Purchase glucophage sr 500 mg visa
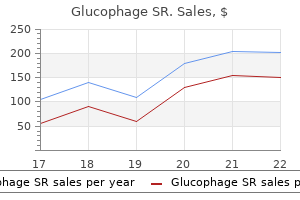
Nearly 90% of urachal malignancies are adenocarcinomas alternative medicine generic glucophage sr 500mg without a prescription, and one third of all primary bladder adenocarcinomas originate from urachal tissue. This coned-down, oblique view shows contrast material in a cone-shaped diverticulum (open arrow) arising from the apex of the bladder. The location of the urachal tumor is supravesical and often midline, immediately posterior to the linea alba. The prognosis for patients with urachal adenocarcinoma is worse than for those with other bladder carcinomas because local invasion frequently has occurred before the diagnosis is made. A Urinary Diversions Urinary diversions are surgical procedures designed to redirect the flow and collection of urine from the bladder. The four most common clinical indications for urinary diversion are the following: (1) management of muscle-invasive bladder cancer; (2) loss of the storage function of the bladder because of neurogenic bladder or congenital anomalies of the lower urinary tract; (3) medically or psychosocially incapacitating urinary incontinence; and (4) intractable symptoms referable to bladder abnormalities. As the paradigm for refluxing, noncontinent urinary diversion, the ileal conduit uses a short segment of distal ileum for collection of urine. Typically, this segment is supplied by the ileocolic artery or a suitable large branch of the terminal superior mesenteric artery. One end of the isolated ileal segment is closed and is secured to either the sacral promontory or the retroperitoneum near the aortic bifurcation. The other end drains externally through a stoma typically placed in the right lower quadrant. This configuration permits continuous drainage of urine into a collecting device attached to the skin. B, Coronal computed tomography image shows a lobulated, multicystic, low-attenuation mass arising from the bladder apex. Low-grade mucinous adenocarcinoma arising from a urachal diverticulum was diagnosed at surgery. Unless an antireflux mechanism is created, free vesicoureteral reflux is expected. To complete the anastomosis between the ileal loop and the left ureter, the latter must pass under the base of the sigmoid mesentery, so it is more likely than the right ureter to be angulated or under tension. The radiologist must be aware of several complications of ileal conduit urinary diversion surgery, which can be classified by the expected time of occurrence (Box 6-19). Both of these complications occur most often at the ureteroileal anastomosis, although extravasation may also be seen from the base of the ileal loop. Late complications include chronic pyelonephritis, stone disease, malignancy, and urinary obstruction caused by stenosis of the ureter, loop, or stoma. Chronic pyelonephritis occurs in 10% to 33% of patients and results from either chronic obstruction or reflux. Urinary tract infection plays a central role in the development of nephrolithiasis, which occurs in approximately 5% of diverted patients. Stone impaction causing obstruction at a narrowed ureteroileal anastomosis is a common presentation. Ureteral stricture resulting from fibrosis is a relatively late complication with an incidence rate of 5% to 7%. Predisposing factors include ischemia, radiation therapy, and urine extravasation. In nearly 20% of patients undergoing cystectomy for bladder cancer, severe ureteral epithelial atypia occurs. In up to 33% of patients, metachronous urothelial cancer in the ureter or renal pelvis may develop after cystectomy and urinary diversion. This complication should be suspected in any patient with ureteral stenosis, and it may be either an early or a late complication. Direct contrast instillation into the ileal loop is not performed routinely during the immediate postoperative period, although it is a valuable examination any time thereafter when stenosis at the ileoureteral anastomosis is suspected. The continent urinary diversion is increasingly being used because it removes the stigma of an external collection appliance and provides an effective alternative for the patient who is unable to maintain dryness with a conduit diversion. Some continent diversions involve the creation of a pouch to collect urine that opens to the abdominal wall and is drained by intermittent selfcatheterization, while others involve the construction of a neobladder that permits emptying through the urethra. The goals of the continent diversion are to create (1) a continence mechanism permitting facile intermittent emptying by self-catheterization; (2) a large-capacity (0. Continent reservoirs can be constructed from the terminal ileum and cecum together (Indiana, King, Mainz, and Penn techniques) or from the small bowel alone (Kock and Camey techniques). Early and other late complications are similar to those described for the ileal loop. A, Routine intravenous urogram performed 6 days after construction of an ileal loop shows mild ureteropyelocaliectasis. B, Three months later, repeat urogram demonstrates a normal collecting system and ileal loop. A, Several stones with a spiked appearance (jack stones) are present within the pouch in the right side of the abdomen. B, Sagittal image shows an ileal segment (arrow) extending from the pouch (created from the terminal ileum and cecum) to a stoma in the periumbilical region. Retrograde urethrography is the imaging study of choice for the evaluation of urethral strictures. The purpose of the radiographic evaluation is to assess the length, location, multiplicity, and severity of the urethral stricture, and to identify concomitant lesions that may complicate urethral obstruction. Mucosal infection causes symptoms of dysuria and urethral discharge, but the presence and severity of these symptoms vary. Local extension of the infection to the posterior urethra, seminal vesicles, or epididymis occurs frequently in the untreated patient and rarely may occur in the patient who seeks prompt treatment. Stricture formation after an adequate course of appropriate antibiotics is thought to be uncommon. When a patient has persistent or recurrent urethritis that appears to be unresponsive to antimicrobial treatment, urethral stricture, or one of its complications, and prostate infection should be investigated. The proximal bulbar urethra is the site of stricture in 70% of patients with gonococcal urethritis because of the rather high concentration of periurethral glands in this area and the dependent position of this portion of the male urethra. Retro- grade urethrogram demonstrates serial, short strictures of the anterior urethra. Urethral stricture resulting from infection or inflammation tends to be multiple and tends to involve the bulbar urethra. Finally, gonococcal urethritis may incite mucosal hyperplasia, resulting in polypoid urethritis or urethritis cystica, which appears as flat, nodular filling defects that may be difficult to distinguish from carcinoma. Tuberculous Urethritis Urethral inflammation caused by Mycobacterium tuberculosis is reported to occur in only 2% of men with upper urinary tract tuberculosis. Antecedent traumatic or infectious urethral stricture is thought to be necessary for its development. However, direct extension of tuberculosis from the prostate gland to the prostatic urethra or from the perineal tissues to the bulbar urethra has been reported. Iatrogenic Stricture Stricture formation may complicate urethral surgery, instrumentation, or catheterization. Iatrogenic strictures most often occur in parts of the urethra that are anatomically fixed and narrow. TheLowerUrinaryTract 235 Trauma Traumatic urethral stricture usually occurs after a straddle injury that has resulted in complete transection of the urethra, whereas partial laceration of the urethra is more likely to heal without significant narrowing. As many as 97% of patients with injuries to the posterior urethra develop strictures requiring repeated dilatations or urethroplasty, regardless of initial treatment. Neoplasm Stricture formation rarely is the sole manifestation of a urethral carcinoma. However, carcinoma should be suspected when stricture formation occurs in an elderly patient with no previous medical history of urethral surgery, instrumentation, or infection. Complications of Urethral Stricture When severe, stricture formation can result in symptoms of urethral obstruction that prompt the patient to seek medical attention. Urethral obstruction may cause several complications that can overshadow the inciting stricture (Box 6-21). In a patient with incompletely treated gonococcal infection, fistulas are seen between the bulbar urethra and the perineum and scrotum (long white arrows) with pooling of contrast in these locations (asterisks). Retrograde urethrogram demonstrates a focal, tight stricture of the bulbar urethra that developed 4 weeks after a straddle injury.
