Order sarafem line
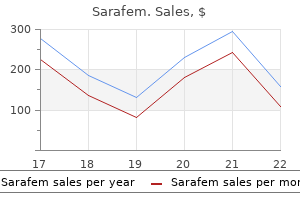
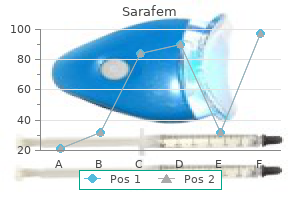
If the femoral head does not move in the acetabulum pregnancy kick counts purchase sarafem once a day, it should not be joined to the femoral shaft. Patient who underwent rotationplasty for treatment of Paley type 3 congenital femoral deficiency. The rotationplasty allows the patient to motor his prosthetic leg as a below-the-knee amputee with excellent function. Preoperative photograph of a patient with Paley type 3 congenital femoral deficiency. Positioning the patient undergoing the superhip procedure is positioned supine on the operating table with a bump placed under the ipsilateral sacrum to tilt the pelvis about 35 to 40 degrees. The patient undergoing the initial femoral lengthening is positioned supine on the operating table with a radiopaque grid placed under the operating table pad. A small bump is placed under the ipsilateral sacrum to allow the extremity to rest in a patella-forward position. Preoperative Planning Preoperative evaluation consists of obtaining radiographs and performing a physical examination as previously described. Patients undergoing a superhip procedure should be prepared and draped to allow access to the iliac crest, gluteal region, adductor region, and the entire lower extremity. The positioning allows access to the pelvis, proximal femur, and the remainder of the lower extremity. This incision gently curves to the posterolateral border of the femur along the level of the posterolateral intermuscular septum. A second S-shaped incision is made from the lateral side of the patellar tendon and is extended proximally in line with the intermuscular septum at the level of the knee joint. If the extremity is significantly short, these incisions become one extended approach. The flap of skin and the subcutaneous tissues are reflected in a full-thickness fashion off the deep fascial layer anteriorly. This is accomplished by releasing the fascia on the tensor fascia lata side of the intermuscular septum. This fascial incision is extended distally to join the anterior margin of the fascia lata that was previously exposed. The fascia lata is cut distally at the tibia and is reflected proximally if a concurrent superknee procedure with knee ligamentous reconstruction is not required. If ligamentous reconstruction is planned, the fascia lata is cut proximally and reflected distally. Its anterior vascular pedicle (ie, lateral femoral circumflex vessels) can be cauterized and cut. The conjoint tendon of the rectus femoris, before it divides into the direct and reflected heads, is transected. If the anterior fascia of the thigh and the fascia of the sartorius muscle are tight, they are released. The lateral femoral cutaneous nerve is identified and protected before releasing the fasciae. The femur should now be adducted, internally rotated, and flexed such that the greater trochanter is brought to the level of the center of the femoral head and the posterior border of the greater trochanter is parallel to the floor. If the proximal femur cannot be placed in this position, there is an abduction contracture of the hip joint. In these cases, the glutei muscles should be elevated off the greater trochanter along with the vastus lateralis muscle as a trigastric flap. The posterior border of the vastus lateralis at the intermuscular septum is identified and dissected free of the femur subperiosteally. The dissection is continued proximally along the posterior aspect of the greater trochanter. It is important to peel a thin layer of cartilage with the flap because the tendinous covering over the trochanter is thin. It is then reflected anteriorly off the intertrochanteric line, leaving the anterior hip capsule intact. The capsule should not be incised, and the pelvic trochanteric ligament running superior to the hip joint capsule should never be cut. During the release, the piriformis tendon should be identified and released, which allows the femur to rotate internally. An alternative approach for patients with mild abductor contractures is to split the iliac crest apophysis and dissect the gluteal muscles in a subperiosteal fashion. This allows the gluteal muscles to slide distally, resolving the abductor contracture. At the completion of the procedure, the iliac crest is then resected by 1 cm to allow for closure of the apophysis with no tension. The femoral head and neck are placed in a neutral orientation to the pelvis by extending and maximally adducting the hip joint. Plate Fixation of Proximal Femur the preferred method of fixation is the hip plate method. The first step is to place a guidewire from the tip of the greater trochanter to the center of the femoral head. A second guidewire is inserted in the center of the femoral neck to the center of the femoral head, at a 45degree angle with the initial guidewire. A point 4 to 6 cm posterior to the anterior superior iliac spine is marked on the skin, and the lateral "bump" is marked on the skin. These two points are connected with a curvilinear line that extends distally on the posterior margin of the vastus lateralis muscle belly. The second incision is a distal S incision that begins at the level of the lateral intramuscular septum on the side of the thigh and proximally at the level of the superior pole of the patella and extends to the lateral margin of the patellar tendon to the tibial tubercle. The fascia lata is reflected distally to its insertion on the tubercle of Gerdy of the proximal tibia. The rectus femoris tendon is the first structure identified as it inserts on the anterior inferior iliac spine. Before release of the psoas tendon, the femoral nerve, which is adjacent to the psoas tendon, is identified and decompressed. The confluent tendinous portions of the hip abductor muscles (gluteus minimis and medius muscles) and the vastus lateralis muscle are sharply dissected off the cartilaginous greater trochanter, creating a continuous musculotendinous sling. This release resolves the abduction contracture and allows access to the piriformis tendon. The chisel should be oriented perpendicular to the straight posterior border of the greater trochanter. At the intertrochanteric level, two wires are inserted perpendicular and parallel to the side plate. The first cut is parallel to the plate, and the second cut is perpendicular to the plate. A second subtrochanteric osteotomy is performed by cutting obliquely from the lateral starting point of the previous parallel cut. The distal femoral segment is extended, abducted, and internally rotated and aligned with the plate allowing the femoral segments to overlap. The bone ends have to overlap because of the constraints of the surrounding soft tissues. A third osteotomy is performed perpendicular to the distal femoral shaft at the level of overlap (usually 1 to 2 cm distal to the second osteotomy site). The distal femoral segment is reduced to the plate and fixation is completed with three or four screws. For type 1b cases (delayed femoral neck ossification), an adjunct treatment can be performed by drilling a channel with a diameter of 3. To expose the ilium, the iliac crest apophysis is split and detached with the periosteum. The outer table of the ilium is subperiosteally dissected, and the hip abductor muscles are lifted from anterior to posterior. It is important to cut the apophysis and periosteum transversely at this level to allow the osteotomy to separate anteriorly. The osteotomy does not enter the sciatic notch but passes anterior and parallel to the level of the triradiate cartilage. Second Kirschner wire is inserted into the femoral neck toward the center of the femoral head, creating a 45-degree angle with the initial guidewire (arrow).
