Effective 18gm nasonex nasal spray
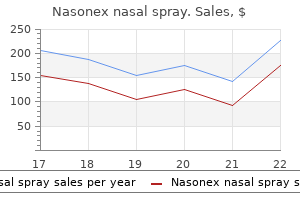
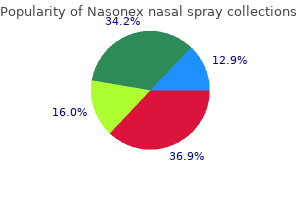
Once a patient is determined to be intolerant of or unable to achieve adequate benefits with standard medical treatments allergy medicine brand names safe 18 gm nasonex nasal spray, surgical options may be considered. Physical examination, upper airway endoscopy, and imaging techniques are available to describe the upper airway anatomy and tailor a comprehensive and multilevel surgical treatment plan appropriately. Sleep-related symptoms and impact on quality of life, including snoring, witnessed apnea, gasping, choking, nocturnal awakenings, nocturia, morning headaches, daytime sleepiness, and cognitive dysfunction b. Sleep efficiency: Poor sleep efficiency may raise concern for unreliable sleep study results or the possibility of comorbid insomnia. Chronic back or neck pain, fibromyalgia, or other pain syndromes that may negatively impact sleep. Opiate pain medication, benzodiazepines, or other medications that can alter nocturnal control of breathing. The pulse generator placement may be adjusted, however, to avoid contact with the stock of a rifle or shotgun. Alcohol: Evening alcohol use has been correlated with increased obstructive respiratory events. Acquired nasal deformity, septal deviation, turbinate hypertrophy, rhinitis, nasal polyps, and other nasal valve pathology may increase upper airway resistance and directly contribute to sleep-disordered breathing. Nasal surgery designed to lower nasal resistance should be considered either in conjunction with or prior to pharyngeal surgery in most cases. Tongue ridging or scalloping suggests relative macroglossia in relation to the size of the mandible. Quality and quantity of dentition has implications on the availability of adjunctive custom mandibular repositioning devices (oral appliance) in the treatment plan. The presence of large palatal tori may reduce operative exposure and make palatal surgery more technically challenging. Position of the hyoid bone: A low or inferiorly positioned hyoid bone suggests a longer pharyngeal airway. To evaluate for chest wall deformity, scars, or other signs of prior surgery or trauma Cranial nerves a. Examination with specific attention to the functional status of the hypoglossal nerves and the facial nerve General health a. Particular attention is paid to the pattern of palatal collapse and the degree of multilevel coupling between the protrusion of the tongue and enlargement of the retropalatal space. Imaging of the facial skeleton may be indicated in select cases preoperatively, particularly in cases of prior man- Relative Contraindications 1. Although other systems may be available in the future, the operative portion of this chapter will focus on the procedure and technology components of the currently available system (Inspire Medical Systems, Minneapolis, Minnesota). The hypoglossal nerve stimulation system consists of three implanted components: (1) an implantable pulse generator in a subcutaneous pocket in the upper chest (asterisk), (2) a stimulation lead with a cuff electrode placed on the medial branch of the hypoglossal nerve in the submandibular space (black arrow), and (3) a sensing lead to detect ventilatory effort placed in the intercostal space facing the pleura (white arrow). The right side is most commonly used for implantation, unless there is a contraindication requiring use of the left side. If accessible, the C1 branch coursing along the inferior aspect of the hypoglossal nerve and innervating the geniohyoid muscle may also be included in the cuff. Placing the pulse generator more laterally near the deltopectoral groove may cause it to interfere with shoulder movement. The incision in the neck for the cuff electrode (red line) is placed in the submandibular triangle. It is placed more anteriorly and superiorly than a standard submandibular gland incision to ease access of the distal branches of the hypoglossal nerve. The chest incision for the pulse generator is placed on the ipsilateral side as the planned neck incision, approximately 4 cm below the clavicle and medial to the deltopectoral groove to avoid restriction of arm movement. Electrical stimulation of the appropriate distal protrusor branches and an adequate respiratory sensing lead waveform are confirmed, followed by visual confirmation of adequate tongue protrusion. The three wounds are then irrigated and closed in a multilayer fashion with absorbable suture. Finally, combination therapy with more than one medical and/or surgical treatment may be required in some patients, particularly those with more severe disease. A common pitfall involves inclusion of a distal lateral retractor branch in the cuff. Intraoperative nerve monitoring and/or observation of tongue movement should identify suboptimal placement of the cuff. Staying anterior to the external jugular vein may avoid troublesome intraoperative bleeding. Subjective adherence rates were high while serious device- and procedure-related adverse events were very low, including no cases of permanent nerve injury. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. Electrical stimulation of nerve branches to which of the following muscles will result in retraction of the tongue To determine the surgical intervention most suitable, the airway is fully evaluated for level, pattern, and degree of airway collapse. It can be performed as an isolated procedure or in combination with those addressing velopharyngeal, oropharyngeal, or nasal obstruction. This is the key mechanism that advances the base of the tongue when the hyoid is suspended to the mandible. Adequate suspension should be obtained without overtightening to avoid suture breakage or complications. Surgical history 1) Tonsillectomy, adenoidectomy, septoplasty, turbinate reduction, rhinoplasty, bariatric surgery c. Epworth sleepiness scale A subjective patient self-assessment tool to determine sleepiness level with various activities. Comparison of preoperative and postoperative scores may assist in the evaluation of subjective outcome measures. Nose Evaluate for deviated septum, inferior turbinate hypertrophy, and nasal valve collapse. Oral cavity and oropharynx Note size and presence or absence of tonsils, ability to visualize the uvula, soft palate, and hard palate for determination of Friedman tongue position. Note whether there is a large amount of subcutaneous adipose tissue or musculature, especially over the hyoid, because this may limit surgical success. Flexible supine nasopharyngoscopy Flexible supine endoscopy is the most important preoperative portion of the examination. This can be done awake in the office and/or under sedation in the operating suite. We prefer drug-induced sedation endoscopy in the operating suite because it best mimics the sleep state. During endoscopy, the level (velopharyngeal, oropharyngeal, or hypopharyngeal), degree, and pattern of upper airway collapse is noted to determine the most suitable surgical intervention. Sleep architecture: Assess hours of sleep per night, number of nighttime awakenings, and use of sleep medications. Sleep-related symptoms: Evaluate for the presence of snoring, witnessed apneas, restless sleep, sleep maintenance or onset insomnia, perspiration during sleep, nocturnal enuresis, nighttime seizures, narcolepsy, and restless leg symptoms. Daytime-related symptoms: Evaluate for the presence of excessive daytime sleepiness, morning headaches, and awakening feeling tired. Hyoid to mandible suspension showing favorable expansion of the hypopharyngeal space. One advantage is to allow for better postoperative evaluation of hypopharyngeal airway collapse with drug-induced supine sleep endoscopy.
