Cheap medex online mastercard
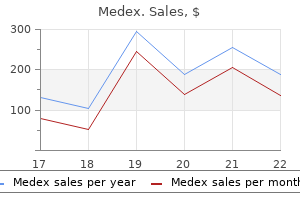
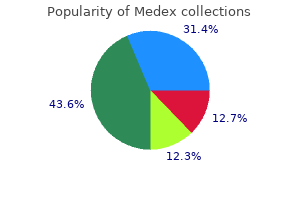
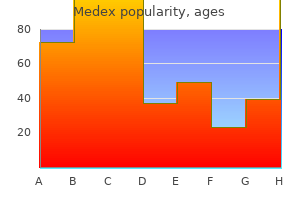
S2 is louder when the diastolic pressure is elevated in the aorta or pulmonary artery anti viral hand sanitizer buy medex 1 mg with mastercard. In conditions where stronger atrial contraction develops to help ventricular filling, a fourth heart sound (S4) may occur immediately before S1 (systole). This is thought to be due to ventricular wall vibration in response to forceful atrial filling. When the cardiac valves undergo pathological changes abnormal sounds called murmurs can sometimes be heard. Under normal conditions blood flow is not turbulent but remains laminar up to a critical velocity. The valve involved and the type of lesion (stenotic or regurgitant) can be identified by the timing of the murmur and the site on the chest wall where it is loudest. In normal individuals without cardiac disease (especially children) soft physiological systolic murmurs can often be heard. Isovolumetric contraction follows, represented by a vertical ascending segment which ends with the opening of the aortic valve. Isovolumetric relaxation follows next as a vertical descending segment ending when the mitral valve opens. The steeper this gradient, the lower the compliance of the ventricle during filling. This is partially dependent on how forcefully the ventricle contracts, and hence is related to ventricular contractility. Increased non-linearity is introduced under ischaemic or hypercontractile conditions and appears as a change in gradient and shift in the curve up or down. The contractile properties of cardiac muscle not only provide the engine to drive the cardiac pump but also give the heart an intrinsic ability to adapt its performance to a continually varying venous return. The Starling curve the above property of isolated cardiac muscle fibres can be applied to the muscle fibres in the walls of an intact ventricle, where the length of muscle fibres is related to the volume of the ventricle. In this case the tension per unit cross section (ventricular wall stress, T), developed in the wall during contraction, is dependent on the end-diastolic volume. The Frank curve Frank demonstrated in isolated muscle fibre preparations that the tension developed on contraction was dependent on the initial length of the fibre. This is because of a decreased compliance of the ventricle that occurs at high filling pressures. Measurement of stroke volume Ventriculography this has been the gold standard for measuring ventricular volumes, to which less invasive measurement methods have been compared. However, it is a cumbersome procedure done in the catheter suite and is not appropriate for repeated estimations. This technique is limited by the approximation made to transform the two-dimensional images of the ventricular into volumes. Thoracic impedance A small alternating current of low amplitude and high frequency is introduced between two sets of electrodes around the neck and lower thorax. The resultant electrical impedance between the neck and thoracic electrodes is measured, and represents the transthoracic impedance. The accuracy of the technique is influenced by several factors, which include intracardiac shunts, tricuspid regurgitation and positive pressure ventilation. The temperature rise is sensed when the warmed blood passes a thermistor in the pulmonary artery. Unfortunately recirculation and build-up of the indicator results in a high background concentration, which limits the total number of measurements that can be taken. First, the steady-state oxygen content of venous (CvO2) and arterial blood (CaO2) are measured. Doppler techniques Ultrasonic Doppler transducers have been incorporated into pulmonary artery catheters, endotracheal tubes, suprasternal probes and oesophageal probes. These probes can then be used to measure mean blood flow velocity through the aorta or any valve orifice. The above factors are based on physiological concepts arising from the performance of isolated muscle preparations. They have become useful in clinical practice when applied to the intact heart, but are difficult or impractical to measure directly. A strict definition for preload can be obtained from the Frank relationship between muscle fibre length and developed tension. Interpretation of these estimates is subject to the following limitations: r Ventricular compliance may not be normal, as it can be reduced by factors such as myocardial ischaemia, ventricular hypertrophy or pericardial tamponade. In a non-compliant ventricle, higher than normal filling pressures may be required to provide adequate preload. The presence of mitral stenosis may require higher than normal filling pressures to achieve adequate preload in the left ventricle. Arterial systolic pressure is often the available measurement, but its accuracy is limited if there is a significant gradient between aorta and ventricle. Afterload In an isolated muscle fibre preparation, afterload is defined as the tension developed during contraction. Thus, afterload is related to the mechanical resistance to shortening of the muscle fibre. In the intact heart, afterload becomes the tension per unit cross section (T), developed in the ventricular wall during systole. The other component is the reactive or frequency-dependent component, which is due to the compliance of the vessel walls and inertia of the ejected blood. This component is dependent on the pulsatile nature of the flow and rapidity of ejection. The slope of the curve then gives the effective elastance (compliance-1) of the arterial system. Contractility Contractility is a poorly defined term describing the intrinsic ability of a cardiac muscle fibre to do mechanical work when it contracts with a predefined load and initial degree of stretch. It is calculated by normalising stroke work for body surface area by using stroke index in its calculation. Ideally these parameters should be controlled during measurement, which is often impractical. Accordingly, pre- and afterload should be recorded during assessment of contractility. The interpretation of contractility measurements is then made at the given pre- and afterload. Other measures of contractility include ejection fraction and ventricular function curves. Ventricular function curves can be plotted between an index of ventricular filling. Factors increasing contractility will shift the curve upwards and to the left while those decreasing contractility will shift it downwards and to the right. Autonomic control of pacemaker discharge rate In vivo, control of the pacemaker rate is mediated peripherally via the autonomic nervous system.
