Order generic fluconazole on line
Furthermore fungi definition science order fluconazole, the pattern and severity of side effects vary from drug to drug in the same patient. This observation suggests that a trial with an alternative opioid should be undertaken if intolerable side effects occur during dose titration. Early and appropriate management of side effects may enhance the patient comfort and permit dose escalation to proceed. Opioid-induced constipation is so common that many practitioners believe that laxatives should always be administered concurrently with the opioid. This probably is the best course in the elderly and others with predisposing factors for constipation. In contrast, addiction is a psychological and behavioral syndrome characterized by psychological dependence (drug craving and overwhelming concern with drug acquisition) and aberrant drug-related behaviors, including drug selling or hoarding, acquisition of drugs from nonmedical sources, and unsanctioned dose escalation. Unlike physical dependence, there is little evidence to support the conclusion that otherwise normal patients with painful medical diseases are at substantial risk of developing addiction from the administration of opioids in a medical context. Concern about addiction should never inhibit the aggressive management of this symptom. Suggested Reading Koyyalagunta D: the anticonvulsant compounds in clinical practice. It was not until the early 1970s that Mirsky and others put forth the notion that this group of drugs might have analgesic properties separate and apart from their primary mood-altering purpose. This notion has stood the test of time, and the results of numerous controlled studies have indeed confirmed it. Given the widespread use of the antidepressant compounds as a first-line treatment for pain, one must wonder if the pharmaceutical companies that first introduced these drugs as antidepressants could turn back the hands of time, they would have introduced them as analgesics. This chapter reviews the clinically relevant pharmacology of the various antidepressant compounds that are thought to be useful in the management of pain with an eye to providing the clinician with a practical road map on how to implement, manage, and discontinue therapy with this heterogeneous group of drugs. It is the modification of the middle ring and the alteration of the amine group on the terminal side chain that have resulted in a variety of clinically useful drugs. This lag in onset of clinically demonstrable improvement suggests that there may be more at play than the simple alteration of monoamine transmitter activity. Some investigators have postulated that it is the normalization of a disturbed sleep pattern that is ultimately responsible for the analgesic properties of these drugs rather than their direct action on monoamine transmitter activity per se. Diseases that affect serum proteins or decrease liver function can alter the serum levels of these drugs. Such side effects include xerostomia, xerophthalmia, constipation, urinary retention, tachycardia, decreased gastric emptying, and difficulties in visual accommodation. The orthostatic hypotension is most likely the result of venous blood pooling in the lower extremity and viscera. This potentially dangerous side effect can range from a mild annoying sensation of transient light headedness when arising to near-syncopal episodes, with falling and head injury distinct possibilities. Other side effects include the blocking of the H2 receptors with resultant decrease in gastric acid production as well as a variety of psychomimetic side effects that can be most upsetting to the patient. These psychomimetic side effects include vivid "Technicolor" dreams, prolonged intense dreaming, restlessness, and occasionally psychic activation. Some drugs in this class seem to produce increased appetite and weight gain, whereas others seem to suppress appetite. The unique side effect of priapism, which occurs in approximately 1:10,000 men when taking trazodone, should also be discussed when implementing treatment with this drug. There is no clinical evidence of addiction in the true sense of the word that occurs when these drugs are discontinued, but some drugs in this class have a propensity to cause a variety of symptoms including insomnia, restlessness, lack of energy, and increased cholinergic activity as manifested by excessive salivation and occasional gastrointestinal distress. Although, in general, the dosages that are required to treat pain are lower than those required to treat severe depression, the advent of mail order pharmacies with their 90-day prescription requirements has made overdose a real issue as doses of amitriptyline of greater than 2000 mg can be fatal, well within the amounts prescribed in a 90-day prescription. Further complicating this clinical picture is the potential for grand mal seizures and a hypercholinergic state consisting of mydriasis, urinary retention, dry mouth and eyes, and delirium. Its efficacy as an analgesic has been studied extensively, and there is significant clinical experience in this setting. Blocking both norepinephrine and serotonin, amitriptyline is an efficacious analgesic but with significant side effects including sedation, orthostasis, and most of the troublesome anticholinergic side effects. It should be used cautiously in patients with cardiac conduction defects owing to its propensity to cause tachycardia and should not be used in patients with narrow angle glaucoma and significant prostatism. Due to its sedative properties, amitriptyline should be given as a bedtime dose starting at 10 to 25 mg at bedtime. The drug can be titrated upward as side effects allow in 10- to 25-mg doses, with care being taken to identify the increases in side effects as the dose is raised. In particular, orthostatic hypotension can be insidious in onset as the dosage of the drug is raised and may lead to falls at night when the patient gets up to use the bathroom. If analgesia is not achieved by the time the dose is raised to 150 mg, the patient should be switched to a different antidepressant compound, preferably from another class of drugs, and/or another adjuvant analgesic could be added such as gabapentin if appropriate. If the patient has partial relief of pain, this drug can be carefully titrated upward to a single bedtime dose of 300 mg. Dosed at 10 to 25 mg every morning and titrated upward to a maximum dose of 150 mg, pain relief will usually be seen at doses of 50 to 75 mg after 2 to 3 weeks of therapy, although improvement in sleep may occur much sooner. These drugs should be used cautiously in patients with cardiac arrhythmia and those prone to psychic activation or agitation. Such psychic activation or agitation may be exacerbated by the concomitant administration of steroids, such as epidural steroid injections. Although the unique side of effect of priapism may limit the use of this drug in men, trazodone has the sedating characteristic of amitriptyline, which is desirable in those patients suffering from sleep disturbance as part of their pain symptomatology without the cardiac, anticholinergic, and orthostatic side effects the drug should be started at a bedtime dose of 75 mg and titrated upward to 300 mg as side effects allow. There is no clinical evidence that addiction in the true sense of the word occurs when these drugs are discontinued, but some drugs in this class have a propensity to cause a variety of symptoms, including lack of energy, and decreased serotonergic activity as manifested by constipation and other side effects. There have been remarkably few fatal overdoses reported in the literature or to the U. Moderate overdoses of up to 30 times the daily dose are associated with minor or no symptoms, whereas ingestions of greater amounts typically result in drowsiness, tremor, nausea, gastrointestinal disturbances, and vomiting. As the side effect profile is minimal, it is usually possible to start this drug at the lower range of the dosages thought to provide analgesia, 20 mg, and titrate upward to 60 mg as side effects allow and efficacy demands. It is taken as a once-a-day dose or twice a day at morning and noon to minimize the side effects of tremors or irritability. There are anecdotal reports that paroxetine may have a lower incidence of ejaculatory side effects compared with fluoxetine. Paroxetine should be started at a dose of 20 mg and titrated upward to 40 mg as side effects allow and efficacy dictates. Sertraline is available as an immediate-release tablet or capsule as well as an oral liquid concentrate. Generally well tolerated, sertraline is taken once a day as a morning dose, starting at 50 mg and titrated upward to 200 mg as side effects and efficacy allow. This drug may also have efficacy for those patients suffering from pain who also exhibit obsessivecompulsive tendencies. They also affect other serotonin receptors, most notably in the gut, which probably accounts for their propensity to cause gastrointestinal side effects, especially during initiation of therapy. This class of drugs undergoes rapid first-pass hepatic metabolism by hepatic enzymes and may compete with other drugs for these enzymes, resulting in increased blood levels of Coumadin and the benzodiazepines, among others. These symptoms are usually self-limited and will actually decrease as the gut accommodates to the increased serotonergic milieu. These side effects include alterations in libido, erectile and orgasmic difficulties, ejaculatory delay, and impotence. The central serotonergic syndrome is characterized by hypertension, fever, myoclonus, and seizures. Tachycardia and, in extreme instances, cardiovascular collapse and death may occur. Chapter 348 Antidepressants 591 Serotonin and Noradrenergic Reuptake Inhibitors Venlafaxine (Effexor) Venlafaxine has been shown to be useful as an analgesic in controlled clinical trials. A reasonable starting dose for pain is 25 mg of venlafaxine every 12 hours, with the dose increased by 25 mg every week as side effects allow and efficacy dictates. Despite their efficacy in the treatment of intractable pain, the unpredictable and sometimes severe side effects of this class of drugs limit their use in pain management to patients for whom other, less problematic treatments have failed and are willing and able to strictly adhere to the dietary and medication restrictions required with these drugs. Given the fact that reboxetine acts primarily on the noradrenergic system, theoretically it is most useful for those patients with pain who are also suffering from significant anergia and depression and cannot tolerate desipramine or nortriptyline. Not currently available in the United States but available in more than 50 other countries, reboxetine is given as a 4-mg twice-daily dose titrating upward by 1 mg each week to 10 mg as side effects allow and efficacy dictates.
