Order 80 mg super levitra with amex
Clinically erectile dysfunction doctor mn purchase 80 mg super levitra fast delivery, malignancy can be suspected when a sudden increase in size or the onset of pain is noticed at the site of an osteochondroma. Destruction of the base or adjacent bone is a clear-cut sign of malignancy of high histologic grade. The malignancies associated with solitary osteochondromas are typically low-grade conventional chondrosarcomas. The pathologic criteria for diagnosis of low-grade chondrosarcoma arising in osteochondroma are based on gross (thickness of the cap) and microscopic features. Increased thickness of the cartilage cap with the formation of discrete, grossly detectable peripheral nodules that may extend outside the fibrous perichondrium is present in the majority of typical cases. Microscopically, the proliferating nodular areas show increased cellularity and clustering of plump chondrocytes that contain enlarged nuclei with an open chromatin structure. Rare examples of dedifferentiated chondrosarcomas associated with osteochondroma have been described. In such instances, the most aggressive component of the lesion with features of malignant fibrous histiocytoma or osteosarcoma can dominate the radiographic and clinical presentation. A, Anteroposterior radiograph of pelvis shows large peripheral chondrosarcoma arising in a cap of an osteochondroma. C, Axial computed tomogram shows large, calcified, soft tissue mass on external surface of ilium. Microscopic islands of secondary low-grade chondrosarcoma were present focally in the cartilage cap of this radiation-induced osteochondroma. Inset, Axial computed tomogram of pelvis showing a calcified mass arising in osteochondroma. C, T1-weighted coronal magnetic resonance image of the case shown in B documenting a lobulated mass representing a chondrosarcoma arising in an osteochondroma of the ischium. A, Anteroposterior radiograph showing a large calcified mass of the right ilium representing a chondrosarcoma arising in an osteochondroma. Note a calcified mass attached to the base of osteochondroma representing a secondary chondrosarcoma. C, Bisected resection specimen showing a large cartilaginous mass associated with a sessile osteochondroma of the ilium. A, Oblique radiograph of pelvis showing a calcified mass arising in the osteochondroma of the right iliac crest. B, T2-weighted coronal magnetic resonance image showing signal enhancement in a cartilage mass associated with an osteochondroma of the right iliac crest. C, Bisected resected specimen showing a cartilage mass associated with an osteochondroma. A-D, Hypercellular hyaline cartilage mass on the surface of osteochondroma consistent with a secondary chondrosarcoma. A-D, Hypercellular cartilage with atypical cartilage cells consistent with a secondary chondrosarcoma associated with osteochondroma. Bonnevialle P, Mansat M, Durroux R, et al: Chondromas of the hand: a report of 35 cases. Gunawan B, Weber M, Bergmann F, et al: Clonal chromosome abnormalities in enchondromas and chondrosarcomas. Matysiakiewicz J, Tomasik P, Miszczyk L, et al: Manifestations, diagnosis and surgical treatment of enchondroma-own experience. Morii T, Mochizuki K, Tajima T, et al: Treatment outcome of enchondroma by simple curettage without augmentation. Schajowicz F: Tumors and tumorlike lesions of bone, ed 2, Berlin, 1994, Springer-Verlag. Hagiwara Y, Hatori M, Abe A, et al: Periosteal chondroma of the fifth toe-a case report. Inoue S, Fujino S, Kontani K, et al: Periosteal chondroma of the rib: report of two cases. Karabakhtsian R, Heller D, Hameed M, et al: Periosteal chondroma of the rib-report of a case and literature review. Lisanti M, Buongiorno L, Bonnicoli E, et al: Periosteal chondroma of the proximal radius: a case report. Luevitoonvechkij S, Arphornchayanon O, Leerapun T, et al: Periosteal chondroma of the proximal humerus: a case report and review of the literature. Mandahl N, Mertens F, Willen H, et al: Rearrangement of band q13 on both chromosomes 12 in a periosteal chondroma. Yildirim C, Ynay K, Rodop O, et al: Periosteal chondroma that presented as a subcutaneous mass in the ring finger. Kozlowski K, Brostrom K, Kennedy J, et al: Dysspondyloenchondromatosis in the newborn. Maffucci A: Di un caso di enchondroma et angioma multiplo: contribuzione alla genesi embrionale dei tumori. Spranger J, Kemperdieck H, Bakowski H, et al: Two peculiar types of enchondromatosis. Zack P, Beighton P: Spondyloenchondromatosis: syndromic identity and evolution of the phenotype. Wang P, Dong Q, Zhang C, et al: Mutations in isocitrate dehydrogenase 1 and 2 occur frequently in intrahepatic cholangiocarcinomas and share hypermethylation targets with gliobastomas. Evidence of mitogenic neurotransmitters present in enchondromas and soft tissue hemangiomas. Aigner T, Loos S, Inwards C, et al: Chondroblastoma is an osteoid-forming, but not cartilage-forming neoplasm. Akai M, Tateishi A, Machinami R, et al: Chondroblastoma of the sacrum: a case report. Azorin D, Gonzalez-Mediero I, Colmenero I, et al: Diaphyseal chondroblastoma in a long bone: first report. Edel G, Ueda Y, Nakanishi J, et al: Chondroblastoma of bone: a clinical, radiological, light and immunohistochemical study. Fadda M, Manunta A, Rinonapoli G, et al: Ultrastructural appearance of chondroblastoma. Mii Y, Miyauchi Y, Morishita T, et al: Ultrastructural cytochemical demonstration of proteoglycans and calcium in the extracellular matrix of chondroblastomas. Ozkoc G, Gonlusen G, Ozalay M, et al: Giant chondroblastoma of the scapula with pulmonary metastases. Romeo S, Szyhai K, Nishimori I, et al: A balanced t(5;17) (p15;q22-23) in chondroblastoma: frequency of the rearrangement and analysis of the candidate genes. Sailhan F, Chotel F, Parot R, et al: Chondroblastoma of bone in a pediatric population. Schajowicz F, Gallardo H: Epiphyseal chondroblastoma of bone: a clinicopathological study of 69 cases. Sjogren H, Orndal C, Tingby O, et al: Cytogenetic and spectral karyotype analyses of benign and malignant cartilage tumours. Sotelo-Avila C, Sundaram M, Kyriakos M, et al: Case report 373: diametaphyseal chondroblastoma of the upper portion of the left femur. Ishida T, Goto T, Motoi N, et al: Intracortical chondroblastoma mimicking intra-articular osteoid osteoma. Kaneko H, Kitoh H, Wasa J, et al: Chondroblastoma of the femoral neck as a cause of hip synovitis. Karabela-Bouropoulou V, Markaki S, Prevedorou D, et al: A combined immunohistochemical and histochemical approach on the differential diagnosis of giant cell epiphyseal neoplasms. Kirchhoff C, Buhmann S, Mussack T, et al: Aggressive scapular chondroblastoma with secondary metastasis-a case report and review of literature. Konishi E, Nakashima Y, Iwasa Y, et al: Immunohistochemical analysis for Sox9 reveals the cartilaginous character of chondroblastoma and chondromyxoid fibroma of the bone. Kunze E, Graewe T, Peitsch E: Histology and biology of metastatic chondroblastoma: report of a case with a review of the literature. Lehner B, Witte D, Weiss S: Clinical and radiological long-term results after operative treatment of chondroblastoma.
