhibition of metabolism. The use of the herb and other traditional Chinese medicines that contain a high proportion of berberine is best avoided in jaundiced neonates and pregnant women (Chan. The European Journal of Clinical Pharmacology reported a study on healthy men, on the effects of ingesting berberine (300 mg, t. Compared to the placebo group, in the berberine-treated subjects the Tmax and T1/2 of midazolam were prolonged from 3. The oral clearance of midazolam was decreased 27%, and the phenotypic indices of 1-h midazolam/1-hydroxymidazolam increased 59%. There were no statistically significant differences in the pharmacokinetic parameters of the other probe drugs, between placebo and the berberine-treated group. While some mushrooms are quite poisonous, many have known medicinal value (Cargill. The description of the antiglycemic and the anti-inflammatory activity of certain mushroom species is given here pro forma because their use is not likely to be implemented as adjunctive treatment for diabetes-although that was the case elsewhere over the years.
Arogyapacha (Trichopus Zeylanicus). Tastylia.
- Dosing considerations for Trichopus Zeylanicus.
- Are there safety concerns?
- Improving stamina, liver disease, peptic ulcer disease, weight loss, fatigue, sexual dysfunction, and improving sexual performance.
- What is Trichopus Zeylanicus?
- How does Trichopus Zeylanicus work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97134
Cheap tastylia 20mg with mastercard
Activation of protein kinase C is a third mechanism whereby hyperglycemia can increase platelet reactivity (Assert medicine woman cast tastylia 20mg discount, Scherk, Bumbure et al. Although hyperglycemia is the sine qua non of diabetes, abnormalities of lipid metabolism are uniformly observed as well. Thus, both hyperglycemia and hypertriglyceridemia increase platelet reactivity in persons with diabetes. During this interval, hyperinsulinemia compensates for insulin resistance and fasting hyperglycemia is not evident. Apoptosis of pancreatic -cells leads to a relative, and ultimately absolute, deficiency of insulin. Both insulin resistance and insulin deficiency can alter platelet reactivity (Schneider. Thus, resistance by the platelet to the effects of insulin (relative insulin deficiency) or absolute deficiency of insulin attenuates insulin-mediated antagonism of platelet activation and thereby increases platelet reactivity. Obese persons who are insulin resistant exhibit increased activation of platelets. Decreased insulin resistance achieved by weight loss, or treatment with pioglitazone (without weight loss), reduced the concentrations of these markers (Basili, Pacini, Guagnano et al. A study published in the journal Thrombosis Research quantified the concentration of plateletderived microparticles in blood, which are released during the activation of platelets. Similar to results in the previous study, the concentration of microparticles was decreased after weight reduction (Murakami, Horigome, Tanaka et al. Thus, insulin resistance appears to increase the activation of platelets, consistent with increased platelet reactivity. Persons with Type 2 diabetes exhibit progressive deficiency of insulin due to pancreatic -cell apoptosis. Accordingly, the relative deficiency of insulin imparted by insulin resistance is magnified by the superimposition of insulin deficiency. Platelet reactivity that is increased in obese persons manifesting insulin resistance will be greater when Type 2 diabetes is also manifest and accompanied by absolute deficiency of insulin. Thus, resistance of the platelet to the effects of these agents promotes increased platelet reactivity. Accordingly, insulin resistance attenuates tonic antagonism of platelet activation and thereby increases platelet reactivity (Schneider. Superoxide has been shown to increase platelet reactivity (Handin, Karabin, and Boxer. Superoxide may increase platelet reactivity by enhancing intraplatelet release of calcium after activation (Schaeffer, Wascher, Kostner et al. Accordingly, oxidative stress that accompanies diabetes promotes greater platelet reactivity through direct effects on platelets and by inducing endothelial dysfunction. An additional mechanism by which inflammation can increase platelet reactivity is by increasing expression of proteins that participate in the activation of platelets. Engagement of this receptor on platelets by immune complexes triggers intracellular signaling events that lead to platelet activation and aggregation. Importantly, these events occur in vivo, particularly in response to pathological immune complexes, and engagement of this receptor on platelets has been causally linked to pathology (Qiao, Al-Tamimi, Baker et al. Thus, the inflammation that accompanies diabetes contributes to increased platelet reactivity that, in turn, contributes to greater inflammation (Schneider. The increased blood viscosity adversely affects the microcirculation, leading to microangiopathy (Cho, Michael, Mooney et al. An analysis of this phenomenon was detailed in a study published in the journal Cardiovascular Diabetology. These results are comparable