Cheap 100 mg fluconazole
Oocysts require a period of 1-2 days outside the host in order to undergo sporulation and become infectious to a new host antifungal rinse for laundry 400mg fluconazole otc. Four sporozoites reside within specific treatment of the infection or reconeach of the two sporocysts contained by the stitution of the immune system with highly oocyst. The considering this pathogen in the differential molecular events controlling oocyst forma- diagnosis of a patient with diarrhea. Oocysts are ing the unsporulated oocysts by microscopy passed in the fecal mass unsporulated and are is the definitive diagnostic test of choice. The oocysts require 1-2 days oocysts can be visualized with modified acidto sporulate after reaching the external envi- fast staining and show autofluorescence when ronment. In patients suffering from other varieties of immunosuppression, disease resembles that induced by Cryptosporidium. Protozoa of Minor Medical Importance 179 therapy for infection in adults and ciprofloxacin is a second line agent that is a less effective option. In many areas of the world, these recommendations are difficult or impossible to follow. Cyclospora cayetanensis Cyclospora cayetanensis causes watery diarrhea in humans and is acquired from contaminated food and water. Ortega characterized this organism as a new coccidian species and named this organism, C. A period of 1-2 weeks is required before oocysts sporu- 180 the Protozoa late, and become infectious. Excystation of sporozoites occurs in the small intestine where they attach to epithelial cells. An initial asexual stage divides, then develops into the sexual stage, resulting in the production of unsporulated oocysts that are then shed into the environment. In general, infections tend to decrease in severity and duration after repeated exposures. Post-infectious immunemediated complications such as GuillianBarre syndrome and reactive arthritis have been reported. Protozoa of Minor Medical Importance 181 way through tissue, probably aided by a poreforming protein similar to that of Entamoeba histolytica. One study conducted in Oklahoma showed that the number of pathogenic free-living amoeba species varied throughout the seasons, and were most prevalent in natural water sources. It is presumed that this unusual environment results in the selection of an abundance of thermally-tolerant organisms, including N. Amoebae lyse their 182 the Protozoa normally found in benthic situations, and only gain access to the water column during periods of lake "turn over. Modifications of these behaviors or only using water that does not contain these amoebae could reduce certain risks. Due to the rarity of this disease, most situations leading to infection must be classified as incidents of unlucky circumstance, especially when one considers the number of visits to hot tubs, spas and natural hot springs, and the number of user hours spent relaxing in them. Infection begins with the excystation of the trophozoite under the contact lens after it is applied to the eye. Partial or total blindAcanthamoeba is a free-living amoeba that ness may ensue if left untreated. The trophozoite as well as the cyst Treatment and Prevention are both approximately 13-23 mm in diameter. Protozoa of Minor Medical Importance 183 forward and simple: use only sterile contact lens cleaning solutions. These products are easily obtained at any drug store as over-thecounter preparations. It was discovered in 1986 in the brain of a mandrill, an Old World monkey that died of encephalitis in the San Diego Wildlife Park. Most patients initially present with painless nodules and skin changes at the site of entry, followed by meningeal symptoms, such as fever, stiff neck, and headache that may progress to severe encephalitic manifestations with incomprehensible speech. Other medications such as voriconazole, flucytosine, pentamidine, azithromycin, clarithromycin, trimethoprimsulfamethoxazole and sulfadiazine may have a role in the treatment of this pathogen. Blastocystis hominis Blastocystis hominis is an anaerobic protozoan of uncertain taxonomic status. The cyst is small, measuring 2 to 5 mm in diameter, and is protected by a multilayer cyst wall. Several cases have been described that defy any interpretation other than illness caused by B. Exceptions have been reported, in which the patient was symptomatic with diarrhea and was treated successfully after diagnosis of B. Protozoa of Minor Medical Importance 185 by its impact on other intestinal pathogens. For many years investigators had been unable to identify a cyst form, but cysts were finally identified both in a mouse model and in human feces. Polish journal of microbiology / Polskie Towarzystwo Mikrobiologow = the Polish Society of Microbiologists 2004, 53 Suppl, 55-60. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 1996, 22 (4), 611-5. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 1998, 26 (5), 1218-9. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 1996, 22 (5), 809-12. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997, 91 (2), 214-5. Water science and technology: a journal of the International Association on Water Pollution Research 2003, 47 (3), 117-22. Drug resistance updates: reviews and commentaries in antimicrobial and anticancer chemotherapy 2004, 7 (1), 41-51. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 1995, 20 (5), 1207-16. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology 2004, 23 (5), 399-402. Three years earlier, William Boog Leishman had made similar observations from a British soldier in Dum Dum, West Bengal, India, and wrote a description nearly identical to the one generated by Donovan. Leishman also submitted his findings to the British Medical Journal back in England. Ronald Ross, then editor of that publication, deduced that each physician had discovered the exact same entity. Slides sent to him by Donovan confirmed the diagnosis as a new parasitic infection. Non-Pathogenic Protozoa Introduction We are constantly confronted with a plethora of microbes whose sole purpose is to colonize us and take advantage of our biochemical systems. The human body can be viewed as a series of ecological niches that select for numerous entities, including viruses, bacteria, fungi, protozoa, helminths, and arthropods. They enter through the gastrointestinal, urogenital, and respiratory tracts, through abrasions, and other portalsw of entry. This is mainly due to the inadequacy of their fundamental biological makeup, preventing them from thriving on or in us, and the resiliency of our microbiome. Our intestinal tract is another good example of "peaceful" coexistence between our symbiotic microbes and us, harboring some 500 species of "friendly" bacteria. This chapter is devoted to a brief mention of a few of those eukaryotic organisms that we routinely harbor, and which do us no harm. The clinician will undoubtedly receive a laboratory result with the name of one or more of them on it. How these "hitchhiker" species should be approached in the context of the clinical setting is the subject of this brief chapter. Under unusual conditions, a few have been shown to be associated with disease, but have never been implicated as the primary cause of illness. At those times, the clinician has a difficult time determining who did what to whom.
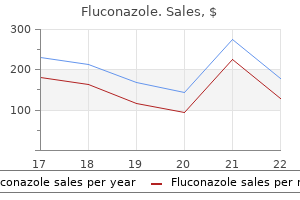
Buy fluconazole cheap online
The conceptual basis of acupuncture finds its origin in the ancient Chinese Taoist religion fungus gnats natural insecticide order fluconazole 200 mg mastercard, which puts forth that all of nature, including humans, is simply an expression of a universal force. Known as yin and yang, this duality is interdependent in that there can be no yin without yang. This interdependent relationality can be best understood by thinking about the relative relationship of Chicago and the rest of the world. Chicago is west of New York City but east of Seattle- that is, Chicago cannot be only east or west, but according to Tao beliefs, must be both east and west simultaneously. Flowing between the yin and yang of all things in nature is a life force called qi or chi. In the human, the omnipresent and dynamic life force flows through a series of pathways known as meridians. Traditional Chinese Medicine states that when there is an imbalance between the flow of oi, then disease may occur. It is believed that by inserting acupuncture needles into one or more of over 300 special acupuncture points along these meridians, the flow of oi can be adjusted to return the yin and yang to a state of equilibrium consistent with health. This physiologic effect is thought to be mediated via the release of endorphins and enkephalins in both the spinal cord and brain, especially in the periaqueductal gray area of the midbrain. Although most patients note only minor discomfort during the insertion of acupuncture needles, an occasional patient complains of pain and refuses further treatment. Infection from improperly sterilized needles has been reported, as has bleeding in patients who are receiving platelet-inhibiting drugs or other anticoagulants. Rare occasions of damage to deep structures from acupuncture needles have also been reported. In: White A, Cummings M, Filshie J [eds]: An Introduction to Western Medical Acupuncture. It has more recently been adopted by the growing group of practitioners who practice alternative and complementary medicine. Originally studied at Yale University in the early 1960s, biofeedback in its most basic form is a process that is designed to train the patient in techniques that are useful in gaining control of basic autonomic functions including heart rate, blood pressure, skin temperature, muscle tension, and the galvanic response. This is most often accomplished by the use of devices that provide the patient with real-time visual and/or auditory feedback as to the status of the physiologic activity being measured. Theoretically, by providing the patient with clear feedback regarding these physiologic processes of which under ambient conditions the patient is not usually aware, it is believed that the patient can learn to modify these autonomic responses to his or her benefit. Types of devices commonly used to assist in biofeedback training include thermistor skin temperature monitors, electromyographic monitors, galvanic skin response monitors, and heart rate monitors (Table 343-1). These devices range from expensive, computer-driven models used for research to simple hand-held models designed for home use. Thermistor skin temperature monitors are one of the most commonly used biofeedback devices and are particularly amenable for home use. Skin temperature biofeedback is useful in helping train the patient to increase the blood flow to the body part being monitored. This increase in blood flow causes a concomitant increase in skin temperature that can be detected by the skin temperature biofeedback device. Because the increased catecholamine release associated with stress causes a decrease in peripheral blood flow, by training the patient to increase peripheral blood flow, stress reduction can be theoretically accomplished. This technique has been extended to other diseases that worsen with stress, such as hypertension, ulcers, asthma, and headaches. The electromyographic biofeedback device is also commonly used to treat pain and associated muscle spasm, as well as other diseases that tend to worsen with stress, such as asthma, headaches, and ulcers. The electromyographic biofeedback utilizes electrodes to measure muscle tension, and the device provides auditory and/or visual feedback to help train the patient to relax the muscles being monitored. This biofeedback approach is frequently combined with other relaxation techniques. Galvanic skin response biofeedback utilizes electrodes to measure the amount of activity of the sweat glands, which increase their activity when the patient is under stress. The electrogalvanic response that is monitored with the galvanic skin response biofeedback device can be useful in training the patient to relax. This technique has been shown to be useful in the management of stress-related diseases. Auditory and/or visual feedback from the heart rate monitor can assist in training the patient to lower his or her heart rate in response to stress. In general, biofeedback is most useful when used as part of a multidisciplinary treatment plan supervised by a health care professional who is well versed in the relationship between stress and the symptoms being treated. The television screen has a built-in speaker used during the audio instructions and the audio-visual biofeedback. Local anesthetics produce anesthesia by reversibly binding to sodium channels and rendering them inactive. This inactivation of the sodium channel causes depolarization of the nerve and produces a reversible inability of the nerve to propagate a nerve impulse. Recent research has shown that the open state of the sodium channel is the primary site of action of local anesthetics and application of local anesthetics to these open sodium channels produces what is known as a state-dependent