Discount 0.5mg requip free shipping
Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in five of nineteen patients administering medications 7th edition ebook cheap requip 0.5mg on line. Comparison of 2 techniques to predict voiding efficiency after inpatient urogynecologic surgery. Massive eversion of the vagina: pathogenesis, diagnosis, and therapy of the "true" prolapse of the vaginal stump. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Laparoscopic sacrocervicopexy for the treatment of uterine prolapse: a retrospective case series report. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. The standardization of terminology for researchers in female pelvic floor disorders. Lentz the gynecologist frequently consults on and treats urologic problems in the female patient. Perhaps the most commonly seen of these problems involves infection and inflammation of the lower tract. Various prevalence studies have reported that approximately 30% of women noted some degree of incontinence during the preceding 12 months. Ten percent of women suffer from weekly incontinence, and 5% have daily incontinence. Urinary incontinence problems increase in incidence with age and, because the number of older women in our population is increasing, this problem is growing in magnitude. A survey of pelvic floor disorders by (Nygaard, 2008) found at least one pelvic floor disorder in 24% of women. At least monthly urine leakage was reported by 7% of women ages 20 to 39, 17% ages 40 to 59, 23% ages 60 to 79, and 32% 80 years of age and older. This study may actually underpredict the prevalence of these disorders because women in the survey may have been successfully treated and not counted. Overweight and obese women were more likely to report urinary incontinence than women of normal weight. Continence depends on a number of factors, including the neurologic control of micturition, the anatomic relationships of the urinary tract, and the specific effects of a number of systemic, infectious, and neoplastic conditions. Older women have additional challenges to the urinary system with comorbid medical conditions, ambulatory difficulties, and cognitive impairments. Not only does the prevalence of urinary incontinence increase with age, but so does the severity. Incontinence has been associated with depression, increased social isolation, falls, hip fractures, and admission to nursing homes, which has additional morbidity. Furthermore, incontinence decreases quality of life 474 and increases costs to society. This chapter discusses the physiology of normal micturition as well as the evaluation and treatment of female lower urinary tract conditions. It is a balance between bladder storage, which is organized primarily in the spinal cord and coordinates urethral closure and detrusor relaxation, and micturition, which is controlled by reflex mechanisms mediated by the brain. Voluntary voiding is a learned function and is not automatic, like heart rate control. Bladder detrusor contractility is stimulated by the activity of the parasympathetic nervous system, mediated primarily through the neurotransmitter acetylcholine. This stimulates muscarinic (primarily M3) receptors in the bladder wall, which then activate detrusor contraction. Sympathetic nerve receptors within the bladder cause bladder relaxation when stimulated. Bladder contraction may also be affected by irritation and inflammation of the bladder wall lining, causing uninhibited contractions. Inhibitory input to the urethral smooth muscle is conveyed by nitric oxide via parasympathetic nerves. Somatic cholinergic motor nerves supply the striated muscles of the external urethral sphincter from the sacral spinal cord. The act of voiding is under the control of four basic autonomic and somatic nervous system feedback loops. The parasympathetic system is involved in the act of voiding via nuclei in S2 through S4 (micturition center) and mediates its activity through the neurotransmitter acetylcholine, directly stimulating muscarinic receptors in the bladder wall. This signal is transmitted via the pelvic nerve and causes the detrusor to contract. Norepinephrine is secreted via this system, stimulating both - and -adrenergic receptors. The bladder contains primarily receptors, stimulation of which causes relaxation of the detrusor muscle. Estrogen and progesterone receptors are present in the bladder and urethra, although their role in affecting continence has not been fully elucidated. Because the neurogenic control of micturition is so complex and depends on the interaction of so many factors, it is understandable that a host of general systemic diseases or diseases involving the nervous system may affect bladder control. These include, but are not limited to , diabetes mellitus, vascular diseases, obesity, cognitive disorders, normal pressure hydrocephalus, demyelinating diseases. The system can be disrupted by a stroke, which is a suprapontine lesions leading to loss of central inhibition, resulting in detrusor overactivity and reemergence of reflex micturition. A spinal cord injury above the lumbosacral level eliminates voluntary control of voiding, leading to acute urinary retention. Later, neurogenic detrusor overactivity occurs from spinal reflex pathways, which are uncoordinated, so the urethral sphincter may not relax simultaneously, leading to detrusorsphincter dyssynergia. Urinary incontinence in the elderly: physiology, pathophysiology, diagnosis, and treatment. Parasympathetic fibers arising in S2-S4 have long preganglionic fibers and pelvic ganglia close to the bladder and urethra. Sympathetic fibers that have long postganglionic fibers discharge norepinephrine to receptors, primarily in the bladder, and receptors, primarily in the urethra. A radical hysterectomy or subsacral cauda equine lesion might disrupt the local reflexes and lead to overflow incontinence because of detrusor and sphincter hyporeflexia. Compounds with atropine-like effects may interfere with the initiation of micturition, whereas those with cholinergic effects may cause bladder overactivity (Table 21. In summary, bladder control depends on the ability of the bladder to store urine under low pressure, which involves inhibition of the detrusor muscle and contraction of the smooth and striated urethral sphincters. Emptying the bladder requires coordination with pelvic floor and urethral sphincter relaxation and detrusor contraction. For urine to pass through the urethra, the maximum urethral pressure must be lower than the intravesical pressure. Intravesical pressure depends on the following: (1) the volume of fluid in the bladder, (2) the part of the intraabdominal pressure transmitted to the bladder, and (3) the tension in the bladder wall related to muscular and nervous system activity and elastic properties. The resting pressure in the bladder is between 20 and 30 cm H2O due to surrounding intraabdominal pressure with little or no pressure added from tension in the bladder wall in normal bladders. The intraurethral pressure depends on the following: (1) striated muscle fibers of the urethral wall, (2) smooth muscle fibers of the urethral wall (a circular and longitudinal layer), (3) vascular content of the urethral submucosal cavernous plexus, (4) passive elasticity of the urethral wall, and (5) the part of the intraabdominal pressure transmitted to the urethra. The urethra has primarily receptors from the sympathetic nervous system, which, when stimulated, cause contraction of the urethral sphincter. The urethral smooth and striated (skeletal) muscles add to the resting urethral tone, whereas the skeletal fibers react when intraabdominal pressure rises, such as with a cough. Anatomically, the exact border between the bladder and urethra is difficult to determine. The functional length of the urethra, however, is that part in which the urethral pressure exceeds the bladder pressure. Urethral pressure varies with age, increasing up to the age of 20 years and then gradually decreasing until menopause. Asmussen and Ulmsten (1976) have demonstrated that the highest pressure zone in the urethra is approximately at the midpoint of the functional urethral length. The submucosal cavernous plexus of vessels, the bulk of the smooth and striated muscle, and the bulk of the autonomic nerve supply are most prominent in the area in which they record the maximum urethral pressure. Urethral pressure can oscillate as much as 25 cm H2O in young women but seldom more than 5 cm H2O in postmenopausal women (Enhorning, 1961). Thus not only is the epithelium of the bladder and bladder neck dependent on hormone stimulation, but probably so is the vascular system of these areas. DeLancey made some interesting observations on functioning periurethral anatomy by studying serial histologic sections of intact pelvic viscera and surrounding tissue and by dissecting 22 fresh and embalmed cadavers (DeLancey, 1986).
