Purchase cleocin gel discount
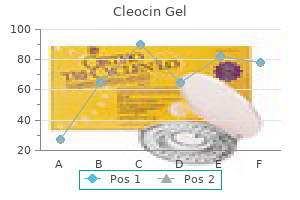
Pneumonia acne keloidalis nuchae icd 10 order 20 gm cleocin gel amex, together with influenza, is the leading cause of death from an infectious disease in the United States. Diagnosis and management of pneumonia require knowledge of host risk factors, potential infectious agents, and environmental exposures. Pneumonia is an infection of the lung tissue caused by a number of different bacteria, viruses, parasites, and fungi, resulting in inflammation of the lung parenchyma and accumulation of an inflammatory exudate in the airways. Infection typically begins in the alveoli, with secondary spread to the interstitium, resulting in consolidation and impaired gas exchange. Infection can also extend to the pleural space, causing pleuritis (inflammation of the pleura, characterized by pain on inspiration). The exudative inflammatory response of the pleura to pneumonia is termed a parapneumonic effusion; when bacterial infection is present in the pleura, this is termed empyema. Bacterial causes of community pneumonia vary by comorbid disease and severity of pulmonary infection (Table 4ͷ). S pneumoniae is the most common organism isolated in community-acquired pneumonia in both immunocompetent and immunocompromised individuals. Several additional organisms require special consideration in specific hosts or because of public health importance (Table 4). For example, patients who have suffered strokes and have impaired ability to protect their airways are at risk for aspirating oropharyngeal secretions. Precautions such as avoiding thin liquids in these patients may decrease the risk of future lung infections. Pathogenesis Pneumonia is disproportionally a disease of the elderly and impaired host; it occurs infrequently in immunocompetent individuals. This can be attributed to the effectiveness of host defenses, including anatomic barriers and cleansing mechanisms in the nasopharynx and upper airways and local humoral and cellular factors in the alveoli. Pulmonary pathogens reach the lungs by one of four routes: (1) direct inhalation of infectious respiratory droplets into Etiology Despite technologic advances in diagnosis, no causative agent is identified in approximately 50% of cases of communityacquired pneumonia. Even in cases in which a microbiologic diagnosis is made, there is usually a delay of several days before the pathogen can be identified and antibiotic susceptibility determined. Symptoms are nonspecific and do not reliably differentiate the various causes of pneumonia. Abrupt changes in direction of airflow in the nasal passages can trap potential pathogens. The epiglottis and cough reflex prevent introduction of particulate matter in the lower airway. The ciliated respiratory epithelium propels the overlying mucous layer (right) upward toward the mouth. In the alveoli, cell-mediated immunity, humoral factors, and the inflammatory response defend against lower respiratory tract infections. Incoming air with suspended particulate matter is subjected to turbulence in the nasal passages and then to abrupt changes in direction as the airstream is diverted through the pharynx and along the branches of the tracheobronchial tree. Particles larger than 10 mm are trapped in the nose or pharynx; those with diameters of 2 mm are deposited on the mucociliary blanket; only smaller particles reach the alveoli. M tuberculosis and Legionella pneumophila are examples of bacteria that are deposited directly in the lower airways through inhalation of small airborne particles. Bacteria trapped in the upper airways can colonize the oropharynx and subsequently be transported into the lungs either by "microaspiration" or by overt aspiration through an open epiglottis (eg, in patients who lose consciousness after excessive alcohol intake). Each cell has about 200 cilia that beat up to 500 times/min, moving the mucus layer upward toward the larynx. The mucus itself contains antimicrobial compounds such as lysozyme and secretory IgA antibodies. Chronic cigarette smokers have decreased mucociliary clearance secondary to damage of cilia and therefore compensate through the cough reflex to clear aspirated material, excess secretions, and foreign bodies. Bacteria that reach the terminal bronchioles, alveolar ducts, and alveoli are inactivated primarily by alveolar macrophages and neutrophils. Opsonization of the microorganism by complement and antibodies enhances phagocytosis by these cells. Impairment at any level of host defenses increases the risk of developing pneumonia. Children with cystic fibrosis have defective ciliary activity and are prone to develop recurrent sinopulmonary infections, particularly with S aureus and P aeruginosa. Patients with neutropenia, whether acquired or congenital, are also susceptible to lung infections with gramnegative bacteria and fungi. Antigenic stimulation of T cells leads to the production of lymphokines that activate macrophages with enhanced bactericidal activity. Extrapulmonary manifestations that may provide clues to the etiologic agents include pharyngitis (Chlamydia pneumoniae), erythema nodosum rash (fungal and mycobacterial infections), and diarrhea (Legionella). The following considerations aid in guiding empiric therapy for a patient who presents with symptoms consistent with pneumonia: (1) Is this pneumonia community acquired or healthcare acquired (eg, hospital, nursing home)? Sources of infection include person-to-person transmission (fecal-oral spread of Shigella), water-borne transmission (Cryptosporidium), food-borne transmission (Salmonella or S aureus food poisoning), and overgrowth after antibiotic administration (Clostridium difficile infection). However, in the majority of cases, symptoms are self-limited, and diagnostic evaluation is not performed. An exception is large outbreaks of food-borne illness, in which epidemiologic investigations may detect patients with milder variants of disease. Environmental factors can be divided into three broad categories based on mode of transmission: (1) water borne, (2) food borne, and (3) person to person. The term "gastroenteritis" classically denotes infection of the stomach and proximal small bowel. Causative organisms include Bacillus cereus, S aureus, and a number of viruses (rotavirus, norovirus). B cereus and S aureus produce a preformed neurotoxin that, even in the absence of viable bacteria, is capable of causing disease. What are the important pathogens for patients with community-acquired pneumonia based on severity of illness and site of care? Although death is a rare outcome of infectious diarrhea in the United States, morbidity is substantial. It is estimated that there are more than 200 million episodes each year, resulting in 1. The morbidity and mortality attributable to diarrhea are largely due to loss of intravascular volume and electrolytes, with resultant cardiovascular failure. The spectrum of diarrheal infections is typified by the diverse clinical manifestations and mechanisms through which E coli can cause diarrhea. Features common to all pathogenic E coli are evasion of host defenses, colonization of intestinal mucosa, and multiplication with host cell injury. Adherence can be nonspecific (at any part of the intestinal tract) or, more commonly, specific, with attachment occurring at well-defined anatomic areas. The bacteria gain entry to the small intestinal lumen through ingestion of contaminated food (left). They elaborate an enterotoxin that is composed of one A subunit and five B subunits. The B subunits bind to the intestinal cell membrane and facilitate entry of part of the A subunit (right). Infectious diarrhea is clinically differentiated into secretory, inflammatory, and hemorrhagic types, with different pathophysiologic mechanisms accounting for these diverse presentations. These organisms attach superficially to enterocytes in the lumen of the small bowel. Stool examination is notable for the absence of fecal leukocytes, although in rare cases there is occult blood in the stools. Clinically, the patient presents with copious diarrhea ("ricewater stools"), progressing to dehydration and vascular collapse without vigorous volume resuscitation. Inflammatory diarrhea is a result of bacterial invasion of the mucosal lumen, with resultant cell death. Patients with this syndrome are usually febrile, with complaints of crampy lower abdominal pain as well as diarrhea, which may contain visible mucous.