block. It is the variations in the aromatic and amine ends that determine the clinically observed properties of a specific local anesthetic under physiologic conditions. Amino amides have an amide link between the intermediate chain and the aromatic end, whereas amino esters have an ester link between the intermediate chain and the aromatic end. These variations in the intermediate chain structure result in significant differences in the two basic classes of local anesthetics. The ester-type local anesthetics are less stable in solution, are rapidly metabolized by plasma pseudocholinesterase, and appear to be associated with rare true allergic reactions. Variables that affect the clinical activity of a given local anesthetic are listed in Table 344-2. It is these properties that give each local anesthetic its unique clinical profile and, to a certain extent, its toxicity profile. The portion of local anesthetic that exists in an ionized and nonionized form when the drug is in equilibrium is unique for each local anesthetic, as is the pH at which this equilibrium occurs. Local anesthetics that have a greater unionized portion at physiologic pH will have a faster onset of action, as it is the nonionized portion of the drug that is able to diffuse across nerve membranes and block sodium channels. It should be noted that this balance is also affected by the pH of the tissues in which the drug is being injected, which explains why infected tissues that have a more acidic pH are harder to block with local anesthetics. Lipid solubility is an extremely important property affecting the clinical profile of local anesthetics, because more than 90% of the nerve cell membrane is composed of lipid and lipid-like substances. As a general rule, lipid solubility is directly proportional to the potency of a given local anesthetic, with increased lipid solubility yielding more rapid diffusion through the nerve cell membrane to allow the blocking of sodium channels. The ease with which a given local anesthetic diffuses through the tissues surrounding a nerve will also affect the time from onset to peak. The more protein bound a local anesthetic, the longer is its duration of action as it attaches itself to protein-rich sodium channels. Conversely, with the exception of cocaine, all local anesthetics produce vasodilatation, which speeds absorption of the local anesthetic. The greater the vasodilating properties of a given local anesthetic, the shorter is its duration of action, all other things being equal. The addition of vasoconstrictors such as epinephrine or Neo-Synephrine to the local anesthetic can help counteract the vasodilating properties of the drug and prolong its duration of action. Ultimately, the toxicity of a given local anesthetic is directly related to the amount of peak circulating levels of the drug. This peak circulating blood level is affected by a number of variables including the chemical structure of the drug, how the drug is distributed, how the drug is metabolized, the speed of administration, the vascularity of the tissue being injected, the presence or absence of vasoconstrictors, and the technique of administration. The distribution of a local anesthetic following its absorption into the bloodstream follows a three-phase model. The first phase is the almost immediate distribution of the drug to highly vascular tissues including the lungs, kidneys, and liver. The second phase is the distribution of the local anesthetic to less vascular skeletal muscle and adipose tissue.
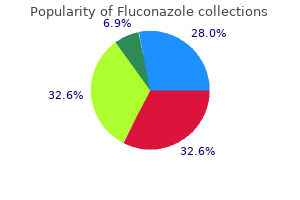
Cheap fluconazole generic
The use of anticonvulsants during pregnancy has been studied extensively in the context of seizure control antifungal burns order cheap fluconazole online, and these data have been extrapolated to the use of this class of drugs in the management of pain. Impaired folate absorption associated with phenytoin and, in all likelihood, carbamazepine and valproic acid is thought to be the cause of a significant increase in neural tube defects in the babies of mothers taking these drugs during early pregnancy. A syndrome known as fetal hydantoin syndrome consisting of mental retardation, microencephaly, and dysmorphic features has been associated with the ingestion of these drugs by parturients. In general, the use of this category of drugs as adjuvant analgesics should be avoided during pregnancy. Medications for the treatment of headache also present special risks for the mother and her fetus. The ergot alkaloids, which are used to abort acute migraine headache, are absolutely contraindicated in pregnancy because of both a propensity to induce uterine contractions and spontaneous abortion and the teratogenic effect on the fetus. Sumatriptan, a selective serotonin agonist drug used to abort acute migraine headache, is also associated with an increased incidence of fetal abnormalities and should not be used during pregnancy. The beta-blocker propranolol, which has gained wide acceptance as a prophylactic agent in the treatment of migraine headache, is probably safer than the other headache drugs mentioned here but should also be avoided, although it is probably safe in the lactating mother. Drugs with high lipid solubility, lower molecular weight, low protein binding, and an active moiety that exists in an unionized state are not only transferred transplacentally but also excreted in breast milk. Although only a small percentage of the maternal dose is excreted in breast milk, the effects of these drugs on the newborn must still be kept in mind. As with pregnancy, an avoidance of any and all drugs whenever possible when the mother is breastfeeding seems a prudent course of action. In general, drugs with longer half-lives and drugs formulated as sustained-release products should be avoided in this setting. Before puberty, headaches are more frequent in boys, but after the onset of puberty, they are more frequent in girls. As with adults, pediatric headaches are most often of benign etiology, but on occasion they can be the harbinger of lifethreatening disease. Despite the relative frequency of these common complaints, most physicians approach the pediatric patient suffering from headache and facial pain with great trepidation. The vast majority of pediatric patients suffering from headache and/or facial pain have a normal physical examination and normal laboratory and radiographic findings. This lack of objective parameters from which physicians may make a diagnosis and initiate treatment runs against the "scientific" approach that they take when evaluating and treating other disease states. Physicians recognize that headache and/or facial pain may represent the harbinger of life-threatening illness; to ignore such symptoms may risk the life of the patient. By gaining an understanding of the common types of headaches and facial pain that affect children and adolescents, physicians can do much to ease their anxiety when evaluating and treating this group of patients. Evaluation of the pediatric patient with headache begins with the taking of a targeted headache history. Special attention should be given to positive responses to factors that cause concern. Obtaining a targeted history is the most important portion of the evaluation of the patient suffering from headache and facial pain. From the history, physicians should be able to recognize the emergence of a specific constellation of symptoms that point to a working diagnosis in most patients with headache and/or facial pain. Failure to obtain a targeted history can lead not only to the implementation Chapter 352 the Pediatric Patient with Headaches 601 of an ineffective treatment plan but also, in some situations, to the failure to recognize life-threatening disease. Obviously, if the targeted history points to a life-threatening disease process, an aggressive course of action is indicated. The following areas of historical information should be explored not only to distinguish sick patients from well ones but also to try to ascertain the specific diagnosis. Age at Onset Headaches that begin in childhood through the second decade of life are most often vascular in nature. Headaches and facial pain that begin later in life are statistically most commonly psychogenic or musculoskeletal ills, such as tension-type headache, nonneuralgic atypical facial pain, and fibromyalgia. Two notable exceptions to this rule are trigeminal neuralgia, which is rarely seen before the third decade unless in association with multiple sclerosis, and temporal arteritis, the incidence of which increases markedly during the fifth and sixth decades. Pitfalls in the age-at-onset portion of the targeted history center around two facts: 1. As one gets older, the chances of systemic illness such as hypertension, glaucoma, stroke, and cancer increase. Children, adolescents, and young adults can all suffer from these systemic illnesses, albeit rarely. Unfortunately, from the point of view of chronologic age, these systemic diseases are rarely suspected in this age group. Chronicity the length of illness sets the direction of the initial history and carries much weight in the "sick" from "well" determination. In general, headaches that have been present for 5 to 6 years are in and of themselves not associated with progressive and life-threatening neurologic disease. This finding leads one to strongly consider a self-limited pain syndrome; hence, the "well" determination. Conversely, the sudden onset of severe headache or the sudden change in the character of a headache or facial pain syndrome that has been stable for many years must be considered to fall in the category of "sick" until proved otherwise. This type of pain manifestation has often been called the "first or worst" syndrome. Patients who fall within this category deserve a high level of concern, and their pain should be viewed as a medical emergency. Pitfalls in evaluation of chronicity include failure to (1) identify ominous changes in a long-standing stable headache or facial pain syndrome; (2) attribute the sudden onset of symptoms to a benign etiology without adequate evaluation. Duration and Frequency of Pain this may provide the best clue to the classification and diagnosis. Although most headache and facial pain syndromes may occur in a seemingly sporadic and random nature, careful questioning may reveal an identifiable pattern to aid in the diagnosis. A headache diary kept for a period of 2 to 3 months may be useful to elucidate this pattern in difficult or confusing cases. In general, vascular headaches and migraine variants such as cyclical vomiting and paroxysmal benign vertigo tend to occur in an episodic fashion, with the duration of pain and associated symptoms ranging from minutes in the case of cluster headache and trigeminal neuralgia to hours in the case of migraine and migraine equivalents. Cluster headache, although extremely rare in the pediatric and adolescent patient population, may be seasonal, with cluster headache having peak occurrences in the spring and fall. Pain that is present on a daily basis and persists for months to years most likely falls under the category of tension-type headache or non-neuralgic atypical facial pain. Onset-to-Peak Time When coupled with the information obtained in the duration and frequency portion of the targeted history, the onset-to-peak time may help further narrow the diagnostic possibilities. A rapid onset-to-peak time (seconds to minutes) should increase suspicion of organic disease. Of particular concern are headaches that worsen with such activities as exercise, Valsalva maneuver, and bending forward. Migraine tends to evolve over several hours, with neurologic symptoms occurring early after onset in the migraine with aura sufferer. Tension-type headache and nonneuralgic atypical facial pain evolve over a period of hours to days and then tend to remain constant. Pitfalls when drawing conclusions regarding the onset-to-peak time of a headache or facial pain syndrome include the special situation in which a syndrome with slow onset-to-peak time. Trigeminal neuralgia is typically described as paroxysmal jablike or shocklike pain in contradistinction to non-neuralgic atypical facial pain, which is more often a dull ache, nagging in character. Tension-type headache is a persistent dull aching, with a constant baseline level of pain and occasional severe exacerbations. Headache associated with lumbar puncture will worsen when the patient assumes the recumbent position. Pitfalls in judging the character of pain include the fact that the patient may be suffering from more than one type of headache and that the most recent or most severe headache may be the one that the patient best remembers even though it is not the most common type for that patient. This is frequently the case in patients with coexistent or mixed headaches with a predominant tension-type component. Premonitory Symptoms and Aurae these are usually associated with vascular headaches, specifically migraine. Among the common premonitory symptoms experienced with migraine are fatigue, elation, depression, changes in libido, craving for certain foods, and abnormal hunger.
