Buy kamagra chewable with a mastercard
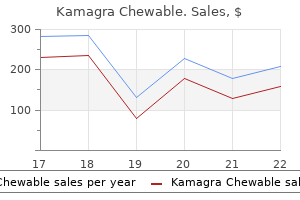
Exercise duration should be at least 20 to 30 minutes and at an exercise frequency of 3 to 5 days/week erectile dysfunction diabetes type 2 treatment generic kamagra chewable 100mg mastercard. Exercise modalities for aerobic training include walking/jogging (treadmill), elliptical trainer, rowing, cycling, and stair climbing. Resistance training is an important part of the exercise program for patients with and without heart disease and is particularly beneficial in those with diabetes, stable heart failure, and older adults. Improvements in muscle strength and endurance with resistance training help with activities of daily living and returning to the workplace. Modality: Common modalities for resistance training include free weights, weight machines, wall pulleys, elastic bands, and calisthenics. Aerobic interval training appears to improve cardiovascular fitness in patients with heart failure and after coronary artery bypass as compared to standard exercise programs; however, limited safety and efficacy data preclude the routine inclusion of aerobic interval training in physical activity recommendations for individuals with cardiovascular disease at this time. How can we encourage our patients to engage in regular physical activity or exercise Healthcare providers should promote physical activity by assessing activity levels in routine office visits and then prescribing it when warranted. Wearable devices that can measure physical activity are now commercially available and are reasonably accurate. Use of these devices to encourage and monitor physical activity offers promise in this effort, and they are currently being investigated in many ongoing studies. Lower referral and enrollment/ completion of cardiac rehabilitation programs are found more commonly in patients who are female, older, and minorities and have lower socioeconomic status and lower education levels, speak languages other than English, lack insurance coverage and social support, and have work constraints. Efforts to address these barriers and improve participation rates are being explored: new home- and Internetbased cardiac rehabilitation programs for lower risk patients and offering individualized programs (woman-specific, lower cost, less intensive options, with counseling and coaching help by nonphysician medical professionals by all means of communication-in person, phone, apps, and Internet). The risk of adverse cardiac events in healthy individuals is extremely low and varies depending on age, gender, level of fitness, and medical conditions. Routine screening electrocardiography for all athletes is not presently recommended. Healthy individuals without cardiovascular disease or symptoms can start mild- to moderate-intensity exercise programs without pre-participation medical evaluation. Unstable coronary heart disease, decompensated heart failure, symptomatic valvular stenosis, severe systemic hypertension, and uncontrolled arrhythmias are absolute contraindications to exercise. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Exercise standards for testing and training: a scientific statement from the American Heart Association. Exercise rehabilitation in peripheral artery disease: functional impact and mechanisms of benefits. Relationship between cardiac rehabilitation and longterm risks of death and myocardial infarction among elderly Medicare beneficiaries. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: preamble, principles, and general considerations: a scientific statement from the American Heart Association and American College of Cardiology. American College of Sports Medicine guidelines for exercise testing and prescription (9th ed. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. How have the cardiac manifestations of human immunodeficiency virus/acquired immunodeficiency syndrome changed over the years Because patients tended to be younger, very little coronary atherosclerosis was noted. It only rarely progresses to tamponade, which is more common in end-stage, cachectic patients who develop elevated intrapericardial pressures caused by low right-sided filling pressures (low-pressure tamponade). The presence of an effusion, however, is an independent predictor of mortality in these patients. Rarely, Kaposi sarcoma can bleed into the pericardium, resulting in tamponade physiology. This tumor is often found in the subepicardial fat around surface coronary arteries. Selenium deficiency increases the virulence of coxsackievirus to cardiac tissue and is reversed by repleting selenium. Low levels of B12, carnitine, growth hormone, and T4 can cause a reversible myopathy. Therapy includes those used for primary pulmonary hypertension, including intravenous epoprostenol and endothelin antagonists. Use of diagnostic stress testing is performed in these patients according the current guidelines for the general population. Based on autopsy studies, these lesions have features of both atherosclerosis and transplant vasculopathy. These lesions reveal diffuse circumferential involvement with smooth muscle cell proliferation and elastic fibers, leading to endoluminal projections. Acute coronary syndrome in human immunodeficiency virus patients: exploiting physiopathology to inform the clinical practice. This is a disorder characterized by selective loss of adipose tissue from subcutaneous areas of the face, arms, and legs, with redistribution to the posterior neck (buffalo hump) and visceral abdomen. Exercise with or without treatment with metformin has been reported to improve body composition in patients with lipodystrophy. Treatment of dyslipidemia should include attempts to manage common comorbid conditions, including obesity, hypertension, and diabetes. Patients should be counseled with regard to the importance of dietary modification, regular exercise, weight loss, tobacco cessation, and adherence to prescribed medical therapy for other comorbid conditions. Pravastatin and ezetimibe, which are not metabolized by the cytochrome P450 pathway, are also safe to use in this setting. Niacin has been shown to reduce triglyceride levels, but it does increase insulin resistance; its benefit is therefore unclear. Fish oil (omega-3 fatty acids) is well tolerated and has been shown to decrease triglyceride levels. Human immunodeficiency virus and heart failure in low- and middle-income countries. Pulmonary hypertension and human immunodeficiency virus infection: epidemiology, pathogenesis, and clinical approach. What a cardiologist needs to know about patients with human immunodeficiency virus infection. What is the leading cause of mortality in patients with rheumatoid arthritis, and what are the most common cardiac manifestations of rheumatoid arthritis What pathophysiologic mechanisms contribute to accelerated atherosclerosis in patients with rheumatoid arthritis These vegetations carry a high risk of thromboembolism, necessitating lifelong anticoagulation. What cardiovascular medications are associated with drug-induced lupus erythematosus Who is at risk for antiphospholipid syndrome, what are its most common cardiovascular manifestations, and how is it typically treated Pathophysiologic mechanisms associated with accelerated atherosclerosis in patients with rheumatoid arthritis. Nonbacterial valvular vegetations (Libman-Sacks vegetations) (arrows) on the mitral valve. Libman-Sacks endocarditis can be observed in patients with systemic lupus erythematosus and is a form of non-bacterial endocarditis. Primary prophylaxis with low-dose aspirin has unproven benefit but may be reasonable in patients with increased cardiovascular risk. Acute thrombotic events are generally treated with heparin followed by long-term anticoagulation with warfarin (target international normalized ratio of 2. The hallmark of cardiac involvement in systemic sclerosis is patchy biventricular myocardial fibrosis. Fibrosis can directly cause systolic and/or diastolic heart failure or can do so indirectly via impaired coronary artery flow reserve.
