Purchase generic snafi online
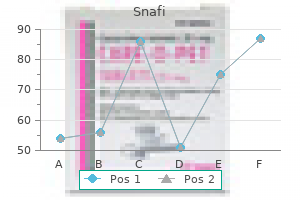
Additional assays continue to be developed using recombinant Echinococcus antigens and may provide better diagnostic sensitivity and specificity erectile dysfunction levitra order snafi overnight. Detection of protoscolices in the cyst fluid allows confirmation of cyst viability. However, to prevent postintervention sclerosis, care must be taken to ensure that the cyst does not communicate with the bile ducts before introducing cysticidal chemicals. A modified technique uses a special catheter system to simultaneously evacuate the cyst contents while infusing the scolicidal agent. Preoperative treatment with albendazole for 1 to 3 months has been shown to significantly reduce the number of viable cysts found at surgery. Optimal therapy has not been adequately studied but may need to be prolonged in some cases. Typically, it is given at a dose of 400 mg twice a day (for patients weighing <60 kg, 15 mg/kg/day divided into two doses) for 3 to 6 months. It is no longer recommended to interrupt treatment for 2 weeks every month of treatment. The response to drug therapy is best monitored by serial imaging studies; cyst disappearance or shrinkage along with increasing cyst density is thought to indicate a positive response. It is much less common in humans, with an incidence in endemic countries ranging from 0. However, increasing urban fox populations, with a noted increase in prevalence of parasite infection among foxes, may pose an increasing health concern for humans. In concert, the incidence of alveolar echinococcosis doubled from 2001 to 2005 compared with previous years. Their gradual invasion of adjacent tissue is tumor-like, and sections of the parasite may "metastasize" to distal parts of the body. Complications include biliary tract disease, portal hypertension, and Budd-Chiari syndrome. Consequently, morbidity and mortality are higher than for cystic (hydatid) echinococcosis. Findings of initial imaging studies are usually highly suggestive of carcinoma or sarcoma, and biopsy may provide the first indication of infection. Advances in the understanding of the molecular biology of Echinococcus have led to active investigation of new targets and new drugs for therapy. Humans acquire inadvertent parasite infection by ingestion of copepods (in water) or by consumption of or prolonged exposure to uncooked meat of plerocercoid-infected animals. These forms branch by lateral division and may detach to spread to other, distal areas of the body. There is local lymphocytic and eosinophilic inflammation surrounding the parasites. Diagnosis is usually by biopsy, although serologic testing has been Other Invasive Cestodes Alveolar Echinococcosis 3472 used in some areas. Clinically the cysts may be difficult to distinguish from cysticercosis or hydatid disease. Because this form of human infection results from egg ingestion and the eggs may have been spread throughout an area by free-ranging definitive hosts such as dogs or humans, infection may be difficult to avoid. It is significant that half of patients with hydatid cysts do not recall specific exposure to dogs, although they may have resided in or visited an area of endemicity. Field trials also indicate that anti-Echinococcus and anticysticercus vaccines can significantly reduce infection in farm animals (sheep and pigs), which may further reduce the level of peridomestic transmission. Performance characteristics and quality control of community based ultrasound surveys for cystic and alveolar echinococcosis. Improvement of liver resectional therapy by adjuvant chemotherapy in alveolar hydatid disease. Long-term disease-free survival after liver transplantation for alveolar echinococcosis. Control of fish tapeworm is more difficult to achieve because the infected fish can range freely and there are nonhuman reservoirs for the tapeworm. Release and survival of Echinococcus eggs in different environments in Turkana, and their possible impact on the incidence of hydatidosis in man and livestock. The ambiguous role of immunity in echinococcosis: protection of the host or of the parasite Relationship between the clinical heterogeneity of neurocysticercosis and the immune-inflammatory profiles. Neurocysticercosis in a child with no history of travel outside the continental United States. Albendazole versus praziquantel in the treatment of neurocysticercosis: a meta-analysis of comparative trials. Cerebral infarct precipitated by praziquantel in neurocysticercosis-a cautionary note. Prevalence of larval Anisakis simplex in pen-reared and wild-caught salmon (Salmonidae) from Puget Sound, Washington. Diphyllobothrium latum outbreak from marinated raw perch, Lake Geneva, Switzerland. Prevalence of Diphyllobothrium latum (Cestoda: Diphyllobothriidae) plerocercoids in fish species from four Italian lakes and risk for the consumers. Prevalence, age profile, and associated risk factors for Hymenolepis nana infection in a large population-based study in northern Peru. Parasitic infections in a closed community: results of a 10-year survey in Willowbrook State School. Intestinal helminthic infections among elementary students of Babile town, eastern Ethiopia. Hymenolepis nana infection: symptoms and response to nitazoxanide in field conditions. Successful treatment of niclosamide- and praziquantel-resistant beef tapeworm infection with nitazoxanide. Effects of deworming during pregnancy on maternal and perinatal outcomes in Entebbe, Uganda: a randomized controlled trial. Neurocysticercosis in Europe: still a public health concern not only for imported cases. Hospitalization frequency and charges for neurocysticercosis, United States, 2003-2012. Prevalence and risk factors for Taenia solium taeniasis and cysticercosis in humans and pigs in a village in Morelos, Mexico. A systematic review of the frequency of neurocysticercosis with a focus on people with epilepsy. Systematic review and meta-analysis estimating association of cysticercosis and neurocysticercosis with epilepsy. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium). Clinical evaluation of the cysticercosis enzyme-linked immunoelectrotransfer blot in patients with neurocysticercosis. A trial of antiparasitic treatment to reduce the rate of seizures due to cerebral cysticercosis. Effects of albendazole treatment on neurocysticercosis: a randomised controlled trial. Meta-analysis: cysticidal drugs for neurocysticercosis: albendazole and praziquantel. Comparison of therapeutic regimen of anticysticercal drugs for parenchymal brain cysticercosis. Efficacy of combined antiparasitic therapy with praziquantel and albendazole for neurocysticercosis: a double-blind, randomised controlled trial. Cysticidal efficacy of combined treatment with praziquantel and albendazole for parenchymal brain cysticercosis. Hydrocephalus secondary to cysticercotic arachnoiditis: a long-term follow-up review of 92 cases. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans.
Rubywood (Red Sandalwood). Snafi.
- Digestive tract ailments, fluid retention, coughs, and other conditions.
- What is Red Sandalwood?
- Are there any interactions with medications?
- How does Red Sandalwood work?
