Cheap keftab 250mg with mastercard
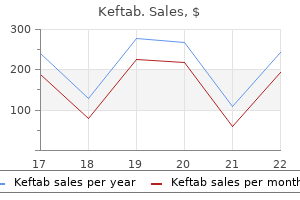
An evidencebased approach to treatment is achieved using detailed investigation to identify the cause of heart failure and the extent of structural and functional abnormalities virus x 1948 buy discount keftab 375mg on line. All Stage C and D patients should be jointly assessed by a multidisciplinary heart failure team including the surgeon. Significant comorbidity, particularly renal and hepatic status, must be taken into consideration before embarking on a particular procedure. Ischemic cardiomyopathy the ischemic cardiomyopathy ventricle contains microenvironments of necrosis or scar tissue together with viable myocardial cells in varying proportions. When more than 50% of the myocardium is impaired, increased wall tension causes subendocardial ischemia, which precipitates left ventricular failure. The relationship between the extent of myocardial infarction, degree of left ventricular dysfunction, and late mortality was defined by Yoshida and Gould. If stunning occurs frequently with incomplete recovery of contractile function, this triggers the development of hibernation. These patients often have marked ischemic dysfunction in non-scarred parts of the ventricles, which can be helped by revascularization. Others have moderate or severe cardiomegaly, reduced cardiac index, and substantial elevation of right atrial pressure with hepatomegaly and fluid retention. The vast majority of patients with ischemic cardiomyopathy are older than 65 years, are smokers with chronic obstructive airways disease, and have peripheral vasculopathy. They often have renal impairment and will never be considered for transplantation. In turn, less than 10% of potential heart transplant candidates (referred as opposed to selected for the waiting list) will eventually receive a donor organ. Studies suggest that as many as 50% of ischemic cardiomyopathy patients referred for cardiac transplantation have hibernating myocardium. Other unfavorable patient characteristics include advanced age, female gender, severity of coronary disease, presence of dysrhythmias, and renal impairment. Myocardial viability index was the only independent predictor of event free survival. Positron emission tomography was used to distinguish stunned from hibernating myocardium. Hibernation was associated with more severe depression of contractility and incomplete recovery. Stunning was present more frequently than hibernation and myocardial morphology determined the degree of functional improvement. First, exercise-induced ischemia may impair papillary muscle function causing mitral regurgitation, pulmonary congestion, and dyspnea. Second, acute myocardial infarction located inferobasally (right coronary or dominant circumflex distribution) can cause sudden posteromedial papillary muscle dysfunction and mitral regurgitation. The third, and largest, group comprises those with progressive left ventricular dilatation, chronic mitral regurgitation, and pulmonary hypertension. Though valve surgery has been widely advocated for these patients, the long-term outcome is not as satisfactory as once thought. Ventricular reconstructive surgery is the successor to left ventricular aneurysmectomy (for full-thickness scar), now that thrombolysis or primary coronary angioplasty limits myocardial infarction before the transmural stage. The scar is then limited to the endocardial surface while the epicardium appears normal through a rim of reperfused muscle. This contrasts with the leather-like appearance of an expanding full thickness scar in a dyskinetic left ventricular aneurysm. Once decompensation begins, functional impairment progresses rapidly as does the risk of surgical mortality. The reconstruction is then begun using a continuous suture passed along the border between endocardial scar and healthy septal and lateral myocardium. Significant doubt has been cast about the efficacy of both mitral valve repair and left ventricular remodeling surgery in ischemic cardiomyopathy. A landmark paper from the Cleveland Clinic provides the best aid to decision-making using prognostic factors for the individual patient. Coronary bypass alone and listing for transplantation appeared to maximize 5-year survival. With persistence and refinement of antirejection therapy, this compelling procedure emerged as an effective solution for a few highly selected patients without significant comorbidity. This contrasts with approximately 100,000 and 12,000 end-stage heart failure patients, respectively, under the age of 65 in these countries. Clearly the scarce donor hearts should be reserved for those most likely to benefit in life expectancy and quality of life. Young patients with congenital heart disease or idiopathic dilated cardiomyopathy fit this category. While arteriopaths with ischemic heart disease comprise the largest cohort of potential candidates, most prove ineligible through heart failure comorbidity or advanced age. With increasingly sophisticated bioengineering, the original temporary external pneumatic blood pumps have evolved into miniaturized fully implantable electrical devices suitable for the long-term treatment of chronic heart failure. Experimental evidence showing that pulse pressure is not necessary in the systemic circulation of large mammals allowed the development of small continuous flow devices. Currently, total artificial hearts (biventricular) are still used in a small number of cardiac transplant candidates. Typically, the patient has acute cardiogenic shock after cardiac surgery, acute inflammatory cardiomyopathies, or myocardial infarction. Criteria for beginning temporary circulatory support include a cardiac index less than 2. The patient is oliguric and acidotic with cool extremities and obtunded mental state. The presence of irremediable renal, hepatic, or respiratory failure is an absolute contraindication to initiating support. Patients older than 70 years have decreased survival, though the potential for weaning is not affected by age. Risk stratification models show preimplantation mechanical ventilation, urine output less than 30 mL/hour, preoperative central venous pressure more than 16 mmHg, hepatic dysfunction (prothrombin time >16 seconds) and increasing serum creatinine and bilirubin levels to be adverse prognostic risk factors. Early deployment based on predictive models (derived from hemodynamic parameters and level of intraoperative inotropic support) provides improved likelihood of survival to hospital discharge. Long-term circulatory support "Destination therapy" is an increasingly realistic alternative to cardiac transplantation and a lifeline for the vast majority of heart failure patients rendered ineligible for transplantation through common heart failure comorbidities. The first is to provide symptomatic relief for the severely debilitated heart failure patient. The second is to extend survival, aiming for at least 5 years of goodquality life. The third objective is cost-effectiveness, by reducing the need for recurrent hospital admissions. First, considerable knowledge and expertise was gained from prolonged bridging to transplantation because of limited donor heart availability. Mechanical unloading improves native heart function, particularly in idiopathic dilated and inflammatory cardiomyopathies. Third, the new axial flow and centrifugal pumps (providing continuous as opposed to pulsatile blood flow) have now been shown to be as effective but safer than the large firstgeneration devices which provide stroke volume and pulse pressure. Patients are discharged from hospital within a few weeks and pursue an active life in the community. Improvement in native heart contractility the failing heart beats more than 120,000 times a day pumping around 7,000 L of blood against an increasing afterload. First the failing ventricle is unloaded thereby promoting functional improvement or rarely recovery in dilated cardiomyopathy patients. Our own clinical experience suggests that rotary blood pump patients experience better survival when native heart contractility improves. Cardiac output is boosted by the native heart and there is less propensity for intraventricular thrombus formation when contractility and segmental wall motion improves. Pulsatility generated by the native left ventricle improves coronary blood flow and there is less risk of coronary thrombosis in obstructed vessels. For many years it has been recognized that ventricular unloading with a blood pump eliminates left ventricular wall stress triggering reversal of the heart failure remodeling process at cellular and molecular level. Mesenchymal stem cells appear to convey reparative processes by angiogenesis, extracellular matrix stabilization, and endogenous stem cell recruitment. Current evidence suggests that intramyocardial injection of bone marrow stem cells is a more effective method of delivery than intracoronary infusion.
