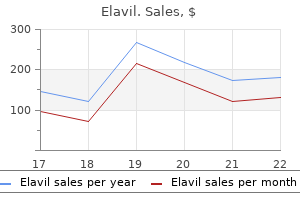
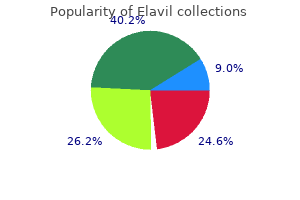
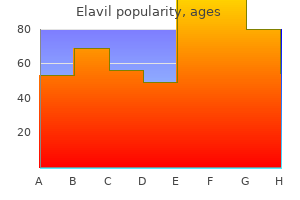
Buy cheap elavil 10 mg
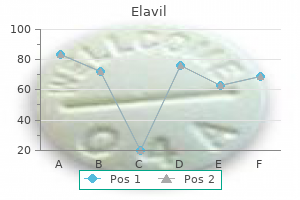
Perforated diverticular disease is staged using the Hinchey classification system laser pain treatment reviews elavil 50 mg visa. This staging system was developed to predict outcomes following the surgical management of complicated diverticular disease. In complicated diverticular disease with fistula formation, common locations include cutaneous, vaginal, or vesicle fistulas. These conditions present with either passage of stool through the skin or vagina or the presence of air in the urinary stream (pneumaturia). Patients should be instructed to eat a fiber enriched diet that includes 30 g of fiber each day. Supplementary fiber products such as Metamucil, Fiber con, or Citrucel are useful. The incidence of complicated diverticular disease appears to be increased in patients risk of perforation requiring a colostomy. However, patients on immunosuppressive therapy, in chronic renal failure, or with a collagenvascular disease have a fivefold greater risk of perforation during recurrent attacks. Surgical therapy is indicated in all lowsurgical risk patients with complicated diverticular disease. The goals of surgical management of diverticular disease include controlling sepsis, eliminating com plications such as fistula or obstruction, removing the diseased colonic segment, and restoring intestinal continuity. These goals must be obtained while minimiz ing morbidity rate, length of hospitalization, and cost in addition to maximizing survival and quality of life. Table 19-3 lists the operations most commonly indicated based upon Hinchey classification and the predicted morbidity and mortality rates. Surgical objec tives include removal of the diseased sigmoid down to the rectosigmoid junction. The current options for uncom plicated diverticular disease include an open sigmoid resection or a laparoscopic sigmoid resection. Laparoscopic techniques have been employed for complicated diverticular disease; however, higher conversion rates to open techniques have been reported. Percutaneous drainage is recommended for abscesses 5 cm with a welldefined wall that is accessible. Con traindications to percutaneous drainage are no percu taneous access route, pneumoperitoneum, and fecal peritonitis. If the patient has significant comorbidities, making operative intervention risky, a limited procedure including intraoperative peritoneal lavage (irrigation), omental patch to the oversewn perforation, and proxi mal diversion of the fecal stream with either an ileos tomy or transverse colostomy can be performed. A limited approach to these patients is associated with a decreased mortality rate. It is often associated with a redundant sigmoid colon, pelvic laxity, and a deep rectovaginal septum (pouch of Douglas). Initially, rectal prolapse was felt to be the result of early internal rectal intussusception, which occurs in the upper to mid rectum. However, only 1 of 38 patients with internal prolapse followed for >5 years developed full-thickness prolapse. Recurrent diverticular disease develops in patients following inadequate surgical resection. Women with rectal prolapse have a higher incidence of associated pelvic floor disorders including urinary incontinence, rectocele, cystocele, and enterocele. Anatomy and pathophysiology Rectal prolapse (procidentia) is a circumferential, fullthickness protrusion of the rectal wall through the anal In external prolapse, the majority of patient complaints include anal mass, bleeding per rectum, and poor perianal hygiene. Other associated findings include outlet obstruction (anismus) in 30%, colonic inertia in 10%, and solitary rectal ulcer syndrome in 12%. Office evaluation is best performed after the patient has been given an enema, which enables the prolapse to protrude. An important distinction should be made between full-thickness rectal prolapse and isolated mucosal prolapse associated with hemorrhoidal disease. Mucosal prolapse is known for radial grooves rather than circumferential folds around the anus and is due to increased laxity of the connective tissue between the submucosa and underlying muscle of the anal canal. If rectal prolapse is associated with chronic constipation, the patient should undergo a defecating proctogram and a sitzmark study. In colonic inertia, a sitzmark study will demonstrate retention of >20% of markers on abdominal x-ray 5 days after swallowing. Full-thickness prolapse associated with redundant rectosigmoid and deep pouch of Douglas (C, D, sagittal view). Transabdominal procedures can be performed effectively with laparoscopic techniques without increased incidence of recurrence. The goal of the transabdominal approach is to restore normal anatomy by removing redundant bowel and reattach ing the supportive tissue of the rectum to the presacral fascia. Colon resection, in gen eral, is reserved for patients with constipation and outlet obstruction. Previously, the presence of internal rectal prolapse identified on imaging studies has been considered a nonsurgical disorder and biofeedback was recom mended. However, only onethird of patients will have successful resolution of symptoms from biofeedback. A circular stapling device is inserted through the anus; the internal prolapse is identified and ligated with the stapling device. Transabdominal approaches have been associated with lower recurrence rates, but some patients with signifi cant comorbidities are better served by a transperineal approach. Common transperineal approaches include a trans anal proctectomy (Altmeier procedure), mucosal proctectomy (Delorme procedure), or placement of a Tirsch wire encircling the anus. The goal of the trans perineal approach is to remove the redundant rec to sigmoid colon. To reduce the internal prolapse and close any rectovaginal septal defect, the pouch of Douglas is opened and mesh is secured to the anterolateral rectum, vaginal fornix, and sacrum. Medical conditions known to contribute to the development of fecal incontinence are listed in Table 19-4. Anatomy and pathophysiology the anal sphincter complex is made up of the internal and external anal sphincter. The majority of patients who suffer from fecal incontinence following obstetric injury do so several years following the birth of their last child. Presentation and evaluation Patients may suffer with varying degrees of fecal incontinence. Beyond the immediate problems associated with fecal incontinence, these patients are often withdrawn and suffer from depression. For this reason, quality-of-life measures have become an Mesh is secured to the anterior and lateral portion of the rectum, the vaginal fornix, and the sacral promontory, allowing for closure of the rectovaginal septum and correction of the internal prolapse. In both procedures, recurrence at 1 year was low (<10%) and symptoms improved in more than threefourths of patients. An anatomic sphincter defect may occur in up to 32% of women following childbirth regardless of visible damage to the perineum. Risk factors at the time of delivery include prolonged labor, the use of forceps, and the important component in the evaluation of patients with fecal incontinence. Anal manometry measures resting and squeeze pressures within the anal canal using an intraluminal waterperfused catheter. Pudendal nerve studies evaluate the function of the nerves innervating the anal canal using a finger electrode placed in the anal canal. Stretch injuries to these nerves will result in a delayed response of the sphincter muscle to a stimulus, indicating a prolonged latency. Finally, ultrasound will evaluate the extent of the injury to the sphincter muscles before surgical repair. The majority of patients with fecal incontinence will have a degree of urinary incontinence. For this reason, patients may present with symptoms of obstructed defecation as well as fecal incontinence. Careful evaluation including cinedefecography should be performed to search for other associated defects.
