Cheap 300mg isoniazid with mastercard
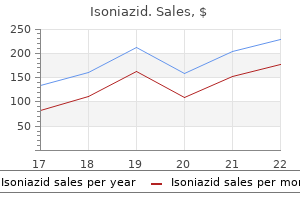
Povidone iodine and silver sulfadiazine dressings are avoided due to the risk of systemic absorption of iodine and silver treatment 002 purchase isoniazid online now, respectively. If skin loss is small, sterile dressings of silver sulfadiazine cream and paraffin-impregnated gauze covered by gauze and cotton tissue can be used for the trunk. Avoiding nonsteroidal anti-inflammatory drugs that are excreted by the kidneys and cause an increased risk of bleeding is important. Staphylococcal scalded skin syndrome is a spectrum of superficial blistering disorders caused by exfoliative toxin of Staphylococcus aureus. In the generalized variant, following a prodrome there is a scarlatiniform eruption that eventuates into formation of flaccid bullae leading to erosions and exfoliation that are more prominent over the flexures. Due to the superficial level of split in the epidermis, there is rapid healing with appropriate treatment usually within 10 days. Investigations are directed toward identifying a potential focus of staphylococcal infection, fluid status of the patient, and any evidence of secondary infection. The primary focus of infection is obscure in children but is detectable in adults in most cases. Hospitalization of the patient with administration of fluids to maintain electrolyte and fluid balance, infection control with antibiotics, and pain management are the mainstay of treatment. Mortality is low in children but is higher in adults on account of an associated immunocompromised state. Nasal, axillary and perineal carriage of Staphylococcus aureus among pregnant women: Identification of strains producing epidermolytic toxin. It can reach almost 60% in adults who have an underlying illness even with initiation of appropriate antibiotics. More extensive involvement in a younger patient is associated with a worse outcome. Exfoliative toxin production by Staphylococcus aureus strains isolated from animals and human beings in Nigeria. Structural similarities and differences in Staphylococcus aureus exfoliative toxins A and B as revealed by their crystal structure. Clinical, microbial and biochemical aspects of the exfoliative toxins causing staphylococcal scalded skin syndrome. Staphylococci, streptococci and the skin: Review of impetigo and staphylococcal scalded skin syndrome. Staphylococcal scalded skin syndrome in adults: A clinical review illustrated with a new case. Staphylococcal scalded skin syndrome and consecutive septicaemia in a preterm infant. Staphylococcal scalded skin syndrome mimicking acute graft-versus-host disease in a bone marrow transplant recipient. Action of staphylococcal exfoliative toxins on epidermal cell cultures and organotypic skin. Development and evaluation of detection systems for staphylococcal exfoliative toxin A responsible for the scalded skin syndrome. Difficulties in the diagnosis and management of staphylococcal scalded skin syndrome. Neonatal staphylococcal scalded skin syndrome: Massive outbreak due to an unusual phage type. Toxic epidermal necrolysis: Clinical findings and prognostic factors in 87 patients. Experience with severe extensive blistering skin disease in a paediatric burn unit. Difficulties in diagnosis and management of the staphylococcal scalded skin syndrome. Antibody reactivity of a standardized human serum protein solution against a spectrum of microbial pathogens and toxins: Comparison with fresh frozen plasma. The next few years saw a surge in the cases of toxic shock syndrome among menstruating women, ascribed to the usage of superabsorbent tampons. The incriminated gram-positive bacteria are Staphylococcus aureus and Streptococcus pyogenes (group A Streptococcus spp. Needless to say, early recognition of symptomatology and causation is of paramount importance, to prevent morbidity and mortality. An Ontario-based prospective study in the early 1990s identified 323 patients with soft tissue infection (48%), hematological bacteremia (14%), and pyogenic pneumonia (11%), in decreasing order of incidence. There is a strong history of precession by myalgia, sore throat, nausea, vomiting, and/or watery diarrhea. The patient presents with orthostatic hypotension or in frank shock; a reduced capillary refill time or decreased urine output may be the presenting complaints in cases of covert shock. However, with tampon usage, oxygen is introduced which modifies the milieu and allows aerobic bacteria to thrive. In cases where no definitive nidus is localized, transient oropharyngeal bacteremia has been suggested, after ruling out the previously mentioned conditions. Signs of systemic toxicity, sepsis, a hyperacute and progressive clinical outcome, and a case fatality rate exceeding 50% distinguish it from toxic staphylococcal syndrome. Extremity pain is the most frequent, but it may also mimic other conditions like pelvic inflammatory disease, serositis (pleural, pericardial, peritoneal), pneumonitis, or an acute coronary event. Approximately 20% have an influenza-like syndrome with fever, myalgia, chills and rigor, nausea, diarrhea, and vomiting [13]. Fever: Fever is the earliest sign, but patients in shock may present with hypothermia [14,15]. Disorientation, mental confusion, or disrupted higher mental functions: this may be seen in 55% of patients [16]. Early distinction from simple cellulitis is often difficult, distinguished by "out-of-proportion" pain. Thrombocytopenia may be seen, which mandates further investigation to establish disseminated intravascular coagulation. Liver function tests show derangement, both with regard to raised bilirubin and transaminases. Serum creatinine phosphokinase levels are elevated, consistent with myalgia and myositis. Renal functions are deranged, representing a prerenal effect, signifying Skin pain-continuous, severe Vesiculobullous formation Table 25. Renal tubular necrosis may ensue if blood pressure correction is not done with alacrity. Dyselectrolytemia is common, with serum calcium levels showing significant reduction [14]. Also, muscle sonography and magnetic resonance imaging may need to be done for pyomyonecrosis. They may show spongiosis, necrotic keratinocytes in the epidermis, and moderate dermal perivascular polymorphonuclear and lymphocytic infiltrate. Staphylococcus aureus, Streptococcus pyogenes: Isolated from a well-defined focus of infection. Having said that, the overall global mortality still rests between 7% and 12% in toxic staphylococcal syndrome. General measures for managing septic shock and acute skin failure must be followed irrespective of the etiological type. It is immune to the inoculum stage [24,25] and acts as a superpotent suppressor of bacterial toxinogenesis. All in all, it acts as a potent immunomodulator in addition to its antibacterial action.