Order 500mg glucophage sr with mastercard
A transverse gray-scale ultrasound image through the mid scrotum shows numerous symptoms jaundice order genuine glucophage sr, tiny nonshadowing echogenic foci distributed diffusely within the parenchyma of both testicles. The presence of more than five of these foci in an imaging field meets the definition of classic testicular microlithiasis. A, Enhanced axial computed tomography image at the level of the mid kidneys, obtained to evaluate abdominal discomfort in this 37-year-old man, reveals a large heterogeneous mass in the region of the left renal hilum, displacing the left renal vein anteriorly (arrow). A longitudinal gray-scale ultrasound image (B) and an image using color Doppler at the same location (C), obtained due to concern for the testicle as the primary neoplastic source, reveal a 4-mm linear calcification with posterior acoustic shadowing located centrally within the testicle (arrowhead in B and C). The calcification was the only remnant of the regressed, primary testicular tumor. Note the presence of the left-sided varicocele, which was new according to the patient, resulting from obstruction of the left gonadal vein by the metastatic adenopathy. Longitudinal gray-scale ultrasound images of the right (A) and left (B) testicles reveal numerous, tiny nonshadowing echogenic foci within the parenchyma of both testicles. In the lower aspect of the left testicle, there is an ill-defined, heterogeneous mass containing cystic areas and several microliths. This tumor contained mostly teratomatous elements with smaller areas of yolk sac and embryonal cell types. After these initial lymph node stations are involved, the paralumbar nodes inferior to the renal hilum or thoracic sites are affected. Local tumor extension into the epididymis or scrotal skin changes the potential lymphatic drainage of the testicular neoplasm. If the epididymis is involved, drainage to the external iliac node chain may occur, and scrotal involvement may lead to inguinal adenopathy. Abdominal lymphatics drain into the thoracic duct and then into the left brachiocephalic vein. Tumors that spread by this route may involve the lungs, mediastinum, or supraclavicular lymph nodes. A notable exception to the primary lymphatic spread of testicular cancers is choriocarcinoma, which is prone to hematogenous metastases. A tumor, node, metastasis classification is available but patients are more practically classified as having lowstage or advanced stage disease (Box 8-10). A longitudinal image of the right testicle, obtained in this male patient after a bar fight, reveals disruption of the echogenic tunica albuginea along the superior surface of the testicle (arrows). The hypoechoic region in the upper portion of the testicle (arrowheads) was proven to be a fracture with surrounding contusion at surgery. Note the scrotal skin thickening and echogenic material surrounding the testicle (asterisks) representing hemorrhage. Violent, blunt scrotal trauma may cause testicular rupture after a minor traumatic episode. On physical examination, extreme tenderness, scrotal ecchymosis, and swelling are frequent findings. It is important to remember that an associated neoplasm can be a cause of testicular rupture after rather a minor trauma. Early surgical exploration and repair of testicular injuries have reduced morbidity and the need for subsequent orchiectomy. If the tunica albuginea of the testicle has been violated, devitalized seminiferous tubules will be extruded into the potential space between the tunica albuginea and tunica vaginalis, and surgical debridement is indicated. In addition to suspected rupture, the presence of a large scrotal hematoma is an indication for exploration. Scrotal ultrasonography is the imaging procedure of choice because it helps to determine whether significant testicular parenchymal disruption has occurred, which is essential information when deciding which patients require emergency surgery, and it can assess the size of a scrotal hematoma (Box 8-11). Furthermore, ultrasonography can be used to exclude the more common causes of scrotal pain, particularly when a history of scrotal trauma is unclear. Ultrasonography correctly predicts the presence of a ruptured testis in nearly 100% of patients with scrotal injury. The presence of tunica albuginea disruption alone has a sensitivity of 50% and specificity of 75% for testicular injury. A focal linear or, more often, a complex and multifocal disruption of the normally homogeneous parenchymal echo pattern suggests the diagnosis of testicular fracture. Solid or semisolid collections around the disrupted testicle may represent hematoma and extruded parenchyma; these collections can be mistaken for the ruptured testicle itself. A, Transverse gray-scale ultrasound image through the mid right testicle shows a poorly defined hypoechoic area in the posterior aspect of the testicle with intact tunica albuginea. B, Transverse image at approximately the same level as A with application of color Doppler imaging shows no internal vascular flow in this area. Although the appearance may mimic an intratesticular neoplasm, clinical context and absence of internal flow favor a hematoma. If the scrotum is enlarged because of the presence of a hematoma, the most common finding in the scrotum after blunt injury, a lower frequency transducer that provides increased depth of field may be necessary to survey the scrotum for a displaced or compressed testicle. Because the testicle originates in the abdominal cavity of the embryo, a cryptorchid testis can be found anywhere along the normal path of testicular descent from the level of the inferior pole of the kidney to the upper scrotum. Based on location and in decreasing order of incidence, the following four types of cryptorchid testis are recognized: retractile, canalicular, abdominal, and ectopic. The retractile testis moves intermittently between the base of the scrotum and the groin and can be observed in up to 80% of patients aged 6 months to 11 years. Retraction, the result of spontaneous or reflexive cremasteric muscle contraction, occurs less commonly after puberty. The canalicular testis is located between the internal and external inguinal rings. The rarest type of malpositioned testicle is ectopic cryptorchidism, in which the testicle is found away from the normal pathway of descent. The most common ectopic site is the superficial 320 GenitourinaryRadiology:TheRequisites inguinal pouch, but other described locations include the femoral canal, the suprapubic region, the perineum, and the opposite hemiscrotum (transverse ectopia). Nonpalpable testes are absent in a significant percentage of patients (15%), a distinction which is important because of the complications associated with the cryptorchid testis in the adult. Infertility, neoplasia, torsion, and trauma are the major reported complications of cryptorchidism. Irreversible histologic changes occur in the cryptorchid testicle by the age of 2 1 2 and are believed to contribute to associated complications of infertility and neoplasia. Even in unilateral cryptorchidism, a defect in the spermatogenesis of the contralateral scrotal testicle may be present because, after surgical correction of cryptorchidism, the mean fertility rate is only 60%. About one third of undescended testes also have anomalies of wolffian duct-derived structures that may have an impact on fertility. This anomaly may be a seminal vesicle cyst, insertion of an ectopic ureter into the vas deferens or seminal vesicle, and agenesis of the epididymis, seminal vesicle, or vas deferens. An estimated 10% of all testicular cancers occur in patients with a history of cryptorchidism, and there is a 40-fold increase in the risk of developing cancer in an undescended testicle. This risk is present only if the undescended testis is left unmanaged after the age of 5; therefore surgical correction is recommended around the age of 2. An abdominal testis is four times as likely to undergo malignant degeneration as is an inguinal testis; interestingly, in patients with a unilateral undescended testis, 15% of testicular cancers occur in the contralateral, normally descended testis. A testicle high in the scrotum or within the inguinal canal can usually be detected by a clinical examination. Sonography may be used to confirm the presence of the undescended testis after an equivocal or difficult examination, when it is located at or caudal to the inguinal ligament. The cryptorchid testicle is frequently small and may be difficult to distinguish from an inguinal lymph node, and therefore identification of the mediastinum is important for confirmation. Because about a quarter of undescended testes are nonpalpable, localization is the main objective of presurgical imaging. Location of an intra-abdominal testicle may be problematic with any imaging modality. Gonadal phlebography relies on the identification of the pampiniform plexus for localization of the cryptorchid testicle, but it is technically challenging, particularly in children aged less than 12 months. Laparoscopy, with direct visualization of the gonadal vasculature, has now been added to the tools available for testicular location, especially when an intra-abdominal position is suspected.