- Dosing considerations for Red Sandalwood.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96397
Buy snafi 20 mg online
Granulomatous amoebic encephalitis caused by Acanthamoeba amoebae of genotype T2 in a human immunodeficiency virus-negative patient impotence yoga pose generic snafi 20 mg on line. Primary amebic meningoencephalitis caused by Acanthamoeba: successfully treated with cotrimoxazole. Development of colorimetric microtiter plate assay for assessment of antimicrobials against Acanthamoeba. Persistently culture positive Acanthamoeba keratitis: in vivo resistance and in vitro sensitivity. Balamuthia mandrillaris granulomatous amebic encephalitis with renal dissemination in a previous healthy child: case report and review of the pediatric literature. Efficacy of novel antimicrobials against clinical isolates of opportunistic amebas. The in vitro efficacy of antimicrobial agents against the pathogenic free-living amoeba Balamuthia mandrillaris. Inhibition of 3-hydroxy-3-methylglutaryl-coenzyme A reductase and application of statins as a novel effective therapeutic approach against Acanthamoeba infections. Successful treatment of Balamuthia mandrillaris amoebic infection with extensive neurological and cutaneous involvement. Chapter 273 Free-Living Amebae 274 Definition Malaria (Plasmodium Species) Rick M. Falciparum malaria usually occurs within 6 months of exposure, but other malarias can occur more than a year after exposure. Polymerase chain reaction is the most sensitive test but is not rapidly available. The campaign, nevertheless, brought regional successes that coincided with other factors to reduce malaria incidence in many areas of the world. As chloroquine became increasingly available in the 1950s to 1970s, death rates from malaria in Africa began to drop, approaching half the level of the prechloroquine years. In Africa, mortality rates declined after the introduction of chloroquine but rose again after the spread of chloroquine resistance across the sub-Saharan region. Increased death rates were observed after chloroquine resistance entered the village, chiefly among children younger than 5 years, the most susceptible age group in highly endemic areas. Although increased international support and funding for prevention, control, and elimination reinvigorated the efforts of malaria control programs, decreasing the incidence of malaria by an estimated 18% globally between 2010 and 2016, the number of cases and deaths have plateaued in the past several years. Apicomplexa are distinguished morphologically by the presence of a specialized complex of apical organelles. During erythrocytic development, a small minority of parasites undergo a switch to sexual-stage development. Gametocytes emerge from erythrocytes in the mosquito midgut as male and female gametes that cross-fertilize to form diploid zygotes, which in turn differentiate into ookinetes that burrow through the midgut wall. Each ookinete develops into an oocyst containing up to 1000 sporozoites, which emerge and are then carried by the insect hemolymph to invade the salivary glands. These processes in the mosquito require an incubation period of about 1 to 2 weeks. Female mosquitoes inject sporozoites into humans while probing the dermis in preparation for taking a blood meal. Shortt and Garnham26 demonstrated in 1948 that sporozoites must first invade and replicate in hepatocytes before they can differentiate into merozoites capable of entering the intraerythrocytic cycle. The injected sporozoites typically take several hours to travel through dermal tissues and migrate across host cell barriers before they enter blood and lymphatic systems and are carried to the liver. Individual infected hepatocytes support the development of 10,000 to 30,000 merozoites, a process that is not associated with symptoms. Once a merozoite35 egresses by protease activity from its host hepatocyte (or from its host erythrocyte in the bloodstream cycle),36 it engages loosely with an uninfected erythrocyte and then reorients so that its apical end faces the cell surface. Anopheline mosquitoes transmit malaria by injecting sporozoites into the human host. Each infected hepatocyte ruptures to liberate 10,000 to 30,000 merozoites that invade circulating erythrocytes. Growth and development of the parasites in red cells result in subsequent waves of merozoite invasion. This asexual blood cycle repeats every 24 (Plasmodium knowlesi), 48 (Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale), or 72 (Plasmodium malariae) hours, leading to amplification of parasite density; paroxysms of chills, fevers, and sweats; and other manifestations of disease. Resumption of hypnozoite development months to years after initial infection can lead to malaria relapse that requires an additional round of drug therapy to treat recurrent symptoms and eradicate blood-stage parasites. A course of primaquine can prevent relapses of malaria, but this treatment may not always be successful because of inadequate patient compliance, interindividual variations of drug metabolism, or variable parasite responses to low or high drug doses. After breaking down their host cell membrane by enzymatic digestion, 24 to 32 merozoites enter the bloodstream and are each capable of infecting a new erythrocyte. Cycles of invasion and growth in erythrocytes produce a parasite biomass that enlarges rapidly, causing fever and leading to pathologic processes, such as erythrocyte loss (anemia), sequestration of infected erythrocytes in microvascular beds (cerebral malaria), and adverse sequelae of inflammatory cascades and cytokine release. It predisposes African children to bacteremia52 and increases the morbidity and mortality associated with other diseases by stressing host systems and producing effects such as dehydration, anemia, and some degree of immune suppression. Malaria is tremendously debilitating to health and impedes economic development through its adverse effects on fertility, population growth, saving and investment, worker productivity, absenteeism, premature mortality, and medical costs. This schematic illustrates how multiple pathogenic events such as cytoadherence, destruction of uninfected erythrocytes, and production of inflammatory cytokines combine to produce the microvascular sequestration and metabolic acidosis that are central to the development of severe disease. These switches may be structured to safeguard sequential expression among variant antigenic genes and thereby promote longevity of infection. High parasite densities,124 increased parasite multiplication rates,125 and evidence of high parasite biomass. Arrows identify numerous small electron-dense protrusions, termed knobs, on the surface of the host erythrocyte. However, obstruction by infected erythrocytes and other blood elements does not generally produce neurologic sequelae akin to those that follow the physical occlusion in thrombotic stroke, because most patients with cerebral malaria who recover can do so rapidly within 48 hours and without such consequences. Systemic sequestration of metabolically active parasites, blood cells, and platelets likely contributes to the metabolic acidosis and thrombocytopenia commonly seen in severe malaria. Metabolic acidosis, hypoglycemia, hyperpyrexia, and nonconvulsive status epilepticus can contribute significantly to the cerebral malaria presentation, as suggested by the rapid clinical improvement of some patients after fluid resuscitation, blood transfusion, dextrose infusion, fever reduction, and anticonvulsant therapy in addition to antimalarial treatment. In children, insulin 3304 levels are appropriate and hypoglycemia is associated with impaired hepatic gluconeogenesis and increased consumption of glucose by hypermetabolic peripheral tissues. Additional processes have therefore been implicated in the pathogenesis of malarial anemia. Excess removal of uninfected erythrocytes may account for up to 90% of erythrocyte loss161 and may be mediated by processes. The contribution of impaired erythropoietic responses to malarial anemia is significant and probably involves general processes also found in other diseases. Although microcytosis and hypochromia are seen in malaria, these findings are often attributable to thalassemias and iron deficiency in endemic areas. In endemic areas where chloroquine resistance is prevalent, the inability of young children to clear their parasitemias with chloroquine contributes to their higher baseline prevalence of anemia when compared with children treated with more effective drugs. Iatrogenic fluid overload and acute renal failure may contribute to the development or worsening of pulmonary edema. Although pulmonary edema usually occurs after other features of severe disease. Dyspnea and increased respiratory rate are features of impending pulmonary edema and often precede other clinical. Pulmonary manifestations of deep breathing and respiratory distress associated with severe malaria may also arise from metabolic acidosis,59 severe acute respiratory infections,152 sepsis-related acute respiratory distress syndrome, aspiration (especially with diminished consciousness or convulsions), and nosocomial pneumonia. Cerebral pathologic processes may result in abnormal breathing patterns, including CheyneStokes respirations and respiratory failure. Anemia is frequently observed as a consequence of acute or chronic infections, or as a result of repeated acute infections. Patients can remain infected and asymptomatic for many years before presenting with fevers, malaise, and splenomegaly decades after they have left an endemic area.
Discount 20 mg snafi fast delivery
Most patients with acute Chagas disease require no therapy other than benznidazole or nifurtimox because symptoms are generally selflimited even in the absence of drug treatment erectile dysfunction treatment after surgery snafi 20 mg discount. The management of the occasional severely ill acute-phase patient with myocarditis or meningoencephalitis is largely supportive. Chronically infected persons should have electrocardiograms performed every 6 months or so because pacemakers have been shown to be useful in the management of arrhythmias seen in chronic Chagas disease. Patients who fail to respond to repeated attempts at this approach are treated surgically. The procedure used most frequently is wide esophagocardiomyectomy of the anterior gastroesophageal junction, combined with valvuloplasty to reduce reflux. Patients with extreme megaesophagus are often treated with esophageal resection with reconstruction using an esophagogastroplasty. In industrialized countries, laparoscopic myotomy is often used to treat idiopathic achalasia. This relatively simple procedure may become the approach of choice for both idiopathic achalasia and Chagas megaesophagus. Patients in the early stages of colonic dysfunction associated with chronic Chagas disease can be managed with a high-fiber diet and occasional laxatives and enemas. Fecal impaction necessitating manual disimpaction may occur, as can toxic megacolon, which requires surgical treatment. Another complication of chagasic megacolon that requires immediate attention is volvulus. This usually occurs when the lengthened and enlarged sigmoid colon twists and folds on itself, causing a constellation of symptoms resulting from obstruction and vascular compromise. Endoscopic emptying can be performed initially in patients without radiographic, clinical, or endoscopic signs of ischemia in the affected area. In either event, however, surgical treatment of the megacolon is eventually necessary because of the high probability of recurrence of the volvulus. A number of surgical procedures have been used to treat advanced chagasic megacolon, and all include resection of the sigmoid colon as well as removal of part of the rectum. Identification of infected persons is important so that they can be monitored for rhythm disturbances and other signs of cardiac disease, as well as gastrointestinal dysfunction, and treated appropriately when indicated. The possibility of congenital transmission is another justification for screening. Over the past decade, substantial evidence has accumulated indicating that treating chronically infected girls and women of childbearing age markedly reduces the probability of congenital transmission to their babies conceived after treatment. Moreover, it is noteworthy that many if not most of the girls and women so treated likely were not cured parasitologically, and in some instances many years had elapsed between treatment and the pregnancies. It merits mention, moreover, that given the potential fetal toxicity of benznidazole and nifurtimox, care must be taken to ensure that chronically infected women of childbearing age are not pregnant when treatment is initiated and that they do not become pregnant during treatment. The courses of acute Chagas disease in seven of these patients were particularly fulminant because of immunosuppressive therapy, which certainly contributed to the definitive diagnoses. Common sense suggested that if serologic screening was warranted in endemic countries from which the 23 million at-risk immigrants living in the United States had come, they should be screened when they presented for donation here. Ten-year incidence of Chagas cardiomyopathy among asymptomatic Trypanosoma cruzi-seropositive former blood donors. Trypanosoma cruzi