Buy genuine super levitra on-line
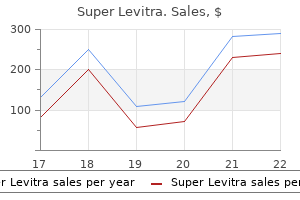
The first one and most common postulates that these tumors represent a common pattern of progression similar to many mesenchymal neoplasms irrespective of their original lineage differentiation erectile dysfunction in the military discount super levitra 80mg overnight delivery. The second theme postulates that malignant fibrous histiocytoma is not a result of dedifferentiation but develops de novo by transformation of mesenchymal stem cells. Using these approaches several mesenchymal differentiation patterns can at least be focally detected in many malignant fibrous histiocytomas to subclassify them as myogenic, myoepithelial, myofibroblastic, lipoblastic, and osteoblastic subtypes. Definition Malignant fibrous histiocytoma is a malignant neoplasm characterized by a mixture of spindle and pleomorphic cells with a prominent storiform arrangement of the spindle cells. These neoplasms in bone formerly were classified as high-grade, pleomorphic, undifferentiated osteosarcomas or high-grade fibrosarcomas. Incidence and Location Malignant fibrous histiocytoma of bone is relatively rare and makes up less than 2% of all primary malignant bone tumors. Malignant fibrous histiocytoma has a predilection for the major long tubular bones, and the femur is most frequently involved. Approximately 30% of cases occur in the knee area with involvement of the distal femoral and proximal tibial metaphyses. Individual cases are reported in other parts of the skeleton, and almost any bone can be involved. It also arises as a dedifferentiation of such low-grade preexisting bone tumors as chondrosarcoma, paraosteal osteosarcoma, low-grade intraosseous osteosarcoma, and giant cell tumor. In addition, a rare autosomal dominant familial syndrome known as diaphyseal medullary stenosis predisposes to the development of malignant fibrous histiocytoma. It is estimated that approximately 30% of patients affected by this syndrome develop malignant fibrous histiocytoma. Radiographically, it is characterized by diffuse diaphyseal medullary stenosis with the overlying cortex showing extensive thickening. Peak age incidence and frequent sites of skeletal involvement in fibrous histiocytoma. National Cancer Institute Surveillance Epidemiology, and End Result Program, 1973-2005. Age-adjusted incidence rate and age-specific frequency, all races, both sexes, 1277 cases. The lesion most frequently involves the metaphyseal parts of long tubular bones and may extend into the epiphysis. The tumor exhibits a geographically destructive growth pattern, but motheaten or permeative patterns also have been described. Typically, there is little or no periosteal new bone formation associated with the tumor. Cortical disruption with poorly demarcated infiltration of the adjacent soft tissue is frequently seen. In more differentiated spindle-cell areas, the tumor can form thick fibrillar deposits surrounding individual cells that mimic osteoid. This feature accounts for earlier inclusion of these tumors in the group of osteosarcomas. The most distinct feature of these tumors is the storiform arrangement of spindle cells, which is present focally in most cases. Angiomatoid malignant fibrous histiocytoma has recently been reclassified and is no longer considered a variant of malignant fibrous histiocytoma on the basis of its distinct pathologic and clinical features. The most frequent types of malignant fibrous histiocytoma in bone are the storiform-pleomorphic and giant cell variants. These designations are descriptive and do not necessarily imply distinct pathogeneses or differences in clinical behavior. The storiform-pleomorphic variant represents a prototype pattern of malignant fibrous histiocytoma. Areas with less differentiated spindle cells exhibit prominent nuclear atypia and brisk mitotic activity. Mononuclear cells with abundant cytoplasm that resemble histiocytes containing pleomorphic, highly atypical nuclei represent undifferentiated mesenchymal components. Giant cells of both the malignant type and the benign osteoclastic type are present. The cytoplasm of these cells is usually densely eosinophilic and can be responsible for superficial mimicry of pleomorphic rhabdomyoblasts. On the other hand, vacuolar change of the cytoplasm can mimic lipoblastic differentiation. Foci of necrosis, scattered foamy histiocytes, and inflammatory cells are frequently present. The presence of numerous multinucleated, osteoclastlike giant cells is a frequent feature of malignant fibrous histiocytoma of bone. The data suggest that predominantly fibroblastic tumors with minimal atypia have a better prognosis than highly atypical lesions. Convincing clinical data supporting the relationship between clinical behavior and complex histologic grading in these tumors are lacking for bone lesions. Nevertheless, modern combined-modality treatment protocols require subdivision of these tumors and other sarcomas into low and high grades. Special Techniques Immunohistochemistry plays little direct role in the diagnosis of malignant fibrous histiocytoma. It is used predominantly to exclude other malignant neoplasms considered in the differential diagnosis. Other markers, such as keratin, S-100 protein, and desmin, are predominantly used to rule out other primary and metastatic neoplasms of bone. A, Lateral radiograph of distal femur of a 28-year-old man with large lytic tumor in shaft with wide zone of transition and anterior cortical destruction. Inset, Axial computed tomogram shows permeative bone destruction and extension into soft tissue. Ill-defined permeative destruction is present in distal metaphysis without associated cortical destruction or periosteal reaction. A, Anteroposterior radiograph showing a destructive permeative lesion involving periacetabular region extending to ischium and pubic ramus. B, Axial computed tomogram of same case as A showing a destructive lesion of the left pelvis with soft tissue extension. C, T1-weighted axial magnetic resonance image of case in A and B showing extensive low density tumor involving the left pelvis and adjacent soft tissue. A, Anteroposterior radiograph showing a destructive moth-eaten lesion of the proximal humerus. B, Fat-saturated T2-weighted coronal magnetic resonance image showing a high signal intensity lesion of the proximal humerus. C and D, Gross photomicrographs of bisected resection specimen showing an intramedullary tumor of the proximal humerus with mixed fleshy and mucinous appearance. B, Intramedullary fleshy tumor of proximal humerus with soft tissue extension and elevation of periosteum seen medially. C, Fleshy intramedullary tumor of the proximal tibia fused with the overlaying cortex. A, Fleshy intramedullary tumor of distal femur with cystic changes and hemorrhage proximally. B, Circumferential soft tissue extension of distal femur with extensive necrosis and multifocal hemorrhage grossly mimicking telangiectatic osteosarcoma. D, Destructive fleshy mass with cortical disruption and soft tissue extension of distal tibia end. A and B, Low and intermediate power views showing plump malignant spindle cells with brisk mitotic activity. A and B, Intermediate and high power views of pleomorphic tumor with scattered multinucleated giant cells with osteoclast-like features. C and D, Low and intermediate power views of a spindle-cell tumor with a somewhat parallel arrangement of cells. A and B, Low and intermediate power views of the advancing edge of malignant fibrous histiocytoma permeating the marrow spaces.