Generic 250 mg keftab free shipping
In addition antibiotics depression discount keftab uk, two studies have shown that trauma systems also reduce trauma morbidity. In 1988, a report card was issued on the current status and future challenges of trauma systems. At that time, an inventory was taken of all state emergency medical service directors or health departments having responsibility over emergency and trauma planning. They were contacted via telephone survey in February 1987, and then were asked eight specific questions on their state trauma systems. Of the eight criteria, only two states, Maryland and Virginia, were identified as having all eight essential components of a regional trauma system. Not limiting the number of trauma centers in the region was the most common deficient criterion. In 1995, another report card was issued in the Journal of the American Medical Association. This report card was an update on the progress and development of trauma systems since the 1988 report. It was a more sophisticated approach, as it expanded the original eight criteria and was more comprehensive. According to the 1995 report, five states (Florida, Maryland, Nevada, New York, and Oregon) had all the components necessary for a statewide system. There are now 35 states across the United States actively engaged in meeting trauma system criteria. In addition to the report card, the Skamania Conference evaluated the effectiveness of trauma systems. The medical literature was searched and all available evidence was divided into three categories: reports resulting from panel studies (autopsy studies), registry comparisons, and population-based research. Panel studies suffered from wide variation and poor interrater reliability, and the autopsies alone were deemed inadequate. Registry evaluation was found to be useful for assessing overall effectiveness of trauma systems. Their critique of trauma registries included the following: there are often missing data, miscodings occur, there may be inter-rater reliability factors, the national norms are not population-based, there is little detail about the cause of death, and they do not take into account prehospital deaths. Despite these deficits, conference participants reached consensus, concluding that registry studies were better than panel studies but not as good as population studies. An advantage over registry studies is attributed to studying and evaluating a large population in all aspects of trauma care, including prehospital, hospital, and rehabilitation. Unfortunately, only a limited number of clinical variables can be evaluated, and it is difficult to adjust for severity of injury and physiologic dysfunction. Despite disadvantages with all three studies, the advantages may be applied to various individual communities to help influence public health policy with regard to trauma system initiation and evaluation. The first is a comparison of mortality rates between Level I trauma centers and hospitals without a trauma center. The in-hospital mortality rate was significantly lower in trauma centers than in nontrauma centers (7. In the global burden of disease study by Murray and Lopez, the world is divided into developed regions and developing regions. This is the sum of life years lost due to premature death and years lived with disability adjusted for severity. One of the most difficult problems that we face in the coming years is how to provide reasonable trauma care and trauma system development in the developing regions of the world. There are few, if any, trauma centers in the urban areas, and certainly none in the rural areas of the same countries. Even if there were such centers or a trauma system, rehabilitation is almost totally lacking, and therefore, the injured person would rarely be able to return to work or productivity after a severe injury. As noted earlier, Europe has in the last century developed some statewide trauma systems. Again, there are no standards for what constitutes a trauma surgeon, and in fact, trauma surgery is a potpourri of different models. One model is exemplified by Austria, where trauma surgery is an independent specialty. Another model incorporates trauma surgical training into general surgery, and this includes France, Italy, the Netherlands, and Turkey. In a third model, the majority of trauma training is given with orthopedic surgery residency training. The largest model provides trauma surgery training within specific specialties without any single specialty having any major responsibility for trauma training, and this model prevails in Denmark, Germany, Portugal, Estonia, Iceland, England, Norway, Finland, and Sweden. Some of the most vexing problems in trauma surgery occur now in North America, particularly in the United States. It is predicted that there will be a major shortage of general surgeons in the United States within the next few years. General surgeons are now older, and more importantly, general surgeons are now subspecializing. In many instances, the hospital will pay their salaries to provide 24/7 calls, usually on a 12-hour shift basis. In some instances, possibly up to one third, various practice groups will pay these hospitalists to take their calls in hospital. Another trend affecting general surgery is the rapid transition to nondiscrimination regarding gender. At least 50% of entering medical students are now female, but only 7% (approximately 500 individuals) apply to surgery. The reasons given are long hours and poor lifestyle, as these women wish to combine professional careers with parenting responsibilities. There is an overall decrease in applications to general surgery, and the reasons for this are complex and multifaceted. Younger medical students and physicians tend to opt out of surgery, and they particularly abhor trauma surgery, because of the time commitment and related lifestyle issues. Another problem, which may be unique to the United States, is the decrease in operative cases in trauma. There has been a shift from penetrating trauma to blunt trauma and another shift to nonoperative management, particularly of liver and spleen injuries. General surgeons have compounded the problem by referring cases to surgeons who specialize in vascular surgery or chest surgery. Interventional radiologists also participate in management of certain traumatic injuries. Another vexing problem in trauma care in the United States is the current demand for on-call pay by specialty surgeons. On average, a neurosurgeon in a Level I hospital would only be called in 33 times in the course of a year. In contrast, orthopedic surgeons average approximately 275 emergency cases during the year. Nevertheless, hospitals are being asked to pay on-call