Buy cheap trihexyphenidyl line
In addition pain treatment who order 2mg trihexyphenidyl mastercard, it is known that at the time of diagnosis, an important number of active cases (<35%) are proven nonreactive, rendering the test unsatisfactory. Ecological study of Paracoccidioides brasiliensis in soil: growth ability, conidia production and molecular detection. In vitro Paracoccidioides brasiliensis biofilm and gene expression of adhesins and hydrolytic enzymes. Endemic regions of paracoccidioidomycosis in Brazil: a clinical and epidemiologic study of 584 cases in the southeast region. Paracoccidioidomycosis: eco-epidemiology, taxonomy and clinical and therapeutic issues. Morphological aspects of Paracoccidioides brasiliensis in lymph nodes: implications for the 3221 52. Paracoccidioidomycosis: epidemiological, clinical, diagnostic and treatment up-dating. Paracoccidioidomycosis in a western Brazilian amazon state: clinical-epidemiologic profile and spatial distribution of the disease. Functional and phenotypic evaluation of eosinophils from patients with the acute form of paracoccidioidomycosis. Pulmonary paracoccidioidomycosis: clinical, immunological and histopathological aspects. Paracoccidioidomycosis in patients infected with and not infected with human immunodeficiency virus: a case-control study. Adrenal function status in patients with paracoccidioidomycosis after prolonged post-therapy follow-up. Phylogenetic and evolutionary aspects of Paracoccidioides brasiliensis reveal a long coexistence with animal hosts that explain several biological features of the pathogen. Cryptic speciation and recombination in the fungus Paracoccidioides brasiliensis as revealed by gene genealogies. Microsatellite analysis of three phylogenetic species of Paracoccidioides brasiliensis. Genome diversity, recombination and virulence across the major lineages of Paracoccidioides. Phylogenetic analysis of Lacazia loboi places this previously uncharacterized pathogen within the dimorphic Onygenales. New Paracoccidioides brasiliensis isolate reveals unexpected genomic variability in this human pathogen. Phylogenetic analysis reveals a high level of speciation in the Paracoccidioides genus. Distinct patterns of yeast cell morphology and host responses induced by representative strains of Paracoccidioides brasiliensis (Pb18) and Paracoccidioides lutzii (Pb01). Paracoccidioides brasiliensis and paracccidioidomycosis: molecular approaches to morphogenesis, diagnosis, epidemiology, taxonomy and genetics. The human fungal pathogen Paracoccidioides brasiliensis (Onygenales: Ajellomycetaceae) is a complex of two species: phylogenetic evidence from five mitochondrial markers. Molecular and morphological data supports the existence of a sexual cycle in species of the genus Paracoccidioides. Presence and expression of the mating type locus in Paracoccidioides brasiliensis isolates. High frequency of Paracoccidioides brasiliensis infection in armadillo (Dasypus novemcinctus): an ecological study. The naked-tailed armadillo Cabassous centralis (Miller 1899): a new host to Paracoccidioides brasiliensis. Characteristics of the conidia produced by the mycelial form of Paracoccidioides brasiliensis. Partial characterization of a Paracoccidioides brasiliensis protein with capacity to bind to extracellular matrix proteins. Gene expression analysis of Paracoccidioides brasiliensis transition from conidium to yeast cell. Genes potentially relevant in parasitic phase of the fungal pathogen Paracoccidioides brasiliensis. A conserved dimorphism-regulating histidine kinase controls the dimorphic switching in Paracoccidioides brasiliensis. Paracoccidioidomycosis: epidemiological features of a 1,000-cases series from a hyperendemic area on the southeast of Brazil. Role of the armadillo Dasypus novemcinctus in the epidemiology of paracoccidioidomycosis. Importance of xenarthrans in the eco-epidemiology of Paracoccidioides brasiliensis. Structural and topographic dynamics of pulmonary histopathology and local cytokine profiles in Paracoccidioides brasiliensis conidia-infected mice. Morphological aspects of Paracoccidioides brasiliensis in lymph nodes: implications for the prolonged latency of paracoccidioidomycosis Climate and acute/subacute paracoccidioidomycosis in a hyperendemic area in Brazil. First description of a cluster of acute/subacute paracoccidioidomycosis cases and its association with a climatic anomaly. Paracoccidioidomycosis in a western Brazilian Amazon state: clinical-epidemiologic profile and spatial distribution of the disease. Inhibition of Paracoccidioides brasiliensis by pesticides: is this a partial explanation for the difficulty in isolating this fungus from the soil The role of gallium-67 scan in defining the extent of disease in an endemic deep mycosis, paracoccidioidomycosis: a predominantly multifocal disease. Pulmonary abnormalities in adult patients with chronic paracoccidioidomycosis: prolonged follow-up after itraconazole therapy. Paracoccidioides-host interaction: an overview on recent advances in the paracoccidioidomycosis. Surface-expressed enolase contributes to the adhesion of Paracoccidioides brasiliensis to host cells. Melanin protects Paracoccidioides brasiliensis from the effects of antimicrobial photodynamic inhibition and antifungal drugs. Interaction of epithelial cell membrane rafts with Paracoccidioides brasiliensis leads to fungal adhesion and Src-family kinase activation. Paracoccidioides brasiliensis lipids modulate macrophage activity via Toll-dependent or independent mechanisms. Human neutrophils produce extracellular traps against Paracoccidioides brasiliensis. Depletion of neutrophils exacerbates the early inflammatory immune response in lungs of mice infected with Paracoccidioides brasiliensis. Depletion of neutrophils promotes the resolution of pulmonary inflammation and fibrosis in mice infected with Paracoccidioides brasiliensis. Indoleamine 2,3-dioxygenase controls fungal loads and immunity in paracoccidioidomycosis but is more important to susceptible than resistant hosts. High interleukin-4 expression and interleukin-4 gene polymorphisms are associated with susceptibility to human paracoccidioidomycosis. M2 macrophages and inflammatory cells in oral lesions of chronic paracoccidioidomycosis. Infection with Paracoccidioides brasiliensis induces B-1 cell migration and activation of regulatory T cells. Dendritic cells primed with Paracoccidioides brasiliensis peptide P10 are therapeutic in immunosuppressed mice with paracoccidioidomycosis. Yeast expressing Gp43 protein as a vaccine against Paracoccidioides brasiliensis infection. Mouse immunization with radioattenuated yeast cells of Paracoccidioides brasiliensis. Immunization with recombinant Pb27 protein reduces the levels of pulmonary fibrosis caused by the inflammatory response against Paracoccidioides brasiliensis. Itraconazole in combination with neutrophil depletion reduces the expression of genes related to pulmonary fibrosis in an experimental model of paracoccidioidomycosis. Incubation period and early natural history events of the acute form of paracoccidioidomycosis: lessons from patients with a single Paracoccidioides spp. Pulmonary paracoccidioidomycosis showing reversed halo sign with nodular/coarse contour.