Generic glucophage sr 500 mg with visa
Patients without clear risk factors are presumed to have primary small bowel obstruction from congenital bands treatment yeast buy glucophage sr 500mg line, internal hernias or primary small bowel tumours. There is marked tenderness over the loop while the remainder of the abdomen is usually soft and not particularly distended. Patients on anticoagulation may develop spontaneous intramural haematomas that can also cause intussusception. Infectious intra-abdominal processes such as diverticulitis or appendiceal abscesses may lead to hypomotility of the adjacent small bowel leading to a segmental paralytic ileus. Diffuse Generalized Abdominal Pain Many patients report abdominal pain that cannot be easily localized to a particular region. Severe and sudden-onset generalized abdominal pain is the initial complaint in many surgical abdominal conditions. Fever, tachycardia or hypotension, and a firm abdomen with diffuse board-like guarding and absent bowel sounds raises concerns of peritonitis from bowel perforation. Perforated duodenal ulcer, diverticulitis and colon cancer are the most likely possibilities in elderly patients. Less frequently, appendicitis may result in the spread of purulent content in the abdomen, leading to diffuse guarding. Patients with haemoperitoneum from blunt or penetrating trauma or ruptured vascular tumours such as hepatocellular carcinoma or hepatic adenoma, may also exhibit board-like abdominal wall rigidity. Finally, severe pancreatitis causing mesenteric and intestinal oedema may produce an abdominal examination consistent with diffuse peritonitis. Ascites Progressive, vague, non-acute and poorly localized abdominal pain in association with a sense of increasing abdominal girth raises a suspicion of new-onset ascites. Patients with advanced liver disease have the stigmata of portal hypertension discussed above. New or progressive ascites in these patients may reflect a new insult to an already failing liver, such as a portal vein thrombosis or hepatocellular carcinoma. In a patient with known ascites, new-onset abdominal pain may be the first symptom of spontaneous bacterial peritonitis. Primary intestinal dysmotility disorders are rare but should be considered in patients with chronic nausea, vomiting, abdominal distension and constipation without a clear aetiology. Most patients with large bowel obstruction have an incompetent ileocaecal valve that allows the colon to be somewhat decompressed as pressure is transmitted to the small bowel. Patients with a competent ileocaecal valve effectively have a closed-loop large bowel obstruction leading to severe pain and progressive abdominal distension with localized peritonitis over the colonic segment involved. The most common causes of large bowel obstruction are colon cancer, incarcerated hernia, sigmoid or caecal volvulus, faecal impaction and diverticular strictures. Classically, left-sided colon cancers tend to present with obstruction while right-sided cancers produce bleeding. Obstructing cancers or impacted faeces may paradoxically produce diarrhoea as liquid stool leaks through the mass. In toxic patients with abdominal distension and diarrhoea, toxic megacolon from overwhelming Clostridium difficile infection must be considered. Pseudo-obstruction describes colonic dysmotility that may be triggered by medications, stress and infection. Patients with pseudo-obstruction usually continue to pass stool and flatus intermittently. Abdominal examination usually reveals a soft abdomen with diffuse mild rebound tenderness without significant guarding. The catheter insertion site should be inspected for erythema or purulent drainage, although these signs may be absent. There may be mild distension and mild diffuse tenderness, but rebound and guarding are unusual. Constipation Chronic constipation causes significant diffuse abdominal pain in elderly patients. In thin patients, dense stool can be palpated in the transverse and sigmoid colon. Rarely, faecal impaction produces the clinical picture of bowel obstruction with nausea, vomiting, abdominal distension and abdominal tenderness. Right Heart Failure Chronic right heart failure may cause hepatic congestion resulting in ascites, hepatomegaly and even splenomegaly. Patients may complain of mild, diffuse or epigastric abdominal pain with associated nausea. Tricuspid stenosis is likely to be present if the pulsations occur just before ventricular systole, while tricuspid regurgitation is more likely if the pulsations occur during systole. Urinary Retention Older patients are also prone to developing acute or chronic urinary retention. Benign prostatic hyperplasia is the most common cause in men, while pelvic floor laxity with the development of a cystocele or rectocele is a common aetiology in women. Some may only report urinary frequency and overflow on questioning as they become accustomed to their chronic symptoms. Physical examination will reveal suprapubic fullness, and palpating the dome of the bladder will make the patient feel an urge to urinate. When the bladder is massively distended, there may be significant tenderness, mimicking peritonitis in some cases. The history may reveal worrisome symptoms such as a change in bowel habit, chronic bloodtinged stools or postmenopausal vaginal bleeding coupled with weight loss, night sweats and fatigue. A firm, palpable mass may be appreciated on abdominal examination if the underlying cancer is sufficiently large. If a rectal cancer is palpated on digital rectal examination, the sphincter tone should be assessed to identify involvement of the sphincter muscles. Ruptured mucoceles of the appendix or ovaries may lead to pseudomyxoma peritonei, in which extensive gelatinous fluid fills the abdomen. The disease is slow to progress, but the presentation is often similar to that of a gynaecological malignancy. Gastroenteritis Fortunately, there are many benign, self-limiting conditions that cause non-acute, generalized abdominal pain. Bacterial or viral gastroenteritis presents with vague, crampy abdominal pain, nausea, vomiting and diarrhoea. Key Points A thorough history and physical examination allow the healthcare provider to formulate a differential diagnosis upon which to base further testing and interventions if necessary. When a patient localizes their abdominal pain to a particular region, the history and physical examination should be tailored to distinguish between the conditions that commonly affect the identified region. Generalized abdominal pain has a vast differential diagnosis, but it is still possible to identify the most likely condition present using detailed history and physical examination skills. A 65-year-old woman presents with complaints of vague, poorly localized abdominal pain over the last 3 weeks. She has also noted some abdominal distension and thin, blood-tinged stools over the last 3 months. A 19-year-old woman complains of progressive right lower quadrant pain over the last 5 days. The abdomen is soft, with tenderness to deep palpation of the right lower quadrant. A 57-year-old man with hypertension and diabetes reports 4 days of right upper quadrant and epigastric pain. The patient has constitutional symptoms suggestive of malignancy and progressive obstructive symptoms without a prior screening colonoscopy. There is no jaundice to suggest cholangitis from choledocholithiasis or cholangiocarcinoma. Gallstone ileus typically presents as a small bowel obstruction, and not with right upper quadrant pain.
Order glucophage sr uk
Rocker Bottom Foot this condition involves the collapse of the longitudinal arches of the foot treatment brown recluse bite buy 500mg glucophage sr with amex, which occurs in diabetic patients with neuropathic arthropathy and sensory neuropathy. Tarsal Tunnel Syndrome Tarsal tunnel syndrome is due to compression of the tibial nerve as it passes into the foot posterior to the medial malleolus with the posterior tibial artery, deep to the flexor retinaculum in the fibro-osseous tunnel. As with carpal tunnel syndrome, the presenting symptoms involve the nerve supply, which include pain, paraesthesia and a burning sensation over the sole of the foot extending to the toes, particularly the first three toes. The cause can be anything that results in compression of the nerve within the tarsal tunnel, including trauma, inflammation or benign tumours. The symptoms can be reproduced by inflating a sphygmomanometer cuff over the ankle for a minute in order to occlude the blood supply to the foot. A careful vascular examination is warranted as there is occasional distal ischaemia. Upon ambulation, the weight is shifted to the lateral aspect of the foot to avoid placing pressure on the navicular bone. A bunion, which is a swollen bursa, is usually present and can be erythematous and painful. On inspection, the laterally deviated phalanx may result in a dorsally displaced and over-riding second toe, which may result in pressure symptoms. The Forefoot 281 Hallux Rigidus this occurs due to degenerative osteoarthritis of the metatarsophalangeal joint. The condition can be idiopathic, secondary to trauma, or may be a consequence of a long history of hallux valgus deformity. On examination, the metatarsophalangeal joint is stiff and pain is elicited on attempted plantar flexion or dorsiflexion. When asked to curl the toe, patients will only have motion of the interphalangeal joint of the big toe. Bunionette A bunionette is a bursal inflammation of the lateral aspect of the head of the fifth metatarsal. Transversely squeezing the metatarsal heads together or palpating between the two metatarsal heads can elicit pain and paraesthesia. Repair has often commenced by the time of diagnosis: callus is seen on this radiograph. Patients usually present with pain just proximal to the toes that increases during walking or standing (especially if barefoot) and is relieved by rest. The patient may also complain of paraesthesias and shooting pain in the corresponding toes. Plain radiographs may initially be negative, but if the clinical suspicion is high, a bone scan will reveal the fracture. Patients present with pain over the dorsum of their toe, as well as corns over the flexed proximal interphalangeal joint. A subungal haematoma is a collection of blood between the toenail and the nail bed secondary to trauma. Patients present with pain and swelling of the toe with dark discoloration underneath the nail. It occurs mostly in the big toe and results in a nail that is detached from the tissues deep to it and has a keratinized and curled horn. Patients present with pain when wearing closed shoes, or as a result of secondary infection or trauma. There is exquisite tenderness in the joint, which is dusky red and swollen from the deposition of urate crystals; the patient resists any movement. The diagnosis is aided by the absence of a bunion, the male predominance and the presence of gouty tophi, usually on the helix of the ear, but also in olecranon bursae and the tendon sheaths of the hands and feet. These deformities may be part of a syndrome and may be associated with talipes deformities. Patients present with pain proximally at the insertion and along the plantar