Diseases
- Partington Mulley syndrome
- Alcaptonuria
- Familial symmetric lipomatosis
- Pulmonary valves agenesis
- Hypotropia
- Sitophobia
- Paraparesis amyotrophy of hands and feet
- Chondroma (benign)
Order cleocin gel overnight
Gametes have undergone meiosis and so contain half the normal number of chromosomes found in zygotic cells acne 19 year old male buy generic cleocin gel on-line. The principle that the amount of product expressed for a particular gene is proportionate to the number of gene copies present per cell. A clinical phenomenon in which the phenotype observed in individuals carrying a deleterious gene appears more severe in successive generations. Possible explanations include ascertainment bias or a multistep mutational mechanism such as expansion of triplet repeats. A term referring to the presence of only one allele at a locus, either because the other allele is deleted or because it is normally not present. Refers to a mutation that has an effect similar to increasing the number of normal gene copies per cell. Refers to a mutation that reduces but does not eliminate the activity of a particular gene product. Most commonly, the process whereby expression of a gene depends on whether it was inherited from the mother or the father. A condition in which certain combinations of closely linked alleles, or haplotypes, are present in a population at frequencies not predicted by their individual allele frequencies. A situation in which mutations of different genes produce similar or identical phenotypes. A form of inheritance that obeys Mendel laws, ie, autosomal dominant, autosomal recessive, X-linked dominant, or X-linked recessive. A situation in which a genetic alteration is present in some but not all of the cells of a single individual. In germline or gonadal mosaicism, the alteration is present in germ cells but not somatic cells. In somatic mosaicism, the genetic alteration is present in some but not all of the somatic cells (and is generally not present in the germ cells). A reduction in zygotic cells from two to one in the number of copies for a particular chromosomal segment or chromosome. Refers to a mutation that imparts a novel function to its gene product and consequently results in a phenotype distinct from an alteration in gene dosage. In a single individual of a variant genotype, penetrance refers to whether or not the variant genotype can be inferred based on defined phenotypic criteria. In a population, reduced penetrance refers to the rate at which individuals of a variant genotype cannot be recognized according to specific phenotypic criteria. The situation that pertains when mutations of a single gene produce multiple different phenotypes. A mutational event that occurs after fertilization and that commonly gives rise to mosaicism. A genetic change that does not result in a phenotype itself but has a high probability of developing a second alteration - a full mutation - which does cause a phenotype. The group of cells set aside early in development that go on to give rise to gametes. A pattern of inheritance or mechanism of gene action in which a particular mutant allele causes a phenotype only in the absence of a nonmutant allele. Thus, for autosomal conditions, the variant or disease phenotype is manifest when two copies of the mutant allele are present. For X-linked conditions, the variant or disease phenotype is manifest in cells, tissues, or individuals in which the nonmutant allele is either inactivated (a heterozygous female) or not present (a hemizygous male). A type of translocation in which two acrocentric chromosomes are fused together with a single functional centromere. A carrier of a robertsonian translocation with 45 chromosomes has a normal amount of chromosomal material and is said to be euploid. Single nucleotide polymorphism - one of the most common types of genetic variation. A deletion, insertion, or more complex rearrangement, usually caused by recombination between repetitive elements. Most structural variants involve deletions or insertions that are relatively small (<10 kb) and do not cause any clinical phenotype. Larger structural variants (>100 kb) are increasingly likely to have clinical effects. A pathogenetic mechanism in which deficiency of a particular enzyme causes disease because the substrate of that enzyme accumulates in tissue or blood. Alterations in length of such simple types of repeats (dinucleotide and tetranucleotide as well) occur much more frequently than most other kinds of mutations; in addition, alteration in the length of trinucleotide repeats is the molecular basis for several heritable disorders. An abnormal situation in which there are three instead of two copies of a chromosomal segment or chromosome per cell. As originally coined, the word polymorphism referred to an allele present in 1% or more of a population; today, the terminology tends to be less rigid and is often described qualitatively, ie, rare and common variants. For an autosomal gene (those that lie on chromosomes 1Ͳ2, carried in two copies per cell), individuals carrying identical copies are homozygous, whereas individuals whose two copies differ from each other are heterozygous. This discussion helps to illustrate the use of the word phenotype, which refers simply to any characteristic that can be measured, with the type of measurement depending on the characteristic. In most genetic diseases, every cell in an affected individual carries the mutated gene or genes as a consequence of its inheritance via a mutant egg or sperm cell (gamete). However, mutation of the gametic cell may have arisen during its development, in which case somatic cells of the parent do not carry the mutation and the affected individual is said to have a "new mutation. Depending on the time of embryogenesis and cell type in which a new mutation arises, an individual may carry the mutation in some but not all of their germ cells (germline mosaicism), some but not all of their somatic cells (somatic mosaicism), or both. It is helpful to begin with a brief review of terms that are commonly used in discussing genetic disease with patients and their families. A mutation is a biochemical event such as a nucleotide change, deletion, or insertion that has produced a new allele. Given a set of defined criteria, recognition of the condition in individuals known to carry the mutated gene is described as penetrance. In other words, if 7 of 10 individuals older than 40 with the type I osteogenesis imperfecta mutation have an abnormal bone density scan, the condition is said to be 70% penetrant by that criterion. Penetrance may vary both with age and according to the set of criteria being used; for example, type I osteogenesis imperfecta may be 90% penetrant at age 40 when the conclusion is based on a bone density scan in conjunction with laboratory tests for abnormal collagen synthesis. Reduced penetrance or agedependent penetrance is a common feature of dominantly inherited conditions that have a relatively high fitness (the extent to which individuals carrying a mutant allele produce offspring relative to individuals who do not carry a mutant allele); Huntington disease and polycystic kidney disease are examples. When the same mutated gene gives rise to a different spectrum of phenotypes, the situation is referred to as variable expressivity. For example, blue scleras and short stature may be the only manifestations of type I osteogenesis imperfecta in a particular individual, whereas a sibling who carries the identical mutation may be confined to a wheelchair as a result of multiple fractures and deformities. In this schematic pedigree of the autosomal dominant condition type I osteogenesis imperfecta, nearly all of the affected individuals exhibit different phenotypic features that vary in severity (variable expressivity). As is shown, type I osteogenesis imperfecta is fully penetrant, because every individual who transmits the mutation is phenotypically affected to some degree. However, if mild short stature in the individual indicated with the arrow had been considered to be a normal variant, then the condition would have been nonpenetrant in this individual. Thus, in this example, judgments about penetrance or nonpenetrance depend on the criteria for normal and abnormal stature. Both reduced penetrance and variable expressivity may occur in individuals who carry the same mutated allele; therefore, phenotypic differences between these individuals must be due to the effects of other "modifier" genes, to environmental interactions, or to chance. Geneticists who study experimental organisms frequently use specific deletions to ensure that a mutated allele causes a loss of function, but human geneticists rely on biochemical or cell culture studies. For autosomal genes, the fundamental difference between dominant and recessive inheritance is that, with dominant inheritance, the disease state or trait being measured is apparent when one copy of the mutated allele and one copy of the normal allele are present. With recessive inheritance, two copies of the mutated allele must be present for the disease state or trait to be apparent. However, for genes that lie on the X chromosome, the situation is slightly different because females have two X chromosomes and males have only one. X-linked dominant inheritance occurs when one copy of a mutant gene causes the disease phenotype (in males and females); X-linked recessive inheritance occurs when two copies of a mutant gene cause the disease phenotype (in females). Because most mutations are amorphic or hypomorphic, however, one copy of an X-linked mutant allele in males is not "balanced" with a nonmutant allele, as it would be in females; therefore, in X-linked recessive inheritance, one copy of a mutant allele is sufficient to produce a disease phenotype in males, a situation referred to as hemizygosity. There are two general principles to keep in mind when considering loss-of-function mutations. Second, for most biochemical pathways, a 50% reduction in enzyme concentration is not sufficient to produce a disease state.