Buy trihexyphenidyl online
Acute abdominal pain as a presenting symptom of varicella zoster virus infection in recipients of bone marrow transplants best pain medication for a uti buy cheap trihexyphenidyl 2mg on-line. Progressive outer retinal necrosis syndrome: a comprehensive review of its clinical presentation, relationship to immune system status, and management. Visceral varicella zoster virus infection after allogeneic stem cell transplantation. Postexposure prophylaxis against varicella-zoster virus infection among recipients of hematopoietic stem cell transplant: unresolved issues. Adenovirus infection in hematopoietic stem cell transplantation: effect of ganciclovir and impact on survival. Invasive adenoviral infections in T-cell-depleted allogeneic hematopoietic stem cell transplantation: high mortality in the era of cidofovir. Approach to adenovirus infections in the setting of hematopoietic cell transplantation. Quantitative real-time polymerase chain reaction for detection of adenovirus after T cell-replete hematopoietic cell transplantation: viral load as a marker for invasive disease. Detection of adeno-associated virus viremia in hematopoietic cell transplant recipients. High lethality of human adenovirus disease in adult allogeneic stem cell transplant recipients with high adenoviral blood load. Intravesical instillation of cidofovir in the treatment of hemorrhagic cystitis caused by adenovirus type 11 in a bone marrow transplant recipient. Cidofovir for adenovirus infections after allogeneic hematopoietic stem cell transplantation: a survey by the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Disseminated adenovirus infection after allogeneic stem cell transplant and the potential role of brincidofovir-case series and 10 year experience of management in an adult transplant cohort. Underutilization of norovirus testing in hematopoietic cell transplant recipients at a large cancer center. Characteristics and outcomes of patients diagnosed with norovirus gastroenteritis after allogeneic hematopoietic stem cell transplantation based on immunochromatography. Management of respiratory viral infections in hematopoietic cell transplant recipients. Human parainfluenza virus infection after hematopoietic stem cell transplantation: risk factors, management, mortality, and changes over time. Human rhinovirus and coronavirus detection among allogeneic hematopoietic stem cell transplantation recipients. Timing and severity of community acquired respiratory virus infections after myeloablative versus non-myeloablative hematopoietic stem cell transplantation. Rhinovirus as a cause of fatal lower respiratory tract infection in adult stem cell transplantation patients: a report of two cases. Impact of corticosteroid treatment and antiviral therapy on clinical outcomes in hematopoietic cell transplant patients infected with influenza virus. Rhinovirus infections in hematopoietic stem cell transplant recipients with pneumonia. Brief communication: fatal human metapneumovirus infection in stem-cell transplant recipients. Epidemiologic and clinical characteristics of coronavirus and bocavirus respiratory infections after allogeneic stem cell transplantation: a prospective single-center study. Combination therapy with aerosolized ribavirin and intravenous immunoglobulin for respiratory syncytial virus disease in adult bone marrow transplant recipients. Parainfluenza virus infections in hematopoietic cell transplant recipients and hematologic malignancy patients: a systematic review. Oral ribavirin for treatment of respiratory syncitial virus and parainfluenza 3 virus infections post allogeneic haematopoietic stem cell transplantation. Immuneglobulin prophylaxis of respiratory syncytial virus infection in patients undergoing stem-cell transplantation. Risk factors for Epstein-Barr virus-related post-transplant lymphoproliferative disease after allogeneic hematopoietic stem cell transplantation. Response to rituximab-based therapy and risk factor analysis in Epstein-Barr virus-related lymphoproliferative disorder after hematopoietic stem cell transplant in children and adults: a study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Impact of stem cell graft on early viral infections and immune reconstitution after allogeneic transplantation in adults. Early identification of Epstein-Barr virus-associated post-transplantation lymphoproliferative disease. Monitoring and preemptive rituximab therapy for Epstein-Barr virus reactivation after antithymocyte globulin containing nonmyeloablative conditioning for umbilical cord blood transplantation. Human herpes 6 virus encephalitis complicating allogeneic hematopoietic stem cell transplantation. Human herpesvirus 6 is associated with status epilepticus and hyponatremia after umbilical cord blood transplantation. Severe hyponatremia caused by syndrome of inappropriate secretion of antidiuretic hormone developed as initial manifestation of human herpesvirus-6-associated acute limbic encephalitis after unrelated bone marrow transplantation. Diagnostic clues to human herpesvirus 6 encephalitis and Wernicke encephalopathy after pediatric hematopoietic cell transplantation. Human herpesvirus 6 infection after hematopoietic cell transplantation: is routine surveillance necessary Human herpesvirus 6 in lung tissue from patients with pneumonitis after bone marrow transplantation. Engraftment failure associated with peripheral blood stem cell transplantation after B19 parvovirus infection. Chronic anemia due to parvovirus B19 infection in a bone marrow transplant patient after platelet transfusion. Exposure of hematologic patients to parvovirus B19 as a contaminant of blood cell preparations and blood products. The prophylactic use of low-dose amphotericin B in bone marrow transplant patients. Intravenous and oral itraconazole versus intravenous and oral fluconazole for long-term antifungal prophylaxis in allogeneic hematopoietic stem-cell transplant recipients: a multicenter, randomized trial. A systematic review and meta-analysis of diagnostic accuracy of serum 1,3-beta-d-glucan for invasive fungal infection: focus on cutoff levels. Late onset Pneumocystis carinii pneumonia following allogeneic bone marrow transplantation. Early onset Pneumocystis carinii pneumonia after allogeneic peripheral blood stem cell transplantation. Dapsone for Pneumocystis carinii prophylaxis in children undergoing bone marrow transplantation. A prospective randomized trial comparing the toxicity and safety of atovaquone with trimethoprim/sulfamethoxazole as Pneumocystis carinii pneumonia prophylaxis following autologous peripheral blood stem cell transplantation. Clinical features and analysis of risk factors for invasive candidal infection after marrow transplantation. Brain abscess following marrow transplantation: experience at the Fred Hutchinson Cancer Research Center, 1984-1992. Invasive fungal infections in recipients of allogeneic hematopoietic stem cell transplantation after nonmyeloablative conditioning: risks and outcomes. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Candidemia in allogeneic blood and marrow transplant recipients: evolution of risk factors after the adoption of prophylactic fluconazole. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Epidemiology of invasive mold infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation. Galactomannan antigen enzyme-linked immunosorbent assay for diagnosis of invasive aspergillosis after hematopoietic stem cell transplantation.