Purchase medex no prescription
Give one half of this fluid in the first eight hours hiv infection rate russia generic medex 5mg otc, and the remainder over the next 16 hours. The exact volume of fluid given depends on vital signs, central venous pressure and urine output. Patients with full-thickness burns of >10% of the body surface area will probably require blood. Patients with severe burns need potent analgesia, which is best given by carefully titrating intravenous opioids. Exclude hypovolaemia and coagulopathy before attempting epidural or spinal analgesia in the acute trauma patient. In patients with multiple rib fractures, including flail segments, a thoracic epidural will provide excellent analgesia. This will help the patient to tolerate physiotherapy and to maintain adequate ventilation. All these factors help to reduce the requirement for intubation and mechanical ventilation. A lumbar epidural will benefit patients with lower limb injuries and, assuming there are no contraindications, this can be placed intraoperatively. Anaesthesia for patients with severe trauma Induction of anaesthesia A smooth induction of anaesthesia and neuromuscular blockade provides optimal conditions for intubating high-risk trauma patients. All anaesthetic induction drugs are vasodilators and respiratory depressants and have the potential to produce or worsen hypotension. There is no evidence that the choice of induction drug alters survival in major trauma patients. Their appropriate use during resuscitation involves a careful assessment of the clinical situation and a thorough knowledge of their clinical pharmacology. The safest strategy is for the anaesthetist to use drugs with which he or she is familiar: the trauma resuscitation room is not the place for experimentation. Anaesthetic requirement is assessed individually, and the risk of awareness kept to a minimum. Patients with severe burns should be stabilised and transferred to the nearest burns centre. The patient with a thermal injury to the respiratory tract may develop airway obstruction rapidly from the oedema. These patients should receive a standard or slightly reduced dose of induction drug. Induction drugs would be inappropriate, but muscle relaxants may be used to facilitate intubation. Give anaesthetic and analgesic drugs as soon as adequate cerebral perfusion is achieved. Suxamethonium retains its status as the neuromuscular blocker with the fastest onset of action, and remains the most popular relaxant for intubation of the acute trauma patient. In the presence of adequate anaesthesia, suxamethonium does not increase intracranial pressure in severe head-injured patients. Rocuronium is almost as fast in onset and is favoured by some trauma anaesthetists. Contrary to more traditional opinions, the longer duration of action in comparison with suxamethonium may be an advantage during trauma patient resuscitation. Intraoperative management the following considerations are of relevance to the anaesthetist during surgery for the severely injured patient: r Prolonged surgery. The combination of hypothermia and massive transfusion will cause profound coagulopathy. This needs frequent monitoring (arterial blood gases) and correction with fluids and inotropes, as appropriate. It is more efficient if surgical teams from different specialties are able to work simultaneously; however, this may severely restrict the space available to the anaesthetist! This may be secondary to direct pulmonary contusion or to fat embolism from orthopaedic injuries. This large vein is consistently located directly medial to the femoral artery in the groin, and as long as the artery is palpable the vein is normally easily cannulated using a Seldinger technique. If a chest drain has been inserted, use the same side for subclavian access unless a major vascular injury is suspected. Chest drainage A tension pneumothorax should be immediately decompressed by insertion of a cannula through the second intercostal space in the mid-clavicular line. Other indications for chest drainage in the trauma patient are simple pneumothorax, haemothorax, and rib fractures in a patient requiring positive pressure ventilation. Do not use a trochar for chest drain insertion: it can cause serious lacerations of the lung and pulmonary vessels. Cannulation of the subclavian vein Central venous cannulation can be difficult in the hypovolaemic patient. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Helical computed tomographic scanning for the evaluation of the cervical spine in the unconscious, intubated trauma patient. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. Prospective validation of computed tomographic screening of the thoracolumbar spine in trauma. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. Clearing the cervical spine in unconscious polytrauma victims, balancing risks and effective screening. Clearing the cervical spine after polytrauma: implementing unified management for unconscious victims in the intensive care unit. Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults. Orotracheal intubation in patients with potential cervical spine injuries: an indication for the gum elastic bougie. Inflammatory mediators in relation to the development of multiple organ failure in patients after severe blunt trauma. It contains the tongue, alveolar arches that comprise the gums and teeth and the openings of the salivary glands. The mucous membrane is stratified squamous epithelium and the opening of the parotid duct lies just above the second molar crown. Posteriorly the oropharyngeal isthmus separates the oral cavity from the oropharynx. The lining consists of mucous membrane, which is stratified squamous epithelium with mucous glands beneath. Teeth Structure Each tooth has a crown, a neck and roots that penetrate the alveolar bone. At the crown the dentine is covered by enamel whereas the dentine of the root is covered by cementum. Nerve supply the teeth of the upper jaw are supplied by the anterior and posterior superior alveolar nerves whereas the teeth of the lower jaw are supplied by the inferior alveolar nerve. The gums of the upper jaw receive supply to the labial surface via the infraorbital and posterior superior alveolar nerves and supply to the lingual surface via the nasopalatine and greater palatine nerves. The gums of the lower jaw receive supply to the labial surface via the Fundamentals of Anaesthesia, 3rd edition, ed. Blood supply the tongue is supplied by the lingual artery and drains via the deep lingual vein into the internal jugular vein. Lymphatic drainage the tip of the tongue drains into the submental nodes, the sides into the submandibular glands and the posterior third into the retropharyngeal and jugulodigastric nodes. It is attached to the mandible and the hyoid bone and rests on the geniohyoid and mylohyoid muscles.
Syndromes
- Take the medicines your doctor told you to take with a small sip of water.
- Upper GI and small bowel series
- Blood culturesBronchoscopy
- Abnormal fat and connective tissue in calf muscles
- Toxic drug reaction (Toxic epidermal necrolysis)
- Hold the object as close to your body as you can.
- Fainting or feeling light-headed
Medex 5mg cheap
Complications the main complications of these nerve blocks are the potential for intravascular injection or vascular trauma hiv infection rate in africa 1mg medex mastercard, as all the injections are made into neurovascular bundles (except the sural nerve). However, the volumes of local anaesthetic are small, the needle used should be no larger than 23 gauge, and aspirating the needle before each injection will minimise the risk. Many patients will be mobilised soon after surgery, and they must be supervised and non-weight bearing whilst the blocks are still working because they will have no sensory or proprioceptive awareness in the sole of the foot if the tibial nerve has been blocked. Inguinal field block Indications Inguinal field block in combination with light general anaesthesia is ideally suited to day case repair of a hernia. If the surgery is to be performed using local anaesthesia as a sole technique, a larger volume of more dilute local anaesthetic is preferable, and the surgeon may need to reinforce the anaesthesia by direct infiltration of the deeper structures within the inguinal canal. Make a skin weal of lidocaine at this point and insert a 22 G short bevel regional block needle, at right angles to the skin, directly downwards through the skin and subcutaneous tissue. Move the needle from side to side in a horizontal plane and a distinct scratching over the surface of the aponeurosis will be felt. The iliohypogastric nerve (T12/L1) lies just deep to the aponeurosis, so once the needle penetrates it, immobilise the needle and inject 5 ml of local anaesthetic. Withdraw the needle to the subcutaneous tissues and infiltrate a subcutaneous, fan-shaped area, using 10 ml of solution to block the terminal fibres of the subcostal nerve (T12). Insert the needle directly down to the tubercle and inject 5 ml of solution around the external inguinal ring to anaesthetise the genitofemoral nerve (L1/2). Make a second fan-shaped subcutaneous infiltration to block any fibres that may cross the midline. Complications There are few important complications, as the technique is mainly one of infiltration together with the discrete blockade of three small peripheral nerves. From the first point of injection, puncture of the peritoneum and viscera is possible if a long needle is used. Inadvertent intravascular injection is always a possibility with the second point of injection, especially the femoral vessels. It is also possible to block the femoral nerve from the same point and the patient may complain of pain in the hernia site and a numb, heavy leg. Analgesia is comparable with that produced by a caudal block and avoids the motor and sensory effects on the legs and the autonomic dysfunction of bladder and bowel control. There are no major complications provided that epinephrine or other vasoconstrictors are not used and intravascular injection is avoided. Anatomy the shaft and glans of the penis are supplied by a pair of nerves (the dorsal penile nerves) which are terminal branches of the pudendal nerve (S2, 3, 4). The perineal nerves (from the other branch of the pudendal nerve) which innervate the anterior part of the scrotum and the midline ventral surface of the penis need to be blocked for complete penile analgesia. Palpate the inferior edge of the pubic symphysis with the non-dominant index finger and insert a 21 G (adult) or 23 G (paediatric) needle at about 45 degrees until it contacts the pubis or passes just caudad to it. After careful aspiration, make a single injection in the midline (both dorsal nerves may be reliably blocked by a single injection). In an adult, inject 7 ml and then inject a further 3 ml as a subcutaneous weal across the midline of the ventral surface of the penis at its junction with the scrotum, starting approximately 1 cm lateral to the midline raphe and finishing 1 cm lateral on the other side. It is important to keep the needle subcutaneous while making this injection as the urethra is superficial at this point. In children the volume needs to be reduced pro rata according to body weight and penile size. The trigeminal nerve supplies the nasopharnyx, palate (V2) and anterior aspect of tongue (V3). The glossopharyngeal nerve supplies the oropharnyx, posterior aspect of tongue and soft palate. The superior laryngeal nerve emerges beneath the inferior edge of the greater cornu of the hyoid before it divides into the internal and external branches. Drugs, doses and volumes Avoid local anaesthetic solutions that contain epinephrine. Technique the technique of local anaesthesia of the upper airway comprises three parts, topical anaesthesia, superior laryngeal nerve block and transtracheal anaesthesia. Local anaesthesia of the upper airway the mucosal surfaces