100 mg kamagra chewable amex
An important characteristic of atrial flutter is that the atrial activation is the same from beat to beat erectile dysfunction over 75 generic 100 mg kamagra chewable. The prevalence is 1% in the general population and increases with age (>10% in octogenarians). If conduction from the atrium to the ventricle occurs in fixed ratios (such as 4:1, as shown here), the ventricular response can also be regular. There is also an association with high-intensity endurance exercise and hereditary components. In addition to stroke risk assessment, a discussion regarding anticoagulation should include an assessment of bleeding risk and involve shared decision making to take into account patient preferences. Several online decision aids have been developed to inform the risk/benefit discussion. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. Transesophageal echocardiographic image of thrombus in the left atrial appendage (arrows). What are the alternatives to anticoagulation for the prevention of stroke and systemic embolism with atrial fibrillation The most commonly used agents are beta-blockers, followed by nondihydropyridine calcium channel blockers (which include diltiazem and verapamil). Digoxin is less commonly used but has a role in more sedentary patients and in those with reduced left ventricular function. Amiodarone may rarely be used as a rate control agent in patients when other agents have failed or are contraindicated, such as in critically ill patients. At 3 years the primary composite endpoint of cardiovascular death, hospitalization for heart failure, stroke, embolism, bleeding, or life-threatening arrhythmic events was similar between the two groups (12. Although there are a number of caveats to this trial, it is reasonable in clinical practice to use a more permissive ventricular target rate as long as symptoms are controlled and the left ventricular function is preserved. What are the reasons to pursue maintenance of sinus rhythm in patients with atrial fibrillation An important reason to consider a rhythm control approach is inability to achieve adequate rate control, especially when associated with a tachycardia-mediated cardiomyopathy. Other factors that might favor trying to maintain sinus rhythm include patient preference and young patient age. Are anticoagulation recommendations different for patients with paroxysmal versus persistent atrial fibrillation If no thrombus is seen, it is reasonable to proceed with cardioversion and then continue anticoagulation for at least 4 weeks afterward. In the former scenario, in which no beats of sinus rhythm are seen, the issue is energy delivery. Things that can improve energy delivery include increasing shock strength (joules), using a biphasic rather than monophasic waveform, changing the shock vector by altering the electrode pad position, pressing on the anterior electrode pad during shock delivery with a gloved hand, or using a drug such as ibutilide prior to energy delivery. Side effects due to amiodarone treatment are common and include organ toxicity to the lung, thyroid, and liver. It also can cause bluish discoloration of the skin, photosensitivity, tremor, peripheral neuropathy, ocular deposits, and optic neuropathy. Monitoring of patients while on amiodarone varies by clinician but includes periodic laboratory testing for liver and thyroid dysfunction, as well as chest radiography and pulmonary function testing. What are some risk factors for torsades de pointes associated with antiarrhythmic drug therapy Ablation, using energy, such as radiofrequency or cryoablation, results in isolation of the electrically active sleeves of myocardium at the pulmonary vein junctions in what is termed pulmonary vein isolation. Ablation is reserved primarily for symptomatic patients refractory to antiarrhythmic medication, although in select patients it may be appropriate as first-line treatment. When is it appropriate to stop anticoagulation after atrial fibrillation catheter ablation Potential complications include access site complications, cardiac tamponade, stroke, pericarditis, phrenic nerve paralysis, pulmonary vein stenosis, and esophageal fistula. Atrial fibrillation in a patient with Wolff-Parkinson-White syndrome ("pre-excited" atrial fibrillation). This pattern is characteristic of atrial fibrillation in a patient with Wolff-Parkinson-White syndrome in which anterograde conduction occurs to varying degrees over the atrioventricular node and the accessory pathway. If the accessory pathway is capable of rapid conduction, the ventricular response can be very rapid and potentially degenerate to ventricular fibrillation and subsequent sudden death. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. What are the causes of narrow complex irregular tachycardias (tachycardias with irregular R-R intervals) How should one go about figuring out the diagnosis of a narrow complex tachycardia What is the initial treatment for acute conversion of supraventricular tachycardia Carotid massage should be performed after carotid bruit is ruled out by applying steady pressure over the carotid sinus for 5 to 10 seconds. What pharmacologic therapies are used for acute conversion of supraventricular tachycardia Adenosine should be used with caution, if at all, in patients after heart transplant (discuss with attending). What therapies are used for patients who are hemodynamically unstable from supraventricular tachycardia What are the success and complication rates for ablation of supraventricular tachycardia Which drug is most commonly implicated in cases of drug-induced atrial tachycardia Digoxin toxicity can cause many arrhythmias; a "classic one" is paroxysmal atrial tachycardia with block. What is the most common ventricular response rate in patients who develop atrial flutter Atrial activity in atrial flutter most commonly occurs at a rate around 300 bpm, although the rate can be somewhat slower in patients on antiarrhythmic agents that slow conduction (such as amiodarone) or in diseased and dilated atria. Therefore, finding a regular narrow complex tachycardia at exactly 150 bpm should raise suspicion of atrial flutter as the causative arrhythmia. Because most cases of atrial tachycardia are due to an autonomic focus and not a reentry, the arrhythmia most commonly does not terminate with cardioversion. Previously it was believed that the risk of embolization during cardioversion for atrial flutter was negligible. However, observational studies have reported rates of embolization with cardioversion of atrial flutter ranging between 1. Although a collective review showed that the rate of embolization with cardioversion for atrial flutter was lower than the rate with atrial fibrillation (2. Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. It depends on the clinical scenario, but the most common mechanism is reentry, followed by automaticity. What is the most common underlying heart disease predisposing to ventricular tachycardia Myocardial scars leading to reentry also occur after surgical correction of congenital heart diseases. It is thought to be generated by triggered activity in the form of delayed afterdepolarizations, typically created in situations of calcium overload. Right ventricular outflow tract bigeminal premature ventricular complex originating under the pulmonic valve.
