Discount 1gr secnidazole fast delivery
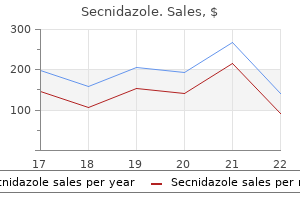
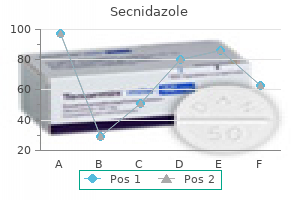
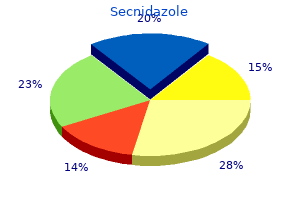
Fine canaliculi within the bone contain interconnecting cytoplasmic processes from the cells medications available in mexico generic secnidazole 1 gr amex. Osteoclasts: large multinucleate cells, lie in small depressions called Howship lacunae, involved resorption and remodelling of bone. Woven bone: this is immature bone with randomly orientated collagen fibers, found during development, associated with healing and repair, remodelled into lamellar bone. Lamellar bone: this is mature bone in which the collagen fibers are orientated in parallel arrays, aligned to withstand stresses on the skeleton. Cortical bone: parallel columns of bone (osteons) with concentric lamellar around central Haversian canals containing neurovascular bundles Cancellous bone: interconnecting network of bony struts with intervening bone marrow. Two forms of bone development: intramembranous ossification (mainly skull bones) and endochondral ossification (bone forms on a template of hyaline cartilage). Synovial joints (diarthroses): permit extensive movement between articular surfaces. Surfaces lined by hyaline cartilage, fibrous capsule lined by synovium, lubricated by synovial fluid. Non-synovial joints: limited movement, bones united by dense collagenous tissues, including dense fibrous tissue (syndesmosis), hyaline cartilage (synchronosis) or fibrocartilage (symphysis). Bands of dense regular connective t issue originating from muscle and inserting into bone to transmit the force of muscle contraction so that movement of joints may occur. The nutrient artery and the epiphyseal arteries enter the bone through nutrient foramina. These openings in the bone arise developmentally as the pathways of the principal vessels of periosteal buds. Metaphyseal arteries arise from periosteal vessels that become incorporated into the metaphysis as the bone grows in diameter. It is composed of hyaline cartilage C and is attached to the cortical bone B of the head of the femur. Both the glycosaminoglycans and collagen are synthesized and maintained by the chondrocytes. Bone Table 15: Summary of bone types and their organization Types of bone Histological features Woven bone, newly calcified Irregular and random arrangement of cells and collagen; lightly calcified Lamellar bone, remodeled Parallel bundles of collagen in thin layfrom woven bone ers (lamellae), with regularly spaced cells between; heavily calcified. Compact bone, ~80% of all Parallel lamellae or densely packed oslamellar bone teons, with interstitial lamellae Cancellous bone, ~20% of all Interconnected thin spicules or tralamellar bone beculae covered by endosteum Major locations Developing and growing bones; hard callus of bone fractures All normal regions of adult bone Synonyms Immature bone; primary bone; bone. All cells except osteoclasts originate from the mesenchymal stem cells, which differentiate into osteoprogenitor cells, osteoblasts, and finally osteocytes and bone lining cells. Bone-lining cells on external bone surfaces are part of the periosteum, hence the term periosteal cells. Bone-lining cells on internal bone surfaces are frequently called endosteal cells. Osteoclasts originate from hemopoietic progenitor cells, which differentiate into bone-resorbing cells. Table 16: Summary of cartilage features in bone Features Hyaline cartilage Elastic cartilage Fibrocartilage Location Percentage of all cells in the bone Function Bone surface, closing cone of resorption canals > 5% Deposits bone matrix; initiates mineralization by releasing matrix vesicles Cuboidal or polygonal, mononuclear cell; basophilic cytoplasm; negative Golgi. The fibrous layer contains fibroblasts, while the osteogenic layer contains progenitor cells that develop into osteoblasts. The osteoblasts are responsible for increasing the width of a long bone and the overall size of the other bone types. After a bone fracture the progenitor cells develop into osteoblasts and chondroblasts, which are essential to the healing As opposed to osseous tissue, the periosteum has nociceptive nerve endings, making it very sensitive to manipulation. Endosteum is a thin vascular membrane of connective tissue that lines the surface of the medullary cavity of long bones. The osteoblasts and osteoprogenitor cells within the endosteum play an important role in remodeling and repair To prevent the bone from becoming unnecessarily thick, osteoclasts resorb the bone from the endosteal side. Endosteal surface is resorbed during long periods of malnutrition, resulting in less cortical thickness. The periosteum is highly active during fetal development, when it generates osteoblasts for the appositional growth of bone. Red Bone Marrow It is vascular and appears red in color due to presence of red blood cells. It consists of network of fine reticular fibers containing blood forming cells, showing all stages of development. At birth it is present in all the bones at all sites, and is an important site of haemopoiesis, but as the age advances the In adults the red marrow is found in the cancellous bone. The population of osteogenic layer of the periosteum is markedly diminished with age and remodelling of bone is in adult life is a very slow process, but osteoblasts below the endosteum are more active than those below the periosteum. Histology A sarcomere is defined as the segment between two neighbouring Z-lines (or Z-discs, or Z bodies). In electron micrographs of cross-striated muscle, the Z-line (from the German "Zwischenscheibe" the disc in between the, I-bands) appears as a series of dark lines. Within the A-band is a paler region called the H-zone (from the German "heller" brighter). H-band is the zone of the thick filaments that is not superimposed by the thin filaments. Within the H-zone is a thin M-line (from the German "Mittelscheibe" the disc in the middle of the sarcomere) formed of, cross-connecting elements of the cytoskeleton. The relationship between the proteins and the regions of the sarcomere are as follows: Actin filaments, the thin filaments, are the major component of the I-band and extend into the A-band. Myosin filaments, the thick filaments, are bipolar and extend throughout the A-band. The giant protein titin (connectin) extends from the Z-line of the sarcomere, where it binds to the thick filament (myosin) system, to the M-band, where it is thought to interact with the thick filaments. Titin (and its splice isoforms) is the biggest single highly elasticated protein found in nature. It provides binding sites for numerous proteins and is thought to play an important role as sarcomeric ruler and as blueprint for the assembly of the sarcomere. Another giant protein, nebulin, is hypothesised to extend along the thin filaments and the entire I-Band. Similar to titin, it is thought to act as a molecular ruler along for thin filament assembly. Several proteins important for the stability of the sarcomeric structure are found in the Z-line as well as in the M-band of the sarcomere. Actin filaments and titin molecules are cross-linked in the Z-disc via the Z-line protein alpha-actinin. The M-band proteins myomesin as well as C-protein crosslink the thick filament system (myosins) and the M-band part of titin (the elastic filaments). The interaction between actin and myosin filaments in the A-band of the sarcomere is responsible for the muscle contraction (sliding filament model). Cardiac muscle consists of individual heart muscle cells (cardiomyocytes) connected by intercalated discs to work as a single functional organ or syncytium. By contrast, skeletal muscle consists of multinucleated muscle fibers and exhibit no intercalated discs. They occur at the Z line of the sarcomere and can be visualized easily when observing a longitudinal section of the tissue. Three types of cell junction make up an intercalated disc-fascia adherens, desmosomes and gap junctions.