to previously published results (Lipinski, and Pretorius. Atomic force measurement indicated that erythrocytes from patients suffering from diabetes are smaller, with a reduced concave depth. A decrease of roughness by about half was noted in the erythrocytes of diabetic patients. In the current analysis, a difference in diameter, height, and concave depth between cells from the healthy and diabetic individuals was seen (Table 1, ibid). The selection of the size of the spectral domains is guided by the structural properties of the erythrocyte membrane (Moroz, Chernysh, Kozlova et al. The first-order surface of the erythrocyte membrane represents the accepted undulate nature of the erythrocyte membrane relating to the macroparameters of the cell. A decrease in roughness measurements in the third-order surface indicates superficial protein structure rearrangement. However, the ultrastructural changes seen in this study are not visible using a traditional light microscope. Hyperglycemia Impairs the Functions of Blood 111 Red cell exposure to high glucose concentrations in vitro is often employed as a model for understanding erythrocyte modifications in diabetes. The journal Redox Biology reported a study that aimed to compare alterations in various red cell parameters, in this type of experiment, to differentiate between those affected by glycoxidation and those affected by energy imbalance. It was found that high glucose concentrations intensified lipid peroxidation and loss of activity of the erythrocyte enzymes glutathione S-transferase and glutathione reductase. These results point to the necessity of careful interpretation of data obtained in experiments, where erythrocytes are subject to treatment with high glucose concentrations in vitro (Viskupicova, Blaskovic, Galiniak et al. Thereafter, plasma membranes were prepared and enzymatic activity, membrane fluidity, and lipid peroxidation were evaluated. In this case, the effect of diabetes appears only during aging (Mazzanti, Faloia, Rabini et al. Human health and disease-indeed life span-are intimately tied to ordinary cellular recycling as body cells age and are replaced. Type 2 diabetes has all the ingredients necessary for more rapidly abbreviating telomeres, thus shortening life span: chronic inflammation and the accompanying unopposed free radical load said to contribute to cardiovascular and heart disease are more than up to the task. Over 15 years of follow-up, 44 out of 606 participants, free of diabetes at baseline, developed incident Type 2 diabetes. In a random-effects meta-analysis of three prospective cohort studies involving 6991 participants and 2011 incident Type 2 diabetes events, the pooled relative risk was 1. The authors concluded that low leukocyte telomere relative length is independently associated with the risk of incident Type 2 diabetes (Willeit, Raschenberger, Heydon et al. A study published in the journal Experimental Biology and Medicine (Maywood) compared leukocyte telomere length and fasting, or post-load glucose levels, in persons who do not receive glucose-lowering treatment. Leukocyte telomere length was measured by the standardized method of quantitative monochrome multiplex polymerase chain reaction in real time. The 2-h post-load plasma glucose levels demonstrated an inverse correlation with leukocyte telomere length, whereas no association between fasting plasma glucose and leukocyte telomere length was found. Waist circumference and systolic blood pressure were inversely related to leukocyte telomere length in men. Oral glucose tolerance test result-based glycemic categories did not show differences between mean leukocyte telomere length in categories of normal fasting plasma glucose and 2-h post-load plasma glucose, diabetes, and impaired fasting glucose/tolerance levels. After the adjustment for age, gender, waist circumference, systolic blood pressure, and fasting plasma glucose, the investigators concluded that 2-h post-load plasma glucose, but not fasting plasma glucose, is inversely related to leukocyte telomere length (Khalangot, Krasnienkov, Vaiserman et al. There is ample evidence that prematurely short telomeres reflect unopposed free radical damage to cell structures, but the role of free radicals in etiology of disease remains to be detailed. This is also clear in the following study published in the International Journal of Cardiology, titled "Telomere length, antioxidant status and incidence of ischaemic heart disease in type 2 diabetes. An accelerated process of vascular aging induced by an increased oxidative stress exposure is suggested as the pathway accounting for this association. However, no studies have explored the relationship between markers of vascular aging, measures of oxidative stress, and risk of ischemic heart disease in Type 2 diabetes. They therefore undertook to determine the association between plasma antioxidant status, marker of cellular aging, that is, leukocyte telomere length, and 10 years risk of ischemic heart disease in patients with Type 2 diabetes. It was found that at baseline, total antioxidant status was associated with leukocyte telomere length.