Diseases
- Trichorhinophalangeal syndrome type I
- Verminiphobia
- Anophthalmia short stature obesity
- Autoimmune peripheral neuropathy
- Eosinophilic granuloma
- Flesh eating bacteria
- Agammaglobulinemia
Buy generic super levitra 80 mg online
The inactive or mature phase merely shows calcified deposits in a dense fibrous stroma impotence 10 order super levitra online. Differential Diagnosis Similar tumoral calcifications can be found in patients with several underlying metabolic calcium disorders, such as chronic renal disease or secondary hyperparathyroidism. Lesions similar to tumoral calcinosis can occur in patients with primary hyperparathyroidism, hypervitaminosis D, milk-alkali syndrome, and scleroderma. It is recommended that lesions be surgically removed as early as possible, when they are small and amenable to complete excision. The terms chondrocalcinosis and calcium pyrophosphate crystal deposition arthropathy were independently applied to the same condition, which is characterized on radiographs by prominent multifocal calcification in the cartilages of joints and intervertebral disks. The term encompasses pseudogout, chondrocalcinosis, and pyrophosphate arthropathy. A, Lateral radiograph of elbow shows coarse deposits of calcific material in region of olecranon bursa. B, Massive calcinosis in soft tissue around parascapular area and axilla in teenage boy. C, Low power photomicrograph shows circumscribed foci of calcific material with central cystification and peripheral foreignbody giant-cell reaction in tumoral calcinosis. D, Higher power magnification shows calcified bodies and more finely dispersed, noncrystalline calcifications. The temporomandibular joint was involved in three patients, and the metatarsophalangeal joint of the great toe was involved in two patients. Long-standing swelling of the affected area was noted in two patients with temporomandibular joint involvement. Two patients had a painful mass of the great toe, which was clinically considered to be gouty tophus. Rapid, progressive myelopathy at an upper cervical level developed in another patient. One patient was asymptomatic, and the lesion was discovered incidentally on imaging studies done for other reasons. None of the patients in our series had radiographic evidence of chondrocalcinosis or clinical symptoms in any other joints. Gross Findings the lesion is a circumscribed, white-gray mass with a more or less chalky appearance. The chondroid cells can be atypical, with variable nuclear size and shape, and can mimic a malignant cartilage tumor. The calcium pyrophosphate dihydrate crystals are removable by decalcification, and their basophilic features are lost in demineralized sections. Differential Diagnosis the metaplastic chondrocytes found in our series of patients sometimes showed cytologic atypia (three patients) analogous to that seen in some patients with synovial chondromatosis and superficially resembled chondrosarcoma. Particularly in decalcified sections from which calcium pyrophosphate dihydrate crystals are lost, atypical features in metaplastic chondrocytes and the presence of myxoid stroma may lead to the histologic misdiagnosis of chondrosarcoma. Grossly, tophaceous pseudogout is a calcified, chalky mass unlike the calcification seen in chondrosarcoma. More important, however, is the identification by polarized light microscopy of birefringent crystals characteristic of calcium pyrophosphate dihydrate. The exact nature of these crystals can be determined by radiographic diffraction or electron probe analysis. Even in the decalcified sections, empty outlines of crystals in the chondroid matrix can be seen, although birefringent crystals are not identified directly. Synovial chondromatosis and chondromas in soft tissue are the other lesions that can be confused with tophaceous pseudogout, especially in the conditions in which a heavily calcified cartilage matrix may obscure the cartilaginous nature. However, the calcified areas of synovial chondromatosis do not contain the rhomboid crystals characteristic of calcium pyrophosphate dihydrate deposition. Indeed, radiographic diffraction studies in both synovial chondromatosis and chondroma of soft tissue show that the mineral deposits represent hydroxyapatite. Treatment and Behavior Tophaceous pseudogout may recur after complete or incomplete surgical excision. A, Radiograph of right hip shows calcified mass in soft tissue adjacent to acetabular margin; this mass represents deposits of calcium pyrophosphate dihydrate in capsule of hip joint (arrows). B, Computed tomogram of case shown in A demonstrates circumscribed calcification in soft tissue that is adjacent to acetabular labium (arrows). The crystals are short rhomboid or, rarely, needle shaped, similar to urate crystals. A and B, Anteroposterior and lateral radiographs of foot show massive calcification of soft tissue around metatarsophalangeal joint of great toe resulting from localized deposit of calcium pyrophosphate dihydrate crystals. B, Computed tomogram of cervical spine of patient shown in A reveals extradural calcific mass compressing dural sac (arrows). A, Calcified tophaceous deposit from plantar aspect of foot shows whitish chalky appearance similar to that seen in monosodium urate tophus. B, Metaplastic chondroid change surrounds islands of basophilic calcified crystalline calcium pyrophosphate dihydrate. D, Compensated polarization microscopy demonstrates positive birefringence of rhomboid calcium pyrophosphate dihydrate crystals. C, Photomicrograph of decalcified specimen showing lobules of myxoid material corresponding to areas of metaplastic cartilage and crystalline material deposits. D, Higher magnification of C showing an interface between hypercellular stroma and myxoid areas with prominent plump histiocytic cells exhibiting nuclear atypia. This description is restricted to the tophaceous form of gout and the basic microscopic features that are helpful in distinguishing this metabolic disorder from a neoplasm. Clinical Data In general, gout is characterized by hyperuricemia and the deposition of monosodium urate crystals in synovial tissues. It is rare in women, but when it does affect a female patient, the onset of symptoms typically occurs in the postmenopausal period. Approximately 50% of the patients with gouty arthritis have nodular deposition of monosodium urate crystals that are referred to as tophi. Patients who have higher levels of uric acid have a high propensity for the development of tophi. Radiographic Imaging the formation of tophi occurs 3 to 40 years (average, 12 years) after the first attack of gout. The intervening stromal tissue shows histiocytic and multinucleated giant-cell reaction. Clinically, it is characterized by an insidious onset of fever, local swelling, and pain in the affected bones. Microscopically, early lesions contain polymorphonuclear (neutrophilic) leukocytic infiltrate in the marrow. Prominent formation of new reactive bone can be a dominant feature in later phases of the disease. Peculiar granulomas made up of collections of neutrophils surrounded by a rim of epithelioid histiocytes can be present, but there is no caseous necrosis. Results of bacterial, viral, and fungal cultures, as well as special stains for infectious organisms, are consistently negative. Some patients may have associated recurrent skin lesions (pustolosis palmoplantaris). In fact, it is postulated that chronic recurrent multifocal osteomyelitis is a manifestation of the spectrum of disorders characterized by sterile neutrophilic infiltrate primarily in the skin referred to as neutrophilic dermatoses. They include palmoplantar pustulosis, psoriasis, acne fulminans, neutrophilic eccrine hidradenitis, acute febrile netrophilic dermatosis, and pyoderma gangrenosum. Marginal erosions of tarsal bones and metatarsals are sharply outlined and completely radiolucent (arrows).
Generic super levitra 80 mg with visa
Finally cough syrup causes erectile dysfunction purchase super levitra 80mg on line, because their receptors recognize "native" antigens that have not been fragmented and presented, B cells actually are at a disadvantage. After all, there are so many different forms in the human population that most of us inherit genes for six different class I molecules. Such a virus might wipe out the entire human population, because no killer T cells could be activated to destroy virusinfected cells. What must be appreciated, however, is that many pathogens do not infect human cells: They are quite happy living and reproducing outside our cells in our tissues or in our blood. Antigen presenting cells only present antigen efficiently when a battle is going on, and helper T cells are educated not to react against our own proteins. Consequently, both the helper T cell and the antigen presenting cell must "agree" that there has been an invasion before a helper T cell can be activated. By requiring that helper T cells only recognize presented antigen, Mother Nature guarantees that the decision to deploy the potentially deadly adaptive immune system is not made by a single cell. As a result, the number of targets that a helper T cell can "see" during presentation far exceeds those available for viewing in a large, folded protein. So far, however, it is not clear how important lipid presentation is for the immune defense. Consequently, I will "stick to the rule" that T cells only recognize protein antigens. Transplantation studies actually began in the 1930s with experiments involving mouse tumors. In those days, tumors were usually induced by rubbing some horrible chemical on the skin of a mouse, and then waiting for a long time for a tumor to develop. Because it was so much trouble to make these tumors, biologists wanted to keep the tumor cells alive for study after the mouse had died. What they observed, however, was that the tumor cells only could be successfully transplanted when the two mice were from a strain of mice in which there had been a lot of inbreeding. And the more inbred the strain, the better the chance for survival of the transplant. This provided the impetus for the creation of a number of inbred mouse strains that immunologists depend on today. Once inbred mouse strains were available, immunologists began to study the transplantation of normal tissues from one mouse to another. In contrast, when this experiment was tried with mice that were not inbred, the transplanted skin turned white within hours (because the blood supply had been cut off) and invariably died. Immunologists figured this immediate graft rejection must be due to some genetic incompatibility, because it did not occur with inbred mice that have the same genes. To identify the genes that are involved in "tissue compatibility" (histocompatibility), immunologists bred mice to create strains that differed by only a few genes, yet which were still incompatible for tissue transplants. Some of their favorite targets are the cells that make up the blood vessels contained within the donated organ. There they meet up with proteins that have been taken into the cell by phagocytosis and cut up into peptides by enzymes. First, most viral proteins normally remain hidden inside an infected cell and are not found on the cell surface. In addition, because protein folding can hide large portions of a protein from view, chopping a protein up into small peptides reveals many potential T cell targets that would be inaccessible in an intact protein. The most important antigen presenting cell during the initial stages of an attack is the dendritic cell, because this cell can activate virgin T cells. In this way, the dendritic cell effectively takes a snapshot of what is going on at the front, carries it to the place where T cells are plentiful, and then does its "show and tell" thing to activate T cells. Macrophages, activated by danger signals, also can function as antigen presenting cells. Consequently, macrophages are most useful for presenting antigen after the adaptive immune system has been activated. At that time, activated macrophages out in the tissues can keep experienced T cells fired up, prolonging the time that they are effective in dealing