Purchase discount isoniazid on line
Symptoms of urethritis in women are similar to those in men medications causing gout buy cheap isoniazid 300mg on-line, including increased frequency of urination and dysuria characterized by pain, discomfort, or burning during urination (Stamm et al. During initial colonization of the cervix, local inflammation with or without mucopurulent discharge is diagnosed as clinical cervicitis. Symptoms are typically nonspecific, such as itching, vaginal discharge, friable, easily bleeding cervical ectopy, dyspareunia, and intermenstrual bleeding. Importantly, more than 70% of initial infections are asymptomatic, and during physical examination a normalappearing cervix is observed in up to 90% of women with asymptomatic chlamydial infection (Geisler et al. Ascending infections can also be asymptomatic, causing chronic damage and inflammation that may directly lead to infertility or subfertility. Some studies have suggested that endometriosis may be linked to chlamydial infection (Debattista et al. Acute salpingitis may result in longterm adverse events, including peritubal adhesions, postinflammatory fibrosis, and tubal occlusion leading to infertility. The ovaries have multiple functions in female fertility, including the production of the hormones estrogen and progesterone, required for regulation of the menstrual cycle, and the development of mature oocytes. In contrast, in women reported as good responders, only 30% reported detectable serum antichlamydial IgG (Keay et al. While the direct role of Chlamydia infection on ovarian function in humans is yet to be determined, recent studies reported that in the absence of clinically confirmed tubal pathology, a reduction in the rate of spontaneous pregnancy was observed in Chlamydia seropositive women (Coppus et al. Further, seropositive women with no clinical evidence of tubule damage or occlusion have a 35% reduction in Chlamydia Trachomatis Urogenital Infections: Epidemiology, Clinical Presentations, and Pathogenesis 141 fecundability (Steiner et al. These data suggest that infection disrupts ovarian function, leading to subfertility. In summary, chronic chlamydial infection can impair female fertility by multiple mechanisms, involving inflammatory responses that damage the fallopian tubes and impair ovarian function. The direct role of infection is unclear by may be associated with miscarriage, still births, and preterm labor (Baud et al. Vertical transmission has significant effects on the neonate, causing infection of the conjunctivae, nasopharynx, rectum, and vagina (Hammerschlag et al. Prior to the introduction of systematic prenatal screening programs, vertical transmission of Chlamydia was the most common infectious cause of neonatal conjunctivitis in the United States (Hammerschlag et al. Chlamydial pneumonitis may adversely affect respiratory functions well into adulthood and also exacerbate asthma (Hansbro et al. The urethra is considered the initial site of Chlamydia infection, which can cause urethritis. Urethritis is the inflammation of the urethra and symptoms include a yellow purulent discharge, mucus with pus, or just clear mucus at the penile meatus. However, large variations in rates have been observed, depending on the type of diagnostic tests used (Bakare et al. Chlamydial infection of the prostatic urethra has been described and was associated with inflammation and presence of bullous lesions in patients with asymptomatic gross hematuria (Kamura et al. While untreated infections may persist, spontaneous resolution of infection commonly occurs (Geisler 2010). The prostate is a small gland surrounding the urethra that produces fluid that facilitates sperm viability and transport, contributing approximately onethird of seminal plasma. Further, males with Chlamydia associated chronic prostatitis reported a three times higher prevalence of premature ejaculation (Cai et al. Chlamydia trachomatis infections account for 31% of cases of epididymitis and are the most common cause in men under 35 years of age (Ostaszewska et al. The primary role of the epididymis is to facilitate the final stages of spermatozoa maturation. As such, inflammation from infection poses significant risk to developing spermatozoa and male fertility. The infection of the testes, leading to orchitis, commonly occurs in conjunction with epididymitis (Mulcahy et al. Like infection of the genital tract, anorectal infections are also often asymptomatic. However, symptoms of anorectal infection may include anal pain, pruritus, bleeding, diarrhea, mucoid discharge, anorectal erythema, discharge or ulceration. This suggests that rectal infections may result from cross contamination with vaginal secretions and is supported by the observation that rectal infection has been reported in women who do not engage in anal sex (Barry et al. This has been demonstrated in parrots/parakeets, sheep, cattle, goats, pigs, and in mice and guinea pigs following experimental infection (reviewed in (Rank and Yeruva 2014)). In most studies, cases of rectalonly carriage were found, and importantly, there was often no correlation between selfreported anal sex and rectal Chlamydia. In infants born to Chlamydiainfected mothers, Schachter and colleagues (1986) found rectal and vaginal infections in 14% of infants and Bell et al. This results in either inguinal syndrome (inflammation of the inguinal lymph nodes) following primary infection of the anterior vulva, penis, or urethra; or anorectal syndrome after primary infection of the posterior vulva, vagina, or anus. This second phase is typically associated with painful symptoms including unilateral lymph node enlargement, inflammation, suppuration, and abscesses in twothirds of patients. Symptoms may also include systemic lowgrade fever, chills, malaise, myalgias, and arthralgias. The third stage is characterized by chronic inflammation and tissue destruction, resulting in the formation of perirectal abscess, fistulas, strictures, and stenosis of rectum. Hemorrhoidlike swellings called lymphorroids may develop, resulting in the obstruction of perirectal and intestinal lymphatics. A resulting chronic edema and sclerosing fibrosis may lead to strictures and fistulas that can cause elephantiasis of the genitals, with penile and scrotal edema and distortion in males, and chronic ulcerative disease of vulva leading to disfiguring fibrosis and scarring in females. The immunological hypothesis posits that an adaptive immune response (delayed type hypersensitivity and/or antibody) by immune T and B cells against chlamydial antigens that have high homology with host antigens is the cause of tissue destruction (Brunham and ReyLadino 2005). The cellular hypothesis proposed by Stephens (2003) posits that tissue damage is due to an overproduction of inflammatory mediators by the infected tissue cells, resulting in an overexuberant innate immune response. The chlamydial heatshock protein 60 (Hsp60) has been proposed as the major candidate antigen that drives pathogenic Tcell responses and potentially anti Hsp60 antibodies as the main cause of tissue destruction under the immunological hypothesis. However, the weight of evidence to support this antigen as a driver of tissue damage is not strong (reviewed in (Stephens 2003; Murthy et al. These mediators may directly damage tissues and/or recruit inflammatory cells that further drive tissue damage as a rapid influx of inflammatory cells is a hallmark of both acute infection and reinfection. In young women, however, cervical ectopy is a common physiological process, where the columnar epithelium of the endocervix protrudes into the vaginal lumen. In mouse models, chlamydial infection of the fallopian tubes (termed oviducts in mice) leads to a rapid influx of neutrophils, which are associated with irreversible scarring and complete blockage of the tubules rendering the mice infertile Chlamydia Trachomatis Urogenital Infections: Epidemiology, Clinical Presentations, and Pathogenesis 147 (Shah et al. However, neutrophil quantity and duration of recruitment directly correlates with oviduct occlusion (Darville et al. Although macrophages appear to play an important role in chlamydial infection and pathogenesis, further research is required. This can affect sperm production and quality, sperm storage and maturation in the epididymis and the function of the accessory glands such as the prostate. Infection of the prostatic urethra was associated with inflammation and presence of bullous lesions in patients with asymptomatic gross hematuria (Kamura et al.
