Discount 25 mg pamelor mastercard
A multicenter anxiety keeping me up at night discount pamelor 25mg, openlabel, observational study of testosterone gel (1%) in the treatment of adolescent boys with klinefelter syndrome or anorchia. Pubertal induction in adult males with isolated hypogonadotropic hypogonadism using long-acting intramuscular testosterone undecanoate 1-g depot (Nebido). Physiological estrogen replacement therapy for puberty induction in girls: a clinical observational study. Use of percutaneous estrogen gel for induction of puberty in girls with Turner syndrome. Low areal bone mineral density values in adolescents and young adult turner syndrome patients increase after long-term transdermal estradiol therapy. Identifying the unmet health needs of patients with congenital hypogonadotropic hypogonadism using a web-based needs assessment: implications for online interventions and peer-to-peer support. Long-term effect of gonadotropin-releasing hormone agonist therapy on final and near-final height in 26 children with true precocious puberty treated at a median age of less than 5 years. Unsustained or slowly progressive puberty in young girls: initial presentation and longterm follow-up of 20 untreated patients. Treated and untreated women with idiopathic precocious puberty: long-term follow-up and reproductive outcome between the third and fifth decades. A significant increase in the incidence of central precocious puberty among Korean girls from 2004 to 2010. Central precocious puberty following the diagnosis and treatment of paediatric cancer and central nervous system tumours: presentation and long-term outcomes. Abnormal timing of menarche in survivors of central nervous system tumors: a report from the Childhood Cancer Survivor Study. Central precocious puberty in children living in Spain: incidence, prevalence, and influence of adoption and immigration. The effect of medroxyprogesterone acetate on adrenocortical function in children with precocious puberty. Control of the rhesus monkey menstrual cycle: permissive role of hypothalamic gonadotropinreleasing hormone. Treatment of true precocious puberty with a potent luteinizing hormone-releasing factor agonist: effect on growth, sexual maturation, pelvic sonography, and the hypothalamic-pituitary-gonadal axis. Some hypothalamic hamartomas contain transforming growth factor alpha, a puberty-inducing growth factor, but not luteinizing hormone-releasing hormone neurons. Transcallosal resection of hypothalamic hamartomas, with control of seizures, in children with gelastic epilepsy. Hypothalamic hamartoma with gelastic seizures in Swedish children and adolescents. Gamma knife surgery for hypothalamic hamartomas accompanied by medically intractable epilepsy and precocious puberty: experience in Mexico. Endocrine long-term follow-up of children with neurofibromatosis type 1 and optic pathway glioma. Circulating growth factor levels are associated with tumorigenesis in neurofibromatosis type 1. Early puberty in internationally adopted girls: hormonal and clinical markers of puberty in 276 girls examined biannually over two years. Sexual precocity after immigration from developing countries to Belgium: evidence of previous exposure to organochlorine pesticides. A single histrelin implant is effective for 2 years for treatment of central precocious puberty. Long-term continuous suppression with once-yearly histrelin subcutaneous implants for the treatment of central precocious puberty: a final report of a phase 3 multicenter trial. Use of a potent, long acting agonist of gonadotropin-releasing hormone in the treatment of precocious puberty. Suppression of the pituitary-gonadal axis in children with central precocious puberty: effects on growth, growth hormone, insulin-like growth factor-I, and prolactin secretion. Long-term observation of 87 girls with idiopathic central precocious puberty treated with gonadotropin-releasing hormone analogs: impact on adult height, body mass index, bone mineral content, and reproductive function. Management of endocrine disease: long-term outcomes of the treatment of central precocious puberty. Results of long-term follow-up after treatment of central precocious puberty with leuprorelin acetate: evaluation of effectiveness of treatment and recovery of gonadal function. Reduction of baseline body mass index under gonadotropin-suppressive therapy in girls with idiopathic precocious puberty. Changes in body mass index in girls with idiopathic central precocious puberty under gonadotropin-releasing hormone analogue therapy: the Spanish Registry. Random luteinizing hormone often remains pubertal in children treated with the histrelin implant for central precocious puberty. Effect of antiandrogen, aromatase inhibitor, and gonadotropin-releasing hormone analog on adult height in familial male precocious puberty. Boys with precocious puberty due to hypothalamic hamartoma: reproductive axis after discontinuation of gonadotropin-releasing hormone analog therapy. Prevalence of polycystic ovary syndrome in young women who had idiopathic central precocious puberty. Psychological assessment of mothers and their daughters at the time of diagnosis of precocious puberty. Trait-specific tracking and determinants of body composition: a 7-year follow-up study of pubertal growth in girls. Slipped capital femoral epiphyses associated with the withdrawal of a gonadotrophin releasing hormone. Use of a gonadotropinreleasing hormone analog to treat idiopathic central precocious puberty is not associated with changes in bone structure in postmenarchal adolescents. Early puberty, negative peer influence, and problem behaviors in adolescent girls. Assessment of stress levels in girls with central precocious puberty before and during longacting gonadotropin-releasing hormone agonist treatment: a pilot study. Cognitive, emotional, and psychosocial functioning of girls treated with pharmacological puberty blockage for idiopathic central precocious puberty. Unexplained anaemia and failure to thrive as initial symptoms of infantile choriocarcinoma: a review. Precocious puberty associated with a pineal cyst: is it disinhibition of the hypothalamic-pituitary axis Testicular adrenal rest tumors develop independently of long-term disease control: a longitudinal analysis of 50 adult men with congenital adrenal hyperplasia due to classic 21-hydroxylase deficiency. Leydig-cell tumour in children: variable clinical presentation, diagnostic features, follow-up and genetic analysis of four cases. Focal lobular spermatogenesis and pubertal acceleration associated with ipsilateral Leydig cell hyperplasia. Gonadotropin-independent familial sexual precocity with premature Leydig and germinal cell maturation (familial testotoxicosis): effects of a potent luteinizing hormone-releasing factor agonist and medroxyprogesterone acetate therapy in four cases. Luteinizing hormone receptor mutations in disorders of sexual development and cancer. Treatment of familial male precocious puberty with spironolactone and testolactone. Long-term follow-up of spontaneous development in a boy with familial male precocious puberty. Nodular Leydig cell hyperplasia in a boy with familial male-limited precocious puberty. Concurrent hormone resistance (pseudohypoparathyroidism type Ia) and hormone independence (testotoxicosis) caused by a unique mutation in the G alpha s gene. Sexual precocity caused by ovarian follicular cysts: spontaneous regression and recurrence with prepubertal gonadotropin levels. A genome-wide association study of men with symptoms of testicular dysgenesis syndrome and its network biology interpretation. Review of ovarian tumors in children and adolescents: radiologic-pathologic correlation. The role of inhibins B and antimullerian hormone for diagnosis and follow-up of granulosa cell tumors. Ovarian dysgerminoma with normal serum tumour markers presenting in a child with precocious puberty. Peripheral precocious puberty due to functioning adrenocortical tumor: description of two cases.