Buy tastylia 20mg cheap
Therefore medications similar to abilify buy tastylia 20 mg without prescription, the authors proposed to determine the prevalence of undiagnosed hypothyroidism in patients with diabetes and the influence of antidiabetes drugs. In normal circumstances, and baring tangible medical evidence of even minimal thyroid dysfunction, it could simply be inadequate dietary intake of iodine. However, as shown above, there is a link between Type 2 diabetes and thyroid dysfunction, and it is not clear which "causes" which: Does thyroid dysfunction contribute to hyperglycemia, or does hyperglycemia contribute to thyroid dysfunction However, as noted above, because of the higher incidence of thyroid dysfunction in people with Type 2 diabetes, it might be wise to try to find out if there is low thyroid function if one suffers from diabetes. Basal metabolic rate is the rate at which the body uses energy while at rest to keep vital functions going, such as breathing and keeping warm. Assuming that one is not on medication(s) that would directly affect these measures, consistently low body temperature (below 98. Using an ear thermometer such as the Braun Thermoscan Ear Thermometer, for example, is the quickest and simplest way to do that. The second and third days of the menstrual cycle are when the most accurate/reliable basal body temperature can be obtained. The healthy adult body should hold about 15 to 20 mg of iodine, and 70% to 80% is stored in the thyroid gland. The body conserves only about 10% to 20% of iodine consumed in daily diet; the rest is excreted from the body. Therefore, supplementing dietary iodine is not invariably medically sound, so it should not be undertaken without express direction by and with supervision of a qualified healthcare provider, as there may be contraindication. Furthermore, there may be other causes of lower body core temperature and depressed metabolism that need to be detected and some, perhaps, can be treated. The basal metabolic rate decreases almost linearly with age since skeletal musculature, which consumes the largest part of energy in the normal human body, decreases and the percentage of fat tissue rises. It is shown that the decrease in muscle mass, relative to total body mass, may be wholly responsible for the age-related decreases in basal metabolic rate (Shimokata, and Kuzuya. A study published in the journal Gerontology reports that the body temperature of older men and women is lower than that of younger people. Another study is that reported in the Journal of Clinical Nursing aimed to determine whether body temperature changes in the elderly. The biological inability to create sufficient core body heat could be linked to obesity. According to a study reported in the journal Chronobiology International, there is "Evidence of a diurnal thermogenic handicap in obesity. In other words, the reduced ability of obese people to spend energy as heat, compared to lean individuals, could result in long-term weight gain of about 4. Keeping that in mind, and assuming that supplementation with dietary iodine is safe, success should be seen in just a few days in the form of normalizing basal body temperature. Supplementing the diet with iodine, described in a later chapter of this book, has been found effective where the cause is iodine deficiency, but one needs to be careful not to take too much of it, too quickly, for that is not good for the thyroid either: too much iodine can also result in hyperthyroidism. This relationship has been detailed in a previous chapter but elements of it are reiterated here because they are relevant to understanding the testing/ monitoring devices that are available. Type 2 diabetes is associated with excessively low (meaning acidic) urine pH, which increases the risk for formation of uric acid kidney stones (nephrolithiasis). A study published in the Clinical Journal of the American Society of Nephrology reports that the overly acidic urine in patients with Type 2 diabetes persists even after controlling for dietary factors, body size, and age. The lower pH is due to a combination of greater net acid secretion and lower use of ammonia buffers in patients with diabetes, which predisposes them to uric acid stone formation (Maalouf, Cameron, Moe et al. Kidney stones are bits of grit formed from minerals in the kidneys or the bladder; they can be terribly painful, block urine flow, and damage the kidneys. Many start out small, like grains of sand; they may hurt, but they will pass by themselves. People with diabetes have higher rates of both, and much higher rates for the uric acid kind, because their urine tends to be more acidic. One study at the Mayo Clinic followed 3500 patients, for 20 years, and concluded that those with diabetes developed 40% more uric acid kidney stones than those without