Order genuine secnidazole on line
As the morula enters the uterus on the third or fourth day after fertilization medicine you cant take with grapefruit order generic secnidazole on-line, a cavity begins to appear, and the blastocyst forms. The inner cell mass, which is formed at the time of compaction and will develop into the embryo proper, is at one pole of the blastocyst. The outer cell mass, which surrounds the inner cells and the blastocyst cavity, will form the trophoblast. The uterus at the time of implantation is in the secretory phase, and the blastocyst implants in the endometrium along the anterior or posterior wall. If fertilization does not occur, then the menstrual phase begins, and the spongy and compact endometrial layers are shed. Advanced morula (16-64 celled) enters the uterine cavity at day 4 to become blastocyst. The ovary shows stages of transformation between a primary follicle and a preovulatory follicle as well as a corpus luteum. At day 6 trophoblast forms two type of cells: cytotrophoblast (inner layer) and syncytiotrophoblast (outer layer). Inner cell mass (embryoblast) of the blastocyst forms a bilayered embryonic disc having two type of cells: dorsal epiblast and ventral hypoblast. Amniotic cavity develops on the dorsal side and epiblast cell layer lies at the floor of amniotic cavity, whereas hypoblast cell layer is at the roof of blastocyst cavity (now called exocoelomic cavity). Illustration of a section of a partially implanted blastocyst (approximately 8 days after fertilization). At first the walls of the amniotic cavity and yolk sac are in contact with trophoblast. Embryology A cavity, the extraembryonic coelom appears and splits the extraembryonic mesoderm into a somatopleuric layer (in contact with trophoblast) and a splanchnopleuric layer (in contact with yolk sac). The trophoblast and underlying somatopleuric mesoderm form a membrane called the chorion. The amniotic cavity is now attached to trophoblast by some mesoderm into which the extraembryonic coelom has not extended. The embryonic disc viewed from the ectodermal side near one edge shows a rounded area called the prochordal plate. A line drawn through the prochordal plate and the primitive streak divides the embryonic disc into right and left halves. Trophoblast differentiates into cyto and syncytiotrophoblast at post fertilization day: a. The cytotrophoblast, meanwhile, forms cellular columns penetrating into and surrounded by the syncytium. By the end of the second week, the blastocyst is completely embedded, and the surface defect in the mucosa has healed. Epiblast cells give rise to amnioblasts that line the amniotic cavity superior to the epiblast layer. Hypoblast cells are continuous with the exocoelomic membrane, and together they surround the primitive yolk sac. By the end of the second week, extraembryonic mesoderm fills the space between the trophoblast and the amnion and exocoelomic membrane internally. When vacuoles develop in this tissue, the extraembryonic coelom or chorionic cavity forms. Extraembryonic mesoderm lining the cytotrophoblast and amnion is extraembryonic somatic mesoderm; the lining surrounding the yolk sac is extraembryonic splanchnic mesoderm. Trophoblast cells invade the epithelium and underlying endometrial stroma with the help of proteolytic enzymes. Implantation may also occur outside the uterus, such as in the rectouterine pouch, on the mesentery, in the uterine tube, or in the ovary (ectopic pregnancies). Embryoblast forms the embryo chiefly and trophoblast contributes to extraembryonic tissue majorly. Syncytiotrophoblast help in endometrial attachment of blastocyst at day 6 itself (implantation in progress). Blastocyst is the stage at the time of implantation where outer cell mass (trophoblast cells) form a fluid-filled sphere with a small group of inner cell mass (embryoblast cells) at one pole. Amnioblasts cells separate from the epiblast and organize to form a thin membrane, the amnion, which encloses the amniotic cavity. Some cells migrate from hypoblast to surround the exocoelomic cavity and form exocoelomic membrane, which lines the internal surface of the cytotrophoblast. The exocoelomic membrane and cavity soon become modified to form the primary umbilical vesicle (primary yolk sac). The embryonic disc then lies between the amniotic cavity and primary umbilical vesicle. The outer layer of cells from the umbilical vesicle forms a layer of loosely arranged connective tissue, the extraembryonic mesoderm. The primitive streak lengthens by the addition of cells at its caudal end; the notochordal process lengthens by the migration of cells from the primitive node. The epiblast and hypoblast together form a flat, ovoid-shaped disk known as the bilaminar embryonic disk. Within the epiblast, clefts develop and eventually coalesce to form the amniotic cavity. Hypoblast cells migrate and line the inner surface of the cytotrophoblast and eventually delimit a space called the definitive yolk sac. The epiblast and hypoblast fuse to form the prochordal plate, which marks the future site of the mouth. Trophoblast the syncytiotrophoblast continues its growth into the endometrium to make contact with endometrial blood vessels and glands. The cytotrophoblast does divide mitotically, adding to the growth of the syncytiotrophoblast. Primary chorionic villi formed by the cytotrophoblast protrude into the syncytiotrophoblast. Extraembryonic somatic mesoderm (somatopleuric mesoderm) lines the cytotrophoblast, forms the connecting stalk, and covers the amnion. The wall of the chorionic cavity is called the chorion and consists of three components: extraembryonic somatic mesoderm, cytotrophoblast, and syncytiotrophoblast. Blastocyst usually implants within the posterior superior wall of the uterus in the functional layer of the endometrium during the progestational (secretory) phase of the menstrual cycle. On average, it occurs during the 20th to the 23rd day after the last menstrual period. It is a week long process, beginning at day 5 (post-ovulation, or post fertilization) and is completed at day 12. On the same day 6, the cells of trophoblast divide mitotically into cytotrophoblast and syncytiotrophoblast. The syncytiotrophoblast invade the endometrium with the help of proteolytic enzymes secreted by its cells. The blastocyst implants deep and completely lies within the endometrium (interstitial implantation). It is important in early embryonic blood supply, and much of it is incorporated into the primordial gut during the fourth week of development. It is the first element seen within the gestational sac during pregnancy, usually at 3 days gestation. It is situated on the ventral aspect of the embryo; it is lined by extra-embryonic endoderm, outside of which is a layer of extra-embryonic mesenchyme. Tertiary yolk sac (part of secondary yolk sac which is not taken up inside the embryonic disc) 47 Self Assessment and Review of Anatomy Primary yolk sac is the vesicle which develops in the second week. Secondary yolk sac is formed when the extraembryonic coelom develops in the extraembryonic mesoderm. Vitelline circulation functions for absorption of nutritive material from the yolk sac to the embryo. Primitive aorta convey the blood to the wall of the yolk sac, which circulate through a wide-meshed capillary plexus and is carried by the vitelline veins to the tubular heart of the embryo.