Purchase requip on line
Breasts Absent and Uterus Present It would seem logical treatment uterine fibroids requip 1 mg on line, as breast development is a biomarker of ovarian estrogen production, that individuals with no breast development and a uterus present have no estrogen production. The phenotype of individuals with either of these causes of low estrogen status is similar. Gonadal Failure (Hypergonadotropic Hypogonadism) Failure of gonadal development is the most common cause of primary amenorrhea, occurring in almost 50% of those with this symptom. Gonadal failure is most frequently caused by a chromosomal disorder or deletion of all or part of an X chromosome, but it is sometimes caused by another genetic defect and, rarely, 17-hydroxylase deficiency. The chromosomal disorders are usually caused by a random meiotic or mitotic abnormality. Reindollar reported that all individuals with gonadal failure and an X chromosome abnormality were shorter than 63 inches in height (Reindollar, 1981). Deletion of the entire X chromosome (as occurs in Turner syndrome) or of the short arm (p) of the X chromosome results in short stature. When ovarian follicles are absent, synthesis of ovarian steroids and inhibin does not occur. Turner syndrome occurs in approximately 1 per 2000 to 3000 live births but is much more frequent in abortuses. In addition to primary amenorrhea and absent breast development, these individuals have other somatic abnormalities, the most prevalent being short stature (<60 inches in height), webbing of the neck, a short fourth metacarpal, and cubitus valgus. Cardiac abnormality, renal abnormalities, and hypothyroidism are also more prevalent. In addition, individuals with 45,X Anomalies Obstetrics & Gynecology Books Full 38 Primary and Secondary Amenorrhea and Precocious Puberty 833 Box 38. In top and center panels, sleep histogram is shown above period of nocturnal sleep. These individuals are generally taller and have fewer anatomic abnormalities than individuals with a 45,X karyotype. In addition, some of them may have a few gonadal follicles and approximately 20% have sufficient estrogen production to menstruate. Isolated phenotypic features of Turner syndrome (without gonadal failure) may also occur in males and is known as Noonan syndrome. Abnormal Sexual Development: A Genetic and Endocrine Approach to Differential Diagnosis. However, if there is deletion of the short arm of the X chromosome (Xp), the individual will be short. A similar phenotype occurs in those with isochrome of the long arm of the X chromosome. Abnormalities in genes involved in gonadal development are expected to be involved. These individuals have normal stature and phenotype, absence of secondary sexual characteristics, and primary amenorrhea. Some of these women have a few ovarian follicles, develop breasts, and may even menstruate spontaneously for a few years. There can be incomplete forms with some degree of testicular tissue, but in this context the "pure" form as a dysgenetic streak as in other forms of ovarian dysgenesis and previously has been referred to as Swyer syndrome. Many of these lesions, particularly pituitary adenomas, result in elevated prolactin levels (see Chapter 39). Only a few such individuals have been described in the literature, but it is important for the clinician to be aware of this entity because, in contrast to those described earlier, these individuals have hypernatremia and hypokalemia. The mineralocorticoid levels are also elevated, because 17-hydroxylase is not necessary for the conversion of progesterone to deoxycortisol or corticosterone. Thus there is excessive sodium retention and potassium excretion, leading to hypertension and hypokalemia. Serum progesterone levels are also elevated because progesterone is not converted to cortisol. In addition to sex steroid replacement, these individuals need cortisol administration. Genetic Disorders with Hyperandrogenism Hyperandrogenism occurs in approximately 10% of women with gonadal dysgenesis. Females with Kallmann syndrome and related forms of gonadotropic deficiency have normal height and an increase in growth of long bones, resulting in a greater wingspan-to-height ratio. Men affected by gonadotropic deficiency have hypogonadism, an increased wingspan-to-height ratio, and altered spatial orientation abilities. Anosmia in Kallmann syndrome must be tested for by blinded testing of certain characteristic smells, such as coffee, cocoa, or orange. They almost always have an associated disorder such as thalassemia major (with iron deposits in the pituitary) or retinitis pigmentosa. Occasionally, this pituitary abnormality has Obstetrics & Gynecology Books Full 38 Primary and Secondary Amenorrhea and Precocious Puberty been associated with prepubertal hypothyroidism, kernicterus, or mumps encephalitis. Estrogen Resistance 835 this rare condition was first described in men and now has been described in a woman (breast absent, uterus present. Endogenous estrogen levels are high, gonadotropins are higher than the normal range (to try to provoke an estrogen response), and the ovaries are cystic. Exogenous estrogen does not normally induce changes except minimal changes with very high pharmacologic doses (Quaynor, 2013). Breast Development Present and Uterus Absent Two disorders present with primary amenorrhea are associated with normal breast development and an absence of a uterus: androgen resistance and congenital absence of the uterus. The former is a genetically inherited disorder, whereas the latter is an accident of development and does not have an established pattern of inheritance. Currently, however, some families choose to have full disclosure and a complete understanding of the abnormality. In addition, because psychologically and phenotypically these individuals are female and have been raised as such, the term gonads should be used instead of testes. These individuals should also be informed that they can never become pregnant because they do not have a uterus and that their gonads must be removed after age 18 because of their high potential for malignancy. The syndrome is caused by the absence of an X-chromosome gene responsible for cytoplasmic or nuclear testosterone receptor function. It is an X-linked recessive or sex-linked autosomal dominant disorder, with transmission through the mother. However, because of a lack of receptors in target organs, there is lack of male differentiation of the external and internal genitalia (Gustafson, 1994). Wolffian duct development, which normally occurs as a result of testosterone stimulation, fails to take place. Thus women with this disorder have no female or male internal genitalia, normal female external genitalia, and a short or absent vagina. Pubic hair and axillary hair are absent or scanty as a result of a lack of androgenic receptors, but breast development is normal or enhanced. Thus in androgen resistance, the absence of androgen action allows even low levels of estrogen to cause unabated breast stimulation. Testes that are intraabdominal or that occur in the inguinal canal have an increased risk of developing a malignancy (gonadoblastoma or dysgerminoma), with an incidence reported to be approximately 20%. Therefore it is usually recommended that the gonads be left in place until after puberty is completed to allow full breast development and epiphyseal closure to occur. After these events occur, which is typically around age 18, the gonads should be removed. It is recommended that those with androgen the Hox genes are important for uterine development, and mutations.
Diseases
- Camptodactyly fibrous tissue hyperplasia skeletal dysplasia
- Banki syndrome
- Osteopetrosis, (generic term)
- Kotzot Richter syndrome
- Chromosome 11-14 translocation
- Cowpox
Cheap 0.5 mg requip amex
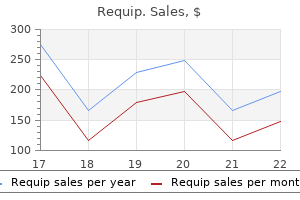
Obstetrics & Gynecology Books Full 33 Neoplastic Diseases of the Ovary Screening symptoms 6 year molars purchase requip discount, Benign and Malignant Epithelial and Germ Cell Neoplasms, Sex-Cord Stromal Tumors Robert L. Gershenson Ovarian cancer is the second most common malignancy of the lower part of the female genital tract, occurring less frequently than cancers of the endometrium but more frequently than cancers of the cervix. However, it is the most frequent cause of death from gynecologic neoplasms in the United States. Cancer Statistics 2015 has reported that approximately 21,290 new cases of ovarian cancer will be diagnosed yearly in the United States, and there will be 14,180 deaths. A major contributing factor to the high death rate from the relatively few cases stems from the frequent detection of the disease after metastatic spread when symptoms direct clinical investigation or raise clinical concern. Surprisingly, most women diagnosed with ovarian cancer do report symptoms for months before diagnosis. As detailed later, only the severity and duration of symptoms differentially segregate cancer patients from noncancer patients. Ovarian cancer in the elderly: an analysis of Surveillance, Epidemiology, and End Results Program data. Despite numerous epidemiologic investigations, a clear-cut cause of ovarian cancer has not been defined. It is thought that these malignancies are related to frequent ovulation, and therefore women who ovulate regularly appear to be at higher risk. Included are those with a late menopause, history of nulliparity, or late childbearing. Conversely, women who have had several pregnancies or who have used oral contraceptives appear to have some protection against ovarian cancer. Casagrande and colleagues related the development of ovarian cancer to ovulatory age-that is, the number of years during which the woman has ovulated. This number would be reduced by pregnancy, breast-feeding, or oral contraceptive use. Schildkraut and associates correlated overexpression of mutant p53 protein in ovarian cancers with reproductive histories and found that overexpression was more likely in those who had high ovulatory cycle histories. In addition, talcum powder used on the perineum has been postulated to increase the risk but, as noted by Cramer and coworkers, it is a weak association. The use of oral contraceptives decreases the risk by approximately 50% after 5 years of use (approximately 10% to 12%/year). The protection increases with duration of use to 10 years and appears to last for approximately 15 years after discontinuation of use. Schlesselman has calculated a decrease of 369 ovarian cancer cases/100,000 women for 8 years of use. Given that the approximate occurrence of ovarian cancer cases in this group would be expected to be1400, such a decrease approximates 25%. Breastfeeding, pregnancy, tubal ligation, and, to a lesser extent, hysterectomy with ovarian preservation also lower the risk of ovarian cancer. It has been suggested that ovulation-inducing drugs such as clomiphene citrate increase the risk of ovarian cancer, as noted by Whittemore and colleagues. Rossing and coworkers reported an increase in risk from a population-based study that suggested that the risk