Purchase cleocin gel 20gm on-line
The non-classical are motor neuron disease-like skin care 1 month before wedding order cleocin gel no prescription, Guillainarr顳yndrome, brachial neuritis, subacute/ chronic sensorimotor neuropathy, neuropathy with vasculitis, autonomic neuropathy, and neuromyotonia. The sensory neuronopathies, with or without motor involvement, are by far the most prevalent type [35]. The onset of sensory neuronopathy is usually subacute and rapidly progressive, but may be acute, subacute, or chronic progressive. Numbness and paraesthesiae may begin in the limbs or face and spread to other regions, including the trunk, or may begin more diffusely. Sensory disturbances typically begin distally, but the distribution is often asymmetric and multifocal in a non-length-dependent manner. Ataxia and gait difficulty are usually early and prominent complaints, aside from shooting or aching limb pains, burning and dysaesthesiae. About half of the patients with features of a sensory neuronopathy also have distal motor involvement, resulting in a sensorimotor neuronopathy. Autoimmune neuropathies (chronic inflammatory demyelinating polyradiculoneuropathy and Guillainarr顳yndrome) have been described as paraneoplastic syndromes, but recently were found in such a low percentage in a large study that the authors suggest that an association by chance is likely [35]. End-plate disorders like Lambert΅aton myasthenic syndrome are discussed in Chapter 21. Recommendations for screening for tumours in paraneoplastic syndromes have recently been proposed [36]. Typically, onset is slow, often in the sixth decade, with gradual progression over years [39]. Electrodiagnostic studies are compatible with an axonal polyneuropathy [37,39,41]. Neurological examination may show indications for small-fibre dysfunction with disturbed temperature and pain sensation, or may be normal. Sensory modalities subserved by the large myelinated fibres (touch-pressure, vibration sense, joint position) are spared. Recently, in this idiopathic group a gain of function mutations in sodium channels Nav1. Signs of a sensory neuronopathy, or ganglionopathy, are numbness and paraesthesiae that may begin in the limbs or face and spread to other regions, including the trunk. Ataxia and forthcoming gait difficulties are often a clue to arrive at the diagnosis. An association between sensory ganglionopathy and inflammatory or immune-mediated disorders was first found in Sjn syndrome but has since been discovered in other autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and autoimmune hepatitis [46]. Peripheral neuropathy in adult type 1 Gaucher disease: a 2-year prospective observational study. Subacute combined degeneration: clinical, electrophysiological, and magnetic resonance imaging findings. Chronic idiopathic polyneuropathy presenting in middle or old age: a clinical and electrophysiological study of 75 patients. Chronic idiopathic axonal polyneuropathy and successful aging of the peripheral nervous system in elderly people. Selected peripheral neuropathies associated with human immunodeficiency virus infection and antiretroviral therapy. Associated signs of systemic illness can sometimes be found in patients with paraproteinaemic neuropathy. If the skin temperature is below 32ۃ, the limbs should preferably be warmed prior to the electrophysiological investigation because this can influence the obtained values. It is caused by a difference in the conduction times of the slowest and fastest axons within a nerve segment. In typical cases, among the first symptoms are pain, numbness, paraesthesia, or weakness in the limbs. This pain is mainly located at the extremities and the back, and might lead to inappropriate orthopaedic referral and a delay in making the diagnosis. If only the legs are involved, other lumbosacral pathology should be excluded (see the section Differential diagnosis). Electrophysiological examination can be helpful to confirm the diagnosis in clinically difficult cases. Motor nerve abnormalities, if any, are moderate and might show increased F-wave latency. Studies in preschool children showed that there can be a diagnostic delay because of a refusal to walk and pain in the legs, initially suggesting such as a myopathy, coxitis, or discitis [19,20]. Thirty-six per cent of patients experience pain in the 2 weeks preceding the onset of weakness. Issues that require attention are prophylaxis for deep vein thrombosis, cardiac and haemodynamic monitoring, pain management, management of possible bladder and bowel dysfunction, adequate eye care (especially in case of facial nerve palsy), psychosocial support, and rehabilitation. A retrospective study demonstrated that these patients frequently have residual disabilities. It is considered that these patients may have a prolonged immune response that causes ongoing nerve damage needing treatment for a longer period of time. Sixty to 80% of patients report severe fatigue, even years after disease onset [40]. Furthermore, 3Ͷ years after onset many patients still experience a great impact on their social life and ability to perform daily activities [42]. More than a third of patients have moderate to severe pain for at least 1 year after onset [21]. This may induce complement activation and destruction of nerves, and antibody activity against sodium channels [4,5,45]. Subsequently this can lead to the destruction of sodium channel clusters, detachment of the paranodal myelin, and axonal degeneration, with invasion of macrophages into the periaxonal space [5,47]. Most patients require long-term treatment for at least 6 months to several years [52]. The symptoms have a chronically progressive, stepwise, or recurrent course, developing over at least 2 months. It is recommended to test for serum and urine paraproteins, fasting glucose, complete blood count, renal function, liver function, antinuclear factor, and thyroid function [50]. Typically, both sensory and motor nerve examinations are abnormal, but pure motor forms and pure sensory forms exist. Steroids the advantages of steroids are their availability and low initial cost, but side effects can be serious. A follow-up study found that patients receiving pulse steroid treatment not only had a faster improvement than with standard prednisolone treatment, but also had slightly longer remissions, relative fewer relapses, and fewer adverse events [65]. Serious adverse effects are rare and can include thromboembolic events, renal failure (mainly in patients with pre-existing renal failure), anaphylaxis (especially in patients with IgA deficiency), or aseptic meningitis. Prognostic factors related to improvement A better outcome is related to younger age at onset, relapsingβemitting course, and absence of axonal damage [81]. However, in almost 80% of patients, the first symptoms appear before the age of 50. Besides medication, attention has to be paid to rehabilitation and managing symptoms such as foot drop, fatigue, and pain. This disorder presents with asymmetrical weakness and sensory loss, and is worse in the arms. In the first years after onset, muscle atrophy is usually mild compared with weakness. However, in patients with longer disease duration muscle atrophy can be more substantial. Other motor symptoms include cramps and fasciculations, which are reported in more than half of patients. Patients do not develop weakness of the respiratory muscles and have a normal life expectancy.
Discount cleocin gel 20 gm without prescription
A normal immune response relies on the careful coordination of a complex network of biological factors skin care urdu tips buy cheap cleocin gel 20 gm line, specialized cells, tissue, and organs necessary for the recognition of pathogens and subsequent elimination of foreign antigens. Dysfunction or deficiency of components of the immune system leads to a variety of clinical diseases of varying expression and severity, ranging from atopic disease to rheumatoid arthritis, severe combined immunodeficiency, and cancer. This chapter introduces the intricate physiology of the immune system and abnormalities that lead to diseases of hypersensitivity and immunodeficiency. The antibody-mediated and cell-mediated immune systems provide specificity and memory of previously encountered antigens. The nonspecific or innate defenses include epithelial barriers, mucociliary clearance, phagocytic cells, and complement proteins. Despite their lack of specificity, these components are essential because they are largely responsible for natural immunity to a vast array of environmental threats and microorganisms. Knowledge of the components and physiology of normal immunity is essential for understanding the pathophysiology of diseases of the immune system. The major cellular components of the immune system consist of monocytes and macrophages, lymphocytes, and the family of granulocytic cells, including neutrophils, eosinophils, and basophils. Derived from hematopoietic stem cells, these fully differentiated effector cells have membrane receptors for various chemoattractants and mediators, facilitating the activation or destruction of target cells. Tissue macrophages are derived from blood monocytes and participate in antigen processing, tissue repair, and secretion of mediators vital to initiation of specific immune responses. These cells, abundant near mucosal surfaces that internalize microorganisms and debris, travel to secondary lymphoid organs where they process and present that antigen in a form recognizable to T lymphocytes. Circulating monocytes are recruited to sites of inflammation where they mature into macrophages. Both monocytes and macrophages contain receptors for C3b (activated bound complement) and the Fc portion of both immunoglobulin G (IgG) and IgE, which facilitate the activation of these cells through antigen-specific and nonspecific immune pathways. Activation of these cells occurs both after binding to immune complexes through exposure to various cytokines and after phagocytosis of antigen or particulates such as silica and asbestos. Proteolytic enzymes and proinflammatory mediators including cytokines, arachidonic acid metabolites, and oxidative metabolites are utilized in the monocytes and macrophages. Structurally, B and T lymphocytes cannot be distinguished visually from each other under the microscope; they can be enumerated by flow cytometric phenotyping or by immunohistochemical methods. The thymus-derived cells (T lymphocytes or T cells) are involved in cellular immune responses. Precursors of T cells migrate to the thymus, where they develop some of the functional and cell surface characteristics of mature T cells. Through positive and negative selection, clones of autoreactive T cells are eliminated, and mature T cells migrate to the peripheral lymphoid tissues. There, they enter the