Cheap adcirca express
However erectile dysfunction specialist doctor generic 20 mg adcirca with amex, it is not useful for combining with penicillin in the treatment of enterococcal endocarditis. Sisomicin Introduced in 1980s, it is a natural aminoglycoside from Micromonospora inyoensis that is chemically and pharmacokinetically similar to gentamicin, but somewhat more potent on Pseudomonas, a few other gram-negative bacilli and haemolytic Streptococci. However, it is susceptible to aminoglycoside inactivating enzymes and offers no advantage in terms of ototoxicity and nephrotoxicity. It can be used interchangeably with gentamicin for the same purposes in the same doses. Amikacin It is a semisynthetic derivative of kanamycin to which it resembles in pharmacokinetics, dose and toxicity. The outstanding feature of amikacin is its resistance to bacterial aminoglycoside inactivating enzymes. Thus, it has the widest spectrum of activity, including many organisms resistant to other aminoglycosides. Netilmicin this semisynthetic derivative of gentamicin has a broader spectrum of activity than gentamicin. It is relatively resistant to many aminoglycoside inactivating enzymes and thus effective against some gentamicin-resistant strains. It is more active against Klebsiella, Enterobacter and Staphylococci, but less active against Ps. Pharmacokinetic characteristics and dosage of netilmicin are similar to gentamicin. Experimental studies have shown it to be less ototoxic than gentamicin and tobramycin, but clinical evidence is inconclusive: hearing loss occurs, though fewer cases of vestibular damage have been reported. Prolonged treatment can induce malabsorption syndrome with diarrhoea and steatorrhoea. It can decrease the absorption of digoxin and many other drugs, as well as bile acids. Small amounts that are absorbed from the gut or topical sites are excreted unchanged by kidney. This may accumulate in patients with renal insufficiency-cause further kidney damage and ototoxicity. Applied to serous cavities (peritoneum), it can cause apnoea due to muscle paralysing action. It is too toxic for systemic administration and is used topically on skin, eye, ear in the same manner as neomycin. However, because of toxic potential it is infrequently used for this purpose; Lactulose (see p. Paromomycin Chemically related to neomycin, this aminoglycoside antibiotic has pronounced activity against many protozoan parasites, including E. An oral formulation was marketed in many countries, including India, in the 1960s for treatment of intestinal amoebiasis and giardiasis, but was soon discontinued when metronidazole gained popularity. For its antibacterial activity in the gut, it can be used as an alternative to neomycin for hepatic encephalopathy. On the 4th day he developed fever, and the total leucocyte count rose to 14000/L, along with signs of chest infection. A sample of bronchial aspirate is sent for bacteriological tests, and it is decided to institute empirical treatment with cefotaxime and gentamicin. Antimicrobial spectrum It is narrow, includes mostly gram-positive and a few gramnegative bacteria, and overlaps considerably with that of penicillin G. In addition, Campylobacter, Legionella, Branhamella catarrhalis, Gardnerella vaginalis and Mycoplasma, that are not affected by penicillin, are highly sensitive to erythromycin. Resistance All cocci readily develop resistance to erythromycin, mostly by acquiring the capacity to pump it out. Alteration in the ribosomal binding site for erythromycin by a plasmid encoded methylase enzyme is an important mechanism of resistance in gram-positive bacteria. Change in the 50S ribosome by chromosomal mutation reducing macrolide binding affinity occurs in some gram-positive bacteria. Bacteria that develop resistance to erythromycin are cross resistant to other macrolides as well. Erythromycin is the first member discovered in the 1950s, Roxithromycin, Clarithromycin and Azithromycin are the later additions. Water solubility of erythromycin is limited, and the solution remains stable only when kept in cold. Mechanism of action Erythromycin is bacteriostatic at low but cidal (for certain bacteria only) at high concentrations. Sensitive gram-positive bacteria accumulate erythromycin intracellularly by active transport which is responsible for their high susceptibility to this antibiotic. Activity is enhanced several fold in alkaline medium, because the nonionized (penetrable) form of the drug is favoured at higher pH. To protect it from gastric acid, it is given as enteric coated tablets, from which absorption is incomplete and food delays absorption by retarding gastric emptying. Erythromycin is widely distributed in the body, enters cells and into abscesses, crosses serous membranes and placenta, but not bloodbrain barrier. Erythromycin stearate: blood levels produced are similar to those after erythromycin base. Erythromycin estolate (lauryl sulfate): it is relatively acid stable and better absorbed after oral administration. However, concentration of free and active drug in plasma may be the same as after administration of erythromycin base. Certain organisms hydrolyse it to liberate the free form intracellularly and are more susceptible to it. Erythromycin stimulates motilin (an upper gastrointestinal peptide hormone) receptors in the g. On the basis of this action erythromycin has been occasionally used to afford short-term symptomatic relief in diabetic gastroparesis. However, tolerance quickly develops to this action (probably due to receptor down-regulation) and undesirable alteration of bacterial flora limit use of erythromycin as a prokinetic agent. Other allergic manifestations are rare with erythromycin base or esters other than estolate. It clears on discontinuation of the drug, and is probably due to hypersensitivity to the estolate ester; erythromycin base or other esters can be given to these patients without recurrence. Though the estolate is acid stable, tasteless and better absorbed, it has been banned in some countries (but not in India). The clinically significant interactions are-rise in plasma levels of theophylline, carbamazepine, valproate, ergotamine and warfarin. Streptococcal pharyngitis, tonsillitis, mastoiditis and community acquired respiratory infections caused by pneumococci and H. It is an alternative drug for prophylaxis Adverse effects Erythromycin base is a remarkably safe drug, but side effects do occur. However, many bacteria resistant to penicillin are also resistant to erythromycin. Diphtheria: For acute stage as well as for carriers-7 day treatment is recommended. Syphilis and gonorrhoea: only if other alternative drugs, including tetracyclines also cannot be used: relapse rates are higher. However, effect on the symptoms depends on the stage of disease when treatment is started. Azithromycin, clarithromycin, and chloramphenicol are the alternative antimicrobials. Corticosteroids may reduce the duration of paroxysmal stage but increase the risk of superinfections and carrier stage; they should be reserved for severe cases only. Adrenergic 2 stimulants may reduce the severity of paroxysms, and are more useful in infants.