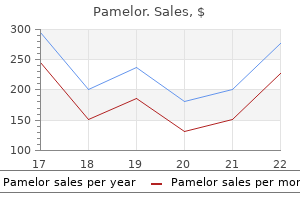
Discount 25 mg pamelor free shipping
These patients have low testosterone concentrations and low to low-normal gonadotropin concentrations and present with sexual dysfunction (reduced libido and erectile dysfunction) anxiety symptoms neck tension purchase on line pamelor, infertility, and gynecomastia. In men with prolactin-secreting macroadenomas, serum prolactin concentrations are usually higher than 250 ng/mL, and they can be higher than 1000 ng/ mL with tumors larger than 2 cm in diameter. Some patients with very large prolactin-secreting macroadenomas have only modestly elevated serum prolactin concentrations, which is caused by an assay artifact from saturation of both the capture and detection antibodies used in two-site sandwich immunoassays. Measurement of prolactin after serial dilution should be considered for all patients with large pituitary tumors and modest hyperprolactinemia. Diseases affecting the pituitary stalk and hypothalamic diseases may cause hyperprolactinemia because of disruption of the hypothalamic hypophyseal portal tract and transport of dopamine from the hypothalamus to the pituitary in the former condition or loss of hypothalamic dopamine-containing neurons in the latter. In contrast, newer atypical antipsychotic medications such as clozapine, olanzapine, quetiapine, ziprasidone, and aripiprazole much less commonly increase prolactin. Other medications that cause hyperprolactinemia less commonly include some tricyclic antidepressants. Selective serotonin and serotonin/norepinephrine reuptake inhibitors in general have minimal to no effect on prolactin concentrations. The mild hyperprolactinemia associated with primary hypothyroidism does not usually suppress gonadotropin secretion significantly or cause clinical secondary hypogonadism in men. However, if primary hypothyroidism is severe and long standing, it may cause slight enlargement of the pituitary gland, which may be confused with a pituitary adenoma. In men with prolactin-secreting macroadenomas, treatment is initiated with a dopamine agonist medication such as bromocriptine or carbergoline. Treatment with these agents may also improve sexual dysfunction, normalize testosterone concentrations, and improve semen quality. In men who remain persistently hypogonadal despite adequate dopamine agonist treatment, testosterone therapy may be initiated to treat manifestations of androgen deficiency. Testosterone is aromatized to estradiol, and this estrogen theoretically might increase prolactin concentrations and tumor growth by direct action on pituitary lactotrophs; this effect may also cause resistance to dopamine agonist therapy. Surgery or radiation therapy may be needed for tumors that are resistant to dopamine agonists, and urgent surgery may be needed for pituitary apoplexy or rapidly progressive tumor mass effects such as visual loss. Medications that cause hyperprolactinemia may be stopped or switched to ones that do not elevate prolactin. Addition of a dopamine agonist while administration of an offending antipsychotic medication is continued should be done with extreme caution, because there is a risk of exacerbating psychosis. Use of opiates or opioid medications, particularly potent, long-acting narcotic analgesics such as methadone (>30 mg daily), controlled-release or intrathecal morphine sulfate or the transdermal fentanyl patch, and drugs of abuse such as heroin (diacetylmorphine) or time-released oxycodone (OxyContin), profoundly suppress gonadotropin secretion, resulting in severe androgen deficiency. Although the benefits and risks of testosterone treatment have not been evaluated in randomized controlled studies,438 testosterone treatment should be considered in cases of secondary hypogonadism due to chronic use of opioids. Administration of sex steroids-androgens, progestins, or estrogens-suppresses gonadotropin secretion by negative feedback mechanisms at the hypothalamus or the pituitary gland or both; chronic administration may cause secondary hypogonadism, resulting in androgen deficiency and impaired sperm production. Synthetic androgens (androgenic anabolic steroids) and testosterone are used by a significant number of teenage boys and men to increase muscle bulk and strength and enhance athletic performance or physical appearance. For these purposes, these androgens are used in extremely high doses in a variety of combinations and patterns for prolonged periods. The prevalence of anabolic steroid abuse ranges from approximately 1% to 6% in various populations, including high school and college students, weightlifters, body builders (who often have muscle dysphoria, an obsessive preoccupation with a muscular appearance), young recreational athletes, and competitive athletes. Because of the androgenic effects of these anabolic steroids, individuals taking these agents may not complain of androgen deficiency symptoms. After discontinuation of even prolonged anabolic steroid use, recovery of the hypothalamic-pituitary-testicular axis usually occurs within weeks to months. However, for unclear reasons, some men experience a protracted period of symptomatic hypogonadism that may last for several months to several years, particularly in older men. Prolonged secondary hypogonadism after androgenic anabolic steroid use often causes sexual dysfunction and depressed mood. Severe symptoms may lead to continued use of these agents and anabolic steroid dependence. Although poorly studied, off-label treatment with clomiphene citrate and aromatase inhibitors have also been reported to stimulate gonadotropin and testosterone secretion in these men. At the doses used for this purpose, it causes severe symptomatic androgen deficiency and suppression of sperm production. A destructive or infiltrative lesion of the pituitary gland or hypothalamus commonly causes impaired pituitary hormone production (hypopituitarism) and gonadotropin deficiency, resulting in androgen deficiency and impairment in sperm production. The prevalence of hypopituitarism has been estimated to be approximately 1 in 2200. Anterior pituitary hormone loss is even less predictable in disease processes involving the hypothalamus, in part because of the more disperse anatomic arrangement in the hypothalamus of nuclei that produce releasing factors for pituitary hormones. Acute destructive processes such as pituitary apoplexy usually cause panhypopituitarism. Diseases of the hypothalamus or high in the pituitary stalk may be associated with diabetes insipidus, which is caused by destruction or retrograde degeneration of neurons producing arginine vasopressin in the supraoptic or the paraventricular nuclei, respectively. Hypothalamic and pituitary stalk diseases may cause hyperprolactinemia due to loss of dopamine-containing neurons or interruption of the hypothalamic hypophyseal portal tract and transport of dopamine from the hypothalamus to the pituitary. Pituitary microadenomas or macroadenomas may produce prolactin, and suprasellar extension of nonsecretory pituitary macroadenomas or those secreting other hormones. Prepubertal boys who have hypopituitarism resulting in gonadotropin deficiency present with delayed puberty and eunuchoidism, and men present with adult androgen deficiency and complaints of reduced libido and erectile dysfunction. Dopamine agonist treatment of prolactin-secreting pituitary adenomas improves pituitary function in 60% to 75% of cases. However, high-dose immunosuppressive glucocorticoid therapy is most commonly associated with a hormone pattern characterized by low testosterone and low-normal gonadotropin concentrations, consistent with secondary hypogonadism. Occasionally, in men receiving glucocorticoid treatment, gonadotropins are high normal or slightly elevated, suggesting primary hypogonadism. Although most commonly observed with high-dose glucocorticoid treatment, daily doses as low as 5. These associated factors play a large role in suppressing gonadotropin concentrations and contribute to the hormonal pattern of secondary hypogonadism associated with chronic organ failure. The degree to which these factors contribute to the clinical and biochemical manifestations of hypogonadism varies considerably among individuals. Therefore, accurate and reliable measurements of free testosterone are needed to establish biochemical androgen deficiency in the presence of chronic systemic illness. In men with cirrhosis, sperm production is commonly impaired, and sperm motility is reduced. In alcoholic cirrhosis, serum estrone and estradiol concentrations are relatively high as a result of increased production of adrenal androgens. Men with severe alcoholic cirrhosis usually have atrophic testes (usually soft in consistency) due to direct toxic effects of alcohol. Its use may contribute to symptoms of androgen deficiency, gynecomastia, and hypogonadism. Protein-calorie malnutrition, complications of cirrhosis such as infection, and continued alcohol abuse contribute to the clinical manifestations and cause of low testosterone in these chronically ill men. A preliminary 12-month double-blind, placebo-controlled study in men with cirrhosis and low testosterone concentrations found that testosterone treatment was safe and increased lean body and bone mass and hemoglobin concentrations and reduced fat mass. These factors suppress gonadotropin concentrations and contribute variably to the clinical and biochemical androgen deficiency seen in individuals with systemic illness. Therefore, it is important to confirm biochemical androgen deficiency in these men by using calculated free testosterone values or measurements of free testosterone by equilibrium dialysis. Malnutrition, wasting (cancer cachexia), systemic inflammation, medication use. Primary or secondary hypogonadism may be present before systemic chemotherapy or radiation therapy, as well as after treatment. A low free testosterone concentration with normal or elevated gonadotropin concentrations was found in 40% to 60% of men with advanced malignancy. In observational cohort studies, low testosterone concentrations are associated with rheumatic autoimmune disease, including rheumatoid arthritis and systemic lupus erythematosus.