Buy discount kamagra chewable 100 mg online
One study shows that erectile dysfunction natural order 100 mg kamagra chewable amex, in infants who did not breathe for more than 20 minutes, about two-thirds of survivors are without major handicap. There are other possible reasons for a delay in establishing spontaneous respiration; we advise that if there is doubt as to whether to continue resuscitation, and if a senior experienced doctor is not available, the baby with a pulse but no breathing should be taken to the neonatal unit for ventilation and further care until more detailed assessment can be undertaken. Post-resuscitation care of the asphyxiated infant the sequelae of birth asphyxia may be divided into early and late. Early sequelae the intensive care management of early sequelae of asphyxia (multiorgan failure) is briefly outlined in Box 5. Renal impairment (see Chapter 18): 20% of asphyxiated infants develop significant renal compromise, and almost all will demonstrate oliguria, proteinuria, haematuria and elevated serum creatinine secondary to acute tubular necrosis; careful fluid management and careful monitoring of gentamicin. Gastrointestinal: necrotizing enterocolitis (see Chapter 17) may occur following a prolonged hypoxic insult; delay enteral feeding and encourage expression of breast milk. This can usually be confirmed by cerebral function monitoring/electroencephalography. Following acute intrapartum asphyxia, those infants who meet certain criteria (see Box 5. This can be achieved by switching off the overhead heater and leaving the baby exposed. The degree of encephalopathy can be confirmed by amplitude-integrated electroencephalography, but this is not essential to initiate cooling. Once the child has been referred to a cooling centre, active cooling using a cooling mattress can be started. Organ donation is possible, either after neurological death criteria or cardiac death criteria. Whole organs or tissues such as heart valves may be used, depending on the degree of ischemic injury. Parents often value this opportunity for something positive to come from their tragedy. Most can cope with the physiological stress of even a prolonged labour by utilizing alternative fuels and diverting blood to vital organs. When these mechanisms are exhausted, the baby may suffer asphyxial damage to a variety of organs, most importantly the brain. For the first time, therapeutic hypothermia offers the prospect of an effective rescue therapy. Normal transition after birth, and avoidance of further complications, can be facilitated by stabilization and resuscitation where necessary. Honest communication between perinatal teams and the parents is vital to ensure an accurate understanding of the likely prognosis for the infant and to explain the aetiology of any insult. British Association of Perinatal Medicine (2011) Guidelines for the investigation of newborn infants who suffer a sudden and unexpected postnatal collapse. Most mothers will carefully scrutinize their newborn baby and will sometimes be anxious about minor features that they discover. Major congenital anomalies will often be obvious to the parents or the midwife and may need immediate explanation. The newborn examination as a screening test In most developed countries, newborn babies are formally examined soon after birth. The purpose of these examinations is partly to reassure parents about any minor abnormalities, and also to detect anomalies which may cause significant harm if left undetected. Historically, the newborn examination was made in hospital, often by the most junior members of the paediatric team. All newborns are examined soon after birth by the attending midwife to check that there is no major congenital anomaly and to establish the sex of the baby. With early discharge home, the examination is increasingly made by community midwives or general practitioners. Approach to the newborn examination Before examining, review any relevant family or obstetric history, including any abnormalities on antenatal ultrasound scan. Ask about the birth and whether the baby needed any intervention or admission to the neonatal nursery. The mother should be present during the examination, and you should ask if she has any concerns about the baby. After careful hand washing, the baby should be undressed completely and examined on a warm surface, ideally with an overhead heater. For this reason this is not usually part of the routine newborn examination, but should be checked if a skeletal dysplasia is suspected. It may be worth leaving this until the end of the examination General appearance Colour the infant should be uniformly pink, but acrocyanosis (blueness of the hands and feet) is not abnormal. Central cyanosis, pallor, jaundice, plethora, bruises and petechial haemorrhages are abnormal and should be investigated further. Posture At term the normal position is with the hips abducted and partially flexed, the knees flexed, and the arms adducted and flexed at the elbow. Limited movement, exaggerated or asymmetrical movements, hypotonia or stiffness must be noted (see below). Skin appearance this varies with gestation; lanugo hair and relatively red skin in preterms and mild cracking and peeling in post-mature babies. African and Asian babies may show relatively little generalized pigmentation at birth, except for the genitalia. Head and neck Face There are many recognizable patterns of abnormalities based on facial features. Many are rare, but chromosomal disorders such as trisomy 21, 18 and 13 should be recognized (see Chapter 8). Cry this should be vigorous, but it should be possible to console the infant by cuddling. A cat-like cry, with microcephaly and hypotonia, is suggestive of cri-du-chat (5p-) syndrome. Plagiocephaly (parallelogram head) is usually seen as a flattening of the occipital region on one side. It is thought to be due to the position the infant has been lying in utero and has no pathological significance. Scaphocephaly (long head with flattened temporo-parietal regions) occurs commonly in premature infants and becomes less obvious with age. Fontanelles: the anterior and posterior fontanelles are very variable in size and are normally soft and flat. Bulging of the fontanelle may be due to raised intracranial pressure and is always abnormal. Craniosynostosis: this term refers to the (rare) premature fusion of one or more of the skull bones. Craniosynostosis causes abnormal head growth, the pattern depending on the affected suture. Craniotabes (ping-pong ball skull) refers to the softening of the skull bones, and with pressure the skull may be momentarily indented before springing out again. It usually has no significance, but congenital rickets, osteogenesis imperfecta or congenital hypophosphatasia may cause craniotabes. If they are too far apart (hypertelorism) or too close together (hypotelorism), this may be part of a generalized syndrome. Conjunctiva this is usually clear, but subconjunctival haemorrhages are not uncommon in otherwise normal infants. Cornea, iris and pupil the cornea should be clear, and a red reflex elicited using an ophthalmoscope. In preterm babies the presence of the tunica vasculosa lentis (a network of capillaries in the lens) may give a streaked appearance to the red reflex. Asking the mother to hold the baby against her chest and examining from over her shoulder can also help. Eyelids Mild lid oedema may be present following a long labour, particularly in a face or brow presentation. Ears Position the top of the pinna should be at or above a horizontal line from the inner and outer canthi of the eye.
Cheap 100mg kamagra chewable with amex
This measures the time to stop bleeding after a standard small wound viagra causes erectile dysfunction purchase kamagra chewable 100 mg with mastercard, as from an Autolet device. Specific factors can be assayed individually, but interpretation may be difficult because of uncertainty as to the normal range in very immature infants. Whereas bleeding may occur from any site, intracranial haemorrhage is the most devastating complication. A transfusion of fetal A1 antigen-positive platelets into the maternal circulation may produce maternal IgG antibodies if the mother is platelet A1 antigen-negative. In-utero treatment consists of fetal platelet transfusion and regular gammaglobulin therapy. Neonatal treatment is valuable, using platelet transfusions, gammaglobulin and steroids. Maternal idiopathic thrombocytopenia Transplacental maternal antibodies cause thrombocytopenia in the neonate, and the mother will usually have thrombocytopenia. The lower the concentration of maternal platelets, the more severely affected the infant may be. It has been suggested that delivery by caesarean section should be undertaken in severely thrombocytopenic fetuses to avoid trauma, but recent evidence suggests that intracerebral bleeds may occur even before the onset of labour. Prednisolone may be given to the severely affected neonate, but the condition is transient, lasting at most 12 weeks. Haemorrhagic disease of the newborn (Vitamin K-deficient bleeding) Classic haemorrhagic disease of the newborn is caused by a deficiency of the vitamin K-dependent clotting factors. About 2 in 1000 babies who do not receive vitamin K will have some bleeding, and 1 in 10 000 will have serious intra-cerebral bleeding. Vitamin K is produced by the bacterial flora of the gastrointestinal tract, but as the newborn infant has a sterile bowel at birth there is little production from this source in the first weeks of life. Clinical features Spontaneous bleeding can occur from any site but is usually gastrointestinal (producing haematemesis or melaena), umbilical, or is associated with circumcision. It occurs late in the first week of life, especially in the breastfed infant owing to the low vitamin K levels in human milk, and nowadays almost only occurs if vitamin K prophylaxis has been missed or declined. Gastrointestinal bleeding in the infant must be differentiated