Purchase secnidazole online
In particular symptoms checklist discount 1gr secnidazole amex, sigmoid colon cancers may involve the ureter or bladder, and as such a urologist should be involved for possible partial cystectomy or ureteral reimplantation. If the resection is considered extensive, the surgeon should have a low threshold for conversion to an alternative approach, such as an open procedure, to optimize exposure and facilitate the dissection. All patients are placed in modified lithotomy (legs in slight hip flexion) or split-leg position with both arms tucked at the sides. Positioning in this manner affords the surgeons numerous advantages including exposure to the anus/rectum for intraoperative colonoscopy if needed. This can be particularly useful for a tumor that may not have been preoperatively tattooed and localized. The "hockey stick" formation allows access to the splenic flexure as well as the pelvis with no need to redock the arms. When performing a left colectomy or sigmoid resection, it is customary to divide the bowel (and potentially the major vascular structures) with an endomechanical linear stapling device of various staple heights. Prior to any mobilization or resection, inspect the abdominal and pelvic cavity to evaluate for any altered anatomy (phlegmon or occult metastatic processes) not previously appreciated or identified on preoperative imaging. In oncologic procedures, the liver is carefully inspected on both anterior and posterior surfaces, and the peritoneum, omentum, and mesentery are examined for metastatic studding. If the latter is identified, biopsy and surgical judgment will dictate how next to proceed-and whether any further resection is necessary or prudent. Ideally, the location is marked in three to four quadrants such that the tattoo is clearly visible on the antimesenteric surface. Marking the lesion in only one quadrant may pose some difficulty in identification if the tattoo lies on the mesenteric border or in a difficult location such as the splenic or hepatic flexures. Once the pathology has been localized, adjustments to the preoperative surgical plan may be required. In the setting of malignancy, the location of the tumor will determine resection margins and vessel ligation. For cancers in the left colon, oncologic margins should be 5 cm proximal and distal to the tumor. Pathology located in the proximal sigmoid colon or distal descending colon may necessitate mobilization of the splenic flexure for appropriate tension-free anastomosis. Similar to a right colectomy, the initial dissection involves the development of the avascular plane between the parietal peritoneum overlying the retroperitoneum and the visceral peritoneum encompassing the mesentery of the left colon. There are multiple approaches to achieve this task including medial to lateral and lateral to medial. The medial-to-lateral mobilization is performed similar to that done on the right side. The dissection proceeds cephalad to the level of the superior pole of the kidney and may continue to the inferior aspect of the spleen. After medial-to-lateral mobilization is completed, the remaining avascular lateral attachments of the colon to the omentum, spleen, and abdominal and retroperitoneal sidewalls should be divided. Remember, when performing a resection of a tumor in the transverse colon, the omentum should be left on the colon and resected with the specimen to ensure adequate margins and an R0 resection. In the presence of a descending colon or distal transverse colon mass, splenic flexure mobilization will be required. Splenic flexure mobilization is generally performed using a combination of approaches. The patient is placed in a reverse Trendelenburg position with the table inclined toward the right. Laterally, the attachments to the abdominal sidewall and spleen are carefully divided while being mindful not to injure the splenic capsule. A critical step in left colectomy is identification of a distal transection point. Distal transection localization is dependent upon both anatomic and physiologic entities. Appropriate mesenteric vascular supply must be accounted for, as well as distal resection margins in the setting of malignancy. For a sigmoid or distal left colectomy, division is generally performed at the level of the proximal rectum, past the splaying of the taenia coli on the antimesenteric surface. Further dissection and transection may be required to get appropriate distal margins. After the abdominal wall is opened appropriately and the peritoneal cavity entered, a wound protector is inserted to protect the skin and soft tissue from contamination during externalization and creation of anastomosis. Through the wound protector, the distal stapled end of the colon and the proximal mobilized colon and mesentery are extracorporealized. In all cases, appropriate maintenance of vascular supply must be ensured to minimize risk of ischemia of the anastomosis. Double-stapled end-end or end-side technique are often used during a left or sigmoid colectomy. It is recommended by the American Society of Colon and Rectal Surgeons that all left-sided anastomoses be tested for leakage. Once confident the anastomosis is secure and viable, the extraction sites and all port sites 10 mm or greater in size are closed. For lesions located in the hepatic flexure and proximal transverse colons, an extended right colectomy is performed with the middle colic artery and vein ligated. To date, laparoscopy remains the most widely used minimally invasive technique with robotic surgery gaining momentum despite unsubstantiated evidence for cost-effectiveness in the treatment of both colon cancer and rectal cancer. It cannot be overstated that minimally invasive surgery is a technique or a "tool" that a surgeon may use to successfully remove pathology. It should be used when the surgeon has determined that an equivalent operation can be performed with regard to patient safety and oncologic outcome when compared with an open approach. Port site recurrences after laparoscopic and thoracoscopic procedures in malignancy. Comparison of open, laparoscopic, and robotic colectomies using a large national database: outcomes and trends related to surgery center volume. Growth of laparoscopic colectomy in the United States: analysis of regional and socioeconomic factors over time. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Functional recovery after open versus laparoscopic colonic resection: a randomized, blinded study. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Bowel obstruction after laparoscopic and open colon resection for cancer: results of 5 years of follow-up in a randomized trial. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. Randomized clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Comparison of laparoscopic colectomy with and without the aid of a robotic camera holder. Teleroboticassisted laparoscopic right and sigmoid colectomies for benign disease. Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation-technical notes and outcome. Laparoscopic-assisted versus open complete mesocolic excision and central vascular ligation for right-sided colon cancer. Modified complete mesocolic excision with central vascular ligation for the treatment of right-sided colon cancer: long-term outcomes and prognostic factors.