Discount pamelor 25 mg with mastercard
The incidence of classic anorexia nervosa is approximately 1 case per 100 anxiety symptoms medications pamelor 25mg mastercard,000 people in the general population. The incidence of anorexia nervosa peaks twice during the teen years, at ages 13 and 17. Anorexia nervosa has an extremely high mortality rate of 9% and is a true medical emergency. Death may result from cardiac arrhythmia, which may be precipitated by diminished heart muscle mass and associated electrolyte abnormalities. Anovulation can persist in up to 50% of anorexic patients, even after normal weight is achieved. Anorexic and bulimic patients exhibit hyperactivation of the hypothalamic-pituitary-adrenal system. Although the Hypothalamic Anovulation Associated With Eating Disorders diurnal variation is maintained, persistent hypersecretion of cortisol occurs throughout the day. The most accepted approaches include individual psychotherapy, group therapy, and behavior modification. Patients with eating disorders should have psychiatric consultation and follow-up. For patients who weigh less than 75% of their ideal body weight, immediate hospitalization and aggressive treatment are recommended. Complications of anorexia nervosa include osteoporosis, estrogen deficiency, and generalized effects of malnutrition. The importance of successful treatment of this disease state is underscored because these women are prone to the development of osteoporosis. For a considerable number of patients, spontaneous recovery of menstrual function takes place after a modification of lifestyle, psychologic guidance, or accommodation to environmental stress. The initial treatment should be directed to a change in lifestyle and tailored to the individual patient. Modification of the stress response through cognitive-behavioral therapy is a logical approach to lowering the endogenous stress levels in women with hypothalamic amenorrhea. This approach was explored in 16 subjects with hypothalamic amenorrhea randomized to cognitive-behavioral therapy or observation for a 20-week period. Approximately 88% of those who underwent cognitive-behavioral therapy had evidence of ovulation, compared with only 25% of those who were observed. If anovulation persists for longer than 6 months or if reversal of the primary cause is not practical. Because these patients are often reluctant to take medications, serial bone density studies of the lumbar spine and femur may be necessary to convince them of the necessity to begin estrogen replacement therapy. If the patient is not at risk for thromboembolism and does not smoke cigarettes, a low-dose combination oral contraceptive is a reasonable replacement option. Chronic Anovulation Associated With Pituitary Disorders the most common pituitary-related causes of anovulation are associated with hyperprolactinemia caused by prolactinomas or other functional or anatomic disorders of the pituitary. These disorders are frequently associated with dysregulation of gonadotropin secretion. Hyperprolactinemia and other pituitary disorders and their relation to reproduction are discussed in Chapter 9. A male escutcheon, hair on the inner aspects of the thighs, and midline lower back hair entering the intergluteal area are hair growth patterns compatible with androgen excess. A moderate amount of hair on the forearms and lower legs by itself may not be abnormal, although it may be viewed by the patient as undesirable and may be mistaken for hirsutism. Compared with hirsutism, virilization is a more severe form of androgen excess and implies significantly higher rates of testosterone production. Measurements of an enlarged clitoris may be used for the quantification of virilization. An increase in clitoral diameter is a much more sensitive indicator of androgen action. The most accurate definition of clitoromegaly involves use of the clitoral index (the product of the sagittal and transverse diameters of the glans clitoris). A clitoral index greater than 35 mm2 is abnormal and correlates statistically with androgen excess. Increased levels of these androgens can lead to hirsutism, which is excessive androgenic hair growth, or to virilization, a more severe form of androgen excess. Androstenedione, the direct precursor of testosterone, is produced in the ovary and the adrenal gland. Androstenedione is the major precursor that is converted directly to testosterone. The conversion fraction of circulating androstenedione to testosterone in extragonadal tissues is about 5% in both men and women. The clinical, biochemical and ovarian morphologic features in women with acanthosis nigricans and masculinization. Depending on the menstrual cycle phase or postmenopausal status, 20% to 30% of testosterone (T) is secreted by the ovary. The rest is accounted for by the conversion of circulating androstenedione (A) to T in various peripheral tissues. Both the adrenal gland and the ovary contribute to circulating A directly or indirectly, depending on the cycle phase or postmenopausal status and chronologic age. In contrast, the direct free testosterone measurements had unacceptably high systematic bias and random variability and did not correlate as well with equilibrium dialysis values. Measuring the levels of all C19 steroids is not clinically necessary for most patients presenting with androgen excess. The likelihood of a neoplasm correlates roughly with increasing testosterone levels. The following tests may be added on the basis of the clinical presentation: serum 17-hydroxyprogesterone. They include unusual causes such as iatrogenic or drug-induced androgen excess, congenital genital ambiguity. Adrenal Nonclassic congenital adrenal hyperplasia Cushing syndrome Glucocorticoid resistance Adrenal tumor. These uncommon causes and relatively more prevalent disorders associated with androgen excess are listed in Table 17. The term extraovarian steroid formation is used synonymously with extraglandular, extragonadal, or peripheral steroid formation in this text. Overall, the prevalence of androgen-excess disorders was found to be as follows: 72. If androgen excess is associated with primary amenorrhea, abnormal in utero sexual differentiation should be strongly suspected. Before embarking on a major workup for hirsutism or virilization, the physician is well advised to rule out exogenous androgen use. It is best to ask the patient to list all prescriptions and over-the-counter medications that she takes on her own, including injections. This is usually more rewarding than asking the patient whether she takes any androgens. Medications that can cause hirsutism or virilization are related to testosterone and include anabolic steroids and similar compounds. In this section, we first define some of the other disorders associated with hirsutism or virilization. This is followed by a simplified treatment Idiopathic Hirsutism Hirsutism is defined subjectively as the presence in a woman of terminal hair growth in a male-distribution pattern that affects quality of life sufficiently to prompt her to seek medical advice. Hirsutism should be distinguished from hypertrichosis, in which the excessive hair growth is not restricted to androgen-dependent areas and comprises vellus or lanugo-type hair. Hypertricosis is considered to be a phenotype not associated with male pattern hair growth and is unlikely to be modified by the known treatments of hirsutism.
Buy pamelor paypal
At this time anxiety effects order pamelor once a day, two-thirds of the total germ cells are intrameiotic primary oocytes; the remaining third can still be viewed as oogonial. The midgestational peak and the postpeak decline are accounted for in part by the progressively decreasing rate of oogonial mitosis, a process destined to end entirely by about the seventh month of intrauterine life. Equally relevant is the increasing rate of oogonial atresia, which peaks at 5 months of gestation. From midgestation onward, relentless and irreversible attrition progressively diminishes the germ cell endowment of the gonad. In contrast, oogonial atresia is destined to end at 7 months of intrauterine life as follicular atresia sets in. Consequently, newborn girls enter life still far from realizing their reproductive potential but having lost as much as 80% of their germ cell endowment. The germ cell mass decreases further to approximately 300,000 by the onset of puberty. Of these follicles, only 400 to 500 (<1% of the total) are recruited for ovulation in the course of a reproductive life span. Between weeks 8 and 13 of fetal life, some of the oogonia depart from the mitotic cycle to enter the prophase of the first meiotic division. This change marks the conversion of these cells to primary oocytes well before actual follicle formation. Meiosis (beginning at about 8 weeks of gestation) provides temporary protection from oogonial atresia, allowing the germ cells to invest themselves with granulosa cells and to form primordial follicles. Oogonia that persist beyond the seventh month of gestation and have not entered meiosis are subject to oogonial atresia; consequently, no oogonia are usually present at birth. This hypothesis is based on the observation that denuded (granulosa-free) oocytes are capable of spontaneously completing meiotic maturation in vitro. At ovulation, the secondary oocyte and the surrounding granulosa cells (cumulus oophorus) are extruded and enter the fallopian tube. Number of germ cells (millions) Granulosa Cell Layer In the developing ovaries of a human female fetus, oocytes initially exist as germ cell clusters before an ovarian follicle is formed. During meiosis, the chromosomes that were inherited from the parents of the individual and stored in gonads are processed to prepare their genetic material for transmission to the offspring. Meiosis occurs exclusively in germ cells and serves two critical purposes: generation of germ cells genetically distinct from the somatic cells and generation of a mature egg (or sperm) with a reduction in the number of chromosomes from 46 to 23. Genetic recombination through crossover of genes between homologous chromosomes and random assortment of (grand-) maternal and (grand-) paternal chromosomes into daughter cells during the first meiotic division are responsible for the first function of meiosis, maintenance of genetic diversity. The second function is provided by a reduction in the number of chromosomes so that each daughter cell, or ovum, receives randomly one chromosome from each of the 23 pairs. During fertilization, the fusion of ovum and sperm, each of which contributes 23 chromosomes, produces a genetically novel individual with 46 chromosomes. The chromosome marked as white in the oogonium (upper left corner) originates from the father of the female fetus, whereas the blue chromosome comes from the mother of the fetus. The random exchange of genes (alleles) between homologous chromosomes (crossover) takes place before the meiotic arrest in the prophase I stage before birth. The transition from primordial to primary follicle is marked histologically by a morphologic change in granulosa cells from squamous to cuboidal. A basement lamina separates the oocyte and granulosa cells from the surrounding stromal cells. The avascular nature of the granulosa cell compartment necessitates contact between neighboring cells. Connexin 37 and other connexins have been demonstrated in gap junctions in follicles. The primordial follicle is composed of a single layer of granulosa cells and a single immature oocyte arrested in the diplotene stage of the first meiotic division. The primordial follicle is separated from the surrounding stroma by a thin basal lamina. The first sign of follicular recruitment is cuboidal differentiation in the spindle-shaped cells inside the basal lamina, which thereafter undergo successive mitotic divisions to form a multilayered granulosa cell zone. The oocyte enlarges and secretes a glycoprotein-containing mucoid substance called the zona pellucida, which surrounds the oocyte and separates the granulosa cells from the oocyte. The secondary follicle is formed by further proliferation of granulosa cells and by the final phase of oocyte growth, in which the oocyte reaches 120 m in diameter, coincident with proliferation of layers of cells immediately outside the basal lamina to constitute the theca. The portion of the theca adjacent to the basal lamina is called the theca interna. Theca cells that merge with the surrounding stroma are designated the theca externa. The secondary follicle acquires an independent blood supply consisting of one or more arterioles that terminate in a capillary bed at the basal lamina. Capillaries do not penetrate the basement membrane, and the granulosa and oocyte remain avascular. The tertiary follicle is characterized by further hypertrophy of the theca and the appearance of a fluid-filled space among the granulosa cells, called the antrum. The fluid in the antrum consists of a plasma transudate and secretory products of granulosa cells, some of which (estrogens) are found there in strikingly higher concentrations than in peripheral blood. The follicle rapidly increases in size under the influence of gonadotropins to form the mature or Graafian follicle. In the Graafian follicle, the granulosa and oocyte remain encased by the basal lamina and are devoid of direct vascularization. The antral fluid increases in volume, and the oocyte, surrounded by an accumulation of granulosa cells. The mature Graafian follicle is then ready to release the ovum by the process of ovulation. Several gene products regulate the transition from primordial to primary follicle, which is marked by a change in the morphologic appearance of granulosa cells from squamous to cuboidal, followed by an increase in granulosa cell layers in the secondary follicle. The granulosa cells, which accumulate around the oocyte, are called cumulus granulosa cells and primarily function to support egg development. The mural granulosa cells in the periphery primarily serve as steroidogenic cells. Theca interna cells are responsible for producing the C19 steroids that diffuse into the neighboring granulosa cells and serve as substrates for estrogen production. Cells that contribute to the theca differentiate from mesenchymal precursor cells present in the ovarian stroma, adjacent to developing follicles. Granulosa cells of the developing follicles appear to secrete factors that regulate theca cell differentiation. Recruitment of a primordial follicle initiates dramatic changes in growth, structure, and function. The follicle destined to ovulate is recruited during the first few days of the current cycle. If a follicle is not recruited, it goes through a process called atresia, during which the oocyte and granulosa cells within the basal lamina die and are replaced by fibrous tissue. During each menstrual cycle, usually one follicle ovulates and gives rise to a corpus luteum. Rupture of this stigma is accompanied by a gentle rather than explosive expulsion of the ovum and antral fluid. Small gap junctions (thin arrows) are observed between processes of the granulosa cell and the oocyte membrane. The follicles are embedded in loose connective tissue of the ovarian cortex and can be subdivided into two functional types: nongrowing (primordial) and growing. This rapid vascularization of the corpus luteum may be guided by angiogenic factors, some of which are detected in the follicular fluid. The corpus luteum is the major source of sex steroid hormones secreted by the postovulatory ovary. The human corpus luteum secretes as much as 40 mg of progesterone per day during the midluteal phase of the ovarian cycle.