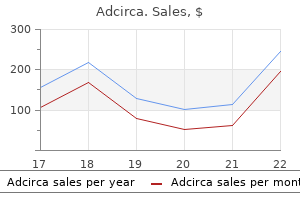
Adcirca 20 mg on-line
Buccally or orally administered phentolamine may have efficacy in some men with sexual dysfunction erectile dysfunction operations cheap adcirca online visa. Sympathomimetics are frequently administered with local anesthetics to slow the removal of the anesthetic by causing vasoconstriction. Thus, phentolamine should be used with caution in patients with a history of peptic ulcer. Additional Adrenergic Receptor Antagonists Ergot Alkaloids the ergot alkaloids were the first adrenergic receptor antagonists to be discovered. Some of the adverse effects of indoramin include sedation, dry mouth, and failure of ejaculation. Propranolol is a competitive receptor antagonist and remains the prototype to which other antagonists are compared. Propranolol is a nonselective adrenergic receptor antagonist with equal affinity for 1 and 2 adrenergic receptors. Agents such as metoprolol, atenolol, acebutolol, bisoprolol, and esmolol have somewhat greater affinity for 1 than for 2 receptors; these are examples of 1-selective antagonists, even though the selectivity is not absolute. These include celiprolol, nebivolol, nipradilol, carteolol, betaxolol, bopindolol, and bevantolol (Toda, 2003). For example, receptor blockade has relatively little effect on the normal heart of an individual at rest but has profound effects when sympathetic control of the heart is dominant, as during exercise or stress. These last drugs have additional cardiovascular properties (especially vasodilation) that seem unrelated to blockade. Conversely, receptor antagonists slow the heart rate and decrease myocardial contractility, if there are sympathetic stimuli to antagonize. However, when the sympathetic nervous system is activated, as during exercise or stress, receptor antagonists attenuate the expected rise in heart rate. Although it had been thought that these effects were due exclusively to blockade of 1 receptors, 2 receptors likely also regulate heart rate in humans (Altschuld and Billman, 2000; Brodde and Michel, 1999). Signal transduction for 3 receptors is complex and includes not only Gs but also Gi/Go; stimulation of cardiac 3 receptors inhibits cardiac contraction and relaxation. The physiological role of 3 receptors in the heart remains to be established (Morimoto et al. The cardiovascular effects of receptor antagonists are most evident during dynamic exercise. Exercise performance may be impaired to a lesser extent by 1 selective agents than by nonselective antagonists. By increasing heart rate, contractility, and systolic pressure, catecholamines increase myocardial O2 demand. Receptor antagonists decrease the effects of catecholamines on the determinants of myocardial O2 consumption. However, these agents may tend to increase the requirement for O2 by increasing end-diastolic pressure and systolic ejection period. The release of renin from the juxtaglomerular cells is stimulated by the sympathetic nervous system by means of 1 receptors, and this effect is blocked by receptor antagonists (see Chapter 26). Some investigators have found that the antihypertensive effect of blockade is most marked in patients with elevated concentrations of plasma renin, compared to patients with low or normal concentrations of renin. However, receptor antagonists are effective even in patients with low plasma renin. The mechanism for this effect is not known, but this delayed fall in peripheral vascular resistance in the face of a persistent reduction of cardiac output appears to account for much of the antihypertensive effect of these drugs. Some receptor antagonists have additional effects that may contribute to their capacity to lower blood pressure. These mechanisms appear to contribute to the antihypertensive effects by enhancing hypotension, increasing peripheral blood flow, and decreasing afterload. This is particularly significant in patients with pheochromocytoma, in whom receptor antagonists should be used only after adequate receptor blockade has been established. Although 1-selective antagonists or antagonists with intrinsic sympathomimetic activity are less likely than propranolol to increase airway resistance in patients with asthma, these drugs should be used only with great caution, if at all, in patients with bronchospastic diseases. If such a drug is indicated, a 1-selective antagonist is preferred because these drugs are less likely to delay recovery from hypoglycemia (DiBari et al. This increased flux of fatty acids is an important source of energy for exercising muscle. Receptor antagonists can attenuate the release of free fatty acids from adipose tissue. In contrast, 1-selective antagonists, including celiprolol, carteolol, nebivolol, carvedilol, and bevantolol, reportedly improve the serum lipid profile of dyslipidemic patients. While drugs such as propranolol and atenolol increase triglycerides, plasma triglycerides are reduced with chronic celiprolol, carvedilol, and carteolol (Toda, 2003). In addition, it may be necessary to use receptor antagonists in conjunction with other drugs. Receptor blockade may cause or exacerbate heart failure in patients with compensated heart failure, acute myocardial infarction, or cardiomegaly. Nonetheless, there is convincing evidence that chronic administration of receptor antagonists is efficacious in prolonging life in the therapy of heart failure in selected patients (discussed in Chapter 29). Symptoms of peripheral vascular disease may occasionally worsen, or Raynaud phenomenon may develop. There is enhanced sensitivity