stipends to neurosurgeons that are quite large, considering the relatively low probability of being called in. Other factors affecting trauma availability by specialty surgeons are freestanding ambulatory surgery centers where the surgeons can often avoid government regulations, do not have to take calls, and have hospitalists care for their patients at night. These problems will be accentuated in the next few years as the elderly population (aged 65 and older) reaches 30% of the total population. Studies in the United States show that the mortality rate for people aged 65 and older in the intensive care unit is 3. Unfortunately, the majority of these elderly patients who are seriously injured do not return to independent lifestyles following acute care. Most of these countries are totally lacking in the infrastructure for provision of a trauma system, including prehospital care, sufficient adequately trained surgeons, and rehabilitation services. International institutions such as the World Bank and World Health Organization would have to take a leading role in providing financial resources and training for prehospital care. This would be a potentially huge sum, because it would require creating and developing adequate communications, ambulances, and properly trained prehospital personnel. Bringing surgeons to Western countries for training has been a problem because many of them do not return to their countries of origin. In my opinion, the optimal way to train these individuals would be for surgical educators from countries with mature trauma systems to spend time educating surgeons in the appropriate medical schools in their home countries. This is also problematic, because the quality of medical schools varies tremendously in developing nations. Furthermore, in addition to surgeons, anesthesiologists, critical care physicians, and nurses would have to be educated as well.
Order generic keftab online
This variant disease was contracted from eating meat from infected cows bacteria 4th grade science purchase line keftab, and many people were concerned that more cases would be found because there was a lag time between consumption of infected beef and onset of clinical manifestations. Two of the cases were associated with ingestion of infected beef in England; the other two cases were possibly related to the ingestion of infected beef from Saudi Arabia. There is some concern about possible transmission of a prion-based disease to humans from the ingestion of squirrels and from deer infected with prion-based cervid wasting disease, which is common is some parts of the United States, but there is no hard evidence for human transmission at present. Approximately 1 percent of people between the ages of sixty and sixty-four have the disease, increasing to almost 40 percent in people older than age eighty-five. The disease is characterized by progressive failure of recent memory, followed by difficulties in thinking, reasoning, and judgment; it is often associated with emotional disturbances such as depression, anxiety, and irritability. The disease is preceded by about six years of declining cerebral function before Alzheimer disease is diagnosed. The course of the disease differs among individuals but usually is fatal in six to eight years, although some of those affected survive more than ten years. Currently about five million people suffer from Alzheimer disease in the United States. Most Alzheimer cases are sporadic, but 5 to 10 percent of cases are associated with inherited autosomal dominant disease. The brains of affected patients exhibit progressive loss of neurons with atrophy of cerebral cortex and compensatory ventricular enlargement (hydrocephalus ex vacuo). Two characteristic histologic changes characterize the disease: neurofibrillary tangles and neuritic (senile or A amyloid) plaques. Neurofibrillary tangles result from degenerative changes affecting the thin, delicate, wirelike neurofilaments located within the cytoplasm of the neurons. Neurofibrillary tangles are mostly composed of a protein termed tau, which in Alzheimer disease is hyperphosphorylated. Tau is associated with the pathogenesis of Alzheimer disease but is also found in other degenerative neurological diseases (termed tauopathies). In general, there is a correlation between the degree of intellectual deterioration and the severity of the histopathologic changes. The brains of patients with advanced Alzheimer disease contain large numbers of neuritic plaques and neurofibrillary tangles, whereas those with mild disease have less striking changes. The other pathway produces a soluble protein that is not associated with disease (the nonamyloidgenic pathway). The mechanism for production of A amyloid protein and neuritic plaque in sporadic Alzheimer disease remains a mystery. The diagnosis of Alzheimer disease is made by excluding other conditions that can impair brain function, such as chronic infections of the nervous system or multiple strokes. Unfortunately, no specific treatment can arrest the relentless progression of the disease, although some drugs may be useful to improve cerebral function temporarily. A second drug (mematine), which inhibits a particular class of nerve cells in the brain that use glutamate to transmit impulses, has become available for treatment of moderate to severe Alzheimer. More drugs are being investigated, but no prevention or cure is yet available despite intensive research efforts. The name of the disease is derived from the characteristic multiple areas of involvement that heal by sclerosis (another name for scarring). The demyelinated areas appear much darker than the adjacent normal white matter because of loss of myelin. The onset of symptoms before the age of fifteen or after the age of forty is rare. Clinically, the disease is characterized by periodic episodes of acute neurologic disturbances, the nature depending on the location of the demyelination. The course of the disease is prolonged and quite unpredictable, with repeated acute episodes followed by remissions extending over many years. Eventually, the neurologic disabilities become permanent as a consequence of multiple areas of glial scarring, which impair conduction of nerve impulses in the brain and spinal cord. A number of measures, however, are available to relieve symptoms and minimize the neurologic disabilities. Corticosteroids and a variety of more potent anti-inflammatory and immunosuppressive agents are used to suppress the autoimmune response and to shorten the recovery from an acute episode. Much evidence indicates that multiple sclerosis is an autoimmune disease, possibly initiated by a viral infection in a genetically predisposed individual that