Generic 25mg pamelor mastercard
Markers of platelet activation anxiety symptoms 97 pamelor 25mg, thrombin generation and fibrinolysis in women with sickle cell disease: effects of differing forms of hormonal contraception. Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: a systematic review. Drug interactions between hormonal contraceptives and psychotropic drugs: a systematic review. T 668 he testes have critical physiologic roles during various stages of development. During puberty, activation of the hypothalamic-pituitary-testicular axis and testosterone production by the testes are necessary for the induction of secondary (adult) male sexual characteristics, stimulation of sexual function, and initiation of sperm production. In adults, testis production of testosterone is required for the maintenance of adult male characteristics (virilization), sexual function, spermatogenesis, and fertility potential. Therefore, disorders of the testis may result in abnormalities in sexual development and function, body habitus and function, and fertility that have profound effects on health and well-being. Klinefelter syndrome is the most common human sex chromosome abnormality and the most common cause of primary hypogonadism, occurring in 1 in 500 to 600 male births. Finally, disordered hypothalamicpituitary-testicular function is commonly associated with chronic systemic illnesses, wasting syndromes, morbid obesity, chronic use of certain medications. These conditions often result in testosterone deficiency that, if severe and prolonged, may contribute to clinical manifestations and morbidity. In prepubertal boys and adults with severe testosterone deficiency, testosterone therapy results in dramatic transformations in body composition and function. Lymphatic drainage from the testes follows the testicular arteries to periaortic lymph nodes; this is a common route for metastasis of testicular cancer. A network of veins that compose the pampiniform plexus provides venous drainage from the testes. The right testicular vein drains into the inferior vena cava, and the left testicular vein empties at a right angle into the left renal vein. Abnormal enlargement of the venous plexus draining a testicle, known as a varicocele, occurs if valves are defective or absent or if there is extrinsic venous compression impeding normal venous drainage. Ninety-eight percent of varicoceles occur in the left scrotum, possibly because of absent or defective valves in the left testicular vein. The presence of a prominent unilateral right-sided varicocele or new-onset varicocele on either side should prompt evaluation for venous obstruction by an abdominal or pelvic malignancy. Rarely, an anatomic anomaly of the superior mesenteric artery that compresses the left renal vein causes a left-sided varicocele; this is known as the nutcracker syndrome. Functional Anatomy and Histology the Testis Adult testes are paired, ovoid organs that hang from the inguinal canal by the spermatic cord (which is composed of a neurovascular pedicle, vas deferens, and cremasteric muscle); they are located outside the abdominal cavity within the scrotum. The left testis hangs lower in the scrotum than the right in about 60% of men, and the right testis hangs lower in approximately 30% of men. Because germ cells constitute most of the testis volume, small testes are usually an indication of significantly impaired spermatogenesis. Fibrous septa that emanate from the tunica albuginea separate the parenchyma of the testis into lobules. The arterial blood supply of the testes is derived primarily from the testicular (internal spermatic) arteries that arise from the abdominal aorta and descend through the inguinal canal in the spermatic cord. This collateral supply permits survival of the testis after a testicular artery ligation associated with surgical fixation of a high undescended testis into the scrotum (orchiopexy). Spermatogonia line the basal lamina of the seminiferous tubules, spermatocytes at various stages of development are present in the middle layers of the tubules, and spermatids at various steps of maturation are present in the luminal aspect of the seminiferous tubules. In the interstitial compartment, there are prominent clusters of Leydig cells (L) nestled between seminiferous tubules, peritubular myoid cells within the basal lamina of the tubules, and scattered blood vessels and macrophages. The position of the testes within the scrotum and the testicular temperature are regulated by the cremasteric muscle. The cremasteric muscle contracts when warming is needed, resulting in shortening of the spermatic cord and drawing of the testis toward the abdomen; when cooling is needed, the muscle relaxes, resulting in lowering of the testis into the scrotum. In addition, the pampiniform venous plexus provides a countercurrent heat exchange mechanism to cool the testis by surrounding the testicular artery with cooler venous blood. A testis temperature slightly lower than core body temperature is important for normal spermatogenesis. Exposure of the testes to higher temperatures, such as with failure of the testes to descend normally into the scrotum (cryptorchidism) or excessive external heat exposure due to frequent, prolonged hot tub use may impair spermatogenesis. Seminiferous Tubule Seminiferous tubules contain epithelium consisting of Sertoli cells that envelop and support germ cells undergoing progressive differentiation and development into mature spermatozoa. Once released into the lumen, mature spermatozoa are transported within seminiferous tubules, which measure up to 70 cm in length and are tightly coiled within lobules of the testis, to the rete testis, Cross section of seminiferous tubule the efferent ducts, the epididymis, and, finally, the vas deferens for ejaculation. The seminiferous tubules are surrounded by a basal lamina composed of an extracellular matrix that serves to separate them from the interstitial compartment, provides structural integrity to the tubules, and regulates the function of cells in contact with it. Undifferentiated spermatogenic stem cells, called spermatogonia, lie along the basal lamina at the periphery of tubules, interspersed between Sertoli cells. Adjacent Sertoli cells surround spermatogonia and form specialized junctional complexes or tight junctions that divide the seminiferous tubule into the basal compartment, in which spermatogonia reside, and the adluminal compartment, which is occupied by differentiating germ cells. Sertoli cell tight junctions impede the passage of large molecules, steroids, and ions into the seminiferous tubule and constitute the cytologic basis of the blood-testis barrier, analogous to the blood-brain barrier. The seminiferous tubule consists of Sertoli cells that surround developing germ cells (middle). Tight junctions between adjoining Sertoli cells separate the seminiferous tubule into basal and adluminal compartments and are the anatomic basis for the blood-testis barrier (bottom). The basal compartment, which contains spermatogonia lining the basal lamina and peritubular myoid cells, is exposed to the interstitial compartment, which contains Leydig cells and blood vessels that deliver endocrine regulators of testis function. The adluminal compartment contains developing spermatocytes, spermatids, and mature spermatozoa that are released into the lumen of the seminiferous tubule. Because of the blood-testis barrier, only Sertoli cells and spermatogonia are directly accessible to endocrine and paracrine regulation from the circulation and cells of the interstitial compartment, respectively. Sertoli cells need to synthesize and secrete many products, some of which are present in the circulation but not accessible to developing germ cells in the adluminal compartment, to nurture and regulate spermatogenesis. Preleptotene spermatocytes undergo an initial round of meiotic division (meiosis I), lasting longer than 2 weeks, to form secondary spermatocytes that contain a haploid complement of chromosomes (1N). Improper segregation of chromosomes (meiotic nondisjunction) resulting in an abnormal number of chromosomes (aneuploidy) occurs in 0. Progressive maturation of spermatids is accompanied by progressive movement of more mature spermatids toward the lumen of the seminiferous tubule. Germ Cell Loss Compared with most other species, the efficiency of spermatogenesis in humans is relatively poor, and the germ cell degeneration and loss that occur predominantly during mitosis and meiosis are major contributors to the low efficiency of sperm production. As men age, increased germ cell degeneration may result in lower daily sperm production. It is hypothesized that germ cell degeneration prevents abnormal germ cells from further development, thereby serving an important quality control function. Organization of Spermatogenesis Histologic examination of a human testis in cross section reveals that germ cells at particular phases of development cluster in six cellular associations, referred to as stages, which together constitute a complete cycle of spermatogenesis. In most mammals, stages are organized sequentially along the longitudinal axis of the tubules so that all of the germ cells present in a cross section of a tubule are in the same stage of spermatogenesis. Although some have proposed a helical pattern of stages along the tubule to explain this seemingly chaotic arrangement, this has not been confirmed by others. Spermatogenesis In male humans, the process of spermatogenesis supports a production rate of approximately 120 million mature spermatozoa per day by the testis (approximately 1000 per heartbeat! Proliferative Phase Based on chromatin staining and pattern, spermatogonia may be classified as A dark (Ad), A pale (Ap), or B spermatogonia. Because of their relatively low mitotic rate, Ad spermatogonia are thought to be the spermatogonial stem cells. However, severe or complete depletion of Ad spermatogonia, such as that which occurs with high-dose x-irradiation or vascular compromise, results in irreversible impairment or loss of sperm production. A small number of Ad spermatogonia undergo mitotic divisions to form Ap and then B spermatogonia. In humans, the rate of formation of B spermatogonia is low, so only a small number of B spermatogonia are available to enter meiosis and undergo further differentiation. B spermatogonia are the most sensitive germ cells to the effects of ionizing radiation, and their numbers are reduced after irradiation of the testes. Groups of spermatogonia remain connected via cytoplasmic bridges, forming a syncytium, and undergo meiosis and spermiogenesis in synchrony.