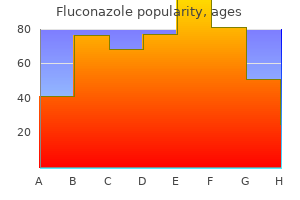
Buy cheap fluconazole 400mg on line
Will present data from human fungus between toes cheap fluconazole 100mg online, animal, and pharmacologic studies that describe the risk of adverse fetal outcomes. Clinical Considerations: this section will present available, relevant information that health care providers can use when counseling pregnant women or prescribing medication during pregnancy. Information included in this section may contain dose adjustments during pregnancy and the postpartum period, adverse reactions (maternal and fetal), and effects of the medication on labor and delivery. Data: this section will include information from animal and human studies that support the risk statements previously presented. For this reason, it is recommended that opioid-dependent parturients avoid acute narcotic withdrawal until after delivery. In this setting, the newborn will almost always also be dependent on opioids and will manifest acute narcotic abstinence syndrome, and a slow tapering schedule of opioids may be required. Although the local anesthetics lidocaine and bupivacaine are generally considered safe for the mother and the fetus, oral mexiletine is considered to be much riskier and should be used only if absolutely necessary. Epidural administration of steroids in combination with lidocaine or bupivacaine is thought to have a reasonably favorable risk-to-benefit ratio, especially in those patients who have failed to respond to less risky measures and are incapacitated by pain. In general, the antidepressant compounds should be avoided as adjuvant analgesics during pregnancy. Some of the selective serotonin reuptake inhibitors have been associated with both fetal cardiovascular abnormalities and cleft lip and palate. The tricyclic antidepressants have also been associated with congenital abnormalities, and, given the usual ameliorating effects of pregnancy on migraine headache, they should be avoided altogether during pregnancy. These premonitory symptoms occur before an attack of migraine without aura (previously called common migraine) or prior to the onset of aura associated with an attack of migraine with aura (previously called classic migraine). Most aurae are ocular symptoms originating in the visual cortex of the occipital lobe. Other examples of aurae include disturbances of smell, feeling, or motor function (Table 352-1). Pitfalls encountered include the fact that many chronic headache sufferers may "adopt" symptoms associated with chronic headaches other than that from which they suffer. These symptoms are gleaned from articles in the lay press and from repeated visits to health care professionals in an attempt to find relief. The acceptance of these symptoms at face value by a physician may lead to an erroneous diagnosis. These symptoms are usually more persistent relative to those associated with migraine. Pain localized to an anatomic structure should be evaluated in the context of common disease entities for that structure. Vascular headache is usually unilateral, although the side may change from attack to attack. Cluster headache is usually localized to the ocular and retro-ocular region, whereas migraine tends to involve the entire hemicranium. Temporal arteritis, which is usually associated with a generalized collagen vascular disease such as polyarteritis nodosum or dermatomyositis in the pediatric and adolescent population, is localized to the temple, but jaw claudication while chewing and generalized aching may confuse the presentation. Tension-type headache is usually bilateral but can be unilateral, often involving the frontal, temporal, and occipital regions. It may manifest as band or caplike tightness in the aforementioned anatomic areas. Trigeminal neuralgia generally involves only one division of the trigeminal nerve (>98%). If the localization of pain overlaps anatomic distribution, non-neuralgic atypical facial pain, referred pain, or local pathology is a more likely explanation. Pitfalls in assessing location include referred pain and sudden changes of anatomic localization during an attack. Special attention should be given to any atypical manifestation or poorly localized pain, because pain referred from tumors of the hypopharynx and posterior fossa can easily be misdiagnosed. Pain that is occipital or unilateral but becomes holocranial during Valsalva maneuver is suggestive of intracranial pathology and probable increased intracranial pressure or may be the result of benign intracranial hypertension. Associated Symptoms the targeted history should include questions regarding other symptoms associated with the painful condition reported. Meningeal signs will occur rapidly after onset of subarachnoid hemorrhage, as will the focal neurologic changes of stroke. Tinnitus or hearing loss in patients with trigeminal neuralgia may indicate an underlying brainstem tumor. Weakness, bowel or bladder difficulties, and sudden visual loss in patients suffering from trigeminal neuralgia may suggest coexisting multiple sclerosis. A pitfall to be avoided is the assumption that all headaches associated with menses are vascular in nature. Many patients may suffer a monthly tension-type headache associated with their menses. Specific questioning regarding infection; previous malignancy; medications that may cause headaches (including topical nitroglycerin); trauma; previous cranial surgery; recent lumbar puncture or myelogram; diseases of the eye, ear, nose, throat, and cervical spine; anemia; thyroid disease; travel out of the country; changes in food, sleep, workplace, and job; and, most important, environmental stress may offer important clues. Precipitating Factors Migraine headache may be triggered by change in diet or sleep habits, tyramine-containing foods, monosodium glutamate, nitrates, motion. Many pediatric and adolescent headache sufferers will give a strong history of motion sickness. Tension-type headache is usually triggered by underlying environmental or physiological stress, depression, fatigue, and, occasionally, abnormalities of the cervical spine. Like migraine, cluster headache may be triggered by alcohol, high altitude, and, occasionally, vasodilating substances. Non-neuralgic atypical facial pain may be caused by stress, bruxism, prolonged dental work, and, occasionally, poorly fitting dental appliances. Past Treatments Many facial pain and headache sufferers have tried various treatment modalities in an effort to obtain pain relief. In evaluating the success or failure of each of these treatment techniques, one may draw a conclusion as to the type of treatment likely to be beneficial as well as the probable diagnosis of the pain syndrome being treated. Pitfalls when exploring this part of the targeted history center around two points: 1. It is often impossible to assess the adequacy of a trial of a given treatment modality in terms of dosage, duration of treatment, and patient compliance. The patient may be using the failure of multiple treatment regimens as a prelude to drug-seeking behavior. This may also manifest itself by the historical finding that the only drugs that have ever been effective in providing pain relief are controlled substances. Environmental Factors As mentioned, contact with vasodilating substances by means of diet or absorption through the skin or respiratory tract may precipitate vascular headache. Stress and pressure in the workplace, video display terminals, industrial fumes, carbon monoxide, high altitude, and airborne contaminants carried by heating and cooling systems also have been implicated as precipitating factors for headache. Previous Diagnostic Tests Physicians must evaluate the adequacy, validity, age, and quality of previous testing when deciding whether or not additional testing is indicated. Factors that would indicate additional testing include a change in a previously stable headache or facial pain problem, onset of a new headache or facial pain problem, a discovery of new systemic illness that may be contributing to or causing the pain problem, or new neurologic findings. If both parents suffer from migraine, there is a 70% to 75% chance that their children will have migraine. If only one parent suffers from the disease, the incidence in offspring drops to 45%. Cluster headache, trigeminal neuralgia, and non-neuralgic atypical facial pain do not appear to be familial in nature. A common pitfall encountered when exploring familial history as part of the targeted history is that headache and facial pain may be a learned behavior, which may explain the clustering of syndromes thought to be nonfamilial throughout several generations of a given family.