of the mouth, oropharnyx, glottis and larynx may be anaesthetised by a combination of topical anaesthesia and discrete nerve blocks. Bier placed two tourniquets on the forearm and injected procaine directly into a vein isolated Indications Intubation of the trachea in patients with difficult airway due to trauma or disease. Depress the tongue and spray a further four puffs onto the posterior part of the tongue and pharynx. Although the superior laryngeal nerve can be topically anaesthetised by placing a pledget soaked in lidocaine 2% into each pyriform fossa with Krause forceps, once the mouth and tongue are blocked, it is more usually blocked discretely as follows. Place the patient supine with the head extended and palpate the hyoid bone just cephalad to the thyroid cartilage. To complete the airway anaesthesia, with the patient in the same position as above, palpate the inferior border of the thyroid cartilage and, having first anaesthetised the skin, insert a 21 G, 2. Although a two-tourniquet technique has been re-evaluated recently, one tourniquet is used in modern practice. Indications Any surgery lasting less than 1 hour below the level of the elbow in the arm or the ankle in the leg. Specially designed double cuff tourniquets are available: these allow the proximal cuff to be blown up while the block is established, and then the distal cuff is inflated over anaesthetised skin for use during surgery and the proximal one deflated. This improves comfort during prolonged procedures, but the patient may still experience deep pain from ischaemic muscle. Wrap a layer of wool padding around the upper arm and place the tourniquet over the padding, ensuring that it is of the correct dimensions for the limb and properly secured. Elevate the limb and use a compression bandage to exsanguinate it or simply compress the axillary artery and keep the arm elevated for three minutes. If blood begins to flow under the tourniquet the procedure should be repeated, using a pressure 150 mmHg above systolic, or an alternative anaesthetic technique considered. Inject the local anaesthetic solution slowly (20 ml per minute) to avoid high intravenous pressures which could force it under the tourniquet. There is also a risk of damage to the peroneal nerve in the region of the head of the fibula if a high tourniquet is applied. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Spread of extradural analgesia following caudal injection in children: a statistical study. The cuff should remain inflated for at least 20 minutes, after which time deflation of the cuff and systemic release of the local anaesthetic drug should not cause untoward reactions, although occasionally some transient minor systemic symptoms such as light-headedness or tinnitus are reported. From this meeting the 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations (International Liaison Committee on Resuscitation 2005) were published. Causes A person suffers a cardiorespiratory arrest either because of a primary cardiac problem or secondary to non-cardiac causes. Other cardiac conditions which may lead to cardiorespiratory arrest include valvular heart disease, cardiomyopathy, myocarditis, endocarditis and conduction defects. An important secondary cause of cardiorespiratory arrest is uncorrected hypoxia resulting from airway obstruction. Hypoxia leads to myocardial failure, which is compounded by the resulting hypercarbia and acidosis. A bradycardia will develop, and this will be followed by an asystolic cardiac arrest unless the airway obstruction is cleared. Other non-cardiac causes of cardiac arrest include: r Hypothermia r Intracerebral haemorrhage r Mechanical massive pulmonary thromboembolism or air embolism tension pneumothorax pneumopericardium cardiac tamponade hypovolaemia r Poisoning Despite trained cardiac arrest teams being present and readily available to manage cardiac arrests in hospital, less than 20% of patients who suffer an in-hospital cardiac Fundamentals of Anaesthesia, 3rd edition, ed. Most unmonitored patients who suffer cardiac arrest have shown evidence of hypoxia and hypotension for several hours prior to their arrest, which either goes unnoticed or is poorly treated. It is therefore imperative that, as well as being able to recognise a patient who is having a cardiorespiratory arrest, systems are put in place to allow early identification and management of those patients who if left untreated will deteriorate and suffer a cardiorespiratory arrest. Checking for a carotid pulse, whether by trained healthcare professionals or by lay rescuers, has been shown to be not only time-consuming but also an inaccurate method of confirming either the presence or absence of circulation.
Purchase discount medex
Their effects are wide-ranging and include stimulation of the inflammatory response antiviral lip cream buy 1 mg medex overnight delivery, regulation of local blood flow, control of membrane transport, modulation of synaptic transmission and modulation of platelet adhesion. A key step in the synthesis of prostaglandins is cyclo-oxygenase, which can be inhibited by non-steroidal anti-inflammatory drugs such as aspirin. Ketones When excessive levels of acetyl-CoA are present, the acetylCoA is diverted to form acetoacetate and -hydroxybutyric acid. Normally glycolysis is responsible for supplying the acetyl-CoA for the citric acid cycle, but if the glycolytic pathway fails, as in uncontrolled diabetes or starvation, acetyl-CoA is obtained from oxidation. This should be differentiated from malnutrition, in which some calorific intake may be present, but which follows a more protracted course accompanied by the effects of chronic lack of protein, fats and essential vitamins and minerals. In starvation, glucose supplies to the brain are a priority, since it is largely dependent on glucose as an energy substrate. However, as glycogen reserves are depleted, blood glucose falls to subnormal levels. Mobilisation of fatty acids occurs to provide energy, and the liver ceases to use glucose as a substrate but uses fatty acids instead. With the depletion of glycogen, gluconeogenesis increases, using amino acid residues derived from the breakdown of muscle protein. Gluconeogenesis takes place in the liver, which also uses glycerol from lipolysis and oxaloacetate. The use of these substrates leads to the accumulation of acetyl-CoA and hence the formation of ketone contributed to by both diet (normal daily intake is about 1 g) and endogenous synthesis. Abnormally high levels of cholesterol result in disease due to deposition of cholesterol in soft tissues and formation of cholesterol-containing plaques in arteries (atherosclerosis). Eicosanoids the eicosanoids are C20 unsaturated fatty acids containing a five-carbon ring. They are derived from arachidonic acid, which is synthesised from linoleic acid, one of the essential fatty acids. Most tissues, including the brain, can ultimately adapt to the use of ketone bodies as a fuel source. Therefore, protein catabolism is quite rapid in early starvation, but as the body shifts to the use of ketone bodies, the rate of protein breakdown decreases. The total reserves of an average adult are sufficient to provide the calorie requirements for about 3 months. Protein synthesis the major proteins synthesised by the liver include albumin, globulins and clotting factors. Plasma albumin correlates well with liver synthetic activity, but with a half-life of about 20 days, it is a poor marker for acute liver injury. Albumin is important in the maintenance of plasma colloid oncotic pressure, and in the transport of drugs, bilirubin and some hormones. Globulins these are a range of lipo- and glycoproteins with transport functions. The liver is the principal site for synthesis and recycling of haptoglobin, which serves to bind and conserve free haemoglobin. These are roughly hexagonal in cross section and possess a central vein from which cords of hepatocytes radiate outwards. In between the lobules are portal spaces through which run a bile duct and branches of the hepatic artery and portal vein. The radial spaces between the hepatocytes are called sinusoids and carry a mixture of arterial and portal blood supplied by the vessels in the portal spaces, towards the centre of the lobule, where it drains into the central vein. The central veins join to form the hepatic vein, which drains into the inferior vena cava. As the blood flows though the sinusoids it is exposed over a large surface area to the hepatocytes, which are highly active metabolically. The walls of the sinusoids are also lined by macrophages known as Kupffer cells, which are an active part of the reticuloendothelial system. The cords of hepatocytes are closely apposed to bile cannaliculi, which drain centrifugally towards the bile ducts in the portal spaces. Protein catabolism the liver is involved in protein catabolism either directly, in turnover of proteins in the hepatocyte, or indirectly, in handling the products of the absorption of dietary proteins or amino acids from peripheral protein turnover. Amino acids or dipeptides from portal or systemic circulations are absorbed by the liver. They may be used as substrates for new protein synthesis, or used for gluconeogenesis. The conversion of amino acids to carbon skeletons may involve transamination, deamination or modification to primary amines. The by-product from deamination is ammonia, which may be converted by the ornithine cycle to ammonia. Detoxification the liver has a major function in the detoxification of steroid hormones. The mechanisms for detoxification are also used for the metabolism of exogenous substances, in particular therapeutic drugs. Cold signals travel via A fibres, and warm signals via C fibres in the spinothalamic tracts. This temperature information is integrated and compared to temperature thresholds. Thermoregulation is currently thought to be based on a series of thresholds that activate thermoregulatory responses when crossed by the integrated temperature information. If the warm threshold is exceeded, heat-loss responses are initiated, which include: r Behavioural modification. A large part of first-pass metabolism may be due to cytochrome activity in the gut mucosa. Similarly, nephrotoxicity after the metabolism of volatile anaesthetic agents may be due to intrarenal metabolism by cytochromes, rather than a consequence of elevated plasma fluoride levels. Drugs that have been modified by phase 1 metabolism are usually left with reactive end groups (such as hydroxyl). The overall result of phase 1 and 2 metabolism is to produce a modified drug structure that is hydrophilic and rapidly eliminated by the kidneys. Thermoregulatory responses There are several effective thermoregulatory responses in the normal human. Vasoconstriction minimally reduces capillary flow but has major effects on the shunts, which act as thermoregulator mechanisms. The effectiveness of this heat source is reduced by the fact that muscle activity also increases blood flow to peripheral tissues, dissipating the heat generated. Normal body temperature is 37 C and thermoregulatory mechanisms maintain this temperature with a standard deviation of about 0. There are normal variations within this range, such as a circadian variation of up to 0. A variation during the menstrual cycle produces a rise in temperature at ovulation. Body temperature may be altered by various factors including exercise, feeding, thyroid disease, infection and drugs. This can increase heat production by up to 100% in infants, but is much less effective in adults. Hypothermic effects of anaesthesia and surgery Anaesthesia has a number of effects on thermoregulation. An individual is unable to control his or her environment, clothing levels or level of voluntary muscle activity. In addition, thresholds are directly affected by anaesthesia, which tends to increase the displacement of the thresholds from normal temperature.