Proven 25mg elavil
The etiology of squamous cell esophageal cancer is related to excess alcohol consumption and/or cigarette smoking midsouth pain treatment center oxford ms order elavil with paypal. Adenocarcinomas arise within dysplastic columnar epithelium in the distal esophagus. Even before frank neoplasia is detectable, aneuploidy and p53 mutations are found in the dysplastic epithelium. These adenocarcinomas behave clinically like gastric adenocarcinoma and now account for >70% of esophageal cancers. By the time these symptoms develop, the disease is usually incurable, since difficulty in swallowing does not occur until >60% of the esophageal circumference is infiltrated with cancer. The disease most commonly spreads to adjacent and supraclavicular lymph nodes, liver, lungs, pleura, and bone. Tracheoesophageal fistulas may develop as the disease advances, leading to severe suffering. As with other squamous cell carcinomas, hypercalcemia may occur in the absence of osseous metastases, probably from parathormone-related peptide secreted by tumor cells. Smaller, potentially resectable tumors are often poorly visualized despite technically adequate esophagograms. Because of this, esophagoscopy should be performed in all patients suspected of having an esophageal abnormality, to visualize the tumor and to obtain histopathologic confirmation of the diagnosis. A thorough examination of the fundus of the stomach (by retroflexing the endoscope) is imperative as well. Endoscopic biopsies of esophageal tumors fail to recover malignant tissue in one-third of cases because the biopsy forceps cannot penetrate deeply enough through normal mucosa pushed in front of the carcinoma. Cytologic examination of tumor brushings complements standard biopsies and should be performed routinely. Positron emission tomography scanning provides a useful assessment of resectability, offering accurate information regarding spread to mediastinal lymph nodes. Routine contrast radiographs effectively identify esophageal lesions large enough to cause symptoms. In contrast to benign esophageal leiomyomas, which result in esophageal narrowing with preservation of a normal mucosal pattern, esophageal carcinomas show ragged, ulcerating changes in the mucosa in association with deeper infiltration, the prognosis for patients with esophageal carcinoma is poor. Fewer than 5% of patients survive 5 years after the diagnosis; thus, management focuses on symptom control. Such esophagectomies have been associated with a postoperative mortality rate of approximately 5% due to anastomotic fistulas, subphrenic abscesses, and respiratory complications. The evaluation of chemotherapeutic agents in patients with esophageal carcinoma has been hampered by ambiguity in the definition of "response" and the debilitated physical condition of many treated individuals. Combination chemotherapy and radiation therapy as the initial therapeutic approach, either alone or followed by an attempt at operative resection, seems to be beneficial. When administered along with radiation therapy, chemotherapy produces a better survival outcome than radiation therapy alone. The use of preoperative chemotherapy and radiation therapy followed by esophageal resection appears to prolong survival as compared with controls in small, randomized trials, and some reports suggest that no additional benefit accrues when surgery is added if significant shrinkage of tumor has been achieved by the chemoradiation combination. Approaches to palliation include repeated endoscopic dilatation, the surgical placement of a gastrostomy or jejunostomy for hydration and feeding, and endoscopic placement of an expansive metal stent to bypass the tumor. Endoscopic fulguration of the obstructing tumor with lasers is the most promising of these techniques. Nonetheless, 21,000 new cases of stomach cancer were diagnosed in the United States, and 10,570 Americans died of the disease in 2010. Gastric cancer incidence has decreased worldwide but remains high in Japan, China, Chile, and Ireland. Migrants from high- to lowincidence nations maintain their susceptibility to gastric cancer, while the risk for their offspring approximates that of the new homeland. The diffuse carcinomas occur more often in younger patients, develop throughout the stomach (including the cardia), result in a loss of distensibility of the gastric wall (so-called linitis plastica, or "leather bottle" appearance), and carry a poorer prognosis. Intestinal-type lesions are frequently ulcerative, more commonly appear in the antrum and lesser curvature of the stomach, and are often preceded by a prolonged precancerous process, often initiated by Helicobacter pylori infection. While the incidence of diffuse carcinomas is similar in most populations, the intestinal type tends to predominate in the high-risk geographic regions and is less likely to be found in areas where the frequency of gastric cancer is declining. In the United States, 30% of gastric cancers originate in the distal stomach, 20% arise in the midportion of the stomach, and 37% originate in the proximal third of the stomach. Etiology the long-term ingestion of high concentrations of nitrates in dried, smoked, and salted foods appears to be associated with a higher risk. The nitrates are thought to be converted to carcinogenic nitrites by bacteria (Table 49-2). Helicobacter pylori infection Endogenous factors favoring growth of nitrate-converting bacteria in the stomach: Decreased gastric acidity Prior gastric surgery (antrectomy) (15- to 20-year latency period) Atrophic gastritis and/or pernicious anemia Prolonged exposure to histamine H2-receptor antagonists a Hypothesis: Dietary nitrates are converted to carcinogenic nitrites by bacteria. Serial endoscopic examinations of the stomach in patients with atrophic gastritis have documented replacement of the usual gastric mucosa by intestinal-type cells. This process of intestinal metaplasia may lead to cellular atypia and eventual neoplasia. Since the declining incidence of gastric cancer in the United States primarily reflects a decline in distal, ulcerating, intestinal-type lesions, it is conceivable that better food preservation and the availability of refrigeration to all socioeconomic classes have decreased the dietary ingestion of exogenous bacteria. Gastric ulcers and adenomatous polyps have occasionally been linked, but data on a cause-and-effect relationship are unconvincing. The inadequate clinical distinction between benign gastric ulcers and small ulcerating carcinomas may, in part, account for this presumed association. In keeping with the stepwise model of carcinogenesis, K-ras mutations appear to be early events in intestinaltype gastric cancer. C-met expression is amplified in about 1 in 5 cases and correlates with advanced stage. Epigenetic changes (especially increased methylation) has been correlated with higher risk of invasive disease. Beta-catenin has been found in the nucleus of tumor cells at the leading edge of invasion. Clinical features Gastric cancers, when superficial and surgically curable, usually produce no symptoms. Anorexia, often with slight nausea, is very common but is not the usual presenting complaint. Weight loss may eventually be observed, and nausea and vomiting are particularly prominent with tumors of the pylorus; dysphagia and early satiety may be the major symptoms caused by diffuse lesions originating in the cardia. Gastric carcinomas spread by direct extension through the gastric wall to the perigastric tissues, occasionally adhering to adjacent organs such as the pancreas, colon, or liver. A careful assessment is of particular importance in patients with atrophic gastritis or pernicious anemia. Diagnosis A double-contrast radiographic examination is the simplest diagnostic procedure for the evaluation of a patient with epigastric complaints. The use of double-contrast techniques helps to detect small lesions by improving mucosal detail. The stomach should be distended at some time during every radiographic examination, since decreased distensibility may be the only indication of a diffuse infiltrative carcinoma. Although gastric ulcers can be detected fairly early, distinguishing benign from malignant lesions radiographically is difficult. The anatomic location of an ulcer is not in itself an indication of the presence or absence of a cancer. Some physicians believe that gastroscopy is not mandatory if the radiographic features are typically benign, if complete healing can be visualized by x-ray within 6 weeks, and if a follow-up contrast radiograph obtained several months later shows a normal appearance. However, we recommend gastroscopic biopsy and brush cytology for all patients with a gastric ulcer in order to exclude a malignancy. Since gastric carcinomas are difficult to distinguish clinically or radiographically from gastric lymphomas, endoscopic biopsies should be made as deeply as possible, due to the submucosal location of lymphoid tumors. TreaTmenT Gastric Adenocarcinoma Complete surgical removal of the tumor with resection of adjacent lymph nodes offers the only chance for cure.