with invaders. Consequently, relatively late in the initial infection or early in a subsequent infection by the same attacker, B cells play a major role as antigen presenting cells. Describe the different roles that activated dendritic cells, activated macrophages, and activated B cells play in the presentation of antigen during the course of an infection. During their lifetimes, dendritic antigen presenting cells can be "samplers," "travelers," and "presenters. This requirement helps insure that T cells will spring into action only when there is real danger, and that only useful weapons will be mobilized. Like the heavy and light chains of the B cell receptor, the genes for, and are assembled by mixing and matching gene segments. As the gene segments are mixed and matched, a "competition" ensues from which each T cell emerges with either an or a receptor, but not both. This makes sense because common invaders are attacking our bodies almost continuously, and the weapons of the innate immune system are useful against a wide variety of these "everyday" enemies. In contrast, only about one in a million B or T cells will have receptors that can recognize a given invader. Consequently, it would not be wise to stockpile B or T cells, because in our entire lifetime, we probably will never encounter the invader which a particular B or T cell could defend against. Indeed, an important feature of the adaptive immune system is that its weapons are made on demand: Only those B and T cells whose receptors can recognize the "invader du jour" are mobilized. T cells with receptors are most abundant in areas like the intestine, the uterus, and the tongue, which are in contact with the outside world. Interestingly, mice have lots of T cells in the epidermal layer of their skin, but humans do not. This serves to remind us that so far as the immune system is concerned, humans are not just big mice. Human and mouse lineages diverged roughly 65 million years ago, and humans are relatively large animals that can live for a long time. Consequently, we would predict that, although similar, the immune systems which evolved to protect these two, very different animals would be different. Moreover, the receptors of T cells in the tongue and uterus tend to favor certain gene segments during rearrangement, whereas receptors in the intestine prefer other combinations of gene segments. The thinking here is that, like players on the innate immune system team, T cells stand watch on the "front lines," and have receptors which are "tuned" to recognize invaders that usually enter at certain locations. Traditional T cells are taught in the thymus not to react against our own self peptides, and although T cells also are found in the thymus, nude mice, which lack a functional thymus, still produce functional T cells. In most cases, it also is not known exactly what the receptors on T cells recognize, but it is believed that, like B cells, T cells focus on unpresented antigen. Consequently, it has been postulated that T cells are designed to kill cells that become stressed as the result of a microbial infection. Because much more is known about traditional T cells than about their nontraditional cousins, and because traditional T cells seem to be the ones that are most important for protecting us from disease, we will limit our discussion in this book to T cells of the traditional variety. Normally, this type of signaling across the cell membrane involves a transmembrane protein that has two parts: an external region which binds to a molecule (called a ligand) that is outside the cell, plus an internal region that initiates a biochemical cascade which conveys the "ligand bound" signal to the nucleus. In humans, this signaling complex is made up of four different proteins:, and (gamma, delta, epsilon, and zeta). The whole complex of proteins (,) is transported to the cell surface as a unit. It can send signals that result in very different outcomes, depending on how, when, and where it is triggered. So this same T cell receptor, depending on the situation, signals death, anergy, or activation. In fact, there are now documented cases in which the alteration of a single amino acid in a presented peptide can change the signal from activation to death!
80mg super levitra overnight delivery
Stroma is minimal and confined to few delicate fibrous tissue strands and blood vessels impotence stress order super levitra visa. D, Higher magnification of C shows uniform tumor cells with minimal amount of cytoplasm. Inset, High power photomicrograph of Homer Wright rosette consisting of a central fibrillar core bounded by concentrically arranged tumor cells. Note the presence of apoptotic dark cells at the interphase of viable and necrotic tumor. D, Higher magnification of the interphase between viable and necrotic tumor tissue showing prominent dark apoptotic cells. In a small number of tumors, the microscopic appearance of tumor cells may deviate from the so-called classic pattern. These features are more often seen in recurrent and treated lesions but can also be present in primary tumors. A delicate, finely granular chromatin pattern and clearly identifiable small to medium nucleoli are characteristic. Immunohistochemical and molecular study allowing differential diagnosis with other small cell malignances may be performed on material obtained for cytologic preparations. The cellularity is high, and the tumor cells are densely packed with almost nonexistent stroma. Two types of cells as defined by light microscopy-a principal type (light with open intact chromatin) and a secondary type (dark with condensed chromatin)-can also be recognized at the ultrastructural level. Minimal amounts of stromal elements associated with endothelial-lined capillaries and occasional larger vessels are seen focally. Centrally located nuclei are oval to round and have outlines with occasional indentations of the nuclear membrane. Some intracytoplasmic reticulum and poorly developed small Golgi centers are present. Ultrastructurally, there is a continuous transition from intact principal cells to dark apoptotic cells, and in some areas, the so-called dark cells can predominate. The ultrastructure of the dark cells may show all the features of nuclear condensation and segmentation described for apoptosis. Before the advent of chemotherapy, the prognosis was dismal, with a 5-year survival rate of less than 20%. The use of multimodality treatment plans of irradiation and multidrug chemotherapy plus surgery has significantly changed this survival rate. Those patients who initially have localized, resectable disease and are treated with multidrug chemotherapy in addition to surgery have a 5-year survival rate of approximately 70%. A-D, Fine-needle aspirate containing undifferentiated round cells with occasional nucleoli and indistinct cytoplasm, occasionally forming rosette-like structures (arrows). Inset, Rosettelike structure formed by circumferential arrangement of tumor cells around central core containing delicate fibrillar cytoplasmic material. A and B, Undifferentiated mesenchymal cells containing sparse cytoplasmic organelles and prominent deposits of glycogen. A, Undifferentiated tumor cells containing sparse cytoplasmic organelles and regular round nuclei with freely dispersed chromatin on occasional nucleoli. Similar to osteosarcoma, it has been shown that surgical removal of the resectable lung metastases improves survival. The incidence of disseminated disease at the time of diagnosis is high, and approximately 15% to 28% of patients initially have metastatic disease. Patients who have resectable lesions of the extremity bones have a better survival rate than those who have lesions affecting the trunk bones, such as the pelvis and the thoracopulmonary region. In addition, lesions in the latter sites are significantly larger at presentation and show extensive soft tissue involvement. Extensive spontaneous necrosis of untreated lesions is a predictor of more aggressive clinical behavior and is linked to lower survival rates. Its presence is considered by some authors to be synonymous with invasion into soft tissue and may signify a higher stage and volume of lesions. Favorable response, which is defined as total or subtotal (90% to 100%) necrosis, appears to be a strong predictor of long-term survival. The link between favorable prognosis and good chemotherapy response has been consistently shown in several independent studies. Moreover, the degree of postchemotherapy necrosis seems to correlate with the rate of disease-free survival. In a study from the Rizzoli Institute, the 5-year disease-free survival rate was 90% for patients with complete necrosis, 53% for those with microscopic residual tumors, and 32% for those whose lesions had gross evidence of residual tumor. Immunohistochemical features of overexpression of the genes involved in the development of drug resistance, such as P glycoprotein, show some promising results, but too few cases have been studied to assess the practical application of these findings. These types of rosettes should not be used as sole microscopic evidence of neural differentiation. Sparse neurosecretory granules are associated with both developing Golgi centers and cell processes. In a recent interinstitutional study involving several centers in the United States and Europe, the analysis of 315 cases showed no association between neural differentiation and more aggressive behavior. In the original report, the authors postulated that this lesion had a distinct pathogenesis and apparently arose in the ribs, predominantly in the periosteum, but could also arise in the soft tissue, and possibly within the lung. The lesions are frequently positive for one or several of the so-called neural markers, including neuron-specific enolase and neurofilaments of 70 kD, and may also express neuroendocrine markers such as chromogranin. The unique features seem to be frequent primitive neural or neuroendocrine differentiation, as well as focal epithelial differentiation. A, Tumor cells with sparse cytoplasmic organelles as seen on low power magnification. B, Centrally placed cytoplasmic processes correspond to core of rosette (asterisk). A, Axonal differentiation of tumor cells with formation of interconnecting cytoplasmic processes (arrows). These two antibodies identify the antigen in formalin-fixed, paraffin-embedded tissue. It is also positive in pediatric lymphomas, lymphocytic lymphoma, and occasionally in rhabdomyosarcoma and even synovial sarcoma. Positivity for neuron-specific enolase is generally disregarded as a specific marker of neural differentiation. On the other hand, if its expression can be correlated with other features of neural differentiation, it provides a valuable tool with which to assess the degree of neural phenotypic expression. A, Intermediate power view of small round-cell tumor with sparse stromal elements. Scattered positivity of individual tumor cells for keratins can be seen in approximately 10% of these tumors. In general, the differential diagnosis of small round-cell tumors of bone include not only the entities described in this chapter, but also a variety of mesenchymal and epithelial (primary and metastatic) tumors that may occur in children, adolescents, and adults. It is recommended that rendering such a diagnosis in an unusual clinical setting should be verified by molecular testing. These cytogenetic techniques can be performed on both conventional cytologic preparations and formalin-fixed paraffin-embedded histologic sections. Such tests are typically designed with multiple primers and are capable of detecting several variants of fusion transcripts. However, this approach is not absolutely safe because the technique can generate false-positive results due to primer annealing to alternative nonspecific sequences. Novel emerging approaches that are not yet widely available are based on genome sequencing technologies and are designed to identify all possible fusions using a panel of primers and massive genomic sequencing. Such tests are capable of detecting all translocations in sarcomas and may dominate future molecular testing of sarcomas.