Syndromes
- Biting your cheek, tongue, or lip
- Develop bubbles of air that can be felt underneath the skin of the chest, neck, arms, and trunk
- Oxazepam (Serax)
- Chest pain or chest tightness
- Swelling of the neck muscles (possibly present at birth)
- Aging changes in hormone production
- Narrowing of the tube that carries urine out of the bladder (urethral stricture) in males
- Male hormone (testosterone) level
- Cough with pink, frothy sputum
- Abdominal CT scan
Order sarafem cheap
The pin is advanced into the head women's health center st petersburg generic sarafem 20 mg overnight delivery, stopping several millimeters below the subchondral bone. I usually prefer to place this pin starting more proximally and anteriorly to the first pin. If needed, a third pin can be added from the greater tuberosity downward into the shaft. This is helpful in small patients for better purchase in the head, but I usually avoid this pin because of a higher rate of soft tissue complications. The shoulder is rotated and the tips of the pins should appear to approach the joint surface and then withdraw with continued rotation. In larger patients near or at skeletal maturity with sufficient bone stock, cannulated screws can be inserted over a wire in the same fashion as described for threaded pins. I have found this technique rarely necessary, but it does avoid the issue of pin management (see below). With a sandbag or towel roll placed between the shoulder blades, the patient is placed supine with the involved side close to the edge of the operating table. Intravenous anesthesia or conscious sedation may be used, but I prefer to perform the reduction under general anesthesia, both for patient comfort and so I can proceed to open reduction if required. If unsuccessful, the clavicle can be grasped and pulled upward, especially in thin patients. Finally, the region can be prepared and draped and a towel clip used percutaneously to grasp the clavicle and reduce it. This is not always the case, however, and the stability should be carefully confirmed. Gentle posterior pressure on the clavicle confirms the stability of the reduction. The shoulder is taken through a range of motion and the reduction checked as well. Finally, intraoperative fluoroscopy is used to confirm symmetry of the sternoclavicular joints. This allows careful exposure of the medial fracture (in the case of a true dislocation) or the physeal fracture site (in the case of a fracture-dislocation). Care should be taken when exposing this area so that dissection does not inadvertently excise the epiphysis. Although descriptions exist of temporary plating or pinning, the risks of these fixation techniques (migration of Kirschner wires, need for plate removal) do not justify Open Reduction the first step in this procedure is ensuring the presence of a pediatric vascular-thoracic surgeon in proximity to the operating room, preferably in the room. The needle is passed through one drill hole, out across the fracture site, and up through the hole in the corresponding fragment. After fixation, the reduction is tested for stability, and after confirmation of such, the wound is closed using standard technique. Under the subcutaneous tissue lies the platysma muscle, which is also split in line with the incision. The clavicle is exposed subperiosteally, beginning laterally and working medially toward the joint. It is crucial to remain subperiosteal with the clip to avoid inadvertent injury to the vessels lying immediately posteriorly. For a pure dislocation, a figure 8 pattern through burr holes will secure the joint. For a fracture-dislocation, it is often easier to use two separate sutures perpendicular to the fracture line. Gapping at the fracture may signify interposed tissue, and the preparation should allow open exposure if required. The surgeon should avoid placing the pins in the region of the axillary and musculocutaneous nerve. The skin should be handled carefully and multiple punctures avoided to minimize soft tissue complications. The surgeon should carefully consider patient age and remodeling capacity before proceeding with surgery. The surgeon should accept less-than-perfect reduction in lieu of open reduction if possible to avoid the complications associated with an open approach. Sternoclavicular joint the surgeon should consider open reduction and stabilization if doubt exists about stability. Closed reduction Open reduction Preoperative imaging can identify potential associated injuries. Operative treatment usually results in satisfactory healing, although several reports note a high rate of complications from operative treatment, including late fracture through a pin hole and late osteomyelitis. Some authors recommend accepting residual displacement unless the patient has symptoms of mediastinal compression, as remodeling of the fracture can be expected; however, that view is not universal. The outcome in these injuries is usually quite good, as remodeling will occur and there is no risk to mediastinal structures. A battery-powered hand drill is helpful for securely grasping the pins and backing them out, as the tips are threaded. They can be checked and redressed if concern exists, and pin care with half-strength peroxide is helpful. In obese patients, or in young patients who may have difficulty with activity restriction in the sling, soft tissue movement around the pins may lead to infection. Removal then requires an additional trip to the operating room, usually at 4 to 6 weeks after surgery. After pin removal, the patients are instructed to begin gentle active-assisted shoulder range of motion. Once healing is complete radiographically, formal physical therapy can be initiated to gain any additional mobility and strength. Most children do well, however, by gradually resuming activities at their own pace. Fracture and retrosternal dislocation of the medial clavicle in a 12-year-old child: case report, options for diagnosis, and treatment in children. The location of the biceps tendon in completely displaced proximal humerus fractures in children. Short-term outcomes after surgical treatment of traumatic sternoclavicular fracture-dislocations in children and adolescents. An axial load to the femur as in a fall from height or a motor vehicle accident may result in hip fracture. The important retinacular vessels that supply the capital femoral epiphysis course along the femoral neck. The lesser trochanter is an apophysis in the child and forms the insertion for the iliopsoas. Much of the greater trochanter is apophyseal and forms the insertion for the hip abductors. Minimally displaced proximal femoral physeal separations have a better prognosis, much like those of an acute slipped capital femoral epiphysis. Untreated they are likely to heal, but there is a possibility of avascular necrosis. Intra-articular fractures of the femoral neck that are undisplaced may heal but also may displace. Displaced fractures have a poor prognosis for healing because they are intra-articular and therefore will not generate much subperiosteal new bone. Extra-articular fractures of the femur (low neck, intertrochanteric, and subtrochanteric fractures) have a good prognosis for healing but tend to result in shortening, external rotation, and sometimes varus if untreated. While simple falls are a frequent cause of hip fractures in the elderly, they are less common in children. There are growth plates beneath the capital femoral epiphysis, the greater trochanteric apophysis, and the lesser trochanteric apophysis. Extra-articular fractures (low neck, intertrochanteric, and subtrochanteric fractures) in children less than 6 years old can be treated by closed manipulation and spica casting. Preoperative Planning the injured hip should be evaluated under anesthesia using fluoroscopy.
Order 20mg sarafem fast delivery
The patient continues in the fracture boot for 5 to 6 weeks menopause the musical las vegas quality 10mg sarafem, at which point maintenance of alignment or radiographic union is confirmed on repeat weight-bearing radiographs. The patient is then allowed to wear regular shoes, and activities are advanced as tolerated thereafter. Full recovery and return to sports or other rigorous activity may require up to 3 to 4 months. Lateral and plantar subluxation (black arrows) is evident on the weight-bearing radiographs, and displacement of normal radiographic landmarks (black lines) confirms injury. Recent studies suggest that pure ligamentous Lisfranc injuries are best managed with open reduction and primary arthrodesis of the medial and middle columns. Definitive surgery is generally delayed 10 to 14 days to allow adequate resolution of soft tissue swelling. Pure ligamentous injuries require rigid screw fixation for the medial and middle column joints and Kirschner wire fixation for the lateral column joints; bony injury patterns, particularly those with more comminution, may require minifragment bridge plate fixation. A third, more proximal and lateral incision may be required to stabilize the cuboid where necessary. Because of the limited soft tissue envelope overlying the midfoot, the importance of meticulous soft tissue handling and maintaining full-thickness soft tissue flaps cannot be overemphasized. Positioning the patient is placed supine with a bolster beneath the ipsilateral hip. Protective padding is placed around the contralateral limb, primarily to protect the peroneal nerve, and the contralateral limb is secured to the table. A sterile bolster is placed beneath the operative limb at the knee to facilitate access to the midfoot and intraoperative fluoroscopy. The lateral incision is centered over the lateral border of the third tarsometatarsal joint. The floor of the tendon sheath is then incised and subperiosteal dissection commences medially, extending to the medial margin of the first tarsometatarsal joint and producing a full-thickness flap. Full-thickness subperiosteal flaps provide access to first and second tarsometatarsal, and medial-middle intercuneiform joints. Gross instability through first tarsometatarsal joint (C) and second tarsometatarsal and intercuneiform joints (D) in a different patient. Care is taken not to violate the adjacent neurovascular bundle, which is maintained within its soft tissue envelope. The underlying third tarsometatarsal joint capsule is identified and a full-thickness subperiosteal flap is developed extending medially toward the lateral portion of the second tarsometatarsal joint, and laterally toward the fourth and fifth tarsometatarsal joints where necessary. Again, the status is noted of each of the tarsometatarsal and intercuneiform joint capsules dorsally, and therefore the extent of instability of each joint. Deep dissection continues medial to extensor digitorum communis tendon and extensor digitorum brevis muscle (A) and exposes the third tarsometatarsal and the lateral portion of the second tarsometatarsal (not visualized here) joints (B). If more than 50% of the articular surface of the medial and middle column joints is involved, primary arthrodesis should be considered, although this is controversial. Arthrodesis of the fourth and fifth tarsometatarsal joints should