Nasonex nasal spray 18gm cheap
Thyroid gland: Most parathyroid glands lie directly posterior to or around the capsule of the thyroid gland; identification and mobilization of the gland are required in fourgland explorations allergy choices buy nasonex nasal spray 18gm with mastercard. Inferior thyroid artery: Parathyroid glands are often located near the junction of the inferior thyroid artery and the recurrent laryngeal nerve. General anesthesia is preferred owing to the need for bilateral exploration, tracheal manipulation, and potentially longer surgical times. Knowledge of thyroid and parathyroid embryology Perioperative Antibiotic Prophylaxis 1. Temporary hoarseness occurs in less than 5% of cases and typically resolves within a few weeks. However, hoarseness may take up to 6 months to fully recover when the parathyroid gland is juxtaposed or posterior to the nerve. Hematomas may occur, usually within the first 4 hours of surgery, although bleeding can happen up to a week later, especially in patients with a bleeding disorder or those who are taking anticoagulants. This occurs in less than 1% of cases and usually requires surgical evacuation to prevent serious compressive sequelae. Infections are extremely rare and should raise the concern of incidental injury to the trachea or esophagus. Generally opening the wound and placing a Penrose drain should suffice as initial management. The skin is marked for thyroid surgery, followed by infiltration of the skin with local anesthesia (epinephrine). A 3- to 4-cm Kocher incision is placed into a line of relaxed skin tension approximately 2 fingerbreadths above the suprasternal notch. Dissection continues through the platysma muscle and the subplatysmal flaps are elevated. The location of the superior parathyroid gland is sought on the posterior and lateral aspects of the thyroid gland. The superior gland should be located near the superior pole of the thyroid, often deep to the plane of the recurrent laryngeal nerve and superior to the intersection of the recurrent laryngeal nerve and the inferior thyroid artery. Blunt dissection of the fibroareolar tissue to expose the thyroid gland using a Kittner or peanut dissector with a Freer elevator is recommended. It is preferable to identify the recurrent laryngeal nerve before any gland is removed. If additional exposure is needed, the superior thyroid artery can be ligated as it enters the superior aspect of the thyroid; the thyroid gland can then be further rotated anteromedially. The inferior parathyroid is usually medial and anterior to the recurrent laryngeal nerve, often overlying the trachea or tracheoesophageal groove in the region of the intersection of the recurrent laryngeal nerve and the inferior thyroid artery. Dissection along the nerve down the tracheoesophageal groove and along the esophagus toward the mediastinum may be required to find the abnormal gland. The search for the inferior gland should include the thyrothymic adipose tissue and the superior aspect of the thymus. After visualizing all four glands, the surgeon will choose one of the following approaches: a. A frozen-section biopsy specimen is obtained to confirm that it is parathyroid tissue before reimplantation is performed with the residual gland (usually a remnant of 50 mg). Cervical thymectomy may be required, especially because ectopic or supernumerary glands can be found in up to 37% of the cases. The tissue overlying the trachea just inferior to the thyroid down to the innominate artery/aortic arch inferiorly, the trachea posteriorly, and the bilateral carotid artery medially should be removed. The appropriate surgical approach will vary from patient to patient and will fall into one of these acceptable surgical treatments. If blood is present it will stain the lymph nodes and adipose tissue located in the paratracheal space, making it more difficult to identify the parathyroid tissue. Bleeding also increases the risk of inadvertent injury to the recurrent nerve or esophagus. Approximately 50 to 70 mg should be preserved in order to avoid damage to the blood supply. Devascularized glands rapidly become dusky and should be removed and reimplanted after frozen section confirms the presence of parathyroid tissue. Autotransplantation to a forearm location may be technically challenging in patients with one or more pre-existing arteriovenous fistulas or grafts in the upper extremities. Incisions should be carefully placed into lines of relaxed skin tension for camouflage. The strap muscle and platysma should be approximated to prevent adhesion of the trachea to the underlying skin. Patients should quickly be transitioned to a nonnarcotic pain medication such as naproxen sodium or acetaminophen. C, Between one half and one quarter of the right superior gland was kept in place and marked with a surgical clip. Remnant of gland minced into pieces smaller than 1 mm3 using scalpel or scissors and ready for transplantation into striated muscle. Recurrent laryngeal nerve injuries are extremely rare, occurring in less than 1% of cases, and most of these injuries are transient neuropraxias. Arteriographic embolization and percutaneous ethanol ablation resulting in transitory hypoparathyroidism has been described in the past; however, this is not commonly recommended. Administration of cinacalcet (Sensipar) can be used in refractory cases or medically fragile patients who cannot undergo surgery. This type of monitoring predicts the cure and is very helpful in persistent or recurrent disease. The benefits extend beyond the economic savings resulting from limited exploration and reduced operating times. Surgery should be tailored according to transplantation status and requires more experience than that called for by typical parathyroid surgery. Parathyroidectomy vs calcimimetics for treatment of persistent hyperparathyroidism after kidney transplantation. Persistent hyperparathyroidism in renal allograft recipients: vitamin D receptor, calcium-sensing receptor, and apoptosis. An economic comparison of surgical and medical therapy in patients with secondary hyperparathyroidism-the German perspective. The National Kidney Foundation recommends the following postoperative treatment of hypocalcemia: the blood level of ionized calcium should be measured every 12 hours for the first 48 to 72 hours after surgery and then twice daily until the patient is stable. The calcium infusion should be gradually reduced when the level of ionized calcium attains the normal range and remains stable. When oral intake is possible, the patient should receive calcium carbonate 1 to 2 g 3 times a day as well as calcitriol of up to 2 g/day, and these therapies should be adjusted as necessary to maintain the level of ionized calcium in the normal range. Parathyroid function as a determinant of the response to calcitriol treatment in the hemodialysis patient. Which is the predominant parathyroid pathology seen in patients with secondary hyperparathyroidism Embryonic parathyroid rests occur commonly and have implications in the management of secondary hyperparathyroidism. Allelic loss on chromosome 11 is uncommon in parathyroid glands of patients with hypercalcaemic secondary hyperparathyroidism. Role of parathyroid intervention in the management of secondary hyperparathyroidism. Secondary and tertiary hyperparathyroidism: causes of recurrent disease after 446 parathyroidectomies. Parathyroidectomy promotes wound healing and prolongs survival in patients with calciphylaxis from secondary hyperparathyroidism. Postoperative hungry bone syndrome in patients with secondary hyperparathyroidism of renal origin. The uremic gangrene syndrome: improved healing in spontaneously forming wounds following subtotal parathyroidectomy.
Diseases
- Choledochal cyst, hand malformation
- Hereditary spherocytosis
- Heart block progressive, familial
- Cicatricial pemphigoid
- Schizophrenia mental retardation deafness retinitis
- Myopathy with lysis of myofibrils
- Sebocystomatosis
- Congenital sucrose isomaltose malabsorption
Order 18gm nasonex nasal spray amex
The massive substernal component was delivered prior to definitive identification of the recurrent laryngeal nerve allergy testing techniques discount 18 gm nasonex nasal spray mastercard. In the absence of amplitude or latency changes, safe delivery without traction injury was accomplished. A continuous laryngeal nerve monitor stimulates (yellow wire) the ipsilateral vagus nerve, monitoring the functional integrity of the recurrent laryngeal nerve during the procedure. A custom, long McCabe is superior to the classic McCabe dissector, a Schnidt, or a right-angle clamp in reaching into deep narrow spaces. Larynx: Examination of the larynx should also assess the pharynx for compression, as well as vocal cord mobility. Pemberton maneuver: the maneuver is performed by having the patient raise both arms against the face for several minutes to see if the patient develops reversible facial flushing or cyanosis, sometimes associated with shortness of breath or stridor. A positive Pemberton sign indicates superior vena cava syndrome causing diminished venous outflow from and venous congestion of the head and neck due to goiter-related compression of the vessels in the mediastinum. Older adult or infirm patients with lesser narrowing may be observed for progression, whereas younger or more symptomatic patients may be offered surgery promptly. Imaging Ultrasound of the neck Prior to thyroidectomy, patients should undergo a formal ultrasound of the neck and thyroid gland to assess the risk of malignancy in the goiter. In the presence of abnormal adenopathy or invasive features, a fine-needle aspiration biopsy may be warranted. Significantly, posterior mediastinum extension is rare in the absence of concomitant anterior mediastinum involvement. A meta-analysis linked extension to specific structures with the need for additional procedures (Table 81. Goiter extension above the fourth vertebrae or above the level of the aortic arch can usually be managed transcervically. Posterior mediastinum extension of the goiter necessitates a thoracotomy for exposure and extirpation. The degree of tracheal compression, described as the percentage reduction in tracheal diameter, should be noted. Any assessment of substernal goiter should include a description of the degree of tracheal compression is described as the greatest percentage reduction in tracheal diameter. Compression greater than 35% is considered prognostic, with near-universal relief of preoperative positional dyspnea. Moreover, laryngeal nerve monitoring may be done intermittently or in real time, using vagal nerve stimulation during the thyroidectomy. A study suggested intermittent laryngeal nerve monitoring results in higher rates of laryngeal nerve palsies. Electromyographic signals suggesting no changes in the amplitude or latency of recurrent laryngeal nerve signals during surgical maneuvers to deliver a large substernal goiter provide real-time feedback regarding the function of the recurrent laryngeal nerve. Substernal goiter Historically, the presence of a substernal goiter has been considered a sufficient indication for surgery. However, specific preoperative factors predict greater improvements in patient symptoms. Improvement or resolution of positional dyspnea varies with the degree of preoperative tracheal compression. Greater than 35% narrowing of the tracheal lumen has been Massive and Substernal Goiter 551 Instruments and Equipment to Have Available 1. In general, longer instruments are needed than those needed for standard thyroidectomy. The tip of the right angle clamp common on many surgical trays may not fit in the tight space between the thyroid goiter and the thoracic inlet. The tip of a McCabe dissector is shorter, and the angle of the tip is wider, making it more suited to dissection in this region. The suction dissector is used to expose planes around the goiter, making tunnels into the mediastinum, whereas the long McCabe ("the Longo") facilitates dissection of