Order 300mg isoniazid with visa
Loss of mismatch repair protein expression in unselected endometrial adenocarcinoma precursor lesions medicine man dispensary order isoniazid online from canada. Mismatch repair protein expression in endometrioid intraepithelial neoplasia/atypical hyperplasia: Should we screen for Lynch syndrome in precancerous lesions K-ras mutations appear in the premalignant phase of both microsatellite stable and unstable endometrial carcinogenesis. Mutation of the Ki-ras protooncogene in human endometrial hyperplasia and carcinoma. Abnormalities of E- and P-cadherin and catenin (beta-, gamma-catenin, and p120ctn) expression in 110 Endometrial premalignant lesions 30. Biopsy histomorphometry predicts uterine myoinvasion by endometrial carcinoma: A Gynecologic Oncology Group study. Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: A Gynecologic Oncology Group study. Significance of concurrent endometrial cancer in women with a preoperative diagnosis of atypical endometrial hyperplasia. Risk of subsequent endometrial carcinoma associated with endometrial intraepithelial neoplasia classification of endometrial biopsies. Endometrial intraepithelial neoplasia with secretory differentiation: Diagnostic features and underlying mechanisms. Pathologic assessment and clinical impacts for endometrial cancer and precursors after progestin treatment. Endometrial intraepithelial carcinoma: A distinctive lesion specifically associated with tumors displaying serous differentiation. A clinical and pathologic comparison between stage-matched endometrial intraepithelial carcinoma and uterine serous carcinoma: Is there a difference. Endometrial glandular dysplasia: A newly defined precursor lesion of uterine papillary serous carcinoma. Endometrial glandular dysplasia: A putative precursor lesion of uterine papillary serous carcinoma. Occurrence of endometrial glandular dysplasia precedes uterine papillary serous carcinoma. Endometrial glandular dysplasia with frequent p53 gene mutation: A genetic evidence supporting its precancer nature for endometrial serous carcinoma. Endometrial serous carcinoma (uterine papillary serous carcinoma): Precancerous lesions and the theoretical promise of a preventive approach. They are usually associated with unopposed estrogen exposure and are often preceded by precancerous lesions. However, both clinicians and pathologists have gradually encountered problems related to the model. As we understand in general, a low-grade stage 1A endometrioid carcinoma should have almost no risk of recurrence or metastasis and, therefore, no staging procedure is necessary. However, many of us, including gynecologic oncologists and pathologists, have more or less encountered unexpected recurrence or distant metastasis from such cases. From all these perspectives, our pathology diagnosis or classification is beyond perfect. This has resulted in an enhanced understanding of molecular and genetic events, reinforcement of the clinicopathologic subgroups originally defined by histologic and clinical features and development of biomarkers informative in identifying previously unknown or poorly described endometrial neoplastic lesions. Although there is much progress made in the field, gynecologic pathology practice remain focused on morphology with the aid of immunohistochemistry to make correct diagnoses. Molecular analysis for endometrial cancer diagnosis is rarely applied in routine practice. Therefore, we will present general clinicopathologic features of the endometrial cancers followed by descriptions of individual histologic types of the cancer in this chapter. Factors that have been identified as causal in the development of endometrial adenocarcinoma include estrogenic stimulation (exogenous or endogenous), prolonged tamoxifen treatment, family history of endometrial cancer and pelvic radiotherapy. The reported relative risk for endometrial cancer in these women has ranged from 1. The strong epidemiological link between obesity and endometrial cancer has been attributed to endometrial stimulation by endogenous estrogens derived from conversion of androgens to estrogens in the adipocytes of obese women. Although there was a positive association between body mass index and endometrial cancer risk, this was substantially reduced after adjusting for serum estrogen levels. There is also evidence suggesting a strong direct association between endometrial cancer risk and circulating estrogen and androgen levels, which can eventually convert to estrogen in peripheral fatty tissue. Women with these tumors are at increased risk of developing endometrial carcinoma. Estrogen-associated endometrial malignancies have no distinctive pathological features. Most are adenocarcinomas of endometrioid type that develop on a background of endometrial hyperplasia. They tend to present at an early stage, to be well-differentiated and to have a favorable prognosis. Although there are many anecdotal reports of endometrial adenocarcinoma and carcinosarcoma following radiotherapy, a definite causal link between endometrial cancer and radiotherapy has not yet been established. The detailed description about the genetic changes can be found in Chapter 8 and in the section Immunohistochemistry and Molecular Features of this chapter. Therefore, many medical centers in the world have instituted universal tumor-screening protocols to identify these patients. Diffuse pelvic pain and abdominal distention, as well as symptoms related to gastrointestinal and ureteral obstruction may occur in patients with more advanced disease. Women with symptoms concerning for endometrial Pathologic characteristics of endometrial cancer / Endometrial carcinoma grading 115 carcinoma are managed with a combination of pelvic ultrasonography, endometrial biopsy and/or dilatation and curettage. Ultrasound is used to measure the endometrial stripe to assess for endometrial thickening; however, the predictive value of the endometrial thickness is relatively low. Detection rates can be increased by performing a hysteroscopic-guided biopsy, but the overall detection rate does not increase significantly compared with routine endometrial curettage. Treatment of endometrial carcinoma is mainly surgical, including total hysterectomy and with or without bilateral salpingo-oophorectomies. Staging procedure including dissection of pelvic and sometimes para-aortic lymph nodes is also performed, although this can be avoided for low-grade, minimally invasive tumors. Adjuvant therapy is recommended in patients with advanced disease but has a less clear role in patients with low-stage tumors. Hormonal management can be applied for poor surgical candidates and women who strongly desire to preserve fertility. When a mixed tumor is encountered, a 10% contribution of each histologic type of cancer is required. It is important to note that severe cytologic atypia should include large pleomorphic nuclei, coarse nuclear chromatin and large irregular nucleoli in more than 50% of the tumor sample. These include cancer grading, depth of myometrial invasion including the patterns of invasion, endocervical invasion (stromal versus mucosal), lymphovascular space invasion, peritoneal ascitic fluid status, margin status, regional lymph node metastasis and distant metastasis. We will describe these pathologic characteristics prior to the discussion of individual histologic types of endometrial cancer as follows. An intact endomyometrial junction should have a relatively smooth and even border. The differences between stromal metaplasia and myometrial invasion is summarized in Table 9. Localizing the endometrial-myometrial junction can be problematic when the normal architecture has been distorted by tumor. Invasion is estimated by measuring the deepest point of tumor infiltration from the level of the endometrial-myometrial junction. This is ideally performed on a full-thickness endomyometrial tissue section that includes the deepest point of invasion, adjacent normal endometrial-myometrial junction and the uterine serosa. When endomyometrial thickness is thicker than 3 cm, a slender bisected section is taken to fit a single cassette or two usual bisected sections are submitted in two consecutive separate cassettes. In reality, however, it is complex due to the following compounding factors: irregular endomyometrial junction, presence of adenomyosis and specific invasive patterns. This complexity is reflected in the relatively high interobserver variability in diagnosing endometrial cancer invasion. Junction between the endometrium and the myometrium in normal uteri is usually irregular. There is loss of stroma and basal glands between the cancerous area and the myometrium. There are many stromal cells with fibroblastic metaplasia between the cancerous glands.