to receptor agonists in patients who have undergone long-term treatment with certain receptor antagonists after the blocker is withdrawn abruptly. The number of receptors on circulating lymphocytes is increased in subjects who have received propranolol for long periods; pindolol has the opposite effect. These receptors are particularly important for promoting bronchodilation in patients with bronchospastic disease, and 2 blockade may cause a life-threatening increase in airway resistance in such patients. Drugs with selectivity for 1 receptors or those with intrinsic sympathomimetic activity at 2 receptors seem less likely to induce bronchospasm. Although experience with the use of adrenergic receptor antagonists in pregnancy is increasing, information about the safety of these drugs during pregnancy still is limited. The manifestations of poisoning with receptor antagonists depend on the pharmacological properties of the ingested drug, particularly its 1 selectivity, intrinsic sympathomimetic activity, and membrane-stabilizing properties. Significant bradycardia should be treated initially with atropine, but a cardiac pacemaker often is required. Selection of the most appropriate drug for an individual patient should be based on pharmacokinetic and pharmacodynamic differences among the drugs, cost, and whether there are concurrent medical problems. Although no clinical advantage of receptor antagonists with intrinsic sympathomimetic activity has been clearly established, such drugs may be preferable in patients with bradycardia. Drugs such as phenytoin, rifampin, and phenobarbital, as well as smoking, induce hepatic biotransformation enzymes and may decrease plasma concentrations of receptor antagonists that are metabolized extensively. However, the antihypertensive effects of receptor antagonists can be opposed by indomethacin and other nonsteroidal anti-inflammatory drugs (see Chapter 38). Receptor antagonists are used in the treatment of hypertrophic obstructive cardiomyopathy, relieving angina, palpitations, and syncope in patients with this disorder. Efficacy probably is related to partial relief of the pressure gradient along the outflow tract. Nitroprusside is an alternative, but when given in the absence of receptor blockade, it causes an undesirable reflex tachycardia. The receptor antagonists are used in the treatment of chronic open-angle glaucoma (see Chapter 69). These agents decrease the production of aqueous humor, which appears to be the mechanism for their clinical effectiveness. In addition, propranolol inhibits the peripheral conversion of thyroxine to triiodothyronine, an effect that may be independent of receptor blockade (see Chapter 43). Propranolol is highly lipophilic and almost completely absorbed after oral administration. The bioavailability of propranolol may be increased by the concomitant ingestion of food and during long-term administration of the drug.
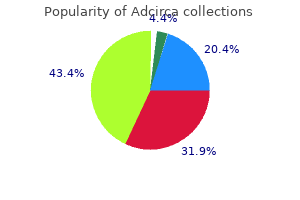
Purchase adcirca australia
The initial concern that aplastic anemia might be a frequent complication of long-term therapy with carbamazepine has not materialized erectile dysfunction remedy purchase adcirca 20 mg overnight delivery. In most cases, the administration of multiple drugs or the presence of another underlying disease has made it difficult to establish a causal relationship. Concurrent administration of carbamazepine may lower concentrations of valproate, lamotrigine, tiagabine, and topiramate. Carbamazepine reduces both the plasma concentration and the therapeutic effect of haloperidol. The metabolism of carbamazepine may be inhibited by propoxyphene, erythromycin, cimetidine, fluoxetine, and isoniazid. Eslicarbazepine competitively inhibits fast voltage-gated sodium channels, stabilizing the inactivated state and the sodium-dependent release of neurotransmitters. Succinimides Ethosuximide Ethosuximide is a primary agent for the treatment of generalized absence seizures. The thalamus plays an important role in generation of 3-Hz spike-and-wave rhythms typical of absence seizures (Huguenard and McCormick, 2007). Ethosuximide reduces this current without modifying the voltage dependence of steady-state inactivation or the time course of recovery from inactivation. Absorption of ethosuximide appears to be complete, with peak Cp occurring within about 3 h after a single oral dose. The major metabolite, the hydroxyethyl derivative, accounts for about 40% of ethosuximide metabolism, is inactive, and is excreted as such and as the glucuronide in the urine. The plasma t1/2 of ethosuximide averages between 40 and 50 h in adults and about 30 h in children. Oxcarbazepine (10,11-dihydro-10-oxocarbamazepine) is a keto analogue of carbamazepine and is a prodrug that is rapidly converted to its metabolite, eslicarbazepine. Oxcarbazepine has a mechanism of action similar to that of carbamazepine but is a less-potent enzyme inducer than carbamazepine. Although most adverse effects are similar to that with carbamazepine, hyponatremia may occur more commonly with oxcarbazepine than with carbamazepine. Plasma Drug Concentrations During long-term therapy, the plasma concentration of ethosuximide averages about 2 g/mL per daily dose of 1 mg/kg. Therapeutic Uses Ethosuximide is effective against absence seizures, but not tonic-clonic seizures. Divided dosage is required occasionally to prevent nausea or drowsiness associated with once-daily dosing. The leukopenia may be transient despite continuation of the drug, but several deaths have resulted from bone marrow depression. Other Antiseizure