Purchase medex with mastercard
Cell-mediated immunity T-cell-independent mechanisms the two T-cell-independent mechanisms are phagocytosis and cytokine release general symptoms hiv infection buy medex with amex. They can then bind, engulf and kill pathogens, utilising oxidant free radicals and peroxides. The inflammatory response the clinical signs of inflammation are heat, redness, swelling, pain, and reduced function. Larger molecules are allowed to pass across the endothelium, and thus plasma enzyme systems reach the site of inflammation. Pathologically inflammation is diagnosed when there are increased numbers of granulocytes, macrophages and lymphocytes in a tissue section. It is thought that Tc cells are important in recognising and destroying virus-infected cells. Histamine and leukotrienes (B4 and D4) these are released by basophils and their tissue equivalent, mast cells, after stimulation by microbes, and result in increased vascular permeability. Leukotrienes are products of arachidonic acid metabolism via the lipoxygenase pathway. Neutrophil adhesion and migration across the endothelium Under normal, steady-state conditions, while leucocytes flow in close proximity to the endothelium they do not adhere to it. The neutrophil then, attracted by chemotactic agents, migrates between endothelial cells and along the subendothelial matrix of collagen, laminin, etc. Macrophages and monocytes also migrate along the same chemotactic gradients and engulf microbes, as well as presenting antigens to T and B lymphocytes as described above. Activated endothelium becomes procoagulant, adhesive, more permeable and produces increased nitric oxide, resulting in smooth muscle relaxation and vasodilatation. Complement Complement components C3a and C5a are inflammatory mediators, and their production is described below. C5a also increases capillary permeability, activates neutrophils and stimulates phagocyte chemotaxis. It has since been realised that complement performs three major functions: r Opsonisation (coating) of bacteria and immune complexes r Activation and attraction (chemotaxis) of phagocytes r Lysis of target cells There are many proteins involved in the complement system, and a detailed account of all of these is not appropriate here. An outline of complement activation is given in the classical and alternative pathways below. C3b attaches to microorganisms or immune complexes and acts as a site of membrane attack complex formation. The small peptide cleaved from C3, C3a, stimulates mast cell degranulation and smooth muscle contraction. C1q can bind to the Fc regions of aggregates of IgG1 or IgG3 molecules bound to antigen (immune complexes). C1q also attaches to single antigen-bound IgM molecules, which are by nature pentameric. Binding of C1q leads to conformation change in the C1 complex resulting in auto-activation of C1r, which in turn activates C1s. The next step is activation of C4 with the production of C4b, which avidly binds surface carbohydrates or proteins: thus complement activation is localised to a surface. As with the coagulation cascade, the large number of steps ensures amplification and offers opportunity for regulation. Inhibitors of the classical pathway help ensure localisation of complement activation. This is achieved by hydrolysis of C3 to form C3i, which in the presence of magnesium is able to associate with Factor B. The above reactions occur in the fluid phase but C3b attaches itself to any adjacent surface. Hypersensitivity Hypersensitivity occurs when an otherwise beneficial immune response is inappropriate or exaggerated, resulting in tissue damage. Type I Type I hypersensitivity, also referred to as immediate hypersensitivity, is an IgE-mediated response. In the skin eczema or urticaria will result; if the antigen is inhaled asthma occurs; in the nasal passages allergic rhinitis (hay fever) develops. This response should be distinguished from the anaphylactoid reaction that can be induced by certain drugs. C3bBb is a C3 convertase and also combines to C3b to act as a C5 convertase, which initiates membrane attack complex formation. Here again is a system in which a large number of reaction steps occurring on a surface produces considerable amplification. Bacteria with surfacebound C3b, C3i or C4b (which implies immunoglobulin binding also) are said to be opsonised, and are readily phagocytosed by neutrophils or macrophages. Formation of the membrane attack complex this is the final common pathway of complement activation. C5b can then aggregate with C6 and C7 to produce C5b67 which, being hydrophobic, attaches to plasma membranes. The resulting C5b678 complex polymerises a number of C9 molecules to form the membrane attack complex (C5b6789n), which is essentially a pore in the cell membrane; lysis is thus produced. This together with complement is deposited on the glomerular and pulmonary basement membranes, and neutrophils attach via their Fc and complement receptors. As they are unable to phagocytose, they discharge their lysosomal contents, which results in damage to the basement membrane. There is often widespread deposition of these immune complexes that activate complement via the classical pathway. Most commonly this is in response to a hapten, which is a molecule too small to induce an immune response. Antigen is presented to Langerhans cells, which interact with sensitised Th cells, and these then release cytokines, activating keratinocytes that release further cytokines to produce the eczematous lesions. The cells responsible for the reaction are Th and Tc cells, macrophages and monocytes. Again, Th cells are critical in the production of these reactions, which result from a continuous antigen stimulus or where macrophages are unable to destroy the antigen. The precise shape and distribution of a muscle, or muscle group, about a joint depends on its particular function. The myosin filaments occupy the central part of the sarcomere and comprise the A band. The A band is transected by the M line, which keeps the myosin filaments in side-by-side alignment. The myosin filaments interdigitate with the thin actin filaments whose ends are joined to the Z line or disc which maintains their spatial arrangement. The area of myosin filaments in the middle of the sarcomere not overlapped by actin filaments is known as the H zone. The myoplasm between the filaments contains glycogen, myoglobin, the enzymes involved in glycolysis and mitochondria. Microscopic structure Muscle cell Muscle cells or fibres are quite large: they are typically about 100 m in diameter, and may run the full length of the muscle. They are multinucleated, are surrounded by a membrane, the endomysium, and are bound into fasciculi. These fasciculi are surrounded by the perimysium, and combine to make up the whole muscle. Myofilaments Thin myofilament the thin actin filament is a helical structure composed of two chains of actin molecules wound around each other. Associated with the tropomyosin at each half turn of the actin/tropomyosin Myofibril the muscle cells or fibres are made up of myofibrils enclosed by the cell membrane (sarcolemma). There are thick filaments composed of myosin and thin filaments that are made up of actin. The heads project from the side of the myosin filament in a helical fashion, with one turn of the helix every six molecules, so that the heads project at 60 to each other and at a distance from each other of 14. Each myosin filament is constructed of two groups of myosin molecules with their tails abutting. There is thus an area bare of myosin heads, or cross-bridge-free region that constitutes the midpoint of the H zone.