is associated with prolonged use of clomiphene insofar as no association was noted with less than 1 year of use. The study was significant but had wide 95% confidence limits, and only 11 cancer cases occurred in the clomiphene group among 3837 women studied in the infertility clinic. Mahdavi and colleagues assembled a review of cohort and case-control studies evaluating the relationship of fertility agents to ovarian cancer. In this report, little evidence supported the hypothesis that ovulation induction substantially increases cancer risk. Furthermore, a large population-based Danish cohort study also failed to demonstrate any increased risk of ovarian cancer among 54,362 women seeking consultation relating to fertility problems. Agents evaluated in this study were gonadotropins, clomiphene citrate, human chorionic gonadotropin, and gonadotropin-releasing hormone. Additionally, no associations were found between these agents and the number of cycles of use, parity, or length of follow-up. However, three reports specifically evaluating the association of these agents and the development of borderline tumor or low malignant potential tumors have suggested that a relationship may exist. The frequent presence of hormone receptors in these lesions, as well as the hyperestrogenic microenvironment, may support this observation. Cramer and coworkers found women with ovarian cancer to have a diet high in animal fat in compared with control subjects, and studies of Risch and associates suggested that saturated fat increases the risk of ovarian cancer, whereas vegetable fiber may reduce it. There are geographic and racial differences in the distribution of ovarian cancers. These cancers occur most frequently in industrialized and affluent countries such as the United States and Western Europe and less frequently in Asia and Africa. Finally, patients with ovarian carcinoma have an increased risk of developing breast and endometrial cancer. Notwithstanding the familial syndromes, major factors appear to be related to the frequency of ovulation and residence in an industrialized country. Risk alteration in these patients through oral contraceptive use is of uncertain impact. Narod and coworkers suggested that it might be possible to reduce incident risk by their administration. Hereditary ovarian cancers are uncommon, accounting for approximately 10% to 15% of all incident cases. However, identification of affected or unaffected women with significant familial risk is important, given their accelerated risk of ovarian and other cancers. In addition, these patients are frequently diagnosed at a younger age (median, 50 years), and unaffected individuals are able to consider prophylactic procedures that can affect their lifetime risk. The term familial ovarian cancer denotes an inherited trait that predisposes to ovarian cancer development. A first-degree relative is a mother, sister, or daughter of an affected individual. As noted in the review by Kerlikowske and colleagues, previous studies suggested an increase from approximately 1. For the woman with a familial history of ovarian cancer (not the dominant genetic hereditary type), periodic surveillance with transvaginal ultrasonography 6 months after the age of 35 years has been suggested (see the ultrasonography discussion presented later in this chapter). Unfortunately, such a strategy has not been shown to be worthwhile or cost effective in disease prevention and may, on occasion, lead to additional tests or unnecessary procedures when a questionable ultrasound result is. The use of prophylactic oophorectomy in patients whose mothers had ovarian cancer has been a controversial topic. Kerlikowske and colleagues and Herbst have provided reasons opposing the widespread use of this practice. However, the use of prophylactic oophorectomy to reduce the risk of ovarian or peritoneal cancer in mutation carriers may have validity. Finch and associates studied 1828 women enrolled in an international registry over an 11-year period ending in 2003. Lynch and associates reported on families with these hereditary ovarian cancers and Table 33. Decreases Breast-feeding Oral contraceptives Pregnancy Tubal ligation and hysterectomy, with ovarian conservation Obstetrics & Gynecology Books Full 33 Neoplastic Diseases of the Ovary study entry, and 783 (43%) did not undergo the procedure. It is reasonable that for patients with a significant family history in whom an operation such as hysterectomy is required, removal of both tubes and ovaries at the time of operation is appropriate. Similarly, mutation carriers who have finished childbearing may reduce their subsequent cancer risk by salpingo-oophorectomy. The recommendation for hysterectomy at this time is controversial but has been advocated by some to ensure complete removal of the fallopian tube (cornual segment). The woman must be aware that peritoneal carcinomatosis, a process resembling serous carcinoma of the ovary, can develop (rarely) despite the removal of both ovaries. Because evidence has suggested a significant proportion of ovarian carcinomas arise for preinvasive intraepithelial carcinomas in the fallopian tube, interest in a two-step approach to removal of the adnexa has arisen. Preserving ovarian function in high-risk women while mitigating risk via removal of the fallopian tubes has appeal for maintaining quality of life and avoidance of the risks from premature castration. Nevertheless, much is unknown regarding the efficacy and safety of this approach, including how strong is the risk mitigation and to what degree does retaining the ovary increase risk of breast cancer in these at-risk women. Fortunately, several prospective clinical trials are under way to address this novel approach to risk reduction surgery (Daly, 2015). The following describes the classification and histology of the major ovarian neoplasms. Pertinent microscopic findings, clinical behavior, and appropriate therapy are presented.
Cheap 1 mg requip overnight delivery
One example is small cell carcinoma medicine cabinets surface mount generic requip 0.25 mg on-line, which is a highly virulent cancer affecting primarily young women (discussed later). Metastatic tumors to the ovary may arise elsewhere in the reproductive tract or from distant sites such as the bowel or stomach (Krukenberg tumors). Tumor-like conditions refer to enlargements of the ovary, such as extensive edema, pregnancy luteoma, endometriomas, and follicular or luteal cysts, none of which are true neoplasms. With the exceptions of metastatic tumors and small cell carcinoma of the ovary, none of these are considered further in this chapter. Epithelial tumors can be categorized as benign (adenoma), malignant (adenocarcinoma), or of an intermediate form, known as borderline tumor or tumor of low malignant potential. The term papillary or the prefix cyst- (as in cystadenoma) is used when the tumor has, respectively, papillae or cystic Table 33. This classification, along with frequency of occurrence of the primary ovarian neoplasms, is shown in Table 33. Epithelial stromal tumors (common epithelial tumors) are the most frequent ovarian neoplasms. The suffix -fibroma (as in adenofibroma) is added when the ovarian stroma predominates, with the exception of a Brenner tumor, which normally contains a large amount of ovarian stroma. The malignant forms account for 40% or more of ovarian cancers, benign forms (serous cystadenomas) occur primarily during the reproductive years, borderline tumors occur in women 30 to 50 years of age, and carcinomas typically occur in women older than 40 years. Molecular investigation of genetic changes associated with lowgrade serous tumors support the reclassification of serous ovarian cancers into low- or high-grade binaries. Currently, a popular theory hypothesizes that high-grade serous carcinoma may arise from fallopian tube epithelium. These cells resemble cells of the endocervix or may mimic intestinal cells, which can pose a problem in the differential diagnosis of tumors that appear to originate from the ovary or intestine. Overall, they can account for approximately 25% of ovarian tumors and as many as 10% of ovarian cancers. In the ovary, these neoplasms are less frequent (approximately 5%) than serous or mucinous tumors, but the malignant variety accounts for approximately 20% of ovarian carcinomas. They may be seen in conjunction with endometriosis and ovarian endometriomas, although an origin from endometriosis is rarely demonstrated. Most endometrioid carcinomas arise directly from the surface epithelium of the ovary, as do the other epithelial tumors. Molecular evaluation of these tumors suggests a homology to similar pathology occurring in the kidney, which may have therapeutic implications. They may be considered unclassifiable if they cannot be placed in any of the categories shown in this table. A solid pattern of abundant polyhedral tumor cells containing abundant clear cytoplasm is present. Note the nest of transition-like epithelium containing spaces with eosinophilic material. Widely varying percentages have been reported for bilaterality in ovarian tumors; the most widely quoted are summarized in Table 33. Malignant epithelial tumors tend to involve both ovaries more frequently than benign epithelial tumors. However, age and menstrual status must also be considered before the appropriate course of action is chosen. A 5- to 8-cm ovarian mass in a woman with regular menses, even if she is in her 40s, is frequently a functioning ovarian cyst, such as a follicular or corpus luteum cyst. Enlargements of this type in young patients in their 20s or early 30s do not automatically require immediate operative intervention and can be observed for two menstrual cycles. A potential exception would be a mass in a woman who is taking oral contraceptives. Because the principal mechanism of contraception is anovulation, the index of suspicion for neoplastic growth should be raised. However, contemporary oral contraceptives have lower sex steroid levels and may permit follicular development. Shushan and colleagues reported on ovarian cysts detected by ultrasonography in pre- and postmenopausal women Obstetrics & Gynecology Books Full 33 Neoplastic Diseases of the Ovary values in the postmenopausal woman. Although not approved for surveillance or diagnosis, the test may complement clinical decision making, particularly if a gynecologic oncologist is not available to perform appropriate staging should cancer be identified. Unilocular 5- to 8-cm cysts are likely to be functional (see Chapter 18), whereas multilocular or partially solid tumors are more likely to be neoplastic. A transvaginal ultrasound scan can reliably detect an ovary larger than 1 cm in diameter. Higgins and associates estimated the upper limit of the volume of a postmenopausal ovary to be approximately 8 cm3 compared with 18 cm3 for the premenopausal ovary. Ten of their patients who exceeded these criteria and had solid or complex echo patterns had neoplastic tumors, and one carcinoma was discovered. An ultrasound