Order 50 mg elavil with amex
Her past medical history is significant only for hypothyroidism for which she takes Review and Self-Assessment 91 pain treatment methods elavil 75 mg amex. A 42-year-old man with cirrhosis related to hepatitis C and alcohol abuse has ascites requiring frequent large-volume paracentesis. Echocardiography is the gold standard for diagnosing constrictive pericarditis as a cause of cirrhosis. Prolonged passive congestion from right-sided heart failure results first in congestion and necrosis of portal triads, resulting in subsequent fibrosis. Venoocclusive disease can be confused with cardiac cirrhosis and is a major cause of morbidity and mortality in patients undergoing liver transplantation. The patient has a medical history of diabetes mellitus, hypertriglyceridemia, and hypertension. He has never had a blood transfusion and has been in a monogamous sexual relationship for 30 years. He has stigmata of chronic liver disease including spider angiomata and caput medusa. He undergoes liver biopsy, which shows fibrosis in a perivenular and perisinusoidal distribution. As opposed to individuals with metabolic syndrome alone, these individuals do not show significant insulin resistance. The aspartate aminotransferase is commonly elevated to more than twice the alanine aminotransferase level. You are asked to consult on a 62-year-old white female with pruritus for 4 months. She has intermittent nausea but no vomiting and denies changes in her bowel habits. There is no history of prior alcohol use, blood transfusions, or illicit drug use. Her past medical history is significant only for hypothyroidism, for which she takes levothyroxine. She is diagnosed with a gastric ulcer and is treated appropriately for Helicobacter pylori. During the course of her evaluation for her abdominal pain, the patient had a right upper quadrant ultrasound that demonstrated the presence of gallstones. She is requesting your opinion regarding whether treatment is 702 Review and Self-Assessment 98. Individuals with cholangiocarcinoma should be referred early for consideration of liver transplantation. Reinfection with hepatitis B typically occurs in 35% or more of patients with liver transplantation. The most common indication for liver transplantation is chronic hepatitis B infection. Upon review of the ultrasound report, there were numerous stones in the gallbladder, including in the neck of the gallbladder. The only reason to proceed with cholecystectomy is the development of gallstone pancreatitis or cholangitis. A 62-year-old man has been hospitalized in intensive care for the past 3 weeks following an automobile accident resulting in multiple long-bone fractures and acute respiratory distress syndrome. His laboratory studies demonstrated a rise in his liver function tests, bilirubin, and alkaline phosphatase. A 55-year-old male with cirrhosis is seen in the clinic for follow-up of a recent hospitalization for spontaneous bacterial peritonitis. Besides complications of end-stage liver disease, he has well-controlled diabetes mellitus and had a basal cell carcinoma resected 5 years ago. The cirrhosis is thought to be due to alcohol abuse, and his last drink of alcohol was 2 weeks ago. He is not a transplant candidate now, but may be after a sustained period of proven abstinence from alcohol. A 27-year-old woman is admitted to the hospital with acute-onset severe right upper quadrant pain that radiates to the back. Her labs show a marked elevation in amylase and lipase, and acute pancreatitis is diagnosed. Which of the following is the best first test to demonstrate the etiology of her pancreatitis A 58-year-old man with severe alcoholism is admitted to the hospital with acute pancreatitis. On examination he has severe epigastric and right upper quadrant tenderness and decreased bowel sounds, and appears uncomfortable. Enteral feeding with a nasojejunal tube has been demonstrated to have fewer infectious complications than total parenteral nutrition in the management of patients with acute pancreatitis. Patients requiring surgical removal of infected pancreatic pseudocysts should be treated with total parental nutrition. Total parenteral nutrition has been shown to maintain integrity of the intestinal tract in acute pancreatitis. A 54-year-old man is admitted to the intensive care unit with severe pancreatitis. Which of the following medications has been shown to be effective in the treatment of acute necrotizing pancreatitis Which of the following statements is true regarding enteral feeding in acute pancreatitis A 47-year-old woman presents to the emergency department with severe mid-abdominal pain radiating to her back. She has had two episodes of emesis of bilious material since the pain began, but this has not lessened the pain. She currently rates the pain as a 10 out of 10 and feels the pain is worse in the supine position. For the past few months, she has had intermittent episodes of right upper and mid-epigastric pain that occurs after eating but subsides over a few hours. Vital signs are as follows: heart rate 127 beats/min, blood pressure 92/50 mmHg, respiratory rate 20 breaths/min, temperature 37. The chest examination shows dullness to percussion at bilateral bases with a few scattered crackles. The pain with palpation is greatest in the periumbilical and epigastric areas without rebound tenderness. There is no evidence of jaundice, and the liver span is about 10 cm to percussion. He notes the pain has not lasted for more than 48 hours and is not associated with meals. His past medical history is remarkable for peripheral vascular disease and tobacco use. He has stopped all alcohol intake for up to a week at a time in the past without withdrawal symptoms. The abdominal examination shows mild epigastric tenderness without rebound or guarding. The liver span is 12 cm to percussion and palpable 2 cm below the right costal margin. After 3 L of normal saline, her blood pressure comes up to 110/60 mmHg with a heart rate of 105 beats/min. Which of the following statements best describes the pathophysiology of this disease Intrapancreatic activation of digestive enzymes with autodigestion and acinar cell injury B. Distant organ involvement and systemic inflammatory response syndrome related to release of activated pancreatic enzymes and cytokines D. A 64-year-old man seeks evaluation from his primary care physician because of chronic diarrhea. He describes them as markedly foul smelling, and they often leave an oily ring in the toilet. He also notes that the bowel movements often follow heavy meals, but if he fasts or eats low-fat foods, the stools are more formed.