Drugs Acetazolamide Acetazolamide, the prototype for the carbonic anhydrase inhibitors, is discussed in Chapter 25. Although it is sometimes effective against absence seizures, its usefulness is limited by the rapid development of tolerance. Ezogabine is rapidly absorbed after oral administration, and absorption is not affected by food. Clinical studies demonstrate the efficacy of felbamate in patients with poorly controlled focal and secondarily generalized seizures (Sachdeo et al. Interestingly, gabapentin also inhibits clonic seizures induced by pentylenetetrazol. Analgesic efficacy of pregabalin is eliminated in these mice; whether the anticonvulsant effects of pregabalin are also eliminated was not reported. Blue pigmentation of skin and lips occurs in as many as one-third of patients maintained on long-term ezogabine therapy. These compounds are not bound to plasma proteins and are excreted unchanged, mainly in the urine. It is also indicated for the management of fibromyalgia and the neuropathic pain associated diabetic peripheral neuropathy, postherpetic neuralgia, or spinal cord injury. Gabapentin monotherapy (900 or 1800 mg/d) is equivalent to carbamazepine (600 mg/d) for newly diagnosed focal or generalized epilepsy (Chadwick et al. In comparison, pregabalin is generally initiated at 50 mg three times a day (150 mg/day) and increase within 1 week to 300 mg/day based on efficacy and tolerability. No major adverse effects have been reported, although minor adverse effects include headache, dizziness, double vision, nausea, vomiting, fatigue, tremor, loss of balance, and somnolence. Lamotrigine suppresses tonic hind limb extension in the maximal electroshock model and focal and secondarily generalized seizures in the kindling model, but does not inhibit clonic motor seizures induced by pentylenetetrazol. One possibility, supported by basic research, is that lamotrigine inhibits synaptic release of glutamate by acting at Na+ channels themselves. Conversely, addition of valproate markedly increases plasma concentrations of lamotrigine, likely by inhibiting glucuronidation. These effects usually are mild to moderate in severity but resolve within 2 weeks of onset during continued treatment. Lennox-Gastaut syndrome is a disorder of childhood characterized by multiple seizure types, mental retardation, and refractoriness to antiseizure medication. A few cases of Stevens-Johnson syndrome and disseminated intravascular coagulation have been reported. The recommended starting dose for brivaracetam is 50 mg twice daily, which may be adjusted to either 25 mg twice daily or 100 mg twice daily, based on patient response and tolerability. The mechanism by which levetiracetam exerts these antiseizure effects is not fully understood. Levetiracetam is rapidly and almost completely absorbed after oral administration and is not bound to plasma proteins. Ninety-five percent of the drug and its inactive metabolite are excreted in the urine, 65% of which is unchanged drug; 24% of the drug is metabolized by hydrolysis of the acetamide group. In patients with hepatic insufficiency, dose adjustment may be required with brivaracetam to 25 mg twice daily and a maximal dosage of 75 mg twice daily. Perampanel seems to have a greater inhibitory effect on seizure propagation than on seizure initiation (Hanada et al. For example, perampanel may decrease the effectiveness of progesterone-containing hormone contraceptives, carbamazepine, clobazam, lamotrigine, and valproate, but it may increase the level of oxcarbazepine. Furthermore, serum perampanel may be decreased when taken with carbamazepine, oxcarbazepine, and topiramate. Rare, but serious, adverse behavioral reactions, including hostility, aggression, and suicidal thoughts and behaviors, independent of clinical history of psychiatric disorder, have also been reported. Mechanism of Action Rufinamide prolongs slow inactivation of voltage-gated Na+ channels and limits sustained repetitive firing, the firing pattern characteristic of focal seizures.
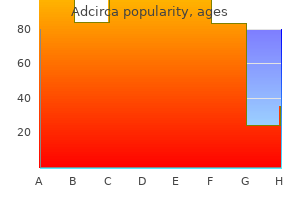
Adcirca 20 mg on line
Antimicrobials are regularly useful in: (i) Cholera: Though only fluid replacement is life saving sudden erectile dysfunction causes adcirca 20 mg with mastercard, tetracyclines reduce stool volume to nearly half. The drug of choice for this superinfection is metronidazole, while vancomycin given orally is an alternative. Probiotics in diarrhoea these are microbial cell preparations, either live cultures or lyophillised powders, that are intended to restore and maintain healthy gut flora or have other health benefits. Diarrhoeal illnesses and antibiotic use are associated with alteration in the population, composition and balance of gut microflora. Recolonization of the gut by nonpathogenic, mostly lactic acid forming bacteria and yeast is believed to help restore this balance. They also note that most of the randomised placebo controlled trials have been carried out in healthcare setting in developed countries, while data from community based studies carried out in resourcepoor countries is minimal. Several probiotic strains, either alone or in combination, have been used in different studies, but the protective effect has been more or less similar, though collation of data is difficult. While probiotics appear to be useful adjuncts to conventional therapy of acute infectious diarrhoea, and are loudly promoted as well as frequently prescribed, convincing evidence of their efficacy is lacking. This prevents them from being accepted as a standard component of