Buy isoniazid with paypal
Centralized monitoring processes provide additional monitoring capabilities that can complement and reduce the extent and/or frequency of onsite monitoring and help distinguish between reliable data and potentially unreliable data medications peripheral neuropathy buy isoniazid 300mg online. Clinical Trial/Study Reports l the sponsor should ensure that the clinical trial reports are prepared and provided to the regulatory agency whether the trial is completed or prematurely terminated. Stakeholders, Resources, and Documents in Clinical Research Chapter 25 371 Regulator the regulatory authority. In this process, the sponsor works with the regulator to submit an application or investigational new drug/new drug application for the new product. The regulator carefully evaluates the submitted documents, which then leads to either approval or rejection. If the regulator discovers any problems of noncompliance, a warning letter may be sent mentioning corrective action that must be taken immediately by the stakeholder responsible. Participants (Subject/Trial Subject) An individual who participates in a clinical trial, either as a recipient of the investigational product(s) or as a control. Ask questions if they do not understand something about the study or their rights and responsibilities as a research participant or need more information. Carefully weigh the risks and benefits when deciding whether to participate in the study. Refrain from signing the consent document until they believe that they understand its content and feel comfortable with their decision to participate. Follow directions for proper use, dosing, and storage of self-administered study medications, providing biological samples and preparing for tests, procedures, or examinations. Follow directions for abstaining from nonstudy-related medications or other contraindicated medications or procedures. This is particularly important for an intervention trial that has a follow-up period after the intervention is completed. Show up at scheduled appointments on time and inform the staff within a reasonable time if they need to reschedule an appointment. Provide truthful answers to questions asked during screening/enrollment and during the study. Report pain, discomfort, nausea, dizziness, and other problems and symptoms they experience during the study. If they decide to withdraw from the study, inform the staff, and follow the procedures for withdrawal. It also serves to protect the rights, integrity, and confidentiality of trial subjects. Documents in Clinical Trials Documents are an essential part of the clinical trial where every activity performed in a clinical trial is captured. Data are recorded in these documents timely, which are usually audited by the sponsor and inspected by the regulatory authority to confirm the integrity of collected data and validity of the trial conducted. Before the final close out of the trial, the monitor reviews both investigator/institution and sponsor files to confirm all documents are placed in appropriate files. These documents should be available for sponsor audits and regulatory inspections. The sponsor and investigator/institution should record the location where all essential documents, including source documents, are placed. The storage system used during the trial and for archiving (irrespective of the type of media used) should provide for document identification, version history, search, and retrieval. These documents should be supplemented or reduced (if not important and relevant), in advance of trial initiation. The investigator/institution should have control of all essential documents and records generated by the investigator/institution before, during, and after the trial. This brochure contains the relevant and current scientific information that is provided to the investigator and other members involved in the trial before initiation of the clinical trial. This information may aid in recognizing and treating possible overdose and adverse drug reactions. The purpose is to thoroughly familiarize the investigator with the appropriate use of the investigational product(s), its possible risks and adverse reactions, specific tests, observations, and precautions that may be needed for a clinical trial. The protocol is shared with the investigator to make him/her thoroughly familiar with the appropriate use of the investigational product(s), which is then signed by the investigator for agreement with the sponsor. The whole clinical trial has to be conducted in compliance with the approved protocol. If there is any noncompliance with the protocol in the study, it is explained and documented by the designated person. The informed consent form is the document where every aspect of the trial is written, which is signed and dated by the subject voluntarily and the form is documented along with any written information provided to the subject. A copy of the signed and dated written informed consent form and any other written information is provided to the subjects before and during conduct of the trial. The informed consent form must be in a language that is easy to understand by the subject and should be signed before participating in the trial. An impartial witness is required during the discussion of informed consent if a subject or legally acceptable representative is unable to read. The trial treatment(s) and the probability for random assignment to each treatment. The reasonably foreseeable risks or inconveniences to the subject and, when applicable, to an embryo, fetus, or nursing infant. When there is no intended clinical benefit to the subject, the subject should be made aware of this. The alternative procedure(s) or course(s) of treatment that may be available to the subject, and their important potential benefits and risks. The compensation and/or treatment available to the subject in the event of trial-related injury. The anticipated prorated payment, if any, to the subject for participating in the trial. The records identifying the subject will be kept confidential and, to the extent permitted by the applicable laws and/or regulations, will not be made publicly available. The person(s) to contact for further information regarding the trial and the rights of trial subjects, and whom to contact in the event of trial-related injury. These measures will result in reduced query generations and improved data integrity. This indirectly informs the data recorder where to write/enter the response and helps to differentiate it visually from the entry fields for other questions Separate the columns with thick lines Provide bold and italicized instructions Minimize free-text responses Position only specified density of questions on each page Page numbering if necessary should be consistent throughout Avoid using "check all that applies" as it forces assumptions about the clinical data Specify the unit of measurement Indicate the number of decimal places to be recorded Use standard data format. Hence, the field corresponding to this question on the module for the particular visit would have the options "yes" or "no. This is the final report submitted to the regulatory authority with document results and interpretation of the trial. Compliance with the guidelines in every aspect, including documentation, is essential. After changing the document, all the subjects should be reconsented and the whole procedure should be documented in source notes. Case Exercise 2 In a pharma drug trial, the subject had participated in the study. The subject gave his consent, but is illiterate; the subject had been accompanied by his son (blood relative). Once involved primarily with dispensing and compounding medications, pharmacists worldwide are increasingly serving as medication experts working as members of interprofessional healthcare teams. Governments and academic institutions increasingly need to reevaluate pharmacy education and the methods used to measure, assure, and improve academic quality. The Action Plan encourages the development of educational systems designed to produce a pharmacy workforce competent to deliver healthcare services that are aligned with the local needs of the country. The Action Plan provides evidence-based guidance and frameworks that can be used to advance pharmacy education and encompasses four domains of action including: (1) development of a vision and framework for education development; (2) development of a competency framework; (3) ensuring a quality assurance system; and (4) building academic and institution capacity. Within healthcare, the quality assurance process supports and facilitates improvements in practice because educational institutions are expected to modify the education provided in an effort to address advances in knowledge and practice. Framework-Based Quality Assurance Systems Development Quality assurance systems vary greatly between countries.
