Order alesse amex
Acid demineralizes and destroys tooth enamel birth control 10 years generic 0.18 mg alesse, dentin, and cementum causing caries. Screening for Lead Exposure Risk assessment screening for lead exposure should be performed at 6 months, 9 months, 1 year, and then annually through age 6 years. Lead levels should be performed at 12 and 24 months, and when a patient is at risk. History Evaluate for risk factors including: History of living in a home built before 1978. Family member occupational exposures such as lead smelting, or patient hobbies such as pottery, fishing, or hunting. Deficiency of iron, zinc, protein, calcium, or vitamin C, which can result in increased absorption of ingested lead. When present, symptoms include headaches, abdominal colic, constipation, lethargy, growth failure, weight loss, vomiting, ataxia, and dental caries. Physical Examination Physical exam findings are nonspecific but may show developmental delay (particularly language delay), short stature, and mental status changes or seizures with severe toxicity. Laboratory Studies and Imaging Venous samples are more accurate than fingerstick capillary values. Treatment Primary prevention is the preferred management, and chelation therapy does not reverse neurocognitive defects in children with lead neurotoxicity. Guidance for effective discipline: Committee on Psychosocial Aspects of Child and Family Health. Managing Elevated Blood Lead Levels Among Young Children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Committee on Practice and Ambulatory Medicine, Bright Futures Periodicity Schedule Workgroup. Periodicity Schedule: Policy Statement 2014 Recommendations for Pediatric Preventive Health Care. Vaccines are not associated with autism: An evidencebased meta-analysis of case-control and cohort studies. Deviation from norms can identify children with nutritional deficiencies, endocrinopathies, and other underlying conditions. Term infants should grow by 30 g/day in the first 1-3 months of life, 20 g/day during 3-6 months of age, and 10 g/day between 6 and 12 months of age. Children who gain <1 kg/year should be monitored closely for nutritional deficiencies. Height Term infants should grow 25 cm in the 1st year, 10 cm during the 2nd year, and 7. It typically increases by 2 cm from 1 to 2 years, and head growth is mostly complete by 4 years of age. Preterm Infants and other Variants from typical Growth Patterns Preterm infant growth goals differ from term infants, and while further study is needed to understand the nutritional needs of preterm infants, the following growth goals can be used as a guide: weight should increase by 15 g/kg/day, length by 1 cm/week, and head circumference by 0. Please see Chapter 18, Endorcrinology, for detailed information on causes of short stature and deviations from typical growth patterns. Formula Feeding Although breast milk should be the first choice for infant nourishment, there are many infant formulas that provide adequate nutrition (Table 2-1). While it is common practice to switch formulas in infants with difficulty gaining weight, frequent physiologic reflux, or other feeding difficulties, there are limited data for this practice. Iron-fortified infant formula is the recommended substitute for infants who are not breastfed. In newborns, this is 2-3 oz every 3-4 hours, and it increases to 4 oz every 3-4 hours at 1 month of age. If powdered formula is used, ensure that family members are following the instructions for mixing it accurately. Complementary Foods Complementary foods (any foods and beverages other than human milk or formula) can be introduced starting between 4 and 6 months of age, when the infant is developmentally ready. There is no specific recommended sequence for introducing foods, as long as essential nutrients that complement breast milk or formula are provided. In general, parents should start with single-ingredient foods and introduce them one at a time at 2- to 7-day intervals. Parents can gradually introduce other pureed foods, soft fruits and vegetables, and soft table foods 2-3 times per day. Toddlers, Children, and Adolescents At 12 months of age, children can be transitioned from breast milk or formula to whole milk containing calcium and vitamin D. Earlier transitioning to whole milk is associated with the development of iron deficiency anemia. Key messages include portion control, making half of your plate fruits and vegetables, making half of your grains whole grains, switching to fat-free or 1% milk, choosing foods with lower sodium, and drinking water instead of sugary beverages. Recommendations for iron intake include: Children ages 9-13 years: 8 mg/day Females 14-18 years old: 15 mg/day Males 14-18 years old: 11 mg/day Recommendations for calcium intake include: Children 4-8 years old: 800 mg/day Children and adolescents 9-18 years old: 1,300 mg/day Adolescents and adults 19 years and above: 1,000 mg/day Limit carbonated soda and fruit drinks. Allow no more than 4-6 oz of 100% fruit juice daily due to its high calorie and sugar content. Evaluating the dietary intake of an adolescent is a fundamental component of health supervision. It is typically detected in the outpatient setting through serial monitoring of growth at routine well-child visits. History History should include questions about diet, stooling, and growth patterns, pregnancy and birth complications, family history, patient and family meal-time behaviors, P. Physical Examination Plot weight, height, and head circumference on growth charts to evaluate percentiles and compare to previously documented records. Focus the exam on clues learned from the history that may support a particular diagnosis. Second-line laboratory evaluation might include fat-soluble vitamin levels, urine organic acids, and serum amino acids. Improvements in weight gain are best measured in weeks and months, so outpatient therapy is preferred. Breastfeeding mothers can pump and provide expressed breast milk in a bottle to better quantify the volume of milk provided. This might include occupational, physical, and speech therapists; psychologists and psychiatrists, a dietician, and a social worker. Clinical Presentation Benign regurgitation occurs shortly after feeding, is nonforceful, and is not associated with weight loss or dehydration. Treatment If no red flags such as weight loss, dehydration, projectile emesis, or bilious emesis are present, reassurance is indicated. Measures to decrease regurgitation include frequent burping during feeds and propping the infant at a 30-degree angle following feeds. Picky Eating Toddlers may reduce their food intake as their rate of growth slows and assert independence by displaying their dislikes of certain foods. If history and physical exam are concerning, further evaluation for food allergy, oral aversion, vitamin deficiency, or other underlying abnormalities may be warranted. Treatment Provide a variety of foods at each meal in all of the basic food groups and allow the child to make choices. Do not pressure the child to eat any particular food as this may result in more significant feeding problems. Children with highly restrictive diets or iron deficiency anemia may need vitamin and mineral supplementation. Evaluation Focus on the medical consequences of obesity such as hypertension, type 2 diabetes and insulin resistance, coronary artery disease, hypercholesterolemia, left ventricular hypertrophy, obstructive sleep apnea, mechanical stress on joints, pseudotumor cerebri, and hepatic steatosis. Schedule frequent visits with overweight and obese patients to encourage small but consistent diet and lifestyle modifications. Bariatric surgery is an extreme but effective treatment in adolescents with severe obesity. Table 2-2 summarizes common findings in children with specific vitamin deficiencies. Iron Deficiency Epidemiology Iron deficiency can occur during infancy, childhood, or adolescence.
