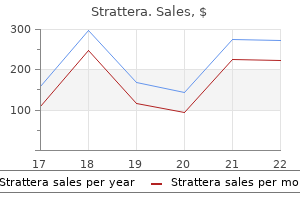
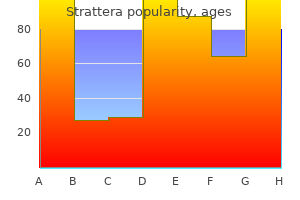
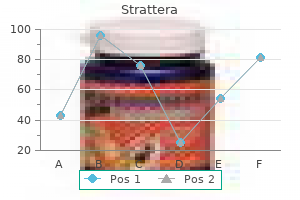
Strattera 18 mg generic
As fresh gas from the machine flowmeters enters the vaporizer inlet symptoms just before giving birth generic strattera 25mg overnight delivery, the concentration control dial setting determines the ratio of incoming gas that flows through the bypass chamber to that entering the vaporizing chamber (sump). The gas channeled through the vaporizing chamber flows over a wick system saturated with the liquid anesthetic and subsequently also becomes saturated with vapor. Thus, flowover refers to the method of vaporization and is in contrast to a bubble-through system that is used in now-obsolete measured flow vaporizers. Each is equipped with an automated temperaturecompensating device that helps maintain a constant vapor concentration output for a given concentration dial setting, and over a wide range of operating temperatures. These vaporizers are agent specific because each is designed to accommodate a single anesthetic agent, and are out-of-circuit, that is, physically located outside of the breathing circuit. Variable bypass vaporizers are used to deliver halothane, enflurane, isoflurane, and sevoflurane, but not desflurane. In principle, it creates a saturated vapor concentration of the liquid agent in the vaporizing chamber and dilutes this to clinically usable concentrations by mixing it with fresh gas from the vaporizer bypass. Therefore, the vaporizer must dilute this 21% concentration to a clinically desirable value indicated on the vaporizer dial. Vaporizer components include the concentration control dial, the bypass chamber, the vaporizing chamber, the filler port, and the filler cap. Using the filler port, the operator fills the vaporizing chamber with liquid anesthetic. The maximum safe fill level is predetermined by the position of the filler port, which is designed to minimize the likelihood of overfilling. If a vaporizer is overfilled or tilted, liquid anesthetic can spill into the bypass via the inlet and outlet chambers. If this were to happen, both the vaporizing chamber flow and the bypass flow could potentially be carrying saturated anesthetic vapor, and an overdose would result. The concentration control dial is a variable restrictor, which controls gas flow through the bypass and through the outlet of the vaporizing chamber. Most of the flow passes straight through the bypass chamber to the vaporizer outlet. Depending on the temperature and vapor pressure of the particular inhaled anesthetic, the fresh gas entering the vaporizing chamber entrains a specific flow of the anesthetic agent saturated vapor. The mixture that exits the vaporizer outlet comprises flow through the bypass chamber, flow through the vaporizing chamber, and flow of entrained anesthetic vapor. The final concentration of inhaled anesthetic (in volumes percent) is the ratio of the flow of the entrained anesthetic vapor to the total gas flow. If the vaporizer dial is set to deliver 1% sevoflurane, the bypass flow will be 2,000 mL/min because 21 mL of sevoflurane vapor will be diluted in a total volume of 2,100 mL (21 + 79 + 2,000); 21/2,100 = 1% by volume. To achieve this the vaporizer concentration dial has created a flow ratio of 2,000:100 or 20:1 between the bypass flow and the flow exiting the vaporizing chamber. When the dial is set to deliver 2% sevoflurane, the vaporizer concentration dial creates a ratio of 950:100, or 9. Each 100 mL of gas leaving the vaporizing chamber will contain 31 mL of isoflurane vapor, the other 69 mL being the gas that entered the vaporizing chamber. The bypass flow must be 3,000 mL because now 31 mL of isoflurane vapor is diluted in a total volume of 3,100 (31 + 69 + 3,000). The vaporizer concentration dial has created a flow ratio 1671 of 30:1 between the bypass flow and the flow exiting the vaporizing chamber. Variable bypass vaporizers incorporate a mechanism to compensate for variations in ambient temperature. To compensate for this, the bimetallic strip of the temperature-compensating valve leans to the right, decreasing the resistance to gas flow through the bypass chamber. This allows more flow to pass through the bypass chamber and less flow to pass through the vaporizing chamber. This increases the resistance to flow through the bypass chamber, causing relatively more flow to pass through the vaporizing chamber and less flow to pass through the bypass chamber. The net effect in both situations is maintenance of relatively constant vapor output concentration despite large swings in ambient temperature. Designing such a vaporizer is difficult because as ambient conditions change, the physical properties of gases and of the vaporizers themselves can change. Even though some of the most sophisticated vaporizing systems now available use computer-controlled components and multiple sensors, they have yet to become significantly more accurate than conventional mechanical flowsplitting (variable bypass) vaporizers. Fresh Gas Flow Rate With a fixed dial setting, vaporizer output can vary with the rate of gas flowing through the vaporizer. The output of all variable bypass vaporizers is less than the dial setting at low flow rates (<250 mL/min). This results from the relatively high density of volatile inhaled anesthetic vapors. At low flow rates, insufficient turbulence is generated in the vaporizing chamber to advance the vapor molecules upwardly. At extremely high flow rates, such as 15 L/min, the output of most variable bypass vaporizers is less than that set on the dial. This discrepancy is attributed to incomplete mixing and failure to saturate the carrier gas in the vaporizing chamber. In addition, the resistance characteristics of the bypass chamber and the vaporizing chamber can vary as flow increases. Temperature Because of improvements in design, the output of contemporary temperaturecompensated vaporizers is almost linear over a wide range of temperatures. Automatic temperature-compensating mechanisms in the bypass chamber maintain a constant vaporizer output with varying temperatures. In addition, the wick systems are placed in direct contact with the metal wall of the vaporizer to help replace energy (heat) consumed during vaporization. Here an expansion element performs the same function as the bimetallic strip in the previous figure. The materials from which vaporizers are constructed are chosen because they have a relatively high specific heat and high thermal conductivity. These factors help minimize the effect of cooling of the liquid anesthetic during vaporization. One proposed mechanism for the pumping effect is dependent on retrograde pressure transmission from the patient circuit to the vaporizer during the inspiratory phase of positive-pressure ventilation. When the back pressure is suddenly released during the expiratory phase of positive-pressure ventilation, vapor exits the vaporizing chamber via both the vaporizing chamber outlet and retrograde through the vaporizing chamber inlet. To decrease the pumping effect, the vaporizing chambers of contemporary variable bypass systems are smaller than those of older model vaporizers. Consequently, no substantial volumes of vapor can be discharged from the vaporizing chamber into the bypass chamber during the expiratory phase of ventilation. This check valve attenuates, but does not eliminate, the pressure increase because gas still flows from the flowmeters to the vaporizer during the inspiratory phase of positive-pressure ventilation. Conversely, the output of some older vaporizers is increased when nitrous oxide is the carrier gas instead of oxygen. Overfilling of vaporizers is minimized because the filler port is located at the maximum safe liquid level. Vaporizers are firmly secured to a vaporizer manifold on the anesthesia workstation and have antispill protection designs. Contemporary interlock systems prevent simultaneous administration of more than one inhaled volatile anesthetic. When 100% O2 is used, the concentration rises by 10% of the set value (not more than 0. Misfilling Vaporizers not equipped with keyed fillers have been occasionally misfilled with the wrong anesthetic liquid. A potential for misfilling exists even on contemporary vaporizers equipped with keyed fillers. Conversely, an isoflurane vaporizer misfilled with sevoflurane will deliver a lower concentration of sevoflurane than that set on the concentration dial.