Generic elavil 10 mg with amex
Glossopharyngeal neuralgia produces similar acute neuropathic symptoms in the distribution of the ninth cranial nerve pain treatment center dr mckellar order elavil amex. Swallow ing, sneezing, coughing, or pressure on the tragus of the ear triggers pain that is felt in the base of the tongue, pharynx, and soft palate and may be referred to the temporomandibular joint. Neuritis involving the max illary and mandibular divisions of the trigeminal nerve. Likewise, similar symptoms may precede visible lesions of herpes zoster infecting the seventh nerve (RamseyHunt syndrome) or trigemi nal nerve. Coronary ischemia may produce pain exclusively in the face and jaw and, like typical angina pectoris, is usually reproducible with increased myocardial demand. Aching in several upper molar or premolar teeth that is unrelieved by anesthetizing the teeth may point to maxillary sinusitis. Giant cell arteritis is notorious for producing head ache, but it may also produce facial pain or sore throat without headache. Patients with subacute thyroiditis often experience pain referred to the face or jaw before the tender thyroid gland and transient hyperthyroidism are appreciated. Burning mouth syndrome (glossodynia) is present in the absence of an identifiable cause. Clonazepam, alphalipoic acid, and cognitive behavioral therapy have benefited some. Its major components, water and mucin, serve as a cleansing solvent and lubricat ing fluid. The major salivary glands secrete intermittently in response to autonomic stimulation, which is high during a meal but low otherwise. The most common eti ology is medication, especially drugs with anticholiner gic properties, but also alpha and beta blockers, calcium channel blockers, and diuretics. Man agement involves eliminating or limiting drying medi cations, preventive dental care, and supplementing oral liquid. Commercial saliva substitutes or gels relieve dryness but must be supple mented with fluoride applications to prevent caries. Sialolithiasis presents most often as painful swelling but in some instances as just swelling or pain. Promotion of salivary secretion with mints or lemon drops may flush out small stones. In adults, acute bacterial parotitis is typically unilateral and most commonly affects postoperative, dehydrated, and debilitated patients. Staphylococcus aureus including methicillinresistant forms and anaerobic bac teria are the most common pathogens. Chronic bacte rial sialadenitis results from lowered salivary secretion and recurrent bacterial infection. The parotid is the principal salivary gland affected, and the tumor presents as a firm, slow growing mass. Malignant tumors such as mucoepidermoid carcinoma, adenoid cystic carci noma, and adenocarcinoma tend to grow relatively fast, depending upon grade. Radiation ther apy (particularly neutronbeam therapy) is used when surgery is not feasible, and it is used postresection for certain histologic types with a high risk of recurrence. The most common concerns regarding care of den tal patients with medical disease are fear of excessive bleeding for patients on anticoagulants, infection of the heart valves and prosthetic devices from hematogenous seeding of oral flora, and cardiovascular complications resulting from vasopressors used with local anesthetics during dental treatment. Patients undergoing tooth extraction or alveolar and gingival surgery rarely experience uncontrolled bleeding when warfarin anticoagulation is maintained within the therapeutic range currently recommended for preven tion of venous thrombosis, atrial fibrillation, or mechan ical heart valve. Embolic complications and death, however, have been reported during subtherapeutic anticoagulation. Therapeutic anticoagulation should be confirmed before and continued through the pro cedure. Patients at risk for bacterial endocarditis should main tain optimal oral hygiene, including flossing, and have regular professional cleaning. Currently, guidelines rec ommend that prophylactic antibiotics be restricted to those patients at high risk of bacterial endocarditis who undergo dental and oral procedures that involve sig nificant manipulation of gingival or periapical tissue or penetration of the oral mucosa. If unexpected bleeding occurs, antibiotics given within 2 h following the pro cedure provide effective prophylaxis. Hematogenous bacterial seeding from oral infection can undoubtedly produce late prosthetic joint infection and therefore requires removal of the infected tissue. However, evidence that late prosthetic joint infection occurs following routine dental procedures is lacking. For this reason, antibiotic prophylaxis is not recommended before dental surgery in patients with orthopedic pins, screws, and plates. It is, however, advised within the first 2 years after joint replacement for patients who have inflammatory arthropathies, immunosuppression, type 1 diabetes mel litus, previous prosthetic joint infection, hemophilia, or malnourishment. Concern often arises regarding the use of vasocon strictors in patients with hypertension and heart disease. Vasoconstrictors enhance the depth and duration of local anesthesia, thus reducing the anesthetic dose and potential toxicity. Precaution should be taken with patients taking tricyclic antidepressants and nonselective beta blockers because these drugs may potentiate the effect of epinephrine. Elective dental treatments should be postponed for at least 1 month after myocardial infarction, after which the risk of reinfarction is low provided the patient is medically stable. Patients who have suffered a stroke should have elective dental care deferred for 6 months. Most patients affected have received highdose aminobisphosphonate therapy for multiple myeloma or metastatic breast cancer and have undergone tooth extraction or dental surgery. Intraoral lesions appear as exposed yellowwhite hard bone involving the mandi ble or maxilla. Patients slated for aminobisphosphonate therapy should receive preventive dental care that reduces the risk of infection and need for future dentoalveolar surgery. Volatile sulfur compounds resulting from bac terial decay of food and cellular debris account for the 20 malodor. Periodontal disease, caries, acute forms of gin givitis, poorly fitting dentures, oral abscess, and tongue coating are usual causes. A few systemic diseases produce distinctive odors: renal failure (ammo niacal), hepatic (fishy), and ketoacidosis (fruity). If no odor is detectable, then pseudohalitosis or even halitophobia must be considered. In addition, ageassociated fatty replacement of salivary acini may reduce physiologic reserve, thus increasing the risk of xerostomia. Poor oral hygiene often results when vision fails or when patients lose manual dexterity and upperextremity flexibility. This is particularly common for nursing home residents and must be emphasized because regu lar oral cleaning and dental care have been shown to reduce the incidence of pneumonia and mortality in this population. Other risks for dental decay include limited lifetime fluoride exposure and preference by some older adults for intensely sweet foods when taste and olfac tion wane. These factors occur in an increasing propor tion of persons over age 75 who retain teeth that have extensive restorations and exposed roots. Consequently, much or the entire tooth can be destroyed before the process is detected. Healthy adults who have not experienced signifi cant alveolar bone loss by the sixth decade do not typi cally develop significant worsening with advancing age. Complete edentulousness with advanced age, though less common than in previous decades, is still present in approximately 50% of Americans age 85. Edentulousness may also worsen obstructive sleep apnea, particularly in those without symptoms while wear ing dentures. Mastication is restored less predictably, and those expecting dentures to improve oral intake are often disappointed. Dentures require periodic adjustment to accommodate inevitable remodeling that leads to a diminished volume of the alveolar ridge. This may be asymptomatic or painful and is indicated by ery thematous smooth or granular tissue conforming to an area covered by the appliance. Durso the health status of the oral cavity is linked to cardiovascular disease, diabetes, and other systemic illnesses.