stimulates an abnormal immune response. Activated T lymphocytes and monocytes target myelin proteins and destroy the myelin insulation, and autoantibodies to myelin-related proteins are found in the cerebrospinal fluid. Dense white areas adjacent to posterior horns of the ventricles and scattered throughout the brain lateral to the ventricles (arrows) are multiple sclerosis plaques. Monozygotic twins show a 25-percent rate of concordance in having the disease, further supporting a role for genetics in susceptibility. The axons of these neurons synapse with neurons in the basal ganglia, where they release the neurotransmitter dopamine, one of the important connections of the extrapyramidal motor system. As a result of the progressive neuron loss in the substantia nigra, fewer fibers are available to release dopamine in the basal ganglia, allowing the concentration of dopamine in the basal ganglia to fall. The muscular rigidity, increased muscle tone, and abnormal repetitive involuntary movements, which are common manifestations of the disease, result from the deranged function of the extrapyramidal system. As is the case with Alzheimer disease, an accumulation of abnormal proteins within neurons is a characteristic of Parkinson disease. For this reason, both Alzheimer and Parkinson diseases as well as Huntington disease and amyotrophic lateral sclerosis are sometimes termed neurodegenerative proteinopathies. In most cases, the cause of the particular disease is unknown (although there are uncommon inherited forms). There is some evidence that proteinopathies may show cell-to-cell transmission of the misfolded abnormal proteins, which act as "infectious agents" spreading within neural tissue of the disease host and leading to additional neuronal injury and death. Parkinson disease is characterized by the presence of Lewy bodies, damaged neurites containing intracellular inclusions that are rich in aggregates of -synuclein, a neuronal protein of uncertain function. Although Parkinson disease starts in the dopaminergic neurons of the midbrain, the disease (as characterized by the presence of Lewy bodies) spreads with time to higher cortical areas and dementia begins to accompany the early motor symptoms. In most cases, the cause of Parkinson disease is unknown although there is some evidence that exposure to pesticides and herbicides increase the risk of disease by 80 percent. About 10 percent of cases are genetic in origin and tend to occur in younger people with increased severity. The manifestations of Parkinson disease can be relieved by a drug called L-dopa, which is converted within the brain into dopamine and raises the concentration of dopamine in the basal ganglia, thereby supplying the neurotransmitter that is deficient. Some surgical procedures also are available to reduce the tremors associated with the disease when they are not controlled adequately by drugs. Electrical stimulation of the electrodes (using an implanted electronic device often located at the collarbone) improves motor function and reduces tremors in the patient. This technique has supplanted previously used surgical destruction of selected brain areas. Treatment, however, does not arrest the progressive neuron loss in the substantia nigra, nor does it stop the progression of the disease. Attempts to transplant dopamine producing cells into the brain of affected patients have largely been abandoned because these treatments had little effect. It is of interest that Lewy bodies were found in the engrafted normal tissue supporting cell-to-cell transmission of the disease. The first manifestations in affected individuals occur between thirty and fifty years of age. The disease progresses slowly and is usually fatal within fifteen to twenty years. These structures are part of the extrapyramidal motor system, which regulates smooth and coordinated muscle movements, and damage to the system gives rise to the abnormal movements characteristic of the disease. The cerebral cortex is also affected, which eventually leads to dementia as the disease progresses. This is another disease in which an increased number of triplet repeats disrupts gene function and leads to disease (see discussion on congenital and hereditary diseases). In Huntington disease, however, the expansion of triplet repeats increases during spermatogenesis (rather than during oogenesis, as occurs in the fragile X syndrome), so the gene with expanded repeats comes from the affected father instead of the mother.
Cost of keftab
However bacteria have nucleus cheap 750mg keftab overnight delivery, if it cannot be completely removed, it may grow large enough to become lethal by occupying space within the skull. The distinction between benign and malignant neoplasms is not always absolute and can, at times, depend on the specifics of a given case. Depending on their location, tumors can be solid (and often embedded in, but discrete from, host tissue), invasive within (and not discrete from) host tissue, or derived from a blood cell or blood cell precursor and found in the circulation (leukemia) or in the lymph nodes or spleen (lymphoma). Although it pushes surrounding normal tissue aside, it does not infiltrate surrounding tissues (is said to be well-circumscribed), nor does it spread by blood and lymphatic channels to distant sites. Histologically, the cells in a benign tumor typically appear mature and closely resemble the normal cells from which the tumor was derived. Benign tumors are generally low grade because they closely resemble the cell of origin. The cleavage plane is easily established, indicating that the tumor is sharply circumscribed and does not infiltrate the adjacent nerve. Note the sharp demarcation between the tumor and surrounding breast tissue (arrow). Cancer cells grow in a haphazard pattern and exhibit great variation in size and structure. Frequently, the infiltrating strands of tumor find their way into the vascular and lymphatic channels. For example, a primary tumor of the colon may metastasize via the blood to the liver. Multiple secondary metastatic tumors in the liver will grow, occupy space, lead to hepatocyte injury, and, ultimately, liver failure and death. The primary factor used to classify any tumor, be it benign or malignant, is the cell or tissue of origin. Therefore, understanding the tissue classifications, including their structure and function in health and disease, is helpful in understanding the names of tumors. Although tumor nomenclature is not completely uniform, sometimes being based on historical names or jargon, certain generalizations are possible. The term polyp is most often used to refer to epithelial lesions that project from the surface of an organ into the lumen (examples being colonic and uterine polyps). Polyps are generally benign when discovered but can become (or sometimes are) malignant. Benign neoplasms are named by adding the suffix -oma Polyp/papilloma Wartlike benign tumor often associated with viral infection. For example, a benign tumor arising from glandular epithelium is called an adenoma. A benign tumor of blood vessels is an angioma, one arising from cartilage is designated a chondroma, and from bone an osteoma. A carcinoma is any malignant tumor arising from surface, glandular, or parenchymal (organ) epithelium. For example, a malignant tumor arising from the urothelium of the urinary bladder is called a urothelial carcinoma of the bladder. A carcinoma arising from the glandular epithelium of the pancreas is termed an adenocarcinoma of the pancreas (aden = gland), and a tumor arising from the squamous epithelium of the esophagus is called a squamous cell carcinoma of the esophagus. Sarcoma is a general term referring to a malignant tumor arising from connective tissue. The exact type of sarcoma is specified by prefixing the term designating the cell of origin. Fibrosarcoma, liposarcoma, myosarcoma, osteosarcoma, and angiosarcoma indicate, respectively, malignant tumors of fibroblasts, fat cells, muscle cells, bone-forming cells, and blood vessels. The term leukemia is applied to any neoplasm of blood-forming tissues found in the bone marrow or circulating in the blood. Neoplasms arising from the precursors of white blood cells usually do not form solid tumors. Instead, the abnormal cells proliferate within the bone marrow, where they overgrow and crowd out the normal blood-forming cells. The neoplastic cells also "spill over" into the bloodstream, where large numbers of abnormal cells can circulate in the peripheral blood. In some cases, these neoplastic cells may populate lymph nodes and spleen rather than circulate. There are some inconsistencies and exceptions to the general principles of nomenclature. Pediatric malignant neoplasms are sometimes denoted with the suffix "blastoma"; some examples being retinoblastoma and nephroblastoma (commonly called Wilms tumor). These cancers are derived from primitive (immature) retinal and renal cells, respectively. Do not be unduly concerned about the exceptions; overall, the general principles of naming tumors are followed. This slow progression gives the oncologist (a physician who specializes in the treatment of cancer) a wide window of time to diagnose and treat the disease before it becomes life-threatening. Colonoscopy (to diagnose potential adenocarcinoma of the colon by physically examining the lower digestive tract) need be done only every seven to ten years in older people because it takes time for the benign polyp detected by the test to become malignant, spread through the colon, and metastasize. Many neoplasms arising from surface epithelium remain localized within the epithelium for many years before evidence of spread into the deeper tissues or to distant sites occurs. Most often cervical cancer begins in an area of the cervix (the transition zone) where the columnar, mucin producing epithelial cells of the cervical canal leading to the uterus meet the squamous epithelial cells that line the face of the cervix. Drawing illustrates progressive changes in cervical epithelium with time, leading to carcinoma in situ. Perhaps as a response to injury, the columnar secretory cells undergo metaplasia (conversion of one differentiated tissue type to another) and become squamous cells. This area of metaplasia is susceptible to the initiation of the process of neoplasia. In a strict sense, the area of dysplasia is precancerous until the neoplastic cells traverse the basement membrane into the body of the cervix. An abnormal Pap test indicates the detection of dysplastic epithelial cells scraped from the surface mucosa of the cervix; if detected early in the course of cervical neoplasia, this is easily treated. Although most clearly demonstrated in the cervix, the gradual progression of metaplasia to dysplasia (early "precancer") to carcinoma in situ, followed in time by invasion and metastasis (cancer or malignant neoplasia), has also been described in the breast, bronchus and lung, urinary tract and skin. The slow progression of histological changes is accompanied by the neoplastic cells gaining additional mutations, Metaplasia Conversion of one differentiated tissue type to another. Leukoplakia A white patch of hyperplastic and usually atypical squamous epithelium on the oral mucosa or genital tract mucosa. Although a determination of dysplasia is made by a pathologist based on changes seen at the cell or tissue level, certain precancerous neoplasms can be visually recognized. Because these lesions have a likelihood of eventually developing into cancer, it is important to recognize them. Prolonged exposure to sunlight, for example, not only causes premature aging of the skin but also causes small, crusted, scaly patches to develop on sun-exposed skin called actinic keratoses ("actinic" refers to sun rays). Precancerous, thick, white patches descriptively called leukoplakia (leuko = white + plakia = patch) may develop in the mucous membranes of the mouth as a result of exposure to tobacco tars from pipe or cigar smoking or from use of smokeless tobacco (snuff and chewing tobacco) and may give rise to squamous cell cancers of the oral cavity (see the discussion on the gastrointestinal tract). Somewhat similar precancerous changes may take place in the epithelium of the vulva (discussion on the female reproductive system) and may develop into vulvar cancer. These neoplastic precancerous conditions should always be treated appropriately to prevent malignant change, which occurs in many, but not all, cases. Some neoplasias appear to be initiated in a particular population of cells present in many organs that serve as a continuing source of differentiated cells to replace populations that are damaged or have died. Such stem cells constitute a self-renewing pool of cells that normally give rise to mature differentiated progeny. Although a neoplasm starts from a single cell, the population of cells within a tumor shows great diversity (tumor heterogeneity). As the tumor grows, additional mutations occur; the mutated cells are selected for rapid growth, survival, ability to escape immune killing, and resistance to therapeutic drugs. The cells in a malignancy undergo a "selection of the fittest," which is defined by their ability to survive, grow, and divide. Although there are many exceptions, malignant lesions generally grow more rapidly than benign lesions. However, the apparent sudden expansion of tumors is a result of exponential growth.