Syndromes
- Complete blood count (CBC)
- You have gastroesophageal reflux disease and aspiration pneumonia (a lung infection caused by breathing the stomach contents into the lungs), a chronic cough, or hoarseness.
- Low blood pressure
- Cough with blood
- Low blood pressure
- Swallowing difficulty (rare)
- Recent insertion of an IUD
Cheap 80 mg super levitra mastercard
The lesion has also decreased in size erectile dysfunction pills in store discount super levitra 80 mg with mastercard, corresponding to a positive response to therapy. B, Two months later, the lesion enhances less uniformly but has enlarged (arrowheads), indicating central necrosis in a progressing lesion that now also involves the adjacent right L4-5 foramen (arrow). Tumor response criteria have been developed to provide a standardized, uniform methodology for determining response in patients undergoing therapy in different clinical trials and at different institutions. Response criteria define the minimal allowable tumor change that constitutes a response and delineate the methods by which change can be measured. Lack of size correlation with successful chemotherapy is a potential pitfall in determining treatment response in primary bone tumors on conventional, anatomic imaging. Nevertheless, some soft tissue sarcomas, such as gastrointestinal stromal tumors, have a tendency to increase in size with successful therapy due to loss of structural integrity. The determination between positive or negative response can be difficult when the lesion increases in central necrosis because this could either be caused by outgrowth of blood supply in a progressing tumor or desired cell death after effective therapy. Typically, the progressing, centrally necrotic lesion will demonstrate stable or increasing soft tissue nodularity along the enhancing rim. Imaging has become an essential tool for evaluating therapeutic response in primary bone tumors. Therapy can be modified based on imaging results, potentially allowing the patient to be changed from ineffective to effective therapeutic agents before surgical resection and histopathologic analysis of the specimen. Bone Metastases Bone sarcomas metastasize most commonly to the lungs but demonstrate a predilection for metastasizing to other bones. C, After chemotherapy, the lesion increased in mineralization but only slightly decreased in size. The functional imaging reflected the histologic response, which included 99% necrosis in the resected specimen. Different imaging modalities demonstrate different physical characteristics of the neoplastic process. Nevertheless, expansile plasmacytomas will develop peripheral mineralization after successful therapy. Tracer uptake on bone scan will typically decrease or increase with healing or progression, respectively. Increasing sclerosis within effectively treated lesions can cause a spurious increase in tracer uptake within the first 3 months of therapy. The majority of bone metastases arise in the medullary cavity, with a small minority arising in the cortex. After successful therapy, T2 signal, T1 signal, and enhancement often diminish while the size of the lesion may or may not diminish. Patients who have undergone resection of their primary tumor and have metastases only to bone could be denied enrollment into clinical trials due to the absence of measurable disease by which to gauge the efficacy of the therapeutic agents. Medical records and patient images were analyzed at 2 to 6 months or 11 to 13 months after the initiation of therapy. Early response identification can allow timely modification of therapeutic regimens, implying that the behavior of bone metastases can be used to guide therapy in these patients. The most common imaging modality used to evaluate for local recurrence is radiography. Serial radiographs are used to restage malignancies and benign tumors with a tendency to recur, such as aneurysmal bone cyst or giant cell tumor of bone (10%-20% recurrence rates with modern therapeutic techniques). Most recurrent primary bone tumors have T1 signal that is isointense to muscle, T2 signal that is high or heterogeneous, and demonstrate internal enhancement after the administration of intravenous contrast. Even tumors that are characteristically cystic or hemorrhagic, such as giant cell tumors, will typically demonstrate foci of nodular enhancement. An exception is aneurysmal bone cyst, which is entirely cystic and enhancement is seen only in the rim. The cystic appearance of recurrent aneurysmal 2 Clinical Considerations and Imaging of Bone Tumors 89 A: 12. Axial computed tomography images of a 24-year-old female with a primary osteosarcoma of the left humerus. Clinic visits, which may or may not include imaging, are typically performed every 6 months for 3 to 5 years for lower grade lesions. For highgrade sarcomas, the patients are followed every 3 months for 2 years, every 4 months for the third year, every 4 to 6 months for the fourth year, and every 6 months for the fifth year. Sarcoma patients are then followed at least once per year for a total of 10 years. The risk of recurrence diminishes with time; the clinical emphasis of later visits shifts to the integrity of the orthopedic reconstruction. Distant Metastases Malignant bone tumors typically metastasize in a predictable fashion, and various imaging studies are used to evaluate the anatomic locations in which metastatic lesions are most likely to occur. Most primary malignant bone tumors are sarcomas and metastasize preferentially to the lungs. B, the lesion was curetted and ablated with hydrogen peroxide, and the cavity was packed with bone graft. A globular area of tracer uptake at the medial aspect of the distal right femur is indeterminate and could be potentially related to the resection arthroplasty. B, Knee radiography was then obtained, and a small focus of osteoid at the area of the area of interest (arrowhead) was indicative of recurrent osteosarcoma. The majority of bone metastases occur in the axial skeleton, although metastases to the extremities are not uncommon. Imaging of the entire skeleton can also aid in the diagnosis of metastases because multiplicity of lesions is common. Bone scan is the most commonly used imaging modality for this indication and is sensitive but not specific for the detection of bony metastases. Conversely, radiography is the initial imaging modality of choice to evaluate a specific area of bone pain in cancer patients at risk for osseous metastases. Advantages over bone scan include increased anatomic resolution and multiorgan system evaluation. A, Bone scan in a 58-year-old breast cancer patient with tracer uptake in the left distal femoral diaphysis that is suspicious for a bone metastasis (arrow). Osteoarthritic changes are incidentally seen at the medial compartment of both knees (arrowheads). The unique strengths of specific imaging modalities are used 2 Clinical Considerations and Imaging of Bone Tumors 93 to perform oncologic staging in the most therapeutically and cost effectively optimal manner. Oncologic imaging can greatly aid the pathologist and other specialists in the care of cancer patients. Kager L, Zoubek A, Kastner U, et al: Skip metastases in osteosarcoma: experience of the Cooperative Osteosarcoma Study Group. Bacci G, Longhi A, Bertoni F, et al: Bone metastases in osteosarcoma patients treated with neoadjuvant or adjuvant chemotherapy: the Rizzoli experience in 52 patients. Shinozaki T, Chigira M, Watanabe H, et al: Osteosarcoma with multiple skeletal metastases. Clinical, biochemical, radiographic, and scintigraphic evaluation of response to therapy. Feldman F, Vanheertum R, Saxena C: 18Fluoro-deoxyglucose positron emission tomography evaluation of benign versus malignant osteochondromas: preliminary observations. Yanagawa T, Watanabe H, Shinozaki T, et al: the natural history of disappearing bone tumours and tumour-like conditions. Ueda T, Naka N, Araki N, et al: Validation of radiographic response evaluation criteria of preoperative chemotherapy for bone and soft tissue sarcomas: Japanese Orthopaedic Association Committee on Musculoskeletal Tumors Cooperative Study.