Buy secnidazole 500mg low price
The needles are left attached to allow the anastomosis to be matured at a later date medications like tramadol generic secnidazole 1 gr with visa. After resection of the failed coloanal anastomosis, the distal end of the colon is grasped with a long Babcock clamp and is pulled through the anal canal. The exteriorized colon is then wrapped in gauze and the gauze roll is secured to the distal colon with metal clips. This will prevent the colon from retracting back into the pelvis during the postoperative period. The colon is pulled through the anal canal and exteriorized for a distance of approximately 10 to 15 cm, after which its viability is confirmed by cutting the most distal edge to demonstrate active arterial bleeding. The colon will subsequently lie directly over the aorta, with the mesocolon oriented posteriorly at the anus. In patients with urethral or vaginal defects from anastomotic fistulas, the colon can be partially rotated so that the mesentery covers the injury. Finally, a presacral drain is placed and a loop ileostomy created prior to abdominal closure. The second stage of the Turnbull-Cutait procedure occurs 7 to 10 days later in the lithotomy position under general anesthesia. The exteriorized colon is then amputated several centimeters distal to the anal verge. It is best to err on the side of leaving behind more rather than less exteriorized colon, as the morbidity of anastomotic dehiscence or stricture far outweighs a mucosal ectropion, which can be easily excised at a later date. Two groups have recently reported their results in patients undergoing the Turnbull-Cutait pull-through procedure, the majority of which were performed for failed low colorectal or coloanal anastomoses. Twenty percent of patients admitted to a significant degree of fecal incontinence, while one-third experienced fecal urgency and used pads. Over the past 30 years, the attitude of surgeons confronted with these patients has evolved from one of trepidation and reluctance to that of optimism and a much more aggressive approach. This has largely been aided by technological advances in preoperative imaging, neoadjuvant and intraoperative radiation therapy, improved surgical techniques, and better intensive care unit care, and the traditional long list of contraindications to resection of a recurrent cancer has been whittled down to only a few. Modern recurrent rectal cancer surgeons accept only three strict contraindications to surgical resection: unresectable extrapelvic metastatic disease, comorbidities precluding major surgery, and inability to achieve a negative margin (R0) resection based on assessment by preoperative imaging. Recent reports from expert centers suggest that nearly 50% of patients with recurrent rectal cancer qualify for an attempted curative resection. In addition, one-third of all surgically treated patients will survive 5 years, 60% of operated patients achieve an R0 resection, and the 5-year survival rate for this group is 50%, the surgical mortality rate has decreased to less than 2%, and quality of life of these patients after surgery is similar to that of primary rectal cancer patients. The resulting mucosal ectropion will usually resolve prior to loop ileostomy closure. The operative specimen consists of the colon, rectum, and bladder removed in en bloc fashion. All imaging should be reviewed in the context of a multidisciplinary team conference so that an individualized treatment plan can be constructed for each patient. Decisions regarding neoadjuvant and intraoperative radiation therapy, sacrectomy, vascular resection and grafting, urologic and gynecologic surgery involvement, and plastic surgery reconstruction are made at this time, and appropriate arrangements are made well in advance. A detailed discussion of the entire spectrum of surgery for recurrent rectal cancer is beyond the scope of this chapter; however, a few general points regarding surgical technique can be made. As previously stated, the ultimate goal in any such operation is the achievement of an R0 resection. To this end, the surgeon must stay committed to the idea of being "one plane deeper" than the lateral-, posterior-, and anterior-most extent of the tumor. This often requires the en bloc resection of adjacent structures such as the urinary bladder and prostate gland in men, the vagina in women, internal iliac vessels, and the sacrum. While resection of these structures adds additional morbidity and quality-of-life issues to an already difficult procedure, ill-advised attempts to "shave" tumor off of these structures in an attempt to preserve them does the patient a disservice as the median survival time in patients undergoing a grossly positive-margin resection (R2) is no different from that of patients not taken to surgery. Axial recurrences have the greatest chance of being removed with clear margins and are often located at the prior anastomosis or in residual mesorectum. Axial recurrences are usually the result of poor primary surgery, with either an inadequate distal resection margin or an incomplete mesorectal excision. Sacral resection at or below the level of S3 are well accepted and carry minimal morbidity, aside from possible urinary and sexual dysfunction. Lateral recurrences, defined as those involving the pelvic sidewall structures, are the most difficult to cure, although a recent study has reported a 50% R0 resection rate in a group of these patients treated with en bloc iliac vessel resection. These authors emphasize that the key to achieving such outcomes is a methodical approach to pelvic sidewall dissection that uses the plane lateral to the internal iliac vessels to expose the obturator internus and piriformis muscles, sacrotuberous and sacrospinous ligaments, and sacral nerve roots for potential en bloc resection. Outcomes following Turnbull-Cutait abdominoperineal pull-through compared with coloanal anastomosis. Meta-analysis of survival based on resection margin status following surgery for recurrent rectal cancer. Pelvic exenteration with en bloc iliac vessel resection for lateral pelvic wall involvement. The topics of evidence-based care in colorectal surgery are immense and diverse, and many have been covered in other chapters of this textbook. In the following pages, we attempt to highlight areas of interest in colorectal surgery, not previously covered, that involve evidence-based care of the colorectal surgery patient. There were no differences noted in readmission rates, surgery-specific complications, or mortality. A similar and significant difference was noted for total hospital stay (including readmission days). The total hospital stay