Buy generic alesse 0.18 mg line
When the O2 pressure within the anesthesia machine decreases below 30 psi birth control z-pack order alesse 0.18mg on line, this valve discontinues the flow of N2O or proportionally decreases the flow of all gases. It is important to realize that this valve will not prevent the delivery of hypoxic gas mixtures or pure N2O when the O2 rotameter is off, because the O2 pressure within the circuits of the anesthesia machine is maintained by an open O2 compressed-gas cylinder or a central supply source. However, volatile anesthetics with identical saturated vapor pressures can be used interchangeably, with accurate delivery of the volatile anesthetic. Laminar flow occurs when gas flows down parallel-sided tubes at a rate less than critical velocity. These systems do not require extensive technical skill on the part of the anesthesia provider for accurate use. Thus, after the zeroing procedure is accomplished, the system is ready for operation. These scavenging systems can be passive (waste gases flow from the anesthesia machine to a ventilation system on their own) or active (anesthesia machine is connected to a vacuum system, then to the ventilation system). Given that most ventilator bellows are powered by oxygen, a leak in the bellows will not add air to the evacuation system. The negative-pressure relief valve is used in active systems and will entrap room air if the pressure in the system is less than -0. In pulmonary alveoli, surface tension is produced by a liquid film lining the alveoli. This occurs because the attractive forces between the molecules of the liquid film are much greater than the attractive forces between the liquid film and gas. Vaporizers 15 are described as having variable bypass, which means that some of the total fresh gas flow (usually less than 20%) is diverted into the vaporizing chamber, and the rest bypasses the vaporizer. Tipping the vaporizers (which should not occur) may cause some of the liquid to enter the bypass circuit, leading to a high concentration of anesthetic being delivered to the patient. The gas that enters the vaporizer flows over (does not bubble through) the volatile anesthetic. The older (now obsolete) Copper Kettle and Vern-Trol vaporizers were not agent specific, and oxygen (with a separate flowmeter) was bubbled through the volatile anesthetic; then, the combination of oxygen with volatile gas was diluted with the fresh gas flow (oxygen, air, N2O) and administered to the patient. Measured-flow vaporizers (nonconcentration calibrated vaporizers) include the obsolete Copper Kettle and Vernitrol vaporizers. With measured-flow vaporizers, the flow of oxygen is selected on a separate flowmeter to pass into the vaporizing chamber, from which the anesthetic vapor emerges at its saturated vapor pressure. By contrast, in variable-bypass vaporizers, the total gas flow is split between a variable bypass and the vaporizer chamber containing the anesthetic agent. Each breath lasts 6 seconds (60 sec/10 breaths), with inspiration lasting 2 seconds (I:E ratio = 1:2). Thus, each breath will last 10 seconds 26 (B) Endotracheal tubes frequently become partially or completely occluded with secretions. They include mucosal trauma, cardiac dysrhythmias, hypoxia, increased intracranial pressure, colonization of the distal airway, and psychologic trauma to the patient. To reduce the possibility of colonization of the distal airway it is prudent to keep the suction catheter within the endotracheal tube during suctioning. Pushing the suctioning catheter beyond the distal limits of the endotracheal tube also may produce suctioning trauma to the tracheal tissue (Tobin: Principles and Practices of Mechanical Ventilation, ed 3, p 1223). Soda lime contains 15% water by weight, and only when it gets dehydrated to below 1. Many of the reported cases of patients experiencing elevated carboxyhemoglobin levels occurred on Monday mornings, when the fresh gas flow on the anesthesia circuit was not turned off and high anesthetic fresh gas flows (>5 L/min) for prolonged periods of time. If the ventilator pressure-relief valve were to stick in the closed position, there would be a rapid buildup of pressure within the circle system that would be readily transmitted to the patient. When N2O and oxygen enter the vaporizing chamber, a portion of the N2O dissolves in the liquid agent. The four phases of the capnogram are inspiratory baseline, expiratory upstroke, expiratory plateau, and inspiratory downstroke. The shape of the capnogram can be used to recognize and diagnose a variety of potentially adverse circumstances. However, the inspiratory baseline may be elevated when the inspiratory valve is incompetent. This occurs because of imperfect matching of ventilation and perfusion in all lung units. The most frequent complication associated with direct laryngoscopy and tracheal intubation is dental trauma. If a tooth is dislodged and not found, radiographs of the chest and abdomen should be taken to determine whether the tooth has passed through the glottic opening into the lungs. Other complications of direct laryngoscopy and tracheal intubation include hypertension, tachycardia, cardiac dysrhythmias, and aspiration of gastric contents. The most common complication that occurs while the endotracheal tube is in place is inadvertent endobronchial intubation. Flexion, not extension, of the neck or a change from the supine position to the head-down position can shift the carina upward, which may convert a midtracheal tube placement into a bronchial intubation. Extension of the neck can cause cephalad displacement of the tube into the pharynx. Lateral rotation of the head can displace the distal end of the endotracheal tube approximately 0. The complications associated with extubation of the trachea can be immediate or delayed; of the immediate complications associated with extubation of the trachea, the two most serious are laryngospasm and aspiration of gastric contents. Laryngospasm is most likely to occur in patients who are lightly anesthetized at the time of extubation. If laryngospasm occurs, positive-pressure bag and mask ventilation with 100% O2 and forward displacement of the mandible may be sufficient treatment. However, if laryngospasm persists, succinylcholine should be administered intravenously or intramuscularly. It occurs most commonly in female individuals, presumably because of the thinner mucosal covering over the posterior vocal cords in comparision with male individuals. This complication usually does not require treatment and spontaneously resolves in 48 to 72 hours. Pulse oximeters measure the alternating current component of light absorbance at each of two wavelengths (660 and 940 nm) and then divide this measurement by the corresponding direct current component. Based on the physical principles outlined above, the sources of error in Spo2 readings can be easily predicted. Pulse oximeters can function accurately when only two hemoglobin species, oxyhemoglobin and reduced hemoglobin, are present. If any light-absorbing species other than oxyhemoglobin and reduced hemoglobin are present, the pulse oximeter measurements will be inaccurate. Fetal hemoglobin has a minimal effect on the accuracy of pulse oximetry because the extinction coefficients for fetal hemoglobin at the two wavelengths used by pulse oximetry are very similar to the corresponding values for adult hemoglobin. In addition to abnormal hemoglobins, any substance present in the blood that absorbs light at either 660 or 940 nm, such as intravenous dyes used for diagnostic purposes, will affect the value of R, making accurate measurements of the pulse oximeter impossible. Gas enters at the bottom of the Thorpe tube and elevates a bobbin or float, which comes to rest when gravity on the float is balanced by the fall in pressure across the float. The rate of gas flow through the tube depends on the pressure drop along the length of the tube, the resistance to gas flow through the tube, and the physical properties (density and viscosity) of the gas. Similarly, the vapor pressure for sevoflurane (160 mm Hg) and enflurane (172 mm Hg) are similar, and at 1 atmosphere the concentration in the vaporizer for these drugs is 160/760, or about 21%. If desflurane (vapor pressure of 669 mm Hg) is placed in a 1-atmosphere pressure vaporizer, the concentration would be 669/760 = 88%. Atmospheric pressure will influence the function of rotameters because the accurate function of rotameters is influenced by the physical properties of the gas, such as density and viscosity. Atmospheric pressure will have little effect on the accurate function of rotameters at low gas flows because laminar gas flow is influenced by gas viscosity (which is minimally affected by atmospheric pressure), not by gas density.