Discount 300 mg isoniazid amex
Mast cell and eosinophil distribution and activation in human endometrium throughout the menstrual cycle medicine 319 pill buy 300mg isoniazid overnight delivery. Polymorphonuclear leukocytes in the endometrium during the normal menstrual cycle. Endometrial plasma cells: Do they indicate subclinical pelvic inflammatory disease Flow cytometric analysis of leukocytes in the human female reproductive tract: Comparison of fallopian tube, uterus, cervix, and vagina. Chronic endometritis: A combined histopathologic and clinical review of cases from 2002 to 2007. Pregnancy outcomes in women with chronic endometritis and recurrent pregnancy loss. Routine antibiotic prophylaxis after normal vaginal birth for reducing maternal infectious morbidity. Xanthogranulomatous endometritis: A challenging imitator of endometrial carcinoma. Female genital tuberculosis- A retrospective clinico-pathologic study of 501 cases. Granulomatous endometritis associated with histologically occult cytomegalovirus in a healthy patient. Ligneous cervicitis and endometritis: A gynaecological presentation of congenital plasminogen deficiency. Polypoid nodular histiocytic hyperplasia associated with endometrioid adenocarcinoma of the endometrium: Report of a case. These descriptive terms replace previous terms that were poorly defined such as menorrhagia, metrorrhagia, polymenorrhea, menometrorrhagia and dysfunctional uterine bleeding (Table 5. It is a classification of potential causes of abnormal uterine bleeding but recognises that although women may have one or more entities, those may be asymptomatic and not contribute to the abnormal bleeding. The morphological picture on its own may be inadequate for a definitive diagnosis. There are no specific morphological features attributable to dysfunctional uterine bleeding and the cause of bleeding in these women remains obscure. The luteal phase inadequacy may be spontaneous or induced by endocrine manipulation strategies such as those used for ovulation induction. A reason for performing endometrial biopsies in two different menstrual cycles is that they can be at variance: an out-of-phase biopsy followed by an in-phase biopsy or vice versa can be seen in about 50% of women being investigated for infertility. Chronological dating should be assigned prospectively rather than retrospectively to avoid inaccuracies caused by the variable length of the luteal phase and the accelerated onset of menses induced by the procedure. Most commonly, the endometrium shows a general lag in glandular and stromal maturation in relation to the presumed day of ovulation. Even in these cases, caution is advised in making this diagnosis given that there is significant observer variation in endometrial dating and considerable anatomical variation in endometrial morphology. The frequency of anovulatory cycles is unknown, but they are common at the extremes of reproductive age just after the onset of menarche and in the perimenopausal period. The endometrium in an anovulatory cycle is subjected to the stimulus of a relative estrogen excess that is unopposed by progesterone. Thus, the endometrium shows persistent proliferative activity at a time of the cycle when a secretory a pattern would be expected, even at the time of menstruation. Caution must be exercised as the proliferative phase can be as long as 22 days in some women. This has led some to use the term disordered proliferative endometrium or, preferably, proliferative endometrium with features of anovulation (see Chapter 8). The resultant endometrial morphology depends on the state of the endometrium at the time this estrogen supply is compromised. If no estrogen has been forthcoming from menarche, a hypoplastic endometrium will result. The loss of estrogen stimulus for a long time in a previously normal endometrium will result in an atrophic endometrium. If estrogen levels are low, the endometrium may be weakly proliferative or inactive. Primary ovarian disease such as premature ovarian failure or ovarian failure secondary to irradiation or ovariectomy will also result in a lack of estrogen. Hypopituitarism and other endocrine disorders such as hyperprolactinemia, which leads to suppression of luteinizing hormone so that ovarian follicles mature but fail to rupture, will also result in low estrogen levels. Hypothalamic dysfunction can result from severe malnutrition, anorexia nervosa, severe stress and other debilitating illness; athletes, particularly those involved in endurance events, have abnormal hypothalamic pulsatility. The presentation of these women may differ according to their age, duration and severity of disease. Commonly, they may have delayed puberty, delayed menarche, absent or infrequent periods or infertility. These appearances are thought to be due to persistence of the corpus luteum with continued progesterone production resulting in delayed and prolonged menstrual bleeding. It has been suggested that many of these cases of irregular shedding of the endometrium are in fact nothing more than very early pregnancy losses occurring at the time of menstruation or the loss of the endometrium prepared for a blastocyst that did not implant, the blastocyst being responsible for the luteotrophic maintenance of the corpus luteum. Clinical review: Adolescent anovulation: Maturational mechanisms and implications. Agerelated changes in luteal dynamics: Preliminary associations with antral follicular dynamics and hormone production during the human menstrual cycle. Formulations of the oral contraceptive pill may be monophasic, delivering the same amount of estrogen and progestin; biphasic, delivering the same amount of estrogen each day while the progestin dose is increased halfway through cycle; triphasic, with three different doses of progestin and estrogen that change approximately every seven days; or quadriphasic which has an estrogen step-down and progestin step-up sequence. Most formulations have 21 active and 7 inactive pills, to mimic the menstrual cycle, with withdrawal bleeding occurring in the last 7 days. The glands are lined by cuboidal epithelial cells lacking nuclear pseudostratification and mitotic activity. They are also used in the management of endometriosis and for contraception in women for whom estrogens are contraindicated. Progestin contraception is administered orally, parenterally as subdermal implants or as a medicated intrauterine device. High-dose progestin-only contraception, such as the injectable depot medication, inhibits follicular development and ovulation as well as having effects on cervical mucus and endometrial thickness. Intermediate-dose progestincontaining implants are inserted subdermally and can be left in situ and are effective for up to three years. Progestinonly contraception can be delivered also through intramuscular injection of a higher dose of a progestin, such as medroxyprogesterone acetate. The effects of progestin treatment on the endometrium depend partly on duration of treatment, partly on the dose and type of progestin used. Progestin treatment is characterised by suppression of endometrial growth, variable endometrial stromal pseudodecidualization and increase in the number of granulated lymphocytes within the endometrium. Microscopic examination in the early stages of treatment shows endometrial glands without mitotic activity and secretory features while the stroma may be edematous. Prolonged use leads to profound endometrial glandular atrophy and florid stromal pseudodecidualization. Depomedroxyprogesterone acetate results in endometrial atrophy after six months use. Various levonorgestrel-releasing intrauterine contraceptive devices are licensed for use as contraceptives and also used for treatment of heavy periods for which no underlying abnormality has been found. The dose of levonorgestrel released directly into the endometrium differs between the different products, which can be left in situ for between three and six years, depending on the product, although likely to be effective beyond the approved duration. Nonmedicated intrauterine contraceptive devices made of plastic or copper and plastic have long been used for contraception. There may be ulceration of surface epithelium, and adjacent glands may show epithelial regenerative changes.