pool of long-lived lymphocytes that recirculate from the blood to the lymph. T lymphocytes are heterogeneous with respect to their cell surface markers and functional characteristics. They are responsible for defense against intracellular pathogens (eg, viruses), tumor immunity, and organ graft rejection. A number of additional T-helper subsets have been discovered that contribute to immune regulation. Mucosal dendritic cells control the generation of regulatory T cells, which modulate inflammatory responses through the secretion of regulatory cytokines. B-lymphocyte maturation proceeds in antigen-independent and antigen-dependent stages. Antigen-independent development occurs in the marrow where pre-B cells mature into immunoglobulin-bearing naive B cells (cells that have not been exposed to antigen previously). In peripheral lymphoid tissues, antigen-dependent activation produces circulating long-lived memory B cells and plasma cells found predominantly in primary follicles and germinal centers of the lymph nodes and spleen. All mature B cells bear surface immunoglobulin that is their antigen-specific receptor. Binding of an antibody-coated cell or foreign substance triggers release of perforin, a pore-forming protein that causes cytolysis. Polymorphonuclear leukocytes (neutrophils) are granulocytes that phagocytose and destroy foreign antigens and microbial organisms. Locally released lysosomal enzymes destroy particles too large to be phagocytosed. Neutrophils contain or generate a number of antimicrobial factors, including oxidative metabolites, superoxide, and hydrogen peroxide, as well as myeloperoxidase, which catalyzes the production of hypochlorite, and proteolytic enzymes, including collagenase, elastase, and cathepsin B. Despite many shared functional similarities to neutrophils, eosinophils are considerably less efficient than neutrophils at phagocytosis. Eosinophil-derived products may play a role in the development of airway hyperreactivity. Basophils play an important role in both immediate- and late-phase allergic responses. Mast cells are basophilic staining cells found chiefly in connective and subcutaneous tissue. They have prominent granules that are the source of many mediators of immediate hypersensitivity and have 30,000Ͳ00,000 cell surface membrane receptors for the Fc fragment of IgE. When an allergen molecule cross-links two adjacent mast cell surfaceΡssociated IgE antibodies, calcium-dependent cellular activation leads to the release of both preformed and newly generated mediators. Mast cells also have surface receptors for "anaphylatoxins" (activated complement fragments, C3a, C4a, and C5a), cytokines, and neuropeptides, such as substance P. Activation by these nonΉgE-mediated mechanisms may contribute to host immunity and provide ties between the immune and neuroendocrine systems. Experimentally, mast cellΤerived mediators promote angiogenesis and fibrogenesis, suggesting their presence in these sites is pathologically relevant. Organs of the Immune System Several tissues and organs play roles in host defenses and are functionally classified as the immune system. Pluripotent stem cells differentiate into lymphocyte, granulocyte, monocyte, erythrocyte, and megakaryocyte populations. In humans, B lymphocytes, which are the antibody-producing cells, undergo early antigen-independent maturation into immunocompetent cells in the bone marrow. Deficiency or dysfunction of the pluripotent stem cell or the various cell lines developing from it can result in immune deficiency disorders of varying expression and severity. The thymus, derived from the third and fourth embryonic pharyngeal pouches, functions to produce T lymphocytes and is the site of initial T-lymphocyte differentiation. Its reticular structure allows a significant number of lymphocytes to migrate through it to become fully immunocompetent thymus-derived cells. In subsequent negative selection, T cells that avidly recognize self-peptides are destroyed, thus removing deleterious selfreactive clones. In some murine models, autoimmune diseases such as systemic lupus erythematosus may develop in mice with defective apoptotic (programmed cell death) pathways in T cells recognizing self-antigen. The thymus also regulates immune function by secretion of multiple hormones that promote T-lymphocyte differentiation and are essential for T-lymphocyteέediated immunity. In mammals, the lymph nodes, spleen, and gut-associated lymphoid tissue are secondary lymphoid organs connected by blood and lymphatic vessels. Lymph nodes are strategically dispersed throughout the vasculature and are the principal organs of the immune system that localize antigen, promote cell-cell interaction and lymphocyte activation, and prevent the spread of infection. Lymph nodes have a framework of reticular cells and fibers that are arranged into a cortex and medulla. B lymphocytes, the precursors of antibody-producing cells, or plasma cells, are found in the cortex (the follicles and germinal centers) as well as in the medulla. The spleen filters and processes antigens from the blood and is functionally and structurally divided into B-lymphocyte and T-lymphocyte areas, similar to those of the lymph nodes. Gut-associated lymphoid tissue includes the tonsils, Peyer patches of the small intestine, and the appendix. Like the lymph nodes and spleen, these tissues exhibit separation into B-lymphocyteΤependent and T-lymphocyteΤependent areas. Mucosal immune responses tend to generate antigenspecific IgA, and with some orally administered antigens, T-cell anergy or tolerance may occur rather than immune stimulation. They target many diverse cell types, can have antiviral, proinflammatory, or antiinflammatory activities, act locally or systemically, and can be redundant in their actions (Table 3ͱ). Mediators may exist in a preformed state in the granules of mast cells and basophils or are newly synthesized at the time of activation of these and some other nucleated cells. Increased awareness of the immunologic and physiologic effects of mediators has led to a better understanding of immunopathology and provides potential targets for future pharmacotherapies. Preformed mediators include histamine, eosinophil and neutrophil chemoattractants, proteoglycans (heparin, chondroitin sulfate), and various proteolytic enzymes.
Consound (Comfrey). Cleocin Gel.
- Skin ulcers, wounds, broken bones, heavy periods, diarrhea, cough, sore throat, gum disease, joint pain, chest pain, cancer, bruises, inflammation (swelling) and sprains when applied to the skin, and other conditions.
- Are there any interactions with medications?
- How does Comfrey work?
- Are there safety concerns?
- What is Comfrey?
- Dosing considerations for Comfrey.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96318
Order cleocin gel 20gm fast delivery
Mitral annular tissue Doppler shows a reversal of the normal Em:Am ratio with mild diastolic dysfunction skin care olive oil generic 20gm cleocin gel free shipping, the degree of reversal increasing in magnitude as the diastolic dysfunction becomes increasingly severe. Mitral annular tissue Doppler shows marked reversal of the Em:Am ratio and a septal E:Em ratio of 18. In late diastole, atrial contraction actively boosts left ventricular filling (unless the patient is in atrial fibrillation). Be alert too for the presence of spontaneous echo contrast, particularly in presence of atrial fibrillation and/or mitral stenosis. Although best seen on transoesophageal echo, spontaneous echo contrast may also be evident during transthoracic imaging. Cor triatriatum dexter is the name given to this condition when it occurs in the right atrium. Additional information can also be obtained from the: right parasternal window apical 3-chamber (long axis) view subcostal window subcostal short axis view suprasternal window aorta view. Causes of aortic stenosis 19 the aortic valve Calcific degeneration of the aortic valve is one of the commonest causes of aortic stenosis. Rheumatic aortic stenosis is less common than rheumatic mitral stenosis, and the two often coexist in the same patient. Sub- and supravalvular obstruction cause a form of aortic stenosis in which the valve itself is unaffected but the obstruction lies below or above the valve. In supravalvular aortic stenosis, which is uncommon, there is a fixed obstruction in the ascending aorta, just above the sinuses of Valsalva, due to a diffuse narrowing or a discrete membrane. Clinical features of aortic stenosis the clinical features of aortic stenosis are summarized in table 19. Many cases of aortic stenosis are detected incidentally, either because of a systolic murmur heard during a routine examination or as an incidental finding during an echocardiogram for other indications. Grade any cusp restriction as mild (restricted in basal third only), moderate (affecting basal and middle third) or severe (affecting entire cusp). Planimetry of the aortic valve orifice area in the parasternal short axis view (aortic valve level) can be challenging, particularly with heavily calcified cusps, and is not routinely recommended. It can sometimes be useful, however, if Doppler estimation of aortic valve effective orifice area (see below) cannot be performed reliably. Use 2D echo to look carefully for a discrete membrane causing obstruction above or below the valve. Colour doppler Colour Doppler imaging will show an increase in flow velocity and/or turbulent flow at valve level and downstream of the stenosis. In mild aortic stenosis, the trace has a more triangular shape with an earlier peak. In contrast, the gradient measured by echo Doppler is an instantaneous gradient it measures the maximum instantaneous pressure difference between the two chambers. Instantaneous gradients are greater than peak-to-peak gradients, and so peak transaortic gradients measured by echo will be higher than gradients measured by cardiac catheterization. If a patient has increased arterial afterload (hypertension) this can lead to underestimation of the severity of aortic stenosis. In such a scenario, double check all your measurements and look carefully at the aortic valve (to judge whether its appearance is consistent with severe aortic stenosis). Such high flows can be seen with co-existent aortic regurgitation, or in clinical conditions associated with a high cardiac output. There is moderate concentric left ventricular hypertrophy with good systolic function. Biological prosthetic valves are generally preferred for older patients or those who wish to avoid the need for long-term anticoagulation, while mechanical prosthetic valves are preferred for younger patients. Balloon valvuloplasty can be used as a bridge to valve replacement in unstable patients, or for patients who need urgent non-cardiac surgery. It can result from a problem with the aortic valve