vessels between the tunnels. Endoscopic visualization is not usually needed, but a good headlight is mandatory. The vast majority of goiters involving the posterior mediastinum also involve the anterior mediastinum. Goiters extending into the posterior mediastinum expand caudally along the esophagus, posterior and deep to the inferior thyroid artery. Substernal goiter surgery is complex, and outcomes after surgery are better when surgery is performed by experienced, high-volume thyroid surgeons. Airway compromise during intubation Intraoperative hemorrhage Recurrent laryngeal nerve injury Hypoparathyroidism and hypocalcemia Tracheal or esophageal injury Surgical Technique After a systematic workup, the patient is brought to the operating room. Intubation Communication between the otolaryngologist and the anesthesiologist is a prerequisite for safe airway management in a patient with an obstructive lesion. Tracheal deviation does not hamper passage of an endotracheal tube, although intubation over a flexible fiberoptic bronchoscope can help to guide advancement and placement of the endotracheal tube with severe deviation. With substantial tracheal compression, a smaller-caliber endotracheal tube may be necessary. Nevertheless, it is prudent for the surgeon to be present during induction of anesthesia. Thoracic consultation the vast majority of substernal goiters may be removed transcervically, without need for additional exposure afforded by osteotomy of the manubrium or sternum. Nevertheless, adhesions from prior surgery or locally invasive thyroid cancer or ectopic thyroid tissue may require added exposure. Patients with a history of sternotomy for cardiac surgery should never undergo repeat sternotomy without the ability for cardiopulmonary bypass, because atrial injury becomes a factor. A large meta-analysis has also linked the need for thoracic exposure based on caudal extent of the goiter (see Table 81. In cases of massive extension the strap muscles may be sectioned and reapproximated with mattress suturing at the conclusion of the case. Retropharyngeal extension of the goiter may be encountered but is less common than substernal extension. A and B, Increased exposure afforded by median sternotomy, allowing increased access to the region surrounding the great vessels, enabling safe complete resection. The recurrent laryngeal nerve is usually in its normal anatomic position, even in cases involving large substernal goiters. However, if the larynx is relatively low relative to the thoracic inlet, it will be difficult to identify the recurrent laryngeal nerve prior to delivering the substernal component into the neck. Dissection of the substernal component can be challenging due to limited exposure afforded by the thoracic inlet. This is particularly the case if there has been prior surgery and the goiter is scarred to the tissues around the thoracic inlet. Palpation into the chest with finger dissection assists with delivery of the substernal component into the neck. If the gland cannot be mobilized and delivered, thoracic surgery consultation for added exposure is mandatory. Thus the substernal component of the gland is often delivered into the neck without dissecting the recurrent laryngeal nerve prior to this maneuver. Moreover, mobilization of the gland out of the chest is frequently associated with substantial bleeding. However, in the presence of a large substernal goiter, the inferior thyroid pedicle may not be well visualized prior to delivering the gland out of the neck. Upon delivering the gland out of the chest, hemostasis must be undertaken with care. Application of manual pressure to the bleeding surface of the thyroid and other areas is followed by meticulous hemostasis. In the vast majority of cases the recurrent laryngeal nerve remains posterior to the thyroid gland; in cases with goiter extension into the posterior mediastinum, the recurrent laryngeal nerve is displaced in an anterior direction. In these cases, finger dissection and mobilization will be associated with a severe traction injury to the nerve. After hemostasis is achieved, the strap muscles are reapproximated which the neck is closed in layers. Assessment of the adequacy of the airway-evaluate for shortness of breath and stridor 2. Airway entry Because goiters are engorged with enlarged blood vessels, intraoperative bleeding is not uncommon. Early ligation of the superior and inferior thyroid pedicles will diminish blood loss.
Quality 18gm nasonex nasal spray
Vascular anomalies (aberrant carotid artery or dehiscent jugular bulb) and glomus tumors may be mistaken for effusion and may need to be ruled out with imaging prior to myringotomy in order to avoid the risks of bleeding and neurovascular complications allergy vertigo order generic nasonex nasal spray online. Postoperative Management Serous effusions do not require treatment with antibiotic drops. However, if bleeding is encountered, with evidence of infection, or if a thick mucoid effusion is identified, use of antibiotic drops with or without steroids for 5 to 7 days may help resolve the infection more rapidly and prevent obstruction of the tube. Follow-up in 1 month followed by every 6 months is recommended until the tube extrudes. Very close monitoring is recommended in patients with complications of acute otitis media requiring tube insertion. Editorial Comment As reviewed by the author, a significant varied list of otologic procedures can be performed in the office or clinic. In order to avoid complications or anxiety and pain to the patient, it is important for the surgeon to realize the limitations imposed by the procedure and tolerance of the patient. The operative skills of the surgeon can be more critical and demanding in this setting. Training and experience in this regard comes from procedures performed in the operating room, where techniques can be mastered in a controlled environment. Intratympanic therapies have transformed the delivery and outcomes of previously limited treatment options. Gentamicin instilled into the middle ear has provided an excellent means of controlling vertigo attacks from Meniere disease, avoiding more complicated operative interventions. Since the patient is fully awake, it is important to have the office equipped with anticipated medications, dressings, and instruments needed to complete these procedures. Intratympanic dexamethasone for sudden sensorineural hearing loss: clinical and laboratory evaluation. Oral vs intratympanic corticosteroid therapy for idiopathic sudden sensorineural hearing loss. Intratympanic dexamethasone for sudden sensorineural hearing loss after failure of systemic therapy. The physician should have a reassuring demeanor to put the patient at ease in this potentially challenging setting. Which of the following agents can be used for topical anesthesia for office-based procedures in otology Which of the following lesions of the ear canal does not require biopsy for diagnosis What is the incidence of hearing loss with low-dose intratympanic gentamicin treatment for Meniere disease Patients may be treated in a variety of settings including an emergency room, clinic, or office. It is important to note that different age- and gender-specific patterns emerge in describing the specific types of foreign bodies found within the external auditory canal. Jewelry was by far the most common foreign body seen in the young population, with beads and earrings being the most frequently identified types. Senior citizens are also uniquely vulnerable to the accidental insertion of disk batteries owing to altered cognition, reduced tactile sensation, and the more frequent use of hearing aids. The most common inorganic object creating this problem, as already stated, is the end of a cotton-tipped applicator. Institutionalized adults and children may use these materials instead of cotton-tipped applicators, medical packing, or earplugs. In this population, if drainage, infection, or odor has not developed, such material may be found only on routine physical examination. Along with using instrumentation to clean their ears, adults also place objects in the ear canal for protection, including devices to minimize water exposure because of recurrent otitis externa or perforation of the tympanic membrane. Materials used for hearing protection can become lodged or break off and remain in the external canal. Examples of such products include silicone putty used for sound or water protection and Silastic occlusive plugs or foam inserts for sound protection. Again, patients become acutely aware of broken off materials remaining in the ear canal. Unless a witness observes a child placing a foreign body in the canal, its presence may not be discovered until routine physical examination detects the object or problems arise because of its presence. Localized aural discharge, cellulitis of the concha and external meatus, or serosanguineous otorrhea would prompt further evaluation. Once water enters the external canal, vegetable materials such as beans and peas can swell and cause obstruction, pain, and maceration. Other materials that have been found in the ear canal include small toys, beads, erasers, crayons, pits from fruit, disk batteries, nuts, and stones. Disk batteries should be removed as soon as possible to avoid the liquefaction necrosis that results when moisture and secretions permit the flow of electrons. Similarly, unsuccessful attempts at removal of the battery that result in trauma and bleeding in the ear canal would also allow flow of current and thus lead to further tissue destruction. Insects occasionally find their way into the ear canals of children and adults alike. These are usually flying insects, but crawling insects may also enter the canal, especially when a person is sleeping. Patients become acutely aware of such a situation because of the noise generated by the insect and the associated pain. Management in this situation becomes more urgent than that called for by inanimate objects. Aural irrigation to remove foreign bodies (other than insects) in the external auditory canal should be avoided because the object is rarely flushed out and skin maceration often results. Live insects should be drowned with alcohol, mineral oil, or topical anesthetics (Pontocaine, Xylocaine). A large nasal suction (10-12 French) device may make sufficient contact with the object to remove it from the canal. Passing a right-angled hook parallel to the object and then beyond it allows optimal placement of instruments for extraction. Injection of a local anesthetic followed by canal dilatation with progressively larger specula may facilitate removal of the foreign body. Ease of extraction is directly proportional to the number of previous failed attempts. Prior treatment 1) If there is a history of previous foreign bodies and infection (Beware of canal stenosis. Surgery 1) If there has been previous otologic surgery, determine its extent and type. Permits planning in terms of the appropriate instrumentation, lighting, the type of anesthesia (if needed), and the method of extraction 2. Exploration of the ear under intravenous sedation or general anesthesia should be considered for patients who may have damage to the ossicular chain or inner ear. General anesthesia will probably be necessary for most children and anxious, uncooperative adults. Patients with acute hearing loss and dizziness should be suspected of injury transmitted to the inner ear. Consider if there is concern for a coexisting foreign body in the tracheobronchial tree 2. Consider if patient has a history of extensive otologic surgery, disease, or the medial extent of the foreign body is in question 3. A large-gauge suction is usually successful in removing most objects from the external auditory canal. Adult or pediatric patients with otorrhea, hearing loss, and obstruction or occlusion of the ear canal who fail to respond to topical and systemic therapy may have pathology of the middle ear and mastoid or foreign bodies causing their symptoms and findings.