Generic 2mg trihexyphenidyl free shipping
The severity of acute side effects may be reduced by initiating treatment with a lower dose of diethylcarbamazine (50 mg on day 1 pain treatment laser purchase 2mg trihexyphenidyl fast delivery, followed by 50 mg three times on day 2 and 100 mg three times on day 3). Hydroceles may be repaired surgically, but prevention of recurrence is contingent on drug treatment. It is not known whether diethylcarbamazine or other antifilarial drugs such as ivermectin and albendazole ameliorate a preexisting lymphatic pathologic process because randomized clinical trials have not been performed. Some studies of mass drug treatment to control filariasis in endemic populations suggest that reducing transmission may decrease the incidence of chronic lymphatic pathologic processes. By 2014, mass drug administration programs had been implemented in more than 60 countries, and it has been estimated that more than 5 billion doses of antifilarial medications have been administered. It is currently believed that at least 5 years of annual mass treatment is necessary to stop transmission because this is the estimated reproductive life span of adult worms. Results of studies in Egypt indicate that this strategy will likely be successful in endemic areas where a good public health infrastructure exists. Microfilariae released from fecund female worms migrate to the blood and have a diurnal periodicity. Epidemiology Loiasis is endemic in coastal and rain forest regions of central and West Africa. Infected individuals usually have a long history of residence in endemic areas with prolonged exposure to infected vectors; however, repeated short durations of intense exposure can also result in infection and morbidity, including in expatriate nonresidents who travel to endemic areas. The main clinical presentation is a Calabar swelling, which represents an angioedematous response to adult worms migrating through subcutaneous tissue. The 10- to 20-cm swelling lesions most commonly appear on the face and extremities and are preceded by itching and pain. Other manifestations include renal complications (hematuria and proteinuria) and encephalitis, which are usually precipitated by treatment with the antifilarial drug diethylcarbamazine. In the case of encephalitis, persons with high-level microfilaremia (>2500 microfilariae/mL) are at high risk. Identification of microfilariae in the blood (which should be obtained during the day) or visualization of an adult worm in the conjunctiva confirms loiasis. Therapy Diethylcarbamazine at a dose of 8 to 10 mg/kg/day for 21 days should be given to persons who do not have microfilaremia. It is most commonly observed in South and Southeast Asia and endemic areas of Brazil and Guyana. Patients are typically middle-aged men (male-to-female ratio, 4: 1) who present with nocturnal asthma, cough, fever, and weight loss. Chest radiographs typically show increased bronchovascular markings with a mottled appearance in the middle and lower lungs. Treatment with diethylcarbamazine leads to symptomatic improvement and reduces eosinophilia and immunoglobulin E levels. If the infection is not treated, progressive interstitial fibrosis and restrictive lung disease may develop. Side effects can be minimized by concurrent administration of antihistamines or corticosteroids. In persons with high-level microfilaremia (>2500/mL), there is a significant risk for renal and central nervous system complications due to the rapid destruction of large numbers of microfilariae. Options include withholding anthelmintic drugs, cytapheresis to remove microfilariae before administration of diethylcarbamazine, and administration of a single dose of ivermectin. In the context of mass drug administration programs in West and central Africa aimed at elimination of onchocerciasis or lymphatic filariasis, it is important that prior screening for coendemic, high-level L. Identification of microfilariae in the skin or eye or adult worms in nodules is required for definitive diagnosis. Microfilariae in the skin are accessed by using a corneoscleral instrument to obtain a 1- to 2-mg biopsy specimen of the dermis overlying both scapulae, iliac crests, and calves. In the research setting, polymerase chain reaction assay can be used to identify persons with light infections that are not detectable by microscopy. Eye disease may be mimicked by other infectious and noninfectious causes of chorioretinitis. Chapter 287 Tissue Nematodes, Including Trichinellosis, Dracunculiasis, Filariasis, Loiasis, and Onchocerciasis Prevention and Control Travelers who plan prolonged residence in endemic areas should take 300 mg diethylcarbamazine weekly as chemoprophylaxis. Therapy Onchocerciasis Onchocerca volvulus is transmitted by blood-feeding Simulium spp. Infection can cause dermatitis, subcutaneous nodules, keratitis, and chorioretinitis. The disease has a great socioeconomic impact because it causes reduced vision ("river blindness") and chronic skin disease in adults. Infection is acquired when female Simulium damnosum sibling species (in Africa) and several other Simulium spp. Onchocerciasis is endemic in West Africa, limited areas of East Africa, and the Arabian peninsula. Mass administration of ivermectin in six endemic countries in the Americas has resulted in interruption of transmission in all geographic regions with the exception of remote border areas of southern Venezuela and northern Brazil. Onchocerciasis in savanna regions of West Africa is characterized by a greater likelihood of reduced vision and blindness compared with rain forest regions. Dermatologic manifestations of infection are common in areas of Africa outside either the rain forest or savanna. Life Cycle of the Parasite Epidemiology Ivermectin, which is effective in killing microfilariae but not adult O. A reduction in skin microfilariae is detectable within 2 weeks but may be incomplete. For expatriates who are more prone than lifelong residents of endemic areas to develop severe pruritus, more frequent treatment with ivermectin. In cases in which loiasis coexists with onchocerciasis (both infections are endemic in some areas of West Africa), the use of ivermectin carries a risk for precipitating encephalopathy in persons with high levels of L. Prevention and Control Control of the Simulium vector by aerial dispersion of larvicides from 1974 to 2002 was highly successful in reducing blindness in 11 countries in West Africa where the savanna form of onchocerciasis was common. The African Program for Onchocerciasis Control is based on mass distribution of ivermectin to reduce morbidity and possibly stop transmission. The latter goal has recently been emphasized as feasible with programmatic changes that include improved mapping of endemic foci, better monitoring tools, and use of drug combinations that kill adult worms. The major pathologic sequelae of clinical significance are due to inflammatory responses to microfilariae. In the skin, these include acute and chronic papular dermatitis, lichenified dermatitis, atrophy, and depigmentation. In the eye, microfilariae that have migrated to the cornea initially elicit punctate keratitis. As described previously, this outcome is most common in savanna forms of onchocerciasis in West Africa. Onchocerca volvulus infection may also cause inguinal lymph node fibrosis and atrophy of the overlying skin that leads to the appearance of hanging groin. Diagnosis the diagnosis should be considered when the previously described signs are present in an individual who has resided in an endemic area. Because Mansonellosis is a poorly understood infection of humans that is asymptomatic in most individuals. Lymphadenopathy, urticaria, pruritus, pulmonary symptoms, and keratitis have been described. Adult worms reside in serous cavities of the body and sheathed microfilariae circulate in the blood. Doxycycline has been shown to be effective in reducing microfilaremia, likely through its ability to eliminate adult worms by killing Wolbachia bacterial endosymbionts.