examination, preferably with a vaginal probe, helps differentiate these adnexal masses (discussed later). In a study of 168 paraovarian tumors, Stein and coworkers noted that only three (2%) were malignant. The three cysts all had solid components; the cysts were 8 to 12 cm size in patients 19 to 48 years of age. It is expressed by approximately 80% of ovarian epithelial carcinomas but less frequently by mucinous tumors. The marker is increased in endometrial and tubal carcinoma, in addition to ovarian carcinoma, and in other malignancies, including those originating in the lung, breast, and pancreas. The specificity appears to be better for increased Ultrasound has helped define criteria to allow conservative followup and the risk of malignancy of some adnexal masses. Goldstein and associates studied 42 postmenopausal patients whose ultrasound scans have shown unilocular cysts smaller than 5 cm in diameter; 28 were explored, and none had malignancy, and 14 were followed for as long as 6 years, with no change in ultrasound appearance. In a clinicopathologic study to define ultrasound criteria of malignancy, Granberg and associates (1989) studied the ovarian tumors in 1017 women. Of 296 with unilocular cysts, only one was malignant and had visible papillary formations on the cyst wall; 60% of these women were older than 40 years. In contrast, malignancy rates were 8% (20 of 229) for multilocular cysts, 65% (147 of 201) for multilocular solid tumors, and 39% (31 of 80) for solid ovarian masses. In a follow-up study of 180 women, the authors noted that 45 of 45 unilocular cysts were benign. In an ultrasound study of cystic ovarian masses in women older than 50 years, Bailey and coworkers noted that unilocular cysts smaller than 10 cm in diameter are rarely malignant, whereas complex cysts or those with solid areas are at high risk of malignancy. Several scoring systems have been proposed to try to determine the risk of an ovarian mass being malignant. Is the finding a simple (unilocular) or complex (multicystic or multilocular with solid components) cyst Others have advocated using transvaginal pulsed Doppler color-enhanced flow studies to differentiate benign from malignant masses. The resistance index, which measures resistance to flow in the vessels, has been used and presumably is low in the presence of neovascularization that is seen with malignant tumors. The vessels of neoangiogenesis are abnormal in their distribution, with disorganized branching and a loss of the muscularis layer, all of which contribute to the decreased resistance to flow. In contrast, Bromley and colleagues, in a study of 33 postmenopausal women, used a cutoff of 0. Valentin and associates evaluated the characteristics of 1066 adnexal masses; 266 were malignant (55 borderline ovarian tumors, 144 primary invasive epithelial cancers, 25 nonepithelial ovarian cancers, 42 metastatic cancers). They reported that borderline and stage I ovarian cancers shared similar morphology but had different characteristics from more advanced-stage tumors.
Generic 0.25mg requip amex
In these families treatment research institute order genuine requip on-line, breast cancer tends to occur at a younger age, and there is a higher prevalence of bilateral disease. These genes function as tumor suppressor genes, and several mutations have been described on each of these genes. Once a woman has developed carcinoma of one breast, her risk is approximately 1% per year of developing cancer in the other breast. Both tamoxifen and raloxifene significantly decrease the relative risk of developing breast carcinoma. The sensitivity of mammography ranges from 80% to 90% and decreases in women with dense breasts. Approximately 20% of breast biopsies in women age 50 are positive, and this figure increases to 33% in women age 70 or older. The classic sign of a breast carcinoma is a solitary, solid, threedimensional, dominant breast mass. Invasive ductal carcinoma is the most common, constituting approximately 70% to 80% of malignancies. About 56% of these abnormalities are trisomic, 20% are polyploid, 18% will be chromosome X monosomies, and 4% will represent unbalanced translocations. Women at risk of cervical insufficiency should be monitored with serial ultrasound examinations from 16 weeks to the end of 24 weeks. Abnormalities occur in the female parent about twice as frequently as in the male, with balanced reciprocal translocations occurring in half of these individuals. Studies that have followed women who had medical, surgical, and expectant management of miscarriage have noted no difference in subsequent pregnancy rates. Care should be taken to avoid a single data point to diagnose an early pregnancy loss. The majority of these women will ultimately achieve a successful pregnancy without any intervention. Risks of ectopic pregnancy include age, pelvic inflammatory disease, prior tubal surgery, smoking, and infertility. Randomized trial data suggest there is no difference in overall subsequent pregnancy outcomes between women who are treated by salpingostomy versus salpingectomy. The overall risk of ectopic pregnancy if a pregnancy occurs after tubal sterilization is about 30%, reaching 50% if the sterilization technique was bilateral tubal fulguration. Several regimens are in use, and at least one third of women with ectopic pregnancies can be treated medically. The vulva contains 1% of the skin surface of the body, but 5% to 10% of all malignant melanomas in women arise from this region. The dysplastic nevus is characterized by being more than 5 mm in diameter, with irregular borders and patches of variegated pigment. The management of nonobstetric vulvar hematomas is usually conservative unless the hematoma is greater than 10 cm in diameter or rapidly increasing. Women usually develop psoriasis during their teenage years, with approximately 3% of adult women being affected. The volume of tissue removed and repeat excisional procedures have been reported to increase the risk for cervical stenosis. The lifetime prevalence of leiomyomas is greater than 80% among African-American women and approaches 70% among white women. Abnormal bleeding is experienced by a third of women with myomas, the most common pattern being intermenstrual spotting. If multiple serial sections of the uterus are obtained, the incidence may exceed 60% in women 40 to 50 years of age. The majority of follicular cysts disappear spontaneously by either reabsorption of the cyst fluid or silent rupture within 4 to 8 weeks of the initial diagnosis. Drainage or fenestration is effective for follicular cysts and poorly effective for cystadenomas. When cysts are drained, it is essential to remember that the cytologic examination of cyst fluid has poor predictive value and poor sensitivity in differentiating benign from malignant cysts. Benign ovarian teratomas vary from a few millimeters to 25 cm, may be single or multiple, and are bilateral 10% to 15% of the time. Fifty percent of patients with an ovarian fibroma will have ascites if the tumor is greater than 6 cm. They usually occur in women between the ages of 40 and 60 and are predominantly unilateral. Adnexal torsion occurs most commonly in the reproductive years, with the average age of patients being in the mid-20s. However, approximately 50% of women with surgically confirmed adnexal torsion will have a normal Doppler flow study. De-torsion and fixation of the ovary is a safe procedure that reduces the risk of recurrence. The risk is similar regardless of whether the condition is managed by conservative surgery with untwisting or adnexal removal without untwisting. Endometriosis lesions produce estrogen locally and have increased secretion of prostaglandins and inflammatory cytokines, which can cause pain and contribute to infertility. Grossly, endometriosis appears in many forms, including red, brown, black, white, yellow, pink, or clear vesicles and lesions. Approximately 10% of teenagers who develop endometriosis have associated congenital outflow obstruction. The two primary short-term goals in treating endometriosis are the relief of pain and the promotion of fertility. There is probably some benefit to abrading endometriosis lesions when seen at laparoscopy. Classic symptoms of endometriosis of the large bowel include cyclic pelvic cramping and lower abdominal pain and rectal pain with defecation, especially during the menstrual period. Pelvic organ prolapse is defined as the descent of one or more compartments of the vagina: the anterior vaginal wall, posterior vaginal wall, uterus (cervix), or apex (vaginal vault or cuff scar after hysterectomy). Pelvic organ prolapse is more likely to be symptomatic when the leading edge protrudes past the hymen; it can be managed expectantly if asymptomatic. Renal function should be evaluated in women with advanced pelvic organ prolapse if the patient declines treatment to reduce the prolapse. An abdominal sacral colpopexy with synthetic mesh appears to have a higher long-term success rate for the vaginal apex, but at the risk of more surgical complications. Parasympathetic nervous system activity via the neurotransmitter acetylcholine stimulates receptors in the bladder wall to activate detrusor contraction. The highest pressure zone in the urethra is approximately midpoint in the functional urethra, which is roughly 0. Retropubic and transobturator midurethral slings have similar success rates for stress incontinence, although with different risk profiles. Approximately 20% of women with urinary incontinence suffer from detrusor overactivity. Over 30% of women reporting urinary incontinence also report fecal incontinence, known as dual incontinence. A common cause of fecal incontinence is damage to the anal sphincter at the time of vaginal delivery, with or without neuronal injury. Approximately 1 in 10 women will develop some fecal incontinence or fecal urgency after one vaginal delivery. At a tertiary colorectal referral clinic, a prospective study showed that further evaluation, including radiologic and physiologic tests, altered the final diagnosis or the cause of fecal incontinence in 19% of cases. It is usually transmitted by individuals who are asymptomatic and unaware that they have the infection at the time of transmission. Symptoms that suggest cervical infection include vaginal discharge, deep dyspareunia, and postcoital bleeding. It should be diagnosed with a minimum of suspicion with the knowledge that overtreatment is preferable to missed diagnosis. Health care workers, women with spinal cord injuries, or those who have had to perform self-catheterization are at higher risk for latex allergy. Routine chest x-rays on all patients often do not impact perioperative management in elective gynecologic surgery, but they should be ordered for women who are 20-pack/ year smokers, women with cardiac or pulmonary symptoms, immigrants who have not had a recent chest film, and women older than 70 years. Enhanced recovery refers to a bundled process with the aim of attenuating pathophysiologic changes and the stress response occurring with surgery.