be avoided if possible. Supplemental allograft mixed with highly concentrated platelet aspirate is then placed within the involved joint spaces. Although the exact reduction maneuver may vary depending on the injury pattern, the first metatarsal is typically supinated (externally rotated) relative to the medial cuneiform. Correction of this rotational deformity is crucial in restoring the medial column and the weight-bearing function of the first ray. The reduction of the remaining midfoot joints depends on an anatomic reduction of the first tarsometatarsal joint. Definitive stabilization is then obtained at the first tarsometatarsal joint with 3. There is typically a distinct cortical "shelf" on the medial cuneiform that provides an excellent buttress for screw purchase. Alternatively, this joint may also be reduced and stabilized before stabilizing the first tarsometatarsal joint. Care is taken not to violate the articulation between the middle and lateral cuneiform. A B the second tarsometatarsal joint is then provisionally reduced and provisionally stabilized with a 1. For a metatarsal base fracture or fracture-dislocation pattern precluding transarticular fixation, bridge plate fixation may be required. The fourth and fifth tarsometatarsal joints are then reduced and definitively stabilized with 1. Because the intermetatarsal ligaments between the third, fourth, and fifth metatarsals are often preserved, these joints may anatomically reduce indirectly, thereby allowing percutaneous stabilization. The tourniquet is deflated and sterile dressings are placed, followed by a bulky Jones dressing and Weber splint. Deep layered closure sealing intra-articular contents and extensor hallucis longus tendon. Injury radiographs must be closely scrutinized preoperatively for proximal joint involvement. During surgery, the status is noted of each of the intercuneiform joint capsules dorsally, and therefore the extent of instability of each joint. There is typically a distinct dorsal crest on both the first metatarsal and medial cuneiform. Because of the hard cortical bone at the diaphysis of the first metatarsal, the screwhead of the distal-to-proximal screw is specifically countersunk to avoid compromise of the dorsal cortex and loss of fixation. With fixation of the Lisfranc joint, the screw must angle slightly dorsally (relative to the plantar foot) to accommodate the normal "Roman arch" configuration in the coronal plane. The Kirschner wires traversing the lateral column joints are removed 6 weeks postoperatively. Weight bearing is not permitted until 10 to 12 weeks postoperatively, at which point weight-bearing radiographs are obtained to confirm maintenance of reduction. The patient is gradually allowed to resume regular shoes, and activity is advanced as tolerated thereafter. In a primary arthrodesis, the limb is immobilized in serial short-leg non-weight-bearing casts for 10 to 12 weeks after surgery, at which point radiographic union is confirmed on weight-bearing radiographs. The patient is then converted to a venous compression stocking and prefabricated fracture boot, and weight bearing is advanced as described previously. We do not routinely remove hardware unless symptomatic or specifically requested by the patient, in which case the implants may be removed at 1 year after surgery. An accurate diagnosis and anatomic reduction are crucial to ensuring satisfactory results. Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation: a prospective, randomized study. Fracture-dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. The fracture begins on the lateral aspect of the fifth metatarsal and may propagate into the metatarsocuboid joint. Operative treatments have included internal fixation with or without bone grafting and bone grafting alone. Pain will be elicited with direct palpation over the base of the fifth metatarsal. Physical examination should include: Direct palpation over the base of the fifth metatarsal: Pain in this region increases suspicion of injury. Direct palpation over the tarsometatarsal joint complex: Pain indicates possible injury to the Lisfranc complex.
Purchase sarafem 20 mg online
It is passed first under the patellar tendon and then through a medial capsular tunnel breast cancer yoga buy cheap sarafem 20mg line. The graft is then passed through a subperiosteal tunnel around the adductor magnus tendon. This extra-articular ligament is tensioned with the knee in 90 degrees of flexion to prevent an extension contracture. To expose the medial side, the medial soft tissue flap is reflected to the midline. An anterior-to-posterior drill hole is made through the epiphysis, and the anterior limb of the fascia lata is passed from anterior to posterior, exiting near the midline posteriorly. Another drill hole that passes through the medial distal femoral epiphysis from anteromedial to posterolateral is made. The ligamentized fascia lata is pulled through the posterior capsule and into the medial femoral epiphyseal tunnel using its leading suture. It is fixed in place with a biotenodesis absorbable screw (Arthrex) after tensioning in flexion. Reverse MacIntosh (extra-articular posterior collateral ligament) procedure is performed by passing the anterior limb of the fascia lata graft under the patellar tendon and through a window created in the medial joint capsule. The graft is then passed through a subperiosteal tunnel under the adductor magnus tendon, looped back onto itself, and secured with nonabsorbable suture. The synovium is then carefully dissected free of the undersurface of the quadriceps muscle proximally and from the patellar tendon distally. Medially, the capsule is incised proximally in a longitudinal fashion, separating the vastus medialis muscle from the vastus intermedius muscle. The quadriceps and patellar tendon are left attached to the patella and the entire extensor mechanism can be shifted medially. The knee joint capsule is dissected away from the synovium medially and laterally. The synovium also is dissected free from the quadriceps tendon and the patellar tendon. Synovium is released from the patella circumferentially, leaving the quadriceps and patellar insertions intact. The hole in the synovium is closed longitudinally with absorbable suture, leaving the patella with the quadriceps and patellar attachments extra-articular. The Grammont procedure is performed as described above, and the patellar tendon is shifted medially. Knee is positioned in full extension, and the new position for the patella is marked on the synovium. Fascia lata graft passes through the advanced medial capsule and is sutured onto itself. If the popliteal angle is greater than 10 degrees, the biceps femoris tendon and medial hamstrings should be released. If the patient has undergone a superhip procedure, the preparatory surgery has been completed and repeat releases of the soft tissues are not necessary. If the preparatory surgery has not been performed and the Dega osteotomy is needed, it should be combined with excision of the fascia lata, superknee reconstruction, or both. Alternatively, the soft tissue releases can also be performed simultaneously with the lengthening procedure. Placement of Femoral Fixator An arthrogram of the involved knee is obtained under fluoroscopy. In the lateral view, the femoral condyles are rotated until they superimpose each other. This is considered a "true lateral of the knee" (note that this is not the patella-forward position-actually the patella will be externally rotated approximately 10 degrees in this position). The center of rotation is the intersection of the posterior cortical line and the distal femoral physeal line. If these are not available, two pin clamp lids can be joined by 30-mm bolts to create a sandwich clamp. The external fixator rail is aligned with the femur in the sagittal view and the most proximal half-pin is inserted at the level of the base of the greater trochanter (this pin should be distal to the apophysis). The lateral view is obtained, and the posterior aspects of the femoral condyles are superimposed to create the perfect lateral view. The hinge reference wire is inserted at the intersection of the posterior femoral cortical line and the distal femoral physis. The first distal half-pin is placed on the anterior row one hole proximal to the hinge-axis pin. Example of pediatric Orthofix rail with a three-hole cube placed on the distal half-pins to allow a third half-pin to be inserted into the distal fragment. Radiograph shows acute valgus correction performed at the osteotomy site for lengthening. Half-pins placed in the anterior half of the femoral diaphysis can result in a fracture either during the lengthening process or after frame removal. The most distal half-pin is placed one hole proximal and anterior to the knee axis reference wire. At this point, the position of the hinge axis is a fixed point to the initial distal half-pin. If concurrent distal valgus deformity is being corrected, a swivel clamp should be used at the proximal clamp site when placing the first two half-pins. Conical washers are placed medial and lateral to the Sheffield clamp to reduce friction. A one-third Sheffield arch is then attached to the clamp and arched medially to be anterior to the tibia. As the first pin is being secured to the Sheffield arch, the knee must be in full extension and reduced. The initial tibial half-pin is placed in an anterior-to-posterior direction, denoted by the empty Ilizarov cube. Clinical photographs of two examples of the Sheffield arch attachment to the tibia. The knee hinge allows for full flexion (A) and extension (B) while protecting the knee from subluxation during lengthening. Clinical photograph shows a completed Orthofix external fixator for femoral lengthening in a patient with congenital femoral deficiency. The knee extension bar is constructed by building Ilizarov cubes from the half-pins to the Sheffield arch. Sockets are used to connect the extension bar to the frame, which allows for easy removal of the bar during physical therapy. The drop-leg test consists of lifting the lower extremity off the bed and fully extending the knee. If the knee flexes with no catching or friction, two additional half-pins are placed in the tibia. If there is friction during the drop-leg test, the hinge and knee rotation axis needs to be examined and adjusted. Usually, the dummy axis pin can be slightly bent and the hinge axis reoriented to the knee rotational axis. A knee extension bar is built using Ilizarov parts and is extended from the previously placed three-hole cube to the Sheffield arch. Another strategy is to attach a separate Ilizarov cube to the protruding ends of the distal femoral half-pins and extend it to the Sheffield arch. At the conclusion of the procedure, Botox, 10 units per kilogram of body weight, is injected into the proximal quadriceps using multiple injection sites. This is to reduce quadriceps muscle spasms and pain during knee flexion stretches. The surgeon should first identify the femoral nerve before performing any releases or tenotomies. Knee flexion contracture should be released with biceps femoris lengthening and posterior capsular release.