diarrhoea therapy. Stronger evidence of efficacy has emerged against antibiotic-associated diarrhoea, but there is no justification yet for routine use of probiotics along with antibiotics. Natural curd/yogurt is an abundant source of lactic acid producing organisms, which can serve as probiotic. It is idiopathic, but appears to have an important immune component triggered by a variety of factors. It may remain restricted to the rectum or extend proximally in a contiguous manner to variable extent upto caecum. Majority of patients have ileocaecal disease upto ascending colon, but in some it may be restricted to the small intestine, while in others to the colon. Because the lesions are transmural, complications like perforation, abscess, fistula, strictures, etc. The former exerts a local antiinflammatory effect, the mechanism of which is not clear. Given during active phase of the disease it reduces number of stools, abdominal cramps and fever, but is less effective than corticosteroids; may be employed for mild to moderate exacerbation. The beneficial effect of sulfasalazine is clearly not due to any antibacterial action (bowel flora remains largely unaffected). However, most of the released sulfapyridine is absorbed in the colon and is responsible for adverse effects like rashes, fever, joint pain, haemolysis and blood dyscrasias. Nausea, vomiting, headache, malaise and anaemia are other frequent dose related side effects. Sufasalazine has also been used as a disease modifying drug in rheumatoid arthritis. The absorbed sulfapyridine moiety appears to be responsible for the therapeutic effect (see p. Interaction with coumarins, furosemide, spironolactone, methotrexate and rifampicin are possible. However, it often aggravates diarrhoea initially by decreasing transit time through the bowels. The pattern of release over the length of jejunum, ileum and colon differs among the different formulations. Side effects noted are nausea, diarrhoea, abdominal pain and headache, but are mild and less frequent. In more severe disease with extraintestinal manifestations and for rapid relief therapy may be initiated with i. Corticosteroids are generally used for short term, and discontinued after remission is induced. However, risks of chronic immunosuppression must be weighed in each patient before instituting therapy with these drugs. Because of long latency of response, they are not suitable for acute flareups of the disease, but have good remission maintaining and steroidsparing property. Although, azathioprine has its own adverse effect potential, the same is rated lower than that of prolonged steroid therapy. Thus, it has a limited role in severe CrD and in patients not responsive to or not tolerating azathioprine. Infliximab produces substantial toxicity, including acute reactions, formation of antibodies and lowering of resistance to infections. Absorbants these are colloidal bulk forming substances like ispaghula, methyl cellulose, carboxy methyl cellulose which absorb water and swell. They modify the consistency and frequency of stools and give an impression of improvement, but do not reduce the water and electrolyte loss. Adsorbants like kaolin, pectin, attapulgite are believed to adsorb bacterial toxins in the gut and coat/protect the mucosa. They were ones very popular ingredients of diarrhoea remedies, but are now banned in India, because there is no objective proof of their efficacy. Anticholinergics Atropinic drugs can reduce bowel motility and secretion, but have poor efficacy in secretory diarrhoeas. They may benefit nervous/drug (neostigmine, metoclopramide) induced diarrhoeas and provide some symptomatic relief in dysenteries, diverticulitis. Opioids In addition to their well recognized antimotility action, opioids reduce intestinal secretion. The receptors are believed to promote absorption and inhibit secretion, while the receptors enhance absorption and decrease propulsive movements. Overall they increase resistance to luminal transit and allow more time for the absorptive processes. The antidiarrhoeal effect is attributed primarily to its peripheral action on small intestine and colon. Due to its abuse potential and availability of loperamide, codeine is seldom, if ever, used for diarrhoea. It is a synthetic opioid, chemically related to pethidine; used exclusively as constipating agent; action is similar to codeine. Atropine is added in subpharmacological dose to discourage abuse by taking several tablets. Abuse liability is rated low, and overdose will produce disturbing atropinic side effects. It has caused respiratory depression, paralytic ileus and toxic megacolon in children. In addition to its opiate like action on motility, loperamide also inhibits secretion. Antimotility drugs these are opioid drugs which increase small bowel tone and segmenting activity, reduce propulsive movements and diminish intestinal secretions while enhancing absorption. Paralytic ileus, toxic megacolon with abdominal distension is a serious complication in young children-fatalities have occurred, probably due to absorption of toxins from the intestines. However, it appears to be the most effective and most suitable of the antimotility antidiarrhoeal drugs. Containing phthalylsulfathiazole, succinylsulfathiazole, sulfaguanidine, neomycin, streptomycin, dihydrostreptomycin. For pediatric use containing diphenoxylate, loperamide, atropine, belladonna, hyosciamine, halogenated hydroxyquinolines. The stools are relatively small volume, liquid but not watery, frothy and are preceded by griping pain in abdomen.