from swallowed maternal blood from antepartum haemorrhage, episiotomy, or cracked nipples. Most centres will now perform Hb electrophoresis to identify if it is predominantly fetal or adult haemoglobin to identify the source of bleeding. Vitamin K prophylaxis Routine administration of intramuscular vitamin K to all newborn babies will prevent bleeding from vitamin K deficiency. However, concerns about the safety of intramuscular vitamin K, in particular the risk of cancer, were raised in the early 1990s, and although there are few data to support this some countries have recommended oral administration of vitamin K in all healthy full-term infants. Failure to give a complete dosage regimen appears to be the reason for the re-emergence of serious late-onset vitamin K deficiency haemorrhage. In rare situations where haemorrhagic tendency still persists after administration of vitamin K, one should exclude the possibility of cystic fibrosis and 1 antitrypsin deficiency. Widespread intravascular coagulation results from the deposition of thrombi in small vessels and the consumption of clotting factors, with consequent haemorrhage. Investigations Blood film showing haemolysis with fragmented and distorted red cells. Treatment this is a complex disorder and haematological consultation will often be necessary. Treatment of the haematological abnormality, including exchange transfusion with fresh whole blood and/or replacement of clotting factors with fresh frozen plasma, platelet concentrates and cryoprecipitate. Coagulation factors are not transferred from the maternal circulation to the fetus. Bleeding in these X-linked recessive diseases occurs when male infants are subjected to surgical procedures such as circumcision, or from either birth trauma or routine sampling of capillary blood. Excessive bleeding typically occurs in the post-traumatic or postoperative settings such as after circumcision. Management A specific diagnosis may be difficult to make at birth because, in the healthy infant, many of the clotting factor assays are low. Homozygous protein C or protein S deficiency causes serious thrombotic events in the postnatal period. The parents, who are usually asymptomatic, are heterozygous for deficiency of the suspected protein. Factor V Leiden, a mutation in coagulation factor V that renders it resistant to cleavage by activated protein C, is now the most common abnormality found in patients with excessive venous thrombosis, such as in cases of neonatal stroke or peripheral ischaemia. Such patients may require anticoagulation such as with low-molecular-weight heparin, especially if they develop life/limbthreatening thrombosis. A left-shift towards higher percentage of immature neutrophils is highly suggestive of infection (see Chapter 10). It often presents with hepatosplenomegaly and cutaneous manifestations (leukaemic skin deposits). Excessive blood loss either in utero (such as feto-maternal or twin-to-twin transfusion) and at birth through accidental bleeding from umbilical cord or trauma to the organs such as liver or skull, is another important cause for anaemia in newborn infant, and should be suspected even though it is not externally obvious. Various haemoglobinopathies that result from a molecular abnormality of haemoglobulin structure result in conditions such as thalassaemias and sickle cell anaemia. On the other hand, a congenital deficiency of certain anticoagulant factors (such as protein-C or -S) may make the blood hypercoagulable, which predisposes to thrombosis and blockage of important blood vessels such as in kidneys or brain (neonatal stroke). Newborn babies are deficient in vitamin K, which is an essential part of the coagulation process. As vitamin K deficiency can lead to lethal haemorrhage, it is now global policy to supplement all babies, particularly those fed on breast milk, with vitamin K. They must be included in the differential diagnosis of any serious or unexplained illness. In other cases, the clinical presentation may not be so acute but if they are undiagnosed and left untreated they can cause serious problems such as growth failure, developmental delay and poor cognitive (intellectual) development. Neonatal screening for conditions, which can have serious consequences and for which treatment is available, is undertaken in most developed countries. The investigation and treatment of endocrine and metabolic diseases can be complex and requires multidisciplinary specialist input. Some are readily and successfully treated, while for others specific treatment is not available. Babies with endocrine and metabolic problems require long-term treatment and follow-up by a specialist team. Glucose and oxygen are the main metabolic substrates of the mature brain, but in the neonate the brain can use alternative metabolic fuels such as lactate and ketones. This is why the brain can function normally, or near normally, despite very low levels of blood glucose. Profound neurological compromise and irreversible damage occur if the brain is deprived of glucose and alternative metabolic substrates. These occur largely in the liver and muscles, but only if liver glycogen is available for rapid breakdown to glucose. The most important substrates are amino acids (particularly alanine), lactate, pyruvate and glycerol. Glycerol is metabolized from adipose tissue and can be directly utilized in gluconeogenesis metabolism. Other products of lipolysis (fatty acids and triglycerides) are metabolized to ketone bodies, which may be used directly in energy production, particularly by the brain. Ketone body production is stimulated by infant feeding, particularly by breast milk.
Order kamagra chewable amex
There is also evidence that sleep deprivation and repetitive hypoxemia augment oxidative stress erectile dysfunction causes & most effective treatment discount 100mg kamagra chewable visa, activate proinflammatory mediators with elevations of C-reactive protein, induce inflammatory cytokines, and promote endothelial dysfunction. Furthermore, high negative intrathoracic pressure is generated during apnea/hypopnea episodes from vigorous inspiratory effort occurring against the collapsed airway. Pathophysiologic effects of sleep apnea and the resultant cardiovascular complications. Other than continuous positive airway pressure, do other therapeutic modalities for obstructive sleep apnea improve blood pressure Have the hemodynamic derangements that occur in obstructive sleep apnea been found to affect myocardial structure or function Since sleep apnea is associated with increased blood pressure, arterial stiffness, and oxidative stress and may be proinflammatory, does it increase the risk of coronary artery disease Since sleep apnea predisposes to ventricular arrhythmias during sleep, does it increase the risk of sudden death Adaptive servoventilation provides servo-controlled inspiratory pressure in addition to positive expiratory pressure. Left ventricular systolic and diastolic function in obstructive sleep apnea: impact of continuous positive airway pressure therapy. Effect of continuous positive airway pressure treatment on pulmonary artery pressure in patients with isolated obstructive sleep apnea: a meta-analysis. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. Because the pathophysiology of claudication is complex, there is not a perfect correlation between anatomic site of disease and location of symptoms. Study demonstrates absent arterial flow in the left posterior tibial and dorsalis pedis arteries. Measurements greater than 55 mm Hg are considered normal and less than 20 mm Hg are associated with nonhealing ulcers. More specifically, blood pressure is measured in both brachial arteries (with the higher systolic blood pressure being used) and is measured using a Doppler instrument with a blood pressure cuff on the lower calf, in both posterior tibial and dorsalis pedis arteries. What are the recommended medical therapies and lifestyle interventions in patients with lower extremity peripheral arterial disease A supervised exercise regimen is recommended as the initial treatment modality for patients with intermittent claudication. Supervised exercise training is recommended instead of unsupervised exercise training. Claudication that severely interferes with quality of life or employment should be treated. Endovascular and open surgical reconstruction have both been extensively used for this purpose. Endovascular options are less invasive, typically performed on an outpatient basis, and associated with lower complication rates. Open surgical options are more durable and best suited for good risk or young patients. Algorithm for the evaluation and management of patients with suspected lower extremity peripheral artery disease. Recommended standards for reports dealing with lower extremity ischemia: revised version. However, endovascular intervention in the infrainguinal segment is associated with inferior patency, particularly when compared with open bypass using venous conduit. Best results are achieved with multidisciplinary approaches that involve interventionalists, surgeons, internists, podiatrists, and infectious disease and endocrine specialists. What are the main complications of open and endovascular infrainguinal interventions Complications of open interventions include cardiac events, respiratory complications, bleeding, wound infection, hernias, and graft failure. Complications associated with endovascular procedures include access site hematoma, bleeding or pseudoaneurysm, vessel rupture, contrast-induced nephropathy or anaphylactic reactions, recurrent stenosis or occlusion, and radiation-related patient injury. Thrombolytic treatment in particular is associated with increased risk of intracavitary, extremity, or intracranial bleeding, which is heavily dependent on the thrombolytic dose and duration of administration. Atherosclerotic-related lesions usually affect the ostium and the proximal 1 cm of the main renal artery. Although it