fascia. Callosities Callosities occur on the plantar aspect of the foot, usually over the metatarsal heads (particularly with a cavus foot), the heel, or on the medial aspect of the big toe. The skin becomes hard and thickened due to the increased pressure over a large surface area. Prolonged exposure of the feet to an unhygienic wet environment (such as in trench warfare) produces swelling of the skin and subcutaneous tissues. They have the same clinical features as ganglia of the hand and wrist (see Chapter 13) but are less common. The lesions usually have pigmentation as a distinguishing feature but may go unnoticed until ulceration occurs. When a melanoma is suspected, the groin nodes and Hard Corns Unlike callosities, hard corns occur over the dorsum of the foot, are painful and are caused by pressure over bony prominences with small surface areas. They usually occur over the first and fifth metatarsal heads with surrounding callosities, and are associated with sensory deficits. Other Conditions the capillary networks of the extremities constrict in the cold, preserving heat. Evaluation of the foot begins with adequate knowledge of the unique anatomy of the foot and a careful history, followed by a physical examination that starts with inspection. These include club foot, pes cavus, pes planus, metatarsus varus and isolated equinus deformity. The hindfoot is subject to arthritis as well as soft tissue and bony traumatic injuries. The toes are subject to acquired deformities such as hammer toes or subungal exostosis, trauma such as subungal haematomas and onychogryposis (which results from trauma to the nail bed), tumourous growths such as subungal glomus tumours, and congenital abnormalities. The soft tissues of the heel and sole can become inflamed with activity, such as with plantar fasciitis, can develop hard and soft corns as well as callosities from pressure on bony prominences or friction, and can develop ulcers secondary to diabetes, central or peripheral nerve injuries. The four deformities seen in club foot are equinus, cavus, varus and metatarsus adductus. Lisfranc injuries typically occur as a result of axial loading onto a plantar-flexed or vertical foot. For each of the following conditions, select the most likely structure to be injured from the list below. Pes cavus is characterized by fixed plantar flexion of the forefoot that does not correct with weight-bearing. Sinus tarsi syndrome is characterized by pain and tenderness on the lateral side of the foot. It is caused by injury to the interosseous talocalcaneal ligament, most commonly due to an ankle sprain. Tarsal tunnel syndrome is caused by compression of the tibial nerve by the flexor retinaculum at the level of the medial ankle. Patients may present with pain, numbness or a burning sensation in the medial or plantar aspect of the foot. It occurs in the paediatric age group between the ages of 4 and 9 years, and is more common in boys. Patients present with pain and swelling in the dorsal-medial midfoot area with difficulty walking. Which one of the following occurs secondary to pressure on bony prominences in the foot Pressure on bony prominences results in hard calluses, callosities and neuropathic ulcers (in patients with diabetes or central/peripheral nerve injuries). This chapter reviews and solidifies the principles of the history and examination of skin conditions that are of surgical relevance, in particular benign premalignant and malignant lesions. Congenital and atopic conditions are those present from birth, although they may not necessarily present in their florid state until later. Note the relation of the onset to any exposure to physical and chemical agents, and remember that the exposure may antedate the skin disorder by a number of months. Similarly, a history of drug or supplement exposure is of essence when a drug eruption is suspected.
Order genuine glucophage sr online
Cylindromas medicine to stop vomiting order glucophage sr 500 mg with amex, also referred to as adenoid cystic carcinomas, may result in airway obstruction and warrant bronchoscopy and coring-out of the tumour to restore airway patency. Other less common lesions include pulmonary hamartomas, fibromas, sarcomas and neurogenic tumours. In inflammatory states, the volume of pleural fluid can increase dramatically, sometimes up to several litres of effusion. It is important to differentiate the aetiology of these effusions, as they may be exudative in the case of infections, or transudative in the case of heart failure. Bloody effusions may be present following traumatic injuries or recent thoracic surgery. Injury to the thoracic duct may result in a milky white, high-volume chylous effusion. Primary Pleural Tumours Mesotheliomas are the most well-defined pleurally based tumours and are linked to asbestos exposure. Mesotheliomas occur many years after exposure and are highly malignant, with only a small subset of patients being amenable to surgical resection. The epithelioid variant is the most commonly resected type; excision usually occurs after the patient has received trimodal therapy involving induction chemotherapy, extrapleural pneumonectomy and radiation therapy. Benign fibrous tumours of the pleura may also occur and, due to their interference with respiratory dynamics and their large size, are usually resected. Less common sources of empyemas are tuberculosis, fungal infections, amoebic abscesses and malignant effusions that subsequently become infected. There are two pleural surfaces: the visceral pleural is intimately associated with the lung parenchyma, and the parietal pleural covers the inner surface of the thoracic cavity. The parietal pleura is innervated by the intercostal nerves, explaining the localized pain associated with pleural disease. Pleuritic pain or pleurisy occurs when there is inflammation of the pleural surfaces leading to pain on expiration, and less commonly on inspiration, as the pleural surfaces slide over each other. This demands extensive decortication of the lung parenchyma as the lung becomes trapped. The goals of treatment of an empyema are, first, evacuation of the purulent effusion, and second, elimination of the pleural space by restoring the ability of the lung parenchyma and diaphragm to expand. If it is not possible to eliminate an infected pleural space, external drainage of the pleural space is sometimes required via an Eloesser flap or Clagett window. Anterior mediastinal lesions include thymomas, thymic carcinomas, thyroid tumours, lymphomas, non-seminomatous germ cell tumours and germ cell tumours. Middle mediastinal lesions include cysts, enteric duplication cysts and embryogenic remnants of bronchial and pericardial development. Posterior mediastinal lesions are represented largely by neurogenic tumours such as ganglioneuromas, neuroblastomas and chemodectomas. In all compartments, rare lesions such as angiosarcomas and leiomyoscarcomas may arise from the visceral structures. Critical to the surgical anatomy of the diaphragm is an understanding of the location of the phrenic nerves, which innervate this important respiratory muscle. The diaphragm has a large central tendon and attaches anteriorly to the xiphoid process, and posteriorly and laterally to the ribs and chest wall. The posterior aspect has diaphragmatic recesses that may extend as low as the 12th rib. The diaphragm allows for passage of the inferior vena cava at T8, the oesophagus and vagus nerves at T10, and the aorta and thoracic duct at T12 via the diaphragmatic hiatus. As a result of these openings, diaphragmatic hernias may occur, which are broadly of two types: congenital and traumatic. Traumatic hernias may occur as a result of fractures of the ribs corresponding to the insertion of the diaphragm, or from rapid exhalation against a closed glottis, for example during highforce abdominal trauma. Traumatic diaphragmatic hernias should be repaired at the time of diagnosis and can often be fixed primarily. Large defects or the presence of devitalized tissue may need the placement of a prosthetic mesh to repair the defect. Eventration refers to an abnormal appearance or contour of the normally dome-shaped diaphragm due to protrusion of abdominal contents through a weakened diaphragmatic musculature. Excision of the diaphragm is sometimes required, for example with extrapleural pneumonectomy for epitheloid mesotheliomas. In such cases, a small rim of tissue is left circumferentially to allow for fixation of a neo-diaphragm composed of synthetic mesh. If it is not feasible to leave such a rim, for example if this will compromise the oncological resection, the neo-diaphragm is instead fixed to the chest wall circumferentially. It enters the chest at the thoracic inlet, running parallel to the vertebral column, and is most easily accessible on the left in its upper joint. It courses through the chest, then becoming more accessible on the right as it leaves the chest via the oesophageal hiatus at T10. Here it lies in close proximity to the thoracic duct and carries with it the left and right vagi. Throughout its course, it lies in close proximity to the aorta, and more cephalad it lies posterior to the membranous trachea. The oesophagus is composed of a circular and a longitudinal muscle layer, with an inner mucosa; it lacks a true serosa. The left chest is filled with abdominal contents, with a mediastinal shift to the right. The stomach and other viscera are sited in the left pleural cavity, and there is a mediastinal shift to the right. These vessels are tiny and numerous, allowing for blunt dissection of the oesophagus without large-volume bleeding via the diaphragmatic hiatus, as during a transhiatal oesophagectomy. Oesophageal Rupture Oesophageal rupture typically follows an episode of retching, resulting in an oesophageal tear. Portal hypertension leads to the development of varices of the oesophagus in conjunction with gastric varices. The presence of oesophageal varices without gastric varices is suggestive of splenic vein thrombosis and, unlike portal hypertension, the treatment is splenectomy. In patients with cirrhosis, severe bleeding can occur from oesophageal varices and is often life-threatening. There is a sensation of early satiety and post-prandial fullness with an associated dull, aching chest pain. Type 3 paraoesophageal hernias should be repaired as they are often associated with gastric volvulus. These are ring-like, mechanical ulcerations that form at the site where the stomach is compressed as it passes through the oesophageal hiatus. Prior to the repair of a hiatus hernia, it is prudent to evaluate the oesophagus for motility disorders as these may occur concurrently and influence the operation performed. Dysphagia Dysphagia is a broad term referring to difficulty swallowing and should be differentiated from odynophagia, which refers to painful swallowing. The barium is indented by the diffuse pattern of bulging varicosities at the lower end of the oesophagus. The cardiac end of the stomach has passed through the oesophageal hiatus alongside the oesophagus and is sited above the diaphragm. In some situations, for example near-total oesophageal obstruction, there is dysphagia to both solids and liquids.