Buy nasonex nasal spray 18gm with mastercard
Elevation of the marginal mandibular nerve can be done by dividing the facial vein low on the gland and elevating the nerve along with the vein allergy medicine 7 month old 18 gm nasonex nasal spray fast delivery. This is best done by incising the fascia over the anterior belly of the digastric muscle and reflecting it posteriorly. The muscle can be identified by the direction of its fibers extending from posterosuperior to anteroinferior (at a significantly different angle from that of the anterior belly of the digastric muscle). The mylohyoid muscle is occasionally difficult to identify, especially with chronically infected glands adherent to the muscle. This muscle may also be dehiscent in areas and lead to difficulty identifying its posterior aspect. The vessels are usually sacrificed to free the overlying portion of the submandibular gland. The lingual nerve can be seen superiorly as a broad band extending from deep to the mandible posteriorly and looping close to the anterior portion of the gland, where it gives rise to nerve roots extending into the submandibular ganglion. Injury is unusual unless previous inflammation has made it difficult to identify the plane deep to the gland. Care must be taken to include dissection of the duct up to the mucosa of the floor of the mouth; otherwise, calculi can be retained in the duct and result in postoperative chronic inflammatory disease of the duct remnant. Bimanual palpation at this stage often helps prevent retained calculi in the duct. A salivary scope can be placed into the duct through the neck in a retrograde fashion if there is concern regarding retained calculi. When the anterior portion of the gland has been freed from the lingual nerve and submandibular duct, the remainder of the gland is easily detached from the underlying fascial planes over the floor of the submandibular triangle. The gland can then be retracted inferiorly with countertraction placed on the soft tissue superior to the gland, and the superior aspect of the gland is dissected free from the soft tissue just inferior to the mandible. Care must be taken to avoid injury to the marginal mandibular nerve where it courses just lateral and superior to the gland. Injury is avoided by either identifying the nerve or by maintaining dissection within a plane immediately adjacent to the substance of the gland. As the gland is reflected inferiorly, the facial artery can be seen indenting the posterosuperior surface of the gland. It is usually divided as it leaves the gland superiorly and then again as it enters the gland, although it can be preserved in noninflamed cases by dissecting the artery free of the gland and individually identifying, dividing, and ligating the feeding vessels extending into the substance of the gland. Particular care should be taken to examine the anterior portion of the triangle deep to the mylohyoid muscle. The platysma muscle, subcutaneous layer, and skin should each be closed separately. The branches of the lingual nerve passing to the submandibular ganglion are divided to free the nerve from the specimen. Care must be taken to ensure that there are no calculi distal in the duct, or postoperative infection in the duct remnant may result. Retraction of the tongue and floor of the mouth, including the lingual nerve, allows visualization of the mylohyoid muscle. Blunt dissection is used to free the submandibular gland from surrounding structures. A drain may be inserted through the incision site, and the mucosa is re-approximated with absorbable suture. Endoscopic Approach There are case reports of endoscopic excision of the submandibular gland via either a transoral or small neck or hairline incision. Techniques are endoscopically assisted but otherwise are similar to those described above. The intraoral approach to submandibular gland excision accesses the submandibular gland from its deep surface, thereby avoiding the marginal mandibular nerve. Although authors have been successful in avoiding marginal nerve injury, overall neurologic injury may be higher with this approach, with one study showing 81% of patients developing transient partial anesthesia of the tongue and 68% developing mild temporary limitation of movement of the tongue, although this was attributed more to edema than to nerve injury. The submental approach has been studied by Roh10 in a prospective randomized fashion, with no increased incidence of injury to the facial nerve found with the submental approach. Roh has also studied the retroauricular approach and had no instances of marginal nerve injury with this approach, although he had two such incidents in the same study while using the traditional transcervical approach. It is important to recognize that even with the traditional transcervical approach reports of transient injury to the marginal mandibular nerve have varied significantly, from 7. However, given this wide variability, we must be cautious in extrapolating the findings of the current small studies to a wider population of surgeons and patients. Nevertheless, the findings of these early studies are promising, and alternative approaches to submandibular gland excision are reasonable to consider in the properly selected patient. The chapter highlights the important anatomy and suggests techniques for avoiding the neurologic complications that are functionally very important. Submandibular sialoadenectomy with local anesthesia in the era of minimally invasive surgery. The new era of robotic neck surgery: the universal application of the retro-auricular approach. Removal of the submandibular gland by a submental approach: a prospective, randomized, controlled study. Editorial Comment Inflammatory disease of the submandibular gland is increasingly managed with minimally invasive techniques. This is better for the patient and allows the surgeon to avoid open surgery in an inflamed or infected difficult surgical field. Intraoral approach for the treatment of submandibular salivary gland mixed tumors. Submandibular gland surgery: an audit of clinical findings, pathology, and postoperative morbidity. Submandibular gland excision: long-term clinical outcome in 139 patients operated in a single institution. Bilateral submandibular gland excision with parotid duct ligation for treatment of sialorrhea in children: long-term results. Malignant tumors vary greatly in behavior, from the indolent (acinic cell carcinoma) to the highly lethal (carcinosarcoma). Metastatic lymphadenopathy from primary skin malignancies is also a common indication for parotidectomy. Lymphoma poses a particular challenge to the parotid surgeon-accurate diagnosis may be available only after open biopsy. Therefore it is important to keep lymphoma in the differential to avoid extirpative surgery for this medically-managed disease. Chronic parotitis is a less common indication for superficial parotidectomy and is recommended for patients who are refractory to medical management or minimally invasive techniques. Fixation is worrisome but may occur in benign tumors that extend through the stylomandibular tunnel into the prestyloid parapharyngeal space or that are inflamed. Malignant degeneration occurs in 5% to 10% of pleomorphic adenomas; although the risks are not well defined, a long-term history or recurrence of pleomorphic adenomas may point to an increased prevalence of carcinoma ex pleomorphic adenoma. However, with a large mass in the tail of the parotid extending beyond 1 cm posterior to the ascending ramus, a small incision can be made parallel to the ramus, 1 cm posterior to it, to obtain tissue for flow cytometry and pathology. This technique is very useful in elderly patients with lymphoma and can be performed in the office. The risk of injury to the facial nerve and its significance must be discussed with all patients. Patients who have malignant tumors must be informed of the plan regarding nerve sacrifice and reconstruction. For tumors at or above the level of the lobule, the incision need not extend onto the neck. This exposes parotid tissue and allows access to the plane in which the nerve courses.