infection study: evidence for autochthonous Trypanosoma cruzi transmission among United States blood donors. Chapter 276 Trypanosoma Species (American Trypanosomiasis, Chagas Disease): Biology of Trypanosomes Prevention Key References the complete reference list is available online at Expert Consult. Screening and treatment of Chagas disease in organ transplant recipients in the United States: recommendations from the Chagas in Transplant Working Group. Large urban outbreak of orally acquired acute Chagas disease at a school in Caracas, Venezuela. Trypanosoma cruzi: parasite persistence in tissues in chronic chagasic Brazilian patients. Trypanosoma cruzi infection reactivation manifested by encephalitis in a Chagas heart transplant recipient. High frequency of adverse reactions and discontinuation with benznidazole treatment for chronic Chagas disease in Milan, Italy. Low incidence of adverse effects using a progressive regimen of benznidazole in Chagas disease. Another disappointing result with implantable cardioverter-defibrillator therapy in patients with Chagas disease. Surgical treatment of Chagas megacolon: critical analysis of outcome in operative methods. Phylogenetic analysis of the Trypanosoma genus based on the heat-shock protein 70 gene. Trypanosomatids are much more than just trypanosomes: clues from the expanded family tree. Evaluation of compliance to congenital Chagas disease treatment: results of a randomised trial in Bolivia. Control and management of congenital Chagas disease in Europe and other non-endemic countries: current policies and practices. Immunization and challenge of mice with insect-derived metacyclic trypomastigotes of Trypanosoma cruzi. Meningoencephalitis caused by reactivation of Chagas disease in patient without known immunosuppression. Chronic American trypanosomiasis: parasite persistence in endomyocardial biopsies is associated with high-grade myocarditis. Trypanosoma cruzi transmission cycle among wild and domestic mammals in three areas of orally transmitted Chagas disease outbreaks. New sylvatic hosts of Trypanosoma cruzi and their reservoir competence in the humid Chaco of Argentina: a longitudinal study. Distantiae transmission of Trypanosoma cruzi: a new epidemiological feature of acute Chagas disease in Brazil. Toward an ecological framework for assessing reservoirs of vector-borne pathogens: wildlife reservoirs of Trypanosoma cruzi across the southern United States. Trypanosoma cruzi among wild and domestic mammals in different areas of the Abaetetuba municipality (Para State, Brazil), an endemic Chagas disease transmission area. Understanding the role of dogs (Canis lupus familiaris) in the transmission dynamics of Trypanosoma cruzi genotypes in Colombia. Chagas disease in Latin American immigrants with dilated cardiomyopathy in New York City. Southern Cone Initiative for the elimination of domestic populations of Triatoma infestans and the interruption of transfusional Chagas disease: historical aspects, present situation, and perspectives. Prevalence of Chagas disease among blood donor candidates in Triangulo Mineiro, Minas Gerais State, Brazil. Congenital transmission of Trypanosoma cruzi in Argentina, Honduras, and Mexico: an observational prospective study. Between a bug and a hard place: Trypanosoma cruzi genetic diversity and the clinical outcomes of Chagas disease. Trypanosoma cruzi Infection Study: evidence for autochthonous Trypanosoma cruzi transmission among United States blood donors. Historical perspectives on the epidemiology of human Chagas disease in Texas and recommendations for enhanced understanding of clinical Chagas disease in the southern United States. Chapter 276 Trypanosoma Species (American Trypanosomiasis, Chagas Disease): Biology of Trypanosomes 3348. Prevalence of Chagas disease in the Latin American-born population of Los Angeles. Prevalence and impact of Chagas disease among Latin American immigrants with nonischemic cardiomyopathy in Los Angeles, California. Results of lookback for Chagas disease since the inception of donor screening at New York Blood Center. Trypanosoma cruzi infection in North America and Spain: evidence in support of transfusion transmission. Epidemiologic and laboratory findings from 3 years of testing United States blood donors for Trypanosoma cruzi. Frequency of the congenital transmission of Trypanosoma cruzi: a systematic review and meta-analysis. Survey of Pediatric Infectious Diseases Society members about congenital Chagas disease.
Discount snafi 20 mg amex
Relapse of New World diffuse cutaneous leishmaniasis caused by Leishmania (Leishmania) mexicana after miltefosine treatment impotence grounds for divorce in tn snafi 20 mg low cost. Therapy of Venezuelan patients with severe mucocutaneous or early lesions of diffuse cutaneous leishmaniasis with a vaccine containing pasteurized Leishmania promastigotes and bacillus Calmette-Guerin: preliminary report. Case report: transient success using prolonged treatment with miltefosine for a patient with diffuse cutaneous leishmaniasis infected with Leishmania mexicana mexicana. Case report: diffuse cutaneous leishmaniasis by Leishmania infantum in a patient undergoing immunosuppressive therapy: risk status in an endemic Mediterranean area. First case report of atypical disseminated cutaneous leishmaniasis in an opium abuser in Iran. Supsrisunjai C, Kootiratrakarn T, Puangpet P, Bunnag T, Chaowalit P, Wessagowit V. Successful treatment of disseminated cutaneous leishmaniasis with liposomal amphotericin B and miltefosine in an eight-year-old girl. Disseminated dermal leishmaniasis caused by Leishmania siamensis in a systemic steroid therapy patient. Liposomal amphotericin B treatment of Old World cutaneous and mucosal leishmaniasis: a literature review. Regardless of tropism, intracellular survival is essential to the pathogenesis of all forms of leishmaniasis. Multiple virulence factors enable Leishmania organisms to survive intracellularly, including lipophosphoglycan and leishmanolysin. The former aids in the transformation of phagosomes into parasitophorous vacuoles by promastigotes. In vitro, amastigotes transform into motile promastigotes and multiply, taking a few days to several weeks to reach detectable levels depending on the inoculum size. Parasite culture and Leishmania molecular assays are generally relegated to reference laboratories, and it is helpful to contact the laboratories in advance to ensure appropriate collection methods. Protocols using matrix-assisted laser desorption/ ionization may allow more widespread future availability of species identification. Each region has different species complexes with a greater or lesser degree of genetic heterogeneity within the complex. In addition, each geographic region has its own unique combination of sand fly vectors, mammalian reservoirs, and human hosts with different genetic backgrounds in varying zoonotic or anthroponotic cycles, leading to different outcomes and treatment responses. Optimal drug treatment regimens for each geographic region and major syndrome are best defined in consideration of demonstrated regional efficacy, available resources, and risk-benefit assessments. In resource-rich countries, the efficacy, safety, availability, and tolerability of drug regimens can be the primary factors regarding choice, whereas in low-resource endemic areas, cost and availability are crucial. In addition to regional differences, variations in trial design, particularly treatment end points, make definitive recommendations difficult. The end points used in clinical trials include clinical, parasitologic, and immunologic cure. Although current chemotherapy options result in a clinical cure, they may seldom lead to true parasitologic cure, with persistence of Leishmania parasites in host tissue being the rule, not the exception. The latter was previously considered two species, but it appears that early explorers from the Old World introduced it into the New World. More than 90% of reported cases from the last 10 years were in Bangladesh, Brazil, Ethiopia, India, South Sudan, and Sudan. As a result of a multinational elimination effort in South Asia, reported cases and deaths in India have decreased by greater than 70% and 95%, respectively, from 2010 to 2015. Clinically apparent cases are typically encountered among infants, young children, and immunocompromised persons. Most areas have focal disease risk with a background of latent or subclinical infection with sporadic clinical cases in rural areas. The clustering of cases in households suggests that humans may also be reservoirs in these settings. There is a marked increase in the number and size of Kupffer cells in the liver, many of which contain amastigotes. Autopsy studies reveal wide dissemination of the parasite with infected mononuclear phagocytes observed in the bone marrow, lymph nodes, skin, and other organs. The sequence of early cytokine responses and the manner in which Leishmania antigens are presented by macrophages and dendritic cells-influenced by vector, parasite, and host factors-may be important variables determining the response to an individual infection. Additionally, the extremes of age and in utero exposure to the parasite are associated with disease. Activation of latent infection is more common in patients who are antibody positive or immunosuppressed and can occur many years after exposure. However, incubation periods are often extrapolated from travelers with known exposure periods, and the latent infection paradigm adds further uncertainty. Individuals may have a subclinical course with spontaneous resolution or progression to overt disease, or they may immediately develop classic kala-azar. Although most patients with fully symptomatic kala-azar will die without intervention, there are reports of spontaneous disease resolution. However, the parasite is not eradicated, and disease can redevelop years later if the infected person becomes immunocompromised. In cases with a subacute or chronic course, there is an insidious onset of fever, weakness, loss of appetite, weight loss, failure to thrive, and abdominal enlargement caused by hepatosplenomegaly. In endemic areas, low-grade symptoms may persist for weeks to months but may not be sufficiently severe to warrant medical attention in low-resource areas, and the condition of such patients may be called subclinical when oligosymptomatic would be more appropriate. Fever may be intermittent, remittent with twice-daily temperature spikes (double quotidian), or, less commonly, continuous. Fever is relatively well tolerated, and older clinical references routinely noted that patients were not acutely ill or toxic in appearance. Acute presentation in nonimmune persons comprises abrupt onset with high fever and chills, sometimes with a periodicity that suggests malaria. The presence of a hard spleen suggests a hematologic disorder or another diagnosis such as schistosomiasis. The liver also enlarges; it usually has a sharp edge, soft consistency, and a smooth surface. Lymphadenopathy is common in patients in Sudan103 but uncommon in other geographic areas. Peripheral edema may be seen late in disease, particularly in malnourished children. Hemorrhage can occur from one or more sites; epistaxis and gingival bleeding may be noted as well as petechiae and ecchymoses on the extremities in late-stage disease. Patients can present with coinfection or acquire secondary bacterial infections during hospitalizations. It is important to recognize and treat clinically significant bacterial coinfections. The laboratory findings include anemia, leukopenia, thrombocytopenia, and hypergammaglobulinemia. Secondary hemophagocytic lymphohistiocytosis is increasingly reported, frequently in children. However, clinical diagnosis can be challenging in patients with atypical presentations such as oligosymptomatic or immunosuppressed patients or in returned travelers presenting to physicians in nonendemic regions months to years after an exposure. Samples for parasitologic diagnosis can be obtained by splenic aspiration, bone marrow aspiration, liver biopsy, and lymph node aspiration. Rarely, amastigotes may also be seen on blood smears or cultured from the buffy coat or blood. Molecular approaches have the potential to replace traditional parasitologic methods due to their diagnostic accuracy even when using blood samples rather than more invasive splenic or bone marrow aspirates. A meta-analysis found a pooled sensitivity and specificity from whole blood of 93% and 96%, respectively. Techniques such as loop-mediated isothermal amplification or recombinase polymerase amplification may offer reliable alternatives for field application but require further standardization and development. Both tests perform well with pooled sensitivities and specificities >90%, but sensitivity is diminished in some regions, particularly East Africa-potentially related to host differences or, for rK39, the extensive diversity of kinesin-related proteins found in East African isolates. In transplant patients, cytokine release assays can be positive in asymptomatic patients but cannot distinguish between latent infection and successfully treated cases. Parasitologic diagnosis is easier with parasites being found in a wide variety of samples including bronchoalveolar lavage fluid, pleural effusions, or biopsy specimens of the oropharynx, stomach, or intestine.