Strattera 18 mg lowest price
Another proposal was antagonistic pleiotropy symptoms after flu shot buy cheap strattera 18mg line, meaning that a single gene has more than one phenotype (effect or trait). Lastly, the disposable soma theory suggested that the organism must allocate energy to bodily functions 2230 and resources that are focused upon early survival, growth, and reproduction while compromising repair functions that would prevent deterioration with age. A new, hierarchical approach to aging groups the mechanisms of aging into three tiers. Each time a cell divides, the telomeres get shorter, and when they become too short, the cell can no longer divide. Most of the genome undergoes gradual demethylation while other, specific regions undergo hypermethylation, leading to disrupted transcription. Lastly, the production, folding, and degradation of proteins within the cell regulate their functionality. The second tier includes antagonistic mechanisms that are primarily beneficial and protect the younger individual from damage or nutrient shortage. Mechanisms in the second tier include senescence, a state in which the cell is alive and metabolically active but is not capable of dividing. The third tier consists of integrative mechanisms which operate when the accumulated damage caused by the primary and antagonistic hallmarks cannot be compensated by tissue homeostatic mechanisms: stem cell numbers 2231 decline with age, suggesting that there has been a failure to replace damaged cells. Deregulated neurohormonal signaling in the aged is implicated in development of diseases such as hypertension, heart failure, diabetes, and malignancies. The newly coined term "geroscience" refers to an interdisciplinary field which aims to understand the relationship between aging and age-related diseases. Studying aging mechanisms across a wide variety of pathologies raises an important question: are aging and disease different processes or are they, at least to some degree, inseparable Elucidating each one of these processes could provide not just insight but potential solutions for the other. Most of the gains in average human life span have been as the result of reducing those factors that cause premature death: predation, accidents, and disease. The inability to thwart aging entirely implies that the human life span is limited, and that if everyone died only of "old age," the age at death would end up being a bell-shaped curve centered at a certain value, probably around age 85. The focus of research has transitioned from just extending the number of years lived (life span) to extending the period during which one is generally healthy and free from serious comorbidities (healthspan). Several interventions (smoking cessation, weight loss, and exercise) have been shown to improve both life span and healthspan. For healthy individuals, reserve peaks at approximately age 30, gradually declines over the next several decades, and then experiences more rapid decline beginning around the eighth decade. For example, the ability to achieve a minimum of four metabolic equivalents appears to confer enough cardiovascular reserve to tolerate the stress of most surgical procedures. Frailty is a result of cumulative declines across multiple physiologic systems, and causing vulnerability to adverse outcomes. Although the diagnosis of frailty is often intuitive, there are two classical ways to define it. The first method is the frailty phenotype which is defined as a clinical syndrome in which three or more of the following criteria are present: unintentional weight loss (10 lb in past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity. A list of symptoms, signs, diseases, and disabilities are surveyed and scored in a binomial fashion (yes/no), and the fraction of the positive deficits from the total number surveyed is calculated. Numerous studies that used a range of assessment tools to determine frailty status have shown that frail patients undergoing surgical procedures had a higher likelihood than nonfrail patients of experiencing mortality, morbidity, complications, increased hospital length of stay, and discharge to an institution. In the general nonsurgical population, trials of exercise (resistance training, aerobic training, balance, and flexibility), nutritional supplements, and pharmaceutical agents show limited success at reversing frailty and improving outcomes. Ideally, an index of physiologic age would be available that would quantify functional reserve. One interesting approach to this objective that is available to the lay public is to quantify many of the known modifiable and nonmodifiable factors that influence life expectancy. Such an approach may be useful for promoting a healthy lifestyle, but does not address the ultimate goal of being able to quantify the reserve of each organ system, including the brain, and predict the risk of common perioperative complications. Is it what happens under 2234 the best of circumstances, or what happens to the "average" person Comparisons of young and elderly subjects may not strictly reflect aging, as the elderly subjects may have experienced a much different diet, lifestyle, and environmental exposure than what the young group will have experienced by the time they become old. Following a group of healthy subjects over a long period is more likely to define the effects of aging, but not all available data come from such longitudinal studies. Studies that examine only the very old may actually underestimate the typical effects of aging because individuals generally do not achieve old age unless there is something intrinsically robust about them. The effect of aging varies considerably from one patient to another, and, disease will interact with aging to further diminish functional organ reserve. Basal metabolism declines with age, with most of the decline accounted for by the change in body composition. Liver mass decreases with age, and accounts for most, but not all, of the 20% to 40% decrease in liver blood flow. Other than the effect of aging on drug metabolism, liver reserve should be more than adequate even in the very old in the absence of disease. Renal cortical mass also decreases by 20% to 25% with age, but the most prominent effect of aging is the loss of up to half of the glomeruli by age 80. Nevertheless, the degree of decline in glomerular filtration rate is highly variable and is likely to be much less than predicted in many individuals, especially those who avoid excessive dietary protein. In women, total body mass remains constant because increases in body fat (upper shaded segment) offset bone loss (middle segment) and intracellular dehydration (lower shaded segment). In men, body mass declines despite maintenance of body lipid and skeletal tissue elements because accelerating loss of skeletal muscle and other components of lean tissue mass produces marked contraction of intracellular water (lower shaded segment). The aged kidney does not eliminate or retain sodium when necessary as effectively as that of a young adult. Similarly, the aged kidney does not retain or eliminate free water as rapidly as young kidneys when challenged by water deprivation or free water excess. In short, fluid and electrolyte homeostasis is more vulnerable in the older patient, particularly when an older patient suffers acute injury or disease and eating and drinking becomes more of a chore. For the most part, functional endocrine decline does not interact with anesthetic management to any significant degree. However, aging is associated with decreased insulin secretion in response to a glucose load, and also increased insulin resistance, particularly in skeletal muscle. Aging also results in decreases in testosterone, estrogen, and growth hormone production. Response times increase, and learning is more difficult, but vocabulary, "wisdom," and past knowledge are better preserved. Fortunately, and contrary to prior belief, the aged brain does make new neurons and is capable of forming new dendritic connections. More difficult to manage is the potential interaction of anesthesia, the stress of surgery, and a brain with minimal reserve. Age is a major risk factor for postoperative delirium and/or cognitive decline (see "Perioperative Complications"). The cause can be either pharmacodynamic, in which case the target organ (often the brain) is more sensitive to a given drug tissue level, or pharmacokinetic, in which case a given dose of drug commonly produces higher blood levels in older patients. Most intravenous anesthetic drugs are highly lipid soluble and so begin to enter tissue even before fully mixed in the blood. The rate of transfer depends on the rate of delivery (concentration times blood flow per gram of tissue), the concentration gradient of the drug between the blood and the tissue 2237 (obviously a high gradient initially), the ease with which the drug crosses the blood and tissue membranes, and the solubility of the drug in the tissue. Thus, the vessel-rich group (brain, heart, kidney, muscle) will acquire drug much more rapidly than the vessel-poor group (fat, bone). Protein binding may affect transfer, with drugs that are highly protein-bound having a lower free concentration and a slower rate of transfer. Given the preceding, there are many ways for a drug bolus to have a more pronounced initial effect on older patients. During the drug redistribution phase the blood concentration typically is higher in older patients, partly because of a mildly contracted blood volume and partly because the reduction in muscle mass limits the rate and amount of drug removal by muscle. By keeping drug blood levels higher for a longer time, more drug will be driven into the other organs of the vessel-rich group such as the brain (often the target organ) or heart. A prime example of this phenomenon is sodium pentothal, and to a lesser degree, propofol. Slower circulation is sometimes hypothesized, but total blood flow to any organ does not appear to decrease beyond that expected from the decrease in organ mass. Ultimately, though, the drug will distribute throughout the body based on tissue mass and solubility. Because most intravenous drugs used in anesthesia are highly lipid-soluble, most of the drug will end up in fat.