Fluconazole 150 mg low price
The virus is transmitted from one person to another by close contact that facilitates the transfer of body fluids antifungal oral rinse 100 mg fluconazole for sale. Intravenous drug abuse is an important mode of transmission because drug users often share the same bloodcontaminated paraphernalia. We have to educate everyone about this disease so that each person can take responsibility for seeing that it spreads no further. Macrophages, which are the tissue-derived descendants of monocytes, can also become infected. Furthermore, fixed tissue phagocytic cells, such as the follicular dendritic cells in the lymph nodes and the microglia of the nervous system (also derived from monocytes), are also sites of infection. Helper T-lymphocytes, macrophages, and their fixed tissue equivalents are essential components of the immune system. Initial infection of an immunologically competent organism stimulates B-cells to produce antibodies, which appear in the circulation within weeks of exposure. Actually, most infected persons enter a latent phase of infection and are asymptomatic for prolonged periods. Cell-mediated and B-cell-mediated immunity ultimately become depressed and the immunosuppressed organism cannot defend itself from infection. Typical symptoms are nonspecific and may include fever, night sweats, nausea, myalgia, headache, sore throat, skin rash, and mild lymph node enlargement. The phase of asymptomatic infection is of variable duration, lasting from a few months to a few years. Persistent generalized lymphadenopathy may develop in patients who are initially asymptomatic. Alternatively, the lymphadenopathy may develop early in the course of infection and persist for months or years. The presence of the virus in the body can be confirmed by additional tests, which are often used to avoid false-positive results. In practice, it is used to determine the ratio of helper T- to suppressor/cytotoxic T-cells. These changes vary with time, the extent of viremia, and the degree of immunosuppression. After some time, the lymph nodes involute and become depleted of lymphocytes, especially in the T-cell-dependent parafollicular zones. Such a microglial response results in the formation of microglial nodules with multinucleated giant cells in the gray matter and subcortical gray matter of the cerebrum. Overshadowing these changes are lesions caused by opportunistic infections, which give rise to meningitis or encephalitis. Of the pathogens affecting the brain, the most important are viruses, such as herpesvirus and cytomegalovirus; fungi, such as Cryptococcus neoformans; and protozoa, such as Toxoplasma gondii. These infections may destroy parts of the brain directly or by occluding blood vessels and causing ischemic infarct. In the initial stages of the disease, the infection is typically localized to the upper respiratory tract and clinically appears to be a nasal infection (rhinitis) or throat infection (pharyngitis). Advanced immunosuppression predisposes the individual to pneumonia, which is often caused by fungi, such as Pneumocystis jiroveci, Aspergillus fumigatus, or Candida albicans. The gastrointestinal tract is also often infected, usually by the same pathogens that infect the lungs. Infections with pathogens that are rarely found in otherwise healthy people are also common. Skin changes may include mild seborrheic dermatitis (itching skin rash) or persistent infections with various viruses (herpesvirus), fungi (dermatomycoses), and bacteria (streptococcal folliculitis). Lymphomas most frequently involve lymph nodes, which appear enlarged, but malignant lymphoid cells may also involve the spleen, liver, and many extranodal sites. Clinically, the disease usually presents in the form of bluish red skin or mucosal nodules. Histologically, these nodules are composed of anastomosing vascular spaces filled with blood. Nevertheless, it may cause extensive bleeding, and the mass lesions may compress vital organs and cause death. However, such drugs are expensive and are not readily available to the citizens of poor countries such as Africa and Asia, who need them the most. However, death can be postponed through vigorous treatment of opportunistic infections and general support of vital functions. Because amyloidosis is a multifactorial disease, which is often related to abnormalities of the immune system or an abnormal response to chronic infection, it is reviewed in this chapter. Instead, amyloid is detected with Congo red, a dye that has the capacity to intercalate into beta-pleated sheets of the fibrils in a peculiar manner. Biochemically, there are several forms of amyloid that are all derived from distinct precursors. It is typically produced by neoplastic B-lymphocytes or plasma cells in patients with malignant lymphoma or multiple myeloma and plasmacytoma. By serum electrophoresis, combined with immunochemistry, it is possible to demonstrate a monoclonal peak of immunoglobulin, or its light chain, in the serum of most patients with this form of amyloidosis. In clinical praxis this form of the disease has traditionally been called primary amyloidosis. This soluble precursor of amyloid is processed by macrophages and laid down in tissues in the form of fibrils that have a beta-pleated structure. Pathology In systemic amyloidosis the deposits of amyloid are seen most often in the wall of small blood vessels. The deposits of amyloid in the blood vessels harden their walls and change their permeability. In the glomeruli, amyloid deposits increase the permeability of the capillary basement membranes, resulting in proteinuria. Deposits of amyloid in the sinusoids of the liver and adrenal glands transform these small caliber vessels into solid, impermeable tubes. Furthermore, the deposits of amyloid compress the parenchymal cells of the liver and adrenals, which combined with ischemia, causes cell atrophy and loss of their specific organ functions. Deposits of amyloid in the heart weaken myocardial contractions and cause heart failure. Clinical Features Amyloidosis presents clinically in many forms, and the symptoms depend predominantly on the organ system involved. Because amyloid deposits may be seen in many small blood vessels, it is customary to take a biopsy sample from the subcutaneous fat, gingiva, or rectum, and examine it microscopically for deposits of amyloid. Kidney or liver tissue that is infiltrated with amyloid is brittle, so the biopsy must be done with extreme care to avoid uncontrollable bleeding. Systemic amyloidosis cannot be treated efficiently and is considered to be a fatal disease. What is the role of the major histocompatibility complex and cytokines in the response to foreign antigens Correlate the pathologic findings and clinical features of respiratory, ocular, and skin manifestations of type I hypersensitivity reactions. What is the pathogenesis and what are the clinical features of graft-versus-host reaction How could one determine whether a unit of donated blood could safely be transfused into a person in need of blood transfusion What is the pathogenesis of hydrops fetus and erythroblastosis fetalis resulting from maternal-fetal Rh incompatibility What clinical-pathological and laboratory findings must be present to allow for the diagnosis of an autoimmune disorder Classify tumors on the basis of their clinical behavior and histopathologic features. List the common forms of carcinoma and sarcoma and their tissue of origin, and describe their benign equivalents. Describe the various approaches to studying the etiology and pathogenesis of cancer. Describe the evidence for viral carcinogenesis in humans, with special emphasis on human papillomavirus, Epstein-Barr virus, and hepatitis B virus. Define oncogenes and tumor suppressor genes and explain their clinical significance. Discuss the changes in cancer incidence that have occurred over the last 100 years and list the three most common forms of cancer in men and women, both past and present. Describe the main contributions of cancer epidemiology to our understanding of neoplasia.