Order adcirca 20 mg without prescription
However does erectile dysfunction cause low libido adcirca 20 mg on-line, 1 receptors exist in most regions of the heart, and their activation prolongs the refractory period and strengthens myocardial contractions. Premature ventricular contractions can appear, which may be followed by multifocal ventricular tachycardia or ventricular fibrillation. Acute toxicity is associated with contraction band necrosis and other pathological changes. Intestinal tone and the frequency and amplitude of spontaneous contractions are reduced. The stomach usually is relaxed and the pyloric and ileocecal sphincters are contracted, but these effects depend on the preexisting tone of the muscle. Inhibition of mast cell secretion is mediated by 2 receptors, while the effects on the mucosa are mediated by receptors; however, other drugs, such as glucocorticoids and leukotriene receptor antagonists, have much more profound anti-inflammatory effects in asthma (Chapters 40 and 46). Glucagon secretion is enhanced via activation of receptors of the cells of pancreatic islets. The result is activation of triglyceride lipase, which accelerates the triglyceride breakdown to free fatty acids and glycerol. In apparent contrast to the effects of receptor activation at presynaptic nerve terminals in the autonomic nervous system (2 receptors), stimulation of receptors causes a more rapid increase in transmitter release from the somatic motor neuron, perhaps as a result of enhanced influx of Ca2+. Epinephrine promotes a fall in plasma K+, largely due to stimulation of K+ uptake into cells, particularly skeletal muscle, due to activation of 2 receptors. These receptors have been exploited in the management of hyperkalemic familial periodic paralysis, which is characterized by episodic flaccid paralysis, hyperkalemia, and depolarization of skeletal muscle. The mechanism of this injury is not yet clear, but and receptor antagonists and Ca2+ channel blockers may afford substantial protection against the damage. It also is used as a topical hemostatic agent on bleeding surfaces, such as in the mouth or in bleeding peptic ulcers during endoscopy of the stomach and duodenum. Norepinephrine Norepinephrine (levarterenol, l-noradrenaline, l-[3,4-dihydroxyphenyl]-aminoethanol) is a major chemical mediator liberated by mammalian postganglionic sympathetic nerves. Cardiac output is unchanged or decreased, and total peripheral resistance is raised. Absorption from subcutaneous tissues occurs relatively slowly because of local vasoconstriction. Epinephrine is available in a variety of formulations geared for different clinical indications and routes of administration, including self-administration for anaphylactic reactions. The intravenous route is used cautiously if an immediate and reliable effect is mandatory. If the solution is given by vein, it must be adequately diluted and injected very slowly. Blood pressure must be determined frequently during the infusion, particularly during adjustment of the rate of the infusion. Precautions, Adverse Reactions, and Contraindications Therapeutic Uses Norepinephrine is used as a vasoconstrictor to raise or support blood pressure under certain intensive care conditions (discussed further in this chapter). Droxidopa can cross the blood-brain barrier, presumably as the substrate of an amino acid transporter. Rarely, gangrene of the fingers or toes has followed prolonged infusion of the drug. In the periphery, it is synthesized in epithelial cells of the proximal tubule and is thought to exert local diuretic and natriuretic effects. The drug also may improve physiological parameters in the treatment of cardiogenic and septic shock. Reduction in urine flow, tachycardia, or the development of arrhythmias may be indications to slow or terminate the infusion. It dilates a variety of blood vessels, including coronary arteries, afferent and efferent arterioles in the kidney, and mesenteric arteries (Murphy et al. Less than 6% of an orally administered dose is absorbed because of extensive first-pass formation of sulfate, methyl, and glucuronide conjugates. Adverse effects are related to the vasodilation and include headache, flushing, dizziness, and tachycardia or bradycardia. It has favorable hemodynamic actions in patients with severe congestive heart failure, sepsis, and shock. In patients with low cardiac output, dopexamine infusion significantly increases stroke volume with a decrease in systemic vascular resistance. Cardiac ischemia and arrhythmias may occur, particularly in patients with underlying coronary artery disease. Receptor agonists may be used to stimulate the rate and force of cardiac contraction. Systolic blood pressure may remain unchanged or rise, although mean arterial pressure typically falls. Cardiac output is increased because of the positive inotropic and chronotropic effects of the drug in the face of diminished peripheral vascular resistance. After administration of receptor antagonists, infusion of dobutamine fails to increase cardiac output, but total peripheral resistance increases, confirming that dobutamine has modest direct effects on adrenergic receptors in the vasculature. Dobutamine has a t1/2 of about 2 min; the major metabolites are conjugates of dobutamine and 3-O-methyldobutamine. Steady-state concentrations generally are achieved within 10 min of initiation of the infusion by calibrated infusion pump. An infusion of dobutamine in combination with echocardiography is useful in the noninvasive assessment of patients with coronary artery disease. Patients with 200 a history of hypertension may exhibit an exaggerated pressor response more frequently. Dobutamine may increase the size of a myocardial infarct by increasing myocardial O2 demand, a property common to inotropic agents. This selectivity, however, is not absolute and is lost at high concentrations of these drugs. This approach typically leads to effective activation of 2 receptors in the bronchi but very low systemic drug concentrations. Consequently, there is less potential to activate cardiac 1 or 2 receptors or to stimulate 2 receptors in skeletal muscle, which can cause tremor and thereby limit oral therapy. This, in turn, depends on the size of the particles in the aerosol and respiratory parameters such as inspiratory flow rate, tidal volume, breath-holding time, and airway diameter. Only about 10% of an inhaled dose actually enters the lungs; much of the remainder is swallowed and ultimately may be absorbed. Successful aerosol therapy requires that each patient master the technique of drug administration. Receptor agonists also may suppress the release of leukotrienes and histamine from mast cells in lung tissue, enhance mucociliary function, decrease microvascular permeability, and possibly inhibit phospholipase A2. Airway inflammation also contributes airway hyperresponsiveness; consequently, the use of anti-inflammatory drugs such as inhaled steroids has primary importance. Side effects are similar to the short- and intermediate-acting sympathomimetic bronchodilators. It can be administered by inhalation or orally for the symptomatic relief of bronchospasm. In general, levalbuterol has similar pharmacokinetic and pharmacodynamics properties as albuterol. A possible association of fenoterol use with increased deaths from asthma, although controversial (Suissa and Ernst, 1997), has led to its withdrawal from the market. Metaproterenol (called orciprenaline in Europe), along Short-Acting 2 Adrenergic Agonists Procaterol. Salmeterol generally is well tolerated but has the potential to increase heart rate and plasma glucose concentration, to produce tremors, and to decrease plasma K+ concentration through effects on extrapulmonary 2 receptors.