Purchase 25mg elavil mastercard
In patients recovering from jaundice pain treatment for pinched nerve buy generic elavil on-line, the urine bilirubin clears prior to the serum bilirubin. Blood ammonia Ammonia is produced in the body during normal protein metabolism and by intestinal bacteria, primarily those in the colon. The liver plays a role in the 342 detoxification of ammonia by converting it to urea, which is excreted by the kidneys. Striated muscle also plays a role in detoxification of ammonia, which is combined with glutamic acid to form glutamine. Patients with advanced liver disease typically have significant muscle wasting, which likely contributes to hyperammonemia in these patients. The ammonia can be elevated in patients with severe portal hypertension and portal blood shunting around the liver even in the presence of normal or near-normal hepatic function. Elevated arterial ammonia levels have been shown to correlate with outcome in fulminant hepatic failure. Serum enzymes the liver contains thousands of enzymes, some of which are also present in the serum in very low concentrations. Enzymes that reflect damage to hepatocytes the aminotransferases (transaminases) are sensitive indicators of liver cell injury and are most helpful in recognizing acute hepatocellular diseases such as hepatitis. Liver cell necrosis is not required for the release of the aminotransferases, and there is a poor correlation between the degree of liver cell damage and the level of the aminotransferases. The normal range for aminotransferases varies widely among laboratories, but generally ranges from 10-40 U/L. Levels of up to 300 U/L are nonspecific and may be found in any type of liver disorder. However, aminotransferase levels decrease quickly, and the liver-function tests rapidly evolve in to one typical of cholestasis. The normal serum alkaline phosphatase consists of many distinct isoenzymes found in the liver; bone; placenta; and, less commonly, small intestine. It is also nonpathologically elevated in children and adolescents undergoing rapid bone growth, because of bone alkaline phosphatase, and late in normal pregnancies due to the influx of placental alkaline phosphatase. Elevation of liver-derived alkaline phosphatase is not totally specific for cholestasis, and a less than threefold elevation can be seen in almost any type of liver disease. In bone diseases, the elevation is due to increased amounts of the bone isoenzymes. In liver diseases, the elevation is almost always due to increased amounts of the liver isoenzyme. If an elevated serum alkaline phosphatase is the only abnormal finding in an apparently healthy person, or if the degree of elevation is higher than expected in the clinical setting, identification of the source of elevated isoenzymes is helpful. First, and most precise, is the fractionation of the alkaline phosphatase by electrophoresis. The second approach is based on the observation that alkaline phosphatases from individual tissues differ in susceptibility to inactivation by heat. Susceptibility to inactivation by heat increases, respectively, for the intestinal, liver, and bone alkaline phosphatases, bone being by far the most sensitive. Values are similarly increased in patients with intrahepatic cholestasis due to druginduced hepatitis; primary biliary cirrhosis; rejection of transplanted livers; and, rarely, alcohol-induced steatohepatitis. Because of this slow turnover, the serum albumin is not a good indicator of acute or mild hepatic dysfunction; only minimal changes in the serum albumin are seen in acute liver conditions such as viral hepatitis, drug-related hepatoxicity, and obstructive jaundice. In hepatitis, albumin levels <3 g/dL should raise the possibility of chronic liver disease. However, hypoalbuminemia is not specific for liver disease and may occur in protein malnutrition of any cause, as well as protein-losing enteropathies, nephrotic syndrome, and chronic infections that are associated with prolonged increases in levels of serum interleukin 1 and/or tumor necrosis factor, cytokines that inhibit albumin synthesis. A general medical clinic study of consecutive patients in whom no indications were present for albumin measurement showed that while 12% of patients had abnormal test results, the finding was of clinical importance in only 0. Globulins are increased in chronic liver disease, such as chronic hepatitis and cirrhosis. In cirrhosis, the increased serum gamma globulin concentration is due to the increased synthesis of antibodies, some of which are directed against intestinal bacteria. This occurs because the cirrhotic liver fails to clear bacterial antigens that normally reach the liver through the hepatic circulation. Diffuse polyclonal increases in IgG levels are common in autoimmune hepatitis; increases >100% should alert the clinician to this possibility. Increases in the IgM levels are common in primary biliary cirrhosis, while increases in the IgA levels occur in alcoholic liver disease. Percutaneous liver biopsy Percutaneous biopsy of the liver is a safe procedure that can be easily performed at the bedside with local anesthesia and ultrasound guidance. Liver biopsy is of proven value in the following situations: (1) hepatocellular disease of uncertain cause, (2) prolonged hepatitis with the possibility of chronic active hepatitis, (3) unexplained hepatomegaly, (4) unexplained splenomegaly, (5) hepatic filling defects by radiologic imaging, (6) fever of unknown origin, (7) staging of malignant lymphoma. Under these circumstances, the biopsy can be performed via the transjugular approach. Ultrasonography Ultrasonography is the first diagnostic test to use in patients whose liver tests suggest cholestasis, to look for the presence of a dilated intrahepatic or extrahepatic biliary tree or to identify gallstones. Ultrasound with Doppler imaging can detect the patency of the portal vein, hepatic artery, and hepatic veins and determine the direction of blood flow. Because of their rapid turnover, measurement of the clotting factors is the single best acute measure of hepatic synthetic function and helpful in both the diagnosis and assessing the prognosis of acute parenchymal liver disease. The prothrombin time may be elevated in hepatitis and cirrhosis as well as in disorders that lead to vitamin K deficiency such as obstructive jaundice or fat malabsorption of any kind. Table 36-1 shows how patterns of liver tests can lead the clinician to a category of disease that will direct further evaluation. Hepatocellular uptake: Uptake of bilirubin by the hepatocyte has carrier-mediated kinetics. This large complex on chromosome 2 contains at least 13 substrate-specific first exons (A1, A2, etc. Unconjugated bilirubin that reaches the gut is partly reabsorbed, amplifying any underlying hyperbilirubinemia. Recent reports suggest that oral administration of calcium phosphate with or without the lipase inhibitor orlistat may be an efficient means to interrupt bilirubin enterohepatic cycling to reduce serum bilirubin levels in this situation. Renal excretion of bilirubin conjugates Unconjugated bilirubin is not excreted in urine, as it is too tightly bound to albumin for effective glomerular filtration and there is no tubular mechanism for its renal secretion. In contrast, the bilirubin conjugates are readily filtered at the glomerulus and can appear in urine in disorders characterized by increased bilirubin conjugates in the circulation. Unconjugated bilirubin ordinarily does not reach the gut except in neonates or, by ill-defined alternative pathways, in the presence of severe unconjugated hyperbilirubinemia [e. In particular, the bone marrow is only capable of a sustained eightfold increase in erythrocyte production in response to a hemolytic stress. Prolonged hemolysis may lead to the precipitation of bilirubin salts within the gallbladder or biliary tree, resulting in the formation of gallstones in which bilirubin, rather than cholesterol, is the major component. Such pigment stones may lead to acute or chronic cholecystitis, biliary obstruction, or any other biliary tract consequence of calculous disease. Ineffective erythropoiesis During erythroid maturation, small amounts of hemoglobin may be lost at the time of nuclear extrusion, and a fraction of developing erythroid cells is destroyed within the marrow. Miscellaneous Degradation of the hemoglobin of extravascular collections of erythrocytes, such as those seen in massive tissue infarctions or large hematomas, may lead transiently to unconjugated hyperbilirubinemia. The resulting unconjugated hyperbilirubinemia resolves with cessation of the medication. As a consequence, most neonates develop mild unconjugated hyperbilirubinemia between days 2 and 5 after birth. Prematurity, often associated with more profound immaturity of hepatic function and hemolysis, can result in higher levels of unconjugated hyperbilirubinemia. A rapidly rising unconjugated bilirubin concentration, or absolute levels >340 mol/L (20 mg/dL), puts the infant at risk for bilirubin encephalopathy, or kernicterus.