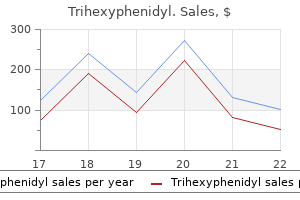
| Comparative prices of Trihexyphenidyl | ||
| # | Retailer | Average price |
| 1 | Rite Aid | 543 |
| 2 | J.C. Penney | 463 |
| 3 | Hy-Vee | 249 |
| 4 | Albertsons | 650 |
| 5 | QVC | 216 |
| 6 | Target | 320 |
| 7 | Ace Hardware | 921 |
Generic trihexyphenidyl 2 mg without a prescription
Postinfectious fatigue can be profound in some individuals and may persist long after the resolution of other clinical symptoms pain treatment center in lexington ky cheap trihexyphenidyl 2mg without prescription. It is unknown whether the pathogenesis of disease is due to enterocyte dysfunction or whether toxins are secreted. Shedding of oocysts in stool can precede the onset of clinical illness, but the disappearance of symptoms and oocysts usually occurs simultaneously. Oocysts may be shed in low numbers during infection, and both concentration of stool specimens and collection of multiple specimens may be required to make the diagnosis. Therefore if cyclosporiasis is suspected, notification of the laboratory is prudent so that appropriate tests can be performed. Therapy Cystoisospora belli under ultraviolet epifluorescence microscopy is both rapid and sensitive, although not specific. The diagnosis may also be made by histopathologic or electron microscope examination of jejunal aspirates or biopsy specimens. Microscopic examination of tissue reveals altered histologic architecture of the small bowel, and loss of the brush border and altered epithelial cell morphology may be noted. Routine hematoxylin and eosin staining of biopsy material may not permit adequate visualization of the organisms. Tissue sections may reveal Cyclospora in supranuclear locations within the cytoplasm, distinguishing them from Cryptosporidium, which are on the surface of enterocytes. It is the only one of more than 200 identified Cystoisospora species that is known to cause human infection. Human infections previously attributed to Cystoisospora hominis are more likely to have been caused either by Sarcocystis species or by misidentified C. Immature Cystoisospora oocysts, each containing a single sporoblast, are excreted in the stool of infected hosts. Ingestion of sporulated oocysts results in the release of sporozoites in the proximal small intestine. Sporozoites may develop into merozoites, with subsequent asexual reproduction occurring within enterocytes; over time, sexual reproduction follows, resulting in the development and passage of immature, unsporulated oocysts in feces. Rarely, sporozoites can migrate out of the intestine to various tissues, where they may remain dormant as cysts and later give rise to extraintestinal disease. Life Cycle Epidemiology Cystoisospora species are found worldwide but predominantly in tropical and subtropical climates, especially in South America, Africa, and Southeast Asia. It is unclear whether most animals develop clinical disease or whether they merely act as paratenic hosts. Pigs are notable exceptions; Cystoisospora suis can cause severe diarrheal disease and death in piglets and has been implicated in outbreaks of disease among nursing piglets. In immunocompetent hosts, Cystoisospora infection is indistinguishable from other noninflammatory intestinal infections. After an incubation period of approximately 1 week, a self-limited diarrheal illness usually develops that lasts 2 to 3 weeks and is characterized by malaise, anorexia, weight loss, abdominal cramps, and profuse watery diarrhea without blood. Biliary tract disease due to Cystoisospora has been described in immunocompetent hosts. Peripheral blood eosinophilia and Charcot-Leyden crystals in stool, both unusual in other protozoan infections, have been reported. Histologic examination of the small bowel of infected patients is relatively nonspecific and reveals villous atrophy, crypt hyperplasia, and lamina propria infiltration with inflammatory cells, particularly eosinophils. Asexual and sexual stages of the parasite can be identified within parasitophorous vacuoles of enterocytes. In case reports of extraintestinal disease, intracellular cysts containing one to three trophozoites were identified in lymph nodes, liver, and spleen. Symptoms induced by experimental challenge with infected meat include nausea, abdominal discomfort, and self-limited nonbloody diarrhea, with symptom severity dependent on the amount of meat consumed. Segmental eosinophilic and necrotizing enteritis attributed to sexual forms of Sarcocystis has been reported; however, causation in these cases was not definitely established. Eosinophilic myositis has been reported, occurring in association with other symptoms, including fever, bronchospasm, transient pruritic rashes, lymphadenopathy, subcutaneous nodules, and arthralgias. The hallmark of the illness was clinically significant myositis that occurred 30 days or more after travel. Sporocysts may be identified in the stool of symptomatic (and asymptomatic) individuals with intestinal sarcocystosis. Brightfield microscopy and fecal flotation wet mounts are optimal, using density gradient media rather than other sedimentation methods. For patients with symptoms suggestive of acute muscular disease, muscle biopsy using conventional histologic staining can demonstrate sarcocysts, although staining may be variable. Myositis and myonecrosis associated with mixed inflammatory infiltrates and sometimes tissue eosinophilia may be seen in cases of acute muscular sarcocystosis. Chapter 283 Cyclospora cayetanensis, Cystoisospora belli, Sarcocystis Species, Balantidium coli, and Blastocystis Species Sarcocystis Species Sarcocystis species, previously known as Sarcosporidia, are zoonotic protozoan parasites. Since the first report of sarcocystosis in mice in 1843, more than 130 species of Sarcocystis have been reported from a wide range of domestic and wild animals. Unlike many other coccidian parasites, Sarcocystis has an obligatory two-host cycle. Definitive and intermediate hosts are generally species specific but have been identified for only half of all Sarcocystis species. Human intestinal sarcocystosis, in which humans are the definitive hosts, is caused by one of two species, Sarcocystis hominis or Sarcocystis suihominis. Humans may also be accidental intermediate hosts for other Sarcocystis species, leading to human muscular sarcocystosis. Through the ingestion of poorly cooked or raw meat containing tissue cysts, humans may serve as definitive hosts for Sarcocystis in pigs (S. Humans may also be incidental intermediate hosts when food or water contaminated with fecal sporocysts is ingested. After consumption of tissue cysts by the definitive host (usually a carnivore), motile bradyzoites emerge from sarcocysts and enter the intestinal lamina propria. Bradyzoites mature into male and female forms, and sexual reproduction follows in the intestinal mucosa; mature oocysts, each of which contains two sporocysts, are formed. The thin walls of oocysts are readily disrupted, leading to shedding of both oocysts and infectious sporocysts in the feces. In contrast, sporocysts are hardy, resisting treatment with bleach, chlorhexidine, and iodophors. After ingestion of sporocysts by the intermediate host (usually an herbivore), sporozoites are released, penetrate the intestinal epithelium, and migrate to vascular endothelium, where they undergo cycles of asexual multiplication. The resulting merozoites are then hematogenously disseminated and invade cardiac or striated muscle cells. Within muscle, the characteristic septate cysts (sarcocysts) containing bradyzoites develop. Sarcocysts become infectious only after they have matured, a process that may take 2 months or more depending on the species. The cycle is complete when mature muscle cysts are eaten by an appropriate definitive host. Although worldwide in distribution, most human cases of Sarcocystis infection have been reported from tropical and subtropical climes, mainly Southeast Asia and, in particular, Malaysia. Identification of Sarcocystis in stool or muscle, or of antibodies in serum, is most often an incidental finding. As many as 20% of residents in some endemic areas are seropositive, reflecting the sanitary conditions and dietary habits in these regions. Studies after an outbreak of 89 cases associated with a trip to Pangkor Island, Malaysia,54 demonstrated molecular identity of the disease isolates with Sarcocystis nesbitti found in the stool of snakes (Naja naja), with the route of transmission presumably being the consumption of water or food contaminated with snake feces. Life Cycle Diagnosis Epidemiology Therapy No specific treatment for Sarcocystis infection is known. Development of symptoms may depend in part on the species of sarcocysts that are ingested. Muscular sarcocystosis can be prevented by reducing individual exposures to sporocyst ingestion. This may be challenging given potential environmental seeding and contamination of food and water; however, drinking filtered, boiled, or bottled water and thorough cooking of food that may be contaminated with sporocysts can mitigate the risk of infection.