Syndromes
- Take the drugs your doctor told you to take with a small sip of water.
- The procedure may need to be done under general anesthesia in a hospital.
- Stopping medications or exposure to substances that may have injured the kidney
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- 2,500 to 3,000 IU/day for children 1 - 8 years
- Bleeding into the knee joint
- Nuclear heart scan (MUGA, RNV)
- Pain medication
- Rapid weight loss or low body fat
- Pneumonia
Purchase generic requip
Effect of second vaginal delivery on anorectal physiology and faecal incontinence: a prospective study medications during pregnancy chart purchase requip online pills. A comparative study of the human external sphincter and periurethral levator ani muscles. Anterior anal sphincter repair can be of long-term benefit: a 12-year case cohort from a single surgeon. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Sacral nerve stimulation for faecal incontinence: results from a single centre over a 10 year period. Obstetric fecal incontinence: role of pelvic floor denervation and results of delayed sphincter repair. Systematic review of sacral nerve stimulation for faecal incontinence and constipation. The use of transanal rectal advancement flaps in the management of fistulas involving the anorectum. Are special investigations of value in the management of patients with fecal incontinence Evidence of pudendal neuropathy in patients with perineal descent and chronic straining at stool. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) faecal incontinence. A comparison between electromyography and anal endosonography in mapping external anal sphincter defects. Efficacy of sacral nerve stimulation for fecal incontinence: results of a multicenter double-blind crossover study. Overlapping anal sphincter repair for faecal incontinence due to sphincter trauma: five year follow-up functional results. The prevalence of fecal incontinence in community-dwelling adults: a systematic review of the literature. Incidence and risk factors for fecal incontinence in black and white older adults: a population-based study. Fecal incontinence in obese women with urinary incontinence: prevalence and role of dietary fiber intake. Artificial anal sphincter for severe fecal incontinence implanted by a transvaginal approach: experience with 32 patients treated at one institution. Anterior sphincter plication and levatorplasty in the treatment of faecal incontinence. Fecal incontinence: an up-to-date critical overview of surgical treatment options. Physiological studies of the anal sphincter musculature in faecal incontinence and rectal prolapse. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Randomized, controlled trial of anal electrical stimulation for fecal incontinence. A prospective, randomized, controlled clinical trial of placement of the artificial bowel sphincter (Acticon Neosphincter) for the control of fecal incontinence. American College of Gastroenterology Practice Parameters Committee: Diagnosis and management of fecal incontinence. The International Consultation on Incontinence 2008-Committee on: "Dynamic Testing"; for urinary or fecal incontinence. Does the radiofrequency procedure for fecal incontinence improve quality of life and incontinence at 1-year follow-up Multiple vaginal deliveries increase the risk of permanent incontinence of flatus and urine in normal premenopausal women. Anorectal and pelvic floor function Relevance of continence, incontinence, and constipation. Endo-anal ultrasound versus endoanal magnetic resonance imaging for the depiction of external anal sphincter pathology in patients with faecal incontinence: a systematic review. The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine: a neurophysiological study. Damage to the innervation of the voluntary anal and periurethral sphincter musculature in incontinence: an electrophysiological study. Abnormalities of the innervation of the urethral striated sphincter in incontinence. Third-degree obstetric anal sphincter tears: risk factors and outcome of primary repair. Method for determining individual contributions of voluntary and involuntary anal sphincters to resting tone. Prevalence and severity of anal incontinence in women with and without additional vaginal deliveries after a fourth-degree perineal laceration. An electromyographic study of the normal function of the external anal sphincter and pelvic diaphragm. Pudendal nerve damage increases the risk of fecal incontinence in women with anal sphincter rupture after childbirth. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Sexual function, quality of life, and severity of anal incontinence after anal sphincteroplasty. Sacral nerve stimulation for fecal incontinence: results of a 120-patient prospective multicenter study. The role of sphincteroplasty for fecal incontinence reevaluated: a prospective physiologic and functional review. Prospective study of the effects of postnatal repair in neurogenic faecal incontinence. The overlapping innervation of the two sites of the external anal sphincter by the pudendal nerves. Anal sphincter tears at vaginal delivery: risk factors and clinical outcome of primary repair. Lentz For clarity of presentation, discussion of infectious diseases of the female genital tract is divided into those of the lower genital tract, the vulva, vagina, and cervix; and those of the upper genital tract, the endometrium and fallopian tubes. However, the female genital tract has anatomic and physiologic continuity, so infectious agents that colonize and involve one organ often infect adjacent organs. To understand the pathophysiology and natural history of infectious diseases of the genital tract, one must keep this continuity in mind. The symptoms caused by infections of the lower genital tract produce the most common conditions seen by gynecologists. Therefore the initial focus of this chapter is on clinical presentation and the differential diagnosis of vulvitis, vaginitis, and cervicitis. Although the most devastating pathologic processes from these diseases occur in sites other than the genital tract, they often obtain entry into the body through the vulvar, rectal, vaginal, or cervical epithelium. When one disease is suspected, appropriate diagnostic methods must be used to detect other infections. Vulvar itching or burning of acute onset and short duration suggests infection or contact dermatitis. The subcutaneous tissue of the vulva also contains specialized structures such as the Bartholin glands. Mucinous secretions from Bartholin glands provide moisture for the epithelium of the vestibule. Following obstruction, there is continued secretion of glandular fluid, which results in the cystic dilation. The differential diagnosis of vulvar cysts also includes mesonephric cysts of the vagina and epithelial inclusion cysts. Mesonephric cysts are generally more anterior and cephalad in the vagina, whereas epithelial inclusion cysts are more superficial. Rarely, a lipoma, fibroma, hernia, vulvar varicosity, or hydrocele may be confused with a Bartholin duct cyst. The cysts may vary from 1 to 8 cm in diameter and are usually unilateral, tense, and nonpainful. However, in chronic or recurrent cysts there occasionally are multiple compartments. In contrast, an abscess of a Bartholin gland tends to develop rapidly over 2 to 4 days with significant symptoms, including difficulty in ambulation.