Effective strattera 10mg
Arterial waveform analysis for the anesthesiologist: Past in treatment 1 buy strattera 18 mg low cost, present, and future concepts. Although the previous analysis is necessarily simplified, it nevertheless illustrates the fundamental principles and requirements of these devices. A stiff arterial line, flushed from a pressurized fluid source, is attached to the arterial cannula in the usual fashion. These values, in the manner estimated by the device, are most useful for assessing relative volume status and for assessing the response to fluid resuscitation. The same contraindications that apply to arterial lines, such as poor or absent collateralization of arterial supply to the extremity, also apply to these devices. There are many disease states, some common, which violate these assumptions and can significantly compromise the accuracy of the device; these are discussed later. Satisfactory operation depends upon good arterial perfusion to the site of measurement and good peripheral arterial cannulation. The pressure transducer system must use appropriate tubing and be flushed and zeroed correctly so that bias, signal dampening, or flail are not seen in the arterial waveform. These artifacts corrupt the frequency spectrum of the arterial waveform, and impair accurate measurement. The use of an intra-aortic balloon pump may distort the arterial waveform to such an extent that the resulting waveform is uninterpretable, rendering the device inoperative. In contrast, all of the current monitors make use of algorithms that depend on information obtained over many cardiac cycles. The FloTrac monitor depends, for example, upon the standard deviation, skewness, and kurtosis of the statistical distribution of arterial pressures obtained over the preceding 20 seconds. With ongoing research and refinement of the devices and their algorithms, this situation appears to be improving. This assumption is violated in the setting of aortic insufficiency, in which there is negative regurgitant flow to the left ventricle. Arterial waveform analysis is expected to demonstrate inaccuracy in this presentation. Use of the entirely noninvasive ClearSight/Nexfin system has so far been limited in clinical practice. The degree to which a new monitoring technique must agree with the gold standard to be clinically useful is a matter of clinical judgment and not a question that can be definitively addressed by statistics alone. Presently, these devices appear to be most useful as guides to fluid resuscitation and for trend monitoring rather than as guides to the administration of inotropes or vasopressors. There are a number of relatively common clinical scenarios in which the accuracy of these devices 1802 can be anticipated to be impaired based upon violation of the underlying physiologic assumptions on which their algorithms depend. In adults, thermoregulation involves the control of basal metabolic rate, muscular activity, sympathetic arousal, vascular tone, and hormone activation balanced against exogenous factors that determine the need for the body to create heat or to adjust the transfer of heat to the environment. Both general and regional anesthesia inhibit afferent and efferent control of thermoregulation. Radiation refers to the infrared rays emanating from all objects above absolute temperature. Perioperative hypothermia predisposes patients to increases in metabolic rate (shivering) and cardiac work, decreases in drug metabolism and cutaneous blood flow, and creates impairments of coagulation. Anesthesiologists frequently monitor temperature and attempt to maintain central core temperature at near-normal values in all patients undergoing anesthesia. Clinical studies have demonstrated that patients in whom intraoperative hypothermia develops are at a higher risk for development of postoperative myocardial ischemia and wound infection compared with patients who are normothermic in the perioperative period. Thermoregulatory responses are based on a physiologically weighted average reflecting changes in the mean body temperature. Contraindications There are no absolute contraindications to temperature monitoring. In patients whose thermoregulatory responses are intact, such as conscious patients or patients receiving light or moderate sedation, continuous temperature monitoring is usually uninformative. Common Problems and Limitations Skin temperature monitoring has been advocated to identify peripheral vasoconstriction but is not adequate to determine alterations in mean body temperature that may occur during surgery. Core temperature sites have been established as reliable indicators of changes in mean temperature. During routine noncardiac surgery, temperature differences between these sites are small. When anesthetized patients are being cooled, changes in rectal temperature often lag behind those of other probe locations, and the adequacy of rewarming is best judged by measuring temperature at several locations. Although liquid crystal skin temperature strips are convenient to apply, they do not correlate with core temperature measurements. Occlusion of one of the carotid arteries for surgery makes the ipsilateral side of the brain 1804 dependent on perfusion from the contralateral carotid artery via the Circle of Willis, creating a risk of ipsilateral ischemia. In the event that the configuration of the sensors is unacceptable, the device displays a pictorial indication of the problem so that the practitioner can attempt to remedy the problem. If the electrical connection between the sensor and the skin is poor, signal reception will be impaired and the device will warn that the sensor impedance. The sensors make use of a conductive electrical gel; this can often be remedied by applying firm but careful pressure to the affected sensor to produce a better electrical contact. However, too much pressure may cause the gel to leak out from under the sensor and cause a "gel bridge," an inadvertent direct electrical connection to a neighboring electrode. In this case, the surplus gel may be wiped away or a new set of sensors may be required. Burst suppression is also seen in unanesthetized comatose patients, although in these patients it carries a grave prognosis. Changes in this ratio appear to correlate clinically with the onset of light sedation. A high level of bicoherence is suggestive that the signals may be generated from a common underlying rhythm. This 1806 relationship between concentration and effect is not seen for all anesthetic agents. However, the use of endtidal agent concentration monitoring assumes that volatile anesthetic gases are used and that their end-tidal concentrations provide a reasonable surrogate for their action on consciousness. Patients with pre-existing cognitive deficits, sensory impairment,144 or known risk of postoperative delirium may benefit from the administration of less anesthesia than would be indicated by end-tidal agent monitoring alone. Mechanically ventilated patients in the intensive care unit are usually 1808 assessed clinically for their level of sedation, but the use of the standard Sedation-Agitation Scale or the Richmond Agitation-Sedation Scale may be impossible in some patients due to therapeutic neuromuscular paralysis. Placement may also be relatively contraindicated in patients with existing superficial injury to the forehead in the region where the sensors will be applied. Disfiguring injury to the forehead has been reported,150 perhaps related to a combination of pressure and irritation from the conductive gel on the sensors. Prone positioning requires vigilant attention to facial features, such as the eyes and nose, to avoid injury by pressure and impingement. This difficulty may relate to our lack of understanding of what "anesthetic depth" 1809 even means. These, even taken individually, are complex and incompletely understood processes. Compared to adults, pediatric patients have more than three times greater incidence of awareness under anesthesia. Future Trends in Monitoring Anesthesiologists have been at the forefront of the incorporation of innovative biomedical devices and technologies into their practice. We will continue to adapt our practice to make use of new technologies to enhance patient safety. There are three trends in device design that appear most likely to lead to further improvements in our practice: greater automated marshaling of monitoring and clinical data, the dissemination of our current devices into wider hospital use, and the development of devices with greater algorithmic sophistication to obtain clinical data less invasively. Overall, improvements in the automated marshaling and display of patient data will assist the anesthesiologist with situational awareness. Moderate sedation may be performed by clinicians untrained in the practice of anesthesia; the effect of this standard will be the dissemination of capnographic equipment previously used only by anesthesiologists to the wider care environment. Anesthesiologists should be at the forefront of educational efforts to ensure that our medical colleagues use these devices appropriately, enhancing patient safety. A trend in the development of biomedical devices is toward devices that use complex algorithmic models to infer clinical data in a less invasive or more rapid manner. These devices are examples of incredible biomedical sophistication, usually the product of decades of scientific research and subsequent engineering refinement.

Purchase 40mg strattera overnight delivery
Bradycardia is reliably treated with atropine or glycopyrrolate medications going generic in 2016 order strattera in united states online, which is often given as a pretreatment for bradycardia prophylaxis as well as its antisialagogue effect. Hypotension can be corrected with phenylephrine or ephedrine and hypertension is treated by decreasing the rate of or stopping, the dexmedetomidine infusion. Deep sedation with any agent should not be confused with awake intubation, during which the patient remains responsive to verbal commands. Administration of an antisialagogue is important to the success of awake intubation techniques, as even small amounts of liquid can obscure the objective lens of indirect optical instruments. Antisialagogues have the secondary benefit of increasing the effectiveness of topical anesthetics by limiting secretions that may act as a barrier to mucosal contact. Additionally, copious salivary secretions will act as an intra-airway foreign body and may cause cough or laryngospasm. As the drying effects of these medications may take some time (approximately 15 minutes), they are often administered in the preoperative waiting area. Vasoconstriction of the nasal passages is required if there is to be instrumentation of this part of the airway. Oxymetazoline is a potent and long-lasting vasoconstrictor commonly used to this effect. As with the antisialagogues, the effects of this medication are not immediate and it is often administered in the preoperative waiting area. If the patient is at increased risk for gastric regurgitation and aspiration, prophylactic measures should be undertaken as discussed above. The airway, from the base of the tongue to the bronchi, is exquisitely sensitive as an evolutionary necessity. Topical anesthesia and injected nerve block techniques have been developed to blunt the protective reflexes and provide airway analgesia. The 1965 clinician should have a thorough understanding of the mechanism of action, metabolism, toxicities, and acceptable cumulative doses of any drug they choose to employ in the airway. In a human study, 400 or 800 mg of lidocaine gel was applied topically to the upper airway. Despite the myriad of local anesthetics available, only those most commonly used in airway preparation will be discussed here. In reality, the choice of local anesthetic employed has little to do with success of the technique of awake intubation; ignoring the other aspects of preparation leads to failure just as readily. Benzocaine, an ester local anesthetic, is popular among some clinicians because of its very rapid onset (<1 minute) and short duration (approximately 10 minutes). It is available in 10%, 15%, and 20% solutions and has been combined with tetracaine in some preparations to prolong the duration of action. With the toxic dose being 100 mg, caution must be taken not to spray too liberally. Absorption of this drug from the respiratory and gastrointestinal tracts is rapid. Toxicity after nebulized application has been reported with doses as low as 40 mg, although the acceptable safe dose in adults is 100 mg by other routes of application. Not only is it a highly effective local anesthetic, but it is also the only local anesthetic that is a potent vasoconstrictor. Cocaine is commonly available in a 4% solution and the total dose applied to the mucosa should not exceed 200 mg in the adult. Cocaine should not be used in patients with known cocaine hypersensitivity, hypertension, ischemic heart disease, preeclampsia, or those taking monoamine oxidase inhibitors. Because cocaine is metabolized by 1966 pseudocholinesterase, it is also contraindicated in patients who are deficient in this enzyme. For awake airway management, local