Buy trihexyphenidyl now
Evaluation of a real-time polymerase chain reaction assay for the laboratory diagnosis of giardiasis regional pain treatment medical center discount trihexyphenidyl online amex. A novel, multi-parallel, real-time polymerase chain reaction approach for eight gastrointestinal parasites provides improved diagnostic capabilities to resource-limited at-risk populations. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. Detection of Giardia lamblia antigens in human fecal specimens by a solid-phase qualitative immunochromatographic assay. Physician use of parasite tests in the United States from 1997 to 2006 and in a Utah Cryptosporidium outbreak in 2007. Comparison of the Triage Micro Parasite Panel and microscopy for the detection of Entamoeba histolytica/Entamoeba dispar, Giardia lamblia, and Cryptosporidium parvum in stool samples collected in Kenya. Comparison of serum antibody response to Giardia lamblia of symptomatic and asymptomatic patients. Comparing serologic response against enteric pathogens with reported diarrhea to assess the impact of improved household drinking water quality. Increased incidence of nitroimidazole-refractory giardiasis at the hospital for Tropical Diseases London: 2008-2013. Giardiasis in the post genomic era: treatment, drug resistance and novel therapeutic perspectives. Late incidence of cancer after metronidazole use: a matched metronidazole user/nonuser study. Pyruvate:ferredoxin oxidoreductase and thioredoxin reductase are involved in 5-nitroimidazole activation while flavin metabolism is linked to 5-nitroimidazole resistance in Giardia lamblia. Nitazoxanide: a review of its use in the treatment of gastrointestinal infections. A meta-analysis of the effectiveness of albendazole compared with metronidazole as treatments for infections with Giardia duodenalis. Therapy-resistant diarrhea due to Giardia lamblia in a patient with common variable immunodeficiency disease. Treatmentladder and genetic characterisation of parasites in refractory giardiasis after an outbreak in Norway. Could giardiasis be a risk factor for low zinc status in schoolchildren from northwestern Mexico Effects of vitamin A supplementation on intestinal barrier function, growth, total parasitic, and specific Giardia spp infections in Brazilian children: a prospective randomized, double-blind, placebo-controlled trial. Effect of mass stool examination and mass treatment for decreasing intestinal helminth and protozoan infection rates in Bolivian children: a cross-sectional study. Partial breastfeeding protects Bedouin infants from infection and morbidity: prospective cohort study. Trichomonas vaginalis is the causative agent of trichomoniasis, a common cause of vaginitis. It has four free flagella and one recurrent flagellum, along the outer margin of the undulating membrane; a costa at the base of the undulating membrane; and an axostyle extending through the cell. The hydrogenosome appears to have a common ancestry with mitochondria based on similarities in protein import. Trichomonas tenax, found in oral gingival and tracheobronchial sites, and Pentatrichomonas hominis, isolated from the intestinal tract, are considered nonpathogenic. Tritrichomonas foetus, which is found exclusively in cattle, is perhaps the nonhuman trichomonad most similar to T. Tritrichomonas foetus can be invasive to the fetus, having been demonstrated in the placenta and the fetal lung, gut, and lymph nodes, and is a known cause of abortion in infected cattle. The trophozoite divides by binary fission and, in natural infections, gives rise to a population in the lumen and on the mucosal surfaces of the urogenital tracts of humans. Natural infection seems to produce immunity that is only partially protective, because reinfection of patients can be as high as 30% on follow-up. The release of the 5X genome sequence data makes the most comprehensive genomic sequence of this parasite available to date. Trichomoniasis is an extremely common infection in the United States and worldwide. In Los Angeles, for example, the prevalence among African-American patients at a public clinic was 38%. There was no significant difference in the detection of the organism between men with and without urethral symptoms (20% and 14. Interestingly, although 2% to 17% of female neonates may have vaginal colonization if the mother is infected, the infection may not be sustained once the maternal effects of estrogen wear off and the vaginal pH becomes neutral. Comparison of direct fluorescent antibody, acridine orange, wet mount, and culture for detection of Trichomonas vaginalis in women attending a public sexually transmitted disease clinic. Signs of infection include vaginal discharge (42%), odor (50%), and edema or erythema (22% to 37%). Colpitis macularis (strawberry cervix) is a specific clinical sign for this infection but is detected with reliability only by colposcopy and rarely during routine examination. The extent of the inflammatory response to the parasite may determine the severity of the symptoms. Factors that influence the host inflammatory response are not well understood but may include hormonal levels, coexisting vaginal flora, and strain and relative concentration of the organisms present in the vagina. Trichomoniasis in men may also rarely cause epididymitis, prostatitis, and superficial penile ulcerations. However, even for skilled diagnosticians, the sensitivity of this test varies from 40 to 60%, and may be less in asymptomatic women. In the latter cases, the trichomonads are often sparser because they prefer a more alkaline pH. Trichomoniasis is most often associated with intermediate vaginal microbiota as defined by Nugent criteria, raising the possibility that T. All of these tests are currently licensed only for vaginal specimens, can be used as point of care tests, and have sensitivities of about 80%. Diagnosis in general is much more difficult for males, with the best culture results obtained by combining urethral swabs and urine sediment into one specimen. Failure to treat the male sexual partner is likely the most common cause of recurrent disease in women and should be explored before assuming that the woman has a strain of T. Although there continues to be some controversy about the safety of metronidazole in pregnancy, there has never been a documented case of fetal malformation attributed to its use, even when it is used in the first trimester. However, there does not appear to be a definitive correlation between in vitro and in vivo resistance. Some authorities have recommended higher doses of oral medication in combination with pharmacy-prepared intravaginal preparations. Tinidazole, with its more favorable pharmacokinetics, may be the drug of choice when resistance is encountered. The cure rate was 92% (22 of 24 patients); no patients discontinued therapy because of side effects. If their infection is left untreated, they may later become symptomatic and may continue to transmit the infection while untreated. In a large multicenter study, after adjusting for demographic, behavioral, and microbiologic variables, T. Prospective studies of treatment of trichomoniasis during pregnancy for the prevention of preterm birth have yielded disappointing results. Among women with asymptomatic infection treated with metronidazole during the second and third trimesters of pregnancy, a trend toward increased preterm delivery was seen compared with the placebo group. In addition, the study was stopped prematurely because of a slow accrual of subjects and the trend for increased risk for preterm delivery in the treatment group. However, this study was actually a subgroup analysis of a larger trial and was not properly designed to determine the effect of treatment of T. Trichomoniasis has also been associated with vaginal cuff cellulitis after abdominal hysterectomy. Chapter 280 Trichomonas vaginalis Key References the complete reference list is available online at Expert Consult. Unique vaginal microbiota that includes an unknown Mycoplasma-like organism is associated with Trichomonas vaginalis infection. Identification of Tritrichomonas foetus in sections of bovine placental tissue with monoclonal antibodies. Proliferative response of human lymphocytes to secretory and cellular antigens of Trichomonas vaginalis.