Purchase pamelor online
Hereditary transmission in the F1 generation of hormonal imprinting (receptor memory) induced in rats by neonatal exposure to insulin anxiety cheap pamelor 25 mg otc. Intergenerational consequences of fetal programming by in utero exposure to glucocorticoids in rats. Fetal and early life determinants of hypertension in adults: implications for study. Fetal thyroid function, birth weight, and in utero exposure to fine particle air pollution: a birth cohort study. Mapping acute systemic effects of inhaled particulate matter and ozone: multiorgan gene expression and glucocorticoid activity. Imprinting disorders: a group of congenital disorders with overlapping patterns of molecular changes affecting imprinted loci. Early nutrition, epigenetic changes at transposons and imprinted genes, and enhanced susceptibility to adult chronic diseases. Beckwith-Wiedemann and Russell-Silver syndromes: from new molecular insights to the comprehension of imprinting regulation. Insulin gene variable number of tandem repeat genotype and the low birth weight, precocious pubarche, and hyperinsulinism sequence. Developmental diethylstilbestrol exposure alters genetic pathways of uterine cytodifferentiation. Neonatal diethylstilbestrol treatment alters the estrogen-related expression of both cell proliferation and apoptosis-related proto-oncogene (c-jun, c-fos, c-myc, bax, bcl-2 and bcl-x) in the hamster uterus. Plasticity in the adrenocorticotropin-related peptides produced by primary cultures of neonatal rat pituitary. Prenatal glucocorticoid exposure modifies endocrine function and behaviour for 3 generations following maternal and paternal transmission. Maternal-fetal glucocorticoid milieu programs hypothalamic-pituitary-thyroid function of adult offspring. Late gestation increase in 11beta-hydroxysteroid dehydrogenase 1 expression in human fetal membranes: a novel intrauterine source of cortisol. Knowledge gaps and research needs for understanding and treating neonatal hypoglycemia: workshop report from Eunice Kennedy Shriver National Institute of Child Health and Human Development. Effects of elevated fetal cortisol concentrations on the volume, secretion, and reabsorption of lung liquid. Targeted disruption of the glucocorticoid receptor gene blocks adrenergic chromaffin cell development and severely retards lung maturation. Pathogenesis of early neonatal hypocalcemia: studies of serum calcitonin, gastrin and plasma glucagon. Longitudinal changes in growth hormone response to growth hormone-releasing hormone in neonatal rhesus monkeys. Testosterone and estradiol concentrations in paired maternal and cord sera and their correlation with the concentration of chorionic gonadotropin. Intrauterine death following intraamniotic triiodothyronine and thyroxine therapy for fetal goitrous hypothyroidism associated with polyhydramnios and caused by a thyroglobulin mutation. Fetal intravenous nutritional supplementation ameliorates the development of embolization-induced growth retardation in sheep. Committing embryonic stem cells to differentiate into thyrocyte-like cells in vitro. In the newborn period, approximately 1 in every 4500 babies has atypical (ambiguous) genitalia and cannot be immediately designated as male or female without further expert evaluation. Sex development is a dynamic process that requires the interaction of many genes, proteins, signaling molecules, paracrine factors, and endocrine stimuli. More detailed explanation of pituitary gonadotrope development is provided in Chapter 23 and of normal and disordered puberty in Chapter 26. Sex Determination and Sex Differentiation Sex determination is the process whereby the bipotential gonad develops into a testis or an ovary. Sex differentiation refers to the development of the internal and external genitalia, as directed by the production of peptide hormones and sex steroids by the developing gonad. Ovarian hormonal secretion in fetal life has little if any effect on sex differentiation. At the time of puberty, estrogen synthesis stimulates breast and uterine development, and eventually coordinated activity of the reproductive endocrine axis results in regular menstrual cycles. Defects in ovarian development therefore usually manifest in adolescence with absent puberty. Ovarian development and differentiation have been viewed in the past as a "default" or passive process, but ovarian development in fact involves many active processes. Studies of gene expression show that a specific complement of genes is implicated in ovarian development and integrity, some of which. The continuous line depicts the rise in fetal serum testosterone, with a peak concentration of about 10 nmol/L (300 ng/dL). Gonadal sex refers to the presence of a testis or ovary after the process of sex determination. Phenotypic (anatomic) sex refers to the appearance of the external genitalia and internal structures after the process of sex differentiation. Chromosomal Sex Chromosomal sex describes the complement of sex chromosomes present in an individual. Other species have different numbers of chromosomes, and they may have different types of sex chromosomes or sexually dimorphic autosomes. Nondisjunction is the failure of a pair of sister chromatids to separate during anaphase. Fertilization by such gametes can give rise to a zygote with an imbalance in sex chromosome number, called sex chromosome aneuploidy. This situation differs from chimerism, which is the existence of two or more cell lines with different genetic origins in one individual. Chimerism can occur through several mechanisms, including double fertilization (dispermy) of a binucleate ovum, fusion of two complete zygotes or morulae before implantation, or fertilization by separate sperm of an ovum and its polar body. The consequences of some of these events in humans are discussed later (see "Sex Chromosome Disorders of Sex Development"). This process is essential for proper distribution of recombined sex chromosomal material to daughter cells as well as for maintaining dosage sensitivity of X-Y pairs, as these regions are not subject to dosage compensation. The search for a testis-determining factor on the Y chromosome began more than 50 years ago. In 1987, Mardon and Page proposed that the sex-determining function of the Y chromosome is located within a 140-kb segment of the short arm, within the Y-specific euchromatic portion. The male-specific regions have undergone rapid evolution, with marked differences even between humans and chimpanzees. Although some of these genes have putative roles in growth, cognition, and tooth development, several genes in the male-specific region are involved in reproductive development, function, and pathology. Several genes on the X chromosome play an important role in sex development in males and females, gametogenesis, and hypothalamic-pituitary (gonadotrope) function. However, most X-linked genes are unrelated to reproductive function and have a diverse range of cellular functions. The first insight into X inactivation came after the identification in 1949 of the X chromatin body. This X chromatin is derived from one of the two X chromosomes in interphase nuclei of these somatic cells. If the initial population of cells is small, skewed X inactivation can occur as a chance event despite random inactivation. A subset of genes on the X chromosome may also be imprinted and only expressed from one allele. Furthermore, recent data suggest that several other X-chromosome genes (especially on the short arm) may escape X inactivation, potentially in a tissue-specific manner, and that sex chromosome gene dosage may regulate autosomal gene networks. Gonadal Sex Gonadal sex refers to whether the gonadal tissue developed as a testis or an ovary. The primitive gonad separates from the adrenal primordium at about 5 weeks but remains bipotential (indifferent) until about 42 days after conception. Several important genes are expressed in the developing urogenital ridge in mice that facilitate formation of the bipotential gonad; they include Emx2, Lim1, Lhx9, M33/Cbx2, Pod1, Six1/4, Map3k4, Wt1, and Nr5a1/Sf1.