itself or from a problem with the aortic root affecting an otherwise normal valve. Causes of aortic regurgitation Valvular causes include: calcific degeneration of the aortic valve bicuspid aortic valve, causing incomplete closure of the valve infective endocarditis rheumatic aortic valve disease connective tissue diseases. Some conditions, such as ankylosing spondylitis, can affect both the aortic valve and the aortic root. Clinical features of aortic regurgitation the clinical features of aortic regurgitation are summarized in table 19. Infective endocarditis and aortic dissection can cause acute aortic regurgitation, in which 164 Making sense of echocardiography Table 19. Echo assessment of aortic regurgitation 2d and M-mode Use 2D and M-mode echo to assess the structure of both the aortic valve and the aortic root: Is it a normal tricuspid aortic valve, or is it bicuspid (or pseudobicuspid), unicuspid or quadricuspid? Are there any features of infective endocarditis (vegetations, aortic root abscess)? Obtain a VtI of the diastolic flow reversal severe regurgitation is indicated by a VtI >15 cm. Pandiastolic flow reversal may also be seen in the abdominal aorta, where it is a specific indicator of severe aortic regurgitation. Although simple in principle, measurement of regurgitant volume is difficult in practice. A easuring the width of the regurgitant jet on colour Doppler too far below the aortic valve, M where it tends to spread out, overestimates severity. In such cases it is generally better to use visual assessment to grade the ratio in terms of small, intermediate or large, and to use this as a gross guide to severity, than to stick slavishly to percentages. There is a dense central jet of aortic regurgitation with a vena contracta width of 0. The calculated aortic regurgitant volume is 78 mL/beat (regurgitant fraction 62 per cent) with a regurgitant orifice area of 0. Management of aortic regurgitation echo surveillance review patients with mildέoderate aortic regurgitation annually and perform an echo every 2 years. Perform an annual echo in patients with a dilated aortic root (especially those with Marfan syndrome or bicuspid aortic valve), or even more frequently if the aorta is enlarging. Surgery may involve aortic valve replacement or repair (where the valve is suitable), together with aortic root grafting where appropriate. Once you have completed the M-mode recording, use colour Doppler to assess valvular flow. Sometimes there can be three papillary muscles if one of them happens to be bifid. Additional information can also be obtained from the: subcostal window subcostal long axis view subcostal short axis view. The mitral valve 173 Causes of mitral stenosis Rheumatic valve disease can affect any of the heart valves (or several in combination), but most commonly affects the mitral valve. Beware of conditions that can cause obstruction of the mitral valve orifice and mimic mitral stenosis, such as left atrial myxoma, infective endocarditis with a large vegetation, ball thrombus or cor triatriatum. It is thought to be an indicator of cardiovascular risk and a marker of coronary artery disease. If annular calcification is massive, it can extend into the mitral leaflets and cause mitral stenosis. Unlike rheumatic mitral stenosis, mitral annular calcification does not affect the leaflet tips or cause fusion of the commissures. Clinical features of mitral stenosis the clinical features of mitral stenosis are summarized in table 20. Patients usually remain asymptomatic until the mitral valve orifice area falls below 2. Pulmonary artery pressure also begins to rise and pulmonary hypertension develops. Once a patient becomes symptomatic, if left untreated the 10-year survival is around 50Ͷ0 per cent. Echo assessment of mitral stenosis 2d and M-mode Use 2D and M-mode echo to assess the structure of the valve and the subvalvular apparatus. Be sure to describe the appearance of the mitral leaflets, mitral annulus, chordae tendineae and papillary muscles: Do the mitral valve leaflets appear normal? In the parasternal short axis view (mitral valve level), if the image quality is good enough, perform planimetry to measure the mitral orifice area. Be careful of high gain settings, which can lead to underestimation of the mitral orifice area. Is there evidence of commissural fusion (shown by the posterior leaflet moving upwards, in the same direction as the anterior leaflet, as it opens during diastole, rather than downwards as a mirror image of the anterior leaflet)? An alternative to the Wilkins score is the commissural calcification score, in which each mitral commissure (anterolateral and posteromedial) is scored according to the degree of calcification seen on the short axis view, with a score of 0 being given for no calcification, 1 for calcium across half a commissure, and 2 for calcium across the whole commissure.
Discount cleocin gel generic
Increased elastic forces predominate in two common disorders skin care 101 order cleocin gel on line amex, diffuse parenchymal fibrosis and obesity. The reduction in lung compliance in fibrotic lung disease, and in chest wall and respiratory system compliance in obesity, increases the work of breathing. Obese subjects also experience increased airflow resistance, largely though not entirely because of their tendency to breathe at lower lung volumes. The underlying physiologic abnormality in emphysema is a dramatic increase in lung compliance. Patients with pulmonary fibrosis have very noncompliant lungs and breathe at low lung volumes. The equal pressure point is not an anatomic site but a functional result that helps to clarify different mechanisms of airflow obstruction. Because the driving pressure of expiratory airflow is principally lung elastic recoil pressure, a loss of lung elasticity that reduces recoil pressure without changing pleural or peribronchiolar pressure will lead to dynamic compression at higher lung volumes. The resultant air trapping contributes to symptomatic dyspnea in patients with obstructive lung disease. Patients with emphysema lose lung elastic recoil and may have severely impaired expiratory flow even with airways of normal caliber. The presence of airway disease will increase the drop in driving pressure along the airways and may generate an equal pressure point at even higher lung volumes. Patients with pulmonary fibrosis may have abnormally high flow rates despite severely reduced lung volumes. A reduction by one half of airway radius leads to a 16-fold increase in airway resistance. Airway caliber is, therefore, the principal determinant of airway resistance under laminar flow conditions. Under conditions of turbulent flow, the driving pressure needed to achieve a given flow rate is proportionate to the square of the flow rate. First, airflow in the normal lung is not laminar but turbulent, at least from the mouth to the small peripheral airways. Thus, where flow is highest (in segmental and subsegmental bronchi), resistance is dependent chiefly on flow rates. Second, in small peripheral airways, where airway caliber is the principal determinant of resistance, repetitive branching creates a very large number of small airways arranged in parallel. Their resistance is reciprocally additive, making their contribution to total airway resistance minor under normal conditions. In the respiratory bronchioles and alveoli, bulk flow of gas ceases and gas movement occurs by diffusion. Many disease states affect bronchial smooth muscle tone and cause bronchoconstriction, producing an abnormal narrowing of the airways. Airways may also be narrowed by hypertrophy (chronic bronchitis) or infiltration (sarcoidosis) of the airway mucosa. Physiologically, the radial traction of the lung interstitium supports the airways and increases their caliber as lung volume increases. Conversely, as lung volume decreases, airway caliber also decreases and resistance to airflow increases. Patients with airflow obstruction often breathe at large lung volumes because higher volumes tend to increase elastic lung recoil, maximize airway caliber, and minimize flow resistance. Analysis in terms of laminar and turbulent flow assumes that airways are rigid tubes. The compressibility of the airways underlies the important phenomenon of effort-independent flow; airflow rates during expiration can be increased with effort only up to a certain point. The explanation for this phenomenon relies on the concept of an equal pressure point. Pleural pressure is generally negative (sub-atmospheric) throughout quiet breathing. Peribronchiolar pressure, the pressure surrounding small, noncartilaginous conducting airways, is closely related to pleural pressure. Hence, during quiet breathing, conducting airways are surrounded by negative pressure that helps to keep them open. For air to flow through a tube, there must be a pressure difference between the two ends. In the case of forced expiration with an open glottis, this driving pressure is the difference between alveolar pressure (the sum of pleural pressure and lung elastic recoil pressure) and atmospheric pressure (assumed to be zero). Frictional resistance causes a fall in this driving pressure along the length of the conducting airways. At some point, the driving pressure may equal the surrounding peribronchial pressure; in this event, the net transmural pressure is zero. Downstream (toward the mouth) from the equal pressure point, pressure outside the airway is greater than the driving pressure inside the airway. This net negative pressure tends to collapse the airway, resulting in dynamic compression. The more forcefully one expires, the more the pressure surrounding collapsible airways increases. These diagrams divide the total work of breathing at the same minute ventilation into elastic and resistive components. In disease states that increase elastic forces (eg, pulmonary fibrosis), total work is minimized by rapid, shallow breathing; with increased airflow resistance (eg, chronic bronchitis), total work is minimized by slow deep breathing. The two components of the work of breathing - elastic forces and resistance to airflow - are affected in opposite ways by changes in frequency and depth of breathing. Elastic resistance is minimized by frequent, shallow breaths; resistive forces are minimized by fewer, larger tidal volume breaths. The set point for basal respiration is that point at which the total work of breathing is minimized. In different diseases, this pattern is altered to compensate for the underlying physiologic abnormality. The amount of energy needed to maintain the respiratory muscles during quiet breathing is small, approximately 2% of basal oxygen consumption. In patients with lung disease, the energy requirements are greater at rest and increase dramatically with exercise. Patients with emphysema may