Elaeis melanococca (Palm Oil). Isoniazid.
- What is Palm Oil?
- Vitamin A deficiency.
- Are there safety concerns?
- Decreasing symptoms of malaria.
- How does Palm Oil work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97083
Cheap 300mg isoniazid with amex
Endometrial biopsy should be abandoned as a routine component of the infertility evaluation medicine 93 2264 buy generic isoniazid pills. Diagnosis of endometrial-factor infertility: Current approaches and new avenues for research. There is then an interval of about six days before the blastocyst, having developed from the zygote through the morula stage in its passage through the fallopian tube, embeds in the endometrium. Thus, at about seven days post ovulation, or at about 21 days of a normal 28-day cycle, the blastocyst implants interstitially within the stroma between the glands of the endometrium. At this time the glands are at the peak of their secretory activity, but the stroma has not shown pre-decidualization yet. Gonadotrophin production by the primitive trophoblast of the blastocyst begins possibly before, but at the latest at the time of, implantation of the blastocyst. Thus, the corpus luteum comes under the influence of the luteotrophic hormones and does not involute as it would do in the absence of a conceptus. Further development of the corpus luteum results in higher levels of plasma progesterone, which sustain the endometrium and lead to the formation of a true decidua. The term is now restricted to the transformed stromal part of the gestational endometrium and to similar mesenchymal tissue elsewhere in the genital tract and, occasionally, outside it, during pregnancy. Decidualization is associated with a marked increase in uterine natural killer cells. The changes produced in the endometrium by prolonged administration of progestins can be termed pseudodecidua. Large numbers of uterine natural killer and myelomonocytic cells and smaller numbers of T cells accumulate, particularly around infiltrating trophoblast cells. This population of interstitial and endovascular trophoblast, sometimes also called intermediate trophoblast, is a mixture of mononuclear cytotrophoblast, multinuclear syncytiotrophoblast and cells that are truly intermediate in form. One of the prime functions of the proliferating cytotrophoblast is to open up the decidual terminations of the spiral arteries. By the 12th day (conceptual age) of pregnancy, there is a system of well-developed lacunae in the trophoblastic syncytium of the implanted embryo. The spiral artery already shows transformation into the uteroplacental artery with intraluminal endovascular trophoblast present. With increase in the extent and depth of trophoblastic invasion, it would seem that the maternal vessels are eroded progressively back to the level of arterioles and venules, thus permitting a through circulation. Prior to the full establishment of circulation, nutrition to the developing conceptus is histiotrophic, being derived from secretions from the endometrial glands. These endovascular trophoblastic plugs restrict the flow of red blood cells into the developing placenta and the relative hypoxemia protects the conceptus from oxidative damage from free radicals. The endovascular trophoblastic cells replace the endothelium and cause much damage to the vessel wall such that the muscular and elastic tissues within the arterial walls are replaced by fibrinoid material. This also corresponds to the approximate time when the conceptus switches from histiotrophic to hematotrophic nutrition. Endovascular trophoblast is present within the lumina of both spiral arteries and has formed a plug in the artery on the right. Some endovascular trophoblastic cells are seen embedded within the fibrinoid matrix of the uteroplacental arterial wall. With further extension of the invading syncytium and more dilatation of blood vessels, the blood supply of the lacunae comes from venous sinusoids. Several spiral arteries are present in the vicinity of the implantation site but with no connections between them, and the lacunar spaces are found in conceptuses at the presomite embryo stage. Placentation 23 cells to permit controlled invasion during placentation so the arteries are effectively transformed by the trophoblast and yet prevent undue penetration of the uterus. The morphological transformation of the spiral arteries from muscular vaso-reactive arteries into compliant distensible arteries provides an increasing blood supply to the growing placenta and conceptus. The first stage, between approximately 6 and 12 weeks of gestation, is limited generally to the intradecidual portions of the spiral arteries and, after a relatively quiescent period, a renewed migratory phase takes place between approximately 16 and 22 weeks of gestation, transforming the myometrial portions of the spiral arteries. The spiral arteries in the decidua vera do not undergo these physiological changes as the extravillous trophoblast migrates only into the decidua basalis from the cytotrophoblastic shell and anchoring villi. Indeed, the decidua vera is distinguished from the basalis by the absence of the extravillous trophoblast, physiological changes or fibrinoid deposition (Summary Box 3. The hatched lines in the intramyometrial and intradecidual segments of the spiral arteries indicate physiological vascular changes, which extend from the origins from the radial arteries to the openings in the intervillous space. The relative proportions of pregnancy tissue, viz decidua, placenta and embryo/fetus, vary depending on the gestational age. Various methods of correlating weight or volume of the conceptual products with complete removal of the gestation have been described, but these are not flawless. Gross examination alone can be unreliable also and is clearly dependent on the experience of the observer and lacks permanent documentation of an intrauterine pregnancy. Universal histological examination of ostensibly normal tissue from induced abortions is difficult to justify because of the large numbers. The theoretical possibility that an occasional abnormal conceptus, such as a molar pregnancy, may be missed does not seem to be a reasonable justification for routine examination because of the low prevalence of molar pregnancy in the population and the frequency that a molar pregnancy will progress to persistent gestational trophoblastic disease. The lay public, however, tends to equate the term abortion with one which is induced, therapeutically, self or criminal, whereas the term miscarriage to them means spontaneous abortion. Spontaneous abortion is usually defined as the involuntary loss of a conceptus before the fetus has attained viability. This seemingly simple definition can be challenging: firstly, the gestational age at which the fetus attains viability is Abortion / Tissue from spontaneous abortions 25 is obtained at termination of pregnancy, then it should be sent for histological examination to confirm successful termination. A cautionary note is that fibrillary tissues that look like villi under the dissecting microscope may sometimes be friable decidua only on histological examination. Little is known about the outcome for an eutopic pregnancy following a procedure for terminating the pregnancy if all tissue examined identifies no products of conception