Order super levitra 80 mg amex
In small anatomic structures (vertebral column erectile dysfunction medications list buy cheap super levitra line, bones of the hands and feet), the lesion may cross a joint space to involve the adjacent bone, providing clear evidence of its local aggressive nature. In some cases, prominent periosteal new bone formation can be present, raising the radiologic suspicion of malignancy. These tumors are likely to recur, do not metastasize, and are characterized microscopically by the presence of so-called epithelioid osteoblasts. Transition to osteosarcoma has not been observed to date, and these rare tumors therefore are not considered to be precursors of conventional osteosarcoma. Incidence and Location this is a very rare tumor, and its true incidence and its age distribution are not exactly known. The original series, reported in 1984, consisted of 15 cases,39 and an update published in 199641 dealt with 21 additional cases of aggressive osteoblastoma. A further 11 cases observed as consultations since 1996 are included in the present chapter. The limited experience with these tumors based on the analyses of 47 cases indicates that they occur in a slightly older group of patients than conventional osteoblastomas. The ages of 47 patients with aggressive osteoblastoma ranged between 7 and 80 years. This indicates that the overall distribution pattern of aggressive osteoblastoma is similar to that of conventional osteoblastoma, with clear predilection for the axial skeleton. The second most frequent location of occurrence is in the small bones of the hands and feet. This distribution pattern is clearly different from that of conventional osteosarcoma, further supporting the close pathogenetic relationship between aggressive osteoblastoma and conventional osteoblastoma. Aside from the personally collected series reported here and based largely on consultation material, the recent literature contains individual case reports of these very rare tumors. Similar to conventional osteoblastoma, it may bleed profusely during curettage because of its rich stromal vasculature. The bone contour can be markedly expanded with a thinned and focally disrupted cortex. Extension into the adjacent soft tissue may be present, often with an encasing shell of reactive bone peripherally. Microscopic Findings Aggressive and conventional osteoblastomas share many of the same microscopic features. The main difference and the most prominent feature of aggressive osteoblastoma is the presence of so-called epithelioid osteoblasts that Text continued on p. A, Ill defined tumor with irregular mineralization pattern and diffuse sclerosis of the adjacent bone involving proximal tibia. B, Mixed lytic and sclerotic tumor with ill defined margins and sclerosis in the adjacent bone of proximal tibia. D, Mixed lytic and sclerotic tumor with ill defined margins involving the medial condyle of femur. A, Radiograph of cervical spine in a 19-year-old man who had pain and paresthesias for 112 years. B, Computed tomogram of case in A shows expanded but well-delimited lesion with focal radiodensities in lateral aspect of vertebra. Although body is involved, lesion appears to originate in lateral and posterior vertebral elements. Patient was a 53-year-old man with 3-week history of back pain radiating to lower extremities. D, Axial section of vertebra shown in A documents eccentric lytic lesion primarily involving vertebral body and extending posteriorly into spinal canal. Patient, a 16-year-old girl, incidentally was found to have osteopoikilosis, which is shown in radiographs of pelvis. B, Lateral view of sacrum shows posteriorly expanded contour of tumor with superimposed aneurysmal bone cyst. C, Computed tomogram reveals expanded lytic lesion with radiopaque delimiting capsule. A, Radiograph of right long finger of a 19-year-old woman shows lytic area of recurrent tumor in middle phalanx. Review of this material and histologic study of recurrence showed aggressive osteoblastoma. C, Sagittally cut amputation specimen shows tumor in middle phalanx that extends into soft tissue on volar aspect. D, Radiograph of thumb metacarpal tumor in a 21-year-old man who had pain and swelling for 5 months. Proximal phalanx shows that bone-forming tumor has caused extensive destruction and has extended into soft tissue. A, Radiograph of a 18-year-old man 3 months before admission shows 5-cm lytic lesion at junction of acetabulum and ramus. B, Large, expanded mass at same site 3 months later is shown in this anteroposterior film. The "blown-out" area of juxtaacetabular bone represents secondary aneurysmal bone cyst superimposed on aggressive osteoblastoma. D, Radioisotope scan shows marked uptake at site of combined bone-forming tumor and secondary aneurysmal bone cyst. A, Anteroposterior radiograph of a 61-year-old woman with 6-month history of increasing left hip pain shows well-circumscribed lytic lesion with central opacity (arrows). B and C, Computed tomograms show lesion adjacent to acetabulum and reactive sclerosis in surrounding bone. D, Specimen radiograph shows multiple areas of patchy density not visible on computed tomogram or plain film. The trabeculae occasionally appear wider and more irregular than those of conventional osteoblastoma. The deposition of osteoid may focally be in a nontrabecular, lacelike pattern surrounding individual cells. As mentioned, the presence of epithelioid osteoblasts is a hallmark of aggressive osteoblastoma. Within the cytoplasm, there is usually a large, clear area that sometimes compresses and displaces the nucleus. The remaining cytoplasm has a few mitochondria and numerous prominent channels of rough endoplasmic reticulum. The cells form loosely cohesive sheets, with the formation of small, irregular, glandlike spaces seen ultrastructurally. The mitotic activity within the epithelioid osteoblasts ranges from 1 to 4 mitoses per 20 high-power fields. Gross and microscopic evidence of secondary aneurysmal bone cyst is frequently present. The distinction from osteosarcoma is based on the absence of cellular atypia, high mitotic rate, atypical mitotic figures, prominent and abundant lacelike osteoid deposition, permeative growth into adjacent bone and soft tissue, and presence of neoplastic cartilage. The presence of a peripheral shell of reactive bone over the soft tissue extensions of aggressive osteoblastomas also helps distinguish this lesion from osteosarcoma. Furthermore, all the comments in the discussion of differential diagnosis of benign osteoblastoma also apply to aggressive osteoblastoma. Personal Comments the principal diagnostic problem with regard to the entities classified as osteoblastoma and aggressive osteoblastoma centers around their distinction from osteosarcoma. This problem is further complicated by a recently proposed category of low-grade osteosarcoma that resembles osteoblastoma (osteoblastoma-like osteosarcoma). Furthermore, there is as yet no evidence that it undergoes spontaneous transformation to osteosarcoma. In our collected series, 19 of the 47 cases have recurred one or more times (40%), which is significantly higher than the 25% risk for benign osteoblastomas. We have not seen a well-documented case of aggressive osteoblastoma that has shown metastatic behavior. All the diagnostic criteria cited are important in evaluating the biologic potential of an osteoblastic tumor. The mere finding of epithelioid osteoblasts does not qualify the lesion as an aggressive osteoblastoma.