Buy nasonex nasal spray with a visa
Nerve function: Evaluate and document preoperative function of the spinal accessory nerve and brachial plexus kaiser oakland allergy shots buy nasonex nasal spray line, because these nerves will be at risk for injury during the dissection. The posterolateral neck dissection is an operation that is typically used in the management of cutaneous cancers of the posterior scalp, auricle, or upper neck. It is done either electively, to stage the clinically node-negative neck, or therapeutically, to treat the node-positive neck. In contemporary practice, this operation is most often used to treat a clinically node-negative neck that has been found to have microscopically positive nodal disease in one or more of the regional nodal basins. The posterolateral neck dissection is an extended neck dissection that is often combined with a comprehensive or selective neck dissection. Anderson Cancer Center wrote a definitive description of this procedure and their results with it. In experienced hands, this operation provides excellent oncologic, functional, and cosmetic results. Systemic imaging may be indicated based on the histology and clinical stage of the disease. During the procedure, fibroadipose node-bearing tissue is removed from the inferolateral portion of the neck where the trapezius and clavicle meet. Extreme caution must be exercised in this region to avoid injury to inferolateral branches of the brachial plexus and the terminal aspect of the spinal accessory nerve. This includes histologic type, location, and previous treatment (history of surgery or radiation treatment for skin cancer). Occupational history: this operation, when performed without complication, can lead to decreased shoulder function for up to 18 months following surgery. Typically this is manifested by a decreased range of motion and strength on shoulder abduction, which, with intervention by a trained physical therapist, can be improved greatly with anticipated return to baseline. Use to confirm or rule out the presence of regional lymph node metastasis to facilitate treatment planning in cases where the finding of lymph node metastasis is indeterminate by cross-sectional imaging criteria. The treatment of occult and clinically node-positive metastasis to the neck from a cutaneous malignancy involving the skin of the posterior scalp, auricle, and upper neck 2. Even in the presence of paralyzing agents, these motor nerves are readily identified by reliable anatomic landmarks and the stimulation provided by electrical dissection. This occurred in only 3 of 55 patients reported in a large series, making this a rare position for this operation. Given the location, this scalp melanoma may require posterolateral neck dissection for gross disease or positive sentinel lymph node biopsy. Disseminated metastases: this operation is contraindicated in patients for whom the procedure would provide neither prolonged survival nor significant palliation. Patients with extensive lymph node metastasis: Those with involvement of the deep muscles of the neck, vertebrae, or carotid artery are advised to consider systemic therapy options that could help to decrease the risk of distant metastatic cancer and potentially make the locoregional disease burden more manageable by resection. Medical comorbidities with increased risk for general anesthesia: Patients deemed to be medically at high risk for general anesthesia who have microscopic lymph node metastasis can be often be managed successfully with radiation therapy alone. Perioperative Antibiotic Prophylaxis First-generation cephalosporin Monitoring None necessary Instruments and Equipment to Have Available 1. The four cutaneous nerves of the cervical plexus are the lesser occipital nerve, great auricular nerve, transverse cervical nerve, and supraclavicular nerve. It then courses inferolaterally through the posterior triangle and passes under the trapezius muscle that it innervates. Trapezius muscle: the upper fibers of the trapezius originate from the spinous processes of C1 to C7, the external occipital protuberance, the medial third of the superior nuchal line of the occipital bone, and the ligamentum nuchae. Inferiorly the fibers travel downward and laterally and insert into the posterior border of the lateral third of the clavicle. This fascia and the external jugular lymph nodes should be entirely removed, as they are important components of the specimen in cutaneous malignancies of the scalp, ear, and/or face. Take care to avoid injury to these nerves and prevent avulsion of the transverse cervical vessels or thoracic duct. Elevating thick superior and posterior skin flaps: the flaps should be elevated in the subcutaneous plane. This is important because the occipital and preauricular lymph nodes can be located within the subcutaneous adipose tissue in this portion of the neck. Failure to gain adequate exposure of both the anterior and posterior neck during the dissection 3. Incompletely visualizing and dissecting the neural structures at risk, such as the spinal accessory nerve and brachial plexus: It is necessary to identify and preserve the spinal accessory nerve in the posterior triangle of the neck. Use extreme caution in this region to avoid injury to inferolateral branches of the brachial plexus and the terminal aspect of the spinal accessory nerve. Chyle leak, bleeding, neural injury: Complications of the posterolateral neck dissection include all of the complications associated with the more standard selective/comprehensive neck dissection. Injury to the spinal accessory nerve: Owing to the extensive inferoposterior and inferior dissections, the risk of injury to the spinal accessory nerve and/or brachial plexus is greater than in more standard neck dissections. Surgical misadventures involving these neural structures can best be avoided by careful dissection of these nerves under direct visualization. Editorial Comment Posterolateral neck dissection is indicated for skin cancers of the upper neck, posterior scalp, and auricle. Primary resection of these cancers can be quite complex, involving resection of the temporal bone, lateral skull base, temporomandibular joint, and/or mandible. The need for facial nerve sacrifice adds further complexity, consequently posing unique reconstructive challenges. Planning of the surgery and incision for posterolateral neck dissection should take into account the extent of the primary resection, type of reconstruction planned. A case series review of 55 patients treated over a 10-year period from 1982 through 1991 with a minimum of 3 years of follow-up at M. Anderson Cancer Center included 35 patients with melanoma, 10 with squamous cell carcinoma, and 10 with other histologic types. In this series, disease was controlled at the site of the primary tumor in 89% of patients (94% of patients with melanoma) and regional disease was controlled in 93% of patients (89% of patients with melanoma). Anderson Cancer Center show that the addition of postoperative adjuvant radiation therapy can enhance locoregional control. Patients in this group had undergone simple lymph node excision (35), selective neck dissection (90), or a radical or modified radical neck dissection (35). The actuarial local, regional, and locoregional control rates in this population at 10 years were 94%, 94%, and 91%, respectively. Potential complications specific to the posterolateral neck dissection include all of the following, except a. All of the following nodal basins should be removed with a posterolateral neck dissection, except the a. Posterolateral neck dissection: preoperative considerations and intraoperative technique. With schwannomas, the nerve fibers of the parent nerve may be draped over the tumor, making it possible to preserve the nerve, although transient postoperative paresis is common. However, in most cases the schwannoma is inseparable from the nerve and the nerve must be sacrificed. Neurofibromas are not encapsulated, and because the nerve fibers are part of the tumor, the nerve cannot be preserved. It is important to distinguish preoperatively between a prestyloid and a poststyloid mass, as this affects the differential diagnosis and may determine the surgical approach. Prestyloid tumors are likely to originate from branches of the mandibular division of cranial nerve V. However, the nerve of origin may not be apparent even at surgery if a tumor has originated from minor, unnamed nerves. It is confined medially by the pharyngobasilar fascia and the superior constrictor muscle of the pharynx. This information permits the surgeon to narrow down the differential diagnosis, to plan the best approach, and to counsel patients preoperatively about possible sequelae. This may influence the surgical approach, and even affect the decision whether or not to do surgery. The surgeon should not be concerned about puncturing the internal carotid artery with a small-caliber needle, as bleeding can be controlled with digital pressure. This is important, as paragangliomas may rarely be hormonally active and may require preoperative embolization.
Chinese Persimmon (Japanese Persimmon). Nasonex nasal spray.
- Dosing considerations for Japanese Persimmon.
- How does Japanese Persimmon work?
- Are there any interactions with medications?
- Are there safety concerns?
- What is Japanese Persimmon?