Artemisia (Wormwood). Elavil.
- Loss of appetite, indigestion, gallbladder disorders, low acid in the stomach, wounds, insect bites, worm infestations, low sexual desire, spasms, and increasing sweating.
- How does Wormwood work?
- Dosing considerations for Wormwood.
- Are there any interactions with medications?
- What is Wormwood?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96713
Elavil 10 mg cheap
Vaginismus: It is the spasms of the perivaginal and levator ani muscles causes dyspareunia (painful intercourse) but in severe stage it prevents vaginal entry of the penis pain treatment center of greater washington purchase elavil overnight delivery. Culdoscope is an endoscopic instrument inserted through the posterior part of fornix of the vagina ii. It is the procedure of operation by which incision is given in the posterior fornix of the vagina ii. If patient having retroflexed uterus the posterior wall of the uterus may also be pierced. Vaginal trauma: Traumatic laceration of the vagina commonly caused by forceful coitus, by accidents or during child birth, which may cause profuse bleeding. It is the infection of the vagina commonly occurs before puberty and after menopause due to thin delicate epithelium of the vagina. Sometimes anterior wall of the vagina prolapsed and drags the urinary bladder Abdomen and Pelvis 243 produces cystocele or urethra produces urethrocele ii. Indication: When the fetal head is held up in the lower part of the birth canal iii. Direction of incision: It is given in the vaginal outlet posterolaterally to avoid injury of the perineal body. Hymen and its medico legal importance: the hymen has got some medico legal importance, presence or rupture of it indicates whether coitus has taken place or not (though it is not the surest sign). The painful sensation arises due to the tension in the wall which stimulates the contraction reflex and an urging for urgent micturition takes place 2. This pain also referred to the cutaneous areas supplied by the same spinal segments supplying the bladder, i. The non-peritoneal area of the base is known as the external trigone of the bladder. The internal urethral orifice is situated at the level of upper border of symphysis pubis b. Deferent ducts: the triangular area between deferent ducts, separated from the rectum by the rectovesical fascia. Peritoneal Relation It is non-peritoneal but in male up to upper end of the seminal vesicles it is peritoneal. Apex It is connected with the umbilicus by the urachus (below) which forms the median umbilical 244 Human Anatomy for Students. The lateral border lies between the superior surface and the inferolateral surfaces 2. Space of Retzius Definition It is a horse-shoe shaped space present between the anterolateral part of the pelvic wall and the sides of the bladder and prostate. Pubo-vesical ligaments (in female) or Pubo-prostatic ligaments (in male) Situation: Two ligaments situated on each sidemedial and lateral. Lateral ligament extends from the neck of the bladder to the tendinous arch of the pelvic fascia on the lateral wall of the pelvis. Median umbilical fold (one in number): It extends as a sheet cover the median umbilical ligament. Median umbilical ligament or fold It is the remnant of the urachus and developed from the allantois. Medial umbilical folds (two in number): It covers the obliterated umbilical artery. Posterior false ligaments (pair of sacrogenital fold): It extends from the lateral angles, of the base of the bladder to the third sacral vertebra. Bladder bed: It consists of number of structures upon which the urinary bladder is situated. By the inter-ureteric ridge which extends between the two ureteral openings, one on each posterolateral angle of the bladder. It is a linear prominent transverse ridge formed by the mucous membrane which is slightly convexity downwards. Apex It is formed by the internal urethral orifice, directed downwards and forwards. Sides Formed by the uretero-urethric ridges caused by muscle of bell (longitudinal muscle of the ureter). It is tense and smooth due to absence of submucous coat and mucous membrane is firmly adherent to the musculature of the urinary bladder. Uvula Vesicae In male it is a rounded elevation just behind the urethral orifice which projects upwards formed by the median lobe of the prostate. Inferior vesical arteries, branch of anterior division of internal iliac artery 3. Venous Drainage It forms the plexus from the infero-lateral surfaces of the bladder and drains in to the internal iliac veins. Parasympathetic supply: From pelvic splanchnic nerves or nervi erigentes (S2, S3 and S4). In old aged man, the uvula vesicae may be enlarged due to enlargement of prostate and act as ball-valve in the internal urethral orifice to obstruct the outflow of urine. When patient will more strain to pass urine the more will be obstruction and the urinary outflow becomes diminished. As uvula vesicae bulges (due to enlargement of prostate) in the internal urethral orifice the urine trickles on the proximal urethra causes frequency of micturition. During cystoscopic examination the interureteric ridge acts as a guide to identify the ureteric orifices for introduction of catheter in to the orifice of ureter as the ridge is seen pale in color. Superior vesical arteries, branch of anterior division of internal iliac artery Structures of the Bladder From outside-inwards 1. Trigonum vesicae-developed from mesoderm of the caudal part of the two mesonephric ducts. Mucous membrane of the rest part developed from the endoderm of the vesico-urethral part of the cloaca. Musculature and other structures derived from the splanchnic layer of the lateral plate mesoderm around the cloaca. Congenital rectovesical fistula: It is due to the incomplete development of urorectal septum and cloacal duct persists. Ectopia vesicae: In this condition the anterior wall of the bladder is deficient, and interior of the bladder is exposed to the anterior abdominal wall, below the infraumbilical part. Urachal fistula: It is the non-obliteration of allantois in which condition the urine comes out through the umbilicus. Urachal cyst: Sometimes proximal and distal portions of allantois obliterate but the intermediate portion remains patent, which forms urachal cyst. Double bladder: Sometimes it may be found and usually associated with double ureters and urethra. Congenital vesico-vaginal fistula: In this case Mullerian eminence projects in to the vesico-urethral part of the cloaca, and then disintegrates and leads to communicate between the urinary bladder and the vagina. Suprapubic cystostomy: It is done just above the symphysis pubis by puncturing the distended urinary bladder (the bladder is distended with about 300 ml of fluid). In female, due to shorter and more dilatable urethra, small calculi, foreign bodies and growths may be removed through the urethra. Urinary incontinence: It occurs due to the involvement of the motor and sensory supply of the bladder, sphincters and lower motor neurons. Dribbling incontinence: It occurs due to the paralysis of sphincter vesicae results from the lesions of sympathetic motor pathways. Stone in bladder: It causes frequency of micturition especially during the day time (due to movements), with flow interrupted and pain. It is a high frequency electrical current by which the tumor breaks in to small pieces that are washed by the water from the urinary bladder. Rupture of urinary bladder: Rupture of urinary bladder may occur in distended bladder, due to injury in lower abdominal wall. Chronic obstruction in micturition: Progressive chronic obstruction in micturition in prostatic enlargement or urethral stricture causes following: a. It is done to see the interior of bladder after distending the bladder with fluid ii. Beginning From the internal urethral orifice at the apex of trigone of the urinary bladder. Preprostatic Part Situation From the neck of the urinary bladder to the superior aspect of the prostate gland. This part is surrounded by the internal sphincter (sphincter vesicae) contraction of the sphincter to prevent the flow of ejaculation towards the urinary bladder.