Purchase trihexyphenidyl 2mg without prescription
Another cost-effectiveness analysis suggested that the clinical and economic benefits of minocycline-rifampin catheters increase with days of catheterization pain after treatment for uti effective 2 mg trihexyphenidyl. Halton and Graves427 reviewed a series of cost-effectiveness studies in 2007 and concluded that use of antibiotic-coated catheters, compared with use of either antiseptic-coated or standard catheters, was both clinically effective and cost-saving. We believe that antiinfective catheters should be implemented only as part of a comprehensive nosocomial bacteremia prevention strategy, which also includes education of staff and adequate skin antisepsis. Further research is needed to define the actual effect of these catheters on bacteremia rates, as well as the most efficacious catheters for different durations of catheterization and different subpopulations of patients. Use of heparin or other anticoagulants has also been advocated as a method for reducing both thrombotic and infectious complications of central venous catheterization. Several anticoagulants have been suggested for use in this setting, and Randolph and coworkers429 noted that cost-effectiveness comparisons of these several preparations. Recombinant tissue plasminogen activator used once weekly instead of heparin three times per week significantly reduced the incidence of both catheter malfunction and bacteremia in another study. Currently, we do not recommend routine use of urokinase or other thrombolytic agents as adjunctive therapy in patients with catheter-related bacteremia. The role of appropriate nurse staffing in preventing catheter-associated infection deserves attention. Increased attention to such details can significantly lower the endemic rate of device-associated infection as well as decrease the number of epidemics of such infections. Sources and outcomes of bloodstream infections in cancer patients: the role of central venous catheters. The impact of hospital practice on central venous catheter associated bloodstream infection rates at the patient and unit level: a multicenter study. Causative organisms and associated antimicrobial resistance in healthcare-associated, central line-associated bloodstream infections from oncology settings, 2009-2012. Short-term peripheral venous catheter-related bloodstream infections: a systematic review. Central line-associated bloodstream infections caused by Staphylococcus aureus in cancer patients: clinical outcome and management. Anti-infective locks for treatment of central line-associated bloodstream infection: a systematic review and meta-analysis. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. A central line care maintenance bundle for the prevention of central line-associated bloodstream infection in non-intensive care unit settings. Continuous passive disinfection of catheter hubs prevents contamination and bloodstream infection. Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. The influence of the composition of the nursing staff on primary bloodstream infection rates in a surgical intensive care unit. Preventing hospital-acquired infections: a national survey of practices reported by U. Sepsis arising from extrinsic contamination of the infusion and measures for control. Impact of mandatory public reporting of central line-associated bloodstream infections on blood culture and antibiotic utilization in pediatric and neonatal intensive care units. Impact of penalties for central line-associated bloodstream infections on blood culture ordering. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Bacteremic sepsis in intensive care: temporal trends in incidence, organ dysfunction, and prognosis. Scanning and transmission electron microscopy of in situ bacterial colonization of intravenous and intraarterial catheters. A prospective study of the mechanisms of infection associated with hemodialysis catheters. Pathogenesis of catheter sepsis: a prospective study with quantitative and semiquantitative cultures of catheter hub and segments. Nationwide epidemic of septicemia caused by contaminated intravenous products: I: epidemiologic and clinical features. Indwelling arterial catheters as a source of nosocomial bacteremia: an outbreak caused by Flavobacterium species. Investigation of an outbreak of central venous catheter-associated bloodstream infection due to contaminated water. Serratia marcescens bacteremia because of contaminated prefilled heparin and saline syringes: a multi-state report. Nosocomial outbreak of Candida parapsilosis fungemia related to intravenous infusions. An outbreak of Candida parapsilosis bloodstream infections in patients receiving parenteral nutrition. Hub colonization as the initial step in an outbreak of catheter-related sepsis due to coagulase negative staphylococci during parenteral nutrition. A clinical trial on the prevention of catheter-related sepsis using a new hub model. Evaluation of dressing regimens for prevention of infection with peripheral intravenous catheters: gauze, a transparent polyurethane dressing, and an iodophor-transparent dressing. Health care-associated bloodstream infections associated with negative- or positive-pressure or displacement mechanical valve needleless connectors. Outbreak of bloodstream infection temporally associated with the use of an intravascular needleless valve. A randomized, prospective clinical trial to assess the potential infection risk associated with the PosiFlow needleless connector. Bloodstream infections associated with a needleless intravenous infusion system in patients receiving home infusion therapy. Bloodstream infection associated with needleless device use and the importance of infection-control practices in the home health care setting. Line-associated bloodstream infections in pediatric intensive-care-unit patients associated with a needleless device and intermittent intravenous therapy. Adequate disinfection of a split-septum needleless intravascular connector with a 5-second alcohol scrub. Comparison of a silver-coated needleless connector and a standard needleless connector for the prevention of central line-associated bloodstream infections. A successful approach to reducing bloodstream infections based on a disinfection device for intravenous needleless connector hubs. Meta-analysis on central line-associated bloodstream infections associated with a needleless intravenous connector with a new engineering design. Serial surveillance cultures of skin and catheter hub specimens from critically ill patients with central venous catheters: molecular epidemiology of infection and implications for clinical management and research. Outbreak of Staphylococcus epidermidis nosocomial infections in patients receiving total parenteral nutrition. Relevance of the catheter hub as a portal for microorganisms causing catheter-related bloodstream infections. Rapid diagnosis of intravascular catheter-associated infection by direct Gram-staining of catheter segments. Prospective randomized trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. The pathogenesis and epidemiology of catheter-related infection with pulmonary artery Swan-Ganz catheters: a prospective study utilizing molecular subtyping. Molecular epidemiology of coagulase-negative staphylococci isolated from immunocompromised patients. Eliminating central line-associated bloodstream infections: a national patient safety imperative. National estimates of central line-associated bloodstream infections in critical care patients.