Diseases
- Chromosome 17, trisomy 17q22
- Seminoma
- Obstructive asymmetric septal hypertrophy
- Hypereosinophilic syndrome
- Rhabdomyolysis
- Cranioa Craniom
- Verloes Gillerot Fryns syndrome
- Urbach Wiethe disease
- Peptidic growth factors deficiency
Cheap pamelor online american express
If a follow-up sonogram in 6 to 8 weeks demonstrates resolution or decrease in size of ovarian cysts anxiety psychiatrist buy pamelor 25mg low cost, no further evaluation is required. Unscheduled bleeding, spotting, and amenorrhea are common menstrual patterns during progestin-only oral contraceptive use, and users should be counseled accordingly. Interpreting signs and symptoms of pregnancy, whether intrauterine or extrauterine, can be challenging. Other Effects Most studies have reported that progestin-only oral contraceptives have little impact on carbohydrate metabolism. A history of ectopic pregnancy does not contraindicate progestin-only oral contraceptive use. Progestin-Only Oral Contraceptives During Lactation Progestin-only oral contraceptives do not interfere with the quality or quantity of breast milk. Package labeling advises delaying administration in lactating women until 6 weeks after delivery. A trial conducted in the United States randomized breastfeeding women to initiate progestin-only compared with combination estrogen-progestin oral contraceptives 2 weeks postpartum. At 8 weeks postpartum, approximately two-thirds of women continued to breastfeed in both groups. It is discrete, avoids the need for user action daily or near the time of sexual intercourse, and avoids the need for partner cooperation (Table 18. The injections can be given every 3 months because low solubility of the microcrystals at the injection site allows pharmacologically active drug levels to persist for several months. Unlike other progestin-only contraceptives, mean estradiol levels may be lower than normal for cycling premenopausal women. Following a 150-mg intramuscular injection, failure rates in clinical trials have ranged from 0. In clinical practice, typicaluser failure rates are 4 failures per 100 woman-years, reflecting the fact that some users do not return for their injections as scheduled. Women who are well informed when they choose this method of contraception are much more likely to become highly satisfied users with high continuation rates. A 2-week grace period (repeat injection without pregnancy testing, up to 15 weeks following the prior injection) is appropriate for women receiving injections every 3 months. Although users may be hypoestrogenic, vasomotor symptoms and vaginal atrophy are uncommon. The newer subcutaneous injection is less painful and is available in a prefilled syringe, offering the potential for self-administration. Otherwise, benefits and risks are similar for intramuscular and subcutaneous administration. Most women have pharmacologically active drug levels and a poor cervical mucus score within 24 hours after injection. Women who are well informed when they choose this method of contraception are more likely to become satisfied users with high continuation rates. During the first months of use, episodes of unpredictable bleeding and spotting lasting 7 days or longer are common. Bleeding decreases with longer duration use, and at 1 year, 50% of women experience amenorrhea; this rate increases to 75% with long-term use. However, a systematic review concluded that there is a lack of high-quality data to support routine clinical use of any interventions to treat persistent unscheduled bleeding with progestin-only contraceptives. Weight changes varied among women choosing different progestin-only methods; however, being of the black race predicted weight gain regardless of the contraceptive chosen. Bone mineral density is defined as the amount of mineral matter per volume of bone and directly correlates with bone strength. For patients with comorbidities and conditions that may impact skeletal health, including an elevated risk of falls, wheelchair use, chronic corticosteroid use, renal disease, or malabsorption, individualized counseling and clinical management along with shared decision making is appropriate. Age-appropriate calcium and vitamin D dietary intake, regular weight-bearing exercise, and smoking cessation should be encouraged for all women. Although these recommendations may benefit the health of patients in general, studies demonstrating that these measures will improve skeletal health outcomes in women using injectable contraception are lacking. However, in some women, fertility is not reestablished until up to 18 months after the last injection. Women who may want to become pregnant within the next year should choose an alternative contraceptive. It is now acknowledged that modern intrauterine contraception not only is highly effective but also is safe for most women to use. Mirena and Liletta are larger higher-dose T-shaped devices with a reservoir containing 52 mg of levonorgestrel. Although Mirena is approved for up to 5 years of use, it provides contraceptive efficacy for a longer duration. Louis, Missouri, provided women (n = 5000) who did not desire pregnancy for at least 1 year with free reversible contraceptives for up to 3 years. Adequate and specific counseling about likely changes in bleeding patterns before placement is essential for increasing patient acceptability. Immediate postpartum insertion (following vaginal or cesarean birth) is also an option (category 2) within 10 minutes of placental delivery as long as there is no evidence of chorioamnionitis or puerperal sepsis. Because expulsion usually occurs within the first few months, women are encouraged to follow up with their care provider within 12 weeks of insertion. However, these concerns have not been substantiated in high-quality clinical trials. In comparative studies, it offers efficacy equal to or greater than other surgical uterine-conserving treatments. Uterine adenomyosis also is a common, benign condition that may be associated with heavy menstrual bleeding and pelvic pain. All subdermal contraceptive implants for clinical use in humans employ progestins. These methods offer an excellent contraceptive option for women who have contraindications to combined hormonal methods and an option for any woman who desires long-term protection against pregnancy that is rapidly reversible. Acceptability studies are needed, and more studies are necessary to determine the lowest effective dose of levonorgestrel required to achieve effective endometrial suppression. In postmenopausal women, tamoxifen increases the risk of endometrial polyps, hyperplasia, and cancer. The ethylene vinyl acetate copolymer of Nexplanon allows controlled hormone release over at least 3 years of use. Each implant is provided in a disposable sterile inserter for subdermal application. Maximum serum concentrations of etonogestrel are usually seen by day 4 after implant insertion. Etonogestrel levels decrease slightly by 1 year and further by 3 years but remain above the threshold needed to suppress ovulation. Despite effective suppression of ovulation, estradiol levels only fall into the early follicular level range, and the implant does not cause hypoestrogenism. In an integrated analysis of 11 international clinical trials that included more than 900 healthy women between 18 and 40 years old, no pregnancies were reported while the etonogestrel implants were in place. Six pregnancies occurred during the first 14 days after etonogestrel implant removal. Including these six pregnancies, the cumulative Pearl index (number of pregnancies per 100 woman-years) was 0. Reported pregnancies among implant users have primarily been due to unrecognized pregnancies at the time of insertion and failure to insert the device. Postmarketing data regarding the etonogestrel implant from Australia found a real-world failure rate of 1. Of the remaining 127 cases, failure to insert the implant resulted in pregnancies in 84 women.
Generic pamelor 25 mg otc
Absorption of calcium and magnesium is impaired by bile salt deficiency anxiety symptoms rapid heart rate order pamelor online pills, unabsorbed free fatty acids in steatorrheic states, and high dietary content of fiber or phytate. Gastric acid is needed to promote dissociation of calcium from anionic components of food or therapeutic preparations of calcium salts. Administration of calcium salts with meals, especially in achlorhydrics, and use of divided doses or more soluble salts such as calcium citrate are commonly used strategies to increase calcium bioavailability. Calcium is thought to be absorbed by two pathways: a saturable transcellular pathway and a nonsaturable paracellular route. Although the necessity of vitamin D for paracellular calcium absorption remains controversial, substantial evidence exists that the hormone enhances this pathway as well. This pathway is thought to involve three steps: entry of calcium into the enterocyte (which is the rate-limiting step), transport across the cell, and extrusion across the basolateral membrane. The activity of these proteins correlates with active calcium transport; however, a causal relationship remains to be established. Chapter 29 Hormones and Disorders of Mineral Metabolism 1215 Transcellular Transport the best studied effect of vitamin D on the enterocyte is the induction of synthesis of the intestinal calcium-binding protein, calbindin-9K. The affinity of calbindin for calcium is approximately four times that of the brush border calcium-binding components, so calcium is preferentially transferred to calbindin. Calbindin serves to buffer the intracellular free calcium concentration during calcium absorption. It associates with microtubules and may play a role in the transport of calcium across the enterocyte. Exit From the Enterocyte can be reversed when mineral ion homeostasis is normalized. Vitamin D administration has been shown to increase the concentration of troponin C, a calcium-binding protein in muscle that plays a role in excitation coupling and increases the rate of uptake of calcium by the sarcoplasmic reticulum. However, recent studies demonstrate that women with vitamin D levels above 30 ng/mL in early and late pregnancy have a lower risk of preeclampsia. Several analogues have been shown to have antiproliferative effects on normal cells as well as on malignant cells in vitro and in xenografts in immunosuppressed mice. Such analogs are currently used for the prevention and treatment of hyperparathyroidism associated with chronic kidney disease. The physiology underlying the differential biologic effects of these analogues is not completely understood. Major homeostatic responses to dietary calcium deprivation or loading are depicted. Arrow thickness indicates relative activity of transport or secretory mechanisms, whereas amounts of hormones or transported ions are related to the size of their notations. Note that the extracellular calcium concentration is well maintained, although different underlying mechanisms are involved in the two circumstances (see text for details). In contrast, the concentrations of these mineral ions in extracellular fluid are quite comparable. Extracellular calcium and phosphate, in particular, exist so close to the limits of their mutual solubility that stringent regulation of their concentrations is required to avoid diffuse precipitation of calcium phosphate crystals in tissues. Serum concentrations and total body balances of the mineral ions are maintained within narrow limits by powerful, interactive homeostatic mechanisms. In contrast, the mechanisms of the phosphate sensing needed for normal homeostasis are not understood. Dietary calcium restriction, for example, is followed by an increase in the efficiency of intestinal calcium absorption. Enhanced intestinal calcium absorption is quantitatively the most important response to calcium deprivation, but a series of other homeostatic events also occur that limit the impact of this stress. Moreover, nonenteral sources of calcium, such as intravenous calcium infusion or excessive net bone resorption (as from immobilization or malignancy), may readily overwhelm the limited homeostatic adaptations that remain once suppressed intestinal calcium absorption is bypassed. In such situations, the kidney rather than the intestine becomes the principal defense against hypercalcemia, and calcium homeostasis becomes critically dependent on adequate renal function. If renal function is impaired in these settings, as frequently occurs clinically, severe hypercalcemia and pathologic calcium deposition in extraskeletal sites may ensue. Note some overlap between normal people and patients with primary hyperparathyroidism, but no overlap between hypercalcemic patients with primary hyperparathyroidism and those with hypercalcemia of malignancy. Advances in techniques for measurement of parathyroid hormone: current applications in clinical medicine and directions for future research. Although it seems plausible that such assays might prove particularly useful in some clinical situations, their role is presently unclear. They offer no advantage over older two-site assays, for example, in diagnosing primary hyperparathyroidism. Two normocalcemic patients with cancer (filled triangles) subsequently became hypercalcemic. The measurements are based on single or double antibody radioimmunoassays or enzyme immunoassays, several of which are sufficiently sensitive to detect calcitonin deficiency. However, the double antibody assays are thought to provide the same information with less sample manipulation. The only clinical use of the calcitonin assay is as a tumor marker, primarily in medullary carcinoma of the thyroid. Nevertheless, because the diagnosis of malignancy as the cause of hypercalcemia is usually clinically obvious, and the Vitamin D Metabolites Several non-radioligand assays are available for determining the levels of vitamin D metabolites. These assays have shown considerable inter-assay variability, leading to misclassification of the vitamin D status of individuals. Regardless of the method used, it has been recognized that a central repository for uniform standards is required for validation of these assays and of the laboratories performing them. Measurement of this metabolite should therefore be performed when vitamin D deficiency is suspected. Impaired 1-hydroxylation can contribute to the hypocalcemia of patients with renal dysfunction, oncogenic osteomalacia, and hereditary defects of vitamin D metabolism (see "Hypocalcemic Disorders"). Assays for the intact hormone are classic sandwich assays with antibodies directed against both the N-terminus and C-terminus of the hormone. In early clinical descriptions of primary hyperparathyroidism, the disease emerged as a distinctly uncommon disorder with significant morbidity and mortality rates, in which nearly all affected patients manifested radiographically significant or symptomatic skeletal or renal involvement, or both. The skeletal involvement in classic primary hyperparathyroidism reflects a striking and generalized increase in osteoclastic bone resorption, which is accompanied by fibrovascular marrow replacement and increased osteoblastic activity. Abnormal parathyroid glands are associated with hypercalcemia in three settings: (1) primary hyperparathyroidism, (2) familial hypocalciuric hypercalcemia, and (3) lithium-induced hypercalcemia. Note the dramatic remodeling associated with the intense region of high bone turnover in the third metacarpal in addition to widespread evidence of subperiosteal, endosteal, and trabecular resorption. The skull may exhibit a finely mottled, "salt-and-pepper" radiographic appearance, with loss of definition of the inner and outer cortices. Dental radiographs typically show erosion or disappearance of the lamina dura due to subperiosteal resorption, often with extension into the adjacent mandibular bone. The erosion and demineralization of cortical bone may lead to radiographic disappearance of some bones, most notably the tufts of the distal phalanges of the hands, the inferolateral cortex of the distal third of the clavicles, the distal ulna, the inferior margin of the femoral neck and pubis, and the medial aspect of the proximal tibia. The clinical correlates of these changes may include aching bone pain and tenderness, "bowing" of the shoulders, kyphosis and loss of height, and collapse of lateral ribs and pelvis with "pigeon breast" and triradiate deformities, respectively. The renal manifestations of classic severe primary hyperparathyroidism include recurrent calcium nephrolithiasis, nephrocalcinosis, and renal functional abnormalities that range from impaired concentrating ability to end-stage renal failure. Associated signs and symptoms include recurrent flank pain, polyuria, and polydipsia. No unique features of the stone disease in primary hyperparathyroidism serve to distinguish it from that associated with other, more common causes of calcium kidney stones. The stone disease more often may be recurrent and severe, and in some patients the stones may be composed entirely of calcium phosphate instead of the pure oxalate or mixtures of oxalate and phosphate more commonly encountered in other disorders.