histologically. Immunohistochemistry using anti-human placental lactogen or anti-keratin antibodies can help in the identification of the extravillous trophoblast. It has been claimed that these are so specific that, when present, intrauterine pregnancy can be ruled in. Women may be managed expectantly, dependent upon symptoms and amount of blood lost, or be managed actively, where the uterine cavity is evacuated formally under anesthesia as it is not possible often to decide whether the abortion has been complete or incomplete. The amount and nature of the material depends upon the gestation, the method of management of the miscarriage and the timing of the abortal tissue in relation to the abortion or fetal demise. The material may include a complete gestational sac with or without a dead fetus and curettings from the uterus. The examination of the fetus and the gestational sac is out of the scope of this monograph. Instead, attention will be concentrated on the histology of the curettage specimens commonly received in the laboratory. In the majority of cases, there is little difficulty in confirming the diagnosis of an abortion or retained products of conception. In many early miscarriages, the failure of embryonic development, together with deficient placental growth, results in the majority of the products of conception consisting of decidua only. Undue emphasis is given to the finding of chorionic villi in uterine curettings, but the presence of villi, per se, does not indicate necessarily an intrauterine pregnancy: it is possible that they are derived from a tubal pregnancy that has aborted spontaneously into the uterine cavity. The only absolute confirmation of an intrauterine pregnancy is the finding of implantation-site changes in the intrauterine decidua. Features of the chorionic villi or decidua to predict if the miscarriage is chromosomally normal are neither specific nor sensitive enough to be of use clinically. The endometrial histology subsequent to a miscarriage is seldom examined unless there is persistent bleeding. In the first two menstrual cycles after miscarriage, curettage findings include proliferative endometrium, proliferative glands with decidualized stroma, endometritis and luteal insufficiency. A true decidua is formed with the appropriate changes within the stroma and glands. In the absence of an intrauterine conceptus, the secondary changes in the gestational endometrium are not seen. Thus, there is no trophoblastic infiltration, fibrinoid matrix deposition or vascular reaction. Curettage material obtained from women with ectopic pregnancy can be quite varied: decidual reaction, secretory endometrium and proliferative endometrium can be encountered. The decidua will show a variable degree of necrosis and cellular infiltration admixed with blood clots or a picture of irregular shedding because of the slow involution of the corpus luteum. If the interval between the embryonic or fetal loss and curettage is long, the original decidua may have disappeared altogether to be replaced by proliferative endometrium and, because the first few cycles may be anovulatory, it is not uncommon to find the characteristic mildly hyperplastic endometrium of the anovulatory cycle.
Discount isoniazid 300 mg with mastercard
Definitive identification to genus and species level can be obtained by immunofluorescence symptoms 8 days after iui 300 mg isoniazid with visa, culture method, or both. Treatment for acanthamebiasis in vivo has not been available, although ketoconazole, flucytosine, pentamidine, sulfadiazine, and polymyxin B were known to be effective in vitro [50]. Bacillary angiomatosis Bacillary angiomatosis is characterized by proliferative vascular lesions, is caused by Bartonella henselae and B. Domestic cat (Felis domesticus) and human body louse (Pediculus humanus) are the transmission vectors for B. Internal organ involvement may result in biliary obstruction and jaundice, gastrointestinal bleeding, encephalopathy, laryngeal obstruction, and asphyxiation. The illness responds well to antibiotic therapy but runs a chronic progressive course in untreated patients and may be fatal [43]. Flesh-colored papules, nodules, pedunculated lesions, and hyperkeratotic, indurated plaques are the usual Schistosomiasis Schistosomiasis (bilharziasis) is a serious systemic parasitic infestation by trematodes of the genus Schistosoma (blood flukes) [52]. During Rickettsial infections 271 exposure to contaminated lakes/rivers in an endemic area, free-swimming cercariae penetrate the human skin and reach the venous circulation within 24 hours and via the portal system are carried to the veins around the rectum, colon (S. Initially, it occurs during the penetration phase presenting as pruritic erythematous maculopapular eruptions (acute cercarial dermatitis) which last for hours to 1 week. Sometimes, ova embolize via the paravertebral venous plexus and get deposited in ectopic sites such as dermis, known as bilharziasis cutanea tarda [54]. Systemic complications arise once the ova initiate granulomatous inflammation in the tissues around veins. S haematobium affects the bladder leading to hematuria, hydronephrosis, and even carcinoma of bladder. Eosinophilia supports the clinically suspected cases, but definitive diagnosis depends on the identification of eggs in stool or urine, biopsy (skin, rectal, or bladder), and serology. Abdominal ultrasonography, endoscopy, and barium enema play an integral role in hepatic and intestinal schistosomiasis [54]. Cutaneous lesions are morbilliform, scarlatiniform, or hemorrhagic, concentrated over the trunk. Desquamation, erythema nodosum, and infarcts may be seen on distal extremities in children. Diagnosis requires a high index of suspicion based on history and physical examination. Early administration of suitable antibiotics, restoration of fluid, and correction of electrolytes, especially hypokalemia, are necessary to reduce mortality. Penicillin G is the drug of choice, and ampicillin, amoxicillin, and doxycycline are other alternatives. The prognosis is good if antibiotics are started within 4 days of onset of symptoms [58]. The organism is endemic in parts of North, Central, and South America [61] and is prevalent in various parts of India [62]. Rash first appears on hands and feet as small, blanchable erythematous macules and spreads centripetally to involve extremities and trunk. Soon, macules develop central petechiae and may progress to skin necrosis and gangrene, requiring amputation [63]. It is more common in developing tropical countries with high rainfall and poor socioeconomic and sanitary conditions. Adult men engaged in recreational water activities or working in sewers, farms, and mines are more affected [57]. It enters into the blood circulation through abraded skin, mucous membranes, or the gastrointestinal tract [58]. Laboratory diagnosis is usually made by documenting a positive serological test for antirickettsial antibodies by indirect immunofluorescent antibody test, latex agglutination, or enzyme immunoassay. Seroconversion usually occurs by the second week of illness, and hence, serology has a limited role in initial treatment. Immunohistochemical staining of a skin biopsy sample is another useful means of diagnosis and offers quick results [64]. The drug of choice for treatment is