was significantly shorter in the laparoscopy cohort (median, 5 days vs. As with the previously mentioned review, the quality of the included studies was graded to be moderate to poor. In general, there are elements supported by extremely strong evidence, such as early initiation of diet and mobilization, and antibiotic prophylaxis (see discussion later), whereas other elements are less well supported. A more recent set of guidelines drew from these recommendations and was reviewed in 2013 by Gustafsson et al. Patients who had mechanical bowel preparation did have fewer abscesses after anastomotic leak than those who did not (0. Other complications, such as fascial dehiscence, superficial infection, and mortality, did not differ between groups. These authors concluded that mechanical bowel preparation before elective colorectal surgery can safely be abandoned. Several studies supported these conclusions for left-sided colon and rectal resections as well. All other end points (wound infection, other septic complications, and nonseptic complications) also favored the no-preparation regimen. Finally, the largest and most thorough meta-analysis was published by Guenaga et al. They found that rates of anastomotic leakage, although slightly higher in the bowel preparation groups, were not significantly different following either low anterior rectal resections or colonic resections. Rates of secondary complications, such as wound infection and extraabdominal complications, were not different between the two groups. They concluded that there was no statistically significant evidence that patients benefit from mechanical bowel preparation. Based on this robust body of evidence, many surgeons began to reduce their use of bowel preparation prior to colorectal surgery. However, interestingly, new evidence is emerging that mechanical bowel preparation with oral antibiotic administration is beneficial prior to elective colorectal surgery. In almost all of the trials mentioned previously, oral antibiotics were not included as part of the mechanical bowel preparation pathway. Many investigators believe that the benefit from bowel preparation stems from the delivery of the oral antibiotics to the colon lumen and mucosa, a process that is enhanced by the mechanical colon cleanse. In light of these concerns regarding the existing bowel preparation literature, a new series of studies have been published evaluating the efficacy of bowel preparations that include oral antibiotics. The results of these studies, which are discussed in more detail later, indicate that, although mechanical preparation alone may not be of benefit, mechanical preparation with oral antibiotics is beneficial in reducing surgical site infection and anastomotic leak following colorectal surgery. These authors found that patients receiving full preparation were less likely to have any surgical site infection (5. They were also less likely to develop postoperative Clostridium difficile colitis (0.
Order secnidazole with american express
Treatment includes a high-residue diet symptoms 8 days post 5 day transfer order online secnidazole, and follow-up endoscopy is performed to confirm complete healing and exclude alternative diagnosis. Management of Irreversible Acute and Subacute Ischemia Acute signs of clinical deterioration during the period of observation (rising temperature, elevated white blood cell count, worsening metabolic acidosis, hemodynamic instability, or peritonitis) suggest colonic infarction and are an indication for operative intervention. Patients with persistent symptoms, such as diarrhea, rectal bleeding, or recurrent sepsis, for more than 10 to 14 days may require operative intervention. Benefits of diagnostic colonoscopy include the ability to make the diagnosis of colonic ischemia visually based on direct observation of affected tissue, as well as obtain tissue samples via biopsy. Colonoscopic findings not specific to colonic ischemia include segmental erythema, edema, friability, superficial or deep ulcerations, luminal narrowing, and intraluminal blood. Dusky, cyanotic mucosa is highly suggestive of gangrene and warrants operative intervention. Colonoscopy should be performed cautiously in the setting of colonic ischemia to decrease the risk of perforation. Carbon dioxide may be superior to room air because it is rapidly absorbed from the colon, thus theoretically decreasing the duration of distention and elevation of intraluminal pressure. Biopsies should be obtained, except in the case of gangrene, to rule out alternative diagnoses. Histology of biopsies from hemorrhagic nodules or bullae typically demonstrates submucosal hemorrhage, whereas biopsies of the surrounding mucosa usually show nonspecific inflammatory changes. As in all resections for colonic ischemia, the specimen must be opened at the time of surgery to ensure normal mucosa at the margins. If at the time of surgery the segmental colitis is found to involve the rectum, a mucous fistula or Hartmann procedure with an end colostomy should be performed. Simultaneous proctocolectomy is rarely indicated but should be performed for gangrene of the rectum. This form of colonic ischemia may frequently be misdiagnosed if not seen during the acute episode. Barium enema studies may show a segmental colitis pattern, a stricture simulating a carcinoma, or even an area of pseudopolyposis. The clinical course of chronic colonic ischemia may be difficult to distinguish from other causes of colitis or stenosis, unless the diagnosis was made during the acute episode. Crypt abscesses and pseudopolyposis, generally considered histologically diagnostic of ulcerative colitis, can also be seen in ischemic colitis. Regardless, de novo occurrence of a segmental area of colitis with stricture in an older patient is most likely ischemic. Elective bowel resection is indicated for patients with chronic segmental colonic ischemia and recurrent episodes of sepsis. The underlying etiology of these septic episodes is likely bacterial translocation from areas of unhealed segmental colitis. Management of Ischemic Strictures Stenosis or stricture of the colon may develop in patients with colonic ischemia. Strictures that produce no symptoms should be observed, and some of them will return to normal over a 12- to 24-month period with no further therapy. Endoscopic dilation of chronic colonic strictures as a result of ischemia is generally not recommended. Management of Specific Clinical Problems Colonic Ischemia Complicating Abdominal Aortic Surgery. Mesenteric arterial reconstruction is not indicated in most cases of abdominal aortic surgery, but it should always be considered to prevent colonic