not be able to increase their ventilation by more than a factor of 2 because the oxygen cost of breathing exceeds the additional oxygen made available to the body. Hemoglobin is a complex tetramer of two alpha and two beta polypeptide chains, each of which contains a heme group with an iron atom in the ferrous form (Fe2+) at its center capable of binding molecular oxygen (O2). Under physiologic conditions, 1 g of fully saturated hemoglobin can carry approximately 1. Therefore, 100 mL of blood containing 15 g/dL of saturated hemoglobin contains 20. Blood oxygen content is the sum of two terms, dissolved oxygen and oxygen bound to hemoglobin. Because of its physical chemistry, hemoglobin saturation has a complex relationship with the partial pressure of oxygen. Interactions among the four polypeptide chains in the heme molecule increase overall affinity for oxygen as each oxygen binding site is filled. This relationship explains the suitability of hemoglobin for its primary physiologic role, the reversible binding to oxygen with uptake in the lungs and release in the tissues. At a temperature of 37у and an oxygen partial pressure of 100 mm Hg (PaO2 = 100), total oxygen dissolved in 100 mL of whole blood is approximately 0. Because basal oxygen consumption in the average adult human is approximately 250 mL/min, dissolved oxygen content would be inadequate to meet metabolic demands. Instead, the high oxygen needs of complex internal organs are met by a soluble protein that binds oxygen rapidly, reversibly, and with a high storage capacity, namely, hemoglobin. B ʹ Pleural pressure (cm H2O) 100 +2 50 +10 0 ͱ0 Ͳ0 0 ͳ0 Distribution of Ventilation & Perfusion Inhaled air and pulmonary arterial blood flow are not distributed equally to all lung regions. In healthy individuals, heterogeneous distribution is due principally to two factors: the effects of gravity and the fractal geometry of repetitive branching of airways and vessels.
Order cleocin gel 20gm overnight delivery
Select a depth setting so that the whole area of interest can be seen skin care cream buy discount cleocin gel 20gm line, but not so deep that it includes irrelevant structures beyond the region of interest. As with depth, sector width is an important determinant of frame rate and should be optimized for each view to include the region of interest but no more. Focus can be fine-tuned with phased-array transducers and should be adjusted for each view so that the beam is focused on the region of interest. Greyscale compression (dynamic range) adjusts the number of shades of grey that are displayed in the image. Lateral resolution, also known as azimuthal resolution, relates to objects that lie side by side, perpendicular to the ultrasound beam, and varies according to how far the objects lie from the transducer. Lateral resolution is also affected by gain settings the higher the gain, the worse the lateral resolution. Temporal resolution, or frame rate, is important in trying to distinguish events that occur close together in time. Frame rate depends upon the time taken to collect all the data required to create one image, which in turn depends upon the sector width and depth. M-mode imaging offers very high sampling rates, typically 1800 times per second, because of the very narrow field of view (see above). Reverberation occurs when ultrasound rebounds several times between two strong specular reflectors before returning to the transducer. Beam width artefact arises because the ultrasound beam has a finite width (especially in the far field) and the machine is unable to discriminate whether a returning echo signal has arisen from the centre of the beam and/or the edge. Beam width artefact can be reduced by focusing the ultrasound beam to minimize its diameter. Signals returning from the side lobe beams are interpreted by the echo machine as having arisen from the central beam, and can be displayed some distance away from the true location of the structure in question. Storage of echo studies can be on videotape, which is relatively inexpensive, although it rapidly becomes cumbersome to store (and to review) studies when large numbers are archived in this way. Digital archiving is now more commonly used, with storage on hard drives or optical disks. Thermal effects are caused by conversion of the mechanical energy of the ultrasound into heat energy as it passes through the tissues. Heat may be generated not just by the ultrasound but also directly by the probe itself. Mechanical effects include cavitation, in which gas bubbles are created as ultrasound passes through the tissues. It is not thought to be a problem during standard transthoracic studies, but is important when bubble contrast agents are used as it can cause resonance and even disruption of the bubbles (p. M-mode and 2D echo have the lowest ultrasound intensity, and pulsed-wave Doppler has the highest intensity (with colour Doppler having an intermediate value). Ensuring safety also requires an awareness of more general hazards such as: risk of electrical shock from damaged or poorly maintained equipment risk of injury from trips and falls, particularly when transferring onto the examination couch risk of infection from inadequate infection control measures. Echo departments should have appropriate risk assessment tools and protocols in place to minimize risks to patients and staff. As well as allowing the assessment of blood flow, the Doppler principle has also, more recently, been applied to the study of myocardial function (tissue Doppler imaging). A classic example is that of a moving ambulance sounding its siren as the ambulance approaches an observer, its siren sounds higher pitched than when it is moving away. It follows from this equation that a large angle between the direction of blood flow and the ultrasound beam will lead to an underestimation of flow velocity, and this is particularly marked for angles >20Ю For this reason, when undertaking echo Doppler studies it is important to align the ultrasound beam with the direction of blood flow as closely as possible. For each time point the grey pixels show the blood flow velocity detected, and the density of the signal. Gain, which amplifies the received signal to increase the brightness of the displayed spectral trace. High gain settings amplify weaker signals that might otherwise not be visible, but increase noise. Velocity range, which alters the vertical velocity scale to a higher or lower range. In order to measure Doppler shift (and hence flow velocity) within the boundaries of the sample volume, the transducer cannot use continuous transmission/reception of ultrasound. Aliasing can also be reduced by: the Doppler velocity scale (as far as possible) at the lowest possible distance from the transducer decreasing the transmitted frequency increasing the angle of incidence. Blood flow is pulsatile, increasing (and then decreasing) in velocity with time during each cardiac cycle. However, blood flow is pulsatile, not constant, so to calculate flow volume (mL per heartbeat) it is necessary to measure the cross-sectional area of the region of interest and to measure the velocity time integral (VtI) of flow in that region. VtI is measured by integrating the area under the spectral envelope this can easily be achieved by tracing the outline of the spectral Doppler envelope and allowing the echo machine software to calculate the VtI. However, rather than measuring blood flow at just a single sample volume, in colour Doppler the blood flow is assessed at multiple points within a pre-selected area. A colour Doppler display colour-codes blood flow according to its direction and the mean velocity within each sample volume. At the edge of the display is a velocity scale, correlating the shade of colour with the measured flow velocity. Although other structures, including the myocardium, move as well, filtering techniques were used to remove the Doppler signals returning from myocardium in order to optimize the signals relating to blood flow. This page intentionally left blank 5 Service provision chapter In addition to the technicalities of performing and reporting an echo study, there are wider issues to consider in relation to providing an echo service. Studies should be triaged according to urgency and systems should be in place to alert clinicians to important abnormalities. Studies should be reported on the day they are performed and should be archived for future reference. Echo rooms should be of adequate size (at least 20 m2 if used for inpatient studies). Equipment maintenance must be carried out regularly, with echo machines being replaced (or having a major upgrade) at least every 5 years. A period of 30ʹ5 min should be allowed for routine studies and up to 1 h for complex studies. Sonographers who undertake and report echo studies unsupervised should have appropriate seniority and accreditation. Undertaking a recognised accreditation programme provides the sonographer with a structured means of attaining a minimum standard in echo. Echo departments need to pay careful attention to health and safety, particularly with regard to musculoskeletal and eye problems, liaising with local occupational health and risk management departments as appropriate. QuAliTy ConTrol It should be the aim of every sonographer, and every echo department, to provide a high-quality echo service. Audit is one of the cornerstones of clinical governance, the process by which healthcare organizations are accountable for continually improving the quality and safety of their services. A method of collecting the data is then chosen, and then the necessary data are collected and analysed. Any deficiencies should be identified (while at the same time recognizing areas of good performance), and a mechanism agreed by which improvements can be made. Any changes should then be implemented and, after an appropriate timescale, the audit cycle should be repeated to see whether the changes have led to the expected improvements. European Association of Echocardiography recommendations for standardization of performance, digital storage and reporting of echocardiographic studies. American Society of Echocardiography recommendations for quality echocardiography laboratory operations. Echo requests must therefore carry appropriate clinical details and contain information about known cardiac diagnoses or previous cardiac interventions/surgery. Clinicians requesting echo studies should be encouraged to include specific questions with their request. However, as with virtually every clinical test, echo has its limitations and can sometimes produce an erroneous result. Specificity the number of people who receive false positive/negative results is determined not only by the sensitivity and specificity of the test, but also by the population prevalence of the disease in question.