Cheap alesse 0.18mg overnight delivery
If respiratory distress is not severe birth control 19th century buy 0.18mg alesse fast delivery, the pharynx can be examined, and asymmetrical swelling of the posterior pharyngeal wall may be observed pushing the uvula and ipsilateral tonsil forward. Even with direct examination, this swelling can be difficult to appreciate at times. A portable lateral neck radiograph taken on inspiration and with the neck in extension (with a physician in attendance) shows marked widening of the prevertebral soft tissues. It should be noted that false-positive radiographic findings of prevertebral soft tissue swelling, in the absence of retropharyngeal pathologic findings, are common when lateral neck radiographs are not taken on inspiration and with the neck extended. When a retropharyngeal abscess is diagnosed, prompt otolaryngologic consultation should be sought to determine whether the mass is fluctuant, necessitating surgical drainage, or if it is in an early cellulitic phase, requiring serial reexamination. A young child presented with high fever, drooling, quiet stridor, and an opisthotonic postural preference. A, Pharyngeal examination in the operating room revealed an intensely erythematous, unilateral swelling of the posterior pharyngeal wall. B, A lateral neck radiograph shows prominent prevertebral soft tissue swelling that displaces the trachea forward. Oral inspection may reveal medial displacement of the tonsil or lateral pharyngeal wall. Abscesses are treated by prompt drainage to prevent rupture with aspiration of purulent material, erosion into vascular structures, and extension to adjacent sites or into the mediastinum. Epiglottitis (Supraglottitis) Epiglottitis, a now uncommon but life-threatening form of acute upper airway obstruction, is an infection caused most often by H. Hence, many younger practitioners have never seen a case, increasing the risk of delayed diagnosis. Epiglottitis is characterized by marked inflammation and edema of the pharynx, epiglottis, aryepiglottic folds, and ventricular bands. The peak age range is 1 to 7 years old, but infants and older children may be affected. Onset is sudden and progression rapid; most patients are brought to medical attention within 12 hours of the first appearance of symptoms. In general, the child is entirely well until several hours before presentation, when he or she abruptly spikes a high fever. This is rapidly followed by progressive quiet stridor, severe throat pain with dysphagia and drooling, and soon thereafter by dyspnea and anxiety. On examination, the child is usually toxic, anxious, and remarkably still, sitting bolt upright with neck extended and head held forward (unless obstruction is mild or fatigue has supervened). Quiet gurgling, stridor, and drooling are evident, along with dyspnea and retractions. This clinical picture is so typical that, when seen, the best course of action after initial assessment is prompt airway stabilization, usually intubation under controlled conditions by experienced personnel in the operating room. At this time, the epiglottis/supraglottis is found to be markedly swollen and erythematous. After airway stabilization, cultures can be obtained and parenteral antimicrobial therapy initiated. Obtaining a radiograph or repeating oral physical examinations before transfer to the operating room is contraindicated; it adds nothing and may precipitate total airway obstruction. On occasion, children present with a similar history but milder symptoms and signs. Respiratory distress is minimal, and visualization of the pharynx can be attempted (without use of a tongue blade) if the child will voluntarily open his or her mouth. This child tried to swallow a tack that punctured and became lodged in the posterior pharyngeal wall. The incident was unwitnessed, and he came to medical attention only when he developed fever and began drooling. High-dose parenteral antimicrobial therapy is necessary whether or not drainage is required. As noted earlier, a retropharyngeal abscess may occasionally form in an older child after a puncture wound of the posterior pharyngeal wall. Parapharyngeal Abscess Lateral neck space abscesses can also occur in infants and young children. The history and clinical picture are nearly identical to those of children with retropharyngeal abscess. A, this infant had high fever, toxicity, and marked, exquisitely tender anterolateral neck swelling with overlying erythema. These manifestations followed a week of upper respiratory tract symptoms and decreased feeding. A to C, these three patients with acute epiglottitis demonstrate the varying degrees of distress that may be seen, depending on age and time of presentation. A, this 3-year-old, seen a few hours after onset of symptoms, was anxious and still but had no positional preference or drooling. B, this 5-year-old, who had been symptomatic for several hours, holds his neck extended with head held forward, is mouth breathing and drooling, and shows signs of tiring. C, this 2-year-old was in severe distress and was too exhausted to hold his head up. D and E, In the operating room, the epiglottis can be visualized and appears intensely red and swollen. SubglotticDisorders Croup or Laryngotracheobronchitis Croup, an acute respiratory illness, is characterized by inflammation and edema of the pharynx and upper airways, with maximal narrowing in the immediate subglottic region. The majority of cases are caused by viral pathogens, with parainfluenza, respiratory syncytial virus, adenoviruses, influenza viruses, and echoviruses being the agents most commonly identified. This lateral neck radiograph demonstrates mild epiglottic swelling and thickening of the aryepiglottic folds. This toddler with moderate upper airway obstruction caused by croup had suprasternal and subcostal retractions. Her anxious expression was the result of mild hypoxia confirmed by pulse oximetry. The disorder primarily affects children between the ages of 6 months and 3 years old. This is probably because their airways are narrower, and the mucosa is both more vascular and more loosely attached than in older children, enabling greater ease of edema collection. Typically the child has had symptoms of a mild upper respiratory tract infection with rhinorrhea, cough, low-grade fever, and perhaps a sore throat for 1 to 5 days before developing symptoms of croup. The child awakens with fever, loud inspiratory stridor, a loud "barky" or "seal-like" cough, and hoarseness. Most patients have a waxing and waning course, with symptoms more severe at night, but it is impossible to predict which night will be the worst. Some patients remain relatively mildly affected throughout the course, whereas others progress either slowly or rapidly to severe distress. Airway drying, probably in part as a result of mouth breathing necessitated by nasal congestion (especially while sleeping), appears to aggravate the cough and possibly the element of laryngospasm. Physical findings are highly variable, depending on degree of distress at the time of presentation. Most affected children are moderately febrile but not toxic and have a loud barky cough and loud inspiratory stridor, with suprasternal and subcostal retractions. Distinguishing the stridor of croup from the wheezing of asthma is most important. Many patients improve substantially as a result of exposure to cool night air during the trip to the emergency department. Some have restlessness or agitation reflecting hypoxia, and a few have severe distress. In these more severely affected patients, stridor may be both inspiratory and expiratory, with generalized retractions. If impairment of airflow is extreme, fatigue supervenes, stridor abates, and retractions diminish. A clinical scoring system that helps in grading severity of distress is presented in Table 24. In mild to moderate cases the pharynx can be visualized and reveals only mild erythema. Radiography can be helpful in demonstrating subglottic narrowing-the "steeple sign". However, this is not necessary for patients with mild disease, and it is contraindicated for those with severe distress.