Discount snafi online visa
Daily fluctuation in egg excretion and dependence on trained microscopists can cause highly variable results erectile dysfunction doctor in houston buy cheap snafi 20 mg on-line, particularly in areas of low disease burden, leading to a false-negative test result. Use of concentration techniques in combination with Kato-Katz is critical for increasing the diagnostic accuracy in epidemiologic mapping and for monitoring mass preventive chemotherapy programs. However, the use of concentration techniques remains labor-intensive and increases the cost of the test by requiring additional equipment. Single-dose oral albendazole, mebendazole, and pyrantel pamoate, used in mass preventive chemotherapy programs, have cure rates of 88%, 95%, and 88%, respectively. This perianal itching is due to inflammation caused by the larvae and eggs during the night. Pruritus ani, if severe, can lead to secondary bacterial infections resulting from aggressive scratching, and also difficulty sleeping. Updated studies in the United States are lacking; the last prevalence study estimated 40 million infections in the 1980s. These activities create a nidus of pruritus, leading to scratching and contamination, especially underneath the fingernails. The infectious eggs can then be transferred via the fecal-oral route to other individuals or through autoinfection to the host. The standard of diagnosis involves use of a clear paddle or adhesive tape that is pressed on the anus early in the morning to capture eggs for visualization with a microscope. Management Life Cycle Pyrantel pamoate (11 mg/kg, maximum of 1 g) is available without a prescription in many locations. Both medications should be given 2 weeks apart and have almost 100% posttreatment cure rates. All household contacts should be treated, given that transmission is so high between family members. Although other hookworm species can cause cutaneous larva migrans (especially the dog and cat hookworm, Ancylostoma braziliense), they do not complete their life cycle in the human host and do not typically induce intestinal or pulmonary pathologic conditions. There are approximately 450 million people chronically infected with hookworm worldwide. The worm will bind to the small intestinal mucosal lining, using cutting plates to consume host blood. The hookworm larvae range in length from 7 to 13 mm, with Ancylostoma being generally larger; the size allows it to take in up to 10 times more human blood than Necator (0. After dermal penetration, the larvae will produce a local pruritic maculopapular rash that will track as the worm begins deeper tissue invasion. The majority of people will be asymptomatic, but some may exhibit a transient pneumonitis. The rash can form a serpiginous or vermicular pattern, usually on the feet (known as "ground itch"), but also on the ankles because the infectious larvae can elevate on blades of grass and ground vegetation. Typical gastrointestinal symptoms include abdominal pain and diarrhea; these symptoms are most severe with initial infections and decrease with chronic exposures. The term hookworm comes from the attachment of the buccal cutting plates to the intestinal mucosa in the small intestine. This unique pathophysiologic feature of the hookworms enables its consumption of red blood cells from the intestinal vasculature. The worms produce anticoagulants at the biting site, which allow continuation of bleeding after detachment. Iron-deficiency anemia is a chronic problem and correlates with worm burden, duration, and recurrence of infection. Growth and cognitive delays are associated in children with moderate and heavy infections (see Table 286. Hookworm and malaria coinfections in pregnancy can lead to especially profound anemia. There is a high degree of variability in the efficacy of oral albendazole (400 mg orally) and mebendazole (500 mg orally). For example, a systematic review found that single-dose mebendazole results in only 15% cure rates, and although single-dose albendazole appears to be a better drug for hookworm, there are highly variable effects of single-dose albendazole when used in deworming programs. In some cases, repeat treatment may improve cure rates, although it has been noted that efficacy can also decrease with repetition. It is found throughout most tropical and temperate climate zones of the world including North America and parts of Europe. The incidence is dependent on poor sanitation, often seen in resource-limited regions of the world. The improper management of human waste and runoff from sewage systems allow for continued transmission. In the lungs, the larvae continue to mature in the alveoli and are eventually coughed up and swallowed. The parasitic females lodge into the small intestine surface (lamina propria) and release eggs that hatch into the rhabditiform larvae. Another mode of infection is the fecal-oral route, in which unwashed fruits or vegetables exposed to night soil (human feces used as a fertilizer) that contain the eggs or larvae are consumed. The majority of infections are clinically asymptomatic, although some can manifest with gastrointestinal symptoms including bloating and abdominal discomfort after eating. A prevalent symptom is a new onset of heartburn that is not related to being supine. Episodic diarrhea is common, although this may alternate with constipation and can mimic irritable bowel syndrome. It has been postulated that the worms are sufficiently small that despite their migration through lung tissue, there is no significant tissue damage or inflammatory response. Early in the infection as the worms travel through the skin, they may leave a serpiginous trail of dermatitis known as larva currens. In chronic infections, urticaria (hives) or pustular eruptions may occur, which is a sign presumably related to allergic sensitization to parasite antigens. Because chronic infections are often clinically asymptomatic, it is not uncommon for the infection to be uncovered after an incidental finding of peripheral blood eosinophilia. Accelerated autoinfection leading to hyperinfection syndrome with an accumulation in the numbers of larvae penetrating the gut and an increase in adult worms in the gut, or even disseminated infection, in which adult worms are found at ectopic extraintestinal sites, is the most dangerous and often fatal condition associated with S. Some of these invade the gastrointestinal mucosa, often carrying enteric bacteria into the bloodstream. The gram-negative (or polymicrobial) bacteremia can lead to meningitis and septic shock. The parasites can cause devastating pulmonary inflammation with widespread pneumonitis and bleeding. Untreated, this process can lead to almost certain death, with mortality estimates ranging from 35% to 100% depending on the study. Hyperinfection rarely occurs in the healthy host, but does occur when the patient is immunosuppressed. Oral corticosteroids have been associated with Strongyloides hyperinfection most commonly. For disseminated strongyloidiasis, daily ivermectin for 14 (or more) days is the standard treatment. In those unable to take oral medication, there are rectal and injectable routes of administration, including subcutaneous routes, that have been used successfully. Although cure is commonplace in acute and chronic strongyloidiasis, treated patients are still at risk for reinfection, because immunity to S. As for other parasitic infections, there is active research to develop vaccines and prevent reinfection,91 and for S. Its ability to cause hyperinfection or disseminated infection in the face of immunosuppression makes its diagnosis, treatment, and ultimate prevention through public health measures or vaccines of paramount importance. Management Chapter 286 Intestinal Nematodes (Roundworms) Clinical Syndromes Over 430 million people are infected with T. Disease prevalence and worm intensity are highest in preschooland school-aged children, with a decline in disease intensity as children age into early adulthood. Trichuris eggs require high humidity, sandy soil, and warm temperatures to embryonate. L1 larvae hatch in the small intestines, penetrate the columnar epithelium, molt, and emerge as immature adult worms. The immature adult worms are then carried to the colon, where they develop into adults. Adult worms secrete natural products, including parasite macromolecules, that reduce the barrier function of the intestinal epithelium, leading to increased mucosal permeability. Egg production can be detected in the stool 3 months after ingestion of embryonated eggs by the host.