Diseases
- Cardiospasm
- Hidradenitis suppurativa familial
- Ectopia cordis
- Spinocerebellar ataxia amyotrophy deafness
- Carcinoma of the vocal tract
- Fechtner syndrome
- Potter syndrome dominant type
- Microcephaly micropenis convulsions
- Hyaloideoretinal degeneration of wagner
- Infantile spasms
Fluconazole 100mg with visa
The lack of contact inhibition that normally prevents cellular overgrowth results in piling of cells and exuberant proliferation antifungal yogurt generic 200 mg fluconazole fast delivery. Because cancer is a multifactorial disease with numerous forms, there are no general rules; for teaching purposes, however, it is convenient to divide the causes of cancer that have been identified thus far into two major groups: (1) exogenous causes and (2) endogenous causes. The distinction of exogenous and endogenous factors has become even more difficult since the discovery that some human cancer genes, so-called oncogenes, are identical to exogenous viral genes. This procedure, called transfection, results in malignant transformation of previously normal cells. Other data are culled retrospectively into a large series that is then analyzed to provide guidance for future medical practice. Still other data are collected prospectively in carefully planned clinical trials. For example, epidemiologic studies have pointed out that lung cancer is caused by tobacco smoking. Asbestosrelated lung cancer and pleural mesotheliomas were first identified by epidemiologic studies. Some familial forms of breast cancer and colon cancer were also identified by cancer epidemiologists. Tumors removed by surgeons can be explanted in vitro and studied under controlled conditions. Have you ever heard of the cancer cell line HeLa, used in many research laboratories worldwide This best known human cancer cell line was isolated in 1941 from a cancer patient at Johns Hopkins University in Baltimore, Maryland. HeLa stands for the first two letters of her first and last name, Henrietta Lacks, the woman from who the tumor cell line was derived. He hypothesized that scrotal cancer developed because of the adverse effects of soot that was rubbed into the scrotal skin when chimney sweeps straddled the chimneys. This observation was received with incredulity and remained forgotten for many years. In 1875, German epidemiologists noted an increased incidence of skin cancer in chemical industry workers who handled tar, which apparently contains the same possible carcinogens as soot. These Japanese scientists painted tar on the ears of rabbits and induced tumors, thus proving that the tar contained carcinogens. The tumors produced in rabbits were linked to dibenzanthracene, a chemical carcinogen isolated in 1929 from tar. In the 1960s, it was shown that tobacco smoke also contains dibenzanthracene and related polycyclic hydrocarbons, which are all capable of inducing cancer in animals. Industrial Carcinogens Humans are exposed to chemical carcinogens in many situations. The most important exposure is in the workplace, because it can be prevented and the risk of cancer can be minimized through proper industrial hygiene. All these forms of cancer can be prevented through proper protection and precautionary measures, which are prescribed by strict workplace regulations in most developed countries. Experimental studies of cancer performed on animals may serve as models for human tumors. The presumptive carcinogens in the environment, such as various chemicals and viruses, are given to animals to produce tumors or simply to study the adverse effects of a potential carcinogenic agent. For example, rabbits were taught to smoke, which enabled scientists to study the adverse effects of tobacco smoke on the lungs. Human genes isolated from tumors may be inserted into mice and studied further in vivo. Such transgenic animals, so called because they carry genes of another species, are excellent models for the study of human oncogenes. The search for causes of a particular cancer usually begins with clinical observation. Any clues about the causation of that cancer based on clinical reasoning must be validated with epidemiologic studies. The carcinogenic potential of the putative carcinogen may be tested in vitro and in vivo. The final proof is at hand when the cancer can be reproduced in animals injected with that carcinogen. The classic story of such a search for causes of common cancer began in 1775, when the British physician Sir Percival Pott reported that the chimney sweeps in England Drugs as Carcinogens Many drugs successfully used in cancer treatment are also carcinogenic. Secondary cancer that develops in patients treated with alkylating agents, such as nitrogen mustard or cyclophosphamide, is an unfortunate complication of such treatment. However, the risk of developing cancer caused by drugs is low, so it is still better to try to cure a potentially lethal cancer, even if there is a slight chance that another will develop many years after. Nevertheless, a secondary, treatment-related cancer develops in 1% to 2% of patients cured of their primary tumors by chemotherapy. Such carcinogens can be classified according to origin, chemical composition, or their mode of action, as listed in Table 4-3. Aflatoxin B1 is, for example, a very potent natural liver carcinogen produced by the fungus Aspergillus flavus. Polycyclic hydrocarbons, such as 3,4-benzpyrene, are important components of tobacco smoke. Tar and fossil fuels used in the manufacturing of gasoline contain the same polycyclic hydrocarbons. It should be noted that steroid and sex hormones also have a polycyclic structure. Endogenous estrogens produced in excess by the ovary and adrenals in some women can cause cancer of the breast and uterus. Many postmenopausal women who take estrogens must weigh the benefits of these hormones against their possible harmful effects, most notably estrogen promoted development of breast cancer. This type of activation of carcinogens is typically mediated by intestinal bacteria. For example, nitrites and nitrates that are ingested in food are converted into nitrosamines, which may have a carcinogenic effect on the large intestine. The liver is the primary organ involved in the degradation or alteration of carcinogens and other chemicals into other compounds. Aromatic amines derived from azo dyes are metabolized in the body and converted into potential carcinogens that are excreted in urine. The initial step is the conversion of the potentially harmful substance-the procarcinogen-into a carcinogen. This conversion is mediated by enzymes locally active in the exposed cells, or in the liver, which acts as the major conversion site for most exogenous chemicals. In the second step, called promotion, the initiated cells can be stimulated to proliferate. Promotion can be achieved through continuous exposure to the carcinogen or to another substance that is not carcinogenic in itself but that can promote the growth of initiated cells. The promoters must be applied until the cells acquire an ability to proliferate on their own and convert to a new cell type (conversion). Progression, the next phase in cancer development, is marked by an acquisition of new genetic features and expansion of cell clones that do not regress after the carcinogen or the promoter has been removed. Proliferation of divergent clones (clonal expansion) accompanied by mutations in the unstable tumor cell genome leads to tumor cell heterogeneity. Newly formed clones vary from one another: some clones become highly invasive, some acquire a propensity for metastases, whereas still others become dormant and do not proliferate at all for long periods of time. Nevertheless, a selection takes place in favor of the most vital clones and to the cells that have adapted best to adverse conditions. Ultimately these clones outgrow all others, spread thought the body, and kill the host. Persons working in the sun, such as fishermen or farmers, are at an increased risk. Skin cancer is most prevalent in the southern United States and is especially common in Australia. Light-skinned persons are at an increased risk because they lack the protective effects of melanin. Individuals lacking these enzymes, such as those with congenital xeroderma pigmentosum, a genetic defect, are particularly sensitive.
50mg fluconazole amex
Pillows are placed under the chest to allow the lumbar spine to be moderately flexed without discomfort to the patient antifungal diaper cream purchase fluconazole 50mg on line. Landmark Technique To block the L1-4 facets using a landmark technique, the spinous process at the level to be blocked is identified by palpation. Bottom row, Oblique fluoroscopic images showing needle placement for the same blocks. To block the L5 facet, the needle tip is placed under fluoroscopic guidance to rest in the groove between the sacral ala and the superior articular process of the sacrum. A foam wedge placed under the pelvis helps rotate the posterior superior iliac crest out of the way. Intra-articular Approach Lumbar facet block using the intra-articular technique may be performed either blind or under fluoroscopic guidance. Landmark Technique To block the L1-4 facet joints using the landmark technique, the spinous process at the level to be blocked is identified by palpation. Medial drift can allow the needle to enter the epidural, subdural, or subarachnoid space and to traumatize the dorsal root or spinal cord. Lateral drift can allow the needle to pass beyond the lateral border of the vertebra and traumatize the exiting nerve roots. The spinal needle is then advanced through the introducer needle until it either enters the facet joint or again impinges on bone. After the needle is felt to be in satisfactory position, the stylet is removed from the 25-gauge spinal needle, and the hub is observed for blood or cerebrospinal fluid. If the aspiration test is negative, 1 mL of solution is injected slowly through the spinal needle. To block the lumbosacral (L5) facet joint using the intra-articular technique, the previously discussed technique is used, but it may be necessary to Chapter 297 Lumbar Facet Block 485 Med. Fluoroscopic Technique If fluoroscopy is used to block the L1-4 joints, the beam is rotated in a sagittal plane from an anterior to posterior position, which allows identification and visualization of the articular pillars of the respective vertebrae and the adjacent facet joints. The introducer needle is then repositioned under fluoroscopic guidance until this small point is visualized pointing directly toward the inferior aspect of the facet joint to be blocked. Then 2 mL of preservative-free local anesthetic is drawn up in a separate 5-mL sterile syringe. After bony contact is made, the spinal needle is withdrawn and the introducer needle repositioned superiorly, aiming toward the facet joint. The 25-gauge spinal needle is then readvanced through the introducer needle until it enters the target joint. To block the lumbosacral (L5) facet joint using the intra-articular technique, the technique discussed earlier is used, but it may be necessary to move the needle insertion point slightly more inferior and lateral to avoid the posterior superior iliac crest. Placing the needle too medially can result in inadvertent subdural, subarachnoid, or epidural injection. Many patients also complain of a transient increase in lumbar pain after injection into the joint. The lumbar epidural space is 5 to 6 mm at the L2-3 interspace with the lumbar spine flexed. After traversing the skin and subcutaneous tissues, the styletted epidural needle will impinge on the supraspinous ligament, which runs vertically between the apices of the spinous processes. The interspinous ligament that runs obliquely between the spinous processes is next encountered, offering additional resistance to needle advancement. Because the Supraspinous ligament Interspinous ligament Epidural fat Subarachnoid space Ligamentum flavum Arachnoid ligament is made up almost entirely of elastin fibers, there is a continued increase in resistance as the needle traverses the ligamentum flavum, owing to the drag of the ligament on the needle. Lumbar epidural nerve block may be carried out with the patient in a sitting, lateral, or prone position. The sitting position is easier for both the patient and the pain management specialist. This position enhances the ability to identify the midline and also avoids the problem of rotation of the spine inherent in the use of the lateral position, which may make identification of the epidural space difficult. Some investigators believe that the effects of gravity on local anesthetics