Buy discount elavil 25mg
It is important that the dietary counseling remain patient-centered and that the goals be practical bayhealth pain treatment center dover de buy elavil uk, realistic, and achievable. Since portion control is one of the most difficult strategies for patients to manage, the use of preprepared products such as meal replacements is a simple and convenient suggestion. An ongoing area of investigation is the use of lowcarbohydrate, high-protein diets for weight loss. Multiple studies have shown that sustained adherence to the diet rather than diet type is likely to be the best predictor of weight-loss outcome. People tend to ingest a constant volume of food regardless of caloric or macronutrient content. Because of the need for close metabolic monitoring, these diets usually are prescribed by physicians specializing in obesity care. The 2008 Physical Activity Guidelines for Americans recommends that adults should engage in 150 min a week of moderate-intensity or 75 min a week of vigorous-intensity aerobic physical activity performed in episodes of at least 10 min, preferably spread throughout the week. Examples include walking, using the stairs, doing home and yard work, and engaging in sport activities. A high amount of physical activity (more than 300 min of moderate-intensity activity a week) is often needed to lose weight and sustain weight loss. Behavioral Therapy Cognitive behavioral therapy 639 is used to help change and reinforce new dietary and physical activity behaviors. When recommending any behavioral lifestyle change, have the patient identify what, when, where, and how the behavioral change will be performed. Because these techniques are time-consuming to implement, they are often provided by ancillary office staff such as a nurse clinician or registered dietitian. When an antiobesity medication is prescribed, patients should be actively engaged in a lifestyle program that provides the strategies and skills needed to use the drug effectively since this support increases total weight loss. The most thoroughly explored treatment is suppression of appetite via centrally active medications that alter monoamine neurotransmitters. The target site for the actions of anorexiants is the ventromedial and lateral hypothalamic regions in the central nervous system (Chap. In contrast, sibutramine (Meridia) functions as a serotonin and norepinephrine reuptake inhibitor. Unlike other previously used anorexiants, sibutramine is not pharmacologically related to amphetamine and has no addictive potential. Orlistat is a potent, slowly reversible inhibitor of pancreatic, gastric, and carboxylester lipases and phospholipase A2, which are required for the hydrolysis of dietary fat in to fatty acids and monoacylglycerols. The drug acts in the lumen of the stomach and small intestine by forming a covalent bond with the active site of these lipases. Taken at a therapeutic dose of 120 mg tid, orlistat blocks the digestion and absorption of about 30% of dietary fat. Tolerability to the drug is related to the malabsorption of dietary fat and subsequent passage of fat in the feces. These effects include flatus with discharge, fecal urgency, fatty/oily stool, and increased defecation. These side effects generally are experienced early, diminish as patients control their dietary fat intake, and infrequently cause patients to withdraw from clinical trials. Serum concentrations of the fat-soluble vitamins D and E and -carotene may be reduced, and vitamin supplements are recommended to prevent potential deficiencies. Two endocannabinoids have been identified: anandamide and 2-arachidonyl glyceride. The brain endocannabinoid system is thought to control food intake by reinforcing motivation to find and consume foods with high incentive value and to regulate actions of other mediators of appetite. Several large prospective, randomized controlled trials have demonstrated the effectiveness of rimonabant as a weight-loss agent with concomitant improvements in waist circumference and cardiovascular risk factors. An emerging theme in pharmacotherapy for obesity is to target several points in the regulatory pathways that control body weight. Bupropion and naltrexone (Contrave), a dopamine and norepinephrine reuptake inhibitor and an opioid receptor antagonist, respectively, are combined to dampen the motivation/ reinforcement that food brings (dopamine effect) and the pleasure/palatability of eating (opioid effect). Another formulation of bupropion with zonisamide (Empatic) combines bupropion with an anticonvulsant that has serotonergic and dopaminergic activity. Lastly, a formulation of phentermine and topiramate (Qnexa) combines a catecholamine releaser and an anticonvulsant, respectively, that have independently been shown to result in weight loss. Weight-loss surgeries fall in to one of two categories: restrictive and restrictive-malabsorptive. In contrast to previous devices, the diameters of these bands are adjustable by way of their connection to a reservoir that is implanted under the skin. The three restrictive-malabsorptive bypass procedures combine the elements of gastric restriction and selective malabsorption. An abundance of data supports the positive impact of bariatric surgery on obesity-related morbid conditions, including diabetes mellitus, hypertension, obstructive sleep apnea, dyslipidemia, and nonalcoholic fatty liver disease. The rapid improvement seen in diabetes after restrictive-malabsorptive procedures is thought to be due to surgery-specific, weight-independent effects on glucose homeostasis brought about by alteration of gut hormones. These complications typically 642 are treated by endoscopic balloon dilatation and acid suppression therapy, respectively. Therefore, selective deficiencies occur uncommonly unless eating habits become unbalanced. In contrast, the restrictivemalabsorptive procedures increase risk for micronutrient deficiencies of vitamin B12, iron, folate, calcium, and vitamin D. Patients with restrictive-malabsorptive procedures require lifelong supplementation with these micronutrients. Timothy Walsh I Evelyn Attia Anorexia nervosa and bulimia nervosa are characterized by severe disturbances of eating behavior. Both disorders occur primarily among previously healthy young women who become overly concerned with body shape and weight. The disorder often begins as a diet not distinguishable at the outset from those undertaken by many adolescents and young women. As weight loss progresses, the fear of gaining weight grows; dieting becomes stricter; and psychological, behavioral, and medical aberrations increase. It is difficult to distinguish neurochemical, metabolic, and hormonal changes that may have a role in the initiation or perpetuation of the syndrome from those that are secondary to the disorder. The resolution of most of these abnormalities with weight restoration argues against an etiologic role. Individuals who pursue interests that place a premium on thinness, such as ballet and modeling, are at greater risk. Further weight loss is viewed by the patient as a fulfilling accomplishment, whereas weight gain is seen as a personal failure. Patients tend to become socially withdrawn and increasingly committed to work or study, dieting, and exercise. As weight loss progresses, thoughts of food dominate mental life and idiosyncratic rules develop around eating. Gastrointestinal motility is diminished, leading to reduced gastric emptying and constipation. Salivary gland enlargement, which is associated with starvation as well as with binge eating and vomiting, may make the face appear surprisingly full in contrast to the marked general wasting. Acrocyanosis of the digits is common, and peripheral edema can be seen in the absence of hypoalbuminemia, particularly when the patient begins to regain weight. Consumption of large amounts of vegetables containing vitamin A can result in a yellow tint to the skin (hypercarotenemia), which is especially notable on the palms. Laboratory abnormalities Mild normochromic, normocytic anemia is frequent, as is mild to moderate leukopenia, with a disproportionate reduction of polymorphonuclear leukocytes. Dehydration may result in slightly increased levels of blood urea nitrogen and creatinine. Serum transaminase levels may increase, especially during the early phases of refeeding. Hypokalemia, often accompanied by alkalosis, suggests self-induced vomiting or use of diuretics. Hyponatremia is common and may result from excess fluid intake and disturbances in the secretion of antidiuretic hormone.