anesthetic therapy is directed to three anatomic areas: the nasal cavity/nasopharynx, the pharynx/base of the tongue, and the hypopharynx/larynx/trachea. First, if during the course of the awake intubation the plan is changed from the oral to the nasal route, preparation is complete. Second, much of the preparation of the nose with local anesthesia will also affect the pharyngeal airway. The palatine nerves arise from the sphenopalatine ganglion located posterior to the middle turbinate. In the noninvasive nasal approach, cotton-tipped applicators soaked in local anesthetic are passed along the lower border of the middle turbinate until the posterior wall of the nasopharynx is reached and left there for 5 to 10 minutes. In the invasive oral approach, a needle is introduced into the greater palatine foramen, which can be palpated in the posterior-lateral aspect of the hard palate 1 cm medial to the second and third maxillary molars. A spinal needle inserted in a superior/posterior direction to a depth of 2 to 3 cm and anesthetic solution (1 to 2 mL) is injected, taking care to avoid intravascular (sphenopalatine artery) injection. The anterior ethmoidal nerve can be blocked by cottontipped applicators soaked in local anesthetic and placed along the dorsal surface of the nose until the anterior cribriform plate is reached. The oropharynx is innervated by branches of the vagus, facial, and glossopharyngeal nerves. The simplest techniques involve aerosolized local anesthetic solution, or a voluntary local anesthetic "swish and swallow. As it also supplies the afferent limb for the pharyngeal (gag) reflex, anesthesia of the glossopharyngeal nerve is key to comfortable awake airway management. Even after local anesthetic topicalization, some patients may still require a glossopharyngeal nerve block for complete ablation of the gag reflex. The branches of the glossopharyngeal nerve are most easily accessed as they transverse the palatoglossal folds. These folds are seen as soft tissue ridges that extend from the posterior aspect of the soft palate to the base of the tongue bilaterally. A noninvasive technique employs anesthetic-soaked cotton-tipped applicators held gently against the inferior most aspect of the contralateral folds for 5 to 10 minutes. When this noninvasive technique proves inadequate, local anesthetic can be injected in a similar manner. Standing on the contralateral side, the operator displaces the extended tongue and a 25-gauge spinal needle is inserted into the fold near the floor of the mouth and an aspiration test is performed. If air is aspirated, the needle has passed through-and-through the membrane and is withdrawn slightly prior to injection. The lingual branch is most readily blocked in this manner, but retrograde tracking of the injectate has also been demonstrated. As the site of needle insertion is behind the palatopharyngeal arch where it is difficult to see, and in close proximity to the carotid artery, this advanced technique will not be described here and the reader is referred to a more authoritative text. A local anestheticsoaked swab placed in the gutter along the base of the tongue is left in contact with the fold for 5 to 10 minutes to produce an ipsilateral glossopharyngeal nerve block. The internal branch of the superior laryngeal nerve provides sensory innervation to the base of the tongue, posterior surface of the epiglottis, aryepiglottic folds, and arytenoids. This branch originates lateral to the cornu of the hyoid bone, pierces the thyrohyoid membrane and travels under the mucosa in the pyriform recess. The external branch of the superior laryngeal nerve supplies motor innervation to the cricothyroid muscle and has no sensory component. In many instances, topical application of anesthetics in the pharyngeal/hypopharyngeal cavities will provide adequate analgesia. For a targeted noninvasive technique, the patient is asked to open their mouth widely and the tongue is grasped with a gauze pad. An invasive block may be performed with the patient supine with the head 1969 extended and the clinician standing on the side of the nerve to be blocked. The clinician identifies the greater cornu of the hyoid bone beneath the angle of the mandible. Using one hand, medially directed pressure is applied to the contralateral hyoid cornu, displacing the hyoid toward the clinician. The needle can then be inserted directly over the ipsilateral greater cornu and "walked" off the bone in an inferomedial direction until it can be passed through the thyrohyoid ligament to a depth of 1 to 2 cm. Before injecting local anesthetic, an aspiration test should be performed to ensure that one has not entered the pyriform sinus or a vascular structure. Sensory innervation of the vocal folds and the trachea is provided by the recurrent laryngeal nerve, another branch of the vagus nerve. Transtracheal injection of local anesthetic is a simple technique that can produce adequate analgesia of these structures.
Cheap 40 mg strattera
The terminal infraorbital nerve penetrates through the inferior orbital fissure to the base of the orbit symptoms webmd purchase strattera on line, to the infraorbital groove and canal (just below the eye and lateral to the nose), and reaches the facial surface of the maxilla. It then divides into the palpebral (lower eyelid), nasal (wing of the nose), and labial nerves (upper lip). The mandibular nerve is the third and largest branch of the trigeminal nerve and the only one to receive motor fibers. It exits the skull posterior to the maxillary nerve through the foramen ovale, forms a short thick trunk, and then divides into anterior and posterior trunks, which are mainly motor and sensory, respectively. The main branch (posterior trunk) continues as the inferior alveolar nerve medial to the ramus of the mandible and innervates the molar and premolar teeth. This nerve curves anteriorly to follow the mandible and exits as a terminal branch (mental nerve) through the mental foramen. Other terminal nerves include the lingual nerve (floor of mouth and anterior two-thirds of tongue) and the auriculotemporal nerve (ear and temple). The roots of the trigeminal nerve arise from the pons and form the large Gasserian (or semilunar) ganglion. The main terminal fibers of the ophthalmic nerve-the frontal nerve-terminate as the supraorbital and supratrochlear nerves and exit their respective foramina. The maxillary and mandibular branches emerge from the skull medial to the lateral pterygoid plate. The maxillary nerve terminates as the infraorbital nerve (through the infraorbital foramen), and the mandibular nerve provides the inferior alveolar nerve (as well as motor branches), which exits at the mental foramen as the mental nerve. The cervical plexus is unique in that it divides early into cutaneous branches (penetrating the cervical fascia) and muscular branches (deeper branches that innervate the muscles and joints), which can be blocked separately (see Specific Techniques section). The transverse processes of the cervical vertebrae form elongated troughs for the emergence of their nerve roots. The trough at the terminal end of the transverse process divides into an anterior and a posterior tubercle, which can often be easily palpated. These tubercles also serve as the attachments for the anterior and middle scalene muscles, which form a compartment for the cervical plexus as well as the brachial plexus immediately below. The compartment at this level is less developed than the one formed around the brachial plexus. The deep muscular branches curl anteriorly around the lateral border of the anterior scalene and then proceed caudally and medially. Many branches serve the deep anterior neck muscles, but other branches include the inferior descending cervical nerve, the trapezius branch of the plexus, and the phrenic nerve, which give anterior branches to the sternocleidomastoid muscle as they pass behind it. The sensory fibers emerge behind the anterior scalene muscle but separate from the motor branches and continue laterally to emerge superficially under the posterior border of the sternocleidomastoid muscle. The branches, including the lesser occipital nerve, great auricular nerve, transverse cervical nerve, and the supraclavicular nerves (anterior, medial, and posterior branches), innervate the anterior and posterior skin of the neck and shoulder. The motor branches (including the phrenic nerve) curl anteriorly around the anterior scalene muscle and travel caudally and medially to supply the deep muscles of the neck. The sensory branches exit at the lateral border of the sternocleidomastoid muscle to supply the skin of the neck and the shoulder. The nerve roots exit the vertebral column via troughs formed by the transverse processes. Occipital Nerve 2369 the ophthalmic branch of the trigeminal nerve provides sensory innervation to the forehead and anterior scalp. The remainder of the scalp is innervated by fibers of the greater and lesser occipital nerves. The greater occipital nerve arises from the posterior ramus of the second cervical spinal nerve (the cervical plexus arises from the anterior rami) and travels in a cranial direction to reach the skin in the area of the superior nuchal line while giving branches to supply the head and laterally toward the ear. Spine Spinal/epidural anesthesia is not discussed in this chapter, but a basic description of the spinal nerves as well as vertebral structures is provided, given their relevance to the performance of other regional blocks. Spinal Nerves the spinal nerves are part of the peripheral nervous system, along with the cranial and autonomic nerves and their ganglia. In addition, all spinal nerves contain sympathetic fibers for supplying blood vessels, smooth muscle, and glands in the skin. The nerves give off sympathetic branches immediately after leaving the intervertebral foramen. Soon after exiting the intervertebral (spinal) foramina, each spinal nerve divides into a larger ventral and a smaller dorsal ramus (branches). The ventral rami course laterally and anteriorly to supply the muscles, subcutaneous tissues (superficial fascia) and skin of the neck, trunk, and the upper and lower extremities (see layout of dermatomes in. The dorsal rami course posteriorly and supply the paravertebral muscles, subcutaneous tissues, and skin of the back close to the midline. It is important to realize that the first cervical (C1) nerve leaves the spinal cord and courses above the atlas (C1 vertebra). Hence the cervical nerves are numbered corresponding to the vertebrae inferior to them. From this point on, all the spinal nerves are named corresponding to the vertebral level above. For example, the T3 and L4 spinal nerves exit below the T3 and L4 vertebrae, respectively. Paravertebral Space the paravertebral space is a bilateral wedge-shaped area between the individual vertebrae, on both sides of and extending the entire length of the vertebral column. The spinal nerves pass through this space, giving off their sympathetic branch and a small dorsal sensory branch before exiting from the intervertebral foramina. The intervertebral foramina at each level lie between the transverse processes and approximately 1 to 2 cm anterior to the plane formed by the transverse processes in their associated fasciae. At this point, the sympathetic ganglia lie close to the somatic nerves, and coincidental sympathetic blockade is usually attained. Orientation of the Vertebral Body Processes 2371 There are variations in the anatomy of the vertebral column that should be considered when determining the desired location for needle insertion during trunk blocks. The plexus consists of five roots, three trunks, six divisions (two per trunk), three cords, and five major terminal nerves. They finally emerge between the scalenus anterior and medius muscles, above the second part of subclavian artery and posterior to vertebral artery. At the lateral border of first rib, each trunk bifurcates into anterior and posterior divisions. Immediately beyond the pectoralis minor muscle, the three cords diverge into the terminal branches, including the median, ulnar, radial, axillary, and musculocutaneous nerves. The phrenic nerve normally descends anterior to the scalenus anterior muscle and crosses the muscle from lateral to medial as it descends and passes under the clavicle and through the superior thoracic aperture into the superior mediastinum, just medial to the external jugular vein. However, there is anatomic variation of the course of the phrenic nerve, and it is not always anterior to the scalenus anterior muscle. Not shown are the many branches, including the medial cutaneous nerves of the forearm and arm, which arise from the medial cord. The axillary nerve is an additional terminal nerve of the upper extremity, but the anatomy and blockade of this nerve will not be discussed here. The anterior view shows branches from the lateral (musculocutaneous and median nerves) and medial (median and ulnar nerves) cords, whereas the posterior view shows branches from the posterior cord (axillary and radial nerves). Anatomic Variation There are many variations in the anatomy of the brachial plexus75 and in the course of the terminal nerves and vascular elements.