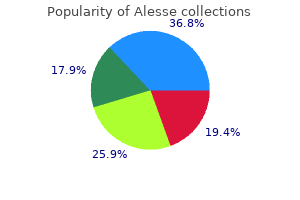
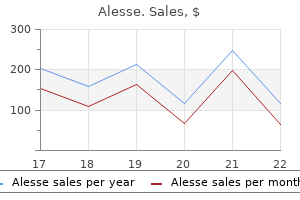
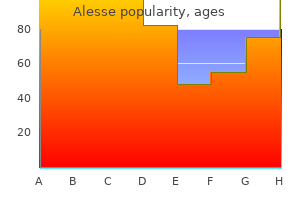
| Comparative prices of Alesse | ||
| # | Retailer | Average price |
| 1 | Tractor Supply Co. | 983 |
| 2 | Staples | 277 |
| 3 | Williams-Sonoma | 224 |
| 4 | Alimentation Couche-Tard | 210 |
| 5 | Meijer | 414 |
| 6 | Dell | 802 |
| 7 | Target | 230 |
Discount 0.18mg alesse free shipping
A 68-year-old asthmatic drunk driver comes into the expenditure per day be the greatest It is indicated for ventricular tachycardia and fibrillation refractory to electrical defibrillation C birth control 6 weeks postpartum buy alesse online from canada. The patient also has a pneumothorax, and high airway pressures are needed to adequately ventilate the patient 168. Three hours later, the ventilator malfunctions and the resident disconnects the patient from the ventilator and hand ventilates the patient with 100% oxygen. The next intervention that should be done, in addition to chest compressions, is A. Removal of urinary catheter by postoperative day 2 Respiratory Physiology and Critical Care Medicine Answers, References, and Explanations 91. If one divides the volume by 10 (number of breaths/min), then one determines the compression volume/breath. This number (mL) can be further divided by the peak inflation pressure (cm H2O) to determine the actual compression factor, which in this case is 5 mL/(cm H2O) (Miller: Basics of Anesthesia, ed 6, p 208; Ehrenwerth: Anesthesia Equipment Principles and Applications, p 364). Compression volume = (Vdelivered - Vmeasured) / Respiratory rate = 5 mL/(cm H2O) Peak airway pressure (cm H2O) 92. The presence of sufficient quantities of methemoglobin in the blood will cause the pulse oximeter to read 85% saturation regardless of the true arterial saturation. Cyanide toxicity is also a possibility in any patient who is receiving nitroprusside. Cyanide toxicity should be suspected when the patient develops metabolic acidosis or becomes resistant to the hypotensive effects of this drug despite a sufficient infusion rate. This can be confirmed by measuring the mixed venous Pao2, which would be elevated in the presence of cyanide toxicity. Thiocyanate toxicity is also a potential hazard of nitroprusside administration in patients with renal failure. The greatest concerns for the anesthesiologist are, however, related to the heart and lungs. As a consequence, obese patients frequently are hypertensive, and many ultimately develop cardiomegaly and left-sided heart failure. This ratio can be used to determine the severity of obstructive airway disease and to monitor the efficacy of bronchodilator therapy (Barash: Clinical Anesthesia, ed 7, p 279). Alveolar ventilation (Va) in neonates is double that of adults to help meet their increased O2 requirements. This increase in Va is achieved primarily by an increase in respiratory rate as Vt is similar to that of adults. The volume of gas remaining in the lungs after a normal expiration is called the functional residual capacity. The volume of gas remaining in the lungs after a maximal expiration is called the residual volume. The volume of gas in ventilated alveoli that are unperfused (and not available for gas exchange) is called the functional dead space. The anatomic dead space together with the functional dead space is called the physiologic dead space. However, measuring the effects of increased Paco2 on ventilation is the most sensitive method of quantifying the effects of drugs on ventilation. The amount of O2 dissolved in plasma is directly proportional to the product of the blood/gas solubility coefficient of O2 (0. The amount of O2 bound to hemoglobin is directly related to the fraction of hemoglobin that is saturated. Hemoglobin species such as carboxyhemoglobin and methemoglobin, dyes such as methylene blue and indocyanine green, and some colors of nail polish will cause erroneous readings. Because the absorption spectrum of fetal hemoglobin is similar to that of adult oxyhemoglobin, fetal hemoglobin does not significantly affect the accuracy of these types of pulse oximeters. The compliance curve is roughly the same as the normal lung, curve C, but volumes have increased. Physiologic factors that affect mixed venous O2 satura- tion include hemoglobin concentration, arterial Pao2, cardiac output, and O2 consumption. Anemia, hypoxia, decreased cardiac output, and increased O2 consumption decrease mixed venous O2 saturation. During sepsis with adequate volume resuscitation, the cardiac output is increased and maldistribution of perfusion (distributive shock) results in an elevated mixed-venous O2 saturation. Mixed venous O2 saturation (Svo2) is related to a number of factors, as shown in this equation: Sv O2 = SaO2 - 2 Hgb where Hgb is hemoglobin concentration, 13. In a 70-kg patient, the vital capacity is approximately 5 L (Stoelting: Pharmacology and Physiology in Anesthetic Practice, ed 4, p 776; Barash: Clinical Anesthesia, ed 7, p 278). Carbon mon- oxide binds to hemoglobin with an affinity 200 times greater than that of oxygen. For this reason, very small concentrations of carbon monoxide can greatly reduce the oxygen-carrying capacity of blood. An acute increase in Paco2 of 10 mm Hg will result in a decrease in pH of approximately 0. The acidosis of arterial blood will stimulate ventilation via the carotid bodies, and the acidosis of cerebrospinal fluid will stimulate ventilation via the medullary chemoreceptors located in the fourth cerebral ventricle. Many feel that if dopamine is needed at rates greater than 10 g/kg/min, one should use epinephrine or norepinephrine infusions instead. Although many cardiovascular drugs are based on a g/kg/min dose, vasopressin is not. Second, alkalosis stimulates the activity of phosphofructokinase, which increases glycolysis and the production of pyruvate and lactic acid. Assisted/controlled modes of mechanical ventilation are used in patients when the muscles of respiration require rest because minimal breathing efforts are required. With the assisted/controlled mode of ventilation, positive-pressure ventilation is triggered by small breathing efforts produced by the patient. These modes are categorized Respiratory Physiology and Critical Care Medicine 41 118. In this case, where the patient is reasonably stable, the three major goals in the management of atrial fibrillation should be considered. These goals are control of ventricular rate, assessment of anticoagulation needs, and conversion to sinus rhythm. In addition, the underlying cause of atrial fibrillation should be sought and treated. Because we do not know when atrial fibrillation developed (after 48 hours, embolic events may occur with conversion to sinus rhythm), it would be best not to convert the atrial fibrillation to sinus rhythm using either ibutilide or procainamide until the patient is adequately anticoagulated. In marginal cases where the duration of atrial fibrillation is uncertain, cardiac consultation and transesophageal echocardiography to exclude atrial thrombus should be performed before cardioversion. A P50 greater than 26 mm Hg describes a rightward shift of the oxyhemoglobin dissociation curve. This increased alveolar volume resulted in mechanical injury and a systemic inflammatory response. It was felt that the stretch and not the pressure (barotrauma) caused the release of the inflammatory cytokinins into the circulation. Recruitment maneuvers (sustained breaths of increased airway pressures) were used to re-expand atelectatic alveoli to avoid atelectrauma. However, results with the recruitment breaths showed only a transient increase in oxygenation and no change in mortality. Randomized controlled studies have shown only limited effectiveness with no overall improvement in mortality or duration of ventilation. The diffusion coefficient of the gas is directly proportional to the square root of gas solubility and is inversely proportional to the square root of the molecular weight of the gas. These changes are caused by progressive stiffening of cartilage and replacement of elastic tissue in the intercostal and intervertebral areas, which decreases compliance of the thoracic cage. In addition, progressive kyphosis or scoliosis produces upward and anterior rotation of the ribs and sternum, which further restricts chest wall expansion during inspiration.