Order trihexyphenidyl 2mg otc
This definition requires a consideration of the factors necessary for disease induction that include dose pain treatment center hartford hospital buy trihexyphenidyl with mastercard, host susceptibility, presence of a pathogen, virulence of a pathogen, and the most commonly absent factor, a portal of entry. For waste to be infectious, therefore, it must contain pathogens with sufficient virulence and quantity that exposure to the waste by a susceptible host could result in an infectious disease. Not only were the majority of hospitals in compliance, but the hospitals frequently treated other hospital waste as infectious, including contaminated laboratory waste (87%), surgery waste (78%), dialysis waste (69%), items contacting secretions (63%), intensive care unit waste (37%), and emergency room waste (41%). No changes in procedures for cleaning, disinfecting, or sterilizing need to be made. It affected only four states (New Jersey, New York, Connecticut, and Rhode Island). The Act required both treatment (any method, technique, or process designed to change the biologic character or composition of medical waste so as to eliminate or reduce its potential for causing disease) and destruction (waste is ruined, torn apart, or mutilated so that it is no longer generally recognizable as medical waste). This term includes stocks and cultures of etiologic agents and microbiology laboratory waste contaminated with etiologic agents. The Act regulated wastes from persons with highly communicable diseases such as class 4 etiologic agents. Several other nonincineration alternatives have been proposed for treating regulated medical waste. Nonregulated medical waste is generally discarded in a properly sited and operated sanitary landfill because this is a safe and inexpensive disposal method. The conflicting information in state and federal regulations is related to the paucity of microbiologic and epidemiologic evidence that medical waste represents a threat to public health. First, with the exception of "sharps" such as needles, which have caused disease only in an occupational setting, there is no scientific evidence that medical waste has caused disease in the hospital or the community. Second, data demonstrate that household waste contains on average of 100 times as many microorganisms with pathogenic potential for humans than medical waste. However, current disinfection and sterilization guidelines must be strictly followed. Powell for recovering papers on disinfection and sterilization in the peer-reviewed literature from 2012 through 2017. Multi-society guideline on reprocessing flexible gastrointestinal endoscopes, 2016. Efficacy of improved hydrogen peroxide against important healthcare-associated pathogens. Occupational risks associated with the use of selected disinfectants and sterilants. The effect of blood on the antiviral activity of sodium hypochlorite, a phenolic, and a quaternary ammonium compound. Bactericidal, virucidal, and mycobactericidal activities of reused alkaline glutaraldehyde in an endoscopy unit. Comparison of liquid chemical sterilization with peracetic acid and ethylene oxide sterilization for long narrow lumens. Guideline for disinfection and sterilization of prion-contaminated medical instruments. Special problems associated with reprocessing instruments in outpatient care facilities. Susceptibility of high-risk human papillomavirus type 16 to clinical disinfectants. Effective high-level disinfection of cystoscopes: is perfusion of channels required Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Use of a daily disinfectant cleaner instead of a daily cleaner reduced hospital-acquired infection rates. Susceptibility of antibiotic-susceptible and antibiotic-resistant hospital bacteria to disinfectants. Use of germicides in the home and the healthcare setting: is there a relationship between germicide use and antibiotic resistance Outbreaks of carbapenem-resistant Enterobacteriaceae infections associated with duodenoscopes: what can we do to prevent infections Transmission of infection by flexible gastrointestinal endoscopy and bronchoscopy. Endoscope reprocessing methods: a prospective study on the impact of human factors and automation. Murray P Preventable tragedies: Superbugs and how ineffective monitoring of medical device safety fails patients. Disinfection and sterilization in health care facilities: an overview and current issues. Evaluation of the ability of different detergents and disinfectants to remove and kill organisms in traditional biofilm. Comparison of ion plasma, vaporized hydrogen peroxide, and 100% ethylene oxide sterilizers to the 12/88 ethylene oxide gas sterilizer. Efficacy of a washer-disinfector in eliminating healthcare-associated pathogens from surgical instruments. Monitoring and improving the effectiveness of cleaning medical and surgical devices. High-level disinfection, sterilization, and antisepsis: current issues in reprocessing medical and surgical instruments. Healthcare outbreaks associated with a water reservoir and infection prevention strategies. Cleaning and disinfection of fiberoptic endoscopes: evaluation of glutaraldehyde exposure time and forced-air drying. The role of patient care items as a fomite in healthcare-associated outbreaks and infection prevention. Contaminated portable equipment is a potential vector for dissemination of pathogens in the intensive care unit. Quantitative assessment on interactions between hospitalized patients and portable medical equipment and other fomites. Evaluation of hospital floors as a potential source of pathogen dissemination using a nonpathogenic virus as a surrogate marker. Feasibility of a combined carrier test for disinfectants: studies with a mixture of five types of microorganisms. Antimicrobial activity of home disinfectants and natural products against potential human pathogens. Efficacy of improved hydrogen peroxide against important healthcareassociated pathogens. Surface disinfection: treatment time (wipes and sprays) versus contact time (liquids). Efficacy of different cleaning and disinfection methods against Clostridium difficile spores: importance of physical removal versus sporicidal inactivation. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. An increase in healthcare-associated Clostridium difficile infection associated with use of a defective peracetic acid-based surface disinfectant. Cleaning and disinfecting environmental surfaces in health care: toward an integrated framework for infection and occupational illness prevention. A note on the fallacy of using alcohol for the sterilization of surgical instruments. Bacterial contamination of keyboards: efficacy and functional impact of disinfectants.