Strattera 10 mg without a prescription
Although cricothyrotomy is the procedure of choice in an emergency situation medications used to treat fibromyalgia order 18 mg strattera fast delivery, it may also be of use in elective situations when there is limited access to the trachea. Cricothyrotomy is contraindicated in children younger than 6 years of age and in patients with laryngeal fractures. Otolaryngologists and other surgical services prefer transtracheal airway access caudad to the cricoid cartilage 1985 whenever feasible due to the high incidence of long-term complications after surgical cricothyrotomy. As an example, the success rate of cannula cricothyrotomy performed by an anesthesia provider is roughly 50%,1 while the success rate of an emergency surgical airway performed by a surgeon or trained prehospital provider is 90% to 100%. A large-bore translaryngeal catheter (14 gauge or larger) attached to a 5- to 10-mL empty or fluid-filled (saline or local anesthetic) syringe is used. From the moment of skin puncture, there should be constant aspiration on the syringe plunger. Free aspiration of air confirms entrance into the trachea (aircontrast technique) but does not indicate the direction that the catheter travels in the larynx; this is important, as cephalad advancement will not provide adequate oxygenation. Once the catheter has been successfully placed, a high-pressure oxygen source should be attached. A 50-psi oxygen source with a metered and adjustable hand-controlled valve and a Luer-lock connector. Insufflation and expiration ratios, as well as driving pressure, are adjusted to provide visible chest excursion and recoil. If a 14-gauge catheter has been placed, this system will deliver a tidal volume of 400 to 700 mL. Low-pressure systems cannot provide enough flow to expand the chest adequately for oxygenation and ventilation. These systems are capable of delivering a constant flow of 15 L/min and have been shown to be effective for resuscitation. For example, using a standard three-way stopcock as a flow diverter is potentially hazardous, as forward flow (inspiration) is never fully stopped. The Enk flow modulator has been used successfully in models of near and complete upper airway obstruction. The clear benefit is the avoidance of air trapping in the lungs, especially when the upper airway is completely obstructed. While both devices facilitated reoxygenation, the Ventrain was associated with superior minute ventilation (4. The Ventrain has also proven effective in both elective and emergent human airway management. Specialized percutaneous cricothyrotomy systems have been developed to improve the ease of transtracheal ventilation. These devices generally provide large-bore access adequate for oxygenation and ventilation with low-pressure systems. Preparation and positioning of the patient are the same as with needle cricothyrotomy. After air is aspirated, the catheter is advanced into the trachea as described earlier. The catheter is removed and the large-bore tracheal cannula, fitted internally with a curved dilator, is threaded onto the wire. Significant resistance on advancement typically indicates that the skin incision needs to be extended. Conclusions Apart from monitoring, management of the "routine" airway is the most common task of the anesthesia provider. Even during the administration of regional anesthesia, the airway must be monitored and possibly supported. The consequences of a lost airway are so devastating that the clinician can never afford a lackadaisical approach. Judgment, experience, the clinical situation, and available resources all affect the appropriateness of the chosen pathway through, or divergence from, the algorithm. Although an increasingly vast array of devices exists, the clinician does not need to be expert in all the equipment and techniques, and no single device can be considered superior to another when viewed in isolation. Rather, a broad range of approaches should be mastered so that the failure of one does not preclude safe airway management and emergency rescue. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. The Airway Approach Algorithm: a decision tree for organizing preoperative airway information. The position of the larynx in children and its relationship to the ease of intubation. The accuracy of locating the cricothyroid membrane by palpation-an intergender study. Ultrasonography for clinical decision-making and intervention in airway management: from the mouth to the lungs and pleurae. The lingual tonsillar hyperplasia in relation to unanticipated difficult intubation: is there any relationship between lingual tonsillar hyperplasia and tonsillectomy Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. A simplified risk score to predict difficult intubation: Development and prospective evaluation in 3763 patients. Predictive value of the El-Ganzouri multivariate risk index for difficult tracheal intubation: a comparison of Glidescope videolaryngoscopy and conventional Macintosh laryngoscopy. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Inadequate preoxygenation during spontaneous ventilation with single patient use self-inflating resuscitation bags. Sniffing position improves pharyngeal airway patency in anesthetized patients with obstructive sleep apnea. The effect of leaving dentures in place on bag-mask ventilation at induction of general anesthesia. Ventilation by mask before and after the administration of neuromuscular blockade: a pragmatic non-inferiority trial. The use of ProSeal laryngeal mask airway in caesarean section-experience in 3000 cases. Endotracheal intubation, but not laryngeal mask airway insertion, produces reversible bronchoconstriction. Difficult airway management practice patterns among anesthesiologists practicing in the United States: have we made any progress A comparative study of positive pressure ventilation via laryngeal mask airway and endotracheal tube. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: a prospective, randomized trial. The incidence of aspiration associated with the laryngeal mask airway: a meta-analysis of published literature. The laryngeal mask airway is effective (and probably safe) in selected healthy parturients for elective Cesarean section: a prospective study of 1067 cases. The incidence of regurgitation during cardiopulmonary resuscitation: a comparison between the bag valve mask and laryngeal mask airway. Survey of laryngeal mask airway usage in 11,910 patients: safety and efficacy for conventional and nonconventional usage. Comparison of the reinforced laryngeal mask airway and tracheal intubation for adenotonsillectomy. Subglottic secretion drainage for preventing ventilator-associated pneumonia: a meta-analysis. An investigation into the quantity of secretions removed by inflated and deflated laryngeal mask airways. The Flex-Tip tracheal tube does not reduce the incidence of postoperative sore throat: a randomized controlled trial. Lingual nerve injury associated with the ProSeal laryngeal mask airway: a case report and review of the literature. Use of the laryngeal tube-S for airway management and prevention of aspiration after a failed tracheal intubation in a parturient. Randomized controlled trial comparing the laryngeal tube and the laryngeal mask in pediatric patients.