Purchase alesse overnight delivery
Myopathy: flaccid weakness birth control pills 24 active discount alesse 0.18mg visa, proximal greater than distal, depressed or absent reflexes; may have elevation of serum creatine kinase, hypertrophy, or myotonia. Differential Diagnosis Based on Localization Central nervous system: stroke, metabolic abnormality, hypoxic ischemic injury. If an infarct is seen, a complete metabolic, hematologic, and cardiac workup is generally undertaken. In neonates, any change in neurologic function should prompt a consideration of infarct. Causes are numerous, but general categories to consider include trauma, arteriopathies, vasospasm, vasculitis, systemic vascular disease, hematologic disorders including neoplasia, prothrombotic states both acquired and congenital, metabolic disorders including mitochondrial and Fabry disease, and congenital and acquired heart disease. Caution: up to 15% of children with known congenital cardiac defects and stroke also have other definable risk factors such as a prothrombotic state. So, the workup of a stroke in a child with congenital cardiac disease should include a search for other causes. The most common presentation involves motor weakness, but a stroke can include loss of any other neurologic function, including sensory abilities, language, or vision. However, up to 1/3 of pediatric strokes present with seizures and over half may experience headache at stroke onset. Lay head of the bed flat unless there is a concern for increased intracranial pressure. There are no randomized controlled trials in children regarding anticoagulation or antiplatelet therapy. However, neonates with stroke have low risk of recurrence; hence, aspirin is not routinely recommended. More aggressive therapy, such as thrombolysis and endovascular procedures, is controversial. Anticoagulation should be started immediately if venous sinus thrombosis is diagnosed, after sending labs for hypercoagulability workup. In sickle cell patients with stroke, consult hematology for urgent exchange transfusion. Pain, extreme enough to mimic encephalopathy, can be a significant part of the presentation in young children. Botulism the infantile form results from ingestion and colonization of Clostridium botulinum, whereas all others result from ingestion of the toxin produced by this organism. Diplopia, dysarthria, dysphagia, and vertigo may be associated with flaccid weakness. Repetitive nerve stimulation gives incremental response but is not always present. Treatment consists of supportive care, and in select cases, botulism immune globulin may be used. Transverse Myelitis Sudden demyelination of the spinal cord (often thoracic) with maximal weakness within days is characteristic. In addition to weakness, sensory deficits, areflexia or hyperreflexia, and bowel and bladder involvement are typically present. In adolescents, consider multiple sclerosis, but there are many causes, including infectious/parainfectious (especially mycoplasma), vascular, and autoimmune. In a hypotonic, weak infant with a smile and good interaction, consider spinal cord involvement. Extensive differential diagnosis Cardiac arrhythmias, apnea, syncope, transient ischemic attack/cerebral hypoperfusion Seizure Jitteriness, startle responses, breath-holding spell Night terrors, narcolepsy-cataplexy, benign nocturnal myoclonus P. The criteria for the diagnosis of pediatric migraine without aura are the occurrence of five attacks fulfilling the following features: Headache attack lasting 1-72 hours Headache has at least two of the following four features: Either bilateral or unilateral (frontal/temporal) location Pulsating quality Moderate-to-severe intensity Aggravated by routine physical activities At least one of the following accompanies headache: Nausea and/or vomiting Photophobia and phonophobia (may be inferred from their behavior) History and Physical Examination Palpate the head: look for evidence of trauma, cutaneous allodynia, temporomandibular joint dysfunction. Remember to get a urine human chorionic gonadotropin in all women because all of these medications are relatively contraindicated in pregnancy. Lumbar puncture relieves headache in idiopathic intracranial hypertension (pseudotumor cerebri); papilledema resolves over weeks-months. In a patient with known epilepsy, the cause is often noncompliance or missed doses of antiepileptic medication, concurrent illness, sleep deprivation, or an unknown factor, but if he or she is febrile, serious infection must be excluded. Treatment Management of first-time afebrile seizure Clinical laboratory studies: Ca2+, Mg2+, phosphorus, and glucose are not typically indicated but may be necessary in some situations. If no cause is found, most first seizures are not treated with antiepileptic medication. However, many neurologists will not commit a patient to antiepileptic medication for one isolated seizure. Consider rectal diazepam (Diastat) for home use for any child with history of status epilepticus. Seizure precautions: no swimming except with supervision in clean pool, encourage showers instead of baths, no activities involving heights or open fires, and no driving until seizure free for at least 6 months (this varies state to state) (Table 21-3). Simple febrile seizures are generalized in onset, are <15 minutes, and do not recur within 24 hours. Complex febrile seizures are focal in nature, last >15 minutes, or recur within 24 hours. Epidemiology the most common age for febrile seizures is 6 months to 3 years; they are rare after 6 years of age. Overall risk in children is 2%-5%; if parent or sibling has had febrile seizures, the risk is 10%-20%. The seizures may occur early in illness as a temperature rises or even before a fever/illness is recognized. Routine laboratory studies are not necessary, unless there is clinical suspicion for metabolic disturbance or serious infection. Prophylactic treatment is not typically recommended because most febrile seizures are self-limited, and medications are not without risks. If an antiepileptic agent is selected, valproate and phenobarbital are effective; phenytoin, carbamazepine, and antipyretics are ineffective. Intermittent diazepam at fever onset is effective, as well, if fever precedes seizure. Rectal diazepam should be prescribed for children with history of prolonged or multiple seizures so that it may be given acutely for seizures lasting >5 minutes. This takes ~10-15 minutes to achieve effective blood levels, so do not redose before 15 minutes. If seizure has clinically stopped, consider possibility of nonconvulsive status if the patient is not waking or arousable. If phenobarbital already used, give fosphenytoin, 10 mg/kg; if fosphenytoin already used, give phenobarbital 20 mg/kg Consider treatment with midazolam infusion, pentobarbital, or other agent to induce pharmacologic coma. Avoid valproate in children <2 and if there is suspicion for mitochondrial disorder. Refractory status typically has an underlying etiology that needs to be addressed; look for abnormal electrolytes, infection, hemorrhage, stroke, genetic or metabolic syndrome, rarely pseudoseizures (Table 21-4). Exchange blood transfusion compared with simple transfusion for first overt stroke is associated with a lower risk of subsequent stroke: a retrospective cohort study of 137 children with sickle cell anemia. Therefore, it has generally been described as a triad of hoarse voice, harsh barking cough, and inspiratory stridor. Typically, the condition affects younger children (6-36 months), with a peak incidence at 2 years of age. Seasonal outbreaks have been described in the fall and winter, although it may occur yearround in some areas. Etiology and Pathophysiology Viral infection is the predominant etiology; parainfluenza virus (types 1, 2, and 3) is the most common agent. Mycoplasma pneumoniae is one of the few nonviral microorganisms that has been reported as an etiologic agent.