- High blood pressure, constipation, hiccough, stroke, excessive fluid, improving blood flow, and reducing body temperature.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97060
Order generic nasonex nasal spray online
External branch of superior laryngeal nerve: this branch supplies the cricothyroid muscle allergy symptoms 0f discount 18 gm nasonex nasal spray with amex. It descends along the inferior constrictor muscle within 1 cm of the superior pole of thyroid. In approximately 20% of cases, the nerve may be closely adherent to the superior pole. Inadequate preoperative localization Failure to identify recurrent laryngeal nerve Insufficient four gland exploration Incorrect diagnosis of primary hyperparathyroidism. In cases of hypercalcemia Reoperative Parathyroidectomy 581 scenario, which can represent secondary hyperparathyroidism, metabolic bone disease with or without vitamin D deficiency, or persistent primary hyperparathyroidism. Parathyroid located in paratracheal groove after adequate mobilization and medial retraction of thyroid gland. Right lateral approach for reoperative parathyroidectomy using methylene blue as an intraoperative adjunct and demonstrating a right superior parathyroid adenoma and a normal inferior gland. Answer It is clear that reoperative surgery represents a challenge due to the increased risk of ectopic gland location, likelihood of multiple gland disease, and the presence of postsurgical scarring from the initial surgical exploration. Nuclear medicine examination with Sestamibi scanning is paramount in identifying metabolically active parathyroid tissue. This allows for the identification of ectopic parathyroid tissue in more than 80% of cases. Failure to preserve adequate volume of functional parathyroid tissue or consider reimplantation of a portion of a gland into a well-vascularized recipient bed Editorial Comment Parathyroid surgery for primary hyperparathyroidism has a high success rate on initial surgery, but reoperative surgery faces special challenges that may include abnormal patient anatomy, scarring from previous surgery, and concomitant thyroid pathology. Detailed review of previous reports and operative attempts, as well as repeat attempts at localization, is essential in maximizing success. When possible, reoperative surgery should be performed by experienced parathyroid surgeons in the presence of intraoperative parathyroid hormone monitoring. Excision efficiency of radioguided occult lesion localization in reoperative thyroid and parathyroid surgery. Reoperative parathyroidectomy: an algorithm for imaging and monitoring of intraoperative parathyroid hormone levels that results in a successful focused approach. Reoperative parathyroidectomy in 228 patients during the era of minimal access surgery and intraoperative parathyroid hormone monitoring. Reoperations for primary hyperparathyroidism - improvement of outcome over two decades. Fewer adverse events after reoperative parathyroidectomy associated with initial minimally invasive parathyroidectomy. Careful patient and family education regarding the symptoms of hypocalcemia (leg cramps, perioral hyperesthesia/tingling) and the need for serious attention to those symptoms 6. Assess and manage vitamin D deficiency as a factor that may prolong hypocalcemia and "bone hunger. Unilateral injury can be observed initially, with expected improvement in several months. Rare use of exogenous parathyroid hormone in refractory cases (costly and requires parenteral administration) 3. Postoperative hemorrhage requires surgical exploration, with identification and ligation of the bleeding vessels. Which of the following is a relative contraindication to repeat parathyroidectomy Elevated serum calcium and decreased urinary calcium in a patient with a family history of similar finding d. Gives a review of the workup and strategies for reoperation on parathyroid disease. Office-based procedures allow for prompt, low-cost diagnosis and management of many otolaryngological conditions. The application of ultrasound guidance improves accuracy as well as diagnostic yield. In addition, the application of technologic advances and adaptive surgical techniques has improved patient outcomes and expanded the breadth of procedures possible in clinical settings, avoiding the risks and costs of general anesthesia for otherwise minor procedures. Sialendoscopy is a procedure well suited for the transition to the clinic setting for management of salivary gland pathology. In-office salivary gland procedures, including sialendoscopy, provide excellent minimally invasive gland-sparing therapy without the need for general anesthesia. Solitary gland symptoms are more suggestive of focal obstruction (sialolithiasis or stricture). Pain with mastication and swelling that persists for more than a few hours, or occurs upon arousal from sleep, is more indicative of temporomandibular joint disorders. Duration of the mass in the neck may impact the decision to pursue further evaluation 1) A persistent or slowly progressive mass in the neck lasting for more than 3 weeks should be screened for malignancy. Oral cavity Examination of the oral cavity may reveal turbid discharge from the salivary ducts, palpable submucosal masses consistent with calculi, or oral cavity lesions. If calculi are palpated, the location and the size of the calculi should be noted. Pharynx/larynx Examination may reveal a primary malignant lesion within the oropharynx, hypopharynx, or larynx responsible for the mass in the neck. In the neck, ultrasound can visualize vital neck anatomy (thyroid, lymph nodes, and vessels), characterize palpable mass in the neck, or visualize nonpalpable malignant adenopathy. Using characteristic imaging criteria, thyroid and neck masses can be radiographically triaged for biopsy (see Chapter 78 and Chapter 64). Magnetic resonance imaging Useful when the clinician suspects soft tissue masses (superficial or deep lobe parotid lesions), vascular lesions (glomus tumors, paragangliomas), or neural tumors (schwannomas, neurofibromas) 4. Angiography May be required for evaluation of carotid body tumors and preoperative embolization. If carotid artery injury or sacrifice is anticipated, angiography may be used to direct therapy (embolization/stenting) or assess for circle of Willis communication (balloon occlusion). The ultrasound enhances accuracy of the biopsy and may help distinguish malignant from benign lesions. In some cases, patients may still require incisional or excisional biopsy to further categorize the type of lymphoma, but following this algorithm, at least other malignancies have been excluded prior to violating the neck. Recurrent acute and chronic sialadenitis Sialendoscopy with or without sialolithotomy effectively relieves salivary gland obstruction related to high viscosity salivary debris, sialolithiasis, or salivary stricture. Ultrasonography is also useful in localizing nonpalpable salivary calculi, directing incisions in the floor Office-Based Procedures 585 of the mouth for salivary calculi, and managing complex salivary strictures (visualization of balloon dilator position, transfacial access to dilated proximal parotid duct for Seldinger technique anterograde dilation). Larger calculi greater than or equal to 4 mm often require the addition of a cutdown and ductotomy or fragmentation of the calculi. Transcutaneous injections and vocal fold motion In addition to the imaging and biopsy guidance afforded by ultrasonography, the ultrasound can also be effective for targeting Botox injections into the salivary glands for sialorrhea or into the muscles of mastication for refractory temporomandibular joint pain with associated muscle hypertrophy (temporalis and masseter). Ultrasound may also be used to map difficult laryngeal anatomy and direct injections into the subglottis (steroid for subglottic stenosis) and vocal folds for augmentation, and direct Botox for spasmotic dysphonia. In many patients, vocal fold and/or arytenoid motion may be seen through the cricothyroid or thyrohyoid membranes. Patients with strong vasovagal reactions Patients who report vigorous vasovagal reactions are not suitable for in-office minor procedures. Antiplatelet therapy or bleeding disorders Patients with bleeding disorders are best managed in an operating room setting. Those on antiplatelet therapy should discontinue therapy prior to elective procedures. If further irrigation is required, due to length of the procedure, the clinician should then transition to sterile saline. One of the challenges with sedation can be the depth of sedation: too little and the patient will move, deleteriously affecting efficacy of the procedure; too much and the respiratory drive and airway protection may be suppressed. In cases where the patient becomes vasovagal, the clinician should have the ability to place the patient in a supine or slightly Trendelenburg position. For salivary procedures, the patient is ideally positioned in the upright sitting position to allow for optimal patient control of secretions and ergonomic positioning for the physician, particularly while performing endoscopy and viewing the monitor. None: Not required unless the patient has a prosthetic implant (heart valve) and sialolithotomy is planned 2.