Purchase 1 mg medex with amex
These three activities produce a rise in intravascular volume and vasomotor tone with the resultant increase in blood pressure mcgraw hill hiv infection cycle works order medex. They are particularly effective when renin levels are raised, such as when sympathetic tone is increased. These drugs act by selective agonism at the imidazoline subtype 1 receptor (I1) in the rostralventrolateral pressor area and ventromedial depressor areas of the medulla oblongata. This area is responsible for sympathetic activity, and an agonist effect at I1 receptors results in a reduction of general sympathetic nervous system activity which produces the desired effect. An example from this group is moxonidine, a centrally acting antihypertensive agent for mild to moderate hypertension. Moxonidine improves insulin release in response to glucose in animal studies, which could favour its use in obese or diabetic hypertensives in the future. It may exacerbate cardiac conduction defects and should be withdrawn slowly over a 2-week period. Caution is necessary when administering moxonidine with benzodiazepines, as the sedative effects of the latter become enhanced. The first site of interference in this cascade is by antagonism of the adrenoceptors responsible for renin secretion. Interference with sodium reabsorption in the renal tubule causes increased sodium loss, and the sodium takes water with it. This interferes with the generation of the interstitial hypertonicity which is used by the collecting duct to reabsorb water. A smaller effect is due to the increased delivery of filtrate to the distal tubule. These are the most efficacious diuretics, causing up to 25% of sodium and water in the filtrate to be excreted. The protein left in the efferent capillaries supplying the remainder of the nephron is therefore more dilute and has a lower oncotic pressure, which reduces reabsorption from the nephron. Subsequently more filtrate enters the loop of Henle, which is the primary site of action of the loop diuretics. In congestive cardiac failure, the venodilatation reduces preload before any diuretic effect is seen. Loop diuretics work as antihypertensives by reducing both blood volume and vascular tone. The vascular effects may be mediated by interference with prostaglandin E2 and I2 degradation. Hydrogen ions are also excreted in exchange for some of the potassium, and bicarbonate concentration increases. Patients on loop diuretics are therefore at risk of hypokalaemia and metabolic alkalosis. Loop diuretics are highly protein-bound, and therefore do not readily pass through the glomerular membrane. They are actively secreted into the proximal convoluted tubule (via the organic acid transport system) and then travel along the tubule to the luminal membrane of the loop of Henle. They are medium-efficacy diuretics, causing up to 10% of sodium and water in the filtrate to be excreted. More sodium reaches the distal tubules, and this results in high potassium loss in the same way as with the loop diuretics, but because this is the main mode of thiazide action potassium loss is a much greater problem. Excretion is by glomerular filtration and by tubular secretion using the uric acid secretion mechanism, which reduces uric acid excretion. They are low-efficacy diuretics, causing only 5% of sodium and water in the filtrate to be excreted, but have the advantage that they conserve potassium and are mainly used to minimise potassium loss caused by more effective diuretics. The decrease in potassium secretion increases the hydrogen ion secretion and thus reduces bicarbonate excretion. Triamterene and amiloride interfere with the sodium channels through which the effects of aldosterone are mediated. The resultant effect is dependent directly upon the number of molecules, and so a large number of molecules is required to produce a clinical effect. Urea is classified as an osmotic diuretic but is actively secreted into the tubule as well. Other examples of carbonic anhydrase inhibitors are methazolamide and dichlorphenamide. Poorly removed by dialysis as highly tissue-bound; digoxin-specific antibody fragments available for treatment of poisoning. The inhaled mode allows a higher concentration of agent to be delivered directly to the bronchial tree, which minimises absorption and accompanying systemic effects. Some drugs are metabolised in the lungs, resulting in a non-hepatic first-pass effect. Typically, only 10% of an inhalationally administered bronchodilator reaches the lungs. Most of this is deposited in the upper airways with little benefit, with about 3% reaching the alveoli. Distribution is little affected by the presence of obstructive airways disease, or by particle size. They are so-named because of their presence in white blood cells (the leuko component) and their chemical bonds (a triene system of double bonds). They are a group of eicosanoids (bioactive lipid derivatives of arachidonic acid). Leukotrienes are produced by the action of the enzyme 5-lipoxygenase, which is found in white blood cells (particularly eosinophils) and mast cells, among other tissues. This selectivity is not absolute, and high doses of these drugs will cause 1 effects (tachycardia, tremor, hyperglycaemia, increased insulin secretion and hypokalaemia). The 2 -agonist salbutamol is the most widely used agent in the treatment of asthma. It is conjugated in the liver and excreted in both conjugated and unchanged forms in urine and faeces. Terbutaline is a similar agent that may Fundamentals of Anaesthesia, 3rd edition, ed. Terbutaline may be used antenatally to stimulate fetal lung surfactant production. These drugs act at muscarinic acetylcholine receptors and so inhibit bronchoconstriction. A small amount of drug is absorbed systemically from the oral mucosa, and this is metabolised by the liver. Antagonism at the (negative feedback) M2 receptor increases acetylcholine release, which may limit the effectiveness of its M1 -mediated bronchodilatation.
Amangura (Ashwagandha). Medex.
- How does Ashwagandha work?
- Are there safety concerns?
- Tumors, tuberculosis, liver problems, swelling (inflammation), ulcerations, stress, inducing vomiting, altering immune function, improving aging effects, fibromyalgia, and other conditions.
- Are there any interactions with medications?
- What is Ashwagandha?
- Dosing considerations for Ashwagandha.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96916
Cheap medex master card
The majority of older children will accept dental extraction with local anaesthesia but if extractions are proposed in more than two quadrants of the mouth then it is unwise to do this all at one sitting because of the inevitable risk of total anaesthesia of the tongue and palate leading to obstruction or aspiration hiv infection pathogenesis proven 5mg medex. General anaesthesia may be necessary for conservative dentistry in those with severe learning difficulties. This may be a prolonged procedure involving multiple restorations and should be carried out with the airway protected by either an endotracheal tube or a laryngeal mask and an absorbent pack in place. Dental drills have an incorporated water spray, which can precipitate laryngeal spasm in the unprotected airway. Adenoidectomy in isolation requires the airway to be maintained via the mouth, either by tracheal tube or by laryngeal mask. Suction clearance of the mouth at the end of the procedure should be carried out under direct vision. Suction at the end must again be carried out under direct vision, but gently, so as not to disturb the tonsillar bed. In both of these cases postoperative analgesia should be provided parenterally before the recovery phase. There are advocates of both spontaneous and controlled ventilation for these procedures. Anaesthesia for myringotomy or suction clearance of the ears can be relatively simple, intravenous or inhalational induction with face mask or laryngeal mask for airway maintenance. Ophthalmic surgery Ophthalmic surgery in the over-5s is usually for squint surgery or penetrating eye injury, probing and syringing of lachrymal ducts being confined to younger children. Squint surgery is usually carried out as a day case, though the facility for overnight stay should always be available. Induction of anaesthesia should include a weight-related dose of a vagolytic drug such as glycopyrrolate to prevent the severe bradycardia which results from even gentle traction on the extraocular muscles. Squint correction causes the same airway access problems for the anaesthetist as other head and neck surgery. The choice of tracheal intubation or laryngeal mask airway is largely a matter of personal preference, though tracheal tubes cause much more emergence laryngospasm than do laryngeal mask airways. In the presence of spaceoccupying lesions, tumour, blood clot or oedema, for example, the fixed volume of contents increases at the expense of the rest. Later, in the presence of a larger space-occupying lesion, the compliance of the intracranial contents is reduced and so the pressure change is unbuffered and there may be damage to tissue, either directly, by distortion of nerve tracts, or by secondary reductions in blood flow. Management of head injury Head injury should be considered significant if there has been certain loss of consciousness (however brief). Extra- and subdural haematomata also behave as large space-occupying lesions, causing compression and distortion of the brain. These include unsteadiness of gait, disorientation, irritability, nausea and vomiting. As the oedema or space occupation increases or becomes more widespread, the compliance is reduced further and cerebral blood flow is compromised, causing hypoxic damage to brain tissue. Cerebral blood flow depends on the cerebral perfusion pressure, which in turn depends on the relationship between mean arterial blood pressure and intracranial pressure. The best response in each category gives a maximum score of 15, indicating minimal injury, while the minimum score is 3, indicating a very poor state with a very poor outcome. The primary injury has already occurred, and any damage done will be largely irreversible. Uncontrollable confusion and irritability may indicate significant brain injury, and indicates the need for intervention. Although it might appear that unconscious patients do not need to be anaesthetised before intubation, this is not so. The sympathoadrenal response to intubation may be minimised by the administration of an adequate dose of induction agent