Buy snafi on line amex
The mandatory conditions for home or outpatient treatment include the presence of a reliable caregiver at home impotence vacuum device buy 20 mg snafi amex, a stable intravenous access, hospital proximity and adequate transportation, and the necessary facilities (telephone, running water, heating, and refrigeration). Antibiotic choices for oral therapy in the absence of risk factors for resistant pathogens include ciprofloxacin plus amoxicillin-clavulanate combination therapy, moxifloxacin monotherapy, or intravenous antibiotics such as ceftriaxone plus amikacin once daily. Recent developments in antibiotic therapy suggest that skin and soft tissue infections due to gram-positive cocci might be safely treated with a single administration of 1. First of all, as previously mentioned, targeted therapies and biologic response modifiers have partially changed the spectrum of infecting pathogens and put patients at a risk that is higher than and different from what was previously realized. The current situation might be different, because the increasing resistance phenomenon does not necessarily affect only high-risk patients but can be present in specific settings, hospitals, or countries in low-risk patients as well, although the shorter duration and severity of neutropenia should still mitigate the clinical course. Therefore once again, every center should make its own choices based on its local epidemiology and every patient should be evaluated separately. The escalation approach consists of starting with piperacillintazobactam or a third-generation cephalosporin (a choice that used to be broad spectrum and active against P. This approach seems to be still appropriate in many countries and centers, especially when resistance rates are low among pathogens commonly causing infections in neutropenia. With this approach, the carbapenems are used as second-line therapy either in patients failing the initial therapy or in case of a documented infection. This was clearly shown by a double-blind, placebo-controlled clinical trial comparing piperacillin-tazobactam with placebo versus the same drug with amikacin, and was confirmed in subsequent meta-analyses. However, in light of increasing resistance, there is a growing concern with this approach, because it has been shown that if the initial regimen fails to cover the pathogen responsible for infection, the outcome can be fatal. Up-front use of ceftazidime-avibactam, meropenem-vaborbactam, or a combination including colistin, if a patient is colonized with carbapenem-resistant Enterobacteriaceae; 4. In the deescalation approach, the key issues are (1) to safeguard the patient and to avoid the risk of undertreating his or her infection, which has the potential to be overwhelming; and (2) to reduce as much as possible the unnecessary use of precious drugs. However, in recent years, because of the decreasing activity of the classic antibiotics used for fever during neutropenia and the shortage of new molecules, choices and strategies have been rediscussed. Indeed, physicians have been forced to diversify empirical regimens based on colonization, local epidemiology, antibiotic policies, and patient-related factors such as clinical presentation, organ failure, and status of the underlying disease. Being ready to review the composition of empirical therapy is mandatory in both cases, in light of the possible need to widen or restrict the antibiotic coverage or focus on a specific pathogen. Previous exposure to broad-spectrum antibiotics, in particular to thirdgeneration cephalosporins 3. Intensive care unit stay 3648 or vancomycin) by reassessing the antibiotic treatment after 48 to 96 hours and by streamlining therapy, based on microbiologic results, whenever possible. However, patients presenting with severe sepsis, septic shock, or suspected bacterial pneumonia and those known to be colonized by resistant pathogens may be started with meropenem plus vancomycin and then deescalated to piperacillin-tazobactam or ceftazidime with vancomycin stopped, if a susceptible pathogen is olated. It frequently contains a combination regimen of ceftazidime-avibactam or colistin, plus an aminoglycoside, tigecycline, or other suitable molecule. This recommendation was based on a very small, open-label, randomized trial published in 1979. Obviously, very careful clinical monitoring was recommended in order to immediately restart antibiotics at first signs of infection relapse or novel infection. In microbiologically documented infection, the recommendation was to treat for at least 7 days. Decreasing the antibiotic selective pressure is crucial for future generations and should be pivotal in modern medicine. Contrary to what is commonly believed, controversies about the dogma that antibiotic therapy should be continued until the end of neutropenia can be traced back to 1988, and the 2008 Infectious Diseases Society of America guidelines left some room for the possibility of stopping empirical therapy before recovery of neutropenia in a clinically stable patient, although providing the shortcut of resuming quinolone prophylaxis. Only two prospective randomized studies in low-risk children found that discontinuation of antibiotics before marrow recovery did not result in deaths caused by bacterial infections or in an increased rate of the recurrence of fever. In this observational study, 3 of 7 patients had relapsing fever due to severe infections. The conclusion was that discontinuing therapy was probably unethical and, in any case, allowed to spare only 3 days of antibiotics. The results of the study in the intention-to-treat analysis show that the clinically oriented approach significantly increased the number of antibiotic-free days from 13. Indeed, the rate of fever recurrences and fungal or bacterial superinfections in the two groups was basically the same and so was the outcome, likely due to timely and adequate interventions. In conclusion, in the face of the antibiotic crisis and the increasing recognition of the importance of maintaining as much as possible the integrity and diversity of the human microbiota, we are forced to rationalize antibiotic intervention in hematologic patients. To adopt stringent criteria for driving empirical choices at the onset of fever and neutropenia and on day 3 to 4 after starting treatment 3. To be acquainted with the concept that a planned progressive succession of antibiotics in fever and neutropenia does not exist, and every patient and every episode should be evaluated separately 4. To accept the idea that in neutropenic patients with fever of unknown origin, empirical antibiotics could be discontinued even before neutropenia recovery, provided close clinical observation as inpatients is maintained with a high level of suspicion for restarting treatment. This practice is based on autopsy studies showing fungal infections undetected during life and on two randomized studies that enrolled, in total, less than 200 patients. In both randomized studies, the statistical power of the observed results was very small. Nevertheless, empirical antifungal therapy in persistently febrile neutropenic patients without a documented infection has become common practice in many cancer centers worldwide, and numerous drugs have been tested for this indication. Except for the first studies, which used persistence of fever and survival as the main end points, almost all other studies used a composite end point that included five criteria: defervescence, no discontinuation for toxicity, treatment of baseline fungal infections, prevention of breakthrough fungal infections, and survival. In general, no drug has been demonstrated significantly more effective than others, and differences were only based on lower toxicity. Of interest, a meta-analysis of the six trials in which empirical treatment was compared with no treatment or preemptive therapy confirmed that empirical antifungal treatment was associated with a lower rate of (diagnosed) invasive fungal diseases, but gave no significant advantage in terms of overall mortality. However, when fluconazole prophylaxis became widely used and reduced Empirical and Preemptive (Diagnostic-Oriented) Antifungal Therapy 3649 the incidence of Candida infections, it became evident that empirical therapy was mainly directed against Aspergillus. In recent years, awareness has grown that the empirical approach results in a tremendous overtreatment of just one symptom (fever) and has encouraged development of a preemptive or, maybe better named, diagnostic-driven approach aimed at treating a fungal disease when highly suggestive, although not conclusive, diagnostic criteria are present (not just fever). In the diagnostic-driven strategy, clinical considerations (fever, thoracic pain, cough), biologic markers. Whether or not any pulmonary infiltrate is enough or typical radiologic signs of invasive aspergillosis are required to start antifungal therapy is a matter of debate. The first one concluded that the diagnostic-driven approach was feasible, associated with less use of antifungal therapy, and without increased mortality with respect to historical controls. As expected, in the arm of preemptive therapy, in which an active diagnostic workup was performed, there were more fungal infections than in the other arm. In this study, patients were stratified by status of underlying disease, and the lower limit of the confidence interval of the difference in survival between the two strategies, among patients in first remission-induction therapy (the highest risk period), was exactly at the 8% predefined delta limit, thus leading the investigators to conclude that noninferiority was not demonstrated in this subgroup. The second is the availability of different antigen detection assays, of which galactomannan is the most important. The third is the turnaround time, which should be no more than 2 to 3 days to allow timely intervention. Finally, it had been demonstrated that a mold-active prophylaxis might lead to a reduction in the sensitivity and specificity of the galactomannan test, therefore lowering its reliability. Indeed, due to low pretest probability, screening with galactomannan in this setting is unhelpful, but targeted testing in case of suspicion of breakthrough invasive aspergillosis has been shown effective. For example, empirical antifungal therapy could be started at clinical suspicion while awaiting the results of diagnostic procedures but then discontinued if the results are not confirmatory. Drugs approved for empirical therapy include liposomal amphotericin B, caspofungin, and itraconazole, whereas there is no drug approved specifically for preemptive treatment. In cases of preemptive treatment, the indirect diagnostic tests, such as galactomannan or (13)-d-glucan, or radiologic imaging may suggest a possible etiology. Therefore the preemptive antifungal treatment is the same as that recommended for first-line therapy. For example, for aspergillosis, it usually has been voriconazole or liposomal amphotericin B. Recently, isavuconazole has been approved for treating invasive aspergillosis and mucormycosis, following the results of a large randomized study that demonstrated noninferior efficacy and better tolerability compared to voriconazole for treatment of aspergillosis, and data of similar efficacy (survival) in 21 patients with mucormycosis compared to 33 treated with amphotericin B. Finally, a new issue of the choice of an antifungal treatment in case of failing mold-active prophylaxis warrants some consideration. Failure of mold-active prophylaxis is suspected when a patient develops signs and symptoms suggestive of a fungal infection without microbiologic documentation. Four possible explanations include (1) the patient was not taking prophylaxis (lack of compliance); (2) the drug was not absorbed (posaconazole) or was metabolized too fast (voriconazole), as shown by inadequate blood levels; (3) the "new" fungal infection is due to a non-Candida/non-Aspergillus fungus intrinsically resistant to azoles; or (4) the "new" fungal infection is due to an azole-resistant Candida or Aspergillus species. In the first two cases, adjusting dosages without changing therapy seems an adequate option, whereas in the third and fourth cases, shifting to another drug family (caspofungin for Candida and lipid amphotericin B for Aspergillus) seems the only possible option.