Effective 500mg glucophage sr
Infection of the epididymis that progresses to the adjoining testicle is referred to as epididymo-orchitis medications like tramadol quality glucophage sr 500 mg. Both pathologies typically present with scrotal pain and swelling, which develop over a couple of days, in contrast to torsion of the spermatic cord, which presents within hours. Associated symptoms include dysuria, urinary frequency, urgency and occasionally fever and urethral discharge. A common cause of isolated orchitis is mumps, in which testicular pain is usually preceded by fever, malaise and parotiditis. On examination, orchitis and epididymitis are characterized by swelling and tenderness of the respective tissue with erythematous and oedematous overlying scrotal skin. In advanced cases, a reactive hydrocele may occur, making scrotal examination more difficult. The most common presenting features are urinary frequency, nocturia, dysuria, fever, suprapubic pain, flank pain, haematuria and pyuria. Delayed diagnosis and intervention often results in significant morbidity and occasionally death. The source of the infection is usually the large bowel, urinary tract or skin of the genitalia. Patients often have multiple comorbidities that compromise the immune system, which precipitates and augments the infection. Sexually Transmitted Infections Gonorrhoea Gonorrhoea is a common infectious condition caused by the bacterium Neisseria gonorrhoeae. Approximately 10 per cent of infected men and 50 per cent of infected women are asymptomatic. The latter is usually caused by infection with Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis or Trichomonas vaginalis. In primary genital herpes, the patient typically starts to experience constitutional symptoms (fever, headache, malaise) and local symptoms (pain, dysuria, itch, urethral and vaginal discharge) after an incubation period between 1 day and 3 weeks. Recurrent genital herpes is common, occurring in up to 90 per cent of patients within the first 12 months. Infection has been associated with changes in the cervical epithelium that may progress to cervical intraepithelial neoplasia and later to invasive carcinoma. The primary route of infection is through sexual contact, but it may also be transmitted from mother to fetus in utero or at birth (congenital syphilis). During the latent phase, which may last many years, affected individuals are usually asymptomatic. The manifestations of tertiary syphilis include symptoms of neurosyphilis and cardiovascular syphilis. More commonly, if the stone partially or totally obstructs the upper urinary tract, it induces renal pain, often referred to as a renal colic. Renal pain is caused by acute distension of the renal capsule, and the discomfort radiates from the flank anteriorly towards the umbilicus. Typically, patients with renal pain usually roll around holding their loin, whereas those with pain due to intraperitoneal disease prefer to lie still to limit irritation of the peritoneum. Note the two dense white shadows at the same level within the dilated collecting system of the right kidney. On rectal examination, prostatic calculi in the peripheral aspect of the gland can often be felt as small hard nodules and can be confused with prostatic adenocarcinoma. Bladder cancer is the fourth and 11th most common cancer diagnosis in men and women, respectively. This male:female ratio is in part due to the difference in exposure to occupational carcinogens and cigarette smoking. Renal and ureteric colic are often associated with nausea and vomiting because of reflex stimulation of the coeliac ganglion. Bladder Calculi Bladder stones usually result from urinary stasis associated with prostatic enlargement, urethral strictures, bladder diverticula and bladder dysfunction. Other predisposing factors include foreign bodies in the bladder, including suture material, ureteral stents, surgical staples and catheters. The ureter then courses downwards and backwards to the level of the ischial spine before turning forwards and medially to enter the posterior wall of the bladder. The anatomical location of the ureter means that it is impalpable even in diseased states. This means that diagnosis of ureteric pathology usually requires urinary tract imaging and/or direct endoscopic evaluation of the ureter. Conditions affecting the ureter typically cause obstruction of the lumen, which can cause severe and spasmodic pain, often referred to as ureteric colic. Ureteric colic usually starts at the costovertebral angle and radiates down into the groin and even into the penis or labia majora. On examination, the findings may include suprapubic fullness and tenderness, and rarely acute urinary retention if the stone has obstructed the bladder neck or urethra. The classic presenting triad of flank pain, gross haematuria and a palpable abdominal mass is rarely seen now as the majority of renal carcinomas are diagnosed at an early stage during abdominal imaging for unrelated and non-specific symptom complexes. Renal carcinoma can give rise to symptoms secondary to local extension, haemorrhage, metastatic spread or paraneoplastic syndromes. Tumour extension into the renal vein can give rise to bilateral peripheral oedema and a varicocele, which supports the role of renal imaging in any man who presents with acute distention of the pampiniform plexus. Other symptoms and signs of advanced disease include weight loss, fever, bone pain, respiratory symptoms and palpable cervical lymphadenopathy. Approximately 20 per cent of patients with a renal cell carcinoma experience systemic symptoms associated with a diverse range of paraneoplastic syndromes. These usually improve and return to normal following treatment by radical nephrectomy. Individuals with this rare hereditary cancer syndrome (1 in 36 000 births) can develop bilateral, multifocal renal tumours and cysts, haemangioblastomas of the cerebellum and spine, phaeochromocytomas, pancreatic islet cell tumours, retinal haemagiomas and epididymal cystadenomas. Typically, the condition presents with a painless abdominal mass in a relatively well child. Pain is unusual but can occur secondary to tumour rupture and haemorrhage following minor abdominal trauma. Renal Pelvis and Ureteric Cancer Over 90 per cent of tumours that occur in the renal pelvis and ureter arise from the epithelial cell lining of the upper urinary tract, and these are referred to as urothelial or transitional cell carcinomas. Most patients present with microscopic or gross haematuria, less common presentations including flank pain, dysuria or symptoms of advanced disease, including weight loss, anorexia and bone pain. Less common forms of bladder cancer include squamous cell carcinoma, adenocarcinoma and neuroendocrine tumours. Adenocarcinoma may develop in the bladder as a secondary metastatic lesion from a primary site in the prostate, ovary, endometrium or rectum. Bladder cancer should be considered and excluded in all patients with unexplained irritative bladder symptoms, especially if they have had exposure to urothelial carcinogens. Patients with advanced disease may present with weight loss, flank pain secondary to ureteric obstruction, and pelvic and/or bone pain. At the time of the initial diagnosis, the disease is confined to the superficial bladder wall (Table 39. Examination carried out under anaesthesia allows a more thorough assessment, when the size of the mass and the location and mobility of the tumour can be determined. If the bladder tumour is immobile and the bladder is fixed in position, this suggests that the cancer has invaded the adjacent organs and or the pelvic side wall. Examination should assess for hepatomegaly and lymphadenopathy, both features of metastatic disease. Urethral Cancer Urethral carcinoma is a rare malignancy that is more common in women, with a female to male ratio of 4:1. The majority of women present with urethral bleeding, urinary frequency and a slow or intermittent urine flow.