ischemia during an open reconstruction for abdominal aortic aneurysm (aneurysmectomy). After elective open aneurysmectomy, colonoscopic evidence of colonic ischemia is present in 3% to 7% of patients. The most important aspect of management of colonic ischemia after aortic surgery is its prevention. If these collateral pathways are intact, postoperative colonic ischemia can be minimized. In this figure, the inferior mesenteric artery is also occluded, so rectal blood flow is dependent on collateral flow from the superior mesenteric artery via the arch of Riolan and the marginal artery and then via the superior rectal vessel to the middle and inferior rectal arteries. At surgery, aortic cross-clamp time should be minimized, and hypotension must be avoided. The difficulty in accurately assessing colonic ischemia after surgery and the significant mortality rates associated with its occurrence mandate that postoperative colonoscopy be performed in high-risk patients. In these cases, colonoscopy needs to be performed postoperatively, and if colonic ischemia is identified, appropriate therapy is begun before major complications develop. Moreover, most patients who undergo open abdominal aortic reconstruction mobilize retained fluid acquired during operation 36 to 72 hours after operation. Thus, in the absence of worsening renal function or infection, the need for fluid or retention of fluid at this point is another harbinger of possible colonic ischemia. Clinical deterioration indicating progression of the ischemic insult to transmural necrosis necessitates reoperation. Primary anastomosis is contraindicated because of potential contamination of the aortic prosthesis in the event of an anastomotic leak. Every effort should be made to protect the aortic graft from contamination; as such, the retroperitoneum overlying the graft should be reperitonealized with retroperitoneal tissues or omentum. Other significant predictors of postoperative colonic ischemia are need for transfusion, renal failure, diabetes, proximal extension of the aneurysm, and female gender, not unlike the risk factors seen in open surgery. A rare form of colonic ischemia involving all or most of the colon and rectum has been identified in a few patients. These patients experience the sudden onset of a toxic pancolitis manifested by bleeding, fever, severe diarrhea, and abdominal pain with or without peritonitis. Management of this condition is similar to that for other forms of fulminant colitis. The histologic appearance of the resected colon is a combination of ischemic changes, severe ulcerations, and necrosis. Acute ischemic colitis in patients with carcinoma of the colon has been recognized for many years. Clinically, patients may have symptoms of colonic ischemia or symptoms related to the primary cancer. However, in most cases the predominant complaints are related to the ischemic episode-sudden onset of mild to moderate abdominal pain, fever, bloody diarrhea, and abdominal tenderness. It is imperative to be aware of the frequent association of colonic ischemia and colon cancer. In addition, during colectomy for carcinoma, examination of colonic resection margins for signs of ischemia is critical because poor blood flow at the anastomosis may result in stricture or leak. Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. Validation of a clinical prediction rule for severe acute lower intestinal bleeding. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Acute lower gastrointestinal bleeding in 1,112 patients admitted to an urban emergency medical center. Proton pump inhibitors: effective first-line treatment for management of dyspepsia. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. Angiodysplasia- an uncommon cause of colonic bleeding: colonoscopic evaluation of 1050 patients with rectal bleeding and anaemia. The role of colonoscopy and radiological procedures in the management of acute lower intestinal bleeding. Scintigraphic detection of gastrointestinal bleeding: a review of current methods.
Order secnidazole online now
In short symptoms cervical cancer buy cheap secnidazole 500mg online, the surgeon must adapt surgical principles to treating "the patient [who has], in most cases, lost more blood than the system could conveniently spare. Except for those caused by therapeutic or erotic misadventures via natural orifice, isolated blunt colon injuries rarely occur. In a survey of more than 200,000 blunt trauma patients, less than a third of the 1% of patients with a hollow viscus injury had colorectal involvement. The cecum, sigmoid, and transverse colon are the most common sites of injury in blunt trauma, but mesenteric avulsion, full-thickness laceration, transection, and devascularization are seen most commonly in the ascending and descending colon. Notably, this occurred in conjunction with advances in evacuation, fluid resuscitation, the availability of banked blood, and antibiotics. Patients with an appropriate history of injury found to have peritonitis or unstable vital signs rarely profit from additional diagnostic procedures not performed in the operating room. Promptly addressing colon injuries is paramount to minimize morbidity and mortality. Delay in diagnosis for blunt injury greater than 5 hours is an independent risk factor for mortality,9 as is delay to operation with penetrating injury. Peritoneal free fluid may be from normal female physiology, preexisting ascites, transudate secondary to resuscitation, or blood from solid visceral or mesenteric injury, as well as from enteric spillage. The lack of free peritoneal fluid, however, has a high negative predictive value for bowel injury. Recognition of the need to break the "trauma triad of death"-the downward spiral of coagulopathy, hypothermia, and acidosis contributing to deteriorating physiology43-changed the conventional operative approach of attempting definitive repair in favor of abbreviated laparotomy. This paradigm shift to prioritize physiology over anatomy is the standard of care for trauma and myriad emergency surgical situations. Hemorrhage is quickly cleared and controlled to allow brisk intraperitoneal exploration. Once bleeding is controlled and while intravascular volume is being restored, attention is turned to contamination. Coloenteric spillage should be attended to rapidly with initial clamping, temporary suture, ligation with umbilical tapes, or stapling devices. Depending on the physiologic status of the patient, definitive suture control or resection is undertaken as deemed prudent. The return for definitive operation generally occurs between 24 and 48 hours and hopefully finds the patient in a clinical and metabolic