Syndromes
- Respiratory distress
- Bleeding
- Infection
- Aneurysm
- Larger-than-average newborn (such as an infant of a diabetic mother)
- Pleural fluid analysis
- Inability to participate in sports
- Medicines (such as levodopa, antidepressants, anticonvulsants)
- Uneven, rapid, racing, pounding, or fluttering pulse
Snafi 20 mg with amex
Among oral treatments most effective erectile dysfunction drugs cheap snafi 20 mg with amex, itraconazole 200 mg daily for 5 or 7 days and fluconazole 300 mg weekly for 2 weeks are effective. Patients usually have to be warned that the pigmentary changes may return to normal only after many months, even when the infection has been successfully treated. The normal skin is colonized in late childhood and adult life by lipophilic yeasts. Morphologically, these are either oval (most common on the scalp) or round (mainly on the trunk), and they were previously called Pityrosporum ovale and Pityrosporum orbiculare, respectively. These organisms have now been reclassified as members of the genus Malassezia, among which there are seven common pathogenic species: Malassezia furfur, Malassezia pachydermatis (not associated with human skin infections), Malassezia sympodialis, Malassezia globosa, Malassezia restricta, Malassezia obtusa, and Malassezia slooffiae. Malassezia species dominate the skin fungal microbiome in core scalp, body, and arm sites of adults. Infections are more common in the tropics and may appear after sun exposure, which may therefore be a trigger factor. Different species of Malassezia obviously play a role in the development of disease, although it is not known why, for instance, M. The first is a folliculitis on the back or upper part of the chest that consists of scattered follicular papules or pustules. In the second form, which is seen in patients with seborrheic dermatitis, there are numerous small follicular papules over the upper and lower portions of the back and chest. This type is similar to the second form, and affected patients usually have severe seborrheic dermatitis. Scrapings or biopsy specimens from lesions show numerous yeasts occluding the mouths of follicles. Treatment with topical azole antifungal agents may be effective, but oral therapy with itraconazole is often necessary. In the early part of the 20th century, seborrheic dermatitis and dandruff of the scalp were thought to be caused by Malassezia yeasts because numerous organisms were present in skin scales. This view was subsequently superseded by the belief that the yeasts were secondary to a hyperproliferative state. Improvement is associated with disappearance of the organisms, and relapse is associated with recolonization. Furthermore, the clinical appearances can be mimicked in animals with the application of both live and killed organisms to the skin. Some patients with seborrheic dermatitis have high titers of antibody to Malassezia species. Two newly described potential pathogenetic mechanisms are the production of irritants, such as oleic acid, or of Malassezia metabolites that are immunomodulatory, such as indolocarbazole and malassezin, on affected skin of seborrheic dermatitis patients. An infiltrate of polymorphs in the epidermis above the dermal papillae is also often seen. Seborrheic Dermatitis Pathogenesis Clinical Manifestations Pityriasis versicolor is usually seen on the trunk or proximal portions of the limbs, although more extensive infections involving the face and waist area occur in the tropics. Lesions may be hypopigmented or hyperpigmented macules that amalgamate to cover the affected area with scaling plaques. Rare clinical variants include some infections that result in anetoderma (localized skin atrophy). The diagnosis can be confirmed through direct microscopic study of lesions, on which the characteristic round yeast forms and short hyphae can be seen. Lesions fluoresce yellow-green under Wood light, Clinical Manifestations the classic features of seborrheic dermatitis make up a range of different clinical appearances. These include erythema and scaling of the central part of the anterior aspect of the chest and the upper part of the back 3210 that are accompanied by a variable degree of itching. On the face, there is erythema with greasy scales in the eyebrows, around the alae nasi, behind the ears, and in the external ears. Scaling on the scalp is accompanied by the appearance of pustules in some patients. Other forms of skin disease, including severe erythroderma in infants and an intertriginous rash in adults, have also been called "seborrheic dermatitis," but these lesions do not appear to be related to the variety discussed here. The main therapy involves the use of topical azole creams or oral azoles such as itraconazole and weak topical corticosteroids such as 1% hydrocortisone. Malassezia is also associated with a form of atopic dermatitis affecting the face in young adults. The infection is confined to the stratum corneum of the palms or soles and occurs mainly in the tropics or subtropics in children or young adults. The typical lesion of tinea nigra is a superficial, scaling, brown or black macule on the palms or soles. The main differential diagnosis is a superficial form of melanoma or a pigmented nevus. The pigmented hyphae can be seen by direct microscopic study of skin scrapings treated with potassium hydroxide. The organism can also be cultured from scrapings, but a dermatoscope can show the very typical pigmented hyphae on the skin. The best therapy is treatment with a topical azole or a keratolytic agent such as Whitfield ointment or 5% to 10% salicylic acid ointment. White piedra is an uncommon infection caused by yeasts of the genus Trichosporon, namely, Trichosporon ovoides (scalp hair), Trichosporon inkin (pubic hair), and Trichosporon asahii (rare in piedra). It is a superficial infection of the hair shafts of the scalp, body, or pubic hair. Trichosporon species may also cause a systemic infection in neutropenic patients (see Chapter 268). White piedra is asymptomatic and manifests as small yellow concretions on the hair shafts. The diagnosis may be confirmed by examining an epilated hair mounted in potassium hydroxide. Each nodule contains fungal hyphae, and the organisms can be cultured from infected hairs without difficulty. Otherwise, coating the hairs with an azole such as econazole or treating the patient with oral itraconazole may cure the infection. Black piedra is another infection of the hair shafts that is caused by a black yeast, Piedraia hortae. The infection manifests as small black nodules on the hairs of the scalp and less commonly elsewhere. These have to be distinguished from pediculosis, but itching is usually absent in black piedra. With direct microscopy, these nodules can be shown to be composed of hyphal elements and small ascospores of the causative agent within a dark cement-containing stroma. Treating hairs with a topical salicylic acid or an azole cream is usually sufficient, although relapse is common. Keratin degradation by dermatophytes relies on cysteine dioxygenase and a sulfite efflux pump. A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Genus- and species-level identification of dermatophyte fungi by surface-enhanced Raman spectroscopy. Prevalence and causative fungal species of tinea capitis among schoolchildren in Gabon. Tinea capitis: study of asymptomatic carriers and sick adolescents, adults and elderly who live with children with the disease. The prevalence of common skin conditions in Australian school students: 4 Tinea pedis. The adherence of dermatophyte microconidia and arthroconidia to human keratinocytes in vitro. Interdigital athletes foot, the interaction of dermatophytes and residual bacteria. Hereditary palmo-plantar keratoderma: incidence of dermatophyte infections and the results of topical treatment with retinoic acid. Trichoscopy as an additional tool for the differential diagnosis of tinea capitis: a prospective clinical study. Systemic antifungal therapy for tinea capitis in children: an abridged Cochrane Review. The evaluation of bifonazole 1% and 40% urea paste in the management of onychomycosis.