Diseases
- Acute myeloid leukemia, secondary
- Sinus cancer
- Osteogenic sarcoma
- McKusick type metaphyseal chondrodysplasia
- Upington disease
- Succinic acidemia
- Meckel like syndrome
- Pulmonary atresia with ventricular septal defect
- Chromosome 6 Chromosome 7
Cheap glucophage sr
It is most commonly seen in the region of the metaphysis of the long bones in children aged between 4 and 10 years medicine gif buy cheap glucophage sr 500mg line. It contains both cartilage and bone and commonly occurs at the metaphyses of the long bones. There is a 10 per cent risk of sarcomatous change in individuals with multiple lesions. Malignant transformation is rare in solitary lesions but occurs in a small proportion of cases where multiple lesions are present. Chondromyxoid fibromas and fibromas are rare benign tumours made up of defined tissue and usually presenting as incidental radiological findings. Its histological characteristics are similar to those of an osteoma, but the lesion exceeds 1 cm in diameter and may be of a considerable size. The expanding osteolytic lesion contains bloody fluid and may be the site of a pathological fracture. Giant Cell Tumour (Osteoclastoma) these are neoplasms made up of osteoclasts that form osteolytic tumours. The majority of tumours occur around the knee, with local swelling, heat and dilatation of the superficial veins. Some tumours recur after excision, and a small proportion are malignant from the outset. The common presentation of the bony deposits is with pathological fractures affecting the ribs and vertebrae. Many osteoscarcomas occur around the knee and the upper end of the femur and humerus. As with most sarcomas, spread of the tumour is usually by the bloodstream to the lungs. About half of the lesions occur in the pelvic girdle and ribs, together with the proximal femur. The presentation is usually of an increasing size of a long-standing swelling in the axial skeleton. They are highly malignant, invading locally and metastasizing to lymph nodes as well as via the bloodstream. Both fibrosarcomas and synovial sarcomas may arise independently of bone, within muscle or subcutaneous tissues. The femur, tibia, humerus and fibula are most commonly involved, but the pelvis and ribs can also be affected. Patients may present with a complication of the metastasis, such as local pain or a pathological fracture. The most common primaries are carcinoma of the breast, bronchus, kidney, thyroid and prostate. The outer surface of bones is a dense irregular connective tissue membrane called the periosteum. In children, the cortical bone is more elastic than it is in adults and is therefore, as a result of plastic deformation, able to tolerate bending without complete fracture. A high index of suspicion is needed to recognize the early development of compartment syndrome, which is a limbthreatening condition that can follow a fracture. Osteoporotic fractures most commonly affect the vertebral bodies, hip and distal radius. A proximal comminuted fracture of the tibia with a 15 cm open wound, massive tissue devitalization and evidence of popliteal artery transection is classified as which one of the following Gustilo and Anderson types The potential complications of a limb compartment syndrome include which one of the following If left untreated or treated late, compartment syndrome in a limb leads to muscle necrosis, nerve damage, myoglobinuria, contractures, limb loss and systemic toxicity. This is infection of the bone that commonly spreads via the bloodstream in children or results from direct contamination in the setting of an open fracture. This is an emergency condition characterized by a swollen joint, severe pain and limitation of the range of motion. Cellulitis is suspected when skin erythema, warmth and tenderness are present, sometimes in the absence of systemic toxicity or deeper infections involving the joints, bones or muscles. It is important to inspect the skin for potential ports of entry of microorganisms. Formerly called reflex sympathetic dystrophy, this refers to chronic pain, swelling and skin changes following trauma or surgery that are usually attributed to an inappropriate response to soft tissue injury. It initially presents with malaise and lethargy, followed by spots on the skin, spongy gums and bleeding from the mucous membranes. This is a cancer of the plasma cells, a subtype of white blood cells that generate antibodies. This is a bone disorder caused by hyperparathyroidism that leads to bone pain and tenderness, deformities and fractures. Achondroplasia is a common cause of dwarfism resulting from a mutation in the fibroblast growth factor receptor 3. Without the ability to perform a proper physical examination, the use of additional diagnostic laboratory testing may be excessive, expensive and lacking the precision that comes only from recognizing important musculoskeletal physical findings. Most flexion movements are forward movements, the major exception being flexion of the knee. Most extension movements are backward movements, the exception being extension of the knee. This usually results from injury, which either damages the long extensor tendon or tears the tendon from the bone. When the hand is subsequently straightened out, the affected finger remains bent and then straightens with a click. The two major types of knee or femoral-tibial angular deformity are genu varum (bow legs) and genu valgum (knock-knees). It is often detected during a routine physical examination as an asymmetry in shoulder height, an apparent discrepancy in leg length and asymmetry of the chest wall. Diagnostic manoeuvres and/or stress tests can be used to further assess joint function and stability. Always check for any associated neurological and vascular effects of joint disease, especially after injury. This may be primary, resulting from a combination of age and hereditary and environmental factors, or secondary, resulting from trauma, infection or underlying rheumatic inflammatory disorders. Osteoarthritis usually affects the weight-bearing joints including the hips and knees (from which crepitus can be felt or heard). It primarily affects the joints of the fingers and toes closest to the nail, resulting in deformed nails and nail beds. Ankylosing Spondylitis In ankylosing spondylitis, spinal disease generally occurs early and results in decreased movement in all planes, together with tenderness at the sites where the ligaments insert onto the bones (enthesitis). The peripheral joints may be involved in patients with ankylosing spondylitis, reactive arthritis or psoriatic arthritis. Unilateral uveitis is the most common extra-articular complication of ankylosing spondylitis. Pain caused by gout can also occur in other joints of the body, such as the knees, wrists, ankles and hands, and tends to subside within the first 24 hours of when the attack occurred. Once the sharp pain around the joints has subsided, more subtle pain and general discomfort can be felt around the affected areas. This can last from just a few days to many weeks before all the pain has completely gone. Crystals are also deposited in gouty tophi in the helix of the ear, in the eyelid and around the elbow joint. Pseudogout is similar to gout but tends to affect the knees in individuals aged 50 years or older. Crystal analysis of the joint aspirate reveals monosodium urate crystals in gout and pyrophosphate crystals in pseudogout. This is a chronic autoimmune inflammatory arthropathy that predominantly affects middle-aged women.
Discount 500 mg glucophage sr
Subcutaneous emphysema may be extensive symptoms gonorrhea order 500mg glucophage sr amex, and can be associated with voice changes and extension into the face and abdominal soft tissues. Subcutaneous emphysema is never life-threatening in isolation, but the cause must be quickly elucidated as it may pose a threat to life. The most impressive and rapidly developing subcutaneous emphysema is associated with major airway injuries such as tracheal injuries. In some cases, forceful exhalation against a closed glottis can result in subcutaneous emphysema. Massive haemoptysis is usually a life-threatening finding, and can result in flooding of the contralateral airway and normal lung with blood, resulting in rapid decompensation. A patient with a massive haemoptysis should be placed with the offending side downwards, and an airway should be established (usually with an endotracheal tube). A device such as a bronchial blocker can then be placed in the bronchus of the affected side, preventing the haemoptysis from filling the airways of the contralateral unaffected side. Massive haemoptysis may require surgical evaluation or angiographic evaluation and treatment. This can usually be associated with dullness to percussion and distant breath sounds on the affected side. Violation of the distal airways in a lung laceration may also produce a pneumothorax (air in the pleural space), which if untreated may result in a tension pneumothorax. Treatment of a tension pneumothorax requires decompression of the affected pleural space. This can be accomplished by needle compression of the hemithorax in the second intercostal space at the midclavicular line. Failure of a pulmonary laceration to heal may result in a chronic air leak, which characterizes an alveolar-pleural fistula. This is a communication between the alveoli and the pleural space that occurs when the parietal pleura in the region of a pulmonary laceration fail to heal. An injury to the distal bronchial airway that fails to heal leads to the formation of a bronchopleural fistula. Alveolar-pleural fistulae are more prone to healing over time than are bronchopleural fistulae. This occurs when the negative intrathoracic pressure created during respiration forces air into the thoracic cavity through the wound, creating a sucking noise. A sucking chest wound is managed by placement of a one-way valve over the wound, which prevents air entry during inspiration but allows air exit during expiration. Patients present with tachycardia, tachypnoea, absent breath sounds on the affected side, difficulty breathing, shortness of breath, increasing anxiety and chest pain. Some pathological states may predispose a patient to spontaneous pneumothoraces; these include lymphangioleiomyomatosis, which predominantly affects women of childbearing age, and connective tissue disorders. They characteristically occur in tall slender adult males or females, are recurrent and can be bilateral. Pneumothoraces may also be iatrogenic and can occur with central venous access, thoracentesis, mediastinal biopsies and mechanical ventilation with high positive end-expiratory pressures. It is due to an asymmetrical development of the costochondral cartilages along the distal one-third of the sternum. It is characterized by an increased Haller index, which is the ratio between the lateral and anteroposterior dimensions of the thoracic cavity. Patients with pectus excavatum most frequently present with decreased exercise tolerance, cardiac arrhythmias (due to compression of the right ventricle of the heart) and increased psychosocial awareness of the deformity. Spontaneous Pneumothorax Spontaneous pneumothoraces occur in the absence of chest trauma. It is characterized by a convex deformity of the chest wall due to an exaggerated asymmetrical development of the costochondral cartilages of the distal thoracic cavity. Like pectus excavatum, it is commonly