accompanied by an opioid agent such as alfentanil. The appropriate muscle relaxant to use for intubation is potentially controversial. This is certainly the case in the normal brain, but recent work suggests that it may not be the case in the injured (and therefore less compliant) brain. A possible solution lies in the administration of a large dose of a non-depolarising relaxant such as vecuronium, given after careful preoxygenation and the application of cricoid pressure. The fasciculations of suxamethonium may be modified or abolished by pre-curarisation with a small dose of a non-depolarising relaxant (such as 20 mg gallamine) or by pretreatment with 0. Subsequently, ventilation of the lungs must be maintained by face mask or laryngeal mask airway until the relaxant reaches maximum clinical effect, so as to avoid coughing and movement, which will increase the intracranial pressure even more than intubation itself. This can be achieved by adequate sedation or general anaesthesia with controlled ventilation and moderate hyperventilation. Inhalational agents should be avoided because of their cerebral vasodilator effect and anaesthesia maintained by repeated bolus or infusions of intravenous agents. Blood loss from scalp wounds may be significant in itself and should not be forgotten. Ambulances should be able to travel quickly but smoothly, without the severe shocks of fast travel. An anaesthetic machine with automatic ventilator, piped gases and full monitoring are essential. In practice this usually means that admissions in the morning are discharged at midday while midday admissions are discharged in the early evening and the facility then closed overnight. For the patient, this means the shortest possible time away from the work or home environment and as little disruption as possible to social circumstances. For the first 24 hours after anaesthesia, there must be a responsible adult present on the premises to care for the patient and to manage untoward events. This can be a difficult and dangerous enterprise and should be carried out with the greatest of care. Other injuries Cervical spine injury (cervical spine protection), chest injury, fractured ribs, pneumothorax excluded If these criteria cannot be fulfilled then the surgery must be carried out on an inpatient basis. If the patient arrives for day surgery without these criteria being satisfied then the operation should be cancelled and admission reorganised. Part of the admission process must be to check that these criteria have been satisfied. The patient must be told to avoid alcohol for 24 hours postoperatively, because the depressant effect of alcohol acts synergistically with the residual anaesthetic drugs and, especially if barbiturate anaesthetics are used, may cause unconsciousness. Patients must be told not to drive vehicles or operate machinery, because their physical and mental reactions may not be good enough to keep them out of danger. Car insurance may be invalidated by driving under the residual influence of anaesthetics, and the police may charge the driver with driving under the influence of drugs. Lifetime or important decisions should not be made in the postoperative period, because patients may be residually disinhibited. Preoperatively the day-case patient must be told these rules in front of a witness, or must sign a form to say that they have been read while not under the influence of anaesthetic drugs. Surgical procedure the types of surgery suitable for day-case work include those with only minor disturbances of nutrition, which last only a short time (usually taken to be less than 45 minutes of anaesthesia) and which do not usually require opioid analgesia afterwards. Surgery where significant blood loss is predicted, or where the abdomen is electively opened, is not suitable (except for minor laparoscopic surgery). Unilateral inguinal hernia repair may be suitable (especially if local anaesthesia is employed), but bilateral repair is not. Surgery should only be carried out by surgeons experienced in the procedure in question. Essential hypertension is not necessarily a contraindication provided control is good. Cardiovascular diseases such as angina, cardiac failure or arrhythmias are unacceptable. Obesity is not acceptable (criteria differ, but body weight >100 kg or body mass index >30 may be taken as exclusion guidelines).
Cheap medex express
The intracellular electrical potential opposes Cl- entry into the cells from the tubular lumen hiv infection stories australia purchase generic medex. Thus, the net result of the Cl- and Na+ antiport systems is the reabsorption of equal amounts of Cl- and Na+ from the lumen into the tubular cells. Up to 20% of NaCl reabsorption in the late proximal tubule occurs by this mechanism. Chloride reabsorption in the proximal tubule Reabsorption of other solutes in the proximal tubule Sodium reabsorption leads to electrical, concentration and osmotic gradients for the reabsorption of such solutes as Glucose Normally, almost all of the filtered glucose is reabsorbed and a negligible amount is excreted. Although most glucose reabsorption occurs in the proximal tubule, more distal parts of the nephron are also capable of reabsorbing glucose. The amount of glucose filtered is directly proportional to the plasma glucose concentration. No glucose is excreted in the urine unless the plasma glucose concentration exceeds about 11 mmol l-1 (200 mg per 100 ml). At this plasma glucose concentration, those nephrons with the lowest capacity for glucose reabsorption (relative to their filtration rate) reach their glucose reabsorptive rate limit, and glucose begins to be excreted. Further increases in plasma glucose concentration saturate the glucose transport process of an increasing proportion of nephrons until, when the plasma glucose concentration is about 22 mmol l-1, no nephrons can absorb their entire filtered glucose load. The type of transport process typified by glucose reabsorption is known as Tm -limited transport. The filtered load of glucose can therefore be far in excess of the reabsorptive capacity of the nephrons, so that glucose is excreted in the urine. This excretion of osmotically active solute causes an osmotic diuresis resulting in water loss from the body and, hence, dehydration and thirst. Relationship of glucose reabsorption to sodium reabsorption Proximal tubular glucose absorption is linked to sodium reabsorption. Symporter carrier proteins that possess both sodium and glucose binding sites transfer sodium ions and glucose molecules simultaneously into the tubular cells. The movement of sodium occurs down its electrochemical gradient (co-transport), thus providing the energy to transfer glucose against its gradient (counter-transport). This in turn depends on the extrusion of sodium from the proximal tubule cells by the sodium pump. Note that in the pars convoluta, the stoichiometry of the glucose sodium co-transport is one glucose molecule per sodium ion, but in the pars recta it is one glucose per two sodium ions. These are for: r Basic amino acids r Glutamic and aspartic acids r Neutral amino acids r Glycine r Cysteine and cystine r and amino acids the functional characteristics of these transport processes are very similar to that for glucose. Amino acid entry into the proximal tubule cells from the lumen is a co-transport process with sodium, the driving force being the sodium gradient. Amino acids are readily filtered at the glomeruli, but negligible quantities are excreted, because there are effective Tm -limited transport processes for amino acids in the proximal tubule. Bones and teeth are salts of calcium and phosphate, and the skeleton accounts for about 80% of the body phosphate content. Normally, the urinary phosphate excretion is <20% of the amount filtered, but above a phosphate concentration of about 1. Urea is the end product of protein metabolism and clinically is measured as blood urea nitrogen. Because urea is a small molecule, it is reabsorbed in the proximal tubule as a consequence of sodium reabsorption. Thus, as sodium chloride and water are abstracted from the proximal tubule, the urea concentration in the tubular fluid tends to increase and so urea is reabsorbed passively by diffusing down its concentration gradient, out of the tubule. The urea handling of the more distal parts of the nephron plays an important part in the process of concentrating the urine, and is considered later. In addition, the 3 distal parts of the proximal tubule are more permeable to Cl- than to other solutes. There are three proximal tubular secretory mechanisms that have a definite Tm limit. Organic acid secretion (and uric acid secretion) takes place in the pars recta, but organic base secretion occurs in the pars convoluta. When a substance is filtered and actively secreted, the total amount excreted in the urine is greater than the amount filtered due to transport from the peritubular capillaries into the tubular lumen. The bicarbonate reabsorption mechanism behaves as if there were a Tm for bicarbonate. However, this apparent Tm can be altered by the rate of H+ secretion, which is itself loosely dependent on the rate of Na+ reabsorption. The rate of proximal tubular sodium reabsorption can be varied by changes in the rate of backflux into the tubule, as well as by changes in the rate of active sodium extrusion from the cells. The rate of backflux is affected by the rate of uptake from the lateral intercellular spaces into the capillaries. Reabsorption from the tubule is finally completed by the uptake of water and solutes into the peritubular capillaries. Consequently, the Starling forces in the peritubular capillaries can be modified by the glomerular filtration process. This glomerulotubular mechanism normally ensures reabsorption of a fixed proportion of the gomerular filtrate by the proximal tubule, i. Uptake forces in the peritubular capillaries the forces governing the movement of fluid across the walls of the peritubular capillaries are Starling forces, i. It consists of a descending limb that passes into the medulla and loops round to become the ascending limb, which passes back into the cortex. The salient process is emphasised below: the loops of Henle do not concentrate the tubular fluid within them, but manufacture a hypertonic interstitial fluid in the renal medulla. Urine is then concentrated by osmosis from collecting ducts as they pass through the medulla. The countercurrent mechanism A proposed mechanism for countercurrent multiplication was described