Purchase keftab canada
Neurological complications are much less frequent than vascular complications but paraplegia can occur secondary to aortic dissection or adventitial hematoma producing spinal cord infarction antibiotic 625mg 125 mg keftab. Rupture may result in balloon entrapment because blood leaks into the system and forms clots, which block full deflation. Notably, 90% of patients who survived to leave hospital were weaned from the pump within one week. The patient age group of over 70 years was the principal determinant of mortality. Sixty-two percent (62%) of the patients were successfully weaned, but only 25% survived to leave hospital. Of the 12 patients included in the report, one recovered sufficiently for device explantation, while 9 of the remaining 11 patients (82%) survived to undergo transplantation with successful hospital discharge in each case. The device is comprised of a bearingless motor, which combines the drive, the magnetic bearing, and the rotor function in a single unit. This device can produce flows up to 10 L/minute under normal physiological conditions with a priming volume of 31 mL. Initial European clinical trials in postcardiotomy cardiogenic shock have been encouraging over mean support periods of 2 weeks, with the longest at 64 days. Overall 30-day mortality was 50%, which compares favorably with that reported for other devices. Device mechanical reliability and relatively low complication rates make the Levitronix pump safe to use for patients who need time for evaluation for cardiac transplantation or a longer-term device. Conduits for the inflow and outflow cannulas are used to improve the safety of decannulation. Through this conduit is introduced the 32 F right-angled wire reinforced venous cannula into the center of the left atrium. Ligatures are placed around the homograft tube to retain the inflow cannula in position. The distal end of the venous cannula is brought through the skin below the sternotomy wound and then filled by raising left atrial pressure. A Dacron polyester fabric graft (8 mm) is then sewn to the ascending aorta with a side clamp. The straight 22 F arterial inflow cannula is inserted through this graft, secured into place by ligatures and brought out through the skin adjacent to the venous cannula. Transoesophageal echocardiography is used to confirm the position of the inflow cannula and the efficacy of de-airing. After protamine administration, the sternotomy wound is closed to allow extubation during support. Once the chest tube drainage is less than 50 mL/hour heparin infusion is given to provide an activated partial thromboplastin time ratio of 1. For recovery after ischemic arrest the support duration is usually less than 7 days. Reoperation for bleeding and decannulation problems are avoided by the use of the conduits. With a view to explant, myocardial function is assessed daily with the pump flow turned down to 2. After sustainable improvement in myocardial function has been achieved, the patient is returned to the operating room, the pump is switched off and the cannulas are withdrawn. To date the Levitronix Centrimag pump has been used in thousands of patients, of whom around 45% of cases have been salvage postcardiotomy support with a mean of 9 days and 53% survival. It is likely that the 47% mortality could have been reduced substantially by anticipating postoperative deterioration and using the blood pump electively to prevent cardiogenic shock during the duration of reversible post-ischemic stunning. The evolving challenge of chronic heart failure management: a call for a new curriculum for training heart failure specialists. Guidelines for the evaluation and management of chronic heart failure in adults: executive summary. Quantative relation of myocardial infarct size and myocardial viability by positron emission tomography to left ventricular ejection fraction and 3-year mortality with and without revascularisation. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. Preoperative positron emission tomographic viability assessment and perioperative and postoperative risk in patients with advanced ischemic heart disease. Severe ischemic left ventricular failure: coronary operation or heart transplantation Time course of functional recovery of stunned and hibernating segments after surgical revascularisation. Ischemically compromised myocardium displays different time course of functional recovery: correlation with morphological alterations. Efficacy of endoventricular patch plasty in large post infarction akinetic scar and severe left ventricular dysfunction: comparison with a series of large dyskinetic scars. Quality of life and economic outcomes with surgical ventricular reconstruction in ischemic heart failure: results from the Surgical Treatment for Ischemic Heart Failure Trial. Low incidence of myocardial recovery after left ventricular assist device implantation in patients with chronic heart failure. Bone marrow cell-induced protection of the human myocardium: characterization and mechanism of action. Neovascularisation of ischemic myocardium by human bone-marrow derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Cardiac repair with intramyocardial injection of allogenic mesenchymal stem cells after myocardial infarction. Hybrid approach of ventricular assist device and autologous bone marrow stem cell implantation in end stage ischemic heart failure enhances myocardial perfusion. Results of a regional study of modes of death associated with coronary artery bypass grafting. Enhanced efficacy of eptifibatide administration in patients with acute coronary syndrome requiring in-hospital coronary artery bypass grafting. Risks of morbidity and mortality in dialysis patients undergoing coronary artery bypass surgery. Detrimental effects of premature use of inotropic drugs to discontinue cardiopulmonary bypass. Coronary artery bypass grafting in patients with severe left ventricular dysfunction: a prospective randomized study on the timing of perioperative intraaortic balloon pump support. Optimal timing of properative intra-aortic balloon pump support in high-risk coronary patients. Comparison of coronary artery blood flow and hemodynamic energy in a pulsatile pump versus a combined nonpulsatile pump and an intra-aortic balloon pump. The current practice of intra-aortic balloon counterpulsation: results from the Benchmark Registry. Vascular complications related to intra-aortic counterpulsation: an analysis of a 10-year experience. Improved results for postcardiotomy cardiogenic shock with the use of implantable left ventricular assist devices. Elective transfer from cardiopulmonary bypass to centrifugal blood pump support in very high-risk cardiac surgery. Antiarrhythmic drug therapy is complicated by significant side effects and may necessitate warfarin for anticoagulation. The Cox-Maze procedure the first effective surgical procedure for atrial fibrillation was introduced clinically at Washington University in St. During the last decade, most groups have replaced the traditional "cut-and-sew" lesions with ablation lines created using various energy sources in an attempt to make the operation simpler and faster to perform. These ablation-assisted procedures have resulted in widespread adoption of the Cox-Maze and a significant increase in the number of operations that are performed annually for atrial fibrillation.