Generic 20mg sarafem free shipping
Intraoperatively menstruation 3 days sarafem 20mg low cost, a graduated approach is necessary, starting with a medial parapatellar approach with lateral release, advancing to quadriceps snip, and lastly to osteotomy or V-Y turndown as needed. Maximum passive flexion to avoid tension on the repair is determined intraoperatively, after capsular closure. The brace is locked in extension at night and with ambulation until the extensor lag is less than 15 degrees. The turndown group had a higher increase in arc of motion than the osteotomy group, but they also had a higher degree of extension lag. The turndown group also had a lower percentage of patients who considered their surgery unsuccessful in relieving pain and return of function, and a lower percentage of patients who had difficulty with kneeling and stooping. Only 5 of 14 patients had extensor lag greater than 5 degrees, with active extension lag averaging 4 degrees (range 0 to 20 degrees). Revision total knee arthroplasty: planning, management, controversies, and surgical approaches. Extensor mechanism failure associated with total knee arthroplasty: prevention and management. The use of a modified V-Y quadricepsplasty during total knee replacement to gain exposure and improve flexion in the ankylosed knee. It originates at the inferior pole of the patella and inserts onto the tibial tuberosity. The extensor mechanism of the knee begins proximally as the quadriceps femoris muscle. Anteriorly, the fibers of the rectus femoris tendon traverse the patella and insert on the tibial tubercle inferior to the patella as the patellar tendon. The fibers of the vastus lateralis muscle expand to the superolateral border of the patella and proximal tibia to form the lateral retinaculum. The fibers of the vastus medialis muscle insert into the superomedial border of the patella and tibia to form the medial retinaculum. Comparison with either immediate postoperative or preoperative films is helpful to establish the diagnosis of a complete rupture of the patellar tendon. Contraindications for surgical reconstruction include: Infection Inability to comply with postoperative immobilization and the physical therapy program For these rare instances, cast or brace immobilization in full extension for 6 to 8 weeks followed by a physical therapy program to regain motion and strength may be appropriate. Progress must be slow, and strengthening exercises should be delayed for at least 3 months. In this chapter, we describe the technique that we use in our institution, consisting of reconstruction with Achilles tendon allograft with or without augmentation with an autogenous semitendinosus tendon graft. Alternatively, if the incision extends too proximally, a sterile tourniquet can be used. The leg is prepared and draped in the standard sterile fashion for joint replacement surgery. Fluoroscopic equipment is in the room with a technician available in case it becomes necessary to use it: eg, for judgment of the joint line, preparation of the tibial box, or placement of the screws to avoid the tibial component. The pneumatic tourniquet is inflated (usually to 250 mm Hg) after the leg has been exsanguinated with an Esmarch bandage. Preoperative Planning Initial evaluation of the patient History Physical examination of the knee Radiographs Previous operative reports should be obtained. The surgeon should be ready to perform revision surgery of any of the components if there is evidence of malrotation or malalignment. Fresh-frozen allografts are preferable to freeze-dried allografts Before anesthesia induction, the allograft is inspected visually to ensure that the specimen is adequate. The dissection is carried down in the midline with conservative elevation of skin and subcutaneous flaps. The calcaneal bone is cut to match the created rectangular space in the proximal tibia. The rectangular patch is used to augment the attempted primary repair, and is sutured in place with no. Before anesthesia induction, visually inspect the allograft to ensure that it is adequate, with at least 3 cm distal calcaneus bone allograft attached to the Achilles tendon. Be ready to perform revision surgery of the total knee components if malrotation or loosening is present. A progressive controlled increase in flexion and strengthening exercises is allowed after 12 weeks. Use of a semitendinosus tendon autogenous graft for rupture of the patellar ligament after total knee arthroplasty: a report of seven cases. Reconstruction of a ruptured patellar tendon with Achilles tendon allograft following total knee arthroplasty. The required ranges of motion for daily activities are as follows4,12: 67 degrees of flexion for normal gait on level ground 83 degrees of flexion to climb stairs 90 to 100 degrees of flexion to descend stairs 93 degrees of flexion to stand from a standard-height chair 105 degrees of flexion to tie a shoe Flexion contractures can be equally disabling: a flexion contracture of more than 15 degrees usually is considered pathologic, because it greatly inhibits normal gait. Lateral: lateral joint capsule and retinaculum with the insertion of the vastus lateralis Distal: patellar tendon the blood supply to the patella is provided by an anastomotic ring of vessels supplied by the geniculate arteries. It is important to try to avoid complete devascularization of the patella, because avascular necrosis can occur. The blood supply to the skin overlying the knee travels from the deeper tissues up through the superficial fascia and does not run superficially. If skin flaps are required at the time of surgery, they must be full-thickness, therefore, to avoid skin necrosis. The exposure can be thought of as a progressive release or "unleashing" of the extensor mechanism. In rare cases, a chronic regional pain syndrome develops, characterized by severe pain, cutaneous hypersensitivity, vasomotor disturbance, and stiffness. Flexion contractures greater than 15 degrees limit the ability to stand up straight and cause substantial fatigue when walking. Direct questions should be asked to determine whether pain control was adequate in the postoperative period. Did the patient have severe pain postoperatively that limited his or her ability to perform physical therapy Does the patient have hypersensitivity of the skin overlying the incision or other complaints that suggest neurogenic pain or a chronic regional pain syndrome Wound drainage that persisted for more than a few days after surgery the use of antibiotics for more than 24 hours postoperatively Persistent pain that is of a different character than the pain the patient had before the surgery Inspect the skin for the presence of a past or present sinus, indicating infection. Densely adherent skin is much harder to close and may represent a higher risk for necrosis. Flexion of less than 90 degrees and a flexion contracture of more than 15 degrees are considered pathologic. If component malposition is identified (eg, internal rotation), the components are revised. The top line marks the epicondylar axis, and the bottom line marks the posterior condylar line; the component in this case is internally rotated. These images are overlaid on each other to determine the rotation; normal is 18 degrees of internal rotation; the component in this case is internally rotated 16 degrees. If either is elevated, an aspiration of the knee joint is obtained and sent for a cell count with differential and cultures, including aerobic, anaerobic, and acid-fast bacilli, and fungi. Patients must have been off antibiotics for at least 2 weeks before the knee aspiration. At the time of revision, additional cultures are taken from within the joint, and an intraoperative frozen section is taken from the synovial tissues. An average of more than 10 polymorphonuclear cells identified within tissue (and not fibrin) is consistent with infection. Nuclear medicine studies, such as a triple-phase bone scan, occasionally are helpful in identifying subtle loosening but are not routinely obtained. If chronic regional pain syndrome is being considered, a sympathetic blockade often is administered. In cases of flexion contracture, dynamic splinting or the use of serial casts can be tried in an attempt to obtain full extension. Patients are sent home with a pump to administer the medication and are carefully monitored by a pain control specialist. The manipulation should be performed using a short-lever arm with the patient completely relaxed until a firm endpoint is reached. It is crucial to work with a pain management specialist and a physical therapist to ensure that stiffness does not recur postoperatively. Flexion contractures are harder to address arthroscopically, but a posterior release can be performed using small, open, medial and lateral incisions. Open arthrolysis with exchange of the modular polyethylene liner1,9,10,13 this procedure also can be performed in selected patients with well-fixed, appropriately aligned components.