Diseases
- Sensorineural hearing loss
- Aplastic crisis
- Acropectorenal field defect
- Discoid lupus erythematosus
- Telfer Sugar Jaeger syndrome
- L?ri Weill dyschondrosteosis
- Multiple hereditary exostoses
- Frontotemporal dementia
- Chanarin Dorfman syndrome ichthyosis
Order genuine strattera line
For patients at high risk medications 2 times a day order strattera 25mg without prescription, both exercise tolerance and the extent of the surgery are taken into account to determine the need for further testing. Most importantly, no preoperative cardiovascular testing should be performed if the results will not change perioperative management. A positive exercise stress test alerts the anesthesiologist that the patient is at risk for ischemia associated with increased heart rate, with the greatest risk in those who develop ischemia after only mild exercise. Noninvasive pharmacologic stress testing before surgery can be used in high-risk patients who either are unable to exercise or have contraindications to exercise. It is generally accepted that those at greatest risk demonstrate regional wall motion abnormalities at low heart rates. Dipyridamole, adenosine, or regadenoson is administered as a coronary vasodilator to assess flow heterogeneity and the presence of a redistribution defect. One study demonstrated that the presence of silent ischemia is a strong predictor of outcome, whereas its absence is associated with a favorable outcome in 99% of the patients studied. The most important determinant with respect to the choice of preoperative testing is the testing expertise of the local institution. Current recommendations are that patients with active cardiac conditions such as unstable angina, congestive heart failure, significant dysrhythmias, and severe valvular disease should undergo noninvasive stress testing before noncardiac surgery. For patients who require vascular surgery and have multiple clinical risk factors and poor functional capacity, it is reasonable to undergo noninvasive stress testing if it will change management. Echocardiography is less invasive and able to assess regional wall motion abnormalities, wall thickness, valvular function, and valve area. Stroke volume can then be calculated by determining the cross-sectional area of the ventricle. Conflicting results exist with regard 1500 to the predictive value of the ejection fraction using either echocardiographic or radionuclide measurements. It is reasonable for those with dyspnea of unknown origin and for those with current or prior heart failure with worsening dyspnea or other change in clinical status to have preoperative evaluations of left ventricular function. Echocardiography has the added advantage of assessing valvular function, which may have important implications for either cardiac or noncardiac surgery. Aortic stenosis has been associated with a poor prognosis in noncardiac surgical patients, and knowledge of valvular lesions may modify perioperative hemodynamic goals and therapy. Hemodynamic indices can be determined, such as atrial and ventricular pressures, as well as pressure gradients across valves. Although a critical coronary stenosis delineates an area of risk for developing myocardial ischemia, the functional response of that ischemia cannot be assessed by angiography alone. In the ambulatory population, many infarctions are the result of acute thrombosis of a noncritical stenosis. Perioperative Coronary Interventions Guidelines to reduce the perioperative risk of noncardiac surgery have recently been reviewed. The value of percutaneous transluminal coronary angioplasty is less well established, and current evidence does not support its use beyond established indications for nonoperative patients. A significant incidence of perioperative death and hemorrhage in patients after stent placement has been reported. Dual antiplatelet therapy, for example, aspirin and clopidogrel, is often used after stent placement. The decision must involve the anesthesiologist, surgeon, cardiologist, and intensivist. For those patients who have a high risk for stent thrombosis, many advocate that at least aspirin be continued in the perioperative period. Also, the anesthesiologist must weigh the risk of regional versus general anesthesia when these patients are taking antiplatelet therapy. Surgery in patients with recent stent placement should probably only be considered in centers where interventional cardiologists are continuously available. The function of these devices can be impaired by electromagnetic interference during surgery. It is important to understand the type of device, its programming, and its underlying clinical need. Perioperative pulmonary complications include atelectasis, pneumonia, exacerbation of chronic obstructive pulmonary disease, pulmonary edema, and respiratory failure requiring mechanical ventilation. Epidemiologic analyses of large clinical databases have substantially increased the understanding of clinical risk factors. Although a preoperative chest radiograph can identify structural lung abnormalities, these are not frequently associated with significant changes in clinical management for the general population. However, cranial procedures also carry an increased risk, as do vascular and neck surgeries. Diaphragmatic dysfunction occurs despite adequate analgesia and is theorized to be caused by phrenic nerve dysfunction. The need for emergency surgery and the need for general anesthesia are also associated with increased risk. Not only can the surgery affect pulmonary function, but general anesthesia also results in mechanical changes, such as a decrease in the functional residual capacity and reduced diaphragmatic function, leading to ventilation/perfusion abnormalities and atelectasis. Subanesthetic levels of intravenous or volatile agents have the ability to blunt the ventilatory response to hypoxemia and hypercarbia as well. Duration of anesthesia is a well-established risk factor for postoperative pulmonary complications, with morbidity rates increasing after 2 to 3 hours. A point value of 3, 3, 2, 2, and 1 were assigned to these predictors, respectively. It is also important to work with the surgeon to plan specific risk reduction strategies, such as epidural analgesia when appropriate, lung expansion methods, and deep venous thrombosis prophylaxis. Intraoperative measures to limit the risk of hospital-acquired pneumonia have been proposed, largely focused on reducing the risk of bacterial contamination of the lung during the perioperative period. For highrisk patient groups, studies support preoperative oral antiseptic decontamination before tracheal intubation as well as the role of specialized endotracheal tubes to decrease the risk of nosocomial pneumonia. Even among smokers who have not developed chronic lung disease, smoking is known to increase carboxyhemoglobin levels, decrease ciliary function, and increase sputum production, as well as cause stimulation of the cardiovascular system secondary to nicotine. Although cessation of smoking for 2 days can decrease carboxyhemoglobin levels, abolish the nicotine effects, and improve mucous clearance, prospective studies showed that smoking cessation for at least 4 to 8 weeks was necessary to reduce the rate of postoperative pulmonary complications. Asthma Asthma is one of the most common coexisting diseases that confront the anesthesiologist. During the patient interview, it is important to elicit information regarding inciting factors, severity, reversibility, and current status. Frequent use of bronchodilators, hospitalizations for asthma, and requirement for systemic steroids are all indicators of more severe disease. After an acute exacerbation of asthma, airway hyperreactivity may persist for several weeks. The possibility of 1506 adrenal insufficiency is also a concern in those patients who have received more than a "burst and taper" of steroids in the previous 6 months. This group of patients should be considered for "stress doses" of steroids perioperatively. Significantly, they found no association with impaired wound healing or infections. For patients using inhaled steroids, they should be administered regularly, starting at least 48 hours prior to surgery for optimal effectiveness. This episodic desaturation, in turn, causes episodic arousal, leading to chronic sleep deprivation with daytime hypersomnolence and even behavioral changes in children. Depending on the frequency and severity of events, it may lead to other changes, such as chronic pulmonary hypertension and right heart failure. The incidence is expected to rise significantly for Americans born after 2000, largely because of the rise in obesity. The majority of diabetics develop secondary disease in one or more organ systems, which must be identified preoperatively so that an appropriate plan can be developed for perioperative management. Peripheral neuropathies and vascular disease make these patients more susceptible to positioning injuries both during and after surgery.

Generic strattera 40 mg fast delivery
Although reports may speculate that needle design is a determinant of nerve or other tissue injury medications 5 rs cheap strattera 18 mg with visa, there is insufficient evidence to fully substantiate this claim. Continuous blocks require larger-bore needles to facilitate catheter introduction. Desired needle length will depend on each specific block and individual patient characteristics. One must keep in mind that longer needles are more prone to bending upon insertion and may therefore benefit from the strength offered by a larger gauge. Recently, catheters have been developed that are amenable to stimulation (an electrode is placed into the catheter tip), thereby enabling more accurate advancement of catheters over substantial distances to provide continuous analgesia. Some studies have suggested that it may be helpful to inject a solution to dilate the perineural compartment to facilitate advancement of the catheter. The recent reintroduction of catheter-over-needle assemblies allows for the needle and catheter to be inserted as a single unit, avoiding the potential problems associated with threading the catheter through the needle. In theory, a catheter introduced over the needle is more stable in the skin and can be targeted to the desired location with good accuracy. There are a number of continuous-infusion devices now available for both inpatient and outpatient use, which allow delivery of dilute local anesthetic concentrations for as long as 72 hours after surgery. Standard precautions are required to maintain sterility of the catheter and the insertion site, but complications have been rare with these techniques and new devices. Traditional block monitoring tools, which rely on application of cold stimuli (ice, alcohol swab) or touch (pinprick, pinch, monofilament), are generally subjective. More objective tools, such as infrared thermal imaging of the block area45,46 and current perception threshold measurement47 have also been studied. The latter has been shown to be a reliable method of monitoring block progression in a clinical setting. The most popular of these are variations on the 0 to 10 scale, with 0 indicating "no pain" and 10 indicating "worst pain imaginable. Assessment of motor blockade is commonly performed by collecting a Bromage score49 or equivalent score based on a graded scale where the lowest score indicates full range of movement and the highest score indicates complete blockade/no movement. The patient exerts force against a transducer to test the body part that has been blocked. Discharge Criteria Stable vital signs are a must in order to fulfill criteria for discharge from the recovery area. In some cases, acceptable evidence of regressing sensory and motor blocks should be present. However, if a long-lasting local anesthetic was used to perform the block or a continuous catheter with an infusion of local anesthetic is used, the block may not show evidence of regression at the time of discharge. Postoperative follow-up is important to confirm that neurologic function has returned to normal. If a deficit is suspected, early 2361 neurologic assessment is critical to determine the appropriate course of management. Specific common risks for certain blocks should be discussed with the patient prior to discharge. When discharging patients from postanesthesia care units while an extremity is still anesthetized. A clear understanding of the information provided is important for both the patient and their caregivers. Written instructions including expected course, common side effects, and 24-hour contact information should be provided. Avoiding Complications In general, regional anesthesia has an excellent safety record. Choosing a suitable patient and applying the right dose of local anesthetic in the correct location are the primary considerations. Careful attention to any unusual responses or reports of pain during block performance, as well as follow-up prior to and after discharge, is equally important, although often overlooked. In general, patients scheduled for extremity, thoracic, abdominal, or perineal surgery should be considered potential