present in pubertal and prepubertal boys who present with an increased psychosocial awareness of the deformity. The right pleural cavity is more lucent than the left, and there is an absence of any lung markings. An aortic aneurysm is less likely to be diagnosed by physical findings on the chest wall. These infectious complications produce much morbidity and in some cases mortality in the hospitalized patient. Those more prone to pulmonary complications include active cigarette smokers, debilitated patients, patients requiring prolonged mechanical ventilation, individuals with altered mental status and those at risk of aspiration. General endotracheal anaesthesia often results in a diminished ability to clear the airway secretions, leading to pooling in the airways. Failure to clear these secretions allows for a nidus of infection to be created, especially if aspiration, poor respiratory mechanics and a decreased ability to cough are present. Pre-existing microbial flora from the oropharynx and gastrointestinal tract or from nasopharyngeal colonization provide the inoculum for the subsequent pneumonia. If pneumonia goes undiagnosed or is unsuccessfully treated, this can result in the formation of a parapneumonic effusion. This complication, along with lung abscess, bronchiectasis, impaired oxygenation and ventilation and a persistent catabolic state, often leads to profound respiratory embarrassment. Patients present with fever, chills, a productive cough or an inability to cough (as in the debilitated post-surgical patient), hypoxia, tachypnoea, tachycardia and pleuritic chest pain. Imaging of the chest reveals lobar consolidation, parapneumonic effusions, atelectasis and a loss of lung volume. Bronchoscopy with bronchoalveolar lavage and culture allows a bacteriology result that will direct appropriate antibiotic therapy. Flexible fibreoptic bronchoscopy performed at the bedside in hospitalized patients has made diagnosis and treatment of this significant problem much more focused. Early parapneumonic effusions should be drained with a tube thoracostomy to prevent an empyema developing. The cartilage expands, creating the palpable mass that is often associated with this process. Costochondritis is usually treated with non-steroidal anti-inflammatory agents, with good results. Patients present with symptoms of pain in the distribution of the affected intercostal nerve and may have a palpable mass on the affected costochondral joint. Other primary neoplasms include chondromas, rhabdomyosarcomas, malignant fibrohistiocytomas and desmoid tumours. Secondary neoplasms such as metastatic breast cancer, prostate cancer or multiple myeloma may also occur. This can be due to mucous plugging of the airway, or a neoplasm occluding the airway. In the post-surgical patient, this is often due to incomplete re-expansion of the lung after general anaesthesia. Splinting (rigidity of the chest muscles) due to pain during normal respiration also results in the development of atelectasis because of incomplete aeration of all the lung fields and a lack of re-expansion of the airways. Failure of the atelectasis to resolve provides a nidus for bacteria and the subsequent development of a pneumonia, with the potential formation of a lung abscess. In young children, atelectasis can also occur after the inhalation of a foreign body that occludes a segment of the airway. Chest Wall Abscesses these may arise as a result of any number or bacterial or mycobacterial pathogens. In the absence of concomitant pulmonary pathology, they may be associated with an infected lymph node or focus of infection in the underlying rib. Underlying tuberculous disease may present in this fashion in an indolent yet persistent course. Fungal or amoebic infections, or hydatid cysts, may also result in lung abscesses. Lung abscesses are characterized by destruction of the pulmonary parenchyma and can be associated with bleeding as a result of erosion of the bronchial arteries. In some cases, disruption of a surrounding airway leads to rupture of the abscess into the airway, and a bronchopleural fistula may arise.
Order generic glucophage sr from india
Impingement syndrome of the shoulder is mechanical irritation of the rotator cuff tendon underneath the anteroinferior portion of the acromion medicine nobel prize 2015 buy generic glucophage sr, especially when the shoulder is placed in the abducted, forward flexed and internally rotated position. The sulcus sign demonstrates the inferior instability, while the load shift test reveals anterior and/or posterior instability. Humeral shaft fractures are associated with radial nerve palsy in up to 18 per cent of cases. The nerve is especially at risk at the junction of middle and distal thirds of the humeral shaft where is emerges from the spiral groove. Injury to the nerve results in weakness of the wrist extensor muscles, resulting in wrist drop. For each of the following conditions, select the most likely association from the list below. Each option may be used once, more than once, or not at all: 1 Radial nerve palsy 2 Axillary nerve palsy 3 Suprascapular nerve palsy 4 Long thoracic nerve palsy 5 Ulnar nerve palsy a Humeral surgical neck fracture b Mid-clavicular fracture c Humerus shaft fracture d Atrophy in the supraspinatus fossa e Medial winging of the scapula Answers a 2 Axillary nerve palsy. The nerve winds around the surgical neck of the humerus approximately 7 cm distal to the tip of the acromion. Loss of sensation over the shoulder area and/or or loss of arm abduction is a potential complication resulting from denervation of the deltoid muscle. On rare occasions, medial cord injury and ulnar nerve palsy, for instance, can occur. Fractures of the humeral shaft, especially at the junction of the middle and distal thirds of the humerus, endanger the radial nerve as it emerges from its spiral groove. Atrophy in the supraspinatus fossa can be appreciated by seeing and palpating a depression over the fossa of the scapula when examining the upper back. It can result from overtension of the nerve secondary to a torn and retracted rotator cuff tendon. Medial winging of the scapula presents with shoulder and scapular pain, weakness when lifting objects and discomfort when sitting on a chair. It is more commonly seen in young athletes due to long thoracic nerve injury from repetitive stretch or chest compression injuries during sports. The serratus anterior muscle is then denervated and the scapula elevates off the chest wall and migrates medially. The tip of the olecranon and the medial and lateral epicondyles form an equilateral triangle when the elbow is flexed. This relationship is preserved in supracondylar fractures but lost in dislocations. Effusions are seen as a bulge emphasizing the concavity between the olecranon and the lateral epicondyle. The triangular sulcus is a landmark for access to the elbow joint as it lies between these two structures and the radial head. An increased angulation is known as cubitus valgus, and decreased angulation as cubitus varus, a common deformity in the malunion of supracondylar fractures. The radial head, and its rotatory movement, is palpable l cm distal to the lateral epicondyle. There is pain along the lateral border of the elbow, which radiates proximally and distally. Grasp the lower forearm in the left hand and, while the patient continues to try to keep the Tennis Elbow (Lateral Epicondylitis) this is a common overuse condition, often provoked by heavy repetitive physical activity involving rotation at the elbow. Radial Tunnel Syndrome this condition causes lateral elbow and radial forearm pain. The problem is produced by radial nerve compression as it passes through the radial tunnel. The pain can be provoked by extension of the middle finger against resistance and by supination of the forearm against resistance. There is pain, aggravated by throwing, and tenderness located at the medial epicondyle at the common flexor origin. In the vicinity of this landmark are other potential compression sites including the medial intermuscular septum proximally and the flexor carpi ulnaris aponeurosis distally. Cubitus valgus or varus deformities, burns and occupational or athletic overuse also predispose to developing this condition. There may be wasting of the muscles of the hypothenar eminence, as well as of the intrinsic muscles of the hand. Rupture of the long head of biceps occurs in the elderly and is due to attrition of the tendon as it passes through the bicipital groove. Biceps and Triceps Tendinitis Bicipital tendinitis causes pain, either proximally along the bicipital groove in the upper arm or distally at the insertion of the tendon over the antecubital fossa. Tricipital tendinitis causes posterior elbow pain and tenderness at the triceps insertion. Arthritis of the Elbow Joint Osteoarthritis Osteoarthritis is manifest by pain, swelling and a loss of range of motion. Occasionally, there are severe degenerative changes including osteophytes, subchondral cysts and intra-articular loose bodies that lead to the symptoms of intermittent locking. Rheumatoid Arthritis/Tuberculosis Rheumatoid arthritis is not uncommon in the elbow, with pain due to intra-articular manifestation, ranging from synovial hypertrophy to soft tissue involvement such as adjacent rheumatoid nodules and periarticular tendon ruptures. The muscle wasting associated with tuberculous infection and joint swelling produces a fusiform configuration across the elbow joint. Rupture of the Biceps the biceps is subject to rupture of its muscle belly at both the proximal and distal attachment. This repetitive microtrauma leads to osteochondritis dissecans and even the appearance of osteochondral loose bodies, resulting in locking and crepitus. This extension overload may lead to the development of osteophytes, chondromalacia and loose bodies. There is posterior pain, tenderness over the olecranon, loss of extension, and pain when the examiner passively extends the elbow with a valgus force. The distal fragment of the humerus is usually displaced posteriorly and tilted dorsally (an extension-type injury). Pain on passive stretch of the fingers is an important red flag for compartment syndrome. Less commonly, the median, radial or ulnar nerve is affected, and these usually undergo a gradual recovery. Malunion is common and may present with an elbow in a valgus, varus, extension or flexion deformity. Intercondylar T-shaped Fractures these fractures constitute adult elbow fractures that are sustained through a fall on the elbow. Such fractures involve the articular surface, and, as in children, the neurovascular structures are also at risk. Fractures of the Epicondyles Fractures of the lateral epicondyle in adults and the epiphysis in children are produced by lateral angulatory forces applied to the fully extended elbow. The lateral epicondyle is subject to delayed or non-union, and healing of the medial epicondylar epiphysis is usually by a fibrous union. Cubitus valgus or varus, degenerative joint disease and ulnar nerve injury are potential complications of these injuries. Fractures of the Olecranon Fractures of the olecranon can range from simple avulsion to a comminuted fracture-dislocation. In a significant fracture, the ability to extend the elbow against gravity, as a result of the action of triceps, is lost. An effusion is present, and the elbow is painful in flexion, extension, and mostly supination and pronation.