state permitting reconstruction. Restoring enteric continuity with delayed anastomosis, diversion, or additional resection can then be performed in less-hurried circumstances. In the event that physiology still precludes complete resolution, the abdominal closure is again temporized with the same plan: return once stable. It remains uncertain, however, if these relate to the open abdomen or are epiphenomenal to the severity of injury necessitating the technique. Predicting patients who might avoid complication by fecal diversion remains difficult, as the complication rate even with colostomy remains high and is likely a proxy for injury severity and comorbidity. Myriad algorithms have been suggested to simplify this process, resulting in three primary paths of treatment. Regardless of treatment method, all patients with suspected colonic perforation should receive immediate antibiotic coverage continued for 24 hours or less, as there is no utility in longer coverage without cause. There remains an unsubstantiated fear of anastomotic leaks and other complications with primary repair; a review of 6817 patients with primary colon injury found that only 9% underwent diversion and, indicative of the severity of injury, the patients managed with stoma formation had a mortality rate almost twice that of patients managed without diversion. While uncommonly needed, colostomy and diverting ileostomy remain important and often lifesaving techniques in selected patients with complex injuries. Although operative exposure has historically revolved around laparotomy, depending on circumstance, laparoscopy may be considered. Sources have reported missed injury rates in laparoscopy up to 4%,65,66 but this is balanced by the ability to reduce nontherapeutic laparotomies dramatically, with rates as low as 0% when laparoscopy was used in penetrating abdominal trauma. If there is any question as to the adequacy of exposure or completeness of laparoscopic evaluation, conversion to an open approach is mandatory. Once the peritoneum is entered, evaluation centers upon control of life-threatening hemorrhage and only secondarily is contamination considered. This allows for identification and treatment of great vessel injury, which a four-quadrant approach generally neglects in favor of the potential for pelvic or solid organ hemorrhage. Given the rarity of isolated colonic injury as the impetus for exploration, the recognition of associated injuries is important. In the setting of penetrating trauma, there is an obvious advantage for the close evaluation of organs near the wound path, but much broader suspicion is required in blunt trauma due to the risk for remote multiorgan injury. Air or feculent staining under an omental or peritoneal layer may be the only finding in some cases, but should trigger a thorough evaluation. The surgeon should not hesitate to mobilize the colon along standard anatomic planes to visualize potential injury. Concerning hematomas must be explored to rule out potentially lethal occult perforation. The splenic flexure, because of its redundancy and multiple tethering attachments, is prone to missed injury and should be fully mobilized for inspection if there is concern. Similarly, the extraperitoneal rectal surfaces should be mobilized along the lateral peritoneum if there is suspicion of injury. In penetrating injuries, the rule of two-as entrance wounds generally have exit wounds-should lead to a search for missed injury if an odd number of wounds is encountered. The surgeon should be able to trace the injury from its entrance into the peritoneal cavity to its conclusion. The inability to do so must be regarded as a missed injury until proven otherwise. Multiple projectiles demand even more minute attention to avoid missing inconspicuous injuries. Whereas penetrating injuries have defined trajectories, blunt traumas typically have no such apparent injury pathways. The more diffuse distribution of energy with blunt mechanism mandates a careful, systematic evaluation of the entire colon. Small areas of partial-thickness disruptions may be imbricated, but larger areas are best resected to avoid the complications of delayed full-thickness necrosis. Adjacent throughand-through perforations are generally best managed by excising the contused segment between the wounds and converting it to a single perforation. Formal resection and reanastomosis is generally wise for destructive injuries, especially if there is any question about vascular supply. While ardent supporters in both camps cite appropriate literature, the choice of hand-sewn versus stapled anastomoses should be left to the experience and comfort level of the surgeon. The colon can be left in discontinuity for up to 3 days to allow for reassessment of viability and a delayed definitive operation. Avoiding an initial stoma-and the accompanying potential complications of difficult abdominal wound closure and the risk of worsening bowel and abdominal wall edema that create possible ischemic limb compromise-must be tempered by the approaching and inevitable mesenteric shortening and visceral block. Once hemorrhage is mitigated and contamination is controlled, more definitive vascular investigation may proceed. If an unnamed mesenteric vessel is injured and compromises the viability of a segment of colon, ligate the vessel and resect the affected bowel. Mesenteric injury in the ileocolic and splenic flexure watershed regions should be viewed suspiciously and resection carried back to well-vascularized tissue, unless a second look to reassess viability is planned. Injuries to the superior mesenteric artery within the first, second, or third portions should never be ligated, due to the near-certain bowel ischemia and necrosis. Similar options exist for injuries to the superior mesenteric vein, dependent on injury burden. Relatively few reports discuss inferior mesenteric artery or vein injury-while less common, therapeutic embolization has also been suggested. One must be cognizant of the course of the ureters, iliac vessels, urinary bladder, and both male and female anatomies. Most of these structures lie anteriorly, so it is safest to approach this region posteriorly. Avoiding the presacral fascia prevents disruption of presacral veins and pelvic autonomic nerves entering the pelvic side walls, but eventually wrapping anterior to be in proximity with anterior rectum at the level of the prostate or upper vagina. Surgical Treatment of Anorectal Injuries Anorectal traumas markedly differ from colonic traumas. For civilian injuries, evidence does not support distal rectal washout,78,79 and it is thought that loose stool may contaminate other spaces.