18 gm nasonex nasal spray with visa
The cooperative patient may assist with exposure by holding his or her own tongue depressor(s) allergy medicine reduce swelling purchase cheap nasonex nasal spray on line. Primary snoring in the setting of significant burden on the patient or bed partner Contraindications 1. Cefprozil 500 mg may be given orally 1 hour before procedure, or clindamycin may be used for patients who are penicillinallergic. The redundant mucosa may be grasped with forceps and truncated at the distal aspect of the musculus uvulae. This step may serve to widen the distance between the tonsillar pillars laterally. A, Preoperative, B, intraoperative, and C, postoperative appearance of anterior palatoplasty. Thus this procedure may be particularly advantageous for the patient with a thick soft palate. Additionally, the safest area to treat is at or near the midline, where the palatal bulk is the greatest. For information on anesthesia, positioning, and perioperative antibiotic prophylaxis, see section "Anterior Palatoplasty. The first mark should be placed in the midline 1 cm below the border of the hard palate; the lateral lesions should each be placed approximately 1 cm away from the initial mark, just above the superior pole of the tonsil on either side. Adjacent radiofrequency applications should be placed a minimum of 8 mm apart to avoid lesion overlap and subsequent mucosal damage. Generous local injection serves to increase interstitial volume and thus decrease the risk of tissue damage. The superior surface of the soft palate can be visualized with a flexible scope during lesion generation; any mucosal blanching during ablation indicates that the needle is too deep and should be withdrawn. For the temperature-controlled devices, an energy level of 400 to 700 joules should be used for midline/paramedian lesions; 300 to 350 joules will suffice for lateral lesions, where the palate is typically thinner. When using plasma-mediated ablation, 10 to 15 seconds of coblation at a power setting of 6 is appropriate for each lesion. The implants themselves as well as associated scarring serve to stiffen the soft palate. There are some anatomic preprocedure considerations for patients undergoing palatal implantation. If the palate and/or uvula is too long, palatoplasty and/or partial uvulectomy could be considered. If the soft palate is too short, this tissue may not be able to safely house the implant. The soft palate is thickest in the midline, and bulk drops off significantly more laterally. The risk of mucosal injury is higher in these lateral areas, especially in the patient whose palate is thin at baseline. The other two should be inserted approximately 3 mm to the left and right of the initial implant, such that there is approximately 2 mm of space between each implant. Introduce the applicator tip to the third marking in a curvilinear fashion, taking care not to bypass the soft palate. The author prefers to have an assistant look into the nasopharynx with a flexible endoscope at this time to make sure the applicator tip is not visible in the nasopharynx. The surgeon may avoid this by viewing the soft palate from above with a flexible laryngoscope. Various sclerosants have been used in the literature, including a 50:50 mix of 2% lidocaine and 99% dehydrated ethanol, 1% to 3% sodium tetradecyl sulfate, and polidocanol. For anesthesia, positioning, and perioperative antibiotic prophylaxis, see section "Anterior Palatoplasty. Some patients, including most who undergo anterior palatoplasty, will require narcotic medications. Of the previously noted procedures, anterior palatoplasty is generally associated with the greatest discomfort; these patients may require narcotics for several days. This is typically self-limited and does not require treatment, but the patient and surgeon should be aware of this potential complication and its impact on the airway. If a patient fails with a certain procedure in the short or long term, one could always consider oral appliance therapy. Office-Based Snoring Procedures 365 often be performed in succession in the appropriate patient. For example, pillar implants may be used to stiffen the palate that has already undergone palatoplasty and/or uvulectomy. Lastly, it should be reiterated that snoring is currently considered medically benign. In general, it seems that a majority of patients undergoing any of these procedures see some meaningful, short-term decrease in snoring. Good, long-term data are relatively lacking; however, the long-term data available indicate that many patients experience a return of snoring symptoms. At 3 to 4 years postprocedure, only 25% of patients and bed partners were noted to be satisfied. Of note, about two-thirds of patients require more than one injection session, with about 15% requiring three or more to achieve these results. Since positive pressure therapy, custom mandibular repositioning appliances, and more involved surgical procedures are often not covered services in the absence of sleep apnea, minimally invasive procedures for the treatment of nonapneic snoring are potentially very applicable to the large population affected by nonapneic snoring. Palatal stiffening procedures may reduce snoring by reducing palatal flutter with low morbidity and risk. Combination therapy to manage all of the specific anatomic and pathophysiologic factors. Diagnosis and treatment of snoring in adults-S1 guideline of the German Society of Otorhinolaryngology, Head and Neck Surgery. Snoring is not associated with all-cause mortality, incident cardiovascular disease, or stroke in the Busselton Health Study. Oral appliance therapy in patients with daytime sleepiness and snoring or mild to moderate sleep apnea: a randomized clinical trial. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. Efficacy of the pillar implant in the treatment of snoring and mild-to-moderate obstructive sleep apnea: a meta-analysis. Patient selection and efficacy of pillar implant technique for treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Radiofrequency ablation treatment of soft palate for patients with snoring: a systematic review of effectiveness and adverse effects. Anterior palatoplasty can increase the anterior-posterior dimension of the velopharynx d. Does drug-induced sleep endoscopy change the treatment concept of patients with snoring and obstructive sleep apnea Radiofrequency volumetric tissue reduction of the soft palate: a new treatment for snoring. Palatal implants for the treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs. Palatal implants in the treatment of obstructive sleep apnea: a randomized, placebo-controlled single-center trial. Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Four-year outcomes of palatal implants for primary snoring treatment: a prospective longitudinal study.

Buy discount nasonex nasal spray 18 gm online
Transverse cervical and internal mammary veins can be used when the paired artery is dissected allergy forecast in austin purchase nasonex nasal spray 18 gm line. Typically the majority of the flap is inset while ischemic to minimize edema of the flap. A tube is created by twisting the elliptical flap over a Montgomery pharyngeal stent (salivary bypass tube). Either a running Connell stitch or interrupted horizontal mattress sutures are used to close the pharynx 4. Evenly spaced interrupted sutures placed with care not to injure the intima will result in a successful anastomosis. Use heparinized saline to ensure complete visualization of proper placement of the sutures. If a coupler is not available or malfunctions, be prepared to sew the veins together. Irrigation of the vein with heparinized saline will keep the vein from collapsing and improve visualization of the edges of the vessel. Turn the head in both directions to ensure the artery and vein do not become kinked. A schematic detailing of one method of flap inset that allows for an external monitoring skin paddle. The skin paddle that will become the neopharynx (A), deepithelialized portion in the neck (B), and triangular external monitor (C). The flap should be elevated so that the distal edge of the skin paddle is not under tension, particularly when the patient turns his/her head. Creation of an inadequate tracheostoma-Half-mattress sutures should be used to bring the edges of the trachea to the skin (refer to chapter on total laryngectomy). Small distances should be between tracheal sutures, with wider distances on the skin flaps. The clavicular attachments of the sternocleidomastoid muscle can also impinge on the stoma. Tension on the proximal suture line-This usually occurs either as a result of poor planning of the skin paddle or inadequately releasing the pedicle so it can reach the most proximal inset on the contralateral side without tension. Final reconstruction of total laryngopharyngectomy with external skin paddle for monitoring. Prick the flap with a 25-gauge needle and expect bright red bleeding after a slight delay. To gain maximal rotation the lateral and medial muscle attachments must be released. This can result in a miscalculation of the medial incision for the skin paddle and result in injury to the perforators. A number of retrospective series from individual institutions have looked at oncologic and functional outcomes after resection and reconstruction of the hypopharynx. Monitor for hematoma-Distinguish between the normal appearance of the bulky pedicle overlying the clavicle. Flap monitoring-Methods and duration vary widely based on surgeon training and preference. Every four hours for the first two days, then every six hours for 1 day, and then twice daily until discharge works well. Of note, the rate of postoperative hypocalcemia, which had been previously found to be more common than fistula,3 was not reported. Late complications reported in other series include stricture, stomal stenosis, permanent feeding tube, and small bowel obstruction (in patients who had a laparotomy for flap harvest). Fistula-a major cause of prolonged hospitalization, delayed oral intake, and delays in adjuvant therapy 1) Recognize new or worsening tenderness, erythema, fever, wound breakdown, change in the drain output, or loss of stable suction drains. Small bowel obstruction (those who have a laparotomy for reconstruction) Mortality Perioperative mortality was 3% in this series. This suggests that the mucosa at risk may be greater than indicated by mucosal appearance and frozen section. Patients who were reconstructed with pedicled flaps were more likely to have a prosthesis placed. The authors note that those who had free flap reconstruction were more likely to have circumferential defects and were less amenable to voice prosthesis placement. There are no randomized studies evaluating the impact of type of reconstruction with swallowing. No reconstruction-oversew esophagus with planned salivary fistula Editorial Comment Hypopharyngeal defects may result from localized resections or from total laryngectomy with partial or total (circumferential) pharyngectomy. Optimal reconstruction of Reconstruction of Hypopharyngeal Defects 349 complex hypopharyngeal defects requires special expertise and experience. Kass has divided the subject into laryngeal preservation and laryngeal sacrifice and provided the surgical armamentarium that is needed to reconstruct defects from relatively simple to extremely complex. As emphasized in the chapter, many hypopharyngeal defects require microvascular expertise. Historically, the jejunal free flap and radial forearm fasciocutaneous flaps were preferred for reconstruction of circumferential defects. The jejunal free flap had significant donor site morbidity and resulted in some problems with succus production and sometimes a very "wet" postlaryngectomy voice. The radial forearm free flap also has donor site morbidity, and stricture was sometimes a problem. The larger volume of soft tissue makes it more versatile for insetting into defects that may involve not only the entire circumference of the hypopharynx but extension into the oropharynx, nasopharynx and cervical esophagus, and/or skin. In addition, the donor site morbidity is considerably less than either the jejunum or radial forearm. Reconstruction of large pharyngeal defects with microvascular free flaps and myocutaneous pedicled flaps. What is the most common late postoperative complication following total laryngopharyngectomy When considering how to reconstruct the hypopharynx what factor is most important What is the most common arterial blood supply to the anterolateral thigh free flap Septocutaneous and musculocutaneous perforators from the profunda femoris, a branch from the femoral artery b. Only septocutaneous perforators from the descending branch of the lateral circumflex femoral artery c. Septocutaneous and musculocutaneous perforators from the descending branch of the lateral circumflex femoral artery d. Atlas of Regional and Free Flaps for Head and Neck Reconstruction: Flap Harvest and Insetting. It is relatively uncommon, representing less than 5% of all esophageal cancers, themselves representing 5% of all digestive system cancers. The aggressive clinical course of this disease is influenced by the high incidence of submucosal spread, ipsilateral or bilateral lymph node metastasis, and the high rate of a second primary cancer in the esophagus. The surgical defects are often quite significant and most of the time circumferential, necessitating challenging reconstructive planning. A multidisciplinary team is therefore required for the proper management of patients with cancer of the cervical esophagus, including a head and neck surgeon, thoracic surgeon, reconstructive surgeon, medical oncologist, radiation oncologist, speech language pathologist, nutritionist, and physiotherapist. Squamous cell carcinoma is the most frequent histologic type of cancer found in the cervical esophagus. Primary adenocarcinoma of the cervical esophagus is rare and may arise from Barrett esophagus. Less common are tumors that arise from heterotopic gastric mucosa without evidence of Barrett disease. Benign lesions occur infrequently, the most common being pedunculated hyperplastic or fibrovascular polyps. Patients with cervical esophageal cancer often have vague and nonlocalizing symptoms, while also being known as long-term smokers and drinkers, thus requiring a thorough head and neck oncologic questionnaire, including the following signs and symptoms: 1) Sore throat 2) Hoarseness 3) Gastroesophageal reflux 4) Heartburn/chest pain 5) Difficulty swallowing: dysphagia, odynophagia, aspiration, globus sensation 6) Hemoptysis 7) Weight loss; often associated with advanced disease 8) Dyspnea 9) Referred otalgia 10) Mass in the neck b. A clear timeline of the signs and symptoms is important to collect because it often provides a preliminary idea of the evolution and progression of the cancer.