Buy generic requip 0.5mg online
Neoadjuvant Chemotherapy Neoadjuvant chemotherapy is practiced as an alternative for patients thought to have substantial operative risk or preoperative disease distribution that could preclude optimal cytoreduction medicine 8 capital rocka discount requip 1mg with mastercard. Several authors have noted the potential benefits to this strategy, including the opportunity to allow for an improvement in performance status, decreasing operative morbidity through less extensive surgery, and increasing the opportunity to achieve an optimal result. Each of these goals has been demonstrated in small, single-institution retrospective and prospective studies. For example, in a series of 85 women treated with either neoadjuvant chemotherapy (n = 57) or primary cytoreduction (n = 28), Morice and associates reported a significant decrease in major morbidity, defined as morbidity requiring a second operation (7% vs. Survival in this trial was similar between the cohorts, although with wide confidence limits. Schwartz and colleagues reported on 59 women undergoing neoadjuvant chemotherapy and compared their surgical morbidity with 206 patients treated in the same time period by a standard approach. They found that patients in the former group had a shorter intensive care unit stay and postoperative hospital stay compared with conventional patients. Because patients in these small trials are selected for treatment based on presenting disease volumes or medical status, it has been difficult to determine whether there is a detriment to survival by this approach. Clearly, patients too infirm to be operated on gain from this approach because if they have chemoresistant disease, surgery would have little value and likely would hasten an adverse outcome. Conversely, patients able to undergo the procedure could have a poorer outcome because there could be further expansion of a large population of resistant clones by delaying cytoreductive disease. Loizzi and coworkers reported a case-control study of neoadjuvant chemotherapy in 60 patients (30 in each group). They documented that although the neoadjuvant cohort was older and represented a poorer performance status, these patients underwent optimal cytoreduction at a favorable rate (76% vs. A critical question to be answered in this methodology is one of biology, which can only be addressed in a prospective clinical study of potentially operable patients. Fortunately, two trials are ongoing to address this question, one of which was recently reported. In this prospective multi-institutional study, 668 evaluable patients were randomized to primary cytoreduction followed by six cycles of platinum-taxane chemotherapy or three cycles of neoadjuvant platinum-based therapy followed by interval cytoreduction and three additional cycles of therapy. Only 10% of patients randomized to interval surgery did not undergo the procedure because of the uncommon event of primary platinum and taxane resistance. Optimal cytoreduction (to <1 cm or to no visible disease) was statistically higher in the neoadjuvant therapy arm. Low rates of primary optimal cytoreduction and relatively low absolute median survivals observed in this study have been raised as criticisms. Postoperative rates of adverse effects and mortality tended to be higher after primary debulking than after interval debulking. Complete resection of all macroscopic disease (at primary or interval surgery) was the strongest independent variable in predicting overall survival. They went on to suggest that complete resection of all macroscopic disease, whether performed as primary treatment or after neoadjuvant chemotherapy, remains the objective whenever cytoreductive surgery is performed. Criticisms for both trials lie in patient selection and surgical effort potentially confounding the interpretation of contemporary management. Interval Cytoreduction cytoreductive surgery is referred to as interval cytoreductive surgery. Rose and colleagues published a prospective trial in 2004 evaluating the role of interval cytoreduction. All patients received three cycles of initial chemotherapy in the form of cisplatin and paclitaxel. Eligible patients were randomly assigned to undergo interval cytoreductive surgery followed by chemotherapy (n = 216) or chemotherapy alone (n = 208). Protocol compliance was good; only 7% of the patients who were randomly assigned to undergo interval cytoreductive surgery did not undergo surgery. Among patients who were randomly assigned to receive chemotherapy alone, 3% had interval cytoreductive surgery. The prevalent strategy has been to add to platinum and taxane therapy or substitute another agent for paclitaxel. It is unclear whether the addition or substitution of available cytotoxic agents in this setting will improve outcomes in primary disease, given the probability for overlapping toxicities. Based on emerging efficacy data regarding angiogenesis inhibition on ovarian cancer response and prevention of progression, several trials were launched with the agent bevacizumab. Additional studies of other molecules targeting one or more processes of angiogenesis as well as novel targets, such as the folate receptor, are being pursued in this setting. A meta-analysis of these studies has been published and concluded that the route of administration "has the potential to improve cure rates from ovarian cancer. This study was also the first to evaluate formally the impact of treatment on health-related quality of life. Assessment was made at baseline after the third cycle, after treatment completion, and 12 months after treatment completion. A clear profile for catheter malfunction risk was not identified, although timing and accompanying surgical procedures were closely scrutinized. In a reflection of these observed adverse events, health-related quality-of-life assessments were significantly lower throughout the trial but returned to parity 12 months after therapy. Unfortunately, toxicity concerns and a number of unanswered fundamental questions regarding efficacy. Clinical investigation with alternative One additional strategy, dose-dense and dose-intense chemotherapy, has received attention based on positive results reported in primary ovarian cancer patients (Katsumata, 2009). Despite just 62% of patients receiving six or more cycles of the dose-dense strategy (vs. Bevacizumab could be added at the discretion of the physician and, if chosen, was to be administered in maintenance until progression. Overall, 84% of patients received bevacizumab and over 87% underwent a primary debulking attempt. Evaluation of Chemotherapy Results Chemotherapy is usually administered every 3 weeks. Mild neutropenia after chemotherapy can be managed expectantly, but for the patient who develops severe neutropenia with fever and an absolute neutrophil count of less than 500 cells/mL, antibiotics are prescribed to prevent septic complications. Second-Look Procedures Second-look laparotomy was introduced in the late 1940s as a method of assessing disease status after primary therapy in patients with colon cancer. In the 1970s, the same procedure was introduced for the treatment of epithelial ovarian cancer. In the field of gynecologic oncology, the rationale for using second-look surgery was that the optimal duration of chemotherapy was unknown (at the time) and the second-look procedure allowed surgeons to decide the optimal duration of exposure to alkylating agents for their patients. The primary concern with prolonged exposure to alkylating agents was the potential for secondary malignancies. Ideally, a second-look procedure would be able to identify the presence or absence of disease, which would help guide subsequent management. Greer and coworkers performed a nonrandomized comparison in patients undergoing second-look laparotomy or clinical follow-up after receiving six cycles of combination chemotherapy with paclitaxel plus cisplatin or carboplatin. In that study, all patients were required to undergo optimal cytoreduction surgery prior to trial entry. The researchers demonstrated that secondlook surgery was not associated with longer survival (in the context of a nonrandomized study). Therefore second-look surgery should only be performed in the setting of a clinical trial. If a second-look laparotomy is performed, it is important to extensively sample the peritoneal surfaces and lymph nodes. Particular attention is paid to areas that contained residual disease at the conclusion of the initial surgical procedure. Maintenance Therapy 759 Unfortunately, many patients develop recurrent disease, even after a negative second-look operation. Rubin and associates noted a high rate of recurrence (45%) in patients with a negative second-look laparotomy. Those who initially have higher-stage and higher-grade tumors are more likely to have a recurrence after a negative second-look operation. However, those who were disease free at 5 years are likely to remain disease free by the subsequent follow-up period. Nonetheless, this high recurrence risk has prompted several authors to consider additional treatment at the identification of a complete response to primary treatment. This is often termed maintenance or consolidation therapy, although the former term is favored, given that the decision for treatment is based on the effect of primary therapy. Several randomized and nonrandomized clinical trials have been conducted in this arena, including hormones, vitamins, radiation therapy, chemotherapy, radioimmunoconjugates, immunotherapy, vaccines, gene therapy, biologic therapy, complementary medicines, and holistic approaches.