Buy generic super levitra on-line
The ratio between the monostotic and polyostotic forms varies among series from 8: 1 to 10: 1 erectile dysfunction nicotine purchase super levitra 80mg overnight delivery. Monostotic fibrous dysplasia affects a single bone, and typically one focus of involvement is identified. Polyostotic fibrous dysplasia is characterized by multiple foci involving several bones. The lesions in polyostotic fibrous dysplasia tend to be unilateral and to involve the bones of one extremity (monomelic polyostotic fibrous dysplasia). More severe forms can exhibit widespread skeletal involvement (polymelic polyostotic fibrous dysplasia). The disease usually manifests during the first three decades of life (approximately 70% of cases). Monostotic fibrous dysplasia may be asymptomatic and is discovered incidentally on radiographs obtained for other reasons. The lesion may occasionally be heralded by mild to moderate pain of long duration. Pathologic fracture, particularly in the long tubular bones, may also be a presenting symptom. In the monostotic form, the most frequent sites of involvement are the ribs, craniofacial bones, proximal femur, and tibia. The monomelic variant of the polyostotic form frequently affects the lower extremity and the homolateral hemipelvis. The polymelic form (the most severe generalized variant) shows widespread involvement of both extremities, the trunk, and craniofacial bones. In girls, precocious puberty usually presents as vaginal bleeding or spotting accompanied by the premature development of breast tissue and pubic hair. In boys, it is associated with testicular and penile enlargement and premature development of pubic and axillary hair. They are classically described as having jagged outlines referred to as a coast of Maine outline. They show some respect to the midline but there are frequent exceptions to this rule. The prevalence of major clinical findings in fibrous dysplasia/Albright-McCune syndrome is described in Table 8-2. Other extraskeletal manifestations include gastrointestinal reflux, gastrointestinal polyps, pancreatitis, and cardiac abnormalities potentially resulting in tachycardia and sudden death. A, Skeletal survey reveals a single lesion involving the left proximal femur proved histologically to be fibrous dysplasia. B, Polyostotic fibrous dysplasia showing multifocal involvements of predominantly left lower extremity. While the spot respects the midline, the borders are smooth and the spots alternate from left to right in a harlequin pattern. A, Plain radiograph of right forearm shows extensive polyostotic fibrous dysplasia and soft tissue mass. The relative age at which any given aspect of the disease is preclinical or clinically evident is depicted. The possibility of spontaneous resolution of the symptoms in a fraction of patients is also provided. The period of time during which abnormal menstruation can be expected is also depicted. Predominantly radiopaque lesions occur more frequently in the craniofacial bones than in other parts of the skeleton. This is related to the particular prevalence of well-mineralized bone trabeculae in fibrous dysplasia of craniofacial bones. In the long tubular bones, the shaft is typically involved, but the metaphyses are also frequently affected. Foci of punctate and ringlike calcification may be present and represent the areas of cartilaginous differentiation that may be found in fibrous dysplasia. This variant of fibrous dysplasia is sometimes referred to as fibrocartilaginous dysplasia. Even the expansile lesions are usually delineated by a thin rim of newly formed bone. This rare form typically occurs in smaller bones, such as the ribs or short tubular bones of the hands and feet. These lesions are sometimes attached to the adjacent bone by a bony stalk or form exophytic sessile masses. This unusual variant of fibrous dysplasia is also referred to as fibrous dysplasia protuberans. Fibrous dysplasia usually has sharp borders, and the bone contour is expanded with a thinned cortex. Areas of cartilaginous tissue are sometimes recognized as discrete translucent blue-white nodules. Hemorrhage and cystic change may be present, and areas of prominent xanthogranulomatous reaction have a yellow appearance. Hemorrhagic, blowout areas usually signify secondary aneurysmal bone cyst formation. Microscopic Findings Fibrous dysplasia is composed of spindle cells that have a whorled or storiform arrangement with interspersed Text continued on p. Note central (intramedullary) location of lesions and their ground-glass appearance. B, Opposite femur of patient shown in A demonstrates anterior bowing and multiple healed fractures and pseudarthrosis of proximal diaphysis. A, Anteroposterior radiograph of humerus shows intramedullary lesion with central opacities. B, T1-weighted magnetic resonance image shows low signal lesion with irregular signal void in heavily mineralized areas, same case as in A. C, A lateral radiograph of left hip shows isolated fibrous dysplasia in intertrochanteric region of femoral shaft. Note ringlike sclerosis of bone at periphery, which is characteristic of fibrous dysplasia in long bones. A, Anteroposterior radiograph of proximal femur shows intramedullary lesion with ill-defined opacities. B, T1-weighted magnetic resonance image shows low signal lesion involving the intertrochanteric region and extending to the femoral neck. A, Lateral radiograph shows radiolucent lesion with sclerotic margins involving calcaneus. B, T1-weighted magnetic resonance image shows low signal lesion of the calcaneus, same lesion as in A. C, Fat suppression sequence reveals signal irregularities within the lesion as well as well-defined low signal intensity (sclerotic) margin, same lesion as shown in A and B. A and B, Plain radiographs of humerus and tibia of same patient show extensive intramedullary involvement of multiple bones with cortical thinning and scalloping. There is asymmetric involvement with more severe changes on right side (monomelic form). A, Extensive skull involvement in polyostotic fibrous dysplasia with AlbrightMcCune syndrome. C, Bowing deformity with transverse fractures on convex side of femur in fibrous dysplasia. B-D, Expansile diaphyseal lesions in humerus, femur, and second metatarsal, respectively, in same patient. A, Lateral radiograph shows sclerotic, well-delineated lesion at distal end of tibia with protrusion posteriorly.
Buy cheap super levitra 80mg on-line
The prototypic example of neoplastic giant cell lesions is a giant cell tumor of bone; giant cell reparative granuloma was traditionally considered as a reactive process chewing tobacco causes erectile dysfunction generic super levitra 80mg line. Recent investigations appear to confirm the neoplastic nature of a giant cell tumor. In contrast, the conditions characterized by overlapping microscopic features in general referred to as giant cell reparative granuloma are subdivided into several categories based on their unique clinical presentation and genetic background. These two groups of conditions are characterized by somewhat distinct but occasionally overlapping microscopic features, and careful correlation with their clinical and radiographic presentations is required for correct classification of these lesions. In addition, the ubiquitous presence of multinucleated giant cells in many unrelated lesions of bone further complicates their classification. Malignant giant cell tumors can arise de novo or through transformation of a preexisting benign condition. Secondary reactive changes in a benign lesion sometimes mimic malignant transformation, and a great deal of expertise may be needed to recognize its benign nature. On the other hand, features of malignancy can be focal and inconspicuous, requiring careful examination of multiple sections. Clinicopathologic correlation on the basis of careful consideration of the radiologic features is of paramount importance in reaching a correct diagnosis in this diverse group of histologically overlapping entities. It 692 is composed of proliferating mononuclear histiocytic/ macrophage cells and multinucleated osteoclast-like giant cells. It frequently undergoes secondary changes that complicate its classic morphology, and its diagnosis can be challenging. In addition, a small proportion of giant cell tumors may be de novo malignant or may develop secondary malignant transformation. In addition, the so-called conventional giant cell tumor may give rise, in extremely rare instances, to distant metastases, typically in the lung. The vast majority of giant cell tumors are solitary lesions, but occasionally they can present as multifocal metachronous and synchronous lesions. The tumor most frequently involves the ends of long bones in skeletally mature individuals. In other skeletal sites, it is almost invariably located in epiphyseal or epiphyseal-equivalent portions of bone. Incidence and Localization Giant cell tumor of bone accounts for approximately 4% of all primary bone tumors. Most patients are between ages 20 and 55 years, and the peak age incidence is in the third decade of life. Approximately 70% of cases are diagnosed in patients between ages 20 and 40 years, and it is very unusual for giant cell tumor to occur in patients younger than age 20 years or older than age 55 years. Although the diagnosis of giant cell tumor in these age groups should be treated with skepticism, the unusual occurrence of giant cell tumor in the first two decades of 10 Giant Cell Lesions 693 life, as well as its occasional presentation in patients older than age 55 years, has been reported. It is extremely rare in the vertebral bodies, but the sacrum is the most common site in the axial skeleton. The association of giant cell tumor with Goltz syndrome (focal dermal hypoplasia), a rare condition in which there are multiple congenital anomalies of skin, teeth, and bone, has been reported. Giant cell tumor may occur more frequently in Chinese people than in people who live in Western countries. The estimated rate in the Chinese population has been reported to account for about 20% of all primary tumors of bone. Radiographic Imaging the radiographic picture of a giant cell tumor is quite characteristic and diagnostic if present in the specific anatomic site of skeletally mature patients. In a small percentage of cases, there can be minimal periosteal reaction when the cortex is breached. The borders, although well defined, usually do not show marginal sclerosis, and trabeculation usually is not present. These changes can be correlated with the microscopic findings of extensive reactive fibrohistiocytic features (see later section). Peak age incidence and frequent sites of skeletal involvement in giant cell tumor. A and B, Anteroposterior and lateral plain radiographs show involvement of lateral condyle. A, Radiograph of knee of an 18-yearold skeletally mature woman with giant cell tumor involving lateral tibial plateau and extending into metaphysis. D, Computed tomogram of tumor shown in C clearly demonstrates dense cortexlike rim surrounding tumor. A and B, Radiographs of right knee of a 31-year-old man who fell and sustained displaced pathologic fracture through medial cortex as well as midarticular surface of femur. C and D, Anteroposterior and lateral radiographs of distal femoral giant cell tumor with impacted pathologic fracture. Patient was a 40-yearold man who noticed aching pain and slight swelling above his knee for 1 year. A, Anteroposterior radiograph of distal femoral giant cell tumor with impacted pathologic fracture. C, Radiograph of left knee of a 54-year-old woman who had pins placed in distal femoral fracture 1 year previously. Fact that giant cell tumor was present was not appreciated, and tumor grew into soft tissue around femur. D, Coronally bisected amputation specimen of case shown in C with giant cell tumor within fractured distal femur and adjacent soft tissue. The quiescent type is characterized by a lytic defect limited to the medullary cavity of the bone with minimal or no involvement of the cortical bone. Usually the defect is surrounded by a more or less clear rim of sclerosis, and fine trabeculation can be present. The active radiologic type is characterized by a thinned, expanded cortex and somewhat unclear margins. The aggressive radiologic type is characterized by a lytic defect with ill-defined margins, invasion of the cortex, and extension of the tumor into surrounding soft tissue. So-called radiologic features of aggressiveness do not necessarily correlate with microscopic criteria of malignancy or the ultimate clinical behavior of the tumor. These are clinically irrelevant and misleading terms because they overlap with terms used to describe histologic features. Radiologic features of aggressiveness with huge destructive lesions, massive invasion into the cortex, and extension of the tumor into surrounding soft tissue are merely reflections of the stage of the disease. They do not necessarily correlate with aggressive histologic features in our experience. Overlap in radiologic presentation with fibrosarcoma, malignant fibrous histiocytoma, multiple myeloma, and other destructive lesions can occur. Consequently, in many cases, the exact radiologic diagnosis of giant cell tumor cannot be made. Nonepiphyseal localization of the lesion sometimes occurs in skeletally mature patients. So-called nonepiphyseal giant cell tumor represents a medical curiosity and is extremely rare. The tumor tissue is well demarcated and usually extends to the articular cartilage. The lesion usually occupies an eccentric position in the epiphyseal end of the bone. It is delimited in its periphery by a thin layer of fibrous and reactive bone tissue. The cortical bone may not be involved, and the original contour of the bone may be preserved. However, more frequently, the original cortex has been destroyed, and the bone contour has been expanded.