Vitis pentaphylla (Jiaogulan). Sarafem.
- Reducing cholesterol levels.
- What is Jiaogulan?
- Dosing considerations for Jiaogulan.
- What other names is Jiaogulan known by?
- Are there safety concerns?
- How does Jiaogulan work?
- Are there any interactions with medications?
- Regulating blood pressure, bronchitis, stomach disorders, ulcers, constipation, gallstones, obesity, cancer, diabetes, sleeplessness (insomnia), backache, pain, improving memory, improving heart function, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96288
10mg sarafem with visa
I prefer a curette because surgeon control is easy and the curette can be passed percutaneously zeid women's health clinic order discount sarafem. I have used various instruments, but drills and burrs tend to burn and occasionally grab tissue, and reamers and circular saws require a larger incision (really not percutaneous, almost the size of a typical open epiphysiodesis). A bony bridge needs to form only at the peripheral margins of the physis both medially and laterally to accomplish an epiphysiodesis. The central part of the physis does not require treatment because it will close spontaneously. The stability of the bone is maintained postoperatively and the patient may continue to ambulate. Preoperative Planning Anticipated remaining growth is determined by one of the following methods: Green-Anderson method10 Mosley graphic method16 Multiplier method18 Menelaus "rule of thumb" method15 I prefer the Mosley straight-line method because growth inhibition is expressed graphically, multiple data entries can be charted to help predict growth more accurately, and the method is easy to calculate in a brief outpatient visit. I perform a proximal fibular epiphysiodesis in addition to the proximal tibial epiphysiodesis if the final discrepancy between the tibia and fibula is anticipated to be more than 1 cm. If the discrepancy is anticipated to be less than 1 cm, I do not perform a proximal fibular epiphysiodesis and have not detected a clinical problem with such a mild discrepancy. A tourniquet is placed on the proximal thigh but is not inflated unless bleeding occurs. Often a lift is used in children until an appropriate skeletal age is reached to perform an equalization procedure. A prosthesis may be necessary if deformities are so severe that adequate length or ambulatory ability cannot be achieved by operative methods. Surgery may be necessary to provide an appropriate stump for the prosthesis, and a percutaneous epiphysiodesis is used occasionally to achieve correct stump length. Ablation of the peripheral margins both medially and laterally in a physis causes bony bridges to form between the epi Femoral epiphysiodesis at distal physis Longitudinal incisions of 3 mm (stab incisions) medially and laterally in the skin at the level of the physis at its peripheral area Tibial epiphysiodesis at proximal physis Longitudinal incisions of 3 mm Medially the incision is 3 mm at the level of the physis at its peripheral area. Laterally the incision is 3 mm at the level of the physis and at the anterior border of the fibula. Fibular epiphysiodesis at the proximal physis the same incision is used for the fibular epiphysiodesis as for the lateral physeal area of the tibia; however, in the epiphysiodesis of the fibula the curette is directed differently to avoid injury to the common peroneal nerve (described below). A radiographic view of the osteotome penetrating the physeal plate to a depth of about 0. The same operative process is repeated on the opposite side of the physeal plate (medially or laterally), again sparing the middle third of the physeal plate. The curette is rotated and advanced to the level of the inner third of the physis. The anticipated area of ablation of the peripheral third of the physis (both medially and laterally). The curette is swept cephalad and caudad in the physis to ablate the peripheral third of the physis, leaving the middle third of the physis intact. A photograph of a specimen demonstrating the ablation of the peripheral third of the physis, leaving the middle third of the physis intact. A photomicrograph of the femoral physis distally demonstrating the ablation of the peripheral third of the physis, leaving the middle third intact. A computed tomography section through the femoral physis distally demonstrates the ablation of the peripheral third of the physis. Note the narrow space in the middle third of the physis, with the neurovascular bundle posteriorly (between the femoral condyles) and the patellofemoral joint anteriorly. Epiphysiodesis of the Fibula Proximally the same incision is used to perform the epiphysiodesis of the fibula as the proximal physis of the tibia laterally. The most superior extent of the fibular epiphysis proximally is usually at the level of the tibial physis. The elastic of the knee immobilizer adds very mild compression to the incision and helps prevent a hematoma or edema. The knee immobilizer brace should not be applied with a force that impedes circulation. To avoid injury of the common peroneal nerve, the curette is directed into the anterosuperior area of the proximal epiphysis and then inferiorly into the physis of the fibula. The surgeon should not exit the cortex of the fibula as the central area is ablated. Another choice is to use a stapling technique (or figure 8 plate-screw), which preserves the physis, rather than epiphysiodesis. Also, I prefer to delay the epiphysiodesis for a short period to ensure that the limb lengths do not reverse the discrepancy. If the limb lengths correct and remaining growth will cause a problematic (reversal) discrepancy, I would perform a contralateral epiphysiodesis. The patient may usually be discharged within the same operative day (outpatient surgery). The knee immobilizer is used for 3 to 4 weeks to protect the extremity from fracture. Radiographs are performed about 4 to 6 months postoperatively to ensure adequate healing. Bony bars at the peripheral margins of the physis are usually observed radiographically by 6 months postoperatively. Correction of the leg-length discrepancy may be determined by periodic radiographs and clinical examinations. During postoperative evaluations the extremity should be evaluated to ensure appropriate length correction and to watch for an angular deformity. Lack of appropriate closure may result in undercorrection and asymmetric closure causes angulation. In nine patients, the epiphysiodesis was combined with a femoral lengthening or femoral shortening. The Moseley straight-line method accurately and efficaciously predicted the timing for percutaneous epiphysiodesis in all but one patient, who had unpredictable growth from hemihypertrophy secondary to a hemangiomatosis. Horton and Olney12 reported the results of 42 percutaneous epiphysiodeses in 26 patients. Stated advantages include a cosmetic scar, short hospital stay, low incidence of complications, and reliability. Canale and coworkers6 reported on 13 children treated by a percutaneous epiphysiodesis; growth plate fusion occurred in all cases. Brax and Gille5 performed a percutaneous epiphysiodesis using a drill and radiographic control in 10 children. They had good results in all but one case and considered the procedure to be minimally traumatic, cosmetically preferable, and safe. Craviari and colleagues7 reported the results of 60 cases followed to skeletal maturity who were treated by a percutaneous epiphysiodesis. Complications comprised hematoma in 2 cases, need for surgical revision in 10 cases, limb deviation in 4 cases, and inverted discrepancy in 2 cases. Gabriel and associates9 reported the results of 29 patients who underwent 56 physeal procedures with a percutaneous epiphysiodesis. The procedure lasted a mean of 36 minutes, and in all patients a physeal closure developed. No unplanned angular growth, no deep infections, and no cases of joint stiffness were reported. Kemnitz and coworkers13 performed a retrospective review of 57 patients who underwent percutaneous epiphysiodesis. Macnicol and Gupta14 reported 35 cases of epiphysiodesis in which a cannulated tube saw was used to ablate the physis. One patient had slight overgrowth of the fibula and another had an unsightly scar; otherwise the results were favorable. Ogilvie and King17 used a low-speed, high-torque drill to create an epiphysiodesis in seven children.