Buy requip 0.25 mg with amex
Long-term follow-up confirms a survival advantage of the paclitaxel-cisplatin regimen over the cyclophosphamidecisplatin combination in advanced ovarian cancer symptoms narcolepsy requip 1 mg on-line. Targeting the tumor blood vessel network to enhance the efficacy of radiation therapy. Obstetrics & Gynecology Books Full 27 Principles of Radiation Therapy and Chemotherapy in Gynecologic Cancer Kurzeder C, Sauer G, Deissler H. Molecular targets of ovarian carcinomas with acquired resistance to platinum/taxane chemotherapy. Survival benefits with diverse chemotherapy regimens for ovarian cancer: meta-analysis or multiple treatments. Radiosensitization of human breast cancer cells by a novel ErbB family receptor tyrosine kinase inhibitor. International Encyclopedia of Pharmacology and Therapeutics- Inhibitors of Ribonucleotide Diphosphate Reductase Activity. Expression of ribonucleotide reductase after ionizing radiation in human cervical carcinoma cells. Obstetrics & Gynecology Books Full 28 Intraepithelial Neoplasia of the Lower Genital Tract (Cervix, Vagina, Vulva) Etiology, Screening, Diagnosis, Management Mila Pontremoli Salcedo, Ellen S. Schmeler Cervical cancer is a leading cause of cancer and cancer-related deaths among women worldwide, with more than 500,000 new cases and 250,000 deaths annually. Cervical cancer was previously the leading cause of cancer-related death among women in the United States. However, the incidence and mortality has decreased by approximately 70% since the 1970s. This decline is largely due to the introduction in 1941 of the Papanicolaou (Pap) smear, which has led to a systemic effort to detect early cervical cancer and precancerous lesions (Papanicolaou, 1941). Cervical cancer is a preventable disease, with excellent tools for prevention (vaccination) and screening (Pap and human papillomavirus testing). Furthermore, there is a treatable preinvasive phase that lasts several years before progressing to invasive cancer. Consistently, the loss of these control mechanisms allows for the expression of the viral E6 and E7 genes. The production of oncoproteins results in the inactivation of the p53 and retinoblastoma tumor suppressors (Munger, 2004). These changes are believed to lead to cell immortalization and rapid cell proliferation. In some women, the transformed cells replicate and, if left untreated, a cancer can develop after a period of several years. The search for a predictive measure to distinguish between women who are infected and will clear the virus and those in whom the infection will persist and who will develop cancer has been difficult. Although it is clear that women who have a compromised immune system from any cause. The initial infection usually occurs during adolescence or early adulthood, with the majority of women clearing the infection within 18 to 24 months (Wheeler, 1996; Moscicki, 1998; Moscicki, 2004; Moscicki, 2008). However, economic, political, and logistical barriers in many low-income countries have limited universal mass vaccination programs. Studies are underway to determine whether two doses of the vaccine provide sufficient protection. In addition, it is not yet known whether vaccination protection is lifelong or whether a booster dose will be required. The patient had a cytology sample reported as a low-grade squamous intraepithelial lesion. Catch-up vaccination should be offered for females aged 13 to 26 years who have not been previously vaccinated (Markowitz, 2014). The uptake in other developed countries (Canada, Australia, the United Kingdom) has been much higher at approximately 70%, likely due to government supported school-based programs. The 1941 monograph by Papanicolaou and Traut remains one of the sentinel breakthroughs in the history of preventive medicine. Their work led to the demonstration that local therapy of precancerous lesions can prevent the development of cancer. Despite the fact that Pap testing has a low sensitivity, widespread Pap testing has reduced the incidence of cervical cancer by 50% to 70%. Generally, in the United States, women who develop invasive cervical cancer have never been screened or have not been screened for many years. Cells are sampled from the transformation zone, which is the area of the cervix where cervical cancer can develop. The transformation zone includes the squamocolumnar junction, which is the area where the squamous epithelium of the ectocervix meets the columnar epithelium of the endocervix. In the past, the collected sample was placed on a glass slide and fixed with alcohol. The sample is now placed in a liquid medium for transport to the laboratory where the slide is prepared. A, Cervix as seen through a speculum, with the spatula being used to obtain a cell sample. Cervical cancer screening should not be performed in women younger than 21 years of age, regardless of age of onset of sexual activity. Of note, these guidelines do not apply to those special populations with additional risk factors and other complicating history. Almost all laboratories in the United States and many in countries throughout the world use this terminology. A sample may be unsatisfactory if there is lack of a label, loss of transport medium, scant cellularity, and contamination by foreign material. If other than normal, the abnormalities are further divided into squamous and glandular. The cytologist may also comment on whether there is evidence of infection, such as yeast, or changes consistent with a diagnosis of bacterial vaginosis. However, biopsies should only be performed if there is suspicion for invasive disease. It is highly unlikely for dysplasia to progress significantly during pregnancy, and in the majority of patients further evaluation can be postponed until 6 to 8 weeks after delivery. If invasive cancer is suspected, cervical biopsies are indicated and can be performed safely during pregnancy. If there is significant concern for a dysplastic lesion, a follow-up with colposcopy or repeat cytology is acceptable at intervals no more frequent than every 12 weeks. If invasive cancer is diagnosed, a conization procedure under anesthesia can be performed. The process still remains reversible at this stage, with approximately 40% regressing spontaneously without treatment. The instrument is placed just outside the vagina after a speculum has been inserted and the cervix brought into view. After any obscuring mucus is removed with a swab, the cervix is carefully examined for the presence of lesions. Dilute acetic acid (3% to 5%) is applied to the cervix, and after 30 to 60 seconds the cervix is again examined. Acetic acid dehydrates the epithelial cells and dysplastic cells with large nuclei will reflect light and appear white. For a thorough and complete exam, the entire transformation zone must be assessed ("satisfactory" colposcopy). If some portions of the transformation zone cannot be visualized as they extend into the endocervical canal or for other reasons, the colposcopy is considered "unsatisfactory" as the examiner is unable determine the presence or extent of abnormal tissue. There is a lack of squamous maturation throughout the thickness of the epithelium. Note that the basement membrane is intact, showing that this process is confined to the epithelial layer only.
Buy requip no prescription
Supraumbilical upper abdominal midline incision for pelvic surgery in the morbidly obese patient medications interactions generic requip 2mg with visa. Screening for pulmonary embolism with a D-dimer assay: Do we still need to assess clinical probability as well Assessment of outpatient treatment of deep-vein thrombosis with low-molecular-weight heparin. Heparin: mechanism of action, pharmacokinetics, dosing considerations, monitoring, efficacy, and safety. Urine culture at removal of indwelling catheter after elective gynecologic surgery: Is it necessary A comparison of subcutaneous lowmolecular-weight heparin with warfarin sodium for prophylaxis against deepvein thrombosis after hip or knee implantation. Subcutaneous low-molecular-weight heparin compared with continuous intravenous heparin in the treatment of proximal-vein thrombosis. Epidemics of diarrhea caused by a clindamycin-resistant strain of Clostridium difficile in four hospitals. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Low molecular weight versus standard heparin for prevention of venous thromboembolism after major abdominal surgery. Role of comuted tomography and magnetic resonance imaging for deep venous thrombosis and pulmonary embolism. Awake epidural anesthesia is associated with improved natural killer cell cytotoxicity in the perioperative period. Decision support increases guideline adherence for prescribing postoperative nausea and vomiting prophylaxis. Prospective trial of early feeding and bowel stimulation after radical hysterectomy. Effect of an intensive glucose management protocol on the mortality of critically ill patients. Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. Efficacy of preemptive analgesia for wound pain after laparoscopic operations in infertile women: a randomised, double-blind and placebo control study. Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Comparison of efficacy and safety of low molecular weight heparins and unfractionated heparin in initial treatment of deep venous thrombosis: a meta-analysis. Use of different D-dimer levels to exclude venous thromboembolism depending on clinical pretest probability. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. Drainage following radical hysterectomy and pelvic lymphadenectomy: dogma or need Early feeding and the incidence of gastrointestinal symptoms after major gynecologic surgery. Influence of catheter type on occurrence of thrombophlebitis during peripheral intravenous nutrition. Necrotizing fasciitis: improved survival with early recognition by tissue biopsy and aggressive surgical treatment. Nausea and vomiting after gynaecological laparoscopy: comparison of premedication with oral ondansetron, metoclopramide and placebo. Nursing considerations in the geriatric surgical patient: the perioperative continuum of care. Ureteral injuries in an obstetrics and gynecology training program: etiology and management. The influence of suture material on vaginal vault granulations following abdominal hysterectomy. The association of intraoperative factors with the development of postoperative delirium. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomized controlled trial. Identification of risk factors for postoperative nausea and vomiting in the peranesthesia adult patient. Prevention and treatment of venous thromboembolism-International Consensus Statement. Systematic review of prophylactic nasogastric decompression after abdominal operations. The effects of stimulation of acupressure point p6 on postoperative nausea and vomiting: a review of literature. Management of urinary retention: rapid versus gradual decompression and risk of complications. Evidence-based interventions for postdischarge nausea and vomiting: a review of the literature. Differential effects of oral and transdermal estrogen/progesterone regimens on sensitivity to activated protein C among postmenopausal women a randomized trial. Managing the spectrum of surgical pain: acute management of the chronic pain patient. Closed-suction drainage versus no drainage following radical abdominal hysterectomy with pelvic lymphadenectomy for stage 1B cervical cancer. A randomized controlled trial of early postoperative feeding in gynecologic oncology patients undergoing intraabdominal surgery. Comparison of subcutaneous lowmolecular-weight heparin with intravenous standard heparin in proximal deep-vein thrombosis. Anterior abdominal wall nerve and vessel anatomy: clinical implications for gynecologic surgery. Effects of acetaminophen on morphine sideeffects and consumption after major surgery meta-analysis of randomized controlled trials. Colour-assisted compression ultrasound in the diagnosis of calf deep venous thrombosis. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infection: a meta-analysis. A comparison of six weeks with six months of oral anticoagulant therapy after a first episode of venous thromboembolism. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared to vaginal and abdominal procedures. Metaanalyses of acustimulations: effects on nausea and vomiting in postoperative adult patients. Central nervous system dysfunction after noncardiac surgery and anesthesia in the elderly. Prokinetic effect of erythromycin after colorectal surgery: randomized, placebo-controlled, double-blind study. Pelvic lymphocysts following retroperitoneal lymphadenectomy: retroperitoneal partial "no-closure" for ovarian and endometrial cancers. Methicillin-resistant Staphylococcus aureus as a common cause of vulvar abscesses. Writing Group for the Christopher Study Investigators: Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. Prevention of abdominal wound disruption utilizing the Smead-Jones closure technique. Prevention of postoperative nausea and vomiting-a multimodal solution to a persistent problem. Use of the long tube in the management of patients with small-intestinal obstruction due to adhesions. A randomized, double-blind evaluation of ketorolac tromethamine for postoperative analgesia in ambulatory surgery patients. If <30 mg/dL lower than last test (or if higher than last test), increase rate by 1 U/hr. Postmeal subcutaneous insulin lispro (Humalog) supplement in addition to insulin infusion when oral intake advances beyond clear liquids: a. If patient eats 50% or less of servings on breakfast, lunch, or supper tray, then give 3 U insulin lispro subcutaneously immediately after that meal. If patient eats more than 50% of serving on breakfast, lunch, or supper tray, then give 6 U of insulin lispro subcutaneously immediately after the meal.