Order adcirca 20 mg on line
Generally vacuum pump for erectile dysfunction in dubai discount adcirca 20 mg online, tremor is benefited more than rigidity; hypokinesia is affected the least. In others, they can be combined with levodopa in an attempt to lower levodopa dose. Anticholinergics are the only drugs effective in drug (phenothiazine) induced parkinsonism. Impairment of memory, organic confusional states and blurred vision are more common in the elderly. The antihistaminics are less efficacious than anticholinergics, but are better tolerated by older patients. There is no proof yet for such a happening, and controlled prospective studies have not detected any difference in the progression of disease due to levodopa therapy. However, appearance of dyskinesias is related to dose and duration of levodopa therapy. Initially, when disease is mild, only anticholinergics or selegiline may be sufficient. However, anticholinergics are often not tolerated by elderly patients, especially males. Combination of levodopa with a decarboxylase inhibitor is the standard therapy, and has replaced levodopa alone. Dyskinesias appear, mostly coinciding with the peak of levodopa action after each dose. Combination of levodopa with decarboxylase inhibitor increases efficacy and reduces early but not late complications. Levodopa alone is now used only in those patients who develop intolerable dyskinesias with a levodopa-decarboxylase inhibitor combination. He now suffers stiffness, shaking and difficulty in getting up from bed in the morning. During the past 60 years psychiatric treatment has witnessed major changes due to advent of drugs which can have specific salutary effect in mental illnesses. The trend has turned from custodial care towards restoring the individual patient to his place in the community. All that could be done before 1952 was to dope and quieten agitated and violent patients. Though it is a powerful pharmacological tool to study monoaminergic systems in brain and periphery, its clinical use in psychiatry lasted only few years. Meprobamate (1954) aroused the hope that anxiety could be tackled without producing marked sedation. This goal has been realised more completely by the development of Chlordiazepoxide (1957) and other benzodiazepines in the 1960s. Interestingly some antiepileptics like carbamazepine, valproate and lamotrigine as well as some atypical antipsychotics, etc. Nevertheless, broad divisions have to be made, primarily on the basis of predominant manifestations, to guide the use of drugs. It is important to make an attempt to characterise the primary abnormality, because specific drugs are now available for most categories. Principal types are: Psychoses these are severe psychiatric illness with serious distortion of thought, behaviour, capacity to recognise reality and of perception (delusions and hallucinations). There is inexplicable misperception and misevaluation; the patient is unable to meet the ordinary demands of life. Prominent features are confusion, disorientation, defective memory, disorganized thought and behaviour. A common form of mood disorder is bipolar disorder with cyclically alternating manic and depressive phases. The relapsing mood disorder may also be unipolar (mania or depression) with waxing and waning course. Neuroses these are less serious; ability to comprehend reality is not lost, though the patient may undergo extreme suffering. Depending on the predominant feature, it may be labelled as: (a) Anxiety An unpleasant emotional state associated with uneasiness, worry, tension and concern for the future. However, it has been interpreted differently by different people; some extend it to cover both chlorpromazine-like and antianxiety drugs, others feel that it should be restricted to the antianxiety drugs only. Phenothiazines Aliphatic side chain: Chlorpromazine Triflupromazine Piperidine side chain: Thioridazine Piperazine side chain: Trifluoperazine Fluphenazine Butyrophenones Haloperidol Trifluperidol Penfluridol Thioxanthenes Flupenthixol Other heterocyclics Pimozide, Loxapine Atypical antipsychotics Clozapine Aripiprazole Risperidone Ziprasidone Olanzapine Amisulpiride Quetiapine Zotepine Pathophysiology of mental illness is not clear, though some ideas have been formed. Antipsychotic (neuroleptic, ataractic, major tranquillizer) useful in all types of functional psychosis, especially schizophrenia. Antimanic (mood stabiliser) used to control mania and to break into cyclic affective disorders. Antidepressants used for minor as well as major depressive illness, phobic states, obsessive-compulsive behaviour, and certain anxiety disorders. Antianxiety (anxiolytic-sedative, minor tranquillizer) used for anxiety and phobic states. Spontaneous movements are minimized but slurring of speech, ataxia or motor incoordination does not occur. All phenothiazines, thioxanthenes and butyrophenones have the same antipsychotic efficacy, but potency differs in terms of equieffective doses. The sedative effect is produced promptly, while antipsychotic effect takes weeks to develop. Performance and intelligence are relatively unaffected, but vigilance is impaired. Extrapyramidal motor disturbances (see adverse effects) are intimately linked to the antipsychotic effect, but are more prominent in the high potency compounds and least in thioridazine, clozapine and other atypical antipsychotics. Chlorpromazine lowers seizure threshold and can precipitate fits in untreated epileptics. Temperature control is knocked off at relatively higher doses rendering the individual poikilothermic. The medullary respiratory and other vital centres are not affected, except at very high doses. This action has shown good correlation with the antipsychotic potency of different compounds. In animals, a state of rigidity and immobility (catalepsy) is produced which resembles the bradykinesia seen clinically. Antipsychotic potency has shown good correlation with their capacity to bind to D2 receptor. Phenothiazines and thioxanthenes also block D1, D3 and D4 receptors, but there is no correlation of such blockade with their antipsychotic potency. Not withstanding the above, reduction of dopaminergic neurotransmission is the major mechanism of antipsychotic action. Thus, antipsychotic property may depend on a specific profile of action of the drugs on several neurotransmitter receptors. The hypotensive action is more marked after parenteral administration and roughly parallels the adrenergic blocking potency. Hypotension is not prominent in psychotic patients, but is accentuated by hypovolemia. Skeletal muscle Neuroleptics have no direct effect on muscle fibres or neuromuscular transmission. However, they reduce certain types of spasticity: the site of action being in the basal ganglia or medulla oblongata.