diabetes. The low pH has also been implicated in metabolic syndrome (Maalouf, Cameron, Moe et al. The American Society of Nephrology reports that insulin resistance has something to do with it because high levels of insulin in the blood are associated with acid urine (Li, Klett, Littleton et al. The body makes buffers, of course, such as ammonia, to neutralize the acid, but insulin resistance seems to lower the production of ammonia, and, adding to that, there is evidence of involvement of the liver. It is reported in the World Journal of Gastroenterology, that perhaps as many as 30% of patients with cirrhosis have diabetes. The article suggests that perhaps Type 2 diabetes, in the absence of obesity and hypertriglyceridemia, may be a risk factor for chronic liver disease (Garcia-Compean, Jaquez-Quintana, Gonzalez-Gonzalez et al. The journal European Urology featured a study aimed to determine what associations exist among the presence and severity of Type 2 diabetes, glycemic control and insulin resistance, and kidney stone disease. The study consisted of an analysis of all adult participants in the 2007 to 2010 National Health and Nutrition Examination Survey. Insulin resistance was estimated using fasting plasma insulin levels and the homeostasis model assessment of insulin resistance definition. When adjusting for patient factors, a history of Type 2 diabetes, the use of insulin, fasting plasma insulin, and HgbA1c were significantly associated with kidney stone disease (Weinberg, Patel, Chertow et al. A study titled "Type-2 diabetes and kidney stones: impact of diabetes medications and glycemic control" was published in the journal Urology. The investigators aimed to evaluate the impact of diabetic medications and glycemic control on the urine pH, 24-h urine stone risk profile, and stone composition. Patients were further assigned to one of two groups depending on whether their diabetic medication was insulin or oral antihyperglycemic. There were no significant differences in other 24-h urine stone risk parameters or stone composition between the groups. The investigators concluded that urine pH is inversely related to HbA1c level and that insulin therapy is associated with higher urine pH than oral antihyperglycemic agents, despite higher HbA1c. This suggested that insulin may modify urine pH independent of glycemic control (Torricelli, De, Gebreselassie et al. Finally, the Journal of the American Society of Nephrology published a report titled "Type 2 diabetes increases the risk for uric acid stones. Because insulin resistance, characteristic of the metabolic syndrome and Type 2 diabetes, results in lower urine pH through impaired kidney ammonia production, and because a low urine pH is the main factor of uric acid stone formation, it was hypothesized that Type 2 diabetes should favor the formation of uric acid stones. Therefore, the distribution of the main stone components was analyzed in a series of 2464 stones from a group of patients with Type 2 diabetes and another group without Type 2 diabetes. The proportion of patients with Type 2 diabetes was significantly higher among uric acid than among calcium stone formers (27. The authors concluded that the strong link of Type 2 diabetes to uric acid stone formation should be added to the list of factors associated with insulin resistance. Therefore, the authors suggest that patients with uric acid stones, especially if overweight, should be screened for the presence of Type 2 diabetes or components of the metabolic syndrome (Daudon, Traxer, Conort et al. Having established by a sample of representative research reports that Type 2 diabetes results in a urine pH that favors kidney stone formation, it might be advisable for any diabetes sufferer to avail himself or herself of simple ways to monitor it. According to a report in the Journal of the American Society of Nephrology, Type 2 diabetes is a risk factor for stone formation (nephrolithiasis) and uric acid stones in particular. In the study cited in that publication, the aim was to identify the metabolic features that raise the risk of uric acid nephrolithiasis in patients with Type 2 diabetes. Three groups of participants were recruited in an outpatient study: those patients who have Type 2 diabetes and are not stone formers, patients who do not have diabetes and are uric acid stone formers, and healthy volunteers. Participants provided a fasting blood sample and a single 24-h urine collection for stone risk analysis. It was found that 24-h urine volume, and total uric acid, did not differ among the three groups. Patients with Type 2 diabetes and small stones had lower 24-h urine pH than healthy volunteers. On the Importance of Monitoring Blood Sugar and Other "Vital Signs" 169 Urine pH was inversely correlated with both body weight and 24-h urine sulfate in all groups.