Cheap requip 1mg
In women with a history of insulin resistance symptoms dust mites purchase 1 mg requip, women who are morbidly obese, and those older than 60 years, glucose levels should be checked at the bedside every 4 to 6 hours during the first postoperative day. The American Diabetic Association recommendations suggest that critically ill patients have better outcomes with tighter glucose control-fasting levels less than 110 mg/dL and postprandial levels less than 140 mg/dL. Ramos and associates have noted an increased incidence of infection by 30% for every increase in glucose of 40 mg/dL over the recommended 110 mg/dL (Ramos, 2008). Sliding scale insulin treatments, though less effective than intravenous infusions in the first 24 hours, are easier to manage. Sliding scale regular insulin is most appropriate for women without a previous history of diabetes and without risk factors, and those with short surgeries who will resume normal activity and diet within 24 hours. Infusions are preferable if glucose levels are elevated significantly, early in the postoperative course and for women with longer surgeries who will not resume regular eating and activity for a few days. The Portland Insulin Protocol allows for control of glucose levels and, with nursing support, can be effective (see Appendix A). When transitioning off insulin infusions, it is reasonable to use the rule of thumb of 80% of the previous 24-hour total insulin dose. In patients who go home at 24 hours, oral medications or insulin may be restarted at the time of discharge with the same dose as that which was used before the operative period. Part of the physiologic stress response to surgery is a drive for gluconeogenesis. Most women experience some nausea for approximately 12 to 24 hours, pass flatus some time during the first 48 hours, and have a spontaneous bowel movement by the third or fourth postoperative day after uncomplicated, benign gynecologic surgery. A randomized controlled trial of a regular diet as the first meal in gynecologic oncology patients undergoing intraabdominal surgery. The current best practice for women after gynecologic surgery including cancer and bowel resections, regardless of age, is clear liquids within 6 hours of surgery and immediate advancement to a regular diet with cessation of nausea and as tolerated by the patient. Traditionally, patients were to have nothing by mouth until the passage of flatus and then given a gradual resumption of diet from clear liquid to full liquid to soft to regular diet, commonly called step-up diets. Several studies have shown that delayed feeding such as this is unnecessary and, in some ways, detrimental. Steed and colleagues, in a study of major gynecologic surgeries, including oncologic cases, compared restricted oral intake with step-up diets to early full diet and found no adverse effects, as well as a shorter length of stay in the early feeding group (Steed, 2002). Similarly, a low-residual diet at 6 hours postoperative followed by a regular diet compared with a traditional delayed feeding and a step-up diet after return of bowel function showed more nausea and emesis in the delayed feeding group, with a shorter length of stay in the early feeding group (Kalogera, 2013) (Table 25. Gan and associates, in the 2014 Consensus Guidelines for the Management of Postoperative Nausea and Vomiting, have recommended certain preventive measures (Gan, 2014). These include avoiding general anesthesia with the use of more regional anesthesia, use of propofol for induction and maintenance, avoidance of nitrous oxide and other volatile anesthetics, adequate hydration, and minimizing the perioperative use of opioids. Obstetrics & Gynecology Books Full 25 Perioperative Management of Complications most important neurotransmitter and intestinal hormone affecting nausea. This multicenter trial documented several important principles for postoperative management. The antiemetic interventions of dexamethasone, ondansetron, and droperidol were found to be equally effective for treating nausea. The repeat use of medications for rescue effects is less efficacious if an agent has been given previously (Apfel, 2004). Previous studies have found that agents such as metoclopramide are ineffective for prophylaxis. Antiemetics in the phenothiazine class, such as promethazine and prochlorperazine, are effective but have some limitations because of side effects of sedation, dry mouth, and extrapyramidal effects, which may be worse for older women. Adynamic (paralytic) ileus is a misnomer, as it is a normal event defined as delayed bowel function of minor to moderate degree in the absence of a mechanical obstruction. The stomach secretes 500 to 1000 mL of fluid/day, making the total output from the upper tract approximately 1 to 1. The right colon resumes full motility in about 24 hours, but the left colon may take up to 72 hours. The incidence and duration of adynamic ileus are less following vaginal or laparoscopic hysterectomy than abdominal hysterectomy. If the delay in bowel function persists longer than 5 to 7 days, the patient has an ileus and one should also consider the possibility etiologies: either a mechanical cause such as a bowel obstruction or some other condition leading to an adynamic, or paralytic, ileus such as an infection or retained foreign body. Ileus, or specifically adynamic ileus, is believed to result from a lack of coordinated motor activity of the intestine, which results in disorganized propulsive activity. Electrical activity is present, but the pathophysiologic problem is continuous activity of the intrinsic inhibitor neurons in the wall of the small intestine. Usually, the process is generalized, but occasionally may be localized, involving only an isolated loop of bowel. Generally, the mechanisms include an increased neurologic inhibition of intestinal motility caused by sympathetic nerve activity, as well as an inflammation within the intestinal wall. Bauer and Boeckxstaens have described leukocytic infiltration secondary to cytokine production from manipulation of the bowel during surgery. The inflammation inhibits the appropriate neuromuscular reactions, which then decrease motility (Bauer, 2004). Postoperative narcotics also contribute to the problem by stimulating the opioid receptors increasing the dyssynchronous contractions that are the hallmark of an ileus, further decreasing motility and increasing pain. The classic symptoms of a prolonged ileus include absence of flatus, abdominal distention, and obstipation. This condition may be associated with abdominal tenderness and the abdomen is usually tympanic to percussion. Nausea and vomiting that persist more than 24 hours after surgery are a cause for concern. Diagnostic films of the abdomen (supine, erect, lateral) may help establish the correct diagnosis but are frequently overutilized (Table 25. Oral administration of radiocontrast material may be both therapeutic and diagnostic. The osmolality of the radiocontrast material is approximately six times greater than that of normal saline. Thus a large amount of fluid enters the small bowel and acts as a direct stimulant of peristalsis. In one study, after preliminary abdominal films were obtained, a dosage of 120 mL of 66% diatrizoate meglumine, 10% diatrizoate sodium (Gastrografin), was administered orally or via nasogastric tube. Passage of liquid stool occurred within a few hours in patients with adynamic ileus. Gastrografin, unlike barium, is nontoxic if it accidentally contaminates the peritoneal cavity during an operation for bowel obstruction. Early carbohydrate intake, as well as postoperative gum chewing, has demonstrated some efficacy in decreasing the rates of postoperative ileus and promoting the return of normal bowel function. In addition, a carbohydrate loading drink the night before surgery and allowing fluids up to 4 hours before surgery may assist with postoperative recovery as well (Kalogera, 2013). It is also known that early feeding decreases the incidence of postoperative ileus, most likely through stimulation of intestinal reflexes. The workup of postoperative ileus should include evaluation of serum electrolyte and magnesium levels, because hypokalemia and abnormal magnesium levels may contribute to the ileus. The management of a postoperative ileus is controversial, with numerous remedies that are unproved but demonstrate isolated, anecdotal success (Table 25. During the period of watchful expectancy, adequate fluid and electrolyte replacement is necessary. Patients experience mild cramping and passage of flatus and regain their appetite with the return of normal peristalsis. If adequate bowel sounds are present, a rectal tube, a Fleet enema, or a rectal suppository may facilitate the initial passage of flatus. Some advocate the routine postoperative administration of a "wetting agent," such as simethicone, to reduce surface tension of intestinal mucus and liberate entrapped gas. Opinions Obstetrics & Gynecology Books Full 25 Perioperative Management of Complications Table 25.