Trusted 20 mg adcirca
In clinical trials the efficacy of ulipristal (30 mg) as emergency contraceptive has been rated equal to that of levonorgestrel (1 erectile dysfunction at the age of 18 adcirca 20 mg fast delivery. Thus, it may have an advantage, if the woman misses to take the drug within 3 days. The antiglucocorticoid activity of ulipristal is weaker than that of mifepristone. Onapristone (a pure progesterone antagonist) and Gestinone (more efficacious in endometriosis) are the other antiprogestins. Combined pill It contains an estrogen and a progestin in fixed dose for all the days of a treatment cycle (monophasic). The progestin is a 19-nortestosterone because these have potent antiovulatory action. While both estrogens and progestins synergise to inhibit ovulation, the progestin ensures prompt bleeding at the end of a cycle and blocks the risk of developing endometrial carcinoma due to the estrogen. Phased pill Triphasic regimens have been introduced to permit reduction in total steroid dose without compromising efficacy by mimicking the normal hormonal pattern in a menstrual cycle. Phasic pills are particularly recommended for women over 35 years of age and for those with no withdrawal bleeding or breakthrough bleeding while on monophasic pill, or when other risk factors are present. Because of our alarming population trends, antifertility drugs are the need of the day. In developing countries particularly, the mortality rate has declined and birth rate has increased due to urbanization. In the earlier part of 20th century, methods of contraception used (condoms, diaphragms, spermicidal creams, foam tablets, etc. Rock and Pincus (1955) announced the successful use of an oral progestin for contraception, separating fertility control from coitus. It was soon discovered that addition of a small quantity of an estrogen enhanced their efficacy; combined pills have become the most popular method of contraception, particularly because the hormone content of the pills has been reduced, minimizing the potential harm and affording other health benefits. With these drugs, fertility can be suppressed at will, for as long as desired, with almost 100% confidence and complete return of fertility on discontinuation. A variety of oral and parenteral preparations are now available offering individual choices. Progestin-only pill (Minipill) It has been devised to eliminate the estrogen, because many of the long-term risks have been ascribed to this component. A low-dose progestin-only pill is an alternative for women in whom an estrogen is contraindicated. Emergency (postcoital) pill these are for use in a woman not taking any contraceptive who had a sexual intercourse risking unwanted pregnancy. Another antiprogestin that has been used, particularly in Europe and China, with high success rate and few side effects is- Mifepristone 600 mg single dose taken within 72 hours of intercourse. Emergency postcoital contraception should be reserved for unexpected or accidental exposure (rape, condom rupture) only, because all emergency regimens have higher failure rate and side effects than regular low-dose combined pill. Injectable these have been developed to obviate the need for daily ingestion of pills. Their major limitations are: (a) Animal data has indicated carcinogenic potential, but there is no proof from human studies despite >30 years of experience. In India approval has been granted for use only under close supervision, but not on mass scale under the National Programme. This may also produce menopause-like symptoms (hot flushes, vaginal dryness, reduced libido). All fixed dose combination injectable preparations of synthetic estrogens and progestins are not allowed in India and discontinued in most countries. They consist of either- (a) Biodegradable polymeric matrices-do not need to be removed on expiry. Inhibition of Gn release from pituitary by reinforcement of normal feedback inhibition. As a result, follicles fail to develop and fail to rupture- ovulation does not occur. Thick cervical mucus secretion hostile to sperm penetration is evoked by progestin action. Even if ovulation and fertilization occur, the blastocyst may fail to implant because endometrium is either hyperproliferative or hypersecretory or atrophic and in any case out of phase with fertilization-not suitable for nidation. This action appears to be the most important in case of minipills and postcoital pill. This action is uncertain but probably contributes to the efficacy of minipills and postcoital pill. The postcoital pill may dislodge a just implanted blastocyst or may interfere with fertilization/implantation. If a woman on combined pills misses to take a tablet, she should be advised to take two tablets the next day and continue as usual. If more than 2 tablets are missed, then the course should be interrupted, an alternative method of contraception used and next course started on the 5th day of bleeding. If pregnancy occurs during use of hormonal contraceptives-it should be terminated by suction-aspiration, because the risk of malformations, genital carcinoma in female offspring and undescended testes in male offspring is increased. If breakthrough bleeding occurs-switch over to a pill containing higher estrogen dose. In women with contraindications for estrogen (see below), a progestin only contraceptive may be used. The adverse effects are dose dependent; most of the past data with high-dose preparations cannot be directly extrapolated to the present-day lowdose preparations which carry relatively minor risk. The following applies primarily to combined oral pill which has been most extensively used. Prolonged amenorrhoea or cycle disruption occurs in few women taking injectables or minipill. Weight gain, acne and increased body hair may be noted due to androgenic action of older 19-nortestosterone progestins. Chloasma: pigmentation of cheeks, nose and forehead, similar to that occurring in pregnancy. Carbohydrate intolerance and precipitation of diabetes in few subjects taking high dose preparations; but this is unlikely with the present pills. Mood swings, abdominal distention are occasional; especially reported with progesterone only contraceptives. Leg vein thrombosis and pulmonary embolism: the older preparations increased the incidence of venous thromboembolism, but this is found to be only marginal with the newer reduced steroid content pills.