candidates for peripheral regional anesthetic techniques. Adamant refusal of regional anesthesia by a patient or, in the case of children, a parent/guardian, is an absolute contraindication to the procedure. Other contraindications include local infection, systemic anticoagulation, and severe systemic coagulopathy. In most cases, schizophrenic patients should only receive regional techniques if general anesthesia is also performed. One must be cognizant of the potential to compound existing neurologic deficits; therefore, clear documentation of the deficits prior to the procedure and a careful discussion of the potential risks and benefits are critical. For every clinical situation, the use of regional anesthesia must be evaluated carefully as a matter of risk versus benefit. For a more detailed discussion of the pharmacology and toxicity of local anesthetics, the reader is referred to Chapter 21. To limit total drug dose, lower concentrations are usually indicated when larger volumes are required to anesthetize poorly localized peripheral nerves or to block a series of nerves. The degree of systemic drug absorption and duration of anesthesia can also vary depending on the site of injection. The highest blood levels of local anesthetic occur after intercostal blocks, followed by caudal, epidural, brachial plexus, intravenous regional, and lower extremity blocks. Equivalent doses of local anesthetic may produce only 3 to 4 hours of anesthesia when placed in the epidural space but 12 to 14 hours in the arm and 24 to 36 hours when injected along the sciatic nerve. Many believe that the addition of epinephrine (1:200,000 to 1:400,000) is advantageous in prolonging the duration of block and in reducing systemic blood levels of local anesthetic, although this has more relevance to local anesthetics like lidocaine and less to ones like bupivacaine. Its use is not appropriate in the vicinity of "terminal" blood vessels, such as in the digits, penis, or ear or when using an intravenous regional technique. However, even small doses of local anesthetic may produce significant side effects when injected into susceptible regions such as the neck. Toxicity can also occur from peripheral absorption of excessive doses of local anesthetic. Patients should be observed carefully for at least 30 minutes following injection since peak blood levels may occur at this time. Animal studies62 and case reports63,64 have shown successful resuscitation from local anesthetic toxicity by intravenous administration of Intralipid 20% (not the 10% lipid of propofol), using one or more boluses (each of 1 to 2 mL/kg or 100 mL) followed by a 30-minute infusion (0. It is important to use this strategy as an acute resuscitation agent only after standard measures have proven ineffective. Nerve Damage and Other Complications Peripheral nerve injury in humans may result from intraneural injection65,66 or direct needle trauma,67 although there are other causes, including those related to the surgical procedures. A hematoma around a peripheral nerve is not of the same significance or risk as that occurring in the epidural or subarachnoid space. It is important to address concerns expressed by patients and to make every effort to relieve any pain or discomfort resulting from various interventions. Clinical Anatomy Anatomical descriptions of major nerve structures, including plexuses and terminal/peripheral nerves are discussed in this section. The section is divided on the basis of regions of the body: head and neck, spine, upper extremity, trunk, and lower extremity. Head and Neck Trigeminal Nerve Sensory and motor innervation of the face is provided by the branches of the fifth cranial (trigeminal) nerve. The roots of this nerve arise from the base of the pons and send sensory branches to the large semilunar (trigeminal or Gasserian) ganglion, which lies on the dorsal surface of the petrous bone. Its anterior margin gives rise to three main branches: the ophthalmic, maxillary, and mandibular nerves. A smaller motor fiber nucleus lies behind the main trigeminal ganglion and sends motor branches to the terminal mandibular nerve. The main terminal fibers of this sensory nerve, the frontal nerve, run to behind the center of the orbital cavity and bifurcate into the supratrochlear and supraorbital nerves. The supratrochlear branch traverses the orbit along the superior border and exits on the front of the face in the easily palpated supraorbital notch; the supraorbital nerve runs in a medial direction toward the trochlea. At the anterior end of this channel, it again moves superiorly to re-enter the skull in the infraorbital canal in the floor of the orbit.
Cheap strattera 10 mg without a prescription
One-lung Ventilation Absolute Indications for One-lung Ventilation Currently treatment yeast purchase strattera 10mg otc, a variety of thoracic surgical procedures such as lobectomy, pneumonectomy, esophagogastrectomy, pleural decortication, bullectomy, and bronchopulmonary lavage are commonly performed. Customarily, the indications are classified either as absolute or as relative (Table 38-1). The absolute indications include life-threatening complications, such as massive bleeding, sepsis, and pus, in which the nondiseased contralateral lung must be protected from contamination. A giant unilateral bulla may rupture under positive pressure, and ventilatory exclusion is mandatory. Finally, during bronchopulmonary lavage for alveolar proteinosis or cystic fibrosis, prevention of drowning the contralateral lung is necessary. Improvements in video-endoscopic surgical equipment and a growing enthusiasm for minimally invasive surgical approaches have contributed to its use. The lung should be well collapsed to provide the surgeon with an optimal view of the surgical field, and to facilitate palpation of the lesion in the lung parenchyma. In addition, it is difficult to place the stapler on a lung that is not completely collapsed, and there is an increase in incidence of postoperative air leak in these circumstances. In some institutions, 80% to 90% of the procedures are now performed using the thoracoscopic approach. The 35% of total flow perfusing the nondependent lung, which was not shunt flow, was assumed to be able to reduce its blood flow by 50% by hypoxic pulmonary vasoconstriction. Upper lobectomy, pneumonectomy, and thoracic aortic aneurysm repair are high-priority indications. These procedures are technically difficult, and optimal surgical exposure and a quiet operative field are highly desirable. Nevertheless, many surgeons are accustomed to operating with the lung collapsed for these cases. These procedures include minimally invasive cardiac surgery, lung volume reduction, thoracic aneurysm repair, thoracic spinal procedures, mediastinal mass resection, thymectomies, and mediastinal lymph node dissection. It is important to distinguish between the need for lung isolation versus lung separation. Whenever the nondiseased lung is threatened with contamination by blood or pus from the diseased lung, the lungs must be isolated to prevent potentially life-threatening complications. Finally, during bronchopulmonary lavage for alveolar proteinosis or cystic fibrosis, protection of the contralateral lung from drowning is necessary. These situations, however, are relatively uncommon and in modern anesthesia practice constitute less than 10% of all thoracic procedures. This includes all the relative indications that are primarily for surgical exposure. One lumen is long enough to reach a main stem bronchus, and the second lumen ends with an opening in the distal trachea. Lung separation is achieved by inflation of two cuffs: A proximal tracheal cuff and a distal bronchial cuff located in the main stem bronchus (see "Positioning Double-lumen Tubes"). The endobronchial cuff of a right-sided tube is slotted or otherwise designed to allow ventilation of the right upper 2582 lobe because the right main stem bronchus is too short to accommodate both the right lumen tip and a right bronchial cuff. This tube design has the advantages of having D-shaped, large-diameter lumens that allow easy passage of a suction catheter, offer low resistance to gas flow, and have a fixed curvature to facilitate proper positioning and reduce the possibility of kinking. The original red rubber Robertshaw tubes were available in three sizes: small, medium, and large. These are available in both right-sided and left-sided versions and in 35 French (Fr), 37 Fr, 39 Fr, and 41 Fr sizes. The advantages of the disposable tubes include the relative ease of insertion and proper positioning as well as easy recognition of the blue color of the endobronchial cuff when fiberoptic bronchoscopy is used. Other advantages are the confirmation of the position on a chest radiograph using the radiopaque lines in the wall of the tube and the continuous observation of tidal gas exchange and respiratory moisture through the clear plastic. The right-sided endobronchial tube is designed to minimize occlusion of the opening of the right upper lobe bronchus. The right endobronchial cuff is doughnut-shaped and allows the right upper lobe ventilation slot to ride over the opening of the right upper lobe bronchus. This tube has a D-shaped wire-reinforced lumen to maintain the tip at a 45-degree angle. The reinforced wall tends to prevent obstruction or kinking of the bronchial lumen, yet at the same time maintains flexibility. This clinical scenario can be seen in patients who have previously undergone a left upper lobectomy and the expansion of the left lower lobe displaces the left main bronchus upward. It is possible to measure the diameter of the left bronchus from the chest radiograph in almost 75% of patients. In patients in whom the left main bronchus cannot be directly measured, the left bronchial diameter can be accurately estimated by measuring tracheal width. The common practice of fiberoptic bronchoscopy has decreased the risk of undetected distal placement or migration of the bronchial tip. The tracheal cuff (high volume, low pressure) can accommodate up to 20 mL of air, and the bronchial cuff can be checked using a 3-mL syringe. A Macintosh laryngoscope blade is preferred for intubation of the trachea because it provides the largest area through which to pass the tube. The insertion of the tube is performed with the distal concave curvature facing anteriorly. After the tip of the tube is past the vocal cords, the stylet is removed and the tube is rotated through 90 degrees. A left-sided tube is rotated 90 degrees to the left, and a right-sided tube is rotated to the right. Advancement of the tube ceases when moderate resistance to further passage is encountered, indicating that the tube tip has been firmly seated in the main stem bronchus. It is important to remove the stylet before rotating and advancing the tube to avoid tracheal or bronchial laceration. Rotation and advancement of the tube should be performed gently and under continuous direct laryngoscopy to prevent hypopharyngeal structures from interfering with proper positioning. Once the tube is believed to be in the proper position, a sequence of steps should be performed to check its location. First the tracheal cuff should be inflated, and equal ventilation of both lungs established. If breath sounds are not equal, the tube is probably too far down, and the tracheal lumen opening is in a main stem bronchus or is lying at the carina. The second step is to clamp the right side (in the case of the left-sided tube) and remove the right cap from the connector. Then the bronchial cuff is slowly inflated to prevent an air leak from the bronchial lumen around the bronchial cuff into the tracheal lumen. This ensures that excessive pressure is not applied to the bronchus and helps avoid laceration. The third step is to remove the clamp and check that both lungs are ventilated with both cuffs inflated. This ensures that the bronchial cuff is not obstructing the contralateral hemithorax, either totally or partially. The final step is to clamp each side selectively and watch for absence of movement and breath sounds on the ipsilateral (clamped) side; the ventilated side should have clear breath sounds, chest movement that feels compliant, respiratory gas moisture with each tidal ventilation, and no gas leak. If the tracheal lumen is connected to an underwater seal system, gas will be seen to bubble up through the water. The bronchial cuff can then be gradually inflated until no gas bubbles are seen and the desired cuff seal pressure can be attained. This test is of extreme importance when absolute lung separation is needed, such as during bronchopulmonary lavage. The upper surface of the blue endobronchial cuff should be just below the tracheal carina. The bronchoscope should then be passed through the bronchial lumen, and the left upper lobe bronchial orifice should be identified. Excellent fiberoptic images of the tracheobronchial tree can be seen by accessing the website thoracicanesthesia. It is therefore essential to recognize and correct such a malposition as soon as possible. In this case, breath sounds are very diminished or not audible over the contralateral side.