Generic 10mg sarafem with amex
Ulna lengthening with or without radius epiphyseal stapling remains a common procedure reported in the literature pregnancy 8 weeks 4 days best buy sarafem, but we do not use this regularly. The treatment for symptomatic radial head dislocation is usually surgical excision once the patient is skeletally mature. In rare instances, however, exostosis excision with ulnar osteotomy may be effective in relocating the radial head. Planning of this is important, as the ability to access the distal ulna is imperative whether the osteochondroma is located on the distal ulna or radius. If the patient has ulnar involvement only, the incision can be placed on the subcutaneous border of the ulna between the flexor carpi ulnaris and the extensor carpi ulnaris. If the patient has osteochondroma of both the radius and ulna, the incision has to be modified to allow exposure of both bones as well as the distal ulna. This is usually done by transecting the distal ulna through the epiphyseal area, leaving the triangular fibrocartilage complex attached to the distal fragment. As stated earlier, in the skeletally immature patient, release of the tether alone is usually adequate. In a skeletally mature patient, a radial osteotomy is performed after exostoses excision and ulnar-tether release. Layered closure is then performed and the extremity is immobilized for 2 weeks, followed by institution of range-of-motion exercises. In individuals close to skeletal maturity, the surgeon should perform excision of the exostoses and ulna-tethering release associated with epiphysiodesis of the distal radius to avoid any further progression of the deformity. In distraction lengthening of the forearm bones, the bone formation takes longer compared to the lower limb because of the lack of weight bearing. Therefore, one of the disadvantages of this technique is that the external fixator must be kept on for several months. To improve the bone formation and reduce the risk of fracture at the lengthening site, dynamization techniques are recommended. When the ulna is lengthened, the cordlike portion of the interosseous membrane tends to pull the radius distally. Otherwise, the cordlike portion of the interosseous membrane should be dissected to prevent migration of the radius. In case of exostosis excision and ulna-tethering release, casting is performed for 4 weeks, followed by range-of-motion exercises and splinting. If an osteotomy was performed, casting is continued until radiographic evidence of healing is seen. In patients who require surgery, we feel that ulnar-tether release, with or without exostoses excision, with or without radial osteotomy, provides the most reliable result with the fewest complications. In selected patients this can greatly improve function, in addition to the improved cosmesis of the extremity. For symptomatic radial head dislocations we prefer excision, as this usually leads to a consistent, reproducible result with little risk. The main complications in progressive distraction lengthening are nerve damage, fractures at the lengthening site, and pin tract infection. When only the ulna is lengthened, the distracting tension is not exerted directly on the neurovascular bundle, with minimal risk of nerve dysfunction. When performing radial head excision, the surgeon has to be careful in the initial dissection to avoid injury to the posterior interosseous nerve as well as to the stabilizing structures of the elbow. Long-term results of surgery for forearm deformities in patients with multiple cartilaginous exostoses. Correction and lengthening for deformities of the forearm in multiple cartilaginous exostoses. Evaluation of the forearm in untreated adult subjects with multiple hereditary osteochondromatosis. Deformities and problems of the forearm in children with multiple hereditary osteochondromata. Hereditary multiple exostoses: anthropometric, roentgenographic, and clinical aspect. Treatment of multiple hereditary osteochondromas of the forearm in children: a study of surgical procedures. Correction of the wrist deformity in diaphyseal aclasis by stapling: report of a case. A practical classification system for multiple cartilaginous exostoses in children. Associated anomalies include Klippel-Feil syndrome, rib deformities, omovertebral bone formation, muscle anomalies, clavicle hypoplasia, tracheoesophageal fistula, anal stenosis, kidney anomalies, diastematomyelia, and scoliosis. Associated congenital anomalies such as congenital scoliosis may progress, thereby changing the appearance of the deformity. In bilateral cases, both shoulders appear to be high, and the neck may appear thick and short. The scapula in Sprengel deformity is abnormally high, has a decreased vertical diameter, and is deformed in shape. The supraspinous region is rotated anteriorly in a convexity near the shape of the dorsal thorax. The scapula in Sprengel deformity may be attached to the lower cervical vertebrae (usually C6) by an abnormal band of tissue, which may be fibrous, cartilage, or bone (ie, omovertebral bone). The trapezius muscle, the levator scapulae muscle, and the rhomboid muscles often are hypoplastic. Associated bony congenital anomalies include Klippel-Feil syndrome, fused ribs, cervical ribs, congenital scoliosis, cervical spina bifida, hypoplastic clavicle, and short humerus. Sprengel deformity occurs as a result of interruption of the normal caudal migration of the scapula during fetal development. Scoliosis and kyphosis as well as deformities of the chest from rib anomalies may be observed. Preoperative Planning Preoperative evaluation of the appearance of the deformity with photographs is advised. The author prefers full-profile photographs taken from the frontal, posterior, and both side views. Motion can be documented by a series of photographs taken with the arms extended, elevated, and abducted. Videos of the patient performing motion activities of the shoulder are helpful to determine the degree of deformity and whether or not the appearance is acceptable. The Cavendish grading scale is helpful in evaluating appearance3: Grade I (very mild): shoulder joints are level, and the deformity is not obvious when the patient is dressed. Preoperative evaluation of shoulder motion Occupational therapy measurement of combined abduction of both shoulders (combined glenohumeral and scapulothoracic movement) as well as other shoulder motion is useful. The author uses radiographs at the extremes of motion to verify the degree of measurements. The anomalies of the shoulder, spine, and rib cage must be evaluated radiographically. Currently, the author uses somatosensory evoked potentials and transcranial electrical motor evoked potentials to evaluate the brachial plexus nerve function during surgery. Baseline values are obtained after the induction of anesthesia, and monitoring is continued during the procedure. Sonography of the spinal cord is helpful in infants younger than about 4 months of age who have congenital spine anomalies. Sonography can be performed through the cartilage of the lamina and spinous process, but after about 4 to 5 months of age, ossification blocks the views. Congenital spine anomalies have a high association with intraspinal abnormalities. Sonography of the kidneys is helpful in cases associated with congenital spine anomalies. Both still and video photography are helpful to record preand postoperative appearance and to document function. In children with mild deformities in which the appearance of the shoulder is acceptable, operative treatment probably is not indicated. Positioning the patient is placed in the prone position with the head positioned as if facing forward. The entire arm, the shoulder, and the posterior thorax back area (ie, superiorly from the high cervical area, inferiorly to the lumbar area, and laterally to the contralateral scapular area) are prepared and draped. Leads for the somatosensory evoked potentials and transcranial electrical motor evoked potentials are positioned on the skin and muscles in sterile fashion.