Purchase tastylia 20 mg line
These factors are likely to influence the balance of homeostatic controls and make it difficult to generalize; nevertheless medications descriptions cheap 10mg tastylia fast delivery, research and knowledge advancement in this area brings hope that potential novel strategies for weight control could be on the horizon. Iodine-induced hyperthyroidism can also result from high iodine intakes, usually when iodine is administered to treat iodine deficiency. Studies have also shown that excessive iodine intakes can cause thyroiditis and thyroid papillary cancer. Cases of acute iodine poisoning are rare and are usually caused by doses of many grams. Acute poisoning symptoms include burning of the mouth, throat, and stomach; fever; abdominal pain; nausea; vomiting; diarrhea; weak pulse; and coma. Some people, such as those with autoimmune thyroid disease and iodine deficiency, may experience adverse effects with iodine intakes considered safe for the general population. Individuals taking these medications on a regular basis should discuss their iodine intakes with their health care providers. There are many other conditions where medications may interact adversely with iodine supplementation. Taking high doses of iodine with anti-thyroid medications can have an additive effect and could cause medical problems. Some of the health-promoting properties have been attributed to the polysaccharides produced by different varieties of mushrooms. A comprehensive review of the medicinal property of mushrooms appears in a report titled "Mushroom polysaccharides: Chemistry and antiobesity, antidiabetes, anticancer, and antibiotic properties in cells, rodents, and humans," published in the journal Foods (Friedman. More than 2000 species of edible and/or medicinal mushrooms have been identified to date. Their health-promoting properties are related to the bioactive compounds they produce including polysaccharides. Although -glucans (homopolysaccharides) are believed to be the major bioactive polysaccharides of mushrooms, other types of mushroom polysaccharides (heteropolysaccharides) also possess biological properties. The mechanisms of bioactive action involve the gut microbiota; that is, the polysaccharides act as prebiotics in the digestive system. Functional Foods Combating Effects of Hyperglycemia and Chronic Inflammation 333 11. The hypoglycemic activity seems to be associated with increased glucokinase activity and promotion of insulin secretion by the pancreas, thus increasing the utilization of glucose by peripheral tissues, inhibiting glycogen synthase kinase activity, and promoting glycogen synthesis (Friedman. According to a report in the International Journal of Medicinal Mushrooms, management of Type 2 diabetes by delaying or preventing glucose absorption, using natural products, is gaining significant attention. The most active extract was subsequently examined in vivo using the oral starch tolerance test in mice. All prepared extracts showed dose-dependent inhibition of -amylase and an increase in glucose transport across yeast cells. The extract (400 mg/kg) and acarbose normalized blood glucose levels at 180 min, when they were statistically similar to values in normal mice. It was found that the 750-mg/kg dose showed the most significant blood glucose reduction (23. In a 21-day study, treated diabetic rats showed significant improvement in fasting blood glucose, body weight, and urine sugar levels as compared to control untreated diabetic rats (Ng, Zain, Zakaria et al. However, there are studies of mushroom effects in glycemic control and related disorders that do not yield encouraging results. For instance, a study published in the journal Scientific Reports aimed to evaluate the efficacy and safety of G. Participants with Type 2 diabetes mellitus and metabolic syndrome were assigned to one of three intervention groups: (a) G. The combined intervention had no effect on any of the primary or secondary outcome measures over the course of the 16-week trial, and no overall increased risk of adverse events with either active treatment. A spice that comes from the turmeric plant contains curcumin commonly used in Asian cuisine. It has a warm, bitter taste and is frequently used to flavor or color curry powders, mustards, butters, and cheeses. There are a considerable number of experimental studies of the effects of curcumin on inflammatory conditions that