Buy generic glucophage sr pills
Diffuse Thickening of the Bladder Wall the most common causes of diffuse bladder wall thickening are bladder nondistention medications you cant drink alcohol with generic 500mg glucophage sr, pancystitis, and trabeculation (Box 6-6). There is diffuse thickening of the bladder wall (asterisk) on this axial T2-weighted image. A large mass (open arrow) invades the perivesical fat extensively (arrow) and has grown to the sidewall of the left hemipelvis. Coned-down view of the bladder demonstrates a focal filling defect with a lobulated margin (open arrow) near the left ureterovesical junction. There is nothing specific about the radiographic appearance of this rare benign neoplasm, which cannot be distinguished from papillary urothelial carcinoma. The bladder mucosa and submucosa show a similar degree of enhancement to the bladder tumor (short white arrows); however, the muscularis propria (arrowhead) is hypoenhancing relative to the tumor, mucosa, and submucosa. Trabeculation Trabeculation of the bladder wall is observed most commonly in patients with chronic bladder-outlet obstruction or neurogenic bladder. Radiographically, trabeculation is a generalized irregularity of the inner or luminal contour of the bladder when the bladder is filled with urine. Bladder wall thickening resulting from detrusor contraction or incomplete relaxation is normal in an underfilled bladder. Cystometry has shown a strong association between radiologic trabeculation of the bladder and detrusor instability, defined as a pressure rise of more than 15 cm H2O during bladder filling. In the absence of detrusor instability, outflow obstruction with high intravesical pressure produces the same effect on the detrusor muscle, and therefore trabeculation. Trabeculation was once thought to result from hypertrophy of the detrusor muscle in response to an increase in bladder outflow resistance. This opinion was based on the frequent correlation of trabeculation with bladder-outlet obstruction, particularly when it resulted from benign prostatic hyperplasia. However, histologic studies of trabeculated bladders have found infiltration of detrusor smooth muscle by connective tissue elements and not muscle hypertrophy. A, Computed tomography demonstrates a soft-tissue mass (arrow) anterior to the apex of the prostate gland. These signs include prostatic impression on the base of the bladder, hooking or J configuration of the juxtavesical ureters caused by elevation of the trigone, and large postvoid residual. A, Coned-down view of the bladder from an intravenous urogram demonstrates diffuse thickening of the bladder wall (small arrows), which has a finely lobulated contour. A focal, rounded filling defect (open arrow) is seen next to a large prostatic impression along the base of the bladder. B, Sonography of the bladder in the transverse plane demonstrates focal enlargement of the median lobe of the prostate as the cause of the rounded filling defect. An elderly patient with benign prostatic hyperplasia presented with severe pelvic pain. Sonography showed multiple hypoechoic areas (arrows) in the wall of the trabeculated bladder. Cystitis Cystitis is inflammation of the urinary bladder wall and may be focal or diffuse. For simplicity of discussion here, cystitis is classified according to etiology (Box 6-7). The term cystitis is often combined with a clinical descriptor, especially if the etiology is multifactorial or unknown (Box 6-8). For instance, viral, radiation, or cyclophosphamide cystitis may manifest as a hemorrhagic cystitis. Polypoid cystitis is a reactive urothelial hyperplasia that protrudes into the lumen of the bladder as a polyplike growth (polypoid pseudotumor). The terms cystitis cystica and cystitis glandularis refer to particular histopathologic variants of chronic cystitis, which may be better characterized as forms of urothelial metaplasia. Cystitis glandularis (intestinal type) has been associated with an increased risk of adenocarcinoma of the urinary bladder and these patients should be monitored closely. Acute cystitis refers to bladder inflammation of recent symptomatic onset and rather short duration. Radiographically, a completely normalappearing bladder is not uncommon, despite the presence of cystoscopic abnormalities such as ulcerations, petechiae, or erythema. Bladder compliance often is decreased in patients with chronic cystitis, and elevated intravesical pressures may cause ureteral dilatation and vesicoureteral reflux. Although the inflammatory process often affects the entire bladder wall (pancystitis), occasionally cystitis is more marked or at least more radiographically apparent focally. A common example is bullous edema, which frequently accompanies pancystitis of various causes. Mechanical cystitis, often resulting from 206 GenitourinaryRadiology:TheRequisites irritation by a foreign body such as a catheter, is also a focal process in many patients. Bacterial cystitis is the most frequent type of infectious cystitis encountered in developed countries. Bacterial cystitis most often occurs in women who are sexually active and is thought to result from retrograde deposition of bacterial flora that normally inhabits the vagina. In women, routine radiographic evaluation is usually not indicated unless cystitis is recurrent or difficult to eradicate. In men, cystitis is most often associated with bladder-outlet obstruction, typically secondary to benign prostatic hyperplasia. Urinary tract calculi, urethral strictures, and urethral catheterization may also predispose to cystitis. Evaluation of the bladder and urethra is indicated with the first episode of bacterial cystitis in men to exclude lower urinary tract anomalies or obstruction. Emphysematous cystitis, an unusual manifestation of bacterial cystitis, is discussed later in the chapter. An unusual manifestation of recurrent bacterial infection is malacoplakia, a granulomatous inflammatory process that affects the urinary bladder and the distal ureter. This disease is more common in immunocompromised patients and in patients with diabetes mellitus and is associated with E. The proffered pathogenesis of malacoplakia is deficient function of lysosomes in macrophages, causing a chronic and ineffective response to urinary tract infection. At histology, basophilic inclusions are seen within macrophages (Michaelis-Gutmann bodies). Normal bladder wall thickness is not well established; however, in general, a wall thickness of 1 to 3 mm of a distended urinary bladder may be considered normal and a thickness greater than 5 mm is considered abnormal. On radiologic imaging studies, malacoplakia usually appears as multiple raised but sessile filling defects, 5 to 10 mm in diameter. Central umbilication of these flat lesions may be seen, and there is a predilection for involvement of the bladder base. When malacoplakia is found in the lower ureter, there may be contiguous areas of stricture. Viral cystitis is most often seen in children and in immunocompromised patients and is rare in immunocompetent adults. Patients typically present with dysuria and gross hematuria, manifestations of a hemorrhagic cystitis. The capacity of the urinary bladder is decreased markedly, and mural nodularity may take the form of multiple polypoid filling defects. Differentiating viral cystitis from sarcoma botryoides in children can be difficult. An important distinguishing feature is reduced bladder capacity; in patients with sarcoma botryoides (a type of rhabdomyosarcoma), the bladder capacity is normal or increased. Schistosomiasis of the urinary bladder is a frequent cause of lower urinary tract disease in patients in underdeveloped countries. Tuberculosis of the genitourinary tract follows hematogenous dissemination from the lung or, less often, from the skin or gastrointestinal tract. Cystitis usually follows spread of renal infection into the collecting system and can be seen in 10% to 20% of patients with chronic urinary tract tuberculosis. Focal, irregular mural filling defects caused by mucosal tuberculomas may be seen early in the course of tuberculous cystitis and can simulate neoplasia. If the infectious process proceeds unchecked, transmural involvement occurs and may result in fibrosis and associated reduction in bladder capacity. Bizarre configurations of the urinary bladder may be observed in chronic tuberculous cystitis when the fibrotic process is nonuniform.