Discount sarafem 20 mg without prescription
Lytic changes become evident on routine radiographs only when cortical destruction approaches 30% to 50% menopause uptodate order sarafem us. In some cases of prostate cancer, reduction in testosterone levels via bilateral orchiectomy or administration of estrogens or antiandrogens may produce dramatic results. Estrogens are no longer used as a first-line agent because of the risk of cardiovascular complication. In older patients with advanced disease, however, the side effects of the drugs may be too severe. The goals for surgical intervention in the patient with metastatic carcinoma to bone are relief of pain; prevention of impending pathologic fracture; stabilization of true fractures; enhancement of mobility, function, and quality of life; and, for some, improved survival. It is generally agreed that a patient must have a life expectancy of at least 6 weeks to warrant operative intervention. Cancer patients, regardless of their age, may have increased difficulty protecting their fixation device or prosthesis secondary to systemic debilitation. A mean score of 7 or below indicates a low risk of fracture; radiation therapy should be considered. A score of 8 or above suggests a substantial risk, and surgical intervention is recommended. Preoperative Planning In many cases, the diagnosis of metastasis to the proximal femur will be made before a fracture occurs. In these cases, it is the responsibility of the orthopedic surgeon to decide whether the patient should receive some form of internal stabilization before radiation therapy is begun. Criteria for the performance of a prophylactic stabilization procedure include the following: 50% cortical lysis A femoral lesion greater than 2. As elucidated in the Mirels score, the peritrochanteric area in general is at high risk for fracturing. These criteria are not perfect, and large errors arise in estimation of the load-bearing capacity of the bone. For example, no system takes into account the histologic subtype, preexisting osteoporosis, and functional demands. Treat with conventional cemented acetabular component with or without rebar (anchorage with large fragment screws) as needed. The lesion creates a deficient medial wall (A), requiring an antiprotrusio device (B). Such cases should be referred to an orthopedic oncologist and are beyond the scope of this chapter. Such lesions have deficient lateral cortices (columns) and dome (A) and necessitate the use of rebar to reconstruct the posterior or anterior columns with either 6. Modest femoral neck lesions may be stabilized with a reconstruction nail, with the exception of renal cell and thyroid carcinoma, in which cases arthroplasty is recommended. Procedure of choice: replacement arthroplasty the decision regarding bipolar versus total hip arthroplasty is a function of acetabular involvement, preexisting arthritis, and life expectancy. Acetabular disease may go unrecognized on plain radiographs in up to 83% of cases. Peritrochanteric metastatic lung cancer treated with screw and side-plate construct that failed within 4 months. For realized and large impending peritrochanteric lesions (B), the surgeon should have a low threshold for replacement arthroplasty (C). A realized intertrochanteric pathologic fracture from metastatic breast cancer was inappropriately treated with a reconstruction nail that went on to hardware failure within 3 months. Long-stem prostheses may be used for extensive femoral involvement, but attention must be paid to cement deployment during the early cure stage, use of a long laparoscopic sucker, or venting. Realized fractures Cemented proximal femoral replacement is the only Subtrochanteric Peritrochanteric Neck Impending fractures An intramedullary reconstruction-type device is strongly recommended. For renal cell and thyroid cancer, the surgeon should proceed with cemented calcar-replacing arthroplasty. A patient with documented metastatic breast cancer to bone presented with a several-week history of progressive aching in the upper thigh. She was walking when she felt a snapping sensation and immense pain and was no longer able to ambulate. Deciding whether femoral stability from a cemented longstem arthroplasty is worth the increased risk of a lifethreatening cardiopulmonary embolic event is difficult. Certain steps listed in the following sections have been shown to minimize this risk, warranting long-stem use in cases of extensive femoral disease. This enables the surgeon to perform arthroplasty as well as extensive instrumentation of the posterior column when necessary. Reconstruction of impending proximal femoral lesions can be performed with the patient in the supine position, placed on a fracture table that allows insertion of a cephalomedullary device and interlocking screws. Approach Standard, but sometimes expanded, anterior, anterolateral, and posterior approaches may be used to access the acetabulum. For posterior column instrumentation, an extensile posterior approach is recommended. Nonunion of a trochanteric osteotomy is a major concern in patients with cancer and should be avoided unless absolutely necessary. Visualization of the posterior column, however, is critical to confirm its mechanical integrity; therefore, an incision of adequate size must be used. The screws are then incorporated in the cement mantle of the acetabular component. Intraoperative photos demonstrating adequate positioning of a combination of pins and screws to augment the cement fixation. If the disease is locally advanced, an extensile iliofemoral approach may be necessary to visualize the inner as well as the outer pelvis. The surgeon places his or her index finger into the sciatic notch and then aims the rebar screw or pin parallel to the notch into the posterior column of bone toward the sacral ala. Because threaded pins do not give adequate proprioceptive feedback, the surgeon is encouraged to use a 3. At least two-preferably three or more-screws or pins are necessary to anchor the reconstruction. Some surgeons use targeting jigs, but I prefer to use a careful freehand technique with the nondominant hand in the defect to target the pin. These anterior pins are cut flush with the crest after they are deployed to the appropriate depth in the defect, ideally capturing the ilium. With the rebar in place and sunk to a depth that does not interfere with the acetabular component also being sunk to the correct depth, version, and verticality, mesh or similar material is placed to limit cement extrusion. Femoral preparation and component placement are performed in a similar systematic fashion. After the femoral neck cut is completed with an oscillating saw, the canal is prepared with flexible reaming and broaching. During long-stem femoral component implantation, a long laparoscopic suction device is used to aspirate the medullary contents before and concurrent with cementation of early-cure state polymethylmethacrylate. The long-stem component is introduced slowly but early during the cement cure state, before the viscosity of the cement has increased. I prefer Simplex P bone cement because of its low viscous qualities on immediate mixing. Once the cement is mixed (1 minute), it is immediately injected into the femur in its early, liquefied cure state using a long cement gun. No distal venting is performed, to avoid potential distal stress risers and minimize operative time. The surgeon may still consider using a longer cemented stem if the appropriate precautionary steps, as outlined earlier, are taken. The iliotibial band is incised longitudinally to permit anterior and posterior exposure. The gluteus maximus is carefully split, with concurrent meticulous ligation of perforating arterioles. Time is taken to localize and protect the sciatic nerve in the retrogluteal area, where it lies immediately behind the external rotators.
Order 10 mg sarafem otc
Close attention to spinal cord monitoring is crucial during the entire reduction maneuver women's health center kalamazoo mi buy generic sarafem online. The rods are templated, cut, and contoured, and then attached to the construct while reduction is maintained. As an alternative, a double split fibular strut graft (modified Bohlman technique) can be inserted from the sacrum to the body of L5 to add anterior column support. The procedure is completed by placing bone graft lateral to the implants along the transverse processes from L4 to the sacrum. Meticulous hemostasis is carried out, and a layer-by-layer closure of the operative site is performed. All needed and appropriate imaging studies must be evaluated carefully to identify all aspects of the deformity-including the degree of the deformity and the type (eg, isthmic vs congenital)-as well as any other spinal deformity that may be present (eg, spina bifida occulta). Care should be taken, especially when pathologies such as spina bifida occulta are present, to prevent iatrogenic neurologic injury. Decompression of at-risk nerve roots is a key component to exposure and operation. Instrumentation Careful preparation should be undertaken before performing instrumentation and reduction. Adequate decompression of all neurologic structures at risk should be ensured to prevent iatrogenic injury. Close attention must be paid to neurophysiologic monitoring during both instrumentation and reduction. This procedure should be done over time to allow for relaxation of the soft tissue structures. Reduction of the slip angle is more important than complete reduction of the slip. In the immediate postoperative period, the hips and knees are flexed and elevated using pillows to alleviate pain. Postoperative anteroposterior and lateral standing spine radiographs are taken before discharge. Activity restriction (ie, avoidance of bending and rotational motion) is carried out until fusion has occurred. The patient may return to sports and strenuous physical activity after 1 year as long as spinal fusion has been confirmed. Adequate precautionary measures should be taken before engaging in any contact sport. Excellent functional outcomes were observed in those cases where a solid fusion was achieved. Another study comparing posterior fusion and reduction with posterior fusion and reduction augmented by anterior column support reported a 39% pseudoarthrosis rate in posterior fusion alone. In the cases augmented with anterior column support, 100% fusion rates were achieved. Pseudoarthrosis may be minimized by using meticulous technique and proper preparation of the graft site. Neurologic complications Root lesions (L5 root) From direct trauma, manipulation of nerve roots, epidural hematoma formation (compression) Cauda equina syndrome Autonomic dysfunction Chronic pain Immediate release of the correction should be done when necessary. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis: a comparison of three surgical approaches. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Spondylolisthesis treated by a single-stage operation combining decompression with in situ posterolateral and anterior fusion: An analysis of eleven patients who had long-term follow-up. This can be accomplished with a number of devices that allow for correction of pelvic obliquity and pelvic rotation while allowing for a solid base on which to attach rods for correction of curves above. One of the most reliable structures in the formation of the spine, even in the dysplastic setting of myelomeningocele, is the sacral ala. Of key importance is identification and release of the ileotransverse ligament traversing between the iliac wing and the L5 transverse process. The dissection of the soft tissues around the sacral ala is done posteriorly with a curette; the surgeon must use caution against inserting tools anterior to the sacral ala for fear of injuring the L5 nerve root or plunging into the retroperitoneal space. The types of pelvic abnormalities associated with spinal deformities include pelvic obliquity, pelvic rotation, and flexion and extension of the sacrum. The L5 nerve root traverses anterior to the ala in an oblique direction progressing from posterior to anterior and superior to inferior obliquely from the neural foramina. Immediately inferior to the pedicle of L5 the nerve transgresses anterior to the sacral ala, separated by a distance of 1. Besides the L5 root, the tissue anterior to the sacral ala is retroperitoneal fat. The sacral ala can usually be clearly visualized as a horseshoe-shaped outline on upright or supine lateral radiographic films. The Ferguson view (45-degree angle) in the frontal plane provides the clearest view of the width. The techniques include cleaning of the soft tissues from the sacral ala with release of the ileotransverse ligament. The sizing of the hook to the size of the sacral ala in its front-to-back diameter can be done at surgery. With a rod clamp positioned to demonstrate the posterior plane, a right-sided S-hook is shown in its correct position. This can be aided by placement of a vise grip on the rod in the plane of the lordosis once the S-portion of the rod is positioned over the sacral ala. The rod is removed from the wound and the three-point bender applied to produce the proper sagittal contours. If the S-hook is used instead, the sagittal contours can be made in the rod independent of the hook position. Initial position of the S-hook on the rod for placement purposes, with 1 cm of rod protruding. A strong cantilever force can be created to correct pelvic obliquity by using two sagittally contoured rods fixed to S-hooks positioned against the sacral ala distracted against the L4 pedicle screws. The pelvis can then be pivoted by grasping the rods above and correcting the pelvic deformity in one maneuver. The final fixation of the S-hook is completed with both set screws firmly tightened. An L4 polyaxial pedicle screw works well to ensure proper pressure and fixation between the L4 screw and the sacral ala. Chapter 67 Anterior Approach for Open Reduction of the Developmentally Dislocated Hip Richard M. In the first trimester, the structures of the joint begin as a single mass of scleroblastema with a globular femoral head that becomes cartilage at 6 weeks. The joint space develops by degeneration at 7 to 8 weeks and the structure of the joint is well apparent by week 11. A round and reduced femoral head influences the concave shape of the acetabulum to develop. Acetabular growth depends on interstitial, appositional, periosteal new bone and secondary centers of ossification growth. In the first two trimesters of fetal life the acetabulum is a hemisphere with a depth 50% of its diameter. However, by the time of birth the depth is only 40% of its diameter, which may contribute to instability at birth. By 8 years of age the acetabular shape is for the most part determined and thus surgical reduction is less advised, especially if the dislocation is bilateral. There is continued growth into adolescence, with the triradiate cartilage fusing by 13 years in girls and 15 years in boys.