Purchase cheap cleocin gel online
Hepcidin binds to ferroportin acne prone skin purchase cleocin gel overnight delivery, a transmembrane protein, inducing its internalization and lysosomal degradation. When iron stores are low, hepcidin production is reduced and ferroportin molecules are expressed on the basolateral membrane of enterocytes, where they transfer iron from the cytoplasm of enterocytes to plasma transferrin. Conversely, when iron stores are adequate or elevated, hepcidin production is increased, resulting in the internalization of ferroportin and Pathology As iron stores are depleted, the peripheral blood smear pattern evolves. In early iron deficiency, the hemoglobin level of the blood falls but individual erythrocytes appear normal. In response to a falling oxygen level, erythropoietin levels rise and stimulate the marrow, but the hemoglobin level cannot rise in response because of the iron deficiency. Other hormones are presumably also stimulated, however, and the resulting "revved-up" marrow usually causes an elevated blood platelet count. There is also substantial anisocytosis and poikilocytosis, seen on the peripheral smear, and target cells may be seen. The target shape occurs because there is a relative excess of red cell membrane compared with the amount of hemoglobin within the cell, so that the membrane bunches up in the center. A low serum ferritin level is diagnostic of iron deficiency, but even in obvious cases, levels can be normal; ferritin levels rise in acute or chronic inflammation or significant illnesses, which can themselves be the cause of iron (blood) loss. Serum iron levels fall in many illnesses, and levels of its serum carrier, transferrin, fluctuate as well, so neither of them is a consistent indicator of iron deficiency, nor is their ratio, the transferrin saturation. If ferritin levels are not diagnostic, measuring serum soluble transferrin receptor (sTfR) can help. TfRs are membrane glycoproteins that facilitate iron transport from plasma transferrin into body cells. Erythroid precursors increase their expression of membrane TfR in the setting of iron deficiency but not anemia of chronic disease. A high ratio of sTfR to ferritin predicts iron deficiency when ferritin is not diagnostically low. Other than observing a hematologic response to empiric iron supplementation, bone marrow biopsy can confirm a diagnosis of iron deficiency. Iron is normally found in the macrophages of the marrow, where it supplies erythrocyte precursors; intracellular hemosiderin is easily visualized with Prussian blue stain. Clinical Manifestations All anemias lead to classic symptoms of decreased oxygencarrying capacity (ie, fatigue, weakness, and shortness of breath, particularly dyspnea on exertion), and iron deficiency is no exception. Decreased oxygen-carrying capacity leads to decreased oxygen delivery to metabolically active tissues, which nonetheless must have oxygen; this leads directly to fatigue. The compensatory mechanisms of the body lead to additional symptoms and signs of anemia. Some patients appear pale not only because there is less hemoglobin per unit of blood (oxygenated hemoglobin is red and gives color to the skin) but also because superficial skin blood vessels constrict, diverting blood to more vital structures. This tachycardia may cause benign cardiac murmurs due to the increased blood flow. Glossitis, where the normal tongue papillae are absent, can occur, as can gastric atrophy with achlorhydria (absence of stomach acid). The achlorhydria may compound the iron deficiency because iron is best absorbed in an acidic environment, but this complication is quite unusual. In children, there may be significant developmental problems, both physical and mental. Iron-deficient children, mostly in developing regions, perform poorly on tests of cognition compared with iron-replete children. Another unexplained but often observed phenomenon in severe iron deficiency is pica, a craving for nonnutritive substances such as clay or dirt. Many patients have no specific symptoms or findings at all, and their iron deficiency is discovered because of anemia noted on a blood count obtained for another purpose. It is of interest that mild anemias (hemoglobins of 11ͱ2 g/dL) may be tolerated very well because they develop slowly. In addition to the physiologic compensatory mechanisms discussed previously (increased cardiac output, diversion of blood flow from less metabolically active areas), there is a biochemical adaptation as well. Other patients who do not present with symptoms directly related to the anemia present instead with symptoms or signs related directly to blood loss. There may be gross blood (hematochezia), which is more common with bleeding sites near the rectum, or black, tarry, metabolized blood (melena) from more proximal sites. Pernicious Anemia Etiology Pernicious anemia is a megaloblastic anemia in which there is abnormal erythrocyte nuclear maturation. Unlike in many other types of anemia such as that resulting from iron deficiency, hemoglobin synthesis is normal. Pernicious anemia is the end result of a cascade of events that are autoimmune in origin. The nervous system is also affected, demonstrating that this is a systemic disease. Besides pernicious anemia, cobalamin deficiency can also be due to bacterial overgrowth in the intestine (because bacteria compete with the host for cobalamin), intestinal malabsorption of vitamin B12 involving the terminal ileum (such as in Crohn disease), surgical removal of the antrum of the stomach (gastrectomy), and, rarely, dietary deficiency, which occurs only in strict vegetarians. Pernicious anemia is most common in older patients of Scandinavian descent and is more commonly found in those of European and African than Asian descent. Pernicious anemia accounts for only a small percentage of patients with anemia, however. The gastric parietal cells are initially affected by an autoimmune phenomenon that leads to two discrete effects: loss of gastric acid (achlorhydria) and loss of intrinsic factor. Pernicious anemia interferes with both the initial availability and the absorption of vitamin B12: Stomach acid is required for the release of cobalamin from foodstuffs, and intrinsic factor is a glycoprotein that binds cobalamin and is required for the effective absorption of cobalamin in the terminal ileum. Evidence for the autoimmune destruction of parietal cells is strong: Patients with pernicious anemia have atrophy of the gastric mucosa, and pathologic specimens show infiltrating lymphocytes, which are predominantly antibody-producing B cells. In addition, 90% or more of patients have antibodies in their serum directed against parietal cell membrane proteins. More than half of patients also have antibodies to intrinsic factor itself or the intrinsic factor-cobalamin complex. What is the most common form of anemia and its most likely cause in a premenopausal woman? Why is the serum ferritin level often not a good indicator of whether anemia is due to iron deficiency? Lastly, corticosteroid therapy, used as firstline therapy for many autoimmune disorders, may reverse the pathologic findings in pernicious anemia. Complete vitamin B12 deficiency develops slowly, even after total achlorhydria and loss of intrinsic factor occur. Cobalamin accepts a methyl group from methyltetrahydrofolate, which leads to the formation of two important intracellular compounds. The first is methylcobalamin, which is required for the production of the amino acid methionine from homocysteine. The second is reduced tetrahydrofolate, which is required as the single-carbon donor in purine synthesis. In cobalamin deficiency, other reduced folates may substitute for tetrahydrofolate (and may explain why pharmacologic doses of folic acid can partially reverse the megaloblastic blood cell changes, but not the neurologic changes, seen in pernicious anemia). However, methyltetrahydrofolate, normally the methyl donor to cobalamin, accumulates. This folate cannot be retained intracellularly because it cannot be polyglutamated; the addition of multiple glutamate residues leads to a charged compound that does not freely diffuse out of the cell. In addition, methionine may serve as a principal donor of methyl groups to these other "substituting" reduced folates; because methionine cannot be produced in cobalamin deficiency, this compounds the problems in purine synthesis. The exact mechanism of the neurologic consequences of pernicious anemia, with demyelination (loss of the myelin sheaths around nerves), is not known. Defects in the methionine synthase pathway have been suggested but not proven experimentally. Instead, observations in cobalamin-deficient gastrectomized rats implicate an imbalance of cytokines and growth factors as a potential mediator of nerve damage. Lack of cobalamin also leads to abnormal myelin synthesis, probably via a deficiency in methionine production (B). The production of succinyl-coenzyme A (CoA) is also dependent on the presence of cobalamin. It is not clear whether a decrease in the production of succinyl-CoA, which may affect fatty acid synthesis, is also involved in the demyelinating disease. The normally tall columnar epithelium is replaced by a very thin mucosa, and there is obvious infiltration of plasma cells and lymphocytes.