Discount keftab on line
Off-pump versus conventional coronary artery bypass grafting: a meta-analysis and consensus statement from the 2004 ismics consensus conference virus spreading discount keftab 250mg with mastercard. Does coronary artery bypass graft surgery improve survival among patients with end-stage renal disease Myocardial revascularization in patients with low ejection fraction < or = 35%: effect of pump technique on early morbidity and mortality. Ten-year experience with single-vessel and multivessel reoperative off-pump coronary artery bypass grafting. Early outcomes in the elderly: a meta-analysis of 4921 patients undergoing coronary artery bypass grafting-comparison between off-pump and onpump techniques. Propensity score analysis of early and late outcome after redo off-pump and on-pump coronary artery bypass grafting. Impact of preoperative neurologic events on outcomes after coronary artery bypass grafting. On-pump versus off-pump coronary artery bypass grafting in a cohort of 63,000 patients. Emergency conversion to cardiopulmonary bypass during attempted off-pump revascularization results in increased morbidity and mortality. Aborted off-pump coronary artery bypass patients have much worse outcomes than on-pump or successful off-pump patients. Health-related quality of life outcome after on-pump versus off-pump coronary artery bypass graft surgery: a prospective randomized study. Propensity case-matched analysis of off-pump coronary artery bypass grafting in patients with atheromatous aortic disease. Propensity case-matched analysis of off-pump versus on-pump coronary artery bypass grafting in patients with atheromatous aorta. Complete revascularization in coronary artery bypass grafting with and without cardiopulmonary bypass. On- and off-pump coronary surgery and perioperative myocardial infarction: an issue between incomplete and extensive revascularization. Trends in aortic clamp use during coronary artery bypass surgery: effect of aortic clamping strategies on neurologic outcomes. Single crossclamp improves 6-month cognitive outcome in high-risk coronary bypass patients: the effect of reduced aortic manipulation. Combined use of off-pump techniques and a sutureless proximal aortic anastomotic device reduces cerebral microemboli generation during coronary artery bypass grafting. Gaseous and solid cerebral microembolization during proximal aortic anastomoses in off-pump coronary surgery: the effect of an aortic side-biting clamp and two clampless devices. The importance of completeness of revascularization during longterm follow-up after coronary artery operations. Incomplete revascularization reduces survival benefit of coronary artery bypass grafting: role of off-pump surgery. Coronary bypass surgery performed off pump does not result in lower in-hospital morbidity than coronary artery bypass grafting performed on pump. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. Fewer grafts performed in off-pump bypass surgery: patient selection or incomplete revascularization Coronary artery bypass graft failure after onpump and off-pump coronary artery bypass: findings from prevent iv. Clinical and radiologic outcome of off-pump coronary surgery at 12 months follow-up: a prospective randomized trial. Meta-analysis of randomized trials comparing offpump with on-pump coronary artery bypass graft patency. Early administration of clopidogrel is safe after off-pump coronary artery bypass surgery. An argument for routine ultrasound screening of the thoracic aorta in the cardiac surgery population. Clinical experience with the novare enclose ii manual proximal anastomotic device during off-pump coronary artery surgery. Evaluation of the pas-port proximal anastomosis system in coronary artery bypass surgery (the epic trial). For similar reasons, female patients with large breasts may be at increased risk for wound-related complications. Optimally, single lung ventilation is employed, however this is not absolutely necessary (if not utilized, reduction in tidal volume and packing of the lung away from the field are helpful maneuvers). Some surgeons use the fifth interspace approach in order to obtain maximal conduit length. Also shown is the port placement for the endo stabilizer which can later be used for insertion of a chest tube. The pericardium is incised longitudinally anterior to the phrenic to the level of the base of the heart. Silastic loops are placed proximally and distally if necessary (note that distal snares are preferably avoided as they may lead to scar lesions and impaired flow). Premedication with lidocaine or another antiarrhythmic should be employed prior to vessel occlusion. Should hemodynamic compromise be encountered following occlusion, the use of an intracoronary shunt may be employed with the vessel occluders released while performing the anastomosis. Whether shunted or not, the anastomosis is created with continuous 7-0 Prolene if the artery is fragile or small. All Rights Reserved space (some authors recommend using a patch of bovine pericardium). A single chest tube is placed and the ribs, pectoral muscle, and skin closed in a standard fashion. Women with large breasts may be challenging as a larger submammary incision may be required or ports may need to pass through breast tissue. Using single lung ventilation, three ports are placed in the left mid-axillary line in the third, fifth, and seventh interspaces (some recommend the fifth interspace port be placed in the anterior axillary line. A 30-degree (either 5 mm or 10 mm) thoracoscope is placed via the fifth space and carbon dioxide insufflation is initiated to a target pressure of 8 mmHg. If hemodynamic compromise occurs, it may be due to hypertensive pneumothorax (especially in patients with compromised left ventricular function). Decreasing the rate of insufflation or evacuating some of the carbon dioxide from the thoracic space should rapidly improve the hemodynamics. Next, a grasper and electrocautery or harmonic scalpel via the third and seventh interspaces are inserted. Two additional port-site incisions allow for the use of an epicardial stabilizer and an apical positioner. The system conveys high definition threedimensional imaging to the surgeon at the console and sensors register finger and wrist movements and translate them, tremor-free, into the motion of the microinstruments in the operative field. Around 2,000 robotic cardiac operations are performed in the United States per year and the number is increasing modestly. As no rib spreading is involved, there is minimal intercostal nerve trauma and less postoperative pain. In our experience, a distance of less than 25 mm from the left heart border to the chest wall can lead to significant technical challenges owing to insufficient working space. Therefore, we reiterate our recommendation to prophylactically cannulate all cases under controlled conditions. Femoral cannulation and endoballoon should only be used in patients without aortoiliac atherosclerosis (~2/3 of patients in our experience). Axillary antegrade perfusion and femoral insertion of the endoballoon is the best option for patients with moderate grades of aortoiliac atherosclerosis. Transthoracic clamping and direct aortic root cannulation for cardioplegia is in its early stages of development; challenges associated with this technique include transthoracic puncture of the ascending aorta, as well endoscopic robotic control of bleeding after catheter removal. We also recommend use of a distal perfusion cannula via superficial femoral artery in all cases to ensure adequate limb perfusion. The aortic endoballoon catheter is inserted into the sidearm of an arterial perfusion cannula and advanced into the aortic root over a guidewire.