20 mg snafi
Sequence variation in the gene encoding dihydropteroate synthetase erectile dysfunction medication for sale order 20 mg snafi visa, the target enzyme of sulfonamides, in human Pneumocystis has been identified. Animal models, which are the principal test system, have facilitated identification of several new types of drugs. A more promising approach has been to investigate drugs that are already licensed for other agents for activity against Pneumocystis. These observations require evaluation in prospective clinical trials before clinicians incorporate them into treatment algorithms. As none of the currently available anti-Pneumocystis drugs used in humans has a "cidal" activity against Pneumocystis, chemoprophylaxis should be continued for as long as the underlying immunosuppressive condition exist. Secondary prophylaxis is given to prevent a recurrence; indications for secondary prophylaxis are similar to those for primary prophylaxis. Indications of giving chemoprophylaxis to patients with other causes of immunosuppression are shown in Table 269. Manipulation of the host innate or adaptive immune response could improve defenses against Pneumocystis while lessening their deleterious effects on the host. Boosting the host immune response might also lessen the need for, or lower the dosage of, antimicrobial drugs. There is accumulating evidence showing Pneumocystis is transmissible in both humans and experimental animal models. In animal models Pneumocystis cysts derived from mice are susceptible to most common disinfectants, except 0. Dapsone may be administered alone or in combination with pyrimethamine and leucovorin (Table 269. Both dapsone and pyrimethamine additionally protect against Toxoplasma gondii but not against bacterial infections. Major side effects include cough and bronchospasm, which can be controlled by use of a -agonist. Administration of aerosolized pentamidine in a health care setting requires a negativepressure room with adequate ventilation and should not be administered to patients with suspected/proven smear-positive tuberculosis because of the risks of nosocomial transmission. A number of other drug regimens have been considered possible Pneumocystis prophylactic agents, but Preventing Exposure 3253 Key References the complete reference list is available online at Expert Consult. The changing trends and profile of pneumocystosis mortality in the United States, 1999-2014. Echinocandin treatment of Pneumocystis pneumonia in rodent models depletes cysts leaving trophic burdens that cannot transmit the infection. Sterol metabolism in the opportunistic pathogen Pneumocystis: advances and new insights. Cell wall antigens of Pneumocystis carinii trophozoites and cysts: purification and carbohydrate analysis of these glycoproteins. Analysis of current antifungal agents and their targets within the Pneumocystis carinii genome. Mechanisms of surface antigenic variation in the human pathogenic fungus Pneumocystis jirovecii. Passive intranasal monoclonal antibody prophylaxis against murine Pneumocystis carinii pneumonia. Search for primary infection by Pneumocystis carinii in a cohort of normal, healthy infants. Pneumocystis jirovecii pneumonia in tropical and low and middle income countries: a systematic review and meta-regression. Enhanced in vivo human immunodeficiency virus-1 replication in the lungs of human immunodeficiency virus-infected persons with Pneumocystis carinii pneumonia. Immunosuppressed surfactant protein A-deficient mice have increased susceptibility to Pneumocystis carinii infection. Protection against Pneumocystis carinii pneumonia by antibodies generated from either T helper 1 or T helper 2 responses. Role of interleukin-23-dependent antifungal immune responses in dendritic cell-vaccinated mice. A new model of Pneumocystis carinii infection in mice selectively depleted of helper T lymphocytes. Adoptive transfer of lymphocytes sensitized to the major surface glycoprotein of Pneumocystis carinii confers protection in the rat. Neonatal T cells in an adult lung environment are competent to resolve Pneumocystis carinii pneumonia. Differential macrophage polarization from Pneumocystis in immunocompetent and immunosuppressed hosts: potential adjunctive therapy during pneumonia. Granulocyte-macrophage colony-stimulating factor in the innate immune response to Pneumocystis carinii pneumonia in mice. Atypical pathologic manifestations of Pneumocystis carinii pneumonia in the acquired immune deficiency syndrome. Review of 123 lung biopsies from 76 patients with Chapter 269 Pneumocystis Species 3254 178. Immune-mediated inflammation directly impairs pulmonary function, contributing to the pathogenesis of Pneumocystis carinii pneumonia. Pulmonary inflammation disrupts surfactant function during Pneumocystis carinii pneumonia. Regulatory T cells dampen pulmonary inflammation and lung injury in an animal model of Pneumocystis pneumonia. An evaluation of the performance of the Dynamiker(R) Fungus (1-3)-beta-D-Glucan Assay to assist in the diagnosis of Pneumocystis pneumonia. Trimethoprim-su lfamethoxazole compared with pentamidine for treatment of Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. A double-blind, randomized, trial of oral trimethoprim-sulfamethoxazole, dapsone-trimethoprim, and clindamycin-primaquine. Sulfa use, dihydropteroate synthase mutations, and Pneumocystis jirovecii pneumonia. Pathobiology of Pneumocystis pneumonia: life cycle, cell wall and cell signal transduction. De novo assembly of the Pneumocystis jirovecii genome from a single bronchoalveolar lavage fluid specimen from a patient. Sequence and structure of the linear mitochondrial genome of Pneumocystis carinii. Sequencing and characterization of the complete mitochondrial genomes of three Pneumocystis species provide new insights into divergence between human and rodent Pneumocystis. Pneumocystis jirovecii can be productively cultured in differentiated CuFi-8 airway cells. Treatment and prevention of Pneumocystis carinii pneumonia and further elucidation of the P. Transcriptome of Pneumocystis carinii during fulminate infection: carbohydrate metabolism and the concept of a compatible parasite. Expression, structure, and location of epitopes of the major surface glycoprotein of Pneumocystis carinii f. Passive immunoprophylaxis with specific monoclonal antibody confers partial protection against Pneumocystis carinii pneumonitis in animal models. Adoptive transfer of specific lymphocyte populations sensitized to the major surface glycoprotein of Pneumocystis carinii decreases organism burden while increasing survival rate in the rat. Immunization with the major surface glycoprotein of Pneumocystis carinii elicits a protective response. Pneumocystis carinii attachment to cultured lung cells by Pneumocystis gp 120, a fibronectin binding protein. Vitronectin binds to Pneumocystis carinii and mediates organism attachment to cultured lung epithelial cells. The carbohydrate recognition domain of surfactant protein A mediates binding to the major surface glycoprotein of Pneumocystis carinii. Surfactant protein D interacts with Pneumocystis carinii and mediates organism adherence to alveolar macrophages. Discordant antibody and cellular responses to Pneumocystis major surface glycoprotein variants in mice.
Discount snafi 20 mg on-line
Overtreatment of asymptomatic bacteriuria: identifying provider barriers to evidence-based care erectile dysfunction workup generic snafi 20 mg online. Reducing antimicrobial therapy for asymptomatic bacteriuria among noncatheterized inpatients: a proof-of-concept study. Effectiveness of an antimicrobial stewardship approach for urinary catheter-associated asymptomatic bacteriuria. Clinician practice and the National Healthcare Safety Network definition for the diagnosis of catheter-associated urinary tract infection. A multifaceted approach to reduction of catheter-associated urinary tract infections in the intensive care unit with an emphasis on "stewardship of culturing". Infection prevention and antimicrobial stewardship knowledge for selected infections among nursing home personnel. Chronic indwelling catheter replacement before antimicrobial therapy for symptomatic urinary tract infection. Two simple rules for improving the accuracy of empiric treatment of multidrug-resistant urinary tract infections. Colonization with third-generation cephalosporin-resistant Enterobacteriaceae on hospital admission: prevalence and risk factors. A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. A prospective, randomized trial of 3 or 14 days of ciprofloxacin treatment for acute urinary tract infection in patients with spinal cord injury. Pre- and postoperative predictors of infection-related complications in patients undergoing percutaneous nephrolithotomy. Systemic inflammatory response syndrome following percutaneous nephrolithotomy: assessment of risk factors and their impact on patient outcomes. Urinary infections in patients with catheters in the upper urinary tract: microbiological study. Nephrostomy tube related pyelonephritis in patients with cancer: epidemiology, infection rate and risk factors. Infectious complications associated with percutaneous nephrostomy catheters: do we know enough Candidemia from a urinary tract source: microbiological aspects and clinical significance. Investigation of the possible association between nosocomial candiduria and candidaemia. Candiduria: a randomized, double-blind study of treatment with fluconazole and placebo. Prevention of hospital-acquired infections: review of non-pharmacological interventions. Vaccine and immunoglobulin are recommended for those with immunocompromising or chronic liver conditions. Rapid decrease in measured antibody levels within months of immunization can occur despite persistence of immune protection. The potential for bloodborne transmission of hepatitis B first was noted in 1885, when Lurman described jaundice in factory workers who had received smallpox vaccine prepared from "human lymph. Central to these was the use of human volunteers, who were given putatively infectious material intradermally, intranasally, or by ingestion of feces, and then observed for development of jaundice. A spate of similar reports followed, describing occupationally acquired hepatitis among nurses, blood bank workers, phlebotomists, house staff, and others. Improved understanding of routes of transmission, more comprehensive and rigorous infection control including needle disposal, and, for hepatitis B, vaccination of workers at risk have helped to decrease, but not eliminate, this occupational risk. In United Kingdom, immune globulin is recommended to be given in conjunction with vaccine only for healthy adults older than 50 years, and those with chronic liver disease or an immunocompromising condition, regardless of age. The virus has caused several large-scale outbreaks among refugees and other displaced populations. Person-to-person spread among household contacts has been demonstrated only in resource-constrained settings, where transmission is attributed to poor sanitation and to communal hand-washing and eating practices. Certain areas in eastern Japan, southwestern France, and the Netherlands have exceedingly high seropositivity rates as a result of these factors. A detailed description of the epidemiology of hepatitis E can be found in Chapter 178. Blood donor screening data from several European countries have also demonstrated variable rates of hepatitis E viremia, ranging Seroprevalence of Hepatitis E in Developed Countries and Risk of Bloodborne Transmission Hepatitis B was the first bloodborne disease recognized to pose an occupational hazard. An early review found a preponderance of cases among pathologists, laboratory workers, and blood bank workers. Compliance with these recommendations has resulted in a 98% reduction in occupationally acquired hepatitis B,65,66 although rare cases continue to occur. In a majority of the cases, no obvious infection-control breaches or overt percutaneous exposures were recognized. Of note, the surgeon had declined hepatitis B vaccine 2 years earlier and then had become infected as the result of an occupational exposure. In one instance, a patient in the preclinical window period for hepatitis B sustained severe trauma and underwent several operations. As with worker-to-patient transmission, clustered cases lead to the identification of transmission more readily than individual transmissions. Clinically significant hepatitis has been reported in patients on dialysis who achieve a minimum protective antibody level but with subsequent decline. In some countries, nosocomial transmission due to unsafe practices continues to account for a substantial proportion of overall hepatitis B cases. Thorough review of the case failed to disclose any overt infection-control breach. Approximately 88% of individuals achieve seroprotective titers after vaccination; suboptimal responses are related to older age, obesity, and smoking. Therefore, serologic testing is routinely recommended for those with an anticipated risk of occupational exposure. Any additional immunization beyond the sixth dose is not recommended for those without a response to two complete series. Other studies conducted in areas of high endemicity have demonstrated breakthrough infection among vaccine responders marked by the development of antibodies against hepatitis B core protein. Vaccinated persons with an unknown response to vaccine should have their antibody titer checked immediately after exposure and should be treated according to the result (see Table 303. The role of antiviral agents such as lamivudine, entecavir, and tenofovir in the management of nosocomial exposure has not been determined. The best long-term management for the hepatitis B vaccine nonresponder is not known. Additional testing did not reveal transmission events originating from the anesthesiologist. In other reports from endoscopy clinics, the transmission may have occurred as a result of inadequate cleaning of the biopsy suction channel of the colonoscope or failure to autoclave some equipment, such as biopsy forceps. The only common link was an anesthesiologist who prepared medications on a cart that was rolled between operating rooms throughout the day without cleaning and disinfection in between. A surgeon may also have become dually infected after a deep needlestick sustained while operating on the same source patient. Review identified several additional possible instances of delta hepatitis transmission in dialysis centers. An additional benefit of hepatitis B vaccination is that the incidence of hepatitis D has also substantially declined. Risk factors for hepatitis C virus transmission to health care workers after occupational exposure: a European case-control study.