Order cheap cleocin gel online
Cardiac Ct beyond coronary angiography: current and emerging noncoronary cardiac applications skin care tools generic 20gm cleocin gel overnight delivery. Current applications and limitations of coronary computed tomography angiography in stable coronary artery disease. Although M-mode has the advantage of high temporal resolution, making it easier to visualize motion of the endocardium, it is nonetheless easier to ensure correct alignment of your measurements. Whatever technique you prefer, be sure to identify end-diastole and end-systole (see box) and the endocardial/epicardial borders correctly. The apical 2-chamber view does not show mitral valve opening very well, and so do not base measurements taken in this view on the timing of mitral valve opening. In the past it has been recommended that such M-mode measurements be taken from leading edge to leading edge, but the improved resolution of contemporary echo machines means that measurements can instead be taken directly from the tissuelood interface. Now trace the endocardial border from the mitral valve annulus all the way down to the apex and then back up to the annulus on the opposite side. Heart failure Heart failure affects 1Ͳ per cent of the adult population and is particularly common in the elderly, affecting 10 per cent of those aged over 70 years. Heart failure is regarded as a clinical syndrome in which patients have the symptoms and signs of heart failure (table 15. Heart failure can be classified as: systolic and/or diastolic acute or chronic left- and/or right-sided high output. It is therefore important to be aware of the limitations of each of the following methods and to use them judiciously. Place the sample volume at the level of the aortic valve annulus, just proximal to the cusps. Using the trace, mark the points where the regurgitant jet velocity reaches 1 m/s and also 3 m/s. At 1 m/s the pressure gradient driving the regurgitant jet is 4 mmHg (Bernoulli equation), and at 3 m/s the gradient is 36 mmHg, giving a change in pressure gradients (dP) between the two velocities of 32 mmHg. Do not use dP/dt if there is acute mitral regurgitation, or if there is significant aortic stenosis or hypertension. The mitral valve leaflets are structurally normal but the annulus is dilated and there is moderate functional mitral regurgitation, with a dP/dt of 986 mmHg/s. If the difference between the onset of aortic and pulmonary flow is 40 ms, significant dyssynchrony is present. If the difference in peak contraction between the two walls is 130 ms, significant dyssynchrony is present. Echo has a key role in the optimisation of device settings following a Crt implant. All the arteries supply branches to the myocardium in their respective territories, and as there is some anatomical variation from one person to the next, there can be a little variability in which vessel is responsible for supplying blood to each territory. Normal wall motion during systole is indicated by an endocardial excursion >5 mm and by wall thickening >50 per cent. Inspect each segment in turn, where possible in two separate views, and score it according to its motion: X = unable to interpret (suboptimal image quality) 1 = normokinetic 2 = hypokinetic Coronary artery disease and regional left ventricular function 137 3 = akinetic 4 = dyskinetic 5 = aneurysmal. An acute coronary syndrome occurs when an atherosclerotic plaque ruptures, exposing the lipid-rich core to the bloodstream. Myocardial ischaemia is frequently assessed by stress echo (see Chapter 8), in which any changes in wall motion are assessed in response to exercise or pharmacological stress. In the classical ischaemic response, the myocardium is normokinetic at rest but its wall motion worsens on stress. Stress echo can also have an important role following myocardial infarction, identifying areas where the myocardium is still viable. Areas of myocardial necrosis are typically akinetic or hypokinetic at rest and remain unchanged with stress. However, sometimes improvement in wall motion is seen with stress, indicating that the myocardium is still viable but is stunned or hibernating. Stunned myocardium is likely to improve spontaneously with time, whereas hibernating myocardium will usually only improve with coronary revascularization. Echo can help in the differential diagnosis of acute chest pain, which includes not just acute coronary syndromes but also conditions such as aortic dissection (p. Echo is also important in the diagnosis of many of the complications of myocardial infarction, discussed later in this chapter. Symptomatic relief can be obtained with glyceryl trinitrate used as required, and with one or more regular anti-ischaemic agents (betablockers, calcium channel blockers, nitrates, nicorandil, ivabradine or ranolazine). Coronary revascularization has an important role in patients with troublesome symptoms or a high risk of coronary events. Echo is also important for assessing the rV in cases of suspected rV infarction (which can occur with an inferior myocardial infarction or on its own). Papillary muscle rupture Acute severe mitral regurgitation can occur following myocardial infarction as a result of papillary muscle dysfunction or rupture. Patients may present with acute pulmonary oedema, cardiogenic shock and a new systolic murmur. Use Doppler assessment to examine the nature and extent of mitral regurgitation, as outlined in Chapter 20. Surgeons are particularly interested in the size and function of the rV which helps predict prognosis. Look for evidence of mural thrombus, which can form as a consequence of impaired wall motion. Embolic risk is generally low, but is greater with mobile or protuberant thrombus than it is with laminated thrombus. Ventricular rupture and cardiac tamponade rupture of the ventricular free wall is uncommon (occurring in 2. However, sometimes the ventricular rupture can be contained by adhesions or thrombosis, causing a more stable (but nonetheless still extremely dangerous) situation which can, if time permits, be repaired surgically. Assess the location and dimensions of the rupture (most cases involve the anterior wall) and the pericardial effusion, and look for features of cardiac tamponade. Patients may present with pleuritic chest pain, fever and a pericardial friction rub. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. Management of acute myocardial infarction in patients presenting with persistent St-segment elevation. This page intentionally left blank 17 Left ventricular diastolic function chapter the diagnosis and management of diastolic heart failure has always been somewhat controversial because it is harder to characterize, and the treatment strategies are less well studied than for systolic heart failure. It certainly seems that there is significant overlap between systolic and diastolic dysfunction and they should not be regarded as mutually exclusive entities. A sweep speed of 25 or 50 mm/s is used initially to look for respiratory variation in peak E and A wave velocities. E wave deceleration time is the time period between the peak of the E wave and the end of the E wave (measured by extrapolating the E wave deceleration slope down to the baseline), and is normally 150Ͳ00 ms. Pulmonary vein flow normally consists of three components: the S wave represents forward flow into the left atrium during ventricular systole, and the smaller D wave represents forward flow during ventricular diastole. Colour doppler Use colour Doppler to look for any coexistent mitral regurgitation. Pressure half-time is a measure of the rate of fall in pressure across the valve specifically, the time taken for the transmitral pressure gradient to fall to half of its initial peak value. An echo Doppler trace displays flow velocity rather than pressure, and the mathematical relationship between pressure and flow velocity means that a fall in pressure gradient to 0. Studies have shown that a mitral valve area of 1 cm2 has a pressure half-time of approximately 220 ms, and that the relationship between pressure half-time and valve area is linear. Pressure half-time is also influenced by the acute haemodynamic changes that occur following mitral valvuloplasty (see p. Continuity equation Mitral valve area can also be calculated using the continuity equation. Failure to planimeter the mitral leaflets at their tips, leading to an overestimation of orifice area.