Purchase keftab overnight delivery
The ureteral openings into the bladder also appear to have a valvular function preventing backflow antimicrobial journal list discount keftab 500 mg without prescription. Renal pelvis/major calyces Expanded upper end of the ureter and divisions of the renal pelvis. Peristalsis the wavelike contractions of the wall of a tubular anatomic structure such as the alimentary tract or ureter which propel luminal contents forward. Podocytes Cells with highly branched cytoplasmic processes covering the glomerular capillaries of the kidneys. The opening of the urethra is located at the base of the bladder, with the ureteral openings on either side and behind the urethral opening. The triangular area at the base of the bladder bounded by the two ureteral orifices posteriorly, and the urethral orifice anteriorly, is called the trigone of the bladder (tri = three). The Nephron the basic structural and functional unit of the kidney is the nephron, with about one million nephrons in each kidney. The glomerulus is a tuft of capillaries supplied by an afferent glomerular arteriole. The capillaries of the glomerulus then recombine into an efferent glomerular arteriole, which in turn breaks up into a network of capillaries that supplies the renal tubules, which ultimately conduct urine to the renal calyces. The site where the afferent arteriole enters the glomerulus and the efferent arteriole exits is called the vascular pole of the glomerulus. The cells of this layer have long, footlike cytoplasmic processes and are usually called podocytes (podos = foot). The capillary tuft is held together and supported by groups of highly specialized cells called mesangial cells (meso = middle + angio = vessel). In addition to their support function, they are also contractile cells that play a role in regulating glomerular filtration by varying the caliber of the capillaries, and they are also phagocytic cells. The cytoplasm is very thin and is perforated by many small holes called fenestrations (fenestra = window). The middle layer is the basement membrane, which supports the capillary endothelium. Filtration is also based on molecular size, with selective passage for lower molecular weight substances. Their highly branched cytoplasmic processes are called foot processes, which are attached to the basement membrane and interdigitate with others from the same cell or adjacent cells. The narrow spaces between adjacent interdigitating pedicels are called filtration slits. The epithelium characteristic of each part of the renal tubule and the collecting tubule are also illustrated. The proximal convoluted tubule is the greatly coiled first part of the tubule, its convolutions being located very close to the glomerulus. The loop of Henle is a U-shaped segment composed of descending and ascending limbs joined by a short segment. The loop descends from the cortex into the medulla and then bends back sharply, returning to the cortex close to the vascular pole of its own glomerulus, where it becomes continuous with the distal convoluted tubule. The distal convoluted tubule, much shorter than the proximal tubule, empties into a collecting tubule that passes through the medulla to drain into one of the minor calyces at the apex of a renal pyramid (renal papilla). The renal tubules selectively reabsorb water, minerals, and other substances that are to be conserved and excrete unwanted materials, which are eliminated. Urine is the glomerular filtrate that remains after most of the water and important constituents have been reabsorbed by the renal tubules and other substances excreted by the renal tubules have been added. For a nephron to function normally, there must be free flow of blood through the glomerular capillaries, the glomerular filter must function normally, the tubules must be able to selectively reabsorb/excrete substances as needed, and the urine formed by the nephron must be able to flow freely from the kidney into the bladder. The kidneys form from masses of primitive connective tissue (mesoderm) located along the back body wall of the embryo. The ureters, renal pelves, renal calyces (the urinary drainage system), and the renal collecting tubules derive from paired tubular structures called ureteric buds. Each bud grows upward from the developing bladder and connects with the kidney that is forming on the corresponding side. Sometimes this developmental process is disturbed, and congenital malformations result. Three of the more common developmental abnormalities are failure of one or both kidneys to develop (renal agenesis), formation of extra ureters and renal pelves, or malpositions of one or both kidneys. Renal agenesis (a = without + genesis = formation) may affect one or both kidneys, but bilateral renal agenesis is uncommon. Agenesis, which often accompanies other congenital malformations, is incompatible with postnatal life. When one kidney is absent, the other kidney enlarges and is able to carry out the functions of the missing kidney. The recognition of this condition, however, is of great importance to the clinician who is treating an individual with kidney disease because one can never assume that the patient has two kidneys. Before a surgeon performs a kidney operation, diagnostic studies must be performed to ascertain that the patient has two kidneys. Sometimes double ureters draining the kidney unite to form a single ureter just before entering the bladder (partial duplication). A complete duplication results when an extra ureteric bud develops and gives rise to a separate excretory system draining the kidney on the affected side. Kidneys that fail to ascend normally are in very close approximation as they develop and may become fused. Renal duplications, malpositions, and fusions often are of little clinical significance. At times, however, drainage of urine may be impeded by the abnormalities, causing the urine to stagnate and predisposing the patient to urinary infections. Another important developmental abnormality called congenital polycystic kidney disease is considered in the section on renal cysts. Nephropathies: An Introduction Interruption of normal function in the kidneys that are related to glomerular malfunction include glomerulonephritis, nephrotic syndrome, and diabetic nephropathy. Renal hypertensive disease results in hypertensive nephrosclerosis associated with vascular injury. Damage to the renal tubules and interstitium of the kidney may result Nephropathies: An Introduction 509 in acute tubular injury and pyelonephritis associated with bacterial infections, which generally have ascended the urinary tract to reach the kidney. Glomerular renal disease that is associated with extreme proteinuria (loss of protein into the urine greater than 3 g/24 hr) defines nephrosis (nephrotic syndrome) and is often associated with edema, which can be widespread and severe (termed anasarca). Nephrotic patients also may have hyperlipidemia and secrete lipids in their urine as fatty casts, aggregated lipids that maintain the cylindrical shape of the tubule where they were formed. Nephrosis Renal disease resulting from excessive protein loss in the urine, caused by various types of renal injury. The signs and symptoms of glomerulonephritis are related to the changes within the glomeruli. Because many glomeruli are damaged or destroyed by inflammation, less blood is filtered and less urine is excreted. As urinary output is reduced, waste products are retained and accumulate in the blood. Other glomeruli, damaged by lysosomal enzymes, are no longer able to function as efficient filters. Protein and red cells leak through the damaged glomerular capillary walls and are excreted in the urine. Frequently, masses of red cells and protein accumulate within the tubules and become molded to the shape of the renal tubules before finally being excreted. These structures, which are called urinary casts, are an important indication of glomerular injury. Patients with glomerulonephritis are often hypertensive and have some degree of renal failure. Depending on the severity of disease, they may also show proteinuria (but not as severe as that in nephritic syndrome).