Alesse 0.18 mg line
Subclinical hyperthyroidism increases the risk of atrial fibrillation in patients older than 60 years and those with heart disease and predisposes to osteoporosis in postmenopausal women; it should be treated in these patients birth control names buy alesse 0.18mg low price. Asymptomatic young patients with mild Graves disease can be observed for spontaneous resolution of hyperthyroidism or the development of symptoms or increasing free T4 levels that warrant treatment. Urgent therapy is warranted when hyperthyroidism exacerbates heart failure or acute coronary syndromes and in rare patients with severe hyperthyroidism complicated by fever and delirium (sometimes called thyroid storm). In patients with clinical heart failure, it should be given only with careful monitoring of left ventricular function. When free T4 approaches the normal range, the doses of methimazole and iodine are gradually decreased. Methimazole is not used in the first trimester because it is associated with certain congenital defects. The dose should be adjusted at 4-week intervals to maintain the plasma free T4 near the upper limit of the normal range to avoid fetal hypothyroidism. The maternal plasma level of thyroidstimulating immunoglobulin should be measured in the third trimester to assess this risk. If the thyroid is enlarged, the examiner should determine whether the enlargement is diffuse or multinodular or whether a single palpable nodule is present. Between 30-50% of people have nonpalpable thyroid nodules that are detectable by ultrasound. These nodules rarely have any clinical importance, but their incidental discovery may lead to unnecessary diagnostic testing and treatment. Diffuse goiter Almost all euthyroid diffuse goiters in the United States are due to chronic lymphocytic thyroiditis (Hashimoto thyroiditis). In rare patients, the gland compresses the trachea or esophagus, causing dyspnea or dysphagia, and treatment is required. Evaluation for thyroid carcinoma with needle biopsy is warranted if there is a dominant nodule (a nodule that is disproportionately larger than the rest). This policy dramatically increases the number of thyroid biopsies and the cost of managing this common condition. Single thyroid nodules Single palpable thyroid nodules are usually benign, but about 5% are thyroid carcinomas. Clinical findings that increase the risk of carcinoma include the presence of cervical lymphadenopathy, a history of radiation to the head or neck, and a family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndromes type 2A or 2B. A hard, fixed nodule, recent nodule growth, or hoarseness due to vocal cord paralysis also suggests malignancy. Most patients with thyroid carcinomas have none of these risk factors, and all palpable single thyroid nodules should be evaluated with needle aspiration biopsy. Patients with thyroid carcinoma should be managed in consultation with an endocrinologist. Thyroxine therapy has little or no effect on the size of single thyroid nodules and is not indicated. Primary adrenal failure is most often due to autoimmune adrenalitis, which may be associated with other endocrine deficits. Hemorrhagic adrenal infarction may occur in the postoperative period, in coagulation disorders and hypercoagulable states, and in sepsis. Less common etiologies include adrenoleukodystrophy that causes adrenal failure in young men and drugs such as ketoconazole and etomidate that inhibit steroid hormone synthesis. Clinical findings in adrenal failure are nonspecific, and without a high index of suspicion, the diagnosis of this potentially lethal but readily treatable disease is easily missed. Symptoms are usually chronic, but shock may develop suddenly and is fatal unless promptly treated. All these symptoms are due to cortisol deficiency and occur in both primary and secondary adrenal failure. Diagnostic Testing the cosyntropin (Cortrosyn) stimulation test is used for diagnosis. This test detects primary and secondary adrenal failure, except within a few weeks of onset of pituitary dysfunction. Hyperkalemia, hyperpigmentation, or other autoimmune endocrine deficits indicate primary adrenal failure, whereas deficits of other pituitary hormones, symptoms of a pituitary mass. Most cases of primary adrenal failure are due to autoimmune adrenalitis, but other causes should be considered. Radiographic evidence of adrenal enlargement or calcification indicates that the cause is infection or hemorrhage. Patients with secondary adrenal failure should be tested for other pituitary hormone deficiencies and should be evaluated for a pituitary or hypothalamic tumor (see Disorders of Anterior Pituitary Function section). Patients should be evaluated for an underlying illness that precipitated the crisis. The dose of hydrocortisone is decreased gradually over several days as symptoms and any precipitating illness resolve, then changed to oral maintenance therapy. Mineralocorticoid replacement is not needed until the dose of hydrocortisone is <100 mg/d. Dexamethasone is used because it does not interfere with measurement of plasma cortisol. Maintenance therapy in all patients requires cortisol replacement with prednisone. Most patients with primary adrenal failure also require replacement of aldosterone with fludrocortisone. Concomitant therapy with rifampin, phenytoin, or phenobarbital accelerates glucocorticoid metabolism and increases the dose requirement. During illness, injury, or the perioperative period, the dose of glucocorticoid must be increased. For minor illnesses, the patient should double the dose of prednisone for 2-3 days. The same regimen is used in patients undergoing surgery, with the first dose of hydrocortisone given preoperatively. The dose can be tapered to maintenance therapy by 2-3 days after uncomplicated surgery. The dose is adjusted to maintain blood pressure (supine and standing) and serum potassium within the normal range; the usual dosage is 0. Patients should be educated in management of their disease, including adjustment of prednisone dose during illness. More specific findings include thin skin, easy bruising, reddish striae, proximal muscle weakness, and osteoporosis. All these tests are very sensitive, and a normal value virtually excludes the diagnosis. If the 24-hour urine cortisol excretion is more than 3-4 times the upper limit of the reference range in a patient with compatible clinical findings, the diagnosis of Cushing syndrome is established. In patients with milder elevations of urine cortisol, a low-dose dexamethasone suppression test should be performed. Urine cortisol is measured during the last 24 hours, and plasma cortisol is measured 6 hours after the last dose of dexamethasone. Failure to suppress plasma cortisol to <2 g/dL and urine cortisol to less than the normal reference range is diagnostic of Cushing syndrome. Testing should not be done during severe illness or depression, which may cause false-positive results. Phenytoin therapy also causes a false-positive test by accelerating metabolism of dexamethasone. After the diagnosis of Cushing syndrome is made, tests to determine the cause are best done in consultation with an endocrinologist. Most incidentally discovered nodules are benign adrenocortical tumors that do not secrete excess hormone. Differential Diagnosis the differential diagnosis includes adrenal adenomas causing Cushing syndrome or primary hyperaldosteronism, pheochromocytoma, adrenocortical carcinoma, and metastatic cancer. The imaging characteristics of the nodule may suggest a diagnosis but are not specific enough to obviate further evaluation. Diagnostic Testing Plasma potassium, metanephrines, and dehydroepiandrosterone sulfate should be measured, and an overnight dexamethasone suppression test should be performed. Patients who have potentially resectable cancer elsewhere and in whom an adrenal metastasis must be excluded may require positron emission tomography. Patients with hypertension (especially if they have hypokalemia) should be evaluated for primary hyperaldosteronism by measuring the ratio of plasma aldosterone (in nanograms per deciliter [ng/dL]) to plasma renin activity (in ng/mL/h). If the ratio is <20, the diagnosis of primary hyperaldosteronism is excluded, whereas a ratio >50 makes the diagnosis very likely.