classically occurs in young women, it can affect both genders at any age. Less common causes of renovascular hypertension include renal artery aneurysms, Takayasu arteritis, atheroemboli, thromboemboli, William syndrome, neurofibromatosis, and spontaneous renal artery dissection. What are American College of Cardiology/American Heart Association class I indications for the referral for diagnostic study to identify clinically significant renal artery stenosis What are the main indications for renal artery stenosis percutaneous revascularization Visceral artery aneurysms are an uncommon form of vascular disease whose pathogenesis and natural history remain incompletely characterized. Their typical presentation involves rupture or erosion into an adjacent viscus, resulting in life-threatening hemorrhage. Nearly 22% of reported visceral artery aneurysms present with rupture, resulting in an 8. The distribution of aneurysms among the visceral vessels includes the splenic artery (60%), hepatic artery (20%), superior mesenteric artery (5. Typical indication for open or endovascular treatment includes size greater than 2 cm and childbearing age in a female patient, because rupture is more common during pregnancy and is associated with very high maternal and fetal mortality. In general, when should patients with an infrarenal or juxtarenal abdominal aortic aneurysm undergo repair What are the relative pros and cons of the treatment options for patients with infrarenal abdominal aortic aneurysm that meets size criteria for repair The impact of this follow-up protocol in terms of impact on renal function and radiation-related injury is currently unclear. What are the anatomic eligibility criteria for endovascular infrarenal abdominal aortic aneurysm repair In addition, fenestrated and branched devices and advanced "snorkel" techniques have enabled physicians to successfully treat juxtarenal and thoracoabdominal aneurysms in high-risk patients with endovascular means. What are the primary indications for treatment of extracranial carotid artery occlusive disease The notion that maximizing medical treatment can be as good as intervention with respect to stroke prevention has been gaining acceptance; however, high-quality data to support it are scarce. What are the relative indications for carotid endarterectomy and carotid stenting What are possible causes of lower limb arterial disease and ischemia or claudication in young patients Atherosclerosis tends to primarily affect older persons; however, it can manifest in younger patients who have familial hyperlipidemic syndromes, Buerger disease (thromboangitis obliterans), or hypercoagulable disorders. Popliteal adventitial cystic disease is also in the differential diagnosis of claudication in young patients; it produces a popliteal stenosis that gives a classic "scimitar sign" on angiography. Exercise-induced compartment syndrome may produce similar symptoms of leg pain with exercise that is relieved by rest. Histologic classification discriminates three main subtypes-intimal, medial, and perimedial-which may be found in a single patient.
Arsenic Trioxide (Arsenic). Kamagra Chewable.
- Food poisoning, insomnia, allergies, anxiety, depression, and obsessive-compulsive disorder (OCD), psoriasis, syphilis, asthma, rheumatism, hemorrhoids, cough, itchy skin, and cancer.
- Treating a certain type of leukemia. A specific prescription-only intravenous medication is used for this purpose.
- What is Arsenic?
- Dosing considerations for Arsenic.
- Are there safety concerns?
- How does Arsenic work?
- Are there any interactions with medications?
- What other names is Arsenic known by?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97169
Discount kamagra chewable 100mg
Skeletal deformities involving the rib cage or alteration in head shape may occur and erectile dysfunction doctors in pa discount kamagra chewable 100mg mastercard, in its most severe form, fractures and frank rickets may be present, but these latter abnormalities are now uncommonly seen radiographically. A baby on full milk feeds of an adapted low-birthweight formula will receive this intake. Premature babies exclusively fed with breast milk will become phosphate-deficient, and in these cases supplementation with phosphorus is necessary. Additional phosphate supplementation is recommended for the first 6 months of life if the baby remains on breast milk alone. The treatment of established metabolic bone disease is to increase phosphate intake so that serum phosphate levels are normal and phosphorus is excreted in the urine. Hypercalcaemia Hypercalcaemia is defined as a serum calcium concentration greater than 2. This is often iatrogenic due to the excessive use of calcium gluconate in intravenous fluid therapy. Disorders of magnesium metabolism Hypomagnesaemia Hypomagnesaemia is defined as a serum magnesium concentration less than 0. Sometimes, hypocalcaemia will not respond to calcium gluconate infusion, but serum calcium levels rapidly increases following magnesium sulphate injections. Hypermagnesaemia Hypermagnesaemia is defined as a serum magnesium level greater than 1. It may occur as the result of magnesium sulphate administration to the mother for severe maternal pre-eclampsia or to the baby for pulmonary hypertension. Preterm infants have greater requirements because of the immaturity of renal tubular reabsorption. Care must be taken in the interpretation of serum sodium, as red cell haemolysis in blood samples obtained by squeezing may lower the apparent serum level. Maternal hyponatraemia following excessive administration of 5% dextrose or oxytocin in labour. In the assessment of infants with hyponatraemia, serum potassium, creatinine and osmolality should be measured as well as urinary sodium and osmolality (or specific gravity). If a preterm baby has poor growth despite adequate calories, check the serum sodium. If it is due to haemodilution (inappropriate antidiuretic hormone secretion or excessive intravenous water) then fluid restriction is the first line of treatment. If it is due to sodium loss, then careful replacement with hypertonic saline according to the equation: where 0. Newborn infants, particularly those born preterm, rapidly become dehydrated and hypernatraemic if fluid intake is reduced or abnormal losses occur where water loss exceeds sodium loss. The newborn kidney is less efficient at excreting excess salt than water, and so hypernatraemia is more likely in very immature infants than in older children. The lack of keratin in the skin of very tiny babies causes excessive transepidermal water loss. With hypernatraemia the serum osmolality is high and this may be associated with intracerebral haemorrhage. Too rapid a reduction in hypernatraemia may be deleterious, resulting in cerebral fluid shifts and convulsions. Potassium metabolism Hyperkalaemia this is defined as a serum potassium concentration greater than 6. Spurious hyperkalaemia occurring with haemolysis during blood sampling which should not be confused with true hyperkalaemia. Pathological causes include renal failure, acidosis, shock, hypoxia and blood transfusion. It is particularly likely to occur spontaneously in very ill, premature infants within 72 hours of birth. Treatment First-line treatment should consist of stopping all potassium-containing fluids. One needs to be careful with use of calcium resonium in pre-terms with poor gut function. Treatment If the hypokalaemia is due to dietary potassium deficiency, the potassium can be replaced orally by adding it to the milk. Intravenous potassium replacement must only be given in the presence of known and adequate renal function, according to the formula: this is given by slow intravenous infusion up to a maximum of 0. Endocrine gland disorders Disorders of thyroid function Hypothyroidism Untreated hypothyroidism is associated with severe intellectual impairment and as such is an important cause of subsequent disability. Because early recognition and effective treatment offer an excellent outcome in the majority of cases, the early detection of congenital hypothyroidism is essential. Screening is performed on heel-prick blood obtained at the same time as the Guthrie test. Clinical features Most infants detected by a screening programme will be clinically normal. The classic signs of severe or untreated hypothyroidism include poor feeding, constipation, abdominal distension, umbilical hernia, mottled skin, coarse puffy facies with a large protruding tongue, hypotonia, hypothermia, failure to thrive, persistent jaundice and both growth and developmental delay. Transient hypothyroidism this refers to babies who have a positive screening test but whose thyroid function subsequently normalizes without treatment. Prenatally acquired causes include maternal thyroid deficiency, antithyroid drugs and thyroid antibodies acquired transplacentally. In the neonatal period the most common transient abnormality is due to topically applied iodinecontaining antiseptics. Enzyme assays may be required in the investigation of inborn errors of thyroid metabolism. Monitoring of the dose will be by growth assessment, physical appearance and thyroid function tests. Prognosis the outcome for congenital hypothyroidism depends on the severity of intrauterine hypothyroidism and the delay in establishing effective treatment after birth. Clinical features the infant is usually growth-restricted and often has a small goitre at birth and develops irritability and diarrhoea, with failure to gain weight despite feeding well. The most important feature is tachycardia, which may not be present at birth but develops rapidly within 48 hours. Management All infants born to thyrotoxic women should be carefully monitored for tachycardia for the first 48 hours of life. Abnormalities of the adrenal gland Neonatal adrenal disorders fall into the categories of hyperplasia and hypoplasia. Clinical presentation Deficiency of 21-hydroxylase presents in one of two ways: Virilization.