Cheap secnidazole amex
The amnion is a large sac containing amniotic fluid in which the fetus is suspended by its umbilical cord medicine dictionary prescription drugs order secnidazole. The fluid (1) absorbs jolts, (2) allows for fetal movements, and (3) prevents adherence of the embryo to surrounding tissues. The fetus swallows amniotic fluid, which is absorbed through its gut and cleared by the placenta. An excessive amount of amniotic fluid (hydramnios) is associated with anencephaly and esophageal atresia, whereas an insufficient amount (oligohydramnios) is related to renal agenesis. The umbilical cord, surrounded by the amnion, contains (1) two umbilical arteries, (2) one umbilical vein, and (3) Wharton jelly, which serves as a protective cushion for the vessels. Two thirds of twins are dizygotic, or fraternal; they have two amnions, two chorions, and two placentas, which sometimes are fused. In cases of conjoined twins, in which the fetuses are not entirely split from each other, there is one amnion, one chorion, and one placenta. Signals initiating parturition (birth) are not clear, but preparation for labor usually begins between 34 and 38 weeks. Labor itself consists of three stages: (1) effacement and dilatation of the cervix, (2) delivery of the fetus, and (3) delivery of the placenta and fetal membranes. Note the changed relations septum transversum, pericardial cavity, heart tube, and cloacal membrane Table 12: Arrangement of important structures of embryo before and after the folding in craniocaudal direction Before folding of embryo Septum transversum lies cranial to the pericardial cavity and heart tube Heart tube lies below the pericardial cavity Prochordal plate After folding of embryo Septum transversum lies caudal to the pericardia[cavity and heart tube Heart tube lies above the pericardial cavity. It contains the allantois and umbilical vessels and will be incorporated into the umbilical cord with the yolk sac (vitelline) stalk (duct). Cotyledons are the compartments (15 to 20) in the placenta formed when decidual septa grow into the intervillous spaces. These septa never reach the chorionic plate so that there is communication between cotyledons. High Yield Points Amniochorionic membrane is formed when expansion of the amniotic cavity obliterates the chorionic cavity causing the amnion to contact the chorion and the two to fuse. Chorionic cavity is the space formed between the extraembryonic mesoderm lining the cytotrophoblast (somatic extraembryonic mesoderm) and that surrounding the yolk sac and embryo (splanchnic extraembryonic mesoderm). The chorionic cavity will eventually be obliterated by expansion of the amniotic cavity and fusion of the amnion with the chorion. Villous chorion formation goes through three stages: primary chorionic villi, secondary chorionic villi, and tertiary chorionic villi. Components Maternal component of the placenta consists of: Decidua basalis, which is derived from the endometrium of the uterus located between the blastocyst and the myometrium. Decidua basalis and decidua parietalis (which includes all portions of the endometrium other than the site of implantation) are shed as part of the after birth. Decidua capsularis, the portion of endometrium that covers the blastocyst and separates it from the uterine cavity, becomes attenuated and degenerates at week 22 of development because of a reduced blood supply. It is in contrast to an area of no villus development known as the smooth chorion (which is related to the decidua capsularis). Fetal surface of the placenta is characterized by the well-vascularized chorionic plate containing the chorionic (fetal) blood vessels. Placental membrane In early pregnancy, the placental membrane consists of the syncytiotrophoblast, cytotrophoblast (Langerhans cells), connective tissue, and endothelium of the fetal capillaries. Hofbauer cells are found in the connective tissue and are most likely macrophages. In late pregnancy, the cytotrophoblast degenerates, and the connective tissue is displaced by the growth of fetal capillaries, leaving the syncytiotrophoblast and the fetal capillary endothelium. The allantois is not functional in humans and degenerates to form the median umbilical ligament in the adult. As the amnion expands, it pushes the vitelline duct, connecting stalk, and allantois together to form the primitive umbilical cord. The right and left umbilical arteries carry deoxygenated blood from the fetus to the placenta. Dizygotic (fraternal) twins are more common and result when two eggs are independently fertilized by two different sperms and are implanted in the uterus wall at the same time. Monozygotic (identical twins) occur when a single egg is fertilized to form one zygote (hence, "monozygotic") which then divides into two separate embryos. Aortic arch branch from the aortic sac to the dorsal aorta traveling in the center of each pharyngeal arch. Initially, there are five pairs, but these undergo considerable remodelling to form definitive vascular Patterns for the head and neck, aorta, and pulmonary circulation. In the rest of the body, the arterial Patterns develop mainly from the right and left dorsal aortae. The right and left dorsal aortae fuse to form the dorsal aorta, which then sprouts posterolateral arteries, lateral arteries, and ventral arteries (vitelline and umbilical). Aortic arch derivatives Dorsal aorta Embryology Aortic arch artery Adult derivative 1. Maxillary artery (portion of) Stapedial and hyoid arteries (portion of) Right and left common carotid artery (portion of) Right and left internal carotid artery (portion of) Right side: Proximal part of right subclavian artery Left side: Arch of aorta (portion of) Regresses Right and left pulmonary arteries (portion of) Ductus arteriosus** *External carotid artery is a de-novo branch: **Right regresses; left is left. Later on the right side, the distal part of aortic arch 6 regresses, and the right recurrent laryngeal nerve moves up to hook around the right subclavian artery. On the left side, aortic arch 6 persists as the ductus arteriosus (or ligamentum arteriosus in the adult); the left recurrent laryngeal nerve remains hooked around the ductus arteriosus. It happens due to disappearance of Right fourth aortic arch and proximal portion of right dorsal aorta. In this case the right subclavian artery is formed by distal portion of right dorsal aorta and right intersegmental subclavian artery (A). Abnormal subclavian artery crosses the midline behind esophagus and trachea creating a vascular ring around them (B). It leads to formation of double aortic arch, which forms vascular ring around trachea and esophagus and may cause compression. Since this abnormal artery crosses the midline behind esophagus and trachea, a vascular ring is formed by right subclavian artery and aortic arch, which may compress the two visceral tubes. Normally, right subclavian artery is contributed by (proximal to distal): Right fourth arch artery, right dorsal aorta and right seventh cervical intersegmental artery. Three systems can be recognized: (1) the vitelline system, which develops into the portal system; (2) the cardinal system, which forms the caval system; and (3) the umbilical system, which degenerates after birth. When this does not happen, the coronary sinus is absent, and the persistent left superior vena cava drains directly into the atrium. Internal jugular vein: It develops from anterior cardinal vein cephalic to the opening of the subclavian vein. Subclavian vein: It develops in the region of the upper limb bud by enlargement of the intersegmental veins in this region. Right brachiocephalic vein: It develops from right anterior cardinal vein above the opening of oblique communicating channel and below the opening of the right subclavian vein. Left brachiocephalic vein: It develops from oblique channel connecting left and right anterior cardinal veins, and left anterior cardinal vein between the opening of communicating channel (vide supra) and left subclavian vein. The first part develops from the right anterior cardinal vein caudal to the oblique transverse anastomosis. As the right common cardinal vein opens into the right horn of sinus venosus, the superior vena cava at first opens into the right horn of sinus venosus. As and when the right horn of sinus venosus is absorbed into the right atrium, the superior vena cava finally opens into the right atrium.