25mg pamelor overnight delivery
Insulin release from the fetal rat pancreas in vitro in response to glucose or pyruvate is minimal but can be stimulated by leucine anxiety 9gag gif buy pamelor 25mg cheap, arginine, tolbutamide, or potassium chloride, indicating that parts of the secretory mechanism are functional in the fetus. Calcium channel activation does not occur in fetal islets in response to initiators of insulin release that cause depolarization of adult islet cells. As is true for insulin, the capacity for glucagon secretion is blunted in the fetus. Hyperglycemia does not suppress fetal plasma glucagon concentrations in rats, monkeys, or sheep, and acute hypoglycemia does not evoke glucagon secretion in the rat fetus. Amino acids, which are important secretagogues for insulin and glucagon in the adult, probably have little role in modulating insulin and glucagon secretion in the preterm fetus, but infusion of alanine into women at term increases both maternal and cord blood glucagon concentrations, indicating a fetal glucagon response to amino acids in the term fetus. The rapid maturation of responsiveness to glucose in the neonatal period in both premature and mature infants suggests that this blunted state may be a secondary result of the relatively stable fetal serum glucose concentrations maintained by placental transfer of maternal glucose rather than a primary, temporally fixed, maturation process. Alternatively, the lack of any enteric signal to the pancreas from feeding via release of incretins may also account for this stability. However, most of the actual mass change takes place in the newborn period and is associated with changes in -cell size rather than number. How much -cell mass is a determinant of progression to type 2 diabetes mellitus is unclear. Insulin and glucagon are normally not necessary for substrate metabolism in the fetus. The fetal respiratory quotient is approximately 1, which suggests that glucose is the primary energy substrate for the fetus. Other substrates, such as amino acids and lactate, may also be used in the human as in the sheep fetus and these, together with glucose, are stored as fat and glycogen in preparation for birth. Early in gestation, hepatic metabolism and substrate utilization appear to be independent of insulin and to be modulated in an autoregulatory fashion by glucose. Fetal insulin plays a role near term, when insulin also has the capacity to increase fetal glucose uptake and lipogenesis. These conditions tend to potentiate the fetal anabolic milieu during the period of rapid growth in the last trimester of gestation. Pancreatic Regulation of Blood Glucose During the neonatal period, the placental source of glucose is lost. A normal term infant has an immediate postnatal fall in blood glucose concentration during the first 2 to 4 hours from values close to maternal concentrations to around 2. Counterregulatory hormones rapidly become active, and these changes result in stabilization of blood glucose concentrations, although adult concentrations are not reached until approximately 72 hours of life. The increase in plasma catecholamines coincident with parturition may be responsible for some of these changes; catecholamines stimulate glucagon and inhibit insulin release. Thus gluconeogenesis is readily demonstrable in the newborn, where nearly 10% of glucose utilization is accounted for by gluconeogenesis from alanine. Plasma free fatty acid concentrations increase postnatally because of the effects of catecholamines and chemical thermogenesis. Oxidation of fatty acids probably provides cofactors (acetyl coenzyme A and the reduced form of nicotinamide adenine dinucleotide) required for gluconeogenesis, as well as sparing glucose for utilization by crucially dependent tissues such as the brain. It has been reported that lactate may be neuroprotective in at-risk babies with hypoglycemia within the first 48 hours after birth, a time period when ketone bodies are unlikely to provide protection. Early feeding for prevention of hypoglycemia in at-risk babies (including infants of mothers with diabetes, small and large for gestational age, and preterm) is the mainstay of management. Dextrose gel is effective in treating neonatal hypoglycemia without affecting breastfeeding. Neonatal diabetes can be permanent and require lifelong treatment or may be transient, in which case the diabetes may spontaneously remit before 18 months of age (60% of cases) (or be so mild as not to require treatment) but will often relapse, usually during adolescence. These patients are responsive to sulfonylurea therapy and do not require insulin treatment. Demand of insulin is so small, and feeding so frequent, that treatment with multiple daily injections is difficult. Increased attention to the primarily genetic nature of early-onset diabetes has resulted in an expanding list of causal genes and an expansion of phenotypic characteristics in syndromic forms. Poorly controlled maternal diabetes mellitus is associated with fetal macrosomia, an increased risk of spontaneous abortion, and fetal malformation. Maternal hyperglycemia also leads to hyperinsulinism and -cell hyperplasia in the infant. Infants of diabetic mothers are prone to polycythemia, renal vein thrombosis, hypocalcemia, respiratory distress syndrome, jaundice, persistent fetal circulation, cardiomyopathy, congenital heart disease, and malformations of other organs. Glucose is transported into the cell by glucose transporters; intracellular glucokinase catalyzes an essential irreversible step for glycolysis. Diagnostic criteria are a glucose infusion rate more than 8 mg/ kg/minute, a laboratory blood glucose less than 3 mmol/L with detectable serum insulin or C-peptide, low serum ketone bodies, and low serum fatty acids. First-line treatment is diazoxide and chlorothiazide, and second-line treatment is octreotide and glucagon. Focal lesions can be cured with surgery, whereas diffuse lesions require near-total pancreatectomy, which usually does not result in a cure and may lead to diabetes mellitus. Together these structures comprise the branchial apparatus, which normally undergoes involution leaving behind derivatives, including the thyroid gland, parathyroid glands, thymus, ultimobranchial body, eustachian tube, middle ear, and external auditory canal. The superior parathyroid glands are derived from the fourth branchial pouch, which also gives rise to the thyroid gland. The third branchial pouch gives rise to the inferior parathyroid glands and the thymus. The parathyroid glands remain intimately connected with their respective branchial pouch derivatives, and parathyroid gland development from the third and fourth pharyngeal pouches proceeds in synchrony with thyroid embryogenesis. Most of the parathyroid gland parenchyma is composed of chief cells (also known as the parathyroid gland principal cells). The chief cells spend most of their time inactive due to normal calcium homeostasis. Near term, fetal parathyroid cells are largely composed of inactive chief cells, with only a few intermediate chief cells containing occasional secretory granules. The fifth pouches contribute paired ultimobranchial bodies that are incorporated into the developing thyroid gland as the parafollicular or C cells that secrete calcitonin. The calcitonin content of C cells in the neonatal thyroid gland is as high as 540 to 2100 mU/g of tissue, values as much as 10 times those observed in the normal adult gland. Transcription Factors Involved in Development of Parathyroid Glands the molecular signaling pathways that are involved in determining the differentiation of the pharyngeal pouch endoderm into parathyroid cells are being elucidated by studies of patients with hypoparathyroidism and appropriate mouse models. These studies have revealed important roles for several transcription factors, which include members of the homeobox (Hox) and paired box (Pax) families. Disruption of the Hox15 gene in mice results in parathyroid gland aplasia, indicating that this gene functions as part of the genetic cascade programming normal thyroid-parathyroid gland development. Deletions of genes encoding several transcription factors in mice result in developmental anomalies that include parathyroid defects, although such abnormalities have not yet been reported in man. This is expressed in the uterus, placenta, amnion, umbilic cord, lactating breast, and fetal parathyroid glands. In animal models, despite maternal hypocalcemia induced by a calcium-restricted diet, vitamin D deficiency, parathyroidectomy, or a vitamin D receptor deletion model, fetuses were reported to be normocalcemic. Studies in fetal sheep and monkeys and measurements in human preterm and term infants indicate that the majority of calcium is transported in the third trimester. Movement of calcium through trophoblastic cytosol, involving intracellular calcium-binding proteins (mainly calbindin D9K), which transport calcium to the basal membrane. Calcium and phosphate are maintained at a higher set-point in the fetus than in the pregnant mother, especially in the third trimester, to meet the demands of fetal bone mineralization. In late gestation, fetal serum concentrations of calcium and phosphate are maintained above the maternal concentrations by approximately 1. Although the molecular mechanism of transplacental calcium transport has been well studied, little is known about the transport mechanism of phosphate and magnesium. In this model, fetal parathyroidectomy decreases placental calcium transport and lowers fetal serum calcium.