Syndromes
- Spina bifida
- Family history
- Use proper lifting techniques.
- Liver necrosis (death of live tissue)
- School-age child development
- Low blood pressure -- develops rapidly
- Have any allergies to medications or numbing medicine
- Stool tests for bleeding
- Nervous system problems caused by a lack of vitamin B12
- The headache occurs with repeated vomiting
Cheap generic kamagra chewable canada
It is associated with persistent and long-lasting improvement in symptoms erectile dysfunction drugs and hearing loss best buy kamagra chewable, exercise capacity and possibly survival. The procedure is performed by injecting 1 to 3 mL of 96% to 98% ethanol into a septal perforator branch of the left anterior descending coronary artery to create a limited myocardial infarction in the proximal septum. The procedure-related mortality rate is 1% to 2%, which is similar to that of surgery. An individual approach is recommended with these two options, taking into account the individual anatomy and the surgical risk. It has also been noted that those with a septal wall thickness greater than 30 mm are less likely to receive benefit. What are the indications for an implantable cardioverter defibrillator in hypertrophic cardiomyopathy Many patients remain asymptomatic or mildly symptomatic for many years and achieve normal life expectancy. Others develop progressive symptoms of heart failure with exertional dyspnea and functional limitation despite medical therapy. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Proposal for contemporary screening strategies in families with hypertrophic cardiomyopathy. Long-term effects of surgical septal myectomy on survival in patients with obstructive hypertrophic cardiomyopathy. Hypertrophic cardiomyopathy: distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Multicenter study of the efficacy and safety of disopyramide in obstructive hypertrophic cardiomyopathy. The basic pathophysiology in restrictive cardiomyopathy is increased stiffness of the ventricular walls as a result of myocardial disease, leading to impaired diastolic filling of the ventricles. Ejection fraction is usually preserved in most cases at least in the early stages but can become severely impaired in end-stage disease, particularly in cardiac amyloidosis. The condition can affect either or both of the ventricles, and they may not be uniformly affected. Approximately half the cases of restrictive cardiomyopathy have an identifiable cause. Hydroxychloroquine, which is commonly used to treated connective tissue diseases, can cause cardiotoxicity (typically after prolonged use), which results in a restrictive cardiomyopathy. Myocardial damage from radiation and anthracycline toxicity can lead to restrictive cardiomyopathy, as can endomyocardial involvement from endomyocardial fibrosis. Although restrictive cardiomyopathy is a rather uncommon cause of heart failure in North America and Europe, it is a relatively common cause of heart failure and death worldwide due to a much higher incidence of endomyocardial fibrosis in tropical regions, including parts of Africa, Central and South America, India, and other parts of Asia. Secondary restrictive physiology develops in the advanced stages of all forms of heart disease, including dilated, hypertensive, and ischemic cardiomyopathy. Most restrictive cardiomyopathies preferentially affect the subendocardium of the heart. Therefore, on tissue Doppler imaging and speckle-tracking echocardiography, tissue velocities and longitudinal strain, respectively, are severely reduced, reflecting severe longitudinal systolic and diastolic dysfunction of the heart. If an infiltrative process is present, the myocardium may appear brighter than normal, with a sparkling or grainy appearance on echocardiography. As with other organs, in amyloidosis there may be protein deposition in myocardial tissue. Apical four-chamber view echocardiogram of a patient with restrictive cardiomyopathy demonstrating dilated atria and normal-sized ventricles. Mitral inflow pattern in a patient with restrictive cardiomyopathy showing augmented early filling E wave (E) with shortened deceleration time and attenuated A waves (A). The classic finding of thickened ventricular walls yet inappropriately normal or even low voltage on the electrocardiogram is common. The diagnosis is usually confirmed, if necessary, by endomyocardial biopsy or with biopsy of another involved organ and the above cardiac findings. Sarcoidosis can lead to non-caseating granulomas infiltrating the myocardium leading to fibrosis and scar formation. Infiltration may be patchy throughout the myocardium, and as a result biopsy yield is often lower than in other infiltrative processes. The hyper-enhancement does not conform to the distribution of a coronary artery territory. Echocardiogram demonstrating the sparkling pattern that can be seen in patients with cardiac amyloidosis. Tissue Doppler imaging demonstrates severely reduced systolic (s), early diastolic (e), and late diastolic (a) longitudinal tissue velocities in cardiac amyloidosis. Myocardial infiltration in the setting of sarcoidosis can lead to heart block and syncope (as a result of infiltration of the conduction system), ventricular arrhythmias (including syncope and sudden death), as well as heart failure. Pulmonary involvement may lead to pulmonary hypertension and its associated effects on right-sided heart function. Endomyocardial biopsy is considered reasonable in the setting of heart failure associated with unexplained restrictive cardiomyopathy. Endomyocardial biopsy may reveal specific disorders, such as amyloidosis or hemochromatosis, or myocardial fibrosis and myocyte hypertrophy consistent with idiopathic restrictive cardiomyopathy. Is cardiac computed tomography or cardiac magnetic resonance imaging useful in cases of possible restrictive cardiomyopathy Both imaging modalities can demonstrate a thickened pericardium, which may suggest constrictive pericarditis rather than restrictive cardiomyopathy. The long arrows point to ventricular thrombus; the arrowheads demonstrate areas of endomyocardial fibrosis. Endomyocardial fibrosis and intracardiac thrombus occurring in idiopathic hypereosinophilic syndrome. Increased filling pressures cause pulmonary and systemic congestion and symptomatic dyspnea. Upon physical examination, the pulse may reflect low stroke volume with low amplitude and tachycardia. Jugular venous pulse is often elevated, with prominent y descent consistent with rapid early ventricular filling. Upon heart examination, S3 gallop may be heard due to abrupt cessation of rapid ventricular filling. Importantly, S4 is rarely heard with cardiac amyloidosis, despite thickened ventricular walls, due to involvement of the left atrium with reduced left atrial contractility even in the absence of atrial fibrillation. Certain drugs such as serotonin, methysergide, ergotamine, busulfan, and mercurial agents cause fibrous endocarditis, which leads to restrictive cardiomyopathy. In addition, both hydroxychloroquine and chloroquine can cause a restrictive cardiomyopathy characterized by intense vacuolization of cardiomyocytes. It may be difficult to distinguish restrictive cardiomyopathy from constrictive pericarditis in the catheterization laboratory. Most important, ventricular interdependence with inspiration is not observed with restrictive cardiomyopathy. Hemodynamics obtained from right heart catheterization in a patient with restrictive cardiomyopathy. When possible, treatment of the underlying cause of restrictive cardiomyopathy is essential. Symptomatic treatment includes loop diuretics to treat systemic and pulmonary venous congestion. Digoxin increases intracellular calcium, thus worsening diastolic function, and may increase the risks of arrhythmias and should be used with caution. There is also evidence that digoxin may bind certain types of amyloid proteins and should therefore be avoided in cardiac amyloidosis. Many patients with restrictive cardiomyopathies will have debilitating hypotension, which can be orthostatic in nature and can also be associated with significant right heart failure.