Purchase strattera on line amex
Burst suppression or isoelectric encephalogram for cerebral protection: Evidence from metabolic suppression studies symptoms ear infection buy 18mg strattera with visa. Relationship between bispectral index values and volatile anesthetic concentrations during the maintenance phase of anesthesia in the B-unaware trial. Comparative effects of ketamine on Bispectral Index and spectral entropy of the electroencephalogram under sevoflurane anaesthesia. Ketamine has no effect on bispectral index during stable propofol-remifentanil anaesthesia. Effect of remifentanil on plasma propofol concentration and bispectral index during propofol anaesthesia. Bispectral index monitoring in the intensive care unit provides more signal than noise. Overestimation of Bispectral Index in sedated intensive care unit patients revealed by administration of muscle relaxant. Irritant contact dermatitis after use of Bispectral Index sensor in prone position. The incidence of intraoperative awareness in children: Childhood awareness and recall evaluation. The differences in the bispectral index between infants and children during emergence from anesthesia after circumcision surgery. Quantitation of beat-to-beat changes in stroke volume from the aortic pulse contour in man. Diastolic flow reversal in the descending thoracic aorta is significant for severe aortic insufficiency. A remarkably versatile tool, real-time echocardiography provides a comprehensive evaluation of myocardial, valvular, and hemodynamic performances. These capabilities attracted the attention of anesthesiologists and surgeons challenged by the unique difficulties of perioperative cardiovascular management. Over the 30 years following the first report of intraoperative echocardiography to assess ventricular function by Barash and colleagues in 1978, echocardiography has emerged as the technique of choice for a wide variety of intraoperative case challenges. The American Society of Anesthesiologists in conjunction with the National Board of Echocardiography has established a second certification pathway in basic perioperative echocardiography, These efforts are unique in intraoperative monitoring and attest to the critical role that accurate and thorough echocardiographic interpretation plays in current anesthetic practice. Principles and Technology of Echocardiography Echocardiography generates dynamic images of the heart from the reflections of sound waves. The ultrasound transducer records the time delay and signal intensity for each returning reflection. Since the speed of sound in tissue is constant, the time delay allows the echo system to precisely calculate the location of cardiac structures and thereby create an image map of the heart. The resulting tissue vibrations create a longitudinal wave with alternating areas of compression and rarefaction. Vibrations of the ultrasound transducer create cycles of compression and rarefaction in the adjacent tissue. The ultrasound energy is characterized by its amplitude, wavelength, frequency, and propagation velocity. The amplitude of a sound wave represents its peak pressure and is appreciated as loudness. The intensity of the sound signal is proportional to the square of the amplitude and is an important factor regarding the potential for tissue damage with ultrasound. Since levels of sound pressure vary over a large range, it is convenient to use the logarithmic decibel (dB) scale: where A is the measured sound amplitude and Ar is a standard reference sound level; I is the intensity and Ir is a standard reference intensity. The Food and Drug Administration limits the intensity output of cardiac ultrasound systems to be below 720 W/cm2 because of concerns of potential tissue injury. The propagation velocity of sound (v) is determined solely by the medium through which it passes. High-frequency, shortwavelength ultrasound is more easily focused and directed to a specific target location. Properties of Sound Transmission in Tissue the propagation of a sound wave through the body is markedly affected by its interactions with the various tissues encountered. These interactions result in reflection, refraction, scattering, and attenuation of the ultrasound signal and determine the resulting appearance of the two-dimensional image. Echocardiographic imaging relies on the transmission and subsequent reflection of ultrasound energy back to the transducer. A sound wave propagates smoothly through uniform tissue until it encounters the interface between two tissues varying in acoustic impedance (a property largely related to the density [] of the tissue and the speed that ultrasound travels). A large interface oriented perpendicular to the sound beam will produce a mirror-like reflection of sound back toward the transducer with only a portion of the signal passing through the interface. Refraction causes a change in direction of propagating sound and occurs when an interface lies oblique to the sound beam. Refraction is an important factor in the formation of artifacts as the transducer mistakenly interprets a reflection from the refracted beam as originating from a cardiac structure located within the intended scanning field. Scattering reflections occur when an ultrasound beam encounters small or irregularly shaped surfaces, such as red blood cells. These reflectors scatter ultrasound energy in all directions so that far less energy is reflected back to the transducer. This type of reflection is the basis of the Doppler analysis of blood flow (see following). Attenuation results in less energy returning to the transducer and 1827 low-quality images with poor signal-to-noise ratios. To combat attenuation, echocardiographers select better penetrating low-frequency signals. Adjusting the gain controls to amplify the weak returning signals makes their appearance brighter on the display. Unfortunately, this increases the brightness of artifactual noise, which negatively impacts the image appearance. Instrumentation Transducers Ultrasound transducers use piezoelectric crystals to create a brief pulse of ultrasound. Conversely, when a sound reflection strikes the crystal, the impact vibrates the polarized particles and generates an electric current. This property allows the piezoelectric crystal to function as both a transmitter and a receiver of ultrasound. The shorter the length of the sound pulses, the better the axial resolution of the system. High-resolution imaging transducers emit sound pulses of just two to four cycles of short-wavelength, high-frequency sound. Beam Shape the ultrasound transducer emits a three-dimensional ultrasound beam similar to a movie projection. Focusing of the beam is used to improve spatial resolution by narrowing the ultrasound beam at the desired depth. The dense, narrow beam is preferred because it provides improved spatial resolution, produces high-intensity reflections, and reduces artifact. Short pulses of high-frequency ultrasound offer the greatest axial resolution but have a decreased tissue penetration. Accordingly, echocardiographers select transmitted frequency based on the particular imaging need. Broad beams produce a "smeared" image of two nearby objects, whereas narrow beams can identify each object individually. Beam size is reduced by selecting high-signal frequencies and minimizing imaging depth. Signal Processing To convert echoes into images, the returning ultrasound pulses are received, electronically processed, and displayed. The oscillator repeatedly cycles the transducer from a brief transmission to a relatively long receive mode. During the receive phase, the reflected echocardiography signals are captured and converted to electrical signals by the piezoelectric crystal. The echocardiography system employs a series of controls, including system gain, time gain compensation, compression, and postprocessing settings (not unlike those available with digital imaging software) to optimize the signal for display.