by Wirz, Hargitay and Kuhn in 1951. The hypertonic interstitium is produced by a small osmotic pressure difference between the ascending and descending limbs of the loops. This small difference is then multiplied into a large longitudinal gradient by the countercurrent arrangement. The ascending limb is not uniform in structure, but possesses both a thin and a thick segment. This limb produces an increase in the osmolality of the surrounding interstitium by the extrusion of sodium and accompanying ions. Both thin and thick segments of the ascending limb are impermeable to water, so that water is unable osmotically to follow the extruded ions. The entry of solutes into the cells across the apical membrane involves co-transport of sodium, chloride and potassium, with the stoichiometry of one Na+, two Cl- and one K+, so the process is electrically neutral. Much of the K+ leaks back into the tubular lumen, so that it is predominantly NaCl which accumulates in the medullary interstitium. This transport can be inhibited by loop diuretics, such as furosemide and bumetanide. The descending limb is permeable to water and, to a lesser extent, is also permeable to NaCl. The fluid within the descending limb will therefore come to osmotic equilibrium with the interstitium. In effect, then, one can consider the transport of NaCl out of the ascending limb as being directed into the descending limb. The fluid in the ascending tubule leaving the medulla and entering the cortex is hypotonic to plasma, with an osmolality of about 100 mOsm kg-1 H2 O. However, some nephrons possess short loops of Henle, and these are unlikely to lower the osmolality of the ascending limb fluid to 100 mOsm kg-1 H2 O.
Purchase medex 1mg without a prescription
In addition antiviral therapy journal generic medex 5mg amex, proteins that are unique to tumors, such as mutant oncogenes, or are overexpressed in tumors also can be recognized by T cells. Endogenously produced proteins are fragmented in the cytosol by proteases in the proteasome. The resultant peptides are transported into the rough endoplasmic reticulum through the action of a specialized transport system. Each chain consists of two extracellular domains (1 and 2; 1 and 2, respectively), a hydrophobic domain, and a short cytoplasmic segment. The and chains of the I-A molecules (A and A) pair with one another, as do the and chains of I-E (E and E). Thus, the bond between peptide and class I molecule is generally weak in the absence of 2-microglobulin, and the binding of 2-microglobulin strikingly stabilizes the complex. Indeed, this process also occurs within the thymus in the generation of the T-cell repertoire, as already discussed. Furthermore, the affinity of an interaction required for positive selection in the thymus appears to be considerably lower that that required for full activation of peripheral T cells. Our modern understanding of T-cell recognition also aids in explaining the phenomenon of immune response gene control of specific responses. In many situations, the capacity to recognize simple antigens can be found in only some members of a species. These include reactive arthritides, gluten-sensitive enteropathy, insulin-dependent diabetes mellitus, and rheumatoid arthritis (see Chapter 44). Indeed, it appears that many of these diseases are due to enhanced or inappropriate immune responses. Their antigen capture activity is dependent upon expression of several surface receptors including Fc receptors, receptors for heat shock proteins, and C-type lectins. As part of the maturation process, they may also acquire the capacity to produce cytokines and express surface molecules that can aid in determining the polarization of T-cell priming. Monocytes and Macrophages (Chapter 19) Cells of the monocyte/macrophage lineage play a central role in immunity. One of the key goals of cellular immunity is to aid the macrophages in eliminating organisms that have established intracellular infections. In general, non-activated macrophages are inefficient in destroying intracellular microbes. Several mechanisms exist for this purpose, including the development of reactive forms of oxygen, the development of nitric oxide, and the induction of a series of proteolytic enzymes, as well as the induction of cytokine production. They have a set of activating receptors that allow them to recognize features associated with virally infected cells or tumor cells. In addition, the immune system may play an important role in the control of the development and spread of some malignant tumors. The responses that actually cause the destruction of the agents that initiate these pathogenic states. In some cases, antibody can be directly protective by neutralizing determinants essential to a critical step through which the pathogen establishes or spreads an infectious process. However, in most cases, the immune system mobilizes powerful nonspecific mechanisms to mediate its effector function. It is beyond the scope of this introductory chapter to present an extended discussion of each of these important cell types. However, a brief mention of some of their actions will help in understanding their critical functions in the immune response. Mast Cells and Basophils (Chapters 20 and 45) Mast cells and basophils play important roles in the induction of allergic inflammatory responses. Granulocytes (Chapter 20) Granulocytes have critical roles to play in a wide range of inflammatory situations. Rather than attempting an extended discussion of these potent cells, it may be sufficient to say that in their absence it is exceedingly difficult to clear infections with extracellular bacteria and that the immune response plays an important role in orchestrating the growth, differentiation, and mobilization of these crucial cells. They migrate to tissue sites in response to the chemokine eotaxin and as a result of their adhesion receptors. Eosinophils store a series of proteins in their secondary granules including major basic protein, eosinophil cationic protein, and eosionphil peroxidase. When released, these proteins are responsible for much of the damage that eosinophils mediate both to helminthic parasites and to the epithelium. Eosinophils have been implicated as important in protective responses to helminths and in the tissue damage seen in allergic inflammation in conditions such as asthma. The classical pathway of complement activation, usually initiated by the aggregation of C1 by binding to antigen/antibody complexes, resulting in the formation of an enzyme, a C3 convertase, that cleaves C3 into two fragments, C3b and C3a. The classical pathway can also be initiated by the aggregation of mannan-binding lectin as a result of binding sugars expressed in the capsules of many pathogenic microbes. The alternative pathway of complement activation provides a potent means of activating complement without requiring antibody recognition of antigen. In addition, C3b, together with elements of the classical pathway (C4b, C2a) or the alternative pathway (Bb, properdin), form enzymes (C5 convertases) that cleave C5, the initial member of the terminal family of proteins. Cleavage of C5 leads to the formation of the membrane attack complex that can result in the osmotic lysis of cells. The Complement System (Chapter 36) the complement system is a complex system of proteolytic enzymes, regulatory and inflammatory proteins and peptides, cell surface receptors, and proteins capable of causing the lysis of cells. The activation of C3 releases proteins that are critical for opsonization (preparation for phagocytosis) of bacteria and other particles, and engages the third set of proteins that insert into biologic membranes and produce cell death through osmotic lysis. The Classical Pathway of Complement Activation the two activation systems for C3 are referred to as the classical pathway and the alternative pathway. The classical pathway is initiated by the formation of complexes of antigen with IgM or IgG antibody. This leads to the binding of the first component of complement, C1, and its activation, creating the C1 esterase that can cleave the next two components of the complement system, C4 and C2. C1 esterase cleaves the chain, releasing C4b, which binds to surfaces in the immediate vicinity of the antigen/ antibody/C1 esterase complex. A single C1 esterase molecule will cause the deposition of multiple C4b molecules. C2 is a single polypeptide chain that binds to C4b and is then proteolytically cleaved by C1 esterase, releasing C2b. The resulting complex of the residual portion of C2 (C2a) with C4b (C4b2a) is a serine protease whose substrate is C3. Cleavage of C3 by C4b2a (also referred to as the classical pathway C3 convertase) results in the release of C3a and C3b. A single antigen/antibody complex and its associated C1 esterase can lead to the production of a large number of C3 convertases. The Alternative Pathway of Complement Activation Although discovered more recently, the alternative pathway is the evolutionarily more ancient system of complement activation. The alternative pathway can be activated by a variety of agents such as insoluble yeast cell wall preparations and bacterial lipopolysaccharide. The C3 convertase of the alternative pathway consists of a complex of C3b (itself a product of cleavage of C3) bound to the b fragment of the molecule factor B. C3bBb is produced by the action of the hydrolytic enzyme, factor D, that cleaves factor B; this cleavage only occurs when factor B has been bound by C3b. Apart from the importance of the alternative pathway in activating the complement system in response to nonspecific stimulants, it also can act to amplify the activity of the classical pathway because the C3 convertase of the classical system (C4b2a) provides a source of C3b that can strikingly enhance formation of the alternative pathway convertase (C3bBb) in the presence of factor D. This C5b/C9 complex behaves as an integral membrane protein that is responsible for the formation of complement-induced lesions in cell membranes. Such lesions have a donut-like appearance, with C9 molecules forming the ring of the donut. In addition to the role of the complement system in opsonization and in cell lysis, several of the fragments of complement components formed during activation are potent mediators of inflammation. C3a, the 9,000-dalton fragment released by the action of the C3 convertases, binds to receptors on mast cells and basophils, resulting in the release of histamine and other mediators of anaphylaxis.