Discount kamagra chewable 100mg online
The prevention of symptomatic hypoglycaemia is one of the most important factors in preventing brain damage in the whole of neonatal medicine erectile dysfunction protocol scam cheap kamagra chewable. It is widely believed that infants with asymptomatic hypoglycaemia are not at risk of adverse neurodevelopmental outcome. However, some studies do suggest that neural dysfunction can occur with blood sugar levels below 2. Specific causes of hypoglycaemia Infants born to diabetic mothers Maternal diabetes is classified as follows: Pregestational: Type 1: the basic cause is beta-cell destruction. The prognosis for the diabetic pregnancy depends on the severity of the diabetes and the quality of diabetic control during pregnancy. The two main factors determining whether maternal diabetes will have an effect on the fetus and baby are the vascular complications that the diabetes causes in the mother, and the blood glucose control during pregnancy. Mothers with vascular complications as a result of diabetes are much more likely to develop hypertension in pregnancy, which may affect fetal growth and well-being. The outcome of pregnancy in diabetic women also depends on glucose control, both before conception and during gestation. Diabetic women should have their diabetes very carefully managed before conception, and combined care through pregnancy by a physician and obstetrician is essential. On this regimen the complications for the fetus are reduced and may be avoided completely. Insulin is a major trophic hormone influencing fetal growth, and hyperinsulinaemic fetuses become macrosomic. They have excessive fat stores and inhibition of lipolysis and -oxidation resulting from hyperinsulinaemia. Birth trauma from cephalopelvic disproportion, difficult instrumental delivery and shoulder dystocia; injuries include intracranial haemorrhage, fractured bones and nerve palsies. Birth asphyxia, which may occur in a poorly controlled diabetic pregnancy and may be related to cephalopelvic disproportion. Chronically elevated maternal glucose levels cause hyperplasia of the islet beta cells in the fetal pancreas with fetal hyperinsulinism. Once the baby is born, the high circulating insulin causes neonatal hypoglycaemia lasting for several days. Insulin has an antagonistic effect on surfactant development, and hyperinsulinaemic babies are at much greater risk of developing respiratory distress due to surfactant deficiency, retained lung fluid or polycythaemia, even at full term. Management Careful control of diabetes during pregnancy decreases many of the complications. Management of the pregnancy involves obsessional diabetic control, planned delivery in a suitably equipped hospital, examination for congenital abnormalities and screening for anticipated complications, especially hypoglycaemia. Published studies give perinatal mortality rates of about 30 per 1000 for diabetic pregnancies, but this has improved considerably with counselling during the periconception period and a better antenatal surveillance of diabetic mothers. Congenital hyperinsulinism this is due to a group of disorders in the regulatory function of pancreatic beta cells resulting in unregulated secretion of insulin and severe neonatal hypoglycaemia. The term nesidioblastosis was previously used to describe congenital hyperinsulinism, but the histological features of it are seen in the normal pancreas and the term is no longer used. Severe resultant hypoglycaemia can be temporarily reversed by glucagon and/or octreotide, an analogue of somatostatin. Occasionally, the hyperinsulinism is due to a localized insulinoma, and full excision of this is curative. More commonly the pancreas is diffusely abnormal, requiring near-total pancreatectomy with removal of up to 95% of the pancreas. Iatrogenic hypoglycaemia this occurs most commonly in infants at risk of hypoglycaemia in whom low blood sugar is detected and aggressive treatment started. Treatment with rapid intravenous injection of concentrated (25% or 50%) dextrose will cause a rapid increase in blood glucose, and in the presence of hyperinsulinism there may be a rebound hypoglycaemia. When the blood glucose is next measured, hypoglycaemia is found as a result of this rebound effect, and another rapid infusion of concentrated dextrose is given with similar effect. Rapid or concentrated injections of dextrose are rarely necessary and should be avoided if possible. When absolutely necessary, they should be followed by a continuous infusion to avoid rebound hypoglycaemia. When insulin is used to treat hyperglycaemia or hyperkalaemia, hypoglycaemia may be induced. Regular blood glucose measurements must be performed on all infants receiving insulin. Hyperglycaemia frequently occurs in the preterm infant who is receiving 10% dextrose intravenously, or in any infant receiving parenteral nutrition. Usually, hyperglycaemia responds to a reduction in the glucose concentration or to alterations in the glucose infusion rate. A full infection screen should always be performed on neonates with high glucose levels or glycosuria. Transient neonatal diabetes mellitus this is very rare and occurs in severely growth-retarded infants. Non-ketotic hyperglycaemia develops as a result of inadequate insulin production by the pancreatic beta cells. Treatment is by correction of electrolyte disturbances and the administration of insulin intravenously. Later, oral hypoglycaemic agents such as sulfonylurea can be substituted for insulin until normal pancreatic function develops. Disorders of calcium, phosphate and magnesium metabolism the metabolism of these three electrolytes is interrelated and not completely understood. Low levels of magnesium inhibit parathyroid hormone secretion, and hypomagnesaemia is commonly found together with hypocalcaemia. Oral cholecalciferol is converted in the liver to 25hydroxyvitamin D and then further metabolized in the kidney to 1,25-dihydroxyvitamin D, which increases the intestinal absorption of calcium and phosphate. Low maternal vitamin D levels cause the fetus to be born with relatively low levels. This hormone is produced in the thyroid and is secreted in response to a high ionized calcium level. Hypocalcaemia Hypocalcaemia is usually defined as a serum calcium concentration less than 1. It is the ionized fraction that determines whether symptoms occur, but few laboratories routinely measure ionized calcium. Furthermore, acidosis causes more calcium to be ionized and alkalosis decreases ionized calcium. For these reasons, infants may exhibit few or no symptoms of hypocalcaemia despite low serum calcium levels, provided that ionized calcium is normal. Early hypocalcaemia this occurs within the first 72 hours of life, although the reasons for this are not fully understood. This is a rare condition and may be inherited in either an X-linked or an autosomal recessive manner.