Purchase discount snafi online
There are two forms of circulating trypomastigotes: long xatral impotence cheap 20 mg snafi with amex, slender organisms that are capable 3349 3350 chancre, and there is an intense mononuclear cell reaction to the parasites, as well as edema and local tissue destruction. After this initial local response the infection evolves over weeks and months into a systemic hemolymphatic illness as the parasites disseminate widely through the lymphatic system and the bloodstream. The parasites first travel from the site of inoculation to regional lymph nodes, where they proliferate and cause an inflammatory response. They then move through the lymphatics into the bloodstream, where multiplication continues. Egress of trypanosomes from vessels into interstitial spaces, where multiplication also takes place, is thought to be facilitated by increased vascular permeability. In stage 1 trypanosomiasis there is widespread lymphadenopathy and histiocytic proliferation, which may be followed by fibrosis. These cells are plasmacytes with vacuolated cytoplasm and pyknotic nuclei that are thought to play a role in the production of immunoglobulin M (IgM). As the disease evolves, an endarteritis with perivascular infiltration of both parasites and lymphocytes may develop in lymph nodes and the spleen. A pancarditis may develop involving all layers of the heart, including the mural and valvular endocardia. A number of hematologic manifestations accompany the development of stage 1 disease. Normocytic anemia is a regular feature in this phase of the illness and is usually accompanied by a brisk reticulocytosis. Several factors are thought to contribute to the anemia, and immune-mediated hemolysis may be important. A moderate degree of leukocytosis is usually present, especially in the early months of the infection, and this is accompanied by polyclonal B-cell activation. High titers of immunoglobulins are a striking and constant feature of the illness. They consist primarily of polyclonal IgM that, for the most part, is not directed against specific parasite antigens. In addition, high levels of circulating antigen-antibody complexes are uniformly present, and these may play a role in the anemia, tissue damage, and increased vascular permeability that facilitate the dissemination of the parasites. Erythrocyte sedimentation rates are elevated, and hypocomplementemia has also been noted. Parasites reach the brain and meninges via the bloodstream and cause meningoencephalitis or meningomyelitis, or both. Edema and hemorrhages may be evident on gross examination of affected areas at autopsy. Trypanosomes are present in perivascular areas, and nests of organisms can be found without apparent relation to blood vessels. The parasite indicated by the arrow is typical of the long, slender forms capable of multiplying in the mammalian host. Once in the midgut of the tsetse flies, stumpy trypomastigotes transform into relatively long, slender procyclic trypomastigotes. After many cycles of multiplication the procyclic forms migrate to the salivary glands, where they differentiate into epimastigotes and continue to multiply. A final transformation occurs as the epimastigotes become nondividing metacyclic trypomastigotes. Transmission takes place when these infective forms are inoculated during a subsequent blood meal. The cycle is completed when the injected metacyclic forms become bloodstream trypomastigotes and begin to multiply in the blood or other extracellular spaces. The capacity of African trypanosomes to multiply in the bloodstream of their mammalian hosts, where they are continually exposed to humoral defenses, constitutes a fundamental difference between the agents of sleeping sickness and Trypanosoma cruzi, the cause of Chagas disease in the Americas. The African trypanosomes are able to evade immune destruction indefinitely because they undergo antigenic variation, a process in which they periodically change the antigenic structure of the coat of glycoproteins that covers the surface of the parasite. The molecular mechanisms that control this complex process have been studied intensively. Presumably, this occurs as a preadaptation to the relatively hostile environment of the mammalian host into which the metacyclics must be inoculated if they are to survive. Virtually all transmission of African trypanosomes to both wild and domestic animals, as well as to humans, takes place in the cyclic fashion just described. There is no evidence that these parasites can be transmitted by insects other than tsetse flies, and mechanical transmission by vectors is not important, although it may occur occasionally. Congenital transmission can occur, but in humans it is extremely rare,8,9 as is transmission by blood transfusion. A small number of laboratory accidents resulting in infection with African trypanosomes have been reported. Interstitial multiplication of the trypanosomes takes place within the 3351 a better understanding of the physiology of disease might influence assumptions about the pharmacokinetic characteristics of drugs in development. Angola, Uganda, South Sudan, and the Democratic Republic of Congo were particularly affected, and even today 80% of reported cases occur in the latter. Although underreporting is a persistent problem, there is no doubt, to the credit of the many organizations involved in these efforts, that the level of control reached to date is impressive. Distinguishing epidemiologic and clinical features of the two diseases are presented in Table 277. These vectors inhabit forests and wooded areas along rivers, where conditions of temperature, moisture, and darkness favorable for them are combined with the availability of mammalian blood. This distribution of the vectors restricts the occurrence of human infection to the tropical rain forests of Central and West Africa. Despite the facts that these tsetse flies adapt to feeding on a variety of mammals and T. The primary determinant of the risk of acquiring the infection is the frequency of contact with the vector. This risk increases during the dry season, when the density of both vectors and humans increases around limited numbers of water holes. Because of this pattern of transmission, West African trypanosomiasis is primarily a problem in rural populations, and tourists rarely become infected with T. This may be an important element in the persistence of the infection in the reservoir between epidemics. This subspecies is transmitted by tsetse flies of the morsitans group, principally Glossina morsitans, Glossina pallidipes, and Glossina swynnertoni. These vectors are widely distributed in savanna and woodland areas of Central and East Africa. Wild animals are the reservoir of this organism, principally antelope such as the bushbuck and hartebeest. These animals are trypanotolerant and generally do not suffer significant morbidity unless weakened by other illnesses. Many other wild and domestic animals can be infected with these parasites, but their importance as reservoirs is minimal because parasitemias are either low or they succumb quickly to the infection. Thus the illness is an occupational hazard for persons such as game wardens who work in areas where infected wild animals and vectors are present. An indurated, painful trypanosomal chancre may develop at the site where parasites were inoculated by an infected tsetse fly. This lesion usually appears 1 to 2 weeks after the bite of the infected fly and resolves spontaneously over several weeks. The chancre may ulcerate and reach a diameter of several centimeters; regional lymphadenopathy may also develop. Thus most patients develop systemic trypanosomiasis without experiencing the symptoms of localized disease. The development of stage 1 (hemolymphatic) disease with dissemination of the parasites is marked by fever, which may appear weeks or months after the acquisition of the infection. The fever is characterized by intermittent bouts of high temperatures lasting for several days, and extended periods may intervene during which the patient is afebrile. As the chronic illness evolves, a wide variety of other signs and symptoms develop. Supraclavicular and cervical nodes are often visibly discernible, and enlargement of the nodes of the posterior cervical triangle, or Winterbottom sign, is a classic finding in persons infected with T. Transient edema is a frequent sign during the hemolymphatic phase of the illness and can occur in the face, as well as in the hands, feet, 3352 and other periarticular areas.