Purchase medex
Opioid lipophilicity is also important for uptake into peridural fat and epidural veins anti viral foods list cheap medex line. First-pass metabolism of orally administered opioids occurs in the liver and the intestinal wall (up to 50%). The lung exerts a significant first-pass effect on several highly lipid-soluble opioids. Prior administration of other lipophilic amines such as propranolol reduces pulmonary uptake, by saturating binding sites. Distribution Opioids undergo variable degrees of protein binding, primarily to 1 -acid glycoprotein, but also to albumin. Fentanyl, sufentanil, and alfentanil also bind to -globulins, while morphine is bound mainly to albumin. Variability in plasma protein concentration only alters the free fraction for highly protein-bound opioids. Those opioids bound to the acute-phase reactant 1 -acid glycoprotein (especially alfentanil) can achieve variable free concentrations in states of inflammation, infection, malignancy and pregnancy. Dilution or states of low protein concentration increase the free fractions of all highly bound opioids, as does competition for binding sites from other drugs that are basic amines. Due to their high lipid solubility, most opioids tend to be widely distributed throughout the body, resulting in a large volume of distribution (Vd). Redistribution thus has a significant effect on the decline in opioid plasma concentrations after bolus dosing and short-term infusions of certain opioids. Uptake by muscle, visceral organs and the lung contributes to this redistribution. Binding to receptor sites depends on receptor affinity and on any non-receptor site binding. The onset and duration of action of an individual opioid therefore represents a complex interaction between its pKa and the pH of plasma and the pH of the biophase, lipid solubility, and both protein and tissue binding. Small amounts of the more hydrophilic opioids may be excreted unchanged in the urine. Receptor kinetics the diffusion of an opioid to its site of action (biophase) is dependent on its lipid solubility, the driving concentration gradient and uptake into surrounding tissue. Opioid lipid solubility is usually quantified by a specific oil/water (usually octanol/water) partition coefficient. In addition, all opioids are weak bases that dissolve into solutions of protonated (ionised) and free base fractions. The relative proportions of these fractions are dependent on the pKa of the specific opioid and the plasma pH. The un-ionised free base form is always more lipid-soluble than the ionised form, and thus the pKa of any particular agonist is another determinant of its lipid solubility in vivo. The concentration gradient driving diffusion is dependent on the dose and percentage protein binding. Only the unbound fraction of un-ionised drug constitutes the diffusible fraction, which provides the concentration gradient for diffusion into the biophase. In the biophase the opioid receptor only recognises the protonated form of the opioid, and ion trapping in the Morphine the biotransformation of morphine is unique among the opioids. The remainder undergoes sulphation (significant in the neonate, where glucuronidation metabolism is immature), 5% is demethylated to normorphine, and a small amount is converted to codeine, with 10% being excreted unchanged in the urine. The excretion of the morphine-glucuronides is directly related to creatinine clearance. Ninety per cent of conjugated morphine is eventually excreted in the urine, and the remainder excreted in bile, sweat and breast milk. There is also some enterohepatic recirculation of morphine and its glucuronides, particularly in the setting of chronic oral therapy. These active metabolites are more hydrophilic and their subsequent metabolism is as for morphine. Codeine Codeine is mainly metabolised in the liver to codeine conjugates and norcodeine, with some urinary excretion of free codeine. This biotransformation is thought to be the major contributor to the analgesia produced by codeine. Due to genetic polymorphisms, 8% of western Europeans are deficient of this enzyme. These individuals require higher doses, although they may still not obtain effective analgesia. One-third of metabolism involves N-demethylation to norpethidine, which is then hydrolysed to norpethidinic acid. Enzyme induction resulting from chronic pethidine use (and carbamazepine therapy) increases the proportion transformed to norpethidine. Fentanyl and sufentanil the high lipid solubility of fentanyl and sufentanil contributes to their large volume of distribution, which causes rapid and continued peripheral tissue uptake, limiting initial hepatic metabolism. This results in greater variability in plasma concentrations (13-fold range for fentanyl) during the elimination phase, particularly with fluctuations in muscle blood flow that may contribute to secondary peaks in plasma concentration after large doses. Fentanyl, sufentanil and alfentanil undergo little unchanged renal excretion, being metabolised in the liver via similar pathways. Variations in the activity of this enzyme are thought to explain the variability in the kinetics and dynamics of alfentanil infusions. Remifentanil Remifentanil is a structurally unique methyl ester that undergoes widespread and rapid extrahepatic metabolism by blood and tissue non-specific esterases. This process is non-saturable and results in a clearance that is several times hepatic blood flow. The primary metabolic pathway is de-esterification to a carboxylic acid metabolite, with 90% of the drug recovered from the urine in this form. This metabolite is also a full agonist at receptors, but has a potency 1/4600 that of the parent compound and is of no clinical significance even in renal failure. The high clearance and low volume of distribution of remifentanil mean that the offset of its effect is due to metabolism rather than redistribution; this explains its very short contextsensitive half-life irrespective of the duration of infusion. All highly lipid-soluble drugs are sequestered into fat stores after prolonged infusions. Even after large single boluses or sequential boluses there is likely to be a delayed clinical recovery because the fall in plasma drug concentration by elimination of drug from the central compartment is retarded by the return of opioid from the peripheral compartments. The context-sensitive half-life for most opioids, except remifentanil, increases with increasing duration of infusion. The pharmacokinetic parameters of opioids are unrelated to absolute body weight except for distribution parameters. Rather, they correspond to lean body weight, and dosages should be on the basis of ideal (estimated lean) body weight. Caution in obese individuals is recommended when giving prolonged infusions of all opioids other than remifentanil, because their larger volume of distribution will prolong the elimination half-life. Renal failure is only of clinical significance for the use of morphine and pethidine. The clearance of the fentanyl congeners is not altered appreciably, although the reduction in plasma proteins may potentially alter the free fraction of the opioid. Surprisingly, the pharmacokinetics of most opioids is unchanged in liver failure, except in the setting of liver transplantation. This demonstrates the substantial metabolic reserve of the liver, particularly in relation to conjugation reactions. It also causes a reduction in plasma proteins and increases in total body water through the formation of oedema, which may alter distribution kinetics and unbound drug fractions. The metabolism of morphine is the least likely to be altered by liver disease, mainly because of the preservation of glucuronidation in all but fulminant liver failure.