Purchase 80mg super levitra with amex
This fact has led radiologists to perform recanalization procedures in which catheters and guidewires are used to dislodge these blocking debris plugs erectile dysfunction doctor dubai super levitra 80mg. This technique, a modification of standard guidewire and catheter technique, can be performed as an outpatient procedure with minimal risks. Recanalization of an interstitial tubal blockage is successful in nearly 90% of patients, and up to 50% of patients can achieve conception after fallopian tube recanalization. Detailed description of fallopian tube recanalization techniques is beyond the scope of this chapter. However, in brief, fallopian tube recanalization is usually guided fluoroscopically after contrast-material hysterosalpingography. The fallopian tube is actually recanalized using a coaxial system comprising a 3-F catheter and a 0. Gentle guidewire probing usually leads to successful fallopian tube recanalization. A selective salpingogram is then performed to confirm successful 386 GenitourinaryRadiology:TheRequisites recanalization and to assess the status of the entire fallopian tube. If necessary, the procedure can then be repeated to recanalize the contralateral tube. Potential complications of fallopian tube recanalization include tubal perforation. Although perforation occurs in approximately 15% of cases, it is self-limited and rarely leads to morbidity or sequela. Clinically significant infection or bleeding is also rarely caused by fallopian tube recanalization. As with other interventional procedures, intraprocedural vasovagal reactions occur occasionally. The cause appears to be psychological stress, and these reactions are readily reversed with infusion of intravascular fluid and atropine, when necessary. Male Infertility Radiologists have a role in the management of male infertility patients. The major role of the interventional radiologists in this regard is in the diagnosis and treatment of some patients with impotence and for occlusion of varicoceles. A majority of men with nonpsychogenic impotence have vascular disorders of the arteries or the veins of the penis. Excessive venous outflow, also known as venous leak, is the most common vascular abnormality causing impotence. Once diagnosed, venous leak can be treated surgically with venous ligation or arteriovenous bypass grafting. As an alternative to surgery, veins draining the penis can be occluded percutaneously after catheterization of the dorsal vein of the penis. Draining veins are then selectively catheterized, followed by ablation of these veins with intravascular sclerosants. A minority of patients with vascular-based impotence suffer from arterial insufficiency. In a small percentage of patients, arterial occlusions develop after focal trauma to the pelvis and perineum. In either case, angioplasty of stenoses or occlusion of the pudendal artery or its branches, including the penile artery and the cavernosal branches, has been disappointing. Long-term patency of these vessels has Blockage Contrast Medium Blockage Fundus Cornua Blockage Balloon Cannula 6-F. A, Diagram of bilateral interstitial fallopian tube occlusion confirmed with hysterosalpingography as the first step in the recanalization procedure. B, Diagram demonstrating advancement of a curved catheter to the left fallopian tube os. C, Radiograph demonstrating selective catheterization of the left fallopian tube os. A radiopaque line (arrow) marks the end of the angiographic catheter at the origin of the fallopian tube. F, Diagram demonstrating performance of a left salpingogram following recanalization. The fallopian tube is patent, with free spillage (arrowheads) into the peritoneal cavity. Alternatively, focal stenosis of one or both hypogastric arteries can be treated successfully with angioplasty. Compared with the smaller arteries supplying the penis, the hypogastric artery has a larger caliber and higher flow rates, factors that likely account for high patency rates with angioplasty treatment. Angioplasty of the hypogastric artery can be performed after diagnostic angiography. Typically, the artery to be treated is approached via puncture of the contralateral common femoral artery. Standard angiographic guidewires and angioplasty balloon catheters are used for treatment. The size of the angioplasty balloon depends on the diameter of the blood vessel as measured during the diagnostic studies. In addition, treatment of other causes of male infertility is being explored at some institutions. Techniques used for fallopian tube recanalization have been extended to treat male patients with ejaculatory duct occlusion. In some instances, this condition can be treated with radiologic recanalization techniques. A catheter and guidewire can be steered through the seminal vesicle and into the ejaculatory duct. Once the guidewire has traversed the ejaculatory duct orifice, it can be advanced into the urethra. This guidewire can be retrieved and used for retrograde balloon dilatation or incision of the ejaculatory duct orifice. This left posterior oblique radio- graph demonstrates contrast opacification of the corpora cavernosa of the penis during chemically induced erection. Normal cavernosography demonstrates opacification of the entire corpora cavernosa bilaterally with minimal, if any, venous filling. There is filling of the dorsal vein of the penis (arrows) as well as minimal venous filling of periprostatic veins (arrowheads) on the right. This periprostatic vein opacification indicates a minimal venous leak in this patient. Needless to say, renal artery angioplasty requires careful and meticulous techniques. Plaques are easily undermined during catheterization, and the result can lead to dissection, distal embolization, and renal artery occlusion. Vasodilators should be administered concurrently with renal angioplasty procedures to avoid excessive arterial spasm and resulting thrombosis. However, the radiologist should be aware of some applications in which percutaneous arterial occlusion techniques are useful in genitourinary radiology. Arterial occlusion is useful in genitourinary radiology to treat active arterial bleeding and arterial venous malformations, to devascularize hypervascular tumors, for nonsurgical renal ablation, and to treat intractable uterine bleeding. Active renal hemorrhage usually occurs after renal trauma, including iatrogenic trauma. With the increased use of percutaneous renal biopsy and transrenal procedures, iatrogenically induced arterial injuries including active bleeding, arteriovenous fistula, or pseudoaneurysm, are not rare. Ideally, superselective catheterization of the bleeding artery should be performed, followed by transcatheter delivery of embolic materials (Table 10-3) such as Gelfoam particles and metal coils to occlude the bleeding end-artery branches. Superselective catheterization and embolization minimizes damage to normal renal parenchyma while preventing further bleeding and avoids the risk of collateral arteries supplying the bleeding focus. Superselective catheterization can usually be achieved with coaxial systems that are available commercially. Gelfoam pledgets can be used initially to devascularize the majority of these arteriovenous fistulae.