Discount pamelor express
The gene is expressed in the follicular cells anxiety ridden buy pamelor 25 mg with amex, and the mutations that lead to haploinsufficiency are associated with an increased rate of follicular atresia. The degree of ovarian failure varies from primary amenorrhea to irregular menses and premature ovarian failure, with ultrasound findings ranging from normal-appearing ovaries to streak gonads with an inconsistent number of primordial follicles found on ovarian biopsy. The dominant clinical feature is the neurologic manifestations of involvement of the central and peripheral nervous system. The hypergonadotropic-hypogonadism is more severe in females because males virilize at puberty. Follicle-Stimulating Hormone Receptor Resistance: Gene Mutations and Hypergonadotropic Hypogonadism. This disorder likely is responsible for most cases of the resistant ovary syndrome. Affected males in these families are normally masculinized at puberty but tend to have small testes. Males have normal differentiation of external genitalia but may have undescended testes; germinal aplasia or hypoplasia and impaired Leydig cell function may be present. Although most patients with Frasier syndrome present with ambiguous genitalia, this diagnosis should be considered for any phenotypic female with end-stage renal disease (due to focal segmental glomerulosclerosis) and sexual infantilism. Williams-Beuren syndrome is a microdeletion disorder, or contiguous-gene-deletion disorder caused by deletion of the Williams-Beuren syndrome chromosome region; it was previously known as Williams syndrome. While it is generally known for its characteristic facial appearance and unusual personality, many other features, including endocrine conditions, occur. However, differentiating the diagnosis of hypogonadotropic hypogonadism from constitutional delay in growth and adolescence remains difficult in spite of decades of study owing to the overlap in physical and laboratory findings for the two conditions (see Table 26. Medical history must elicit all symptoms of chronic or intermittent illnesses and all details pertaining to growth and development. Has puberty failed to occur, or did it begin but failed to progress or even regress Poor linear growth and poor nutritional status during the neonatal period and childhood may reflect long-standing abnormalities of development. Family history may reveal disorders of puberty or infertility, anosmia, or hyposmia in relatives and delay in the age at onset of puberty in parents or siblings. Recalled age of pubertal onset is relatively reliable in women but less often accurate in men. A history of consanguinity is important in the detection of autosomal recessive disorders. A growth chart is plotted to represent graphically growth velocity from birth (see Chapter 25). Late-onset growth failure usually indicates a serious condition requiring immediate evaluation. The height velocity should be documented over a period of at least 6 months, preferably 12 months. The U/L segment ratio and the arm span are measured Chapter 26 Physiology and Disorders of Puberty 1113 Delay in onset of secondary sexual development after 13. Questionnaires with pictures are used to allow a child to determine his or her own stage of puberty in some studies but do not replace the physical examination, as there is a tendency to overestimate development early in puberty and underestimate it late in puberty. The length and width of the testes are measured in boys, or the volume is assessed using an orchidometer. The length and diameter of the gently stretched penis are determined in boys, and the diameter of glandular breast tissue and areolar size are determined in girls. Obese boys often appear to have a small penis because of excessive adipose tissue surrounding the phallus; only when the fat is retracted can the full extent of phallic development be assessed. The extent of pubic and axillary hair is assessed, as is the degree of acne or comedones. The possibility of cryptorchidism or retractile testes should be determined if no testes are palpated in the scrotum. Determination of olfaction is important because many patients with Kallmann syndrome wait years for the correct diagnosis to be made even in the presence of classic findings; physicians must remain alert to the possibility of this diagnosis and to the fact that congenital anosmia may not be noted by the patient or family for years. Complete physical examination, including the lungs, heart, kidney, and gastrointestinal tract, is important in the search for a chronic disorder that may delay puberty. Genetic testing is available either by targeted evaluation or by panels developed by the commercial laboratories for hypogonadotropic hypogonadism. This is more easily carried out when there is an autosomal dominant, autosomal recessive, or X-linked condition than for oligogenetic conditions at present. Ultrasound evaluation of the uterus and ovaries provides useful information about the state of development of these structures but only if the ultrasonographer has experience with children and young adolescents. Assessment of karyotype should be considered for all undiagnosed short girls, even in the absence of somatic signs of Turner syndrome and especially if puberty is delayed or unexplained short stature is involved. Karyotype assessment should be performed for boys with suspected Klinefelter syndrome stigmata or behavior. The rate of growth in these patients is usually appropriate for bone age; a decrease in growth velocity occurs in some normal children just before the appearance of secondary sexual characteristics and may awaken concerns if such a pattern occurs in these subjects. The onset at puberty correlates better with bone age than with chronologic age in delayed puberty, although bone age is not any better at estimating the onset of puberty in normal boys than is chronologic age and cannot be considered a highly accurate test. Under 3 years of age, children may have peaks of gonadotropins and sex steroids similar to pubertal subjects. Measurement of an 8 am serum testosterone level provides an accurate indication of impending pubertal development; a value of greater than 0. This technique may help predict spontaneous pubertal development, but it still requires considerable watching and waiting. These methods require continued evaluation before they become standard clinically. Watchful waiting may remain the procedure of choice when a patient does not fulfill the delineated criteria and does not fall into a diagnosable grouping. Sometimes, years of observation are necessary to detect the appearance of spontaneous and progressive signs of secondary sexual development or to document rising concentrations of gonadotropins or gonadal steroids before the diagnosis is clear. Treatment of Delayed Puberty and Sexual Infantilism Patients with constitutional delay in growth and adolescence ultimately have spontaneous onset and progression through puberty. Often, reassurance and continued observation to ensure that the expected sexual maturation occurs are sufficient. These individuals may be unable to participate in the dating activities their friends are starting; smaller size may lead them to avoid participation in athletics; immature appearance may lead to ridicule, especially in the locker room; and schoolwork may suffer because of their poor self-image. Some children feel such intense peer pressure and low self-esteem that only the appearance of signs of puberty can reassure them and enable them to participate in sports and social activities with their peers. Poor Chapter 26 Physiology and Disorders of Puberty 1117 self-image in late-maturing boys may carry into adulthood, even after normal puberty ensues. Growth retardation appears more often responsible for most of the stress rather than the delay in pubertal development itself. For psychologic reasons, for boys 14 years old or older who show no signs of puberty, a 3-month to 6-month course of testosterone enanthate, cypionate, or cyclopropionate (50-mg dose given intramuscularly every 4 weeks) may be helpful. Decades of experience confirm no effect on adult height of low dosages in the short term. Although the use of exogenous androgens may improve self-image and start the secondary sexual changes of puberty, low-dose androgen use does not increase final height. If during the 3 to 6 months after discontinuing gonadal steroid therapy spontaneous puberty does not ensue or the concentrations of plasma gonadotropins and plasma testosterone in boys or plasma estradiol in girls do not increase, the treatment may be repeated. When treatment is discontinued after bone age has advanced, for example, to 12 to 13 years in girls or 13 or 14 years in boys, patients with constitutional delay usually continue pubertal development on their own, whereas those with gonadotropin deficiency do not progress and may regress. Oral testosterone undecanoate was successfully used for less than 1 year in a large study of boys with constitutional delayed puberty with apparently no ill effects. Delayed puberty in this situation is usually a result of inadequate nutrition and low weight or excessive energy expenditure. When weight returns to normal values, puberty usually occurs spontaneously, although there will likely be months of delay. Treatment with T4 allows normal pubertal development in hypothyroid patients with delayed puberty. The transition of care from the range of age normally considered to be adolescence, administered by a pediatric practitioner, to adult life, administered by a practitioner experienced in adult endocrinology, presents important implications for a change in the manner in which medical care is presented. Prevent the potential short-term and long-term psychologic, personality, and social handicaps of delayed puberty.