Cheap 100mg kamagra chewable
This may be important in pathological situations erectile dysfunction drugs free sample generic kamagra chewable 100mg mastercard, and reinforcement of the enterohepatic circulation will increase unconjugated bilirubin levels in prematurity, small bowel obstruction, functional bowel obstruction and pyloric stenosis. As jaundice is common it is essential to have a clinical method for determining its severity. Proper lighting (ideally daylight) is important for detecting subtle levels of jaundice. It is no longer used as it has been proven to be unreliable, particularly in non-Caucasian babies. It can provide a useful screening test in babies 35 weeks or more and more than 24 hours of age. TcB has good correlation with total serum bilirubin, but may have limitations in specific situations. Pale stools might suggest that the normal passage of bile from the liver into the duodenum is blocked. Management the first investigation in any jaundiced newborn is to take a careful history. Current postnatal age of the infant and when baby first became clinically jaundiced. Neurological signs: hypertonia, opisthotonus, fits, abnormal eye movements, abnormal cry. Abdominal distension: associated with bowel obstruction, bowel stasis or hypothyroidism. In assessing the significance of jaundice in a newborn infant the following guidelines may be useful. Investigations should be carried out under the following circumstances: Any infant who is visibly jaundiced in the first 24 hours of life. Any infant who has the clinical signs of obstructive jaundice (dark urine, pale stools). Bilirubin in the urine indicates that the conjugated fraction of bilirubin should be estimated in the laboratory and causes of conjugated hyperbilirubinaemia considered. Unconjugated hyperbilirubinaemia Causes the causes (and timing of onset) of unconjugated hyperbilirubinaemia are shown in Table 19. In any baby presenting with jaundice in the first 24 hours of life it is important to exclude a haemolytic cause for the unconjugated hyperbilirubinaemia. Breastfeeding infants are more likely to develop jaundice secondary to a lower caloric intake and increased enterohepatic circulation of bilirubin. The causes of prolonged (lasting >10 days) or late-onset unconjugated hyperbilirubinaemia are shown in Box 19. These conditions can lead to rapid rises in the bilirubin level, and often need early and aggressive treatment to prevent complications. Physiological jaundice Physiological jaundice is a term used by clinicians to describe jaundice for which no underlying cause is identified, and is therefore a diagnosis of exclusion. The major cause is increased bilirubin production (due to increased haemoglobin levels at birth and a shortened red cell lifespan). Decreased bilirubin excretion (due to low concentrations of the hepatocyte binding protein, low activity of glucuronosyl transferase, and increased enterohepatic circulation) also contributes to the development of physiological jaundice. Infection Bacterial infections, particularly septicaemia and urinary tract infections, may cause unconjugated hyperbilirubinaemia. Occasionally, severe bacterial infection may cause hepatocellular damage with a conjugated form of jaundice. Breastfeeding and jaundice Breastfeeding-associated jaundice is the term used to refer to the increased bilirubin levels seen during the first week of life in almost two-thirds of infants who are breastfed. It is probably due to calorie and fluid deprivation in the first few days of life and delayed passage of stools, as it can be reduced by an increased frequency of breastfeeding during the first few days of life. Breast milk jaundice is prolonged jaundice that extends until the first 3 months of life. Characteristically, it is a form of non-haemolytic, unconjugated hyperbilirubinaemia and should be diagnosed primarily by the exclusion of other aetiologies in a thriving infant, and by its time course. An excess of this enzyme causes increased enteric absorption of bilirubin, thus increasing the hepatic bilirubin load. In this respect, breast milk jaundice can be thought of as an extension of physiological jaundice, and the greater the consumption of this enzyme in milk the higher is the concentration of neonatal serum bilirubin. Breast milk jaundice does not require any treatment and is not an indication to abandon breastfeeding; however, babies with high bilirubin levels should be kept under review. Delayed passage of meconium this increases the risk of jaundice due to increased enterohepatic absorption of bilirubin. Liver transplantation has been successful in some severe cases; in milder cases phenobarbitone may lower the serum bilirubin. The aim is to identify the infant at risk of acute bilirubin encephalopathy and thereby prevent it occurring by commencing appropriate treatment. Prolonged unconjugated hyperbilirubinaemia requires additional investigation when present for more than 14 days. Investigations for prolonged unconjugated hyperbilirubinaemia are listed in Box 19. Management Prevention Early feeding reduces the incidence of jaundice by preventing dehydration and the elevation of free fatty acids. The maintenance of an adequate fluid intake is an essential part of the care of a jaundiced baby. In addition, feeding will overcome bowel stasis and minimize the effects of the enterohepatic bilirubin circulation. Breastfeeding-associated jaundice is minimized by frequent, early breastfeeding in the first 3 days of life. The conversion process is rapid, but the excretion of the molecule out of the skin is slow. Phototherapy is the standard of treatment and has resulted in a decline in the number of exchange transfusions being performed. Even relatively short durations of exposure to sunlight can cause burning and increases the long-term risk of developing skin cancer. Phototherapy can be delivered from either overhead or underneath the baby (or both). Devices essentially differ in their colour spectrum, energy output and total dose of light delivered. Given equivalent light sources, other factors that might influence the effectiveness of phototherapy include the number of lights, the distance from the light source to the infant, the time spent in phototherapy, and the surface area of skin exposed. Various thresholds for commencing phototherapy and for monitoring at-risk infants have been developed by different organizations. Once therapy has been commenced, serum bilirubin estimates will be necessary to assess the severity of jaundice because the skin colour becomes unreliable. Diarrhoea: phototherapy decreases bowel transit time and induces lactose intolerance; both are important causes of diarrhoea and consequent fluid loss. Retinal damage: the eyes are thought to be vulnerable to phototherapy but this has never been proved. Early discharge and home management of jaundice the introduction of early discharge programmes for healthy term infants has resulted in the need for jaundice to be diagnosed and or treated at home. The resurgence of kernicterus is probably also related to the combination of early discharge and breastfeeding. This may result in dehydration if the baby feeds poorly and there is a lack of recognition of severe hyperbilirubinaemia. Predicting which infants might require treatment using direct and indirect techniques of measuring serum bilirubin at age 24 hours has been suggested, but more research is required to identify sensitive methods. Home treatment has been facilitated by the introduction since 1990 of the BiliBlanket (MedNow Inc.