Buy nasonex nasal spray with amex
To facilitate this allergy symptoms 6 dpo discount 18 gm nasonex nasal spray fast delivery, the bedside assistant must provide strong lateral and medial retraction with the Yankauer suctions in the depths of the incision as it is made. Horizontal incision at the anterior margin to allow the tumor to drop into the operative field. Establishing the depth of resection via the medial margin the specimen is removed and brought to the pathology department for orientation and margin analysis. If the margins are deemed close or positive, methylene blue is used to ink the region of concern on the patient, and re-resection is performed. Multiple Valsalva maneuvers are performed, and meticulous hemostasis is obtained with electrocautery and hemoclips, as needed. Arista absorbable hemostatic powder (Davol, Providence, Rhode Island) is applied to the resection bed. A nasogastric tube is placed under direct visualization and secured contralateral to the operative field for enteric access. If significant edema of the tongue is anticipated, patients may be kept intubated. This is important because irreversible compression and potential airway compromise may occur if the patient inadvertently bites a wire-reinforced tube while intubated. Undercutting the cancer at the horizontal anterior resection line instead of angling the instruments forward toward the hyoid bone 3. These arteries are usually exposed during the resection and should be ligated at multiple positions to prevent potential major postoperative hemorrhage. In addition, ligating the lingual artery in the neck at the time of staged or concurrent neck dissection should be performed. The resection is then performed from medial to lateral following the previously made horizontal incision. It is important to angle the instruments anteriorly in an imaginary line from the plane of the retractor blade to the hyoid because the tendency is to prematurely truncate the specimen here. Angling the vector of the resection appropriately facilitates a wide anterior margin of muscle. At the lateral aspect of the base of the tongue, the lingual artery and its dorsal lingual branch will be encountered at a depth of approximately 1 to 2 cm. If significant bleeding is encountered here from an inadvertently transected artery, external neck pressure at the greater cornu of the hyoid applied by the bedside assistant can be helpful. If the patient is felt to be at risk for postoperative airway compromise based on the extent of cancer resection or notable residual edema of the tongue or pharynx, he or she is typically kept intubated for 24 to 48 hours; otherwise he or she may be extubated. We had previously administered intravenous dexamethasone 6 mg every 6 to 8 hours until discharge followed by a Medrol Dose Pack upon discharge. However, we are shifting our protocol toward a single dose of intraoperative intravenous dexamethasone of 10 mg with subsequent steroids only if edema of the airway or tongue is noted. A prophylactic nasogastric feeding tube (Dobhoff) is placed while the patient is in the operating room for enteral access. Most patients are then started on a diet of clear liquids and advanced to a mechanical soft diet as tolerated. If swallowing assessment demonstrates significant dysphagia and/or aspiration, patients are discharged with tube feeds at home. If there is concern for malnutrition, a consultation with a nutritionist is obtained to guide appropriate caloric supplementation. Significant postoperative pain is expected after resection of the base of the tongue. Patients are started on a patient controlled analgesia pump and transitioned to oral narcotics as tolerated. Nonsteroidal anti-inflammatory drugs are typically avoided within the first 2 weeks post operative given the risk for bleeding. Patients are instructed to swish and spit with Peridex at least 4 times/day to maintain oral hygiene and increase comfort. Although these approaches were used by some, the majority of cancers of the base of the tongue were treated with combined chemotherapy and radiation. Transoral robotic versus open surgical approaches to oropharyngeal squamous cell carcinoma by human papillomavirus status. We routinely ligate the lingual, facial, and superior thyroid arteries preoperatively during the neck dissection. In our experience, this maneuver not only decreases intraoperative bleeding that can obscure visualization but also minimizes the risk for catastrophic bleeding. All vessels greater than 2 mm that are encountered during the resection are clipped in multiple locations. The lingual artery or its dorsal lingual branch is typically encountered at the lateral aspect of the resection. When identified, multiple clips are placed along the exposed portion of the artery. The danger with postoperative bleeding is the risk of aspiration and subsequent airway compromise rather than exsanguination. The patient is then brought to the operating room immediately to explore the wound and control the bleeding. Inadvertent injury to the teeth can occur from retractor manipulation during surgery. Care is taken to place a tooth guard to protect the maxillary dentition prior to transoral exposure. If teeth are loosened during the procedure, they are removed to prevent aspiration. In the event of chipped or avulsed teeth, the patient is referred for dental care. In the event of major postoperative hemorrhage, all of the following should be performed, except a. Positioning the pivot point of the camera arm at the level of the oral commissure d. Its axial plane defines the superior boundary of the oropharynx, incompletely separating it from the nasopharynx above. The soft palate comprises approximately one-third of the palate, with the more anteriorly positioned hard palate making up the remainder; the junction between the hard and soft palates also separates the oral cavity from the more posteriorly located oropharynx. In contrast to the hard palate, the soft palate is a mobile structure that is suspended from the posterior aspect of the hard palate via the palatine aponeurosis. The thicker, anterior portion of this tendon constitutes the majority of the anterior soft palate, whereas the posterior aspect of the soft palate is mainly comprised of muscle (levator veli palatine, tensor veli palatini, palatoglossus, palatopharyngeus). At its most posteroinferior extent, the free margin of the soft palate contains a conical muscular projection, the uvula. Functionally, the soft palate is a dynamic structure that is critical for velopharyngeal competence. Elevation of the soft palate puts it into contact with the posterior pharyngeal wall, sealing it off from the nasopharynx. In this way, function of the soft palate is critical to velopharyngeal competence. Importantly, benign tumors of the soft palate are extremely rare, and any soft palate lesion should be considered malignant until proven otherwise. Etiologic factors contributing to squamous cell carcinoma are alcohol and tobacco. Although the most common benign salivary gland tumor of the soft palate is pleomorphic adenoma, it is estimated that nearly 50% of minor salivary gland tumors in the oropharynx are malignant. The most common of these malignancies are adenoid cystic carcinoma and mucoepidermoid carcinoma. The soft palate is a dynamic structure whose function is critical for velopharyngeal competence. There is a high incidence of cervical lymph node metastasis associated with cancer of the soft palate (particularly with squamous cell carcinoma). Treatment of both necks is recommended for squamous cell cancers involving or approaching the midline. Reconstruction of the soft palate is complex, and reconstitution of a functional velopharyngeal sphincter is key. Symptoms range widely from asymptomatic to odynophagia, dysphagia, otalgia, airway compromise, oral bleeding, weight loss, changes in speech, and a mass in the neck. Early lesions are often found incidentally due to dental examinations, ill-fitting dentures, and office physical examinations but also may present at more advanced stages. Patients may have hearing loss due to middle ear effusion secondary to Eustachian tube dysfunction.