Purchase 2 mg trihexyphenidyl mastercard
Another factor influencing the pathogenesis of infusate-associated infection is the composition of the fluid pain treatment for labor order trihexyphenidyl 2mg visa. The microbiology of outbreaks of infusate-related sepsis is somewhat monotonous; pathogens such as Enterobacter, Citrobacter, and Serratia predominate. No infusate is entirely free of risk; even sterile water for injection can support the growth of Burkholderia cepacia. A randomized study examining the effects of a redesigned protective hub found these hubs to be associated with a significantly lower rate of catheter sepsis and culture-positive catheter hubs,31 suggesting that the hub is a common portal of entry for bacteria. Other investigators have incriminated the hub-tubing junction (particularly when it does not allow a good fit) in the pathogenesis of epidemics of coagulase-negative staphylococcal infection. Sherertz36 estimated that the hub, lumen, or both contributed two-thirds of the microorganisms that infected long-term catheters and that one-fourth of the microorganisms were from the skin. Conversely, some newer technologies may be associated with increased risks for catheter-associated infection. Needleless intravenous systems were developed to provide a safer workplace environment for health care providers, and needle-free devices now constitute more than 80% of access devices and are recommended for all tubing/catheter access. Similarly, Safdar and Maki55 determined that most catheter-related bacteremias occurring with short-term noncuffed central catheters were extraluminally acquired and derived from the cutaneous microflora. Atela and coworkers49 conducted a prospective study to assess the turnover of superficial skin colonization by performing serial quantitative cultures of skin and the catheter hub. Strains recovered from the targeted superficial skin sites demonstrated a poor correlation both with strains from previous skin cultures and with catheter tip isolates. Herwaldt and colleagues examined the source of coagulase-negative staphylococcal bacteremias in hematology-oncology patients and found that the same strain was identified in both skin and blood cultures in only 6 of 20 episodes. Of importance, these investigators were unable to identify colonization with the same strain for the majority of bacteremias; only 4 of the 21 nosocomial bloodstream infections were preceded by colonization with the same strain. Most nosocomial coagulase-negative staphylococcal bacteremias in this study appeared to result from extrinsic introduction of the organism. Contamination of Skin at the Device Insertion Site (Extraluminal Source) Granulocytopenia Immunosuppressive chemotherapy Hematologic malignancy (versus solid tumor)440 Loss of skin integrity. Manipulating the system for repositioning, for obtaining a sample, or for any other reason increases the likelihood that the catheter may become contaminated. The physician cannot alter most such patient-related factors; however, these data can be used when evaluating the risks associated with, the necessity for, and the duration of intravenous therapy. Several catheter characteristics or properties have been suggested to be associated with an increased risk for catheter-associated infection. Catheters that irritate the vascular intima and provoke thrombogenesis and catheters that are made of intrinsically thrombogenic materials are likely to be associated with an increased risk for device-associated infection. A clear association has been established between the thrombogenicity of a catheter and the risk for device-associated infection. Because of methodologic difficulties in performing appropriate scientific studies to characterize relative risk, many of these risk factors have been identified either retrospectively or in the epidemic setting. In a rabbit model, silicon catheters are easier to infect with Staphylococcus aureus than are those made of polyurethane, Teflon, or polyvinyl chloride. Similarly, increasing the number of lumens in a catheter has been suggested to increase the risk for catheter-associated infections. Several studies have suggested that the use of multiple-lumen catheters is associated with an increased risk for catheter-associated infection compared with the use of single-lumen catheters,42,91,92 although not all studies have found this difference. Formation of a bacterial biofilm is now thought to be a virtually universal phenomenon that begins within 3 days after insertion of intravascular devices. For example, risks for infection with pulmonary artery catheters may be higher because of the manner in which they are used. They are frequently repositioned to obtain accurate readings, they are used to obtain samples for the measurement of cardiac output, and they can be used to obtain mixed venous blood to measure oxygen and carbon dioxide tensions. Catheter management, including both insertion and maintenance, also may influence risk for infection. Several studies have shown that catheters placed by less experienced personnel are at increased risk for infection. In contradistinction to the patient-related factors, such hospitalrelated factors can often be altered for patient benefit. Nurse staffing variables, including nurse-to-patient ratio, level of training, and permanent assignment to the unit ("float" nurse vs. One study of patients with hematologic malignancies and having Hickman catheters inserted identified a predominance of gram-negative organisms (68%) causing catheter-related bacteremias in this nonneutropenic population. Serratia marcescensb Candida albicansc Candida tropicalisc Pseudomonas aeruginosad Klebsiella spp. In addition to the presence of an indwelling intravascular device, several clinical features should alert the physician to the possibility of device-associated bacteremia. Salient features of device-associated sepsis that help distinguish it from other bacteremic syndromes are listed in Table 300. In general, blood culture results positive for coagulase-negative staphylococci, S. Although none of these criteria specifically identifies the intravascular device as the source of sepsis, the presence of these clinical findings should at least raise the possibility of device-associated bacteremia. Cultures of the catheter tip have been reported to be of variable and limited value. Catheter tip cultures should not be performed for diagnosis of bacteremia related to subcutaneous venous ports; instead, culture of the material inside the port reservoir is more sensitive. The authors noted that most infected catheters yield confluent growth when using the semiquantitative technique. Given the current differences in microbiology and in intravascular devices now in use, these studies are less relevant in the 21st century than they were 40 years ago. Cleri and coworkers149 reported a technique for quantitatively culturing catheters in broth. This system, which is slightly more cumbersome for the laboratory, was considered by these authors to have three advantages over the system described by Maki and colleagues: (1) the ability to detect organisms within the lumen, (2) the ability to evaluate relative numbers of organisms from different catheter segments, and (3) the ability to compare relative numbers of organisms present in mixed infections. The latter authors advocated the use of semiquantitative cultures because of the ease with which this test is performed. Siegman-Igra and colleagues154 conducted a meta-analysis of catheter culturing techniques and suggested that the accuracy increases for catheter segment cultures with increasing quantitation. The increase in accuracy is primarily due to the increased specificity of the more quantitative tests. They found that quantitative catheter segment culture was the only method associated with sensitivity and specificity greater than 90%. Safdar and colleagues156 also found that qualitative culture of the catheter segment was the least accurate of the tests they studied, primarily because of poor specificity. Although the relative merits of these various procedures remain to be definitively delineated, the ease of performing the semiquantitative technique described by Maki and coworkers144,145 has kept this procedure in widespread clinical use. Kite and colleagues159 have published a description of an endoluminal brush method, suggesting that this procedure can be used without sacrificing the intravascular line. Although these authors suggest that the procedure is substantially more sensitive and more specific than the semiquantitative technique, only 1% of 692 infectious disease physician survey respondents recently reported using this method. Whereas several additional studies have underscored the usefulness of the Isolator system, one study has suggested that results obtained with traditional blood cultures may be complementary to those obtained with the Isolator system and that, whenever feasible, both approaches should be used. They determined that quantitative or semiquantitative culture of the catheter, combined with two blood cultures (one peripheral and one through the catheter), is most accurate for short-term central catheters. As noted previously, several studies have recommended a differential comparison of quantitative cultures obtained peripherally and quantitative cultures obtained by drawing blood back through the suspected catheter to document the occurrence of catheter-acquired sepsis. In addition, despite the evidence that quantitative blood cultures are useful in diagnosing intravascular catheter bacteremias, many clinical microbiology laboratories do not offer this service because of the cost and complexity.