is enhanced in the sitting position, improving the ability to block the S1 nerve roots, which can be difficult because of their larger size. After the patient is placed in optimal position with the lumbar spine flexed and forearms resting on a padded bedside table, the skin is prepared with an antiseptic solution. Then 1 mL of local anesthetic is used to infiltrate the skin, subcutaneous tissues, and supraspinous and interspinous ligament at the midline. Smaller, shorter needles are being used more frequently with equally good results. The needle stylet is removed and a well-lubricated 5-mL glass syringe filled with preservative-free sterile saline is attached. Alternatively, the physician can simply use a 12-mL plastic syringe filled with the intended injectate for the following loss of resistance maneuver. This approach has the advantage of not attaching and removing the glass syringe with the attendant risk of inadvertently moving the needle out of the epidural space. A small amount of contrast medium may also be injected through the needle to confirm placement within the epidural space. Most experienced pain management specialists do not require the added step to correctly place the needle into the epidural space. When satisfactory needle position is confirmed, a syringe containing 10 to 12 mL of solution to be injected is carefully attached to the needle. If cerebrospinal fluid is aspirated, the epidural block may be repeated at a different interspace. Subsequent nerve blocks are carried out in a similar manner, substituting 40 mg of methylprednisolone for the initial 80-mg dose. Daily lumbar epidural nerve blocks with local anesthetic and/or steroid may be required to treat the previously mentioned acute painful conditions. Chronic conditions such as lumbar radiculopathy, spinal stenosis, vertebral compression fractures, and diabetic polyneuropathy are treated on an every-other-day to once-a-week basis or as the clinical situation dictates. If the lumbar epidural route is chosen for administration of opioids, 5 to 7 mg of preservative-free morphine sulfate formulated for epidural use is a reasonable initial dose in opioid-tolerant patients. More lipid-soluble opioids such as fentanyl must be delivered by continuous infusion via a lumbar epidural catheter. An epidural catheter may be placed into the lumbar epidural space through a Hustead needle to allow continuous infusions. Although some experienced pain practitioners perform this technique without radiographic guidance, many pain practitioners use fluoroscopy to aid in needle placement to help avoid placing the needle too deeply into the spinal canal and inadvertently injecting into the intrathecal space, subdural space, or the spinal cord. Because the procedure is usually done in the prone position, special attention to patient monitoring is mandatory. With the patient in the prone position on the fluoroscopy table, the end plates of the affected vertebra are aligned. The skin is then prepared with an antiseptic solution, and a skin wheal of local anesthetic is placed at a point overlying or just lateral to the tip of the superior articular process of the level below the indicated neural foramen. Failure to impinge on bone at the point may indicate that the needle has passed into and through the spinal canal and rests within the intrathecal space. After this bony landmark is identified, the needle is redirected inferiorly into the targeted spinal nerve canal. Special care should be taken when performing left upper lumbar transforaminal blocks to avoid advancing the needle beyond the halfway point of the foramen on lateral view to avoid damage to the segmental artery of Adamkiewicz, which lies in the superior ventral aspect of the foramen with its attendant risk of spinal cord ischemia and paraplegia. The contrast should be seen to flow proximally around the pedicle into the epidural space. The injection of contrast should be stopped immediately if the patient complains of significant pain on injection. After satisfactory flow of contrast is observed and there is no evidence of subdural, subarachnoid, or intravascular spread of contrast, 6 mg of betamethasone suspension/solution or 20 to 40 mg of methylprednisolone or triamcinolone suspension with 0. Injection of the local anesthetic and/or steroid should be discontinued if the patient complains of any significant pain on injection. Transient mild Chapter 299 Lumbar Subarachnoid Block 489 pressure paresthesia is often noted. After satisfactory injection of the local anesthetic and/or steroid and washout of contrast by the local anesthetic and steroid solution is noted, the needle is removed and pressure is placed on the injection site.
Order fluconazole 150 mg on line
For patients who do not respond to these treatment modalities fungus gnats get rid purchase fluconazole 100 mg on line, injection of the Achilles tendon with local anesthetic and steroid may be a reasonable next step. Differential Diagnosis Achilles tendinitis is generally easily identified on clinical grounds. Because a bursa is located between the Achilles tendon and the base of the tibia and the upper posterior calcaneus, coexistent bursitis may confuse the diagnosis. Stress fractures of the ankle may also mimic Achilles tendinitis and may be identified on plain radiographs or radionuclide bone scanning. The pain of metatarsalgia worsens with prolonged standing or walking for long distances and is exacerbated by improperly fitting or padded shoes. Signs and Symptoms On physical examination, pain can be reproduced by pressure on the metatarsal heads. Callus formation will often be present over the heads of the second and third metatarsal and can be distinguished from plantar warts by the lack of thrombosed blood vessels, which appear as small dark spots through the substance of the wart when the surface is trimmed. The patient with metatarsalgia will often exhibit an antalgic gait in an effort to reduce weight bearing during the 314 Section 3 Painful Conditions Differential Diagnosis Primary pathology of the foot including gout and occult fractures may mimic the pain and disability associated with metatarsalgia. Entrapment neuropathies such as tarsal tunnel syndrome may also confuse the diagnosis, as may bursitis and plantar fasciitis of the foot, both of which may coexist with sesamoiditis. Sesamoiditis occurs when sesamoid bones beneath the heads of the metatarsal bones that are present in some individuals develop inflammation. The muscles of the metatarsal joints and their attaching tendons are also susceptible to trauma and to wear and tear from overuse and misuse and may contribute to forefoot pain. Primary and metastatic tumors of the foot may also present in a manner analogous to arthritis of the midtarsal joints. Ligamentous laxity and flattening of the transverse arch may also be present, giving the foot a splayed-out appearance. Treatment Initial treatment of the pain and functional disability associated with metatarsalgia should include a combination of the nonsteroidal anti-inflammatory agents or cyclooxygenase-2 inhibitors and physical therapy. For patients who do not respond to these treatment modalities, injection of the affected metatarsal heads with local anesthetic and steroid may be a reasonable next step. Testing Plain radiographs and ultrasound imaging are indicated in all patients who present with metatarsalgia to rule out fractures, intermetatarsal bursitis, and to identify sesamoid bones that may have become inflamed. Magnetic resonance imaging of the metatarsal bones is indicated if joint instability, occult mass, or tumor is suspected. Radionuclide bone scanning may be useful in identifying stress fractures that may be missed on plain radiographs of the foot. Occurring twice as commonly in women, plantar fasciitis is thought to be caused by an inflammation of the plantar fascia. On physical examination, the patient will exhibit point tenderness over the plantar medial calcaneal tuberosity. Pain will be increased by dorsiflexing the toes, which pulls the plantar fascia taut, and then palpating along the fascia from the heel to the forefoot. Magnetic resonance imaging of the foot is indicated if occult mass or tumor is suspected. Stress fractures of the metatarsals or sesamoid bones, bursitis, and tendinitis may also confuse the clinical picture. Initial treatment of the pain and functional disability associated with plantar fasciitis should include a combination of the nonsteroidal anti-inflammatory agents or cyclooxygenase-2 inhibitors and physical therapy. For patients who do not respond to these treatment modalities, injection of the plantar fascia with local anesthetic and steroid may be a reasonable next step. This alteration in processing of this information appears to lead to a central sensitization with hyperexcitability of both motor and sensory neurons. Signs and Symptoms Initially, the pain will manifest in a single extremity or unilateral face that the sufferer will describe as burning and distressing in nature. The complaints of pain will often seem out of proportion to the degree of trauma that the patient has sustained. Any stimulus of the affected body part will result in an exacerbation of pain with hyperalgesia (an increased response to noxious stimuli) and allodynia (a painful response from a stimulus that does not ordinarily elicit pain) is often present. This pain is nondermatomal, and it does not follow the distribution of a specific peripheral nerve. Later in the course of the disease, plain radiographs can provide useful diagnostic information as the trophic changes associated with the disease become more apparent. Quantification of temperature abnormalities of the affected body part compared with the contralateral side with digital thermography or temperature probes may also be of value. Early functional limitations are identified on careful manual muscle and range of motion testing. Occupational therapy Chapter 201 Rheumatoid Arthritis 317 consisting of tactile desensitization of the affected skin may also be of value. Opioid analgesics and benzodiazepines should be avoided to prevent iatrogenic chemical dependence. Underlying depression and behavioral abnormalities may require psychiatric intervention as a part of a multimodality treatment plan. The possibility of an infectious etiology has gained new credence as the pathophysiologic processes behind Lyme disease are being elucidated. Patients between the ages of 22 and 55 are most often affected, with increasing incidence with age. Ill-defined morning stiffness most often will progress to symmetrical joint pain with calor, tenosynovitis, and fusiform joint effusions. The wrists, knees, ankles, fingers, and bones of the feet are most often affected, although any joint can be affected. Ultimately, the destruction of the cartilage and supportive bone will result in severe disability and pain. Carpal tunnel syndrome and the other entrapment neuropathies such as tardy ulnar palsy are the result of proliferation and thickening of the affected connective tissue. Rheumatoid nodules over bony prominences, or extensor surfaces, or in juxta-articular regions 6. Radiographic changes including erosions or bony decalcification localized in or adjacent to the involved joints (From American College of Rheumatology Subcommittee on Osteoarthritis Guidelines: Arthritis Rheum 2000; 43:1905-1915. Vasculitis and anemia can also occur and, if undiagnosed, can lead to life-threatening multisystem organ failure. Pericarditis and pleuritis herald significant extra-articular disease and must be treated aggressively. These T-helper cells produce cytokines that facilitate the inflammatory response and contribute to ongoing joint damage. Increased adhesion molecules contribute to inflammatory cell emigration and retention in the synovial tissue. Increased macrophage-derived lining cells are prominent along with some lymphocytes and vascular changes in early disease. Lymphocytes that infiltrate the synovial tissue are primarily T-helper cells, which can produce proinflammatory cytokines. These cells produce a variety of other substances that damage the joint, including fibrin, prostaglandins, collagenase, and interleukin-2. This ongoing inflammatory response leads to thickening of the synovium of the affected joints with pannus formation. As the disease progresses, osteochondral destruction and pannus formation become more evident. Fusiform soft tissue swelling, concentric loss of the joint space, and periarticular loss of bone are also seen, as are marginal erosions of the articular surfaces, which have lost their protective articular cartilage.