would affect us, such as oxidative stress, atherosclerosis, diabetes, and more. However, due to the nature of the experimental procedures, they are often performed on animal models. The beneficial effects of curcumin are then, of necessity, extrapolated from those studies but, in all fairness, the extrapolation is not unreasonable. A study published in the Medical Science Monitor aimed to determine the protective effect of curcumin against oxidative stress in chemically stressed rats. Then, the levels of oxidative stress, and antioxidant enzymes, were determined in various tissues. Functional Foods Combating Effects of Hyperglycemia and Chronic Inflammation 335 Hyperglycemia resulted in increased lipid peroxidation and protein components in red blood cells and other tissues, and it altered antioxidant enzyme activities. The authors concluded that curcumin appears to be beneficial in preventing diabetes-induced oxidative stress in rats despite unaltered diabetic (hyperglycemic) status (Suryanarayana, Satyanarayana, Balakrishna et al. A study on human volunteers, published in the Indian Journal of Physiology and Pharmacology, in 1992, aimed to assess the effects of curcumin administration on the serum levels of cholesterol and lipid peroxides in healthy volunteers given 500 mg of curcumin per day, for 7 days. In fact, the ability of curcumin to control blood glucose levels was reported in the journal Diabetes Care in a clinical study of prediabetes. The aim of the study was to determine whether curcumin could delay development of Type 2 diabetes in a prediabetic population. Participants meeting criteria of prediabetes were assigned to receive either curcumin or placebo capsules for 9 months. The investigators concluded that a 9-month curcumin intervention in a prediabetic population significantly lowered the number of prediabetic individuals who eventually developed diabetes. In addition, the curcumin treatment appeared to improve overall function of -cells, with very minor adverse effects. Therefore, this study demonstrated that the curcumin intervention in a prediabetic population may be beneficial (Chuengsamarn, Rattanamongkolgul, Luechapudiporn et al. The Evidence Based Complementary and Alternative Medicine review cites extensive animal model (mostly rats) studies on the effects of curcumin on hyperglycemia and related cardiovascular and metabolic disorders. Some of these are summarized here and specific reference citations can be obtained in the original text (see Zhang, Fu, Gao et al. However, several researchers claimed that curcumin has no significant effect on blood glucose. Nevertheless, there are a number of clinical studies that support curcumin as an adjunctive treatment in Type 2 diabetes. For instance, the Indian Journal of Clinical Biochemistry reported a study that aimed to determine the effect of turmeric as an adjunct to antidiabetic therapy. Biochemical parameters were assessed at the time of recruitment for study and after 4 weeks of treatment. The investigators concluded that turmeric supplementation as an adjuvant in Type 2 diabetes patients on metformin treatment had an additional beneficial effect on blood glucose, oxidative stress, and inflammation (Maithili Karpaga Selvi, Sridhar, Swaminathan et al. Finally, an animal model study published in the journal Plant Foods for Human Nutrition is noteworthy for its focus on the possible beneficial effects of turmeric on the polyol pathway relevant to cataract formation. The aim of the study was to determine the effect of turmeric and its active principle, curcumin, on diabetes mellitus in a rat model. Alloxan was used to induce diabetes and the turmeric or curcumin that was administered to diabetic rats significantly reduced blood sugar and glycosylated hemoglobin levels. Moreover, the activity of Functional Foods Combating Effects of Hyperglycemia and Chronic Inflammation 337 sorbitol dehydrogenase, which catalyzes the conversion of sorbitol to fructose, was lowered significantly on treatment with turmeric or curcumin. The authors concluded that curcumin was more effective in attenuating diabetes-related changes than turmeric (Arun, and Nalini. It detailed a dose-escalation study to determine the maximum tolerable dose and safety of a single oral dose of curcumin in healthy volunteers. They were given increasing doses of curcumin ranging from 500 to 12,000 mg, and safety was assessed for 72 h after administration.