doxycycline at a dose of 100 mg twice daily for adults and 2. Suspicion of diagnosis is important when patients present with characteristic features in endemic regions. Epidemic typhus Epidemic typhus is a potentially lethal, louse-borne, exanthematous disease caused by Rickettsia prowazekii. The infection is transmitted to human beings by the body louse Pediculus humanus corporis. The organisms cause damage to endothelial cells, resulting in multiorgan vasculitis. Involvement of end arteries may result in gangrene of the distal extremities, nose, earlobes, and genitalia. In severe cases, vasculitis may result in coma, multiorgan system failure, and death. The mortality rate in untreated, otherwise healthy patients may reach 20%, but may reach as high as 60% in elderly debilitated patients [65]. Other common associated findings include severe myalgias, arthralgias, and nonspecific constitutional symptoms (malaise, anorexia, chills). Central nervous system involvement is very common, and delirium, coma, and seizures may develop. Early administration of doxycycline is recommended in patients with suspected epidemic typhus, even before confirming the diagnosis. The patient should be investigated to assess severity of internal organs involvement and appropriate supportive therapy should be initiated. Prevention and treatment of louse infestations are the most important preventive measures [67]. Fatal Chromobacterium violaceum bacteraemia in rural Bandundu, Democratic Republic of the Congo. Fatal septicaemia from Chromobacterium violaceum: Case reports and review of the literature. Chromobacterium violaceum infection: A clinical review of an important but neglected infection. Two cases of severe sepsis due to Vibrio vulnificus wound infection acquired in the Baltic Sea. Outbreak of cutaneous anthrax in a tribal village: A clinico-epidemiological study. Update on meningococcal disease with emphasis on pathogenesis and clinical management. Cutaneous Nocardia brasiliensis infection in an immunocompetent host after ovarian cystectomy: A case study. Clinical findings of 40 patients with nocardiosis: A retrospective analysis in a tertiary hospital. Primary cutaneous Nocardia brasiliensis infection isolated in an immunosuppressed patient: A case report. Noma neonatorum from multidrugresistant Pseudomonas aeruginosa: An underestimated threat Sixty-three cases of Mycobacterium marinum infection: Clinical features, treatment, and antibiotic susceptibility of causative isolates. Fatal disseminated Mycobacterium marinum infection with bacteremia in a patient misdiagnosed as pyoderma gangrenosum.
Order isoniazid paypal
Medium vessel involvement is infrequent and is often associated with cryoglobulinemia [8 treatment genital warts discount 300 mg isoniazid,9]. Its histopathology shows perivascular and periappendigeal lymphocytic infiltrate, while lacking the interface changes of lupus erythematosus. Other skin findings can include vitiligo, lichen planus, cutaneous amyloidosis, livedo reticularis, and erythema nodosum [4,5]. Xerosis of skin is the most common Extracutaneous manifestations Patients have dry eyes and dry mouth as a result of lymphocytic infiltration in the lacrimal and salivary glands, respectively (Table 43. Renal involvement most commonly occurs as chronic tubulointerstitial nephritis, while glomerular involvement is associated with poor prognosis. It can lead to symptomatic hypokalemia, which can present as sudden-onset quadriparesis, and can rarely cause respiratory arrest. Its diagnosis can be confirmed by documenting hypokalemia and hyperchloremic metabolic acidosis. Potassium supplementation should be started immediately with careful monitoring [15,16]. The 10-year risk of developing lymphoma has been documented to be 4% in patients with cutaneous vasculitis and/or low C4 levels [17,18]. Apart from vasculitis and hypocomplementemia, the presence of persistent salivary gland enlargement, lymphadenopathy, cryoglobulinemia, glomerulonephritis, and lymphopenia also increase the risk of lymphoma [19,20]. Cryoglobulinemia can be associated with life-threatening systemic vasculitis, such as affecting the kidneys, gastrointestinal, and central nervous system [9]. Skin findings include palpable purpura that can become necrotic and ulcerate, erythematous papules, ecchymoses, dermal nodules, urticarial lesions, livedo reticularis, and digital gangrene [21]. Digital gangrene Digital gangrene may develop as a complication of cryoglobulinemic vasculitis or Raynaud phenomenon. Xerosis-related complications Patients with xerophthalmia often develop blepharitis either due to staphylococcal infection or due to frequent rubbing of the eyelids. A more serious but less frequent complication is corneal ulceration and perforation. Due to reduced salivary secretions, patients with xerostomia are at risk of developing dental caries. Salivary glands can become swollen and are prone to recurrent attacks of bacterial infections, due to impaired salivary flow [4,5,23]. Treatment strategies for different cutaneous manifestations are summarized in Table 43. Drawing from the experience from other rheumatic diseases, hydroxychloroquine is often used for fatigue, muscle, and joint pains. Females are affected more frequently than males (female-to-male ratios range from 3. Usually, it is nonerosive but occasionally erosions and an arthritis mutilans-like picture may develop [40]. Most patients develop an inflammatory myopathy during the course of their disease; however, it is rarely present at the onset of the disease. Pericarditis is the most common manifestation of cardiac involvement, although endocardium (conduction abnormalities) and myocardium can also be involved [43]. Other organ system involvement is milder and less common and includes esophageal dysmotility, trigeminal neuralgia, glomerulonephritis, and cytopenias. Notably, patients have less severe neurological and renal involvement as compared to systemic lupus erythematosus [33,44,45]. Early in the course of the disease, it has cutaneous-predominant findings along with nonspecific constitutional symptoms such as easy fatigability, myalgias, and arthralgias. Raynaud phenomenon is the earliest skin manifestation and is present in almost all patients. Patients can develop painful digital ulcers, and even digital infarcts/gangrene in severe cases. The diagnosis can be confirmed by visualizing the soft-tissue calcification on radiography [56]. Extraglandular organ system involvement can include skin, joints, heart, lungs, gastrointestinal tract, kidney, nervous system, and hematological system. Hydroxychloroquine is often used for musculoskeletal pains, while internal organ involvement is treated with systemic corticosteroids and other immunosuppressives such as methotrexate, azathioprine, cyclosporine, cyclophosphamide, and mycophenolate mofetil. Other options in refractory cases may include plasmapheresis and stem cell transplantation. Pulmonary artery hypertension requires treatment with endothelin receptor antagonists (bosentan, ambrisentan), phosphodiesterase-5 inhibitors (sildenafil, tadalafil), and/or prostacyclins [33]. Antiphospholipid syndrome: Clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. The prevalence and incidence of mixed connective tissue disease: A national multicentre survey of Norwegian patients.