Cheap alesse master card
The family must be well informed on the diagnosis birth control pills high blood pressure buy line alesse, and play an active role in the gender decision of the child. With an intact thirst mechanism, copious water drinking (>2 L/m2/day) may maintain normal osmolalities. However, problems with thirst mechanism or insufficient water intake lead to hypernatremic dehydration. Etiology (Table 18-6) Clinical Presentation and Laboratory Studies Clinical characteristics: polyuria, polydipsia (water intake >2 L/m2/day) Urine osmolality <300 mOsm/kg and serum osmolality >300 mOsm/kg, urine specific gravity <1. Terminate the test if weight loss approaches 3% to 5% of initial body weight or if orthostatic hypotension, serum osmolality >300, serum sodium >145, or urine osmolality increases to normal. Vasopressin test: used to differentiate between a nephrogenic and central etiology (Table 18-8) Give vasopressin 0. Monitor urine output, concentration, and water intake (water intake is limited to documented output during deprivation test) for an additional 2 hours. Titrate to allow 1-2 hours of breakthrough urine output (2-3 mL/kg/hr) with specific gravity <1. Clinic Presentation Hyponatremia (Serum sodium <135), in the setting of euvolemia or hypervolemia with decreased urine output and inappropriately concentrated urine (Urine Osm >100 mOsm/kg and Urine Sodium >30 mEq/L). Diagnosis cannot be in the setting of hypothyroidism, adrenal insufficiency, renal insufficiency or diuretic use. If the newborn screen is normal, consider recheck at 2-6 weeks in infants with Down syndrome, family history of dyshormonogenesis, or maternal thyroid disorder. Treatment Institute treatment as soon as the diagnosis is confirmed to optimize neurologic development. Test every 3 months in first year of life Test every 4 months between 1-3 years old Test every 6 months until growth is complete Test 4-6 weeks after dose is changed Aim for free T4 in upper end of normal. There is decreased absorption of thyroxine with soy formula as well as with iron and calcium supplements. It is necessary to assess compliance when reviewing abnormal thyroid function tests while on therapy. It is important to exclude coexisting pathology such as multiple endocrine neoplasia syndrome before a surgical procedure particularly if medullary carcinoma. Treatment Monitor status regularly if the child is nonsymptomatic from the goiter. Some endocrinologists prefer using thyroid medication in euthyroid patients to reduce the size of the goiter. Fetal growth is dependent on maternal factors (placental sufficiency, maternal nutrition, etc. It is common to see shifts in the growth curve in the first 18 months when children are adjusting to their genetic potential growth isopleth. There is a mild deceleration in growth velocity before initiation of pubertal growth spurt. Children have normal growth velocity, normal timing of development and puberty, and bones fuse at the appropriate age. Infants are born with weights below the 10th percentile for their gestational age. Age of menarche in mother and age of physical changes or cessation of growth in father may give information that supports the diagnosis of constitutional growth delay. Determination of the arm span and U/L ratio (lower segment is the measurement from the symphysis pubis to the floor) is useful to determine the etiologies of short stature. Examples: Short arm span or small legs and normal trunk (increased U/L ratio) may indicate skeletal dysplasia or hypothyroidism. The pattern of growth of a normal child is very consistent, and deviations in the process may warrant concern and further evaluation. Always measure it without shoes, and when plotting the patient in the growth curve, be as accurate as possible regarding the actual age of the child. Be sure to correct for genu recurvatum or leg length asymmetries when obtaining the measurements. Do not forget that pediatric patients do not shrink, so if unsure of your measurement, remeasure the patient again. The tendency to round off numbers becomes problematic when an inch is the measure. Up to an age of 2 years, a hemiskeletal bone age is more accurate; after that, obtain a left hand/wrist radiograph using the method of Greulich and Pyle. Growth hormone stimulation tests are needed because of the pulsatile nature of growth hormone release. A growth hormone level by itself is meaningless in the evaluation of short stature. Provocative agents include clonidine, L-dopa, arginine, insulin, glucagon, and growth hormone-releasing hormone. Up to 25% of normal children fail any given stimulation test, so it is important to consider the rest of the clinical picture and document abnormal results using two different agents to classify a patient as growth hormone deficient. It is considered a pass if the stimulation test has a peak growth hormone response >8 ng/mL. Cost: expensive (~$52,000 per inch of growth) Potential adverse effects: slipped capital femoral epiphysis, glucose intolerance/diabetes, pseudotumor cerebri, scoliosis. Pubertal changes are a consequence of increased gonadotropins and sex steroid secretion. Adrenarche: increased adrenal androgen that causes sexual hair and typically occurs at approximately the same time as puberty. It may coincide with the onset of puberty and generally occurs before testosterone levels have reached adult levels. Typically, the progression is breast development, initiation of growth spurt, pubic hair, and, lastly, menarche (initiation of monthly menstrual periods). Typically, the progression is testicular growth, followed by pubic hair development, and finally the peak growth spurt. Breast and pubic hair progression is determined by a comparison method with the Tanner stages. In girls, assess the vaginal mucosa for estrogen exposure (pink color, thickened mucosa, mucoid secretions). Before age 8 in girls, but can be as early as 6 year old in African American or Hispanic girls. Plasma ultrasensitive estradiol levels and testosterone levels at time of obtaining gonadotropins, respectively, in girls and boys are helpful on making this diagnosis. Pelvic ultrasound provides information on uterine and ovarian size and hormonal stimulation, as well as possible ovarian cyst or tumor. Patients should also have an endocrine evaluation if >5 years have elapsed between the first signs of puberty and completion of genital growth in boys or menarche in girls (or if no menarche by 16 years). For patients allergic to penicillin/cephalosporins, alternatives include meropenem, imipenem, or aztreonam. Add vancomycin (dosing per age and renal function) after 48 hours of persistent fever. Add antifungal therapy, amphotericin B or voriconazole, if fever lasts for >5 days. Check serum -fetoprotein and human chorionic gonadotropin to differentiate germ-cell tumors from lymphomas. Treatment High risk: empiric therapy of prednisone 40 mg/m2/day divided four times a day and/or radiotherapy should be given. Treatment: pericardiocentesis may relieve cardiac symptoms, but the underlying etiology must ultimately be treated. Monitor closely for an acute, surgical abdomen because these patients are at a high risk for perforation. Treatment Broad-spectrum antibiotics to cover Gram-negative enterics and anaerobes. Surgical intervention is reserved for patients with bowel perforation or other dire complications.