Buy sarafem overnight delivery
The nails are of differing diameter women's health center heritage valley cheap sarafem 20mg fast delivery, inducing a valgus moment that needs to be controlled in a cast. For stable fractures, progressive weight bearing is initiated in reliable patients. Unstable or comminuted fractures require waiting until visible callus is present before weight bearing. Depending on fracture stability, dynamization of the fixator is initiated early, after sufficient callus is seen. The frame is removed in the office or the operating room after healing is noted radiographically. Patients treated with plate fixation begin a progressive weight-bearing program, with immobilization discontinued after sufficient radiographic healing is present, usually by 6 weeks. Patients treated with elastic intramedullary fixation are usually splinted for 7 to 10 days, followed by progressive weight bearing. The plan is modified based on fracture stability, soft tissue injury, and patient reliability. Patients with substantial (over 50%) cortical contact may begin weight bearing as tolerated after soft tissue healing has occurred. It is better to overimmobilize in questionable cases to avoid malalignment and regain motion later with aggressive physiotherapy. Removal of symptomatic hardware (ie, nails or plate) should be delayed until fracture healing and remodeling are complete. I prefer to remove elastic nails electively in all patients 6 to 9 months after injury, as the nails will become completely intramedullary with significant continued growth, thus making late removal extremely difficult. Myers and coworkers10 reported a significant complication rate in high-energy tibial fractures treated with external fixation, including delayed union, malunion, leg-length discrepancies, and pin-tract infections. Kubiak and colleagues8 reported 2 delayed unions, 2 malunions, and 3 nonunions in a series of 15 patients managed with external fixation, although these appear to have occurred in open injuries. They reported higher functional scores in their patients treated with elastic intramedullary nailing compared to external fixation. Operative techniques usually require additional procedures for removal of pins or prominent nails or plates. Obviously, operative complications do not occur in nonoperatively treated patients. External fixation or flexible intramedullary nailing for femoral shaft fractures in children: a prospective, randomised study. Ender nail fixation in long bone fractures: experience in a level I trauma center. Problems of operative and non-operative treatment and healing in tibial fractures. Operative treatment of tibial fractures in children: are elastic stable intramedullary nails an improvement over external fixation Flexible titanium nailing for the treatment of unstable pediatric tibial fracture. Chapter 17 Open Reduction and Internal Fixation of Tibial Tuberosity Fractures Ernest L. There have also been reports of associated injuries such as quadriceps tendon injury, cruciate ligament tears, and meniscal injury. Patients with minimally displaced fractures may extend the knee, but with obvious discomfort. In the acute fracture there is a sudden onset of pain and it is difficult to ambulate. This is unlike Osgood-Schlatter disease, in which the onset is more chronic and there may be radiographic findings of a chronic condition such as calcification anterior to the secondary center of ossification. The second, or apophyseal stage, occurs at age 8 to 12 years in girls and 9 to 14 years in boys. The secondary center of ossification forms, but it is not connected to the epiphysis of the proximal tibia. The third, or epiphyseal, stage is when the "tongue" of the apophysis and the epiphyseal bone are continuous. The ages for the third stage are 10 to 15 years for girls and 11 to 17 years for boys. The insertion is lateral to the midline; thus, the fracture fragment is centered lateral to the midline. This is important when considering the approach for intra-articular visualization. Bleeding from its proximal branches as it retracts into the anterolateral compartment may lead to compartment syndrome. If it is a nondisplaced fracture or the separation is minimal, a contralateral comparison radiograph may help confirm the diagnosis. There is a significant force that the quadriceps mechanism is able to generate, and this overcomes the strength of the epiphysis and the surrounding periosteum. The other mechanism of injury is sudden passive knee flexion while the quadriceps is contracted. It has been hypothesized that individuals with this fracture may have quadriceps strength that is greater then their peers. In nondisplaced fractures where patients can perform a straight-leg raise, a long-leg cast may be used for treatment. Close radiographic follow-up is needed for the first 2 weeks to ensure the fracture does not become displaced. Even in the nondisplaced fractures, percutaneous screw fixation may allow earlier immobilization and prevent 6 to 8 weeks of casting. The table should allow good anterior and posterior views to be obtained with fluoroscopy. The tourniquet can be used to keep the field dry, allowing for good visualization of the fracture fragments and the joint reduction. The tourniquet, however, may prevent the quadriceps from being freely mobilized and may make reduction more challenging. The proximal extent is the midpatella and the distal aspect is a few centimeters distal to the tibial tubercle fracture bed. There is a significant amount of hematoma formation and torn periosteum; thus, the incision length allows the surgeon to define the appropriate anatomy and prepare the fragment for reduction. Since the tubercle and the fracture are on the lateral aspect of the proximal tibia, a lateral parapatellar approach will give better visualization of the fracture and intra-articular reduction. The lateral approach also limits any damage to the infrapatellar branch of the saphenous nerve. Lateral radiograph of a 13-year-old girl who sustained a tibial tuberosity fracture. There is commonly a long periosteal flap of the proximal tibia seen with the elevated fragment that needs to be extracted from the fracture. The distal, medial, and lateral extent of the fracture should be surgically defined with sharp dissection. For the type of fracture that exits the anterior part of the knee joint, the surgeon must visualize the knee joint. This can be accomplished by looking into the knee through the fracture or by a parapatellar approach. Specifically, the surgeon must ensure the meniscus is not injured or interposed in the fracture before reduction. Often the articular surface can be first reduced and the distal aspect then reduced into the base. A 15-year-old boy with a displaced tibial tuberosity fracture that enters the joint surface. Initial postoperative lateral radiograph after open reduction and internal fixation. Despite initial fluoroscopic views indicating an adequate reduction, the radiographs indicate a poor reduction. The lateral meniscus was impeding the prior reduction and it was removed from the fracture site. Provisional Kirschner wires may be placed to hold the reduction before screw fixation. Bicortical purchase is not imperative due to the thin posterior cortex in this region. It is important to prevent vascular injury posterior to the knee joint in this region.