Purchase elavil us
A high prevalence of gallstones is found among first-degree relatives of gallstone carriers and in certain ethnic populations such as American Indians as well as Chilean Indians and Chilean Hispanics pain medication for a uti buy elavil discount. Although most cholesterol stones have a polygenic basis, there are rare monogenic (mendelian) causes. An additional disturbance of bile acid metabolism that is likely to contribute to supersaturation of bile with cholesterol is enhanced conversion of cholic acid to deoxycholic acid, with replacement of the cholic acid pool by an expanded deoxycholic acid pool. An increased deoxycholate secretion is associated with hypersecretion of cholesterol in to bile. Most individuals with supersaturated bile do not develop stones because the time required for cholesterol crystals to nucleate and grow is longer than the time bile spends in the gallbladder. An important mechanism is nucleation of cholesterol monohydrate crystals, which is greatly accelerated in human lithogenic bile. Accelerated nucleation of cholesterol monohydrate in bile may be due to either an excess of pronucleating factors or a deficiency of antinucleating factors. Cholesterol monohydrate crystal nucleation and crystal growth probably occur within the mucin gel layer. A third important mechanism in cholesterol gallstone formation is gallbladder hypomotility. If the gallbladder emptied all supersaturated or crystal-containing bile completely, stones would not be able to grow. Ultrasonographic studies show that gallstone patients display an increased gallbladder volume during fasting and also after a test meal (residual volume) and that fractional emptying after gallbladder stimulation is decreased. Biliary sludge is a thick, mucous material that, upon microscopic examination, reveals lecithin-cholesterol liquid crystals, cholesterol monohydrate crystals, calcium bilirubinate, and mucin gels. Biliary sludge typically forms a crescent-like layer in the most dependent portion of the gallbladder and is recognized by characteristic echoes on ultrasonography (see below). The presence of biliary sludge implies two abnormalities: (1) the normal balance between gallbladder mucin secretion and elimination has become deranged and (2) nucleation of biliary solutes has occurred. It should be emphasized that biliary sludge can develop with disorders that cause gallbladder hypomotility; i. Two other conditions are associated with cholesterolstone or biliary-sludge formation: pregnancy and rapid weight reduction through a very low-calorie diet. There appear to be two key changes during pregnancy that contribute to a "cholelithogenic state": (1) a marked increase in cholesterol saturation of bile during the third trimester and (2) sluggish gallbladder contraction in response to a standard meal, resulting in impaired gallbladder emptying. Although biliary sludge is a common finding during pregnancy, it is usually asymptomatic and often resolves spontaneously after delivery. Gallstones, which are less common than sludge and frequently associated with biliary colic, may also disappear after delivery because of spontaneous dissolution related to bile becoming unsaturated with cholesterol postpartum. Other important factors known to predispose to cholesterol-stone formation are summarized in Table 45-1. Demographic/genetic factors: Prevalence highest in North American Indians, Chilean Indians, and Chilean Hispanics, greater in Northern Europe and North America than in Asia, lowest in Japan; familial disposition; hereditary aspects 2. Obesity, metabolic syndrome: Normal bile acid pool and secretion but increased biliary secretion of cholesterol 3. Estrogens stimulate hepatic lipoprotein receptors, increase uptake of dietary cholesterol, and increase biliary cholesterol secretion b. Natural estrogens, other estrogens, and oral contraceptives lead to decreased bile salt secretion and decreased conversion of cholesterol to cholesteryl esters 5. Increasing age: Increased biliary secretion of cholesterol, decreased size of bile acid pool, decreased secretion of bile salts 6. Brown pigment stones are composed of calcium salts of unconjugated bilirubin with varying amounts of cholesterol and protein. They are caused by the presence of increased amounts of unconjugated, insoluble bilirubin in bile that precipitates to form stones. Deconjugation of an excess of soluble bilirubin mono- and diglucuronides may be mediated by endogenous -glucuronidase but may also occur by spontaneous hydrolysis. Pigment stone formation is especially prominent in Asians and is often associated with infections in the gallbladder and biliary tree (Table 45-1). Diagnosis Procedures of potential use in the diagnosis of cholelithiasis and other diseases of the gallbladder are detailed in Table 45-2. Failure to image the gallbladder in the presence of biliary ductal visualization may indicate cystic duct obstruction, acute or chronic cholecystitis, or surgical absence of the organ. An ultrasound study showing a distended gallbladder containing a single large stone (arrow), which casts an acoustic shadow. The most specific and characteristic symptom of gallstone disease is biliary colic that is a constant and often long-lasting pain (see below). Biliary colic begins quite suddenly and may persist with severe intensity for 15 min to 5 h, subsiding gradually or rapidly. It is steady rather than intermittent as would be suggested by the word colic, which must be regarded as a misnomer, although it is in widespread use. An episode of biliary pain persisting beyond 5 h should raise the suspicion of acute cholecystitis (see below). Complaints of vague epigastric fullness, dyspepsia, eructation, or flatulence, especially following a fatty meal, should not be confused with biliary pain. Such symptoms are frequently elicited from patients with or without gallstone disease but are not specific for biliary calculi. Biliary colic may be precipitated by eating a fatty meal, by consumption of a large meal following a period of prolonged fasting, or by eating a normal meal; it is frequently nocturnal, occurring within a few hours of retiring. Natural history Gallstone disease discovered in an asymptomatic patient or in a patient whose symptoms are not referable to cholelithiasis is a common clinical problem. The natural history of "silent," or asymptomatic, gallstones has occasioned much debate. A study of predominantly male silent gallstone patients suggests that the cumulative risk for the development of symptoms or complications is relatively low-10% at 5 years, 15% at 10 years, and 18% at 15 years. Patients with diabetes mellitus and gallstones may be somewhat more susceptible to septic complications, but the magnitude of risk of septic biliary complications in diabetic patients is incompletely defined. Patients with very large gallstones (>3 cm in diameter) and patients having gallstones in a congenitally anomalous gallbladder might also be considered for prophylactic cholecystectomy. Laparoscopic cholecystectomy is a minimal-access approach for the removal of the gallbladder together with its stones. Its advantages include a markedly shortened hospital stay, minimal disability, as well as decreased cost, and it is the procedure of choice for most patients referred for elective cholecystectomy. These data indicate why laparoscopic cholecystectomy has become the "gold standard" for treating symptomatic cholelithiasis. In carefully selected patients with a functioning gallbladder and with radiolucent stones <10 mm in diameter, complete dissolution can be achieved in 50% of patients within 6 months to 2 years. The advantages and success of laparoscopic cholecystectomy have largely reduced the role of gallstone dissolution to patients who wish to avoid or are not candidates for elective cholecystectomy. However, patients with cholesterol gallstone disease who develop recurrent choledocholithiasis after cholecystectomy should be on longterm treatment with ursodeoxycholic acid. The organisms most frequently isolated by culture of gallbladder bile in these patients include Escherichia coli, Klebsiella spp. Acute cholecystitis often begins as an attack of biliary pain that progressively worsens. As with biliary colic, the pain of cholecystitis may radiate to the interscapular area, right scapula, or shoulder. Peritoneal signs of inflammation such as increased pain with jarring or on deep respiration may be apparent. Vomiting is relatively common and may produce symptoms and signs 464 of vascular and extracellular volume depletion.