Purchase 150mg fluconazole free shipping
The needle is removed and pressure is placed on the injection site to avoid hematoma formation fungus allergy symptoms buy fluconazole online now. Ultrasound-guided lumbar plexus block utilizing the fascia iliaca technique is performed by placing the patient in the supine position. The inguinal creased on the affected side is identified, and a linear high-frequency ultrasound transducer is placed in an oblique plane perpendicular with the inguinal ligament. The femoral vein lies medial to the femoral artery and is easily compressible by pressure from the ultrasound transducer. Color Doppler can be utilized to aid in the identification of the femoral artery and vein. When these anatomic structures are clearly identified on oblique ultrasound scan, the ultrasound transducer is slid along the inguinal ligament toward the anterior superior iliac spine until the space between the fascia iliaca and the lateral aspect of the iliacus muscle is clearly defined. At that point, after careful aspiration, a small amount of preservative-free sterile saline is injected under real-time ultrasound imaging to utilize hydrodissection to reconfirm the position of the needle tip within the fascia iliacus compartment. Once the position of the needle tip is reconfirmed, after careful aspiration, 25 to 30 mL of 1. As mentioned earlier, an intravenous catheter can be placed into the fascial sheath to allow continuous infusion of local anesthetic. The proximity to the femoral artery and vein makes the possibility of local anesthetic toxicity real when performing lumbar plexus block using the Winnie 3-in-1 approach. Persistent paresthesia secondary to trauma to the the Fascia Iliaca Technique Landmark Technique the patient is placed in the supine position. Postblock groin and back pain, as well as ecchymosis and hematoma of the groin, occur often enough that the patient should be warned of such prior to beginning lumbar plexus block using the Winnie 3-in-1 technique. The proximity to the spinal cord and exiting nerve roots makes it imperative that lumbar plexus block using the psoas technique be performed only by those well versed in the regional anatomy and experienced in interventional pain management techniques. Postblock back pain from trauma to the paraspinous musculature is not uncommon after lumbar plexus block using the psoas compartment technique. Note the anechoic collection of local anesthetic just beneath the plane of the fascia iliaca. The technique is also useful to provide surgical anesthesia for the lower extremity when combined with lateral femoral cutaneous, sciatic, and obturator nerve block or lumbar plexus block. It is used for this indication primarily in patients who would not tolerate the sympathetic changes induced by spinal or epidural anesthesia and who need lower extremity surgery. Femoral nerve block with local anesthetic can be used diagnostically during differential neural blockade on an anatomic basis in the evaluation of lower extremity pain. If destruction of the femoral nerve is being considered, this technique is useful as a prognostic indicator of the degree of motor and sensory impairment that the patient may experience. Femoral nerve block with local anesthetic may be used to palliate acute pain emergencies, including femoral neck and shaft fractures, and for postoperative pain relief while waiting for pharmacologic methods to become effective. Femoral nerve block with local anesthetic and steroid is occasionally used in the treatment of persistent lower extremity pain when the pain is thought to be secondary to inflammation or when entrapment of the femoral nerve as it passes under the inguinal ligament is suspected. Femoral nerve block with local anesthetic and steroid is also indicated in the palliation of pain and motor dysfunction associated with diabetic femoral neuropathy. Destruction of the femoral nerve is occasionally used in the palliation of persistent lower extremity pain secondary to invasive tumor that is mediated by the femoral nerve and has not responded to more conservative measures. The roots fuse together in the psoas muscle and descend laterally between the psoas and iliacus muscles to enter the iliac fossa. The femoral nerve gives off motor fibers to the iliac muscle and then passes beneath the inguinal ligament to enter the thigh. The femoral nerve is just lateral to the femoral artery as it passes beneath the inguinal ligament and is enclosed with the femoral artery and vein within the femoral sheath. It also provides sensory fibers to the knee joint as well as the skin overlying the anterior and medial thigh. If paresthesia is not elicited, the needle is withdrawn and redirected slightly more medially until paresthesia is obtained. Once paresthesia in the distribution of the femoral nerve is elicited, the needle is withdrawn 1 mm, and the patient is observed to be sure he or she is not experiencing any persistent paresthesia. Subsequent daily nerve blocks are performed in a similar manner, substituting 40 mg of methylprednisolone for the initial 80-mg dose. A point just lateral to the pulsations of the femoral artery, the inguinal ligament and the inguinal crease are then identified and prepared with antiseptic solution. The iliacus muscle is identified with the femoral nerve lying between the muscle and the pulsatile femoral artery. At that point, after careful aspiration, a small amount of solution is injected under real-time ultrasound imaging to utilize hydrodissection to reconfirm the position of the needle tip. Once the position of the needle tip is reconfirmed, after careful aspiration, the remainder of the solution is slowly injected under ultrasound guidance. There should Landmark Technique the patient is placed in the supine position with the leg in neutral position. A point just lateral to the pulsations of the femoral artery and just inferior to the inguinal ligament is identified and prepared with antiseptic solution. Because paresthesia is elicited with this technique, needle-induced trauma to the femoral nerve remains a possibility. By advancing the needle slowly and then withdrawing the needle slightly away from the nerve, needleinduced trauma to the femoral nerve can be avoided. The technique is also useful to provide surgical anesthesia for the lower extremity when combined with lateral femoral cutaneous, femoral, and sciatic nerve block. Obturator nerve block with local anesthetic can be used as a diagnostic tool during differential neural blockade on an anatomic basis in the evaluation of hip pain. If destruction of the obturator nerve is being considered, this technique is useful as a prognostic indicator of the degree of motor and sensory impairment that the patient may experience. Obturator nerve block with local anesthetic may be used to palliate acute pain emergencies, including postoperative pain relief, while waiting for pharmacologic methods to become effective. Obturator nerve block with local anesthetic is also useful in the management of hip adductor spasm, which may make perineal care or urinary catheterization difficult. Obturator nerve block with local anesthetic and steroid is also useful in the treatment of persistent hip pain when the pain is thought to be secondary to inflammation or entrapment of the obturator nerve. Destruction of the obturator nerve is occasionally indicated for the palliation of persistent hip pain after trauma to the hip that is mediated by the obturator nerve. The nerve leaves the medial border psoas muscle and courses inferiorly to pass the pelvis, where it joins the obturator vessels to travel via the obturator canal to enter the thigh. The anterior branch supplies an articular branch to provide sensory innervation to the hip joint, motor branches to the superficial hip adductors, and a cutaneous branch to the medial aspect of the distal thigh. Landmark Technique To perform obturator nerve block, the patient is placed in the supine position with the legs slightly abducted. A point 1 inch lateral and 1 inch inferior to the pubic tubercle is then identified and prepared with antiseptic solution. Fluoroscopic-Guided Technique the patient is placed in the supine position on the fluoroscopy table with the legs slightly abducted. A 22-gauge, 3-inch needle is slowly advanced perpendicular to the skin until the needle is felt to impinge on the superior pubic ramus. The depth of bony contact is noted, and the needle is withdrawn and redirected laterally and slightly inferiorly. When needle tip position is confirmed to be in proximity to the obturator nerve, after careful aspiration for blood, 6 mL of 1. Ultrasound-Guided Technique To perform ultrasound-guided obturator nerve block, the patient is placed in the supine position with the leg in neutral position. A point just lateral to the pulsations of the femoral artery, the inguinal ligament, and the inguinal crease is then identified and prepared with antiseptic solution. A linear high-frequency ultrasound transducer is placed in an oblique plane perpendicular with the inguinal ligament along the inguinal crease. Color Doppler can be utilized to aid in the identification of the femoral and obturator arteries and veins. When these anatomic structures are clearly identified on oblique ultrasound scan, the ultrasound transducer is moved medially until the pectineus muscle, which looks like a "breaching whale," is visualized. Just medial to the medial aspect of the pectineus muscle lie the adductor longus, brevis, and magnus muscles, which are stacked on top of one another like a double decker sandwich. The skin over the posterior buttock on the affected side is then identified and prepared with antiseptic solution.