Buy cheap alesse 0.18 mg online
Studies have shown that high-dose nebulized budesonide (2 mg) is superior to placebo and as effective as dexamethasone in reducing symptom scores birth control pills zoloft generic alesse 0.18mg online, but the cost-benefit ratio limits its use. It affects children of all ages, with a peak around 3-6 years of age, although its incidence has declined significantly since Haemophilus influenzae type B immunization was introduced in 1998. Direct invasion by the inciting agent causes inflammation of the epiglottis, aryepiglottic folds, ventricular bands, and arytenoids. Subsequently, there is accumulation of inflammatory cells and edema fluid where the stratified squamous epithelium is loosely adherent to the anterior surface and the superior third of the posterior portion of the epiglottis. Diffuse infiltration with polymorphonuclear leukocytes, hemorrhage, edema, and fibrin deposition occurs. Inspiration tends to draw the inflamed supraglottic ring into the laryngeal inlet. Clinical Presentation Epiglottitis is a rapidly progressing illness in previously healthy individuals. If patient is in little distress, and the diagnosis is unclear, a lateral neck radiograph may be obtained, which shows the classical thumbprint sign that represents a swollen epiglottis and aryepiglottic folds. The definitive diagnosis requires direct visualization of a red swollen epiglottis under laryngoscopy, but this examination should be attempted only in a controlled setting in collaboration with an anesthesiologist and an otolaryngologist. The differential diagnosis includes foreign body aspiration, anaphylactic reaction, angioedema, caustic ingestion, thermal injury, inhalation injury, and laryngotracheobronchial and retropharyngeal infection. Treatment Airway stabilization and maintenance must be performed quickly and early in the course. An artificial airway should be available next to the patient, and it should always be ready for use. A cause of acute airway obstruction, this condition may potentially be life threatening. Most patients are <3 years of age (usually 3 months to 2 years), although older children may be affected. Invasion of opportunistic bacterial organisms, often following an upper airway viral infection, causes subglottic edema with ulcerations, copious and purulent secretions, and pseudomembrane formation. The illness then evolves rapidly with high fever and signs of airway obstruction, including stridor, cough, drooling, and supine positioning (preference to lie flat). Diagnosis Diagnosis is clinical with classical signs of epiglottitis and croup absent. Direct visualization of the trachea via laryngoscopy demonstrates thick, abundant, and purulent secretions. The differential diagnosis includes epiglottitis (although no dysphagia, and patient may lie flat), croup (although voice is normal and there is a lack of a barky cough), and laryngeal and retropharyngeal abscess. Choice of therapy includes broad-spectrum antibiotics with antistaphylococcal activity. Younger children are typically at higher risk because of oral exploration and immaturity of their swallowing functions. This situation may be life threatening; it is the leading cause of accidental death by ingestion in younger children. Etiology and Pathophysiology Ingested food and toy parts are aspirated into the airways, causing choking. Impaction of the larynx is particularly dangerous, although most particles travel well into the airways and lodge in the intrathoracic area. The foreign particle provokes localized airway inflammation with mucosal edema, inflammation, and development of granulation tissue. Clinical Presentation In general, following a witnessed aspiration or choking episode, patients develop a loud persistent cough along with gagging and stridor. However, the symptoms manifested are largely dependent on the localization of the particle, its size, and its composition. Foreign bodies in the larynx may cause hoarseness, aphonia, croupy cough, odynophagia, wheezing, and difficulty breathing, depending on the degree of obstruction. Foreign bodies in the trachea can cause what has been described as an audible slap, a palpable thud, and wheezing. Regardless of the position of the foreign body, if the event is unwitnessed and the particle remains lodged in the airway for a prolonged period of time, the patient usually develops a chronic cough with or without wheeze that is often treated as asthma. Position of the patient has no effect on the degree of airway obstruction, as in epiglottitis. Asymmetric findings on chest auscultation may provide a diagnostic clue but should not serve as an exclusion criterion. The diagnosis should also be entertained when a child exhibits unexplained symptoms that fail to respond to standard medical treatment, such as treatment for asthma or antibiotic therapy for suspected pneumonia. Inspiratory and expiratory chest films may show a "ball-valve" effect or persistent hyperinflation of the area suspected to be lodging the particle. If suspicion is high, referral for laryngoscopy and rigid bronchoscopy is often the only method of visualizing (and removing) the foreign body. The differential diagnosis includes epiglottitis, viral laryngotracheobronchitis, bacterial tracheitis, asthma, pneumonia, airway malacia, and psychogenic cough. Treatment Management usually involves removal of the foreign body via bronchoscopy (typically rigid) for appropriate control of the airway. If the particle remains in the airway for a prolonged period of time, potential complications may arise, including bronchial stenosis, distal bronchiectasis, tracheoesophageal fistula, abscess formation, and airway lacerations or perforation. It is usually most prominent during winter and early spring, with annual epidemics in temperate climates. It occurs in the first 2 years of life (0-24 months), and it peaks at 6 months of age (2-8 months). Large droplets survive up to 6 hours on surfaces and up to 30 minutes in the hands. This infection is the leading cause of infant hospitalization and the leading cause of lower respiratory tract infection in infants and small children, with two-thirds of the infants infected in their 1st year and universal infection by 2 years of age. Parainfluenza virus (second most common cause) this virus is unstable in the environment, but spread occurs from respiratory secretions. Type 1 (5%-12%) and type 2 (1%-5%) are responsible for outbreaks in the fall, and type 3 (8%-15%) occurs predominantly in the spring to fall. Rhinovirus (causes 3%-8% of the cases) Transmission is by aerosol or direct contact. Most cases are mild and self-limited, but shedding may last up to 3-4 weeks (peak, 2-7 days). Pathophysiology Disease occurs by invasion of the smaller bronchioles by the viral particles followed by viral colonization and replication. This causes necrosis of ciliated cells and proliferation of nonciliated cells, causing impaired clearance of secretions, submucosal edema, and congestion, which results in plugging of bronchioles (mucus and debris) and peripheral airway narrowing. The increased respiratory effort is secondary to inflammatory obstruction of the small airways (bronchioles) because of edema. Their airways are easily plugged by mucus or inflammatory debris because their collateral pathways of ventilation (pores of Cohn and Lambert) are less well developed, have more mucous glands, and are more collapsible in response to pressure changes. Pertinent physical examination findings include tachypnea (60-80 breaths per minute), hyperexpanded chest, nasal flaring, use of accessory muscles, widespread fine crackles, prolonged expiration, diffuse wheezes, and decreased breath sounds. Risk factors for severe disease include prematurity, age <12 weeks, chronic pulmonary disease, congenital airway anomalies, congenital heart disease, immunodeficiency, neurologic diseases, and history of poor feeding. Infants born prematurely and those younger than 2 months may be at risk for apnea, which may be unrelated to respiratory distress. Aids to confirm diagnosis and predict the course of the illness include nasopharyngeal swab for viral diagnostics (enzyme-linked immunosorbent assay, direct P. Other less-timely approaches include viral culture and serology for viral antibodies. Routine radiographs are not recommended but may be helpful if there is suspicion of bacterial pneumonia.